Course
Coronary Stent Placement Beginners Guide
Course Highlights
- In this Coronary Stent Placement Beginners Guide: All you Need to Know course, we will learn about the procedure of coronary stent placement.
- You’ll also learn about potential complications of coronary stent placement.
- You’ll leave this course with a broader understanding of conditions requiring coronary stent placement.
About
Contact Hours Awarded: 2
Course By:
Keith Wemple
RN, BSN, CCRN-CMC, SRNA
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Heart disease is the leading cause of death in the United States, accounting for 1 in every 5 deaths in 2021 (8). Coronary artery disease is the most common chronic heart condition, affecting 1 in every 20 adults over age 20 (8).
You have probably taken care of a patient with coronary artery disease in your own practice. You have also probably heard about stents being placed. But what does that really mean? And how does it impact you and the care you give that patient? This course will answer those questions and give you confidence when caring for patients with coronary disease.

Self-Quiz
Ask Yourself...
- What do you know about coronary artery disease?
- What do you already know about coronary stents?
Coronary Stent Placement
First, let’s discuss what a coronary stent is. Essentially, a stent is a small metal scaffolding that is used to hold open a narrowed blood vessel. Coronary stents are scaffolding that are placed in the coronary arteries. They somewhat appear like a tiny Chinese finger trap; when they are compressed, they widen and open, and when they are stretched, they become thinner and close.
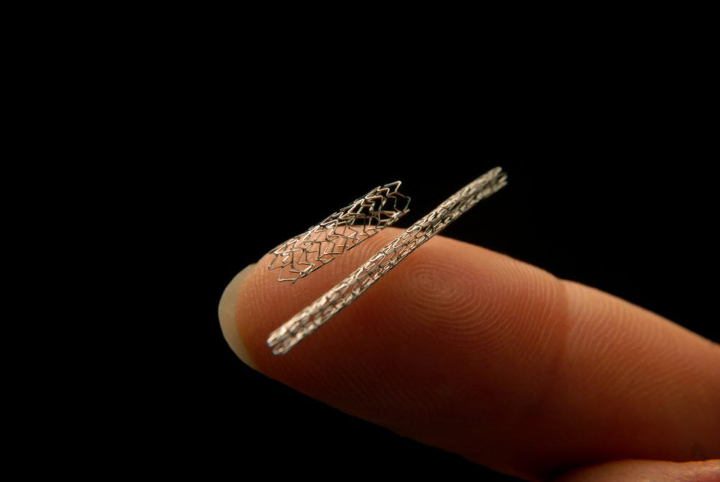
(2)
You may have seen “drug eluting stent” or “DES” in the chart when talking about coronary stents. There are 2 main types of stents that can be used to open the coronary arteries: bare metal and drug eluting stents. Drug eluting stents are by far the most common, as they offer many benefits. The drug eluting stent is coated with drug to help prevent the space inside the stent from closing off again (5).
Bare metal stents have largely been replaced by drug eluting stents since they were introduced in 2001 (2). You may still see some bare metal stents though, and they do offer an advantage in certain situations.
The most common reason a bare metal stent is used today is because it requires the patient to be on anticoagulation for a shorter period of time (5). This can be useful when the patient requires surgery but is having their heart function optimized first. Surgeons dislike bleeding, so they will defer surgery until a patient can hold the anticoagulation for the procedure.

Self-Quiz
Ask Yourself...
- What information have you seen documented on patients with coronary stent placements?
- What are some common blood thinners you have seen prescribed?
- What are the potential side effects of anticoagulation therapy?
Coronary Anatomy
To better understand coronary angiography and stent placement let’s do a quick review of coronary anatomy. The coronary arteries are the blood vessels that provide blood supply to the muscle of the heart. The coronaries come off the base of the aortic valve and sit on the outside of the heart. Here is a picture you can reference.
