Course
Spinal Fusion Surgery and Aftercare
Course Highlights
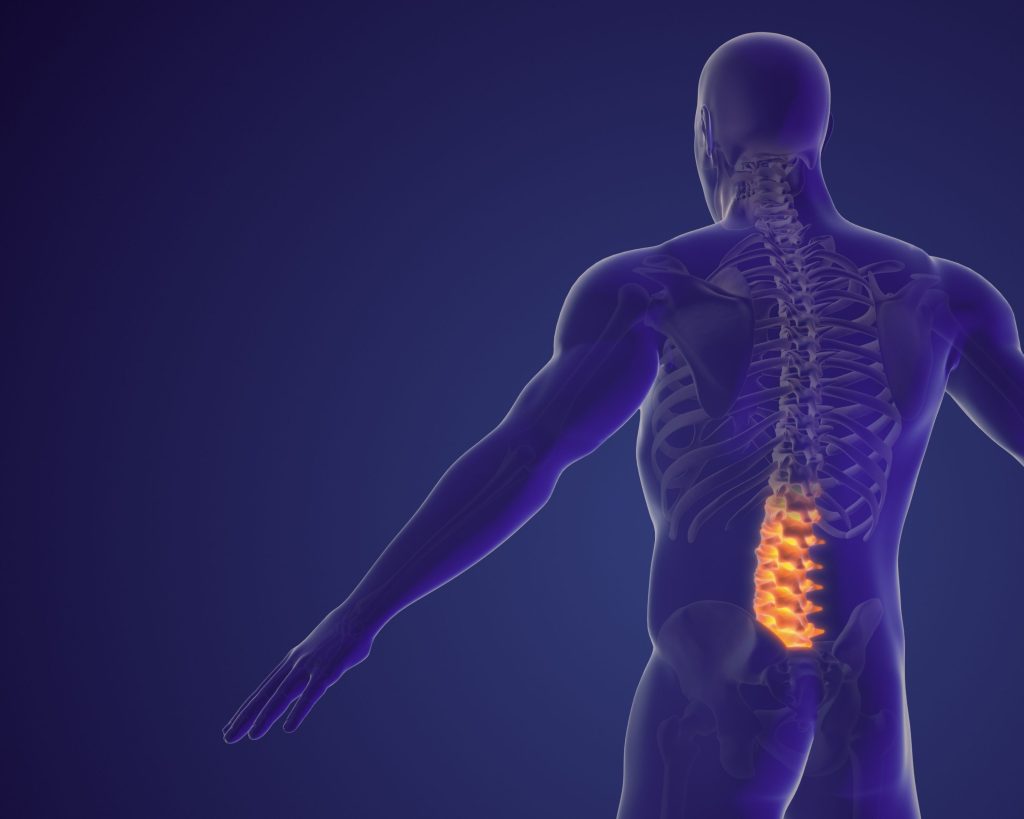
- In this Spinal Fusion Surgery and Aftercare course, we will learn about anatomy and physiology of the spine.
- You’ll also learn the epidemiology of low back pain (LBP).
- You’ll leave this course with a broader understanding of the characteristics of those needing spinal fusion.
About
Contact Hours Awarded: 2
Course By:
Elaine Enright, ADN, BSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
The spine consists of 33 bony vertebrae. These contiguous vertebrae are named by their location in the body. Cervical (head and neck), thoracic (chest and torso), lumbar (low back), sacral (pelvis), and coccyx (tail bone). Fibrocartilage pads or discs separate the 24 vertebrae of the spine. The cervical spine allows for the twisting and turning of the neck, while the lumbar spine allows for support to the body, flexibility to twist and bend, and load sharing while lifting, pushing, and pulling (2).
