Course
Total Hip Arthroplasty
Course Highlights
- In this Total Hip Arthroplasty course, we will learn about signs and symptoms that indicate the need for evaluation for a total hip arthroplasty.
- You’ll also learn three risk factors for post-operative infection following a total hip arthroplasty.
- You’ll leave this course with a broader understanding of two ways to minimize the risk of developing a deep vein thrombosis following a total hip arthroplasty.
About
Contact Hours Awarded: 1
Course By:
Kasee Wiesen, DNP, APRN, FNP-C
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Total hip replacements or total hip arthroplasty (THA) are becoming more common. The average age of a person to have a total hip arthroplasty is 65.7 years; persons of any age may receive one. According to data collected from the Centers for Medicare & Medicaid Services (CMS) Medicare/Medicaid Part B National Summary, from 2000 to 2019, the estimated annual volume of THAs increased by 177%, and based on this trend, it is estimated that by 2040, THA procedures will increase by 176% [5].
Due to the predicted increase in THA procedures, it is important to have a strong understanding of the procedure, including who may benefit from it, possible postoperative complications, and what to expect during the recovery period.
Definition
What Does a Hip Replacement Entail?
- In simplified terms, a total hip arthroplasty involves replacing the damaged bone or cartilage of the hip with a prosthesis.
- The femoral head may be removed and replaced with a metal stem, which may be cemented or “press fit” into the center of the femoral bone. A metal or ceramic ball is placed on the end of the metal stem.
- The acetabulum is removed and replaced with a metal socket which is held in place by either cement or screws.
- A metal, plastic, or ceramic spacer is inserted between the new ball and socket to provide a smooth, gliding surface [7].
Anatomy of the Hip
- The hip is a ball-and-socket joint and one of the largest weight-bearing joints in the body. It consists of two major parts—the femoral head and the acetabulum.
- The femoral head is the top of the femur and is ball-shaped.
- The acetabulum is the socket in your pelvis and is where the femoral head fits [2].
- Other vital parts of the hip include:
- Cartilage, which covers the end of the femoral head and provides cushion and shock absorption when you walk. The synovium wraps around the bones of the hip and provides lubrication, which allows your hip to move smoothly. The bursa is a fluid-filled sac that provides a smooth surface for the bones, muscles, and tendons to move on [8].
- Ligaments form the joint capsule by connecting the femoral head to the acetabulum, stabilizing the hip. And tendons connect the muscles to the bones of the hip [8].
- Five major muscle groups assist with hip stability and mobility, including the gluteal muscles, adductor muscles, iliopsoas muscle, quadriceps, and hamstrings [2].
- Blood vessels provide blood supply to the hip and nerves, including the sciatic nerve that runs through the hip [8].
Signs and Symptoms
Signs you may experience indicating the need for a hip replacement include persistent hip pain despite taking pain medication. This pain may be described as tightness or stiffness and could start in the anterior hip, groin, buttock, or trochanter region and radiate to the thigh or knee. The pain is typically worse with movement, including walking, going up and down stairs, and standing. Depending on the severity of symptoms, the pain may also occur at rest [3].
Indications For a Total Hip Arthroplasty
- Osteoarthritis, also known as degenerative joint disease or wear and tear of the joint, occurs when the cartilage, which covers the end of the bones and helps the joint move smoothly, is damaged [6].
- Rheumatoid Arthritis (RA) is an autoimmune disorder that causes inflammation of the joints throughout the body. The inflammation caused by RA wears down the cartilage, leading to damaged and deformed joints [6].
- Osteonecrosis occurs when the blood supply to the hip joint is interrupted, possibly leading to bone collapse and deformity. This may occur following a traumatic event, such as a fracture or dislocation of the hip [6].
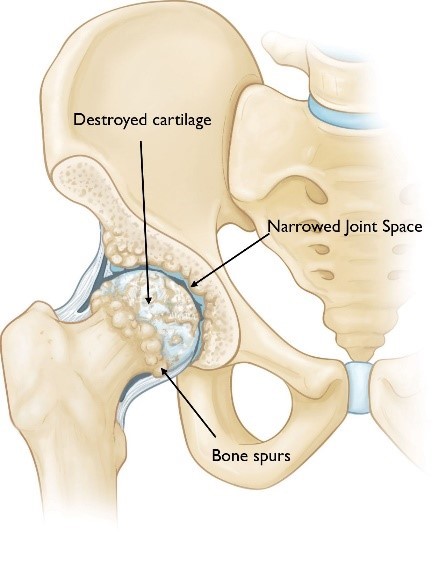
Image 1. Osteoarthritis [5]

Self-Quiz
Ask Yourself...
- What is one supportive structure of the hip?
- What are the two major parts of the hip?
- What are two possible signs or symptoms that would warrant further evaluation of the hip?
