Transcutaneous Pacing Review
Contact Hours: 2
Author(s):
Sandy A. Salicco, MSN, RN, CCRN
Course Highlights
- In this Transcutaneous Pacing Review course, we will learn about at least three reasons a person would need to have a transcutaneous pacemaker applied, including appropriate cardiac arrhythmias.
- You’ll also learn correct placement and care of transcutaneous pacemaker pads.
- You’ll leave this course with a broader understanding of proper settings and functions of the transcutaneous pacemaker to assure best possible patient outcomes.
Introduction
Transcutaneous Pacing (TCP), also known as External Pacing, is an intervention that an RN or APRN could apply at the bedside should a patient become unstable and meet the specific criteria. This usually requires a certain thorough and documented competency and will depend on the facility’s requirements. Like many procedures that are high risk but low volume, such as transcutaneous pacing, it is often highly recommended to do an annual review or skills fair to help nurses care for patients who could benefit from its use.
Knowledge about external pacing is also provided with Advanced Cardiovascular Life Support (ACLS) training. Still, due to time constraints, an overview is usually given, but it is not a step-by-step competency. ACLS is a mandatory requirement in critical care settings, such as in an ED, ICU, or PACU, to name a few, but it is only required for renewal every two years. [2]
Background History
Transcutaneous pacing was first introduced by Zoll and associates in 1956 as a novel method of treating asystole and significant bradyarrhythmias. However, the high current densities that the skin electrodes required to pace the cardiac tissue in those early devices caused painful stimulation of the cutaneous nerves and underlying skeletal muscles. [6]
With the development of transvenous pacing leads later in the 1950s, interest in external pacing waned. Transvenous pacing has been the mainstay of urgent temporary pacing since then, although the significant time and operator skill needed to implement the technique are less than ideal. As a result, noninvasive pacing reemerged in the 1980s as a therapy for bradycardia and asystole. Technical advances, including large adhesive electrodes and ECG filtering, have largely overcome the early problems of extreme discomfort and interpretation of capture on the ECG. [6]
External noninvasive pacing offers several advantages over invasive pacing. It is widely available on most crash carts, along with defibrillator units. It is easy to perform and requires minimal training and, therefore, may be instituted by physicians, nurses, and paramedics. Because it can be performed quickly, noninvasive pacing can be initiated almost immediately, eliminating the setup and the insertion time of invasive techniques (transvenous and epicardial pacing). Noninvasive pacing carries a much smaller risk of serious complications than invasive techniques, and it is more cost-effective. [6]
Indications
Transcutaneous Pacing TCP is a temporary bridge to help stabilize a patient until cardiac function and cardiac output return to normal, such as in a reversible medication overdose, as can be the case with digoxin toxicity. Another indication would be for severe bradycardia that cannot be controlled with medication, such as atropine or epinephrine. TCP, the “bridge,” can be applied quickly and with little complication until a permanent pacemaker can be implanted as needed. [1][4][5][6]
Bradyarrhythmias
Bradycardia, in and of itself, is not necessarily an automatic given for the application and use of TCP. However, those who are symptomatic because of a reduction in cardiac output, as evidenced by a drop in blood pressure, or a change in level of consciousness may benefit the most. This is also known as being hemodynamically unstable.
Examples of common bradyarrhythmias rhythms, often associated with the use of TCP in the unstable patient (there may be others), are shown below:
Sinus bradycardia (not responsive to medications) [9]:

Atrioventricular (AV) heart block,s including second- and third-degree heart blocks (with a slow ventricular response) [9]:


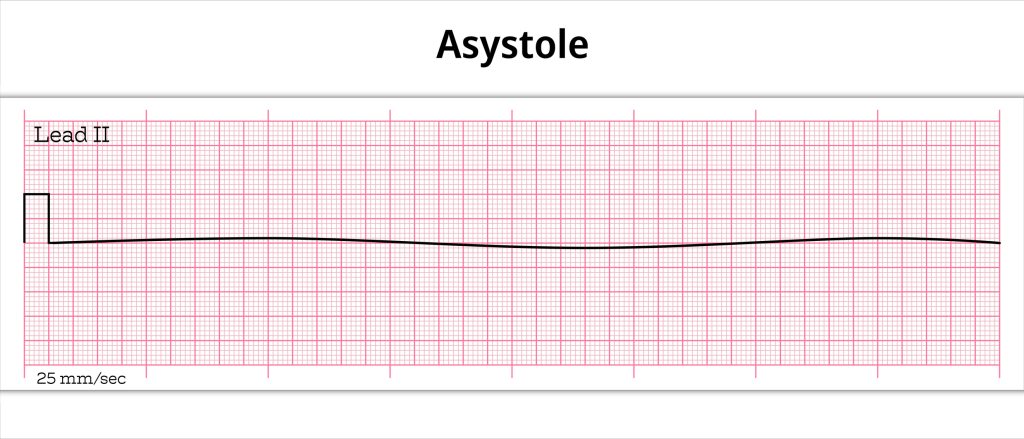
Asystole (asystolic cardiac arrest, only if used early) [9]:
NOTE: All of these bradyarrhythmias must be symptomatic, as there have been cases when a patient has had a complete heart block but remains hemodynamically stable. In this case, the patient may eventually need a permanent pacemaker, but the bridge of TCP may not be necessary. The patient will still need to be monitored continuously and carefully until the permanent pacemaker has been inserted.
