Spinal Cord Injury: Bowel and Bladder Management
Contact Hours: 2
Author(s):
Charmaine Robinson MSN-Ed, BSN, RN, PHN, CMSRN
Course Highlights
- In this Spinal Cord Injury: Bowel and Bladder Management course, we will learn about bladder dysfunction that can occur in patients with spinal cord injuries.
- You’ll also learn ways nurses can help patients with spinal cord injuries start a bowel and bladder regimen.
- You’ll leave this course with a broader understanding of ways nurses can manage bowel dysfunction in patients with spinal cord injuries.
Introduction
Imagine one day you can walk and take care of your own needs. Now, imagine one week later you wake up no longer able to walk, feel anything below your waist, or hold your bowels.
This is a reality for many people who sustain spinal cord injuries. Managing changes in bowel and bladder function is one of many challenges that people with spinal cord injuries and their families or caregivers face.
This course will provide learners with the knowledge needed to assist patients with spinal cord injuries with bowel and bladder management to improve the quality of life in this group.
Ask yourself...
- What are some societal misconceptions or stereotypes about people with spinal cord injuries?
- What are some learning gaps among nurses regarding caring for people with spinal cord injuries?
- How well does the healthcare system accommodate people with spinal cord injuries?
- How often do you care for a spinal cord injury patient?
- What challenges have you encountered when caring for patients with spinal cord injuries?
Spinal Cord Injuries: The Basics
Spinal Cord Function
Before defining a spinal cord injury, it is important to understand its function. The spinal cord is a structure of the nervous system nestled within the vertebrae of the back and helps to distribute information from the brain (messages) to the rest of the body [1].
These messages result in sensation and other neurological functions. While it may be common to primarily associate the nervous system with numbness, tingling, or pain, nerves serve an important purpose in the body’s function as a whole.
Spinal Cord Injury Definition
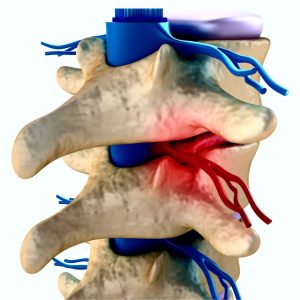
When the spinal cord is injured, messages from the brain may be limited or entirely blocked from reaching the rest of the body. Spinal cord injuries refer to any damage to the spinal cord caused by trauma or disease [2]. They can result in problems with sensation and body movements.
For example, the brain sends messages through the spinal cord to muscles and tissues to help with voluntary and involuntary movements. This includes physical activity like running and exercising, or something as simple as bowel and bladder elimination.
Spinal Cord Injury Causes
Spinal cord injuries occur when the spinal cord or its vertebrae, ligaments, or disks are damaged [3]. While trauma is the most common cause of spinal cord injuries in the U.S., medical conditions are the primary cause in low-income countries [4] [2].
Trauma
- Vehicle accidents: Account for 40% of all cases [2]
- Falls: Accounts for 32% of all cases [2]
- Violence: Includes gun violence and assaults; accounts for 13% of all cases [2] [5]
- Sport-related accidents: Account for 8% of all cases [2]
Medical Conditions
- Multiple Sclerosis (MS): Damage to the myelin (or insulating cover) of the nerve fibers [1]
- Amyotrophic Lateral Sclerosis (ALS): Lou Gehrig’s disease, damage to the nerve cells that control voluntary muscle movements [1]
- Post-Polio: Damage to the central nervous system caused by a virus [1]
- Spina Bifida: Congenital defect of the neural tube (structure in utero that eventually forms the central nervous system) [1]
- Transverse Myelitis (TM): Inflammation of the spinal cord caused by viruses and bacteria [1]
- Syringomyelia: Cysts within the spinal cord often caused by a congenital brain abnormality [1]
- Brown-Sequard Syndrome (BSS): Lesions in the spinal cord that cause weakness or paralysis on one side of the body and loss of sensation on the other [1]
- Cauda Equina Syndrome: Compression of the nerves in the lower spinal region [1]
Spinal Cord Injury Statistics
According to the World Health Organization, between 250,000 and 500,000 people worldwide are living with spinal cord injuries [4]. In the U.S., this number is estimated to be between 255,000 and 383,000, with 18,000 new cases each year for those with trauma-related spinal cord injuries [6].
