Course
Smoking Cessation
Course Highlights
- In this Smoking Cessation course, we will learn about the epidemiologic and etiologic influences on smoking addiction and cessation.
- You’ll also learn the pathophysiological effects of smoking on the human body and the clinical signs and symptoms of smoking-related disease.
- You’ll leave this course with a broader understanding of evidence-based treatments and nursing interventions for smoking cessation.
About
Contact Hours Awarded: 1
Author: Kimberlee Emfield Rowett, DNP, MSN, MBA, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Tobacco products have been around for centuries, but it wasn’t until the 1880s that the Bonsack machine was developed by an American Inventor, James Bonsack. This ultimately led to the mass production of cigarettes, followed by aggressive marketing that paved the way for pipe-smoking and tobacco-chewing habits in the United States. Since then, a lot has changed surrounding the culture and scientific evidence of the harmful effects of all tobacco products (1).
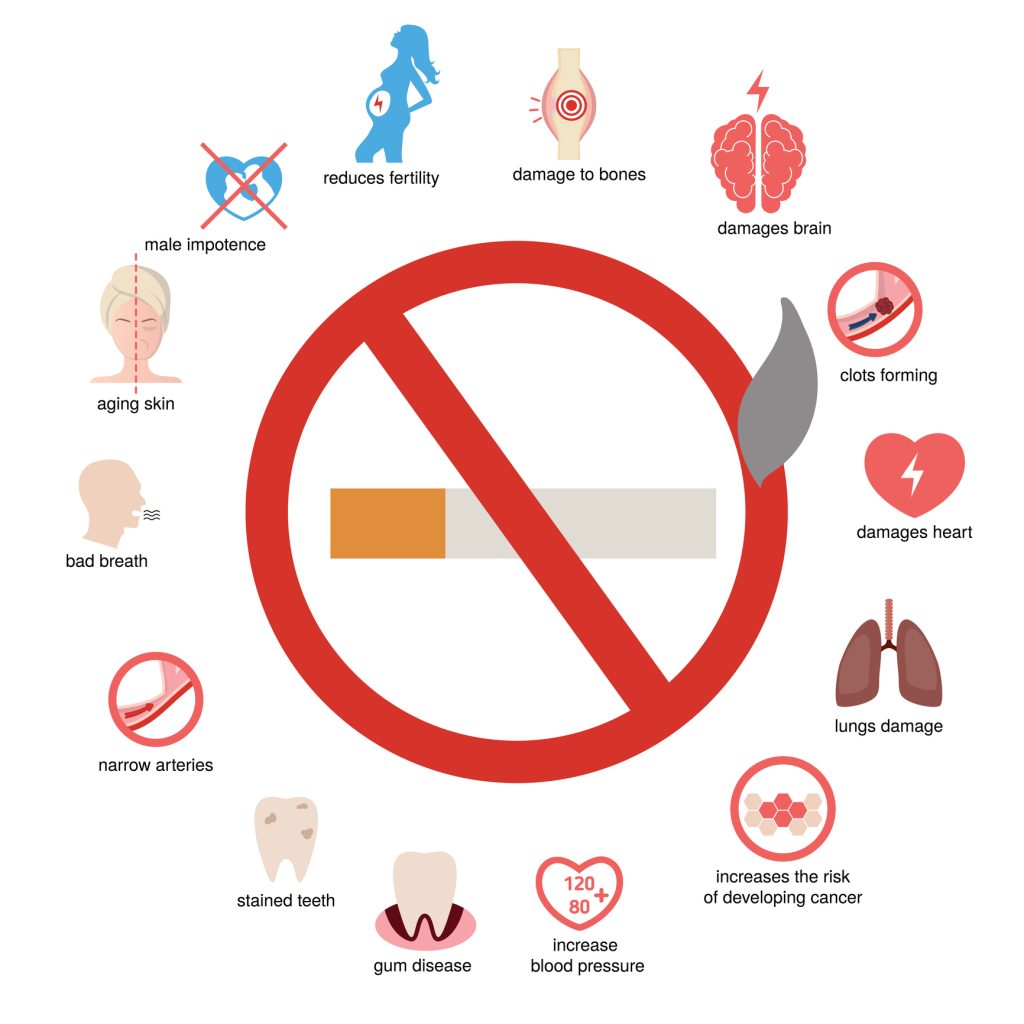
In 1962, the Royal College of Physicians reported on the deleterious health effects of smoking. The US surgeon general followed this by identifying similar research supporting the US population to quit smoking (1). Some of the most experienced side effects and health complications of cigarette smoking include cancer, heart disease, stroke, lung diseases such as COPD, type 2 diabetes, negative reproductive health impact, and autoimmune diseases such as rheumatoid arthritis.
