Course
Tricuspid Valve Replacement
Course Highlights
- In this Tricuspid Valve Replacement course, we will learn about valvular disease and clinical and anatomical factors that lead to requiring tricuspid valve replacement.
- You’ll also learn the clinical manifestations and anatomical variations associated with tricuspid atresia, regurgitation, and stenosis.
- You’ll leave this course with a broader understanding individualized care plans and interventions for patients with tricuspid valve disorder, interventions, and postoperative care, as well as medical management.
About
Contact Hours Awarded: 2
Author: Molina Allen, MSN, RN, CCRN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
The tricuspid valve is a tri-leaflet conduit between the right atrium and the right ventricular. Its leaflets can be damaged or diseased, and they may not function as expected. The valve’s importance is to provide the pressure required to move blood through to the right atrium and, ultimately, the pulmonary system (1, 3).
Three main issues can occur with the tricuspid valve: atresia, regurgitation, and stenosis. Medical treatment is the initial treatment for mild to moderate tricuspid valvular conditions; however, surgical interventions are required to prevent complications from the cardiac system having to overcompensate for the dysfunction of the right heart. Symptoms typically worsen over time, progressing from fatigue and weakness to hepatic involvement, palpitations, and edema (1, 2).

Self-Quiz
Ask Yourself...
- When thinking about the primary function of the tricuspid valve, how does this contribute to the body’s overall circulation?
- When discussing with a patient, how can the nurse reiterate that being without symptoms does not mean the valve functions appropriately?
- Heart failure can be debilitating and affect many aspects of a patient’s life. How would you best approach this topic with a newly diagnosed patient?
History/Background
As heart surgery advanced with innovative treatments and improved outcomes, valve management expanded beyond medical therapy. The tricuspid valve is the most difficult to treat, with the highest mortality rates. Traditionally, repairs were attempted for moderate valve disease; however, surgical replacement is required for severe valvular heart disease. For 1.6 million Americans who are affected by mild to severe tricuspid disease, the only option was surgery to repair or replace the valve in conjunction with medical management (8).
Valve repairs had been successfully executed since the 1920s; however, valve replacement was impossible until the heart-lung bypass machine was developed. With this innovative medical advancement, open heart surgery became a reality. The first mechanical valve repair occurred in 1952 at Georgetown University (7).
The first mechanical valve was designed as a tube with a ball inside to block the opening when pressure decreased. Towards the end of the decade, advances were made with the ability to utilize donor grafts. There are two types of biological grafts, made of harvested tissue. An allograft is garnered from a deceased human donor, while a xenograft is a prosthesis that is obtained from pig or cow tissue (7).
Until 2020, replacing the tricuspid valve required open heart surgery. Another option available to patients with higher surgical risks or who have already had a sternal approach is transcatheter tricuspid valve replacement. This minimally invasive approach decreases the recovery time, reduces infection risk, and may be an alternative for patients when surgery is contraindicated (8).

Self-Quiz
Ask Yourself...
- How has innovation and open-heart surgery changed the lives of patients you saw in the community and your career?
- What factors may affect the consideration of a bioprosthesis versus a mechanical one?
- Should cultural preferences affect the choice of valve?
- Significant advancements in cardiovascular treatments have occurred in the last 75 years. What other influences have affected health outcomes for cardiac patients?
General Information
Tricuspid valve replacement is considered a high-risk procedure as these patients are often medically complex with comorbidities that carry their own risk of morbidity and mortality. Most patients that undergo the risk are because valve repair has already been attempted and resulted in complications such as right ventricular dysfunction (5). Long-term studies have shown superlative outcomes with valve replacement over repair for survival rates and function of the tricuspid valve (10).
Tricuspid valve surgery inherently carries a higher risk of thromboembolic manifestations when mechanical devices are used. This risk is higher when hypokinesis of the right ventricle is present. On the other hand, biological prostheses are prone to tissue dysfunction and rapid degeneration in younger patients. Older patients who develop carcinoid syndrome or have renal failure have an increased risk of prosthesis degeneration as well. Cardiovascular surgeons often attempt to repair the tricuspid valve rather than replace it, as it can reduce the need for long-term anticoagulation therapy (5).
Guideline-directed medical therapy may manage symptoms without intervention until they are intolerable to the patient. When symptoms become severe, stages C and D, there are limited options for adequate treatment unless repair or replacement is attempted (15). Research has shown the benefit of continued medical therapy in combination with tricuspid valve replacement. This group showed improved clinical outcomes and had an overall lower rate of any cause of mortality (8).
Specific comorbidities have been found to coincide with tricuspid dysfunction. These include hypertension, hyperuricemia, cerebrovascular disease, and certain arrhythmias. Common arrhythmias include complete atrioventricular block, atrioventricular nodal reentrant tachycardia, sick sinus syndrome, and atrial fibrillation (10).

Self-Quiz
Ask Yourself...
- Tricuspid valve replacement is a high-risk surgery. How does this affect the decision-making process for the multidisciplinary care team and the patient?
