Ruptured Appendix: Evaluation and Treatment
Contact Hours: 1.5
Author(s):
Tabo Mwikisa-Kelly DNP, MSN, RN, CNEcl
Course Highlights
- In this Ruptured Appendix: Evaluation and Treatment course, we will learn about the signs and symptoms of a ruptured appendix.
- You’ll also learn risk factors that could lead to a ruptured appendix.
- You’ll leave this course with a broader understanding of the types of treatment that can be used to treat ruptured appendicitis.
Introduction
Appendicitis is one of the most common causes of emergent abdominal surgeries worldwide. Appendicitis occurs due to inflammation of the appendix’s lining in the abdomen. When appendicitis is left untreated or not diagnosed early, it can lead to serious complications such as a ruptured appendix, also known as a perforated appendix. Although appendicitis can affect nearly anyone, it is more prevalent in younger people who are assigned as male at the time of birth, between their second and third decade of life. [1][2][4]
In the United States (US), it is estimated that 7% of the population is affected by appendicitis, with approximately 280,000 reported appendectomy cases annually. Most cases happen between the ages of 5 and 45. Over the years, there has been a decrease in the number of incidents of appendicitis in Western countries compared to countries with newly emerging economies due to dietary changes that comprise high fiber [8][10].
Despite advances in medicine and with the creation of diagnostic tools, acute appendicitis continues to be misdiagnosed as patients may present with atypical symptoms that also mimic other disease processes. Therefore, it contributes to morbidity and mortality rates that are associated with complications from appendicitis, especially with the elderly [7]. However, clinicians need to be cognizant of how appendicitis can affect different age groups and patient populations.
Case study:
A 62-year-old male with a history of Diabetes Mellitus and recurrent Urinary Tract Infections (UTIs) presented to the local Emergency Department (ED) with nausea and vomiting for 8 days. When asked about their intake in the last 24 hours, the patient stated, “I had a bit of chicken broth and a few sips of water, but that made me throw up right away.”
The patient also reported having abdominal pain around the umbilicus and in the right lower quadrant for a couple of days. They noted that the pain intensified and suddenly improved within 24 hours. The patient also reported chronic problems with constipation. The patient’s last bowel movement was a week ago. Upon admission to the ED, the following were the vitals: Temperature, 39 C, Heart rate 112, Blood Pressure 91/60. The patient appears to be lying in the fetal position because he reports that it helps relieve abdominal pain.
Definition
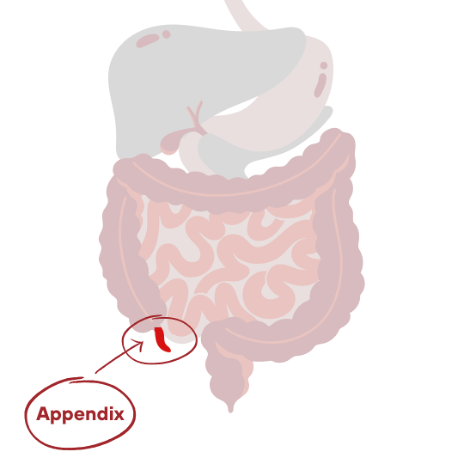
A ruptured appendicitis, also known as a perforated appendix, is a life-threatening serious complication of acute appendicitis that may require immediate surgery. When appendicitis is left untreated or symptoms are not recognized on time, it could lead to a ruptured appendix [7]. Appendicitis occurs due to the inflammation of the lining of the appendix vermiform. The appendix is a small finger-like hollow tubular structure resembling a worm at the base of the cecum (pouch-like structure) that connects the small intestine to the colon (large intestine). Perforation varies and can occur due to pus-filled pockets, leading to peritonitis [4].
The appendix varies from 5cm to 35cm, with the average length being 8 – 10 cm. It is found within the visceral peritoneum of the abdomen and can vary by location, with retrocecal being the most common. A perforated appendix can lead to other serious medical complications, such as peritonitis, which is the inflammation of the peritoneum or abscess formation in the abdomen.
Appendiceal perforation contributes to increased morbidity and mortality, which can result from sepsis, which occurs in 17 – 32 % of patients [6][7]. It is recommended that patients with moderate to high-risk factors receive surgical consultation to help reduce the mortality resulting from perforation. The most significant risk factors include time from the onset of symptoms to the time the patient arrives at the emergency department and risk for sepsis, which can be ruled out from vital signs and lab work, including WBC count [6].