It was also determined that secondhand smoke could negatively impact the health of those exposed. This can lead to coronary heart disease, stroke, and lung cancer. Secondhand smoke contributes to over forty thousand adult deaths and 400 infant deaths per year (2).
Despite these facts, it took until 1978 for US smoking percentages to drop to 33 of US citizens, leaving a majority of smokers to be those of the female gender or associated with poverty (1). In 2022, approximately 1 in 5 adults reported current tobacco product use, still accounting for 20% of Americans (3).
Indicating that the support of patients with both a history of and current use of tobacco products is needed. Nurses play a crucial role in promoting smoking cessation in those who currently use it. The nurse should assess and document the patient’s tobacco use and history, as well as assess their current and previous efforts in smoking cessation, their barriers to quitting, and their current desire to complete smoking cessation efforts. This course will explore how the nurse can best approach these topics to correctly identify, assess, implement, and educate patients on the importance of smoking cessation.

Self-Quiz
Ask Yourself...
- How might our understanding of long-term health consequences influence how we approach patient education surrounding smoking cessation efforts?
- In what ways can a nurse balance the promotion of smoking cessation with empathy for patients who struggle with nicotine addiction?
Definition
When supporting patients through smoking cessation efforts, the nurse needs to understand various definitions used in this regard. Certain terms may be used interchangeably, and the nurse should be mindful of using the correct terms when describing and educating the patient on smoking cessation efforts (4).
First, smoking is defined as the inhalation of smoke from burning tobacco, either through cigarettes, cigars, or pipes. This may be referred to as smoking tobacco or nicotine use. Cigarette addiction is a term used to describe a chronic, relapsing disorder characterized by the compulsive consumption of tobacco. Smoking cessation would then be the process of quitting smoking, which can involve medical, behavioral, or psychological interventions (4).
Other commonly used terms when discussing smoking cessation include exposure, smokeless tobacco, smokers, tobacco, and tobacco use. Exposure is defined as contact with a substance by swallowing, breathing, or direct contact. Additionally, exposure can be short—intermediate or long-term. Smokeless tobacco is a form consumed using a different approach, such as chewing or snuffing. Smokers are defined as individuals who smoked at least 100 cigarettes during their lifetime and currently smoke (4).
Tobacco is an agricultural product processed from the leaves of a Nicotiana plant. It is consumed, used as a pesticide, and sometimes added to medicines. Tobacco use would then be utilized in the current or past tense. When tobacco use is discussed, frequency (or how often), amount used, and product type should also be identified (4).

Self-Quiz
Ask Yourself...
- How does understanding the definition of cigarette addiction help nurses provide more effective support to patients attempting to quit?
- What potential challenges may patients face in their smoking cessation journey?
Epidemiology
When discussing the importance of smoking cessation, the epidemiology of smoking is an important topic to discuss as well. According to the World Health Organization (WHO), tobacco kills up to half of its users who don’t quit. Tobacco kills more than 8 million people per year, including 1.3 million non-smokers who are exposed to secondhand smoke. In 2020 alone, 22.3% of the world’s population used tobacco. Unfortunately, 80% of the 1.3 billion tobacco users worldwide come from low- to middle-income countries (5).
In the United States alone, there are approximately 1 in 5 adults currently use tobacco products. Smoking cigarettes has a higher prevalence in non-Hispanic American Indian or Alaska natives, people with disabilities, those with severe generalized anxiety disorder, and severe depression. Non-Hispanic black adults are also commonly known to use menthol-flavored cigarettes. Some contributing disparities include age, race or ethnicity, education level, and geographic areas (3).
While these numbers can be discouraging for patients who are struggling with quitting, it is essential to set realistic expectations for patients as they begin this smoking cessation journey. Most adults who smoke cigarettes want to quit, but only half tried to quit in the last year. Of those, 1 in 10 adults succeed in quitting any given year. The challenge here is that those who want to quit do not receive the appropriate advice, assistance, or treatment to quit smoking for good (3).
