Course
Rotator Cuff Treatment and Recovery
Course Highlights
- In this Rotator Cuff Treatment and Recovery course, we will learn about and improve understanding of the anatomy and pathophysiology of rotator cuff injuries.
- You’ll also learn and improve understanding of the anatomy and pathophysiology of rotator cuff injuries.
- You’ll leave this course with a broader understanding of knowledge of rotator cuff pathophysiology and treatments to provide patient education for individuals with rotator cuff tears, especially for those undergoing surgery.
About
Contact Hours Awarded: 2
Course By:
Jillian Hay-Roe BSN, CIC
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
If you ever care for patients with orthopedic problems, you will certainly be familiar with shoulder injuries. You may already have first-hand experience with your own shoulder injury. Shoulder pain affects millions of people every year, necessitating medical care to provide relief and restore function. Since this is such a common problem, it is worthwhile to explore this subject in depth. There is a high likelihood that you or someone you know personally has experienced this affliction.
This course will primarily focus on rotator cuff tears, as it is the most common diagnosis for people presenting with shoulder pain. First, we need to review the basics of shoulder anatomy. Then, we will delve into how to diagnose and finally fix the shoulder problem. The primary focus will be on perioperative nursing care with specifics that apply to rotator cuff repair surgery. Important points to provide during patient education will also be covered.
Basic Shoulder Anatomy
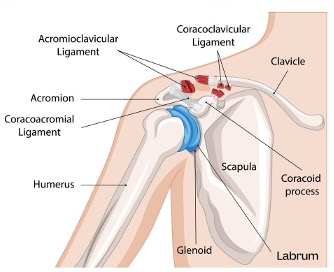
The shoulder joint, also known as the glenohumeral joint, has the most extensive range of motion of any joint in the human body. Within the shoulder are several muscles, tendons, and ligaments that are collectively referred to as the rotator cuff. The three primary bones that make up the shoulder include:
- Humerus – the bone that supports the upper arm. The top of this bone ends in a spherical shape covered in slippery articular cartilage that can rotate around in the socket joint of the shoulder blade.
- Scapula – the triangular-shaped bone in the back, also known as the shoulder blade. The ball and socket connection made between the scapula and the humerus is referred to as the glenoid.
- Coracoid Process – The point where shoulder muscles attach to the bone.
- Acromion – the highest point of the bone that meets the clavicle (collarbone) to form the acromioclavicular (AC) joint.
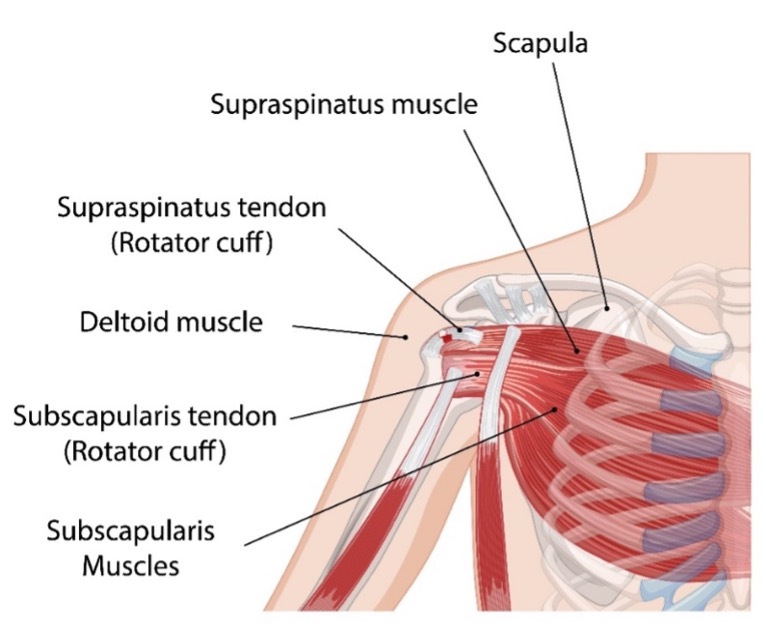
Four primary muscles make up the rotator cuff. The muscles end in tendons which attach to the bones and support the function of the shoulder.
- Supraspinatus – This muscle is positioned at the top of the shoulder underneath the clavicle and attaches to the top of the humerus. This functions to abduct the humerus.
- Subscapularis – This functions to internally rotate and abduct the humerus.
- Infraspinatus – This functions to externally rotate the humerus.
- Teres Minor – This is right below the infraspinatus muscle and assists with external rotation and abduction of the humerus.
Other important components that make up the shoulder joint:
- Bursa – Small sacs of fluid that provide lubrication to help the tendons glide smoothly when moving the arm.
- Labrum – The cup of cartilage that holds the head of the humerus, which adds to the glenoid surface area and serves as an attachment point for several ligaments and tendons. It helps to provide shoulder stability.
- Ligaments – These are bands that form a capsule to hold the shoulder joint together. Important structures include the glenohumeral ligaments and the coracromial ligaments.
- Synovium – A thin membrane that produces synovial fluid which lubricates the joint.
The muscles and bones of the chest and back also provide support to the shoulder joint. These include the pectoralis major and minor, the deltoids, the biceps, the trapezius, and the serratus anterior.
(1,5)
[A, B]