- What is one possible cause of needing a total hip arthroplasty?
Pre-Operative Evaluation
Every patient should undergo a preoperative evaluation before progressing with total hip arthroplasty. This is essential to ensure the appropriateness of the surgery, determine if additional testing needs to be completed before surgery, identify any health concerns that need to be monitored closely before and after surgery, and assist with surgical planning [5].
Consult with Orthopedics
Before proceeding with a total hip arthroplasty, an orthopedic specialist will consult to determine its appropriateness and whether the patient would benefit from the surgery. This evaluation often includes an X-ray, MRI, and physical exam [5].
Once the surgeon determines a patient would benefit from a THA, they will review the surgical procedure and discuss possible risks and complications of the surgery and post-operative planning (discharge placement, physical therapy, occupational therapy, etc.). The orthopedic surgeon will also refer the patient to their primary care provider (PCP) for a presurgical evaluation [5].
Pre-surgical Evaluation
The PCP typically completes the presurgical evaluation with instructions from the orthopedic surgeon and anesthesia. The PCP will perform a thorough history and physical examination, which includes updating family and surgical history, completing a head-to-toe assessment, ordering diagnostic tests, and determining if additional testing, such as an echocardiogram or preoperative clearance by a specialist, is needed prior to surgery [5].
Diagnostic Tests
Diagnostic tests completed before the THA include a complete blood count (CBC), basic metabolic panel (BMP), and urinalysis to ensure no evidence of a urinary tract infection. Other laboratory studies include prothrombin time (PT), international normalized ratio (INR), and activated partial thromboplastin time (aPTT). An electrocardiogram (EKG) may be completed based on risk factors such as personal cardiac history, obesity, age, and extensive family cardiac history [5].
Surgical Procedure
During the preoperative evaluation, the orthopedic surgeon will discuss the best approach for the patient. The three most common approaches for a THA are:
- Posterior—most common for primary and revision THA
- Direct Anterior—gaining popularity as there are reports this approach leads to decreased risk of dislocation
- Anterolateral—least commonly used approach [9]
Regarding the material used for the artificial hip, there are many different types of designs and materials used, but they all consist of two primary components:
- The ball component which is made of a strong metal or ceramic material
- The socket component is made of a durable cup of plastic, ceramic, or metal [7].
The prosthetic pieces may be cemented into place or “press fit” into the bone, which allows the bone to grow onto the components. The orthopedic surgeon evaluates the quality and strength of the bone and other factors to determine which method will be used. A combination of a cemented stem and a non-cemented socket may also be used [7].
On average, the surgery takes 1-2 hours. During this period, the orthopedic surgeon will remove the damaged cartilage and bone and place the prosthetic implants. This allows the prosthetics to restore the hip’s alignment and function [7].

Self-Quiz
Ask Yourself...
- What are two diagnostic tests that may be performed pre-operatively to ensure the patient is safe to move forward with surgery?
- What is the most common approach for a total hip arthroplasty?
Possible Complication Following a Total Hip Arthroplasty
Blood Clots
Patients who have undergone a total hip arthroplasty are at increased risk of developing a deep vein thrombosis or DVT. Each patient must be assessed before surgery by a physician or advanced practice provider and deemed low, intermediate, or high risk of developing a post-operative DVT—and based on these results, the appropriate medication regimen needs to be prescribed to minimize the risk [4].
- Low risk includes:
-
- Planned fast-track total hip arthroplasty
-
- Outpatient total hip arthroplasty
- Intermediate risk:
-
- Older than 60 years old
-
- Bilateral total hip arthroplasty
-
- Diabetic
-
- Greater than Class I heart failure
-
- Atrial fibrillation
-
- Varicose Veins
- Those deemed high risk include:
-
- Greater than Class I heart failure per the New York Heart Association
-
- Prior DVT within the last five years
-
- Atrial fibrillation treated with an anticoagulant
-
- Thrombophilia or hypercoagulable state
-
- Active Cancer
-
- Morbid obesity is classified as a body mass index (BMI) greater than 40
-
- Greater than 70 years old
Low-dose aspirin has been deemed effective in DVT prophylaxis for total hip arthroplasty, and studies have demonstrated that 81mg to 100mg a day is just as effective as a more potent dose. Those classified as intermediate or high risk may need enoxaparin, warfarin, another antiplatelet or anticoagulant, and a pneumatic device for DVT prophylaxis [4].
Early mobilization is also essential to minimize the risk of DVT development following total hip arthroplasty [4].