- How would you explain the risk versus benefit ratio for a procedure with high morbidity and mortality rates to the patient?
- Informed consent is essential in procedures and surgeries that are high-risk. What is the nurse’s role in ensuring that the patient is autonomous and active in the decision-making process?
- What ethical considerations should be considered with the influence of innovative and new technologies versus patient comorbidities and lifestyle choices?
- What patient characteristics are important when discussing a high-risk treatment versus a more palliative approach to care?
Pathophysiology
The cardiac system has four valves separating the four chambers of the heart: tricuspid, pulmonic, mitral, and aortic. As blood flows from the body, it first passes through the tricuspid valve between the right atrium and the right ventricle. It then moves from the right ventricle to the pulmonary arterial system via a pulmonic valve. Once blood returns to the lungs to the heart, it veers through the mitral valve between the left atrium and ventricle. It finally passes through the aortic valve as the flow continues through the arterial system to transport oxygen and nutrients to vital organs and the peripheral system (2).
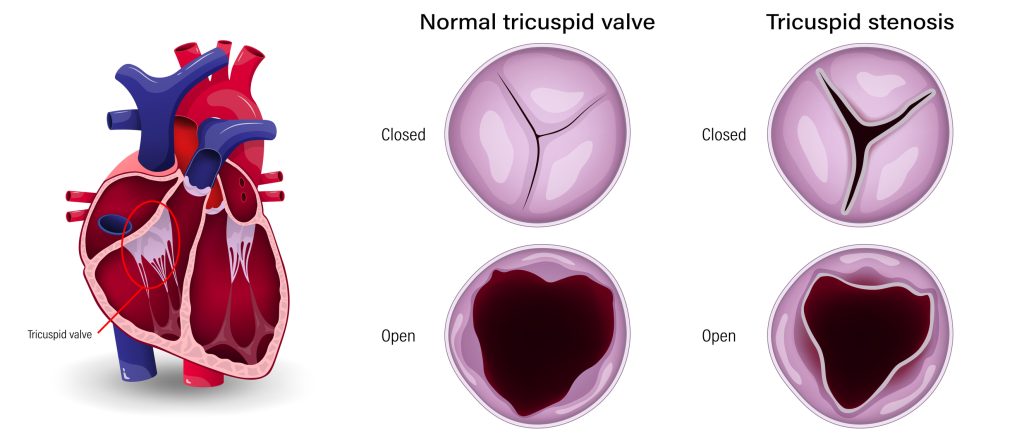
The tricuspid valve is the largest of the four cardiac valves and consists of three leaflets: septal, anterior, and posterior. It may also be referred to as the correct atrioventricular valve. With tricuspid dysfunction, there may be anomalies in the shape or number of leaflets. Approximately 40% of patients have more or fewer leaflets than expected, at times up to 6 (17). Three main conditions affect the tricuspid valve: atresia, regurgitation, and stenosis.
Tricuspid atresia is a congenital cardiac defect where the infant is born without a tricuspid valve. Congenital heart disease affects approximately 81 per 10,000, with tricuspid atresia being the third most common cyanotic congenital heart disease. It occurs at a rate of about 1.2 live births per 10,000 (4). Surgery is required within the first year of life as the mortality rate is exceptionally high without treatment.
This heart defect is categorized as cyanotic, as blood flow is restricted, limiting the amount of blood that can flow through to the right ventricle (1). The function of this valve is halted due to the formation of a muscular dimple within the right atrium. It may also involve fusions between the leaflets, causing membranes to develop where the flap should move freely, thereby restricting movement (4).
Tricuspid regurgitation may occur as a primary or secondary disorder. The abnormal anatomy of the tricuspid valvular apparatus defines the primary category. Secondary is due to dilatation of the right atria or ventricle. This is the most common cause of tricuspid regurgitation seen in adults, with imaging noting that the valvular construction is intact. In addition to the right atrium or ventricular dilatation, this disorder may also be caused by dilatation of the tricuspid annulus or tethering of the tricuspid valve leaflet (1, 12).
Pulmonary hypertension is a factor as rising proper ventricular systolic pressures lead to the cavity enlargement of the right ventricle and dilatation of the annulus. Thus, the tricuspid leaflets cannot adapt to the structural modifications. Specific cardiomyopathies that lead to pulmonary hypertension include hyperthyroidism, atrial fibrillation, pulmonic valve stenosis, and left-sided heart disease (13).
In tricuspid stenosis, the valve is narrowed or impeded. This may occur in conjunction with regurgitation. The right atrium enlarges as the blood flow is restricted and proper ventricular pressures are low. This prevents blood from circulating to the lungs to deliver oxygen (1).
Overwhelmingly, the cause of tricuspid stenosis is due to rheumatic fever. Other causes may be carcinoid syndrome, systemic lupus erythematosus, infectious vegetation, and congenital defects. Involvement of the mitral valve is commonly seen to coincide with rheumatic heart disease.
It can also be the result of implantable cardioversion/defibrillation leads becoming fused to the subvalvular structures in the presence of continuous pacing. Regardless of the root cause, the effects are unbalanced pressures between the right atrium and right ventricle with accompanying systemic fluid overload (14).
