Course
Tuberculosis: What You Need to Know
Course Highlights
- Upon completion of this course, learners will be able to:
- Name the responsible bacteria that causes tuberculosis infection as well as risk factors and areas highly impacted
- Understand how tuberculosis infection is transmitted and how to prevent the spread of infection
About
Contact Hours Awarded: 4
Course By:
Alesha Campbell
ACNPC-AG
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
In this course, learners can expect to learn the foundations of tuberculosis, including its epidemiology, pathophysiology, and transmission. They will also learn the clinical signs and symptoms of tuberculosis and the treatment regimen in depth. Additionally, they will learn about areas that require further research.
Introduction
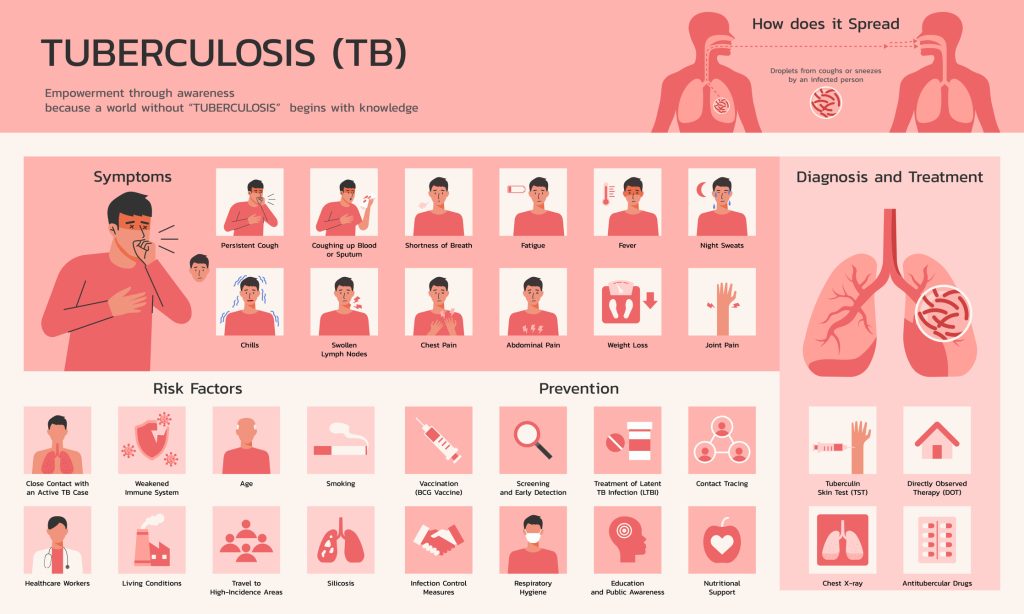
Tuberculosis is an infection caused by the bacteria Mycobacterium tuberculosis. Tuberculosis infection has a high incidence worldwide, especially in poorer countries. Tuberculosis infection has the highest cause of mortality of all infectious agents. The World Health Organization (WHO) aims to reduce the number of deaths sustained by tuberculosis infections worldwide. To achieve this goal, awareness is essential. Healthcare professionals should be aware of the signs and symptoms of the disease, test for the disease, determine the types of tuberculosis infections, and ensure successful treatment of the disease.
There is no current vaccine that is effective against tuberculosis infection. Treatment of tuberculosis is complex and involves the use of multiple drugs for a prolonged period. This article will discuss the definition of tuberculosis infection, assessment findings, epidemiology, transmission, pathophysiology, clinical signs and symptoms, diagnosis, etiology, treatment, self-management, and research findings related to tuberculosis infection.
Definition
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis (M. tuberculosis) and can be divided into two groups: latent tuberculosis and active tuberculosis. In latent tuberculosis, the immune system is exposed to bacteria, but no active infection is present (15). Active tuberculosis refers to an active infection with tuberculosis. Tuberculosis usually affects the lungs and can be referred to as pulmonary tuberculosis. Additionally, it can affect virtually all other organs, including the brain, lymph nodes, kidneys, and spine, called extrapulmonary tuberculosis (16).
Tuberculosis is a global problem and the leading cause of death from an infectious agent. Treatment is complicated and presents many challenges. In addition, the emergence of drug-resistant tuberculosis infections has been problematic. Tuberculosis is a highly contagious infectious agent when in the form of active pulmonary tuberculosis. Prevention of tuberculosis transmission is a globally recognized problem.

Self-Quiz
Ask Yourself...
- What bacteria causes tuberculosis infection?
- What is tuberculosis, which infects the lungs?
- What term is used to classify tuberculosis outside of the lungs?
Assessment
Screening
The first step in assessing clients with suspected tuberculosis infection is screening. Screening should be done for those considered at high risk for contracting disease. The U.S. Preventative Task Force recommends screening high-risk individuals for latent tuberculosis (9). Screening for tuberculosis starts with a questionnaire for at-risk individuals inquiring about the classic symptoms of an active tuberculosis infection.
Screening usually involves administering the tuberculin skin test of a blood draw to rule out exposure to tuberculosis. If one of these tests is positive, further diagnostics are necessary, usually a chest x-ray, which can rule out active tuberculosis infection. High-risk clients are listed below.
- Chronic diseases: Some high-risk chronic diseases that should be screened for tuberculosis include HIV infection, dialysis clients, clients taking immunosuppressive medications, especially TNF factor antagonists for rheumatoid arthritis or Crohn’s, those with cancer, a pre-existing lung condition, especially silicosis, diabetes, or elderly clients.
- Contact with a tuberculosis-positive person: People who have come in contact with someone with an active tuberculosis infection must be screened.
- Foreign-born individuals: Those who have migrated to the United States from a high-risk country should be screened. These geographic areas include the following (9):
- Latin America
- The Caribbean
- Africa
- Asia
- Eastern Europe
- Russia
Additional risk factors: Additional risk factors for contracting tuberculosis include those who are homeless, IV drug abusers, skilled nursing facility dwellings, prisoners, and some health care workers (9).

Self-Quiz
Ask Yourself...
- What chronic diseases carry a higher risk of contracting tuberculosis?
- What areas of the world are foreign-born individuals more at risk of getting tuberculosis?
- What living situations suggest that screening might be appropriate for an individual?
History
Constitutional symptoms: The client may report constitutional symptoms such as fever, chills, night sweats, or fatigue
Gastrointestinal symptoms: Gastrointestinal symptoms may include decreased appetite and unintended weight loss
Respiratory symptoms: The client often has a persistent cough that lasts more than two to three weeks. Hemoptysis, or coughing up blood, is also common. The client may also report pleuritic chest pain.