The spinal column also protects the spinal cord and the nerves within it. There are many etiologies for disruption of the discs, such as herniation and protrusion, traumatic injuries, infections, and vascular damage (3); which may apply pressure to the spinal cord nerves, causing pain, numbness, less range of motion (ROM), and weakness in the extremities. There are several invasive and non-invasive approaches to caring for clients experiencing LBP. These include stretching exercises, walking, medication, brace use, and physical therapy. Suppose the pain and weakness become disabling for clients who then cannot perform ADLs or independent activities of daily living (IADLs), or for those with severe acute injuries. For these clients, surgery may be an option.

Self-Quiz
Ask Yourself...
- Where can you find more information on how chronic back LBP affects the neurological system?
- Which parts of the spine are usually fused in humans?
- Can you further define the parts of the spine and their job?
- What are some other non-invasive for LBP?
Epidemiology
Chronic Low back pain (CLBP) is the leading cause of disability in Western countries (1). CLBP has a high socio-economic burden on society (1, 3). In one study, clients filled out questionnaires with complaints about CLBP. These questionnaires focused on “disability, quality of life, workability, psychosocial work environment, and productivity.” (1). Included in this study were 1502 clients with an average of 46.3 plus or minus 12.8 years of age over some time. The impact of CLBP on society in the Netherlands was high. A minority of clients in this study had the highest number of disabilities, with the authors hypothesizing this probably caused the highest cost for this diagnosis (1).
In another study (3), the incidence of spinal cord injury has increased over the last 30+ years (3). Falls and motor vehicle accidents accounted for the highest number of spinal cord injuries, with more men and the elderly accounting for them (3). Economically, the costs of spinal cord injury is higher than most other chronic diseases owing to the rate of chronic disability. The mean cost in acute situations ranged from $30,770 to $612,590, with inpatient rehabilitation costing $19,536 to $443,044 the first-year post-injury across Western countries. (5) In the U.S. alone, total charges have increased exponentially since 1997, with higher costs associated with long-term or permanent disability (5).
The number of cases of CLBP has gone from 236 to 1298 within the last 30 years or so, and approximately $3,000,000 per chronic lifelong disability. Globally, the cost is anywhere from $250,000 to $500,000 per client per year (6). Scientists have concluded that earlier spine decompression will lower costs (5).

Self-Quiz
Ask Yourself...
- Can you find more statistics on the impact of CLBP in your area?
- What do you think is the reason more males are diagnosed with spinal cord injury?
- Why do you think spinal cord injury has increased over the last two decades?
- Where can you find more information on the total cost of this problem?
Assessment
As previously stated, chronic low back pain is the most common diagnosis of disability in Western countries. Clients who see a provider will need a complete workup for this complaint. The provider will provide a full evaluation of clients with LBP seeking treatment. For the initial encounter, X-rays of the spine and entire history, including location, duration of pain, and any associated weakness, numbness, and restricted range of motion, will be obtained (4).
A gait evaluation should be included in the physical exam, which may indicate an unstable spine, and strength, reflex, and vascular circulation must be included in the first encounter (2). There are four “red flags” that should be aggressively treated when discovered during a history and physical (2). These are bowel and bladder issues, infection, which may indicate an IV drug user, suspicion of cancer, and trauma from an accident, fall, or assault (2).
At this juncture, if the client’s injury is minor, the provider may prescribe oral steroids and pain medication along with six weeks of physical therapy (2). An MRI typically will not be done unless this conservative treatment fails. Steroid injections may also be utilized as a less invasive treatment and may give the patient temporary or prolonged relief.
When the MRI is obtained, degenerative findings may be found in the discs and the facet joints. The facet joints allow each vertebra to be connected to the adjoining vertebra (4). Some prognostic tests may be performed to understand and help the provider determine if the client is a candidate for spinal fusion. In a Netherlands study, surgeons disagreed on whether these prognostic tests predicted which clients were suitable for spinal fusion (4).
However, the participants in the Netherlands study recommended that clients be assessed in a multidisciplinary setting, such as a spine center, including behavioral assessments and physical symptoms in chronic LBP clients. Most spine centers have this capacity as they practice in a biopsychosocial setting (4). As with any other treatment in medicine, LBP should initially be treated with noninvasive protocols and progress to the next step if the prior treatment does not work. Spinal fusion is the most invasive (4).