American Heart Association Guidelines for Bradycardia
The American Heart Association has specific guidelines for the management of Bradycardia – see the following outline summary of their algorithm [2]:
- Bradycardia for an adult patient is less than 60bpm
- The patient would only fit TCP criteria if hemodynamically unstable – i.e., poor perfusion
- Signs would include altered mental status, possible chest pain, hypotension, or any signs of shock
- If unstable, make sure BLS / ACLS protocols are followed and placed on all relative monitors
- Cardiac (identify and document the rhythm), B/P, and Pulse Oximetry
- Continue to monitor often for Adequate perfusion
- If Poor or Declining perfusion:
- Prepare for Transcutaneous Pacing – (Locate appropriate machine, pads, etc., and speak with patient/family about this option)
- Consider Atropine 0.5 mg IV while awaiting Pacer (*May give up to 3 mg total dose in increments).
- If Atropine is ineffective in increasing pulse and perfusion, begin pacing
- Consider Epinephrine (2-10 µg/min) or Dopamine 2 – 10 µg/ kg per minute as infusion while awaiting Pacer, or if pacing is ineffective
- Next:
- Prepare for Transvenous Pacing
- Treat all contributing causes (*See section below regarding same)
- Get expert consultation – i.e., Emergency Physician, Intensivist, or Cardiologist
Possible Causes of Bradycardia
Some causes of bradycardia include:
- Medications, especially cardiac specific such as digoxin and beta blockers
- Myocardial Infarction (MI), especially an Inferior Wall (IWMI) that causes atrioventricular blocks that can often be transient
- Electrical conduction defects, which often occur with advanced age
- Severe hypothermia
In very rare cases, TCP may be used in certain types of Ventricular Tachycardia, such as in postoperative atrial flutter, but only after all other options have been exhausted [4]
Ask yourself...
- What are 2-3 possible reasons a patient may need a transcutaneous pacemaker (TCP)?
- Does every patient with bradycardia of any type need TCP?
- What medications may decrease heart rate? Can you name at least two?
- Are you aware of reversal agents that can be used for medications that decrease heart rate?
- What medications can be used to speed up heart rate therapeutically? Can you name at least two?
- If medications or transcutaneous pacing is not working and you cannot feel a pulse, what is the next nursing action you must take immediately?
- Can an LPN/LVN ever be assigned to a patient with a TCP?
Contraindications of Transcutaneous Pacing
Contraindications of transcutaneous pacing include:
- Prolonged asystole
- Severe hypothermia
- Asymptomatic hemodynamically stable patients
Ask yourself...
- Which of the following patients would fit the emergent need and, therefore, be considered for the application of TCP?
-
- Any adult patient with a core body temperature of 35.2° C
- A 36-year-old athlete with a resting HR of 48 bpm (seen as sinus bradycardia on the EKG), B/P 110/68, and no other issues
- A 54-yeard-old patient who had an IWMI and now has a second-degree heart block, an HR of 54, B/P of 116/ 64, and a decline in the level of consciousness
- A 93-year-old patient with a resting heart rate of 36 bpm (seen as severe bradycardia on EKG), B/P 100/60, no change in mental status, and able to do ADLs at home
- A 45-year-old with unresolvable chest pain, sinus bradycardia of 42 bpm, B/P of 90/60, pulse ox (SaO2) of 92%, pale and diaphoretic, and speaking incoherently
Pacemaker Application and Procedure
The following is the pacemaker application process [1][3][4][7][10][11]:
Prior to Beginning the Procedure
Before starting, be absolutely certain that Pacer Mode has been turned on!
