Course
Texas APRN Bundle
Course Highlights
- In this course, we will learn about Texas nursing jurisprudence and ethics.
- You’ll also learn the basics of sexual assault as a public health problem and its impact on the state of Texas.
- You’ll leave this course with a broader understanding of commonly prescribed opioids for pain management and understand their side effects and indications of use.
About
Contact Hours Awarded: 20
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
Texas Nursing Jurisprudence and Ethics
Texas Nursing Jurisprudence and Ethics
Introduction - Texas Nursing Jurisprudence and Ethics
The purpose of this course is to review nursing ethics and jurisprudence specifically as these relate to Texas state nursing practice and law (1). Each state nursing board works to promote the safety and welfare of clients in their state by ensuring nurses are competent to practice nursing safely.
As outlined by the Texas Board of Nursing continuing education requirements, Nursing Jurisprudence and Nursing Ethics Board Rule 216.3, all nurses, including APRNs, must complete the required two contact hours of CNE relating to nursing jurisprudence and ethics before the end of every third two-year licensing period. This requirement applies to licensing periods that began on or after January 1, 2014. All new nurses must also pass the Nursing Jurisprudence Exam (NJE) (2,3).
Requirements also outline that education includes information related to the Texas Nursing Practice Act, the Board's rules, including Standards of Nursing Practice, the Board's position statements, principles of nursing ethics, and professional boundaries. Nurses are named in negligence and malpractice lawsuits that may claim unethical behavior/conduct, practice outside the scope of licensure, or lack of nursing supervision. Nurses must understand their state nurse practice act, scope of practice of nurse licensure, standards of practice, ethics, and professional boundaries to avoid litigation (2).

Self Quiz
Ask yourself...
- What is the number of contact hours required by the Board of Nursing in Texas Nursing Jurisprudence and Ethics before the end of every third two-year licensing period?
- What are the categories of required course information that must be contained?
- What training have you had regarding Texas jurisprudence and ethics?
- How do you feel that ethics have changed throughout your years of practice?
- Where can you find Texas' nurse practice act?
The Texas Nursing Practice Act – Overview
Registered Nurse Scope of Practice
The Texas Nursing Practice Act (NPA) defines the legal scope of practice for professional registered nurses (RNs) (4). "Professional nursing" means performing an act that requires substantial specialized judgment and skill, the proper performance of which is based on knowledge and application of the principles of biological, physical, and social science as acquired by a completed course in an approved school of professional nursing. The term does not include acts of medical diagnosis or the prescription of therapeutic or corrective measures. Professional nursing involves: (4)
- the observation, assessment, intervention, evaluation, rehabilitation, care, and Counsel, or health teachings of a person who is ill, injured, infirm, or experiencing a change in normal health processes.
- The maintenance of health or prevention of illness.
- A physician, podiatrist, or dentist orders medication administration or treatment.
- The supervision or teaching of nursing.
- The administration, supervision, and evaluation of nursing practices, policies, and procedures.
- The requesting, receiving, signing for, and distributing prescription drug samples to patients at practices where an advanced practice registered nurse is authorized to sign prescription drug orders as provided by Subchapter B, Chapter 157.
- The performance of an act delegated by a physician under Section 157.0512, 157.054, 157.058, or 157.059.
- The development of the nursing care plan.
The RN accepts responsibility for practicing within the legal scope of practice, is prepared to work in all healthcare settings, and may engage in independent nursing practice without supervision by another healthcare provider. The RN, focusing on patient safety, must function within the legal scope of practice and by the federal, state, and local laws, rules and regulations, and policies, procedures, and guidelines of the employing health care institution or practice setting. The RN provides safe, compassionate, and comprehensive nursing care to patients and their families with complex healthcare needs (5).
Self Quiz
Ask yourself...
- What does the term "Professional nursing" mean?
- What is professional nursing performance based on in Texas nursing jurisprudence and ethics?
- Does professional nursing include medical diagnosis or the prescription of therapeutic or corrective measures?
- Does professional nursing involve the supervision or teaching of nursing or the development of the nursing care plan?
- Can an RN engage in independent nursing practice without the supervision by another health care provider?
Texas Nursing Jurisprudence and Ethics - Board Rules
Texas Board of Nursing, Chapter 217, Rule §217.11, Standards of Nursing Practice (6)
The Texas Board of Nursing regulates nursing practice within the State of Texas for Vocational Nurses, Registered Nurses, and Registered Nurses with advanced practice authorization. The standards of practice establish a minimum acceptable level of nursing practice in any setting for each level of nursing licensure or advanced practice authorization. Failure to meet these standards may result in action against the nurse's license even if no actual patient injury resulted (6).
- Standards Applicable to All Nurses. All vocational nurses, registered nurses, and registered nurses with advanced practice authorization shall:
- Know and conform to the Texas Nursing Practice Act, the Board's rules and regulations, and all federal, state, or local laws, rules, or regulations affecting the nurse's current area of nursing practice.
- Implement measures to promote a safe environment for clients and others.
- Know the rationale for and the effects of medications and treatments and shall correctly administer the same.
- Accurately and completely report and document:
- The client's status, including signs and symptoms, is as follows:
- Nursing care rendered.
- Physician, dentist, or podiatrist orders.
- Administration of medications and treatments.
- client response(s).
- contacts with other healthcare team members concerning significant events regarding the client's status.
- Respect the client's right to privacy by protecting confidential information unless required or allowed by law to disclose the information.
- Promote and participate in education and counseling to a client(s) and, where applicable, the family/significant other(s) based on health needs.
- Obtain instruction and supervision as necessary when implementing nursing procedures or practices.
- Make a reasonable effort to obtain orientation/training for competency when encountering new equipment and technology or unfamiliar care situations.
- Notify the appropriate supervisor when leaving a nursing assignment.
- Know, recognize, and maintain professional boundaries of the nurse-client relationship.
- Comply with mandatory reporting requirements of Texas Occupations Code Chapter 301 (Nursing Practice Act), Subchapter I, which includes reporting a nurse:
- Who violates the Nursing Practice Act or a board rule and contributed to the death or severe injury of a patient.
- Whose conduct causes a person to suspect that the nurse's practice is impaired by chemical dependency or drug or alcohol abuse?
- Whose actions constitute abuse, exploitation, fraud, or a violation of professional boundaries.
- Whose actions indicate that the nurse lacks knowledge, skill, judgment, or conscientiousness to such an extent that the nurse's continued practice of nursing could reasonably be expected to pose a risk of harm to a patient or another person, regardless of whether the conduct consists of a single incident or a pattern of behavior.
- Except for minor incidents (Texas Occupations Code §§301.401(2), 301.419, 22 TAC §217.16), peer review (Texas Occupations Code §§301.403, 303.007, 22 TAC §217.19), or peer assistance if no practice violation (Texas Occupations Code §301.410) as stated in the Nursing Practice Act and Board rules (22 TAC Chapter 217).
- Provide, without discrimination, nursing services regardless of the age, disability, economic status, gender, national origin, race, religion, health problems, or sexual orientation of the client served.
- Institute appropriate nursing interventions that might be required to stabilize a client's condition and prevent complications.
- Clarify any order or treatment regimen the nurse has reason to believe is inaccurate, non-efficacious, or contraindicated by consulting with the appropriate licensed practitioner and notifying the ordering practitioner when the nurse decides not to administer the medication or treatment.
- Implement measures to prevent exposure to infectious pathogens and communicable conditions.
- Collaborate with the client, members of the health care team, and, when appropriate, the client's significant other(s) in the interest of the client's health care.
- Consult with, utilize, and make referrals to appropriate community agencies and health care resources to provide continuity of care.
- Be responsible for one's continuing competence in nursing practice and individual professional growth.
- Make assignments to others that consider client safety and are commensurate with the educational preparation, experience, knowledge, and physical and emotional ability of the person to whom the assignments are made.
- Accept only those nursing assignments that consider client safety and are commensurate with the nurse's educational preparation, experience, knowledge, and physical and emotional ability.
- Supervise nursing care provided by others for whom the nurse is professionally responsible.
- Ensure the verification of current Texas licensure or other Compact State licensure privileges and credentials of personnel for whom the nurse is administratively responsible when acting in the role of nurse administrator.
- Standards Specific to Vocational Nurses. The licensed vocational nurse practice is a directed scope of nursing practice under the supervision of a registered nurse, advanced practice registered nurse, physician's assistant, physician, podiatrist, or dentist. Supervision is the process of directing, guiding, and influencing the outcome of an individual's performance of an activity. The licensed vocational nurse shall assist in the determination of predictable healthcare needs of clients within healthcare settings and:
- Shall utilize a systematic approach to provide individualized, goal-directed nursing care by:
- Collecting data and performing focused nursing assessments.
- Participating in the planning of nursing care needs for clients.
- Participating in developing and modifying the comprehensive nursing care plan for assigned clients.
- Implementing appropriate aspects of care within the LVN's scope of practice.
- Assisting in the evaluation of the client's responses to nursing interventions and the identification of client needs.
- Shall utilize a systematic approach to provide individualized, goal-directed nursing care by:
-
- Shall assign specific tasks, activities, and functions to unlicensed personnel commensurate with the educational preparation, experience, knowledge, and physical and emotional ability of the person to whom the assignments are made and shall maintain appropriate supervision of unlicensed personnel.
- May perform other acts that require education and training as prescribed by board rules and policies, commensurate with the licensed vocational nurse's experience, continuing education, and demonstrated licensed vocational nurse competencies.
- Standards Specific to Registered Nurses. The registered nurse shall assist in the determination of healthcare needs of clients and shall:
- Utilize a systematic approach to provide individualized, goal-directed nursing care by:
- Performing comprehensive nursing assessments regarding the health status of the client.
- Making nursing diagnoses serves as the basis for the care strategy.
- Developing a plan of care based on the assessment and nursing diagnosis.
- Implementing nursing care.
- Evaluating the client's responses to nursing interventions.
-
- Delegate tasks to unlicensed personnel in compliance with Chapter 224 of this title, relating to clients with acute conditions or in acute environments, and Chapter 225, relating to independent living environments for clients with stable and predictable situations.
- Standards Specific to Registered Nurses with Advanced Practice Authorization. Standards for a specific role and specialty of advanced practice nurses supersede standards for registered nurses where conflict between the standards, if any, exists. In addition to paragraphs (1) and (3) of this subsection, a registered nurse who holds authorization to practice as an advanced practice nurse (APN) shall:
- Practice in an advanced nursing practice role and specialty by the authorization granted under Board Rule Chapter 221 of this title (relating to practicing in an APN role; 22 TAC Chapter 221) and standards set out in that chapter.
- Prescribe medications in accordance with the prescriptive authority granted under Board Rule Chapter 222 of this title (relating to APNs prescribing; 22 TAC Chapter 222) and standards set out in that chapter and compliance with state and federal laws and regulations relating to the prescription of dangerous drugs and controlled substances. (4)

Self Quiz
Ask yourself...
- Why is it important for Texas Nursing Jurisprudence and Ethics that a nurse know the rationale for and the effects of medications and treatments before administering these to a client?
- Are there negative consequences if a nurse is not trained to perform a task or procedure? If so, what are 1-2 consequences of lack or training or errors?
- How do nurses utilize a systematic approach to providing individualized, goal-directed, nursing care?
- What challenges of appropriate delegation have you encountered and how have you over come them?
- What techniques have helped you to be successful in delegation?
The Board's Position Statements
15.28 The Registered Nurse Scope of Practice (See also the LVN Scope of Practice) (7)
The Board of Nursing recommends that all nurses utilize the Scope of Practice Decision-Making Model (DMM) when deciding if an employer's assignment is safe and legally within the nurse's scope of practice (8).
The Texas Board of Nursing (BON or Board) is authorized by the Texas Legislature to regulate the nursing profession to ensure that every licensee is competent to practice safely. The Texas Nursing Practice Act (NPA) defines the legal scope of practice for professional registered nurses (RN) (4, 9).
The RN takes responsibility and accepts accountability for practicing within the legal scope of practice, is prepared to work in all healthcare settings, and may engage in independent nursing practice without supervision by another healthcare provider. With a focus on patient safety, the RN must function within the legal scope of practice and in accordance with federal, state, and local laws, rules, and regulations. In addition, the RN must comply with policies, procedures, and guidelines of the employing health care institution or practice setting. The RN provides safe, compassionate, and comprehensive nursing care to patients and their families with complex healthcare needs (9).
This position statement aims to provide direction and recommendations for nurses and their employers regarding the safe and legal scope of practice for RNs and to promote an understanding of the differences in the RN programs of study and between the RN and LVN levels of licensure. The LVN scope of practice is interpreted in Position Statement (9).
Every nursing education program in Texas must ensure that their graduates exhibit competencies outlined in the Board's Differentiated Essential Competencies of Graduates of Texas Nursing Programs Evidenced by Knowledge, Clinical Judgements, and Behaviors. These competencies are included in the program of study so that every graduate has the knowledge, clinical judgment, and behaviors necessary for RN entry into safe, competent, and compassionate nursing care. The DECs serve as a guideline for employers to assist RNs in transitioning from the educational environment into nursing practice. As RNs enter the workplace, the DECs are the foundation for developing the RN scope of practice (9).
Completion of ongoing, informal continuing nursing education offerings and on-the-job training in an RN's area of practice serves to develop, maintain, and expand competency. Because the RN scope of practice is based upon the educational preparation in the RN program of study, there are limits to expanding the scope. The Board believes that successfully transitioning from one level of nursing practice to another requires the nurse to complete a formal education program. (10)
The RN Scope of Practice
The professional RN advocates for the patient and the patient's family and promotes safety by practicing within the NPA and the BON Rules and Regulations. The RN provides nursing services that require substantial specialized judgment and skill. The planning and delivery of professional nursing care are based on knowledge and application of biological, physical, and social science principles as acquired by a completed course of study in an approved school of professional nursing. Unless licensed as an advanced practice registered nurse, the RN's scope of practice does not include acts of medical diagnosis or the prescription of therapeutic or corrective measures. RNs utilize the nursing process to establish the plan of care in which nursing services are delivered to patients. The level and impact of the nursing process differ between the RN and LVN, as well as the levels of RN education (9).
Assessment
The comprehensive assessment is the first step and lays the foundation for the nursing process. The thorough evaluation is the initial and ongoing, extensive data collection, analysis, and interpretation. Nursing judgment is based on the assessment findings. The RN uses clinical reasoning and knowledge, evidence-based outcomes, and research as the basis for decision-making and comprehensive care (9).
Based upon the comprehensive assessment, the RN determines the physical and mental health status, needs, and preferences of culturally, ethnically, and socially diverse patients and their families using evidence-based health data and knowledge synthesis. Surveillance is an essential step in the comprehensive assessment process. The RN must anticipate and recognize changes in patient conditions and determine when reassessments are needed (9).
Patient Diagnosis/Problem Identification/Planning
The second step in the nursing process is nursing diagnosis and problem identification. The role of the RN is to synthesize comprehensive assessment data to identify problems, formulate goals/outcomes, and develop plans of care for patients, families, populations, and communities using information from evidence-based practice and published research in collaboration with these groups and the interdisciplinary health care team (9).
The third step in the nursing process is planning. The RN synthesizes the data collected during the comprehensive assessment to identify problems, make nursing diagnoses, and formulate goals, teaching plans, and outcomes. A nursing plan of care for patients is developed by the RN, who is responsible for coordinating nursing care for patients. Teaching plans address health promotion, maintenance, restoration, and risk factors prevention. The RN utilizes evidence-based practice, published research, and information from patients and the interdisciplinary healthcare team during the planning process (9).
Implementation
Implementing the plan of care is the fourth step in the nursing process. The RN may begin, deliver, assign, or delegate specific interventions within the care plan for patients within legal, ethical, and regulatory parameters and consider health restoration, disease prevention, wellness, and promotion of healthy lifestyles (9).
The RN's duty to patient safety when making assignments to other nurses or delegating tasks to unlicensed staff is to consider the education, training, skill, competence, and physical and emotional abilities of those to whom the assignments or delegation is made. The RN is responsible for reasonable and prudent decisions regarding assignments and delegation. The RN's scope of practice may include the supervision of LVNs or other RNs. Supervision of LVN staff is defined as the process of directing, guiding, and influencing the outcome of an individual's performance and activity. The RN may have to directly observe and evaluate the nursing care provided depending on the LVN's skills and competence, patient conditions, and level of urgency in emergent situations (9).
The RN may determine when to delegate tasks to unlicensed personnel and maintain accountability for how they perform the tasks. The RN is responsible for supervising the unlicensed personnel when tasks are delegated. The proximity of supervision depends upon patient conditions and the skill level of the unlicensed personnel. In addition, teaching and counseling are interwoven throughout the implementation phase of the nursing process. (10,11)
Evaluation and Reassessment
A critical and final step in the nursing process is evaluation. The RN evaluates and reports patient outcomes and responses to therapeutic interventions compared to benchmarks from evidence-based practice and research findings and plans any follow-up care and referrals to appropriate resources that may be needed. The evaluation phase is one of the times when the RN reassesses patient conditions and determines if interventions were effective and if any modifications to the care plan are necessary (9).
Essential Skills Used in the Nursing Process
Communication
Communication is an essential and fundamental component used during the nursing process. The RN must communicate verbally, in writing, or electronically with healthcare team members, patients, and their families in all aspects of the nursing care provided to patients. The patient record or nursing care plan must appropriately document these communications. Because RNs plan, coordinate, initiate, and implement a multidisciplinary team's approach to patient care, collaboration is crucial to communication. When patient conditions or situations exceed the RN's level of competency, the RN must be prepared to seek out other RNs with greater competency or other health care providers with differing knowledge and skillsets and actively cooperate to ensure patient safety (9).
Clinical Reasoning
Clinical reasoning is another integral component of the nursing process. RNs use critical thinking skills to problem-solve and make decisions in response to patients, their families, and the healthcare environment. RNs are accountable and responsible for the quality of nursing care provided and must exercise prudent and professional nursing judgment to ensure the standards of nursing practice are always met (9).
Employment Setting
When an employer hires an RN to perform a job, the RN must ensure that it is safe and legal. Caution must be exercised to stay within the legal parameters of nursing practice when an employer may not understand the limits of the RN's scope of practice and makes an assignment that is not safe. Before engaging in an activity or assignment, the RN must determine whether he or she has the education, training, skill, competency, and physical and emotional ability to carry out the activity or assignment safely. The RN must always provide patients with safe, compassionate, and comprehensive nursing care (9).
Summary of RN Scope of Practice
The RN, with a focus on patient safety, must function within the legal scope of practice and by the federal, state, and local laws, rules and regulations, and policies, procedures, and guidelines of the employing health care institution or practice setting. The RN functions under his or her license and assumes accountability and responsibility for the quality of care provided to patients and their families according to the standards of nursing practice. The RN demonstrates responsibility for continued competence in nursing practice and develops insight through reflection, self-analysis, self-care, and lifelong learning (9).
The table below offers a brief synopsis of how the scope of practice for nurses differs based on educational preparation and level of licensure. These are minimum competencies but also set limits on what the LVN or RN can do at his or her given level of licensure, regardless of experience (9).
Synopsis of Differences in Scope of Practice for Licensed Vocational, Associate, Diploma and Baccalaureate Degree Nurses (10)
Synopsis of Differences in Scope of Practice for Licensed Vocational, Associate, Diploma and Baccalaureate Degree Nurses (4)
| Nursing Practice |
LVN Scope of Practice Directed/Supervised Role |
ADN or Diploma RN Scope of Practice Independent Role |
BSN RN Scope of Practice Independent Role |
| Education |
|
|
|
| Setting |
|
|
|
| Assessment |
|
|
|
| Nursing Diagnosis/ Problem Identification/ Planning |
|
|
|
| Implementation |
|
|
|
|
Evaluation
|
|
|
|
Nursing board Position Statements are not laws, but they provide direction for nurses on issues of concern to the Board relevant to public protection. These Position Statements are reviewed annually for relevance and accuracy to current practice, the Nurse Practice Act, and Board of Nursing rules. Examples of Position Statements include the following: (9)
- Nurses Carrying out Orders from Physician Assistants
- Role of the Licensed Vocational Nurse in the Pronouncement of Death
- LVNs Engaging in IV Therapy, Venipuncture, or PICC Lines
- Educational Mobility
- Nurses with Responsibility for Initiating Physician Standing Orders
- Board Rules Associated with Alleged Patient "Abandonment"
- The Role of LVNs & RNs in the Management and Administration of Medications via Epidural or Intrathecal Catheter Routes
- The Role of the Nurse in Moderate Sedation
- Performance of Laser Therapy by RNs or LVNs
- Continuing Education: Limitations for Expanding Scope of Practice
- Delegated Medical Acts
- Use of American Psychiatric Association Diagnoses by LVN, RNs, or APRNs
- Role of LVNs & RNs As School Nurses
- Duty of a Nurse in any Practice Setting
- Board's Jurisdiction Over a Nurse's Practice in Any Role and Use of the Nursing Title
- Development of Nursing Education Programs
- Texas Board of Nursing/Board of Pharmacy Joint Position Statement on Medication Errors
- Nurses Carrying Out Orders from Advanced Practice Registered Nurses (APRN)
- Nurses Carrying Out Orders from Pharmacists for Drug Therapy Management
- Registered Nurses in the Management of an Unwitnessed Arrest in a Resident in a Long-Term Care Facility (9)

Self Quiz
Ask yourself...
-
What are advantages for nurses to consistently use the nursing process during care and documentation of care of clients?
-
How could communication breakdown among employee nurse team members impact a client's care?
-
Are nursing board Position Statements laws?
-
Name one example of a nursing board Position Statement.
-
What do RNs use to problem-solve and make decisions regarding care of clients, when it comes to Texas Nursing Jurisprudence and Ethics?
Principles of Texas Nursing Jurisprudence and Ethics
Professional Boundaries
15.29 Professional Boundaries including use of social media by nurses (11)
The purpose of this Position Statement is to guide nurses regarding expectations related to professional boundaries, including social media, and to provide nurses with guidance to prevent boundary violations (5).
In keeping with its mission to protect public health, safety, and welfare, the Texas Board of Nursing (BON or Board) holds nurses accountable for knowing, recognizing, and maintaining professional boundaries of the nurse-patient/client relationship. The term professional boundaries is defined as the appropriate limits that the nurse should establish in the nurse/client relationship due to the nurse's power and the patient's vulnerability. Professional boundaries refer to the provision of nursing services within the limits of the nurse/client relationship, which promote the client's dignity, independence, and best interests and refrain from inappropriate involvement in the client's relationships and the obtainment of the nurse's gain at the client's expense (5).
The National Council of State Boards of Nursing (NCSBN) defines professional boundaries as the spaces between the nurse's power and the patient's vulnerability. The nurse's power comes from the nurse's professional position and access to sensitive personal information. The difference in personal information the nurse knows about the patient versus the personal information the patient knows about the nurse creates an imbalance in the nurse-patient relationship. Nurses should respect the power imbalance and ensure a patient-centered relationship (5).
Common to the definition of professional boundaries from the Texas Board of Nursing and the NCSBN is that a nurse abstains from personal gain at the client's expense and refrains from inappropriate involvement with the patient or the patient's family (5).
Duty of a Nurse in Maintenance of Professional Boundaries
There is a power differential between the nurse and the patient. The patient depends on the nurse's knowledge and relies on the nurse to advocate for the patient and ensure actions are taken in the patient's best interest. The nurse must protect the patient, establishing and maintaining professional boundaries in the nurse-patient/client relationship. Under or over-involvement can harm the patient and may interfere with the nurse-patient relationship. Visualizing the two ends of the spectrum may assist the nurse in knowing, recognizing, and maintaining the professional boundaries of nurse-patient relationships (5).
Patients each have their own unique needs and abilities. The boundary line for any one patient may change over time and may not be the same as the boundary line for another patient. It is up to the nurse to assess and recognize the patient's needs, adjusting the nursing care accordingly. Every nurse is responsible for knowing, identifying, and maintaining the professional boundaries of the nurse-client relationship (5).
Boundary Violations
A violation of professional boundaries is one element of the definition of "conduct subject to reporting [Tex. Occ.Ide Sec. 301.401(1)(C)]. A professional boundary violation is also considered unprofessional conduct [22 TAC §217.12 (6)(D)]. Some of the specific categories of professional boundary violations include but are not limited to, physical, sexual, emotional, or financial boundary violations (5).
Use of Social Media and the Protection of Health Information
Social media and other electronic communication are expanding exponentially as the number of social media outlets, platforms, and applications available continues to increase. Nurses play a significant role in identifying, interpreting, and transmitting knowledge and information within healthcare. As technological advances expand connectivity and communication, rapid knowledge exchange and dissemination can pose risks to patients and nurses. While the Board recognizes that using social media can be a valuable tool in healthcare, there are potentially severe consequences if misused. A nurse's use of social media may cause the nurse to unintentionally blur the lines between the nurse's professional and personal life (5).
Online postings may harm patients if protected health information is disclosed. In addition, social media postings may reflect negatively on individual nurses, the nursing profession, the public's trust in the nursing profession, or the employer and may jeopardize careers. In an NCSBN survey, many responding boards reported receiving complaints about nurses misusing social media sites. The survey results indicated that boards fired by employers have disciplined nurses and are criminally charged for the inappropriate or unprofessional use of social media (5).
To ensure the mission to protect and promote the welfare of the people of Texas, the Texas Board of Nursing supports the guidelines and principles of social media use by the NCSBN and the American Nurses Association. By the NCSBN guidelines and Board rules, it is the Board's position that (5):
Nurses have an ethical and legal obligation to maintain patient privacy and confidentiality. When using social media, nurses do not identify patients by name or post or publish information that may lead to patient identification. Limiting access to postings through privacy settings is not sufficient to ensure privacy. Nurses must promptly report any identified breach of confidentiality or privacy (5).
Nurses maintain professional boundaries in the use of electronic media. The nurse must establish, communicate, and enforce professional boundaries with patients online. Nurses do not refer to patients disparagingly, even if the patient is not identified, or transmit information that may be reasonably anticipated to violate patient rights to confidentiality or privacy or otherwise degrade or embarrass the patient (5).
Nurses must provide nursing services without discrimination and not make threatening, harassing, profane, obscene, sexually explicit, racially derogatory, homophobic, or other offensive comments (5).
Nurses must be aware of and comply with all laws and rules, including employer policies regarding using electronic devices, including employer-owned computers, cameras, and personal devices. In addition, nurses must ensure appropriate and therapeutic use of all patient-related electronic media, including patient-related images, photos, or videos, by applicable laws, rules, and institutional policies and procedures (5).
The use of social media can be of tremendous benefit to nurses and patients alike, for example, the dissemination of public safety announcements. However, nurses must know the potential consequences of disclosing patient-related information via social media. Nurses must always maintain professional standards, boundaries, and compliance with local, state, and federal laws. All nurses must protect their patients' privacy and confidentiality, which extends to all environments, including social media (5).
The following are ways to avoid problems when using social media:
- Never post any healthcare-related images, client information, or even general client information
- Only use your organization's name or a client or family member's name to post content about or speak for your employer if your organization authorizes you to follow their specific policy and procedures.
- Never post comments about a client, even if the client is not named.
- Never post photos or videos of your healthcare organization or clients
- Never post any comments about your employer or other team members
- Never use obscenity, profanity, racial slurs, sexually inappropriate comments, homophobic comments, threats, harassing/abusive language, or any other offensive comments. Never post any image that contains the above content.
Prevention of Boundary Violations
The ability of a client to rely on employees as concerned and caring individuals who remain objective in their guidance is one of the tents of a safe, therapeutic relationship. The relationship may no longer be objectively therapeutic when staff interacts with patients personally. Accepting gifts, financial transactions, and romantic entanglement could lead to various negative consequences for an organization, employee, or client. Many organizations enforce a non-fraternization policy between employees and current or former clients. While there are exceptions, the expectation is that employees are not to establish a personal relationship with a current or former client. Organizations do recognize that there are times when peers, friends, family, or neighbors of employees seek treatment. In these circumstances, the relationship must remain the nature it was before admission if in the client's best interest, and the treatment plan should address the relationship to best meet the client's therapeutic needs. Employees should also notify a supervisor when an individual with whom he or she has a relationship is admitted for treatment (5).
Texas Nurses are required to comply with mandatory reporting requirements of Texas Occupations Code Chapter 301 NPA Subchapter I, which include reporting a nurse (11):
- Who violates the NPA or a board rule and contributed to the death or severe injury of a patient.
- Whose conduct causes a person to suspect that the nurse's practice is impaired by chemical dependency or drug or alcohol abuse?
- Whose actions constitute abuse, exploitation, fraud, or a violation of professional boundaries.
- Whose actions indicate that the nurse lacks knowledge, skill, judgment, or conscientiousness to such an extent that the nurse's continued practice of nursing could reasonably be expected to pose a risk of harm to a patient or another person, regardless of whether the conduct consists of a single incident or a pattern of behavior.
The exception is for minor incidents, peer review, or peer assistance if there is no practice violation as stated in the Nursing Practice Act and Board rules (6, 11).
Organizations also take many precautions to ensure appropriate employee-client relationships, including (13):
- Criminal background checks of employees
- Employee, student, and volunteer education regarding therapeutic boundaries and issues and consequences of any violations
- Mandatory, supportive, and confidential reporting of any violation
Employee supervision also includes the identification of early signals that an employee may be crossing therapeutic boundaries and the institution of appropriate interventions. Employees educate clients regarding the importance of maintaining a therapeutic relationship and proper boundaries. Organizations work to ensure adequate supervision of staff and appropriate supervision of clients, such as increased observation or same-gender staff working with a client when appropriate (13).
There must be mandatory reporting by any employee who becomes aware of a boundary violation. The employee should report this immediately to their supervisor, who will evaluate the nature and severity of the claim and initiate an investigation of the situation. In conjunction with Human Resources and Risk Management, the immediate supervisor will determine whether an accused employee should be put on immediate leave pending investigation results and whether mandatory reporting of the allegations to outside agencies is required. Legal Counsel may also be consulted when necessary. An employer may not suspend or terminate employment or otherwise discipline, retaliate, or discriminate against a person who reports, in good faith, or advises a nurse of the nurse's rights and obligations (5, 9, 11, 12).

Self Quiz
Ask yourself...
- Why is it important to Texas Nursing Jurisprudence and Ethics for a nurse to maintain professional and appropriate boundaries with a client?
- Name two examples of how social media may cause a nurse to blur the lines between his/her personal and professional life?
- Is reporting of boundary violations mandatory? If so, name two examples of when a nurse should report.
- How do organizations take precautions to ensure appropriate employee-client relationships?
- List two examples of nurses whom a nurse in Texas would report for violations of the Nurse Practice Act.
Unprofessional Conduct - Rule §217.12
The following unprofessional conduct rules are intended to protect clients and the public from incompetent, unethical, or illegal conduct of licensees. The purpose of these rules is to identify behaviors in the practice of nursing that are likely to deceive, defraud, or injure clients or the public. Actual injury to a client need not be established. These behaviors include but are not limited to: (all from 5)
1.Unsafe practice – actions or conduct including, but not limited to:
- Carelessly failing, repeatedly failing, or exhibiting an inability to perform vocational, registered, or advanced practice nursing in conformity with the standards of a minimum acceptable level of nursing practice set out in §217.11 of this chapter.
- Failing to conform to generally accepted nursing standards in applicable practice settings.
- Improper management of client records.
- Delegating or assigning nursing functions or a prescribed health function when the delegation or assignment could reasonably be expected to result in unsafe or ineffective client care.
- Accepting the assignment of nursing functions or a prescribed health function when the acceptance of the assignment could be reasonably expected to result in unsafe or ineffective client care.
- Failing to supervise the performance of tasks by any individual working pursuant to the nurse's delegation or assignment.
- Failure of a clinical nursing instructor to adequately supervise or to assure adequate supervision of student experiences.
2. Failure of a chief administrative nurse to follow standards and guidelines required by federal or state law or regulation or by facility policy in providing oversight of the nursing organization and nursing services for which the nurse is administratively responsible.
3. Failure to practice within a modified scope of practice or with the required accommodations, as specified by the Board in granting an encumbered license or any stipulated agreement with the Board.
4. Conduct that may endanger a client's life, health, or safety.
5. Inability to Practice Safely – a demonstration of actual or potential inability to practice nursing with reasonable skill and safety to clients by reason of illness, use of alcohol, drugs, chemicals, or any other mood-altering substances, or as a result of any mental or physical condition.
6. Misconduct – actions or conduct that include, but are not limited to:
- Falsifying reports, client documentation, agency records, or other documents.
- Failing to cooperate with a lawful investigation conducted by the Board.
- Causing or permitting physical, emotional, or verbal abuse or injury or neglect to the client or the public, or failing to report same to the employer, appropriate legal authority and/or licensing Board.
- Violating professional boundaries of the nurse/client relationship including but not limited to physical, sexual, emotional, or financial exploitation of the client or the client's significant other(s).
- Engaging in sexual conduct with a client, touching a client in a sexual manner, requesting, or offering sexual favors, or language or behavior suggestive of the same.
- Threatening or violent behavior in the workplace.
- Misappropriating, in connection with the practice of nursing, anything of value or benefit, including but not limited to, any property, real or personal of the client, employer, or any other person or entity, or failing to take precautions to prevent such misappropriation.
- Providing information, which was false, deceptive, or misleading in connection with the practice of nursing.
- Failing to answer specific questions or providing false or misleading answers in a licensure or employment matter that could reasonably affect the decision to license, employ, certify, or otherwise utilize a nurse.
- Offering, giving, soliciting, or receiving, or agreeing to receive, directly or indirectly, any fee or other consideration to or from a third party for the referral of a client in connection with the performance of professional services.
7. Failure to pay child support payments as required by the Texas Family Code §232.001, et seq.
8. Drug diversion – diversion or attempts to divert drugs or controlled substances.
9. Dismissal from a board-approved peer assistance program for noncompliance and referral by that program to the Board.
10. Other drug-related actions or conduct that include, but are not limited to:
- Use of any controlled substance or any drug, prescribed or unprescribed, or device or alcoholic beverages while on duty or on call and to the extent that such use may impair the nurse's ability to safely conduct to the public the practice authorized by the nurse's license.
- Falsification of or making incorrect, inconsistent, or unintelligible entries in any agency, client, or other record pertaining to drugs or controlled substances.
- Failing to follow the policy and procedure in place for the wastage of medications at the facility where the nurse was employed or working at the time of the incident(s).
- A positive drug screen for which there is no lawful prescription.
- Obtaining or attempting to obtain or deliver medication(s) through means of misrepresentation, fraud, forgery, deception and/or subterfuge.
11. Unlawful practice – actions or conduct that include, but are not limited to:
- Knowingly aiding, assisting, advising, or allowing an unlicensed person to engage in the unlawful practice of vocational, registered, or advanced practice nursing.
- Violating an order of the Board, or carelessly or repetitively violating a state or federal law relating to the practice of vocational, registered, or advanced practice nursing, or violating a state or federal narcotics or controlled substance law.
- Aiding, assisting, advising, or allowing a nurse under Board Order to violate the conditions set forth in the Order.
- Failing to report violations of the Nursing Practice Act and/or the Board's rules and regulations.
12. Leaving a nursing assignment, including a supervisory assignment, without notifying the appropriate personnel.
There is a Texas State Board of Nursing Disciplinary Matrix that nurses can review to see the process followed when a review of a nurse's conduct is necessary. The Board will consider public safety, the seriousness of the violation, and any aggravating or mitigating factors. Other factors considered include the presence of multiple violations, prior violations, and costs which could result in a more severe disciplinary action. (13)

Self Quiz
Ask yourself...
- Name two examples of unsafe nursing practice that will result in a nursing board review.
- Is violating boundaries of the employee-client relationship considered misconduct?
- Is failing to report violations of the Nursing Practice Act misconduct?
- Is failing to report violations of the Nursing Board's rules and regulations misconduct?
- Name two examples of unsafe nursing practice that will result in a nursing board review.
- Is violating boundaries of the employee-client relationship considered misconduct?
- Is failing to report violations of the Texas Nursing Jurisprudence and Ethics misconduct?
- Is failing to report violations of the Nursing Board's rules and regulations misconduct?
- What qualifies as an unlawful practice?
- What policies does your facility have regarding drug screening and reporting?
Provisions of the Code of Ethics for Nurses
Provision 1
The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person. (1)
Provision 2
The nurse's primary commitment is to the patient, whether an individual, family, group, community, or population. (1)
Provision 3
The nurse promotes, advocates for, and protects the rights, health, and safety of the patient. (1)
Provision 4
The nurse has authority, accountability, and responsibility for nursing practice, makes decisions, and takes action consistent with the obligation to provide optimal patient care. (1)
Provision 5
The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth. (1)
Provision 6
The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care. (1)
Provision 7
The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy. (1)
Provision 8
The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities. (1)
Provision 9
The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy. (1)

Self Quiz
Ask yourself...
- Who is a Texas nursing jurisprudence and ethics-oriented nurse primarily committed to?
- Name two examples of how a nurse advocates for a client.
- Name three ways a nurse committed to Texas nursing jurisprudence and ethics protects a client's rights.
- Which of the abovementioned provisions have you found to be the most challenging to meet?
- What resources are available in your area to help navigate difficult ethical situations?
Case Study
Rachel is a 13-year-old adolescent female client admitted to an inpatient behavioral health unit for bipolar disorder, alcohol and marijuana abuse, and borderline personality disorder. The client has a history of sexual promiscuity, lying, and has alleged abuse and rape by history. Rachel approaches the Charge RN at bedtime, saying that an employee and she "have been having sex" many times over the course of two weeks and that she realizes now that "she should have told someone". The alleged employee is currently on duty.
As Charge RN, using what you learned about Texas Nursing Jurisprudence and Ethics, how would you respond, and what are your next steps?
Conclusion - Texas Nursing Jurisprudence and Ethics
When a nurse is named in a negligence or malpractice lawsuit, it can create stress for the client, the employee, and the employer. A nurse maintaining professional, ethical, and jurisprudent conduct will help to ensure standards of practice are consistently followed. Maintaining appropriate boundaries with clients at all times helps maintain a therapeutic employee-client relationship.
It is important that nurses understand their state nurse practice act, the scope of practice of nurse licensure, standards of practice, ethics, and professional boundaries in order to maintain professionalism, meet performance standards, and avoid a breach of duty, injury, and litigation.
Resources
Educational Requirements:
Texas Board of Nursing (2010), Differentiated Essential Competencies (DECs) of graduates of Texas Nursing Programs. (12)
Texas Occupations Code, Chapter 301 (12)
Nursing Practice Act (NPA) Section 301.002, Definitions (12)
Rule 217.11 - Standards of Nursing Practice (12)
Scope of Practice Position Statements: (12)
- Position Statement 15.28 The Registered Nurse Scope of Practice Web version for viewing
- Position Statement 15.14 - Duty of a Nurse Web version for viewing
- Position Statement 15.14 - Duty of a Nurse - HHSC/DADS/BON poster
For the complete list of position statements, click here. (12)
Texas Nursing Forensics
Texas Nursing Forensics
Introduction
In the United States, sexual assault was historically considered a judicial problem; however, it is now considered a major public health concern because of the health and psychological effects on individuals. The problem most notably emerged in the public eye in the 1960s with the women's liberation movement. In recent times the #METOO movement has increased awareness of the problem, and many organizations have surfaced to assist the assaulted. This course will focus on the problem in rural areas in the state of Texas and how nurses working in these facilities can best assist patients who have been sexually assaulted.