Self-Quiz
Ask Yourself...
- What constitutional symptoms should history focus on?
- What gastrointestinal signs should medical personnel look for in a suspected tuberculosis client?
- How long is a typical cough associated with pulmonary tuberculosis?
Physical Exam
Initially, vital signs should be assessed, including temperature, heart rate, blood pressure, respiratory rate, and pulse oximetry. A full head-to-toe exam should be performed. Pulmonary tuberculosis is the most common form, so a respiratory exam should be the focus for most clients. Exams of other body systems can be evaluated for other sites of tuberculosis infection, such as other organ involvement. The respiratory exam should include lung sounds, breathing effort, and how much oxygen the client requires.

Self-Quiz
Ask Yourself...
- What vital signs should be assessed in a client with tuberculosis?
- What body system should be the focus of the physical exam?
Epidemiology
Tuberculosis has the highest incidence of death of any infectious agent (9). Approximately one-fourth of the world population is infected with tuberculosis, approximately 2 billion people (4). In the United States, approximately 13 million people are infected with the disease (4). Most of those infected have a latent tuberculosis infection. Untreated latent tuberculosis has a 5-10% chance of progressing to active tuberculosis (4). Tuberculosis was responsible for one million deaths in 2022 (23). It is estimated that 1.3 million people die each year from tuberculosis (7). There are 1.7 billion people globally that are currently infected with M. tuberculosis. However, not all of them will develop an active tuberculosis infection (7).
Poverty is a considerable risk factor for tuberculosis, and the highest number of cases of tuberculosis are reported in the following countries: India, Indonesia, South Africa, Nigeria, the Philippines, Pakistan, Bangladesh, and China (12). Additionally, in all countries, people with low incomes are at a higher risk of contracting tuberculosis. In the United States, tuberculosis is 15 times higher in those that are foreign-born (9). HIV is a significant risk factor for developing active tuberculosis infection. In those with HIV, the risk of reactivation of tuberculosis is 18 times higher than in the general public (1).
There is both encouraging and discouraging news regarding the evolution of tuberculosis management. Unfortunately, there has been an increase in drug-resistant tuberculosis, which makes treating these individuals challenging. The rate of tuberculosis diagnosis, however, is decreasing by approximately 2 % per year (9). The WHO’s End TB Strategy aims to decrease tuberculosis infection incidence by 4-5% (5). The global treatment success rate is 83%, and the mortality rate since 1990 has decreased by 47% (9).

Self-Quiz
Ask Yourself...
- What percentage of latent tuberculosis will progress to an active tuberculosis infection?
- What are the four countries that have the highest number of tuberculosis cases?
- What is the percentage of treatment success rate of tuberculosis globally?
Transmission
The three ways tuberculosis present are pulmonary tuberculosis, extrapulmonary tuberculosis, and miliary tuberculosis. Pulmonary tuberculosis is the most common presentation of tuberculosis and describes tuberculosis infection of the lungs. Extrapulmonary tuberculosis describes tuberculosis that is outside of the lungs. This most commonly occurs in the lymph nodes, pleural space, bones, joints, and central nervous system. Miliary tuberculosis is the term used to describe tuberculosis infection that has spread to the bloodstream. Extrapulmonary tuberculosis cannot be transmitted to another individual without pulmonary tuberculosis unless an open abscess is present (9). The client diagnosed with extrapulmonary tuberculosis should always be checked for pulmonary tuberculosis.
Pulmonary tuberculosis is highly contagious. It becomes aerosolized in one- to five-mm-diameter particles (9). Another susceptible individual then inhales these particles. Clients with active pulmonary tuberculosis need to be placed in airborne precautions. This includes identifying the patient in a negative air pressure room and staff and visitors wearing a particulate respirator such as an N-95 mask. If clients need to leave the room, they should wear surgical masks (9).
The CDC outlines three criteria for being considered non-infectious. First, the client should have three consecutive negative sputum smears in eight-hour to twenty-four-hour intervals, with one sputum collected early in the morning (9). Second, the client’s symptoms should improve, and lastly, the client must be compliant with treatment for a minimum of two weeks (9).