Self-Quiz
Ask Yourself...
- Why would a provider not go straight to MRI instead of X-rays first in a client with LBP?
- What might be the most critical aspect to assess in the history and physical of a client with LBP?
- Do you know if your facility or town where you are employed has a spine center?
- Why might a behavioral health specialist be necessary in a spine center?
Etiology
Tiny blood vessels surrounding the spinal cord deliver oxygen, nutrients, and chemo-modulators to the spine (2). When these are damaged through injury or degeneration, there is inflammation and pain along the injured nerve root (2). Clients may experience radiation of pain to the buttocks, lower limbs, and in the case of a neck injury, radiation to the shoulders and upper limbs.
Nurses know that age and lifestyle of our older population can cause back pain from bony and disc degeneration, arthritis, etc. We all know nurses and other health care workers who are on their feet for a 12-hour shift to have back pain or injury. Have you ever twisted the “wrong” way and had back pain? This is prevalent among clients standing all day, loading and unloading parcels or other heavy lifting positions. It is not unusual for anyone to have back pain. Even poor posture can cause LBP.
Motor vehicle accidents with or without seat belts are prevalent causes of spinal cord injury. Furthermore, we’ve all heard about athletes injuring their spine in a game, maybe football or rugby, or even a damaging fall during play. Just about any sport can cause trauma to the spine, including head and neck trauma. If the trauma is severe, it could cause paraplegia or quadriplegia. Less traumatic injuries may cause life-long or chronic instability and disability.
It is a known fact that sudden trauma may cause injury to the spine (6). Injuries are classified as Primary injuries and are the initial diagnoses made immediately after trauma. This phase may show fragmented bone tearing to the ligaments and destruction of the tissues. There can be hemorrhaging and disruption of the glial membrane (6). Injuries are classified by severity, including length of spinal cord compression and the extent of the injury (6). Post-injury, many of the cell types located in the spine are disrupted, causing more damage to the spinal cord.
Secondary injury is triggered by the primary injury, causing more chemical and mechanical issues. These issues result in neurological dysfunction. Cells become more permeable; there is ischemia, damage to the vascular system, inflammation, free radical production, and other concerns (6). There might be hemorrhaging, which triggers the invasion of white blood cells to spinal tissues, including T and B lymphocytes, neutrophils, monocytes, and macrophages (6).
Three phases of secondary injury cause further disruption. They are acute, subacute, and chronic (6). Spinal ischemia, edema, and excitotoxicity occur in the acute phase, which overlaps with the subacute phase, causing more cellular interruption and neuroinflammation with necrosis of tissues (6).
Three weeks after the injury, scar tissue forms, protecting the non-damaged nerves and stopping phagocytosis (6).

Self-Quiz
Ask Yourself...
- Can you think of other types of traumas that may cause spinal cord injury?
- Where can you find more in-depth information about the pathophysiology of spinal cord injury?
- What causes scar tissue to form?
- What roles do the B and T cells perform in this injury?
Candidates for Surgery
So, when is surgery indicated for a spinal cord-injured client? Today, with the aging population, more spinal surgery is performed to alleviate lower back pain due to degeneration of the spine. As we age, the fluid that keeps the discs mobile decreases, causing the discs to shrink (7). This creates bone spurs, thus pressuring the nerves and causing pain and decreased mobility (8). This is more common in people who smoke, are overweight or obese, or those who do heavy labor (7).
Of course, in an acute injury such as a motor vehicle accident or other major trauma, surgery may be performed immediately in extreme cases or when the client is stabilized. Clients with LBP caused by herniated discs, spinal stenosis, vertebral fractures, and spondylolisthesis with severe unrelenting pain are good candidates for spinal surgery.