- Pacemaker Functions noted below as shown by Arrow (all color coordinated)
- There is the Pacer Dial, the Output (mA / electricity) Dial and the Rate Dial (ppm)
- *NOTE: Front of Monitor/ Defibrillator / Pacer will look a little differently, depending on the Manufacturer
- Two Manufacturers’ Monitors are pictured below:

Image 1. Zoll r Series® [9]
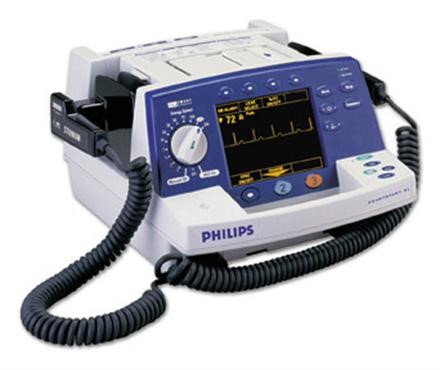
Image 2. Philips HeartStart XL® [7]
Preparation
- When possible, the skin should be clean and dry (soap & water, or alcohol wipes are appropriate)
- Hair should be removed but not shaved with a straight-edge razor (most facilities use a hair clipper). This allows for the best conduction between pad and skin.
- Make sure pacer pads are ready to be used/applied (*There should be two external pacer pads per package)
- The package should not be opened prior to use (as conduction gel may become dry)
- Check to be certain the date on the package is current/ not expired (or else this could cause poor function)
- Always have a spare pair of pacer pads available while the patient is receiving TCP therapy (in an emergency, you will not have time to retrieve a new set)
- Check to make sure that wires/cables have no frays or tears
- Remove any jewelry that could be in close contact with electrodes (e.g., neck chains & piercings) as this could lead to burns during pacing due to electrical conduction
Application
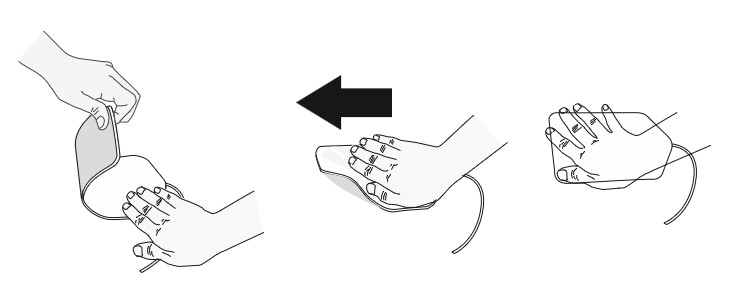
The application process is as follows [7][11]:
- Most manufacturers recommend the anterior/posterior placement of the pads – also known as transthoracic pacing (*i.e. on the back and avoid placement over spine and the precordium)
- The pads may also be placed on right upper quadrant of chest and left lower quadrant of chest – also known as anterior/lateral positioning
- Make sure the patient has no implantable devices (e.g. infusion port). If so, avoid placing a pad over the device, as this could cause harm
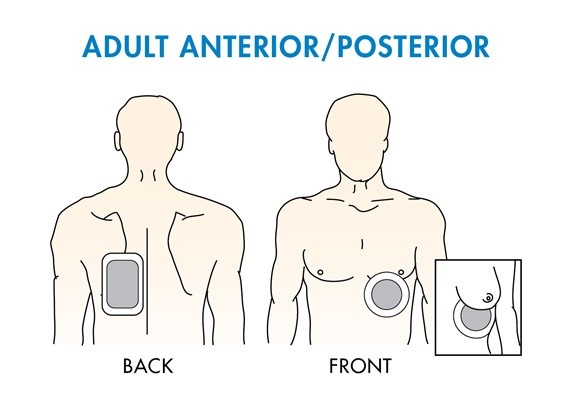
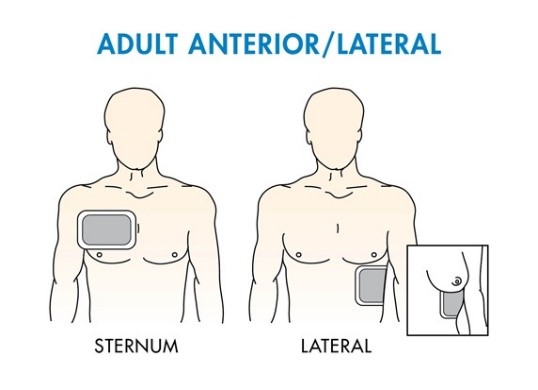
- When securing pads in place, gently, but firmly apply and press from one end to the other, working out any possible air bubbles [7][11]. Air bubbles will provide poor pacing outcomes and possibly cause burns to the skin.