Self Quiz
Ask yourself...
- Aside from the hospital, what other setting might you encounter victims of sexual assault?
- In your opinion, what factors contribute to limited care for victims of sexual assault in rural areas?
- What types of psychological problems do you suspect victims of sexual assault may struggle with?
- When was the last time you received training in nursing forensics?
- How has the assessment and management of victims of assault changed since you have been in practice?
- Have you seen an increased incidence of sexual assault occur since you have been in practice? How has your facility managed the change?
- How has technology impacted the reporting and documenting of assault?
- What policies and procedures does your facility have regarding victims of assault?
- What resources does your community offer to help victims of assault?
- What policies does your facility have regarding the management of forensics in victims of assault?
Statistical Evidence
National Statistics
According to the Rape Abuse and Incest National Network (RAINN) (1), every 68 seconds someone is sexually assaulted in the United States, and every nine minutes, that victim is a child (1). Only 25 out of every 1,000 perpetrators will end up in prison (1).in less than every 80 seconds, a person is sexually assaulted. In 2015 the Texas Statewide Sexual Assault Prevalence Study found that 33.2% of adult Texans or 413,000 individuals reported having been sexually assaulted at some point during their lives (2).
Each year in the United States (1):
- 80,600 inmates are sexually assaulted or raped
- 60,000 children were victims of “substantiated or indicated” sexual abuse
- 433,648 people 12 and older were sexually assaulted or raped
- 18,900 military personnel experienced unwanted sexual contact
- 1 out of every 6 women have been the victim of attempted or completed rape in her lifetime (14.8% completed, 2.8% attempted)
- 1 in 3 men have experienced an attempted or completed rape in their lifetime
- More women and children are sexually assaulted than men, and that girls under 18 years of age are at the highest risk. According to RAINN (1), men and boys, especially college-aged, are also at risk with transgender students at the highest risk of this group.
Most common locations where sexual assault occurs in the U.S. (1):
- 55% at or near the victim’s home
- 15% in an open public space
- 12% at or near a relative’s home
- 10% in an enclosed but public area (i.e. parking garage or lot)
- 8% on school property
Activities the victims were doing when they were assaulted (1):
- 48% were sleeping or performing another activity at home
- 29% were traveling to and from work or school, or traveling to shop or run errands
- 12% were working
- 7% were attending school
- 5% were doing an unknown or other activity
Sexual Assault on Children (1):
- 1 in 9 girls and 1 in 20 boys under the age of 18 experience sexual abuse or assault
- 2 out of 3 victims of sexual assault or rape (under the age of 18) are age 12 – 17
- Victims of sexual assault or rape under the age of 18 are about 4 times more likely to develop symptoms of drug abuse and PTSD as adults, and about 3 times more likely to experience a major depressive episode as adults

Self Quiz
Ask yourself...
- What statistic surprised you the most? Why?
- Do you feel that these statistics represent what you see in your area? Why do you think that is the case?
- What factors do you think contribute the highest number of sexual assault cases occurring in the home?
- What are some strategies to help victims feel safe reporting their sexual assault?
- What strategies can communities use to protect children from sexual assault?
- In your opinion, what factors impact the reduced reporting from men after being sexually assaulted?
- What education can you provide to victims regarding the incidence of sexual assault?
- What policies does your facility have regarding children who are suspected victims of assault?
- What role does a community and or public health nurse play in the education and prevention of sexual assault?
- How has the education and management of sexual assault prevention changed since you have been in practice?
Texas Statistics
The latest statistics on sexual assault in the state of Texas were from 2018 and is as follows (2):
- Total number of reported sexual assault incidents was 19,816, a 9.4% increase from the prior year
- Of victim-to-offender relationships, 11% were romantic, 14% parental/child, 19% other family, and 55% other.
- Victims were 88% were female and 12% male
- Victims who were aged 10 – 14 were the group with highest number of cases
- Of all victims, 82% were white, 17% black, and 1% American Indian/Alaskan Native, Asian, or Native Hawaiian/Pacific Islander
Location of sexual assault incidents in Texas in 2018 (2):
- 16,015 in residents/homes
- 2,041 in unknown or other areas
- 657 in a hotel/motel
- 718 in school/college
- 710 in a highway/road/alley
- 506 in a parking lot/garage
- 268 in fields/woods
- 185 in commercial/office buildings
- 176 in drug stores, doctor’s offices, or hospitals

Self Quiz
Ask yourself...
- Do you think the care should be different for a patient sexually assaulted by a family member versus a romantic partner?
- The age of sexual assault is younger in Texas (10 to 14) than the country (12 to 17). What strategies can Texas employ for prevention?
- What is the benefit of knowing statistical evidence about sexual assault?
- What might need to be considered when caring for a male patient who had been sexually assaulted versus a female patient?
- What are your thoughts on the incidence of sexual assault in Texas in comparison to that of the U.S.?
- Have you seen an increase in sexual assault in your area? What do you feel has contributed to that?
- Do you feel that the Texas statistics listed above are accurate? Or do you think that they are higher or lower? Why?
- Which population group have you encountered most frequently in practice?
- How does your education and communication change in different genders, ages, and ethic groups who are victims of sexual assault?
- What prevention techniques have you seen to help prevent the incidence of sexual assault?
The Basics: Sexual Assault
What is Sexual Assault?
Sexual assault, also termed sexual violence, is described as “any type of unwanted sexual contact, including words and actions of a sexual nature against a person’s will and without their consent; a person may use force, threats, manipulation, or coercion to commit sexual violence” (3). Sexual assault is often defined separate from rape. Rape consists of penetration, whether vaginally, anally, or orally. Sexual assault is any type of unwanted sexual content and is not limited to rape. Sexual abuse, as described by the American Psychological Association (APA) "is unwanted sexual activity, with perpetrators using force, making threats or taking advantage of victims not able to give consent" (3). Assault can be the product of domestic abuse, gang violence, date rape, and incest. Assault can be inflicted on any age or gender and often occurs by someone who is related to or knows the victim.
What is SANE?
In many parts of the United States, Sexual Assault Nurse Examiners (SANE), nurses who are expertly trained in performing forensic examinations and collection of evidence, are utilized (5). SANEs are nurses who specialize in forensic nursing. In forensic nursing, the health and legal system intersect (10). SANE programs began as early as the 1970s. At that time, nurses noticed that victims of sexual assault were not provided high quality care like other patients were in the emergency department. Nurses also noticed that the victims were very concerned about STDs and pregnancy and needed special treatment. Over the next 20 years, the forensic specialty grew, and the First SANE programs were started in Tennesse, Minnesota, and Texas. Today, Texas registered nurses working in the emergency departments must learn the SANE process to perform the forensics exams and evidence collection by completing a 2-hour educational program.

Self Quiz
Ask yourself...
- Why do you think sexual assault has changed from a judicial problem to a health problem?
- How can nurses contribute to a decrease in the costs associated with sexual assault?
- What organizations in Texas can you connect with to learn more about sexual assault and how you can impact the problem?
- Where can you find more information on SANE programs?
- What additional training can you complete to help better prepare you to manage sexual assault victims?
- What is the definition of sexual assault?
- How many nurses are available in your facility who are SANE nurses?
- What resources does your facility and community offer to help pay for the cost of becoming a SANE nurse?
- What additional resources are you aware of to assist with the management of sexual assault victims?
- What barriers to identifying sexual assault have you encountered? How have you overcome them?
Nursing's Role
Sexual assault is an extremely traumatic experience. Those affected can have a wide range of issues, emotionally, spiritually, physically, and psychologically. Nurses working in the emergency department are often first responders. Compassion, empathy, and privacy are a hallmark of excellent practice when caring for patients who have been sexually assaulted.
Many patients will experience shock and disbelief. "Why me? Will I be okay?" or "It's no big deal, I'm fine" (6). There may be "fear of responses from friends, family, the public, and criminal justice providers" (7). Victims of rape may also have concerns about pregnancy, STIs, and HIV/AIDS. These patients may feel their world has turned upside down. They may be scorned, told it was deserved, and fear their names could be made public (7).
In order to provide excellent care, all gender identities must be taken into consideration, as well as age and sexual orientation. No bias or judgment should be displayed to the patient. Customs, beliefs, religious, and spiritual needs should also be considered during the visit
Team Collaboration
Working with all personnel in the emergency department is essential. From paramedics, law enforcement officers, family, or anyone accompanying the patient to physicians, social workers, and forensic medical examiners, each professional has a specific skill set and role in the patient's care. Teamwork among these groups of individuals will provide the best possible outcomes for the patient. Team members involved in a victim’s care may include (8):
- “Community-based advocates
- Law enforcement officers
- SANEs, physicians or nurses trained in sexual assault medical forensic evidence collection
- Law enforcement victim service advocates
- District Attorney’s Office personnel, legal victim advocates and attorneys”
Interview
The interviewing nurse should actively listen, believe what the patient discloses, validate the patient’s feelings, maintain confidentiality, and honor the patient’s decisions on what to do about the assault. When caring for patients who have sexually assaulted, treating the whole person rather than the "problem" alone is vital. Repeating information back to the patient can help to elicit more precise information. Repeating information can also help to validate what the patient is saying, creating an atmosphere of trust. Consider that patients may not want to talk about the assault, as reliving it could bring out unwanted emotions.
If the patient arrives alone, the nurse should inquire if the patient wants a companion or an advocate to be present. An advocate could be a family member, friend, member of the clergy, or social worker. The patient can choose if they want someone present. Care must be taken to ensure the patient feels comfortable, as the presence of someone emotionally involved (or even the assaulter themselves) may deter the patient from being open and honest. An interpreter should also be arranged if needed, with the patient's consent.
If the patient has not alerted the local police, the nurse should inquire if they wish to report the assault and if so, the police should then be called. If available, a sexual assault response team (SART) should be immediately contacted. It is of the utmost importance to remember that the patient always makes the primary decision of what to do surrounding the case. Also, the patient must give consent first before any decisions are made. Admitting the patient to a private room in a quiet area of the emergency department lessens interruptions from outside sources.

Self Quiz
Ask yourself...
- Does your facility have a Sexual Assault Response Team (SART)?
- Have you ever taken care of a patient who had been sexually assaulted?
- What are some strategies you can employ if your emergency department does not have a private room to interview a victim of sexual assault?
- What is the protocol at your facility if a parent brings their child into the emergency department with sexual assault injuries?
- What techniques during the interview process of a sexual assault victim have you found to be unsuccessful?
- What techniques during the interview process of a sexual assault victim have you found to be successful?
- What types of collaboration have you seen in the facilities where you have worked?
- What role does law enforcement play in managing victims of sexual assault?
- What education do you provide to patients regarding STIs after sexual assault?
- How do you ensure the privacy of victims after admitting them to the hospital?
Assessment
After obtaining consent to perform the assessment, the patient should be advised of every step before each part of the exam. The patient should be informed they have total control of what is happening. It is important for the nurse to help the patient understand they always have the right to refuse any and all steps in the examination.
When performing the initial assessment and gathering information, documentation must include a very detailed and complete history, including any physical trauma to the patient’s body. The history should include any bruises, lacerations, or other visual injuries and how and when they occurred. The nurse should perform the interview slowly, giving the patient time to process and answer each question. The patient may or may not want to identify the person who assaulted them and should not be coerced into doing so.
A complete medical, surgical, and gynecologic history, in the case of a female patient, and any new symptoms occurring after the assault should be asked. Drug allergies, medications, and any alcohol or illegal drugs used at the time of the event are also documented. A compassionate and empathic tone should always be used to allow the patient to feel safe. The patient should not feel any judgment from any emergency department personnel. Patients should be given the opportunity and encouraged to grieve and react during this time. They should feel comfortable enough to ask and answer questions throughout the interview.
According to Texas law, nurses must obtain written consent from the patient. During the complete physical exam, the nurse will be charged with ensuring physical evidence of the assault from clothing or body fluids is not disturbed. Also, during this time, suicidality and emotional support should be assessed. Providing expert treatment for patients who have been sexually assaulted is of utmost importance. When available, a SANE nurse will perform the forensic examination. This examination is vital to collect and preserve physical evidence from the patient while also assessing life and limb injuries. If a SANE nurse is unavailable, as may be the case in Texas's rural areas, a "medical forensic examiner" will perform the examination.


Self Quiz
Ask yourself...
- How would you handle a situation in which a patient who has recently been sexually assaulted does not want to participate in the physical assessment?
- Are you familiar with medical forensic examiners?
- How often does your facility audit documentation?
- How might a nurse address their own biases when caring for a victim of sexual assault?
- What barriers to assessment have you encountered? How have you overcome them?
- Do you have to receive written consent from a patient before a physical exam?
- What policies does your facility have regarding the psychosocial assessment of patients of sexual assault?
- How do you ensure that your patient stays informed of their care while respecting their emotions?
- How can a complete medical, surgical, and gynecological history improve patient care and outcomes?
- What is a medical forensic examiner?
Documentation
When documenting the case, the nurse should use open-ended questions to elicit the patient's best and clearest responses. Documentation must be complete and exact, including every stage of the assault with times, dates, and descriptions, with consideration for the patient's emotional state and ability to recall. Using motivational interviewing can be helpful as well. Documenting in the patient’s own words is best practice. Nurses should try their best to document all of the following about the case (8):
- “All those present during the patient’s history and examination
- Time, date, and location of assault(s)
- Contact and/or penetrative acts by suspect(s)
- Was the suspect injured in any way, if known?
- Use of lubricant, including saliva
- Patient’s actions between the sexual assault and arrival at the facility (brushing teeth, using mouthwash, smoking, vaping, changing clothes, vomiting, swimming, showering, or bathing)
- Was a condom used?
- Did ejaculation occur? Where?
- Any weapon use or physical force, or threat of weapon use or physical force?
- Description of condition of clothing (and was clothing torn or stained prior to assault?)”
In the case of a minor, a parent will give consent, and if no parent is available or is the assaulter, the child will be turned over to the appropriate child and family services in the state. If the assaulted patient has dementia or is an elder with cognitive issues and is therefore unable to consent, adult protective services should be contacted (8). There are also rules governing military sexual offenses. Remember when documenting these cases, whether using handwritten or electronic medical records, any and all information is subject to HIPAA.

Self Quiz
Ask yourself...
- What skills do you have that could best be used when caring for patients who have sexually assaulted?
- How would you, as the initial contact, approach an individual who has been sexually assaulted?
- What skills would you need to learn or improve when caring for a patient who has been sexually assaulted?
- Currently, do you feel capable of caring for a patient who has been sexually assaulted without judgment and with compassion?
- What documentation policies do you have at your facility regarding sexual assault victims?
Texas Forensic Law
The Texas government code 420.031 (9) describes the protocol that must be taken to develop and protect evidence collection in a sexual assault case. Since a major part of Texas is rural, the code was enacted to protect and care for patients and the collected evidence in areas where a SANE nurse is not available. In these cases, a medical forensic examiner may perform the exam and evidence collection.
A medical forensic examiner is described as any practitioner Medical Doctor, Registered Nurse, Nurse Practitioner, or Physician's Assistant who has undergone a minimum of 2 hours of training in forensic evidence collection. The law outlines requirements in the collection and preservation of evidence. In 2019, the code was amended to require written informed consent from the patient or guardian for release of the evidence and must be gained prior to the history and physical. Obtaining consent also carries important psychological implications after a sexual assault since the patient's right to consent was violated by the assaulter. Sexual assault examination teams should always be involved as early as possible.
Texas Forensic Law: Statute of Limitations
The statute of limitations for sexual assault cases can be defined as a deadline in which a person can report a sexual assault. The statute of limitations vary per state and the length of time for reporting can depend on whether the case is criminal or civil. Criminal cases are committed against the state and prosecuted by the state; civil cases occur between individuals/groups and are prosecuted by a civil court (i.e. family court or personal injury cases) (12). In Texas, the statute of limitations varies by age and whether the case is criminal or civil. The following are general statute of limitations regarding sexual assault in Texas (13)(14). The legal age of sexual consent in Texas is 17.
For adults, the statute of limitation is 10 years from the victim’s 18th birthday. As of 2019, victims of sexual assault can file a personal injury claim for injuries arising from childhood sexual abuse up to 30 years from the incident.
There is no statute of limitations if:
- During the investigation of the offense, biological matter (evidence) is collected, and the matter has not yet been subjected to forensic DNA testing
- Forensic DNA testing results show that the matter does not match the victim or any other person whose identity is readily ascertained
- Probable cause exists to believe that the defendant has committed the same or a similar sex offense against five more victims
- Continuous sexual abuse of young child or disabled individual occurs
- Indecency with a child occurs

Self Quiz
Ask yourself...
- How would you handle a situation in which an adult patient wants to file a claim for a sexual assault that occurred 35 years ago?
- If your 16-year-old patient does not want to file a police report on her boyfriend who sexually assaulted her, how would you respond?
- In which situation would you involve social services?
- How often do you make reports to child or adult protective services?
- How do you become a medical forensic examiner?
- What is a statute of limitations in Texas?
- When is there no statute of limitations?
- What is the difference between criminal and civil cases?
Texas Forensic Law: Evidence
Sexual assault evidence can be found in several areas, including the crime scene, the patient's body, skin, hair, nails and clothing, and other items belonging to the patient (11). There is a specific kit used to collect this evidence. As described by RAINN, the kit is best known as a RAPE or Sexual Assault Evidence Kit (SAEK) and is inclusive of the items listed below (11):
- Bags and paper sheets to put on the floor and collect clothing or other evidence that may fall off the patient while undressing,
- A comb to collect evidence from hair
- Forms for documentation
- Envelopes and containers for the evidence
- Instructions on use of the kit
- Sampling materials and swabs
Types of evidence collected are usually skin samples, scrapings from fingernails, and oral, genital, and anal swabbing internal and external. Directions on how to collect this evidence are included in the kit. The forensic examiner can also use special types of photography to document internal injurie. (11). Personal cameras should never be used. Remember, it is the law that the patient consents to each part of the exam.
As described by RAINN, prior to the forensic exam, it is best if the patient has not changed clothes, combed their hair, brushed their teeth, tried to clean the area, showered, or bathed, or used a restroom. If needing to use the restroom, a urine sample should be collected, educating the patient not to cleanse the perianal area. If they have already showered or bathed and have not arrived at the emergency room yet, emergency personnel need to educate the patient to keep the clothes they were wearing and any other belongings they had with them at the time of the assault in a paper bag in order to preserve the evidence (11). If the patient comes to the emergency department up to 7 days after being sexually assaulted, the exam can still be performed. After the 7 days, it is at the forensic examiner's discretion whether the exam should be performed. Collecting and protecting forensic evidence is a legal, moral, and professional responsibility (12).
Any medical witness who testifies in court is held in the highest regard and as experts in sexual assault cases (5). Courts will closely scrutinize the chain of custody, and if broken, it can cause a conflict in the case and question of validity. Cases may be heard in criminal, civil, juvenile, military courts, or grand juries. If a forensics examiner is called to be a "fact" witness, no opinions on the case will be heard. Only the procedures that were performed on the patient will be admitted, and if the testifier is not the professional who performed the examination, they may be questioned regarding SANE protocols.
If called upon to be an expert witness, the SANE nurse not only has knowledge of protocols but can educate and give opinions to the court. In either case, the necessity for excellent knowledge of SANE protocols is important. Nurses must be comfortable testifying in court as it is a rigorous and stress-provoking experience. Working with your organization's lawyers and prosecutors, as well as reviewing the case extensively, will prepare the nurse to testify in a case (5).

Self Quiz
Ask yourself...
- Have you ever used a sexual assault evidence kit (SAEK)?
- If your emergency department does not have a SAEK, how would you obtain one?
- How well do you feel you could testify in court?
- Where in your facility can you find support if you had to testify?
- What policies does your facility have regarding forensic evidence?
- What training has your facility provided regarding forensic evidence collection?
- What is a medication witness?
- What policies does your facility have in place regarding photographing and placing images in the patient's chart?
- How does your facility store and protect forensic evidence that has been collected?
- What is the time period in which the medical forensic examiner should perform an exam?
Texas Law: Chain of Custody
In order to protect the patient and evidence for the courts, a chain of custody of the evidence must be followed precisely. Failure to comply does not mean the evidence is not admissible in the courts; however, the more complete the evidence, the better chance of conviction of the assaulter. Texas A&M's nursing program offers a chain of evidence handbook outlining each step in the collection of evidence. The information below highlights the collection process from that handbook (8).
Collection of Evidence and Packing
- “Collect evidence so that it will be admissible as evidence in legal proceedings later. Therefore, chain of custody must be maintained and documented throughout the entire patient assessment and evidence collection processes.
- Chain of custody documents the dates and times of everyone who handles every piece of evidence, from the time it is collected through to legal proceedings."
- Evidence should be labeled with patient’s name, date of birth, unique identifier number, examiner’s initials, date, and time.
- If adult patient chooses non-reporting method, the external SAEK is labeled only with the unique identifier number (often the medical record number or the Track-Kit barcode). The Track-Kit identifier can be utilized.
- Consider also labeling additional evidence not included in the kit (i.e., clothing collected when patient is reporting to law enforcement) with Track-Kit labels without the barcode.
- Evidence inside the SAEK is labeled according to standard facility procedure. Follow facility protocols on non-reporting evidence collection.
- Consider providing a card with the unique identifier for the patient if the Track-Kit identifier is not utilized.”
Chain of Custody Documentation
Documentation must include:
- Receipt of evidence
- Storage of the evidence
- Transfer of the evidence
- Date and time of each transfer
- The printed name and signature of each person in possession of or transferring the evidence
- Signatures of all persons transferring or receiving the evidence


Self Quiz
Ask yourself...
- Does your facility evidence collection protocol vary from what is listed above? In what ways?
- At your facility, what is the protocol if the evidence is mishandled or mislabeled?
- Aside from nurses, who else might handle the evidence kit?
- Can you think of any other that should be documented that are not listed above?
- What is the chain of custody?
Swab and Evidence Collection
Explain the reason and process for collection prior to collecting from each site. Nurses can use this time to take digital photos (depending on facility protocol). There should be two swabs used from each site." (8).
Evidence must be kept in sight of the person collecting it at all times. After collected, the evidence must be dried and contained in the SAEK kit and sealed per kit instructions until it can be handed over to the appropriate law enforcement official and opened only by crime lab personnel. Each emergency department should have a locked storage space to provide temporary custody of collected evidence until it can be transferred to the appropriate persons or lab. If a patient is transferred to another facility, the chain of custody again must be documented according to the law.
The law in Texas allows an adult to choose whether to report the assault to law enforcement. If the person chooses not to report, evidence will still be collected and preserved for up to 5 years post-assault. In the case of child sexual assault, elder abuse (over 65), or disabled persons, all medical personnel must report the case to law enforcement as mandatory reporters. Texas caregivers are also required to give patients an information sheet describing where to find appropriate services for the sexually assaulted. This document can be found on the Texas consumer protection website or here: Information for Survivors of Sexual Assault (texas.gov)

Self Quiz
Ask yourself...
- Where can you find more information on the Texas Code of law on sexual abuse?
- Why is it so important to maintain the chain of custody?
- How might you handle a situation in which a victim of sexual assault decides not to report the case to the police?
- How comfortable are you with collecting evidence?
- What resources can you direct patients to regarding the reporting of sexual assault?
Physical and Emotional Effects
After a sexual assault, patients can experience anxiety and depression, post-traumatic stress disorder (PTSD) and turn to alcohol and/or substance abuse. There may be feelings of fear, denial, guilt, shame, loss of self, loss of control, and anger (8). They may feel like their world has been turned upside down, life has stopped, or they cannot move forward. They may feel ashamed and wonder if, in some way, they were responsible. They may not feel safe in their own space and may lack trust.
In domestic cases, the patient may be concerned about their attacker. They may worry that their attacker will be prosecuted and sent away. Daily life can be disrupted to the point of self-isolation and loss of the patient's job, family, and social life. A patient may become disabled to the point of homelessness and poverty. Many may feel the attack is transparent and that others can tell they have been assaulted just by looking at them. Flashbacks can occur at any time, and they may experience nightmares of being chased or attacked. They may also have constant thoughts of the abuse, causing insomnia and intense anxiety.

Self Quiz
Ask yourself...
- If you have cared for victims of sexual assault before, what is the most common effect from the assault that you have witnessed?
- What are some ways to support victims?
- How can nurses support the families of victims?
- If you are giving shift report to the next nurse after caring for a victim of sexual assault, what are the most important pieces of information you will share?
- What are some indicators that the victim may be suffering from PTSD?
Support for Victims
Patients who have been sexually assaulted may contemplate and attempt suicide (8). These issues can extend into long periods of time, with unknown triggers bringing flashbacks or repeated negative feelings. Patients should be informed that their feelings are normal, and each person heals in different ways and in different timeframes. Ongoing support and therapy can assist the patient in recovery as well as self-help and group programs. There are many online, telephone, and in-person programs for victims as well as organizations to assist with ongoing issues. For example, the Rape, Abuse & Incest National Network (RAINN) program can be helpful in advocating for patients and guiding them on their journey to recovery. The National Sexual Violence Resource Center is also a helpful resource.
Many psychologists and therapists work explicitly with victims of sexual assault. The attorney general of the state of Texas website has information and resources for all crime victims. Having a trained sexual assault counselor at the emergency visit time can be of great assistance with the initial contact and subsequent referrals to professionals. Compassionate, empathic, and supportive care by emergency nurses at the initial contact can positively impact the patient's road to a safe and healthy recovery.
Physical injuries must also be considered using clinical assessment, radiology, MRIs, and CT scans when necessary. Laboratory collection for STDs (sexually transmitted diseases), pregnancy in females, possible HIV, and other illness exposures are also a consideration during the physical exam and history taking. Follow-up care for these injuries with subsequent laboratory tests and appointments made with appropriate specialists should be made.
Follow up
Ideally, the nurse could schedule a telephone call with the patient in 2-3 days to assess how they are doing and for continued support and referrals. At that time, the patient may have more questions or concerns that the nurse can help with and provide for follow-up care and resources. A list of educational programs and therapists who specialize in sexual assault and support groups should be supplied to the patient at the time of the visit and subsequent phone calls. There is no handbook on how to recover from trauma; it is an individual journey that is experienced solely by each person. However, there are many resources to assist a patient who has been sexually assaulted at the time of the event and long after.

Self Quiz
Ask yourself...
- What skills would you need to care for the initial emotions of shock and disbelief of a sexually assaulted patient?
- What questions might you ask a patient in a follow-up phone call?
- Where would you find resources to assist patients that have been sexually assaulted?
- How would you handle a situation in which a victim of sexual assault declines help?
- How do you feel you can change or improve your communication with sexual assault victims?
Conclusion
Sexual assault has become a major health problem in the United States. The state of Texas has implemented a code of laws to identify, protect, and collect evidence from patients who have experienced this crisis. The utilization of SANE nurses is common in major metropolitan area hospitals, but many rural areas in that state are not equipped with the program. To properly care for these patients and collect and protect evidence appropriately, Texas has mandated education for emergency department nurses not served by SANE personnel.
It is imperative that emergency department nurses become educated on the use of SAEK kits for evidence collection and chain of custody protocols. The utilization of the SANE method allows for standardized care that is safe, and protective of the patient and their rights.

Self Quiz
Ask yourself...
- Before reading this course, how much did you know about SANE or forensic nursing?
- What legal changes might help reduce the number of sexual assault cases nationally and in Texas?
- What societal changes might contribute to a reduction in child and elderly sexual assault cases?
- In your opinion, what is the most important intervention in the care of patients who have been sexually assaulted?
- How might nurses prepare for the emotional toil of encountering child sexual assault cases?
- What was the most memorable part of this course?
- How might this course change your practice moving forward?
Nurse Advocacy: Elder Abuse
Introduction
The term “advocate” refers to an individual that supports and promotes the interests of another person (1). As nurse advocates, we protect our patients against incompetency while safeguarding their wellbeing (2). As a nurse advocate in a suspected elder abuse situation, we are obligated, by law, to identify, report, and protect individuals experiencing elder abuse. As trusted members of the healthcare team, we are often the first interaction with a patient (and their family). Therefore, we are in a pivotal position to assess a situation for suspected abuse and neglect, while assuring patient safety, appropriate treatment, and improved outcomes.
Statistically, it is believed that approximately one in 10 Americans over the age of 60 years has experienced some type of elder abuse (3). As our aging population continues to grow, the likelihood of increased rates of elder abuse is a national concern. Nurse professionals often interact with the aging community and must be educated on the many aspects of caring for a person in a suspected abuse situation.

Self-Quiz
Ask Yourself...
- As a nurse, have you ever taken care of a suspected elder abuse case? What were some initial patient examination findings that raised the level of suspicion for abuse?
- With regard to caring for your suspected elder abuse victim, what were your observations as to the mental status of the alleged victim? Were they fearful and hesitant to discuss the situation, or did they welcome your inquiry?
Statistics
The aging population is facing many challenges related to finances, health and well-being, and safe secure housing options. In 2023, Senior List, a site dedicated to researching senior related products and services, reported some alarming statistics regarding the occurrence of elder abuse on a worldwide scale.
From financial fraud to nonfatal assaults and exploitation, it is estimated that “one in 10 older adults will experience some form of elder abuse, and many endure multiple types of abuse simultaneously” (4). The World Health Organization estimates that “320 million seniors will suffer from some form of elder abuse by the year 2050” (4).
According to a 2019 report by the Office of Inspector General, “1 in 5 emergency room visits among nursing home residents was attributed to abuse or neglect” (5). As the world population of elder persons continues to grow, the occurrence of elder abuse may also continue to grow, due to mental and physical decline, challenges with limited incomes, growing healthcare costs, and lack of appropriate age-related resources and support systems.

Self-Quiz
Ask Yourself...
- What types of financial challenges are elderly persons facing today? Have these challenges changed over the past few decades?
- What types of challenges are the elder population facing with respect to healthcare coverage?
Types of Elder Abuse
According to the World Health Organization, there are many types of elder abuse. In 2022, it was estimated that approximately one out of every six adults over the age of 60 had been subjected to some form of abuse in the prior calendar year (6). While rates are higher in institutions such as nursing homes and related long term care facilities, many forms of elder abuse occur in the home setting (6). The following list highlights various types of elder abuse. Any intentional act (or lack of appropriate action) that results in harm or distress to an older person is considered abuse.
Psychological Abuse
Psychological abuse is any action (or even the threat of action) that causes fear of violence or humiliation, a feeling of hopelessness, or isolation. This abuse may manifest itself as threats, verbal abuse, and intimidation tactics.
Physical Abuse
Physical abuse is any action that causes physical harm or injury to an elder person. This abuse may present itself as unexplained cuts, bruises, and broken bones.
Financial Abuse / Financial Exploitation
Financial abuse/exploitation is any action taken against an elder person’s money, belongings, or financial related documents. Financial exploitation can include unauthorized removal of money from bank accounts, fraudulent transfer of funds, unauthorized use of one’s savings and property, and internet scamming.
Sexual Abuse
Sexual abuse is any kind of sexual contact that occurs without the person’s consent. This abuse may present as unexplained sexually transmitted infections, torn or bloodied undergarments, difficulty walking, bruising on genitalia or inner thighs, and possible internal injuries.
Neglect
Neglect is a unique form of elder abuse, in that the abuse occurs from the lack of doing something (omitting care) versus the actual infliction of injury. Forms of neglect may include withholding medications and necessary medical treatment, withholding basic food and fluid requirements, and not seeking appropriate medical care for the elderly person when indicated. Victims of neglect may often present with dehydration, in under medicated (subtherapeutic) states, and often lacking basic hygiene care (dirty, soiled diapers or undergarments, disheveled appearance, malnourished).
Other Abuse Signs/Symptoms
Other signs and symptoms that may indicate elder abuse can include unintentional weight loss, a noted withdrawal from family and friends, unusual financial transactions, and a lack of basic medical needs such as routine medications and assistive devices (glasses, hearing aids, dentures). Further explanation is needed in these situations, as (the perception of) abuse and neglect may actually be the result of extenuating circumstances unrelated to actual abuse.