Infection
The two most common types of infection following a THA are surgical site infection and prosthetic joint infection. A surgical site infection can range from cellulitis to deep infections, resulting in full-thickness necrosis. Depending on the severity, the patient may need to return to the operating room for an incision and debridement (I&D) and may require hospitalization for intravenous antibiotics. Approximately 1% to 2% of people will have a prosthetic joint infection, and risk factors for developing include morbid obesity, smoking, IV drug use, and poor oral hygiene. Patients with uncontrolled diabetes, chronic renal and/or chronic liver disease, malnutrition, and HIV are also at risk. Those who develop a prosthetic joint infection may need to undergo an I&D, possible revision of the THA procedure, and IV antibiotics for an extended period [9].
Important steps are taken preoperatively, intraoperatively, and postoperatively to decrease the risk of infection. Not only does the development of prosthetic joint infection increase morbidity, but it is also a burden on the healthcare system [4].
It is important to factor in preoperative risk factors for developing a prosthetic joint infection and eliminate or treat any risks if possible. Below is a list of factors that increase the risk of infection following a THA.
- A hemoglobin A1C more significant than 7
- Obesity is classified as a BMI greater than 35
- Malnutrition as indicated by serum albumin less than 3.5
- Renal insufficiency
- Anemia is classified by a hemoglobin less than 9
- Smoking
-
- It is recommended to quit smoking at least four weeks before THA.
-
- Studies have shown that smoking leads to a 1.8-fold risk of developing a prosthetic joint infection.
- Recent history of intra-articular injection
-
- Waiting three months after the last intra-articular injection is recommended before moving forward with THA.
- Inflammatory arthritis
- Previous septic arthropathy
- Systemic infection [4]
The orthopedic surgeon, anesthesia provider, and operating room staff can help minimize the risk of prosthetic joint infection intraoperatively by
- Limiting traffic in the OR
- Double gloving and changing of gloves every 30 to 60 minutes
- Iodine and alcohol-based solutions for skin preparation
- Changing of the blade following skin incision
- Reduce operative time when possible.
-
- Prolonged operative time increases the risk of wound contamination.
- Irrigation of incision site with pulsed lavage
- Prophylactic administration of antibiotic
-
- First-generation cephalosporin or clindamycin given within 30 minutes of the incision
- Vancomycin when concerned for Methicillin-resistant Staphylococcus aureus (MRSA)
- Minimizing blood loss [4]
Total Hip Arthroplasty Dislocation
Approximately 1% to 3% of people will experience a THA dislocation, with 70% occurring within the first month following surgery. Recurrent dislocations following a THA often result in a revision THA.
Risk factors for experiencing a THA dislocation include:
- Greater than 70 years old
- History of prior hip surgery
- Drug or alcohol abuse
- Neuromuscular conditions or disorders
- Component malpositioning [9].
Other possible complications [4][9]:
- Postoperative femur fracture
- Instability of the hip
- Inequality in leg lengths
- Sciatic nerve palsy
- Vascular injury
- Iliopsoas impingement

Self-Quiz
Ask Yourself...
- In the pre-operative evaluation, what are three possible risk factors that increase the risk of postoperative infection following a THA?
- What are three steps that can be done intraoperatively to reduce the risk of post-operative infection following a THA?
- How long before surgery is it recommended a person should quit smoking to lessen the risk of post-operative infection?
- What are two factors that classify a patient as high-risk for a DVT following a THA?
Recovery From Total Hip Arthroplasty
Follow Up and Activity Level
Follow-ups with the surgeon will occur routinely following discharge from the hospital but will vary depending on your surgeon’s preference and the risk for complications following the procedure [3].
Early mobilization following THA is crucial in achieving optimal postoperative outcomes. Physical therapy is one tool used to increase mobility. It is typically prescribed following discharge and continues for several weeks to months following surgery [3].
Regular, non-impact activities such as walking, stair-climbing, swimming, golf, light tennis, and biking are encouraged once pain and strength allows. However, high-impact activities including manual labor, heavy lifting, and high intensity sports such as running should be avoided until cleared by the surgeon. Yoga and Pilates can often be re-introduced if caution is used and avoidance of extremes in range of motion to avoid dislocation [3].
Pain Management
Adequate pain management with minimal side effects is crucial for those who have undergone THA—as this allows for early mobilization of the patient and decreased morbidity following surgery. This begins before the surgery with education and exercise, which lead to improved functional outcomes following surgery. During the surgery and for 24 hours following surgery, the use of intravenous acetaminophen has a positive impact on pain, leading to decreased use of morphine. Administer acetaminophen with a non-steroidal anti-inflammatory drug or a cyclo-oxygenase-2-selective inhibitor either preoperatively or intraoperatively and continue post-operatively to achieve greater pain control.
It is recommended that pain management intraoperatively should be achieved using spinal or general anesthesia. A single-shot fascia iliaca block or local infiltration analgesia could be performed, and if the patient has received spinal anesthesia for the surgery, intrathecal morphine 0.1 mg could be considered. A dose of intravenous dexamethasone can be administered intraoperatively for its analgesic and anti-emetic effects.