Self-Quiz
Ask Yourself...
- What anatomical structure of the shoulder is most likely to be injured?
- What areas of the shoulder may be susceptible to inflammation when injured
Pathophysiology
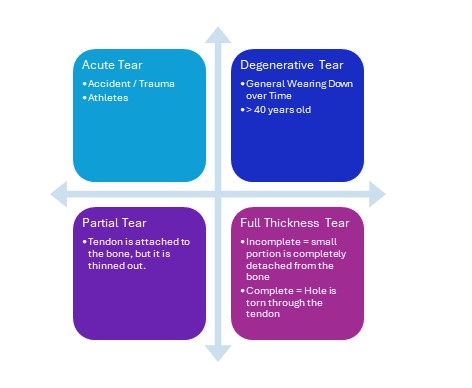
One of the most common shoulder injuries is a rotator cuff tear, where the tendon is separated from the bone. These injuries are classified as an acute tear, which is related to an accident or trauma related injury; or a degenerative tear, which is the result of gradual wearing down of the tendon over time. In many cases the tendon starts to fray and then will eventually tear when strained.
Separation of the tendon from the bone can vary in severity. The tear may only be partial, where only a thin amount of tendon remains attached to the bone. The tear can also be classified as a full-thickness tear. When a small portion of the tendon is completely detached from the bone, it is considered a full thickness incomplete tear. With a full thickness complete tear, a hole has been torn through the tendon. The most common tear is with the supraspinatus muscle tendon.
(2)
Case Study
A 52-year-old female, Ms. Smith, presents with shoulder pain. She has been a lifelong swimmer and still goes to swim laps several days a week. She reports pain on both sides, only a small amount of pain on the left, but significant pain on the right. The nurse practitioner suspects a degenerative rotator cuff tear.

Self-Quiz
Ask Yourself...
- What factors contributed to this patient’s injury?
Epidemiology – How Common is this?
Rotator cuff tears are very common. It is estimated that 2 million cases are diagnosed annually. Degenerative tears are the most common and begin to become more prevalent after the age of 40. People who often need to lift or perform overhead activities, like baseball pitchers or painters are also at high risk. (1) There are at least 75,000 rotator cuff repair surgeries done annually in the United States, and that number has shown continued growth annually. (3)
Clinical Signs and Symptoms
Pain is the most common presenting symptom that prompts patients to seek treatment. Common complaints are pain or weakness during specific movements when using the shoulder and being unable to move the joint completely in certain positions. Patients may describe that they have pain even at rest that makes it difficult to sleep. Patients who have experienced a more acute injury may describe that they heard a ‘pop’ or ‘snap’ when the injury occurred. Others, who have a degenerative injury may not have pain, and may just experience weakness and limitations in range of motion. Because the shoulder joint allows movement in more directional planes than any other joint in the body, a thorough range of motion assessment is important to help to diagnose areas of injury (2).

Self-Quiz
Ask Yourself...
- A 30-year-old patient presents with shoulder pain. What are some of the likely causes for shoulder pain?
- The average age of a patient seen by an orthopedic surgeon is 62 years old. What would you suspect the most common diagnosis and surgical repair made for this surgeon would be?
Assessment
Assessment consists of physical exam and imaging studies. Components of the physical exam will include:
- Subjective Assessment:
- Patient reports of pain
- Sensation – burning, aching, dull, sharp, etc.
- Severity – utilize pain scale, changes in pain severity with movement
- Aggravating factors – which movements increase pain
- Relieving factors – e.g. medications, ice, activity modification
- Activities of daily living (ADL) limitations – Shoulder pain can be severe enough that it causes pain at rest and can cause sleep disturbances. Trouble getting dressed is often reported, specifically, women putting on a bra. Shoulder problems can prevent people from being able to work and keep athletes out of the game.
- Physical Assessment:
- Obvious physical deformities – asymmetry, swelling, tenderness upon palpation
- Arm strength
- Presence of crepitus
- Cervical Spine Exam
- Range of Motion: Several different tests identify range of motion to help determine areas of shoulder injury. They include some of the following:
(4,5)
Range of Motion Tests
|
[D] |
|
Rotator Cuff Muscle Injury Tests |
|
|
Supraspinatus Test
Patient abducts both arms to 90° then brings them forward with a 30° forward flexion. Then the patient will push upward against resistance. This muscle is then further tested with the empty can test which is done by rotating the arms from a thumbs up position to a thumbs down position.
|
[E] |
|
Infraspinatus and Teres Minor Testing
Have the patient flex the forearms at 90° with palms facing up. Then have the patient rotate shoulders moving the forearms out to the sides against resistance. |
[D] |
|
Subscapularis
Ask the patient to put the back of their hand on the small of their back. Then passively pull the hand away from the back until full internal rotation of the shoulder away from the back. Ask the patient to keep holding their hand in place away from their back. If the patient is unable to hold their hand away, this is called a positive internal rotation lag sign. For the Gerber’s Lift Off test ask the patient to move their hand away from their back against resistance. |
[F] |
|
Impingment Tests (5)
|
|
|
Neer’s test
This test allows demonstration of pain during passive abduction of the arm. The provider will stabilize the scapula, then the arm is turned so that the thumb points down, then it is lifted in the air.
|
[G] |
|
Hawkins-Kennedy Test
The provider will hold the upper arm 90° at the scapular plane (i.e. upper arm is up in the air parallel to the ground). The elbow is bent to 90°. While the upper arm is supported in the air, the lower arm is turned passively into internal rotation. If this elicits pain, the test is positive.
|
[D] |
Imaging Studies
Typically, the next step is to get an X-ray. The X-ray will not show the muscle and tendon tear, but it will be used to identify contributing causes. X-rays will be used to find problems with the bones which can be contributing to shoulder problems. This may include injuries to surrounding bones, for example, if the injury was the result of a fall and the clavicle was fractured.
X-rays can show the presence of bone spurs, also known as osteophytes. These may be causing pain by digging into the muscle or nerves causing an impingement. Wearing cartilage can also be seen on an X-ray, which indicates arthritis. More on that below.
To look at the soft tissues, an MRI will be ordered. These allow the provider to visualize the presence and location of a tear, the severity of the tear, and even if the tear is fresh or in healing stages. These can be up to 95% effective in helping to diagnose a rotator cuff tear. Alternatively, a CT scan and ultrasound may be sufficient to visualize injuries, particularly for dislocations and signs of adhesive capsulitis (also known as frozen shoulder).
(2,5)
Case Study
The nurse practitioner assesses Ms. Smith and has the following significant findings:
| Left Shoulder | Right Shoulder | |
| Pain at rest | 0/10 | 1-2/10 |
| Pain upon movement | 1/10 | 6-8/10 |
| ROM Forward Flexion | 100° | 30° |
| Supraspinatus test | 5/5 | 2/5 |
| Neer | Positive Left < Right | Positive |
| Hawkins-Kennedy | Negative | Positive |

