Course
Respiratory Failure in Chronic COPD
Course Highlights
- In this Respiratory Failure in Chronic COPD course, we will learn about Chronic Obstructive Pulmonary Disease.
- You’ll also learn risk factors, prevalence, and incidence of COPD.
- You’ll leave this course with a broader understanding of the treatment for respiratory failure in COPD.
About
Contact Hours Awarded: 1
Course By:
Tracey Long PhD, APRN-BC, CCRN, CDCES, CNE, COI
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Case Scenario:
BW is a 62-year-old white male seen in the Primary Physician’s office for shortness of breath on exertion, fatigue, and dizziness for the past month. He has been smoking 2 packs per day for 20 years. He works in an auto assembly plant in Kentucky and has hypertension. His vital signs are 148/90, pulse 88, respirations 22, tympanic temperature 98.8, and Sp02 93. He has been on Lisinopril 10 mg tab once daily.
Upon inspection, he is short of breath just walking into the clinic and smells of cigarette smoke. Upon physical exam, his heart sounds are audible without murmurs or dependent edema in his legs. He does have congested and tight lung sounds bilaterally with expiratory crackles. He admits to smoking 2 packs of cigarettes daily. With his smoking history and current clinical symptoms, what is the suspected diagnosis?
As a health care professional, what would you do first? Is this a medical emergency? What diagnostic tests should be completed? What is the probable diagnosis? What were the patient’s risk factors? How common is this? The scenario is unfortunately all too common for people with chronic obstructive pulmonary disease.
Definitions
Chronic Obstructive Pulmonary Disease (COPD) is a chronic and irreversible respiratory disease characterized by airway obstruction or restriction. It is the fourth leading cause of death (1,3). Correct diagnosis and management are important for quality of life and prevention of early death for approximately 16 million patients with COPD in the U.S. and over 65 million worldwide (2, 24).
According to the Centers for Disease Control, more than 143,000 adults die annually from COPD in the U.S. (3). COPD is not contagious or curable, but rather a group of progressive lung diseases characterized by obstructed airflow.
Types of COPD
COPD is characterized by inflammation of the airways and severe air flow restriction both in and out of the lungs. COPD is an umbrella term that includes chronic bronchitis, emphysema, asthma, and COPD. Some people may have combinations of COPD and emphysema or COPD and chronic bronchitis.
It is generally caused by long-term exposure to environmental irritants such as smoke, second-hand smoke, air pollution, fumes, and wood smoke. Although the overall term for each of these diseases is COPD, clinicians refer to COPD as a specific disease process, most seen among long-term cigarette smokers with chronic airway obstruction from inflammation. COPD can also be further described as obstructive or restrictive.
A key characteristic of any type of COPD is limited airflow, which results in hypoxia and carbon dioxide retention. The patient doesn’t have the full ability to exhale as alveoli loses elasticity resulting in poor exchange of oxygen and carbon dioxide. Because of the trapped air, the alveoli often develop air pockets, and the chest becomes expanded with the retention of carbon dioxide (4).
Emphysema is a type of COPD that shares the common clinical symptoms of shortness of breath and airway obstruction. Commonly seen in people with a long-term history of smoking, it is noted uniquely in the clinical presentation as a “pink puffer.” The term comes from the clinical appearance of patients with emphysema who have a pink flushed appearance from the lack of oxygen, poor cardiac output and increased work of breathing. The damage is deep within the lungs from overinflated alveoli where air has become trapped from the inability to exhale out the carbon dioxide.
Chronic smoking damages the flexibility of the alveoli making them stiff and ineffective. Instead of many small air sacs, they become stretched and floppy and less effective in moving oxygen into and out of the capillaries. Often because the work of breathing takes all their energy, they prefer to breathe rather than eat, so they experience weight loss and muscle wasting due to the lack of oxygen. Emphysema has also been called COPD Type A (5).
The prevalence of emphysema indicates that 90% of cases are seen in people over the age of 45 (6). Rates of diagnosis have also been increasing among women showing the similar trends of COPD now equalizing among women and men.
Chronic bronchitis is a type of COPD characterized by inflammation, airway irritation, and mucus buildup in the main bronchus. The clinical diagnosis is defined as a persistent cough that produces phlegm and mucus, for at least three months per year in two consecutive years (6). Symptoms include chronic cough trying to rid the airway of thick mucus and phlegm. There are two types of bronchitis acute and chronic. Acute bronchitis is generally caused by colds and flu. The temporary infection causes inflammation with irritation to the bronchus and bronchioles and results in coughing and shortness of breath.
Women have chronic bronchitis at twice the rate of men (3,7). Age increases the risk factor as people over age 65 have a rate of 64.2 per 1,000 persons compared to the age group of 18-44 the rate drops to 28 per 1,000 (6). Prevalence trends also reveal that non-Hispanic whites have a higher risk than African American blacks and Hispanics.
Chronic bronchitis is also characterized by cough; however, it does not go away with antibiotics or treatment as it is caused by smoking or other environmental pollutants such as dust, air pollution, or unsafe work environments of coal, asbestos, or irritants to delicate respiratory tissues. Although acute bronchitis can be “cured” with pharmacological interventions and time for healing, there is no cure for chronic bronchitis. Treatment is focused on relief from annoying cough symptoms and supporting the airway. Bronchodilators are the mainstay of therapy.
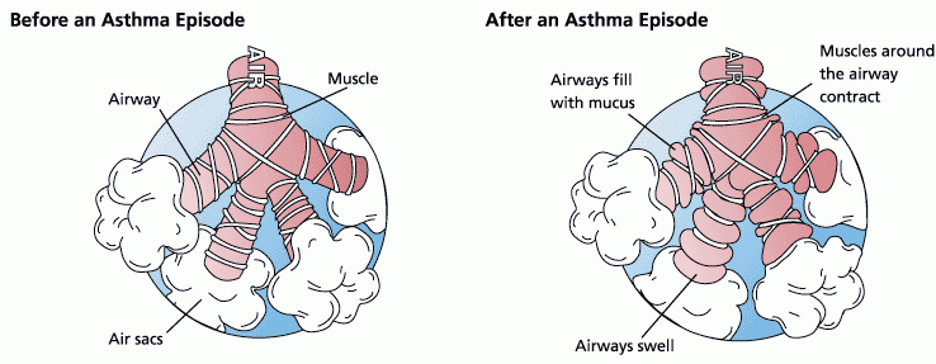
Asthma and COPD may result in the same airflow resistance. Still, as the cause of COPD is generally from smoking, asthma is from other respiratory irritants such as air pollution or environmental triggers like dust, mold, pet dander, and more. Asthma is a form of COPD characterized by spasms of the bronchi in the lungs and is an overreaction and spasm of the bronchial airways (8). Normally the bronchiole tubes can dilate and constrict depending on nervous system messages, however, in asthma the bronchus and bronchiole tubes constrict and overreact to environmental and even emotional triggers causing severe difficulty breathing and airflow.