Self-Quiz
Ask Yourself...
- Psychological abuse may manifest itself as a feeling of hopelessness in an elder person. What other mental health issues may also heighten the risk of feelings of hopelessness?
- What do you think are some ways an alleged (elder abuse) perpetrator may psychologically abuse their victim?
- Have you ever taken care of a patient suffering from suspected neglect? What signs and symptoms did you observe?
- What are some reasons that a primary caregiver may appear to withhold an elder person’s routine medication?
- Unintentional weight loss in an elder person may indicate neglect. What other assessments should be done regarding such weight loss?
Risk Factors and Protective Factors
There are certain individual characteristics that put an elder person at risk for abuse. Persons with poor physical and mental health often do not have the ability to seek appropriate care within their community. Additionally, those who suffer from forms of cognitive impairment or physical disability may inadvertently place themselves in vulnerable situations.
Finally, those with low income and lack of a support system, especially those living alone, are at higher risk of becoming victims. Protective factors place an elder person at a lower risk for abuse. These include good health, financial stability, appropriate physical activity/physical ability, and a strong social support system. The important thing to remember is that elder abuse can occur across all cultures, races/ethnicities, and socioeconomic levels. There are no single identifiers that confirm or exclude an elder person from possible abuse.
Conversely, alleged perpetrators of elder abuse may suffer from issues that increase the risk of abuse to an elder person. Untreated medical and mental health issues such as mental illness, illegal substance abuse, and financial instability may all heighten the risk of abuse. Alleged abusers may be male or female, and in “almost 60% of elder abuse and neglect incidents,” the perpetrator is a family member” (7). “Two thirds of perpetrators are adult children or spouses,” who thus have had the opportunity to be well versed in knowing the victims physical and/or mental vulnerabilities (7).
Additionally, alleged perpetrators of elder abuse often have no other means of support, aside from the victim’s social security checks, personal savings, and housing (8). Many have a prior criminal record, suffer from mental illness or disabilities themselves, and frequently have a history of drug and alcohol abuse (8).

Self-Quiz
Ask Yourself...
- You suspect that an alleged elder abuse perpetrator is suffering from mental illness. What are your obligations to the suspected victim, in terms of their safety and well-being?
- How would you explain to the suspected victim that you must report your concerns to the local authorities? Consider your understanding of the term, “mandated reporter” as a licensed healthcare professional.
- How is the reporting of suspected abuse different (in your place of employment) for elder persons residing at home versus a long-term care facility?
- Why do you think that the majority of elder abuse perpetrators are immediate family members?
Prevention
The prevention of elder abuse is multifaceted. There is no single answer/action that prevents abuse in this vulnerable population. However, there are guidelines in place to maximize an elder person’s safety and well-being. The overall goal of elder abuse prevention is to lower the risk factors associated with heightening the occurrence of abuse. As nurses, we are in a pivotal position to advocate for the elder patient, as well as identify potential resources to benefit both patient and family (9).
The “accusation” of suspected abuse will most likely be ill-received. Caregivers, family members and others close to the elder person may feel threatened, defensive, and angry when a healthcare professional discusses their concerns over what appears to be suspected elder abuse.
The suspected victim may also feel humiliated, embarrassed, and fearful of law enforcement involvement. The suspected victim has most likely been abused by someone who has violated their trust and taken advantage of them. Therefore, it is possible that many victims of abuse are fearful of further retaliation, especially if the alleged perpetrator is an immediate family member.
When possible, the members of the healthcare team should interview caregivers and all suspected abusers separately from the alleged victim. Sometimes, subtle discrepancies between the suspected abuser and the victim interview may give unique insights worthy of further investigation.
Consider the following scenario. An elderly patient arrives via ambulance, from her private home, and appears malnourished, incontinent, and confused. As you document your findings, a team member voices concerns over suspected abuse. You are told the patient lives with an immediate family member. Initial calls are made to alert authorities of a possible elder abuse situation. The family member arrives, and states they are the patient’s primary caregiver.
- The primary caregiver is the 19-year-old granddaughter. What are your initial concerns over what appears to be neglect?
- The primary caregiver is the 78-year-old husband, appearing frail, walking with a cane, obviously undernourished. Do your concerns change?
- The primary caregiver is a 45-year-old son, unemployed, avoiding eye contact, appearing disheveled. Any additional concerns?
The nurse advocate must remain objective, nonjudgmental, and empathetic while investigating the situation. What initially appears as intentional abuse and neglect may also be due to the fact that many caregivers are also overwhelmed by the complexity of the situation, whether it be lack of knowledge, financial insecurity or mental/physical disabilities themselves.
The goal of nurse advocacy in these challenging situations is to fully assess not only the health and well-being of the elder, but that of the caregiver. All related documentation on a suspected abuse case must remain objective, reflecting only actual statements made by the patient and accompanying caregiver/ family member, as well as physical examination findings.
For guidance on medical record documentation when elder abuse is suspected, visit Documenting in the Medical Record by Stanford Medicine. ***Always check with your current worksite for site specific protocols/guidelines regarding approved documentation standards.
The current elder population is growing rapidly. By 2030, one in six people in the world will be aged 60 years or over. At this time the share of the population aged 60 years and over will increase from one billion in 2020 to 1.4 billion.
Common age-related health conditions occur often leading to complex medical issues at a time when finances, family/community support, safe housing options, and available resources may be in limited supply (10). Over time, the once healthy vibrant elder person can become frail, malnourished, depressed and isolated. This is the pivotal point in which many nurses first cross paths with the elder person.
A multidisciplinary team approach may be needed to address the various physical, mental and emotional needs of a vulnerable elder, dependent on the current health status, physical needs, and financial means. Team goals should include efforts to return the elder person to an environment best suited to support healthy eating, physical activity, a safe and affordable living environment, accessible transportation, and a supportive community.
Depending on the health status of the individual, the goal can vary the spectrum, from independent living to nursing home placement. Again, these efforts are best addressed by a multidisciplinary team approach.
In the acute phase, when elder abuse is suspected (or confirmed), the safety of the victim is the highest priority. As nurses, we are mandated to report all suspected abuse, including that of vulnerable adults. Your specific workplace should have written protocols regarding the reporting of suspected abuse, as well as guidelines of documentation of the suspected abuse.
Failure to do so may result in a variety of penalties, including but not limited to fines as well as criminal charges (ranging from misdemeanor to felony charges). It is imperative that you, as a licensed professional, become familiar with your state’s mandatory reporting laws (11).

Self-Quiz
Ask Yourself...
- Reflect on your current worksite. What community resources are available to assist with patient safe housing in suspected abuse cases?
- What members of your worksite multidisciplinary team can assist you with cases of suspected elder abuse?
- Do you feel comfortable in the role of nurse advocate? If not, what recommendations could you make to your organization to improve staff education in this area?
Reporting
As stated previously, a nurse’s workplace should have written protocols in place to report suspected elder abuse. The majority of states also have written guidelines in place for reporting suspected abuse. The United States Department of Health and Human Services also offers guidelines for all persons in the reporting of such abuse.
If the person is in immediate or life-threatening danger, the local authorities should be notified through 9-1-1. In the event that abuse is suspected, but there is no immediate threat to life or limb, the recommendation is to notify the local adult protective services (APS) or police department (12).


Self-Quiz
Ask Yourself...
- As a nurse professional, how can you advocate for the elder person / aging population outside of your worksite environment?
- As life expectancy rates continue to climb, what areas can healthcare professionals improve on with respect to elder patient care (assessment, documentation guidelines, treatment protocols)?
- Do you, as a nurse advocate, feel that there are any barriers to elder patient care that need to be addressed at your worksite? What outside agencies are available to assist you?
End of Life Considerations
According to the position statement on end of life care from the American Nurses’ Association, nurses “are often ideally positioned to contribute to conversations about end of life care and decisions, including maintaining a focus on patients’ preferences, and to establish mechanisms to respect the patient’s autonomy” (13). Similarly, a statement entitled “The Right to Self Determination” from the Code of Ethics for Nurses with Interpretive Statements also emphasizes the nurse’s role in end of life planning and care:
“The importance of carefully considered decisions regarding resuscitation status, withholding and with-drawing life-sustaining therapies, forgoing nutrition and hydration, palliative care, and advance directives is widely recognized. Nurses assist patients as necessary with these decisions. Nurses should promote advance care planning conversations and must be knowledgeable about the benefits and limits of various advance directive documents. The nurse should provide interventions to relieve pain and other symptoms in the dying process consistent with palliative care standards and may not act with the sole intent of ending a patient’s life” (13).
What these statements say is that nurses have ethical roles and responsibilities that are fundamental to nursing practice. Nurses should ensure that both patients and family members understand the options and treatments that have been presented to them, and should ensure that the patient’s autonomy is being respected throughout all aspects of their care. Nurses are first and foremost patient advocates, and this is especially crucial during the end of life stage. Nurse advocacy during this time can encompass anything from symptom and pain management, culturally sensitive care provision, and ethical decision making (14).
Talking to Patients and Families
Talking to a patient and their family about end of life care can be a huge challenge for nurses. In addition to managing patients’ and families’ emotions, nurses must manage their own emotions and approach the subject with professionalism as well as empathy.
Often, during the end of life planning phase, patients will go through the five stages of grief, as outlined in the book “On Death and Dying” by Elizabeth Kubler-Ross. The five stages of grief include (14):
Denial: Usually a temporary defense, patients may say that they’re fine, or that this is some mistake.
Anger: Once the patient is no longer in denial, anger is often the next stage. It may be difficult to care for the patient during this stage, as they may misplace their angry feelings on their caregivers.
Bargaining: At this stage, the patient seeks ways to postpone death – often in the form of promising to reform a lifestyle in exchange for more life.
Depression: This stage may involve the refusal of treatments or visitors, and the disconnection from people, love, and affection.
Acceptance: The final stage, which is not reached by all patients. In this stage, the patient has come to terms with their mortality and has accepted that death will happen.
It is important for the nurse to understand these five stages, as most patients will be experiencing one or more of the stages during the end of life process.
Here are some helpful techniques for nurses to use when talking to patients about hospice or end of life planning, according to the American Academy of Family Physicians (15):
Make sure you have time.
While this may seem impossible while on a shift when you have other patients, it’s imperative that a nurse allow enough time to have this difficult conversation. This is not a conversation that can be rushed – rushing through the conversation may make a nurse miss important details that the patient has shared.
Turn off your phone.
Minimizing distractions during these difficult conversations will ensure that the nurse can get ample information from this patient and family interaction.
Listen to the patient.
Above all, listen to what the patient is saying. Begin the conversation by asking what the patient and their doctor have already discussed. Be sure that the plan of care has been reviewed with the doctor prior to this conversation, then have the patient repeat their plan of care as they understand it. If there are major differences in the plan of care and what the patient says, this may warrant further conversation with the health care team to clarify and identify knowledge gaps.
Learn what the patient’s goals are.
Active listening is crucial during the conversation phase of end of life care planning. Once the nurse has determined that the patient understands the options that have been presented, it is vital to ask them what their goals are for palliative and comfort care. Understanding a patient’s goals can help identify what resources will be best suited for their individual needs.
Conversations surrounding end of life care should happen as soon as possible. Do not wait until the patient is no longer able to participate in the discussion. Encourage the presence of family members, but be sure to respect the patient’s wishes regarding who is involved in the planning process. Other members of the healthcare team that should be included in the planning process include social workers, patient navigators (if applicable in that setting), and any primary and specialist physicians involved in the patient’s care.

Self-Quiz
Ask Yourself...
- How important do you think nurses are to the decision-making process for end of life care?
- Why is it important to include the patient and family in conversations about end-of-life care?
- What are some ways in which abuse can occur during the end of life stage?
- If you were a hospice nurse and suspected elder abuse, to whom should you report this?
Additional Resources
The Elder Abuse Guide for Law Enforcement (EAGLE)
Use this website to review state-specific elder justice laws.
https://eagle.usc.edu/state-specific-laws/
National Adult Protective Services Association
Use this website to find specific contact information for your state location
https://www.napsa-now.org/help-in-your-area
ElderCare Locator/ United States Administration on Aging
Use this website to connect with services for older adults and families.
https://eldercare.acl.gov/Public/Index.aspx
World Elder Abuse Awareness Day
June 15th has been declared World Elder Abuse Awareness Day (WEAAD). For more information, visit https://eldermistreatment.usc.edu/weaad-home/. The website offers multi-language downloads on elder abuse facts, as well as social media guides, awareness campaigns, elder justice groups, and associated tool kits.
Conclusion
As the elder population continues to grow, so does the risk of elder abuse. As nurse professionals, we must continue to advocate for the safety and well-being of our aging population. We must continue to stay informed and educated on identifying abuse throughout the age spectrum.
Lastly, we must be knowledgeable of our own available resources to best assist the elder population and their basic needs, including food and shelter, access to healthcare, and transportation, as well as community wide support services.
Texas Tick-Borne Diseases
Introduction
Ticks are more than just a bothersome pest; they are carriers of debilitating diseases. Tickborne diseases are unfortunately increasing in incidence. Clinicians should expect tickborne disease in patients presenting with flu-like symptoms during the spring and summer months. This is especially true in regions with rich biodiversity like Texas.
We will review the most common types of ticks and the diseases they carry. These diseases, while potentially severe, are treatable, especially when caught early. The course will review symptoms, stages, and the epidemiology of tick-borne diseases.
It is meaningful to explore the diagnostic tests and treatment protocols for tick-borne illnesses, including the use of antibiotics and supportive care measures. Prompt diagnosis and treatment can prevent complications and death.
We will closely examine the pharmacokinetics of each medication used to treat the diseases, including the uses, mechanism of action, side effects, and contraindications. Counseling patients on preventative measures for protective clothing and tick repellents during outdoor activities can help minimize the risk of infection.
Introduction to Ticks
Ticks found in Texas encompass a variety of species, each with their unique characteristics and disease implications. Ticks are most active in the warmer months of spring and summer. The most common ticks in Texas are the Lone Star tick, American dog tick, Black-legged tick, and the Brown dog tick. These species vary in appearance, habitat preferences, and the diseases they can transmit.
Lone Star Tick
Lone Start Tick (Amblyomma Americanum): A distinct white dot or "lone star" on the female's back helps this tick to be identified easily. It is found throughout Texas, especially in wooded, bushy areas. Lone star ticks are known for transmitting diseases such as Ehrlichiosis and Southern Tick-Associated Rash Illness (STARI). In addition to their competence for pathogen transmission, Amblyomma Americanum (A. Americanum) has recently been associated with delayed red meat allergy (7).
American Dog Tick
American Dog Tick (Dermacentor variabilis): This tick prefers grassy areas with little to no tree cover. It primarily targets dogs but will bite humans and can transmit Rocky Mountain spotted fever and Tularemia.
Black-legged Tick
Black-legged Tick (Ixodes scapularis): This tick is also called the deer tick. It is prevalent in the eastern and northern parts of Texas. This tick is known for transmitting Lyme disease, Anaplasmosis, and Babesiosis to humans. The black-legged tick prefers wooded and brushy habitats.
Brown Dog Tick
Brown Dog Tick (Rhipicephalus sanguineus): Unlike other ticks, the brown dog tick is more adapted to dryer environments and can live and reproduce indoors.
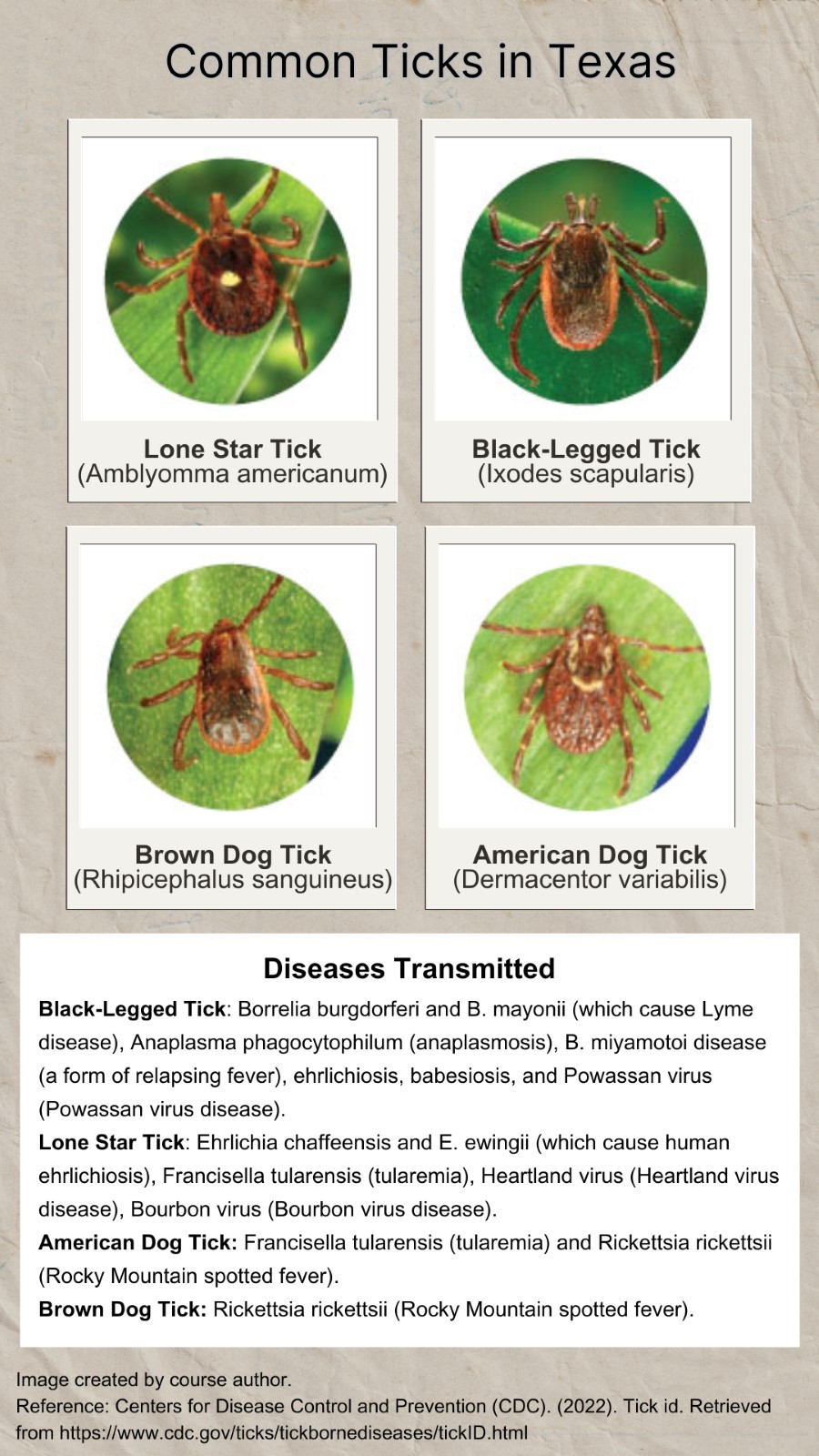
Image 1. Common Ticks in Texas (3)

Self Quiz
Ask yourself...
- Can you name the most common ticks found in Texas?
- Do you notice defining features among each tick mentioned above?
- Can you discuss the diseases that each tick transmits?
- What seasons are ticks most active?
- What training have you had regarding ticks at your facility?
- Do you feel that you have seen an increase or decrease in tick-related bites?
- What is a lone star tick?
- What is an American dog tick?
- What is a black legged tick?
- Define a brown dog tick.
Tick-Borne Diseases in Texas
Ticks are vectors for a wide array of bacterial, protozoan, and viral pathogens causing such diseases as Lyme borreliosis, spotted fever rickettsioses, anaplasmosis, tularemia, ehrlichiosis, babesiosis, and the recently emerging viruses: Heartland (HRTV), Powassan (POWV) and Bourbon (BRBV).
These vectors are found in many geographic areas of Texas and unfortunately have a steady increase in presence. Cases of tick-borne diseases have more than doubled in the last decade in the United States and territories, and account for 77% of all vector-borne disease reports (7).
Lyme Disease
Lyme disease (LD) is caused by the bacterium Borrelia burgdorferi and rarely, Borrelia mayonii. It is transmitted to humans through the bite of infected black-legged ticks. Lyme disease is the most frequently diagnosed tick-borne illness in the United States, however, it oddly has a low incidence in the state of Texas.
The incubation period is 3–30 days (5). Research shows the probability of host infection gradually increases as tick attachment continues, reaching 70% after 72 hours of attachment and a greater than 90% probability of infection after a complete tick blood meal (13).
Clinically, B. mayonii-infected patients show higher loads of spirochetes in the blood, and some have had focal or diffuse rash, or developed neurological symptoms.
There is significant research that explores and combats this bacterium’s ability to avoid immune detection and response. Similar to other blood-borne pathogens, LD spirochetes have developed multiple strategies to overcome innate immunity, thereby avoiding clearance by the immune system of the host by ways such as changing their surface composition (13). This action makes it difficult for the immune system to create antibodies against it.
Early clinical signs and symptoms (3 to 30 days after a tick bite) include (5):
- Erythema migrans (EM)— This is a worrisome “target” or “bull’s-eye” rash. It is a red annular or homogeneous rash at the site of a tick bite. The rash typically expands slowly over several days and may feel warm to the touch (5). EM occurs in 70–80% of infected individuals (5) [See image 2].
- Headache
- Fever
- Chills
- Malaise or fatigue, myalgia, arthralgia § Lymphadenopathy
Lyme disease that is not treated will progress to disseminated disease for about 60% of patients with varied manifestations (5) Rheumatologic signs and symptoms are particularly delayed and can cause severe damage to the joints, heart, and nervous system (5).
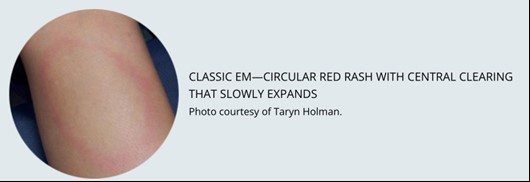
Image 2. Class Erythemia migrans rash (5)
Anaplasmosis and Ehrlichiosis
Anaplasmosis, known as human granulocytic anaplasmosis (HGA), is a disease caused by the bacterium Anaplasma phagocytophilum (A. Phagocytophilum). These bacteria are spread to people by tick bites primarily from the black-legged tick (Ixodes scapularis) and the western black-legged tick (Ixodes pacificus). The first case of human anaplasmosis was described in 1990 when a patient in Wisconsin developed a severe febrile illness following a tick bite and died two weeks later (6).
Anaplasma organisms are small, gram-negative, and intracellular. A. phagocytophilum targets neutrophils, alters their function in the host, and forms morulae within vacuoles. The majority of damage it causes is thought to be related to host inflammatory processes. Since Ixodes ticks are also carriers for Lyme disease, babesiosis, and tick-borne encephalitis, coinfection with multiple diseases can and does occur in humans.
Ehrlichiosis, known as Human Monocytic Ehrlichiosis (HME), is similar to anaplasmosis in molecular structure but is less commonly found than anaplasmosis.
The median age of patients with anaplasmosis and ehrlichiosis is around 50 years old (6).
Doxycycline is the drug of choice for adults and children of all ages with anaplasmosis (5).
Clinical signs and symptoms of anaplasmosis and ehrlichiosis are non-specific and typically include:
- Fever
- Headache
- Muscle aches
- Fatigue
Spotted Fever Group Rickettsioses
Spotted fever group rickettsioses (spotted fevers) are a group of diseases caused by similarly structured bacteria. Rocky Mountain Spotted Fever is within this group of diseases and is considered the most serious and most commonly reported spotted fever group rickettsiosis in the United States (5). These bacteria are spread to people through the bite of infected mites and ticks. The ticks responsible are typically the American dog ticks (Dermacentor variabilis), Rocky Mountain wood tick (Dermacentor andersoni), and the brown dog ticks (Rhipicephalus sanguineus) (5).
Spotted fevers have a wide range of signs and symptoms, including (5):
- Eschar - dark scab at the site of the tick bite
- Fever
- Headache
- Rash
Doxycycline is the treatment of choice for all spotted fever infections (5).
Tick-borne Relapsing Fever
Tick-borne relapsing fever (TBRF) is an infection caused by certain species of Borrelia bacteria. Relapsing fever Borrelia infections are categorized into three main groups based on the vector that transmits the bacteria: soft ticks, hard ticks, and body lice. These diseases differ in their epidemiology and severity.
TBRF is uniquely caused by soft ticks, instead of hard ticks (like the other diseases). Soft ticks are generally found in animal burrows, dens, caves, or human dwellings such as huts, cabins, or sheds. The disease is often linked to someone recently sleeping in a rustic cabin in the mountains. Soft ticks have a wrinkled body appearance and do not latch as long as hard ticks (5).
The main symptoms of TBRF are:
- High fever (e.g., 103° F)
- Headache
- Muscle and joint aches.
The fever comes in a unique pattern of lasting roughly 2-7 days, followed by 4-14 days without fever, followed by another 3 days of fever. Without antibiotic treatment, this process can repeat several times.
Babesiosis
Babesiosis is an emerging tick-borne disease caused by parasites of the genus Babesia (9). This disease has increasing incidence worldwide and a risk of human-to-human transmission through blood transfusion.
The majority of those infected by babesiosis remain asymptomatic or present with mild flu-like symptoms (9). However, in susceptible populations, such as the elderly or immunocompromised individuals, symptoms can include severe anemia, acute respiratory distress, organ failure, and death (9).
Tularemia
Tularemia is caused by infection with the bacteria Francisella tularensis. Transmission routes include tick bite, deer fly bite, inhalation, ingestion, and skin contact with infected animals (4). Signs and symptoms of tularemia can vary widely depending on the route of exposure and subtype of F. tularensis. Tularemia can become serious or fatal without adequate treatment.
Possible signs and symptoms include (4):
- Fever, chills
- Headache
- Malaise, fatigue
- Anorexia
- Myalgia
- Chest discomfort
- Non-productive cough
- Sore throat
- Vomiting, diarrhea
- Abdominal pain
- Localized or regional lymphadenopathy
- Cutaneous ulcer at the site of bite/infection
- Photophobia
- Vision impairment/loss
- Conjunctivitis
General laboratory findings:
- Hyponatremia
- Leukocytosis
- Thrombocytopenia
- Elevated hepatic transaminases
- Elevated creatine kinase
- Elevated erythrocyte sedimentation rate
- Myoglobinuria
- Sterile pyuria
Viral Pathogens: Heartland (HRTV), Powassan (POWV) and Bourbon (BRBV)
Arboviral disease is a broad term used to describe infections caused by a group of viruses spread by the bite of infected arthropods (insects) such as mosquitoes and ticks (15). These include Heartland (HRTV), Powassan (POWV) and Bourbon (BRBV). Other diseases spread by the bite of an infected tick are bacterial infections and babesiosis (a parasitic infection), which are not arboviruses. It is important to note that if a highly suspected infected individual (positive for symptoms and tick bite) does not have improvement of symptoms following an antibiotic regimen, a viral pathogen from a tick may be the culprit.

Self Quiz
Ask yourself...
- How does the length of time an infected tick is attached correlate with the probability of acquiring Lyme disease?
- What is the most common sign of Lyme disease?
- Which ticks transmit anaplasmosis and ehrlichiosis?
- Can you describe the presentation of patients infected with Rickettsioses or tularemia?
- What bacteria are known to cause Lyme disease?
- What is erythema migrans?
- What are three signs of Anaplasmosis and Ehrlichiosis?
- What are the symptoms of tick-borne relapsing fever?
- What is babesiosis?
- What viral infections are linked to ticks?
Removal of Ticks
Imagine you are evaluating a patient who has not removed a tick attached to their skin. It is imperative that you quickly, yet appropriately, remove it manually (unless your facility has another method). There are other commercially available tick-removal devices, but there are currently no substantial studies that have evaluated their usefulness.
The Centers for Disease Control and Prevention (CDC) provides the following steps as a guide on how to manually remove a tick:
- Apply gloves and clean the area well.
- Use blunt forceps (tweezers). Do not use sharp forceps.
- Grasp the tick as close to the skin’s surface as possible, and pull upward with steady, even pressure.
- Do not squeeze or puncture the tick’s body.
- Do not twist or jerk the tick (this can cause the mouth-parts to break off and remain in the skin)
- If you notice the mouth-parts remain on the skin after removal, grasp and pull with tweezers.
- After removing the tick, thoroughly clean the bite with an antiseptic solution.

Self Quiz
Ask yourself...
- When removing a tick, why is it important to get as close to the skin’s surface as possible?
- Why do you think it’s recommended to avoid squeezing or puncturing the tick’s body?
- What types of forceps should you use when removing a tick?
- What should you clean the skin with after the removal of a tick?
- Have you ever had to remove a tick? What was your experience like?
Medications Used to Treat Tick-Borne Diseases
The treatment of tick-borne diseases often involves antibiotics, with the choice of medication depending on the specific disease diagnosed. It would be helpful to consult an infectious disease specialist about individual patient treatment plans as the specific duration of treatment can vary based on each disease, the severity of symptoms, and individual patient traits.
Here's a brief overview of treatments for some of the most common tick-borne diseases:
Lyme Disease
The first-line treatment for Lyme disease is typically oral antibiotics, with doxycycline, amoxicillin, and cefuroxime axetil being the most commonly prescribed. In cases of more severe Lyme disease, intravenous antibiotics, such as ceftriaxone, may be used. Depending on a person’s age, medical history, underlying health conditions, pregnancy status, or allergies, these regimens may need to be adjusted. The table below outlines treatment regimens for the erythema migrans rash, which is the most common manifestation of early Lyme disease.

Table 1. Treatment Regimen for Erythema Migrans Rash (5)
Rocky Mountain Spotted Fever (RMSF)
Doxycycline is the treatment of choice for RMSF for both adults and children. Early treatment is critical to prevent severe disease complications.
Ehrlichiosis and Anaplasmosis
Doxycycline is also the preferred treatment for both ehrlichiosis and anaplasmosis, regardless of the patient's age.
Southern Tick-Associated Rash Illness (STARI)
Although the cause of STARI is not well understood, doxycycline may be used to treat the rash and possible infection, similar to the treatment for Lyme disease.
Babesiosis
This disease is typically treated with a combination of atovaquone and azithromycin. In more severe cases, clindamycin and quinine may be used instead.
Tularemia
Treatment can include several different antibiotics, such as gentamicin, streptomycin, doxycycline, or ciprofloxacin (4). The table below outlines treatment regimens for Tularemia.
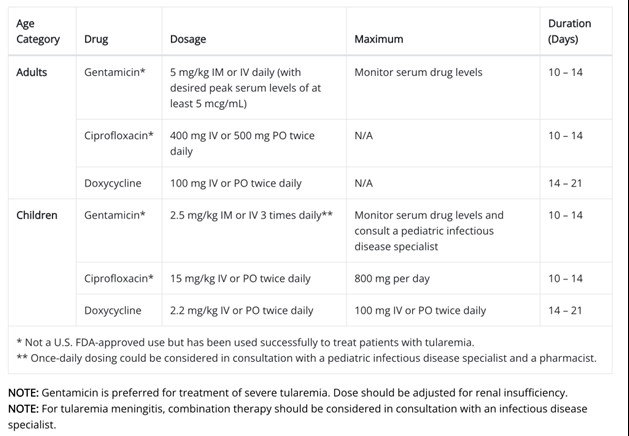
Table 2. Treatment Regimen for Tularemia (4)

Self Quiz
Ask yourself...
- Can you name the various factors to consider when prescribing treatment for a tick-borne disease?
- Why is it important to get a thorough medical history before prescribing antibiotics?
- Do you have experience with intravenous antibiotic administration?
- What are some patient education topics on these diseases and why treatment is necessary?
- What education should you provide to patients being started on doxycycline?
- What education should you provide to patients being started on amoxicillin?
- What education should you provide to patients being started on cefuroxime?
- What is the medication of choice to treat Rocky Mountain spotted fever?
- What is the treatment regimen for tularemia?
- What is the treatment regimen for babesiosis?
Antibiotics that Inhibit Protein Synthesis
When treatment is initiated for patients with tick-borne diseases, the prescriber needs to understand the pharmacokinetics of antibiotics that inhibit protein synthesis and biochemistry. Examples of these antibiotics include tetracyclines, chloramphenicol, macrolides, lincosamides, streptogramins, oxazolidinones, mupirocins, and peptide deformylase inhibitors (1). Knowledge of the mechanisms of action of antibiotics in interfering with the life cycle of these bacteria is critical in evaluating patient outcomes.
Protein synthesis is an essential process in all cells, including bacterial cells. The ribosome performs protein synthesis by translating the genetic information encoded in messenger RNAs (mRNAs) into proteins. The bacterial ribosome is composed of three RNA chains (16S, 23S, and 5S) and more than 50 proteins assembled into two individual subunits. These include the small 30S and large 50S subunits, which join together to form the 70S ribosome. To proceed efficiently and translate the information, many protein factors need to interact sequentially with the ribosome.
Keep this process in mind as we discuss antibiotic drugs in effectively treating tick-borne diseases.
Doxycycline
Pharmacologic Category
Antibiotic, Tetracycline Derivative
Uses: Labeled Indications
- Acne
- Actinomycosis
- Acute intestinal amebiasis
- Clostridium: Treatment of infections caused by Clostridium spp. when penicillin is contraindicated.
- Ehrlichiosis and Anaplasmosis
- Gram-negative infections: Treatment of infections caused by Escherichia coli, Enterobacter aerogenes, Shigella spp., Acinetobacter spp., Klebsiella spp. (respiratory and urinary infections), and Bacteroides spp.; Neisseria meningitidis (when penicillin is contraindicated).
- Gram-positive infections: Treatment of infections caused by Streptococcus spp., when susceptible.
- Listeriosis
- Malaria prophylaxis
- Mycoplasma pneumoniae: Treatment of infections caused by Mycoplasma pneumoniae.
- Ophthalmic infections
- Periodontitis
- Relapsing fever: Treatment of relapsing fever caused by Borrelia recurrentis.
- Respiratory tract infections
- Rickettsial infections: Treatment of Rocky Mountain spotted fever, rickettsialpox, and tick fevers caused by Rickettsiae.
- Sexually transmitted infections
- Infections caused by Staphylococcus aureus (doxycycline is not the drug of choice in the treatment of any type of staphylococcal infection).
Mechanism of Action
All tetracyclines have the same mechanism of action to block the protein synthesis of bacteria.
Tetracyclines inhibit protein synthesis by binding to the 30S subunit of the ribosome (1). Essentially, the drug inhibits the binding of amino-acyl tRNA to the A-site of the ribosome. The 7S ribosomal protein is part of the binding site. Tigecycline also binds at the A-site of the 30S subunit of the ribosome and inhibits bacterial protein synthesis.
Tetracyclines can bind equally well to both prokaryotic (70S) and eukaryotic (80S) ribosomes. Eukaryotic cells are not affected by the antibiotic because they do not accumulate tetracycline in the cell. This makes tetracyclines selective against bacteria. Tetracyclines may also cause alterations in the cytoplasmic membrane (1).
Pharmacodynamics
Absorption: (Oral) Almost completely absorbed from the gastrointestinal tract (GI) tract; average peak plasma concentration may be reduced by high-fat meal or milk (16).
Distribution: Widely distributed into body tissues and fluids including synovial, pleural, prostatic, seminal fluids, and bronchial secretions. Saliva and cerebral spinal fluid (CSF) penetration is poor.
Protein binding: >90%
Bioavailability: Reduced at high pH; may be clinically significant in patients with gastrectomy, gastric bypass surgery, or who are otherwise deemed achlorhydric.
Metabolism and Excretion: Not hepatic; partially inactivated in the GI tract by chelate formation. 20-40% excreted unchanged in the urine; some inactivation in the intestines and enterohepatic circulation with excretion in bile and feces.
Half-life: 14-17 hours (longer time frame in severe renal impairment)

Figure 1. Pharmacodynamics of Doxycycline
Adverse Effects
1% to 10% has reported the following (16):
- Cardiovascular: Hypertension (3%)
- Central nervous system: Anxiety (2%), pain (2%)
- Endocrine & metabolic: Increased lactate dehydrogenase (2%), increased serum glucose (1%)
- Gastrointestinal: Diarrhea (5%), upper abdominal pain (2%), abdominal distention (1%), abdominal pain (1%), xerostomia (1%)
- Hepatic: Increased serum aspartate aminotransferase (2%)
- Infection: Fungal infection (2%), influenza (2%)
- Neuromuscular & skeletal: Back pain (1%)
- Respiratory: Nasopharyngitis (5%), sinusitis (3%), nasal congestion (2%)
Contraindications/Precautions
Hypersensitivity to doxycycline, other tetracyclines, or any component of the formulation. Contraindicated in infants and children younger than eight years of age, during the second or third trimester of pregnancy, and breastfeeding (16).
Patient Education
- Instruct the patient to finish the entire dose as directed, even if feeling better, and take missed doses as soon as possible unless it is almost time for the next dose.
- Advise patient to avoid taking antacids, calcium, magnesium-containing medications, sodium bicarbonate, and iron supplements within 1-3 hours of oral doxycycline.
- Caution patient to use sunscreen and protective clothing to prevent photosensitivity reactions.
- Advise patient to report signs of superinfection (black, furry overgrowth on the tongue, vaginal itching, discharge, watery or foul-smelling stools) or intracranial hypertension (headache, blurred vision, diplopia).

