Course
Rhode Island Renewal Bundle
Course Highlights
- In this Rhode Island Substance Abuse course we will learn about the most common types of substance abuse, and why it is important for nurses to recognize each type and treat accordingly.
- You’ll also learn the basics of the signs and symptoms of each type of substance abuse.
- You’ll leave this course with a broader understanding of substance abuse in general, and substance abuse in adolescents.
About
Contact Hours Awarded: 10
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Rhode Island Substance Abuse
Introduction
Substance abuse is described as “a pattern of using a substance (drug) that causes significant problems or distress” (1). As of 2020, 37.309 million Americans were currently using illegal drugs (2). Medical professionals are on the front lines of recognizing, treating and providing support to individuals who suffer from substance abuse. This Rhode Island Substance Abuse course will walk you through the different types of substances abused, the prevalence of that abuse, the symptoms one experiences while using that substance, overdose symptoms, and how to counteract an overdose. You will also learn about substance abuse in adolescents, and prevention methods currently being used to combat substance abuse in adolescents.

Self-Quiz
Ask Yourself...
- What do you think are the most abused substances?
- What knowledge do you hope to gain by completing this Rhode Island Substance Abuse course?
Alcohol
Alcohol abuse is the second most common type of substance abuse, with the first being tobacco use (3). While many individuals in the United States can drink alcohol and it is not considered abuse, there are some individuals whose drinking causes harm or distress. In the case of alcohol use disorder, harm or distress is described as alcohol leading to health problems, or trouble while at home, work, school or with law enforcement (3).
There are several signs and symptoms of alcohol use disorder that help one to determine if their loved one needs help. As health care providers, it is important to understand the signs and symptoms to properly help and treat those who are experiencing alcohol use disorder. Symptoms can range from mild to severe, depending on the number of symptoms experienced (5) and include:
- Unable to limit the amount of alcohol consumed
- Wanting to decrease the amount consumed, but being unsuccessful
- Spending a large amount of time obtaining alcohol, drinking alcohol, or recovering from alcohol use
- Having a strong craving or urge to drink alcohol
- Not completing major obligations at work, school or home due to alcohol use
- Continuing to drink alcohol even though you know it is causing problems physically, at work, home, or in relationships
- No participating in social activities or work-related functions to consume alcohol
- Developing a tolerance to alcohol so more is needed to elicit the same effect
- Experiencing symptoms of withdrawal, such as, nauseas, sweating and shaking when you are not drinking
While the above signs and symptoms are typically ones that do not have a medical component attached, alcohol use disorder impacts nearly every organ and system in the body. This widespread impact can have a detrimental effect on an individual suffering from alcohol use disorder (4) such as:
- Neurologic
– Ischemic stroke
– Hemorrhagic stroke - Cardiac
– Cardiomyopathy
– Arrhythmias
– Ischemic heart disease
– Hypertension - Lung
– Acute respiratory distress syndrome
– Pneumonia - Liver
– Steatosis
– Steatohepatitis
– Fibrosis
– Cirrhosis
– Alcohol associated hepatitis
– Liver cancer - Pancreas
– Acute and chronic pancreatitis - Gastrointestinal
– Gut leakiness
– Microbial dysbiosis
– Colorectal cancer
Clear patterns have emerged between alcohol use disorder and increased risk for certain types of cancers (4):
- Head and neck cancer
– Oral cavity
– Pharynx
– Larynx - Esophageal Cancer
- Liver Cancer
- Breast
- Colorectal Cancer
Knowing the effects of chronic alcohol use on the body is important in understanding the treatment methods that will be needed. Treatment options range from spiritual to medical, with many individuals utilizing more than one option (6).
- Detox and withdrawal
– This treatment option is typically done in an inpatient setting. Treatment begins with detoxification, which leads to withdrawal symptoms. These symptoms can be medically managed, and occasionally require sedating medications. Detox and withdrawal generally take 2 to 7 days. - Psychological counseling
– This treatment option will help the individual better understand their problem with alcohol and provide support on the psychological aspects of alcohol use disorder. This type of treatment can be done individually or in a group setting. - Oral medications
– Disulfiram is a medication that helps to curb one’s want for alcohol. While the drug doesn’t remove the urge to drink, it will produce a physical reaction to consuming alcohol in the form of flushing, nausea, vomiting and headaches.
– Naltrexone is used to block the good feelings alcohol causes, which can aid in recovery.
– Acamprosate is used to help curb cravings of alcohol and is generally used in combination with Naltrexone. - Injected medication
– Vivitrol is the injected version of Naltrexone and is injected once a month. Injected medications may be easier, or more consistently used than oral medications. - Medical treatment
– As we’ve learned, alcohol use disorder comes with a large amount of health concerns. These concerns typically require medical treatment in the form of medication, surgery, outpatient care, etc. - Spiritual practice
– It has been shown that individuals involved in some type of spiritual practice find it easier to maintain recovery.

Self-Quiz
Ask Yourself...
- What are the five most common types of cancers associated with alcohol use disorder?
- Have you personally taken care of someone with alcohol use disorder? Did they exhibit any symptoms or illnesses listed above?
Marijuana
Marijuana, also known as cannabis, weed or pot, refers to the dried flowers, leaves, stems and seeds of the cannabis plant. In one cannabis plant there are over 100 compounds ranging from tetrahydrocannabinol (THC) to cannabidiol (CBD) (7). While THC and CBD have the same molecular structure, the difference in how the atoms are arranged accounts for the different effects on the body. THC is the main psychoactive compound in cannabis, which produces the high sensation, while CBD, although psychoactive, does not produce the high sensation (8).
Marijuana is the most used federally illegal drug in the United Stated. In 2019, the CDC reported that 48.2 million, or ~18% of Americans have used marijuana at least once. There are several ways to use marijuana, including: smoking in joints, blunts, or bongs, vaping via electronic vaporizing devices, mixing or infusing into foods or drinks, or inhaling oil concentrates (7).
There are many health risks associated with using marijuana, in any form. It is estimated that 3 in 10 people who use marijuana have marijuana use disorder (7).
The risks include:
Brain Health
Since marijuana is a psychoactive drug, the main effect is on brain function. Marijuana specifically affects the parts of the brain responsible for memory, learning, attention, decision making, coordination, emotions and reaction time.
Heart Health
Marijuana is known to make the heart beat faster, which can make blood pressure higher immediately after use. This can lead to an increased risk of stroke, heart disease or vascular disease.
Lung Health
Inhaled marijuana can cause damage to lung tissues and small blood vessels, as well as scarring to the lung. More research is being done to understand the effects of secondhand marijuana smoke.
Mental Health
While the relationship is not fully understood, marijuana has been linked to social anxiety, depression and schizophrenia.
Unintentional Poisoning
There is a greater risk for unintentional poisoning with edibles (marijuana baked or put into food or drinks) than with inhaled marijuana. This risk is because children can easily mistake food with marijuana in it. In some instances, emergency medical care has been required.
As marijuana becomes legal, and readily available across many states, teenagers are gaining better access to it. The CDC reports that 37% of high school students in the United States have reported using marijuana. This use can come with impacts to their developing brains, resulting in (7):
- Difficulty thinking and problem-solving
- Problems with memory and learning
- Reduced coordination
- Difficulty maintaining attention
- Problems with school and social life

Self-Quiz
Ask Yourself...
- What is the difference between THC and CBD?
- What were the 5 health risks listed?
- Were you aware of the health risks associated with marijuana used? Do the health risks surprise you?
Prescription Medicines
Prescription drug abuse is classified as the abuse of a prescription medication that is taken in a way not intended by the prescriber. This abuse can be by the person who the drug was initially prescribed for, or from someone taking another person’s prescription medication. The National Center for Drug Abuse Statistics show that 6% of Americans over the age of 12 abuse prescriptions in a year, and 12% of prescription drug abusers are addicted. This is perpetuated by 4 out of 5 pharmacy filled prescriptions being opioids (10).
Prescription medication is sectioned off into three categories: opioids, anti-anxiety medications/sedatives/hypnotics, and stimulants. Signs and symptoms of prescription drug abuse vary depending on the type of drug used (9). Opioids are a type of medication that is used to treat pain. These medications usually contain oxycodone or hydrocodone. Opioids are the leading cause of drug overdose death, with 74.8% of drug overdose death being from Opioids (11).
The signs of symptoms of opioid drug abuse include (9):
- Constipation
- Nausea
- Feeling high
- Slowed breathing rate
- Drowsiness
- Confusion
- Poor coordination
- Increased dose needed for pain relief
- Worsening or increased sensitivity to pain with higher doses
Anti-anxiety medication, sedatives and hypnotics are used to treat anxiety and sleep disorders. Some medications used for these disorders are alprazolam (Xanax), diazepam (Valium), and zolpidem (Ambien).
The signs and symptoms of drug abuse by these types of medications are (9):
- Drowsiness
- Confusion
- Unsteady walking
- Slurred speech
- Poor concentration
- Dizziness
- Problems with memory
- Slowed breathing
Stimulants are a type of medication used to treat attention-deficit/hyperactivity disorder (ADHD) and certain sleep disorders. Some medications used to treat these disorders include methylphenidate (Ritalin, Concerta, and others), dextroamphetamine-amphetamine (Adderall XR, Mydayis) and dextroamphetamine (Dexedrine).
Signs and symptoms of drug abuse by these types of medications are (9):
- Increased alertness
- Feeling high
- Irregular heartbeat
- High blood pressure
- High body temperature
- Reduced appetite
- Insomnia
- Agitation
- Anxiety
- Paranoia
Medical complications differ depending on the type of medication abused. Opioids can decrease respiratory rate with the potential for breathing to stop altogether. They can also cause a coma, and lead to death. Anti-anxiety/sedatives/hypnotics can cause memory problems, low blood pressure and slowed breathing. Like opioids, they can also lead to coma or death. Abrupt withdrawal of these medications can lead to an overactive nervous system and seizures. Stimulants can increase the bodies temperature, produce heart problems, high blood pressure, seizures or tremors, hallucinations, aggressiveness, and paranoia (9).
Opioids can be reversed with a medication called Naloxone. This medication works by binding to the opioid receptors, then reversing and blocking the effects of other opioids. It is used to restore an individual’s breathing and can be given through injection or nasal spray. If Naloxone is given outside of a medical facility, emergency personnel should be contacted immediately (18).

Self-Quiz
Ask Yourself...
- Were you surprised to learn that most prescriptions filled in pharmacies are opioids?
- Think about the number of children who are on ADHD medication. Do you think they or their guardians should receive in-depth training and education on the potential dangers of that medication?
- What symptoms were similar? What symptoms were different?
Methamphetamine
Methamphetamine is a highly addictive, man-made, central nervous system stimulant. This drug increases heart rate, body temperature, respiration, and blood pressure. It also enhances one’s energy, attention, focus, pleasure, and excitement (12). It has commonly been referred to as meth, ice, speed, and crystal. Research has shown that 2.5 million Americans aged 12 or older reported using methamphetamine within the past year. 53% of those individuals met diagnostic criteria for methamphetamine use disorder, but less than 1 in 3 received substance use treatment within the past year (13).
There are four ways methamphetamine can be used: smoking, swallowing (pill), snorting, or injecting the powder that has been dissolved in water or alcohol. While methamphetamine produces a high quickly, it also fades quickly. This produces what is called and “binge and crash” pattern of use. This type of use is where an individual will take the drug every few hours for several days at a time, resulting in lack of food and sleep (14).
There is a substantial amount of long-term health effects from methamphetamine use. Those who inject methamphetamine are at a higher risk for contracting infectious diseases like HIV and hepatitis C.
Other long-term problems include (14):
- Extreme weight loss
- Severe dental problems
- Intense itching which can lead to skin sores and infection from scratching
- Anxiety
- Changes in brain structure and function
– Changes have been noted to the brain’s dopamine system which has resulted in problems with coordination and verbal learning.
– Severe changes have also been noted to the areas of the brain that deal with emotion and memory - Confusion and memory loss
- Sleeping problems
- Violent behavior
- Paranoia
- Hallucinations
Due to the effect methamphetamine has on the body, an overdose often leads to a stroke, heart attack, or organ problems. Because of this, it is imperative health care providers restore blood flow to the affected part of the brain for a stroke, restore blood flow to the heart in the event of a heart attack, or treat the organ issues that present (14). Treatment for methamphetamine use disorder focuses on cognitive-behavioral therapy and motivational incentives, such as vouchers or small cash rewards that encourage individuals to remain drug-free. There is currently no FDA approved medication to treat a methamphetamine addiction (14).

Self-Quiz
Ask Yourself...
-
What are the 10 long-term effects methamphetamine can have on the body as noted in this Rhode Island Substance Abuse course?
-
Have you seen any of these long-term effects in your nursing practice?
-
Does it surprise you that there is no medication to treat a methamphetamine overdose?
Cocaine
Cocaine is a highly addictive stimulant drug that is derived from the leaves of the coco plant that is native to South America. Dealers of cocaine may add in other drugs to the cocaine, such as amphetamine or synthetic opioids, like fentanyl. Adding in synthetic opioids can be especially dangerous and lead to overdose and even death (15). Over 5 million Americans reported current cocaine use in 2020, with nearly 1 in 5 overdose deaths reported (13).
There are several ways in which cocaine can be used: in powder form it can be snorted or rubbed into an individual’s gums, the powder can be dissolved and injected into the bloodstream, or if the cocaine is in crystal form, it can be heated and smoked. Injecting cocaine produces a faster and more intense high but is short-lasting. Cocaine affects the brain by increasing the amount of dopamine produced. This increase of dopamine floods the brain’s reward circuit, which reinforces drug-taking behavior. Repeated cocaine use can lead to the brain’s reward circuit becoming less sensitive, which leads to individuals taking stronger and more frequent doses to achieve the same high as before (15).
The effects of cocaine are felt almost immediately and can disappear within a few minutes to an hour. There are several health effects from using cocaine (15):
- Extreme happiness and energy
- Mental alertness
- Hypersensitivity to sight, sound, and touch
- Irritability
- Paranoia
- Constricted blood vessels
- Dilated pupils
- Nausea
- Increase in body temperature and blood pressure
- Increased or irregular heartbeat
- Tremors/muscle twitches
- Restlessness
There are several long-term effects of cocaine use. These effects can range from common, to being dependent on the method of use (15)
- Malnourished due to a decreased appetite
- Movement disorders
- Irritability
- Restlessness
- Auditory hallucinations
- Snorting cocaine
– Loss of smell
– Nosebleeds
– Frequent runny nose
– Problems with swallowing - Smoking cocaine
– Cough
– Asthma
– Respiratory distress
– Higher risk for infections like pneumonia - Consuming cocaine by mouth
– Severe bowel decay due to reduced blood flow - Injecting cocaine
– Increased risk of contracting HIV, hepatitis B and C, and other blood-borne diseases
– Skin or soft tissue infections
– Scarring or collapsed veins
A cocaine overdose is similar to that of a methamphetamine overdose, with the inclusion of seizures. Like methamphetamine, it is critical that health care providers restore blood flow to the heart and brain in the event of a heart attack or stroke. If an individual presents with a seizure due to a cocaine overdose, the first action to be taken is to stop the seizure. Cocaine mirrors that of methamphetamine use in terms of increased dopamine in the brain. This leads to an addictive nature, as well as needing more drug overtime to produce the same high (15).
Unfortunately, there is no FDA medication approved to treat cocaine use disorder.
There are several behavioral therapy options available (15):
- Cognitive-behavioral therapy
- Contingency management or motivational incentives
- Therapeutic communities
– These are residences in which people can recover from substance use disorders with other individuals who understand their addiction, all while being drug-free - Community based recovery groups

Self-Quiz
Ask Yourself...
- How many Americans stated they had used cocaine in 2020? Did that number surprise you? Did you think it would be higher or lower?
- While a cocaine overdose may be similar to that of a methamphetamine overdose, what additional overdose symptom can happen with cocaine use?
- There are four methods in which cocaine can be used, what long-term side effects stem from those four methods?
Heroin
Heroin is a type of drug made from morphine, which is derived from the seed pod of opium poppy plants (16). According to the CDC, over 19% of all opioid overdose deaths in 2020 involved the use of heroin (17). Heroin can be found as a white or brown powder, or a black tar like substance. Like cocaine and methamphetamine, heroin can be injected into the bloodstream, snorted, or heated and smoked. Additionally, some individuals mix heroin with cocaine, or alcohol. This created an even higher risk for an overdose, and potentially death (16).
The effects of heroin on the body are like those of prescribed opioids. When heroin reaches the brain, it is turned into morphine, which binds to opioid receptors. This causes the user to feel what is described as a rush, or a pleasurable sensation. How intense the rush is, is determined by how much drug has been taken and how quickly it attaches itself to the opioid receptor (16).
Along with the rush, there are several short-term effects that people may experience when using heroin (16):
- Dry mouth
- Warm, flushing of the skin
- Heaving feeling in their arms and legs
- Nausea
- Vomiting
- Severe itching
- Clouded mental functioning
- Being in a back-and-forth state of consciousness and semi-consciousness
Individuals with heroin use disorder may experience some of the following long term health effects (16):
- Insomnia
- Collapsed or damaged veins from injecting the drug
- Damaged tissues on the inside of the nose due to snorting the drug
- Infection in the lining of the heart and the valves
- Abscesses
- Constipation and stomach cramping
- Liver and kidney disease
- Lung complications, like pneumonia
- Mental disorders like depression and antisocial personality disorder
- Sexual dysfunction in men
- Irregular menstrual cycle in women
- Increased risk for blood borne diseases such as HIV and hepatitis C
Heroin overdoses, along with opioid overdoses, have been increasing in the United States. A heroin overdose depresses one’s heart rate as well as breathing, leading to hypoxia. However, Naloxone is a medication that can reverse opioid overdoses, if given the correct way. Naloxone can be injected or snorted and has recently been approved for over the counter dispense in several states (18).
Those who suffer from heroin use disorder have a wider variety of treatments at their disposal. Behavioral therapies include cognitive-behavioral therapy as well asl contingency management. It has been shown that these behavioral therapies work best when used in-conjunction with medications.
There are three different types of medications available to those with heroin use disorder (16):
Methadone
This is an opioid receptor full agonist, which means it attaches itself to and actives an opioid receptor to help ease withdrawal symptoms of heroin cravings
Buprenorphine
This is an opioid receptor partial agonist, which means it attaches itself to and partially activates opioid receptors to help ease withdrawal symptoms and heroin cravings
Naltrexone
This is an opioid receptor antagonist, which means it prevents heroin from binding to opioid receptors, blocking the effects

Self-Quiz
Ask Yourself...
- What plant is heroin derived from? Were you aware of this before this course Rhode Island Substance Abuse course?
- Have you been educated on the proper way to administer Narcan to an individual suffering from a heroin or opioid overdose? Do you feel like this is something all health care professionals should be educated on?
- What are the three medications approved for treatment of heroin use disorder?
Hallucinogens
Hallucinogenic drugs are described as a group of drugs that alter a person’s awareness of their surroundings, thoughts, and feelings (19). In 2019 it was estimated that 5.5 million people in the United States used hallucinogens within that past year (20). Hallucinogenic drugs are split into two categories: classic hallucinogens and dissociative drugs. Like the name suggests, both types of hallucinogens can cause the user to experience hallucinations, but dissociative drugs can also cause the user to feel out of control or disconnected from their body (19).
Common classic hallucinogens include (19):
D-lysergic acid diethylamide (LSD)
Considered one of the most powerful mind-altering chemicals. This drug is a clear or white odorless material, made from lysergic acid. Lysergic acid is found on fungus that will grow on rye and other grains.
4-phosphoryloxy-N, N-dimethyltryptamine (Psilocybin)
This hallucinogenic is also referred to “magic mushrooms” or “shrooms” since it is found on certain types of mushrooms in South America, Mexico, and the United States.
Mescaline (Peyote)
Peyote comes from a small, spineless cactus, but may also be synthetic. While it is illegal in the United States, it can be used in religious ceremonies in the Native American Church.
N, N-dimethyltryptamine (DMT)
A chemical found in some Amazonian plants. It can be made into a tea called Ayahuasca or smoked if synthetically made.
251-NBOMe
This is a synthetic hallucinogen that is like LSD and MDMA but is more potent. It was originally developed for use in brain research. It has also been referred to as “N Bomb” or “251”.
Common dissociative drugs include (19):
Phencyclidine (PCP)
This drug was initially developed for surgery in the 1950’s, but due to its serious side effects it is no longer used. It can be found in several forms, such as: tablets, liquid, and white crystal powder.
Ketamine
This drug is used as an anesthetic for both humans and animals and is typically stolen or sold illegally from veterinary offices. Ketamine comes in powder, pills, or liquid form.
DXM (Dextromethorphan)
This drug is used as a cough suppressant and muscus-clearing ingredient in over-the-counter cold and cough medicines. It can be found in syrup, tablet or gel capsule form.
Saliva divinorum (Salvia)
This is a plant that is common to southern Mexico and Central and South America. It’s leaves or typically chewed, or the juice that is extracted from them is drank. Saliva can also be inhaled.
The short- and long-term side effects of hallucinogens are different depending on the type and category of hallucinogenic used. Short-term side effects for classic hallucinogens are (19):
- Hallucinations
- Increased heart rate
- Nausea
- Intensified feelings and sensory experiences
- Changes in sense of time
- Increased blood pressure, breathing and body temperature
- Loss of appetite
- Dry mouth
- Sleep problems
- Uncoordinated movements
- Excessive sweating
- Panic
- Paranoia
- Psychosis
There are two specific long-term side effects of classic hallucinogens. These side effects are typically seen in individuals with a history of mental illness but can happen to anyone (19).
Persistent Psychosis
- This refers to a series of continuing mental problems that include:
- Visual disturbances
- Disorganized thinking
- Paranoia
- Mood changes
Hallucinogen Persisting Perception Disorder (HPPD)
This is a recurrence of certain drug experiencs like hallucinations or visual disturbances. These typically happen without warning and can occur any time after drug use.
Antidepressants and antipsychotic medicals have been used to improve an individual’s mood, as well as treat psychosis. Behavioral therapies have been used to help individuals cope with fear or confusion associated with visual disturbances.
Short-term side effects for dissociative drugs have been known to appear within a few minutes of taking the drug and can last hours or days. If the dosage is low, dissociative drugs can cause the following effects (19):
- Numbness
- Disorientation and loss of coordination
- Hallucinations
- Increase in the user’s blood pressure, heart rate and body temperature
If higher doses of dissociative drugs are taken the following side effects may occur (19):
- Memory loss
- Panic and anxiety attacks
- Seizures
- Psychotic symptoms
- Amnesia
- Inability to move
- Mood swings
- Trouble breathing
The long-term side effects of dissociative drugs are still being researched. However, repeated and prolonged use of PCP has been known to result in addiction. The following long-term effects may continue for a year or more after the drug use stops (19):
- Speech problems
- Memory Loss
- Weight Loss
- Anxiety
- Depression and suicidal thoughts
Most classic hallucinogen use will not result in an overdose but tend to have extremely unpleasant experiences when taken in higher doses. There have been some serious medical emergencies and fatalities that have been reported by 251-NBOMe. Overdose becomes more likely with dissociative drugs. High doses of PCP have been known to cause seizures, coma, and death (19).
Due to the nature of hallucinogens, there is a high risk of bodily harm due to the alteration of the user’s perception and mood (19):
- Users could attempt things they wouldn’t normally do when not under the influence, such as jumping out of a window or off a building.
- Users could experience a profound sadness or feeling of hopelessness leading to suicidal feelings and/or suicidal actions.
- Psilocybin users could accidently consume a poisonous mushroom that look like psilocybin, which can result in severe illness or death.