Age/Gender
Globally, young adult males (age 20 to 29) and males over the age of 70 are most at risk. In the U.S., males are also at highest risk, and the average age of this group is 43 [2].
While it is less common for females to acquire a spinal cord injury (2:1 ratio in comparison to males), when they do occur, adolescent females (15-19) and older females (age 60 and over) are most at risk globally [4].
Race/Ethnicity
In the U.S., since 2015, around 56% of spinal cord injuries related to trauma occurred among non-Hispanic whites, 25% among non-Hispanic Black people, and about 14% among Hispanics [6].
Mortality
People with spinal cord injuries are 2 to 5 times more likely to die prematurely than those without these injuries (WHO, 2013). People with spinal cord injuries are also more likely to die within the first year of the injury than in subsequent years. In the U.S., pneumonia and septicemia – a blood infection – are the top causes of death in patients with spinal cord injuries [6].
Financial Impact
Spinal cord injuries cost the U.S. healthcare system billions each year [6]. Depending on the type, spinal cord injuries can cost from around $430,000 to $1,300,000 in the first year and between $52,000 and $228,000 each subsequent year [6].
These numbers do not account for the extra costs associated with loss of wages and productivity, which can reach approximately $89,000 annually [6].
Ask yourself...
- What is one function of the spinal cord?
- What is one way to prevent spinal cord injuries in any group?
- Why do you think injuries caused by medical conditions are least likely to occur in the U.S.?
- Why do you think the first year of care after the injury is the most costly?
Think about someone you know (or cared for) who had a spinal cord injury.
- Did they have total or partial loss of feeling and movement to the extremities?
- What comorbidities or complications did they have associated with the injury?
- In what ways did the injury affect their overall quality of life?
Spinal Cord Injuries: Types and Complications
Four Levels of the Spinal Cord
- Cervical (vertebrae C1 – C8): Neck; controls the back of the head down to the arms, hands, and diaphragm
- Thoracic (vertebrae T1 – T12): Upper mid-back; controls the chest muscles, many organs, some back muscles, and parts of the abdomen
- Lumbar (vertebrae L1 – L5): Lower back; controls parts of the lower abdomen, lower back, parts of the leg, buttocks, and some of the external genital organs
- Sacral (vertebrae S1 – S5): Lower back; control the thighs down to the feet, anus, and most of the external genital organs
Types of Spinal Cord Injuries
Spinal cord injuries may be classified by level and degree of impairment. There are four types of spinal cord injuries [5].
Injury Level
- Tetraplegia or Quadriplegia: Injury at the cervical level; loss of feeling or movement to the head, neck, and down. People with this type of spinal cord injury have the most impairment.
- Paraplegia: Injury at the thoracic level or below; limited or complete loss of feeling or movement to the lower part of the body.
Impairment
- Incomplete spinal cord injury: Some sensations and mobility are below the level of injury as the spinal cord can still transmit some messages from the brain.
- Complete spinal cord injury: Total loss of all sensation and mobility below the level of injury. Spinal cord injuries of this type have the greatest functional loss.

Spinal Cord Injury Complications
Complications from spinal cord injuries can be physical, mental, or social and can impact overall quality of life. There are six common complications of spinal cord injuries [2].
Depression
Studies show that 32.9% of adults with disabilities experience frequent mental distress [7]. Mental distress may be related to functional limitations, chronic disease, and the increased need for healthcare services. Up to 37% of people with spinal cord injuries develop depression [2].
Pressure injuries
People with spinal cord injuries may have problems with circulation and skin sensation, both risk factors for pressure injuries. Some may be bedridden or wheelchair-bound, which also places them at risk for pressure injuries. Up to 80% of people with spinal cord injuries will have a pressure injury during their lifetime and 30% will have more than one [2].
Spasticity
Around 65%—78 % of people with spinal cord injuries have spasticity [2]. Spasticity is uncontrolled muscle tightening or contraction. The damage from spinal cord injuries causes misfires in the nervous system, leading to muscle twitching, jerking, or stiffening.
Autonomic dysreflexia
In some people with spinal cord injuries, a full bladder or bowel distention can cause a potentially dangerous condition called autonomic dysreflexia. The full bladder or bowel triggers a sudden, exaggerated reflex that increases blood pressure. This condition is also associated with a severe headache, low heart rate, cold skin, and sweating in the lower body [8].