Self-Quiz
Ask Yourself...
- What are possible diagnoses for Ms. Smith based on the given assessment data?
- Are there any other orders you would anticipate?
- A patient presents with shoulder pain. In what order should the provider move through their exam?
- A provider strongly suspects the cause of shoulder pain to be arthritis. What imaging studies would the provider need to order?
Treatment
Unless the tear was substantial, for example, one resulting in a traumatic acute injury, non-surgical treatment is sufficient. Evidence supports that there is improvement in pain and function in 80-85% of people without surgical intervention. (2).
- Rest – Limit movements of the shoulder that aggravate the tendon tears. The tear can worsen over time if it continues to be strained. A sling is typically not necessary. ⁸
- Ice – May also help reduce swelling and decrease pain.
- Over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs) – Can be taken as needed for pain. If non-opioid pain medications are not sufficient to keep pain tolerable, other therapies should be considered before a long-term opioid prescription regimen should be considered.
These treatments are common sense, and most people try them before even seeking advice from a provider. The next treatments do require a provider’s order.
- Physical therapy and home exercise programs – Strengthening supportive muscles while preventing further injury to the tear can help to improve function.
- Cortisone steroid injections – Steroids that have an anti-inflammatory effect are injected directly into the shoulder area. The injection itself can be painful and is often administered in combination with a local anesthetic. Cortisone injections are not effective for approximately one-third of patients.
For the patients who do experience relief, it is only expected to last temporarily. It may last for a few weeks or months. Injections should only be administered once every three months to avoid other negative effects from the repeated use of steroids. The efficacy also tends to decline after repeated injections.
- Peripheral Nerve Stimulators (PNS) – This is a therapy developed in the 1960s where electrical currents are sent to innervate specific nerves to decrease pain. This may be a helpful therapy for individuals who haven’t had relief from other modalities and who are not good candidates for repair surgery. (6) The electrodes can be implanted surgically, or with surface skin electrodes with Transcutaneous electrical nerve stimulation (TENS).
- Platelet-rich plasma – (PRP) Is a relatively new treatment that is increasing in popularity as research continues to determine its efficacy. For PRP, a blood sample of approximately 30-60mL is drawn from the patient. The sample is then centrifuged to separate blood components. The patient’s plasma, which has a high level of concentrated platelets, is then injected back into the injured joint area. It is hypothesized that the platelets release growth factors that aid in tissue repair. (9). A word of caution: this therapy may not be covered by health insurance.
- Surgical – While it is always best to avoid surgery unless necessary, health insurance often also requires evidence that several non-surgical options are attempted. If there has not been improvement, often over six months, surgery is then typically recommended for patients.
(2,7)
Case Study
The orthopedic surgeon reviews Ms. Smith’s imaging results and performs a focused physical exam. The surgeon, Dr. Brone, explains that she has a supraspinatus tear on the right side as well as a significant acromial bone spur causing an impingement. The doctor identified a small bone spur on the left, and signs of typical muscle degeneration associated with aging, but no major areas for concern. There is evidence of some bilateral cartilage degeneration bilaterally.
Dr. Brone has discussed treatment options with Ms. Smith. She had to stop swimming about three weeks ago due to the pain and has been taking NSAIDs PRN. She will start using ice. She is interested in learning more about PRP treatment since she had a friend report good results when she received it for Tennis Elbow.

Self-Quiz
Ask Yourself...
- What exercises and activity parameters should the doctor recommend to Ms. Smith?
- If the patient states they are miserable with shoulder pain and wishes to proceed directly to surgery, how should the healthcare provider respond?
- A patient states their sibling had a similar shoulder problem, and nothing helped much. How should the healthcare provider respond?
Rotator Cuff Repair Surgery
Rotator cuff repairs are almost always considered to be elective surgery, and relatively safe. Shoulder surgeries were originally performed as open repairs, with a traditionally long incision. However, these are now only rarely done if the tear is large and complex, for example, if a tendon transfer or graft repair is needed.
Most rotator cuff repairs are done arthroscopically, where only three to five small incisions (approx. 1cm long) are made. A very small camera, called an arthroscope, is inserted and it allows the surgeon to visualize the area and make the repair. The surgery is usually 1-2.5 hours long and can be done in an outpatient surgery center. In some cases, the patient may only need a mini-open repair, where only a single incision is needed, which is about 3cm long. The patient can go home after spending an hour or two in the recovery room.
(7)
Pre-operative Care
Standard pre-operative care will apply to a shoulder surgery patient. Nurses often prepare the patient for surgery, which includes providing education about what to expect on the day of surgery. They will review the patient’s medical history and medications and alert the surgeon and anesthesiologist if there are any red flags to be further assessed.
Once the patient has arrived at the surgery center, a pre-operative nurse will review medical history, informed consent with the surgeon that he has completed, and perform a brief physical assessment. The pre-op nurse will get the patient into a gown, make sure there is IV access in the non-operative arm, and apply a cardiac ECG monitor, blood pressure cuff, and pulse oximetry. They may also prepare prophylactic IV antibiotics that should be administered no more than one hour before surgery start time. Throughout the perioperative process, along with the OR nurse, they make sure safety time-out checks are performed.
A Note about Informed Consent
It is the physician’s responsibility to conduct informed consent with the patient prior to the surgery. Informed consent means that the surgeon has explained what will happen during the surgery, the benefits and risks of the procedure in a way that the patient understands. The patient must have the opportunity to have any questions answered. It is the duty of the nurse to ensure that all aspects of the conversation have occurred between the doctor and patient, or their guardian/power of attorney. The patient and doctor will then sign an informed consent document that contains all this information. The nurse may need to also sign the document that they witnessed the informed consent process. On the day of surgery, the informed consent document will be verified to ensure that it was properly completed and that the correct procedure is being done for the correct patient.
Rotator Cuff Surgery Benefits and Risks Discussed
The benefits of the surgery are straightforward. The procedure is being done because it will help restore shoulder function and reduce pain, overall improving the patient’s quality of life. The surgery is necessary due to the nature of the tear, natural healing and other conservative treatments have proven to be ineffective at allowing the patient to return to baseline status.
The risks for any surgery always include the possibility of infection. During the surgery a variety of complications can occur, for example, accidentally hitting a blood vessel leading to uncontrolled bleeding. Nerve injury or permanent damage similarly may occur. Muscle detachment may occur, particularly the deltoid muscle. Tendon retear may occur, the larger the initial tear was, the higher the chance a retear may occur. The patient may develop stiffness, and lose range of motion, from scarring or adhesions. Adhering to home exercise programs and physical therapy will greatly reduce the chances of this happening.
While some risks can happen during the surgery, there are chances problems will arise after the patient has been discharged. Patients should be educated that they need to adhere to discharge instructions, so they don’t cause a problem leading to a negative outcome.
(7)