Self-Quiz
Ask Yourself...
-
What are the two categories of hallucinogens?
-
How many hallucinogens are derived from plants? What plants are they?
Substance Abuse in Adolescents
Substance abuse and opioid overdose deaths are beginning to affect school systems. In 2017, 2.2 million adolescents between the ages of 12-17 stated they were currently using illicit substances (21).
Brain growth and development, particularly during one’s adolescent years, has been highly studied and reviewed. One area of the brain that is still developing during adolescents is the prefrontal cortex. This area of the brain is responsible for allowing one to assess situations, make decisions, and keep emotions and desires under control (21). Because this area of the brain is still developing, it places adolescents at an increased risk of trying drugs and continuing them (21).
Substance use during one’s adolescent years has the potential to create several long-term negative effects. It is estimated that 90% of individuals with addictions began using substances during their adolescent years (22). There are several factors that can lead to substance use. These risk factors include family history of addiction, mental health concerns, behavioral or impulse control problems, exposure to trauma, and environmental factors (22).
Multiple studies have shown that the science of prevention may affect the probability of later problems (23). The main goal in adolescent substance abuse prevention is to reduce risk factors and overall enhance/reinforce protective factors (23). Depending on the addiction, medication may be used in combination with a form of behavioral therapy or counseling.
There are several types of behavioral therapies:
Cognitive-Behavioral Therapy
Helps individuals recognize, avoid and cope with situations in which they may use drugs.
Contingency Management
Uses positive reinforcement for attending counseling sessions, remaining drug-free, or taking prescribed medications.
Motivational Enhancement Therapy
Focuses on strategies that make the most of an individual’s readiness to change their current behavior and enter treatment.
Family Therapy
Focuses on utilizing the family to address influences on drug patterns and improve overall family function.
Twelve-Step Facilitation
Delivered in 12-week sessions. There are no medical treatments, but allow the individual to social and complementary support.
Follows 12 steps of acceptance, surrender, and active involvement in recovery

Self-Quiz
Ask Yourself...
- How many adolescents stated they had tried illicit substances in 2017?
- What is the estimated percentage of individuals with addictions who began using substances in their adolescent years?
- There are five different forms of behavior therapy listed in this Rhode Island Substance Abuse course, what are they?
Conclusion
Substance abuse in the United States is on the rise, with many hospitals and health care centers seeing an increase in patients. Understanding the different types of substances used, their short- and long-term symptoms, overdose symptoms, and medication options will help prepare you to care for these individuals. It is equally important to understand the behavioral therapy options for those with substance use disorders, and advocate for them while they are in your care.
Alzheimer’s Nursing Care
Introduction
Alzheimer’s disease is a destructive, progressive, and irreversible brain disorder that slowly destroys memory and thinking. Alzheimer’s is the most common cause of dementia in older adults (1). For most people who have Alzheimer’s disease, symptoms first appear in their mid 60’s (1).
Studies suggest more than 5.5 million Americans, most 65 or older, may have dementia caused by Alzheimer’s (1). It is currently listed as the sixth leading cause of death in the United States. It is essential to understand the signs and symptoms of Alzheimer’s dementia and how to manage the care of a patient, family member, or friend suffering from the disease.
Dementia is the loss of cognitive functioning, such as thinking, remembering, reasoning, and behavioral abilities, such as a decreased ability to perform activities of daily living (1). The severity of dementia ranges from mild to severe. Dmentia’s mildest stage often begins with forgetfulness, while its most severe stage consists of complete dependence on others for general activities of daily living (1).
History of Alzheimer’s
Alzheimer’s disease is named after Dr. Alois Alzheimer. In the early 1900s, Dr. Alzheimer noticed changes in the brain tissue of a patient who had died of an unknown mental illness. The patient’s symptoms included memory loss, language problems, and unpredictable behavior.
After her death, her brain was examined and was noted to have abnormal clumps known as amyloid plaques and tangled bundled fibers, known as neurofibrillary or tau tangles (1). These plaques and tangles within the brain are considered some of the main features of Alzheimer’s disease. Another feature includes connections of neurons in the brain. Neurons are a type of nerve cell responsible for sending messages between different parts of the brain and from the brain to other parts of the body (1).
Scientists are continuing to study the complex brain changes involved with the disease of Alzheimer’s. The changes in the brain could begin ten years or more before cognitive problems start to surface.
During this stage of the disease, people affected seem to be symptom-free; however, toxin changes occur within the brain (1). Initial damage in the brain occurs within the hippocampus and entorhinal cortex, which are the parts of the brain that are necessary for memory formation. As the disease progresses, additional aspects of the brain become affected, and overall brain tissue shrinks significantly (1).

Signs and Symptoms & Diagnosis of Alzheimer’s Disease
Memory problems are typically among the first signs of cognitive impairment related to Alzheimer’s disease. Some people with memory problems have Mild Cognitive Impairment (MCI) (2). In this condition, people have more memory problems than usual for their age; however, their symptoms do not interfere with their daily lives.
Older people with MCI are at increased risk of developing Alzheimer’s disease. The first symptoms of Alzheimer’s may vary from person to person. Many people display a decline in non-memory-related aspects of cognition, such as word-finding, visual issues, impaired judgment, or reasoning (2).
Healthcare providers use several methods and tools to determine the diagnosis of Alzheimer’s Dementia. Diagnosis and evaluation involve memory, problem-solving, attention, counting, and language tests. Healthcare providers may perform brain scans, including CVT. MRI or PET is used to rule out other causes of symptoms.
Various tests may be repeated to give doctors information about how memory and cognitive functions change over time. They can help diagnose different causes of memory problems, such as stroke, tumors, Parkinson’s disease, and vascular dementia. Alzheimer’s disease can be diagnosed only after death by linking clinical measures with an examination of brain tissue in an autopsy (3).

Self-Quiz
Ask Yourself...
- Have you experienced a patient in your practice with dementia or Alzheimer’s disease? What did their symptoms look like?
- What standard diagnostic tools do healthcare providers use to diagnose this disease?
- What is the definitive diagnosis of Alzheimer’s disease?
Stages of Disease
Mild Alzheimer’s
People experience significant memory loss and other cognitive problems as the disease progresses. Most people are diagnosed in this stage (1).
- Wandering/getting lost
- Trouble handling money or paying bills
- Repeating questions
- Taking longer to complete basic daily tasks
- Personality/behavioral changes (1)
Moderate Alzheimer’s
In this stage, damage occurs in the area of the brain that controls language, reasoning, sensory processing, and conscious thought (1).
- Memory and confusion worsen.
- Problems recognizing family and friends
- Unable to learn new things
- Trouble with multi-step tasks such as getting dressed
- Trouble coping with situations
- Hallucinations/delusions/paranoia (1)
Severe Alzheimer’s
- Plaques and tangles spread throughout the brain, and brain tissue shrinks significantly.
- Cannot communicate
- Entirely dependent on others for care
- Bedridden – most often as the body shuts down

Self-Quiz
Ask Yourself...
- What are some of the signs and symptoms that differentiate each stage of Alzheimer’s disease?
- A person is in what stage of Alzheimer’s disease when they struggle to recognize family members and friends?
Prevention
Many aging patients worry about developing Alzheimer’s disease and dementia. Especially if they have had a family member who suffered from the disease, patients may worry about genetic risk. Although there have been many ongoing studies on the prevention of the disease, nothing has been proven to prevent or delay dementia caused by Alzheimer’s disease (2).
More research suggests that women are more likely to develop dementia and Alzheimer’s compared to men. Further research is needed to determine the role between genetics, sex, and Alzheimer’s risk (4).
A review led by experts from the National Academies of Sciences, Engineering, and Medicine found encouraging yet inconclusive evidence for three types of interventions related to ways to prevent or delay Alzheimer’s Dementia or age-related cognitive decline (2):
- Increased physical activity
- Blood pressure control
- Cognitive training

Treatment of the Disease
Alzheimer’s disease is complex and is continuously being studied. Current treatment approaches focus on helping people maintain their mental function, manage behavioral symptoms, and lower the severity of symptoms. The FDA has approved several prescription drugs to treat those diagnosed with Alzheimer’s (3).
Treating symptoms of Alzheimer’s can provide patients with comfort, dignity, and independence for a more significant amount of time while simultaneously assisting their caregivers. The approved medications are most beneficial in the early or middle stages of the disease (3).
Cholinesterase inhibitors are prescribed for mild to moderate Alzheimer’s disease; they may help to reduce symptoms. Medications include Rzadyne®, Exelon®, and Aricept® (3). Scientists do not fully understand how cholinesterase inhibitors work to treat the disease; however, research indicates that they prevent acetylcholine breakdown. Acetylcholine is a brain chemical believed to help memory and thinking (3).
For those suffering from moderate to severe Alzheimer’s disease, a medication known as Namenda®, which is an N-methyl D-aspartate (NMDA) antagonist, can be prescribed. This drug helps to decrease symptoms, allowing some people to maintain certain essential daily functions slightly longer than they would without medication (3).
For example, this medication could help a person in the later stage of the disease maintain their ability to use the bathroom independently for several more months, benefiting the patient and the caregiver (3). This drug works by regulating glutamate, an essential chemical in the brain. When it is produced in large amounts, glutamate may lead to brain cell death. Because NMDA antagonists work differently from cholinesterase inhibitors, these rugs can be prescribed in combination (3).

Self-Quiz
Ask Yourself...
- Is there a cure for this disease?
- What are some of the treatment forms that have been used for the management of Alzheimer’s disease?
- Can medications be used in conjunction with one another to treat the disease?
Medications to be Used with Caution in those Diagnosed with Alzheimer’s
Some medications, such as sleep aids, anxiety medications, anticonvulsants, and antipsychotics, should only be taken by a patient diagnosed with Alzheimer’s after the prescriber has explained the risks and side effects of the medications (3).
Sleep aids: They help people get to sleep and stay asleep. People with Alzheimer’s should not take these drugs regularly because they could make the person more confused and at a higher risk for falls.
Anti-anxiety: These treat agitation and can cause sleepiness, dizziness, falls, and confusion (3).
Anticonvulsants: These are used to treat severe aggression and have possible side effects of mood changes, confusion, drowsiness, and loss of balance.
Antipsychotics: they are used to treat paranoia, hallucinations, agitation, and aggression. Side effects can include the risk of death in older people with dementia. They would only be given when the provider agrees the symptoms are severe enough to justify the risk (3).
Caregiving
Coping with Agitation and Aggression
People with Alzheimer’s disease may become agitated or aggressive as the disease progresses. Agitation causes restlessness and causes someone to be unable to settle down. It may also cause pacing, sleeplessness, or aggression (5). As a caregiver, it is essential to remember that agitation and aggression are usually happening for reasons such as pain, depression, stress, lack of sleep, constipation, soiled underwear, a sudden change in routine, loneliness, and the interaction of medications (5). Look for the signs of aggression and agitation. It is helpful to prevent problems before they happen.
Ways to cope with agitation and aggression (5):
- Reassure the person. Speak calmly. Listen to concerns and frustrations.
- Allow the person to keep as much control as possible.
- Build in quiet times along with activities.
- Keep a routine.
- Try gently touching, soothing music, reading, or walks.
- Reduce noise and clutter.
- Distract with snacks, objects, or activities.
Common Medical Problems
In addition to the symptoms of Alzheimer’s disease, a person with Alzheimer’s may have other medical conditions over time. These additional health conditions can cause confusion and behavior changes. The person may be unable to communicate with you about their circumstances. As a caregiver, it is essential to watch for various signs of illness and know when to seek medical attention for the person being cared for (6).
Fever
Fever could indicate potential infection, dehydration, heatstroke, or constipation (6).
Flu and Pneumonia
These are easily transmissible. Patients 65 years or older should get the flu and Pneumonia shot each year. Flu and Pneumonia may cause fever, chills, aches, vomiting, coughing, or trouble breathing (6).
Falls
As the disease progresses, the person may have trouble with balance and ambulation. They may also have changes in depth perception. To reduce the chance of falls, clean up clutter, remove throw rugs, use armchairs, and use good lighting inside (6).
Dehydration
It is important to remember to ensure the person gets enough fluid. Signs of dehydration include dry mouth, dizziness, hallucinations, and rapid heart rate (6).
Wandering
Many people with Alzheimer’s disease wander away from their homes or caregivers. As the caregiver, it is essential to know how to limit wandering and prevent the person from becoming lost (7).
Steps to follow before a person wanders (7)
- Ensure the person carries an ID or wears a medical bracelet.
- Consider enrolling the person in the Medic Alert® + Alzheimer’s Association Safe Return Program®.
- Alert neighbors and local police that the person tends to wander and ask them to alert you immediately if they are seen alone.
- Place labels on garments to aid in identification.
Tips to Prevent Wandering (7)
- Keep doors locked. Consider a key or deadbolt.
- Use loosely fitting doorknob covers or safety devices.
- Place STOP, DO NOT ENTER< or CLOSED signs on doors.
- Divert the attention of the person away from using the door.
- Install a door chime that will alert when the door is opened.
- Keep shoes, keys, suitcases, coats, and hats out of sight.
- Make sure not to leave a person who has a history of wandering unattended.

Self-Quiz
Ask Yourself...
- What are the basic implementations you can make as a caregiver to make handling confusion and aggression easier in a patient with Alzheimer’s?
- What are some of the types of medical problems that people with Alzheimer’s may face, and how can they be monitored for prevention?
Conclusion
Alzheimer’s is a sad, debilitating, progressive disease that robs patients of their lives and dignity. As research continues on the causes, treatment, and prevention of the disease, healthcare workers and caregivers need to know the signs and symptoms of a patient with Alzheimer’s disease and potential coping mechanisms and management strategies of the disease. More information on the disease is available through several various resources, including:
Family Caregiver Alliance
800-445-8106
NIA Alzheimer’s and Related Dementias Education and Referral Center
800-438-4380
Negative Pressure Wound Therapy (Wound Vac)
Introduction
Negative pressure wound therapy (NPWT), also known as a wound vac, can be a powerful tool in combatting acute and chronic wounds. It relies on generating a negative pressure on the surface of a difficult wound to promote wound healing.
The goal of this course is to develop an understanding of mechanism of action of NPWT, discuss appropriate nursing assessment of these wounds, evaluate adjunct treatment options and troubleshooting support tips.
We will review basic concepts of the integumentary system and the normal wound healing process to support the rationale of NPWT.
Definition
Negative pressure wound therapy (NPWT) is the application of sub-atmospheric pressure to help reduce inflammatory exudate and promote granulation tissue in an effort to enhance wound healing (4). The idea of applying negative pressure therapy is that once the pressure is lower around the wound, the gentle vacuum suction can lift fluid and debris away and give the wound a fighting chance to heal naturally.
NPWT has a long and interesting history. The idea of suctioning fluid from wounds as therapy is not a new concept. The process was first called “cupping” and was described in Ebers Papyrus around 500 BC; historians tell us that a form of wound suction was used around 1000 BC in China, 600 BC in Babylon and Assyria, and in 400 BC by Greeks who heated copper bowls over wounds to remove blood and fluids (5).
Modern medicine has built upon a very old concept. Thankfully, nurses have a slightly easier tool in NPWT devices than heating copper bowls.

Self Quiz
Ask yourself...
- Can you name the various methods of wound treatments that you have encountered?
- Do you recognize how negative pressure can create suction?
Indications for Use
Negative pressure wound therapy is widely used for the management of both acute and chronic wounds. This therapy is helpful for a broad range of wounds, from pressure ulcers to closed surgical incisions.
The system is now implemented routinely for open wounds, such as open fractures, fasciotomies, diabetic foot ulcers, and infected wounds. Delayed wound healing and difficult wounds are seen more commonly in elderly patients and those with comorbidities (1).
It’s important to review the basic anatomy of our integumentary system, types of wounds, and barriers to healing to understand the usefulness of NPWT.
Basic Anatomy of Integumentary System
Our integumentary system is considered the body’s largest organ. Our skin acts as a shield against heat, light, bacteria, infection, and injury. Other functions include body temperature regulation, storage of water and fat, sensory function, prevention of water loss, and a basic storage compartment for the organs (6).
The skin is made up of 3 layers. Each layer has unique functions:
- Epidermis
- Dermis
- Subcutaneous fat layer (hypodermis)
The epidermis is the thin outer layer of our skin, it contains squamous cells, basal cells, and melanocytes (gives skin its color). The dermis is the middle layer of skin, it contains blood vessels, hair follicles, sweat glands, nerves, lymph vessels, fibroblasts, and sebaceous glands (6). It is important to remember that the dermis contains nerves and nerve receptors.
The subcutaneous fat layer is the deepest layer of skin and is made up of a network of collagen and fat cells; this layer conserves the body's heat and protects the body from injury by acting as a shock absorber (6).