Asthma is characterized by wheezing from restricted airflow, chest tightness, and increased mucus from the inflamed airways, which worsens the restriction and impedes airflow. Unlike emphysema, which is seen in older patients who have had years of smoking history, asthma is seen in people of all ages and often first manifests during childhood.
When asthma develops in younger children, it may often resolve independently as the child’s respiratory system grows and matures. Other children may continue to suffer from asthma for the rest of their lives and require maintenance medications to keep the airways open. There has been a correlation between asthma and eczema indicating an autoimmune response. Combinations of eczema (atopic dermatitis) and allergic rhinitis indicate a risk of developing other allergies and asthma as immunoglobulins (antibodies) respond to the allergen (8).
A natural body defense against high levels of immunoglobulins is closing the airways to prevent the invading pathogen from further entering the body. In the case of asthma, this natural defense mechanism becomes the problem as airways spasm and even threaten to close.
For many children with asthma, there is a genetic link to a deficiency of a protein in the skin, which normally helps strengthen the skin from pathogens and allergens. Without the protein, the skin is more irritated by environmental allergens and microbes and the body responds quickly with hives, eczema, and the resulting antibodies (8).
Asthma affects 25 million in the United States and is the most common chronic disease of childhood. As high as 95% of patients with asthma also suffer from chronic rhinitis (9).
Case Scenario:
In our earlier scenario, the diagnosis of COPD was determined.
- What symptoms did the patient present with and what were his risk factors?
- What were the triggers that caused COPD?
- What type of COPD does he have?

Self Quiz
Ask yourself...
- What conditions are included in the umbrella term chronic obstructive pulmonary disease (COPD)?
- Compare and contrast COPD with asthma and emphysema.
- How would you explain to a patient what COPD is?
Statistics About COPD
Chronic obstructive pulmonary disease is the third leading cause of death in the United States and is largely irreversible and fatal (3). It is projected that with the increasing prevalence of smoking in developing countries and the aging populations, the prevalence of COPD is expected to rise over the next 30 years. Prevalence indicates how many people currently have the disease and approximately 1 of every 13 Americans aged 18 years and older has COPD.
Data is collected annually from two major surveys including the National Health Interview Survey (NHIS) and the Behavioral Risk Factor Surveillance System (BRFSS). It is the third leading cause of death for people of most racial and ethnic groups in the United States (10). In the United States, COPD is most common among Caucasians and those with a history of smoking. COPD develops over time and is an obstructive or restrictive expiratory airway due to chronic bronchitis, emphysema, or asthma (9).
Approximately 26 million Americans have been diagnosed with COPD and many more yet undiagnosed. It is the third leading cause of death next to cardiovascular disease and cancer. It is seen more in men and women older than 40 years of age, often due to years of chronic smoking.
It is more common in men than women, but rates of COPD among women increase as women smoke. It is estimated from previous studies that 8% of the U.S. population adults have been told by a health-care provider that they have COPD (11, 12, 2).
The incidence and prevalence vary by state and worldwide statistics are unknown as more than 50% of people formally diagnosed with low pulmonary function were not even aware of the diagnosis (13, 14). According to the World Health Organization, approximately 65 million have some form of COPD, however much of the data on morbidity and mortality from COPD comes from first-world countries and is estimated to be approximately 5% of all deaths worldwide (5). In states with higher rates of smokers, there is a direct correlation to a higher incidence of COPD.
Morbidity and Mortality
Morbidity is the term for the cost and consequences of a disease. Illness from COPD has a large impact on the American health system. According to the CDC estimates, COPD costs our country approximately $50 billion annually in both direct and indirect health care (15).
The rates of COPD also correlate with states that have the highest smoking populations, which include the Southeast and Midwest states, such as Alabama and Kentucky. Because COPD is mostly caused by environmental pollutants, of which smoking is the number one cause, other environmental pollutants found in these states are industrial pollutants from factory workers and represent 31% of those who have never smoked (7). In developing countries or poor homes, such rates may also include cooking with fuel instead of electricity.
Female smokers are 13 times more likely to die from COPD than other female non-smokers and male smokers are 12 times more at risk to die from COPD than a counterpart non-smoking male (7). The cost of COPD for people over age 65 also has increased to almost $30 billion in direct healthcare costs and another $20 billion in direct mortality and morbidity costs.
The additional costs include loss of work and ability to function as 51% state their ability to function at work is limited and 70% claim it limits physical ability. Social and family activities are also limited as patients with COPD have difficulty walking, participating in leisure activities they once enjoyed and even performing activities of daily living on their own.
Case Scenario:
Our 62-year-old white male is given the diagnosis of COPD and asks the provider how he developed it, whether is there a cure, and what is his prognosis. The provider tells him that his 20-year history of smoking, which equals 40 pack years (20 years times 2 packs/day 40) is the main cause of his COPD. He has additional risk factors of being a white male and working with industrial pollutants in his job. Unfortunately, there is no cure for him, but he can receive treatment for the symptoms. His prognosis depends on his ability to stop smoking. The reality is that he has increased his morbidity by 12 times by choosing to smoke. The provider then offers him an explanation of the function of his lungs and the treatment options.

Self Quiz
Ask yourself...
- What is the incidence and prevalence of COPD in the US?
- How does COPD compare with worldwide statistics?
- What are the risk factors for COPD?
- What risk factors can contribute to the mortality and morbidity of COPD?
Physiology of Breathing
The internal pressure in the thoracic cavity is negative compared to the positive atmospheric air pressure. When the diaphragm contracts it opens the thoracic cavity allowing air to rush into the bronchioles and fill the alveoli. When the pressure within the lungs exceeds the external pressure by filling with air, the reverse occurs when the diaphragm relaxes, and the air is then pushed out of the bronchioles and lungs to exhale. However, COPD alters this effective function. Because the diaphragm does 80% of breathing, when the alveoli trap air, the diaphragm becomes flattened making complete contraction of the diaphragm ineffective in pulling the thoracic cavity open, which further reduces the airflow coming into the airway.
On the tissue of the bronchiole tubes, the two major receptors for the nervous system are the muscarinic and beta receptors. Muscarinic receptors cause smooth muscle contraction making the lumen of the bronchiole tube smaller. In contrast, the beta receptors will cause relaxation of the muscle causing bronchodilation.
Ideally, the goal for people with COPD is to increase beta receptor activity (dilation of airways) and inhibit muscarinic receptors. The two main classes of medications will act on either of the receptors to open the airways. Because people with COPD also have inflammation of the airways, the third major mechanism to change this vicious cycle of airway over-reactivity is with an anti-inflammatory, such as inhaled corticosteroids (4, 16).
COPD is caused by bronchoconstriction and inflammation making air passage in and out of the lungs more difficult. This reduction in effective airflow creates a state of hypoxia, resulting in hypoxemia. The obstruction can be caused by mucus or narrowing of the bronchus and bronchiole tree creating airway resistance.