Respiratory problems
If the diaphragm function is affected, as with cervical spinal cord injuries, breathing difficulties may occur. People with lumbar spinal cord injuries can even have respiratory problems, as the abdominal muscles are used to breathe.
Sexual problems
Due to changes in muscle function and depending on the degree of damage, people with spinal cord injuries may have problems with arousal and climax due to altered sensations and changes in sexual reflexes.
Changes in bowel and bladder function
Many people with spinal cord injuries lose bowel control. Bowel problems can include constipation, impaction, and incontinence. They may also have problems with urination, such as urinary retention.
Ask yourself...
- Why might a person with a disability experience mental distress?
- In what type of spinal cord injury does a person lose all sensation and mobility below the waist?
- Why are people with spinal cord injuries at risk for pressure injuries?
- How can spinal cord injuries affect a person’s personal relationships?
- What is the difference between tetraplegia and paraplegia?
- What education can you provide to patients and their families when trying to prevent pressure injuries in patients with a SCI?
- How does the function of a patient’s bowel and bladder change after a spinal cord injury?
Bowel and Bladder Dysfunction in Spinal Cord Injuries
This section will cover the normal function of the bowel and bladder and the types of bowel and bladder dysfunction in patients with spinal cord injuries.

Ask yourself...
Think about a time you assisted with bowel or bladder management in someone with a spinal cord injury.
- What types of activities were included in their bowel or bladder regimen?
- What challenges did you encounter during bowel or bladder care?
- What difficulties did they express about managing their bowel or bladder program?
- In what ways did you assist them in managing their own bowel or bladder program?
Normal Bowel and Bladder Function
In normal bowel and bladder function, when the rectum or bladder fills with stool or urine and presses on area nerves (stimulation), the message is sent to the spinal cord, which sends it to the brain. The brain gives the person the “urge” feeling, allowing an option to control the elimination.
Whatever decision the person makes, the brain sends the message back to the spinal cord, which in turn sends a message to the elimination muscles (anal and bladder sphincters) to either relax or stay closed until the person is ready. In people with spinal cord injuries, the messages are limited or blocked, leading to problems with bowel and bladder control [9] [10].
Bowel Dysfunction with Spinal Cord Injuries
Reflex hypertonic neurogenic bowel occurs when a rectum full of stool presses against area nerves, sending a message to the spinal cord, but it stops there. The message never gets to the brain, so the person never gets the urge.
As a result, a reflex is set off, prompting the spinal cord to send a message to the anal muscle (sphincter) instead, causing it to relax and release the stool. This condition leads to bowel incontinence and usually occurs in spinal injuries at the cervical and thoracic levels [9] [10].
Flaccid hypotonic bowel occurs when a full rectum stimulates area nerves, but the message does not even reach the spinal cord, so there is no reflex. The anal sphincter is always in a relaxed state.
As a result, the bowels are empty when full, which can occur at any time without the person being able to control it. This condition results in bowel incontinence and can lead to constipation as the patient does not have the urge and may not have the ability to push. This condition usually occurs in spinal injuries at the lumbar level [9] [10].
Bladder Dysfunction with Spinal Cord Injuries
Reflex neurogenic bladder occurs when the bladder automatically starts to contract after filling with a certain amount of urine. The person has no urge to go, as the messages are either limited or blocked from reaching the brain, leading to loss of bladder control. Like the reflex hypertonic neurogenic bowel, the full bladder triggers nerves that set off a reflex, prompting the spinal cord to send messages to the bladder, releasing urine outside of the person’s control [9] [10].
A contractile bladder occurs when it loses muscle tone after a spinal cord injury, lessening its ability to contract, leading to bladder distention and dribbling of urine. People with this condition must use urinary catheters to help empty the bladder [9].

Ask yourself...
- What is one role of the brain in bowel and bladder function?
- Which type of bowel dysfunction occurs in thoracic-level spinal cord injuries?
- In which type of bowel dysfunction might a suppository be most effective?
- In which type of bladder dysfunction does the bladder lose muscle tone?
- What is a neurogenic bowel?
- What is a flaccid hypotonic bowel?
- Describe a neurogenic bladder.