In 2022, 50% of adults who smoked and saw a healthcare provider received advice on how to quit, while 49.2% reported receiving assistance in quitting. Less than 4 in 10 adults who smoked cigarettes in 2022 used proven treatments to quit – such as approved medication or counseling. Additionally, 38.3% of adult smokers who tried to quit received counseling or medication. However, only 5.3% used counseling and medication despite the combination being more successful than the individual interventions alone (3).
By understanding these statistics, the nurse can educate the patient on implementing both approaches for a more successful outcome. While counseling may not be available to all patient populations, even brief advice of less than 3 minutes improves the chances of quitting successfully. The nurse can be pivotal in a patient’s smoking cessation journey. Just 3 minutes of the nurse’s time is highly cost-effective and improves patient outcomes, thus a great return on investment in the healthcare system (3).


Self-Quiz
Ask Yourself...
- Why might smoking rates remain higher in certain demographic groups?
- How might understanding disparities in smoking rates help nurses tailor their smoking cessation interventions?
Etiology
It is essential to know the etiology of smoking when supporting patients in their smoking cessation journey. By understanding the underlying causes or potential risk factors for developing a smoking habit, the nurse can support the patient in addressing these concerns. Addressing the root cause of a smoking habit improves the probability of quitting and supports the patient’s holistic health.
Having a nicotine addiction may occur because of various factors. An addiction, in general, is defined as a mental or emotional dependence on a substance. Physical dependence occurs when the body gets used to the substance. This dependency is arguably more serious than a mental or emotional one, as a lack of consumption of the substance may manifest withdrawal symptoms. For tobacco, these may include difficulty sleeping, anxiousness, mood changes or instability, and an increase in hungry queues (5).
Nicotine affects the patient’s body and brain in a few key aspects. First, nicotine floods the brain’s “reward circuits” with dopamine. Dopamine is a chemical naturally found in the body that communicates to the brain that something is pleasurable, leading to the desire to continue tobacco consumption. Additionally, because of the flood of dopamine, the other dissatisfactory thoughts and emotions a patient may feel without the substance subsided, giving the patient a sense of bliss despite challenges still being present in their overall well-being (5).
As a patient continues to consume tobacco products, the body begins to build a tolerance for the nicotine. This is often why smokers begin with a few cigarettes per day and gradually increase their consumption over time. Similarly, if the increase does not occur when nicotine tolerance is present, the patient may experience withdrawal symptoms (5).
Beyond the mental and physical influences over a patient’s choice to smoke and potential nicotine addiction, other factors may be at play. First, psychosocial influences may contribute to patients trying and continuing to consume cigarettes and other tobacco products. This includes environmental factors, such as stress, peer pressure, and social norms.
Genetic factors are a second influencer, as research suggests that certain genetic traits increase an individual’s risk for nicotine addiction. Certain genetic variations can impact the metabolism of nicotine, thus increasing their need for additional amounts of tobacco consumption. This increase then exponentially increases the rate of consumption and the risk of developing an addiction (5).

Self-Quiz
Ask Yourself...
- How can understanding the role of genetics in nicotine addiction help nurses identify patients who may be at a higher risk for smoking addiction?
- In what ways can a nurse help address the psychosocial and environmental factors contributing to a smoking habit?
Pathophysiology
In addition to understanding the etiology of tobacco use, understanding the pathophysiology will improve the nurse’s ability to support patients wanting to implement smoking cessation efforts properly. Epidemiological studies have linked smoking with coronary artery disease, among other serious medical complications. Smoking impacts the respiratory, cardiovascular, and endocrine systems, increases the risk of cancer, and affects the metabolic state due to the significant harm tobacco has on nearly every organ in the body (6).
Globally, cigarette smoking is the leading cause of preventable cardiovascular morbidity and mortality. Approximately one in ten cardiovascular deaths are related to smoking. This is due to the development of atherosclerosis, myocardial infarction, stroke, peripheral arterial disease, and abdominal aortic aneurysm (7). Cigarette smoke provides exposure to nicotine, carbon monoxide, and reactive oxygen species (ROS).