- Be certain that you read and follow directions written by the individual manufacturer (*often placement positions with pictures are also on the package of each set of pads for Quick Reference)
Pacer Settings
- Check Settings: There are primarily two settings or modalities to prepare when using TCP [7][11]:
- Output Current: Range is usually 0-140 mA
- Current will depend on the size of the patient – also known as an impedance to flow – the larger the patient’s chest, the more mA will be required to pace the heart
- Use the minimal amount to get capture for maximum patient comfort
- In most average-sized patients, 40-80 mA should suffice to provide capture
- Lower stimulation currents produce less skeletal muscle contraction and are better tolerated and less painful to the patient
- Rate: 30-180 ppm (pulses per minute)
- You may also choose to set on-demand (when needed) or asynchronous pacing (paces at a set rate). The minimal setting for heart rate that will provide adequate cardiac output is recommended (Note: this will vary by individual and may not fit the standard 60-100 bpm)
- Output Current: Range is usually 0-140 mA
- Set Rate: Set the rate 10-20 bpm (ppm) above the patient’s underlying/intrinsic rate. If the patient has an absent heart rate, set the rate at 100
- Start Electricity: Start the mA (electricity) at zero and gradually increase until a pacer spike with capture is noted and the patient has a pulse
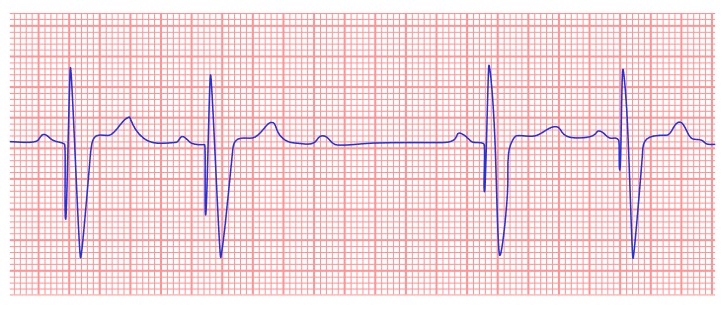
- Special Note: If the patient has an intrinsic heart rate (beats spontaneously), make sure you can visualize a clear R-wave configuration with sound amplitude – if no or poor R-wave is seen, consider changing the Lead Selection on the Monitor
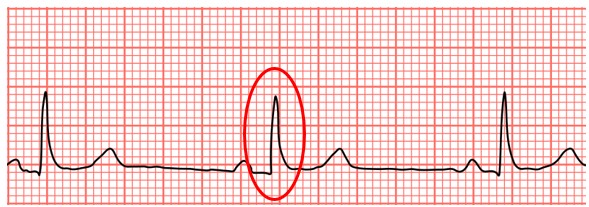
Image 3. Example of R-wave configuration in Lead II [9]
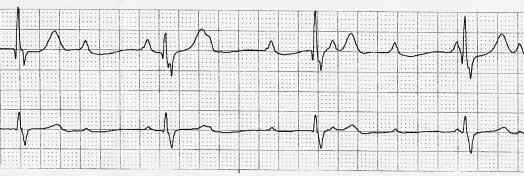
- True Capture with TCP (Pacer spike with wide QRS Complex):
- It is important to recognize when pacing stimulation has produced a ventricular response (capture). Determination of capture must be assessed both electrically and mechanically in order to ensure appropriate circulatory support of the patient
- The patient must also have a palpable pulse with each complex (usually a core pulse such as brachial, femoral, or carotid at the very least)
- The patient should also have a measurable (and often improving) blood pressure
- It is important to recognize when pacing stimulation has produced a ventricular response (capture). Determination of capture must be assessed both electrically and mechanically in order to ensure appropriate circulatory support of the patient
- Level of consciousness should also improve (more awake, alert, and responsive) – in the absence of opioids and/ or sedatives.