Self-Quiz
Ask Yourself...
- What type of tuberculosis is contagious?
- What mode of transmission is tuberculosis spread by?
- What precautions should be taken to prevent tuberculosis from spreading among healthcare personnel caring for clients with the disease?
- What criteria must be met for a client to be considered no longer contagious?
Pathophysiology
Pathophysiology of Transmission of Tuberculosis to an Active Infection
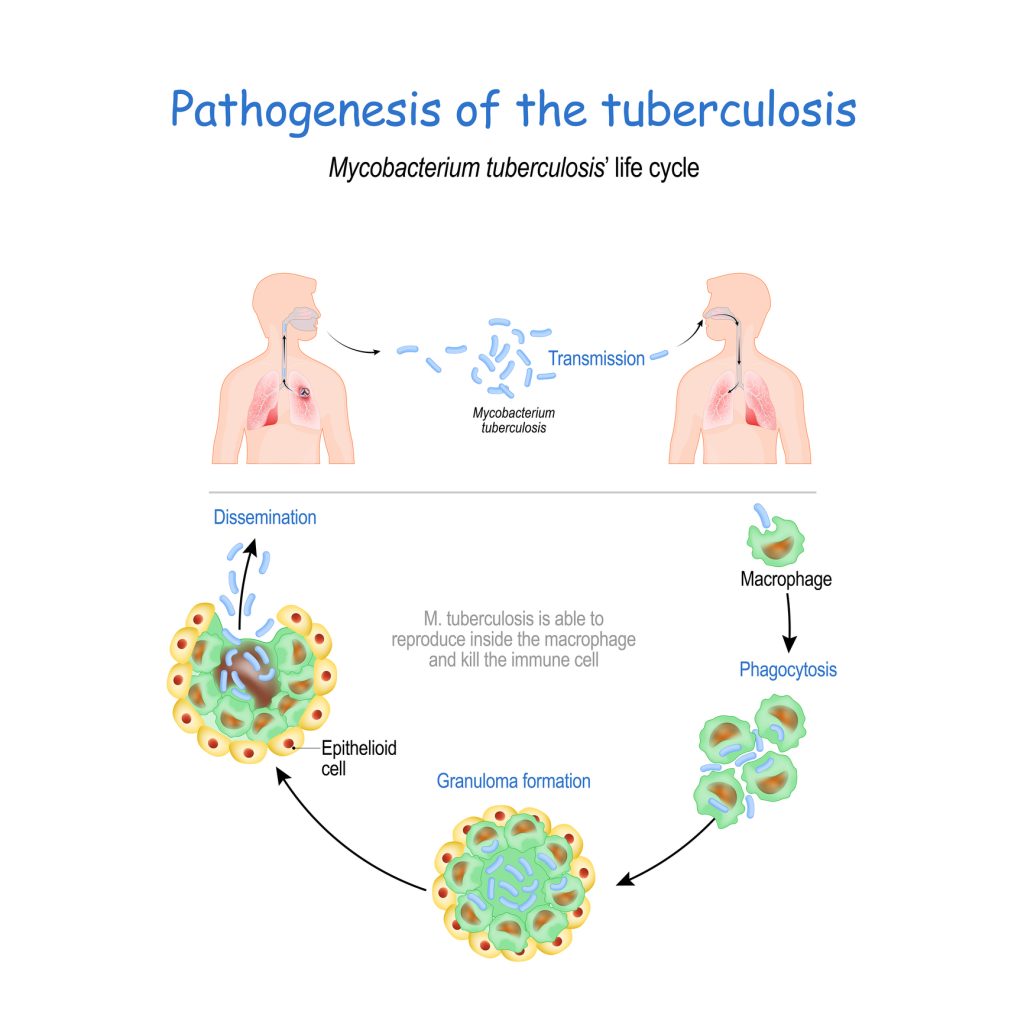
There are six steps involved in transmitting Mycobacterium tuberculosis to an active infection. The first step is aerosolization. A source with active pulmonary tuberculosis infection gives off infectious particles. Most commonly, in pulmonary tuberculosis, the actively infected person coughs or sneezes and spreads aerosolized M. tuberculosis particles in the air. The M. tuberculosis survives airborne and is then inhaled by a susceptible host (12).
The second step is macrophage phagocytosis. In the alveolar sacs, the M. tuberculosis bacilli come into contact with macrophages in the alveoli in the lungs. The bacilli bind to the macrophages via mannose receptors, scavenger receptors, complement receptors, Fc receptors, and surfactant protein receptors (12). The bacilli then phagocytosed into the macrophages. Once this occurs, the bacilli activate toll-like receptors (TLR) and release mycelial-arabinogalactan-peptidoglycan (MAGP), deoxyribonucleic acid (DNA), and ribonucleic acid (RNA) into the cytosol of the cell (8). Many processes then occur, and the host’s immune system is activated. The immune system utilizes blood vessels as a way for the immune cells to attack the bacilli while also allowing the bacteria to reach systemic circulation and spread to other parts of the body (12). This initiates bacteremia and the inflammatory response in the body.
The third step in the process is phagolysosome blockage and replication. M. tuberculosis replicates in the macrophages after it stops the fusion of the phagosome and the lysosome. The macrophage and M. tuberculosis travel from the alveolar space to the lung parenchyma (12). Once M. tuberculosis reaches the lung parenchyma, the immune system forms a granuloma around it, also known as tuberculoma (12). This causes inflammation in the lungs.
Next, the T-helper response occurs. After three weeks of infection with M. tuberculosis, the infection has proliferated and possibly spread to other organs. The T-helper cells are activated, and a cluster of differentiation 4 (CD4+) response occurs (12). Cell-mediated immunity has three primary effects. A type IV hypersensitivity reaction occurs, which is what causes the positive Mendel-Mantoux test (12). Interferon-gamma is released, which aids in activating macrophages (12). Lastly, granuloma development occurs, leading to many macrophages responding to the initial lesion (12).
The fifth step of the process is granuloma formation. A granuloma is a shell of immune cells surrounding bacteria. Activated macrophages that cannot eliminate the bacteria release tumor necrosis factor (TNF) alpha. The TNF alpha differentiates monocytes into epithelioid histiocyte cells, which form encased granulomas containing M. tuberculosis (12). Some of the cells fuse to form giant cells. The granulomas are formed from macrophages and lymphocytes containing M. tuberculosis (12).
The last step in the process is clinical manifestations and active tuberculosis. These can be classified as primary and secondary tuberculosis. Primary tuberculosis occurs when the immune system cannot contain the initial infection (12). This often happens with immuno-compromised individuals. Latent tuberculosis occurs when the immune system and granulomas contain M. tuberculosis but cannot eliminate it. This can progress to a secondary tuberculosis infection at a later time. When the body becomes immunocompromised later, the M. tuberculosis inside the granuloma can reactivate (12). This can result in pulmonary, extrapulmonary, or military tuberculosis (12).

Self-Quiz
Ask Yourself...
- What is the first step in the transmission of Mycobacterium tuberculosis?
- What are formed in the lungs around the bacteria inside the alveoli?
- What immune cells are found in granulomas?
Pathophysiology of Active Tuberculosis Infection Manifestations
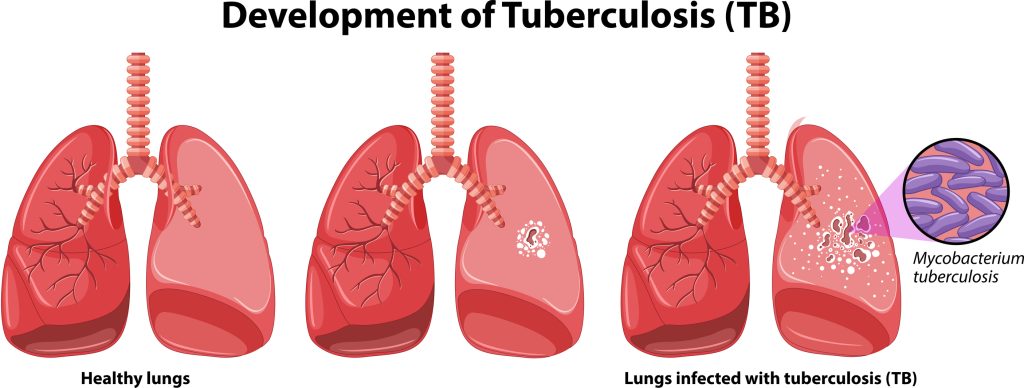
Acute respiratory failure is a common complication of pulmonary tuberculosis. The tuberculosis bacteria damage the alveoli in the lungs and causes inflammation. Inflammation increases extravascular lung water, creating a V/Q mismatch (23). Additionally, interstitial granulomatous infections, obliterative endarteritis, and destruction of air spaces by the granulomas and cavitating lesions also contribute to acute respiratory failure (23). This damage to the lung tissue can lead to acute respiratory distress syndrome (ARDS).

Self-Quiz
Ask Yourself...
- What area of the lung is typically affected by pulmonary tuberculosis?
- How does pulmonary tuberculosis lead to respiratory failure?
Clinical Signs and Symptoms
Tuberculosis infection can be either a latent tuberculosis infection or an active tuberculosis infection. Active tuberculosis infection can be further categorized as pulmonary tuberculosis, extrapulmonary tuberculosis, or miliary tuberculosis. Symptoms of tuberculosis depend on what type of tuberculosis occurs in the individual.
Latent Tuberculosis
In latent tuberculosis, the client is infected but does not have an active disease. These clients are asymptomatic. Two standard tests are used to screen for tuberculosis: the tuberculin skin test and the interferon-y release assay (7). Both of these tests will detect latent and active tuberculosis infection; however, they cannot differentiate between them. The tuberculin skin test uses Mantoux, which is injected intradermally and reads later. The interferon-y release assay is a blood test that measures immune reactivity to M. tuberculosis (9).