This design was created on Canva.com on September 28, 2023. It is copyrighted by Abbie Schmitt, RN, MSN and may not be reproduced without permission from Nursing CE Central.
Types of Wounds
Negative pressure wound therapy is primarily used to treat complex wounds that are non-healing or at risk of non-healing. It is also indicated for acute wounds when the wound cannot be closed due to the risk of infection, active infection, skin tension, or swelling (7).
Closure or skin grafting of acute wounds, such as open fractures or burns, are at high risk for infection due to microorganisms becoming trapped in the soft tissue leading to abscess development.
Examples of possible wounds to apply NPWT (1):
- Diabetic foot ulcers
- Bed sores
- Skin graft fixation
- Burns
- Crush injuries
- Sternal/abdominal wound dehiscence
- Fasciotomy wounds
- Animal bites
- Frostbite
Barriers to Healing
Age
- Increased risk of tearing and shearing due to thinning of epidermis and decrease in elastin
- Phases of healing are prolonged
- Increased risk of dehiscence as the dermis has slower contractility
- Skin more susceptible to bacterial growth and infections as pH becomes more neutral with age
Co-morbidities
- Cardiopulmonary Disease
- Oxygen-transport pathways are affected
- O2 necessary for wound healing
- Diabetes Mellitus
- High glycemic levels predispose patients to infection
- Microvasculature and neuropathic components of DM increase the risk for impaired healing
- Poor glycemic control can increase the risk of ulceration and delayed healing
- Immune-suppressing conditions (Cancer, HIV, immunosuppressive therapy, immunosuppression syndrome)
- Inflammatory phase (immunology) is impaired
- Increased risk for infection
Impaired Perfusion and Oxygenation
- Peripheral Vascular Impairment
- Proper perfusion is required for growth of new tissue and immunological responses of the tissue.
- Arterial insufficiency (blood flow to extremities) leads to necrosis or lack of response to edema.
Neurological Impairment
- Peripheral neuropathy
- Complication related to DM, alcoholism, chemotherapy
- Loss of neuronal signaling and transmission
- Loss of the sensory ability to recognize and react to sensations of touch, pressure, temperature, pain. Example: patient leaving foot on hot surface because there was no pain sensation, leading to burn wound.
- Spinal cord injury

Self Quiz
Ask yourself...
- Are you familiar with the layers and components that make up the integumentary system?
- Have you ever cared for a patient with a chronic wound?
- What are some ways the elderly population is at higher risk for prolonged wound healing?
Mechanism of Action
The mechanism of action is dependent on applying negative pressure, which is below atmospheric pressure, to the wound. This pressure allows the gentle vacuum suction to lift fluid and exudate away from the wound to enhance healing (3).
The vacuum is gentle because powerful suction would remove newly formed tissue as well. The mechanism of action is not only in removing fluid and debris from the tissue, but the pressure causes stimulation of the growth of granulation tissue at a macroscopic and microscopic level.
The porous foam shrinks in size with the application of negative pressure and exerts strain on the wound bed, which leads to macro- and micro-deformation of the wound (3). Microdeformation is simply a term used to describe microscopic tissue cell reactions. This reaction can be compared to a battery jump-start of a car; the stimulation causes the battery to engage.
NPWT systems consist of a sterile foam sponge, a semi-occlusive adhesive cover, a fluid collection system or canister, and a suction pump (1). The foam sponge is applied to the wound and covered. A fenestrated tube is embedded in the foam and the wound is sealed with adhesive tape to make it airtight, and the machine delivers continuous or intermittent suction, ranging from 50 to 125 mmHg (1).

This design was created on Canva.com on October 1, 2023. It is copyrighted by Abbie Schmitt, RN, MSN and may not be reproduced without permission from Nursing CE Central.
Proper application of the NPWT is important for the mechanism of action to be effective. Research supports that NPWT is effective at creating a stable wound environment, reduces inflammation and bacterial load, improves tissue perfusion, and stimulates granulation tissue and angiogenesis (1).
Imagine you want to plant a garden in a swampy location, you would first need to divert the water and algae from the land, cover it with a greenhouse with consistent heat and pressure, and cultivate the soil for optimal growth. Similarly, NPWT creates the most ideal conditions possible for tissue regeneration.

Self Quiz
Ask yourself...
- Can you name the components of NPWT?
- Have you ever applied a wound vac dressing?
- Are you familiar with the other semipermeable materials that serve as a filter?
Contraindications
NPWT would be contraindicated for the following:
- Wounds involving untreated osteomyelitis.
- Wounds that have exposed blood vessel
- Wounds with exposed nerves, anastomotic sites, or organs
- Wounds including open joint capsules
- Malignant wounds
- Wounds with necrotic tissue; it is recommended to excise first
The following wounds could benefit from NPWT, but caution should be given (5):
- Wounds with visible fistula
- Wounds with exposed bone or tendon
- The bone or tendon should be isolated from direct pressure
- Patient with clotting disorders or that are taking anticoagulants, due to an increased risk of bleeding.
- Compromised microvascular blood flow to the wound bed.

Self Quiz
Ask yourself...
- Can you think of reasons a malignant, cancerous wound should not have NPWT?
- Have you ever dressed a wound prior to or following debridement?
Assessment
A focused assessment should be done for patients with NPWT devices in place, both on the machine settings, the dressing, and the wound itself. Thorough documentation of the wound is essential to see the progression of wound healing.
Suction Device Settings:
- Continuous or intermittent
- Pressure Setting: Range of pressure settings from -40mmHg to -200mmHg, which can be tailored for different types of wounds (7). This is set by the medical provider.
Laboratory assessment is meaningful in wound care. Labs can be used to assess oxygenation or indicators of infection (6).
Dressing Assessment
The appearance of the NPWT and dressing should be clean, dry, intact, and sealed. The tubing should not be twisted or kinked, and the clear adhesive dressing should not be wrinkled or overlapping. Please see below an example of the appropriate appearance of a dressing.
Wound Assessment:
- Anatomic location
- Type of wound
- Degree of tissue damage
- Description of wound bed
- Wound size
- Wound edges and surrounding skin
- Signs of infection
- Pain
Anatomical Location
Anatomical terms and numbering should be used to make sure the location of each wound is documented. Patients often have more than one wound, so the treatment needs to be specified for each wound.
Wound Base
Assess the color of the wound base. Healthy granulation tissue appears pink and moist due to the new capillary formation. The appearance of slough (yellow) or eschar (black) in the wound base should be documented and communicated to the health care provider (1).
This tissue may need to be removed to optimize healing. If any discoloration or duskiness of the wound bed or wound edges are identified, the suction should initially be reduced or switched off (7).
Type and Amount of Exudate
Assess the color, thickness, and amount of exudate (drainage) The amount of drainage from wounds is categorized as scant, small/minimal, moderate, or large/copious.
Terms are used when describing exudate: sanguineous, serous, serosanguinous, and purulent (6).
- Sanguineous: fresh bleeding
- Serous: Clear, thin, watery plasma
- Serosanguinous: Serous drainage with small amounts of blood noted
- Purulent: Thick and opaque. The color can be tan, yellow, green, or brown. This is an abnormal finding and should be reported to a physician or wound care provider.
Wound Size
Wounds should be measured on admission, wound vac dressing changes, or as needed for abnormal events. Many healthcare facilities use disposable, clear plastic measurement tools to measure the area of a wound.
Consistent measurement is vital to the assessment of wound healing.
- Measure the greatest length, width, and depth of the wound in centimeters
- Examples of wound classification tools:
- NPUAP staging system for pressure injuries
- Payne-Martin classification system for skin tears
- CEAP (clinical, etiologic, anatomic, and pathophysiology) system for venous ulcers
Tunneling or Undermining
Tunneling is when a wound has moved underneath the skin, making a “tunnel.” The depth of tunneling can be measured by gently inserting a sterile, cotton-tipped applicator into the tunnel and noting the length from the wound base to the end of the tract (7). Undermining occurs when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound’s edge.
Healing Process
It is important to recognize the entire process of normal wound healing. There are four phases of wound healing: hemostasis, inflammatory, proliferative, and maturation (6).
Hemostasis begins immediately after injury, involving platelet aggregation and activation of clotting factor (6). A platelet “plug” is formed as fibrinogen converts to fibrin and binds to itself. Vasoconstriction occurs at this time, decreasing blood loss and allowing clot formation.
The inflammatory phase begins right after the injury and the injured blood vessels leak and cause localized swelling. The swelling, warmth, pain, and redness present during this stage of wound healing are related to the release of white blood cells, growth factors, nutrients, and enzymes to help control bleeding and prevent infection (6).
The proliferative phase of wound healing involves “rebuilding” with new tissue made up of collagen and extracellular matrix; granulation tissue is built stronger with proper oxygen and nutrients.
Key nursing knowledge: Dark granulation tissue can indicate infection, ischemia, or poor perfusion. The maturation phase of wound healing is when collagen is remodeled, aligns along tension lines, water is reabsorbed so the collagen fibers can lie closer together and cross-link, and the wound fully closes (1).
There are three types of wound healing: primary intention, secondary intention, and tertiary intention.
Primary intention means that the wound healing is supported by sutures, staples, glue, or otherwise closed so the wound heals beneath the closure (6).
Secondary intention must happen when the edges of a wound cannot be approximated, or “brought together,” so the wound heals with the production of granulation tissue from the bottom up (6).
Wounds that heal by secondary intention are at higher risk for infection, so contamination prevention is essential. Pressure ulcers are an example of wounds that heal by secondary intention.
Tertiary intention refers to a wound that needs to remain open, often due to severe infection. Wounds with secondary and tertiary intention have longer healing times (2).

Alternatives when NPWT fails
- Hyperbaric Oxygen Therapy (HBOT):
- HBOT is a treatment in which the wound is exposed to pure oxygen in a pressurized chamber to enhance wound healing (3).
- Bioengineered Tissue:
- Skin grafting or bioengineered tissue to promote tissue growth and healing.
- Skin grafts are considered as a treatment option if a wound is so large that it can’t close on its own. In this procedure, skin is taken from another part of your body – usually your thigh – and transplanted onto the wound (2).
- Some grafts are made from human cell products and synthetic materials. Studies have shown that these increase the chances of poorly healing venous leg ulcers closing faster. (2)
- Electrical Stimulation Therapy:
- Electrical stimulation therapy applies electrical currents to stimulate wound healing and tissue generation (4). It may be used to treat chronic wounds or pressure ulcers.

Self Quiz
Ask yourself...
- Have you ever cared for a patient with a wound that was unable to be stitched or sutured?
- Can you describe the importance of thorough, descriptive documentation of multiple wounds?
- Can you think of barriers to the normal wound healing process?
Adjunct Treatment Options
When selecting an adjunctive therapy for wound management, the patient's medical history, overall health, co-morbidities, ambulation status, psychosocial aspects, environmental factors, and the specific needs of the wound should all be considered. Each patient is unique, and an individualized care plan is the goal.
Treatment of the underlying contributing disorder will be essential. For example, a patient with uncontrolled diabetes that has led to poor circulation can benefit from glycemic control.
Take a look at the larger, holistic picture. It can be helpful for the healthcare team to create a concept map of problems that contribute to the wound.
Topical Agents and Dressings
Various creams, ointments, or dressings can promote wound healing and prevent infection. One example is silver-based products, which are commonly used in reducing bacterial burden and treating wound infection (4).
Nutrition Therapy for Wound Healing
Patients with wounds would benefit from nutrition consultation and ongoing support.
Nutrients from foods help the body build and repair tissue and fight infection. An increase in calories and protein is important, as well as blood sugar control for diabetics.
Vitamins C, D, B-6, B-12, folate, and others aid in repairing tissues (6). Minerals such as iron, magnesium, calcium, zinc, and others support the cardiovascular system making sure cells have enough oxygen, the nervous system, and immunological function (6).
Compression Therapy
Compression therapy uses pressure to reduce swelling and improve blood flow to the wound. There are common compression devices or stockings available. It is frequently used to treat venous leg ulcers (6).
Hyperbaric Oxygen Therapy (HBOT)
HBOT can also be used as an adjunct treatment in which the patient breathes pure oxygen in a pressurized chamber to increase the amount of oxygen in the blood, which enhances wound healing (3).

Self Quiz
Ask yourself...
- Have you ever provided patient education on how nutrition impacts the immune system and wound healing?
Troubleshooting Tips
You may encounter complications with the wound dressing or the wound vac equipment. The most common complications associated with NPWT are pain, bleeding, and infection (7).
The wound therapy relies on an adequate seal similar to a regular vacuum, so a loss of suction can result in ineffective treatment. If loss of seal occurs, the nurse should assess the seal around the wound dressing and note if the transparent adhesive sealant tape has either been misapplied or has come off due to poor contact with the underlying skin.
A loss of suction could also result from incorrect placement of the suction drain tube, loss of battery power, blockage of the suction drain tube, or if the suction device is full of output (7). Sometimes the location of the wound leads to difficulty in keeping the dressing seal in place; for example, the abdomen or near joints, so movement can misplace the dressing and break the seal. Patient education is key to maintaining proper suction.
Troubleshooting Tips:
- Confirm the machine is on and set to the appropriate negative pressure.
- Make sure the foam is collapsed and the NPWT device is maintaining the prescribed therapy and pressure.
- Assess the negative pressure seal and check for leaks.
- Check for kinks in the tubing and make sure all clamps are open.
- Avoid getting the machine wet.
- Assess the drainage chamber to make sure it is filling correctly and does not need changing.
- Address alarm issues:
- Canister may be full
- Leak in the system
- Low/dead Battery
- The device should not be turned off for more than two hours without ordered discontinuation.
- If the device is off, apply a moist dressing and notify the provider immediately.

Self Quiz
Ask yourself...
- Can you name reasons the NPWT device may sound an alarm?
- Can you think of barriers to proper suction? (ex: kinks in tubing, full canister, etc.)
Case Study
Mr. Smith is a 59-year-old male presented to his primary care provider and referred to general surgery; diagnosed with lymphedema and multiple, copiously draining ulcerations on the left lower extremity.
The patient presented with lymphedema and multiple ulcerations on the left lower extremity with copious amounts of drainage. This is an ongoing, worsening issue for over 8 months and has failed to respond to compression, foam dressings, or hydrocolloid dressing.
The hospitalist has ordered surgical consultation, who scheduled debridement of the wounds and application of a wound vac following the procedure; Negative pressure wound therapy (NPWT) orders in place.
CHIEF COMPLAINT: "The sores on my feet are draining more and I can no longer go to work because my boots do not fit on my foot.” He also reports a loss of appetite, chills, and loss of sensation to his left lower extremity.
HISTORY OF PRESENT ILLNESS: Patient is a 59-year-old truck driver who has previous medical history of DM Type II, hypertension requiring use of anti-hypertensive medication, and hyperlipidemia (non-compliant with medication regimen). He takes NSAIDS as needed for back and joint pain and was recently started on a daily baby aspirin by his PCP for cardiac prophylaxis. He denies alcohol intake. He reports smoking a pack of cigarettes per day.
PHYSICAL EXAMINATION: Examination reveals an alert and oriented 59-YO male. He appears anxious and irritated. Vital sips are as follows. Blood Pressure 155/90 mmHg, Heart Rate 120/min - HR Thready - Respiratory Rate - 20 /minute; Temperature 98.0
ENT/SKIN: Facial pallor and cool, moist skin are noted. No telangiectasia of the lips or oral cavity is noted. Wound: 3 cm x 2 cm x 1 cm wound to lateral LLE. Wound base is dark red with yellow-green drainage present. Removed 4 x 4 dressing has a 5 cm diameter ring of drainage present. The surrounding skin is red, warm, tender to palpation, and with a dusky appearance to the entire LLE.
CHEST: Lungs are clear to auscultation and percussion. The cardiac exam reveals a regular rhythm with an S4. No murmur is appreciated. Peripheral pulses are present but are rapid and weak. A positive Stemmer sign was noted and palpable pedal pulses with mild symptoms of venous insufficiency were noted.
ABDOMEN/RECTUM: The abdomen reveals a rounded abdomen. Bowel sounds are present.

Self Quiz
Ask yourself...
- Discuss abnormal findings noted during History & Physical Examination.
- Evaluate additional data to obtain possible diagnostic testing, treatment, nursing interventions, and care plans.
- Discuss how the patient’s comorbidities may be attributed to prolonged wound healing.
- What suction settings would the nurse expect to be ordered?
Conclusion
Hopefully, upon completion of this course, you feel empowered and curious about the use of negative pressure wound therapy (NPWT). Wound vacs can be a powerful tool in combatting acute and chronic wounds, it is a well-documented concept throughout history.
The nurse should be knowledgeable on the integumentary system makeup and types of wounds this therapy is indicated for. The mechanism of action of NPWT is critical knowledge when assessing the healing of a wound. Adjunct treatment options and troubleshooting support tips are also meaningful in the care of patients with NPWT.
Nutritional Interventions to Promote Wound Healing
Introduction
The medical field is an ever-evolving and constantly changing arena. Advances in technology and an increased understanding of how the body works have produced newer and better procedures and techniques in healing. These initiatives, as innovative as they may be, still depend on the body’s ability to heal itself as the foundation of the recovery process.
In turn, the body needs proper nutrition to support the healing process within itself. Nutrition is often overlooked by nurses even though it is arguably the most critical aspect of physical healing.
Factors That Impact Wound Healing
Wound healing is a complex process. There are a myriad of factors that impact the body’s ability to heal and recover from an injury. Comorbidities, genetic disorders, medications, and, in some cases, disease treatments (chemotherapy, radiation, steroids, etc.) can all have the potential to slow, change, or interfere with normal wound healing (2). For this course, we will discuss a few of the more common factors that nurses will undoubtedly come across during their practice.
Diabetes
It is estimated that this growing, global disease will impact forty million people by the year 2030. It has been proven that diabetes is responsible for more than one hundred changes in wound healing.
These alterations have been seen across all four phases of wound healing. Platelet activation, epithelialization, collagen deposition, and granulation tissue formation are among the alterations that take place with diabetes. Worsening renal function/failure and peripheral vascular disease as a result of diabetes also affect the wound-healing process (2).
Renal Failure
Though most patients who have chronic kidney disease or renal failure also have multiple comorbidities that cause the renal problem, renal failure does, independently, bring a risk of diminished wound healing. Tissue edema, delayed granulation, chronic inflammation, and decreased vessel formation are all ways that renal failure impacts wound healing.
Hemodialysis, a life-sustaining treatment of chronic renal failure, adds fuel to the fire when it comes to risks of diminished wound healing. Protein and water-soluble vitamins and nutrients are lost through the dialysis process. This includes zinc and iron and will lead to deficiencies in these needed nutrients. Further, patients on hemodialysis and patients who receive a kidney transplant as treatment for renal failure are both at higher risk for developing infections (2).

Smoking
Smoking causes multiple alterations within the body at the molecular level that affect normal wound healing. Vasoconstriction caused by smoking worsens wound ischemia. The highly documented negative impact that smoking has on wound healing has led physicians to decline some elective surgeries due to the risk of poor wound healing (2).
Infection
It is not fully understood how infection alters wound healing. It is believed to be a multifactorial process that has a range of properties that can be progressive in nature; infection-necrosis-sepsis-death. The bacteria create an environment where the collagen that repairs the injured tissue is destroyed (2).
Obesity
Obesity complicates virtually every disease process including normal wound healing. Wound healing complications due to obesity include increased rates of infection, hematomas, and dehiscence. Local hypoxia is also a complication that impacts wound healing (2).
Age
Aging also has an impact on wound healing. During the aging process, the skin loses elasticity, thickness, and water content. There is also a decrease in the skin’s blood vessels as it ages, reducing the capacity for oxygenation and nutrients. Wound closure becomes slower with aging; by age forty, the amount of time for an identical wound to heal doubles from age twenty. After the age of fifty, dermal collagen decreases by one percent per year (2).
Malnutrition
Malnutrition or undernutrition has a variety of effects on wound healing. Good nutrition is essential for proper wound healing and the overall recovery of the body after an injury.
Malnutrition can lead to the loss of immune function which will affect the body’s response to infection. With malnutrition, the skin becomes thin and frail thus more apt to develop wounds. Pressure wounds are also more likely as fat deposits over pressure points become depleted. The lack of energy during malnutrition leads to immobility, increasing the possibility of wounds. Collagen synthesis is also decreased (5).

Self Quiz
Ask yourself...
- Name three factors that can affect wound healing.
- How does age and aging impact wound healing?
- What are two ways that malnutrition impacts wound healing?
Phases of Wound Healing
Once again, wound healing is a complex process. From a simple pin prick to a stage-four decubitus ulcer, the wound healing process itself remains the same. The body will go through the four phases of wound healing to repair the damage.
Hemostasis
The first phase of wound healing is hemostasis. Whether by surgery or trauma, the body attempts to achieve hemostasis at the time of the injury. The intrinsic and extrinsic coagulation cascades are activated by the body.
Vasoconstriction takes place while platelet aggregation occurs to form a fibrin clot. This is all in an effort of the body to stop the bleeding to bring about hemostasis. As the platelets arrive at the site of injury, cytokines and growth factors are released by the platelets to initiate the inflammation process (3) (4) (5).
Inflammation
Inflammation is the second phase of wound healing. It starts once hemostasis has been re-established. During this phase, the previous vasoconstriction reverses and the vessels dilate.
This brings blood to the injury site along with neutrophils, macrophages, monocytes, and other inflammatory cells. Phagocytosis is initiated and the wound is cleansed by the removal of bacteria. The wound site will swell and there may be some restrictions in mobility to the affected area (3) (5).
Proliferation
Phase three is proliferation. In this phase, rebuilding of the wounded tissue begins. The number of fibroblasts increases and begins to build a collagen network and prepare the wound base for new granulation tissue.
At the same time, new blood vessels are created; a highway for oxygen and nutrients to be supplied to the site. By the end of this phase, the foundation will have been laid for full epithelialization (3) (5).
Remodeling
The final phase of wound healing is remodeling. Epithelialization is in full swing once granulation tissue has filled the wound. This process stimulates skin integrity restoration.
Scar tissue is formed as proteins such as collagen and elastin along with keratinocytes are produced. The wound closes and begins to strengthen and appear “normal”; it may take a couple of years for the site to return to its fully functional pre-injured status (3).