Chronic bronchitis is a chronic productive cough lasting three months during two consecutive years. Emphysema is a permanent enlargement of the alveoli, which prevents normal elastic recoil during respiration. People with asthma develop an obstruction of the airway and airflow. Those with asthma who have a reversible airflow obstruction are not considered to have COPD, however, when the airflow remains chronically obstructed, which is not reversible, they are diagnosed with COPD (4, 16).
The lungs become scarred from chronic inflammation and continual irritation from mucus buildup as the lungs attempt to protect themselves from environmental irritants such as smoke. This cycle of irritation, inflammation, and attempts to recover continues until the compensation efforts create disruptive symptoms that often drive the patient to seek medical care. A productive cough with mucus is an effort of the lungs and trachea to rid itself of the irritant, however, the mucus soon becomes a problem, such as seen in chronic bronchitis, and often known as a “smoker’s cough.”
Effects of Smoking
Smoking, as the number one cause of COPD, destroys the fine hairs, or cilia, in the bronchiole tubes and trachea, which are supposed to push up foreign substances and pathogens from the lower airway up into the upper airway to be expelled by a cough. The additional pathology from smoking affects not only the lungs but also the circulatory system (9,17). Nicotine paralyzes the cilia and the tar within cigarettes or cigars further destroys their integrity.
Additionally, the chemicals in cigarette smoke create nicks within the fine endothelial lining of the arteries throughout the body allowing a “shelf” for cholesterol and fat to build up upon. Generally, the public is aware of cigarette smoking as the most common cause of lung cancer, however, most people are unaware of the damage to the circulatory system, which is also the most common cause of atherosclerosis, or narrowing of the arteries.
In addition, nicotine competes with oxygen further stimulating erythropoiesis, or formation of new red blood cells, which can often lead the blood to become thick and sticky. Atherosclerotic plaques narrow an artery and hinder blood flow. The result is the surface of a bulging atherosclerotic plaque sometimes tears, exposing material that stimulates clot formation. Clots and ruptured plaque material can then break away from the wall, be carried by the blood, and clog arteries downstream.
Atherosclerosis can damage tissues throughout the body:
- Blockages in the carotid arteries can reduce or block blood flow to the brain, causing a stroke.
- Obstructions in the peripheral arteries in the legs can cause claudication (pain when walking) gangrene and deep vein thrombosis (DVT).
- Resultant DVTs can travel to the lungs causing a pulmonary embolism and respiratory arrest.
- Atherosclerotic obstructions in the intestines cause ischemic bowel.
- In the coronary arteries, atherosclerotic obstructions cause heart attacks (17).
At the cellular level, DNA is disrupted by nicotine and tars from smoking, which leads to mutations in cellular replication that are out of control, known as cancer. One-third of all cancer deaths are caused by tobacco and smoking. In addition to disruptions in normal DNA creation of proteins, hormones are disrupted affecting lower estrogen and testosterone levels, thyroid problems, and reproduction issues.
Within the blood system itself, white blood cells and red blood cells stay elevated from smoking. High white blood cells indicate to your body they are in a state of infection, which continues the cycle of inflammation and attempts to repair. As formed elements in the blood (RBCs and WBCs) increase, nutrients, minerals, and precious oxygen decrease by sheer volume and availability to be transported by blood.
The image below illustrates a comparison of clear vs congested alveoli from smoking.
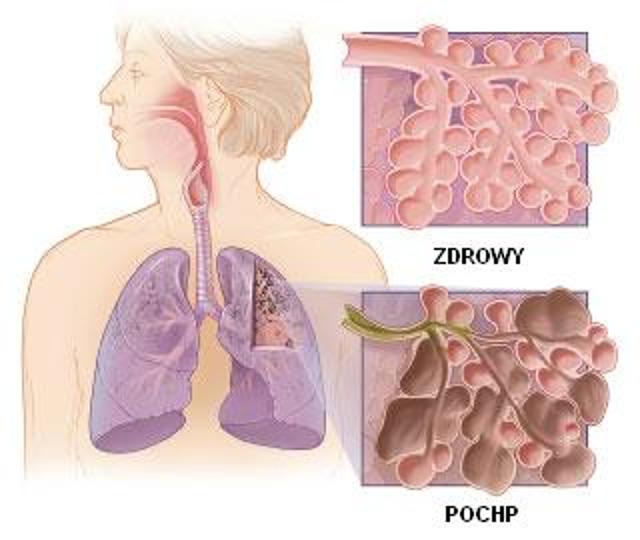
(34)
Case Scenario:
Mr. BW has discovered that the result of 20 years of smoking has compromised his lungs’ ability to inhale and exhale. Unfortunately, his symptoms of shortness of breath and persistent cough were his only indicators. The Provider will order additional diagnostic studies to confirm the diagnosis including spirometry, lab tests to establish a baseline, and a chest x-ray.

Self Quiz
Ask yourself...
- What is the pathology of COPD within the bronchioles?
- What is the pathology of COPD within the alveoli?
- How do the lungs attempt to compensate for congested alveoli?
- What are the results of lab work?
- What resources do you have to teach patients about the effects of smoking on their lungs?
- What other complications for the body does smoking cause?
Risk Factors
A valid and costly concern for Health Maintenance Organizations and insurance companies is that numerous patients are hospitalized for acute exacerbations of their COPD, which could have been avoided by careful management by their primary physician.
A hospitalization from a COPD exacerbation can cost thousands of dollars. The national guidelines and the GOLD standard for COPD diagnosis and management were created from numerous clinical research and studies (18). The GOLD standard for COPD has been accepted as a national standard and adopted by HEDIS measures for insurance reimbursement and Center for Medicare Services (CMS).
By surveying and tracking reports of people with COPD across all states, improvements can be made in identifying communities at risk who may benefit from awareness, outreach and public health efforts in prevention, treatment, and control of the disease. Efforts to survey patients with COPD in all states have been made by the Centers for Disease Control using the Behavioral Risk Factor Surveillance System (BRFSS) (12).
Of those who self-identified as COPD, 76% stated they received a diagnostic breathing test, 64% felt the shortness of breath negatively impacted their quality of life, and 55% were taking at least one medication for their COPD (11). Because the spirometry test can be costly, it is not used as a general screening tool for COPD. Currently, there is no public screening tool in use due to cost.
Predisposing factors include environmental pollutants and also include secondhand smoke, genetic factors of Alpha 1-antitrypsin (AAT) deficiency, recurrent or chronic lower respiratory infections or disease, and age over the fifth decade of life.

Self Quiz
Ask yourself...
- Picture your patients who have COPD, emphysema, chronic bronchitis, and asthma.
- How are they the same? How are they different?
- What similarities in medications did they receive?
- What were the interventions applied for each?
Symptoms of COPD
Most symptoms of COPD are due to difficulty breathing and obstruction or restriction to airflow in and out of the lungs (28). Dizziness, fatigue, shortness of breath and even hypertension are all related to hypoxia, a lack of adequate oxygenation to body tissues. As in any condition, a thorough history must be taken to include symptoms and signs visible to the healthcare professional. It is said as much as 90% of diagnoses made can be determined by a good history.