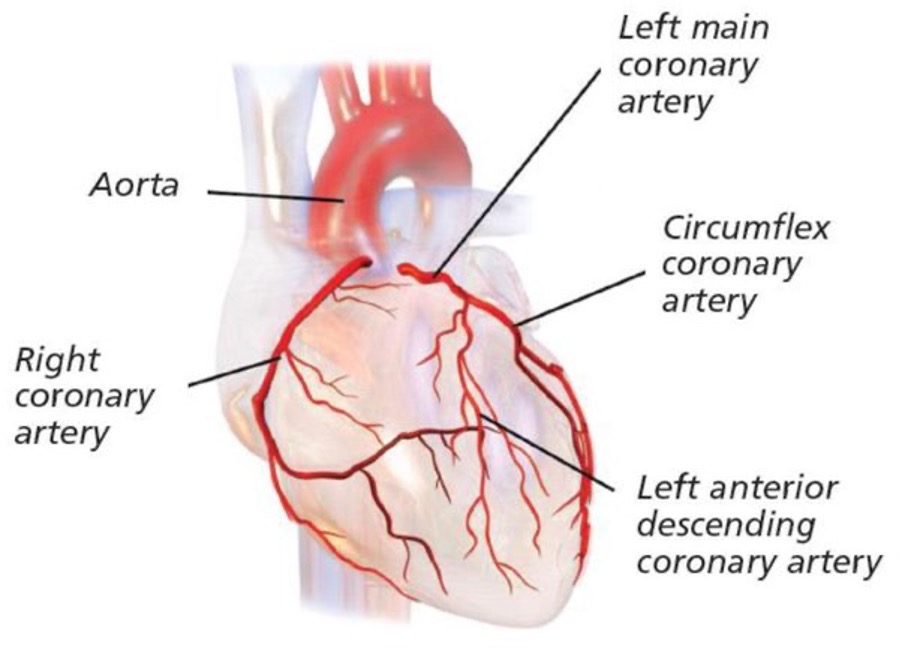
(6)
There are 3 main coronary arteries: the right coronary artery, the left anterior descending artery, and the left circumflex artery (9). The right coronary artery supplies blood to – you guessed it – the right side of the heart. Importantly, in most people the right coronary artery also supplies blood flow to the inferior and posterior walls of the heart, as well as the sinus and atrioventricular nodes (9). The right coronary artery is often abbreviated “RCA” on cath lab reports. If you see “right dominant circulation” documented, that means the right coronary artery feeds the posterior wall of the heart (9).
The left anterior descending artery supplies blood to the anterior wall of the left ventricle and the septum of the heart (9). Because it feeds a large part of the left ventricle, blockage of the left anterior descending artery is a common cause of heart failure (3). The left anterior descending artery is usually abbreviated “LAD” on Cath lab reports.
The left circumflex artery carries blood to the lateral portion of the left ventricle, and in 20% of people continues to supply the posterior wall of the heart (9). If the circumflex artery supplies the posterior wall, the patient is said to have left dominant circulation (9). The circumflex artery is often shortened to “circ” when reading cardiology notes.
There are several branches off each of these 3 main arteries, but we don’t need to dive that deep. There is 1 more artery you should be aware of, however. The left main artery is a short artery that quickly branches into the left anterior descending and circumflex arteries (9). The left main is important because if the patient has a blockage of their left main, they lose blood supply to 2 of the 3 main coronary arteries – yikes!

Self-Quiz
Ask Yourself...
- What do you already know about coronary arteries?
- What problems might a patient with a blockage of their RCA have?
- How does this differ from a patient with a blockage of their LAD?
How Stents are placed
Coronary stents are placed in the cardiac catheterization lab, or the Cath lab as most people call it. The procedure where stents are placed is called coronary angiography, often referred to as a coronary angio or just “angio” for short (10).
The procedure involves making a small incision over an artery and inserting a catheter into the artery (10). Typically, this is done using the radial artery in the wrist or the femoral artery in the groin, with the radial artery being the preferred choice (3). The catheter is then advanced along the artery until it reaches the heart.