Epidemiology
Appendicitis is one of the leading causes of emergent abdominal surgeries worldwide. More than 280,000 cases of appendicitis occur here in the United States annually. Studies have shown there are higher incidences of appendicitis among male patients at 8.6% and 6.7% in female patients [1][11]. Cases of appendicitis were found to increase by 10 % during the summer months, which is often associated with dehydration. Acute appendicitis is associated with morbidity and increased mortality in 7% of the population, which is the equivalent of ¼ million [6].
Perforation of the appendix in pregnant women is associated with 2.6 to 10 percent of fetal loss. 5 % to 10 % of those cases are in the elderly, 65 years and older, with complications occurring in 1% to 5 % of patients who have appendicitis. Appendicitis affects all demographics, although in terms of population, it is more common in whites and less common in blacks and Hispanics [4][12].
The appendix’s function is unknown, although research suggests it supports the immune system. The intestinal portion of the appendix continuously secretes mucus, keeping the mucosal lining moist and keeping bacteria away from the mucosa. Intraluminal pressure builds when bacteria become trapped in the appendiceal lumen due to an obstruction of the appendix, causing the appendiceal wall to weaken due to ischemia. This leads to tissue necrosis in the appendix, possibly leading to a burst (perforation) [8] [9].
When the appendix is obstructed, intestinal gut flora increases, i.e., Escherichia coli, Bacteroides fragilis, Pepto streptococcus, and Pseudomonas. The bacteria cause an immune response, increasing the white blood cell level in the body as pus accumulates in the appendix. These multifaceted events cause abdominal pain due to the aggravation of the visceral fibers in the peritoneal cavity, commonly found in the right lower quadrant, known as McBurney’s point [9].
Etiology
The function of the appendix is not really known or fully understood. Sometimes, the appendix is considered useless but may have some immune protective properties. However, the appendix shows a correlation associated with a blockage that is thought to be caused by an obstruction in the lumen from various etiologies. The possible causes of appendicitis are discussed below. When the appendix is obstructed, it increases mucus production and overgrowth of bacteria that cause tension in the appendix, eventually leading to necrosis followed by perforation [1][6].
The most common causes of appendicitis include:
- Lymphoid tissue hyperplasia
- Lymphoid follicles in the abdominal mucosa can outgrow in children and adolescents between the ages of 8 and 20. They can also outgrow in response to an inflammatory virus, such as measles or adenovirus, that obstructs the appendix.
- Fecaliths ‘poop rock’
- A hard lump of feces that is common in the elderly due to constipation.
- Neoplasm: i.e., carcinoid tumor or adenocarcinoma.
- This could be a source of appendicitis that is often found in patients 55 and older. Therefore, colorectal cancer screening can be useful in identifying early malignancy, as there is an association between acute appendicitis and colon cancer.
- Undigested seeds, parasites (e.g., pinworm infection)
- Rare congenital disorders (e.g., agenesis, duplication, and replication)
- Inflammatory bowel disease [1]
Risk Factors
Risk factors that contribute to appendicitis [1][6][12]:
- Ruptured appendicitis is associated with older age due to narrowing in the orifices compared to younger children.
- Consuming a sugary diet, family history, cystic fibrosis, decreased water intake or dehydration, cigarette smoking, and environmental risk factors such as air pollution.
- Pregnancy, typically in the third trimester, as the uterus pushes on the appendix. Advancements in pregnancy cause it to migrate in a counterclockwise direction.
- Delay in diagnosing appendicitis increases the risk of ruptured appendicitis. Therefore, a detailed patient history is helpful in early diagnosis.
Ask yourself...
- Can you list inflammatory factors that are known to cause acute appendicitis?
- List some risk factors that may contribute to acute/perforated appendicitis.
Assessment
Clinical presentation of patients with appendicitis can be challenging as it mimics other abdominal medical problems. Therefore, it is important to collect a thorough history. Appendicitis often occurs suddenly and without warning. Initially, the onset of appendicitis can start as generalized abdominal or periumbilical pain [6] [11].
The classic sign of acute appendicitis is generalized periumbilical pain that shifts to the abdomen’s right lower quadrant (RLQ). Assessment should include abdominal guarding, rigidity, and RLQ tenderness, usually at McBurney’s point. In pregnant women, pain is in the abdomen’s flank and upper right quadrant. Diagnosis is based on imaging studies and the patient’s clinical presentation [4][12].
Ask yourself...
- Can you describe assessment findings that would assist clinicians in diagnosing appendicitis or ruptured appendix?
- What are the consequences of delayed diagnosis of acute appendicitis?