Self-Quiz
Ask Yourself...
- What two screening tests are used to detect tuberculosis infection?
- Which screening test is a blood test?
Pulmonary Tuberculosis
Many symptoms of an active pulmonary tuberculosis infection are constitutional symptoms. These symptoms may include fever, chills, night sweats, unintended weight loss, anorexia, and fatigue. A persistent cough is common and often present for over two to three weeks. This cough typically starts as non-productive and progresses to a productive cough with sputum (9). Hemoptysis is also common. Clients may complain of chest pain, which is usually pleuritic and increases with inspiration (9).
Complications are common in pulmonary tuberculosis, especially acute respiratory failure, including ARDS. In clients requiring mechanical ventilation, pneumothorax and ventilator-associated pneumonia are additional complications seen in pulmonary tuberculosis (23). Significant hemoptysis and bleeding in the lungs may also occur.
Pulmonary tuberculosis can be detected on radiology films, including a chest X-ray or CT scan. These findings may vary but typically include opacities. They may or may not show cavitation (23). Sputum cultures should also be obtained on all clients with suspected pulmonary tuberculosis. Ideally, sputum cultures should be obtained early in the morning.

Self-Quiz
Ask Yourself...
- What are some common symptoms associated with pulmonary tuberculosis?
- What are some complications associated with pulmonary tuberculosis?
- How is pulmonary tuberculosis diagnosed?
Extrapulmonary Tuberculosis
Extrapulmonary tuberculosis symptoms can happen concurrently with pulmonary tuberculosis or without pulmonary tuberculosis. One area that may be affected by M. tuberculosis is the central nervous system (CNS). CNS involvement is rare but is typically the most severe. This often results in altered mental status. CNS involvement can result in tuberculosis meningitis or cerebral tuberculomas (23).
Symptoms of tuberculosis meningitis include headache, fever, vomiting, malaise, fatigue, and anorexia (23). Those with cerebral tuberculoma, if the lesion is large enough, may present with cranial nerve palsies or seizures. Radiology imaging assists in the diagnosis of CNS-associated tuberculosis infections. In addition, the client may have cerebral spinal fluid sent for analysis.
Hyponatremia is secondary to cerebral salt waste or syndrome of inappropriate antidiuretic hormone (SIADH) is common in CNS-associated tuberculosis infections. Hydrocephalus can occur as a complication of a CNS tuberculosis infection, which can lead to increased intracranial pressure and even comatose states (23). Increased intracranial pressure may also occur from cerebral edema, tuberculomas, or hyponatremia. Intraventricular monitoring or drainage may be necessary in these cases.
Gastrointestinal tuberculosis and tuberculosis-associated peritonitis can affect about one-third of clients presenting with pulmonary tuberculosis (23). Symptoms of gastrointestinal tuberculosis may include abdominal pain, ascites, or weight loss. A complication of gastrointestinal tuberculosis can consist of an acute abdomen from strictures or bowel obstruction (23). Radiology imaging may be utilized to diagnose gastrointestinal tuberculosis, and occasionally, testing of ascites fluid that was drained, or a biopsy may be performed (23).
Tuberculosis infection involved in the pericardium may cause pericarditis or pericardial effusions. Symptoms associated with pericarditis include chest pain that may be relieved by leaning forward or shortness of breath. Pericardial effusion symptoms include chest pain or pressure, shortness of breath, fatigue, and anxiety. Pericardial effusions may progress to cardiac tamponade.
Symptoms of cardiac tamponade include hypotension, distended neck veins, and muffled heart sounds. Cardiogenic shock may also occur in the setting of tuberculosis pericarditis or cardiac tamponade. EKG and echocardiogram are utilized to diagnose pericarditis or pericardial effusion associated with tuberculosis infection.
Adrenal insufficiency can be a complication of infection with M. tuberculosis, either through direct involvement in the adrenal glands or through disseminated seeding from miliary tuberculosis (23). Symptoms of adrenal insufficiency include hypotension that may require vasopressors, hyponatremia, hypokalemia, anemia, and skin pigmentation (23). Diagnosis is typically based on clinical judgment, especially in shock requiring vasopressors.
Lymph node involvement and lymphadenopathy may be found on radiology films. Additionally, tuberculosis infection can be in the airways outside the lung tissue and may cause airway obstruction if found in the larynx or retropharyngeal spaces (23). This is not an exhaustive list of extrapulmonary tuberculosis findings but are findings the health care specialist may come across.

Self-Quiz
Ask Yourself...
- What are some sites of the body extrapulmonary tuberculosis can present in?
- What are the symptoms of gastrointestinal tuberculosis?
- How are tuberculosis pericarditis and pericardial effusion diagnosed?
- What are symptoms suggestive of adrenal insufficiency from tuberculosis infection?
Miliary Tuberculosis
Miliary tuberculosis is an infection with M. tuberculosis that has spread to the bloodstream. Those with miliary tuberculosis can have any of the above symptoms of pulmonary or extrapulmonary tuberculosis in addition to sepsis. Symptoms of sepsis include fever, chills, hypothermia, hypotension, tachycardia, tachypnea, fatigue, and altered mental status. Laboratory findings include an elevated white blood cell count (WBC) or low WBC, elevated lactic acid, and there may be evidence of organ dysfunction such as elevated liver enzymes or creatinine. Diagnosis of miliary tuberculosis usually includes radiology imaging such as x-rays, CT scans, MRIs, or ultrasounds. Additionally, blood cultures should be drawn. A mycobacterial culture will isolate M. tuberculosis.
A serious complication that can occur with miliary tuberculosis is disseminated intravascular coagulation (DIC). As miliary tuberculosis infection has spread to the bloodstream, it can be carried to any other body site and cause extrapulmonary tuberculosis. Miliary tuberculosis is the most frequent cause for CNS tuberculosis as M. tuberculosis travels through the bloodstream and can travel to the brain (23). The client can also go into septic shock, although this is rare among immunocompetent individuals (23). Multiorgan failure is another complication of sepsis from miliary tuberculosis infection.


Self-Quiz
Ask Yourself...
- What is the definition of miliary tuberculosis?
- What are the symptoms associated with miliary tuberculosis
- What are some complications that can occur secondary to miliary tuberculosis?
Diagnosis
As discussed above, two screening tests are utilized to screen for tuberculosis. These tests include the Mantoux skin test and the interferon-y release test. However, neither of these tests can differentiate a latent tuberculosis infection from an active one. The tuberculin skin test uses Mantoux injected intradermally. A palpable induration with erythema occurs if the client has been exposed to tuberculosis, indicating a positive test (9). This test is read 48-72 hours after the Mantoux is injected intradermally, which requires adequate follow-up from the individual.
A standard interferon-y release test is known as the interferon-gold and is now the most commonly performed screening test for tuberculosis. Active tuberculosis infection is based on symptoms, and a chest x-ray will show infiltrates or consolidations, which often have cavitations in the lungs.