Self Quiz
Ask yourself...
- How many phases of wound healing are there?
- Name all the phases of wound healing in order.
- What happens during the proliferation phase of wound healing?
How Does Nutrition Impact Healing?
Nutrition is, perhaps, the most important underlying aspect of wound healing. The mechanism of wound healing and the role nutrition plays in that process is very complex.
Adding nutritional interventions to the wound healing care plan is generally low cost and will increase the probability of a full recovery. Nutrition is essential for all phases of the healing process. It is the foundation of wound healing.
The malnourished patient will have difficulty progressing through the wound healing phases. Proper nutrition will also help prevent wounds such as pressure ulcers from developing in the first place.
Understanding which nutrients are needed through the phases of wound healing will help to devise a nutritional plan of care. Energy is required in all the phases of wound healing and is only made possible through proper nutrition (3).

Self Quiz
Ask yourself...
- In what phase of wound healing is proper nutrition essential?
Common Deficiencies
Nutrients and proteins are the building blocks of life. They are needed for growth, maintenance, and healing of the body. Many types of nutrient deficiencies greatly impact the healing process. Here, we will discuss some of the more common nutrient deficiencies.
Iron
Iron plays a key role in the synthesis of hemoglobin. Hemoglobin delivers oxygen throughout the body; oxygen is required through all phases of wound healing. Iron deficiencies can lead to anemia and decreased tissue perfusion. An iron deficiency will also affect protein synthesis, macrophage function, and overall wound strength (3) (6).
Vitamin A
When it comes to wound healing, vitamin A quickens collagen synthesis and the overall inflammatory phase. A deficiency in vitamin A decreases collagen production, epithelization, and tissue granulation (9).
Vitamin B
There are eight vitamins included in the vitamin B complex. Each of the eight vitamins has its own daily recommended intake. Vitamin B promotes cell proliferation and promotes normal metabolism. In the presence of a wound, some dietitians promote doubling the daily recommended intake of the B vitamins (3).
Vitamin C
Vitamin C (ascorbic acid) assists with iron absorption. It is also essential in the process of collagen formation. Without vitamin C, the immune response cannot take place as needed. There are many sources of vitamin C readily available for everyday consumption (6).
Zinc
Zinc is used through all phases of the wound-healing process. It is used to initiate and modulate enzyme function throughout the wound healing phases. It affects immunity and assists in fibroblast proliferation and collagen production. It is also needed for granulation tissue formation (5) (6).
Amino Acids
Protein and amino acids are another set of nutrients that are highly essential in wound healing. The blood’s most abundant amino acid, glutamine, provides the body’s preferred energy source, glucose. Increased levels of glutamine have been shown to help with wound strength and increase the levels of mature collagen.
Generally, the body is able to produce enough glutamine for regular function. In times of stress on the body, such as a wound, glutamine is sought out in the diet. Arginine assists in modulating the collagen deposits, increases new vessel formation, and aids in wound contraction (3).

Self Quiz
Ask yourself...
- Name three common nutrient deficiencies that the nurse may encounter.
- What are two amino acids that play key roles in wound healing?
- An iron deficiency can lead to what issues?
- Which phases of wound healing require zinc to complete the phase?
Special Considerations
Tube Feedings
Patients who use tube feedings or enteral feedings are in a unique situation when it comes to wound healing and nutrition. Once a proper nutrition assessment has been performed, a tailor-made nutrition-rich diet can be formulated and administered directly into the gut.
Studies have shown that different formulas with supplemental nutrients have increased the ability of the body to heal faster than those without supplements. With tube feedings, patients don’t need to prefer the taste of one formula over another as it is delivered through the tube.
The amount of formula can also be adjusted as the patient’s needs change. Though some formulas may have side effects such as diarrhea, the overall benefits usually outweigh such side effects (8).

Self Quiz
Ask yourself...
-
What considerations are there for patients with tube feedings?
-
What is a pitfall when using tube feedings to deliver full nutrition?
Chronic and Terminal Illness
Autoimmune, inflammatory, and cancers are among the chronic and terminal diseases that are under special consideration when it comes to wound healing. These types of diseases can interrupt the immune/inflammatory response of the body thus prolonging the phases of wound healing.
When a wound develops on a patient who is immunocompromised, there is a higher incidence of wound infection which will delay wound healing. In many of these diseases, there may be circulatory issues that decrease the body’s ability to provide the affected area with nutrient-rich blood.
Chronic illnesses often decrease the patient’s energy levels. This can lead to immobility and increases the risk of wounds developing.
Further, for many of these types of issues, the treatment itself can have adverse effects on wound healing. Chemotherapy, radiation therapy, and immunosuppressants all decrease the body’s ability to heal and increase the rates of infection in wounds (2).

Self Quiz
Ask yourself...
- What are three types of chronic or terminal diseases?
- What issue is an immunocompromised patient at risk for?
- What are two treatments for chronic illness that can affect wound healing?
Supplements
Nutritional supplements have been shown to improve wound healing and recovery outcomes. It is important that the supplements are given under the supervision of a provider as too much of some nutrients can have a detrimental effect on wound healing.
A proper nutrition screening should be performed on all patients with wounds so that the nutrition plan can be tailored to the individual patient. These improvements to wound healing with nutritional supplementation differ based on the type of wound and the overall health of the patient.
The patient should be monitored and reassessed regularly by a dietitian. Again, there is no cookie-cutter supplement regimen.
Another factor to consider with supplements is the ease of following the supplement regimen. Hard to swallow pills or foul-tasting food/liquids may have a negative impact on the patient’s ability to adhere to the supplement regimen.
Allowing the patient to choose (with the input of the provider) the method of supplement delivery along with a choice of flavors will help increase compliance with the prescribed regimen (1).

Self Quiz
Ask yourself...
- What should be done prior to starting dietary supplements?
- Who should assess and reassess a patient’s dietary status?
- Why is the method of supplement delivery important?
Patient Education
Throughout the entire wound healing process, patient education is a must. Not only is it important so that the patient can make an informed decision about their care, but the patient should understand what is going on with their bodies.
Education fuels compliance. A comprehensive nutrition assessment will not only provide a baseline of the patient’s nutritional status but will also help identify gaps in the patient’s understanding.
This is where the education can be focused to best help the patient meet their wound healing goals. Education must include which foods contain which nutrients, the amount of these foods to eat, and which foods will interact with the absorption processes of the nutrients.
Discussing normal daily requirements and the requirements needed during wound healing is also needed (1).

Self Quiz
Ask yourself...
- Why is education important when discussing nutrition and wound healing?
Conclusion
Nutrition plays a key role in wound healing. There are many factors that affect the body’s ability to acquire and use the needed nutrients. One of the most important considerations that we as healthcare providers need to put into practice is determining a patient’s nutritional status.
A nutritional assessment should be done on patients with wounds so that a proper plan of care can be developed. Often, nutrition is an afterthought when in reality it is the foundation on which other treatments should be built upon.
Once this has been established, the patient’s plan of care can be implemented and must include nutritional education. Needed supplements to increase the patient’s ability to heal can be added or removed as necessary when the reassessments have been completed.
Ostomy Management
Introduction
Newton's law of gravity states: what goes up, must come down; similarly, the normal human gastrointestinal system has a law that what goes in, must come out. When disease inhibits the normal process, ostomy procedures are a life-saving intervention.
There are around one million people living with an ostomy or continent diversion in the US, and approximately 100,000 ostomy surgeries are performed annually in the US (1). We will build a stronger understanding of various types of ostomies, indication for the need, site selection, stoma care, complications, and patient education.
Types of Ostomies
An ostomy is a surgically created opening that reroutes stool or urine from the abdomen to the outside of the body through an opening called a stoma (9). The term stoma refers to the portion of the bowel that is sutured into the abdomen (9).
When you look at a stoma, you are looking at the lining (the mucosa) of the intestine. The color is similar to the mucosa inside your mouth and cheek. Throughout various healthcare environments, you may hear the terms ostomy or stoma interchangeably. The purpose of an ostomy is to bypass a diseased portion of the gastrointestinal tract that is not functioning properly or has been removed (2).
Ostomies are placed proximal to the diseased area, comparable to building a dam in a river to stop the flow of fluid and divert it somewhere else. An ostomy can be temporary or permanent.
There are three most common types of ostomies: ileostomy, colostomy, and urostomy (9). We will discuss these types, but it is important to recognize that gastrostomy, jejunostomy, duodenostomy, and cecostomy procedures are also done.
- Ileostomy: A stoma is attached at the end of the small intestine (ileum) to bypass the colon, rectum, and anus.
- Colostomy: A stoma is attached to a portion of the colon to bypass the rectum and anus.
- Urostomy: A stoma is attached to the ureters (the tubes that carry urine from the kidney to the bladder) to bypass the bladder.
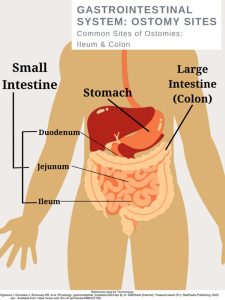
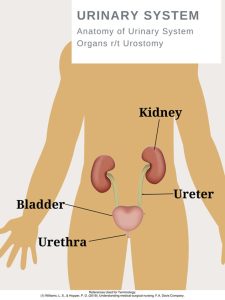
Ileostomy
The small intestine has three parts that are compact and folds over itself: the duodenum, jejunum, and the ileum. An ileostomy has a stoma attached and created from the ilium. The ileum is the final and longest segment of the small intestine (9).
The ileum terminates at the ileocecal valve, which controls the flow of digested material from the ileum into the large intestine and prevents the backup of bacteria into the small intestine (9). If a patient has this type of ostomy, the colon distal to the ostomy has a form of disease or disorder such as cancer. There are two main types of ileostomies, loop, and end ileostomy.
Loop ileostomy
In a loop ileostomy, a loop of the small bowel is lifted and held in place with a rod due to resection or repair to the distal bowel (Will). This ostomy is technically two stomas joined together (4). Loop ileostomies are typically temporary and will be closed or reversed through an operation in the future.
End ileostomy
In an end ileostomy, the ileum is surgically separated from the colon, the colon is removed or left to rest, and the end of the ileum is brought to the surface through the abdomen to form a stoma. Although end ileostomies are sometimes temporary and later rejoined, they are usually permanent (9).
Colostomy
A colostomy may be formed as an ascending, transverse, descending, or sigmoid colostomy (9). It is named according to the location of placement. An end colostomy is constructed from the ascending, transverse, descending, or sigmoid colon and has one opening for fecal elimination.
Loop Colostomy
The creation of a loop stoma takes a loop of the colon (usually the transverse colon) and pulls it to the outside of the abdominal wall (9). In this type of ostomy, the entire bowel is not dissected but left mostly intact.
End Colostomy
In end colostomies, the proximal end of the colon is dissected and pulled out of the abdominal cavity, which becomes the stoma (9). Additional procedures may involve repairing or removing portions of the distal colon or rectum.
Urostomy
Kidneys have an important job of filtering waste and excess fluid from your blood. This process creates urine, which then travels from the kidneys to the bladder through tubes called ureters (8). If the bladder is damaged or diseased, ostomies are a life-saving method of creating safe passage for the urine.
A urostomy is a surgical opening in the abdominal wall that redirects urine away from a bladder that’s diseased, has been injured, or isn't working properly (8). The bladder is either bypassed or removed (called a cystectomy) during surgery. Following the surgery, urine exits the body through a stoma.

Self Quiz
Ask yourself...
- Have you ever witnessed a GI or Urinary Surgery?
- Do you have experience with GI / Urinary procedures like a colonoscopy?
Indication for Ostomy Placement
Gastrointestinal Tract Ostomy
- Cancer
- Colorectal
- Rectal
- Trauma/ Injury
- Significant Disorders
- Crohn’s disease
- Ulcerative Colitis
- Diverticulitis
- Bowel perforation from a ruptured diverticulum or abscess
- Bowel obstruction
- Infection (9)
Urinary Tract Ostomy
- Bladder Cancer
- Neurogenic bladder disease (damage to the nerves that control the bladder)
- Birth defects
- Chronic inflammation of the bladder (9)

Self Quiz
Ask yourself...
- Have you cared for a patient with a new ostomy?
- Can you list reasons a patient is a candidate for an ostomy?
Site Selection
Wound, ostomy, and continence nurses (WOCN) play a vital role in site selection. Patients should have a pre-operative consultation prior to surgery. During this consultation, the nurse acts as an advocate and educator to prepare these patients for the physical and emotional path ahead of them. A significant amount of time should be spent with the patient before surgery to determine a stoma incision site (exit of ostomy).
It is important to make the presence of the ostomy (and collection bag) as comfortable as possible, striving to reduce the hindrance to ease movements and ability to wear their typical clothing (9). Studies show that preoperative education and stoma site marking has been directly responsible for improving quality of life and decreasing peristomal skin and pouching complications (4).
Site Assessment:
Locate positions for a site within the rectus muscle (4).
Observe the abdomen in various positions sitting, standing, or lying down.
Ask the patient about the types of clothing they wear most often. Examples: Level of pants (low, high), use of belts, dresses, etc. (9)
Determine a location that is visible to the patient, as they will need to see the site well for stoma care.
Avoid skin or fat folds (folds increase chances of leakage)
Avoid scars, bony prominences, and the umbilicus (4).

Self Quiz
Ask yourself...
- Locate places on yourself that would be appropriate for an ostomy site
- Can you think of reasons patients need to be able to see the site?
- Do you have a wound care nurse at your past or present workplace?
Post-operative Care
Post-operative care following ostomy placement is vital. The post-operative nurse assigned to this patient should read the surgery documentation to determine the type of procedure performed, intraoperative findings, type of stoma created, any advanced diseases, and unexpected events during surgery (2).
The nurse should be aware of the level of invasiveness; was this a laparoscopic, robotic, or open surgery? This type of surgery can have an impact on the post-op care plan and length of stay (2). Teaching can begin as soon as they are able to comprehend and focus on understanding new skills.
The stoma will gradually decrease in size over the weeks following the surgery. For a patient with a new ostomy, postoperative assessments should be done per facility protocol and the stoma should be inspected at least every 8 hours (9).
Note the type of closure (staples, sutures, liquid bonding agent), presence of abdominal drains, and presence of urinary catheter (C2). Assess for pain and address accordingly with repositioning, cold/heat therapy, and ordered pain medications. Assess for bowel sounds. Palpate the abdomen and note firmness and tenderness levels. Document strict Intake and Output for these patients.
Stoma Assessment:
Note the Appearance/ Color: The stoma should be pink to red in color, moist, and firmly attached to the surrounding skin (9). If the stoma appears bluish, it indicates inadequate blood supply; if the stoma appears black, necrosis has occurred. Immediate notification is needed from the provider, as the need to return to surgery will be assessed.
- Note the Presence of edema.
- Note the Surrounding skin
- Note any Ostomy Discharge
- Amount
- Color / Consistency
- Note any Bleeding
- Monitor for rupture or leakage.
Diet
Once bowel sounds and activity return, the patient’s diet may resume (2). Typically, patients are offered clear liquids to determine their ability to tolerate fluids. Nurses should encourage the patient to chew thoroughly, eat small frequent meals, and ambulate frequently to assist in gas movement and peristalsis (2).

Self Quiz
Ask yourself...
- Do you have experience with post-operative abdominal surgery?
- Explain possible respiratory or cardiovascular assessments that would be helpful for these patients
Stoma Care
Nursing Consideration / Reminders
Ostomy pouching system needs to be changed every 4 to 7 days, depending on the patient and type of pouch.
Patients should be encouraged to participate in stoma care. Instruct the patient to empty the pouch when it is one-third to one-half full as they become heavy and more prone to spilling or leaks.
Table 1. Ostomy Change Procedure SAMPLE (Always check with your agency policy)
| Steps | PURPOSE |
| 1. Perform hand hygiene. | This prevents the spread of germs and microorganisms. |
| 2. Gather supplies. |
Supplies:
|
| 3 Create privacy. Lift bed to comfortable height. |
Attention to psychosocial needs is imperative. Proper body mechanics is important for nurse. |
| 4. Place waterproof pad under pouch. | The pad prevents the spilling of effluent on patient and bed sheets. |
|
5. Remove ostomy bag. Apply non-sterile gloves. Support / hold the skin firmly with your other hand, apply adhesive remover if needed. Measure and empty contents. Place old pouching system in a garbage bag.
|
The pouch and flange can be removed separately or as one. Gentle removal helps prevent skin tears. Remove flange by gently pulling it toward the stoma. |
| 6. Clean stoma gently by wiping with warm water. Do not use soap. |
Aggressive cleaning can cause bleeding. If removing stoma adhesive paste from skin, use a dry cloth first. Soaps can irritate the stoma. Clean stoma and peristomal skin |
| 7. Assess stoma and peristomal skin. |
Stoma skin should be pink or red in color, raised above skin level, and moist (2). Skin surrounding the stoma should be intact and free from wounds, rashes, or skin breakdown. |
|
8. Measure the stoma diameter using the pre-cut measuring tool (or tracing template). Trace diameter of the measuring guide onto the flange and cut the outside of the pen marking. |
The opening should match the size of stoma. If there is skin exposed between the stoma and edge of the flange with an ileostomy, the drainage contains enzymes that will break down the skin (9). Cut out size to fit stoma, assess fit once cut. |
|
9. Prepare skin.
|
Paste can be applied directly to the skin or flange. |
|
10. Apply Flange
|
Press gently around the periphery of the stoma to create a seal |
|
11. Apply the ostomy bag Close the end of the bag with clip (follow the manufacturer’s instructions) |
Involve patient with this process, understanding instructions. |
| 12. Apply pressure to ostomy pouch to help with adhering to skin. | Heat/ warmth from hand can activate some flanges. |
| 13. Clean us supplies, perform hand hygiene. | Remove trash as quickly as possible to reduce odor. |
| 14. Document Procedure |
Example: Date/time: flange change complete. Stoma pink, moist, warm. Peristomal skin intact. Patient instructed in cutting flange to correct size, verbalized understanding of frequency of change. See ostomy flowsheet. (Abbie S., RN) |
| Data Source: Carmel, Colwell, J., & Goldberg, M. (2021). Wound, ostomy and continence nurse’s society core curriculum: ostomy management (Second Edition). Wolters Kluwer Health. | |

Self Quiz
Ask yourself...
- Are you familiar with your facility's ostomy care protocol (if appropriate)?
- How can the nurse implement safety measures with ostomy care?
- Do you feel comfortable with ostomy care documentation?
Complications
Ostomy Leakage
One of the most common and troublesome complications is leakage (4). Proper preoperative site selection (away from skin folds) is important. Patient education on proper techniques and supplies can aid in the prevention of leakage.
Educate patients on the risks of changing the ostomy too often. Frequent appliance changes lead to pain and frustration, as well as financial expenses on supplies (4). Leakage is more common in the early postoperative period but can also develop with weight changes later.
Interventions involve thickening the stool with antidiarrheals to form more solid excretion and pouching techniques to bolster the height of the stoma off of the peristomal skin (4). Helpful tips also include heating the appliance with a hair dryer before application, lying flat for several minutes following application, making sure the peristomal skin is dry before application, and the possible use of a fine dusting of stomal powder and skin sealant prior to application (4). Leakage is frustrating for patients, so support and encouragement is vital.
Mucocutaneous Separation
The stoma is sutured to the skin of the abdomen with absorbable sutures during surgery (4). Mucocutaneous separation is a complication that can occur if the sutures securing the stoma become too tight or if blood flow to the area is restricted (9). This complication requires appropriate treatment because the pouch leakage will occur from the open pocket.
The goal of treatment is to keep this open pocket covered properly until the wound heals on its own and closes. Appropriate covering of the opening can include an absorbent product such as an alginate, followed by a cover dressing such as a hydrocolloid, which is covered with the ostomy pouch (4).
Early High Ostomy Output
Early high ostomy output (HOO) is defined as ostomy output greater than fluid intake occurring within 3 weeks of stoma placement, which results in dehydration (4). This is more common with ileostomies (4). Strict Input and Output records are a vital nursing intervention. The most important treatment for this complication is hydration to prevent renal failure, which is typically done intravenously (4).
The site of a patient’s colostomy will impact the consistency and characteristics of the excretion. The natural digestive process of the colon involves the absorption of water, which causes waste from the descending colon to be more formed. Waste from an ileostomy or a colostomy placed in the anterior ascending colon will be a bit more loose or watery (2).
Peristomal Skin Issues
Irritant Contact Dermatitis (ICD) is the most common peristomal skin complication following ostomy placement (9). ICD is characterized by redness; loss of epidermal tissue; pain; and open, moist areas.
Newer and inexperienced patients and caregivers will increase the size of the pouching system opening to get a better seal and stop leakage (2) However, this only contributes to more skin breakdown and irritation. Patients may also develop a fungal rash, have allergic rashes to the ostomy appliance, or folliculitis (4).