For patients with particular characteristics, such as post-lead implantation of a cardiac implantable electronic device, multivalvular disease, and left heart failure, the presence of tricuspid regurgitation is correlative to poor outcomes and increased mortality. If left untreated, follow-up at 1, 2, and 4 years has respective mortality rates of 30, 50, and 70% (17).

Self-Quiz
Ask Yourself...
- How can a nurse ensure that the patient fully understands the pathophysiology of their disease process?
- How can nursing assessments guide a patient’s care in diagnoses such as this that are progressive?
- Effective communication is essential for complicated diseases with multiple comorbidities. What communication techniques would enhance patient care?
- How do you use evidence-based care to assist a patient in making an informed decision about complicated decisions?
- Have you been involved in situations where the patient’s understanding of their treatment options did not align with the care team’s recommendations? How did you advocate for the patient?
Signs and Symptoms
The signs and symptoms of tricuspid valve dysfunction may vary depending upon the severity of clinical presentation. Mild tricuspid atresia or regurgitation dysfunction may cause fatigue, heart murmurs, palpitations, and chest discomfort or pain. These may be managed with medications such as diuretics, anti-arrhythmics, and treatment aimed at alleviating heart failure.
Valve disease is staged, and treatment will differ, requiring increasingly aggressive treatment to manage symptoms as it progresses. The four categories and characteristics of valvular dysfunction are described as follows (all from 15):
- Stage A – The patient has risk factors for valve disease by being asymptomatic,
- Stage B – Present disease is mild to moderate but not causing symptoms.
- Stage C – Heart valve disease is severe, but the symptoms are managed.
- Stage D – Valve disease is severe, as is the source of symptoms.
As the patient progresses to Stage D, symptoms are caused by right-sided heart failure that inevitably occurs. Symptoms can include the following:
- Low cardiac output, especially during exertion
- Shortness of breath and dyspnea
- Elevated jugular venous pressure
- Pleural effusions
- Ascites
- Edema
- Arrhythmias
- Fatigue
- Chest pain
- Dizziness and syncope
- Hemoptysis
- Cyanosis

Self-Quiz
Ask Yourself...
- Health literacy can significantly affect a patient’s journey through the healthcare system. What strategies do you employ to assist patients to understand and report their symptoms?
- What strategies can a nurse use to encourage patients to report their symptoms, especially when the onset may be subtle and slow?
- How would your prior experiences influence your approach to caring for a patient with a complex diagnosis, such as tricuspid valve dysfunction?
Diagnostic Testing and Evaluation
The patient’s clinical presentation guides treatment. Regular follow-ups will monitor for changing signs or symptoms. Patients with valvular disease should be educated to notify their primary care provider of increasing symptoms or feeling unwell that cannot be attributed to any other disease process or event.
A thorough history and physical will develop the patient’s baseline and symptom presence and determine if the disease has progressed to signs that align with valve dysfunction and heart failure. The healthcare team will also want to establish a baseline electrocardiograph reading to record cardiac electrical activity and assess for cardiac arrhythmias that may be currently present. This will also assist with determining the effectiveness of treatments or medicinal therapy (15).
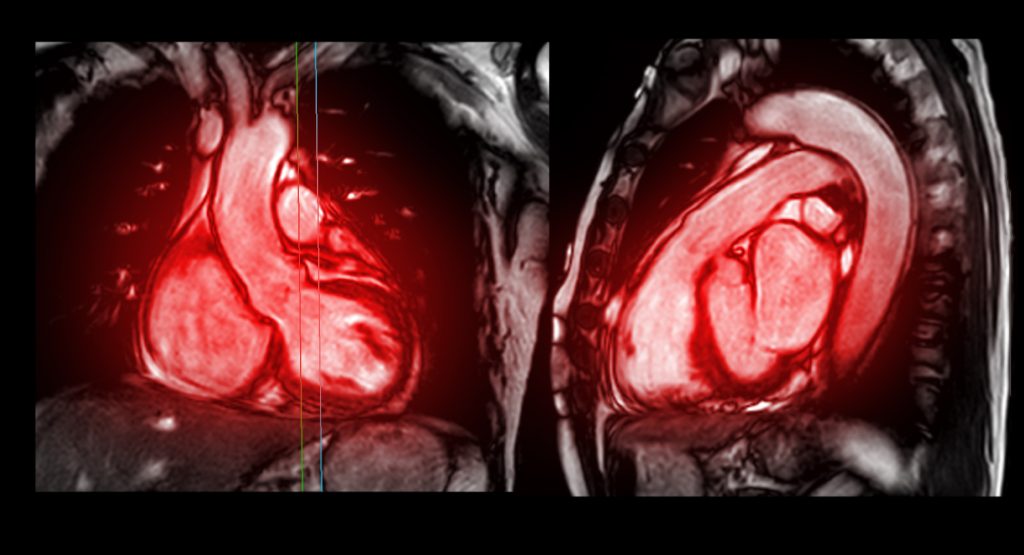
The first test typically used to assess valvular dysfunction is transthoracic echocardiography (TTE). This will reveal the valve chambers’ functionality, size, shape, and severity based on their effects on pulmonary and systemic blood flow.