Self-Quiz
Ask Yourself...
- A 16-year-old patient requires shoulder surgery. Who should be involved in the informed consent process?
Case Study
After a few months with no improvement, Ms. Smith decides to proceed with surgery. The patient is told she can shower starting the day after surgery and lightly clean the surgical wounds. A week later, the patient attends the boat party decides to go swimming and ends up developing an infection. The patient had assumed that since she could shower, it would be okay if the wound got wet when swimming. The patient required an extensive antibiotic course to treat the infection.

Self-Quiz
Ask Yourself...
- Who is responsible for providing the patient with education about preventing complications? When should this teaching be done?
- After the surgeon discusses informed consent, the patient is very concerned about the risks involved. How can the healthcare provider respond?
A Note about Nerve Blocks
A nerve block is a procedure done before surgery to provide analgesia for the patient. This procedure is done by administering an injection of a numbing medication around a major nerve, which will cause an extremity to be numb for several hours. The effects of the nerve block can last anywhere from 6-24 hours. Most patients cannot feel or move their entire arm after the block is performed. This helps reduce the amount of anesthetic medication given to the patient during surgery and reduce the amount of pain, and subsequent opioid medication the patient will need post-operatively. Typically, a nerve block procedure will then be performed by an anesthesiologist, and nurses may need to assist with this procedure.
(10)
Interscalene Nerve Block Procedure
The anesthesiologist uses a point of care ultrasound machine to locate the brachial plexus nerve roots, at the interscalene location, which they find at the base of the neck where it meets the top of the shoulders. They then will use a long needle to inject between 15-30mL of bupivacaine, or other similar numbing medication just around the nerve. Prior to this, the patient will either be given moderate sedation or will already be put under surgical anesthesia. Pre-op sedation is done with a benzodiazepine, like Midazolam (Versed©) and possibly an opioid like Fentanyl. Of course, each process will vary between each surgery center, and each anesthesiologist, who develops a custom plan for each patient.
nerve block is usually done with sedation for a few reasons. Moderate sedation allows the patient to feel relaxed. Most people already feel some degree of anxiety before surgery. Allowing the patient to relax helps decrease the chances the patient will flinch or move during this procedure.
The procedure involves a large needle injecting a large amount of fluid close to the neck, which can be a scary experience for people, even though it only causes minor discomfort. Besides, the patient is already NPO and will be receiving general anesthesia for the surgery anyway. However, it is helpful to keep the patient somewhat awake because they can let the anesthesiologist know if they feel nerve contact, which is a zing or electrical sensation down the nerve if the needle has made contact.
(10)
Nerve Block Risks
Prior to the nerve block, the anesthesiologist should review risks and benefits with the patient and obtain informed consent. A nerve block is a safe procedure, however, there is a chance that permanent paralysis can result if the nerve itself is accidentally injected or injured. When performing this injection, the needle is moved around with ultrasound guidance, so aspiration is done throughout the procedure to ensure that blood return is not present, indicating that the needle tip has not inadvertently entered a blood vessel or the nerve itself. Nurses often help with aspirating and injecting the syringe so that the anesthesiologist has both hands available to manipulate the needle and ultrasound probe
Perioperative nurses should be familiar with how to care for patients undergoing moderate sedation, which includes monitoring their vital signs, particularly their respiratory status. The patient may need supplemental oxygen and be reminded to take deep breaths. The perioperative team should also be familiar with the potential for local anesthetic systemic toxicity (LAST) which is often simply referred to as lidocaine toxicity. Although very rare, perioperative healthcare workers need to receive education about this syndrome.
Another syndrome requiring healthcare education especially for upper extremity nerve blocks is Horner’s syndrome. It is “caused by local anesthesia spread to the cervical sympathetic chain causing an ipsilateral stellate ganglion block, with a reported incidence in 6% to 12% of cases.” (Juels MD & Juels, 2023)This is temporary and goes away when the nerve block wears off.
Hoarseness may also occur and may also be exacerbated by intubation during surgery. Patients may also feel like they cannot take a deep breath due to suppressed feeling in the diaphragm nerve. Breathing difficulty should always be assessed for other possible causes. Swallowing should also be assessed in the post-operative period to make sure patients do not have problems.
(10).