Self Quiz
Ask yourself...
- What are other uses for doxycycline?
- Can you describe the mechanism of action of these antibiotics that inhibit protein synthesis?
- Can you name adverse effects and patient education topics for doxycycline?
- How is doxycycline metabolized in the body?
- What is the onset of doxycycline?
- What education would you provide to patients being started on doxycycline?
- What is a contraindication to doxycycline?
- What age group should be avoided when administering doxycycline?
- What is the peak of doxycycline?
- What is the duration of doxycycline?
Aminoglycosides
Aminoglycosides include streptomycin, neomycin, kanamycin, amikacin, gentamicin, tobramycin, sisomicin, netilmicin, plazomicin, and others (2). Gentamicin and streptomycin are recommended in the treatment of tularemia, so we will closely examine this group.
ALERT: US Boxed Warning for Aminoglycosides
Toxicity (17):
As with other aminoglycosides, gentamicin is potentially nephrotoxic. The risk is greater with impaired renal function and prolonged therapy. Neurotoxicity, manifested by ototoxicity (both vestibular and auditory) can occur in patients treated with gentamicin.
Clinicians should closely monitor renal function and eighth cranial nerve function, especially in patients with reduced renal function at the onset of therapy. Assess urine for decreased specific gravity, increased excretion of protein, and the presence of cells or casts (17). Routinely check serum urea nitrogen (BUN), serum creatinine, or creatinine clearance (CrCl). Monitor serum concentrations of aminoglycosides to ensure adequate levels and to avoid potentially toxic levels.
Avoid concurrent use of other potentially neurotoxic and/or nephrotoxic drugs: cisplatin, cephaloridine, kanamycin, amikacin, neomycin, polymyxin B, colistin, paromomycin, streptomycin, tobramycin, vancomycin, and viomycin (2). Avoid the concurrent use of gentamicin with potent diuretics.
Pregnancy
Aminoglycosides can cause fetal harm when administered to a pregnant woman.
Gentamicin
Pharmacologic Category
Antibiotic, Aminoglycoside
Uses
Treatment of serious infections: Sepsis, meningitis, urinary tract infections, respiratory tract infections, peritonitis, bone infections, skin, and soft tissue infections, caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species, Escherichia coli, Klebsiella species, Enterobacter species, Serratia species, Citrobacter species (2).
Mechanism of Action
As with all aminoglycosides, gentamicin interferes with ribosomal peptide/protein synthesis (14). It binds to 16S rRNA (located on the smaller 30S component of the ribosome of the bacteria), stops its functionality, and halts ongoing protein synthesis (14). Aminoglycosides are not able to penetrate the hydrophobic bacterial cell membrane and are only active against aerobic bacteria because an electron transport system used during the cell’s respiratory cycle is needed to accomplish this (2).
Pharmacodynamics/Kinetics
Absorption: Intramuscular: Rapid and complete
Oral: Poorly absorbed
Distribution: Primarily into extracellular fluid (highly hydrophilic); high concentration in the renal cortex.
Protein binding: <30%
Half-life elimination:
- Adults: ~2 hours
- Neonates: <1 week: 3 to 11.5 hours; 1 week to 1 month: 3 to 6 hours
- Infants: 4 ± 1 hour
- Children: 2 ± 1 hour
Time to peak, serum:
- IM: 30 to 90 minutes
- IV: 30 minutes after a 30-minute infusion
Excretion: Urine
Clearance: Directly related to renal function
- Neonates: 0.045 ± 0.01 L/hour/kg
- Infants: 0.1 ± 0.05 L/hour/kg
- Children: 0.1 ± 0.03 L/hour/kg
- Adolescents: 0.09 ± 0.03 L/hour/kg
Adverse Effects
Some adverse effects include (17):
- Cardiovascular: Edema, hypertension, hypotension, phlebitis, thrombophlebitis
- Central nervous system: Abnormal gait, ataxia, brain disease, confusion, depression, dizziness, drowsiness
- Dermatologic: Alopecia, erythema, pruritus, skin rash, urticaria
- Endocrine & metabolic: Hypocalcemia, hypokalemia, hypomagnesemia, hyponatremia, weight loss
- Gastrointestinal: Anorexia, Clostridioides difficile-associated diarrhea, decreased appetite, enterocolitis, nausea, sialorrhea, stomatitis, vomiting
- Genitourinary: Casts in urine (hyaline, granular), oliguria, proteinuria
- Hematologic & oncologic: Agranulocytosis, anemia, thrombocytopenia
- Hepatic: Hepatomegaly, increased liver enzymes
- Hypersensitivity: Anaphylaxis, anaphylactoid reaction, hypersensitivity reaction
- Local: Injection site reaction, pain at injection site
- Neuromuscular & skeletal: Arthralgia, muscle cramps, muscle fatigue, weakness
- Ophthalmic: Visual disturbance
- Otic: Auditory impairment, tinnitus
- Renal: Decreased creatinine clearance, decreased urine specific gravity, increased blood urea nitrogen, increased serum creatinine, polyuria, renal failure (high trough serum concentrations), renal tubular necrosis
- Respiratory: Dyspnea, laryngeal edema, pulmonary fibrosis, respiratory depression
- Miscellaneous: Fever
Streptomycin
Pharmacologic Category
Antibiotic, Aminoglycoside
Uses
Primarily used for treating aerobic gram-negative bacterial infections, such as tularemia, brucellosis, tuberculosis (in combination with isoniazid, pyrazinamide, and rifampin), and certain cases of endocarditis when combined with beta-lactam antibiotics (14).
Mechanism of Action
Interferes with bacterial protein synthesis by binding to 30S ribosomal subunit resulting in a defective bacterial cell membrane (2). These actions inhibit the bacteria from creating the needed ongoing protein synthesis.
Pharmacodynamics/Kinetics
Absorption:
- Oral: Poorly absorbed
- IM: Well-absorbed
Distribution: Distributes into most body tissues and fluids except the brain; small amounts enter the CSF only with inflamed meninges.
Protein binding: 34%
Half-life elimination:
- Newborns: 4 to 10 hours
- Adults: 2 to 4.7 hours (prolonged with renal impairment)
Time to peak: IM: Within 1 to 2 hours
Excretion: Urine (29% to 89% as unchanged drug); a small amount (1%) excreted in bile, saliva, sweat, and tears (18)
Adverse Reactions
Adverse reactions include (18):
- Cardiovascular: Hypotension
- Central nervous system: Drug fever, facial paresthesia, headache, neurotoxicity
- Dermatologic: Exfoliative dermatitis, skin rash, urticaria
- Gastrointestinal: Nausea, vomiting
- Genitourinary: Azotemia, nephrotoxicity
- Hematologic & oncologic: Eosinophilia, hemolytic anemia, leukopenia, pancytopenia, thrombocytopenia
- Hypersensitivity: Anaphylaxis, angioedema
- Neuromuscular & skeletal: Arthralgia, tremor, weakness
- Ophthalmic: Amblyopia
- Otic: Auditory ototoxicity, vestibular ototoxicity
- Respiratory: Dyspnea

Self Quiz
Ask yourself...
- What are other uses for aminoglycosides?
- Can you describe the mechanism of action of gentamicin and streptomycin?
- Can you name the adverse effects of these drugs?
- How is gentamycin excreted from the body?
- What is the primary use of streptomycin?
- What is the primary use of amoxicillin?
- What education would you provide to a patient being started on gentamicin?
- What education would you provide to a patient being started on streptomycin?
- How is streptomycin excreted from the body?
- Which method of administration has the best absorption for streptomycin?
Compound Use of Atovaquone and Azithromycin for Babesiosis
The current arsenal for the treatment of human babesiosis includes atovaquone, azithromycin, clindamycin, and quinine. The first-line compound typically used is atovaquone and azithromycin. Atovaquone is used to treat several human diseases, including Pneumocystis jirovecii pneumonia, toxoplasmosis, and malaria. In apicomplexan parasites such as the genus Babesia, atovaquone targets the cytochrome bc1 complex of the mitochondrial electron transport chain (9). Azithromycin is a relatively broad-spectrum antibiotic indicated for the treatment of numerous bacterial infections; it is a well-characterized protein synthesis inhibitor, which in apicomplexan parasites targets the translation machinery in the apicoplast (9).

Self Quiz
Ask yourself...
- Are single or compound antibiotics currently used in the treatment of babesiosis?
- Can you describe the possible adverse effects of using multiple antibiotics?
Tick Testing
The Department of State Health Services (DSHS) and the University of North Texas Health Science Center (UNTHSC) Tick-Borne Disease Research Laboratory have teamed up to test ticks for disease agents in the Borrelia, Ehrlichia, and Rickettsia genera using molecular methods (11).
Ticks should be submitted to the DSHS Zoonosis Control office for identification after which they will be forwarded to UNTHSC for testing (11). There is no charge for testing, however, this service is available only to Texas residents submitting ticks found at a location within Texas. Only ticks that were attached to a human should be submitted (11).
For free testing of ticks found in the environment or on pets, visit the Texas Tick Project. The program is designed for tick surveillance, not disease diagnosis. If infected with a tick-borne pathogen, individuals usually develop symptoms before the test results are available.

Self Quiz
Ask yourself...
- Should ticks from the family dog be sent in for testing in this program?
- Can you describe the purpose of the testing program?
- Are you familiar with the removal and examination of ticks?
- Should a Texas resident who removed a tick while vacationing in North Carolina send this tick into the program for testing?
Prevention and Control
It is meaningful to provide teaching on prevention tips if you notice a patient is at high risk for encountering a tick outdoors. This includes patients who enjoy hobbies outdoors (such as hiking) or whose job duties involve spending a significant amount of time outdoors.
Prevention teaching:
- Always inspect yourself, family members, and pets from head to toe for ticks after spending time outdoors.
- Keep grass trimmed and remove overgrowth.
- Remove bird feeders and other food sources that attract wildlife, such as deer, that can carry ticks.
- Discuss tick and flea prevention methods with your veterinarian if you have pets.
- Move picnic tables, swing sets, and outdoor lawn furniture away from trees and shrubs.
Upcoming Research
Significant research studies are being conducted on the treatment and prevention of tick-borne diseases, however, there is a need for prevention of the spread of tick bites. One interesting study is exploring the prevalence of common tick-borne pathogens in white-tailed deer and coyotes in south Texas (19). Identifying vehicles (various wildlife) that carry these tiny ticks over long distances can help researchers treat wildlife for ticks and ultimately slow the spread. Upcoming research relies on effective collaboration between medical professionals, wildlife and ecological professionals, researchers, and policymakers.
The current evidence on babesiosis is not comprehensive and treatment consists of combinations of atovaquone and azithromycin or clindamycin and quinine (9). These drug compounds are associated with mild or severe adverse events and a rapid emergence of drug resistance, thus highlighting the need for new treatment therapies to combat Babesia parasites.

Self Quiz
Ask yourself...
- What are some ways to prevent tick attachment?
- Can you name examples of wildlife carriers or “vehicles” for ticks?
- What education can you provide to the community about preventing and controlling tick bites?
- How has the care of tick bites changed since you have been in practice?
- What role can community and public health nurses play in the education of tick bite prevention?
Conclusion
Ticks aren’t just annoying—they’re also a source of serious illnesses. As tickborne diseases become more common, healthcare professionals should be alert to the possibility of these diseases in patients who have flu-like symptoms in the spring and summer, especially in areas rich in wildlife, such as Texas.
This course provided information on prevalent ticks and the illnesses they transmit, as well as the symptoms, progression, and medications used to treat each pathogen. The pharmacokinetics, adverse effects, and uses are meaningful components of treating patients who are infected with a tick-borne disease.
Non-Opioid Chronic Pain Management
Introduction
Chronic pain is common and debilitating condition, affecting about one in five people globally (6). Musculoskeletal conditions such as back pain are typically the most common conditions leading to chronic pain, followed by headache, orofacial pain, and visceral pain (6). Fibromyalgia and neuropathic pain are also prevalent.
About one-third of people with chronic non-cancer-related pain are prescribed opioid analgesics; however, long-term research finds that the potential harms likely outweigh the benefits.
Chronic pain can be difficult to treat, and management is often suboptimal. The most common non-opioid drug treatment is paracetamol (acetaminophen) and non-steroidal anti-inflammatory drugs, but they need to be used with caution and for short periods because of the risk of serious adverse events with long-term use (6)
We will dive into the pharmacokinetics of various non-opioid pain management options and explore this option for optimal outcomes for patients with chronic pain.
Definition
Pain is a subjective term. The one experiencing the pain is responsible fordescribing and rating it. Pain can be associated with actual or potential tissue damage or abnormal functioning of nerves. It may be classified as acute, chronic, or cancer pain. Pain may also be categorized as adaptive or maladaptive.
- Adaptive (Physiologic) Pain
-
- Nociceptive Pain – Examples include touching something hot or sharp.
- Inflammatory pain – Examples include trauma or surgery.
- Maladaptive (Pathologic) Pain
-
- Pathophysiologic pain (e.g., postherpetic neuralgia, diabetic neuropathy, fibromyalgia, irritable bowel syndrome, chronic headaches) is often described as chronic pain.
- It results from damage or abnormal functioning of nerves in the central nervous system (CNS) or peripheral nervous system (PNS). Pain circuits sometimes rewire themselves anatomically and biochemically, resulting in chronic pain, hyperalgesia, or allodynia (condition in which the pain stimulus typically should not cause pain, like “touch” on sunburned skin).
The steps in processing pain are: (10)
- Transduction – Stimulation of nociceptors.
-
- Nociceptors, located in somatic and visceral structures, are activated by mechanical, thermal, and chemical stimuli.
- Noxious stimuli may cause release of cytokines and chemokines that sensitize and/or activate nociceptors.
- Conduction – Receptor activation leads to action potentials that continue along afferent fibers to the spinal cord.
-
- Stimulation of large-diameter, sparsely myelinated fibers stimulate sharp, wider spread pain.
- Stimulation of small-diameter, unmyelinated fibers produce aching, poorly localized pain.
- Transmission – Synapse occurs in the spinal cord’s dorsal horn, releasing excitatory neurotransmitters.
-
- The signal to the brain’s higher cortical structures.
- Perception – Experience of pain happens when signals reach higher cortical structures.
-
- Relaxation, meditation, and distraction can lessen pain.
- Anxiety and depression can exacerbate pain.
- Modulation – Attributing factors can possibly include glutamate, substance P, endogenous opioids, γ-aminobutyric acid (GABA), norepinephrine, and serotonin.
The margin between neurons and immune cells within the CNS may facilitate chronic pain (10).
Somatosensation encompasses sensations such as touch, pressure, temperature, itch, and pain. Somatosensory information is transmitted from primary afferent fibers in the periphery into the central nervous system via the dorsal horn of the spinal cord (9). There are many therapies that target the dorsal horn functions as an intermediary processing center for this information, comprising a complex network of excitatory and inhibitory interneurons.

Self-Quiz
Ask Yourself...
- How would you describe the factors associated with chronic pain?
- Do you have experience with patients that have various forms of chronic pain?
- Can you describe the involvement of neurotransmitters in the signaling of nerve impulses?
- How does conduction vary between sparsely myelinated and unmyelinated fibers within the nervous system?
Overview of Non-Opioid Therapies for Chronic Pain Management
|
Non-Opioid Therapies for Chronic Pain Management (** Pharmacokinetics discussed in this course) |
|
|
Non-Opioid Drug Class |
Description |
|
Acetaminophen |
|
|
Nonsteroidal Anti-Inflammatory Drugs |
|
|
Anticonvulsants** |
|
|
Antidepressants** |
|
|
Topicals: Medicated Creams, Foams, Gels, Lotions, Ointments, Patches |
|
|
Interventional Pain Management |
|
|
Chronic Pain Therapies |
Description |
|
Self-Care |
|
|
Complementary Therapies |
|
|
Rehabilitation Therapies |
|
|
Behavioral And Mental Health Therapies |
Psychiatrists, clinical social workers, and mental health counselors provide therapies that identify and treat mental disorders or substance abuse problems that may serve as barriers to pain management. |

Self-Quiz
Ask Yourself...
- Can you name the benefits of using non-opioid pain management therapies when compared with opioid medications?
- Are you familiar with complementary chronic pain therapy?
- What are some common roadblocks to therapeutic pain management for those with opioid addictions?
- Can you name other medical professions that can become involved in the care planning for patients experiencing chronic pain?
Pharmacokinetics of Anticonvulsants
Anticonvulsants
Gabapentin and pregabalin are the most common anticonvulsants, or anti-epileptics, used for the treatment of chronic pain. These medications inhibit the alpha-2-delta subunit of voltage-gated calcium channels, which are involved in releasing nociceptive neurotransmitters. A number of systematic reviews strongly recommended using gabapentin for neuropathic pain and was backed by high-quality evidence.
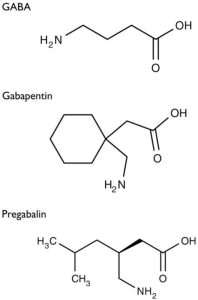
Figure 1. Structure of GABA, Gabapentin, and Pregabalin (1)
Gabapentin
Gabapentin [1-(aminomethyl)cyclohexane acetic acid] is an anti-epileptic agent and was originally developed as a gamma-aminobutyric acid (GABA)-mimetic compound to treat spasticity (1). Research found that it also has potent anticonvulsive effects. Initially approved only for use in partial seizures, it has evolved into an effective treatment agent for chronic pain syndromes, especially neuropathic pain.
Gamma-aminobutyric acid (GABA) was known to be a key inhibitory neurotransmitter, whose inhibition could cause seizures. Lipophilic groups were added to the carbon backbone to increase the bioavailability of GABA, as it does not penetrate the blood–brain barrier.
Gabapentin, available only as oral preparations, is absorbed in the small intestine by a combination of diffusion and facilitated transport. Its transport from the gut, following oral administration, is facilitated by its binding to a receptor (not yet identified) linked to a saturable l-amino acid transport mechanism (1).

Self-Quiz
Ask Yourself...
- Can you explain what Gabapentin was originally developed as?
- What is the cellular makeup of a GABA compound?
Gabapentin Drug Class
Gabapentin drug classes include: (16)
- Anticonvulsant, Miscellaneous
- GABA Analog
Gabapentin Uses
Gabapentin can be used in the management of postherpetic neuralgia (PHN) in adults, fibromyalgia, and various neuropathic pain (16).
Gabapentin Mechanism of Action
Gabapentinoids inhibit calcium-mediated neurotransmitter release through effects on α2δ-1 subunits, which inhibit forward movement of α2δ-1 that originates in the dorsal root ganglion within their endosomal compartments, causing processes that stimulate glutamate uptake by excitatory amino acid transporters (EAATs) (1). Na+-dependent excitatory amino acid transporters (EAATs) are the major transport mechanisms for extracellular glutamate removal in the CNS. EAATs-mediated clearance of amino acid glutamate released by neurons is vital to signaling and to prevent toxic accumulation of this amino acid in the extracellular space (11).
Glutamate is an amino acid and excitatory neurotransmitter that can stimulate all the CNS neurons— a capability that is unique to glutamate and explains why it is commonly known as the “master switch” (3). During this reuptake process, the cells can either reuse the glutamate or synthesize it back to glutamine, which is the form for storing for future use. Many different types of glutamate receptors exist, though they are classified into just two main categories: metabotropic and ionotropic. Ionotropic receptors are further divided into three main types of receptors: AMPA, harmac, and NMDA (3). Drugs can target these receptors to reduce glutamate release. Among the types of drugs that do so are anticonvulsants, mood stabilizers, and N -methylD-aspartate (NMDA) receptor antagonists (3).
Gamma-aminobutyric acid (GABA) is a powerful inhibitory neurotransmitter in the CNS. Glutamate and GABA work together to aid in the regulation of neurotransmitters and coordination with voltage-gated ion channels and G protein– coupled receptors (GPCRs) in the CNS (3).
GABA is synthesized from glutamate-by-glutamate decarboxylase (GAD) and is stored in synaptic vesicles. GABA-A receptors are the primary effector of the GABA-mediated inhibitory postsynaptic potential (IPSP). GABA-B receptors are responsible for the metabotropic effects of GABA and for the inhibition of voltage-gated calcium channels, the opening of potassium channels, and the release of glutamate and monoamines (3). Two main neurotransmitters regulate the sleep and wake function switch: histamine and GABA. The sleep encourager releases GABA, while the wake promoter, located within the tuberomammillary nucleus (TMN) of the hypothalamus, releases histamine (3). This is essentially why antihistamines can result in drowsiness.
Mechanisms not directly related to neurotransmitter release at dorsal horn include inhibition of descending serotonergic facilitation, stimulation of descending inhibition, anti-inflammatory actions, and influence on the affective component of pain.
Gabapentinoids do not bind to plasma proteins, and they are actively transported across the blood–brain barrier by LAT-1. The peak level in cerebrospinal fluid levels take significantly longer than the peak plasma levels, with a median time of 8 hours (1). Both are highly water-soluble and the volume of distribution of each is 0.8 and 0.5 L/kg for gabapentin and pregabalin, respectively.
Essential mechanisms of actions:
- α2δ-1 subunits are transported to the dorsal horn from their site of production in DRG (dorsal root ganglion) cell bodies. Elevated levels in the dorsal horn are associated with the development of neuropathic pain (1).
- Gabapentinoids inhibit the accumulation of α2δ-1 in the pre-synaptic terminals in the dorsal horn and reduce response to painful stimuli.
- α2δ-1 allows enhanced neurotransmitter release at decreased calcium influx.
- Analgesic effects are mediated by the facilitation of descending noradrenergic inhibition, decrease of descending serotonergic facilitation, and by cortical mechanisms affecting the limbic system (1).
- Stimulation of the uptake of glutamate by the excitatory amino acid transporters (EAAT).
- Suppression of the inflammatory response to injury.
- Modulation of the affective component of pain.

Self-Quiz
Ask Yourself...
- How would you describe the role of Na+-dependent excitatory amino acid transporters (EAATs) within the CNS?
- How do the gabapentinoids travel across the blood-brain barrier?
- Can you describe how analgesic effects can impact the limbic system?
- Can you name certain chronic conditions that may be associated with chronic inflammation?
Gabapentin Pharmacodynamics/Kinetics
The pharmacodynamics/kinetics of gabapentin is as follows: (17)
- Absorption: Variable
-
- Proximal small bowel by L-amino transport system
- Saturable process
- Dose-dependent
- Protein binding: <3%
- Metabolism: Not metabolized
- Immediate release:
-
- 900 mg/day: 60%
- 1,200 mg/day: 47%
- 2,400 mg/day: 34%
- 3,600 mg/day: 33%
- 4,800 mg/day: 27%
- Extended release: Variable; increased with higher fat content meal
- Half-life elimination:
-
- Adults, normal: 5 to 7 hours
- Increased half-life with decreased renal function
- Anuric adult patients: 132 hours
- Adults during hemodialysis: 3.8 hours
- Time to peak
-
- Adults: 2 to 4 hours
- Extended release: 8 hours
- Excretion: Proportional to renal function; urine (as unchanged drug)
- Clearance: Apparent oral clearance is directly proportional to CrCl
Gabapentin Adverse Effects
Adverse effects are common with gabapentinoids resulting in a discontinuation rate of at least 11%, but serious adverse events are uncommon. The substitution of gabapentin with pregabalin in gabapentin responders resulted in improved pain relief and fewer adverse events.
Central nervous system effects
Dizziness, somnolescence, and gait disturbances are the most common adverse effects. The effects often occur during the initiation of treatment and can diminish after several weeks of treatment. Visual blurring can also occur (1).
Other common side effects affecting the central nervous system (CNS) include impaired concentration, confusion, memory loss, altered mood, movement disorders, sleep disorder, speech impairment, and vertigo (1).
Most adverse reactions have a clear dose–response relationship with increased risk of complications with higher doses. However, ocular adverse effects such as amblyopia and blurred vision appeared at lower doses of pregabalin (1)
Respiratory depression
Respiratory depression has been reported when used in combination with opioids, resulting in an increased risk of accidental opioid-related mortality (1). Clinicians should be aware of this prior to prescribing multiple medications. A large primary care database review showed that 21.8% of patients with a new prescription for gabapentin and 24.1% of patients with a new prescription for pregabalin received additional prescriptions, primarily for opioids (1). Dose adjustments are recommended for patients with compromised respiratory function, respiratory or neurological diseases, renal impairment, and elderly people due to the higher risk of experiencing severe respiratory depression.
Weight gain
Weight gain is common with gabapentinoids and can affect up to one-fourth of all patients treated (This is a common reason for patients to stop taking it). However, the extent of weight gain appears to be moderate. The majority of patients treated with pregabalin for one year maintain weight within ±7% of their baseline or initial weight (1). Weight gain is related to dose and duration of use but not to body mass index, gender, age, and development of edema (1).
Gastrointestinal effects
Gastrointestinal adverse effects such as abdominal distension, abnormal appetite, constipation, dry mouth, and nausea are common side effects and are dose-related, all except constipation (1).
Misuse
There is potential for abuse of gabapentinoids, particularly in individuals with a history of opioid abuse (1). Both gabapentinoids have been reported to stimulate feelings of sociability, euphoria, calm and relaxation, which can lead to misuse. Abuse potential of pregabalin is higher as compared to gabapentin due to its pharmacokinetic properties (1). All anticonvulsants are associated with increased risk for suicidal thoughts and behavior (12).
Withdrawal
Withdrawal symptoms are common and appear between 12 hours and 7 days after cessation of use, with most cases occurring between 24 and 48 hours (1). Other symptoms include tachycardia, palpitations, anxiety, sweating, restlessness, hypertension, tremor, gastrointestinal symptoms, paranoia, auditory hallucinations, and suicidal ideation – all similar to the withdrawal effects of benzodiazepines and alcohol (1). Patients with psychiatric comorbidities and the elderly may be at an increased risk of withdrawal. Clinicians should do a slow tapering schedule for patients at higher risk for withdrawal. A slower tapering schedule such as a twice-weekly reduction of 10–25% of the dose has been suggested to minimize the risk of withdrawal effects (1).
Toxicity
The risk for toxicity is higher in patients with chronic kidney disease and those on dialysis (1). Toxicity may present with increased sedation, confusion, unsteady gait, myoclonus, ataxia, episodic leg spasm, asterixis and tremulousness (1).
Guidelines on recommendations for dose reductions based on creatinine clearance are available for prescribers. Patients on hemodialysis might require supplemental doses following dialysis due to it removing approximately 35% of gabapentin and 50–60% of pregabalin (1).
Gabapentin Dosing
Fibromyalgia
Initial: Oral: 100 to 300 mg once daily at bedtime; increase dose gradually based on response and tolerability every 1 to 2 weeks to a target dose of 1.2 to 2.4 g/day in divided doses (17)
Neuropathic pain
Note: For chronic use, an adequate trial with gabapentin may require two months or more. For critically ill patients with neuropathic pain, gabapentin may be a useful component of multimodal pain control (17).
Immediate release: Oral: Initial: 100 to 300 mg 1 to 3 times daily; increase dose based on response and tolerability to a target dose range of 300 mg to 1.2 g 3 times daily (17).
Extended release: Oral: Initial: 300 mg at bedtime; increase dose based on response and tolerability to a target dose of 900 mg to 3.6 g once daily (17).
Postherpetic neuralgia
Immediate release: Oral: 300 mg once on day one, 300 mg twice daily on day two, and 300 mg 3 times daily on day two, then increase as needed up to 1.8 to 3.6 g/day in divided doses (17).
Extended release: Oral: Initial: 300 mg once daily; increase by 300 mg each day up to 900 mg once daily. Further increase as needed up to 1.8 g once daily (17).


Self-Quiz
Ask Yourself...
- Can you discuss the side effects of gabapentin?
- How is gabapentin excreted?
- Can you name the contraindications for taking this medication, specifically associated with respiratory distress?
- Do you have experience with educating patients on a tapered dosing schedule?
Pregabalin
Pregabalin was originally approved by the U.S. Food and Drug Administration (FDA) as an anti-epileptic drug, also called an anticonvulsant. It works by reducing the conduction of impulses in the brain that cause seizures. Pregabalin also affects chemicals in the brain that send pain signals across the nervous system.
Pregabalin Drug Class
Pregabalin is classified as a Schedule V prescription drug (16). Schedule V drugs are defined as drugs with lower potential for abuse than Schedule IV by the U.S. Drug Enforcement Administration (DEA).
Pregabalin Uses
Pregabalin is used to treat pain caused by neuropathic pain associated with spinal cord injury, fibromyalgia, diabetic neuropathy, post-herpetic neuralgia, and management of postherpetic neuralgia (1, 12).
Pregabalin Mechanism of Action
Pregabalin binds to alpha-2-delta subunit of calcium channels within the CNS and lowers calcium influx at the nerve terminals, which inhibits excitatory neurotransmitter release (16). These excitatory neurotransmitters including glutamate, norepinephrine (noradrenaline), serotonin, dopamine, substance P, and calcitonin gene-related peptide (16).
Glutamate was discussed earlier in the course, but it is important to closely examine norepinephrine, as it relates to pain. Norepinephrine is another monoamine neurotransmitter in the catecholamine family, and it serves as both a neurotransmitter and a hormone (3). The sympathetic nervous system, which becomes activated during stressful or painful events, activates norepinephrine as the neurotransmitter primarily responsible for the “fight or flight” response (3). The sympathetic system is highly influenced by changes in the serum norepinephrine concentration and is associated with the regulation of heart rate and blood pressure.
By binding presynaptically to the alpha2-delta subunit of voltage-gated calcium channels in the CNS, it is essentially thought to calm the conduction of pain impulse. In addition, pregabalin prevents the alpha2-delta subunit from being transported from the dorsal root ganglia to the spinal dorsal horn, which may also contribute to the mechanism of action and use in chronic pain in those with spinal cord injuries (1).
Although structurally related to GABA, it does not bind to GABA or benzodiazepine receptors. Pregabalin may also affect descending noradrenergic and serotonergic pain transmission pathways from the brainstem to the spinal cord.
Alpha (α 2δ )-ligands modulate neurotransmitter release and increase membrane hyperpolarization and the seizure threshold.
Pregabalin Pharmacodynamics/Kinetics
The pharmacodynamics/kinetics of gabapentin is as follows: (16)
- Onset of action: Effects may be noted as early as the first week of therapy.
- Absorption
-
- Extended release: Approximately 30% lower when administered while fasting.
- Distribution: Vd: 0.5 L/kg
- Protein binding: 0%
- Bioavailability: ≥90%
- Half-life elimination: Adult: 6.3 hours
- Time to peak, plasma:
-
- Extended release: Median is 8 hours with food (Average 5 to 12 hours)
- Immediate release, Adults: Within 1.5 hours fasting; 3 hours with food
- Excretion: Urine (90% as unchanged drug; minor metabolites)
Pregabalin Adverse Effects
Central nervous system effects
Dizziness (3% to 45%), drowsiness (≤36), fatigue (4% to 11%) is included among adverse effects (16).
Ataxia, balance impairment, abnormal gait, euphoria, confusion, disturbance in attention abnormal thinking, neuropathy, myasthenia, insomnia, memory impairment, vertigo, speech disturbance, anxiety, paresthesia, intoxicated feeling, lethargy, and nervousness have also been reported (16).
Cardiovascular
Peripheral edema (4% to 16%), facial edema (1% to 3%), chest pain (2%), hypertension (2%), hypotension (2%) has been reported.
Endocrine & metabolic
Weight gain (2% to 14%) is noted.
Ophthalmic
Visual field loss (13%) and blurred vision (≤12%) have been noted.
Gastrointestinal
Constipation, increased appetite, nausea, flatulence, vomiting, abdominal distension, and abdominal pain are among the reported adverse effects.
Endocrine & metabolic: Fluid retention (2% to 3%), hypoglycemia (2% to 3%), decreased libido (≥1%)
Hematologic & oncologic
Thrombocytopenia (3%) has occurred.
Pregabalin Dosing
Fibromyalgia
Immediate release: Oral: Initial: 75 mg twice daily; may increase to 150 mg twice daily within one week based on response and tolerability; maximum dose: 450 mg/day (manufacturer’s labeling). Note: A lower initial doses of 25 to 50 mg at bedtime is suggested by many experts (8).
Neuropathic pain
Immediate release: Oral: Initial: 25 to 150 mg/day once daily or in two divided doses; may increase in increments of 25 to 150 mg/day at intervals ≥1 week based on response and tolerability up to a usual dose of 300 to 600 mg/day in two divided doses (16).
Postherpetic neuralgia
Immediate release: Oral: Initial: 150 mg/day in divided doses (75 mg twice daily or 50 mg three times daily); may increase to 300 mg/day within one week based on response and tolerability; after 2 to 4 weeks, may further increase up to the maximum dose of 600 mg/day (16).
Extended release: Oral: Initial: 165 mg once daily; may increase to 330 mg once daily within one week based on tolerability; after 2 to 4 weeks, may further increase up to the maximum dose of 660 mg/day (16).