- How is a contractile bladder different from a neurogenic bladder?
The Nurse’s Role in Bowel and Bladder Management
This section will cover how nurses can assess, intervene, and teach when caring for patients with spinal cord injuries who have bowel and bladder dysfunction.
Ask yourself...
Think about your experiences with patients with spinal cord injuries and their families or caregivers.
- How knowledgeable was the patient about their bowel or bladder care?
- In what ways was the family or caregiver involved in the plan of care?
- Did the family or caregiver have any learning gaps that needed to be addressed?
- What difficulties did the family or caregiver express to you about their role?
Nurse Assessments
When caring for patients with spinal cord injuries, nurses should obtain a detailed bowel and bladder history, including diet, fluid intake, medications, and elimination patterns/habits [11]. Many of these patients may already manage their bowel and bladder care at home.
If so, the nurse should obtain the patient’s current regimen and communicate the information to the physician. Based on the patient’s current illness/condition, the physician may choose to continue the regimen or adjust it as needed.
Questions the nurse can ask the patient:
- What does your typical diet consist of?
- How much fluid do you drink on a daily basis?
- How often do you have a bowel movement or urinate?
- Do you schedule your bowel movements with assistance from medications?
- Are there certain body positions or things you do to help you pass stool more easily?
- How often do you use an intermittent urinary catheter for bladder relief?
- How much time do you spend on your bowel and bladder regimens?
- Do you care for all of your elimination needs, or does someone help you?
- How does your bowel and bladder dysfunction affect your quality of life?
Some assessments may be observed. For example, nurses may notice that the patient has a surgically placed permanent suprapubic urinary catheter or colostomy (when the bowel is cut somewhere above the level of the rectum and diverted to the outside of the abdomen).
Nurse Interventions
Since many patients with spinal cord injuries have problems with bowel and bladder function, elimination must be scheduled. Nurses can help by implementing bowel and bladder programs and providing education and support to patients, families, or caregivers.
Regimens
Follow the patient’s home bowel and bladder regimen (as ordered). This may include maintaining intermittent catheterization every few hours or administering suppositories daily.
For patients who do not have a regimen already or wish to modify their current one, encourage them to pay attention to how often they urinate and pass stools, elimination problems, foods that alleviate or worsen the problem, and medications or other things that help. This can be done through a diary.
Dietary Considerations
Educate patients on the importance of a fiber-rich diet to avoid constipation. Patients should also be made aware that high-fat foods, spicy foods, and caffeine can alter gut dynamics and lead to bowel incontinence episodes [12].
Fluid Intake
Some patients may avoid drinking enough water to avoid bladder complications (e.g., frequent incontinent episodes) [12]. However, nurses should educate patients on the importance of adequate fluid intake to prevent constipation. Patients should be made aware that bladder and bowel elimination regimens go hand in hand.
Bladder Elimination
For bladder dysfunction, help patients perform intermittent urinary catheterization as needed or place a temporary urinary catheter (as ordered).
Bowel Elimination
For bowel dysfunction, administer ordered suppositories and laxatives to help the bowels move (use suppositories in conjunction with the level of sensation the patient has near the anus/rectum) [9]. Changes in body position may help as well.
While many of these interventions may not work in some patients with spinal cord injuries, bowel irrigation (water enemas) may be helpful [11]. If all other measures have failed, surgical placement of a colostomy may be indicated [11].
Emotional Support
Ensure privacy and sensitivity during all elimination care, as patients may experience embarrassment or frustration.
Education for Families or Caregivers
Educate families or caregivers on the importance of helping patients stay consistent with their elimination regimen, follow diet and fluid intake recommendations, and comply with medication orders.
Referrals
Inform the physician if interventions are ineffective or if the patient, family, or caregiver has a special need (e.g., counselor or dietician). Refer patients and families or caregivers to support groups as needed.
Support Groups and Resources
Christopher and Dana Reeve Foundation
Christopher Reeve – an actor who was left paralyzed after an equestrian accident – and his wife Dana’s legacy lives on through their foundation, an organization that advocates for people living with paralysis [13].
Miami Project to Cure Paralysis
In response to his son, who acquired a spinal cord injury during college football, NFL Hall of Famer Nick Buoniconti and world-renowned neurosurgeon Barth A. Green, M.D. started a research program aimed at finding a cure for paralysis and discovering new treatments for many other neurological injuries and disorders [14].