Further testing may include a chest X-ray. This is especially important for patients who have developed symptoms. This imaging will show the heart size, pulmonary involvement via the presence or absence of pulmonary vascular congestion, and visualization of the pericardium or aorta calcifications.
A transesophageal echocardiogram (TEE) is a diagnostic ultrasound that can produce intricate heart images. This differs from a TTE as rather than imaging from outside the body, through the chest, a slender wand with a small transducer is passed through the oral cavity into the esophagus. This allows imaging with greater detail and captures the posterior of the heart. Doppler ultrasound and color Doppler are adjunctively used for improved visualization of blood flow through the chambers.
A TEE may also identify any abnormal masses, anomalies in structure, or other abnormal findings, such as atrial thrombus, especially within the left atrial appendage that is prone to restrictive flow or any intracardiac abscesses (15)
Cardiac magnetic resonance imaging (MRI) is an alternative method for evaluating left ventricular volumes and function, aortic disease, or severity of valve malfunction. For imaging that would identify vegetation, infection, or inflammation as a possible cause or reason for symptom exacerbation, a Positron Emission Tomography (PET) is the gold standard if there is exertional dyspnea only as a symptom, a nuclear stress test may be ordered to assess for exercise capacity.
The healthcare team may order a right heart cardiac catheterization to evaluate valves more closely. This diagnostic study uses a femoral or radial approach to guide a catheter to the superior vena cava and into the cardiac chambers for hemodynamic monitoring, visualization of the chamber with fluoroscopy and contrast, and evaluation for pulmonary pressures.
Diagnostic testing via cardiac catheterization in Stages A and B shows no clinically or diagnostic significant changes in cardiac pressures or discernable symptoms. Stage C elicits hemodynamic changes in a dilated right ventricle (RV) and right atrium (RA). The waveform for the RA will be elevated with a “c-V” wave. Symptoms that coincide with these findings include elevated venous pressures; however, the patient does not exhibit any symptoms. With Stage D, the hemodynamic monitoring will be similar to Stage C, yet the patient will be considerably more symptomatic. Common clinical symptoms and presentation include elevated venous pressures, dyspnea on exertion, edema, ascites, and fatigue (15).
Suppose the decision is made to proceed with surgery. In that case, testing specific before valve intervention includes dental examination, which will rule out possible sources of infection so that this may be treated and reduce the risk of postoperative complications. Further CTs and other diagnostic testing will be done to assess chamber and valve measurements to select the correct sizing for mechanical or biological prosthetic placement.

Self-Quiz
Ask Yourself...
- Diagnostic testing may induce anxiety in a patient; what interventions have you found successful in the past that could alleviate fear in a patient undergoing a surgical workup?
- How does the choice of imaging method relate to the patient’s presentation of symptoms?
- Should imaging results or patient symptoms drive care?
- In your practice, how has diagnostic imaging affected treatment decisions?
Types of Surgeries/Procedures
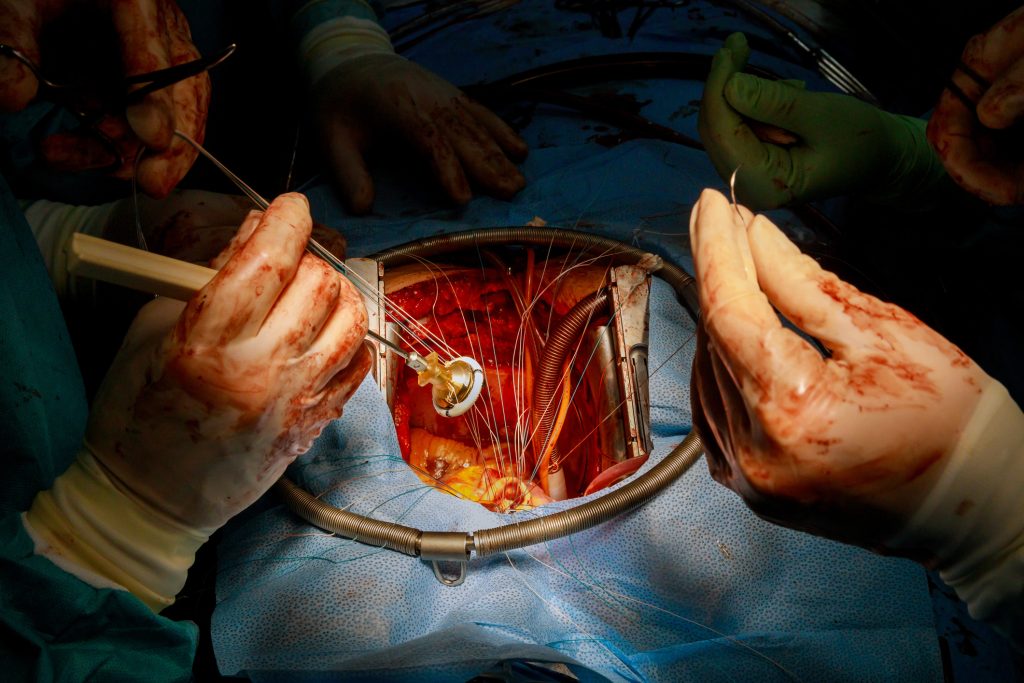
Open Heart
Open heart surgery is a major medical procedure that is performed under general anesthesia. The chest is surgically opened, exposing the sternum. A sternotomy is performed, cutting through the breastbone and separating to open the chest, revealing the heart and lungs. Blood flow is bypassed via a cardiopulmonary bypass pump. This biomedical equipment is operated by a healthcare provider called a Perfusionist.