On the base of the aortic valve where the left ventricle pumps blood into the aorta lies the coronary sinus (9). The coronary sinus is the opening that leads into the coronary arteries. The catheter is passed through the coronary sinus and into the coronary arteries (10). During the procedure, patients receive large amounts of intravenous heparin to prevent clots from forming on the equipment (3). Fluoroscopy is used as a guide while advancing the catheter; fluoroscopy is a form of X-ray that allows for real-time imaging (10).
Once inside the coronary arteries, radiopaque dye is injected into the coronary arteries and fluoroscopy images are taken (3). The dye shows up dark on the fluoroscopy images and allows the proceduralist to visualize the coronary arteries. This imaging allows the proceduralist to identify any narrowing in the coronary arteries.
The proceduralist then advances a balloon over the catheter inside the narrowed section of artery (10). The balloon is inflated to push open the narrowing, an intervention called angioplasty (10). Angioplasty itself only temporarily relieves the problem of occluded coronary arteries, which is where our stents come in (3).
Once the narrowing has been opened up with the balloon, the balloon is deflated, and a stent added over the balloon (10). The balloon is then reinflated to open the stent and press it into the walls of the artery where the narrowing was (10). The balloon and catheter can then be removed, and the stent remains in place inside the coronary artery.
The stent remaining in artery works as a scaffolding to hold the walls of the vessel open, providing a more permanent repair to the narrowing (3).
The image below is from the National Heart Lung and Blood Institute, it demonstrates stent placement.
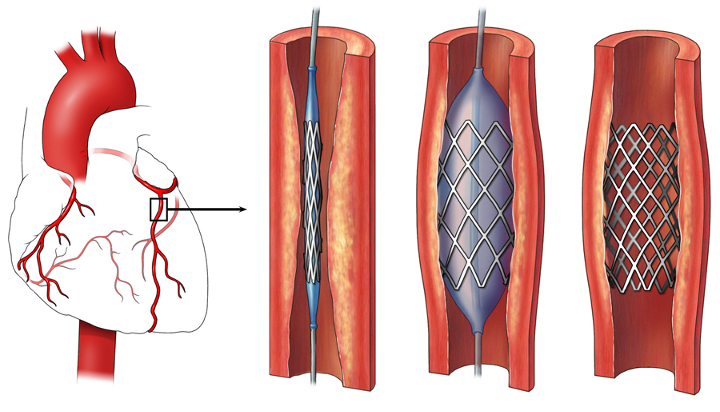
(1)

Self-Quiz
Ask Yourself...
- Does your facility have a Cath lab? If not where is the nearest Cath lab?
- What do you think may be complications of inflating a balloon inside the arteries?
Pre-Procedure Considerations
Before the procedure, patients should be given 325mg of aspirin and a loading dose of another antiplatelet drug, most commonly clopidogrel (Plavix) (3). If the patient is experiencing a heart attack, stabilizing measures should be used while waiting for the procedure.
You may remember the acronym MONA from nursing school for treatment of a heart attack. MONA stands for Morphine, Oxygen, Nitroglycerine and Aspirin (3). Nitroglycerine is the first treatment for ischemic chest pain, as it helps dilate the coronary arteries so that more blood can get through (3). Morphine is the second-line treatment for chest pain. Morphine provides pain relief and also reduces pre-load on the heart, so it doesn’t have to work as hard (3). Oxygen should be administered for a pulse oximeter reading below 92% (3). Keeping blood oxygen levels high helps maintain oxygen supply to the ischemic heart muscle. Finally, aspirin works as an antiplatelet drug to prevent platelets from aggregating and clotting off the artery (3).
If the patient had previously received fibrinolytics, it is recommended that they wait 2 hours before proceeding with a coronary angiogram to prevent serious bleeding (3).

Self-Quiz
Ask Yourself...
- What are side effects to watch for with nitroglycerine?
- What side effects might a person receiving a loading dose of blood thinners experience?
- How would you get a patient to cardiac surgery emergently?
Post-Procedure Considerations
Following a coronary angiogram, the patient must be monitored for a number of hours. The access site from the procedure must be closely monitored in the first several hours for rebleeding or hematoma formation (more on that soon) (3).