Nicotine is the leading cause of smoking-induced hemodynamic changes. Free radicals, ROS, and reactive aldehydes from cigarette smoke aid in developing endothelial dysfunction, impeding the ability to create nitric oxide (NO). Cigarette smoke also impacts cardiac remodeling, as it induces a prothrombic state, vascular inflammation, lipid profile alterations, and metabolism changes (8).
In the respiratory system, smoking leads to inflammation, oxidative stress, and damage to the cilia of the lungs. This increases a patient’s susceptibility to respiratory infections and chronic diseases such as chronic obstructive pulmonary disease (COPD), emphysema, and lung cancer (9). Tobacco use is also associated with other types of cancer, such as mouth, throat, bladder, pancreas, kidney, and cervix (10).

Self-Quiz
Ask Yourself...
- How does smoking-induced damage to the cardiovascular and respiratory systems highlight the importance of early intervention in smoking cessation?
- Given the wide-ranging effects of smoking on multiple organ systems, how can the nurse educate patients about the long-term risks of smoking?
Clinical Signs and Symptoms
While smoking itself may not have symptoms, patients may exhibit sure signs and symptoms based on the organ system the cigarette smoke is impacting. Because of this, the signs and symptoms will be broken down into the most commonly experienced symptoms in each system. Respiratory symptoms may include chronic cough, wheezing, shortness of breath, frequent respiratory infections, and sputum production.
Cardiovascular symptoms may consist of hypertension, chest pain, and signs of peripheral artery disease, including leg pain with walking. Systemic symptoms may include reduced exercise tolerance, fatigue, and impaired health after surgery or injury. It is also important to note the signs and symptoms of withdrawal, as patients participating in a smoking cessation plan may be at risk for experiencing such symptoms. Withdrawal symptoms include irritability, anxiety, difficulty concentrating, increased appetite, and cravings when attempting to quit smoking (2).

Self-Quiz
Ask Yourself...
- How can recognizing clinical signs and symptoms of smoking-related disease early on help nurses intervene effectively?
- What strategies can a nurse employ to differentiate between symptoms caused by smoking-related diseases versus that of nicotine withdrawal?
Treatment
Treatment for smoking ultimately focuses on discontinuing use through smoking cessation programs. Smoking cessation efforts should be personalized based on the patient’s unique situation, barriers, and motivation for quitting. Some interventions that may be included in a patient’s smoking cessation plan include pharmacological treatment as well as behavioral treatments.
Pharmacological treatment includes nicotine replacement therapy (NRT), bupropion (Zyban), varenicline (Chantix), and other medications. NRT includes nicotine patches, gums, lozenges, nasal sprays, and inhalers. It is used to reduce withdrawal symptoms typically experienced when reducing nicotine intake. By gradually reducing the intake of nicotine and providing an alternative route to smoking, the habits associated with smoking can eventually be redirected.
Bupropion is typically used as an antidepressant. The purpose of this non-nicotine medication is to reduce craving and reduce withdrawal symptoms as well. The way bupropion works also helps lessen the reward effects of smoking.
Varenicline is another great medication option for smoking cessation, as it stimulates nicotine receptors in the brain to mirror the chemical impact smoking would have. This can reduce cravings and decrease withdrawal symptoms while also blocking the pleasurable effects of smoking. Lastly, other medications may include clonidine and nortriptyline, among others, used off-label for similar effects above (11).


Self-Quiz
Ask Yourself...
- How can nurses determine the most appropriate smoking cessation treatment for patients?
- What role does combining pharmacological treatments with behavioral therapies play in increasing the success of smoking cessation?
Nursing Interventions
Smoking history is an essential component of any initial and subsequent patient assessment. Because of the harmful effects associated with tobacco products, the current and past smoking history needs to be appropriately assessed and documented. Some of the detrimental effects of the use of tobacco products include cardiovascular disease, respiratory conditions, and certain cancers – all of which are considered preventable.
Beyond assessing and documenting a patient’s tobacco use, the nurse should be prepared to educate the patient on the importance of smoking cessation. Beyond preventing disease, quitting the use of tobacco products reduces symptoms often associated with smoking. Reversing these symptoms can happen quickly, as soon as 20 minutes after quitting. This is vital information to share with patients who are struggling with motivation to the correct support and structure to carry out smoking cessation efforts and/or programs (12).