Venous blood is removed from the patient to a reservoir that oxygenates and filters. The oxygenated blood is then returned to the arterial system for the perfusion of organs while the heart is kept in stasis (9). Bypass perfusion is established via the ascending aorta with drainage from the bicameral or right atrium. Hypothermia may be induced if clinically indicated.
Hypothermia is the induction of a body core temperature below 35 ° C. It is used in cardiac surgery to prevent ischemic injury of organs and the central nervous system. This is accomplished by decreasing oxygen consumption and energy demand, which leads to decreased cellular metabolism (11). A circulatory arrest can be achieved by slowing the metabolic system required to perform complex cardiac surgery.
A secondary open approach is to incision through the right thoracic cavity. This is referred to as a lateral thoracotomy, creating a window to the patient’s chest cavity. A heart-lung bypass is still required. As a smaller area is opened, operative time, bleeding risk, and chest tube insertion time are lessened. There are fewer complications, and the post-surgical intensive care unit days of admission were reduced (4, 5).
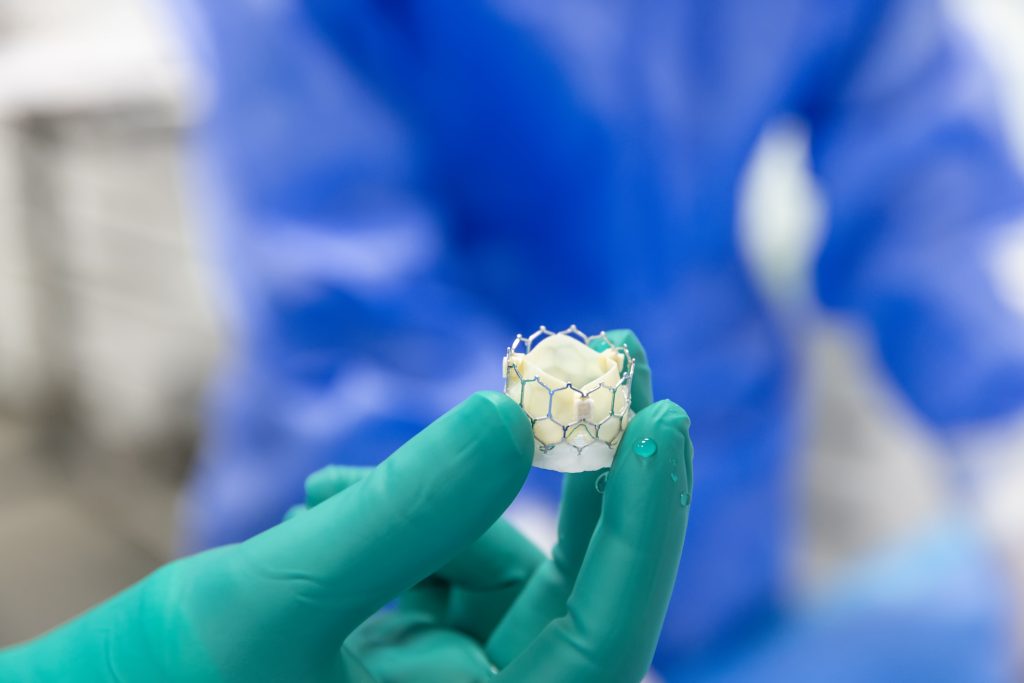
Transcatheter
Transcatheter tricuspid valve replacement is an alternative treatment that is less invasive and has a shorter recovery time than the open heart approach. Instead, the introduction site for catheters to deploy this device may be transfemoral, trans jugular, or transatrial. After approximately 10 years of trials and studies, this approach is becoming more common at extensive medical facilities.
A range of different types and companies provide these valve devices with up to 90% success. There are some downfalls to this approach, such as, depending on the manufacturer, higher rates of success with severe tricuspid regurgitation versus mild, as well as high mortality rates in hospitals. The rate of conversion to surgical intervention was as high as 5%. All devices available for a transcatheter approach are mechanical (17).
Types of Valves
At five years, there was no statistical difference in failure rate between the bioprosthetic and mechanical valves. There was also noted to be no difference in the need for reoperation between the two valves (5). After five years, some studies suggest mechanical valves are more likely to fail than bioprosthetic valves. In the past, mechanical valves were connected to electric disturbances and arrhythmia, such as atrial fibrillation.
