Supporting a Patient after Fetal Demise
Contact Hours: 1
Author(s):
Claudia Keck Ph.D., RN, CRRN
Course Highlights
- In this Supporting a Patient after Fetal Demise course, we will learn about clinical considerations and the management of fetal demise.
- You’ll also learn the impact of fetal demise on the emotional, physical, and psychosocial dimensions of the client.
- You’ll leave this course with a broader understanding of social and cultural factors that affect a client’s coping with fetal demise.
Introduction
Fetal demise or fetal death is defined as the delivery of a fetus showing no signs of life as indicated by the absence of breathing, heartbeats, pulsation of the umbilical cord, or definite movements of voluntary muscles. Fetal demise can happen at any time during pregnancy and is classified according to gestational age. A death that occurs before 20 weeks gestation is usually classified as a spontaneous abortion; those occurring after 20 weeks or a birth weight equal to or greater than 350 grams constitute a fetal demise or stillbirth.
In the United States, termination of pregnancy for fetal anomalies and labor induction for pre-viable premature rupture of membranes are reported as terminations of pregnancy and not as stillbirths. Fetal demise accounts for the 5th leading cause of death worldwide [11][12]. Fetal demise has profound traumatic effects on parents/guardians and families. Healthcare providers play a pivotal role in the care of clients and families who suffer a pregnancy loss. This course will focus on supporting a client after fetal demise/stillbirth.
Trends in the United States
In 2021, a total of 21,105 fetal deaths at 20 weeks of gestation or more were reported in the United States, accounting for a 5.73 fetal mortality rate per 1,000 live births and fetal deaths. The fetal mortality rate increased by 1% from 2020 to 2021. Fetal mortality rates in the United States vary by race and ethnicity. Infants of Black women had the highest mortality rate (9.89), followed by infants of Native Hawaiian or Other Pacific Islander and American Indian or Alaska Native (9.87 and 7.48, respectively), Hispanic (4.82), White (4.85), and Asian (3.94) women. Fetal mortality rates also differ by maternal age. In 2021, fetal mortality rates were highest for females under age 15 (13.14) and aged 45 and over (11.36) [7].
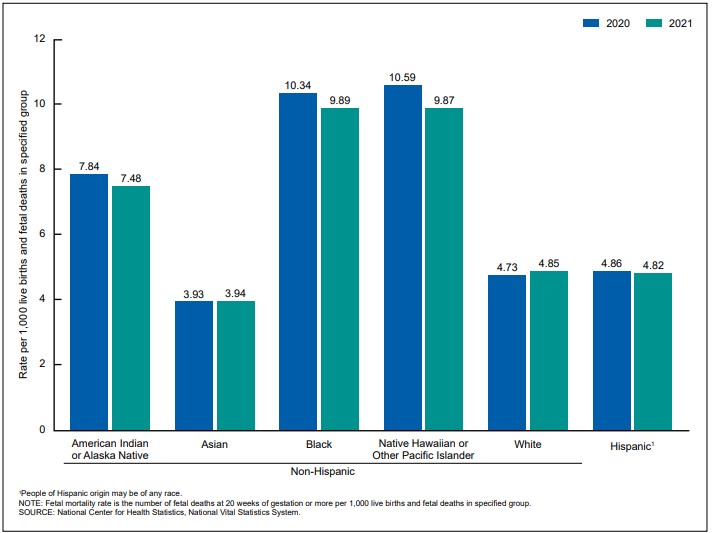
Figure 1. 2020 – 2021 U.S. Fetal Deaths Among Non-Hispanic Cultural Groups (Resource: National Center for Health Statistics, National Vital Statistics System)
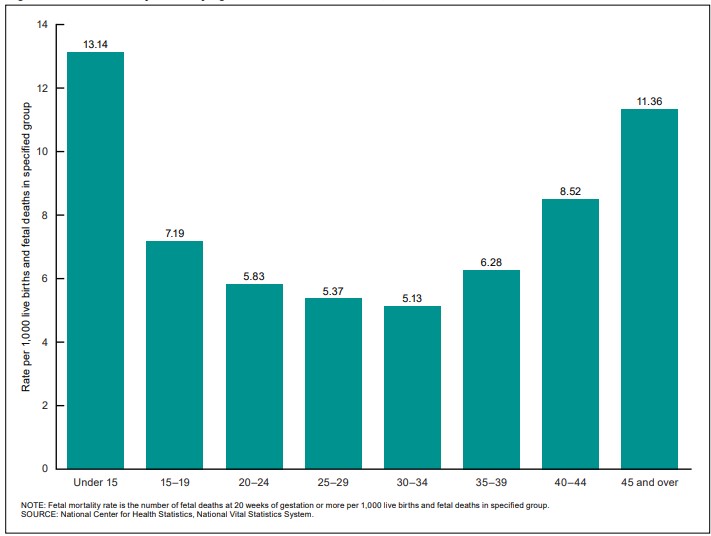
Figure 2. U.S. Fetal Deaths Among Age Groups (Resource: National Center for Health Statistics, National Vital Statistics System)
Ask yourself...