Self-Quiz
Ask Yourself...
- Can you discuss the side effects of pregabalin?
- What is the half-life for this medication?
- Can you describe the mechanism of action of this medication?
- How can the classification or schedule of a drug impact prescribing?
Warnings for Gabapentin and Pregabalin
Warnings for gabapentin and pregabalin include the following risk factors, dosing and monitoring considerations, and patient education needs (1).
The FDA is warning that serious breathing difficulties may occur in patients using gabapentin (Neurontin, Gralise, Horizant) or pregabalin (Lyrica, Lyrica CR) who have respiratory risk factors. Risk factors include the use of opioid pain medicines, and conditions that reduce lung function, such as chronic obstructive pulmonary disease (COPD) (14). The elderly are also at higher risk.
Health care providers should start gabapentinoids at the lowest dose and monitor patients for symptoms of respiratory depression and sedation. Patients with underlying respiratory disease and elderly patients are also at increased risk and should be managed similarly.
Clinicians should assess the risk of misuse, dependence, and diversion.
Patients should be made aware of the importance of dosage titration, the titration process, and the requirement to take a stable regime for a few weeks before assessing for improvement in pain. Patients often misunderstand that gabapentinoids cannot be taken as needed and that taking an additional dose does not result in improved pain (1)
Patients must be warned about the potential alteration in concentration for certain tasks, such as using heavy equipment or driving.
Pharmacokinetics of Antidepressants
Antidepressants
Antidepressants, including tricyclic antidepressants (TCAs) and selective norepinephrine reuptake inhibitors (SNRIs), have shown to have analgesic effects by primarily blocking the reuptake of norepinephrine, thereby enhancing the pain-modulating pathway activity. TCAs also block peripheral sodium channels, which can also help reduce pain.
Serotonin and norepinephrine reuptake inhibitors (SNRIs) and tricyclic antidepressants (TCAs) are the most common classes of antidepressants used to manage chronic neuropathic pain.
All currently available antidepressants enhance monoamine neurotransmission by one of several mechanisms; the most common mechanism is inhibition of the activity of SERT, NET, or both. The serotonin transporter (SERT) is a glycoprotein with 12 transmembrane regions embedded within the axon terminal and cell body membranes of serotonergic neurons (2). As serotonin outside of the cells bind to receptors on the transporter, changes occur in the transporter and serotonin (2). Na+, and Cl− then are transported into the cell. Binding of intracellular K+ results in the release of serotonin inside the cell. The transporter is released into its original state.
At therapeutic doses, about 80% of the activity of the transporter is inhibited (2).
Ultimately, the increased availability of monoamines for binding in the synaptic cleft results in a cascade of events that enhance the transcription of some proteins and the inhibition of others (2). The inhibiting effects are most desirable for reduction of chronic pain.
We will use the pharmacokinetics of the tricyclic antidepressant (TCA), Amitriptyline, and selective norepinephrine reuptake inhibitor (SNRI), Duloxetine, to explore the research on use.
The SNRIs differ from the TCAs in that they lack the potent antihistamine, α-adrenergic blocking, and anticholinergic effects of the TCAs. As a result, the SNRIs tend to be favored over the TCAs in the treatment of pain syndromes because they are often tolerated better (2).
- Tricyclic antidepressant (TCA): Pharmacokinetics of Amitriptyline
- Serotonin norepinephrine reuptake inhibitors (SNRIs): Pharmacokinetics of Duloxetine
Tricyclic Antidepressants (TCA)
The first indication that tricyclic antidepressants (TCAs) may help with neuropathic pain came from a 1960 study that found that patients treated with imipramine experienced chronic pain relief. There have been many studies since that support the effectiveness of TCAs on chronic pain.
Amitriptyline
Example of tricyclic antidepressant (TCA) used in chronic pain management.
Amitriptyline Drug Class
Antidepressant, Tricyclic (Tertiary Amine)
Amitriptyline Uses
Used to treat major depressive disorder (unipolar), unipolar major depressive disorder, and management of chronic neuropathic pain.
Amitriptyline Mechanism of Action
The N-type calcium ion channel is an established target for the treatment of neuropathic pain. The channel consists of a unique α1 pore-forming subunit and auxiliary α2-δ and β subunits (6). The general structure of the α1 subunit is similar to that of other voltage-gated ion channels.
The mechanism of action involves increasing the synaptic concentration of serotonin and/or norepinephrine in the central nervous system by stopping their reuptake by the presynaptic neuronal membrane pump (Wil-A).
Amitriptyline is a tertiary amine with strong binding affinities for alpha-adrenergic, histamine (H1), and muscarinic (M1) receptors (13). Chronic treatment with amitriptyline desensitizes presynaptic receptors, producing long-lasting changes in monoaminergic neurotransmission (13).
Amitriptyline Pharmacodynamics/Kinetics
- Onset of action: Responses may vary per individual; however, 4 to 8 weeks of treatment are needed before determining if a patient is partially or non-responsive; desired therapeutic effect for pain reduction may take as long as 1 to 3 weeks.
- Absorption: Rapid, well absorbed.
- Distribution: Vd: 18 to 22 L/kg
- Protein binding: >90%
- Metabolism: Rapid; hepatic N to demethylation to nortriptyline (active), hydroxy derivatives and conjugated derivatives
- Bioavailability: 43% to 46%
- Time to peak, serum: 2 to 5 hours
(Wil-A)
- Amitriptyline has a half-life of 10 to 28 hours (13)
- Excretion: Amitriptyline and its metabolites are primarily excreted by the kidney (13)
- Special Populations: Elderly: May have increased plasma levels
- Amitriptyline can cross the placental barrier (13)
Amitriptyline Dosage Formulations
Amitriptyline dosage formulations come in oral tablets of 10 mg, 25 mg, 50 mg, 75 mg, 100 mg, and 150 mg.
Adult Dosing: For chronic pain, therapy can initiate a dose of 10 to 20 mg daily. The dose can be increased by 25 mg every 3 to 7 days, with a maximum of 150 to 300 mg/day. If the dose requires adjustment, it is preferable to change the bedtime dose. In cases of therapy cessation, the clinician should gradually taper to avoid withdrawal (13).
Plasma Levels: It is difficult to directly correlate plasma levels with desired, therapeutic effects. However, determining plasma levels might be useful in identifying toxicity with excessively high levels or in whom noncompliance is suspected.
Older adult patients have decreased hepatic metabolism and increased intestinal transport time, so plasma levels are usually higher for any given oral dose of amitriptyline for this population.
Amitriptyline Side Effects
Amitriptyline, due to its alpha-adrenergic receptor blockade, can cause orthostatic hypotension, dizziness, and sedation. Anticholinergic side effects include blurred vision, dry mouth, urinary retention, tachycardia, acute angle glaucoma, constipation, and confusion (13). Antihistamine side effects secondary to its histamine (H1) receptor binding property include sedation, increased appetite, weight gain, confusion, and delirium (13).
It can increase the risk of bone fracture and bone marrow suppression.
Amitriptyline Warnings
Anticholinergic Effects
May cause anticholinergic effects (constipation, xerostomia, blurred vision, urinary retention); use with caution in patients with decreased gastrointestinal motility, increased intraocular pressure (IOP), narrow-angle glaucoma, paralytic ileus, urinary retention, BPH, xerostomia, or visual problems (Wil-A).
CNS Depression
May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (e.g., operating machinery or driving).
Fractures
Bone fractures have been associated with antidepressant treatment (Wil-A)
Hematologic Effects
TCAs may rarely cause bone marrow suppression; monitor for any signs of infection and obtain CBC if symptoms are evident (e.g., fever, sore throat).
Orthostatic Hypotension
May cause orthostatic hypotension; use with caution in patients at risk of this (cerebrovascular disease, cardiovascular disease, hypovolemia, or concurrent medication use which may predispose to hypotension/bradycardia).
Therapy is relatively contraindicated in patients with symptomatic hypotension.
Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) and Hyponatremia
Associated with the development of syndrome of inappropriate antidiuretic hormone secretion (SIADH) and hyponatremia, predominately in the elderly (Wil-A).
Cardiovascular Risk
In a scientific statement from the American Heart Association, amitriptyline may exacerbate underlying myocardial dysfunction (WIL-A). Amitriptyline can also cause heart rate variability, slow intracardiac conduction, induce various arrhythmias, and cause QTc (corrected QT) prolongation (13).
Use with caution in patients with diabetes mellitus, hepatic impairment, or renal impairment (Wil-A).
A major contraindication is the coadministration with or within 14 days of Monoamine oxidase inhibitors (MAOIs); avoid coadministration with cisapride and avoid during the acute recovery phase following myocardial infarction (Wil-A).
Clinicians must monitor elderly patients carefully and obtain amitriptyline serum levels based on their clinical assessment. Clinicians should adjust amitriptyline dose according to the patient’s clinical response and not based on plasma levels (13).
Alternatives to Amitriptyline
Other TCAs that may be helpful in chronic pain management is Desipramine, Imipramine, and Nortriptyline.
Amitriptyline is more sedating and has increased anticholinergic properties than other TCAs (13).


Self-Quiz
Ask Yourself...
- Can you discuss the mechanism of action for Amitriptyline?
- What would you consider the most worrisome adverse effects?
- What are some common anticholinergic properties and effects?
- Why is the half-life and peak time important in the administration and prescribing of a medication?
Selective Norepinephrine Reuptake Inhibitors (SNRIs)
As mentioned earlier, serotonin and norepinephrine reuptake inhibitors (SNRIs) are one of the most common classes of antidepressants used to manage chronic neuropathic pain.
Duloxetine
Example of selective norepinephrine reuptake inhibitor (SNRI) used in chronic pain management.
Duloxetine Drug Class
Antidepressant, Serotonin/Norepinephrine Reuptake Inhibitor.
Duloxetine Uses
Duloxetine can be used to manage major depressive disorder (MDD), generalized anxiety disorder (GAD), fibromyalgia, diabetic peripheral neuropathy, and chronic musculoskeletal pain.
Duloxetine Mechanism of Action
Duloxetine is a potent inhibitor of neuronal serotonin and norepinephrine reuptake and a weak inhibitor of dopamine reuptake.
Serotonin is another monoamine neurotransmitter derived from tryptophan; the majority of the serotonin found in the body is located in the enterochromaffin cells of the gastrointestinal tract, with the rest within in the CNS, where it regulates mood, sleep, and appetite (3).
Duloxetine inhibits serotonin and norepinephrine reuptake and enhances dopamine levels within the prefrontal cortex (5). The mechanism of action behind the increase in dopamine levels involves the inhibition of norepinephrine transporters; the transporters have an attraction for dopamine. Therefore, inhibition of norepinephrine transporters can lead to an increase in dopamine. This increase in dopamine specifically occurs in the prefrontal cortex, where dopamine transporters are scarce, and reuptake relies more heavily on norepinephrine transporters (5).
Duloxetine works to reduce neuropathic and chronic pain states by increasing the activity of noradrenergic and serotonergic neurons in the descending spinal pathway of the dorsal horn (5). These descending neurons decrease the activity of dorsal horn neurons, which essentially suppresses excessive input from reaching the brain. The hypothesis is that a deficiency in these inhibitory signals resulting in less signals perceived as pain being delivered.
Duloxetine has no significant activity for muscarinic cholinergic, H1-histaminergic, or alpha2-adrenergic receptors. Duloxetine does not possess MAO-inhibitory activity.
Duloxetine Pharmacodynamics/Kinetics
- Absorption: Well-absorbed.
- Protein binding: >90%; primarily to albumin and alpha1-acid glycoprotein.
- Metabolism: Hepatic, via CYP1A2 and CYP2D6; forms multiple metabolites (inactive).
- Half-life elimination (adults): ~12 hours (range: 8 to 22 hours); ~4 hours longer in elderly women.
- Time to peak: 5 to 6 hours; food delays by 1.7 to 4 hours (15).
Duloxetine has an elimination half-life of about 12 hours (range 8 to 17 hours) and its pharmacokinetics are reliant on the dose (18). Plasma concentrations are typically stable after three days of dosing.
Elimination of duloxetine is mainly through hepatic metabolism involving two P450 isozymes, CYP2D6 and CYP1A2 (18). Orally administered duloxetine hydrochloride is well absorbed. There is a median two-hour lag until absorption begins with maximal plasma concentrations occurring six hours post dose (18).
Food does not affect the maximal concentration of duloxetine, but it delays the time to reach peak concentration from 6 to 10 hours and it marginally decreases the extent of absorption (AUC) by about 10% (18). There is a three-hour delay in absorption and a one-third increase in apparent clearance of duloxetine after an evening dose as compared to a morning dose (18).
Duloxetine is highly bound (>90%) to proteins in human plasma, binding primarily to albumin and α1-acid glycoprotein (18). The plasma protein binding of duloxetine is not changed by renal or hepatic impairment. About 70% is excreted and found in the urine as metabolites of duloxetine; about 20% is excreted in the feces (18).
Duloxetine Dosing for Management of Chronic Pain
Low back pain: 30 mg can be given once daily for one week and increased up to 60 mg once daily as tolerated as an adjunct therapy. Maximum dose: 60 mg/day.
Neuropathy: 60 mg can be administered initially; however, lower starting doses may be appropriate depending on patient tolerance. Maximum dose: 60 mg/day.
Duloxetine Side Effects
Side and adverse effects of the cardiovascular, gastrointestinal, central nervous system, such as headaches and drowsiness, and fatigue, are common (5). Duloxetine has a very low anticholinergic impact.
Common adverse effects of duloxetine include: (5)
- Headache
- Drowsiness
- Fatigue
- Nausea
- Xerostomia
- Abdominal pain
- Weight loss
- Weakness
- Insomnia
- Dizziness
- Change in libido
- Diaphoresis
- Tremor
Serious adverse effects of duloxetine include:
- Suicidality
- Serotonin syndrome
- Hepatoxicity
- Mania
- Syncope
- Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
- Hyponatremia
Duloxetine Warnings
Warnings for duloxetine include the following information (5).
Duloxetine is contraindicated in patients with concurrent or recent (within 14 days) use of monoamine oxidase (MAO) inhibitors, uncontrolled angle-closure glaucoma, or hypersensitivity to duloxetine.
Duloxetine should also be avoided in patients with liver failure or severe renal dysfunction (5). Also avoid using duloxetine in patients receiving treatment with linezolid or intravenous methylene blue due to an increased risk of serotonin syndrome (5)
Precautions and Warning in Special Population:
- Duloxetine is FDA pregnancy category C, which means risk to fetal development cannot be ruled out.
- Caution is necessary when prescribing duloxetine in the geriatric population.
Monitor for suicidal ideation, especially when starting treatment, altering the dose, and after discontinuation of therapy.
Caution should be exercised when using anticoagulants or antiplatelet medications along with duloxetine therapy.
Laboratory workup should include monitoring serum creatinine, blood urea nitrogen (BUN), transaminase levels, blood glucose levels, and HgbA1c in diabetic patients.
Sodium levels require follow-up when prescribing duloxetine in the geriatric population.
Duloxetine Toxicity
Signs and symptoms of toxicity include serotonin syndrome, seizures, somnolence, syncope, tachycardia, diarrhea, and vomiting (5).
Signs of serotonin syndrome include agitation, disorientation, diaphoresis, hyperthermia, tachycardia, nausea, vomiting, myoclonus, dilated pupils, dry mucous membranes, and increased bowel sounds; clonus and hyperreflexia are particularly common in serotonin syndrome (5).
There is no antidote to duloxetine overdose; cyproheptadine and cooling measures may be considered for toxicity or overdose (5).


Self-Quiz
Ask Yourself...
- Can you discuss the mechanism of action of duloxetine?
- Can you name the signs of serotonin syndrome?
- How can inhibiting neuronal serotonin and norepinephrine reuptake improve symptoms of pain or depression?
- Is there an antidote to duloxetine overdose?
Nursing Considerations
It is meaningful to remember that pain is subjective and should be determined by each patient. Those with chronic pain spend a significant amount of time in out-of-hospital environments, in their homes and in their community settings.
There is no “one size fits all” care plan for those with chronic pain. Personalized care is a collaborative process that should be used in chronic condition management in which patients, caregivers, and healthcare providers can identify and discuss problems and develop plans and goals to empower them in their own care. Individualized care can improve aspects of physical health, mental health, and the ability to self-manage conditions.
Nursing should utilize appropriate pain assessment tools and identify changes in levels of pain. Pain intensity, pain relief, and medication side effects must be assessed regularly. The frequency of assessment depends on the type of pain, analgesic used, route of administration, and concomitant medications.
Current Research and Opportunities
Chronic pain affects more than 100 million people in the United States (4). The U.S. is currently in the midst of an opioid epidemic with increased opioid use over the last two decades. Research is extensively focused on treatment alternatives, including medications, physical therapy, exercise, injections, and neuromodulation.
Conclusion
Clinicians face difficult decisions when managing chronic pain in their patients. There is an increasing need for meaningful use of non-opioid options. Research supports the positive outcomes of therapies such as anticonvulsants, antidepressants, and various other alternatives. Knowledge of the unique pharmacokinetics of each therapy is essential for clinicians.
SSRI Use in Major Depressive Disorder
Introduction
When hearing the phrase selective serotonin reuptake inhibitors, what comes to mind? If you're an advanced practice registered nurse (APRN) with prescriptive authority, you've heard of SSRIs before. Even as a nurse or maybe before nursing school, conversations about prescription drug use and mental health existed every so often.
Presently, patients seek guidance and information on various health topics from APRNs, including medication management, women's health, and mental health. The information in this course will serve as a valuable resource for APRNs with prescriptive authority of all specialties, education levels, and backgrounds to learn more about SSRIs and major depressive disorder (MDD).
Defining SSRIs
What Are SSRIs?
Selective serotonin reuptake inhibitors, known as SSRIs, are a type of pharmacological drug class. SSRIs have existed for the past several decades as a class of prescription medications that can manage major depressive disorder (MDD) and other mental health conditions (1).
While this course focuses explicitly on SSRI use in MDD management, SSRIs are also Food and Drug Administration (FDA) approved to manage obsessive-compulsive disorder (OCD), panic disorder (PD), post-traumatic stress disorder (PTSD), and social anxiety disorder (SAD). In addition, several off-label uses for SSRI include management for binge eating disorder and menopausal vasomotor symptoms.
How and Where Are SSRIs Used?
SSRIs are commonly prescribed to manage MDD and other mood disorders in the U.S. and around the world in pediatric, adult, and geriatric populations (1, 2). SSRIs can be taken by mouth as a pill, capsule, or liquid oral solution. Presently, SSRIs cannot be offered via intravenous, rectal, buccal, or injection routes.
What Is the Clinical Criteria for Prescribing SSRIs?
Clinical criteria for prescribing SSRIs can vary depending on the intention for the SSRI. In the case of MDD, several factors can play a role in the clinical criteria for prescribing SSRIs. A patient's adherence to swallowing a pill daily, dosage given the patient's weight, medical history, and MDD concerns, and prior experience with other medications can influence prescribing SSRIs. When considering prescribing SSRIs for MDD management, consider assessing the patient for MDD first, taking a detailed health history, and discussing the risk versus benefits of starting SSRIs for this patient (1, 3).
What Is the Average Cost for SSRIs?
Cost for SSRIs can significantly vary depending on the type of SSRI, insurance, dosage, frequency, and other factors. Cost is among leading reasons why many patients cannot maintain their medication regime (4). If cost is a concern for your patient, consider reaching out to your local pharmacies or patient care teams to find cost-effective solutions for your patients.
What Is Major Depressive Disorder (MDD)?
Major depressive disorder (MDD) is a mental health condition in which a person has consistent appetite changes, sleep changes, psychomotor changes, decreased interest in activities, negative thoughts, suicidal thoughts, and depressed mood that interfere with a person's quality of life (5). According to the Diagnostic and Statistical Manual of Mental Health Disorders, a patient must have at least five persistent mood related symptoms, including depression or anhedonia (loss of interest in activities once enjoyed), that interferes with a person's quality of life to be formally diagnosed with MDD. Note that MDD does not include a history of manic episodes, and pediatric populations can present with more variable MDD symptoms (5). As an APRN, you can assess for MDD by doing a detailed patient health history or having a patient complete the Patient Health Questionnaire-9 (PHQ-9) - a depression assessment tool (5).


Self Quiz
Ask yourself...
- What are some medication administration options for SSRIs?
- What populations can be prescribed SSRIs?
SSRI Pharmacokinetics
Drug Class SSRIs
Selective serotonin reuptake inhibitors, known as SSRIs, are a type of pharmacological drug class part of the antidepressant drug class. They can be prescribed at various dosages depending on the patient history, severity of major depressive disorder (MDD), other medication use, and other factors based on patient-centered decision making. Currently, SSRIs that are FDA approved for MDD management include paroxetine, sertraline, citalopram, escitalopram, vilazodone, and fluoxetine. SSRIs can be prescribed for the oral route and are available via capsule, tablet, or liquid suspension/solution. SSRIs can be taken at any time of day. They can be taken with or without food, though vilazodone in particular is recommended with food. SSRIs are often prescribed to be taken once a day, sometimes twice a day, depending on the severity of MDD. Health care provider professional discretion and patient condition should guide therapy (1).
SSRIs are metabolized by and known to affect the cytochrome P450 system. CYP2D6 inhibitors include escitalopram, citalopram, sertraline, paroxetine, and fluoxetine. Fluoxetine and fluvoxamine are inhibitors of CYP2C19. Fluvoxamine is an inhibitor of CYP1A2. Consider reviewing a patient's medication history and health history prior to prescribing SSRIs (1).
SSRIs Method of Action
SSRI method of action has been subject to several studies, especially in the last few years. Serotonin is a neurotransmitter that plays a role in mood and other bodily functions. It can be measured in plasma, blood, urine, and CSF (6). It is important to note that serotonin is rapidly metabolized to 5-hydroxyindoleacetic acid (5-HIAA) (6). SSRIs work by inhibiting the reuptake of serotonin at certain chemical receptors, thereby increasing serotonin activity and concentration (1). SSRIs inhibit the serotonin transporter (SERT) at the presynaptic axon terminal.
By obstructing the SERT, a higher amount of serotonin (5-hydroxytryptamine or 5HT) remains in synaptic clefts. This higher amount of serotonin can then stimulate postsynaptic receptors for a more extended period (1). While SSRIs can increase serotonin activity, there is some evidence that suggests the possibility of long-term SSRI use reducing serotonin concentration (6). In addition, the clinical response to SSRIs in patients with MDD can take anywhere from a few to several weeks to emerge (7). While some research suggests that there are initial improvements in mood, evidence remains inconclusive as to the exact time SSRIs can take to provide a therapeutic response for patients (7). Also, while research suggests that SSRIs can increase serotonin levels, there is still mixed evidence on the exact method of action for SSRIs (7).
As a result, it is important to counsel patients that SSRIs can take a few weeks to provide a therapeutic response and to monitor mood and symptoms while taking SSRIs.
SSRI Side Effects
Every medication has the possibility of side effects, and SSRIs are no exception. Fortunately, SSRIs are known to have less side effects than other drug classes of antidepressants, such as monoamine oxidase inhibitors (MAOIs) or tricyclic antidepressants (TCAs). The most commonly known side effects of SSRIs include weight gain, sleep changes, headache, gastrointestinal issues, drowsiness, orthostatic hypotension, and sexual function changes (1).
Sleep changes can include an increased desire to sleep, increase in the amount of time sleeping, or insomnia. Gastrointestinal issues can include an upset stomach, nausea, or dry mouth. Mood changes, such as anxiety, are possible side effects as well. Sexual function changes can include erectile dysfunction, libido changes, impaired orgasmic response, and vaginal dryness (1, 8).
There are more serious possible side effects of SSRIs as well. For instance, SSRIs have the possible side effect of QT prolongation, which if left untreated or undiagnosed, can lead to fatal cardiac arrythmias (1, 8). In particular, the SSRI citalopram has been shown to have more of a risk for QT prolongation compared to other SSRIs. Also, like any other medication that can possibly increase levels of serotonin in the body, there is a possibility of serotonin syndrome as a complication of SSRI use. Possible serotonin syndrome clinical manifestations include increased blood pressure, increased sweating, increased reflex ability, and increased dry eyes (8). Due to the wide varied range of side effects, patient counseling, monitoring, and education is essential when prescribing SSRIs.
SSRI Black Box Warning
In 2004, the FDA issued a black box warning for SSRIs and other antidepressant medications due to the possible increased risk of suicidality in pediatric and young adult populations (up to age 25). When considering SSRI use in patients under 25 and knowing MDD is a risk factor for suicidality, having a conversation with the patient about risks versus benefits must be considered. However, in the past several years since the FDA's warning, there is no clear evidence showing a correlation between SSRIs and the increased risk of suicidality (1, 8). Health care provider professional discretion and patient condition should guide therapy.
SSRI Alternatives
MDD can be a complex, chronic condition to manage with varying clinical presentation and influence on a patient's quality of life. There are several alternatives to SSRI use, such as: (1, 9)
- Other prescription drugs
- Serotonin-norepinephrine reuptake inhibitors (SNRIs). Commonly known SNRIs include milnacipran, venlafaxine, desvenlafaxine, duloxetine, and levomilnacipran.
- Atypical antidepressants. Commonly known atypical antidepressants include bupropion and mirtazapine.
- Tricyclic antidepressants (TCAs). Commonly known TCAs include amitriptyline, desipramine, imipramine, clomipramine, doxepin, and nortriptyline.
- Monoamine oxidase inhibitors (MAOIs). Commonly known MAOIs include phenelzine, tranylcypromine, isocarboxazid, and selegiline.
- Psychotherapy, such as cognitive behavioral therapy (CBT) or interpersonal therapy
- Electroconvulsive therapy (ECT)
- Vagus Nerve Stimulation (VNS)
- Transcranial Magnetic Stimulation (TMS)

Self Quiz
Ask yourself...
- What are some possible side effects of SSRIs?
- What are some pharmacological alternatives to SSRIs?
Nursing Considerations
Nurse’s Role
What Is the Nurses' Role in SSRI Patient Education and Management?
Nurses remain the most trusted profession for a reason, and APRNs are often pillars of patient care in several health care settings. Patients turn to nurses for guidance, education, and support. While there is no specific guideline for the nurses' role in SSRI education and management, here are some suggestions to provide quality care for patients interested in or currently taking SSRIs to manage current or suspected major depressive disorder (MDD).
- Take a detailed health history. Often times, mental health symptoms, such as depressive thoughts or anxiety, are often dismissed in health care settings, even in mental health settings. If a patient is complaining of symptoms that could be related to major depressive disorder, inquire more about that complaint. Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient's complaint is not being taken seriously by other health care professionals, advocate for that patient to the best of your abilities.
- Review medication history at every encounter. Often times, in busy clinical settings, reviewing health records can be overwhelming. While a vast number of people take SSRIs, many are no longer benefiting from the medication. Ask patients how they are feeling on the medication, if their symptoms are improving, and if there are any changes to medication history.
- Ask about family history. If someone is complaining of symptoms that could be related to MDD, ask if anyone in their immediate family, such as their parent or sibling, experienced similar conditions.
- Be willing to answer questions about mental health and SSRIs. Society can often stigmatize open discussions of prescription medication and mental health. SSRIs are no exception. There are many people who do not know about the benefits and risks of SSRIs, the long-term effects of unmanaged MDD, or possible treatment options. Be willing to be honest with yourself about your comfort level discussing topics and providing education on SSRIs and MDD.
- Communicate the care plan to other staff involved for continuity of care. For several patients, MDD management often involves a team of mental health professionals, nurses, primary care specialists, pharmacies, and more. Ensure that patients' records are up to date for ease in record sharing and continuity of care.
- Stay up to date on continuing education related to SSRIs and mental health conditions, as evidence-based information is always evolving and changing. You can then present your new findings to other health care professionals and educate your patients with the latest information. You can learn more about the latest research on SSRIs and mental health by following updates from evidence-based organizations.
Identifying Major Depressive Disorder
How can nurses identify if someone has major depressive disorder?
Unfortunately, it is not possible to look at someone with the naked eye and determine if they have MDD. APRNs can identify and diagnose if someone has MDD by taking a complete health history, listening to patient's concerns, having patients complete the PHQ-9 questionnaire and communicating any concerns to other health care professionals (9).
Patient Education
What should patients know about SSRIs?
Patients should know that anyone has the possibility of experiencing side effects of SSRIs, just like any other medication. Patients should be aware that if they notice any changes in their mood, experience any sharp headaches, or feel like something is a concern, they should seek medical care. Due to social stigma associated with mental health and SSRI use, people may be hesitant to seek medical care for fear of being dismissed by health care professionals (1, 6). In addition, side effects (that interfere with the quality of life) are often normalized (1, 6). However, as more research and social movements discuss mental health and SSRI use more openly, there is more space and awareness for SSRI use and mental health.
Nurses should also teach patients to advocate for their own health in order to avoid progression of MDD and possible unwanted side effects of SSRIs. Here are important tips for patient education in the inpatient or outpatient setting.
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors)
- Tell the health care provider of any existing lifestyle concerns, such as alcohol use, other drug use, sleeping habits, diet, menstrual cycle changes (need to identify lifestyle factors that can influence SSRI use and MDD)
- Tell the health care provider if you notice any changes in your mood, behavior, sleep, sexual health (including vaginal dryness or erectile dysfunction), or weight (possible changes that could hint at more chronic side effects of SSRIs)
- Tell the health care provider if you have any changes in urinary or bowel habits, such as increased or decreased urination or defecation (potential risk for SSRI malabsorption or possible unwanted side effects)
- Tell the nurse of health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life
- Keep track of your mental health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes)
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality is a possible side effect for SSRI use)
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries
- Tell the health care provider if you notice any changes while taking medications or on other treatments to manage your MDD (potential worsening or improving mental health situation)


Self Quiz
Ask yourself...
- What are some possible ways you can obtain a detailed, patient centric health history?
- What are some possible ways APRNs can educate patients on SSRIs and major depressive disorder?
Research Findings
What Research on SSRIs exists presently?
There is extensive publicly available literature on SSRIs via the National Institutes of Health and other evidence-based journals.
What are some ways for people who take SSRIs to become a part of research?
If a patient is interested in participating in clinical trial research, they can seek more information on clinical trials from local universities and health care organizations.

Self Quiz
Ask yourself...
- What are some problems that can occur if SSRIs are not managing major depressive disorder symptoms adequately?
- What are some reasons someone might want to enroll in SSRI clinical trials?
Case Study
Case Study Part 1
Susan is a 22-year-old Black woman working as a teacher. She arrives for her annual exam at the local health department next to her place of work. She reports nothing new in her health, but she says she's been feeling more tired over the past few months. Susan reports having some trouble sleeping and trouble eating but doesn't feel too stressed overall. She heard one of her friends talking about SSRIs and wants to try them, but she's never taken prescription medications long-term before. She also thinks she might have some depression because she looked at some forums online and resonated with a lot of people's comments.

Self Quiz
Ask yourself...
- What are some specific questions you'd want to ask about her mental health?
- What are some health history questions you'd want to highlight?
- What lab work would you suggest performing?
Case Study Part 2
Susan agrees to complete bloodwork later this week and thinks she might have a family history of depression. She said that no one in her family talks about mental health, but she heard about depression from her friends recently and family a long time ago. She's back in the office a few weeks later, and her labs are within normal limits. Susan states she's still feeling fatigued and feeling a bit more hopeless these days. She denies thinking about hurting herself or others.

Self Quiz
Ask yourself...
- How would you discuss Susan's mental health concerns?
- How would you explain to Susan the influence of lifestyle, such as sleep, diet, and environment, on mood?
Case Study Part 3
Susan completed the PHQ-9 questionnaire and had a high score. After discussing her responses with her, you diagnose her with MDD. Susan admits that she is open to trying SSRIs. She is also open to seeing a therapist, as she states that she's never been to therapy. She would like resources on any therapy services, medication options, and non-pharmacological options to help her manage her condition.

Self Quiz
Ask yourself...
- Knowing Susan's concerns, what are some possible non-pharmacological management options for her MDD?
- What are some major SSRI side effects to educate Susan on?
Conclusion
Major depressive disorder is a complex chronic health condition that affects many people nationwide. SSRIs are often a first-line pharmacological option for MDD management. However, clinical presentation and symptom management with SSRIs can vary widely. While some patients would prefer a low-dose SSRI, others will need a higher dose and possible extra medication management. Education and awareness of SSRIs can influence the lives of many people.
Controlled Substances
Introduction
Pain is complex and subjective. The experience of pain can significantly impact an individual's quality of life. According to the National Institute of Health (NIH) (40), pain is the most common complaint in a primary care office, with 20% of all patients reporting pain. Chronic pain is the leading cause of disability, and effective pain management is crucial to health and well-being, particularly when it improves functional ability. Effective pain treatment starts with a comprehensive, empathic assessment and a desire to listen and understand. Nurse Practitioners are well-positioned to fill a vital role in providing comprehensive and empathic patient care, including pain management (23).
While the incidence of chronic pain has remained a significant problem, how clinicians manage pain has significantly changed in the last decade, primarily due to the opioid epidemic. This education aims to discuss pain and the assessment of pain, federal guidelines for prescribing, the opioid epidemic, addiction and diversion, and recommendations for managing pain.
Definition of Pain
Understanding the definition of pain, differentiating between various types of pain, and recognizing the descriptors patients use to communicate their pain experiences are essential for Nurse practitioners involved in pain management. By understanding the medical definition of pain and how individuals may communicate it, nurse practitioners can differentiate varying types of pain to target assessment.
According to the International Association for the Study of Pain (27), pain is "an unpleasant sensory and emotional experience associated with actual or potential tissue damage or terms of described such in damage." The IASP, in July 2020, expanded its definition of pain to include context further.
Their expansion is summarized below:
- Pain is a personal experience influenced by biological, psychological, and social factors.
- Pain cannot be inferred solely from activity in sensory neurons.
- Individuals learn the concept of pain through their life experiences.
- A person's report of an experience in pain should be respected.
- Pain usually serves an adaptive role but may adversely affect function and social and psychological well-being.
- The inability to communicate does not negate the possibility of the experience of pain.


Self Quiz
Ask yourself...
- Analyze how changes to the definition of pain may affect your practice.
- Discuss how you manage appointment times, knowing that 20% of your scheduled patients may seek pain treatment.
- How does the approach to pain management change in the presence of a person with a disability?
Types of Pain
Pain originates from different mechanisms, causes, and areas of the body. As a nurse practitioner, understanding the type of pain a patient is experiencing is essential for several reasons (23).
- Determining an accurate diagnosis. This kind of pain can provide valuable clues to the underlying cause or condition.
- Creating a treatment plan. Different types of pain respond better to specific treatments or interventions.
- Developing patient education. A nurse practitioner can provide targeted education to patients about their condition, why they may experience the pain as they do, its causes, and treatment options. Improving the patient's knowledge and control over their condition improves outcomes.
Acute Pain
Acute pain is typically short-lived and is a protective response to an injury or illness. Patients are usually able to identify the cause. This type of pain resolves as the underlying condition improves or heals (12).
Chronic Pain
Chronic pain is diagnosed when it continues beyond the expected healing time. Pain is defined as chronic when it persists for longer than three months. It may result from an underlying disease or injury or develop without a clear cause. Chronic pain often significantly impacts a person's physical and emotional well-being, requiring long-term management strategies. The prolonged experience of chronic pain usually indicates a central nervous system component of pain that may require additional treatment. Patients with centralized pain often experience allodynia or hyperalgesia (12).
Allodynia is pain evoked by a stimulus that usually does not cause pain, such as a light touch. Hyperalgesia is the effect of a heightened pain response to a stimulus that usually evokes pain (12).
Nociceptive Pain
Nociceptive pain arises from activating peripheral nociceptors, specialized nerve endings that respond to noxious stimuli. This type of pain is typically associated with tissue damage or inflammation and is further classified into somatic and visceral pain subtypes.
Somatic pain is most common and occurs in muscles, skin, or bones; patients may describe it as sharp, aching, stiffness, or throbbing.
Visceral pain occurs in the internal organs, such as indigestion or bowel spasms. It is more vague than somatic pain; patients may describe it as deep, gnawing, twisting, or dull (12).
Neuropathic pain
Neuropathic pain is a lesion or disease of the somatosensory nervous system. Examples include trigeminal neuralgia, painful polyneuropathy, postherpetic neuralgia, and central poststroke pain (10).
Neuropathic pain may be ongoing, intermittent, or spontaneous pain. Patients often describe neuropathic pain as burning, prickling, or squeezing quality. Neuropathic pain is a common chronic pain. Patients commonly describe allodynia and hyperalgesia as part of their chronic pain experience (10).
Affective pain
Affective descriptors reflect the emotional aspects of pain and include terms like distressing, unbearable, depressing, or frightening. These descriptors provide insights into the emotional impact of pain on an individual's well-being (12).