National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR)
The National Institute on Disability, Independent Living, and Rehabilitation Research, a part of the U.S. Department of Health and Human Services’ Administration for Community Living, helps people with disabilities integrate into society, employment, and independent living [15].
Paralyzed Veterans of America (PVA)
A group of World War II veterans who returned home with spinal cord injuries started this organization to support those with spinal cord injuries and dysfunction. Today, the organization focuses on quality health care, research and education, benefits, and civil rights for affected veterans [16].
The United Spinal Association supports people with spinal cord injuries and those in wheelchairs. The organization advocates for disability rights like access to healthcare, mobility equipment, public transportation, and community support. Support groups can be found on their website [17).
Ask yourself...
- What is one question a nurse can ask a patient to obtain a bowel and bladder history?
- How can nurses help patients with spinal cord injuries start or modify a bowel or bladder regimen?
- When might a colostomy be indicated for a patient with a spinal cord injury?
- What type of referral might be ordered for a patient with a spinal cord injury who has bowel or bladder dysfunction?
Conclusion
Spinal cord injuries can have devastating effects on patients and their families. Managing basic bodily functions, such as bowel and bladder elimination, should be easy for these patients.
When nurses learn how to effectively help patients with spinal cord injuries better manage their own bowel and bladder regimens, quality of life and health outcomes may be improved for this group.
References + Disclaimer
- United Spinal Association. (n.d.). What is spinal cord injury/disorder? Retrieved from https://unitedspinal.org/what-is-spinal-cord-injury-disorder-scid/
- United Spinal Association. (2022). Spinal cord injuries facts and stats. Retrieved from https://unitedspinal.org/spinal-cord-injury-facts-and-stats/
- U.S. Department of Health and Human Services, National Institutes of Health. (2022). What causes spinal cord injury (SCI) and how does it affect your body? Retrieved from https://www.nichd.nih.gov/health/topics/spinalinjury/conditioninfo/causes
- World Health Organization. (2013). Spinal cord injury. Retrieved from https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury
- National Institute of Neurological Disorders and Stroke. (2023). Spinal cord injury. Retrieved from https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury
- National Spinal Cord Injury Statistical Center. (2023). Traumatic spinal cord injury statistics: Facts and figures at a glance. Retrieved from https://www.nscisc.uab.edu/public/Facts%20and%20Figures%202023%20-%20Final.pdf
- Centers for Disease Control and Prevention. (2020). Many adults with disabilities report frequent mental distress. Retrieved from https://www.cdc.gov/ncbddd/disabilityandhealth/features/adults-with-disabilities-mental-distress.html
- Allen K. J. & Leslie S. W. (2023). Autonomic dysreflexia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482434/
- Bowel and Bladder Community. (n.d.). Spinal injuries. Retrieved from https://www.bladderandbowel.org/help-information/spinal-injuries/
- Shepherd Center. (n.d.). Bowel function after SCI. Retrieved from https://www.myshepherdconnection.org/sci/bowel-care/function-after-sci
- Emmanuel A. (2019). Neurogenic bowel dysfunction. F1000Research, 8, F1000 Faculty Rev-1800. https://doi.org/10.12688/f1000research.20529.1
- Gater, D. R., Bauman, C., & Cowan, R. (2020). A primary care provider’s guide to diet and nutrition after spinal cord injury. Topics in spinal cord injury rehabilitation, 26(3):197–202. https://doi.org/10.46292/sci2603-197
- Christopher & Dana Reeve Foundation. (2023). Our mission. Retrieved from https://www.christopherreeve.org/community/about-us/history-of-the-reeve-foundation/
- University of Miami, Miller School of Medicine. (n.d.). About us. Retrieved from https://www.themiamiproject.org/about-us/
- U.S. Department of Health and Human Services, Administration for Community Living. (n.d.) Advancing independence, integration, and inclusion throughout life. Retrieved from https://acl.gov/
- Paralyzed Veterans of America. (n.d.). Mission statement. Retrieved from https://pva.org/about-us/mission-statement/
- United Spinal Association. (2023). About us. Retrieved from https://unitedspinal.org/our-story/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