A history of difficulty breathing or shortness of breath after exercise, and exposure to environmental triggers can help identify the development of asthma. Clinical symptoms include wheezing, recurrent cough (worse at night and early morning), recurrent shortness of breath, and chest tightness with moderate activity.
The classic symptom of COPD is shortness of breath. At first, there may be little to no symptoms with COPD, however, because it is a chronic and progressive disease of deteriorating lung capacity and airflow, the symptoms inevitably develop and worsen. Wheezing, shortness of breath, chest tightness, and cough are classic symptoms that also lead to weight loss, muscle loss, and difficulty with daily activities.
Early Symptoms
- Daily morning cough
- Shortness of breath- especially on exertion
- Wheezing
Moderate Symptoms
- Ongoing productive cough
- Chest tightness
- Fatigue
- Loss of appetite if breathing through the mouth
- Sputum- clear and colorless, may be frothy.
- Change in mental alertness.
- Weakness
Late-Stage Severe Symptoms
- Dizziness
- Pallor
- Cyanosis
- Chronic cough-throughout day (smoker’s cough)
- Waking up feeling suffocated
- Blue lips, skin, and nails
- Inability to lie down.
- Irritability and headaches
- Difficulty sleeping
A pneumonic to help you remember the symptoms of COPD is the acrostic “Lung Damage” which stands for:
L-Lack of energy
U-Unable to tolerate activity
N-Nutrition deficit
G-Gas abnormality (respiratory acidosis)
D- Dry or productive cough
A- Accessory muscle use and Abnormal lung sounds
M- Modification of skin color
A- Anterior/Posterior diameter increase
G- Gets in tripod breathing position
E- Extreme dyspnea
Quality: From mild to severe
The quality of shortness of breath varies from mild to severe. Mild is seen in the initial stages of COPD and is common upon exertion, which limits activities of daily living whereas severe shortness of breath and symptoms cause the work of breathing to occupy their entire thoughts and energy. Because asthma is classified in four ways, step 1: mild intermittent, step 2: mild persistent, step 3: moderate persistent, and step 4: severe persistent, the quality of cough and shortness of breath must be determined from mild to severe and quantified by how many days per week the patient is in distress breathing.
Triggers: Exercise
COPD can be triggered by allergies and pollutants. Determining the type of trigger is essential in asthma to teach prevention of acute exacerbations and better preparation.
Occurrence: Predictable or Unpredictable
The use of a home peak flow meter should be used to help identify the current condition of the lungs and airways. Acute exacerbations can be better diagnosed by identifying if the acute event was predictable, such as based on poor weather conditions and air quality, and exercise, or unpredictable without any known trigger (28).
Wheezing
- There are 741 causes of wheezing and COPD is only one cause.
- Identify the characteristics of wheezing.
- Identify the time of day and activities when wheezing starts and stops.
Chronic Cough
- How long have you had the cough?
- How do you describe the cough?
- Is it productive or dry?
- Is it only in the morning or throughout the day?
- When is the cough worse in the day?
- Is the cough related to meals?
- Environmental exposures
Sputum
- What color is the sputum?
- What is the consistency: clear, frothy, pink, thick, thin?
- When is sputum worse during the day?
Breathing Difficulties
- Do you have trouble breathing in or out or both?
- How fast are you breathing?
- Do you use oxygen?
Cyanosis
- What is blue: skin, nails, face, lips?
Irritability/Headache
- What is the nature of the headache?
- What makes the headache worse or better?

Self Quiz
Ask yourself...
- What are the classic clinical symptoms of asthma, chronic bronchitis, and emphysema?
- How are they alike?
- How are they different?
Diagnostic Tests for COPD and Respiratory Failure
Spirometry
Results of extensive quantitative research have concluded that the recommendation for diagnosis of COPD is the use of spirometry (18). The HEDIS measure assesses the percentage of adults over the age of 40 with a diagnosis of COPD who were diagnosed by spirometry. Although the HEDIS measure is to use spirometry for diagnosis, it continues to be underused (19).
Based on the Global Initiative for Chronic Obstructive Lung Disease (20), most patients with COPD have moderate to severe disease due to late or incorrect diagnosis, which increases the overall medical costs and number of exacerbations experienced by the patient. It has been suggested by organizations specializing in respiratory care that the use of spirometry for both diagnosis and management become standardized.
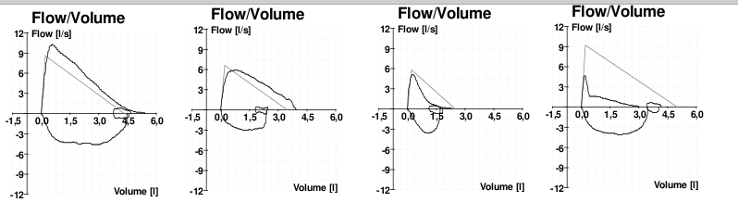
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) is the executive summary for diagnosis and management of COPD (20). Ever since 1947, the ratio of vital capacity (FVC) to forced expiratory capacity in 1 second (FEV1) has been the scientific parameter physicians have used to measure lung health (21). The GOLD standard established in 2001 identified the FEV1/FVC < .70 “rule of thumb” to define airflow obstruction.
Other authorities however have proposed other ranges from <.75% by the American Thoracic Society to < 0.75-0.80 by the Global Initiative for Asthma in 2015 (22). These variations have been developed due to the variations among ethnic groups studied in research that determined the values. The differential diagnoses included COPD, asthma, heart failure, bronchiectasis, pulmonary edema, pneumonia, or cancer.
Correct completion of a spirometry test is essential for a valid diagnosis of COPD. Although there are variations with machines, the basic concept is to have the patient breathe deeply and then forcefully exhale for one full minute. The measurements are collected after three separate attempts, which measure the forced expiratory effort (FEV1) in one minute. Remember to identify gender, ethnicity, and height on the machine as each impacts total lung capacity, and the result is calculated based on these factors and performance. Less than 70% of FEV1 may indicate COPD.
Image. Depiction of Spirometry Testing to Diagnose COPD
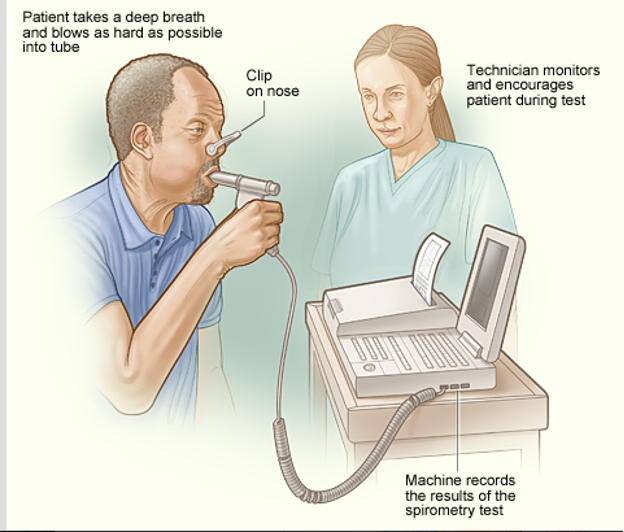
(34)
Classifying COPD
Because treatment for COPD is contingent upon spirometry results, the spirometry needed to be completed to determine the stage of damage to the lungs. The FEV1/FVC ratio for this patient came back to 60% which is below the 70% predicted value and diagnostic for Stage II COPD. A chest X-ray was also ordered to rule out any other diagnosis being considered. It came back negative. ABGs, an EKG, and an echocardiogram could have been completed but were not at this time.