Self Quiz
Ask yourself...
- How can nurse practitioners effectively elicit patient descriptors to accurately assess the type of pain the patient is experiencing?
- Expand on how pain descriptors can guide interventions even if the cause is not yet determined.
- What strategies ensure patients feel comfortable describing their pain, particularly regarding subjective elements such as quality and location?
Case Study
Mary Adams is a licensed practical nurse who has just relocated to town. Mary will be the utilization review nurse at a local long-term care facility. Mary was diagnosed with Postherpetic Neuralgia last year, and she is happy that her new job will have her mostly doing desk work and not providing direct patient care as she had been before the relocation. Mary was having difficulty at work at her previous employer due to pain. She called into work several times, and before leaving, Mary's supervisor had counseled her because of her absences.
Mary wants to establish primary care immediately because she needs ongoing pain treatment. She is hopeful that, with her new job and pain under control, she will be able to continue a successful career in nursing. When Mary called the primary care office, she specifically requested a nurse practitioner as her primary care provider because she believes that nurse practitioners tend to spend more time with their patients.
Assessment
The assessment effectively determines the type of treatment needed, the options for treatment, and whether the patient may be at risk for opioid dependence. Since we know that chronic pain can lead to disability and pain has a high potential to negatively affect the patient's ability to work or otherwise, be productive, perform self-care, and potentially impact family or caregivers, it is imperative to approach the assessment with curiosity and empathy. This approach will ensure a thorough review of pain and research on pain management options. Compassion and support alone can improve patient outcomes related to pain management (23).
Record Review
Regardless of familiarity with the patient, reviewing the patient's treatment records is essential, as the ability to recall details is unreliable. Reviewing the records can help identify subtle changes in pain description and site, the patient's story around pain, failed modalities, side effects, and the need for education, all impacting further treatment (23).
Research beforehand the patient's current prescription and whether or not the patient has achieved the maximum dosage of the medication. Analysis of the patient's past prescription could reveal a documented failed therapy even though the patient did not receive the maximum dose (23).
A review of documented allergens may indicate an allergy to pain medication. Discuss with the patient the specific response to the drug to determine if it is a true allergy, such as hives or anaphylaxis, or if the response may have been a side effect, such as nausea and vomiting.
Research whether the patient tried any non-medication modalities for pain, such as physical therapy (PT), occupational therapy (OT), or Cognitive Behavioral Therapy (CBT). Note any non-medication modalities documented as failed therapies. The presence of any failed therapies should prompt further discussion with the patient, family, or caregiver about the experience. The incompletion of therapy should not be considered failed therapy. Explore further if the patient abandoned appointments.
Case Study
You review the schedule for the week, and there are three new patient appointments. One is Mary Adams. The interdisciplinary team requested and received Mary's treatment records from her previous primary care provider. You make 15 minutes available to review Mary's records and the questionnaire Mary filled out for her upcoming appointment. You see that Mary has been diagnosed with Postherpetic Neuralgia and note her current treatment regimen, which she stated was ineffective. You write down questions you will want to ask Mary. You do not see evidence of non-medication modalities or allergies to pain medication.

Self Quiz
Ask yourself...
- What potential risks or complications can arise from neglecting to conduct a thorough chart review before initiating a pain management assessment?
- In your experience, what evidence supports reviewing known patient records?
- What is an alternative to reviewing past treatment if records are not available?
Pain Assessment
To physically assess pain, several acronyms help explore all the aspects of the patient's experience. Acronyms commonly used to assess pain are SOCRATES, OLDCARTS, and COLDERAS. These pain assessment acronyms are also helpful in determining treatment since they include a character and duration of pain assessment (23).
| O-Onset | S-Site | C-Character |
| L-Location | O-Onset | O-Onset |
| D-Duration | C-Character | L-Location |
| C-Character | R-Radiate | D-Duration |
| A-Alleviating | A-Associated symptoms | E-Exacerbating symptoms |
| R-Radiating, relieving | T-Time/Duration | R-Relieving, radiating |
| T-Temporal patterns (frequency) | E-Exacerbating | A-Associated symptoms |
| S-Symptoms | S-Severity | S-Severity of illness |
Inquire where the patient is feeling pain. The patient may have multiple areas and types of pain. Each type and location must be explored and assessed. Unless the pain is from a localized injury, a body diagram map, as seen below, is helpful to document, inform, and communicate locations and types of pain. In cases of Fibromyalgia, rheumatoid arthritis, or other centralized or widespread pain, it is vital to inquire about radiating pain. The patient with chronic pain could be experiencing acute pain or a new pain site, such as osteoarthritis, that may need further evaluation and treatment (23).
Inquire with the patient how long their pain has been present and any associated or known causative factors. Pain experienced longer than three months defines chronic versus acute pain. Chronic pain means that the pain is centralized or a function of the Central Nervous system, which should guide treatment decisions.
To help guide treatment, ask the patient to describe their pain. The description helps identify what type of pain the patient is experiencing: Allodynia and hyperalgesia indicate centralized pain; sharp, shooting pain could indicate neuropathic pain. Have the patient rate their pain. There are various tools, as shown below, for pain rating depending on the patient's ability to communicate. Not using the pain rating number alone is imperative. Ask the patient to compare the severity of pain to a previous experience. For example, a 1/10 may be experienced as a bumped knee or bruise, whereas a 10/10 is experienced on the level of a kidney stone or childbirth (23).
Besides the 0-10 rating scale and depending on the patient's needs, several pain rating scales are appropriate. They are listed below.
The 0-5 and Faces scales may be used for all adult patients and are especially effective for patients experiencing confusion.
The Defense and Veterans Pain Rating Scale (DVPRS) is a five-item tool that assesses the impact of pain on sleep, mood, stress, and activity levels (20).
For patients unable to self-report pain, such as those intubated in the ICU or late-stage neurological diseases, the FLACC scale is practical. The FLACC scale was initially created to assess pain in infants. Note: The patient need not cry to be rated 10/10.
| Behavior | 0 | 1 | 2 |
| Face | No particular expression or smile | Occasional grimace or frown, withdrawn, disinterested | Frequent or constant quivering chin, clenched jaw |
| Legs | Normal position or relaxed | Uneasy, restless, tense | Kicking or legs drawn |
| Activity | Lying quietly, in a normal position, or relaxed | Squirming, shifting back and forth, tense | Arched, rigid, or jerking |
| Cry | No cry wake or asleep | Moans or whimpers: occasional complaints | Crying steadily, screams, sobs, frequent complaints |
| Consolability | Content, relaxed | Distractable, reassured by touching, hugging, or being talked to | Difficult to console or comfort |
(21).
Assess contributors to pain such as insomnia, stress, exercise, diet, and any comorbid conditions. Limited access to care, socioeconomic status, and local culture also contribute to the patient's experience of pain (23). Most patients have limited opportunity to discuss these issues, and though challenging to bring up, it is compassionate and supportive care. A referral to social work or another agency may be helpful if you cannot explore it fully.
Assess for substance abuse disorders, especially among male, younger, less educated, or unemployed adults. Substance abuse disorders increase the likelihood of misuse disorder and include alcohol, tobacco, cannabis, cocaine, and heroin (29).
Inquire as to what changes in function the pain has caused. One question to ask is, "Were it not for pain, what would you be doing?" As seen below, a Pain, Enjoyment, and General Activity (PEG) three-question scale, which focuses on function and quality of life, may help determine the severity of pain and the effect of treatment over time.
| What number best describes your pain on average in the past week? 0-10 |
| What number best describes how, in the past week, pain has interfered with your enjoyment of life? 0-10 |
| What number determines how, in the past week, pain has interfered with your general activity? 0-10 |
(21).
Assess family history, mental health disorders, chronic pain, or substance abuse disorders. Each familial aspect puts patients at higher risk for developing chronic pain (23).
Evaluate for mental health disorders the patient may be experiencing, particularly anxiety and depression. The Patient Health Questionnaire (PHQ4) is a four-question tool for assessing depression and anxiety.
In some cases, functional MRI or imaging studies effectively determine the cause of pain and the treatment. If further assessment is needed to diagnose and treat pain, consult Neurology, Orthopedics, Palliative care, and pain specialists (23).
Case Study
You used OLDCARTS to evaluate Mary's pain and completed a body diagram. Mary is experiencing allodynia in her back and shoulders, described as burning and tingling. It is exacerbated when she lifts, such as moving patients at the long-term care facility and, more recently, boxes from her move to the new house. Mary has also been experiencing anxiety due to fear of losing her job, the move, and her new role. She has moved closer to her family to help care for her children since she often experiences fatigue. Mary has experienced a tumultuous divorce in the last five years and feels she is still undergoing some trauma.
You saw in the chart that Mary had tried Gabapentin 300 mg BID for her pain and inquired what happened. Mary explained that her pain improved from 8/10 to 7/10 and had no side effects. Her previous care provider discontinued the medication and documented it as a failed therapy. You reviewed the minimum and maximum dosages of Gabapentin and know Mary can take up to 1800mg/day.
During the assessment, Mary also described stiffness and aching in her left knee. She gets a sharp pain when she walks more than 500 steps, and her knee is throbbing by the end of the day. Mary rated the pain a 10/10, but when she compared 10/10 to childbirth, Mary said her pain was closer to 6/10. Her moderate knee pain has reduced Mary's ability to exercise. She used to like to take walks. Mary stated she has had knee pain for six months and has been taking Ibuprofen 3 – 4 times daily.
Since Mary's pain is moderate, you evaluate your options of drugs for moderate to severe pain.


Self Quiz
Ask yourself...
- How do you assess and evaluate a patient's pain level?
- What are the different types of pain and their management strategies?
- How do you determine the appropriate dosage of pain medications for a patient?
- How do you assess the effectiveness of pain medications in your patients?
- How do you adjust medication dosages for elderly patients with pain or addiction?
- How do you address the unique challenges in pain management for pediatric patients?
- What is the role of non-pharmacological interventions in pain management?
- How do you incorporate non-pharmacological interventions into your treatment plans?
Opioid Classifications and Drug Schedules
A comprehensive understanding of drug schedules and opioid classifications is essential for nurse practitioners to ensure patient safety, prevent drug misuse, and adhere to legal and regulatory requirements. Nurse practitioners with a comprehensive understanding of drug schedules and opioid classifications can effectively communicate with colleagues, ensuring accurate medication reconciliation and facilitating interdisciplinary care. Nurse practitioners’ knowledge in facilitating discussions with pharmacists regarding opioid dosing, potential interactions, and patient education is essential (49).
Drug scheduling became mandated under the Controlled Substance Act. The Drug Enforcement Agency (DEA) Schedule of Controlled Drugs and the criteria and common drugs are listed below.
|
Schedule |
Criteria | Examples |
|
I |
No medical use; high addiction potential |
Heroin, marijuana, PCP |
|
II |
Medical use; high addiction potential |
Morphine, oxycodone, Methadone, Fentanyl, amphetamines |
|
III |
Medical use; high addiction potential |
Hydrocodone, codeine, anabolic steroids |
|
IV |
Medical use, low abuse potential |
Benzodiazepines, meprobamate, butorphanol, pentazocine, propoxyphene |
| V | Medical use; low abuse potential |
Buprex, Phenergan with codeine |
(Pain Physician, 2008)
Listed below are drugs classified by their schedule and mechanism of action. "Agonist" indicates a drug that binds to the opioid receptor, causing pain relief and also euphoria. An agonist-antagonist indicates the drug binds to some opioid receptors but blocks others. Mixed antagonist-agonist drugs control pain but have a lower potential for abuse and dependence than agonists (7).
| Schedule I | Schedule II | Schedule III | Schedule IV | Schedule V | |
| Opioid agonists |
BenzomorphineDihydromor-phone, Ketobemidine, Levomoramide, Morphine-methylsulfate, Nicocodeine, Nicomorphine, Racemoramide |
Codeine, Fentanyl, Sublimaze, Hydrocodone, Hydromorphone, Dilaudid, Meperidine, Demerol, Methadone, Morphine, Oxycodone, Endocet, Oxycontin, Percocet, Oxymorphone, Numorphan |
Buprenorphine Buprenex, Subutex, Codeine compounds, Tylenol #3, Hydrocodone compounds, Lortab, Lorcet, Tussionex, Vicodin |
Propoxyphene, Darvon, Darvocet | Opium, Donnagel, Kapectolin |
| Mixed Agonist -Antagonist | BuprenorphineNaloxone, Suboxone |
Pentazocine, Naloxone, Talwin-Nx |
|||
| Stimulants | N-methylampheta-mine 3, 4-methylenedioxy amphetamine, MDMA, Ecstacy | Amphetamine, Adderal, Cocaine, Dextroamphetamine, Dexedrine, Methamphetamine, Desoxyn, Methylphenidate, Concerta, Metadate, Ritalin, Phenmetrazine, Fastin, Preludin | Benapheta-mine, Didrex, Pemolin, Cylert, Phendimetra-zine, Plegine | Diethylpropion, Tenuate, Fenfluramine, Phentermine Fastin | 1-dioxy-ephedrine-Vicks Inhaler |
| Hallucinogen-gens, other | Lysergic Acid Diamine LSD, marijuana, Mescaline, Peyote, Phencyclidine PCP, Psilocybin, Tetrahydro-cannabinol | Dronabinol, Marinol | |||
| Sedative Hypnotics |
Methylqualine, Quaalude, Gamma-hydroxy butyrate, GHB
|
Amobarbitol, Amytal, Glutethamide, Doriden, Pentobarbital, Nembutal, Secobarbital, Seconal |
Butibarbital. Butisol, Butilbital, Florecet, Florinal, Methylprylon, Noludar |
Alprazolam, Xanax, Chlordiazepoxide, Librium, Chloral betaine, Chloral hydrate, Noctec, Chlorazepam, Clonazepam, Klonopin, Clorazopate, Tranxene, Diazepam, Valium, Estazolam, Prosom, Ethchlorvynol, Placidyl, Ethinamate, Flurazepam, Dalmane, Halazepam, Paxipam, Lorazepam, Ativan, Mazindol, Sanorex, Mephobarbital, Mebaral, Meprobamate, Equanil, Methohexital, Brevital Sodium, Methyl-phenobarbital, Midazolam, Versed, Oxazepam, Serax, Paraldehyde, Paral, Phenobarbital, Luminal, Prazepam, Centrax, Temazepam, Restoril, Triazolam, Halcion, Sonata, Zolpidem, Ambien |
Diphenoxylate preparations, Lomotil |
(41).

Self Quiz
Ask yourself...
- What are the potential risks and benefits of using opioids for pain management?
- How can nurse practitioners effectively monitor patients on long-term opioid therapy?
- What are the potential risks and benefits of using long-acting opioids for chronic pain?
- How do you monitor patients on long-acting opioids for safety and efficacy?
Commonly Prescribed Opioids, Indications for Use, and Typical Side Effects
Opioid medications are widely used for managing moderate to severe pain. Referencing NIDA (2023), this section aims to give healthcare professionals an overview of the indications and typical side effects of commonly prescribed Schedule II opioid medications, including hydrocodone, oxycodone, morphine, Fentanyl, and hydromorphone.
Opioids are derived and manufactured in several ways. Naturally occurring opioids come directly from the opium poppy plant. Synthetic opioids are manufactured by chemically synthesizing compounds that mimic the effects of a natural opioid. Semi-synthetic is a mix of naturally occurring and man-made (35).
Understanding the variations in how an opioid is derived and manufactured is crucial in deciding the type of opioid prescribed, as potency and analgesic effects differ. Synthetic opioids are often more potent than naturally occurring opioids. Synthetic opioids have a longer half-life and slower elimination, affecting the duration of action and timing for dose adjustments. They are also associated with a higher risk of abuse and addiction (38).
Hydrocodone
Mechanism of Action and Metabolism
Hydrocodone is a Schedule II medication. It is an opioid agonist and works as an analgesic by activating mu and kappa opioid receptors located in the central nervous system and the enteric plexus of the bowel. Agonist stimulation of the opioid receptors inhibits nociceptive neurotransmitters' release and reduces neuronal excitability (17).
- Produces analgesia.
- Suppresses the cough reflex at the medulla.
- Causes respiratory depression at higher doses.
Hydrocodone is indicated for treating severe pain after nonopioid therapy has failed. It is also indicated as an antitussive for nonproductive cough in adults over 18.
Available Forms
Hydrocodone immediate release (IR) reaches maximum serum concentrations in one hour with a half-life of 4 hours. Extended-release (ER) Hydrocodone reaches peak concentration at 14-16 hours and a half-life of 7 to 9 hours. Hydrocodone is metabolized to an inactive metabolite in the liver by cytochrome P450 enzymes CYP2D6 and CYP3A4. Hydrocodone is converted to hydromorphone and is excreted renally. Plasma concentrations of hydromorphone are correlated with analgesic effects rather than hydrocodone.
Hydrocodone is formulated for oral administration into tablets, capsules, and oral solutions. Capsules and tablets should never be crushed, chewed, or dissolved. These actions convert the extended-release dose into immediate release, resulting in uncontrolled and rapid release of opioids and possible overdose.
Dosing and Monitoring
Hydrocodone IR is combined with acetaminophen or ibuprofen. The dosage range is 2.5mg to 10mg every 4 to 6 hours. If formulated with acetaminophen, the dosage is limited to 4gm/day.
Hydrocodone ER is available as tablets and capsules. Depending on the product, the dose of hydrocodone ER formulations in opioid-naïve patients is 10 to 20 mg every 12 to 24 hours.
Nurse practitioners should ensure patients discontinue all other opioids when starting the extended-release formula.
Side Effects and Contraindications
Because mu and kappa opioid receptors are in the central nervous system and enteric plexus of the bowel, the most common side effects of hydrocodone are constipation and nausea (>10%).
Other adverse effects of hydrocodone include:
- Respiratory: severe respiratory depression, shortness of breath
- Cardiovascular: hypotension, bradycardia, peripheral edema
- Neurologic: Headache, chills, anxiety, sedation, insomnia, dizziness, drowsiness, fatigue
- Dermatologic: Pruritus, diaphoresis, rash
- Gastrointestinal: Vomiting, dyspepsia, gastroenteritis, abdominal pain
- Genitourinary: Urinary tract infection, urinary retention
- Otic: Tinnitus, sensorineural hearing loss
- Endocrine: Secondary adrenal insufficiency (17)
Hydrocodone, being an agonist, must not be taken with other central nervous system depressants as sedation and respiratory depression can result. In formulations combined with acetaminophen, hydrocodone can increase the international normalized ratio (INR) and cause bleeding. Medications that induce or inhibit cytochrome enzymes can lead to wide variations in absorption.
The most common drug interactions are listed below:
- Alcohol
- Benzodiazepines
- Barbiturates
- other opioids
- rifampin
- phenytoin
- carbamazepine
- cimetidine,
- fluoxetine
- ritonavir
- erythromycin
- diltiazem
- ketoconazole
- verapamil
- Phenytoin
- John’s Wort
- Glucocorticoids
Considerations
Use with caution in the following:
- Patients with Hepatic Impairment: Initiate 50% of the usual dose
- Patients with Renal Impairment: Initiate 50% of the usual dose
- Pregnancy: While not contraindicated, the FDA issued a black-boxed warning since opioids cross the placenta, and prolonged use during pregnancy may cause neonatal opioid withdrawal syndrome (NOWS).
- Breastfeeding: Infants are susceptible to low dosages of opioids. Non-opioid analgesics are preferred.
Pharmacogenomic: Genetic variants in hydrocodone metabolism include ultra-rapid, extensive, and poor metabolizer phenotypes. After administration of hydrocodone, hydromorphone levels in rapid metabolizers are significantly higher than in poor metabolizers.
Oxycodone
Mechanism of Action and Metabolism
Oxycodone has been in use since 1917 and is derived from Thebaine. It is a semi-synthetic opioid analgesic that works by binding to mu-opioid receptors in the central nervous system. It primarily acts as an agonist, producing analgesic effects by inhibiting the transmission of pain signals (Altman, Clark, Huddart, & Klein, 2018).
Oxycodone is primarily metabolized in the liver by CYP3A4/5. It is metabolized in the liver to noroxycodone and oxymorphone. The metabolite oxymorphone also has an analgesic effect and does not inhibit CYP3A4/5. Because of this metabolite, oxycodone is more potent than morphine, with fewer side effects and less drug interactions. Approximately 72% of oxycodone is excreted in urine (Altman, Clark, Huddart, & Klein, 2018).
Available Forms
Oxycodone can be administered orally, rectally, intravenously, and as an epidural. For this sake, we will focus on immediate-release and extended-release oral formulations.
- Immediate-release (IR) tablets
- IR capsules
- IR oral solutions
- Extended-release (ER) tablets
Dosing and Monitoring
The dosing of oxycodone should be individualized based on the patient's pain severity, previous opioid exposure, and response. Initial dosages for opioid naïve patients range from 5-15 mg for immediate-release formulations, while extended-release formulations are usually initiated at 10-20 mg. Dosage adjustments may be necessary based on the patient's response, but caution should be exercised. IR and ER formulations reach a steady state at 24 hours and titrating before 24 hours may lead to overdose.
Regular monitoring is essential to assess the patient's response to treatment, including pain relief, side effects, and signs of opioid misuse or addiction. Monitoring should include periodic reassessment of pain intensity, functional status, and adverse effects (Altman, Clark, Huddart, & Klein, 2018).
Side Effects and Contraindications
Common side effects of oxycodone include:
- constipation
- nausea
- sedation
- dizziness
- respiratory depression
- respiratory arrest
- hypotension
- fatal overdose
Oxycodone is contraindicated in patients with known hypersensitivity to opioids, severe respiratory depression, paralytic ileus, or acute or severe bronchial asthma. It should be used cautiously in patients with a history of substance abuse, respiratory conditions, liver or kidney impairment, and those taking other medications that may interact with opioids, such as alcohol (4).
It is also contraindicated with the following medications and classes:
- Antifungal agents
- Antibiotics
- Rifampin
- Carbamazepine
- Fluoxetine
- Paroxetine
Considerations
- Nurse practitioners should consider the variations in the mechanism of action for the following:
- Metabolism differs between males and females: females have been shown to have less concentration of oxymorphone and more CYP3A4/5 metabolites.
- Infants have reduced clearance of oxycodone, increasing side effects.
- Pediatrics have 20-40% increased clearance over adults.
- Reduced clearance with age increases the half-life of oxycodone.
- Pregnant women have a greater clearance and reduced half-life.
- Impairment of the liver reduces clearance.
- Cancer patients with cachexia have increased exposure to oxycodone and its metabolite.
- Maternal and neonate concentrations are similar, indicating placenta crossing (4)
Morphine

Mechanism of Action and Metabolism
Morphine is a naturally occurring opioid alkaloid extracted from the opium poppy. It was isolated in 1805 and is the opioid against which all others are compared. Morphine binds to mu-opioid receptors in the brain and spinal cord, inhibiting the transmission of pain signals and producing analgesia. It is a first-line choice of opioid for moderate to severe acute, postoperative, and cancer-related pain (8).
Morphine undergoes first-pass metabolism in the liver and gut. It is well absorbed and distributed throughout the body. Its main metabolites are morphine-3-glucuronide and morphine-6-glucuronide. Its mean plasma elimination half-life after intravenous administration is about 2 hours. Approximately 90% of morphine is excreted in the urine within 24 hours (8).
Available Forms
Morphine is available in various forms, including.
- immediate-release tablets
- extended release tablets
- oral IR solutions
- injectable solutions
- transdermal patches
Dosing and Monitoring
Morphine is hydrophilic and, as such, has a slow onset time. The advantage of this is that it is unlikely to cause acute respiratory depression even when injected. However, because of the slow onset time, there is more likelihood of morphine overdose due to the ability to “stack” doses in patients experiencing severe pain (Bistas, Lopez-Ojeda, & Ramos-Matos, 2023).
The dosing of morphine depends on the patient's pain severity, previous opioid exposure, and other factors. It is usually initiated at a low dose and titrated upwards as needed. Monitoring pain relief, adverse effects, and signs of opioid toxicity is crucial. Reevaluate benefits and harms with patients within 1 to 4 weeks of starting opioid therapy or of dose escalation. General recommendations for initiating morphine (Bistas, Lopez-Ojeda, & Ramos-Matos, 2023).
Prescribe IR opioids instead of ER opioids.
Prescribe the lowest effective dosage, below 50 Morphine Milligram Equivalents (MME) /day.
Side Effects and Contraindications
Because morphine binds to opioid receptors in the brain and spinal cord, is metabolized in the liver and gut, and has a slow onset, the following side effects are common:
- Constipation
- Nausea
- Vomiting
- Sedation
- Dizziness
- Respiratory depression
- Pruritis
- Sweating
- Dysphoria/Euphoria
- Dry mouth
- Anorexia
- Spasms of urinary and biliary tract
Contraindications of morphine are:
- Known hypersensitivity or allergy to morphine.
- Bronchial asthma or upper airway obstruction
- Respiratory depression in the absence of resuscitative equipment
- Paralytic ileus
- Risk of choking in patients with dysphagia, including infants, children, and the elderly (8)
Concurrent use with other sedating medications: Amitriptyline, diazepam, haloperidol, chlorpromazine
Morphine interacts with the following medications:
- Ciprofloxacin
- Metoclopramide
- Ritonavir
Considerations for Nurse Practitioners
Assess for medical conditions that may pose serious and life-threatening risks with opioid use, such as the following:
- Sleep-disordered breathing, such as sleep apnea.
- Pregnancy
- Renal or hepatic insufficiency
- Age >= 65
- Certain mental health conditions
- Substance use disorder
- Previous nonfatal overdose
Fentanyl
Mechanism of Action and Metabolism
Fentanyl is a synthetic opioid more potent than morphine and was approved in 1968. Fentanyl is an agonist that works by binding to the mu-opioid receptors in the central nervous system. This binding inhibits the transmission of pain signals, resulting in analgesia. Fentanyl is often used for severe pain management, particularly in the perioperative and palliative care settings, or for severe pain in patients with Hepatic failure (8).
It is a mu-selective opioid agonist. However, it can activate other opioid receptors in the body, such as the delta and kappa receptors, producing analgesia. It also activates the Dopamine center of the brain, stimulating relaxation and exhilaration, which is responsible for its high potential for addiction (8).
Indications for fentanyl are as follows:
- Preoperative analgesia
- Anesthesia adjunct
- Regional anesthesia adjunct
- General anesthesia
- Postoperative pain control
- Moderate to severe acute pain (off-label)
Available Forms
- Fentanyl is available in various forms, including:
- transdermal patches
- injectable solutions
- lozenges
- nasal sprays
- oral tablets (8)
Dosing and Monitoring
Fentanyl is metabolized via the CYP3A4 enzyme in the liver. It has a half-life of 3 to 7 hours, and 75% of Fentanyl is excreted in the urine and 9% in feces.
The dosing of fentanyl depends on the route of administration and the patient's needs. For example, transdermal patches are typically applied every 72 hours, while injectable solutions are titrated to achieve the desired analgesic effect. Monitoring should include assessing pain levels, respiratory rate, blood pressure, and sedation scores (8).
Fentanyl is most dosed as follows:
- Post-operative pain control
- 50 to 100 mcg IV/IM every 1 to 2 hours as needed; alternately 0.5 to 1.5 mcg/kg/hour IV as needed. Consider lower dosing in patients 65 and older.
PCA (patient-controlled analgesia): 10 to 20 mcg IV every 6 to 20 minutes as needed; start at the lowest effective dose for the shortest effective duration - refer to institutional protocols (8).
Moderate to severe acute pain (off-label) 1 to 2 mcg/kg/dose intranasally each hour as needed; the maximum dose is 100 mcg. Use the lowest effective dose for the shortest effective duration (8).
Side Effects and Contraindications
Common side effects of fentanyl include:
- respiratory depression
- sedation
- constipation
- nausea
- vomiting
- euphoria
- confusion
- respiratory depression/arrest
- visual disturbances
- dyskinesia
- hallucinations
- delirium
- narcotic ileus
- muscle rigidity
- addiction
- loss of consciousness
- hypotension
- coma
- death (8).
The use of fentanyl is contraindicated in patients in the following situations:
- After operative interventions in the biliary tract, these may slow hepatic elimination of the drug.
- With respiratory depression or obstructive airway diseases (i.e., asthma, COPD, obstructive sleep apnea, obesity hyperventilation, also known as Pickwickian syndrome)
- With liver failure
- With known intolerance to fentanyl or other morphine-like drugs, including codeine or any components in the formulation.
- With known hypersensitivity (i.e., anaphylaxis) or any common drug delivery excipients (i.e., sodium chloride, sodium hydroxide) (8).
Considerations for Nurse Practitioners
Nurse practitioners prescribing fentanyl should thoroughly assess the patient's pain, medical history, and potential risk factors for opioid misuse. They should also educate patients about the proper use, storage, and disposal of fentanyl. It should be used cautiously in patients with respiratory disorders, liver or kidney impairment, or a history of substance abuse. Fentanyl is contraindicated in patients with known hypersensitivity to opioids and those without exposure to opioids.
Alcohol and other drugs, legal or illegal, can exacerbate fentanyl's side effects, creating multi-layered clinical scenarios that can be complex to manage. These substances, taken together, generate undesirable conditions that complicate the patient's prognosis (8).
Hydromorphone
Mechanism of Action and Metabolism
Hydromorphone is a semi-synthetic opioid derived from morphine. It binds to the mu-opioid receptors in the central nervous system. It primarily exerts its analgesic effects by inhibiting the release of neurotransmitters involved in pain transmission, thereby reducing pain perception. Hydromorphone also exerts its effects centrally at the medulla level, leading to respiratory depression and cough suppression (1).
Hydromorphone is indicated for:
- moderate to severe acute pain
- severe chronic pain
- refractory cough suppression (off-label) (1)
Available Forms
Hydromorphone is available in various forms, depending on the patient’s needs and severity of pain.
- immediate-release tablet
- extended release tablets
- oral liquid
- injectable solution
- rectal suppositories
Dosing and Monitoring
The immediate-release oral formulations of hydromorphone have an onset of action within 15 to 30 minutes. Peak levels are typically between 30 and 60 minutes with a half-life of 2 to 3 hours. Hydromorphone is primarily excreted through the urine.
The dosing of hydromorphone should be individualized based on the patient's pain intensity, initiated at the lowest effective dose, and adjusted gradually as needed. Close monitoring of pain relief, adverse effects, and signs of opioid toxicity is essential. Patients should be assessed regularly to ensure they receive adequate pain control without experiencing excessive sedation or respiratory depression.
The following are standard dosages that should only be administered when other opioid and non-opioid options fail.
- Immediate-release oral solutions dosage: 1 mg/1 mLoral tablets are available in 2 mg, 4 mg, and 8 mg.
- Extended-release oral tablets are available in dosages of 8 mg, 12 mg, 16 mg, and 32 mg.
- Injection solutions are available in concentrations of 1 mg/mL, 2 mg/mL, 4 mg/mL, and 10 mg/mL.
- Intravenous solutions are available in strengths of 2 mg/1 mL, 2500 mg/250 mL, ten mg/1 mL, and 500 mg/50 mL.
- Suppositories are formulated at a strength of 3 mg (1).
Side Effects and Contraindications
Hydromorphone has potential adverse effects on several organ systems, including the integumentary, gastrointestinal, neurologic, cardiovascular, endocrine, and respiratory.
Common side effects of hydromorphone include:
- Constipation
- Nausea
- Vomiting
- Dizziness
- Sedation
- respiratory depression
- pruritus
- headache
- Somnolence
- Severe adverse effects of hydromorphone include:
- Hypotension
- Syncope
- adrenal insufficiency
- coma
- raised intracranial pressure.
- seizure
- suicidal thoughts
- apnea
- respiratory depression or arrest
- drug dependence or withdrawal
- neonatal drug withdrawal syndrome
- Hydromorphone is contraindicated in patients with:
- known allergies to the drug, sulfites, or other components of the formulation.
- known hypersensitivity to opioids.
- severe respiratory depression
- paralytic ileus
- acute or severe bronchial asthma (1).
Caution should be exercised in patients with:
- respiratory insufficiency
- head injuries
- increased intracranial pressure.
- liver or kidney impairment.
Considerations for Nurse Practitioners
As nurse practitioners, it is crucial to assess the patient's pain intensity and overall health status before initiating Hydromorphone. Start with the lowest effective dose and titrate carefully for optimal pain control. Regular monitoring for adverse effects, signs of opioid toxicity, and therapeutic response is essential. Educate patients about the potential side effects, proper dosing, and the importance of not exceeding prescribed doses. Additionally, nurse practitioners should be familiar with local regulations and guidelines regarding opioid prescribing and follow appropriate documentation and monitoring practices.
Additional Considerations
In terminal cancer patients, clinicians should not restrain opioid therapy even if signs of respiratory depression become apparent.
Hydromorphone requires careful administration in cases of concurrent psychiatric illness.
Specific Patient Considerations:
- Hepatic impairment and Renal Impairment: Initiate hydromorphone treatment at one-fourth to one-half of the standard starting dosage, depending on the degree of impairment.
- Pregnancy considerations: Hydromorphone can traverse the placental barrier and induce NOWS.
- Breastfeeding considerations: Nonopioid analgesic agents are preferable for breastfeeding women.
- Older patients: hydromorphone is categorized as a potentially inappropriate medication for older adults (1).
Tramadol

Mechanism of Action and Metabolism
Tramadol is a Schedule IV opioid medication with a higher potential for dependency and misuse than non-opioid medications. It binds to opioid receptors in the central nervous system, inhibiting the reuptake of norepinephrine and serotonin. It also has weak mu-opioid receptor agonist activity.
The liver metabolizes tramadol mediated by the cytochrome P450 pathways (particularly CYP2D6) and is mainly excreted through the kidneys.
Tramadol is used for moderate to severe pain.
Available Forms of Tramadol include:
- Immediate-release-typically used for acute pain management.
- Extended-release-used for chronic pain.
Dosing and Monitoring
Tramadol has an oral bioavailability of 68% after a single dose and 90–100% after multiple doses and reaches peak concentrations within 2 hours. Approximately 75% of an oral dose is absorbed, and the half-life of tramadol is 9 hours (18).
Tramadol dosing should be individualized based on the patient's pain severity and response.
The initial dose for adults is usually 50-100 mg orally every 4-6 hours for pain relief. The maximum daily dose is 400 mg for immediate-release formulations and 300 mg for extended-release formulations (18).
It is essential to monitor the patient's pain intensity, response to treatment, and any adverse effects. Regular reassessment and adjustment of the dosage may be necessary.
Side Effects and Contraindications
Tramadol is responsible for severe intoxications leading to consciousness disorder (30%), seizures (15%), agitation (10%), and respiratory depression (5%). The reactions to Tramadol suggest that the decision to prescribe should be carefully considered.
Common Side Effects of Tramadol Include:
- Nausea
- Vomiting
- Dizziness
- Constipation
- Sedation
- Headache
- CNS depression
- Seizure
- Agitation
- Tachycardia
- Hypertension
- reduced appetite
- pruritus and rash
- gastric irritation
Serious side effects include:
- respiratory depression
- serotonin syndrome
- seizures
Contraindications
Tramadol is contraindicated in patients with:
- history of hypersensitivity to opioids
- acute intoxication with alcohol
- opioids, or other psychoactive substances
- Patients who have recently received monoamine oxidase inhibitors (MAOIs)
Additionally, the following can be observed in tramadol intoxication:
- miosis
- respiratory depression
- decreased level of consciousness
- hypertension
- tremor
- irritability
- increased deep tendon reflexes
Poisoning leads to:
- multiple organ failure
- coma
- cardiopulmonary arrest
- death
Considerations for Nurse Practitioners
Tramadol has been increasingly misused with intentional overdoses or intoxications. Suicide attempts were the most common cause of intoxication (52–80%), followed by abuse (18–31%), and unintentional intoxication (1–11%). Chronic tramadol or opioid abuse was reported in 20% of tramadol poisoning cases. Fatal tramadol intoxications are uncommon except when ingested concurrent with depressants, most commonly benzodiazepines and alcohol (18).
Tramadol poisoning can affect multiple organ systems:
- gastrointestinal
- central nervous system: seizure, CNS depression, low-grade coma, anxiety, and over time anoxic brain damage
- Cardiovascular system: palpitation, mild hypertension to life-threatening complications such as cardiopulmonary arrest
- respiratory system
- renal system: renal failure with higher doses of tramadol intoxication
- musculoskeletal system: rhabdomyolysis
- endocrine system: hypoglycemia, serotonin syndrome (18)
Cannabis
Mechanism of Action and Metabolism
Cannabis is classified as a Schedule I status. It contains various cannabinoids, with delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) being the most studied. THC primarily acts on cannabinoid receptors in the brain, producing psychoactive effects, while CBD has more diverse effects on the nervous system. These cannabinoids interact with the endocannabinoid system, modulating neurotransmitter release and influencing various physiological processes (32).
Similar to opioids, cannabinoids are synthesized and released in the body by synapses that act on the cannabinoid receptors present in presynaptic endings (32). They perform the following actions related to analgesia:
- Decrease the release of neurotransmitters.
- Activate descending inhibitory pain pathways.
- Reduce postsynaptic sensitivity and alleviate neural inflammation.
- Modulate CB1 receptors within central nociception processing areas and the spinal cord, resulting in analgesic effects.
- Attenuate inflammation by activating CB2 receptors (32).
- Emerging research shows cannabis is indicated for:
- Migraines
- chronic pain
- back pain
- arthritic pain
- pain associated with cancer and surgery.
- neuropathic pain
- diabetic neuropathic pain when administered early in the disease progression.
- sickle cell disease
- cancer
- inflammatory bowel disease (32)
Available Forms
Cannabis refers to products sourced from the Cannabis sativa plant. There are differences between cannabis, cannabinoids, and cannabidiol (CBD). Cannabinoids are extracted from the cannabis plants. Cannabinoid-based treatments, such as dronabinol and CBD, are typically approved medical interventions for specific indications. THC (9-tetrahydrocannabinol) is the psychoactive component of the cannabis plant. CBD is a non-psychoactive component (32).
Cannabis can be consumed in different forms, each with a different onset and duration. Patients may have individual preferences, including:
- smoking/vaporizing dried flowers.
- consuming edibles
- tinctures or oils
- applying topicals (32)
Dosing and Monitoring
Inhaling marijuana via the lungs by smoking or vaping causes maximum plasma concentration within minutes. Psychiatric effects begin within seconds to a few minutes after inhalation and peak after 15 to 30 minutes. The effect diminishes throughout 2 to 3 hours (32).
Oral ingestion of marijuana causes psychiatric effects that typically occur between 30 and 90 minutes and reach maximum effect after 2 to 3 hours. Ingested marijuana effects last about 4 to 12 hours (32).
Dosing cannabis is challenging due to variations in potency and individual responses. Start with low doses and titrate slowly to achieve the desired effect while minimizing side effects. Regular monitoring is crucial, including assessing symptom relief, adverse effects, and potential drug interactions. Encourage patients to keep a diary to track their cannabis use and its effects (32).
Side Effects and Contraindications
Cannabis can exacerbate mental health conditions such as anxiety and psychosis. Common side effects of cannabis include (32):
- Dizziness
- dry mouth
- increased heart rate
- impaired memory
- psychoactive effects
Contraindications include:
- Pregnancy
- Breastfeeding
- heart disease
- respiratory conditions
- history of substance abuse
- mental health disorders

Self Quiz
Ask yourself...
- How do you address patients' misconceptions about pain medications?
- What are the mechanisms of action for commonly prescribed pain medications?
- How do these mechanisms of action contribute to pain relief?
- What are the potential side effects and risks associated with commonly prescribed pain medications?
- How do you educate patients about the risks and benefits of pain medications?
- How do you manage patients who require high-dose opioids for pain management?
- Is medical cannabis legal in your State? If yes, are you familiar with the prescribing guidelines?
- Do you have any personal biases against the use of medical cannabis? Why or why not?
Case Study
Mary is agreeable to trying an increased dose of Gabapentin. Mary would also like to see a counselor to discuss her past and get help with her anxiety. You made an appointment for Mary to see a Licensed Clinical Social Worker in your clinic.
You read the side effects and warnings for Gabapentin, and it is unsafe to use Gabapentin and Tramadol together since they are both depressants. You order a non-steroidal drug for Mary's somatic knee pain and make a consult for imaging studies on her left knee. You also make a referral to Orthopedics.
You educated Mary about the side effects of Gabapentin and scheduled a follow-up appointment. The day after Mary began her treatment with the increased Gabapentin, you called Mary to follow up on its effect. Mary still has pain, but she is not having any untoward side effects. Gabapentin may not work immediately so you will schedule a follow-up call in 3 days.