Self-Quiz
Ask Yourself...
- What is important for the patient to know about the nerve block post-operatively?
- The patient asks why the surgeon doesn’t inject numbing into their shoulder during the surgery. How can the nurse or anesthesiologist respond?
Inside the Operating Room
OR Table Positioning
The patient is either positioned in a lateral decubitus position or beach chair position. Each comes with pros and cons.
| Lateral Decubitus | Beach Chair | |
| Position | Patient lays flat on their non-operative side with knees flexed and the head neutral. A beanbag is used to help support the position. The patient is then tilted upward 30 degrees. The operative arm is wrapped in a stockinet or coban wrap and pulled up and away in a traction device. | The patient is supine on an operating table that allows the patient to be in an upright high fowler sitting position. A light foam piece is placed around the head so it can be secured in a neutral position. |
| Key Considerations | The traction allows the arm to be moved in several different directions allowing for change in access points. Only 10-20 pounds of weight should be used for traction. | Placing a cushion beneath the knees prior to elevating the trunk, maintain neutral alignment of the head and use a positioning device to control the arm. |
| Pros | Traction increases the working area for the surgeon inside the joint. | Anatomic position is maintained |
| Cons | May require repositioning or reaching around the arm to access all areas |
Risk of cerebral hypoperfusion Patient’s head can block access to certain areas |
Positioning is very important so that the surgeon can access the structures at the precise necessary angles. For both positions, the circulator nurse must ensure that there is adequate padding underneath the body. Bony prominences, in particular, should be checked. Even specialty booties or padding are placed on the feet to protect the ankles.
Sequential compression devices (SCDs) are typically included in facility protocol to prevent the development of VTE (venous thromboembolism) and are applied to the calves of any patient undergoing a procedure that is anticipated to be an hour or longer. The patient will have safety straps applied to keep them in place on the operating room table.
(3,11,13)
Once the patient is safely positioned on the operating room table the skin anti-septic preparation can begin. One member of the surgical team will hold the patient’s operative limb up and away from the body. Another member will cleanse the patient’s skin extensively, far exceeding the boundaries where surgery will be performed. Cleaning starts with the incision areas first, the top of the shoulder and will extend outward to the chest to near the top of the nipple line, down the arm, cleaning the axilla last. Typically, a colorful chlorhexidine solution will be used, either by itself or in combination with an alcohol solution. The bright color of the solution helps indicate the areas that have been prepped.
After the solutions have been applied and allowed to dry (usually a few minutes), a stockinet is applied over the hand and rolled up the forearm. This will be secured with a coban and will allow the arm to be held into place in either traction or on the beach chair attachment positioner. Drapes with adhesive edges will be placed, covering the entire patient except for the surgical arm. The incision sites will be marked. The shoulder may be covered with a transparent surgical adhesive drape (IO-ban, which is similar to a Tegaderm except bigger and thicker and has an antimicrobial solution embedded in it) that the surgeon cuts directly through.
(11)

Self-Quiz
Ask Yourself...
- If the sterile technique is broken during the prepping phase, how should the surgical team proceed?
- Why would SCD sleeves be applied to the patient’s calves if this is an upper extremity surgery?
- Why are surgical patients at higher risk of blood clots?
Time Out
Before any surgery or invasive procedure, a time-out needs to be conducted. During the time-out all members of the surgical team must be present and need to stop any tasks they are currently doing to participate. Timeouts are also completed before anesthesia is given and before nerve block procedures. The surgeon is ultimately responsible for initiating the surgical time-out procedure, but the circulator often takes an active role in going through the checklist items. During the time out, all members are expected to speak up if they think that there is a problem. Elements of the time-out procedure include:
- Correct Patient: The correct patient is verified with two identifiers on the patient’s name band, and that these match the completed informed consent document. Allergies are reviewed.
- Correct site/side/procedure: The team should agree on what repairs are being done on the correct limb and the expected procedure method. The site will be visibly marked on the patient’s skin.
- Correct equipment: All implants are present and unexpired. All equipment is sterile and working. Pre-operative MRI and X-ray images are available.
(14)

Self-Quiz
Ask Yourself...
- Can you imagine some scenarios that would cause someone to speak up regarding a concern during the time out?
- Why is it important that all members of the surgical team (anesthesiologist, scrub technician, circulating nurse, surgeon) participate in the pre-surgical time-out?
OR Circulator Nursing Duties
In addition to the standard tasks performed by an OR circulator nurse in any surgery, the following are specific for shoulder arthroscopic procedures:
- Arthroscopic Fluid – Sterile fluid is continually irrigated through the joint space which inflates the working area for surgeons to make necessary repairs. It also decreases bleeding. An important role of circulator nurses is to monitor fluid bags and change them out as needed during the procedure.
- Arthroscopy Tower – During the surgery, the nurse may also need to assist in adjusting arthroscopic screen images and monitors.
- Implants – To reattach the torn muscle tendon back onto the bone, the surgeon will implant permanent sutures and anchors into the patient. Nurses often work with implant manufacturer sales representatives who are present in the operating room during the surgery. Nurses must make sure that the correct sizes and materials are available and have not expired (3). The materials used for the anchor components have continued to evolve, and current popular options include:
- PEEK (Polyether ether ketone) – A non-degradable plastic. The patient can safely undergo airport metal detector screenings and MRIs without any concerns.
- Soft anchors – Sutures are passed through a fabric anchor sleeve or tape made of an ultrahigh molecular weight polyethylene (non-metallic). The advantages to this suture type are that they require a smaller hole in the bone and cause less disruption to the cartilage. However, these work better in patients with high-quality cortical bone.
(13)