- What is the definition of fetal demise?
- What is the fetal mortality rate in the United States?
- What racial group is most affected by fetal death in the U.S.?
- What age group is most affected by fetal death in the U.S.?
Causes and Risk Factors for Fetal Demise
In many cases, the exact cause of fetal demise remains unknown. Prevalent risk factors associated with fetal demise include [8][10][12].
- Non-Hispanic black race,
- Maternal age less than 15 years and greater than 35
- Multiple gestations
- Placental insufficiency
- Placental insufficiency
- History of a previous stillbirth
- Previous adverse outcomes such as preterm delivery, growth restrictions, or preeclampsia
- Male sex of the fetus
The most common comorbid pregnancy conditions are [10][12]:
- Hypertension
- Diabetes
Pregestational and gestational diabetes increases the risk of stillbirth twofold to fivefold. Chronic maternal hypertension increases the risk of stillbirth 2-4 times.
Further conditions that are linked to stillbirth [10][12]:
- Acquired and inherited Thrombophilia
- Thyroid disorders
- Systemic lupus erythematosus
- Renal disease
- Cholestasis of pregnancy
- Assisted reproductive technology
- Obesity (body mass index above 30)
- Infections
- Maternal cocaine, methamphetamine, and other illicit drug use
- Smoking tobacco (greater than 10 cigarettes per day)
Studies have shown that chromosomal and genetic abnormalities were found in 6-13% of stillbirths [10][14].
Ask yourself...
- What are some of the risk factors associated with fetal demise?
- What are the most common comorbid pregnancy conditions linked to fetal demise?
- How does pregestational and gestational diabetes affect the risk of stillbirth?
Clinical Considerations and Management
Diagnosis of Fetal Death
Fetal demise (fetal death) refers to situations in which the fetus is no longer alive, but the uterus has not yet started to expel its contents. Clinical findings might include [12]:
- Vaginal bleeding
- Absent fetal heart sounds on auscultation
- Failure to feel fetal movements
- A uterus that is significantly smaller than the expected size
Fetal demise is confirmed by ultrasonic examination and diagnosed by [12]:
- Visualization of the fetal heart and the absence of cardiac activity

Delivery Options
State laws and policies related to stillbirth impact the management of fetal demise. Methods and timing of delivery after stillbirth depends on gestational age at the time of fetal demise, maternal obstetric history, and maternal preference. After a fetus dies, labor will usually begin naturally within 2 weeks. Labor can also be induced; methods for labor induction vary based on gestational age. Before 28 weeks of gestation, vaginal and oral misoprostol or high-dose oxytocin infusion are commonly used. Cervical ripening with a transcervical Foley catheter might be utilized. A procedure called dilation and evacuation (D&E) is commonly used in the second trimester. Delivery by cesarean section is rare, with fetal demise, and is associated with potential maternal morbidity [10][12].
Care After a Fetal Demise
After fetal demise, clients will experience physical effects that occur after giving birth. Clients will experience vaginal bleeding. In the first few days after birth, the blood is usually bright red and heavy; it will seem like a heavy menstrual period. Over time, bleeding will become lighter. Inform your client that light spotting or bleeding can last up to 6 weeks.
Instruct your client to [4][10]:
- Use pads instead of tampons.