In another study, they indicated that spinal surgery had increased by over 70% between 1996 and 2001, with a continued increase between 1998 and 2014, with a total increase of 137% (15). This number reflects cervical, thoracic, and lumbar surgeries (8). These numbers also increased due to a better understanding of the pathophysiology of the spine, diagnostic tools that are newer and better, and newer technology to perform the surgery. Minimally invasive surgery and better outcomes have also contributed to the increase in spinal surgery while helping to decrease the number of repeated surgeries (8). In the next section, we will discuss the types of spinal surgery, from the earliest type of surgery to the newest.


Self-Quiz
Ask Yourself...
- Can you find the number of spinal surgeries performed in your facility or hospital in your area?
- Can you find the cause of bone spurs in the spine?
- Can you research why spinal surgery may not be indicated in some clients?
- Where can you find how many spinal surgeries are performed in a year?
History of Spinal Surgery
We will begin this section with the history of spinal surgery. As far back as the 5th century BC, Hippocrates was able to describe abnormalities in the spine, such as scoliosis, lordosis, and kyphosis. (10). He felt that spinal problems were caused by consistent poor posture, especially in the case of young people with scoliosis (10).
Five centuries later, Claudius Galen, using his knowledge of anatomy and physiology, devised chest binders and jackets to attempt to fix scoliosis. He also encouraged singing loudly to stimulate the rib cage (10). His books were the staple for curing spinal abnormalities until Vesalius came along and made diagrams of human cadavers (10). His drawings and Galen’s descriptions were the most used strategies (10).
During the Middle Ages, when religion was the universal belief, medical experts believed that scoliosis was divine justice since there was no distinct division between the church and state. (10) This era saw clients placed on a rack as a treatment to correct curvatures. In 1761, Francois LeVacher made the first brace, enabling clients to be mobile during treatment (10).
In 1780, the first orthopedic hospital was built in Switzerland, hoping that orthopedic medicine would expand and create a place for disabled people to get treatment (10).
In 1839, a physician named Jules Guerin attempted the first surgery to correct spinal abnormalities (10). In the 1880s, plaster casts were used to keep the spine straight in children (10). Continuing with the idea of stabilizing the spine, another surgeon used celluloid bars, steel, and silk wiring (10).
In 1955, Dr. Paul Harrington invented the “Harrington Rod.” This procedure attached to the spine and kept it rigid until it straightened. Similar rods were adapted with more flexibility than the Harrington rod (10). The FDA approved Intervertebral Spinal fusion in 1996, leading to a rapid rate of spinal fusions. Today, minimally invasive spinal fusion is state-of-the-art for this surgery (8).

Self-Quiz
Ask Yourself...
- Can you find more history on spinal surgery?
- Have you ever cared for a client with a cast after back surgery?
- Can you research the Harrington Rod?
- What type of surgery was performed when the FDA first approved intervertebral surgery?
Types of Contemporary Spinal Surgery
After many years of searching for the best way to repair spinal abnormalities, fusion surgery has been named the most common type. It is used to correct several deformities, including scoliosis,
congenital deformities, and those issues caused by aging, disc disease, spinal stenosis, trauma, infection, and tumor” (8). Iliac bone graft has been the most common bone used in grafting; however, donor complications and the scarcity of bone have made its widespread use infrequent (7). Bone Morphogenetic Proteins (BMPS) used during surgery help accelerate bone growth. Other common BMPs are being used to promote bone growth as well (7).
Depending on the location of the injury, there are different approaches to spinal surgery. Laminectomy refers to the removal of the lamina (the arch of the vertebra) in spinal stenosis to relieve pressure on the nerve. This is also called decompression surgery (11). Another surgery for L 4-5 and L5-S1 uses the anterior retroperitoneal approach, allowing for an efficient discectomy without damage to the posterior neural structures. This surgery corrects Lordosis; however, it can cause vascular and visceral issues (8).