Perfusion of the affected limb should also be monitored, as damage to or occlusion of the artery from the procedure can lead to limb ischemia (3). Pulse, color, warmth, mobility, and sensation of the limb should be assessed frequently (3).
Patients will be placed on bedrest for the first few hours of recovery if the femoral artery was used. Bedrest often includes the patient lying flat, as sitting up increases pressure on the groin and the access site (3). If the patient had a stent placed for a myocardial infarction, it is recommended they remain in the hospital for 24-48 hours with ECG monitoring (5).


Self-Quiz
Ask Yourself...
- What nursing interventions can you use to improve comfort for a patient on bed rest?
- How comfortable are you assessing limb perfusion?
- If you can’t palpate a pulse, do you have doppler available to locate a pulse?
- Do you have a cardiac surgeon where you work?
Potential Complications
There are some complications associated with coronary stent placement that you should be aware of. Ballooning-open the arteries can cause a showering of plaque downstream, potentially causing blockages further down the coronary artery (3). It is also possible that a stent can be placed such that it blocks one of the branches coming off the artery (11). This is usually referred to as “jailing” the branch. Jailing a branch of the coronary artery may cause ischemia to that area of the heart, but most of the time does not impede blood flow enough to cause a problem (11).
It is also possible that a coronary artery may dissect from the pressure of the balloon inflating (14). These complications are generally known by the proceduralist at the time of the procedure. The interventionalist will treat these complications as appropriate but will still require close monitoring of the patient’s condition afterwards.
In the immediate post-procedure recovery, there are some important complications to be mindful of. The site where the artery was accessed can re-open and/or rebleed (3). When this happens significant blood loss can occur. The recommended treatment is to hold firm pressure until a stable clot forms and the bleeding subsides.
Bleeding can also occur under the skin and form a hematoma. This will present as swelling around the access site and may be painful to the patient (12). If left untreated this can result in compartment syndrome (12). The treatment of choice is firm pressure over the hematoma to stop the bleeding and allow the blood to be reabsorbed (12).
Rarely, with the femoral approach, can a retroperitoneal bleed develop (12). Rather than developing a hematoma in the groin where it is easily detected, bleeding happens behind the artery in the lower abdomen.
Symptoms of retroperitoneal bleed are:
- Severe low back pain
- Hypotension
- Decreased hemoglobin levels
(12)
Treatment of a retroperitoneal bleed requires a vascular repair of the damaged artery, either in the Cath lab or the operating room.
If the stent was placed to treat a myocardial infarction, complications related to the infarction should also be monitored for. We won’t discuss all the considerations for myocardial infarction (maybe next time) but immediately post-procedure there are a few complications to consider.
Ventricular rhythms around a myocardial infarction are common, so patients should have continuous ECG monitoring (4). Acute heart failure and cardiogenic shock can also develop after a myocardial infarction (12). Mechanical complications can also develop after a heart attack, which present as a new heart murmur, or sudden onset changes in blood pressure, work of breathing and consciousness (12). If the patient develops a mechanical complication, this often requires emergent cardiac surgery (12).

Self-Quiz
Ask Yourself...
- How confident are you in identifying a heart murmur?
- Do you have the means to handle a retroperitoneal bleed where you work?
- How would you activate these resources?
- If a patient is experiencing ongoing chest pain after the procedure, what might happen?
When Stents are Placed
Coronary stents are placed to provide long term relief of coronary artery disease. As you have probably gathered, this procedure is not without risks. Because of this, stents are generally not placed unless the benefits outweigh the risks of the procedure.
During the coronary angiogram the proceduralist measures how occluded the artery is. Generally, once the artery is 80% or more occluded the benefits of placing a stent are believed to outweigh the risks (3).
An important exception to this rule is when the patient has a chronic total occlusion, sometimes abbreviated CTO by people who want to finish their charting as quickly as possible. A chronic total occlusion is when the artery is 100% blocked at some point, but the body has rerouted blood flow around the blockage so that the heart muscle is still receiving its blood supply (3). This rerouting of blood flow is called collateral circulation or just “collaterals” on angiogram reports (9).