Key interventions for patients wishing to start a smoking cessation program include nursing assessment, education, behavioral support, follow-up appointments, and collaboration with other healthcare professionals. First, a nursing assessment should consist of the patient’s smoking history, their readiness to quit, and their specific barriers to cessation. Next, education should be provided on health risks associated with smoking, the benefits of quitting, treatment options available, and informed decision-making.
Third, behavioral support will vary from patient to patient. Stress management, coping skills, and structured environments that reduce smoking triggers are some that can support patients in their plans. Regular follow-up appointments are crucial in monitoring progress and encouraging and managing setbacks. Finally, multidisciplinary care team collaboration is essential to holistically supporting patients (13).

Self-Quiz
Ask Yourself...
- How can nurses effectively assess a patient’s readiness to quit smoking?
- How can nurses collaborate with other healthcare professionals to provide a more comprehensive and supportive smoking cessation plan?
Definition
When supporting patients through smoking cessation efforts, the nurse needs to understand various definitions used in this regard. Certain terms may be used interchangeably, and the nurse should be mindful of using the correct terms when describing and educating the patient on smoking cessation efforts (4).
First, smoking is defined as the inhalation of smoke from burning tobacco, either through cigarettes, cigars, or pipes. This may be referred to as smoking tobacco or nicotine use. Cigarette addiction is a term used to describe a chronic, relapsing disorder characterized by the compulsive consumption of tobacco. Smoking cessation would then be the process of quitting smoking, which can involve medical, behavioral, or psychological interventions (4).
Other commonly used terms when discussing smoking cessation include exposure, smokeless tobacco, smokers, tobacco, and tobacco use. Exposure is defined as contact with a substance by swallowing, breathing, or direct contact. Additionally, exposure can be short—intermediate or long-term. Smokeless tobacco is a form consumed using a different approach, such as chewing or snuffing. Smokers are defined as individuals who smoked at least 100 cigarettes during their lifetime and currently smoke (4).
Tobacco is an agricultural product processed from the leaves of a Nicotiana plant. It is consumed, used as a pesticide, and sometimes added to medicines. Tobacco use would then be utilized in the current or past tense. When tobacco use is discussed, frequency (or how often), amount used, and product type should also be identified (4).
Current and upcoming Research
Beyond the current pharmacological and behavioral support, some current and upcoming research indicates that new options are available now or in the near future.
First, genetic factors influence nicotine dependence. This insight allows genetic markers to be tested to determine if a genetic predisposition is at play. This knowledge enables smoking cessation efforts to be personalized and adjusted accordingly (14).
Next, there are emerging medications that target nicotine receptors and other pathways that provide positive reinforcement for smoking habits. This emerging medication can replace the need for the smoking habit, all while being effective in reducing the addiction to nicotine and reducing side effects associated with tobacco and/or current smoking cessation medications (15).
Additionally, access to new and improved digital health interventions means more patients have greater access to appropriate support. Mobile apps, text messages, and online platforms are popular tools that can be utilized to improve smoking cessation efforts and success. These advancements also improve real-time support, monitoring, and access (16).
Additional research being explored includes the role of epigenetics in smoking behavior and cessation complications or barriers. Epigenetics consists of a combination of an individual’s disease risk, the heritable traits of the patient’s family, and the current cell function of the patient. Age, environmental factors, and childhood trauma are all considered to be additional factors impacting epigenetics (17). A further area of research includes the effectiveness of e-cigarettes as a smoking cessation aid (18).

Self-Quiz
Ask Yourself...
- How might discovering genetic markers influence nicotine dependence influence the way a nurse personalizes smoking cessation treatments?
- What are some potential risks and advantages of incorporating digital health interventions into a smoking cessation program?
Conclusion
Smoking cessation is a vastly necessary health intervention that aids in preventing disease and improving a patient’s holistic health. Nurses play a pivotal role in smoking cessation through assessment, education, support, interventions, and follow-up.
Through the utilization of evidence-based practices and treatments, as well as ongoing research, nurses can successfully reduce the burden of smoking cessations and related diseases, as well as improve the possibility of patients quitting smoking for good.