Spinal fusion has come a long way from casts and braces. This surgery melds two or more vertebrae to stabilize the back and uses pins and plates to fuse the vertebrae (13). It can relieve pain associated with several diagnoses, such as spinal stenosis, scoliosis, fractured vertebrae, disc herniations, tumors, and degenerative disc disease (13). To correct the spine, the surgeon will choose the best approach to the injured vertebrae.
The anterior approach will be done through the lower abdomen and can be used for cervical and lumbar spine fusions (13). Two other methods may be used depending on the site of the problem. These are the side or posterior approaches located on either side of the body or the back. The surgeon will determine which approach will be the most advantageous for the vertebrae that need repair. To stabilize the spine, a surgeon uses “plates, screws, and rods (13)” to realign the spine (13). Some clients may use a back brace to stabilize the spine while recovering.
Since the first fusion performed by Dr. Russell A. Hibbs in 1911, there have been many revisions and newer techniques for performing this surgery (8). “With the advent of endoscopic and technology,” older versions such as microscopic surgery have been replaced with endoscopic surgery, a much safer, more efficient means to correct spinal problems (8, 9). Its benefits are also minimally invasive, needing a smaller incision than older fusions.
Two types of decompression are presented here:
Ipsilateral decompression for laminectomy. This procedure is performed while the patient has an epidural in place but stays awake. A stab wound is made at the site, and a dilator is inserted to enable the surgeon to move the skin wherever it is needed. It is equipped with lighting to locate the damaged lamina. Endoscopic tools are then placed, and the laminectomy is performed (9).
Contralateral decompression is like ipsilateral decompression; however, this surgery involves different locations to reach the damage. The surgeon can move higher or lower to get the areas that need repair (9). Both of these procedures are performed under endoscopy (9).
Another minimally invasive spine surgery is a microdiscectomy. This surgery removes a portion of a disc that has herniated and is causing pain. In Facetectomy, the facets of a vertebra, which can put pressure on the nerve, can be trimmed or removed. Foraminotomy is performed when the opening for the spinal nerve is enlarged due to bony overgrowth into the space.
When a spinal bone is fractured, the surgeon may also use cement to fuse the vertebrae, and this bond is delivered to the fractured part of the bone. This procedure is usually used for severe, disabling pain that is not repaired with pain medication or bracing.
The newest type of spinal surgery to discuss is minimally invasive surgery using robots. Surgeons guide the robots’ hands in performing this surgery using computer-generated equipment. The surgeon can better visualize the area of concern and control every aspect of surgery via these computer-directed robots than by using his gloved hands. The client may experience faster recovery, fewer complications, less time in the OR, and lower radiation exposure.

Self-Quiz
Ask Yourself...
- What more information can you find on the history of spinal fusion?
- Where can you locate more in-depth information regarding minimally invasive back surgery?
- How do you feel about surgeons using robots to perform this surgery?
- How did Hippocrates learn about the human body?
Nursing Roles in Spinal Injury
Like many surgeries, spinal fusions may have complications. Excessive bleeding, nerve damage, infection at the operative site, and blood clots are a few of them (13). Surgeons usually give prophylactic antibiotics before the operation and pain medicine immediately after surgery. Nurses are always responsible for the client, whether during pre-op or post-op and when the client goes home. Nurses have a role in every level of care perioperatively.
Wherever the nurse encounters the client, they immediately prioritize the client and their needs, including past medical history, medications, the site of the pain, how much pain they are having, and the duration of pain the client is experiencing. They also record the client’s support systems and psychosocial well-being (15).
If not an emergency or life-threatening injury, the surgical pre-op should be done several weeks before surgery. Of course, this includes the provider’s history and physical and any imaging that may need to be done (14). The nurse will take vital signs and educate the client regarding the surgery, complications, and any instructions needed before testing, which may include neurophysiological testing and MRI. The nurse is also involved with the interprofessional team to ensure the client receives optimal physical and psychological care (14).