- Why would it be important for older adult patients to follow up with colorectal cancer screening following a diagnosis of ruptured appendicitis?
- Which age group would be at risk for developing acute appendicitis from fecolith?
Clinical Signs and Symptoms
Stomach pain is the most common symptom of acute appendicitis. The onset of symptoms can lie in the patient’s pelvis or behind the cecum.
- Low-grade fever or fever of greater than 38 C, nausea, vomiting, diarrhea, constipation, trouble passing gas, abdominal bloating, leukocytes (WBC > 10 000).
- Abdominal guarding
- General malaise
- Rebound tenderness: removal from the area will cause the patient to scream, resulting in peritonitis and rebound tenderness.
Location is important and aids in diagnosing appendicitis. Although abdominal pain is usually described as unusual, specific characteristics of abdominal pain are useful in diagnosing appendicitis. Abdominal pain can occur before other symptoms arise, which can be vague and often described as improved. Initial stomach pain can be peri-umbilical pain for 24 – 48 hours. After that, it can become more severe due to peritoneal pain, which could be an indication of sepsis [6][8].
Ask yourself...
- What are the common signs and symptoms of appendicitis?
- What is the classic sign of appendicitis?
Additional Findings
- Tenderness in the rectum.
- In children, right flank pain is also present.
- Men may experience hemi-scrotal pain, which later turns into mild diffuse stomach pain; therefore, a rectal exam may be used to rule out appendicitis.
- Pregnant women may experience GERD, RUQ pain, pelvic pain, malaise, and epigastric pain. It is more common in the third trimester.

Ask yourself...
- Describe the clinical presentations that may suggest acute appendicitis in different patient population groups (i.e., pregnant or children).
- What would be the role of conducting a digital rectal exam when ruling out appendicitis?
- Can you name indications a pregnant woman may present when they have acute appendicitis?
Diagnosis
Diagnosis of acute appendicitis can be challenging because symptoms can present with different clinical presentations and may mimic other disease processes. A physical exam consistent with the clinical manifestation helps diagnose acute appendicitis. Therefore, a thorough history and examination are crucial in the early diagnosis of acute appendicitis as they can help prevent life-threatening conditions such as ruptured appendicitis.
Clinicians must remain vigilant that pregnant women can have acute appendicitis. Below are some tests to diagnose acute appendicitis/ruptured appendicitis [3][6].
Physical Examination
- McBurney’s point is a classic sign effective in diagnosing acute appendicitis when used in conjunction with imaging and lab work. During acute appendicitis, rebound tenderness and pain are felt by an individual when pressure is applied and released from the right lower quadrant. McBurney’s point is 1.5 to 2 inches in an oblique line between the umbilicus and the right anterior superior iliac spine.
- Rovsing’s sign is positive when deep palpation in the left lower quadrant (LLQ) causes a paradoxical pain in the right lower quadrant (RLQ). This occurs due to the irritation of the overlying peritoneum. A barium swallow test should be used to confirm diagnosis [11].
- Obturator sign: The patient experiences pain when their right knee is flexed to a nighty degree angle, while the right hip is internally rotated by moving the ankle away from the hip.
- Psoas sign: This is conducted by having an individual lie on their left side while flexing their right thigh backward. When inflamed, the appendix causes pain in the RIF with extension and flexion of the right hip against resistance.
- Dunphy sign: A sharp pain in which the RQL is caused by a voluntary cough, which is an indication that suggests localized peritonitis.
Laboratory Evaluation
Lab work should be used with another test for a more accurate diagnosis of acute appendicitis.
- A White Blood Count (WBC) > 10,000 is reflected in 80% of all cases of acute appendicitis. WBCs between 20 000 and 30 000 can be due to a ruptured appendix or neutrophilia. Due to their physiologic status, leukocytosis may not be a reliable indicator in pregnant women.
- C-reactive protein (CRP) with levels > 1mg/dL can help identify other causes of inflammation.
- Urinary beta-hCG 9 differentiates appendicitis from early ectopic pregnancy in women.
- Urinalysis is used to rule out Urinary Tract infections or kidney stones, and pregnancy tests—CBC is used to rule out infection…
- Amylase, liver, pancreatic, and renal function tests.
- Basic Metabolic Panel (BMP) can be used to check for electrolyte imbalances and dehydration.
- Pelvic exam of women of childbearing age is useful in diagnosing because many gynecological conditions do mimic acute appendicitis, colitis, pyelonephritis IBD, and Diverticulitis; 50% of patients have perforation by the time they undergo surgery.