Currently, COPD is classified based on severity by a post-bronchodilator FEV1 score from spirometry. The most recent recommendations also include consideration of both the spirometry results of the FEV1 and the patient’s symptoms to determine the class and severity of COPD. Spirometry confirms the diagnosis, and the pulmonary function test classifies the severity. According to the GOLD standards, which are reviewed annually, the current classes are as follows in the table below:
| STAGE | Symptoms | Post Bronchodilator FEV1 |
| 1 | Mild | >80% |
| 2 | Moderate | 50-80% |
| 3 | Severe | 30-50% |
| 4 | Very severe | < 30% |
Case Scenario:
The patient was tested with spirometry and given a prescription for a short-acting bronchodilator to be used as needed and a daily long-acting bronchodilator. He was encouraged to stop smoking and given smoking cessation resources and options including a group support class, and pharmaceuticals for nicotine replacement for a tapered withdrawal. The patient refused information about smoking cessation.
(35)
Medical Management and Treatment of COPD
Unfortunately, there is no cure for COPD. Any damage done to the airways and the lungs is not reversible. Although currently there is no medical cure available for lung tissue damage, adopting regular medical care and consistent lifestyle changes can help slow the progression of the disease.
The major goals of COPD treatment are:
- Relieve symptoms.
- Slow the progression of the disease.
- Improve exercise tolerance.
- Prevent and manage complications.
- Improve overall health.
The current GOLD Standards are established by numerous research studies and the CDC and include the following (20):
- The Global Initiative for Chronic Obstructive Lung Disease (GOLD) is the standard for diagnostic and treatment guidelines.
- General interventions are comfort measures based on the severity of the symptoms and causative factors.
- Smoking cessation should be mandatory as it is the number one causative factor. Smoking cessation should be discussed at every visit.
- The selection of inhalers depends on the age of the person.
- Nutrition management should be included as 25% of COPD patients are malnourished as eating competes with breathing so meals are limited. Encourage higher calorie supplements such as Ensure to deliver needed nutrients.
- Pharmacological therapy is based on spirometry and the stage of disease. For stage 1 short-acting bronchodilators (SABA) are prescribed as needed for shortness of breath. For stage II, a SABA plus a long-acting bronchodilator (LABA) should be prescribed. Stage III should have a SABA, LABA plus an inhaled glucocorticoid if the patient has frequent exacerbations. Stage IV patients need all given to a stage III plus cardiopulmonary rehabilitation and possibly 02 delivery. All patients should receive an annual flu vaccine, once pneumonia vaccine after age 65, and every 5-10 years for high-risk patients
(16)
Oxygen Use
Because the issue with COPD is decreased airflow, the main goal of therapy is to help the patient’s lungs provide sufficient oxygen to the body.
If the patient is short of breath, hypoxemia, or has obvious signs of heart failure, oxygen should be titrated to saturation levels >93% (4).
The concerns are oxygen toxicity and vasoconstriction. Oxygen causes constriction of the coronary, cerebral, renal, and other key vasculatures. If perfusion decreases with blood hyper-oxygenation, the administration of oxygen may place tissues at increased risk of hypoxia. Hyperoxia reduces coronary blood flow by 8% to 29% in normal individuals and in patients with coronary artery disease or chronic heart failure. Although oxygen supplementation is a modality used only in the end stages of COPD it is still a fundamental intervention.
Care must be taken when giving oxygen to patients with COPD as their drive for inhalation is based on carbon dioxide retention, which they become used to. If additional oxygen is given, it may decrease the drive to breathe and further complicate oxygenation.
Patient Education
Patients need to be taught about the possible cause and treatment plan, so they remain a member of the care plan team. Modification of triggers should be taught first if possible, such as smoking, alcohol, and caffeine cessation. Behavior lifestyle changes are ideal including weight loss. Patients should be taught that as a chronic disease, there is no cure.
Advance directives should be taught and put in place. Antibiotics should be given by prescription to fill upon worsening of symptoms after seeing their clinician, according to the GOLD standard. Patients should be taught to conserve their energy and plan for activity. Patients should be taught how to use a peak flow meter at home to measure their breathing ability and alert their provider if they reach the red target zone. They should be taught the COPD action plan, and how to use a home peak flow meter to detect airflow and to become active participants in their care (9,27).
Image. Peak Flow Meter for home use

(36)

Self Quiz
Ask yourself...
- Which tool is used for home use to determine general airflow through the lungs?
- What does pulmonary rehabilitation include?
- What are some general lifestyle recommendations for someone with COPD?
- What patient education can you provide about weight and nutrition for someone with chronic COPD?
Medications
Medications are used to manage all forms of COPD and be used as monotherapy, dual therapy, or multi-drug therapy per the GOLD Guidelines tier algorithm for COPD control and management (25).
The two main categories of medications that open the airways are the beta 2 bronchodilators, which can be remembered with the pneumonic “BAM” that include bronchodilators, anticholinergics such as ipratropium and methylxanthines that stimulate the bronchioles to open such as theophylline.
The second class of medications are the anti-inflammatories that can be remembered by the acronym “SLM,” which includes steroids, leukotrienes, and mast cell stabilizers.
|
Drug Class |
Action |
Brand Names |
|
Bronchodilators:
|
|
|
|
Beta 2 -Short acting (SABA) |
Dilate bronchi |
Albuterol (rescue inhaler) Salbutamol, Terbutaline |
|
Long-Acting Beta Agonists (LABAs) |
Act on Beta 2 receptors bronchodilator |
Advair, Serevent, Foradil, Oxis, Salmeterol, Formeterol |
|
Short Acting Beta Agonists (SABAs) |
Act on Beta 2 receptors to Broncho dilate |
Albuterol, Ventolin, Proventil, Spiriva |
|
Anticholinergics/ Antimuscarinics (LAMA) |
Increase sympathetic system to open airways |
Ipratropium, tiotropium |
|
Methylxanthines |
Beta 2 stimulation to open bronchioles |
Aminophyllin, Theophyllin, Unidur, Theodur |
|
Anti-inflammatories: |
|
|
|
Steroids (Inhaled Corticosteroids) |
Decrease inflammation in the lower airways |
Fluticasone, Advair, Flovent, Pulmicort, Symbicort, Asmanex, Alvesco, mometesone |
|
Steroid (Nasal) |
Decrease inflammation in the upper airways |
Nasonex, Nasacort, Veramyst |
|
Leukotriene Antagonists (LTRAs) |
Non-steroidal anti-inflammatory |
Singulair, Accolate |
|
Allergy Medications |
Antihistamine Anti IgE blockers |
Xolair, Claritin/Clarinex, Allegra, Zyrtec, |
|
Mast Cell Stabilizers |
Decrease release of histamine |
Cromolyn |
|
Phosphodiesterase-4 PDE-4 Inhibitors |
Suppress inflammation |
Roflumilast |
Remembering the physiology of the airways is largely controlled by two main nervous system receptors, the muscarinic and beta receptors, blocking the muscarinic or stimulating the beta receptors will increase the airways. Another way to remember the different kinds of medication used for COPD is to remember the drug name endings. The muscarinic antagonist drugs end in “ium” such as ipratropium, tiotropium, and umeclidinium.