Self Quiz
Ask yourself...
- Can you name measures to prevent leakage?
- Have you cared for a patient with Irritant Contact Dermatitis?
- Are you familiar with bulking agents for stool?
Patient Education
Patient education is a key aspect is caring for a patient with an ostomy, this process begins prior to surgery and remains constant throughout encounters. If you have not received specialized training on wound and ostomy care, you should reach out to the Wound, Ostomy and Continence Nurse (WON) within your healthcare setting to become involved if they are not already.
However, each nurse has a meaningful impact on discussing and managing expectations for life with an ostomy, including stoma care, complications, managing ostomy output, maintaining pouching appliances, and resources. Patients may feel inadequate and uneasy about caring for their stoma.
Nurses need to meet the unique learning needs of each patient and caregiver, providing education in verbal information, written pamphlets, online resources, videos, and demonstrations. The United Ostomy Associations of America, Inc. (UOAA), is a nonprofit organization that serves as an excellent resource for information, support, advocacy, and collaboration for those living with ostomies.
Nurses should be aware there is an “Ostomy and Continent Diversion Patient Bill of Rights” (PBOR) that outlines the best practices for providing high-quality ostomy care during all phases of the surgical experience (1). There are numerous national resources for patients, as well as community-based and online ostomy support groups.
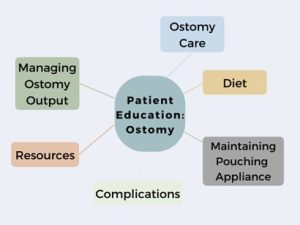

Self Quiz
Ask yourself...
- Can you think of methods to assess patient knowledge on ostomy care?
- What are creative ways to involve an ostomy patient in care?
- Not all patients are savvy with online supply ordering, can you think of other ways to order supplies if they are not?
Promotion of Body Image and Self-Esteem
Ostomy surgery can have a major impact on how patients perceive themselves. A person’s body image is how they see themselves when they look in the mirror or how they picture themselves in their mind.
There are stigmas surrounding ostomies, such as being odorous, unhygienic, and unattractive due to the stoma, but the truth is that ostomies save lives and make life possible. Positivity should surround the conversation. Confirmations such as beauty, strength, celebration, and hope are meaningful.
Ways to become involved in celebrating ostomies:
- Become familiar with the United Ostomy Associations of America (UOAA) and their initiatives.
https://www.ostomy.org/ostomy-awareness-day/
National Ostomy Awareness Day on October 7, 2023
Worldwide Virtual Run for Resilience Ostomy 5k
- Social Media Sites
Celebrate Body Positivity for those with ostomies
Intimacy Encouragement
Conclusion
Ostomy care is an essential nursing skill. If you are caring for a patient with an ostomy, remember that this is a major life-altering event and condition. Reflect on ways to provide individualized care by understanding various types of ostomies, site selection, stoma care, complications, and patient education. Empower and encourage these ostomy patients’ confidence in themselves.
Diabetes Management Updates
Introduction
Diabetes Mellitus (DM), also known as diabetes, is a condition in which the body develops high levels of blood glucose due to the inability to produce insulin or for the cells to use insulin (1) effectively. If left untreated or mismanaged, it can lead to health complications such as heart disease, chronic kidney disease, blindness, nerve damage, oral and mental health problems (1)(15).
There are several classifications of DM, and the following will be discussed: T1DM, T2DM, gestational diabetes, and idiopathic diabetes.
Classifications of Diabetes
Type 1 Diabetes Mellitus (T1DM)
T1DM is formerly known as juvenile diabetes or insulin-dependent diabetes and usually occurs in children and young adults (1). Although, it can also occur at any age and accounts for 5 – 10% of cases. T1DM develops when one’s own immune system attacks and destroys the beta cells that produce insulin in the pancreas (6).
Type 2 Diabetes Mellitus (T2DM)
T2DM, formerly known as adult-onset diabetes or non-insulin-dependent diabetes, develops because of the body's inability to use insulin effectively. It is the most common type of diabetes and mainly occurs in adults aged 30 years and older (1). However, it is also becoming common in children and young adults due to obesity. It accounts for 90% of the population diagnosed with diabetes (6).
Gestational Diabetes
Gestational Diabetes occurs during pregnancy and in women who have never had a previous diagnosis of diabetes. It is a result of pregnancy hormones that are produced by the placenta or because of the insufficient use of insulin by the cells (1). Gestational diabetes can be temporary or in some cases can become chronic. It is also likely that children whose mothers have gestational diabetes can develop diabetes later in life (6).
Prediabetes
Prediabetes, also referred to as impaired glucose tolerance, is a stage when a person is at risk of developing diabetes. If well managed through proper diet management and exercise, this can help with the prevention or delay of type 2 diabetes (1).
Other Forms of Diabetes
Other forms of diabetes include monogenic diabetes syndrome, diabetes from the removal of the pancreas or damage to the pancreas from disease processes such as pancreatitis or cystic fibrosis, and drugs or chemical-induced diabetes from glucocorticoids used to treat HIV/Aids or organ transplant (1) (6).

Self Quiz
Ask yourself...
- What are the four named types of diabetes?
- What are the differences between T1DM and T2DM?
- What is the most common type of diabetes?
Statistical Evidence/Epidemiology
Diabetes is now ranked as the 8th leading cause of death in the United States (6). There is no known cure for diabetes. It is one of the fastest-growing chronic diseases and the most diagnosed noncommunicable disease. It is also one of the leading causes of chronic kidney disease, adult blindness, and lower limb amputations (6).
In 2019, it was estimated that 37.3 million American adults have diabetes, which equals 11.3% of the population (4). Of those, 41% were men and 32% were women. 28.7 million were diagnosed with diabetes, and 8.5 million were undiagnosed.
There are 96 million American adults who are prediabetic, which means they are at risk of developing diabetes, but their blood glucose levels are not high enough to be diagnosed with diabetes (5).
Most of the population that is pre-diabetic is 65 years old or older. Type 2 diabetes accounts for 90% to 95% of cases (5). The risk of developing diabetes increases with age.
The prevalence of diabetes is much higher in both black and Hispanic/Latino adult men and women. Men are more likely to develop diabetes compared to women. Due to the rise in obesity in younger adults, there has been an increase in the number of new cases of diabetes in black teens (4).
The figure below represents trends in incidence of type 1 and type 2 diabetes in children and adolescents 2002–2018; results show the incidence of type 2 diabetes has significantly increased (4)
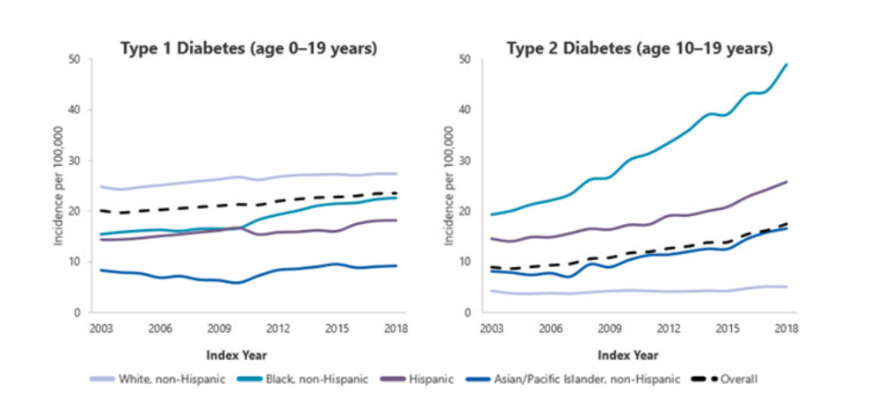

Self Quiz
Ask yourself...
- What is one of the major comorbidities caused by diabetes?
- What age group is at risk for developing type 2 diabetes?
- What is a risk factor that is contributing to the rise of diabetes in younger adults?
Etiology and Pathophysiology
In normal glucose metabolism, blood glucose is regulated by the two hormones insulin and glucagon (11). Insulin is secreted by the beta cells in the Islet of Langerhans in the pancreas and glucagon is secreted by the alpha cells in the pancreas.
When there is an increase in blood glucose, the function of insulin is to reduce blood glucose by stimulating its uptake in the cells. Glucose is stored as glycogen in the liver and muscles or as fat in the adipose tissues. When blood glucose levels start to fall, glucagon promotes the release of glycogen from the liver, which is used as a source of energy in the body (8) (13).
When there is a deficiency of insulin or a decreased response of insulin on the targeted cells in the body, it leads to hyperglycemia (high blood glucose). Meaning that the glucose that remains in the blood is not able to get to the cells. Diabetes develops mainly because of lifestyle and genetic factors (13).
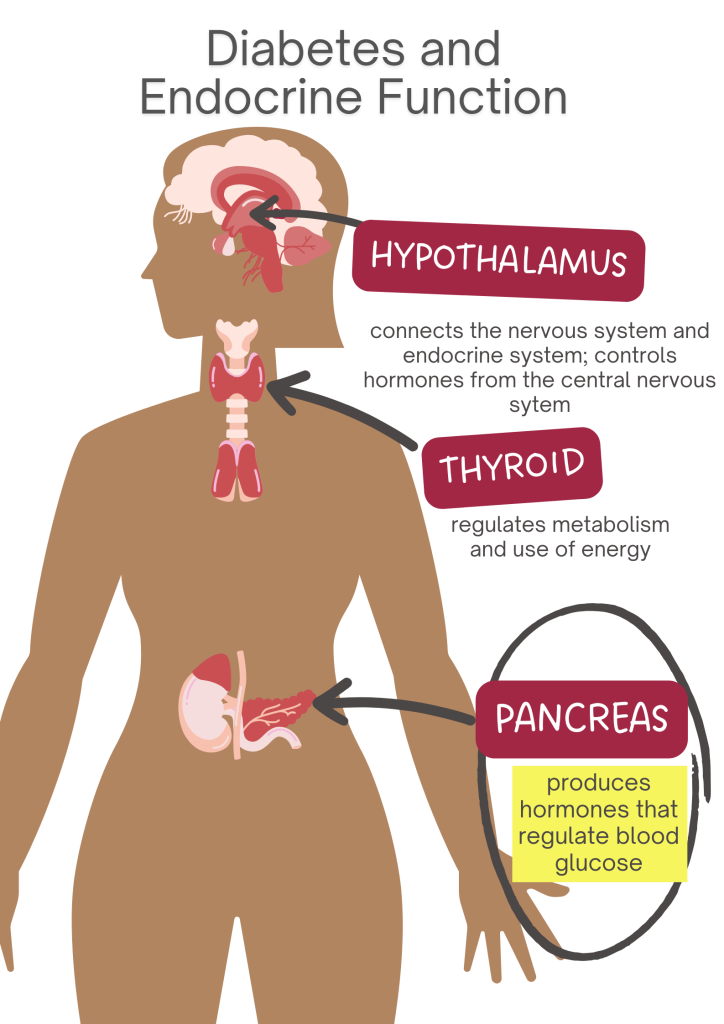
T1DM
The etiology is not well understood, though it is thought to be influenced by both environmental and genetic predispositions that are linked to specific HLA alleles. T1DM is considered an autoimmune disorder that is characterized by T-cell-mediated destruction of the pancreatic B-cells (13).
As a result, this leads to complete insulin deficiency and ultimately hyperglycemia, which requires exogenous insulin. The rate of destruction of the pancreatic B-cell-specific disorder is known to develop rapidly in infants and children or gradually in adults (8)(13).
T2DM
The etiology of T2DM is characterized by decreased sensitivity to insulin and decreased secretion of insulin. Insulin resistance occurs due to the disruption in the cellular pathways that result in a decreased response in the peripheral tissues, particularly the muscle, liver, and adipose tissue.
T2DM diabetes can progress slowly and asymptomatically over a period. Obesity and age can play a key role in the homeostatic regulation of systemic glucose because they influence the development of insulin resistance, which affects the sensitivity of tissues to insulin. Therefore, most patients with type 2 diabetes are overweight or obese 7) (8).

Self Quiz
Ask yourself...
- What are the two hormones that are responsible for maintaining blood glucose levels in the body?
- Can you describe the etiologies of both T1DM and T2DM?
- What are some of the factors that contribute to T2DM?
Diagnostic and Screening tools
There are a variety of tests that are used to diagnose and monitor diabetes. These vary based on the type of symptoms that a patient may have. Diagnosis of DM requires at least two abnormal test results, which should include fasting glucose and A1C. The tests should be one of two from the same sample or two abnormal test results drawn on different days (3).
The recommended diagnosis guidelines for diabetes must be based on the following criteria:
- Fasting Plasma Glucose (FPG) concentration with results greater than 126 mg/dL. This test involves measuring blood glucose at a single point. To have accurate results, the test should be conducted after one has had nothing to eat or drink for at least 8 hours (3).
- Glycated hemoglobin (Hb A1C) is indicative of the average levels of blood glucose in a period of two to three months. Results greater than 6.5% mean diagnosis of diabetes. This blood test does not require fasting. The A1C test is not suitable for pregnant women or those who have certain blood conditions (anemia) - NIDDK. This test should only be used for prediabetes screening (3).
- Oral Glucose Tolerance Test (OGTT): prior to conducting this test, an FPG level needs to be measured. One must ingest 75 grams of glucose liquid. Thereafter, their glucose level is measured 2 hours after they have taken the liquid. Test results greater than 200 mg/dL are indicative of diabetes. This test is commonly used in pregnant women (3).
- Random plasma glucose of 200 mg/dL. This test is suitable when one has symptoms of hyperglycemia, which are polydipsia, polyuria, and polyphagia (3).
Screening
Screening is generally recommended for adults aged 45 or older regardless of present risk factors. The updated recommendation guidelines for prediabetes screening include adults 35 years and older who are overweight or obese (3).
Screening for Prediabetes
Prediabetes is associated with the impairment of blood glucose levels between 100 – 125 mg/dL. The diagnosis of prediabetes should be confirmed with glucose testing when there is impaired glucose tolerance with plasma levels between 140 – 199 mg/dL 2 hours after one has ingested 75g of oral glucose. A1C levels of prediabetes are between 5.7% to 6.4% (3).
Screening for Pregnant women
It is recommended that all pregnant women between 24 – 28 weeks be screened for gestational diabetes to avoid missing those that are at risk. A positive 3-hour OGTT test of greater than 140 mg/dL meets the criteria for diagnosis (3).
Medication Management
Monitoring of blood glucose levels in patients is useful in determining the effectiveness of antidiabetic medication. To achieve better patient outcomes, it is important to recognize individual needs (11).
It is recommended that the approach to medication management should be based on each patient's hyperglycemic index and should include the following: the presence of comorbidities, risk of hypoglycemia, vascular disease, life expectancy, and disease duration (3).
When the management of diabetes cannot be achieved through diet and exercise alone, oral antidiabetic agents are the preferred treatment (14). Oral antidiabetics can help maintain and achieve glycemic goals for patients who are diagnosed with T2DM) (10)(14).
Diabetes Education and patient engagement is essential to managing diabetes (11). There are several classes of anti-diabetic medication. Below are some of the most utilized antidiabetic medications (9)(14).
Biguanides
Metformin is the only medication in this category.
- It is considered the 1st line of treatment in patients with T2DM unless contraindicated.
- Metformin helps to decrease hepatic glucose production.
- Decreases intestinal absorption of glucose by improving insulin sensitivity. Must be titrated initially to minimize adverse effects.
- Avoided in clients with chronic kidney disease.
- Side effects: Lactic acidosis, hypoglycemia.
GLP 1- Receptor Agonists (RAs)
Mimics glucagon-like peptide 1 (GLP -) hormone. Binds to GLP-1 receptors stimulate glucose-dependent insulin release and delay gastric emptying, which increases satiation.
- Known to have cardiovascular benefits.
- Can be taken orally or subcutaneously.
- Special considerations: Can cause weight loss, GI side effects such as nausea, vomiting and diarrhea, dehydration, increased satiation (fullness), acute pancreatitis, and reactions at the injection sites.
- Some labels may require renal dose adjustment.
- GLP - 1 RAs should be considered before starting clients on insulin to help reduce A1C then oral antihyperglycemic medications are not effective in treating diabetes.
Sulfonylureas 2nd generation
Stimulates insulin release in pancreatic beta cells.
- Risk for prolonged hypoglycemia. Therefore, it should be avoided with the concurrent use of insulin.
- Can cause weight gain.
- Can cause photosensitivity.
- Avoid use in clients with sulfa allergies and photosensitivity.
- Avoid use in clients with chronic kidney disease and liver disease.
Dipeptidyl Peptidase (DPP) - 4 inhibitors
Prevents DPP-4 enzymes from breaking down to GLP-1 hormone.
- Neutral weight.
- Monitor for acute pancreatitis, which can cause joint pain.
- May require renal dose adjustment with these brands: Saxagliptin (Onglyza), Sitagliptin (Januvia), and Alogliptin. Linagliptin does not require dose adjustment.
Sodium-Glucose transporter - 2 (SGLT-2) inhibitors
Reduce the reabsorption of glucose by up to 90%, therefore promoting the exclusion of glucose from the body.
- Known to have cardiovascular benefits for clients with cardiovascular disease.
- Use with caution in clients with increased risk of fractures.
- Avoided in clients with diabetic ketoacidosis and those prone to have frequent urinary tract infections.
- This medication should be avoided in clients with pure poor kidney function due to volume depletion and hypotension.
- There’s also a risk for Fournier gangrene.
Thiazolidinediones
Pioglitazone and rosiglitazone can help reduce insulin resistance which promotes improved sensitivity to insulin. As a result, it can help reduce the A1C levels.
- Can cause weight gain.
- Potential risk for heart failure when taking thiazolidines (brands: pioglitazone, rosiglitazone).
- Generally, it is not recommended for clients with renal impairment as medication has the potential to cause fluid retention.
- Risk for bone fractures, bladder cancer, and increased LDL cholesterol (rosiglitazone).
- Thiazolidines do not cause hypoglycemia and can be used in combination with other antidiabetic medications including insulin.

Self Quiz
Ask yourself...
- Which class of antidiabetic medications are known to put patients at risk for bone fractures?
- Can you name a condition that thiazolidines and sulfonylureas 2nd generation are generally not recommended for?
- What is a common side effect in both thiazolidines and sulfonylureas?
- What class of medication is suitable for clients with insulin resistance?
- Can you name two antidiabetic medications that can be used in combination with other antidiabetics because it has the benefit of not causing hypoglycemia?
Insulin therapy
Insulin therapy is commonly recommended for patients with T1DM. It can be used to help prevent the development and progression of diabetes (2). The ideal insulin regimen should be tailored based on individual needs and glycemic targets to better contend with physiological insulin replacement to maintain normoglycemia. Insulin therapy is also recommended for patients with hemoglobin A1c of greater than 9% - 10% and when symptoms of hyperglycemia are present (3).
Other Diabetes Interventions
The automation of glucose monitoring devices and insulin delivery systems is revolutionizing glucose management mainly because it promotes lifestyle flexibility and improved glucose management (2).
- Glucose Monitoring Devices- these devices are ideal for clients who are on insulin regimens and may become the standard for assessing glycemic controls in clients with DM (7).
- Continuous Glucose Monitoring (CGM)- devices that are inserted subcutaneously and measure interstitial blood glucose levels. CGMs are devices that are used to provide glucose readings, trends, and alerts to the user in real-time to inform diabetes treatment decisions. (2)(3)
- Importance- CGM is recommended for all patients with diabetes who receive treatment with intensive insulin therapy, defined as three or more insulin injections per day for all individuals with hypoglycemia (frequent, several, nocturnal) (3).
- Known to reduce hyperglycemia and A1C levels.
- Insulin Pump Therapy- also known as Continuous Subcutaneous Insulin Infusion (CSII) has had notable advances over the years. CSII is recommended for those with type 1 diabetes, although in recent studies, conventional CSII is also recommended for use in T2DM patients (2)(3). CSII is a small computer that is programmed to deliver fast-acting insulin continuously to the body using mechanical force via a cannula that is inserted under the skin (2).
- It is more precise and flexible in insulin dosing.
- Known to improve glycemic control.
- Cheaper than using Multi-Dose Insulin.
- Automated Insulin Delivery Systems (AIDS) - This is a diabetes management system that utilizes an insulin pump in conjunction with an integrated CGM and computer software algorithm (3).
- Advantages: precision and flexibility with insulin dosing.
- Recommended for T1DM: Achieve glycemic targets with less burden.

Self Quiz
Ask yourself...
- What is the main type of insulin used in CSII pumps?
- What type of diabetes category is more suitable for using CSII?
Upcoming Research
Islet cell transplant has been a biological solution to help treat patients with T1DM due to poor graft survival rates. Future research will focus on manipulating the beta cells in the pancreas to make them more viable. Other treatments that have been recently made available include incretins and Amylin which improve the absorption of insulin in the body (1).
- The development of other types of insulin that can be administered by inhalation.
- The development of immunosuppressant drugs that will help treat T1DM.