Self-Quiz
Ask Yourself...
- What instructions should the nurse give to a post-op rotator cuff patient regarding going through metal detectors or having an MRI?
Arthroscopic Surgery Specifics
The surgical implements are inserted via very small incisions, usually only 1 cm long, and referred to as portals. Multiple portals are needed to place the necessary arthroscopic camera, irrigation fluid, and instruments. There may be references made to an angle of visualization and an angle of approach while the surgeon adjusts the instrumentation.
- Posterior Portal – This is used for initial viewing. It is placed in the back in a ‘soft spot’ by the medial glenoid, lateral humeral head, and superior rotator cuff. It is about 3cm distal to and medial to the posterolateral corner of the acromion.
- Anterolateral – This can be used when performing work on the acromion or when completing a subscapularis repair. It is in line with the anterior acromion about 3 cm distal to the lateral edge.
- Lateral – This is used for debriding the tear and for preparation of repair. It is made in line with the posterior clavicle and 4 cm lateral to the acromion.
(3,7)
During surgery, many different elements of shoulder injury may be repaired. A rotator cuff repair surgery may incorporate several elements of the following procedures.
- Acromioplasty – Refers to the removal of bone spurs (osteophytes) on the acromion (the endpoint of the acromial process where it meets the end of the clavicle).
- Bursectomy – Inflamed burse tissue is removed
- Subacromial decompression – This includes performing a bursectomy, coracoacromial ligament release, and acromioplasty.
- Debridement – Removal of injured and fragmented pieces of tissue, tendon, and bone. It is essentially cleaning up any debris found in the joint area.
- Biceps Tenodesis – If the patient has bicep tendonitis (described below), the patient may also require the damaged portion of the top of the bicep tendon to be removed and reattached to the top of the humerus.
- Labral Tears:
- SLAP Repair – stands for superior labrum anterior and posterior. For this injury, the biceps tendon is torn from the top of the labrum.
- Bankart Repair – Another type of labral tear when it is torn is called a Bankart Lesion. This usually is caused by a shoulder dislocation injury.
- A posterior labral tear can also occur at the back part of the socket.
The suture implants are most often performed as a double row, as there is evidence of a higher chance of success. However, in instances where there is the chance of a ‘high-tension repair,’ the surgeon may opt for a single-row repair.
After the surgery has been completed, the portals will be closed, either with surgical glue or with sutures, then covered with sterile strips (small white stickers). An outer bandage will then be applied. The OR nurse along with the scrub technician will complete an instrument count to make sure that no unintentional items, like suture needles, were left inside the patient. Drapes are removed, the anesthesiologist begins to arouse the patient, and they are placed back onto a gurney to be brought into the Post-Anesthesia Care Unit (PACU).

Self-Quiz
Ask Yourself...
- A patient had a rotator cuff repair completed with subacromial decompression and debridement. How can the nurse explain what was completed in layman’s terms?
- A patient asks the nurse why they have several small incisions, instead of one large one. How should the nurse respond?
- The patient asks the nurse if the stitches will dissolve or if they need them removed. How can the nurse respond?
- What should the nurse include about implanted sutures?
Case Study
The surgeon’s operative note states the following procedures were done for Ms. Smith:
Right arthroscopic rotator cuff repair, subacromial decompression, biceps tenodesis.

Self-Quiz
Ask Yourself...
- Ms. Smith asked the perioperative nurse how the surgeon fixed her shoulder. How should the nurse answer this question in layman’s terms?
Post-Operative Care
Post-operative care for a rotator cuff surgery patient is usually straightforward and routine, especially when the patient has received an effective interscalene nerve block. These patients most often awake with no feeling in their post-operative arm, and therefore no pain. Without needing opioids and less anesthesia, they also tend to have less nausea. Routine postoperative care applies, which includes monitoring vital signs, assessment of the level of consciousness, surgical site dressing and distal extremity appearance and circulation, pain, nausea, and PO tolerance.
Most patients are discharged directly home, usually within an hour or two of leaving the OR. The PACU nurse needs to review education again, preferably with the support person who will be taking the patient home.
When patients have received a nerve block, the arm will need to be placed in a simple sling. The reason is because the patient won’t have control or feeling in their arm, and they are at risk of accidentally injuring a dangling arm. After the nerve block has worn off, it is up to the surgeon’s direction on how long the patient should wear the sling for. For more simple repairs, the sling can sometimes be discontinued after the nerve block has worn off. For the occasional complicated repair, sometimes a bulky shoulder immobilizer is applied post-operatively.
(7)
Post-Operative Education
Post-Operative Education should be reviewed at many different points throughout the patient care experience. It should start with physician consultation appointments and continue the day of surgery, both pre- and post-operatively. Anxiety and the effects of anesthesia can greatly impact the patient’s ability to recall instructions, so repetition is important. Including the patient’s supportive caregivers is very helpful.
- General Recovery – Review the expected side effects of anesthesia, which include tiredness, and limited mental abilities.
Patients should be given information on what symptoms may constitute an emergency, and when they should follow up with their doctor.
- Dressing and Wound Care – Surgeons have varying preferences about when it is okay to remove the bandage and resume showering. The surgeon may allow the patient to shower the day after surgery, and some prefer the patient to wait until their follow-up appointment. All are recommended to wait for incisions to heal for a few weeks before the patient can submerge the area in water through swimming or bathing. Signs and symptoms of infection or complications such as bleeding should also be reviewed.
- Activities and Movement – Again, depending on the type of repair made and surgeon’s preference, there will be limitations on when the patient can resume different activities. The patient should be encouraged to encourage light circulation in the extremities by wiggling fingers, doing wrist circles. Lifting weights should be avoided, and even simple activities such as opening a door or reaching across to put on a seatbelt may need to be cautioned against. Many patients will be referred to physical therapy for a few weeks into post-operative recovery to strengthen the repaired muscles. Patients should be advised to sleep in an upright semi-fowler position for at least the first few nights after surgery. This will help reduce swelling in the shoulder from occurring overnight, and an overall decrease in pain.
- Pain management – A big category of education is on pain management. Patients experience great pain relief following the nerve block. However, once this wears off 6-24 hours later, pain can be very unpleasant. For most patients, the first three days are the worst. Things should then continue to improve each day. There are three main analgesic interventions:
-
- Non-pharmacologic – The most common is applying ice to the effected shoulder. This helps reduce swelling and thereby pain. It is important that patients are reminded to protect the skin with a towel and to keep the incisions dry. They want to remove the ice at regular intervals so that blood can recirculate to the area which promotes tissue healing. Positioning and small movements can also help.
-
- Non-opioid Medications – Non-steroidal anti-inflammatory medications (NSAIDS). These are appropriate for mild to moderate pain (approximately 2-6/10 of a numeric pain scale).
-
- Opioid Medications – Opioids (e.g. Oxycodone, Percocet, Tramadol) are being prescribed with increasingly strict parameters. These drugs are very effective in treating pain, but they must be taken with caution. Surgeons should prescribe only a small quantity of medications, initially just enough to get the patient through the first three days. Patients requiring pain relief for severe pain (> or = 7/10) should be evaluated by the provider for prescription renewal. Nurses should highlight safety concerns about not driving while on opioids, and not mixing with alcohol or cannabinoids. They should also be informed about common side effects of nausea and constipation, and how to reduce these.
If patients try to stoically recover without using any medications, they may avoid using the arm at all. This will decrease circulation and the healing process, overall leading to a suboptimal outcome. They may not achieve full recovery of range of motion or strength.
Patients can use all three pain relief strategies simultaneously. They should also wean off opioid medications as soon as it is tolerable, and just take NSAIDS until they are no longer needed.
(7)