An additional screening test that may be utilized for hospitalized patients, especially those with a coexisting HIV infection, is the lipoarabinomannan (LAM) urinary test (7). This test has the benefits of being cost-effective and convenient as it is a point-of-care test. It is currently recommended for hospitalized patients with coexisting HIV infection and CD4 counts less than 100 or critically ill hospitalized clients (7).
Etiology
The bacteria Mycobacterium tuberculosis causes tuberculosis infection. The latent form of tuberculosis is quite prevalent worldwide, specifically in areas of poverty. Countries with a heavy burden of tuberculosis infection include India, Indonesia, South Africa, Nigeria, the Philippines, Pakistan, Bangladesh, and China (12). As discussed above, tuberculosis is spread by a person with active pulmonary tuberculosis by the airborne route. When the infected person coughs, airborne droplets are created, and other individuals can inhale them. Once infected, the person typically gets a latent tuberculosis infection. However, primary active infections sometimes occur as well.
In immunocompetent individuals, tuberculosis infection stays dormant in the latent tuberculosis phase. However, in immunocompromised persons, this infection may become active. This is especially common with those who are also infected with the human immunodeficiency virus (HIV). Other diseases that can cause immune compromise include diabetes mellitus, silicosis, and renal failure.
Clients who take immunosuppressive drugs after organ transplantation or for autoimmune diseases are at increased risk for active tuberculosis infection as well. The risk of a latent tuberculosis infection transitioning to an active tuberculosis infection is highest within the first two years after the latent tuberculosis infection is contracted (5).

Self-Quiz
Ask Yourself...
- What is the infectious bacteria that causes tuberculosis infection?
- What countries have a high prevalence of tuberculosis infections?
- What conditions can cause an individual to be more likely to develop an active tuberculosis infection?
Treatment
This section is separated into the treatment of latent tuberculosis versus an active tuberculosis infection, which are treated differently. Additionally, details on the specific agents used to treat tuberculosis will be discussed. Latent tuberculosis is not always treated; however, treatment of latent tuberculosis effectively prevents progression to an active tuberculosis infection. This has important implications in decreasing the cases of active tuberculosis and preventing transmission of the disease to other individuals. Additionally, screening for drug-resistant tuberculosis is essential. A sputum sample is collected, and resistance against minimal rifampin should be done for every client (12).
Many of these drugs have multiple potential adverse effects. Clients need to understand the importance of compliance with treatment and will need to be educated on the possible adverse effects and what to report to their provider.
Latent Tuberculosis
There are three preferred treatment regimens for latent tuberculosis infection as follows:
- Isoniazid plus rifapentine: This regimen consists of three months of isoniazid (Niazid) and rifapentine (Priftin) (4). Due to increased compliance, this is preferred over isoniazid only once daily for nine months (4). It is done under directly observed therapy, which is given in the presence of healthcare personnel.
- Rifampin only: Rifampin (Rifadin) can be given alone daily for four months (4). There are many drug interactions with rifampin. Rifabutin (Mycobutin) has fewer side effects and may be used if isoniazid is contraindicated, and rifampin may not be used due to drug interactions (4).
- Isoniazid plus rifampin: This regimen consists of isoniazid (Niazid) daily and rifampin (Rifadin) for three months.

Self-Quiz
Ask Yourself...
- How often and for how long is isoniazid plus rifapentine indicated?
- What factor might limit the use of rifampin only?
- How often and for how long is the regimen of isoniazid plus rifampin indicated?
Active Tuberculosis
- Treatment of isoniazid-susceptible, rifampin-susceptible tuberculosis in adults: This treatment regimen consists of a four-drug combination of isoniazid (Niazid), rifapentine (Priftin), Pyrazinamide (Rifater), and moxifloxacin (Avelox) (19).
- Isoniazid 300 mg daily for 17 weeks
- Rifapentine 1,200 mg daily for 17 weeks
- Pyrazinamide weight-based dosing for 8 weeks: 40-55kg 1,000 mg, 55-75 kg 1,500 mg, greater than 75 kg 2,000 mg.
- Moxifloxacin 400 mg daily for 17 weeks
- Treatment of non-severe, presumed isoniazid-susceptible, rifampin-susceptible tuberculosis in children: This treatment regimen consists of a four-drug combination of isoniazid (Niazid), rifampin (Rifadin), pyrazinamide (Rifater), and ethambutol (Myambutol). It consists of an intensive phase utilizing all four drugs followed by a continuation phase utilizing only isoniazid and rifampin (19). All of the drugs are weight-based for children.
- Isoniazid 10-15 mg/kg for 16 weeks
- Rifampin 10-20 mg/kg for 16 weeks
- Pyrazinamide 35 mg/kg for 8 weeks
- Ethambutol 20 mg/kg for 8 weeks
- Treatment of rifampin-resistant, fluoroquinolone-resistant tuberculosis: Treatment of rifampin-resistant and fluoroquinolone resistant tuberculosis is managed with three drugs. This includes bedaquiline (Sirturo), pretomanid (Dovprela), and linezolid (Zyvox) (19).
- Bedaquiline 400 mg daily for 2 weeks, followed by 200 mg three times a week for 24 weeks
- Pretomanid 200 mg daily for 26 weeks
- Linezolid 600 mg daily for 26 weeks
- Treatment of rifampin-resistant fluoroquinolone tuberculosis: Treatment of rifampin-resistant fluoroquinolone-susceptible tuberculosis is managed the same as that of rifampin-resistant fluoroquinolone tuberculosis, with the addition of a fourth agent. This regimen includes bedaquiline (Sirturo), pretomanid (Dovprela), linezolid (Zyvox), and moxifloxacin (Avelox) (19).
- Bedaquiline 400 mg daily for 2 weeks, followed by 200 mg three times a week for 24 weeks
- Pretomanid 200 mg daily for 26 weeks
- Linezolid 600 mg daily for 26 weeks
- Moxifloxacin 400 mg daily for 26 weeks

Self-Quiz
Ask Yourself...
- What is the treatment regimen for adult rifampin-susceptible fluoroquinolone-susceptible tuberculosis infection?
- What is the treatment for non-severe presumed isoniazid-susceptible, rifampin-susceptible tuberculosis infection in children?
- What is the treatment regimen for rifampin-resistant fluoroquinolone-resistant tuberculosis infection?
- What is the treatment regimen for rifampin-resistant fluoroquinolone-susceptible tuberculosis infection?
Isoniazid
- Adverse effects: Increased liver enzymes are common in isoniazid treatment and occur in 10-20% of patients (6). Neuropathy is also common, and vitamin B6 can be given with this drug to prevent or treat neuropathy associated with isoniazid use (9). Other adverse effects include rash, agranulocytosis, anemia, thrombocytopenia, hepatitis, systemic lupus erythematosus (SLE), rhabdomyolysis, and seizures (6).
- Contraindications: Acute liver disease is a contraindication to isoniazid use.
- Monitoring: Hepatic enzymes, including aspartate aminotransferase (AST) and alanine aminotransferase (ALT), should be checked prior to initiating isoniazid therapy and monthly during therapy (6).