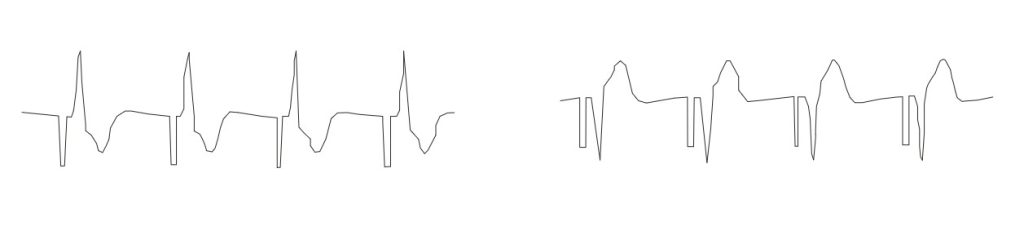
Image 4. Simulated Rhythm, Captured (two differed configurations) [11]
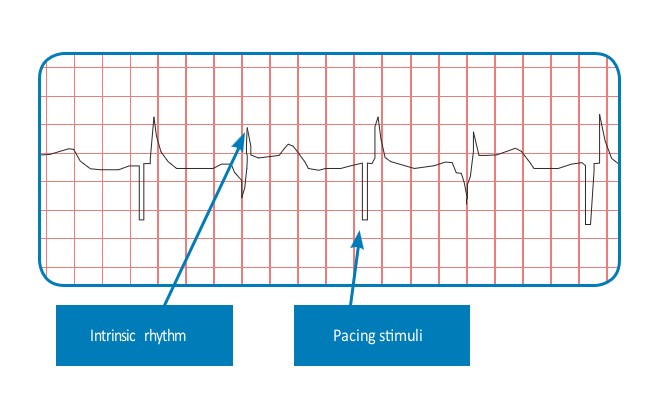
Image 4. Simulated Rhythm, Non-Captured [8]
**Very Important Note: Even if a patient has a beautiful complex on the EKG tracing, paced or not, a pulse needs to be checked routinely, especially if the patient is unconscious. Remember, the heart has both electrical and mechanical functions. An electrical complex without a pulse can be Pulseless Electrical Activity (PEA), and essentially the patient may die if not recognized quickly! [2]
Ask yourself...
- What should the nurse do if they notice that the TCP pads package indicates that they are outdated?
- Are all cardiac monitors the same? What special feature must a cardiac monitor have to perform TCP?
- Do you understand the rationale as to why air bubbles must be removed under the pacer pads?
- Name two locations to check for a core (central) pulse.
- Do you know how to set your patient’s proper heart rate (bpm)?
- Do you know what value (number) to set the mA (electricity) at the start of the TCP?
- What is PEA?
- What complex must be present, and must the pacer spike be followed to ensure capture?
The Nurse’s Role / Considerations
The following interventions should be implemented by the nurse when managing TCP [1][3][4][5][7][11]:
- Whenever possible, inform the patient and/ or family of the situation and treatment plan and give informed consent
- The physician of record should explain consent – explaining the risks, benefits, & alternatives
- The nurse is the witness to the signature of the patient/family
- Consent is only waived in a life-threatening emergency, and the appropriate physician must clearly document it.
- Assure the patient/family that some type of analgesia will be administered, as well as possible sedation, as this can be a rather painful procedure.
- Closely monitor the patient when utilizing TCP. This often requires 1:1 or 1:2 nurse-to-patient ratio
- Obtain education and training on all aspects of TCP, including cardiac rhythms, before application, as well as how to monitor the rhythms induced by TCP.
- Be aware of the types of medications that may be utilized during TCP and be able to administer and monitor them appropriately.
- This includes the actions, side effects, and the possible use of reversal agents as needed.
- Most often, these are pain medications that may include opioids and sedatives, which may be used alone or in combination.
- Medications are usually physician-driven or facility-specific based on the facility formulary.
- Periodically check for the patient’s intrinsic/underlying rhythm
- Know how to operate the device properly. Proper operation of the device, together with correct electrode placement, is critical for obtaining optimal results. Every operator must be thoroughly familiar with these operating instructions.
- Complete an in-service when new to a facility or unit or when the facility purchases new equipment.
- Perform an annual review and or competency, at minimum, (especially if low volume of use). This is an ethical nursing responsibility based on area one chooses to work.
Ask yourself...
- What are at least three considerations that are the responsibilities of the nurse regarding the use of TCP therapy on a patient?