- Call the healthcare provider promptly if bleeding soaks through more than two large pads in an hour for two hours or more or if they are passing large clots
An antibiotic is usually prescribed to prevent infection. Instruct your client to:
- Call the healthcare provider immediately if they have a temperature higher than 100 F
- Report chills, severe pain, or any other concerning symptoms
To avoid infections, instruct your client to:
- Avoid putting anything into their vagina, such as tampons, menstrual cups, or douching
- Abstain from vaginal sex for a week
Pain is common after giving birth, especially after pains that feel like menstrual cramps or labor contractions. Afterpains help the uterus shrink back to its pre-pregnancy size. Teach your client to:
- Use pain relief medications such as ibuprofen or non-steroidal anti-inflammatory drugs as needed
Breastmilk usually starts coming in within a few days after delivery, and the client may experience breast soreness, lactation, or engorgement. To relieve breast soreness and lactation, instruct your client to:
- Place cold or gel packs on their breasts
- Use pain relievers as needed, such as ibuprofen or acetaminophen
- Use breast pads to collect leaking breast milk
- Wear a firm supportive bra
Ask yourself...
- How is fetal demise diagnosed?
- What would you teach your client about vaginal bleeding after fetal demise?
- When should the client call the healthcare provider immediately?
- How can a client avoid infections after fetal demise?
- How can pain be managed after fetal demise?
- What would you advise a client to do in case of breast pain after fetal demise?
Decision-Making Support
Parents/guardians should be provided with full information about any important decisions to be made regarding themselves or their baby. Adequate time, empathy, and support need to be given to allow the client to consider and organize all options available. If possible, discuss options before the baby is born [6][11].
Discussions aimed to support client choice [6][11]:
- Diagnosis and subsequent care before, during, and after birth
- Recommendations about labor and birth
- Laboratory tests are recommended to assess maternal well-being
- Postmortem examinations such as external examination and birth weight
- Fetal autopsy: it’s one of the most useful diagnostic tests to determine the cause of death.
- Fetal laboratory studies such as genetic analysis
- Pathological examination of the cord, membranes, and placenta
- Options for burial, cremation, and funerals
Presentation of information:
- Options/information must be presented in a sensitive, clear, and non-biased fashion
- Parents/guardians should be offered written information to supplement discussions
- Confirmation of understanding should be obtained
- Written consent must be obtained for any invasive procedures on the baby, including tissues taken for genetic analysis
Ask yourself...
- What discussions will you have with a client who experiences fetal demise to support them in making decisions regarding themselves or their baby?
- How should information be presented to the client after fetal demise?
Psychosocial Considerations and Management
Psychological Health Effects of Fetal Demise
Fetal demise can have significant short and long-term psychological effects on a client, which health professionals often underestimate. Fetal demise is associated with particularly severe grief and a complex mourning process. The individual response to fetal loss may vary and can be affected by religion, culture, age, and stage of pregnancy [5]. Common psychological effects include [5][9][13]:
- Anxiety
- Stress
- Depression
- Grief
- Misplaced guilt
- Sleep difficulties
- Fatigue
- Emotional shock
- Panic and Phobia
- Post-traumatic stress disorder (PTSD)
- Suicidal ideation
Support Interventions
For most clients, the death of a baby is a tormenting and painful source of grief. Given the impact that fetal demise has on the mental health of clients, healthcare interventions must consider clients’ feelings, negative emotions, mental states, and coping mechanisms. Interventions designed to assist grieving clients and their families while undergoing fetal loss include [13]:
- Educating clients and their families about the grieving process: Explain to parents/guardians that there is no set time frame for resolution or incorporation of grief and that the grief experience is unique to each person experiencing it
- Acknowledging and normalizing varied grief responses.
- Allowing the client and family to see and hold the baby as long as desired.
- Allowing participation in rituals such as cutting the umbilical cord, naming the baby, bathing, and dressing the baby.
- Create memories to support parents/guardians in developing a bond with their baby, and create a sense of identity for the child: photographs, palms and footprints, locks of hair, and the blanket baby was wrapped in. A box that holds the items of memories should be offered to the family before hospital discharge.
- Call the baby by their name
- Have arrangements with representatives of all common faiths and nonreligious spiritual organizations as a source of guidance and support.
- Prepare a private room outside the ward for the client and family, away from the sounds of other birthing clients and babies, and have a bed for the partner available.
- Place a special sticker on the notice board and room’s door wherein a bereaved client is located so that all staff know their condition.
- Offering bereavement counseling services, mental health services, and contacts for peer support groups
Therapeutic communication is key when caring for a client after a fetal demise, yet it can be hard to know what to say [5].
Some things you might say:
- “I’m very sorry that you have lost your baby.”