Self Quiz
Ask yourself...
- In this case study, Mary has insurance. How might your practice be different were Mary not insured?
- In your experience, what are the possible reasons for Mary's knee pain not being a part of her previous treatment record?
- Consider how your assessment of Mary's needs differs from the above-mentioned case study.
- Explain the rationale for decisions made by the nurse practitioner in the case study mentioned above and if your decisions would differ.
Opioid Use, the Opioid Epidemic, and Statistics
The use and misuse of opioids has become a pressing public health concern, leading to a global epidemic. The history of opioid use, the opioid epidemic, and associated statistics provide essential context for healthcare professionals in addressing this public health crisis. More importantly, it is estimated that 1 in 4 patients receiving prescription opioids in primary care settings will misuse them. In addition, 50% of opioid prescriptions are written by primary care providers, including nurse practitioners (22). Understanding the factors contributing to the epidemic and the magnitude of its impact is crucial for effective prevention, intervention, and treatment strategies.
History of Opioid Use
Opioids have a long history of medicinal use, dating back to ancient civilizations. They have been a drug of choice for pain relief for thousands of years. The introduction of synthetic opioids in the 19th century, such as morphine and later heroin, revolutionized pain management. However, their potential for addiction and misuse soon became apparent (16).
The Opioid Epidemic
The opioid epidemic refers to the surge in opioid misuse, addiction, and overdose deaths. The epidemic gained momentum in the late 1990s with increased prescribing of opioids for chronic pain (43).
No doubt, increased prescribing put opioids in the hands of consumers, but increased prescribing resulted from a multifactorial influence. One of the main influences was aggressive marketing by pharmaceutical companies, which has been well publicized. However, due to the long history of underprescribing pain medications for fear of misuse and addiction, the medical community was primed to expand its opioid prescribing practices (31).
A historical event that increased comfort with prescribing opioids, in the writer's opinion, was the introduction of the Medicare Hospice Benefit in 1986. Medical directors must be contracted or employed by hospices, and these medical directors had or soon gained pain management expertise. To further promote hospice and effective pain management, the hospice medical directors, with newly acquired skills, provided education throughout medical communities about pain management and specifically to decrease the fear of using opioids. Pharmacies and attending physicians grew accustomed to giving opioids for home use. Hospice care is for terminally ill patients, defined as a life expectancy of 6 months or less. Still, the reality is that hospice discharges 12 to 40% of patients for ineligibility and other reasons.
A more prominent factor in increasing opioid prescribing was the 1996 American Pain Society's introduction of pain as "the 5th Vital sign." Soon after, The Joint Commission promoted pain as "the 5th Vital Sign" and began compliance surveys in healthcare organizations requiring pain assessment details to be as prominent as blood pressure and heart rate. The Joint Commission cited a quote from 1968 by a nurse from the University of California Los Angeles, Margo McCaffrey, who defined pain as "…Whatever the experiencing person says it is, existing whenever s/he says it does." The Joint Commission accreditation programs pursued pain management as part of the accreditation process throughout its healthcare accreditation programs, including hospice accreditation by 1989 per TJC Timeline (48).
The National Institute of Health published an article about the Joint Commission's role in the opioid epidemic, particularly regarding the definition of pain, "This definition emphasizes that pain is a subjective experience with no objective measures. It also stresses that the patient, not the clinician, is the authority on the pain and that their self-report is the most reliable indicator of pain. This set the tone for clinicians: Patients are always to be trusted to report pain accurately” (45).
Statistics on the Opioid Epidemic
In the United States alone, over 500,000 people died from opioid overdoses between 1999 and 2017. The number of opioid-related overdose deaths continues to increase, with synthetic opioids, mainly illicitly manufactured Fentanyl, playing a significant role in recent years (46). Fentanyl-laced drugs, such as marijuana, are increasingly sold knowing and unknowingly to introduce medications with a high addiction rate, thus creating new consumers. This practice can potentially increase deaths due to the imprecise nature of manufacturing (16).
Opioid-related hospitalizations have also risen substantially. In 2014, there were approximately 1.27 million hospitalizations related to opioids in the United States. These hospitalizations not only place a burden on healthcare systems but also reflect the severe consequences of opioid misuse (3).


Self Quiz
Ask yourself...
- Have you experienced changes to your practice because of the opioid epidemic? If so, what are the changes?
- What is your opinion on the validity of Margo McCaffrey's definition of pain?
- What factors influence your willingness or unwillingness to prescribe opioids?
Federal Regulations on Opioid Prescribing
The history of substance use disorder prevention that promotes opioid recovery and treatment for patients and communities can be traced back to the early 20th century. However, the current approach to addressing opioid addiction and promoting healing has evolved significantly in recent times (36).
In the early 1900s, health professionals treated opioid addiction with punitive measures, including incarceration and moralistic approaches. The focus was on punishing individuals rather than providing effective treatment. This approach persisted for several decades until the mid-20th century when the medical community started recognizing addiction as a medical condition rather than a moral failing (36).
The Controlled Substances Act (CSA), introduced in 1970, was a response to increasing drug abuse and illicit drug trafficking in the United States. The CSA is a federal law regulating the manufacture, possession, distribution, and use of certain substances, including drugs and medications, that can potentially cause abuse and dependence. Its primary purpose is to combat drug abuse, reduce drug-related crimes, and protect public health and safety. The Drug Enforcement Agency (DEA) plays a crucial role in enforcing the CSA by monitoring and controlling controlled substance production, distribution, and use (31).
In the 1990s, the significant increase in opioid prescribing, leading to a surge in opioid addiction and overdose deaths, prompted a shift in focus toward prevention. Efforts were made to educate healthcare providers about the risks of overprescribing opioids and to implement prescription drug monitoring programs to track and prevent abuse (36).
The Comprehensive Addiction and Recovery Act (CARA) was signed into law in 2016 to expand access to treatment and recovery services for opioid addiction. This legislation allocated funding for prevention, treatment, recovery, and support services while promoting evidence-based practices and programs (36).
The Centers for Disease Control and Prevention (CDC) published guidelines in 2016 for prescribing opioids for chronic pain, which was updated in 2022. These guidelines emphasize the importance of non-opioid alternatives, using the lowest effective dose for the shortest duration, and assessing the benefits and risks of continued opioid therapy (13).
Furthermore, the Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT) was signed into law in 2018, providing additional resources to address the opioid crisis. This legislation expanded access to medication-assisted treatment (MAT), increased the availability of naloxone, a medication used to reverse opioid overdose, and enhanced support for recovery housing (36).
In recent years, there has been a growing recognition of the importance of a comprehensive approach to opioid addiction, including harm reduction strategies, increased access to naloxone, and the integration of mental health services. Communities and organizations have been working together to address the underlying issues contributing to addiction, such as poverty, trauma, and social determinants of health (50).
Overall, the history of substance use disorder prevention that promotes opioid recovery and treatment has evolved from a punitive approach to a more compassionate and evidence-based model. Efforts are now focused on prevention, early intervention, and expanding access to comprehensive treatment and support services for individuals and communities affected by opioid addiction (36).
The most current federal regulations on opioid prescribing for healthcare providers are the amendments to the CSA in 2018, which added new rules to limit the quantity and duration of opioid prescriptions for acute pain to seven days. In 2022, the CDC updated recommendations to the Clinical Practice Guidelines for Prescribing Opioids for Pain.
The 2022 CDC guidelines are summarized below (13):
- Non-opioid therapies should be considered the first-line treatment for chronic pain.
- Establish clear treatment goals with patients, including realistic pain management and functional improvement expectations.
- Conduct a thorough risk assessment for potential harms before initiating opioid therapy.
- When opioids are used, start with the lowest effective dose and consider immediate-release opioids instead of extended-release or long-acting opioids.
- Prescribe the lowest effective dose for the shortest duration possible, typically three days or less and rarely exceeding seven days.
- Reassess benefits and risks within one day after prescribing opioids, including checking the prescription drug monitoring database.
- Avoid prescribing opioids and benzodiazepines concurrently whenever possible due to the increased risk of overdose and death.
- Offer naloxone to patients at increased risk of opioid overdose, including those with a history of overdose, substance use disorder, or concurrent benzodiazepine use.
- When opioids are no longer needed, taper the dose gradually to minimize withdrawal symptoms.
- Arrange an evidence-based treatment for patients with opioid use disorder, including medication-assisted treatment (Naltrexone, Buprenorphine, or Methadone).

Self Quiz
Ask yourself...
- What are the guidelines general for prescribing opioids for acute pain?
- How do these guidelines differ for chronic pain management?
- Discuss how federal regulations impact the practice of nurse practitioners in terms of opioid prescribing.
- Describe the potential benefits and challenges nurse practitioners face when adhering to federal regulations on opioid prescribing.
- How can nurse practitioners navigate and stay updated with evolving federal regulations surrounding opioid prescribing to ensure safe and effective care?
- How do you ensure appropriate documentation when prescribing controlled substances?
Safe Prescribing and Prescription Monitoring Program
Prescription Drug Monitoring Programs (PDMP) are state-run electronic databases that track.
the prescribing and dispensing of controlled substances. PDMPs are designed to improve patients.
care and safety by giving clinicians access to patients' prescription histories, allowing them to make informed decisions when prescribing controlled substances. PDMPs help identify patients at risk of substance misuse or prescription drug overdose. They also enable clinicians to identify potential drug interactions and prevent opioid diversion (14).
PDMPs collect and store data from pharmacies and prescribers in a centralized database. Clinicians can access this database to review a patient's prescription history, including the types of medications prescribed, the prescribers involved, and the dispensing pharmacies (14).
In many states, PDMP use is mandated by law, and nurse practitioners may be required to register and use the system. It is essential to understand state-specific laws and regulations regarding PDMP use.
PDMPs have some limitations, such as incomplete data or delays in reporting. The CDC emphasizes that clinicians should use PDMP data for their clinical assessment and other relevant information to make informed decisions about prescribing controlled substances. Still, PDMP cannot be used as the sole basis for denying or providing treatment (14).
Case Study
After five days on Gabapentin, Mary was doing well, and her neuropathic pain had decreased to 3/10. However, Mary suffered a fall after her knee "gave out" and injured her knee and back. She was in severe pain, and her family drove her to the ER. The ER doctors saw Mary, and orthopedics were consulted. Mary has surgery scheduled for a knee replacement a week from now.
Mary was prescribed Vicodin because she was in excruciating pain, but her prescription only allowed enough medication for two days. Mary has made an appointment with you to renew her prescription.
You evaluate Mary because you know that concomitant use of Gabapentin and opioids puts Mary at risk for respiratory depression and possible side effects, including accidental overdose.
Mary stated she has been more alert the past 24 hours and is afraid her functional status will continue to decline if she does not have more Vicodin because the pain in her back and knee makes it difficult to stand. You assess Mary. Mary stated she occasionally drinks alcohol but has not had a drink since she moved. She has no familial history of substance abuse or mental health disorders.
Mary's mother stayed at her house to help her for the first 24 hours after Mary's return from the ER, but Mary is providing her care now.
You check the PDMP database and see that Mary was prescribed eight pills she has taken over the last 48 hours.
Since the Vicodin has been effective without untoward side effects, and Mary's function is improving, you decide to refill the prescription of Vicodin. You will taper the dose to three Vicodin daily for two days and two for one day. Mary will be near her appointment for a knee replacement as well.


Self Quiz
Ask yourself...
- What are the potential benefits and drawbacks of using PDMPs in your practice?
- How can PDMPs help you identify potential drug abuse or diversion cases among your patients? Can you provide examples from your own experience?
- In what ways do PDMPs impact your decision-making process when prescribing controlled substances?
- What are the key considerations when prescribing controlled substances?
- How do you ensure responsible prescribing practices for controlled substances?
Preventing Opioid Use Disorder
As previously discussed, opioid addiction is a growing concern worldwide, affecting individuals from all walks of life. According to the CDC, "Anyone who takes prescription opioids can become addicted to them" (14).
As frontline healthcare professionals, nurse practitioners must recognize the signs of opioid addiction to provide timely intervention and support. This section will outline the key indicators of opioid addiction.
Physical Symptoms
Physical symptoms are often the first noticeable signs of opioid addiction. These symptoms may include constricted pupils, drowsiness, slurred speech, impaired coordination, and increased sensitivity to pain. Additionally, individuals struggling with opioid addiction may exhibit frequent flu-like symptoms, such as a runny nose, sweating, itching, or gastrointestinal issues.
Behavioral Changes
Opioid addiction can significantly impact an individual's behavior. These may include increased secrecy, frequent requests for early prescription refills, doctor shopping (seeking prescriptions from multiple healthcare providers), neglecting personal hygiene, and experiencing financial difficulties due to excessive spending on opioids (37).

Social Isolation
Opioid addiction often leads to social withdrawal and isolation. Individuals struggling with opioid addiction may distance themselves from family, friends, and social activities they once enjoyed. They may exhibit erratic mood swings, become defensive or hostile when confronted about their drug use, and display a general lack of interest in previously important activities (30).
Psychological Changes
The psychological impact of opioid addiction is significant. Individuals with opioid addiction may exhibit increased anxiety, depression, irritability, and restlessness. They may also experience cognitive impairments, memory lapses, and difficulties in decision-making. Healthcare professionals should be attentive to these changes, as they can indicate opioid addiction (51).
Tolerance and Withdrawal Symptoms
The development of tolerance and withdrawal symptoms are critical signs of opioid addiction. Individuals may require increased dosages of opioids to achieve the desired effect, indicating a growing tolerance. Furthermore, withdrawal symptoms such as muscle aches, nausea, vomiting, insomnia, and intense cravings for opioids may occur when the drug is discontinued or reduced abruptly (51).

Self Quiz
Ask yourself...
- Discuss how nurse practitioners can contribute to preventing opioid use disorder.
- Explain how nurse practitioners effectively communicate the risks and signs of opioid misuse without stigmatizing or alienating patients.
- What are the signs of opioid addiction or misuse in patients?
- How do you approach patients who may be at risk for opioid addiction?
- How do you ensure appropriate documentation when prescribing controlled substances?
Opioid Overdose
The management of opioid overdose, withdrawal, and addiction requires a comprehensive approach that combines pharmacological interventions with psychosocial support. Naloxone remains a vital tool for reversing opioid overdose, while medications such as Methadone, buprenorphine, and naltrexone play crucial roles in withdrawal and addiction treatment (National Institute of Health, 2023). Nurse practitioners must stay vigilant and informed about the evolving landscape of medications. This section aims to provide a comprehensive review of medications and treatment strategies for opioid overdose, withdrawal, and addiction and is excerpted from the NIH (40).
Naloxone
Mechanism of Action and Metabolism
Naloxone is an opioid receptor antagonist. It works by binding to opioid receptors and displacing any opioids present, thereby reversing the effects of opioid overdose. It has a higher affinity for opioid receptors than most opioids, effectively blocking their action.
Naloxone is indicated for emergency intervention of opioid overdose. It effectively reverses respiratory depression and other life-threatening effects. Studies suggest the potential benefits of combining naloxone with other medications, such as buprenorphine (see below), to improve outcomes. Initiatives promoting community-based naloxone distribution programs have shown promising results in reducing opioid-related deaths.
Available Forms
Naloxone is available in various formulations:
- Intranasal
- Intramuscular
- Intravenous
- auto-injectors.
The most used form is the intranasal spray, which is easy to administer and requires no specialized training. Intranasal naloxone formulations have gained popularity due to their ease of use and increased availability. A recent study showed that the non-FDA-approved compound spray was far less effective than either FDA compound (15).
Dosing and Monitoring
The recommended initial dose of naloxone for opioid overdose is 2mg intranasally or 0.4mg to 2mg intramuscularly or intravenously. If the patient does not respond within 23- minutes, additional doses may be administered every 2-3 minutes. Continuous monitoring of the patient's respiratory status is essential, as repeat doses may be required due to the short half-life of naloxone.
Side Effects and Contraindications
Naloxone has been shown not to affect individuals without opioids in their system.
Common side effects of naloxone include
- Withdrawal symptoms: increased heart rate, sweating, and agitation
- nausea
- vomiting
- headache
Contraindications include known hypersensitivity to naloxone and situations where the use of naloxone may be unsafe or not feasible.
Considerations for Nurse Practitioners
Fentanyl and other opioids have a rapid onset, and the need to act quickly is paramount. As mentioned previously, the ease of use and higher plasma concentrations using the FDA-approved 4-mg FDANxSpray device compared with the locally compounded nasal sprays should be considered when ordering Naloxone (15).
Fentanyl and other potent synthetic opioids may require multiple administrations of naloxone to achieve reversal of an overdose (Chiang, Gyaw, & Krieter, 2019). As a nurse practitioner prescribing naloxone, it is crucial to assess the patient's risk factors for opioid overdose, such as a history of substance use disorder or chronic pain management. Education regarding the proper administration of naloxone should be provided to the patients and their caregivers. Additionally, it is essential to provide resources for follow-up care, including addiction treatment and ongoing support.
Methadone
Mechanism of Action and Metabolism
Methadone is a long-acting opioid agonist that effectively suppresses withdrawal symptoms and reduces cravings. It binds to the same opioid receptors in the brain as other opioids. It relieves withdrawal symptoms and reduces cravings by blocking the euphoric effects of opioids, thus helping individuals with opioid dependence to achieve stability (33).
Available Forms
Methadone is available in oral tablets and liquid formulations. The oral tablet is the most used form and is typically administered once daily (33).
Dosing and Monitoring
Methadone dosing is individualized based on the patient's response and needs. Initially, the dose often started low and gradually increased until the patient reached a stable dose. Dosing may need to be adjusted based on the patient's response, adherence, and any changes in their overall health. Regularly monitoring the patient's vital signs, urine drug screens, and assessment of their withdrawal symptoms and cravings is essential.
Side Effects and Contraindications
Common side effects of methadone include:
- Constipation
- dry mouth
- drowsiness
- sweating
- weight gain
- respiratory depression
Contraindications include:
- known hypersensitivity to methadone
- severe asthma
- respiratory depression
- certain heart conditions (33).
Considerations for Nurse Practitioners
As a nurse practitioner prescribing methadone, conducting a comprehensive assessment of the patient's medical history, current medications, and substance use history is crucial. Opioid treatment programs or specialized clinics are often involved in methadone treatment, so collaboration and coordination of care with these programs are essential. Regularly monitoring the patient's progress, adherence, and potential side effects or drug interactions is essential. Additionally, providing education on the risks and benefits of methadone and the importance of adherence to the prescribed regimen is crucial for successful treatment outcomes.
Buprenorphine
Mechanism of Action and Metabolism
Buprenorphine is a partial opioid agonist with a ceiling effect that minimizes the risk of overdose while reducing withdrawal symptoms. Buprenorphine is a partial opioid agonist that binds to the same receptors as other opioids but produces a weaker response. It has a high affinity for the mu-opioid receptors, which helps reduce cravings and withdrawal symptoms in individuals with opioid dependence.
Available Forms
Buprenorphine is available in different formulations, including sublingual tablets, buccal films, and extended-release injections. The sublingual tablets have different strengths, such as 2mg, 4mg, 8mg, and 12mg. Buprenorphine is taken as a daily tablet or weekly or monthly injection.
Dosing and Monitoring
The dosing of buprenorphine varies depending on the individual's opioid dependence severity and treatment phase. Initially, a low dose (e.g., 2-4mg) is given, and it may gradually increase to a maintenance dose of 8-24 mg daily. Regular monitoring is essential to assess the patient's response, adherence, and potential side effects.
Side Effects and Contraindications
Common side effects of buprenorphine include:
- Constipation
- Nausea
- Headache
- Insomnia
- Sweating
Serious side effects are rare but can include:
- Respiratory depression
- Allergic reactions
Buprenorphine is contraindicated in individuals with:
- Severe respiratory insufficiency
- Acute intoxication with opioids
- Known hypersensitivity
Considerations for Nurse Practitioners
Nurse practitioners can prescribe buprenorphine for opioid dependence treatment under the Drug Addiction Treatment Act (DATA). To become eligible, they must complete specific training requirements and obtain a waiver from the Substance Abuse and Mental Health Services Administration (SAMHSA). Nurse practitioners should assess patients thoroughly, including their opioid use history, comorbidities, and medication compatibility, while ensuring appropriate counseling and referral for comprehensive treatment (40).
Clonidine + Lofexidine
Mechanism of Action and Metabolism:
Both Clonidine and Lofexidine are alpha-2 adrenergic agonists. They work by stimulating alpha-2 receptors in the brain, which reduces sympathetic outflow and norepinephrine release. This results in decreased sympathetic activity, leading to various effects such as reduced blood pressure, decreased heart rate, and alleviated withdrawal symptoms (28).
Available Forms
Clonidine is available in oral tablets and patches. Lofexidine is available in oral tablets and is taken as needed (40).
Dosing and Monitoring
For opioid withdrawal, the Clonidine dose ranges from 0.1-0.3 mg every 4-6 hours. Lofexidine is usually initiated at 0.53 mg three times daily, and the dose can be increased to 2.88 mg daily. Monitoring blood pressure and heart rate is essential during treatment (40).
Side Effects and Contraindications:
Common side effects of both medications include:
- dry mouth
- sedation
- dizziness
- constipation
- orthostatic hypotension (40).
Both medications are contraindicated in patients with:
- Hypotension
- Bradycardia
- heart block
- history of hypersensitivity to the drugs (40).
Considerations for Nurse Practitioners:
An early study of lofexidine vs. clonidine for withdrawal symptoms showed that treatment with lofexidine resulted in lower withdrawal symptoms, fewer mood problems, less sedation, and hypotension. There were no significant differences in craving levels, morphine metabolites in urine, or dropout rates when both were compared.
Lofexidine can be a safe option for outpatient treatment as it does not lead to hypotension. However, nurse practitioners must closely monitor patients' blood pressure and heart rate during treatment and educate them about possible side effects. If patients experience any concerning symptoms, they should inform their nurse practitioner immediately.
Gradual dose reduction of Clonidine is crucial to prevent rebound hypertension. Before prescribing either medication, nurse practitioners should assess for any contraindications or potential drug interactions (19).
Emerging Therapies for Withdrawal
Extended-release naltrexone: Naltrexone is an opioid receptor antagonist that blocks the effects of opioids, reducing the risk of relapse. It is taken as a monthly injection.
Alpha-2 adrenergic agonists: Emerging evidence suggests the potential use of dexmedetomidine and guanfacine for managing opioid withdrawal symptoms.
Medication-Assisted Treatment (MAT):
Methadone was introduced in the 1960s and marked a significant turning point in opioid addiction treatment or MAT. Along with counseling and behavioral therapies, MAT became the cornerstone of opioid addiction recovery.
Examples of medications used:
- Methadone
- Buprenorphine:
- Naltrexone:
Adjunctive Pharmacotherapies:
Antidepressants: Selective serotonin reuptake inhibitors and tricyclic antidepressants may help manage co-occurring depression and anxiety.
Anticonvulsants:
Medications like Gabapentin and pregabalin show promise in reducing opioid cravings and improving treatment outcomes.


Self Quiz
Ask yourself...
- What are the mechanisms of action for commonly prescribed addiction medications?
- What are the potential risks and benefits of using benzodiazepines for pain management?
- How do you assess and manage patients with co-occurring pain and substance use disorders?
- What are the guidelines for prescribing addiction medications like buprenorphine or methadone?
- How do these medications work in the treatment of opioid use disorder?
- What are the potential side effects and risks associated with addiction medications?
- How do you support patients in their recovery from opioid use disorder?
- How do you address patients' concerns and fears about addiction medications?
- What are the federal guidelines around prescribing addiction medications for nurse practitioners?
- How do these guidelines influence your prescribing practices?
Other Substance Use Disorders
Patients in pain may struggle with Substance Use Disorders other than Opioid Use Disorder. Substance use disorders may often occur with mental health conditions such as anxiety, depression, and bipolar disorder. In addition, many individuals engage in polydrug use. Understanding the most common Substance Use Disorders aids in a comprehensive assessment of the patient and the development of appropriate treatment plans (28).
Alcohol Use Disorder (AUD):
The prevalence of AUD worldwide was estimated to be 9.8% in men and 5.5% in women in 2016 (28).
Cannabis Use Disorder (CUD):
the prevalence of CUD in the United States increased from 2.18% in 2001-2002 to 2.89% in 2012-2013. (28).
Cocaine Use Disorder:
According to the National Survey on Drug Use and Health (NSDUH), in 2019, approximately 1.9 million Americans aged 12 or older had cocaine use disorder in the past year (44).
Methamphetamine Use Disorder:
A study published in Drug and Alcohol Dependence reported that the prevalence of methamphetamine use disorder in the United States was estimated to be 0.2% in 2015-2016 (6).

Self Quiz
Ask yourself...
- What are the options available for managing opioid addiction and withdrawal?
- How can nurse practitioners support patients in their recovery from opioid addiction?
- What strategies can nurse practitioners employ to effectively engage and build trust with patients reluctant to disclose or seek help for substance abuse disorders?
- How can nurse practitioners collaborate with other healthcare professionals and community resources to provide comprehensive care and support for patients with substance abuse disorders?
- What techniques or tools can nurse practitioners employ to start these sensitive conversations with new patients?
- How do you assess and manage patients experiencing opioid withdrawal symptoms?
- What are the non-pharmacological interventions for managing opioid withdrawal?
- How do you educate patients about the risks and benefits of addiction medications?
- How do you monitor patients on addiction medications for adherence and progress?
- What are the drug potential interactions with commonly prescribed addiction medications?
Drug Diversion and Illegal opioids
Misuse of opioids is facilitated by diversion and is defined as "the transfer of drugs from lawful to unlawful use" (24). Most commonly, this occurs when family and friends share prescribed opioids with other family and friends. Opioids and other controlled drugs are also diverted from healthcare facilities. Statistics show that healthcare facility diversion has increased since 2015 (24)
Diversion affects patients, healthcare workers, healthcare facilities, and public health. Patients experience substandard care due to ineffective pain management and impaired healthcare workers. In addition, affected patients are at risk of infections from compromised syringes (24).
Healthcare employees who divert are at risk of overdose and death. If caught, they face criminal prosecution and malpractice suits. Healthcare facilities also bear the cost of diverted drugs via internal investigations, follow-up care for affected patients, regulatory fines for inadequate safeguards, and declining public trust (24).
Despite the enormous consequences of drug diversion, healthcare facilities have implemented few processes to detect and deter the diversion of controlled substances (24).

Self Quiz
Ask yourself...
- What protocols can nurse practitioners implement to prevent drug diversion within their healthcare setting?
Patient Teachings and Considerations
Opioids have significant side effects and carry a risk of addiction and overdose. Nurse practitioners can decrease the risks of misuse and addiction by educating patients on appropriate disposal, safe storage, and potential signs of addiction. Taking additional time to provide teaching nurse practitioners can promote patient safety, informed decision-making, and responsible opioid use.
Safe Storage and Disposal:
- Teach patients to store opioids securely, out of reach of children, pets, visitors, and non-caregiver family members, to prevent accidental ingestion or misuse (13). Only the caregiver, if applicable, or the patient should have access to pain medications.
- Instruct patients on proper disposal methods, such as using drug take-back programs or mixing opioids with undesirable substances (e.g., coffee grounds) before throwing them away (11) (13).
Medication Adherence:
- Emphasize the importance of taking opioids as prescribed, at the correct dose and frequency, to achieve optimal pain relief.
- Encourage patients to notify their healthcare provider if they experience inadequate pain control or side effects (35).
Potential Side Effects:
- Educate patients about common side effects of opioids, including constipation, nausea, sedation, and respiratory depression.
- Discuss strategies to manage side effects, such as maintaining adequate hydration, consuming a fiber-rich diet, and using over-the-counter laxatives as needed (11).
Risk of Dependence and Addiction:
- Explain the potential for opioid dependence and addiction, especially with long-term use or a history of substance abuse.
- Encourage patients to promptly report signs of opioid misuse, such as craving, loss of control, or continued use despite negative consequences (51).

Avoiding Alcohol and Other Central Nervous System Depressants:
- Instruct patients to avoid consuming alcohol or other medications that can enhance the sedative effects of opioids, increasing the risk of respiratory depression.
- Advise patients to contact the Nurse Practitioner before starting new medications, including over-the-counter drugs or herbal supplements (2).
Driving and Operating Machinery:
- Inform patients about the potential impairment caused by opioids, including reduced alertness, reaction time, and coordination.
- Advise patients to avoid driving or operating heavy machinery while taking opioids until they know how the medication affects them (14).