Additionally, a new drug called glycopyrrolate is muscarinic so drugs that end in “ate” will remind you that the drug “ate” the effects of muscarinic receptors. All the respiratory beta-agonist drugs end in “ol” (similar to cardiac beta blockers ending in “ol”). Drugs such as formoterol, salmeterol, and albuterol are beta-agonists and increase the airway diameter. The inhaled corticosteroids end in “one” like fluticasone or mometasone.
A medication grid can help you remember the progression of adjunct medication for both COPD and asthma. Whereas treatment for COPD starts on the left and moves towards the right, asthma begins with an ICS and moves to the left as adjunct medications.
Advancement of treatment also depends on the frequency of the use of the SABA, rescue inhaler. If someone with COPD is using a SABA more than 2x/week then they would advance from a LAMA to adding on an LABA and then later the third class of medication the ICS.
In contrast, someone with asthma who is using the rescue inhaler more than two times/week would have started with only an ICS medication, but now needs to advance to the LABA and then lastly add on the LAMA. If the patient with COPD or asthma is not using the rescue inhaler (SABA) more than two times weekly, then they do not need to advance in medication treatment. For asthma, the first medication is a SABA, then ICS. They will never use a LABA without using the ICS. The last medication to use for asthma is a LAMA.
For COPD, the first class of medication to use after the SABA, is the LAMA, and then advance to the LABA, with the last medication added will be the ICS.
Many pharmaceutical companies will create dual combination therapies for ease of use.
|
COPD |
LAMA |
LABA |
ICS |
ASTHMA |
|
®SABA |
“ium” |
“ol” |
“one” |
¬SABA |
Inhaled Medications
Modes of delivery for each of these drugs can be in inhaled medications such as metered dose, breath-activated, or oral form.
Inhaled medications for COPD use different mechanisms to open the airways. Spacers may be used to help increase drug delivery. Nebulizers can also be used for oxygen or are given through liquid drugs via a face mask. Each medication, many can be given intravenously to critically ill patients.
Each class of medication is described below.
Bronchodilators
Inhaled bronchodilators are the key medications to opening the airways as they act on the beta receptors of the bronchiole tubes to cause bronchodilation.
Bronchodilators relax the smooth muscles around the bronchiole air tubes which dilate the bronchioles allowing more area of air to pass through. Most bronchodilators are taken with inhalers, so the medication goes directly to the airway. Short-acting bronchodilators (SABA) versus long-acting bronchodilators (LABA) work directly on opening the airways.
The short-acting agonists are for an acute exacerbation when the airway closes suddenly, whereas the long-acting bronchodilator agonists (LABAs) are to be taken daily on a regular schedule to maintain the patency of the airways. Generally, SABAs are more expensive than LABAs. Each has a rapid onset of action and can be used symptomatically or before exercise.
Short-acting beta 2 agonists work within several minutes for 3-5 hours, compared to long-acting beta 2 agonists, which last 12 hours. Each includes side effects similar to drugs that mimic the sympathetic system including fine tremors, muscle cramps, nervous tension, palpitations, tachycardia, sleep disturbances, hypokalemia, and occasionally paroxysmal bronchospasm.
Anti-Muscarinic/ Anti-cholinergic
This class of medication causes bronchodilation and reduces mucous secretion by blocking muscarinic receptors in the lung. They have a longer action and greater bronchodilator effect than the B2 agonists and are used in both COPD and asthma. Side effects cause dry mouth, nausea, constipation, and can cause urinary retention so must be used with caution for those patients with bladder problems and glaucoma. Short-acting anti-muscarinic can be inhaled or nebulized and includes ipratropium. The long-acting tiotropium can only be given by an inhaler.
Methylxanthines
This class stimulates the beta 2 receptors in the lungs to allow bronchodilation and includes theophylline. It can be given orally, or by IV. This class works by inhibiting phosphodiesterase or blocking adenosine. This class is often given in acute asthma. Side effects include gastrointestinal upset and cardiac palpitations, tachycardia, arrhythmias, headache, insomnia, and convulsions.
Steroids
Inhaled corticosteroids (ICS) are generally the second adjunct therapy suggested by the GOLD Guidelines and help reduce inflammation in the airways and lungs.
Inhaled steroids should not be used as monotherapy but should be used in combination with a bronchodilator. Because this class is a steroid, it may increase blood sugar levels and complicate control for patients who also have diabetes. This class of medications also may cause oral thrush as the oral inhaler delivers glucocorticoids directly to the mouth. It is recommended that this class of oral inhaler be given last for COPD and then the mouth be rinsed immediately after ingestion. On the contrary, it is often the first class of medications for asthma after short-acting bronchodilators.
They can be given via various routes including inhalation (Beclomethasone and Budesonide), orally in the form of prednisolone, and IV in the form of hydrocortisone.
Systemic side effects of long-term corticosteroids are numerous and affect each body system. Blood sugar levels rise in the endocrine system, the muscular-skeletal system produces myopathy; neurologically growth retardation and psychiatric disturbances, and impaired wound healing, sodium, and water retention for the skin; and glaucoma and central redistribution of fat are some of the common side effects.
Leukotriene Receptor Antagonists
This class is used to block the effects of leukotrienes which would normally stimulate the mast cells to release histamine. When histamines are released, vasodilation and fluid movement to the site are natural reactions of the inflammatory response, which is the cause of many symptoms of COPD.
In blocking this reaction, lungs may have less mucus build up and air can move more easily in ventilation. Omalizumab (Xolair), which costs a lot, is given orally. It is an anti-IgE monoclonal medication and is used in severe cases of asthma.
Side effects include gastrointestinal disturbances, headache, insomnia, arthralgia, myalgias and rare bleeding disorders.
Phosphodiesterase-4 (PDE-4) Inhibitors
If COPD symptoms continue, this class of medication may be added. It is the newest class of medications and suppresses inflammation in the airways.

Self Quiz
Ask yourself...
- What are the common side effects of bronchodilators?
- What patient education needs to be discussed regarding the use of inhalers?
- What class of medications decrease inflammation seen in COPD?
- What class of medications opens the bronchioles?