With bioprosthetic valves, both porcine and bovine are prone to critical tears and stenosis due to calcification and leaflet thickening. This occurs more often with porcine than bovine. It is also more likely that these patients receiving a bovine or porcine valve will require pacemaker insertion (5).
Mechanical valves require long-term anticoagulation due to a higher risk of thromboembolic events. The need for blood thinners also leads to a higher risk of gastrointestinal and cerebral bleeding overall. It is recommended that the patient receiving mechanical valves be placed on optimal anticoagulation therapy with close monitoring to prevent complications (5).

Self-Quiz
Ask Yourself...
- How can simulation training enhance nurses’ preparedness for high-risk procedures, and what are the limitations of such training?
- How would you approach a patient differently if assessing a patient for potential open-heart surgery versus a non-invasive procedure?
- How are open heart surgery’s potential risks and benefits compared to alternative treatments, such as medication or catheter-based interventions?
- What role does patient education have in preparing someone for the emotional and physical aspects of open-heart surgery?
Risk and Complications
The primary risks associated with tricuspid valve replacement include surgical complications that are associated with any surgical or procedural intervention. Patients may experience complications related to anesthesia, the potential for valve malfunction, and the need for lifelong anticoagulation therapy, mainly if a mechanical valve is used.
There is also the risk of developing subsequent cardiac issues, such as right heart failure, even after successful surgery. In addition to the previously discussed risks and complications related to the specific surgical or procedural approach or type of valve placed, the postoperative period has unique challenges. These include the following potential risks and complications (all from 15):
- Bleeding or hemorrhage
- Infection
- Thrombosis
- Arrhythmias
- Myocardial infarction
- Peripheral or mesenteric ischemia
- Organ dysfunction
- Stroke
- Renal failure
- Requiring tricuspid valve re-intervention
- Access site/vascular complication
- Cardiac structural complications such as perforation, cardiac tamponade,
- Need for pacemaker or cardiac implantable electronic device (defibrillator) related to new arrhythmias or conduction disorders
- Death from cardiovascular cause or any cause

Self-Quiz
Ask Yourself...
- How do you use critical thinking and intuition to anticipate potential patient risks and complications?
- What healthcare risks do you find personally unacceptable to take?
- How might cultural beliefs affect a patient’s understanding and acceptance of open heart surgery?
- What ethical considerations arise when discussing the significant and potentially debilitating or fatal risks with patients and their families, especially regarding informed consent?
- What are the most significant risks associated with the treatment options for tricuspid valve replacement? Why do you think these risks stand out?
Post Op Monitoring
The post-cardiac surgical patient will be cared for in an intensive care unit for at least a few days before transferring to a step-down unit.
In the immediate postoperative phase, paying close attention to hemodynamics and optimizing myocardial oxygen supply and demand is essential. The cardiac index (CI) provides optimal systemic perfusion at greater than 2.2 L/min/m2. The patient will return with a Swan-Ganz catheter, which can be used to obtain cardiac pressure, draw blood to test for mixed venous oxygen saturation and assess the adequacy of tissue perfusion. A fiber-optic oximetric pulmonary artery catheter placement may continuously monitor this measurement.
Low cardiac output is an early indication of acute right heart failure. For these patients, this requires prompt detection and intervention. This is determined by right ventricular dilatation and dysfunction and can be measured via pulmonary artery pressures, which decrease from the baseline of systemic arterial pressures. Even subtle changes should be communicated with the surgical team and cardiologist immediately to prevent decompensation and hemodynamic instability.
Cardiogenic shock can occur quickly and is associated with inferior post-surgical outcomes. Medications used to treat include inotropic support and vasopressors. Common medications administered include dobutamine, levosimendan, epinephrine, or milrinone should be rapidly installed, possibly combined with vasopressor. Supportive care with afterload reduction may be accomplished with inhaled or systemic pulmonary vasodilators (3, 8, 15, 16, 17).
Hypothermia is defined as a temperature below 36°C. Patients are often cooled during cardiac surgery to slow cellular metabolism and will require slow rewarming to prevent complications. This can affect blood glucose levels, coagulation factors, electrolyte imbalances, and neurological responsiveness (11).
Renal failure is a concern after cardiopulmonary bypass and with an elevated risk of low cardiac output. Strict input and output documentation is essential to identify a change in urine output. At least 0.5-1.5 mL/kg/hour is usual; however, this may be lower after surgical intervention. The nurse should promptly report output under 0.5 ml/kg in an hour (15, 17).
The cardiac patient will likely return from surgery with femoral venous and arterial sheaths in place. These must be removed as soon as possible to prevent infection. This can be safely done by a trained nurse or cardiovascular technicians once coagulation factors have reached optimal levels to control hemorrhage.
Refer to unit protocol and orders for guidance, as this may differ between the healthcare provider’s preference and facility policy. The activated clotting time is typically used to guide this process, with a level of 150 or below being standard for removing an arterial sheath (15, 17, 18).