Self Quiz
Ask yourself...
- Can you name two recently developed medications to help with insulin absorption in the body?
Conclusion
Diabetes is a complex disease that requires a multi-disciplinary and patient-centered approach to help with effective management. Regular and early screening are necessary for those at risk for developing diabetes. Most importantly, ease and access to choices of managing diabetes are necessary.
Hospice and Palliative Care: What’s the Difference?
Introduction
Hospice and palliative care are unique health concepts often incorrectly used interchangeably. During my career as a hospice and palliative care nurse, I often heard the question, "What's the difference between Hospice and Palliative Care?"
I usually answered with a common phrase the Hospice and Palliative Care community uses to explain the difference, "All Hospice is palliative care, but not all Palliative Care is hospice." The statement is accurate but still confusing.
This course aims to shed light on these topics and emphasize the importance of enhancing end-of-life care, but let's start with Merriam-Webster's dictionary definitions.
- Hospice: "a program designed to provide palliative care and emotional support to the terminally ill in a home or homelike setting so that quality of life is maintained, and family members may be active participants in care” (4).
- Palliative: "relieving or soothing the symptoms of a disease or disorder without effecting a cure” (4).
The Merriam-Webster definitions help to clarify the differences further: Hospice is a program, and palliative care is a practice. They are two distinct approaches to providing comprehensive medical care and support for patients with serious illnesses, and they have essential differences worth exploring.
This course aims to delve into the different types of care, their philosophy, eligibility criteria, duration of services, and common myths and misconceptions surrounding hospice and palliative care. Additionally, it highlights nurses' crucial role as advocates and resources in these specialized fields.

Hospice Care
The modern hospice movement originated in the late 1960s in the United Kingdom, primarily through the work of Dame Cicely Saunders. Saunders, a nurse, and social worker, recognized the need for specialized care for patients with terminal illnesses. She founded St. Christopher's Hospice in London in 1967, which became the model for modern hospice care (12).
Saunders emphasized care that was less focused on disease treatment and more focused on an individual's physical, emotional, social, and spiritual needs. This approach prioritized providing comfort, pain management, and dignity for patients nearing the end of life (12).
The concept of hospice care gained international recognition and spread to other countries. By 1974, the first hospice program in the US was formed in Connecticut, and the hospice movement expanded rapidly (11).
Hospice care was primarily provided by volunteers who went into families' homes to care for their loved ones when no curative care was available. These same volunteers helped write the federal regulations adopted as the Medicare Hospice Benefit (MHB) in 1982 (5).
It is essential to discuss the MHB because the US government benefit made hospice a fundamental part of comprehensive medical care. It is the benefit through which most patients nearing the end of life receive care, and it has defined how we provide hospice care throughout the United States.
An integral part of hospice care is visits from a nurse, social worker, chaplain, and nurse aides. In addition, the patient and family have access to a hospice physician specializing in Hospice and Palliative Care (5). Hospice care focuses on providing compassionate, holistic, patient-centered care for individuals with terminal illnesses. The primary goal is to enhance the quality of life for patients and their families by addressing physical, emotional, social, and spiritual needs (5).
The MHB covers 100% of the financial cost for hospice services, including medications, supplies, and treatments required due to a terminal illness. The medicines commonly covered under the hospice benefit are for treating pain, nausea, anxiety, and other distressful symptoms, such as constipation (5).
Who can receive this care?
The MHB was designed for patients who are terminally ill with a six-month life expectancy, as determined by a physician (5). Life expectancy is one of the critical differences between Palliative Care and Hospice Care.
Healthcare providers, unlike statisticians or actuaries, are unskilled at predicting a six-month or less life expectancy. As part of the hospice federal regulations, local coverage determinations set by government intermediaries help healthcare providers determine who meets the criteria and, therefore, is eligible for hospice.
Key indicators predicting the end of life due to a specific disease process have been defined so that we can compare each patient to determine their eligibility for hospice care. Some key indicators are activity level, the times the patient has sought emergent care or has been hospitalized in the past six months, weight loss, and neurological status.
Patients generally receive hospice care when curative care is no longer an option. This is another crucial difference between Hospice and Palliative Care. There are exceptions, commonly for children, where curative and hospice care are provided. This is termed "concurrent" care.
How long do they receive services?
The key indicators that hospice physicians use to determine eligibility are based on averages of patients who have died with the specifically defined disease process. However, the average time to death is unreliable when judging how long an individual may live.
Therefore, hospice care is provided for as long as the patient's condition remains terminal, according to local coverage determinations, and they choose to continue receiving this specialized type of palliative care. In fact, the MHB has no end date, and the duration of services may vary depending on the progression of the illness and the patient's preferences.
For example, patients with chronic illnesses, such as heart failure, chronic obstructive pulmonary disease (COPD), and Alzheimer's, tend to have a less predictable trajectory of terminal illness due to periods of exacerbation and stability, which are common. Patients with chronic diseases tend to have a longer stay in hospice care. A waxing and waning pattern of decline is less typical with cancer-related disease, and these patients generally use fewer days of hospice care.

Self Quiz
Ask yourself...
- What is your understanding of the philosophy behind hospice care?
- How do you determine the appropriate duration of services for a hospice patient?
Palliative Care
The long-held theory regarding palliation, or soothing symptoms as defined by Merriam-Webster, is that if the treatment causes suffering with the result of a cure, the benefit of the treatment outweighs the burden. In other words, a person should be able to tolerate suffering for a positive end result. On the other hand, if no cure is available, suffering is inhumane.
Palliative Care emerged as an integral part of hospice care, focusing on providing comfort and support to patients with terminal illnesses (14). However, for people without terminal illnesses, some treatments and symptoms of curable diseases are so intolerable that patients may be unable or unwilling to continue curative treatment. Why should patients and families not receive physical, psychosocial, or spiritual support simply because they are not at the end of life?
The need for Palliative Care beyond hospice was identified in other healthcare settings, such as hospitals and home care. Over time, the philosophy and principles of Palliative Care gained recognition beyond the hospice setting. This led to the development of specialized palliative care services that aimed to provide comprehensive support to patients with serious illnesses, regardless of their prognosis (14).
In 1990, the World Health Organization (WHO) formally defined palliative care, emphasizing its holistic approach. The WHO defines palliative care as improving the quality of life of patients and their families facing life-threatening illnesses by preventing and relieving suffering through early identification and treatment of pain and other physical, psychosocial, and spiritual problems (13).
The American Academy of Hospice and Palliative Medicine (AAHPM) was established to promote and advance Palliative Care, and it has now become a recognized medical specialty. Palliative care education programs, certifications, and fellowships have been established to ensure the development of skilled professionals who provide palliative care (14).
Palliative Care is an essential part of healthcare, aiming to improve the quality of life for patients with serious illnesses and their families. It focuses on relieving symptoms, addressing psychosocial and spiritual needs, and enhancing communication and decision-making throughout the illness trajectory.
Philosophy
Palliative care aims to improve the quality of life for patients who suffer regardless of life expectancy, a key differentiator from hospice care. Palliative care focuses on symptom management, pain relief, and addressing patients' and their families' physical, emotional, and psychosocial needs.
Who can receive this care?
In the modern healthcare system, "palliative" is often used to define comfort care for patients with "serious illnesses." Palliative Care is available to individuals of any age and at any stage of a serious illness, including those undergoing curative treatments. It can be provided concurrently with curative treatments, such as chemotherapy and radiation, another differentiator from hospice care. Individuals with serious illnesses may receive palliative care during a hospitalization, at home, or office visits.
How long do they receive services?
Unlike Hospice Care, Palliative Care can be provided for an extended duration even if the patient's condition is not terminal. The duration of services varies based on the individual's needs.

Self Quiz
Ask yourself...
- How does Palliative Care differ from Hospice care in terms of philosophy and approach?
- Can you explain the eligibility criteria for receiving palliative care?
Common Myths and Misconceptions
| Myth |
Fact |
|
Hospice care hastens death. |
Studies show that patients with the same diagnosis and burden of illness live longer with hospice than without (2). |
|
Palliative care is only for people who are dying. |
Palliative care is available to people of any age and stage of serious illness. |
|
Hospice is a place. |
Hospice is a form of care provided to people wherever they reside. |
|
Palliative care is only available in hospitals. |
Palliative care is available in hospitals, at home, or in a doctor's office. This is dependent on the availability of practitioners in your area. |
|
Hospice is only for the last days of life. |
Hospice is for the terminally ill with a life expectancy of 6 months or less and continues as long as a person remains terminally ill (15). |
|
Palliative care is only for the elderly. |
Palliative care is for all individuals with a serious illness. |
|
Hospice is the same as Palliative Care. |
Hospice is palliative care for the terminally ill. Palliative care is for all patients receiving curative treatment no matter the stage of illness, depending on the Palliative Care team's defined practice. |
|
Hospice and Palliative Care mean you are giving up hope. |
Hospice and Palliative Care aim to manage symptoms and improve the quality of life. |
|
Hospice and Palliative Care are expensive and not covered by insurance. |
Hospice care is 100% covered by Medicare and most other insurance (15). Palliative care is covered as a medical practitioner's visit in most Palliative Care programs. |

Self Quiz
Ask yourself...
- What are common misconceptions you have encountered regarding hospice or palliative care?
- How did you resolve the misconceptions surrounding palliative and hospice care?
Handling Difficult Conversations
Conversations, especially regarding end-of-life, are difficult for the clinician, the patient, and the family. Sensitive conversations also take time, patience, and empathy. Often, more time than a general practitioner or clinician has available. In my experience, patients approaching the end of life are often referred to as Palliative Care practitioners because of the practitioner's experience with difficult conversations. I also believe this referral practice is part of the confusion in understanding the difference between Palliative and Hospice Care.
Palliative Care Practitioners are not the only ones with the time and the skill to broach difficult conversations. Nurses also play a critical role in facilitating difficult conversations about end-of-life decisions, goals of care, and advance care planning.
Nurses often spend more time with patients and families than other disciplines. The relationship and trust nurses build with patients and caregivers makes them especially adept at starting difficult conversations.
A nurse must take the following actions before, during, and after a difficult conversation (3).
- Build a strong relationship with the patient and their family through active listening, empathy, and creating a safe space for open communication.
- Assess the patient's and family's readiness and preferences to engage in discussions. Ask patients and families questions regarding the amount and detail of information they want and the personspeople that need to be involved in decision-making. This information helps to tailor the discussion.
- Use practical communication skills such as clear and concise language aimed at providing information in a way that is understandable and sensitive to the emotional needs of the patient and family.
- Begin the conversation by assessing the patient and family's understanding of the diagnosis and prognosis to address any misconceptions or gaps in knowledge and ensure everyone is on the same page.
- Engage in a collaborative discussion about the patient's goals and values. Exploring their priorities and preferences regarding treatment options, symptom management, and quality of life helps align the care plan with the patient's values and wishes.
- Acknowledge and validate emotions, offering support and empathy throughout the conversation. Referral to appropriate psychosocial or spiritual support services may be necessary.
- Document the discussion and decisions made in the patient's medical records. Follow-up conversations should be scheduled to address any further questions, concerns, or changes in the patient's condition or preferences (3).
Should you find yourself in a position to start a difficult conversation, the following practical framework may be of assistance (3):
- Set aside time and make a plan to minimize interruptions.
- Before the conversation, take a moment to center yourself and release stress.
- Acknowledge the family and offer support by inquiring about their immediate needs.
- Open the conversation by asking what the patient and family know about their condition.
- Repeating what they know, ask them how they want to experience the time they have left.
- Empathize and allow them time to discuss and consider what they want.
- Based on their desires, educate them about the options for care.
- Consult with the interdisciplinary team and make appropriate referrals.

Case Study
Emily is a registered nurse who works the day shift on a bustling med-surg floor. She has a reputation for excellent communication skills and the ability to handle difficult conversations with empathy and grace, but she admits she never feels comfortable doing so. When she must have a difficult conversation, she uses a structured format to guide her to maintain her composure and empathy. Emily needed to use this framework when the physician asked her to talk to the family of Mr. Johnson about hospice care.
Mr. Johnson was a 75-year-old man admitted with advanced pancreatic cancer. His condition was deteriorating rapidly, and it was clear that curative treatments were no longer effective. Mr. Johnson's wife, Judy, was consistently by his bedside, her worry and sadness evident in her eyes. Emily knew Mrs. Johnson needed a plan because the fear of not knowing can be far worse than the reality. Emily asked her co-workers to cover for her other patients for the next 20 minutes so she could have a conversation about hospice.
Emily approached the room; she stopped momentarily and took a deep, centering breath. She released the day's stress and gave herself space to focus on this task. Emily gathered her thoughts and reminded herself of the framework she would use. She knew this conversation would be challenging but discussing the next steps in Mr. Johnson's Care was necessary. She entered the room with a warm smile, acknowledging both Mr. and Mrs. Johnson.
Emily began by asking how Mr. Johnson was feeling, allowing him to express any concerns or symptoms he was experiencing. She listened attentively, validating his feelings, and reassuring him that his comfort was a top priority.
After addressing Mr. Johnson's immediate concerns, Emily asked, "Mr. Johnson, what has the doctor told you about your prognosis?" Mr. and Mrs. Johnson began to verbalize that they knew Mr. Johnson was not getting better and was worsening. Mr. Johnson offered that the doctor told them curative care was not an option and that his prognosis may be short. Emily noticed Mrs. Johnson's eyes welling up with tears as Mr. Johnson spoke. Sensing her emotional distress, Emily offered her a comforting hand.
Emily asked, "How do you see spending your remaining time?"
Mr. Johnson quickly stated, "I want to go home."
Mrs. Johnson had a worried look on her face. Emily turned to her, and Mrs. Johnson stated, "I don't know how I can care for him at home."
Emily reassured Mrs. Johnson that this was a fear expressed by many spouses experiencing similar circumstances. Then, Emily introduced the concept of hospice care, explaining that it could provide specialized support and comfort to Mr. Johnson in the comfort of his own home. She highlighted the benefits of hospice, such as nurse visits, pain management, emotional support, and assistance with daily activities by an aide.
Understanding the gravity of the situation, Mr. Johnson and his wife looked at each other, their love and concern evident. After a moment of silence, Mr. Johnson nodded, expressing his willingness to explore hospice care to enhance his quality of life during this challenging time.
Emily continued the conversation, outlining the next steps and assuring the couple that the hospice team would work closely with them to develop a customized care plan. She provided them with a referral to hospice and assured them that she would be available to answer any questions.
As the conversation came to a close, Emily thanked Mr. and Mrs. Johnson for their trust and assured them that their decision was an essential step towards ensuring Mr. Johnson's comfort and dignity. She could see more lightness in Mrs. Johnosn's eyes. She was standing taller and breathing easier.
Emily left the room, knowing that this difficult conversation had set the foundation for a new chapter of Care focused on providing the support and compassion that Mr. Johnson and his wife deserved.
Nurse Role as Advocate
Nurses are the center of the interdisciplinary team, often providing communication and updates from patients and families to other practitioners such as social workers and physicians. The focused time they spend with patients in guided conversations and daily assessments allows nurses to gain a more in-depth understanding of the patient, family dynamics, and care goals.
A particular time of vulnerability for patients and families is during a serious illness and at the end of life. Nurses are responsible for advocating for patients' rights, respecting their wishes, and facilitating open communication between healthcare providers, patients, and their families. They play a pivotal role in ensuring the patient's voice is heard, and their needs are met.
Here are some ways nurses advocate for patients:
- Patient-centered care: Nurses help guide decision-making processes and ensure care aligns with the patient's values and goals when they ensure patients' preferences, values, and goals are at the center of their care (18).
- Shared decision-making: Nurses facilitate shared decision-making between patients, families, and healthcare providers by acting as intermediaries, ensuring patients' voices are heard and respected during discussions about treatment options, advanced directives, and end-of-life care planning (19).
- Psychosocial and spiritual needs: Nurses advocate for patients by providing emotional support, facilitating discussions about fears and concerns, and connecting patients with appropriate resources (20).
- Pain and symptom management: Nurses advocate for optimal comfort by assessing and addressing patients' physical distress, collaborating with the healthcare team, and advocating for timely interventions (21).
- Patient autonomy: Nurses who involve patients in decision-making processes, including information about treatment options, risks, and benefits, support patients in making informed choices (24).
- Informed consent: Nurses ensure patients understand the nature of their treatment, potential risks, and alternatives serve to advocate for informed consent (23).
- Healthcare disparities: Nurses who identify and address healthcare disparities based on race, ethnicity, socioeconomic status, or geographic location work toward eliminating inequitable healthcare (8,10).
By advocating for patients during these critical times, nurses can help ensure that patients’ wishes are respected, their quality of life is optimized, and they receive compassionate and patient-centered care.

Self Quiz
Ask yourself...
- How is advocacy different with hospice and palliative care patients than patients with non-serious illness?
- During your career, in what ways have you advocated for patients with serious illness?
Providing Resources
To provide comprehensive care, nurses must be knowledgeable regarding hospice and palliative care and what each provides. Educating families and patients about their options is a great way to provide emotional support and help them navigate complex medical decisions.
As part of the MHB and many other insurers, hospice care is funded 100%. As a result, hospices are required to provide a specific set of resources (15). Medicare and private insurers frequently cover the cost of a Palliative Care practitioner on a per-visit basis. Thus, Palliative Care resources can vary widely per program. Knowing what resources are available through your local palliative care program is essential. Below is a chart of common hospice and palliative care resources and their benefits.
| Resource | Hospice | Palliative | Benefits |
| MD | Yes | Yes | Palliate symptoms through medical assessment and treatment. |
| NP | Maybe | Often | Palliate symptoms through medical assessment and treatment. |
| Registered nurse | Yes | Maybe | Care coordination, assessment, monitoring, symptom management, education, and communication with interdisciplinary teams. |
| Social Work | Yes | Maybe | Assist with community resources, counseling, advance directives, and other support. |
| Chaplain | Yes | Maybe | Assist with spiritual support, counseling, and connecting patients with their church affiliation and practices. |
| C.N.A. | Yes | Rare | Assist patients with physical care such as bathing and dressing. This is often a great support to caregivers. |
| Dietician | Yes | Rare | Assist and support patient’s dietary needs. |
| Pharmaceuticals | Yes | No | Alleviate common symptoms. |
| Medical Supplies | Yes | No | Wound care, other treatments, continence, and cleanliness needs. |
| DME | Yes | Maybe | Supports a patient’s ability to be independent. |
| PT, OT, ST | Yes | Able to make referrals | Support to maintain function, non-pharmacological pain management, assistance with communication, swallowing, wound care, and ADL support. |

Self Quiz
Ask yourself…
- How do you advocate for patient’s rights and ensure their wishes are respected in your healthcare setting?
- How do you support patients and their families during difficult conversations about end-of-life decisions?
- How do you provide emotional support to patients and families in need?
- What strategies do you employ to ensure effective communication between patients, families, and the interdisciplinary team?
- How do you manage your emotional well-being when working with families and patients nearing the end of life?
Becoming a Hospice or Palliative Care Nurse
Even though Hospice and Palliative Care are different, the skills and qualities of successful hospice and palliative nurses are similar. As previously discussed, Hospice and Palliative Care payment differs, with Palliative Care primarily funded by payment to medical practitioners. Because of the funding, it is rare for Palliative Care practices to employ nurses to the same degree as hospice. Many Palliative Care programs do not have nurses in their daily practice but may have them for patient follow-up or coordination of care.
For this education, we are focused on the requirements of becoming a hospice and palliative care nurse, understanding that positions for Hospice nursing are more prolific than strictly Palliative Care nurses.
Educational Requirements
While many nurses can specialize in a specific area of care, for example, geriatric, cardiac, critical care, surgical, or emergency care, hospice, and palliative care nurses care for patients with a wide range of illnesses, ages, and abilities.
Hospice and palliative care nurses need to understand the ordinary course of numerous conditions in multi-aged patients to anticipate, prepare, and quickly palliate symptoms of the specific disease. They must be skilled in the assessment of patients and able to detect subtle changes in conditions that affect the patient’s plan of care.
Certain requirements need to be met to become a hospice and palliative care nurse (17). Here are the general requirements:
- Licensure: Current, unrestricted license as a registered nurse (RN) or licensed practical/vocational nurse (LPN/LVN) in the state where they practice. The specific licensure requirements may vary by state.
- Certification: Hospice nurses are often required to have specialized certifications related to hospice and palliative care. The most common certification for hospice nurses is the Certified Hospice and Palliative Nurse (CHPN) credential, offered by the Hospice and Palliative Credentialing Center (HPCC). This certification demonstrates expertise in providing care to patients with life-limiting illnesses. This certification requires two years of hospice experience for eligibility to take the certification test (16).
- Education and Experience: There are no specific education requirements for hospice nurses required by regulatory bodies. However, most hospice agencies prefer nurses with a bachelor’s degree in nursing (BSN) or higher. As written above, hospice and palliative care patients range in age and illness. Therefore, many agencies also prefer nurses with two years of experience in a medical-surgical healthcare setting (17).
- Training: Hospice nurses must receive comprehensive training in hospice care and be knowledgeable about the philosophy, principles, and practices of hospice and palliative care. The hospice agency typically provides this training and covers pain management, symptom control, psychosocial support, communication, and end-of-life care (17).