Case Scenario:
Our patient in the case scenario was given a medication regimen to begin with. Initially, he was referred to a smoking cessation program for behavioral management. The patient thought he could try to quit smoking on his own and did not attend any of the classes or use the resources. He was also inconsistent in the use of his medications due to financial barriers. His symptoms became worse after getting a cold, and he presented again to the emergency department with severe shortness of breath, coughing, weakness, pallor, use of accessory muscles to breathe, and heart palpitations. The Emergency Department physician diagnosed him with respiratory failure.
Complications of COPD
Respiratory failure is an extremely serious complication of uncontrolled COPD. Acute exacerbations need to be treated immediately for airway management. Complications of COPD can become life-threatening beyond just shortness of breath and limitations of activities and include pneumonia, heart disease, hypertension, cardiac arrhythmias, and congestive heart failure.
Although COPD may be controlled, it may also suddenly become worse due to any additional respiratory problem such as a cold or flu. If additional symptoms of fever, difficulty breathing, chest tightness, or increased coughing develop, patients should see their primary care provider immediately for treatment.
In addition to the complications of ineffective breathing, the body is stimulated to make more red blood cells to compensate for hypoxia in the tissues. This results in thickened blood, possible risk for thromboembolism formation, and pulmonary hypertension as the pressure within the lungs increases.
The blood flow from the pulmonary artery backs up into the heart and can eventually lead to left-sided heart failure. If a patient is a smoker, the chronic irritation to the alveoli tissue also stimulates the inflammatory response, which creates vasodilation, release of histamines, and alveolar stiffening. With chronic hypoxia, the patient will also develop chronic hyperventilation as a compensatory mechanism. failure.
Respiratory Failure
The inability to get enough oxygen into the blood can cause respiratory failure, causing a buildup of carbon dioxide, which can damage tissue and organs, and eventually death. Symptoms include shortness of breath, extreme fatigue, tachycardia, pallor, cyanosis of the lips, coughing, and possible collapse.
The inability to sustain adequate breathing may require support from a ventilator (23). High carbon dioxide levels can additionally cause blurred vision, confusion, headache, cyanosis, respiratory acidosis, and damage to the brain and kidneys. Blood pH levels that change from high carbon dioxide will disrupt normal fluid and electrolytes and further damage the entire body.
Diagnosing respiratory failure involves performing many of the same tests used to diagnose COPD including diagnostic imaging like a chest x-ray, bronchoscopy, and lung imaging tests such as computed tomography (CT). Structural abnormalities within the lung tissue or detection of fluid accumulation within it can be identified by CT or magnetic resonance imaging (MRI). It also includes additional blood tests including arterial blood gas (ABG) analysis to determine the severity by measuring oxygen and carbon dioxide levels providing insights into acid-base disturbances.
Blood tests such as a complete blood count (CBC) and basic metabolic panel (BMP) may be performed to assess for signs of infection, electrolyte imbalances or any systemic irregularities that might contribute to respiratory comprise. Additional diagnostic procedures could include collecting cultures of sputum or blood to identify pathogens responsible for infections like pneumonia that may lead to respiratory failure. Electrocardiography (ECG) may also be conducted to evaluate cardiac function and rule out causes that resemble respiratory distress such as heart failure. After determining the root cause of respiratory failure, treatment plans can be customized.
Treatment of Respiratory Failure
In addition to the above-listed medications, oxygen support may be needed. Based on the severity of respiratory failure oxygen support may include a noninvasive positive pressure ventilation such as a nasal cannula or mask (26). More severe respiratory failure may advance to bag-mask ventilation or mechanical ventilator. The most severe may require a tracheostomy to place a breathing tube directly into the trachea to stabilize and support oxygenation (25). Each intervention requires additional careful nursing attention, assessment, and interventions.
The treatment for respiratory failure depends on its source and severity. Relieving airway obstruction, managing exacerbations of chronic lung diseases, or managing fluid overload may be included treatments. Supportive measures, including bronchodilators, corticosteroids or diuretics may be taken as supplements to optimize respiratory function and relieve symptoms.
Close monitoring of vital signs, oxygen saturation levels and arterial blood gases enables clinicians to titrate therapies appropriately while interventions to maintain hemodynamic stability and avoid complications like aspiration or ventilator-associated pneumonia are integral parts of comprehensive care. Collaboration among multidisciplinary teams is vital in creating tailored treatment strategies tailored specifically for individual patient needs and optimizing results in respiratory failure management.
Case Scenario Summary
Because our patient in the evolving scenario presented quickly to the emergency department, he was able to get prompt attention and ventilator support. He remained on a ventilator for five days, received medication for pneumonia, and had a positive outcome.
This time, he was more convinced of the seriousness of his COPD and began a smoking cessation program after discharge. He received financial assistance for his medication, enrolled in a COPD action plan, and followed through with his home health nurse’s recommendations. It was difficult, but with the help of an interdisciplinary team, he extended his life with a chronic condition.
Conclusion
COPD is a chronic and incurable condition that includes three subcategories of chronic respiratory conditions including asthma, chronic bronchitis, and emphysema. Risk factors include smoking and exposure to environmental allergens and pollutants that trigger the lungs and alveoli to become inflamed and produce mucus resulting in narrowed airways. COPD is a condition of restricted airflow and causes complications throughout the body related to chronic hypoxia.
Assessment is based on a history of exposures to allergens, mainly cigarette smoking, symptoms, physical exam, and spirometry test. Clinical symptoms include shortness of breath, coughing, wheezing, and dyspnea. Diagnostic tests include spirometry as the GOLD standard and may include radiography to visualize the size of the lungs.
Treatment includes management of symptoms, medications, lifestyle modifications, and education for pulmonary rehabilitation to avoid acute exacerbations and improve the quality of life. There is no cure but there are many classes of medications to assist with bronchodilation and decrease inflammation of airways and lungs. Respiratory failure is the most severe complication of uncontrolled COPD and requires additional support of oxygenation. Although there is no cure, the prognosis depends on the severity of the condition and the ability to respond to treatment.
Resources
- With information that includes how to stop smoking, the ALA is committed to "Fighting for Air" and publishes a highly informative website about lung diseases and lung disorders.
- This respected U.S. government resource offers information about COPD, including a list of relevant publications and resources for further research.
- A good source for up-to-date developments, this digest is published by the COPD Foundation.
- GOLD works with healthcare professionals and public health officials to raise awareness of COPD and to improve the prevention and treatment of this lung disease for patients around the world. Their website includes information about World COPD Day.
- National Heart, Lung, and Blood Institute:
- A global perspective on COPD, including world statistics and NGO and government-sponsored efforts to combat the disease
References + Disclaimer
- Xu JQ, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2018. NCHS Data Brief, Number 355. Hyattsville, MD: National Center for Health Statistics; 2020.
- Centers for Disease Control and Prevention. National Vital Statistics System detailed mortality data at the Wonder Database website. http://wonder.cdc.gov.