Pain is initially kept under control with opioid and non-opioid medications as well as non-pharmaceutical methods.
Staff and visitors must enforce strict hand hygiene to prevent infection of the approach site, whether it is open sternal, via thoracotomy, or a peripheral transcatheter vascular insertion.

Self-Quiz
Ask Yourself...
- What would be the advantages and disadvantages of caring for a patient who has already undergone significant cardiac surgery versus one who has never had a procedure?
- Your patient has a history of opioid dependence; how would this affect your approach to a pain relief regimen?
- How can a nurse manager implement strategies to reduce the likelihood of patient complications in the ICU?

Nursing Considerations
Pre-surgical
Whether the choice for valve replacement is through open heart surgery, thoracotomy, or transcatheter, each carries several risks and requires the same preoperative workup. The patient should be prepared for the latter two options to potentially transition to open heart surgery if there are complications (17, 18).
A full history and physical must be taken to assess the patient’s cardiovascular and pulmonary systems and note any comorbidities, including renal issues, coagulopathies, and previous surgeries.
Diagnostic testing is likely to occur several weeks before planned surgeries. An echocardiogram and right heart catheterization to assess valve structure and function are standard procedures (17, 18, 19).
Laboratory testing will include a complete blood count, metabolic panel, and coagulation factor tests.
Post-surgical
After the surgery or procedure, several nursing interventions will improve patient outcomes. Aiming nursing interventions to promote sleep, reduce stress, and increase activity can exponentially enhance outcomes.
Vital signs must be frequently monitored and promptly documented, with critical results outside parameters communicated to the advanced care team. Signs of hemodynamic instability, fluid overload, or altered perfusion must be assessed closely. The nurse must also frequently assess the patient’s level of consciousness and neurological status, especially in the immediate postoperative period, to recognize any signs of stroke or altered perfusion (17, 19).
Patient and caretaker teaching will be fundamental and should continue throughout the patient’s entire healthcare stay to improve the patient’s quality of life and health progression.
Patient/Family Education
Post-cardiac procedure education is essential for patients and their families to facilitate recovery and improve outcomes. After a cardiac procedure, patients may experience a range of physical and emotional changes. It is essential to understand the importance of adhering to post-procedure instructions provided by the multidisciplinary healthcare team (17, 18, 19).
Patients and their caretakers must understand the signs of potential complications such as chest pain, shortness of breath, bleeding from incisional or access sites, or signs of infection. The nurse must ensure that these symptoms are reported to their provider immediately and to seek assistance for any medical emergency.
Education must also be aimed at understanding the importance of taking ordered medications as prescribed. These medications, such as anticoagulation and treatment to prevent heart failure, are critical for preventing complications and promoting heart health (15, 17, 19).
Lifestyle modifications play a fundamental role in recovery. Patients should be encouraged to adopt a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats, with salt and sugar intake restrictions. Regular physical activity, tailored to the individual’s capacity and guided by a healthcare provider, is also essential. Patients should aim to gradually increase their activity levels, focusing on aerobic exercises that can enhance cardiovascular endurance (19).
Follow-up appointments with healthcare providers are necessary for ongoing evaluation and adjustments to the treatment plan. Empowering patients and families with knowledge and resources enhances their engagement in recovery and helps cultivate a supportive environment conducive to healing. In summary, comprehensive education and support for patients and families are instrumental in achieving successful recovery results in post-cardiac procedures (18, 19).

Self-Quiz
Ask Yourself...
- How would the patient’s social circle and support system influence outcomes and well-being after a major surgery?
- What recent innovations have significantly contributed to recovery time for patients undergoing major surgery?
Upcoming/Current Research Findings
As rheumatic fever is one of the highest causes of valvular heart disease, there is ongoing research into preventative treatment, such as vaccine development and methods to halt disease progression. A secondary cause is disease caused by calcification of the leaflets, for which there are no current therapies to prevent this. Other research is focused on identifying the optimal time to intervene as this is currently subjective and driven by effects on patient lifestyle due to symptom progression. It is often thought that this is too late in the process to improve the high morbidity and mortality rates associated with tricuspid valve dysfunction. A more proactive approach may be to base intervention timing on myocardial structure, function, and left ventricular involvement rather than waiting until the patient becomes symptomatic (15).

Self-Quiz
Ask Yourself...
- How do you define a complication in healthcare, and how might that definition vary depending on the situation or perspective?
- Do these definitions change for you when considering the risks of not proceeding with treatment in cases of high mortality risk?
Conclusion
Effective patient care for tricuspid valve replacement involves a multidisciplinary approach, encompassing thorough preoperative assessment, patient education, and focused postoperative monitoring. Discussions about the potential risks and benefits must be personalized, considering the patient’s overall health status, underlying conditions, and symptom effects on the patient’s well-being and ability to participate in daily activities. Long-term follow-up care and medical management are required to manage complications and monitor the prosthetic valve’s function.