Self-Quiz
Ask Yourself...
- You are taking care of a patient who has a history of substance misuse and states they cannot take opioids during their recovery. How would the nurse develop a pain control plan of care for this patient?
- A patient states they were scared to take their opioid medications because they were afraid of addiction. What problems would the nurse anticipate? What should the nurse assess for?
- A patient’s family member asks the nurse when they should give the patient the next dose of pain medication when they get home. How can the nurse respond?
Other Painful Shoulder Problems
Arthritis – Another common cause of pain that can affect all joints, including the shoulder. As is the case with other joints, arthritis is the result of the deterioration of cartilage and/or synovial fluid surrounding the joint, resulting in decreased mobility and an increase in pain. Non-surgical treatments for arthritis are similar to rotator cuff injuries, including activity modification and medications. However, when these fail, a typical surgical intervention is a total shoulder replacement (arthroplasty). In this surgery the head of the humerus, and/or the glenoid socket of the scapula will be removed and replaced with prosthetic implants. For patients without significant comorbidities, these procedures can also be performed in an outpatient surgery center.
Adhesive Capsulitis– Also known as a Frozen Shoulder. The connective tissue that covers the ball and socket of the shoulder starts to become inflamed, thicken and become tighter over time. Adhesions are thick bands of tissue that form, making the capsule tighter, making it difficult and painful to move the shoulder. This condition can last from months to up to three years to fully resolve naturally. Medical interventions can include:
- Steroid injections
- Hydrodilation – A large volume injection of fluid into the shoulder joint to expand and stretch the shoulder joint capsule)
- Arthroscopic surgery – Breaking up adhesions is often part of a rotator cuff surgery, and is rarely done just for this condition
- Shoulder manipulation under anesthesia – Typically, the shoulder joint will be anesthetized with an interscalene nerve block (the same that is done prior to rotator cuff surgery). Additional moderate sedation is usually given, then the orthopedic physician manually moves the shoulder to break up the capsule scar tissue. The entire procedure is very quick, under five minutes. Since this procedure most often utilizes moderate sedation for the nerve block and the procedure, nurses play a role in the treatment team.
Physical therapy is very important to follow up with after a medical treatment is done for the shoulder to ensure adhesions don’t reform. Pro Tip: Patients should apply heat and take a NSAID before doing stretches or physical therapy. Utilize ice to reduce inflammation after an exercise set.
Impingement Syndrome is “characterized by pain experienced through an arc of elevation as the shoulder abducts. It occurs when the subacromial structures are actively brought into contact with the acromion and coracoacromial ligament during the act of elevating the arm” (Phillips, 2014). This can lead to tendinitis or bursitis. These can occur concurrently. Bursitis, inflammation of the bursa sacs that cover the shoulder capsule, may also occur without associated impingement syndrome (5).
(2,5)
Biceps tendinitis¹² – Inflammation or degeneration of the long head of the biceps tendon. It causes anterior shoulder pain and often occurs with other shoulder problems.
Shoulder Instability⁹ – Patients will present with feelings that their shoulder “gave out.” This is when the head of the humerus partially or completely popped out of the glenoid fossa. This can occur from genetic reasons of having hyperlax ligaments, or it can be the result of trauma to the area.