Self Quiz
Ask yourself…
- What is your experience with the importance of certification as perceived by patients and families?
- What is your experience with the importance of certification as perceived by healthcare professionals?
Skills and Qualities
Hospice and palliative care nurses must thrive on working independently since more than 80% of hospice and palliative care is provided in patient's homes. While hospice and palliative care are under the management of the physician, the hospice nurse is the primary assessor and at the patient's bedside.
Hospice nurses must be organized, have firm boundaries, and be able to systematize their practice to see multiple patients in one day, with the requirements of driving, documenting, communicating with the interdisciplinary team, and providing care according to the individual patient care plan. In addition, they must provide support and education to the patients and their families.
Nurses in hospice and palliative care settings require excellent communication, empathy, and the ability to navigate complex ethical dilemmas and difficult conversations.

Self Quiz
Ask yourself...
- How do you stay current on the latest research and best practices regarding caring for patients with serious illnesses or at the end of life?
- Can you describe a situation where you had to manage complex pain or symptoms?
- What additional training or education have you pursued to better manage patients with serious illnesses or near the end of life?
Conclusion
In conclusion, Hospice and Palliative Care represent two distinct but interconnected approaches to providing comprehensive medical care for individuals with serious illnesses. While hospice care focuses on terminal patients and aims to enhance their quality of life, Palliative Care addresses the needs of individuals at any stage of a serious illness.
Nurses are crucial in advocating for patients, facilitating difficult conversations, and providing resources to support patients and their families. By understanding the philosophy, eligibility criteria, and duration of hospice and palliative care services, nurses can contribute to the holistic well-being of patients in these specialized fields.
As society continues to recognize the importance of providing comprehensive end-of-life care and support for patients with serious illnesses, it is crucial to foster awareness, education, and support for hospice and palliative care services. By doing so, we can collectively work towards enhancing the experiences of those facing life-limiting illnesses, offering comfort, compassion, and dignity throughout their journey.
Navigating Difficult End of Life Conversations
Introduction
Talking about death is generally difficult for the average person. It is even considered taboo in some cultures or situations. For some nurses, having end of life conversations is a routine part of the profession. A hospice nurse, for example, carries the responsibility of managing care for a dying patient, and ultimately informing the patient’s family that death is imminent.
A lack of training, experience, or confidence in this area could result in poor delivery, unrealistic expectations, and an overall negative dying experience. Most people do not have experience or even a baseline when it comes to death and dying. This makes end of life conversations much more important in the delivery of patient care.
Perspectives About Dying and Death (Philosophical, Psychological, and Spiritual)
Philosophical
The human experience of death and dying is not one sided. On the contrary, there are many things to be considered to understand it fully. This goes beyond a scientific approach. An understanding of philosophical reasoning related to death is imperative to provide a thorough explication of the human dying experience. Historically, death has been an intrinsic part of life throughout various civilizations.
Ancient Egyptians spent much time preparing for the next life. Life was perceived as a dream that passed quickly. Death was viewed as eternal. Egyptians believed that the dead would make their way over to The Kingdom of Orisis, where they would spend eternity.
Ancient Greek civilization also viewed death in a particular light. According to San Filippo, “Greeks perceived death as a release of the soul from the body. The soul, which was considered to be part of the mind, was believed to be immortal. It was considered that the soul lived before the body and would live again in another life” (1).
Lastly, it has been noted that when it comes to fearing death, people create philosophies and theologies due to an inability to visualize our own death and afterlife.
Psychological
The psychological aspect of death is just as important as the physical. The thought of death alone has the potential to evoke various memories and feelings. You will typically find that a person either accepts or fears death (positive outlook vs negative outlook). This can be a fear of suffering, pain, or of the unknown. These views are typically formed based on past experiences with death.
Often, a person may have no underlying baseline when it comes to dying or death. That first experience with death can potentially shape someone’s entire perspective. Fearing death could be attributed to a fear of the unknown, lack of relatable experience, a negative experience, or a lack of communication regarding death, due to a cultural taboo, for example.
On the other hand, things like faith, positive experiences, and imminent death may cause someone to be more accepting of death. Often, someone facing imminent death may be forced to think about it and come to terms with it. In a study of terminally ill patients facing death, “The participants were afraid of death and earnestly desired to live but felt that death was imminent. To escape their distress, they attempted to accept the situation by thinking that all lives are finite, and death had to be accepted” (2). This is an example of coming to terms with an impending death and accepting it.
Spiritual
Spiritual perspectives on death should be considered when discussing views on dying. History shows that humans have long held beliefs that life does end when the body dies. Many tend to believe that once a person dies, their soul is then freed, and can go on to another life or be reincarnated into someone or something else. Religious ideologies contain a vast amount of knowledge and wisdom regarding death. “Religion and spirituality help individuals make sense of what awaits them near the end of life and help the dying cope with their terminal condition” (7).
What happens after death may vary from one religion to the next. Many religions also have a heaven or heaven like final place where the deceased can rest and be with other who have also died. One of the oldest ideologies of human history is the belief that there can be life after death.

Self Quiz
Ask yourself...
- Historically, how has death been viewed in different civilizations?
- Why might a patient fear death and dying?
- What causes patients to be more accepting of death?

Impact on Nurses
Imagine working as a hospice nurse. Your sole purpose is to provide end-of-life care for terminally ill patients. This includes providing information on what to expect at the end of life. At any given time, you have patients that could be imminently dying.
You are a source of knowledge and comfort for a patient and their family during this time. In the end, you will likely be there when the patient takes their last breath. How can one prepare to handle this scenario time and time again? Should a nurse feel sadness for a patient that was expected to die, or should they emotionally separate themselves?
The latter may prove hard to do. The reality is that nurses are frequently exposed to death and dying in a variety of settings. A patient’s dying process can be planned or not and this distinction may mean different things for different people. Typically, nurses are taught skills to help prevent death.
This may be a hard thought process to overcome when the goal is not curative, but comfort focused. These patient interactions help to shape a nurse’s feelings on death and dying. “Nurses are frequently exposed to dying patients and death in the course of their work. This experience makes individuals conscious of their own mortality, often giving rise to anxiety and unease.
Nurses who have a strong anxiety about death may be less comfortable providing nursing care for patients at the end of their life” (3). This ‘death’ anxiety could lead to disastrous outcomes for both the nurse and the patient. Nurses should be aware of their own thoughts and attitudes towards death, and how these could affect their ability to provide patient care.
Caring for the dying involves both skill and emotional support from nurses. Younger nurses and nurses with less experience with death may have greater difficulty caring for dying patients. End of life education and an introspective look at oneself are imperative when it comes to providing quality care. “Nurses’ professional experience is positively correlated with their position, professional level (rank), EOL care experience, competence in EOL, and another knowledge.
Nurses who have a positive attitude seem more likely to have more competence in dealing with patients’ symptoms at EOL and better knowledge of EOL care (3). The more palliative knowledge nurses had, the more competence they felt. Moreover, competence dealing with patients’ symptoms in EOL care was correlated with older nurses” (8). Positive conversations about death and dying usually lead to a positive dying experience.
To reach this point, nurses and other healthcare professionals need to know how to have these conversations. In a society that is so focused on the living, receiving education on death can be difficult. When death is perceived as a part of life, only then will people feel more comfortable talking about it.

Self Quiz
Ask yourself...
- What role do nurses play in death and dying?
- In what ways are nurses affected by death?
- How do previous experiences shape our views about death?
- What are some potential indicators of a nurse’s ability to provide quality care at EOL?
Communication Strategies
Many people are uncomfortable talking about death and dying and tend to shy away from such conversations. This may also be true for nurses. Talking about death should not be a formidable task. Nurses should be able to comfortably implement these conversations in their practice when needed. Effective communication is imperative throughout a patient’s trajectory.
Conversations about death and dying can impact patient care. “Research has shown that talking about and planning the EOL is important for how the final days in a patient’s life may play out and is associated with reduced costs as well as a higher quality of care in the final weeks of life” (4). In a society so focused on life, it may be difficult for nurses and other health professionals to obtain the skills needed to confidently speak with patients about death.
To effectively talk to patients about death, nurses should first be willing to initiate and discuss the topic. There are important strategies to remember when talking about the end of life. “Qualitative research on the end of life has revealed that medical personnel should consider the following strategies when conducting EOLD: open and honest conversation, setting treatment goals, and balancing hope with reality” (13).
Patients should also be encouraged to express their thoughts, fears, and to ask questions. It is also important to be honest and forward with patients. No “beating around the bush”. This means using words like “dying” and “death” while having these conversations.
One communication strategy, VALUE, “recommends to value and appreciate statements of family members, acknowledge their emotions, as well as to listen and ask questions to understand who the patient was as a person” (9). Nurses should keep the following in mind: a patient’s comfort level with death, goals of care, expectations, and cultural factors. Having this knowledge will help to guide the conversation.
Lastly, when a nurse feels confident and exhibits calmness while talking about death, a patient will more than likely feel the same way.

Self Quiz
Ask yourself...
- How do conversations about death impact patient care?
- What can nurses do to effectively communicate with their patients about death?
- What strategies should be utilized when talking about death?
Stages of Grief
Nurses are not immune from experiencing grief or loss. We mourn personally and we mourn alongside our patients and their families. “Grief and loss are something that all people will experience in their lifetime. The loss may be actual or perceived and is the absence of something that was valued. An actual loss is recognized and verified by others while others cannot verify a perceived loss.
Both are real to the individual who has experienced the loss. Grief is the internal part of the loss; it is the emotions related to the loss” (4). Grief allows a person to begin to deal with the pain associated with loss and to heal. There are five stages of grief which were identified in Dr. Elisabeth Kübler-Ross in her book Death and Dying.
- Denial: This stage Is not necessarily about denying that the loss happened. Instead, it is more about denying the feelings associated with the loss. Denial lets us face our feelings of grief. “As an individual is able to accept that this loss is their reality, they will be able to move into the healing process and denial will begin to diminish” (5).
- Anger: A grieving person may feel anger towards a variety of people associated with the loss. This is a normal and a necessary part of the healing process. “Under the anger is the individual’s pain. Anger provides structure, and that is better than preceding numbness. It can be a challenge for some to feel the anger; sometimes it is easier to try and suppress the anger. Feeling anger and addressing anger is part of the grieving process” (5).
- Bargaining: Grieving people may begin to say things to themselves like, “If this__, then this __”, or “I will do anything if you take the hurt away” (5). This stage may occur at any point in the grief process. Once this step is reached, the person can begin to move through the stages in different ways.
- Depression: This stage involves a realization that the situation is real. “Empty feelings come forward, and one’s grief moves in on a deeper level than before. This type of depression is not a sign of mental illness; although reaching out for help may be the right step. It is an appropriate response to a great loss. An individual may withdraw from their daily life activities, and they may feel a fog of intense sadness” (4). Depression after a major loss is normal and necessary in the healing process.
- Acceptance: Entering this final stage does not mean one is completely okay with what has happened. In fact, one may never be as they once were prior to the loss. “Acceptance, as a stage, is about accepting that this is their new reality, and it is permanent. Life cannot go on as it once did, but through acceptance, life can and will go on” (5). Individuals in this stage must realize that change is necessary to adjust to the new normal.
Not everyone experiences grief in the same way. Grief is a very personal experience that affects people in different ways. Nurses should be familiar with the stages of grief to be able to offer optimal patient care to grieving patients and their families. This includes recognizing signs of depression and possible suicidal ideation, providing empathy, compassion, education, and resources to those in need.

Self Quiz
Ask yourself...
- What are the stages of grief?
- Why should nurses be familiar with the stages of grief?
- What purpose does grief serve?
End of Life Process
Phases of Dying
Although everyone experiences death differently and on their own terms, there are two main pathways that most people take before dying. The dying process can be broken up into two phases: the transitioning phase, and the actively dying phase. The amount spent in each phase varies from person to person.
The transitioning phase usually begins 2-3 weeks prior to death. Major changes in function and the ability to do activities of daily life are observed during this time. Patients may even begin falling prior to entering this phase. Becoming bedbound is common as one will begin to spend most of their time sleeping.
This means decreased responsiveness, less interest in normal activities and hobbies, decreased interaction with family and friends, and an overall decline in one’s interest in external factors. It is possible to be roused during this phase, but this may only be possible in short intervals. It is not uncommon for transitioning patients to speak to or about loved ones that have already passed away. They may even report seeing deceased family in the room with them (11).
This should not be feared and is an important part of a person’s dying process. Incontinence may also begin during this time and briefs will be needed. Perhaps one of the most noticeable and difficult changes to witness, especially by friends and family, is changes in appetite. Patients will begin to show less interest in food and liquids. A greater difficulty swallowing will become apparent. “Refusal of food and fluid by a dying person is a common occurrence, particularly as the body slowly shuts down, and this may be the evidence signifying an actively dying process rather than starvation” (11).
Lastly, symptoms like restlessness, agitation, and pain may arise and detract from one’s comfort level. Although most patients will spend about two weeks transitioning, time can vary from days to weeks. The transitioning phase can also be skipped altogether, depending on the person.
Once the transitioning phase has concluded, the actively dying phase will begin. Actively dying immediately precedes death. This phase is usually short, lasting about 48 hours. Once actively dying, death is imminent, and a patient is expected to pass away at any moment. This phase is markedly different from the previous phase, and symptoms tend to become more apparent. “The following five changes constitute objective evidence of the end of life: diminished daily living performance, decreased food intake, changes in consciousness and increased sleep quantity, worsening of respiratory distress, and end-stage delirium” (12).
One key difference is one’s ability to response to tactile or verbal stimuli. The actively dying patient is obtunded and no longer responds to external forces. There could be slight reactions, but nothing meaningful. This is a comatose state.
There are many observable changes, including changes in vital signs. Blood pressure begins to drop, heart rate speeds up and eventually slow, respiratory rate picks up, and temperature may become elevated. Respiratory differences tend to be the most common observable changes. Cheyne-Stokes may occur, and the overall breathing pattern can be very irregular. Apnea is also common (11).
Many patients experience what is known as the “death rattle”. This very noticeable sound is due to an accumulation of secretions in the upper airway. This is a hallmark of the actively dying phase, but it is not experienced by everyone. “Death rattle is a strong predictor of imminent death, and nearly 80% of people die within 48 hours after its onset” (11).
Skin changes also occur. The body may become cool to touch, cyanosis may develop in the nail beds of fingers and toes, and mottling can occur usually beginning in the lower extremities and later spreading to other parts of the body. Skin may also become very pale. Urine output will decrease and become concentrated as evidenced by an amber color.

Self Quiz
Ask yourself...
- What are the dying phases?
- What changes are observed when someone is transitioning?
- What are some expected physical changes in the active dying phase?
- What education should a nurse provide to someone taking care of a patient that is actively dying?
Nursing Assessment and Care
Since there are so many drastic changes observed during the transitioning phase, proper education is crucial for caregivers. Nurses should reassure them that what the patient is experiencing is normal and to be expected. “At the end of life, most patients are in a state of lethargy, wherein their consciousness progressively declines, and sleep duration increases; therefore, it is necessary to provide appropriate explanations to patients and their families so that they can accept these symptoms as part of the natural end-of-life process” (12).
Family members usually try to wake the sleeping transitioning patient and have them attempt activities that could be done in the past. This is dangerous for the pt and can lead to injuries and more agitation. Becoming bedbound is a major change and puts the patient at risk for pressure injuries and increased pain. Fragile skin combined with new episodes of incontinence are topics that should be discussed, and proper supplies should be used.
Other potential barriers to a peaceful transitioning period are force feeding and aspiration. Nurses should provide education on what is acceptable and needed at this point. Patients will not die of hunger or lack of water. Allowing the patient to eat and drink small amounts is okay (12).
This amount will decrease as the body starts shutting down. Ice chips can be used while the patient is still alert. Utilizing mouth swabs with water is enough to hydrate the oral cavity and keep the patient comfortable until the end. During this time, symptoms can seemingly come out of the blue.
A once calm patient can become highly agitated in a short period of time. Medications should be added timely to ensure that the patient has a peaceful death. Information on medication and interventions to control uncomfortable end of life symptoms like pain, agitation, and restlessness should be provided to caregivers. Hospice patients, for example, have a comfort kit with various medications to use during this time.
Medications can be used as needed or scheduled to keep patients comfortable. (12). As the patient enters the actively dying phase and becomes less alert and aware, it is important that friends and family continue to talk to the patient and keep conversations positive around the patient. Hospice nurses, for example, are sure to tell caregivers that hearing is the last thing to go, so they should continue to speak to their loved one. Since vital signs start to become abnormal, reassurance is usually needed to keep family comfortable.
Not all vital signs need to be taken in the final stages. Taking blood pressure, for example, could cause discomfort. Death education related to respiratory changes is imperative. “Abnormal breathing patterns such as shallow breathing sound become increasingly common starting 1 week before death” (12).
Caregivers should be informed that breathing too fast or too slow at this point is not an emergency and there are things that can be done to promote comfort like applying oxygen, keeping the head of the bed upright, and keeping the room cool. Medications can also be given to decrease the death rattle. It should be noted that patients do not experience discomfort from the death rattle.
Lastly, not having a bowel movement or passing urine during the last few days of life is normal and interventions are not needed. Education and support are especially important during the final phases of life. With their peaceful words and deep knowledge base, nurses can be instrumental in facilitating a peaceful death.

Self Quiz
Ask yourself...
- Is it reasonable to obtain vital signs every two hours? Why or why not?
- If the family expresses concern about changes in bowel or urinary habits, what can you say to reassure them?

Resources and Support
Planning, coordinating, and executing quality end of life care can be challenging for health care workers. This period can also be one of the most challenging times for both patients and their loved ones. There are available resources for health care workers, patients, and their loved ones that provide information on end-of-life care.
Hospice care is an invaluable resource and source of support. This is available to terminally ill patients with a life expectancy of 6 months or less.” Hospice care is the term given to the care provided when a patient is given a prognosis of death within 6 months, and they do not pursue curative treatments They focus on improving the quality of life which can mean many things” (10).
Care can be provided in any setting that a patient calls home. The hospice team includes a medical director, registered nurse, chaplain, social worker, home health aide, and often a nurse practitioner. Symptoms and care can be managed at home with the help of covered medications, supplies, and medical equipment. Hospice allows patients to reach their goal of dying peacefully at home. A bereavement team also provides support during the process. (10?)
Palliative care, another form of comfort care, can also be utilized to maintain comfort at the end of life. Unlike hospice, patients receiving palliative care do not need to have a life expectancy of 6 months or less. “Research found that timely EOL care discussions allowed family members to make use of hospice and palliative care services sooner and maximize their time with the patient” (6).
Nurses should be educated in other end of life resource topics such as advanced directives, POLST (Physician Orders for Life Sustaining Treatment), and Durable Medical Power of Attorney. Looking ahead and having meaningful discussions regarding end-of-life planning can help prevent the stress of needing to address these things when death is imminent.