In 2001, Professor Henrik Kehlet developed and implemented the Enhanced Recovery After Surgery (ERAS) program (17). This novel plan was devised to accelerate recovery from surgery. It requires members of the whole care team to be educated on the process and respond appropriately, which will speed up the client’s recovery (17). As part of this process, before surgery, the client should have “several regular preoperative exams,” health education, and nutrition preparation (17). This will enhance and reduce recovery as the client can know what to expect (17).
The critical components of ERAS are multimodal approaches that lead to a significant reduction in the undesirable sequelae from surgery and accelerate recovery” (18). The nurse is very involved in the ERAS program perioperatively and in rehabilitation. Nurses record data on a platform shared by the members of the individual client. This allows all members to be up to date on the client’s status and be able to step in when needed (18).
As part of the nursing process in the hospital post-operatively, the nurse will also continuously measure peak flow to determine the potential need for intubation when cervical vertebrae are involved (16). If intubated and ventilated, the nurse must monitor settings for optimal ventilation and oxygenation (16). Frequent and effective pulmonary hygiene is also indicated if no respiratory therapist is available (16).
Medications such as opioids, NSAIDs, muscle relaxers, and Tylenol may be ordered for the client. Clients who do not have relief from these medications may also receive Gabapentin or pregabalin (16). The nurse will continuously assess for pain and administer the appropriate medications. Another consideration is preventing venous thromboembolism and using compression boots to keep circulation intact. Heparin usually is administered at the same time. (16).
Managing bowel and bladder functions is essential if the injury is at or above the sacral level. When the client can, a bladder and bowel regime will be started in the hospital before discharge to rehab (18). The nurse monitors skincare and nutrition to prevent decubiti from forming. Frequent turning, using lotion on the skin, and lambswool padding will help keep the skin intact (18).
There are six steps in the ERAS program as follows: (17)
- Preadmission: Screening for surgery, including education, cessation of smoking and alcohol, nutritional education, and medical history
- Immediately prior to surgery, Start IVs and prophylaxis to prevent thromboembolisms and infection, shave the surgical site, monitor vital signs, use warm blankets and heated fluids, use vasopressors for blood pressure control, and take intake and output measurements.
- Perioperative: Compression stockings or pneumatic boots, carbohydrate drink given 2 hours before surgery, and vital sign monitoring.
- Intraoperative: Foley catheter placement prn, standardized anesthesia, oxygen, fluid balance, prophylaxis for nausea and vomiting, if necessary, a nasogastric tube and removal of it before reversing anesthesia, and lastly, wound healing.
- Postoperative:
- Postoperative day 1: 6 hours after surgery, begin nutrition. 8 hours after surgery, begin mobilizing g the client, restrict fluids as ordered, heparin, control of nausea and vomiting, and monitor vital signs.
- Postoperative day 2: Discontinue IV fluids and Foley catheter, diet as tolerated with high nutritional value, laxatives, and IV pain medication.
- Postoperative during the rest of the hospitalization: Normal diet, again with high nutrients, oral pain medications, active mobilization, bed to chair, and a beginning to walk. Continue with heparin.
- Day of discharge: Oral thromboembolism prophylaxis and a telephone call at home

Self-Quiz
Ask Yourself...
- How do you feel about using an algorithm such as ERAS?
- How is the ERAS protocol different from the procedure your facility uses?
- What do you think could be included in the ERAS protocol?
Research
Various techniques have been suggested to facilitate and improve spinal fusion surgery. The advancement of technology over many years has promoted new therapies for spinal surgery, although not all surgeons are well-versed in these recommendations (18). These new intraoperative techniques have helped stabilize better and avoid a second surgery; however, more studies need to be done to perfect this.
One of the newer techniques is adding Recombinant human Bone morphogenetic proteins (rhBMPs), growth factors, to the graft. This allows for quicker bone growth in minimally invasive spine surgery. This technique, however, only applies to clients with degenerative disc disease (20). There is concern, as well, that these proteins could cause some severe side effects if used in cervical fusions (20). Several rhBMPs are being studied that give even better results (18).