- Centers for Disease Control and Prevention (2023). COPD Prevalence and Incidence. Retrieved from https://www.cdc.gov/copd/data-and-statistics/national-trends.html
- Jarvis, C. (2024). Physical Examination and Health Assessment. 9th ed. Elsevier Publishing.
- World Health Organization (2018). Chronic Respiratory Diseases: Burden of COPD. Retrieved from http://www.who.int/respiratory/copd/burden/en/
- American Lung Association (2024). Trends in COPD (Chronic Bronchitis and Emphysema): Morbidity and Mortality. Retrieved from https://www.lung.org/lung-health-diseases/lung-procedures-and-tests
- Pietrangelo, A. (2015). COPD by the Numbers: Facts, Statistics, and You. Healthline. Retrieved from https://www.healthline.com/health/copd/facts-statistics-infographic
- American Academy of Allergy, Asthma, and Immunology (2016). Immunologic Insights into Triggers of Asthma. Retrieved from https://education.aaaai.org/asthma-education/2016VAM4305
- Glass, C. (2022). Chronic Obstructive Pulmonary Disease (COPD). Family Practice Guidelines, 5th ed. Springer Publisher Co. New York, NY.
- Mozzafarian,D., Benjamin, E., Go, A., Arnett, D., Blaha, M., Cushman, M., de Ferranti, S., Despres, J., Fullerton, H., e al (2015). Heart disease and stroke statistics- 2015 update: a report from the American Heart Association. Circulation Jan 27;131(4): e29-322. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/25520374
- Kosacz, N. (2012). Chronic Obstructive Pulmonary Disease Among Adults-United States, 2011. Morbidity and Mortality Weekly Report. Centers for Disease
- Control and Prevention. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6146a2.htm
- Centers for Disease Control and Prevention (2013). National Center for Health Statistics. Behavioral Risk Factor Surveillance Survey, 2011. Analysis performed by the American Lung Association Research and Health Education Division using SPSS software. COPD (2017). Right Diagnosis of COPD. Retrieved from http://www.rightdiagnosis.com/c/copd/intro.htm
- Centers for Disease Control and Prevention (CDC). (2016). Overweight and Obesity. Retrieved from https://www.cdc.gov/obesity/
- Halpin, D. M. G., & Criner, G. J. (2020). Global initiative for the diagnosis, management, and prevention of chronic obstructive lung disease. The 2020 GOLD science committee report on COVID-19 and chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine, 202(2), 156-164. https://doi.org/10.1164/rccm.202005-1589ST
- Guarascio, A., Ray, S., Christopher, K., Self, T. (2013). The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinical Economics and Outcomes Research. 5:235-245. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3694800/
- Grossman, S., & Porth, C. (2014). Porth’s pathophysiology: concepts of altered health states. Ninth Edition. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.
- National Heart, Lung, and Blood Institute (2018). COPD Action Plan. Retrieved from
- https://www.nhlbi.nih.gov/health-topics/education-and-awareness/COPD-national-action-plan
- Global Initiative for Chronic Obstructive Lung Disease. (2020). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2020 report. Retrieved from https://goldcopd.org/wp-content/uploads/2019/11/GOLD-2020-REPORT-ver1.0wms.pdf
- NCQA.org (2016). Incorporating HEDIS Measures and Newer Therapies to Improve COPD Treatment Adherence and Outcomes. Retrieved from http://www.ncqa.org/education-events/seminars-and-webinars/live-seminars-webinars/improving-copd-treatment-adherence-and-outcomes
- Global strategy for asthma management and prevention (2015). Global Initiative for Asthma (GINA). Retrieved from: http://www.ginasthma.org/
- Brusasco, V. and Pellegrino, R. (2016). “Spirometry in Chronic Obstructive Pulmonary Disease. From Rule of Thumb to Science”, American Journal of Respiratory and Critical Care Medicine, Vol. 193, No. 7 (2016), pp. 704-706. doi: 10.1164/rccm.201511-2239ED. https://www.cdc.gov/copd/index.html
- U.S. Department of Health and Human Services: Healthy People 2020. U.S. Government Printing Office, Washington, DC, 2020. Retrieved from
- https://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Clinical-Preventive-Services
- National Heart, Lung, and Blood Institute. What is Respiratory Failure? Retrieved from https://www.nhlbi.nih.gov/health/respiratory-failure#:~:text=Respiratory%20failure%20is%20a%20serious,made%20in%20the%20body’s%20cells.
- Lopez-Campos, J. L., Tan, W., Soriano, J. B. (2016). Global burden of COPD. Respirology, 21(1), 14-23. https://doi.org/10.1111/resp.12660
- Kory, P., & Pellegrino, E. (2018). Treatment of acute exacerbations of chronic obstructive pulmonary disease. American Family Physician, 98(12), 739-745. https://www.aafp.org/afp/2018/1215/p739.html
- Rochester, C. L., Vogiatzis, I., & Holland, A. E. (2017). An official American Thoracic Society/European Respiratory Society policy statement: Enhancing implementation, use, and delivery of pulmonary rehabilitation. American Journal of Respiratory and Critical Care Medicine, 195(11), 1523-1533. https://doi.org/10.1164/rccm.201704-0785ST
- Criner, G. J., Bourbeau, J., Diekemper, R. L., Ouellette, D. R., Goodridge, D., Hernandez, P., Curren, K., Balter, M. S., Bhutani, M., Camp, P. G., Celli, B. R., Dechman, G., Dransfield, M. T., Fiel, S. B., Foreman, M. G., Hanania, N. A., Ireland, B. K., Marchetti, N., … & Varela, M. V. (2015). Executive summary: Prevention of acute exacerbation of COPD: American College of Chest Physicians and Canadian Thoracic Society guideline. Chest, 147(4), 883-893. https://doi.org/10.1378/chest.14-1677.
- Tan Y, Van den Bergh O, Qiu J, von Leupoldt A. The Impact of Unpredictability on Dyspnea Perception, Anxiety, and Interoceptive Error Processing. Front Physiol. 2019 May 3; 10:535. doi: 10.3389/fphys.2019.00535. PMID: 31130876; PMCID: PMC6509155.
- Wiki Images. (n.d.). COPD. Wikimedia https://commons.wikimedia.org/wiki/File:Copd.JPG
- Wiki Images. (n.d.). Asthma: Before and after. https://commons.wikimedia.org/wiki/File:Asthma_before-after.png#/media/File:Asthma_before-after.png
- Wiki Images. (n.d.) Spirometry NIH. https://commons.wikimedia.org/wiki/File%3ASpirometry_NIH.jpg
- Wiki Images. (n.d.). COPD. Wikimedia. Flow Volume Curve. https://commons.wikimedia.org/wiki/Category:Chronic_obstructive_pulmonary_disease#/media/File:Spirometry.png
- Wiki Images. (n.d.). COPD. Wikimedia. Peak flow meters for home use. https://commons.wikimedia.org/wiki/File%3ATwo_Peak_Flow_Meters.jpg
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