- “This must be difficult for you.”
- “I care about you and your family. Please tell me what I can do to help.”
Things not to say:
- “Don’t worry, you’re young. You can always have another baby.”
- “It wasn’t meant to be.”
- “It was probably for the best.”
- “At least you have other children.”
Active listening is also an important skill for healthcare professionals caring for clients after fetal demise. It can help build trust and rapport with a client and improve communication. Healthcare providers should aim to be fully present, client-focused, and attentive during conversations and reflect on what has been said.
Mental Health Screenings
Grief, depression, anxiety, and stress measurement can help healthcare providers understand how clients cope with loss and identify areas where additional support may be needed [13]. Commonly used mental health screening tools used after fetal demise include:
- The Perinatal Grief Scale (PGS) measures grief following a reproductive loss.
- The Edinburgh Postpartum Depression Scale (EPDS) indicates the intensity of depression.
- The DASS-21 scale assesses depression, stress, and anxiety.
Bereavement care needs to be individualized to recognize bereaved parents/guardians’ personal, cultural, or religious needs. Time needs to be spent with the grieving parent to understand their wishes and needs. When caring for a client/couple/family experiencing fetal demise, it is important to convey compassion, empathy, and sensitivity.
To support a client’s emotional health advise them to do the following [13]:
- Rest whenever you can. Being tired can make it harder to cope with emotions.
- Try to eat healthy foods and get some exercise.
- Tell your family and friends what they can do.
- Talk to your doctor or midwife about how you are coping.
- Think about making a memory book of your pregnancy and baby.
- You might consider a ceremony, such as a blessing or a memorial service.
- Try to talk to others who have gone through this loss.
Societal Considerations
Worldwide, fetal loss is associated with stigma, shame, and guilt. Women report after losing a baby, they are made to feel silent about their grief, either because stillbirth is still so common or because they are perceived as unavoidable. This can lead to disenfranchised grief; “grief that persons experience when they incur a loss that is not or cannot be openly acknowledged, publicly mourned, or socially supported”. Healthcare providers need to show sensitivity and empathy, recognize the baby and his death, and allow space for clients to talk about how they feel [3][15].
Cultural Considerations
Cultural beliefs and practices surrounding death vary greatly amongst different situations and groups and highly influence an individual’s experience, grief, adjustment, and support needs. In some cultures, fetal demise is believed to emerge from bad omens, witchcraft, or immorality, and individuals who experience losses are frequently shunned and even abandoned by their partners and families. Further, some groups consider grieving for a stillbirth unacceptable, potentially prolonging and complicating the grief reaction. Cultural norms also influence the behavior and actions of healthcare workers. Healthcare providers’ knowledge and understanding of key religious and cultural beliefs and rituals can greatly facilitate difficult discussions and decision‐making around the time of the death of a baby [13].
Cultural considerations in client care after a stillbirth should include:
- Avoiding assumptions and stereotyping
- Understanding and supporting cultural expressions of grief
- Sensitive communication
- Linguistic services
- Acknowledge cultural groups’ support systems
- Supporting cultural rituals

Considerations for Healthcare Providers
Healthcare professionals often lack confidence in their ability to provide good quality care for parents/guardians who experienced fetal demise. Targeted education and training can help to prepare healthcare providers and increase confidence in providing stillbirth care. All healthcare providers who interact with clients after a fetal loss should aim to attend professional development opportunities and become familiar with the principles of bereavement care [2][10].
Further, healthcare professionals who care for bereaved clients before, during, or after the death of a baby will be emotionally affected. They might experience sadness, anger, guilt, grief, or helplessness and experience psychological trauma. Training, organizational support, and self-care interventions can help reduce negative psychological outcomes among those providing support to clients after a fetal demise [2][10].
Ask yourself...
- What are some psychological health effects of fetal demise on a client?
- What support interventions should be offered to a client after fetal demise?
- What are some commonly used scales that allow measuring of grief, depression, anxiety, or stress of a client that experienced fetal demise?
- What advice would you give a client after fetal demise to support their emotional health?
- What are some cultural considerations in client care after a stillbirth?
- What emotional effects might healthcare providers experience while caring for a client who experienced fetal demise?
Conclusion
In the U.S., 21,105 babies were stillborn in 2021. It is devastating for parents/guardians when a baby dies, and the experience can cause a range of mental and physical distress for a client. Sensitive, personalized support interventions that address the client’s needs are vital to prevent short and long-term negative outcomes.