- Does the nurse need training and/or certification in basic cardiac rhythms and arrhythmias?
- If you give your patient a narcotic while on TCP, do you know the reversal agent to have on standby if needed?
- If you used a sedative, e.g., versed, do you know what reversal agent to have on standby if needed?
- Is it important for the nurse to have regular refresher training on the application and monitoring of a patient receiving TCP?
- Is the nurse responsible for attaining the consent for TCP?
Trouble Shooting (Complications)
The following are complications of TCP [3][4]:
Failure to Capture
A complication of TCP is failure to capture (no ventricular capture beat). This means that there are pacemaker spikes with no QRS complex following; this means that the pacemaker is not functioning properly, which will not deliver optimal cardiac output for the patient (see below) [9]:
Nursing Actions:
- Check pads to make sure they are on and intact
- Be certain cables are connected correctly
- Check the patient’s pulse to ensure there is some cardiac output
- Change pacer pads as needed (this may especially be needed if in place for several hours or if the patient should become diaphoretic)
- Increase output current (mA) gradually – 2 mA at a time
Undersensing
A second complication of TCP is undersensing (also known as ventricular undersensing). This means that the pacemaker is firing random pacer spikes regardless of the ventricular activity that is present. The proper function should be a pacer spike, followed immediately by a QRS complex (see below) [9]:

Nursing Actions:
- Check pads to make sure they are on and intact
- Be certain all cables are connected correctly
- Check the patient’s pulse to ensure there is some cardiac output
- Change pacer pads as needed (this may especially be needed if in place for several hours or if the patient should become diaphoretic)
- Change pacer pad locations (per manufacturer recommendations)
Oversensing
A third complication of TCP is oversensing. This means the pacemaker is not “seeing” or sensing that a pacer spike and QRS complex are “needed” based on the programmed settings. Rather, it is “over-seeing” something that is not there. The proper function should be no pauses, and each complex (pacer spike with QRS) should happen at an equal distance from each other (see below) [9]:
Nursing Actions:
- Check pads to make sure they are on and intact
- Be certain all cables are connected correctly
- Check the patient’s pulse to ensure there is some cardiac output
- Change pacer pads as needed (this may especially be needed if in place for several hours or if the patient should become diaphoretic)
- Change pacer pad locations (per manufacturer recommendations)
Cutaneous Burns
A fourth complication of TCP is cutaneous burns. This can happen even with the best of care and proper lead placement
Nursing Action:
- Remove once transient arrhythmia is gone and the patient is stable
- Remove when there is a permanent transvenous pacemaker implanted and functioning properly
- Only remove when the patient is hemodynamically stable
- May be removed once the patient is pronounced dead, per facility and state protocols
- Examine skin under the pads as there can be evidence of burns that may require additional treatment
- Take pictures per facility protocol
- Inform physician
- Consult wound care specialist and apply recommended therapy as ordered
Ask yourself...
- What should the nurse do if he/ she notices that the TCP pads package indicates that they are outdated?
- How many sets of pacer pads should the prudent nurse have readily available when preparing to begin TCP?
- If you feel the TCP therapy is not working correctly, can you name at least 2-3 steps to take when troubleshooting almost every scenario?
- Is it important for the nurse to have regular refresher training on the application and monitoring of a patient receiving TCP?
- What steps should a nurse take should a burn be discovered under the TCP pad?
Case Studies
Case Study 1
A 65-year-old man is brought to the emergency department after he was found unconscious in his bedroom. His wife states that she found an empty bottle of her husband’s depression medication beside him. The patient has a medical history significant for major depressive disorder with atypical features. He made a suicide attempt a year ago. His blood pressure is currently 110/80 mm Hg, and his heart rate is 55 bpm and is regular, but thready. An electrocardiogram reveals a complete heart block. Aggressive resuscitative efforts, including medications, have failed thus far, and the patient’s condition is rapidly deteriorating.
Ask yourself...
- Is there a need for TCP? If Yes, why? If not, why not?
- What possible cardiac rhythm(s) would you expect to see?
- Would you know how to identify each on a monitor strip?
- Can you name the contributing causes of the various rhythms?
- Could any patient’s medications have contributed to his / her current condition? If so, which one(s)?
- If you had to use transcutaneous pacing, would you feel comfortable with the setup and facilitation?
- If TCP was on the patient, and settings were decided, how would you confirm that it was working well for the patient?