Self-Quiz
Ask Yourself...
- What percentage of clients develop increased liver enzymes during isoniazid treatment?
- What monitoring is required during treatment with isoniazid?
Rifapentine
- Adverse effects: Common adverse effects of rifapentine include elevated liver enzymes, rash, clostridium difficile infection (C. diff), anemia, arthralgias, headache, conjunctivitis, and hemoptysis. Serious adverse effects include Steven Johnson Syndrome (SJS), drug reaction with eosinophilia and systemic symptoms (DRESS), and neutropenia (21). Clients should also be instructed that their body fluids may have an orange color.
- Contraindications: Contraindications include hypersensitivity reaction to rifamycins.
- Monitoring: Hepatic enzymes should be checked prior to the initiation of therapy. Those with abnormal hepatic enzymes should also be monitored during treatment.

Self-Quiz
Ask Yourself...
- What should clients be informed of that may occur to their body fluids?
- What are the side effects of rifapentine?
Rifampin
- Adverse effects: Rifampin has numerous drug interactions and should be checked against the client’s current medication list. Other adverse effects include rash, pruritus, agranulocytosis, disseminated intravascular coagulation (DIC), hepatotoxicity, nephrotoxicity, renal failure, interstitial lung disease, and DRESS. Orange staining of body fluids occurs, and clients should be educated on this.
- Contraindications: Rifampin should not be used if the client has a previous hypersensitivity reaction. Additionally, there are multiple drug interactions, and rifampin cannot be used with certain drugs.
- Monitoring: Rifampin resistance can be problematic. Before starting treatment, the client should be tested for susceptibility of the tuberculosis infection to rifampin. Before initiating rifampin therapy, the client should have hepatic enzymes, including AST, ALT, and bilirubin levels, creatinine, and a complete blood count (CBC) drawn (21). If there are lab abnormalities, these should also be monitored throughout treatment. If the client is at risk for bleeding, coagulation studies may also need to be monitored.

Self-Quiz
Ask Yourself...
- What are the potential side effects of rifampin?
- What testing should be done before the initiation of therapy with rifampin?
- What are the contraindications of rifampin?
Pyrazinamide
- Adverse effects: Adverse effects of pyrazinamide include hyperuricemia or gout, elevated hepatic enzymes, arthralgias, and myalgias (18).
- Contraindications: Contraindications of pyrazinamide use include active gout and severe hepatic damage.
- Monitoring: Hepatic enzymes and uric acid levels should be checked prior to the initiation of pyrazinamide therapy. If signs of gout or liver impairment occur or if initial levels are abnormal, they may need to be monitored throughout therapy as well. Clients should be instructed to report new-onset joint pain to their provider.

Self-Quiz
Ask Yourself...
- What are the contraindications to therapy with pyrazinamide?
- What monitoring should be done with pyrazinamide treatment?
Moxifloxacin
- Adverse effects: Moxifloxacin has many potential adverse effects. Common adverse effects include hypokalemia, abdominal pain, constipation or diarrhea, nausea, vomiting, elevated hepatic enzymes, dizziness, headache, dry eyes, eye pain, and reduced visual acuity (13). More severe adverse reactions include aortic aneurysm or dissection, prolonged QT interval, Torsades de pointes, SJS or toxic epidermal necrolysis (TEN), hyperglycemia or hypoglycemia, myasthenia gravis, Guillain-Barre syndrome, tendonitis or tendon rupture, neuropathy, increased intracranial pressure, seizures, retinal detachment, paranoia, suicidality, renal failure, or serum sickness caused by the drug (13).
- Contraindications: Contraindications are hypersensitivity to moxifloxacin or other quinolone antibiotics.
- Monitoring: Clients should be monitored for adverse reactions. Diabetic clients should monitor their blood glucose levels. In those with liver cirrhosis, an EKG should be monitored as well (13).

Self-Quiz
Ask Yourself...
- What arrhythmias may occur with the use of moxifloxacin?
- What monitoring needs to occur with treatment with moxifloxacin?
Ethambutol
- Adverse effects: Adverse effects of ethambutol include hepatotoxicity, optic neuritis, and hypersensitivity or anaphylactic reaction.
- Contraindications: Ethambutol should generally be avoided in clients with optic neuritis.
- Monitoring: Before initiating therapy with ethambutol, baseline laboratory results should include CBC, liver function tests, renal function tests, and visual acuity (6).

Self-Quiz
Ask Yourself...
- What adverse effects may occur with ethambutol use?
- What are the contraindications of ethambutol usage?
Bedaquiline
- Adverse effects: Adverse effects of bedaquiline include chest pain, QT prolongation, abdominal pain, nausea, elevated hepatic enzymes, arthralgia, headaches, and hemoptysis (2).
- Contraindications: Bedaquiline causes QT prolongation in approximately 61% of clients. Other QT-prolonging agents should be avoided or utilized cautiously when administered in addition to bedaquiline.
- Monitoring: Before initiating bedaquiline therapy, a baseline EKG should be done to check for QT prolongation. In addition, an EKG should be done 2 weeks after initiation of treatment and as needed during therapy (2). Before initiating bedaquiline, clients should also get baseline liver function tests and electrolytes drawn, including calcium, magnesium, and potassium. Electrolytes and liver function should be monitored throughout treatment as well.

Self-Quiz
Ask Yourself...
- How frequently does QT prolongation occur in clients on bedaquiline therapy?
- What monitoring should be done before and during treatment with bedaquiline?
Pretomanid
Adverse effects: Pretomanid is another drug with multiple potential adverse effects. Common adverse effects include acne, rash, pruritus, abnormal weight loss, hypoglycemia, abdominal pain, decreased appetite, nausea, vomiting, diarrhea, indigestion, elevated amylase levels, elevated hepatic enzymes, musculoskeletal pain, headaches, visual impairment, cough, hemoptysis, lower respiratory tract infection, and pleuritic pain (17). More serious adverse effects include prolonged QT interval, lactic acidosis, anemia, myelosuppression, hepatotoxicity, peripheral nerve disease, and disorder of the optic nerve (17).
Contraindications: When used to treat tuberculosis infection, if a client is unable to take linezolid or bedaquiline, pretomanid should not be utilized, as it is only effective at treating tuberculosis when used in combination with these drugs.
Monitoring: Before initiating pretomanid therapy, the client should have laboratory tests drawn, including a CBC and hepatic function tests, including ALT, AST, alkaline phosphatase, and bilirubin levels. These labs should be repeated 2 weeks after initiation of therapy. Hepatic enzymes should be monitored monthly while on treatment and as needed if symptoms of hepatotoxicity occur. Symptoms of hepatoxicity should be monitored, and clients will need to be educated on the signs and symptoms and instructed to report these symptoms to their healthcare provider immediately. These symptoms include fatigue, anorexia, nausea, jaundice, dark urine, liver tenderness, and hepatomegaly (17). Clients will also need to be instructed to report any symptoms of visual impairment. If symptoms of visual impairment occur, a prompt ophthalmic examination should be performed (17).