Providing a client with understandable information, discussing options with them, empathy, caring, and tailoring care to their individual needs from the time of diagnosis to hospital discharge and follow-up are key.
References + Disclaimer
- Ayebare, E., Lavender, T., Mweteise, J. et al. (2021, June 25). The impact of cultural beliefs and p practices on parents’ experiences of bereavement following stillbirth: a qualitative study in Uganda and Kenya. BMC Pregnancy Childbirth 21, 443. https://doi.org/10.1186/s12884-021-03912-4
- Bezerra, N. A., Santos, C. N. S. D., Silva, A. T. C. S. G. D., Linhares, F. M. P., & Morais, S. C. R. V. (2024, Mar 15). Nursing care for parents who have experienced fetal demise: integrative review. Revista brasileira de enfermagem, 77(1), e20220811. https://doi.org/10.1590/0034-7167-2022-0811
- Bohn J. A. (2023, April 15). When Words Fail: “Miscarriage,” Referential Ambiguity, and Psychological Harm. The Journal of Medicine and Philosophy, 48(3), 265–282. https://doi.org/10.1093/jmp/jhad013
- Cohen, R., What Happens After a Miscarriage? An Ob-Gyn Discusses the Options. (2022, June). The American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/experts-and-stories/the-latest/what-happens-after-a miscarriage-an-ob-gyn-discusses-the-options.
- Cuenca D. (2023, January 22). Pregnancy loss: Consequences for mental health. Frontiers in global women’s health, 3, 1032212. https://doi.org/10.3389/fgwh.2022.1032212
- Fernández-Férez, A., Ventura-Miranda, M. I., Camacho-Ávila, M., Fernández-Caballero, A., G Granero-Molina, J., Fernández-Medina, I. M., & Requena-Mullor, M. D. M. (2021, May 24). Nursing Interventions to Facilitate the Grieving Process after Perinatal Death: A Systematic Review. International journal of environmental research and public health, 18(11), 5587. https://doi.org/10.3390/ijerph18115587
- Gregory, E. C.W., Valenzuela C. P., & Hoyert, D. L. (2023, July 26). Fetal Mortality: United States, 2021. National Vital Statistics report. U.S. Department of Health and Human Services. https://www.cdc.gov/nchs/products/nvsr.htm
- Khan, Erum & Jamil, Mahwash & Chanderparkash, Reeta & Irfan, Sheikh & Yousf, Sana & B Basharat, Ayesha. (2021, August 10). Intrauterine fetal death: Five years’ experience in a secondary care hospital. The Professional Medical Journal. 28. 1076-1082. https://doi.org/10.29309/TPMJ/2021.28.08.4721
- Liu, S., & Shefaly, S., (2021, May). Psychosocial interventions on psychological outcomes of p parents with perinatal loss: A systematic review and meta-analysis. International Journal of Nursing Studies. https://doi.org/10.1016/j.ijnurstu.2021.103871
- Management of Stillbirth: Obstetric Care Consensus No, 10. (2020). Obstetrics and gynecology, 135(3), e110–e132. https://doi.org/10.1097/AOG.0000000000003719
- Maslovich MM, Burke LM. Intrauterine Fetal Demise. (2022 Oct 31). StatPearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557533/
- Ross, M. G., Burwick, R. M., Smith, C. V., Joy, S., & Mattingly, P. J., (2023, June 05). Evaluation of Fetal Death. Medscape. https://emedicine.medscape.com/article/259165-ooverview?&icd=login_success_email_match_fpf
- Salgado, H. O., Andreucci, C. B., Gomes, A. C. R., & Souza, J. P. (2021, January 06). The perinatal bereavement project: development and evaluation of supportive guidelines for families experiencing stillbirth and neonatal death in Southeast Brazil-a quasi-experimental before-and-after study. Reproductive health, 18(1), 5. https://doi.org/10.1186/s12978-020-01040-4
- Stanley, KE, et al. (2020). Causal genetic variants in stillbirth. The New England Journal of Medicine. https://www.nichd.nih.gov/newsroom/news/090320-stillbirth-genes
- World Health Organization (2024). Why we need to talk about losing a baby. https://www.who.int/news-room/spotlight/why-we-need-to-talk-about-losing-a-baby
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