Other growth factors are being studied for this surgery, such as platelet-derived growth factors, which are still pre-clinical (18). Other ongoing studies aim to ” block the multiple mechanisms of progressive pathogenesis” to promote neurogenesis (19).
At Northwestern College, a new injectable therapy is being trialed by sending “bioactive signals to trigger cells,” which help regenerate new axons severed in spinal accidents (22). During a trial on paralyzed animals, the result was their ability to walk again within a month (22). They found five critical transformations with this trial. This one-time injection sends bioactive signals to cells, which harness “dancing molecules” to reverse paralysis.
- The researchers found that scar tissue significantly diminished by not allowing it to form.
- The myelin sheath that insulates the layer of axons around the cells was reformed.
- Blood vessels form around the damaged site to bring nutrients to the cells.
- Severed axons or extensions of the neurons, regenerated.
- Some damaged motor neurons endured.
These “dancing molecules” are tuned to the motion of molecules to find them and connect with receptors (22). Once connected to these receptors, the dancing molecules prompt the axons to regrow. The axons are connected between the body and the brain, and if severed, they cause loss of feeling or paralysis (22). In another study, methylprednisolone was applied topically to the injured area with some success (19).
“The current research is beginning to target the cascading mechanism leading to secondary injury” (19). These studies aim to alter inflammation of the nerves, reduce free radicals from further damaging the spine, and improve blood flow (19).


Self-Quiz
Ask Yourself...
- Where can you find newer research on spinal surgery?
- What information can you retrieve on the rhBMPs and how they repair the spine?
- What do you imagine spinal surgery will look like in the future?
Conclusion
Spinal surgery has come a long way from Hippocrates to today. We have discussed the different types of braces, from cement to implanted rods to even putting clients on a rack to straighten the spine. We know the number of clients with CLBP significantly burdens health care costs and companies paying for disability and work absences. While looking at the types of surgery presently used, we learned that there are potentially new biological agents to assist in bone healing. Learning about ERAS and how nurses are critical is an excellent step toward how teams should exist and work together to improve all surgeries.
References + Disclaimer
- Dutmer, A. L., Schiphorst Preuper, H. R., Soer, R., Brouwer, S., Bültmann, U., Dijkstra, P. U., Coppes, M. H., Stegeman, P., Buskens, E., van Asselt, A. D. I., Wolff, A. P., & Reneman, M. F. (2019). Personal and societal impact of low back pain: The groningen spine cohort. Spine, 44(24), E1443–E1451. https://doi.org/10.1097/BRS.0000000000003174
- Chester J. Connally III;
- Ding, W., Hu, S., Wang, P., Kang, H., Peng, R., Dong, Y., & Li, F. (2022). Spinal cord injury: The global incidence, prevalence, and disability from the global burden of disease study 2019. Spine 47(21), 1532-1540. https://journals.lww.com/spinejournal/Fulltext/2022/11010/Spinal_Cord_Injury__The_Global_Incidence,.8.aspx
- Zhang, Y., Jiang, Y., Zou, D., Yuan, B., Ke, H. Z., & Li, W. (2021). Therapeutics for enhancement of spinal fusion: A mini-review. Journal of Orthopaedic Translation, 31, 73-79. https://doi.org/10.1016/j.jot.2021.11.001