Self-Quiz
Ask Yourself...
- What are the severe potential adverse reactions associated with pretomanid therapy?
- What symptoms of hepatotoxicity should clients be instructed to monitor for?
- What other symptoms should clients be instructed to report to their healthcare provider?
Linezolid
- Adverse effects: Common adverse effects of linezolid include diarrhea, nausea, vomiting, and headaches. More serious adverse effects include hyponatremia, lactic acidosis, syndrome of inappropriate antidiuretic hormone (SIADH), C. difficile infection, myelosuppression, peripheral neuropathy, seizures, disorder of the optic nerve, and serotonin syndrome (11).
- Contraindications: Contraindications to linezolid use include prior sensitivity reaction to the drug and concomitant use with a monoamine oxidase inhibitor (MAOI) or within two weeks of an MAOI.
- Monitoring: A CBC should be drawn weekly with those on linezolid therapy, especially for those at high risk for myelosuppression, severe renal impairment, hepatic impairment, or those receiving other medications that may cause bone marrow suppression and those with chronic infections. Sodium levels should also be monitored, especially in those taking diuretics or at risk for SIADH (11). Visual function testing should be done in those taking linezolid longer than three months or in those with acute visual changes.

Self-Quiz
Ask Yourself...
- What are the potential serious adverse effects of linezolid?
- What are the contraindications of linezolid therapy?
- What monitoring is necessary for clients taking Linezolid?
Special Treatment Considerations for the Critically Ill Patient
Several factors can lead to increased gut absorption of antibiotics in the critically ill patient. Due to this, critically ill clients may require IV administration of anti-tuberculosis medications. Nephrotoxicity is another concern for critically ill clients and may require renal dosing of the medicines. Pharmacists can assist with this dosing and therapeutic drug levels may need to be monitored as well.
If hepatotoxicity occurs in a critically ill client, it may require adjustments to the regimen, such as switching or discontinuing certain drugs (23). This may require prolonged treatment with streptomycin, levofloxacin and ethambutol (23). Rifampicin and isoniazid can be slowly reintroduced when liver function returns to normal.
Steroids may be utilized in critically ill clients in septic shock or multi-organ failure. However, the evidence is still unclear on the benefits of steroids (23). Antiplatelets are another potentially helpful adjunctive therapy; however, the evidence remains unclear. Aspirin may help prevent complications such as vasculitis or stroke (23).


Self-Quiz
Ask Yourself...
- When might a critically ill patient require IV anti-tuberculosis therapy?
- What conditions might warrant steroid use?
Self-Management
Treatment of tuberculosis is long-term, as long as up to 6 months, and therefore, clients must manage their disease. Additionally, the regimen includes multiple drugs the client needs to take. Clients must be educated on the necessity to complete the entire drug regimen to prevent drug-resistant tuberculosis. One strategy the WHO recommends is directly observed therapy, where the client takes the medication under the supervision of a medical professional to increase compliance (10). This method is taxing for medical professionals and clients who need transportation to and from a physician’s office to receive their medications. Clients need to be educated on the potential side effects of the drugs and how to manage the side effects to increase compliance.
Since directly observed therapy can be very taxing for the client, some clients may be left to manage their medications at home with self-monitoring logs. They may utilize tools like a smartphone application or digital pillboxes (7). More research is needed into ways that clients can safely and adequately manage their own medications.
Clients will also need to be compliant with follow-up sputum cultures. Many of the medications utilized to treat tuberculosis require laboratory monitoring prior to and during therapy, and clients will need to be compliant with laboratory draws throughout their treatment.
Along with medication management and laboratory needs, clients must also manage the disease. As discussed above, active tuberculosis infection has many symptoms that the client will have to live with and manage. Clients may adjust their lifestyles to cope with and manage their symptoms. To manage fatigue, clients should be educated on getting enough sleep and avoid overexertion. Proper nutrition is also essential to the healing process. Smoking and alcohol cessation are important as well.
The clients also must isolate themselves while they are contagious. This is another important educational point that healthcare workers must make to the clients to ensure they are not spreading the disease to others. The client must be educated that they should wear a respirator when they need to go out in public. They should be taught to cover their faces when coughing and sneezing correctly. Ventilating the room, they stay in is also essential. Isolation can lead to psychological problems such as anxiety and depression.

Self-Quiz
Ask Yourself...
- Why is it essential for clients to complete their entire medication regimen?
- What lifestyle modifications might be necessary for clients with active tuberculosis infection?
- What is a strategy WHO recommends for clients to increase compliance with tuberculosis medications?
- What self-management practices decrease the spread of tuberculosis infection to others?
Research Findings
There is currently a lot of research on tuberculosis, especially diagnosis, treatment strategies, and prevention. Research is also being done on tuberculosis biomarkers that may help identify a person’s risk for infection, disease, likelihood of cure, and protection (7). Multiple reports with correlation in this field have been reported, but no current clinically relevant tool exists. However, it may be available in the future.
One prominent area of research is the development of a tuberculosis vaccine. The invention of an effective tuberculosis vaccine could potentially irradicate tuberculosis infection. There is currently a vaccine, bacilli Calmette-Guerin (BCG), which may provide moderate protection for infants and children, specifically for severe forms of tuberculosis such as miliary tuberculosis (1).
However, there is no effective vaccine for tuberculosis prevention, and this vaccine does not benefit adults. A vaccine trial is currently in motion and in phase three of the trial (3). The trial occurs in five sub-Saharan African countries and two in East Asia, two areas of high tuberculosis prevalence (3). Phase two of this vaccine trial showed a 54% reduction in developing active pulmonary tuberculosis (3).
Diagnosing tuberculosis infection and resistance is also a challenge. Sputum cultures are the most accurate way to diagnose tuberculosis infection. Still, due to tuberculosis being a slow-growing bacterium, it can take up to two weeks for the culture to grow. Genotypic testing is one area of interest currently. One recently developed test is the Xpert MTB/RIF test, which detects genetic material from M. tuberculosis bacteria and rifampin resistance (7). This test, however, remains restricted at this time and is not widely utilized.
Another challenge is the current treatment regimens for tuberculosis. Current drug-susceptible tuberculosis treatments last at least four months, while drug-resistant tuberculosis infections last six and a half months. These regimens also consist of three to four drugs that the client needs to take. Many of these drugs have adverse effects as well.
Additionally, to increase compliance, the WHO recommends directly observed therapy, which puts a burden on healthcare and clients. Shorter treatment regimens with better-tolerated drugs are needed. This requires new antibiotics and drug combinations, requiring more clinical trials and candidates (5).