Collateral blood flow develops slowly over time, indicating that the blockage is a chronic and not an acute problem. You can think of this like a bone that was broken years ago and healed on its own. It probably didn’t heal completely normally but is functional and may not be worth going through a procedure to correct it.

Self-Quiz
Ask Yourself...
- Can you think of any other problems that aren’t treated urgently when they are more chronic?
- How many of your typical patients have coronary artery disease?
Conditions Requiring Stent Placement
The main reason for coronary stent placement is treatment of coronary artery disease. Coronary artery disease is a chronic condition of plaque buildup inside of the coronary arteries (9). This causes the arteries to narrow and impedes blood flow to the heart muscle. Over time this lack of blood flow to the heart muscle can cause heart failure (9). In fact, coronary artery disease is the leading cause of heart failure (8).
Coronary artery disease manifests as shortness of breath or chest discomfort with activity (9). The most serious manifestation of coronary artery disease is acute myocardial infarction, or a heart attack.
A myocardial infarction occurs when the heart muscle does not receive enough blood flow (9). The typical cause for this is a coronary artery that is chronically narrowed by coronary artery disease suddenly becomes completely occluded (9). The plaque that has formed inside the coronary artery ruptures from the turbulent blood flow through the narrowing (9). This triggers the body to form a blood clot at this site of injury. The blood clot then fully occludes the artery, causing a sudden loss of blood flow to the heart muscle (9).
The definitive treatment for a myocardial infarction is coronary stent placement or coronary artery bypass (3).
Not everyone that has a heart attack has a diagnosis of coronary artery disease. Many times, people don’t know they have coronary artery disease until an angiogram is done. Some conditions that raise a red flag for coronary artery disease are atherosclerosis, tobacco use, hyperlipidemia, hypertension, and diabetes (8).
Coronary artery disease is basically atherosclerosis in the arteries of the heart, so the connection there is easy to understand. Smoking predisposes the arteries to plaque formation and atherosclerosis. Hyperlipidemia means there is too much cholesterol in the blood, so it is much more likely to start building up inside the coronaries. Hypertension and diabetes often coincide with coronary artery disease and can make the condition worse.

Self-Quiz
Ask Yourself...
- What conditions are associated with coronary artery disease?
- How many of your typical patients have one of these conditions?
- What are the hallmark symptoms of a heart attack?
- What lifestyle changes can lower a person’s risk of coronary artery disease?
Recovery
Patients will typically recover in the hospital for anywhere from a few hours to a few days. The length of stay depends on the post-operative course and the reason for the procedure. If the procedure was scheduled for known coronary artery disease, then the length of stay may be a few hours to overnight observation. If the procedure was done to treat an acute myocardial infraction, then it is recommended that patients stay at least 2 days for monitoring (4).
Patients do have some limitations during their recovery. Patients should avoid strenuous activity and not lift more than 10 pounds for at least 3 days after their procedure. Strenuous activity increases the likelihood of the arterial access site rebleeding.
Patients should also keep the access site covered and not wash it for 24 hours. Patients should be educated on possible complications related to the access site and advised to seek help if a complication does occur.
For follow-up testing, patients will require an echocardiogram. If the patient has a new diagnosis of coronary artery disease or an acute myocardial infarction that required a stent placement, they should have an echo performed before leaving the hospital (7). An echo should be repeated approximately one month after discharge for patients who had a heart attack (7).
Cardiac rehabilitation is also recommended for all patients recovering from a heart attack (3). Cardiac rehab is a form of monitored exercise that watches for cardiac symptoms while the patient exercises. It helps patients return to normal function and helps reduce readmission to the hospital (3).