Imaging
Below are the different types of imaging that can be used to diagnose acute appendicitis and complications [4][13].
- Computed Tomography (CT)
- The most precise in diagnosing appendicitis and any indications of inflammation. CT scan is used when the diagnosis is an unclear diagnostic test of choice – most specific and sensitive.
- Ultrasonography
- Preferred in pregnant women and young children as the test does not transmit radiation.
- Magnetic Resonance Imaging (MRI)
- Used to diagnose appendicitis in children and pregnant women as there’s no exposure to radiation. Complementary MRI is used when the diagnosis of appendicitis is unclear.
- Abdominal X-rays
- It can be used to rule out obstruction.
The Alvarado Scoring System is a test used to predict the need for surgical intervention in acute appendicitis based on the following components: tenderness in the right lower quadrant and Leukocytes each get awarded 2 points. Migration RLQ, anorexia, nausea, and fever each get a point. 37.5 degrees Celsius, rebound pain, elevated temperature, and a shift in the WBC count each get a point. The score determines the need for surgical intervention when it is greater than 7 [4].
Ask yourself...
- How would you describe McBurney’s and Dunphy’s signs?
- What is the rationale for using urinalysis to rule out appendicitis?
- Name the diagnostic test with the most sensitivity to acute appendicitis.
- Why is the WBC count not a reliable indicator in pregnant women?
- Describe a test that can be useful in differentiating an ectopic pregnancy from acute appendicitis in a woman of childbearing age.
Treatment
Appendectomy is a commonly performed surgery in patients with appendicitis. According to current guidelines, ultrasound should be the first step. Current guidelines suggest that early surgical intervention can help lower the risk of perforation. The recurrence of appendicitis was found to occur five years later in patients who were treated with antibiotics. Surgical intervention may be a laparoscopic or open appendectomy [4][10].
Antibiotic therapy: Conservative antibiotic management has proven successful in 91 % of cases [5]. Commonly used intravenous (IV) antibiotics are Ertapenem 1 gram or ceftriaxone 1 gram and metronidazole 1500mg, levofloxacin 750mg QD. It is recommended that pregnant women receive antibiotics in category A or B. Prophylactic antibiotics must be administered before every appendectomy is performed [10].
Fluid resuscitation: Aggressive crystalloid therapy to treat dehydration or sepsis.
Percutaneous drain: This is necessary for patients with large abscesses around the appendix. An interval appendectomy can be performed after the fistula closes.
Other treatment modalities: Endoscopic retrograde appendicitis therapy (ERAT), which uses endoscopic intervention to drain pus, extract the fecalith, and place a stent when needed [11].
Pain management and antiemetic management: Opioids, nonsteroidal anti-inflammatory drugs, and Tylenol can be used to control pain. Antiemetic medication, such as ondansetron and metoclopramide, can treat nausea [9].

Ask yourself...
- Besides an appendectomy, can you name a treatment modality that may be used to treat a ruptured appendix?
- What three main lab tests can be used to diagnose suspected acute appendicitis?
- After reviewing the diagnosis for raptured appendicitis, name the test that is most sensitive in diagnosing acute appendicitis.
- What would be the indication for using a Urinalysis in diagnosing acute appendicitis?
Safety Considerations
Patients who are older than 55 years and older should be screened for colon cancer as it may be the source of acute appendicitis [11].
In pregnant women, appendicitis must be differentiated from ectopic pregnancy. Pregnant women experience RUQ pain because of the superior displacement of the cecum and appendix shifts. Urinary beta-hCG 9 differentiates appendicitis from early ectopic pregnancy in women.
Ask yourself...
- A nurse is caring for a pregnant patient with suspected appendicitis. What diagnostic test should the nurse anticipate will be used on the patient?
- What is the rationale for conducting a pelvic exam on a woman of childbearing age who is suspected of having acute appendicitis?
Complications
Complications such as peritonitis and appendiceal abscesses occur in 2 -6 % of patients. Raptured appendicitis could lead to some of the following complications [9]:
- Intrabdominal abscess, ileus, peri appendiceal abscess, and subphrenic abscess form under the diaphragm.
- Septic shock.
- Organ failure
- Infertility
- Dehiscence of wounds
- Surgical infection of the wound
- Fetal loss due to peritonitis
- Incorrect diagnosis
Research Findings
Diagnosing acute appendicitis can be challenging. Therefore, clinical tools such as the Alvarado scoring system can assist clinicians in improving their diagnosis. Over the years, there have been changes to how ruptured appendicitis is treated. Most recent studies have led to different approaches.