- Could you name 2-3 indicators confirming the patient’s hemodynamic status improves once TCP is initiated?
Case Study 2
A 92-year-old patient comes into the ER complaining of a GI upset. She says she has had this on and off for about a week. She has mild hypertension and takes olmesartan 20 mg once a day. She says she has a “touch of arthritis” and takes an occasional aspirin or two.
On a brief general assessment, she is noted to be awake, alert, and oriented to person, place, and time. She moves all extremities fairly well and uses no assistive devices. She admits to wearing bifocals and says her hearing is not as good as it used to be, but she does not use hearing aids. She says she still drives, but not far, only to places like church and the grocery store.
The nurse took her vital signs, and these are the current results: B/P 118/76, HR 36, RR 16, T 97.5F.
Due to her HR, the nurse decides to place her on the cardiac monitor (in the lead II and V2), and the following rhythm is noted [9]:
The nurse asks her if she ever feels dizzy or lightheaded, especially with activity, but the patient denies it.
Ask yourself...
- Is there a need for TCP? If Yes, why? If not, why not?
- What possible cardiac rhythm(s) would you expect to see?
- Would you know how to identify each on a monitor strip?
- Can you name the contributing causes of the various rhythms?
- Could any patient’s medications have contributed to his / her current condition? If so, which one(s)?
- If you had to use transcutaneous pacing, would you feel comfortable with the setup and facilitation?
- If TCP was on the patient, and settings were decided, how would you confirm that it was working well for the patient?
- Could you name 2-3 indicators confirming the patient’s hemodynamic status improves once TCP is initiated?
Conclusion
Transcutaneous pacing can be a valuable therapeutic technique to increase cardiac output and tissue perfusion, especially to vital organs such as the brain, lungs, and kidneys. It can be rapidly initiated by those who are trained to do so and monitored fairly easily. [1]
External pacing is one of the quickest and easiest methods for treating multiple conduction abnormalities. Furthermore, it can be used under various circumstances, ranging from drug-induced electrical disturbances to conduction system inhibition secondary to myocardial infarction. It can be applied in a variety of settings. [3]
Non-invasive pacing carries a much smaller risk of serious complications than invasive techniques and is more cost-effective; however, it is only a temporary treatment option. [1]
References + Disclaimer
- Adams, A., & Adams., C. (2021). Transcutaneous pacing: An emergency nurse’s guide. Journal of Emergency Nursing, pp 326-330. Retrieved from: https://www.sciencedirect.com/science/article/ on 5/15/2024
- American Heart Association (AHA). (2020). Advanced cardiovascular life support: Student manual.
- Craig, K. (2006). How to provide transcutaneous pacing. Cardiac insider.
- Crofoot, M., Sarwar, A., & Weir, A. (2022). External pacemaker. Stat Pearls [Internet]. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK519567/ on 6/7/2024, and Retrieved from: http://journals.lww.com/nursing on 5/30/2024
- Deal, Ahn, Wang, & Solomon (2011). Transcutaneous and transvenous cardiac pacing. American College of Emergency Physicians. Retrieved from: https://www.acepnow.com/article/transcutaneous-transvenous-cardiac-pacing/ on 6/18/2024.
- Doukky, R., Bargout, R., Kelly, R., & Calvin, J. (2003). Using transcutaneous cardiac pacing to best advantage. Journal of Critical Illness, 18(5):219-225. Manuscript last reviewed February 15, 2019.
- Philips. (2019). Non-invasive transcutaneous pacing. Retrieved from: https://www.documents.philips.com/assets/20191003 on August 9, 2024.
- Sovari, A., Kocheril, A., & Assadi, A. (2021). Transcutaneous cardiac pacing. Medscape. Retrieved from: https://emedicine.medscape.com/article/98939 on 5/13/2024.
- Wikimedia (ND). Wikimedia Commons, the free media repository. Retrieved from https://commons.wikimedia.org/wiki/Category:Images on 5/30/2024.
- Zoll Medical Corporation (2014). OneStep® Pacing. Retrieved from: www.zoll.com on 5/28/2024.
- Zoll Medical Corporation (2018). R Series® ALS Operators Guide. Retrieved from https://www.zoll.com/-/media/public-site/products/r-series-defibrillators on 6/25/2024.
- Zoll Medical Corporation (2024). External pacing technology. Retrieved from: https://www.zoll.com/medical-technology/pacing on 5/13/2024.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