Patients receiving a stent should be on dual anti-platelet therapy (DAPT) to prevent the stent from closing off. For a drug eluting stent, the patient should be on aspirin and another antiplatelet such as clopidogrel for 6-12 months (3). For a bare metal stent, the patient should be on aspirin and clopidogrel for 1-3 months (3). These patients generally will stay on 81mg of aspirin indefinitely.

Self-Quiz
Ask Yourself...
- What is your institution’s policy on monitoring after coronary stent placement?
- Does your institution have education materials for post-stent placement?
- If not, where might you find educational materials?
- How many of your typical patients are on low dose aspirin?
Nursing Implications
So, out of all that information, what do you need to know as a nurse? Understanding the basics of the procedure can help you to educate your patients who may have questions about it. Knowing what conditions necessitate coronary stent placement will help you anticipate when the procedure will be needed. And being knowledgeable about potential complications will help you be prepared and focus your assessments. To bring all this together let’s look at a case study.
Case Study
A patient, Tom Thompson, comes to the emergency department where you work complaining of chest pain and shortness of breath. Mr. Thompson has a history of hyperlipidemia and hypertension and is a current smoker. His vitals: BP 150/90, HR 100, SpO2 88% on room air, Temp 37C and 7/10 chest pain.
- What diagnosis are you concerned about for Mr. Thompson?
- Given his presentation and vitals what treatments should we consider?
A troponin and 12-lead ECG are ordered for suspected myocardial infarction. In the meantime, the provider orders sublingual nitroglycerine to be given and you start the patient on 2L of oxygen via nasal cannula.
After these treatments Mr. Thompson’s vitals are BP 120/70, HR 88, SpO2 95% on 2L, Temp 37C and 2/10 chest pain. Testing confirms that Mr. Thompson is having a myocardial infarction and is scheduled to go to the Cath lab as soon as a room becomes available.
- What other measures should be taken to prepare Mr. Thompson for the Cath lab?
You remind the provider that the patient needs informed consent for the procedure and ask for orders to administer a loading dose of aspirin and clopidogrel for the procedure. Mr. Thompson is nervous about the diagnosis of a heart attack, but consents to the procedure. After the provider leaves, you give Mr. Thompson his aspirin and clopidogrel as his daughter arrives. She asks about the procedure and Mr. Thompson looks to you to explain.
- What details about the procedure can you recall?
- How would you explain this to the patient and his family?
Mr. Thompson receives his coronary angiogram and is transferred to the cardiac unit for monitoring. You receive the following report from the Cath lab: “Mr. Thompson is ready for pickup from room 1 in the Cath lab. He got 2 of Versed, 100 of fentanyl and 5000 of heparin for the procedure. He has a right fem site and has a stent to the LAD. Vitals are stable on room air, now chest pain free.”
- Based on this report, what complications should you monitor for in Mr. Thompson?
- What assessments will you perform?
Mr. Thompson is transferred to the cardiac unit and placed on the monitor. His vitals are stable, but 30 minutes later when you check his access site you notice swelling in his groin, his leg is cold to the touch, and he reports his leg is “numb”.
- What complication(s) is Mr. Thompson experiencing?
- What is an appropriate intervention?
You apply firm pressure over the hematoma for 5 minutes. After 5 minutes, the swelling has resolved, and Mr. Thompson reports his leg feels “better”. The next 2 days in the hospital are unremarkable and Mr. Thompson is set to discharge home.
- What education do you provide Mr. Thompson about recovery after coronary stent placement?
- What medications do you anticipate Mr. Thompson will be discharged with?
Conclusion
Coronary stent placement is a fairly common procedure used to treat coronary artery disease and heart attacks. It involves accessing an artery and using catheters to open a narrowed coronary artery. A stent is then placed to prevent the area from occluding again.
There are some complications of the procedure, such as hematoma, rebleeding and limb ischemia. Patients should remain in the hospital for monitoring of these complications for at least 4-6 hours and up to 2 days. As nurses, understanding the basics of the procedure, as well as pre- and post-procedure considerations will help us better care for these patients.
Even if you don’t work in cardiology, you are almost certain to take care of a patient with coronary artery disease. Understanding a little more about the treatment of this disease should aid you in treating these patients.