Self-Quiz
Ask Yourself...
- What preventative measures may be developed to help prevent and possibly eradicate tuberculosis?
- What diagnostic testing research is currently being done?
Conclusion
Tuberculosis remains a global health problem, with approximately ¼ of the world’s population carrying a latent form of tuberculosis infection. Tuberculosis has the highest mortality rate of any infectious agent, and there is currently no vaccine against it. Screening high-risk individuals for tuberculosis can help prevent it. Tuberculosis infection is caused by the agent Mycobacterium tuberculosis.
TB is highly contagious when active pulmonary tuberculosis infection exists. Diagnosing tuberculosis can be complex as many tests for cultures may take weeks to return with confirmative results. Tuberculosis most commonly manifests as pulmonary tuberculosis but can manifest in any part of the body. People who are immune compromised are at high risk of latent tuberculosis becoming an active tuberculosis infection. The highest number of tuberculosis cases are found in areas of poverty.
Treatment of tuberculosis infection requires a minimum of a three to four-drug regimen and a minimum of four months of treatment, which can bring compliance issues. Drug-resistant tuberculosis is on the rise and more challenging to treat. Direct observation therapy may be utilized to help increase drug compliance in those treated for active tuberculosis. There is still much research needed to meet the WHO goal of reducing the death toll and number of active tuberculosis cases.
References + Disclaimer
- Alsayed, S. S., & Gunosewoyo, H. (2023). Tuberculosis: Pathogenesis, current treatment regimens and New Drug Targets. International Journal of Molecular Sciences, 24(6), 5202. https://doi.org/10.3390/ijms24065202
- Bedaquiline. Micromedex (electronic version). Merative; 2024 (Accessed February 22, 2025). Available from: https://www.micromedexsolutions.com
- Burki, T. (2024). Pivotal tuberculosis vaccine trial begins. The Lancet, 403(10432), 1125. https://doi.org/10.1016/s0140-6736(24)00579-8
- Centers for Disease Control and Prevention. (2020, February 13). Guidelines for the treatment of latent tuberculosis infection: Recommendations from the National Tuberculosis Controllers Association and CDC, 2020. Centers for Disease Control and Prevention. https://www.cdc.gov/mmwr/volumes/69/rr/rr6901a1.htm?s_cid=rr6901a1_w
- Dartois, V. A., & Rubin, E. J. (2022). Anti-tuberculosis treatment strategies and drug development: Challenges and priorities. Nature Reviews Microbiology, 20(11), 685–701. https://doi.org/10.1038/s41579-022-00731-y
- Ethambutol. Micromedex (electronic version). Merative; 2024 (Accessed February 22, 2025). Available from: https://www.micromedexsolutions.com
- Furin, J., Cox, H., & Pai, M. (2019). Tuberculosis. The Lancet, 393(10181), 1642–1656. https://doi.org/10.1016/s0140-6736(19)30308-3
- Isoniazid. Micromedex (electronic version). Merative; 2024 (Accessed February 22, 2025). Available from: https://www.micromedexsolutions.com
- Kelly, A. M. (2019). Tuberculosis. Nursing Clinics of North America, 54(2), 193–205. https://doi.org/10.1016/j.cnur.2019.02.008
- Li, J., Zhang, L., Zhou, J., Wang, G., Zhang, R., Liu, J., Liu, S., Chen, Y., Yang, S., Yuan, Q., & Li, Y. (2022). Development and validation of self-management scale for tuberculosis patients. BMC Infectious Diseases, 22(1). https://doi.org/10.1186/s12879-022-07483-3
- Linezolid. Micromedex (electronic version). Merative; 2024 (Accessed February 22, 2025). Available from: https://www.micromedexsolutions.com
- Maison, D. P. (2022). Tuberculosis pathophysiology and anti-VEGF intervention. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 27, 100300. https://doi.org/10.1016/j.jctube.2022.100300
- Moxifloxacin. Micromedex (electronic version). Merative; 2024 (Accessed February 22, 2025). Available from: https://www.micromedexsolutions.com
- Nahid, P., Mase, S. R., Migliori, G. B., Sotgiu, G., Bothamley, G. H., Brozek, J. L., Cattamanchi, A., Cegielski, J. P., Chen, L., Daley, C. L., Dalton, T. L., Duarte, R., Fregonese, F., Horsburgh, C. R., Ahmad Khan, F., Kheir, F., Lan, Z., Lardizabal, A., Lauzardo, M., … Seaworth, B. (2019). Treatment of drug-resistant tuberculosis. an official ATS/CDC/ERS/IDSA Clinical Practice guideline. American Journal of Respiratory and Critical Care Medicine, 200(10). https://doi.org/10.1164/rccm.201909-1874st
- Pai, M., Dewan, P. K., & Swaminathan, S. (2023). Transforming tuberculosis diagnosis. Nature Microbiology, 8(5), 756–759. https://doi.org/10.1038/s41564-023-01365-3
- Peloquin, C. A., & Davies, G. R. (2021). The treatment of tuberculosis. Clinical Pharmacology & Therapeutics, 110(6), 1455–1466. https://doi.org/10.1002/cpt.2261
- Pretomanid. Micromedex (electronic version). Merative; 2024 (Accessed February 22, 2025). Available from: https://www.micromedexsolutions.com
- Pyrazinamide. Micromedex (electronic version). Merative; 2024 (Accessed February 22, 2025). Available from: https://www.micromedexsolutions.com
- Rahlwes, K. C., Dias, B. R. S., Campos, P. C., Alvarez-Arguedas, S., & Shiloh, M. U. (2023). Pathogenicity and virulence of mycobacterium tuberculosis. Virulence, 14(1). https://doi.org/10.1080/21505594.2022.2150449
- Rifampin. Micromedex (electronic version). Merative; 2024 (Accessed February 22, 2025). Available from: https://www.micromedexsolutions.com
- Rifapentine. Micromedex (electronic version). Merative; 2024 (Accessed February 22, 2025). Available from: https://www.micromedexsolutions.com
- Saukkonen, J. J., Duarte, R., Munsiff, S. S., Winston, C. A., Mammen, M. J., Abubakar, I., Acuña-Villaorduña, C., Barry, P. M., Bastos, M. L., Carr, W., Chami, H., Chen, L. L., Chorba, T., Daley, C. L., Garcia-Prats, A. J., Holland, K., Konstantinidis, I., Lipman, M., Battista Migliori, G., … Nahid, P. (2025). Updates on the treatment of drug-susceptible and drug-resistant tuberculosis: An official ATS/CDC/ERS/IDSA Clinical Practice guideline. American Journal of Respiratory and Critical Care Medicine, 211(1), 15–33. https://doi.org/10.1164/rccm.202410-2096st
- Tan, D. T., & See, K. C. (2024). Diagnosis and management of severe pulmonary and extrapulmonary tuberculosis in critically ill patients: A mini review for Clinicians. World Journal of Critical Care Medicine, 13(2). https://doi.org/10.5492/wjccm.v13.i2.91435
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