Opioids should not be used routinely for postoperative pain management but instead on an as-needed basis when the other medications are not providing adequate relief. Epidural anesthesia, lumbar plexus block, femoral nerve block, and Gabapentin have been demonstrated to be beneficial for pain management during and following THA. However, they are associated with a higher risk of side effects, and therefore, it is recommended that they are not used routinely.
TENS units are not recommended post-operatively as limited data demonstrates their benefits following a THA [1].
Wound Care
Following a THA, sutures, staples, or both are used to close the incision. These will remain in place until follow-up, which typically occurs 10-14 days postoperatively. At this appointment, the surgeon will assess the incision and remove the sutures or staples if indicated.
Typically, it is advised to leave the dressing on until a follow-up appointment or dressing change instructions are provided before discharge from the hospital. Do not submerge or soak the wound in water until fully healed or told okay to do so by the surgeon to ensure adequate wound healing and minimize the risk of infection [7].
Blood Clot Prevention
Education regarding DVTs and how to minimize the risk of development post-operatively should begin in the preoperative phase. This includes education on what a DVT is, including signs and symptoms, early mobilization and use of pneumonic devices in the postoperative period, and use of antiplatelets or anticoagulants pre- and post-operatively based on risk factors and recommendations from the surgeon. [4 & 10].


Self-Quiz
Ask Yourself...
- What is key in optimizing post-operative outcomes following a THA?
- What is one way to minimize the risk of DVT formation following a THA?
- What common over-the-counter medication is used during the post-operative phase to achieve greater pain management?
- What are two activities that should be avoided until directed by the orthopedic surgeon at the follow-up appointment?
Outcomes
The goal after THA is to decrease hip pain and increase hip mobility. Most people experience noticeable improvement three months after surgery, and the improvement of symptoms can continue through the first year. Even with a successful surgery, there is a chance a person may not be able to return to all activities they could do prior to the hip pain [6].

Self-Quiz
Ask Yourself...
- What are two possible complications of a THA?
- What are two pain management options no longer recommended due to limited data demonstrating benefit following a THA?
- What is one reason to achieve adequate pain control following THA?
- What type of activities are recommended in the initial post-operative phase?
- Which over-the-counter medication has been deemed effective in preventing DVT post-operatively in low-risk patients?
- What has been deemed essential to minimize the risk of DVT development following a THA?
Conclusion
Total hip arthroplasties are a very common surgical procedure with the number of cases expected to increase over the next 15 years. It is important to discuss all your options prior to moving forward with a THA procedure.
References + Disclaimer
- Anger, M., Valovska, T., Beloeil, H., Lirk, P., Joshi, G.P., Van de Velde, M., Raeder, J. (2021). PROSPECT guideline for total hip arthroplasty: a systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia, 76 (8), 1082-1097. https://doi.org/10.1111/anae.15498
- Arthritis Foundation. (n.d.). Anatomy of the hip. https://www.arthritis.org/health-wellness/about-arthritis/where-it-hurts/anatomy-of-the-hip
- Erens, G.A. & Crowley, M. (2023). Total hip arthroplasty. UpToDate. Retrieved from https://www.uptodate.com/contents/total-hip-arthroplasty?search=total%20hip%20arthroplasty%20&source=search_result&selectedTitle=1%7E146&usage_type=default&display_rank=1#H392071945
- Fontalis, A., Berry, D.J., Shimmin, A., Slullitel, P.A., Buttaro, M.A., Li, C., Malchau, H., Haddad, F.S. (2021). Prevention of early complications following a total hip replacement. SICOT-J, 7 (61). https://doi.org/10.1051/sicotj/2021060
- Hedge, V., Stambough, J.B., Levine, B.R., Springer, B.D. (2023). Highlights of the 2022 American Joint Replacement Registry Annual Report. Arthroplasty Today, 21(101137). https://doi.org/10.1016/j.artd.2023.101137.
- Mayo Clinic. (2022, February 22). Hip replacement. https://www.mayoclinic.org/tests-procedures/hip-replacement/about/pac-20385042
- Sheth, N.P. & Foran, J.R.H. (2024, February). Total hip replacement. The American Academy of Orthopaedic Surgeons. https://orthoinfo.aaos.org/en/treatment/total-hip-replacement/
- The Cleveland Clinic. Hip joint. https://my.clevelandclinic.org/health/body/24675-hip-joint
- Varacallo, M., Luo, T.D., Johanson, N.A. (2023, August 4). Total hip arthroplasty techniques. Stat Perles Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507864/
- Yu, X., Wu, Y., & Ning, R. (2021). The deep vein thrombosis of lower limb after total hip arthroplasty: what should we care. BMC Musculoskeletal Disorders, 22(1), 547. https://link.springer.com/article/10.1186/s12891-021-04417-z
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