Ultimately, the decision to proceed with tricuspid valve replacement should be based on carefully evaluating patient-specific factors, aligning clinical goals with the patient’s needs and preferences, and ensuring a comprehensive plan for perioperative and postoperative care.
References + Disclaimer
- Mahboobi, S., Sharma, S., & Ahmed, A. (2025). Tricuspid valve repair. In StatPearls. Retrieved on February 24, 2025 from https://www.ncbi.nlm.nih.gov/books/NBK559179/
- Norris, T. L. (2019). Porth’s Pathophysiology: Concepts of Altered Health States (10th edition). Wolters Kluwer.
- Ferri, F. (2022). Ferri’s Clinical Advisor. Elsevier.
- Minocha, P., Horenstein, M., & Phoon, C. (2024). Tricuspid atresia. In StatPearls. Retrieved on February 24, 2025 from https://www.ncbi.nlm.nih.gov/books/NBK554495/
- Qadeer, M. A., et al. (2024). Tricuspid valve replacement with mechanical versus biological prostheses: a systematic review and meta-analysis. Journal of Cardiothoracic Surgery, 19(636), 1-13. Retrieved on February 24, 2025 from https://doi.org/10.1186/s13019-024-03014-0
- American Heart Association. (2025). Problem: Tricuspid valve stenosis. In Heart Valve Problems and Causes. Retrieved on February 24, 2025 from https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/problem-tricuspid-valve-stenosis
- Stemmler, S. (2024). Evolution of heart-valve repair. In History. Retrieved on 02/24/2025 from https://www.barnesjewish.org/Curiosus-Mag/Article/ArtMID/6756/ArticleID/3322/EVOLUTION-OF-HEART-VALVE-REPAIR#:~:text=The%20first%20mechanical%20mitral%20valve,cow%20(called%20a%20xenograft).
- Wang, Y., Liu, Y., Meng, X., Zhai, M., Jin, P., Lu, F., & Yang, J. (2024). Comparing outcomes of transcatheter tricuspid valve replacement and medical therapy for symptomatic severe tricuspid regurgitation: a retrospective study. European Journal of Medical Research, 29(407), 1-13. Retrieved on February 24, 2025 from https://doi.org/10.1186/s40001-024-01947-9
- Ismail, A., Semien, G., Sharma, S., Collier, S., & Miskolczi, S. (2024). Cardiopulmonary bypass. In StatPearls. Retrieved on February 24, 2025 from https://www.ncbi.nlm.nih.gov/books/NBK482190/
- Furuta, A., Shinkawa, T., Okugi, S., Yoshida, H., & Niinami, H. (2023). Tricuspid valve replacement provides better long-term survival and tricuspid function than repair in patients with systemic right ventricles. JTCVS, 15, 382-393. https://doi.org/10.1016/j.xjon.2023.06.013
- Goco, R., Hudziak, D., Bis, J., Mendrala, K., Morkisz, L., Podsiadlo, P., Kosinski, S., Piatek, J., & Darocha, T. (2021). The role of deep hypothermia in cardiac surgery. International Journal of Environmental Research and Public Health, 18(13), 1-14. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8297075/pdf/ijerph-18-07061.pdf
- American Heart Association. (2024). Problem: Tricuspid valve regurgitation. In Heart Valve Problems and Causes. Retrieved on February 28, 2025 from Problem: Tricuspid Valve Regurgitation | American Heart Association
- Mulla, S., Asuka, E., Bora, V., Sharma, S., & Siddiqui, W. (2024). Tricuspid regurgitation. In StatPearls. Retrieved on February 28, 2025 from https://www.ncbi.nlm.nih.gov/books/NBK526121/
- Adamo, M et al. (2024). Epidemiology, pathophysiology, diagnosis and management of chronic right-sided heart failure and tricuspid regurgitation: a clinical consensus statement of the heart failure association (HRA) and the European Association of Percutaneous Cardiovascular Interventions (EAPCI) of the ESC. European Journal of Heart Failure, 26, 18-33. https://doi.org/10.1002/ejhf.3106
- Otto, C. et al. (2021). 2020 ACC/AHA Guideline for managing patients with valvular heart disease. Circulation, 143, e72-e227. https://doi.org/10.1161/CIR.0000000000000923
- Hahn, R., et al. (2025). Transcatheter valve replacement in severe tricuspid regurgitation. The New England Journal of Medicine, 392(2). https://doi.org/10.1056/NEJMoa2401918
- Hausleiter, J. et al. (2025). Transcatheter tricuspid valve replacement. Journal of the American College of Cardiology, 85(3), 265-291. https://doi.org/10.1016/j.jacc.2024.10.071
- Millar, L. M., Lloyd, G., & Bhattacharyya, S. (2022). Care of the patient after valve intervention. Heart, 108(19), 1516-1523. https://doi.org/10.1136/heartjnl-2021-319767
- Wang, S., Zhou, K., & Zhang, W. (2023). Application progress of nursing intervention in cardiac surgery. World Journal of Clinical Cases, 11(33), 7943-7950. https://doi.org/10.12998/wjcc.v11.i33.7943
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