Self-Quiz
Ask Yourself...
- A patient with bicep tendinitis asks if they need surgery, how should the nurse respond?
- What treatments does the nurse anticipate for a patient with shoulder instability who has recently had a dislocation after a fall?
- A patient with shoulder arthritis asks if physical therapy would help. How should the nurse respond?
- A frozen shoulder patient asks the nurse the following questions, how should the nurse respond?”
- How did I develop a frozen shoulder?
- Should I wear a sling?
- Are there any activity restrictions?
Conclusion
At this point, you hopefully know more about a single joint than you ever wanted to know. The shoulder contains several structures, which if they deviate from their standard physiologic process, can become problematic. Shoulder pain is so common, that fortunately there are many remedies available, and they are continually improving. If shoulder pain does not improve naturally with time and activity adjustment, shoulder surgery is a relatively easy procedure. Nurses play an important role when providing perioperative care to patients. They assist with procedures, ensure patient safety, and as always, provide patient education.
References + Disclaimer
- McCausland, C., Sawyer, E., Eovaldi, B. J., & Varacallo, M. (2023, August 8). Anatomy, Shoulder, and Upper Limb, Shoulder Muscles. Stat Pearls [Internet]. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK534836/
- Athwal, G. M., & Armstrong, D. A. (2022, June). Rotator Cuff Tears. Retrieved August 2024, from OrthoInfo: https://orthoinfo.aaos.org/en/diseases–conditions/rotator-cuff-tears/
- Thanarajah, T., Lo, i. K., & Sabo, M. T. (2021, June 17). Rotator cuff repair techniques: Current concepts. Journal of Clinical Orthopedic Trauma, 149-156. doi:10.1016/j.jcot.2021.03.006
- Genovese MD, M. (n.d.). How to conduct a Shoulder Exam. Retrieved from Standfordmedicine25: https://stanfordmedicine25.stanford.edu/the25/shoulder.html
- Phillips, N. (2014, June 17). Tests for diagnosing subacromial impingement syndrome and rotator cuff disease. Shoulder Elbow, 6(3), 215-221. doi:10.1177/1758573214535368
- Chitneneni, A., Hasson, J., Uritis, I., Viswanath, O., Berger, A., & Kaye, A. (2022, August 25). Peripheral Nerve Stimulation for Chronic Shoulder Pain Due to Rotator Cuff Pathology. Orthopedic Reviews, 14(3), 37494. doi:10.52965/001c.37494
- Athwal MD, G. S., Armstrong MD, A. D., & Wiater MD, J. M. (2022, June). Rotator Cuff Tears: Surgical Treatment Options. Retrieved from Orthoinfo: https://orthoinfo.aaos.org/en/treatment/rotator-cuff-tears-surgical-treatment-options/
- Jeon, I.-H., & Kholinne, E. (2020, August). To sling or not to sling the shoulder after rotator cuff repair: which side are you on? Annals of translational medicine, 8(15), 972. doi:10.21037/atm.2020.03.197
- Giovannetti de Sanctis, E., Franceschetti, E., De Dona, F., Palumbo, A., Paciotti, M., & Franceschi, F. (2021, January). The Efficacy of Injections for Partial Rotator Cuff Tears: A Systematic Review. Journal of Clinical Medicine, 10(1), 51. doi:10.3390/jcm10010051
- Juels MD, A., & Juels, P. (2023, August 14). Delayed Horner Syndrome After Interscalene Block. (K. Sibert MD, Ed.) Anesthesiology News, The Frist Series. Retrieved from https://www.anesthesiologynews.com/The-Frost-Series/Article/08-23/Delayed-Horner-Syndrome-After-Interscalene-Block/70980?ses=ogst#:~:text=Horner%20syndrome%20is%20caused%20by,%25%20to%2012%25%20of%20cases.&text=Hoarseness%20may%20occur%20if%20local,%25%20
- Patel, D. K., Fedorka MD, C. J., & Fuller MD, D. A. (2022, August 23). Prepping and Draping Series: Shoulder Cooper University Hospital. Retrieved from American Academy of Orthopaedic Surgeons: https://www.aaos.org/videos/video-detail-page/25605__Videos
- Athwal MD, G. S. (2021, October). Biceps tendinitis. Retrieved from OrthoInfo: https://orthoinfo.aaos.org/en/diseases–conditions/biceps-tendinitis
- Drezo. (2019, March 4). Operating Room Setup. Retrieved from Musculoskeletal Key: https://musculoskeletalkey.com/operating-room-setup-2/
- Freundlich, R. E., Bulka, C. M., Wanderer, J. P., Rothman, B. S., Sandberg, W. S., & Ehrenfeld, J. M. (2020). Prospective Investigation of the Operating Room Time-Out Process. Anesthesia and analgesia, 130(3), 725–729. https://doi.org/10.1213/ANE.0000000000004126
Image References
- Norin, O. (2021). Closeup of skeleton scapula model. Retrieved from https://unsplash.com/photos/gray-concrete-horse-figurine-on-white-table-tAXaNziaNio
- brgfx. (n.d.). Shoulder Impingement Syndrome. Retrieved from Freepik: https://www.freepik.com/free-vector/understanding-shoulder-impingement-syndrome_221845164.htm#fromView=search&page=1&position=26&uuid=28e2c1b2-39d6-4a61-b8f2-686c2d53dacc
- brgfx. (n.d.). Rotator Cuff Tear. FreePik. Retrieved from https://www.freepik.com/free-vector/rotator-cuff-tear-illustration_222492656.htm#query=shoulder%20anatomy&position=25&from_view=keyword&track=ais_hybrid&uuid=3f658d11-d8fc-48d5-8291-9e2555aade83
- Almaollim, H., Kalantan, D., Alharbi, L., & al., e. (2021). Approach to Musculoskeletal Examination. In H. Amoallim, & M. Cheikh (Eds.), Skills in Rheumatology. Singapore: Springer. doi:10.1007/978-981-15-8323-0_2
- 8photo. (n.d.). Young Man Gesturing Isolated. Free Pik. Retrieved from https://www.freepik.com/free-photo/close-up-young-man-gesturing-isolated_12986782.htm#fromView=search&page=2&position=3&uuid=c066c260-7661-4ef7-83e7-77dad556dc66
- Image from Microsoft Word Stock Images
- Nasch92. (2018). A test for subacromial impingement. Retrieved from https://commons.wikimedia.org/w/index.php?curid=71498555
- Lee, J. M., Ji, J.-H., Park, S.-E., Suh, D., & Song, K.-J. (2024, April 17). Arthroscopic cuff repair: footprint remnant preserving versus debriding rotator cuff repair of transtendinous rotator cuff tears with remnant cuff. BMC Musculoskeletal Disorders, 25(302). doi:10.1186/s12891-024-07431-z
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