Patients who are considered with mild or moderate cases of perforated appendectomies are treated with antibiotics and drainage and followed by an interval appendectomy 6 – 8 weeks following treatment.
Studies have shown that there is an increase in carcinoids, a slow-growing type of neuroendocrine tumor that affects the appendix in younger patients who are below the age of 50 [2]. Antibiotics and drainage of localized abscesses can be used to avoid surgery [5].
Ask yourself...
- Describe what the term interval appendectomy means.
- Name 4 complications that could result from ruptured appendicitis.
Nursing Considerations and Patient Teaching
- Keep patient NPO when there is suspicion of acute appendicitis.
- Ensure that the patient has Intravenous access as ordered in anticipation of fluid resuscitation, hydration, and antibiotic treatment.
- Educate the patient to avoid strenuous exercise whilst recovering from a ruptured appendix until cleared by the doctor.
- Educate the patient to take antibiotics as prescribed.
- Educate the patient not to ignore constipation. The patient should be on a stool regimen as ordered by the healthcare provider.
- Monitoring incision for dehiscence.
- Educate patients to monitor for fever and when to call the health care provider when they have a drain or after surgical intervention following appendicitis.
Ask yourself...
- What nursing interventions should a nurse anticipate completing when caring for a patient with suspected appendicitis?
- List some patient education points a nurse should give to a patient diagnosed with acute appendicitis.
Conclusion
The prognosis of appendicitis is often considered good when early diagnosis and interventions are executed. The Standard treatment is open or laparoscopic surgery. Prompt diagnosis is key to preventing ruptured appendicitis. Differential diagnoses based on the patient’s age, population, and gender could assist with better diagnosis.
References + Disclaimer
- National Institute of Diabetes and Digestive and Kidney Diseases. (2021). Retrieved from https://www.niddk.nih.gov/health-information/digestive-diseases/appendicitis/treatment
- Appendiceal Cancer in the National Database, Increasing Frequency, Decreasing Age and Shifting Histology. Journal of the American College of Surgeons. DOI: 10.1097/XCS.00000000000000172.
- Echevarria, S., Rauf, F., Hussain, N., Zaka, H., Farwa, U. E., Ahsan, N., Broomfield, A., Akbar, A., & Khawaja, U. A. (2023). Typical and Atypical Presentations of Appendicitis and Their Implications for Diagnosis and Treatment: A Literature Review. Cureus, 15(4), e37024. https://doi.org/10.7759/cureus.37024
- Kyle, J. A. (2019). Acute Appendicitis in Adults. https://www.uspharmacist.com/article/acute-appendicitis-in-adults
- Alajaimi J, Almansoor M, Almutawa A, Almusalam MM, et al. Are antibiotics the new appendectomy? Cureus. 2023 Sep 1;15(9): e44506.
- Lotfollahzadeh S, Lopez RA, Deppen JG. Appendicitis. [Updated 2024 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493193/
- Potey, K., Kandi, A., Jadhav, S., & Gowda, V. (2023). Study of outcomes of perforated appendicitis in adults: a prospective cohort study. Annals of medicine and surgery (2012), 85(4), 694–700. https://doi.org/10.1097/MS9.0000000000000277
- Walter K. (2021). Acute Appendicitis. JAMA. 2021;326(22):2339. doi:10.1001/jama.2021.20410
- Craig.S. (2022). Appendicitis. Medscape. Retrieved from https://emedicine.medscape.com/article/773895-overview?form=fpf&scode=msp&st=fpf&socialSite=google&icd=login_success_gg_match_fpf
- Yadao, S., Lamture, Y., & Huse, S. (2022). Uses of Antibiotics Alone in Case of Uncomplicated Appendicitis. Cureus, 14(8), e28488. https://doi.org/10.7759/cureus.28488
- Krzyzak, M., & Mulrooney, S. M. (2020). Acute Appendicitis Review: Background, Epidemiology, Diagnosis, and Treatment. Cureus, 12(6), e8562. https://doi.org/10.7759/cureus.8562
- Rebarber, A., Jacob, B. P., Levine, D., & Weiser, M. (2019). Acute appendicitis in pregnancy. UpToDate, Charles J Lockwood, MHCM, Deborah Levin, Martin Weiser, UpToDate.
- D’Souza, N., Hicks, G., Beable, R., Higginson, A., & Rud, B. (2021). Magnetic resonance imaging (MRI) for diagnosis of acute appendicitis. Cochrane Database of Systematic Reviews, (12).
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