Self Quiz
Ask yourself...
- What strategies can nurse practitioners employ to effectively communicate the risks and benefits of opioid use while ensuring they clearly understand the potential side effects and the importance of adhering to the prescribed regimen?
- How can nurse practitioners promote patient engagement and shared decision-making regarding opioid pain management, considering the potential for dependence and addiction?
- How can nurse practitioners assess a patient's knowledge and understand the safe storage and disposal of opioids?
Case Study
You take some extra time with Mary to educate her on the taper dose of Vicodin, the potential for harm, and the risk of opioids, especially when used concomitantly with Gabapentin. You let Mary know it is unsafe to use alcohol, not only with Vicodin but also with Gabapentin. You let Mary know that Vicodin has a risk of dependency and misuse and, therefore, she will be monitored carefully. You also educate that Mary should store the Vicodin away from visibility by anyone but herself since she can self-administer her medication. You let Mary know that Vicodin can cause constipation and that she should increase her water intake and take a stool softener.
You ask Mary to call you if her pain is not adequately relieved or if her medications run out before the three days.
You let Mary know that if she does stop taking the Vicodin before she has completed all the medication, she should dispose of it by mixing the pills with liquid and coffee grounds to make them unpalatable to animals and others.
Mary complied with your education, completed her course of Vicodin, and was scheduled for surgery. Mary's social worker helped her communicate with her new employer and delayed her start date until after her recovery.
During her recovery, Mary received physical therapy and a short course of pain medication managed by her orthopedist.
Mary returned to the clinic for a follow-up visit after completing her therapy and before starting work. Mary's pain level in her knee is 3/10, and she already feels like she can walk further than pre-surgery. Gabapentin has continued to help Mary's neuropathic pain in her back, and she reports 2/10. Mary looks forward to beginning her new job and is optimistic about the future.
Conclusion
Pain management is the leading cause of primary care appointments and chronic pain is the leading cause of disability. Yet, prescribing opioids for primary care patients is also a factor in drug misuse and the opioid epidemic. Nurse practitioners are challenged to appropriately treat pain and effectively control diversion, addiction, and death from overdose.
It is imperative that nurse practitioners use evidence-based practices to assess, appropriately intervene, and educate about the benefits and potential harm caused by treatment with opioids. Nurse practitioners must stay up to date with the current federal regulations regarding PDMPs, clinical prescribing guidelines, and emerging treatments for pain and opioid abuse disorders.
References + Disclaimer
- American Nurses Association. (2015). Code of ethics with interpretative statements. Silver Spring, MD: Author. Available from URL: http://www.nursingworld.org/MainMenuCategories/EthicsStandards/CodeofEthicsforNurses/Code-of1.
- Texas Administrative Code, RULE §216.3 Continuing Competency Requirements. Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=N&p_rloc=193277&p_tloc=&p_ploc=1&pg=85&p_tac=&ti=22&pt=11&ch=216&rl=3
- Texas Administrative Code, RULE §217.1 Nursing Jurisprudence Exam (NJE). Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=P&p_rloc=123209&p_tloc=&p_ploc=1&pg=111&p_tac=&ti=22&pt=11&ch=216&rl=3
- Texas Administrative Code, RULE 217.11 Standards of Nursing Practice. Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=N&p_rloc=113468&p_tloc=&p_ploc=1&pg=103&p_tac=&ti=22&pt=11&ch=216&rl=3
- Texas Administrative Code, RULE §217.12 Unprofessional Conduct. Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=N&p_rloc=133132&p_tloc=&p_ploc=1&pg=104&p_tac=&ti=22&pt=11&ch=216&rl=3
- Texas Board of Nursing, Nursing Board Position Statements. Available from URL: https://www.bon.texas.gov/practice_bon_position_statements_content.asp#15.28
- Texas Board of Nursing, Professional Boundaries Including the Use of Social Media by Nurses. Available from URL: https://www.bon.texas.gov/practice_bon_position_statements_content.asp#15.28
- Texas Board of Nursing, Rule §213.33(b)-Texas Board of Nursing Disciplinary Matrix. Available from URL: https://www.bon.texas.gov/pdfs/disciplinaryaction_pdfs/discp-matrix.pdf
- Texas Board of Nursing, Texas Board of Nursing Position Statement. Available from URL: https://www.bon.texas.gov/pdfs/practice_dept_pdfs/position_statements_pdfs/15.28mar20.pdf
- Texas Board of Nursing, Texas Board of Nursing – Practice – Registered Nurse Scope of Practice. Available from URL: https://www.bon.texas.gov/practice_scope_of_practice_rn.asp
- Texas Board of Nursing, The Registered Nurse Scope of Practice. Available from URL: https://www.bon.texas.gov/practice_bon_position_statements_content.asp#15.28
- Texas Board of Nursing Website, Available from URL: bon.texas.gov
- (2003) Institute on Domestic Violence and sexual assault. The University of Texas at Austin A Health survey of Texans: A focus on Sexual Assault Retrieved from: https://sites.utexas.edu/idvsa/?s=focus+on+sexual+assault
- (2015) The University of Texas. Stephen Hicks school of Social Work HEALTH AND WELL-BEING: Texas Statewide Sexual Assault Prevalence Study Final Report Retrieved from: https://sites.utexas.edu/idvsa/files/2019/03/TX-SA-Prevalence-Study-Final-Report.pdf
- (2015) National Alliance to End Sexual Violence. The Costs and Consequences of Sexual Violence and Cost-Effective Solutions. Retrieved from: https://endsexulavilolence.org/where_we_stand/costs-consequences-and-solutions
- (2021) Miller, Ted R; Cohen, Mark A; Wiersema, Brian; Victim Costs and Consequences: A New Look National Institutes of Justice Retrieved from: https://www.ojp.gov/pdffiles/victcost.pdf
- Office of Justice Programs. Office of Victims of Crime. SANE Program Development and Operation Guide. Retrieved from: https://www.ovcttac.gov/saneguide/introduction/what-is-a-sane
- Prescott Valley, Arizona official government site. Retrieved from: https://www.pvaz.net/DocumentCenter/View/8943/Common-Feelings-of-Survivors-of-Sexual-Assault
- RAINN articles: What is a SANE/SART? Retrieved from: https://www.rainn.org/articles/what-sanesart
- Texas A&M, College of Nursing, et al. Texas Attorney General Sexual Assault Prevention and Crisis Services Program. TEXAS EVIDENCE COLLECTION PROTOCOL Retrieved from: https://nursing.tamu.edu/documents/txecp-final-08212019.pdf
- Texas Legislature Online. Evidence Collection Protocol Kits. Retrieved from: https://statutes.capitol.texas.gov/Docs/GV/htm/GV.420.htm
- (2021) RAINN state database, Texas. Understanding Statute of Limitations of Sex Crimes Retrieved from: https://apps.rainn.org/policy/policy-crime-definitions.cfm?state=Texas&group=7
- RAINN. Stat Pearls. What is a Sexual Assault Forensic Exam? Retrieved from: https://rainn.org/articles/rape-kit 3/2/2021
- (2020) Slate, Melissa, RN, BA, MA, Forensic Evidence Collection for Nurses. Retrieved from: https://www.Rn.org/courses/coursematerial-173.pdf
- Victims of Trafficking and Violence Protection Act of 2000, Pub. L. No. 106-386 (2000). https://www.govinfo.gov/content/pkg/PLAW-106publ386/pdf/PLAW-106publ386.pdf
- 22 U.S. Code § 7102—Definitions. (n.d.). LII / Legal Information Institute. https://www.law.cornell.edu/uscode/text/22/7102
- Homeland Security. (2022). What Is Human Trafficking? https://www.dhs.gov/blue-campaign/what-human-trafficking
- United States Department of Defense (n.d.) Trafficking in Persons 101. https://ctip.defense.gov/Portals/12/Trafficking_in_Persons_101_Fact_Sheet_2020.pdf
- National Human Trafficking Hotline. (2023). Myths & Facts. https://humantraffickinghotline.org/en/human-trafficking/myths-facts
- United States Department of State (2022). Understanding Human Trafficking. https://www.state.gov/what-is-trafficking-in-persons/
- Department of Health and Human Services USA (2017). FACT SHEET: Human Trafficking. https://www.acf.hhs.gov/sites/default/files/documents/otip/fact_sheet_human_trafficking_fy18.pdf
- United States Department of Labor (2022). 2022 List of Goods Produced by Child Labor or Forced Labor. https://www.dol.gov/sites/dolgov/files/ILAB/child_labor_reports/tda2021/2022-TVPRA-List-of-Goods-v3.pdf
- Homeland Security. (2022). What is Forced Labor? https://www.dhs.gov/blue-campaign/forced-labor
- United States Department of State (n.d.). What Is Modern Slavery? https://www.state.gov/what-is-modern-slavery/#recruitment
- Polaris Project (2021). Human Trafficking 101. https://polarisproject.org/human-trafficking-101/
- Polaris Project (2023). Vulnerabilities and Recruitment. https://polarisproject.org/vulnerabilities-and-recruitment/
- Polaris Project (2023). Love and Trafficking. https://polarisproject.org/love-and-trafficking/
- National Human Trafficking Hotline (2023). Recognizing the Signs. https://humantraffickinghotline.org/en/human-trafficking/recognizing-signs
- National Human Trafficking Hotline (2023). Human Trafficking. https://humantraffickinghotline.org/en/human-trafficking
- Texas Attorney General (n.d.). Red Flags for Labor Trafficking. https://www.texasattorneygeneral.gov/human-trafficking-section/signs-trafficking/red-flags-labor-trafficking
- United Against Human Trafficking (2020). Prostitution and Human Trafficking: What’s the Difference? https://uaht.org/prostitution-and-human-trafficking/
- United States Department of State (2020). 2020 Trafficking in Persons Report. https://www.state.gov/wp-content/uploads/2020/06/2020-TIP-Report-Complete-062420-FINAL.pdf
- National Human Trafficking Resource Center (n.d.). Recognizing and Responding to Human Trafficking in a Healthcare Context. https://humantraffickinghotline.org/sites/default/files/Recognizing%20and%20Responding%20to%20Human%20Trafficking%20in%20a%20Healthcare%20Context_pdf.pdf
- Mukherji, P. (2015). Recognizing Human Trafficking Victims in the Emergency Department. Emergency Medicine Reports. https://www.reliasmedia.com/articles/134799-recognizing-human-trafficking-victims-in-the-emergency-department
- Hachey, L. M., & Phillippi, J. C. (2017). Identification and Management of Human Trafficking Victims in the Emergency Department. Advanced Emergency Nursing Journal, 39(1), 31–51. https://doi.org/10.1097/TME.0000000000000138
- Office for Victims of Crime Training and Technical Assistance Center (2012). Human Trafficking. https://www.ovcttac.gov/downloads/resourceLibrary/General/Color_HumanTraffickingResourcePaper12_final_508c_9132012.pdf
- Human Trafficking Institute (2019). On this day in history: The Trafficking Victims Protection Act passed in Congress. https://traffickinginstitute.org/on-this-day-in-history-the-trafficking-victims-protection-act-passed-in-congress/
- Office of the High Commissioner for Human Rights (2000). Protocol to Prevent, Suppress and Punish Trafficking in Persons Especially Women and Children, supplementing the United Nations Convention against Transnational Organized Crime. https://www.ohchr.org/en/instruments-mechanisms/instruments/protocol-prevent-suppress-and-punish-trafficking-persons
- Alliance to End Slavery and Trafficking (ATEST). (2017). Summary of the Trafficking Victims Protection Act (TVPA) and Reauthorizations FY 2017. https://endslaveryandtrafficking.org/summary-trafficking-victims-protection-act-tvpa-reauthorizations-fy-2017-2/
- Child Welfare Information Gateway (2023). Human Trafficking and Child Welfare: A Guide for Caseworkers. https://www.childwelfare.gov/pubPDFs/trafficking_caseworkers.pdf
- Polaris Project (2018). On-ramps, intersections, and exit routes: A roadmap for systems and industries to prevent and disrupt human trafficking. Health Care. https://polarisproject.org/wp-content/uploads/2018/08/A-Roadmap-for-Systems-and-Industries-to-Prevent-and-Disrupt-Human-Trafficking-Health-Care.pdf
- Office for Victims of Crime Training and Technical Assistance Center (n.d.) Human Trafficking Task Force e-Guide. https://www.ovcttac.gov/taskforceguide/eguide/3-operating-a-task-force/34-addressing-common-operational-challenges/interpreters/
- National Human Trafficking Training and Technical Assistance Center (n.d.). Barriers that prevent identification. https://nhttac.acf.hhs.gov/soar/eguide/observe/Barriers_to_Screening_and_Responding
- National Human Trafficking Training and Technical Assistance Center (n.d.). Language accessibility communication and language assistance. https://nhttac.acf.hhs.gov/soar/eguide/ask/Language%20Accessibility
- Substance Abuse and Mental Health Services Administration (2022). Trauma and violence. (2022) https://www.samhsa.gov/trauma-violence
- SAMHSA’s Trauma and Justice Strategic Initiative (2014). SAMHSA’s concept of trauma and guidance for a trauma-informed approach
- National Human Trafficking Training and Technical Assistance Center (2018). Adult human trafficking screening tool and guide. https://nhttac.acf.hhs.gov/sites/default/files/2018-07/adult_human_trafficking_screening_tool_and_guide.pdf
- National Human Trafficking Hotline (2008). Potential indicators of human trafficking https://humantraffickinghotline.org/en/resources/potential-indicators-human-trafficking
- National Human Trafficking Training and Technical Assistance Center (n.d.). Create and maintain safety. https://nhttac.acf.hhs.gov/soar/eguide/ask/Safety_is_Top_Priority
- Toney-Butler, T. J., Ladd, M., & Mittel, O. (2023). Human Trafficking. Stat Pearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK430910/
- Baldwin, S.B., Barrows, J., Stoklosa, H. (2017). Protocol Toolkit for Developing a Response to Victims of Human Trafficking. HEAL Trafficking & Hope for Justice. https://healtrafficking.org/wp-content/uploads/2022/08/HEAL-Trafficking-Protocol-Toolkit.pdf
- Texas Constitution and Statues (2015). Human Resources Code, Chapter 48: Investigations and protective services for elderly persons and persons with disabilities. https://statutes.capitol.texas.gov/Docs/HR/htm/HR.48.htm
- Texas Constitution and Statutes (2023). Family Code, Title 5: The parent-child relationship and the suit affecting the parent-child relationship. https://statutes.capitol.texas.gov/Docs/FA/htm/FA.261.htm
- Texas Health and Human Services Commission (2016). Welcome to the Texas Department of Family Abuse Hotline Website. https://www.txabusehotline.org/Login/Default.aspx
- Texas Human Trafficking Prevention Task Force (2014). Introduction to Human Trafficking: A Guide for Texas Education Professionals. https://www.texasattorneygeneral.gov/sites/default/files/files/divisions/criminal-justice/IntroHumanTrafficking2014.pdf
- National Human Trafficking Training and Technical Assistance Center (n.d.). Law Enforcement. https://nhttac.acf.hhs.gov/soar/eguide/resources_by_profession/Law_Enforcement
- Center for Substance Abuse Treatment (US) (2014). Trauma-Informed Care in Behavioral Health Services. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); Treatment Improvement Protocol (TIP) Series, No. 57.) Chapter 3, Understanding the Impact of Trauma. https://www.ncbi.nlm.nih.gov/sites/books/NBK207191/
- Treatment (US), C. for S. A. (2014). Understanding the Impact of Trauma. In Trauma-Informed Care in Behavioral Health Services. Substance Abuse and Mental Health Services Administration (US). https://www.ncbi.nlm.nih.gov/sites/books/NBK207191/
- Survivor Alliance (n.d.) Overview for Survivors. https://www.survivoralliance.org/survivors-overview
- Dovydaitis T. (2010). Human trafficking: the role of the health care provider. J Midwifery Women’s Health: 55(5):462-7. Doi: 10.1016/j.jmwh.2009.12.017. PMID: 20732668; PMCID: PMC3125713.
- Texas Health and Human Services (2023). Texas Human Trafficking Resource Center https://www.hhs.texas.gov/services/safety/texas-human-trafficking-resource-center
- US Department of Health & Human Services. (n.d.). Multidisciplinary Treatment and Referral Team. https://nhttac.acf.hhs.gov/soar/eguide/resources/Building_a_Referral_Network
- SimpliMBA (2023). SWOT Analysis. Retrieved from https://www.simplimba.com/swot-analysis-for-personal-development/
- Legal Information Institute. (n.d.). Advocate. Cornell Law School. https://www.law.cornell.edu/wex/advocate
- Morris, G. (2023, June 20). How nurses can advocate for patients. https://nursejournal.org/articles/how-to-advocate-for-patients/
- The National Council on Aging. (n.d.). Get the facts on elder abuse. https://www.ncoa.org/article/get-the-facts-on-elder-abuse
- Clark, A. (2023, August 24). 2023 Elder Abuse Statistics. https://www.theseniorlist.com/caregiving/elder-abuse/statistics/
- Nursing Home Abuse Center. (2023, November 17). Nursing home abuse and neglect statistics explained. https://www.nursinghomeabusecenter.com/nursing-home-abuse/statistics/#:~:text=Emotional%20Nursing%20Home%20Abuse%20Statistics&text=According%20to%20a%20survey%20of,during%20a%2012%2Dmonth%20period.
- World Health Organization (WHO). (2022, June 13). Abuse of older people. https://www.who.int/news-room/fact-sheets/detail/abuse-of-older-people
- The National Council on Aging. (n.d.). Get the facts on elder abuse. https://www.ncoa.org/article/get-the-facts-on-elder-abuse
- Elder Abuse Guide for Law Enforcement (EAGLE). (n.d.). Recognizing elder abusers – a guide for law enforcement. https://eagle.usc.edu/law-enforcement-resources/recognizing-abusers/
- American Psychological Association. (2022). Elder abuse: How to spot warning signs, get help, and report mistreatment. https://www.apa.org/topics/aging-older-adults/elder-abuse
- World Health Organization: WHO. (2022, October 1). Ageing and health. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
- Carlson, K. (2023, September 8). Understanding a nurse’s role as a mandated reporter. https://nursejournal.org/resources/understanding-nurses-role-as-a-mandated-reporter/#:~:text=What%20types%20of%20abuse%20are,who%20have%20experienced%20sexual%20abuse.
- Digital Communications Division (DCD). (2022, December 9). How do I report elder abuse or abuse of an older person or senior? U.S. Department of Health and Human Services. https://www.hhs.gov/answers/programs-for-families-and-children/how-do-i-report-elder-abuse/index.html
- https://www.nursingworld.org/~4af078/globalassets/docs/ana/ethics/endoflife-positionstatement.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3241064/
- https://www.aafp.org/fpm/2008/0300/p18.html
- Bhattacharjee, M. K. (2022). Chemistry of antibiotics and related drugs (2nd ed.). Springer. https://doi.org/10.1007/978-3-031-07582-7
- Beauduy C.E., & Winston L.G. Aminoglycosides & spectinomycin. Vanderah T.W.(Ed.), [publicationyear2] Katzung’s Basic & Clinical Pharmacology, 16th Edition. McGraw-Hill. https://accesspharmacy.mhmedical.com/content.aspx?bookid=3382§ionid=281754807
- Centers for Disease Control and Prevention (CDC). (2022). Tick id. Retrieved from https://www.cdc.gov/ticks/tickbornediseases/tickID.html
- Centers for Disease Control and Prevention (CDC). (2024). Tularemia: for clinicians. Retrieved from https://www.cdc.gov/tularemia/clinicians/index.html
- Centers for Disease Control and Prevention (CDC). (2022). Tickborne diseases of the United States: A reference manual for healthcare providers. Retrieved from https://www.cdc.gov/ticks/tickbornediseases/TickborneDiseases-P.pdf
- Columbia University Irving Medical Center. (2021). Anaplasmosis. Retrieved from https://www.columbia-lyme.org/anaplasmosis.
- Mendell, N. L., Reynolds, E. S., Blanton, L. S., Hermance, M. E., Londoño, A. F., Hart, C. E., Quade, B. R., Esterly, A. T., Hendrix, C. B., Teel, P. D., Bouyer, D. H., & Thangamani, S. (2019). Detection of Rickettsiae, Borreliae, and Ehrlichiae in Ticks Collected from Walker County, Texas, 2017-2018. Insects, 10(10), 315. https://doi.org/10.3390/insects10100315
- Pace EJ, O’Reilly M. Tickborne Diseases: Diagnosis and Management. Am Fam Physician. 2020 May 1;101(9):530-540. PMID: 32352736.
- Renard, I., & Ben Mamoun, C. (2021). Treatment of Human Babesiosis: Then and Now. Pathogens (Basel, Switzerland), 10(9), 1120. https://doi.org/10.3390/pathogens10091120
- Texas Department of State Health Services (DSHS). (2023). Tick-borne diseases. Retrieved from https://www.dshs.texas.gov/tick-borne-diseases.
- Texas Department of State Health Services (DSHS). (2023). Tick submission and testing. Retrieved from https://www.dshs.texas.gov/tick-borne-diseases/tick-submission-testing
- Vallerand, A. H., & Sanoski, C. A. (2023). Davis’s drug guide for nurses (Eighteenth edition.). F.A. Davis Company.
- Walter, L., Sürth, V., Röttgerding, F., Zipfel, P. F., Fritz-Wolf, K., & Kraiczy, P. (2019). Elucidating the Immune Evasion Mechanisms of Borrelia mayonii, the Causative Agent of Lyme Disease. Frontiers in immunology, 10, 2722. https://doi.org/10.3389/fimmu.2019.02722
- Waters M, Tadi P. Streptomycin. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555886/
- Wang Y, Griffiths A, Brackney DE, Verardi PH. Generation of Multiple Arbovirus-like Particles Using a Rapid Recombinant Vaccinia Virus Expression Platform. Pathogens. 2022; 11(12):1505. https://doi.org/10.3390/pathogens11121505
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Doxycycline. Access Pharmacy. Retrieved from https://accesspharmacy.mhmedical.com/drugs.aspx?gbosID=426591
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Gentamicin. Access Pharmacy.
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Streptomycin. Access Pharmacy. Retrieved from https://accesspharmacy.mhmedical.com/drugs.aspx?gbosID=425268#monoNumber=425268§ionID=243273707&tab=tab0
- Yu, S., Modarelli, J., Tomeček, J. M., French, J. T., Hilton, C., & Esteve-Gasent, M. D. (2020). Prevalence of common tick-borne pathogens in white-tailed deer and coyotes in south Texas. International journal for parasitology. Parasites and wildlife, 11, 129–135. https://doi.org/10.1016/j.ijppaw.2020.01.005
- Chincholkar M. (2020). Gabapentinoids: pharmacokinetics, pharmacodynamics, and considerations for clinical practice. British journal of pain, 14(2), 104–114. https://doi.org/10.1177/2049463720912496
- DeBattista C (2024). Antidepressant agents. Vanderah T.W.(Ed.), Katzung’s Basic & Clinical Pharmacology, 16th Edition. McGraw Hill. https://accesspharmacy.mhmedical.com/content.aspx?bookid=3382§ionid=281751777
- Demler, T. L., & Rhoads, J. (Eds.). (2018). Pharmacotherapeutics for advanced nursing practice. Jones & Bartlett Learning.
- Dey S, Vrooman BM. Alternatives to Opioids for Managing Pain. [Updated 2023 Jul 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK574543/
- Dhaliwal JS, Spurling BC, Molla M. (2023). Duloxetine. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549806/
- Ferreira G E, Abdel-Shaheed C, Underwood M, Finnerup N B, Day R O, McLachlan A et al. Efficacy, safety, and tolerability of antidepressants for pain in adults: overview of systematic reviews BMJ 2023; 380 :e072415 doi:10.1136/bmj-2022-072415
- Fraser G.L., & Riker R.R. (2020). Critical care: pain, agitation, and delirium. DiPiro J.T., & Yee G.C., & Posey L, & Haines S.T., & Nolin T.D., & Ellingrod V(Eds.), Pharmacotherapy: A Pathophysiologic Approach, 11e. McGraw Hill. https://accesspharmacy.mhmedical.com/content.aspx?bookid=2577§ionid=234136370
- Goldenberg, D.L. (2019). Treatment of fibromyalgia in adults not responsive to initial therapies. Post TW, ed. UpToDate. Waltham, MA: UpToDate Inc. http://www.uptodate.com.
- Harding, E. K., Fung, S. W., & Bonin, R. P. (2020). Insights Into Spinal Dorsal Horn Circuit Function and Dysfunction Using Optical Approaches. Frontiers in neural circuits, 14, 31. https://doi.org/10.3389/fncir.2020.00031
- Macintyre, P. E., & Schug, S. A. (2021). Acute pain management : a practical guide (Fifth edition.). CRC Press.
- Malik, A. R., & Willnow, T. E. (2019). Excitatory Amino Acid Transporters in Physiology and Disorders of the Central Nervous System. International journal of molecular sciences, 20(22), 5671. https://doi.org/10.3390/ijms20225671
- Schwinghammer T.L., & DiPiro J.T., & Ellingrod V.L., & DiPiro C.V.(Eds.), (2021). Pharmacotherapy Handbook, 11e. McGraw Hill. https://accesspharmacy.mhmedical.com/content.aspx?bookid=3012§ionid=253436360
- Thour A, Marwaha R. Amitriptyline. (2023). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537225/
- U.S. Food and Drug Administration (FDA). (2020). FDA warns about serious breathing problems with seizure and nerve pain medicines gabapentin (Neurontin, Gralise, Horizant) and pregabalin (Lyrica, Lyrica CR). Retrieved from https://www.fda.gov/drugs/drug-safety-and-availability/fda-warns-about-serious-breathing-problems-seizure-and-nerve-pain-medicines-gabapentin-neurontin
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Amitriptyline. Retrieved from Access Pharmacy. https://accesspharmacy.mhmedical.com/drugs.aspx?GbosID=426455#monoNumber=426455§ionID=243191387&tab=tab0
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Pregabalin. Retrieved from Access Pharmacy. https://accesspharmacy.mhmedical.com/drugs.aspx?GbosID=426994#monoNumber=426994§ionID=243281218&tab=tab0
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Gabapentin. Retrieved from Access Pharmacy. https://accesspharmacy.mhmedical.com/drugs.aspx?GbosID=426662#monoNumber=426662§ionID=243246336&tab=tab0
- Accessdata.fda.gov (FDA). (n.d.). Cymbalta. https://www.accessdata.fda.gov/drugsatfda_docs/label/2007/021427s009s011s013lbl.pdf
- Chu A. and Wadhwa R. Selective Serotonin Reuptake Inhibitors. (2023). In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK55440
- Woodall, A. and Walker, L. (2022). A guide to prescribing antidepressants in primary care. Prescriber, 33: 11-18. https://doi.org/10.1002/psb.2006
- Bains N. and Abdijadid S. Major Depressive Disorder. (2023). In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559078/
- Rohatgi, K. W., Humble, S., McQueen, A., Hunleth, J. M., Chang, S. H., Herrick, C. J., & James, A. S. (2021). Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. Journal of the American Board of Family Medicine: JABFM, 34(3), 561–570. https://doi.org/10.3122/jabfm.2021.03.200361
- Lam, M. K., Lam, L. T., Butler-Henderson, K., King, J., Clark, T., Slocombe, P., Dimarco, K., & Cockshaw, W. (2022). Prescribing behavior of antidepressants for depressive disorders: A systematic review. Frontiers in Psychiatry, 13, 918040. https://doi.org/10.3389/fpsyt.2022.918040
- Moncrieff, J., Cooper, R. E., Stockmann, T., Amendola, S., Hengartner, M. P., & Horowitz, M. A. (2023). The serotonin theory of depression: a systemic umbrella review of the evidence. Molecular Psychiatry, 28, 3243-3256. https://doi.org/10.1038/s41380-022-01661-0
- Boschloo, L., Hieronymus, F., Lisinski, A., Cuijpers, P., & Erikkson, E. (2023). The complex clinical response to selective serotonin reuptake inhibitors in depression: a network perspective. Translational Psychiatry, 13, 2-25. https://doi.org/10.1038/s41398-022-02285-2
- Hirsch, M., Birnbaum, R. J. (2023). Selective serotonin reuptake inhibitors: Pharmacology, administration, and side effects. UptoDate. Retrieved 12 Jan 2024 from https://www.uptodate.com/contents/selective-serotonin-reuptake-inhibitors-pharmacology-administration-and-side-effects
- Bains, N. & Abdijadid, S. (2023). Major Depressive Disorder. In: StatPearls: Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559078/
- Abi-Aad, K., & Derain, A. (2023, August 17). Hydromorphone. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK470393/
- Adler, J., Ballantyne, J., Chou, R., Davies, P., Fanciullo, G., & Fine, P. (2009). Clinical Guidelines for the Use of Chronic Opioid Therapy in Chronic NonCancer Pain. The Journal of Pain, 113-130.
- Ahmad, F., Rossen, L., Sutton, P., & & Talih, M. (2018). Provisional drug overdose. National Vital Statistics Reports, pp. 1-12.
- Altman, R., Clark, M., Huddart, R., & Klein, T. (2018, October 28). Pharm GKB Summary: Oxycodone Pathway, Pharmacokinetics. Retrieved from Pharmacogenet Genomics: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6602093/#:~:text=Approximately%2072%25%20of%20an%20oxycodone,oxycodone%20is%20unconjugated%20%5B70%5D
- Atrux-Tallau, N., naimi, Z., & Jaudinot, E. (2022, November 4). Pharmocokinetics of Morphine Sulfate Orodispersible tablets and Bioequivalence with Immediate-Release Oral Morphine Sulfate Formulations in Healthy Adult SubjectsUnder fastin Conditions. Retrieved from Clinical Drig Investigation: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9705466/
- Baldwin, G., Compton, W. M., Han, B., Houry, D., Jones, C. M., & Vivolo-Kantor, A. (2021, September 24). Methamphetamine use in the United States: epidemiological update and implocations for prevention, treatment and harm reduction. Annual New York Academy of Science. New York: National Institute of Health.
- Berg, K. A., & Clarke, W. P. (2018). Making Sense of Pharmacology: Inverse Agonism and Functional Selectivtiy. International Journal of Neuropsychopharmacology, 962-977.
- Bistas, K., Lopez-Ojeda, W., & Ramos-Matos, C. (2023, May 29). Fentanyl. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK459275/
- Blyth, F., Briggs, A., Hoy, D. G., March, L. M., & Schneider, C. H. (2019). The Global Burden of Musculoskeletal Pain-Where to From Here? American Journal of Public Health, 35-40.
- Bramanti, P., Cavalli, E., Mammana, S., Mazzon, E., & Nicoletti, F. (2019). The neuropathic pain: An Overview of the current treatment and future therapeutic approaches. International Journal of Immunopathology and Pharmacology, 33.
- Brennan, F., Carr, D., Cousins, M., & Pain, D. (2013). Pain Management: A Fundamental Human Right. Anesthesia and Analgesia, 224-227.
- Carver, A. C., & Foley, K. (2003). Types of Pain. In D. Kufke, & R. W. Pollock, Cancer Medicine. Hamilton: Holland Frei Cancer Medicine.
- Centers for Disease Control and Prevention. (2022). CDCs Clinical Practice Guidelines for Prescribing Opioids. Retrieved from Opioids: https://www.cdc.gov/opioids/healthcare-professionals/prescribing/guideline/index.html?s_cid=DOP_Clinician_Search_Paid_001&gclid=CjwKCAjwrranBhAEEiwAzbhNtVKOCMzLLnwhfj7B2D_aBCZM_SryNcEyXl0GRigmorFhKve2ekCVrhoCNYQQAvD_BwE
- Centers for Disease Control and Prevention. (2023, August 8). Opioids. Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/opioids/basics/epidemic.html#print
- Chiang, N., Gyaw, S., & Krieter, P. A. (2019). Comparison of the Pharmacokinetic Properties of Naloxone Following the Use of FDA-Approved Intranasal and Intramuscular Devices Versus a Common Improvised Nasal Naloxone Device. Journal of Clinical Pharmacology, 1078-1084.
- Cicero, T., & Ellis, M. &. (2017). The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA, 673-681.
- Cofano, S., & Yellon, R. (2022, October 24). Stat Pearls: Hydrocodone. Retrieved from National Institutes of Health: https://www.ncbi.nlm.nih.gov/books/NBK537288/
- Dart, R., Hoyte, C., & Nakhee, S. (2021). A Review on Tramadol Toxicity: Mechanism of Action, Clinical Presentation, and Treatment. Forensic Toxicology, 293-310. Retrieved from Forensic Toxicology: https://link.springer.com/article/10.1007/s11419-020-00569-0
- Delsignor, R. e. (2001). Lofexidine versus clonidine in rapid opiate detoxification. Journal of Substance Abuse Treatment, 11-17.
- Department of Defense Veterans Association. (2023). Defense and Veterans Pain Rating Scale. Retrieved from VA.gov: https://www.va.gov/PAINMANAGEMENT/docs/DVPRS_2slides_and_references.pdf
- Department of Health and Aged Care. (2013, January 20). FLACC Pain Scale. Retrieved from health.gov: https://www1.health.gov.au/internet/publications/publishing.nsf/Content/triageqrg~triageqrg-pain~triageqrg-FLACC
- Donaldson, S. L. (2017). Provider-Based Interventions to Mitigate Risk for Opioid Pain Medication Abuse Among Adult Patients in a Primary Care Setting.
- Dydyk, A. M., & Grandhe, S. (2023, January 29). Pain Assessment. Retrieved from STAT PEARLS: https://www.ncbi.nlm.nih.gov/books/NBK556098/#:~:text=Pain%20is%20the%20most%20common,pain%20in%20the%20United%20States.
- Fan, M., Hamilton, M., Hyland, B., & Tscheng, D. (2019). Diversion of Controlled Drugs in Hospitals: A Scoping review of Contributors and Safeguards. Journal of Hospital Medicine.
- GeriatricPain.org. (2022, January). Fast Facts: Selected Pain Assessment Tools. Retrieved from Geriatricpain.org: Geriatricpain.org https://geriatricpain.org/selected-pain-assessment-tools-fc
- Haffajee, R., Jena, A., Weiner, S., & & Kesselheim, A. (2019). Mandatory use of prescription drug monitoring programs. Journal of the American Medical Association, 1667-1668.
- International Association for the Study of Pain . (2020, July 16). IASP Announces Revised Definition of Pain. Retrieved from International Association for the Study of Pain: https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
- JAMA. (2023). Substance Use and Addiction Medicine. Retrieved from JAMA Network: https://jamanetwork.com/collections/5921/substance-use-and-addiction-medicine
- John, W. S., Schwartz, R. P., Subramanian, G., & Wu, L.-T. (2018). Prevalence, Patterns and correlates of multiple substance use disorders among adults. Drug and Alcohol Dependency, 79-87.
- Jones, C., Einstein, E., & Compton, W. (2018). Changes in synthetic opioid involvement in drug overdose deaths in the United States. JAMA, 1819-1821.
- Kalava, A., King, K. C., & Preuss, C. V. (2023, April 29). Perscription of Controlled Substances: Benefits and Risks. Retrieved from STAT PEARLS: https://www.ncbi.nlm.nih.gov/books/NBK537318/
- Khalid, N., Patel, P., & Singh, A. (2023, January). Cannabis Versus Opioids for Pain. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK573080/
- Kreutzwiser, D., & Tawfic, Q. (2020). Mathadone for Pain Management. A Pharmacotherapeutic Review, 827-839.
- Kroenke, K., Spiter, R., Williams, J., & Lowe, B. (2011, Nov). An ultra-brief screening scale for anxiety and depression: the PHQ-4. From Principles of Neuropathic Pain Assessment and Management, 613-21. Psychosomatics 2009.
- Manchikanti, L., Kaye, A., Knezevic, N., McAnally, H., Slavin, K., Trescot, A., & Hirsch, J. (2018). Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians guidelines. Pain Physician, S3-S92.
- Marquez, C. B. (2020). Changing the outlook toward the problem of opioid addiction: From “War on Drug” to “Public Health Emergency”. Seton Hall: Law Student Scholarship.
- Marsch, L., Borodovsky, J., & Dallery, J. (2019). Advances in the psychosocial treatment of addiction: The role of technology in the delivery of evidence-based psychosocial treatment. The Psyciatric Clinics of North America, 585-596.
- McLellan, T., & Volkow, N. (2016). Opioid Abuse in Chronic Pain-Misconceptions and Mitigation Strategies. New England Journal of Medicine, 1253-1263.
- National Institute of Drug Abuse (NIDA). (2023, August 30). Prescription Opioid Drug Facts. Retrieved from National Institute on Drug Abuse: https://nida.nih.gov/publications/drugfacts/prescription-opioids
- National Institute of Health. (2023, August 25). Medications for Opioid Overdose, Withdrawal, & Addiction. Retrieved from National Institute of Drug Addiction: https://nida.nih.gov/research-topics/opioids/medications-opioid-overdose-withdrawal-addiction-infographic
- Pain Physician. (2008). Opioid Special Issue. Pain Physician, S133-S153.
- Ransford, e. a. (2019, February 08). The Ransford Pain Drawing . Retrieved from compassionandsupport.org: https://compassionandsupport.org/wp-content/uploads/sites/2/2019/08/PainScaleRansford.pdf
- Rudd, R. A., Zibbell, J., & Gladden, M. (2016). Increases in drug and opioid overdose deaths-Untied States. Morbidity and Mortlity Weekly Report, 1378-1382.
- SAMHSA. (2020). Key Substance Use and Mental Health Indicators in the United States: Ressults from the 2019 National Survey on Drug Use and Health. SAMHSA.
- Scalpel, S. (2016, November). The Joint Commission Deserves Some Blame for the Opioid Crisis. Retrieved from Missouri Medicine: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6139759/
- Scholl, L., Seth, P., Kariisa, M., Wilson, N., & Baldwin, G. (2019). Drug and opioid-involved overdose deaths-Unioted States, 2013-2017. Morbidity and Mortatlity Weekly Report 67, 1419-1427.
- Stauffer, L., & Gibson, S. (2017). The Nurse’s Role in Identifying and Educating Patients At Risk for Opioid Abuse. AAACN Viewpoint, 1.
- The Joint Commission. (2023, January). The Joint Commission History Timeline. Retrieved from JointCommission.org: https://www.jointcommission.org/-/media/tjc/documents/tjc-history-timeline-through-2022.pdf
- Toombs, K., Kral, L., Colleran, C., & & Varney, S. (2018). Nurse practitioner-pharmacist collaboration in pain management: Strategies for success. . Journal of the American Association of Nurse Practitioners, 141-148.
- U.S. Food and Drug Administration. (2023, May 23). FDA. Retrieved from Information about Medication Assisted Treatment (MAT): https://www.fda.gov/drugs/information-drug-class/information-about-medication-assisted-treatment-mat
Volkow, N., Jones, E., Einstein, E., & Wargo, E. (2019). Prevention and Treatment of Opioid mIsuse and Addiction: A Review. JAMA Psychiatry, 208-216.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