References + Disclaimer
- Henningfield, J., & Rose, Christine A. (2024, December 13). The antismoking movement. Encyclopædia Britannica. https://www.britannica.com/topic/smoking-tobacco/The-antismoking-movement
- Centers for Disease Control and Prevention. (2024, September 17). Cigarette smoking. https://www.cdc.gov/tobacco/about/index.html
- Centers for Disease Control and Prevention. (2024b, September 17). Current cigarette smoking among adults in the United States. https://www.cdc.gov/tobacco/php/data-statistics/adult-data-cigarettes/index.html
- World Health Organization. (2023, July 31). Tobacco. https://www.who.int/news-room/fact-sheets/detail/tobacco
- American Cancer Society. (2024, November 19). Why people start using tobacco, and why it’s hard to stop. Why People Start Using Tobacco, and Why It’s Hard to Stop | American Cancer Society. https://www.cancer.org/cancer/risk-prevention/tobacco/guide-quitting-smoking/why-people-start-using-tobacco.html
- Gallucci, G., Tartarone, A., Lerose, R., Lalinga, A. V., & Capobianco, A. M. (2020, July). Cardiovascular risk of smoking and benefits of smoking cessation. Journal of thoracic disease. https://pmc.ncbi.nlm.nih.gov/articles/PMC7399440/
- Centers for Disease Control and Prevention. (2024d, September 17). Health effects of cigarettes: Cardiovascular disease. https://www.cdc.gov/tobacco/about/cigarettes-and-cardiovascular-disease.html#:~:text=Smoking%20is%20a%20major%20cause,from%20cardiovascular%20disease%20and%20death.
- Seo, Y.-S., Park, J.-M., Kim, J.-H., & Lee, M.-Y. (2023). Cigarette smoke-induced reactive oxygen species formation: A concise review. Antioxidants, 12(9), 1732. https://doi.org/10.3390/antiox12091732
- Centers for Disease Control and Prevention. (2024a, May 15). Respiratory care settings and smoking cessation. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/hcp/patient-care-settings/respiratory.html
- Centers for Disease Control and Prevention. (2023b, October 13). Smoking and cancer. https://www.cdc.gov/tobacco/campaign/tips/diseases/cancer.html
- National Institutes of Health. (2021, April 12). What are treatments for tobacco dependence? https://nida.nih.gov/publications/research-reports/tobacco-nicotine-e-cigarettes/what-are-treatments-tobacco-dependence
- Piedmont Healthcare. (2024). Schedule your appointment online. Benefits and Facts on Quitting Smoking. https://www.piedmont.org/living-real-change/never-too-late-to-quit-smoking
- Gaddey, H. L., Dakkak, M., & Jackson, N. M. (2022, November 15). Smoking cessation interventions. American Family Physician. https://www.aafp.org/pubs/afp/issues/2022/1100/smoking-cessation-interventions.html#:~:text=The%20U.S.%20Public%20Health%20Service,Table%2015%E2%80%939
- Goldberg, L. R., & Gould, T. J. (2022). Genetic influences impacting nicotine use and abuse during adolescence: Insights from human and rodent studies. Brain Research Bulletin, 187, 24–38. https://doi.org/10.1016/j.brainresbull.2022.06.007
- Lengel, D., & Kenny, P. J. (2023, September). New medications development for Smoking Cessation. Addiction neuroscience. https://pmc.ncbi.nlm.nih.gov/articles/PMC10373598/
- Cobos-Campos, R., Cordero-Guevara, J. A., Apiñaniz, A., de Lafuente, A. S., Bermúdez Ampudia, C., Argaluza Escudero, J., Pérez Llanos, I., & Parraza Diez, N. (2023). The impact of digital health on Smoking Cessation. Interactive Journal of Medical Research, 12. https://doi.org/10.2196/41182
- Fang, F., Andersen, A. M., Philibert, R., & Hancock, D. B. (2023). Epigenetic biomarkers for smoking cessation. Addiction Neuroscience, 6, 100079. https://doi.org/10.1016/j.addicn.2023.100079
- Auer, R., Schoeni, A., Humair, J.-P., Jacot-Sadowski, I., Berlin, I., Stuber, M. J., Haller, M. L., Tango, R. C., Frei, A., Strassmann, A., Bruggmann, P., Baty, F., Brutsche, M., Tal, K., Baggio, S., Jakob, J., Sambiagio, N., Hopf, N. B., Feller, M., … Berthet, A. (2024). Electronic nicotine-delivery systems for Smoking Cessation. New England Journal of Medicine, 390(7), 601–610. https://doi.org/10.1056/nejmoa2308815
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