Self-Quiz
Ask Yourself...
- What can you use from this course in your daily practice?
References + Disclaimer
- What to expect when getting a stent. National Heart Lung and Blood Institute. 2022. Accessed November 16, 2023. https://www.nhlbi.nih.gov/health/stents/during.
- Boardman H, J F, EE N, et al. Which stent is best for heart attacks? Evidently Cochrane. January 18, 2023. Accessed November 16, 2023. https://www.evidentlycochrane.net/which-stent-heart-attacks/.
- Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for Coronary artery revascularization: A report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. 2022;145(3). doi:10.1161/cir.0000000000001038
- Sandau KE, Funk M, Auerbach A, et al. Update to practice standards for electrocardiographic monitoring in hospital settings: A scientific statement from the American Heart Association. Circulation. 2017;136(19). doi:10.1161/cir.0000000000000527
- Feinberg J, Nielsen EE, Greenhalgh J, Hounsome J, Sethi NJ, Safi S, Gluud C, Jakobsen JC. Drug‐eluting stents versus bare‐metal stents for acute coronary syndrome. Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No.: CD012481. DOI: 10.1002/14651858.CD012481.pub2. Accessed 18 November 2023.
- Chelsea and Westminster Hospital. Your coronary angiogram and coronary angioplasty. NHS choices. Accessed November 18, 2023. https://www.chelwest.nhs.uk/your-visit/patient-leaflets/medicine-services/your-coronary-angiogram-and-coronary-angioplasty.
- Virani S, Newby LK, Arnold S, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of … Journal of the American College of Cardiology. 2023. Accessed November 21, 2023. https://www.jacc.org/doi/10.1016/j.jacc.2023.04.003.
- Heart disease facts. Centers for Disease Control and Prevention. May 15, 2023. Accessed November 19, 2023. https://www.cdc.gov/heartdisease/facts.htm#:~:text=due%20to%20death.-,Coronary%20Artery%20Disease,killing%20375%2C476%20people%20in%202021.&text=About%201%20in%2020%20adults,have%20CAD%20(about%205%25).&text=In%202021%2C%20about%202%20in,less%20than%2065%20years%20old.
- Widmaier EP, Raff H, Strang KT, Vander AJ. Chapter 12: Cardiovascular Physiology. In: Vander’s Human Physiology: The Mechanisms of Body Function. McGraw Hill; 2023:362-444.
- Society for Cardiovascular Angiography and Interventions. Angiogram/cardiac catheterization. SCAI – Seconds Count. Accessed November 21, 2023. https://www.secondscount.org/test/angiogramcardiac-catheterization.
- Bhargava B, Waksman R, Lansky AJ, Kornowski R, Mehran R, Leon MB. Clinical outcomes of compromised side branch (stent jail) after coronary stenting with the NIR stent. Catheter Cardiovasc Interv. 2001 Nov;54(3):295-300. Doi: 10.1002/ccd.1287. PMID: 11747152.
- Kirsten Andersen, Marianne Bregendahl, Helen Kaestel, Mette Skriver, Jan Ravkilde, Haematoma after Coronary Angiography and Percutaneous Coronary Intervention via the Femoral Artery Frequency and Risk Factors, European Journal of Cardiovascular Nursing, Volume 4, Issue 2, 1 June 2005, Pages 123–127, https://doi.org/10.1016/j.ejcnurse.2005.02.003
- Guy S. Reeder, Identification and Treatment of Complications of Myocardial Infarction, Mayo Clinic Proceedings, Volume 70, Issue 9, 1995, Pages 880-884, ISSN 0025-6196, https://doi.org/10.4065/70.9.880.
- Fischman DL, Vishnevsky A. Management of Iatrogenic Coronary Artery Dissections: Failing to Prepare Is Preparing to Fail. JACC Case Rep. 2021 Mar 17;3(3):385-387. Doi: 10.1016/j.jaccas.2021.01.023. PMID: 34317542; PMCID: PMC8311007.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