Self Quiz
Ask yourself...
- What care options are there for patients at the end of life?
- What is the difference between palliative and hospice care?
- What tools can the nurse use to help patients in end-of-life planning?
Conclusion
End of life conversations have a profound impact on not only patient care, but also on the dying process itself. Research shows that when implemented appropriately, these conversations improve patient relationships with healthcare workers, lead to better outcomes, and allow for a more positive dying experience. Nurses play a critical role in end-of-life processes in many different settings. With education, practice, experience, and confidence, nurses can incorporate conversations about death and dying to provide quality care.
References + Disclaimer
- Substance Abuse / Chemical Dependency. Substance Abuse / Chemical Dependency | Johns Hopkins Medicine. (2019, November 19). Retrieved December 23, 2022, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/substance-abuse-chemical-dependency
- Substance abuse and addiction statistics [2022]. NCDAS. (2022, June 18). Retrieved December 23, 2022, from https://drugabusestatistics.org/
- Alcohol abuse. Harvard Health. (2014, December 5). Retrieved December 23, 2022, from https://www.health.harvard.edu/addiction/alcohol-abuse
- U.S. Department of Health and Human Services. (n.d.). Alcohol’s effects on the body. National Institute on Alcohol Abuse and Alcoholism. Retrieved December 26, 2022, from https://www.niaaa.nih.gov/alcohols-effects-health/alcohols-effects-body
- Mayo Foundation for Medical Education and Research. (2022, May 18). Alcohol use disorder. Mayo Clinic. Retrieved December 26, 2022, from https://www.mayoclinic.org/diseases-conditions/alcohol-use-disorder/symptoms-causes/syc-20369243
- Mayo Foundation for Medical Education and Research. (2022, May 18). Alcohol use disorder. Mayo Clinic. Retrieved December 26, 2022, from https://www.mayoclinic.org/diseases-conditions/alcohol-use-disorder/diagnosis-treatment/drc-20369250
- Centers for Disease Control and Prevention. (2022, December 12). Marijuana and public health. Centers for Disease Control and Prevention. Retrieved December 26, 2022, from https://www.cdc.gov/marijuana/index.htm
- Holland, K. (2022, September 14). What’s the difference between CBD vs. THC? Healthline. Retrieved December 26, 2022, from https://www.healthline.com/health/cbd-vs-thc#psychoactive-components
- Mayo Foundation for Medical Education and Research. (2022, October 25). Prescription drug abuse. Mayo Clinic. Retrieved December 27, 2022, from https://www.mayoclinic.org/diseases-conditions/prescription-drug-abuse/symptoms-causes/syc-20376813
- Prescription drug abuse statistics. NCDAS. (2022, May 2). Retrieved December 27, 2022, from https://drugabusestatistics.org/prescription-drug-abuse-statistics/
- Centers for Disease Control and Prevention. (2022, June 2). Death Rate Maps & Graphs. Centers for Disease Control and Prevention. Retrieved December 27, 2022, from https://www.cdc.gov/drugoverdose/deaths/index.html#:~:text=Opioids%E2%80%94mainly%20synthetic%20opioids%20(other,of%20all%20drug%20overdose%20deaths).
- Meth addiction: Facts, statistics & how meth changes you. American Addiction Centers. (2022, October 21). Retrieved December 28, 2022, from https://americanaddictioncenters.org/meth-treatment/facts
- Centers for Disease Control and Prevention. (2021, November 18). Other drugs. Centers for Disease Control and Prevention. Retrieved December 28, 2022, from https://www.cdc.gov/drugoverdose/deaths/other-drugs.html
- U.S. Department of Health and Human Services. (2022, December 19). Methamphetamine drug facts. National Institutes of Health. Retrieved December 28, 2022, from https://nida.nih.gov/publications/drugfacts/methamphetamine
- U.S. Department of Health and Human Services. (2022, December 19). Cocaine drug facts. National Institutes of Health. Retrieved December 28, 2022, from https://nida.nih.gov/publications/drugfacts/cocaine
- U.S. Department of Health and Human Services. (2022, December 19). Heroin drug facts. National Institutes of Health. Retrieved December 30, 2022, from https://nida.nih.gov/publications/drugfacts/heroin
- Centers for Disease Control and Prevention. (2022, May 23). Heroin. Centers for Disease Control and Prevention. Retrieved December 30, 2022, from https://www.cdc.gov/opioids/basics/heroin.html
- U.S. Department of Health and Human Services. (2022, December 19). Naloxone drug facts. National Institutes of Health. Retrieved December 30, 2022, from https://nida.nih.gov/publications/drugfacts/naloxone
- U.S. Department of Health and Human Services. (2022, December 20). Hallucinogens drug facts. National Institutes of Health. Retrieved December 30, 2022, from https://nida.nih.gov/publications/drugfacts/hallucinogens
- Shmulewitz, D., & Walsh, C. (2022, August 18). New Study estimates over 5.5 million U.S. adults use hallucinogens. Search the website. Retrieved December 30, 2022, from https://www.publichealth.columbia.edu/public-health-now/news/new-study-estimates-over-55-million-us-adults-use-hallucinogens
- Drugs, brains, and behavior: The science of addiction. (2020, June). Retrieved April 10, 2021, from https://d14rmgtrwzf5a.cloudfront.net/sites/default/files/soa.pdf
- Risk factors for addiction. (2017, February 14). Retrieved April 10, 2021, from https://drugfree.org/print/article.php?id=60743
- Gray, K. M., & Squeglia, L. M. (2018). Research Review: What have we learned about adolescent substance use?. Journal of child psychology and psychiatry, and allied disciplines, 59(6), 618–627. https://doi.org/10.1111/jcpp.12783
- Alzheimer’s disease fact sheet. (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet
- Preventing Alzheimer’s disease: What do we know? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/preventing-alzheimers-disease-what-do-we-know
- How is Alzheimer’s disease treated? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/how-alzheimers-disease-treated
- Castro-Aldrete, L., Moser, M. V., Putignano, G., Ferretti, M. T., Diemch, A. S., and Chadha, A. S. (2023). Sex and gender considerations in Alzheimer’s disease: The Women’s Brain Project contribution. Frontiers in Aging Neuroscience, 15, 1-11. https://doi.org/10.3389/fnagi.2023.1105620
- Cararini, C., Russo, M., Dono, F., Barbone, F., Rispoli, M. G., Ferri, L., Di Pietro, M., Digiovanni, A., Ajdinaj, P., Speranza, R., Granzotto, A., Frazzini, V., Thomas, A., Pilotto, A., Padovani, A., Onofrj, M., Sensi, S. L., & Bonanni, L. (2021). Agitation and Dementia: Prevention and Treatment Strategies in Acute and Chronic Conditions. Frontiers in neurology, 12, 644317. https://doi.org/10.3389/fneur.2021.644317
- Alzhimer’s Disease: Common Medical Problems. (n.d.). Retrieved January 9, 2024, 10, 2021, from https://www.nia.nih.gov/health/alzheimers-caregiving/alzheimers-disease-common-medical-problems #7 Wandering and Alzhimer’s Diease. (n.d.). Retrieved January 9, 2024, from https://www.nia.nih.gov/health/alzheimers-changes-behavior-and-communication/wandering-and-alzheimers-disease
- Agarwal, P., Kukrele, R., & Sharma, D. (2019). Vacuum assisted closure (VAC)/ negative pressure wound therapy (NPWT) for difficult wounds: A review. Journal of clinical orthopaedics and trauma, 10(5), 845–848. https://doi.org/10.1016/j.jcot.2019.06.015
- Baranoski, & Ayello, E. A. (2020). Wound care essentials: practice principles (5th ed.). Wolters Kluwer.
- George, J. et al. (2017). Negative pressure wound therapy: principles and usage in orthopedic surgery. In: Shiffman, M., Low, M. (eds) Pressure Injury, Diabetes and Negative Pressure Wound Therapy. Recent Clinical Techniques, Results, and Research in Wounds, vol 3. Springer, Cham. https://doi.org/10.1007/15695_2017_53
- McNichol, Ratliff, C., & Yates, S. (2021). Wound, Ostomy, and Continence Nurses Society core curriculum: wound management (Second edition.). Wolters Kluwer Health.
- Shiffman, M.A. (2017). History of negative pressure wound therapy (NPWT). In: Shiffman, M., Low, M. (eds) Pressure Injury, Diabetes and Negative Pressure Wound Therapy. Recent Clinical Techniques, Results, and Research in Wounds, vol 3. Springer, Cham. https://doi.org/10.1007/15695_2017_50
- Williams, L. S., & Hopper, P. D. (2019). Understanding medical-surgical nursing. F.A. Davis Company.
- Zaver V, Kankanalu P. Negative pressure wound therapy. (2022). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK576388/
- Basiri, R., Spicer, M. T., Levenson, C. W., Ormsbee, M. J., Ledermann, T., & Arjmandi, B. H. (2020). Nutritional supplementation concurrent with nutrition education accelerates the wound healing process in patients with diabetic foot ulcers. Biomedicines, 8(8), 263. https://doi.org/10.3390/biomedicines8080263
- Beyene, R. T., Derryberry, S., & Barbul, A. (2020). The effect of comorbidities on wound healing. Surgical Clinics of North America, 100(4), 695–705. https://doi.org/10.1016/j.suc.2020.05.002
- Bishop, A., Witts, S., & Martin, T. (2018). The role of nutrition in successful wound healing. Journal of Community Nursing, 32(4), 44–50.
- Ellis, S., Lin, E. J., & Tartar, D. (2018). Immunology of wound healing. Current Dermatology Reports, 7(4), 350–358. https://doi.org/10.1007/s13671-018-0234-9
- Ghaly, P., Iliopoulos, J., & Ahmad, M. (2021). The role of nutrition in wound healing: An overview. British Journal of Nursing, 30(5), S38–S42. https://doi.org/10.12968/bjon.2021.30.5.s38
- Manley, S., & Mitchell, A. (2022). The impact of nutrition on pressure ulcer healing. British Journal of Nursing, 31(12), S26–S30. https://doi.org/10.12968/bjon.2022.31.12.s26
- Smith-Ryan, A. E., Hirsch, K. R., Saylor, H. E., Gould, L. M., & Blue, M. M. (2020). Nutritional considerations and strategies to facilitate injury recovery and rehabilitation. Journal of Athletic Training, 55(9), 918–930. https://doi.org/10.4085/1062-6050-550-19
- Talaska, K. (2020). A comparison of two protein supplements on the healing of stage iii and iv pressure injuries in enterally fed, ventilator dependent long – term care residents. Louisiana Tech Digital Commons. https://digitalcommons.latech.edu/theses/48
- Wei boon, Y., Azizan, N., Hasnol, E., Krishnan, K., Rajeswaran, S., Yin chow, J., Irwan, N., Indrajoth, P., Maran, munirah ismail, P., & Ismail, M. (2022). Potentials of immunonutrition in wound healing: A review. Jurnal Sains Kesihatan Malaysia, 20(2), 23–33. https://doi.org/10.17576/jskm-2022-2002-03
- Burgess-Stocks, Gleba, J., Lawrence, K., & Mueller, S. (2022). ostomy and continent diversion patient bill of rights. Journal of WOCN : Wound, Ostomy, and Continence Nursing., 49(3), 251–260. https://doi.org/10.1097/WON.0000000000000876
- Carmel, Colwell, J., & Goldberg, M. (2021). Wound, ostomy and continence nurse’s society core curriculum: ostomy management (Second edition.). Wolters Kluwer Health.
- Estrada, D. M. L., Benghi, L. M., & Kotze, P. G. (2021). Practical insights into stomas in inflammatory bowel disease: what every healthcare provider needs to know. Current Opinion in Gastroenterology, 37(4), 320–327. https://doi.org/10.1097/MOG.0000000000000737
- Hedrick, T. L., Sherman, A., Cohen-Mekelburg, S., & Gaidos, J. K. J. (2023). AGA Clinical Practice Update on Management of Ostomies: Commentary. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association, 21(10), 2473–2477. https://doi.org/10.1016/j.cgh.2023.04.035
- Hill, B. (2020). Stoma care: procedures, appliances and nursing considerations. British Journal of Nursing, 29(22), S14–S19. https://doi.org/10.12968/bjon.2020.29.22.s14
- Ogobuiro I, Gonzales J, Shumway KR, et al. Physiology, gastrointestinal. [Updated 2023 Apr 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537103/
- United Ostomy Associations of America, Inc. (2018). Know your ostomy pouching system & supplies. https://www.ostomy.org/know-your-ostomy-pouching-system-supplies/
- Urostomy and continent urinary diversion. (2006). U.S. Dept. of Health and Human Services, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
- Williams, L. S., & Hopper, P. D. (2019). Understanding medical-surgical nursing. F.A. Davis Company.
- American Association of Clinical Endocrinology (2021). What you need to know about diabetes. About Diabetes. https://www.aace.com/disease-and-conditions/diabetes/what-you-need-know-about-diabetes
- Berget, C., Messer, L. H., & Forlenza, G. P. (2019). A Clinical Overview of Insulin Pump Therapy for the Management of Diabetes: Past, Present, and Future of Intensive Therapy. Diabetes spectrum: a publication of the American Diabetes Association, 32(3), 194–204. https://doi.org/10.2337/ds18-0091
- Blonde, L., Umpierrez, G. E., Reddy, S. S., McGill, J. B., Berga, S. L., Bush, M., … & Weber, S. L. (2022). American Association of Clinical Endocrinology clinical practice guideline: developing a diabetes mellitus comprehensive care plan—2022 update. Endocrine Practice, 28(10), 923-1049.
- Center for Disease Control and Prevention. (2022). Estimates of diabetes and its burden in the United States. National diabetes statistics report. cdc.gov/diabetes/data/statistics-report/index.html
- Center for Disease Control and Prevention. (2022). Prevalence of both diagnosed and undiagnosed diabetes. https://www.cdc.gov/diabetes/data/statistics-report/diagnosed-undiagnosed-diabetes.html
- Center for Disease Control and Prevention. (2023). What is Diabetes? https://www.cdc.gov/diabetes/basics/diabetes.html
- ElSayed, N. A., Aleppo, G., Aroda, V. R., Bannuru, R. R., Brown, F. M., Bruemmer, D., … & Gabbay, R. A. (2023). 7. Diabetes technology: standards of care in diabetes—2023. Diabetes Care, 46(Supplement_1), S111-S127.
- Galicia-Garcia, U., Benito-Vicente, A., Jebari, S., Larrea-Sebal, A., Siddiqi, H., Uribe, K. B., Ostolaza, H., & Martín, C. (2020). Pathophysiology of Type 2 Diabetes Mellitus. International journal of molecular sciences, 21(17), 6275. https://doi.org/10.3390/ijms21176275
- Ganesan, K., Rana, M. B. M., & Sultan, S. (2018). Oral hypoglycemic medications.
- Feingold, K. R., Anawalt, B., Boyce, A., Chrousos, G., Dungan, K., Grossman, A, & Kopp, P. (2020). Oral and injectable (non-insulin) pharmacological agents for type 2 diabetes. South Dartmouth (MA).
- E. (2022). Pancreas hormones. https://www.endocrine.org/patient-engagement/endocrine-library/hormones-and-endocrine-function/pancreas-hormones
- Kreider, K. E. (2021). Patient-centered medication selection for type 2 diabetes: A collaborative, patient-centered approach that considers a variety of factors will be most effective. American Nurse Journal, 16(11), 33-37.
- Banday, M. Z., Sameer, A. S., & Nissar, S. (2020). Pathophysiology of diabetes: An overview. Avicenna journal of medicine, 10(4), 174–188. https://doi.org/10.4103/ajm.ajm_53_20
- Draznin, B., Aroda, V. R., Bakris, G., Benson, G., Brown, F. M., Freeman, R., & American Diabetes Association Professional Practice Committee. (2022). 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2022. Diabetes care, 45(Suppl 1), S125-S143.
- World Health Organization. (2023). https://www.who.int/news-room/fact-sheets/detail/diabetes
- Hospice and Palliative Nurse’s Association. (2023, September 14). Hospice and Palliative Credentialing Center. Retrieved from AdvancingExpertCare.org: https://www.advancingexpertcare.
- Connor, S., Fitch, K., Iwaski, K., & Pyenson, B. (2006). Comparing Hospice and Nonhospice Patient Survival Among Patients Who Die Within a Three-Year Window. Journal of Pain and Symptom Management, 238-46.
- Coyle, N., Ferrell, B., & Paice, J. (2023). Oxford Textbooks in Palliative Medicine. In Oxford Textbook of Palliative Nursing. New York: Oxford Academic.
- Encyclopedia Brittanica. (2023, September 14). Retrieved from Merriam-Webster.com: https://www.merriam-webster.com/
- National Hospice and Palliative Care Organization. (2023, September 14). Hospice Care Overview For Professionals. Retrieved from NHPCO.org: https://www.nhpco.org/hospice-care-overview/ References:
- Cho, J., & Trent, A. (2006). Validating a decisional conflict scale. Medical Decision Making, 26(4), 373-380.
- Mullaney, T., et al. (2019). Informed consent: The role of the nurse. Journal of Radiology Nursing, 38(2), 177-183.
- Betancourt, J. R., Green, A. R., & Carillo, J. E. (2002). Cultural competence in health care: Emerging frameworks and practical approaches. The Commonwealth Fund.
- Institute of Medicine. (2000). To err is human: Building a safer health system. National Academies Press.
- American Nurses Association. (2019). Nursing: Scope and standards of practice. American Nurses Association
- National Hospice and Palliative Care Organization. (n.d.). History of Hospice Care. Retrieved from https://www.nhpco.org/about/hospice-care/history-of-hospice-care/
- Hospice UK. (n.d.). The History of Hospice Care. Retrieved from https://www.hospiceuk.org/about-hospice-care/the-history-of-hospice-care
- Philosophy 1. World Health Organization. (202).0 Palliative Care. Retrieved from https://www.who.int/news-room/fact-sheets/detail/palliative-care
- American Academy of Hospice and Palliative Medicine. (n.d.). History of Hospice and Palliative Medicine. Retrieved from https://aahpm.org/about/history-of-hospice-and-palliative-medicine
- Centers for Medicare & Medicaid Services. (n.d.). Medicare Benefit Policy Manual: Chapter 9 – Coverage of Hospice Services Under Hospital Insurance. Retrieved from https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c09.pdf
- Hospice and Palliative Credentialing Center. (n.d.). CHPN – Certified Hospice and Palliative Nurse. Retrieved from https://www.nhpco.org/certification/chn-certified-hospice-nurse/
- National Hospice and Palliative Care Organization. (nice.d Nurse.). Hosp. Retrieved from https://www.nhpco.org/about/hospice-care/hospice-nurse/
- Patient-centered care(Reference: Institute of Medicine. (2014). Dying in America: Improving quality and honoring individual preferences near the end of life. National Academies Press).
- Shared decision making(Reference: Elwyn, G., et al. (2012). Shared decision making: A model for clinical practice. Journal of General Internal Medicine, 27(10), 1361-1367). 4.
- Psychosoc(Reference: Balboni, T. A., et al. (2010). Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Internal Medicine, 170(15), 1109-1117).
- Pain and symptom management (Reference: Ferrell, B. R., et al. (2017). Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. Journal of Clinical Oncology, 35(1), 96-112).
- Institute of Medicine. (2014). Dying in America: Improving quality and honoring individual preferences near the end of life. National Academies Press.
- Breen, C. M., Abernethy, A. P., & Abbott, K. H. (2011). Conflict associated with decisions to limit life-sustaining treatment in intensive care units. Journal of General Internal Medicine, 26(4), 389-394.
- Elwyn, G., et al. (2012). Shared decision making: A model for clinical practice. Journal of General Internal Medicine, 27(10), 1361-1367.
- Balboni, T. A., et al. (2010). Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Internal Medicine, 170(15), 1109-1117.
- Ferrell, B. R., et al. (2017). Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. Journal of Clinical Oncology, 35(1), 96-112.
- San Filippo, D. (2006). Philosophical, Psychological & Spiritual Perspectives on Death & Dying. Faculty Publications. 31. https://digitalcommons.nl.edu/faculty_publications/31
- Kyota, A. & Knda, K. (2019). How to come to terms with facing death: a qualitive study examining the experiences of patients with terminal cancer. https://doi.org/10.1186/s12904-019-0417-6
- Peters, L. et al. (2013). How death anxiety impacts nurses’ caring for patients at the end of life: a review of literature. The open nursing journal, 7, 14–21. https://doi.org/10.2174/1874434601307010014
- Bergenholtz, H. et al. (2020). Talking about death and dying in a hospital setting- a qualitative study of the wishes for end-of-life conversations from the perspective of patients and spouses. https://doi.org/10.1186/s12904-020-00675-1
- Oates J.R. & Maani-Fogelman P.A. (2022). Nursing Grief and Loss. https://www.ncbi.nlm.nih.gov/books/NBK518989/
- Bodi, S., Matus, C., & Hickey, D. (2022). Right place, right time: Facilitating end-of-life conversations. The Journal of family practice, 71(2), 74–79. https://doi.org/10.12788/jfp.0333
- Pentaris, P., & Tripathi, K. (2022). Palliative pProfessionals’ Views on the Importance of Religion, Belief, and Spiritual Identities Toward the End of Life. International journal of environmental research and public health, 19(10), 6031. https://doi.org/10.3390/ijerph19106031
- Lin, H. Y. et el. (2021). Nurses’ knowledge, attitude, and competence regarding palliative and end-of-life care: a path analysis. PeerJ, 9, e11864. https://doi.org/10.7717/peerj.11864
- Becker, C. et al. (2020). Communication challenges in end-of-life decisions. Swiss medical weekly, 150, w20351. https://doi.org/10.4414/smw.2020.20351
- Oates J.R. & Maani C. V. Death and Dying. [Updated 2022 Nov 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK536978/
- Ijaopo, E. O. et al. (2023). A Review of Clinical Signs and Symptoms of Imminent End-of-Life in Individuals With Advanced Illness. Gerontology & geriatric medicine, 9, 23337214231183243. https://doi.org/10.1177/23337214231183243
- Lee, E. K. et el. (2021). End-of-Life Assessments and Communication for Dying Patients and Their Families. Journal of hospice and palliative care, 24(3), 194–197. https://doi.org/10.14475/jhpc.2021.24.3.194
- Onishi H. (2021). Communication at the End of Life. Journal of hospice and palliative care, 24(3), 135–143. https://doi.org/10.14475/jhpc.2021.24.3.135
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