- Willems P. (2013). Decision making in surgical treatment of chronic low back pain: The performance of prognostic tests to select patients for lumbar spinal fusion. Acta orthopaedica. Supplementum, 84(349), 1–35. https://doi.org/10.3109/17453674.2012.753565
- Malekzadeh, H., Golpayegani, M., Ghodsi, Z., Sadeghi-Naini, M., Asgardoon, M., Baigi, V., Vaccaro, A. R., & Rahimi-Movaghar, V. (2022). Direct cost of illness for spinal cord injury: A systematic review. Global Spine Journal, 12(6), 1267–1281. https://doi.org/10.1177/21925682211031190
- Anjum, A., Yazid, M. D., Fauzi Daud, M., Idris, J., Ng, A. M. H., Selvi Naicker, A., Ismail, O. H. R., Athi Kumar, R. K., & Lokanathan, Y. (2020). Spinal cord injury: Pathophysiology, multimolecular interactions, and underlying recovery mechanisms. International Journal of Molecular Sciences, 21(20), 7533. https://doi.org/10.3390/ijms21207533
- Zhang, Y., Jiang, Y., Zou, D., Yuan, B., Ke, H. Z., & Li, W. (2021). Therapeutics for enhancement of spinal fusion: A mini review. Journal of Orthopaedic Translation, 31, 73–79. https://doi.org/10.1016/j.jot.2021.11.001
- Reisener, M. J., Pumberger, M., Shue, J., Girardi, F. P., & Hughes, A. P. (2020). Trends in lumbar spinal fusion-a literature review. Journal of spine surgery (Hong Kong), 6(4), 752–761. https://doi.org/10.21037/jss-20-492
- Lim, K. & Sardhara, J. (2022). Endoscopic decompression for lumbar spinal canal stenosis: A technical note. Journal of Spinal Surgery, 9(1), 40. doi: 10.4103/joss.joss_37_21
- Tarpada, S. P., Morris, M. T., & Burton, D. A. (2016). Spinal fusion surgery: A historical perspective. Journal of Orthopaedics, 14(1), 134–136. https://doi.org/10.1016/j.jor.2016.10.029
- Försth, P., Ólafsson, G., Carlsson, T., Frost, A., Borgström, F., Fritzell, P., Öhagen, P., Michaëlsson, K., & Sandén, B. (2016). A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. The New England Journal of Medicine, 374(15), 1413–1423. https://doi.org/10.1056/NEJMoa1513721
- Kim, S. J., & Mobbs, R. J. (2021). Systematic review of the top 10 ranked spine articles in the last 10 years [2011-2021]. Annals of Translational Medicine, 9(13), 1090. https://doi.org/10.21037/atm-21-2393
- American Academy of Orthopedic Surgeons. (n.d.). Spinal fusion. https://orthoinfo.aaos.org/en/treatment/spinal-fusion
- Bertrand D., et al. (2022). The Spine Journal 24(8), 1485-1494. https://www.thespinejournalonline.com/article/S1529-9430(24)00155-4/abstract
- Lall, M.P. (2018). Nursing care of the patient undergoing lumbar spinal fusion. Journal of Nursing Education and Practice, 8(5). doi: https://doi.org/10.5430/jnep.v8n5p44
- Hills T. E. (2020). Caring for patients with a traumatic spinal cord injury. Nursing, 50(12), 30–40. https://doi.org/10.1097/01.NURSE.0000721724.96678.5a
- Hou, Q., Luo, X., Li, H., Hou, Y. & Zhang, Z. (2022). The role of nursing in enhanced recovery after surgery programs in accordance with spine surgery. Journal of Integrative Nursing. doi:10.4103/jin.jin_08_20
- Zhang, Y., Jiang, Y., Zou, D., Yuan, B., Ke, H. Z., & Li, W. (2021). Therapeutics for enhancement of spinal fusion: A mini review. Journal of Orthopaedic Translation, 31, 73–79. https://doi.org/10.1016/j.jot.2021.11.001
- Varma, A. K., Das, A., Wallace, G., 4th, Barry, J., Vertegel, A. A., Ray, S. K., & Banik, N. L. (2013). Spinal cord injury: a review of current therapy, future treatments, and basic science frontiers. Neurochemical Research, 38(5), 895–905. https://doi.org/10.1007/s11064-013-0991-6
- Northwestern Now. (2021). ‘Dancing molecules’ successfully repair severe spinal cord injuries. https://news.northwestern.edu/stories/2021/11/dancing-molecules-successfully-repair-severe-spinal-cord-injuries/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
