Course
Understanding Multiple Sclerosis
Course Highlights
- In this Understanding Multiple Sclerosis course, we will learn about the types of Multiple Sclerosis (MS) and the impact MS has on daily living for patients affected by this disease.
- You’ll also learn about the clinical manifestations and complications of MS.
- You’ll leave this course with a broader understanding of the treatment options for MS.
About
Contact Hours Awarded: 3
Course By:
Charmaine Robinson
MSN-Ed, BSN, RN, PHN, CMSRN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
You finish paying for your hot dog and soda and head back to the stands. Your first professional football game! As the game starts, you take a look at your favorite team – strong, quick, and talented pro-ball players who have never lost a game. The countdown starts and the game begins. Both teams begin to disperse onto the field.
Suddenly, the players on your favorite team all remove their helmets for no apparent reason, leading to a string of injuries. The opponent team scores an easy touchdown. Your favorite team ultimately loses the game. Your hot dog is suddenly no longer appetizing. Curious how this football game relates to multiple sclerosis? As we go through the course, we will make the correlation.

Definition
The purpose of the neurological system is to transmit electrical impulses (messages) from the brain to the body in order to carry out various functions within the body (like movements and sensations). Ideally, the brain, spinal cord, and nerves should all work together seamlessly.
Multiple sclerosis (MS) occurs when the neurological system struggles to transmit messages, ultimately preventing the body from functioning properly. While researchers have not yet discovered the root cause, they do know that autoimmunity plays a role. MS is a chronic inflammatory neurodegenerative autoimmune disease in which the body damages its brain, spinal cord, and optic nerves [4, 9].
Autoimmune disease occurs when the immune system attacks healthy cells (tissues/organs/structures), mistaking them for foreign bodies. The immune system attacks the body just as it would an invading bacteria, virus, or transplanted organ. There are over 80 autoimmune diseases associated with different organs, glands, and body systems [8]. Examples include Type 1 diabetes (attack on the pancreas), rheumatoid arthritis (attack on the joints), Grave’s disease (attack on the thyroid), Crohn’s disease (attack on the bowels), and lupus (attack on multiple organs and tissues). In MS, the immune system attacks the central nervous system (CNS), more specifically, a structure called myelin.

Self-Quiz
Ask Yourself...
- What is the first image that comes to your mind when you hear the words “multiple sclerosis”?
- How often do you encounter people who have MS?
- Where in your facility can you locate information about MS?
- What other autoimmune diseases have you encountered during your practice?
Learning Activity: The Game of Football
Before we get started on making the correlation between MS and football, let’s quickly go over the basics of football. The goal of the game of football is for each team to “run” the ball past their opponents to the opposite end of the field, ultimately scoring a touchdown. Teams must work together to protect their player who is running the ball. They do this by attacking their opponents (or preventing their opponents from tackling the player with the ball). Keep this in mind as we progress through the course.
Global and National Findings
Although MS may not get the same recognition that many other conditions receive, the disease is more common than previously thought. The World Health Organization (WHO) estimates 1.8 million living with MS around the world [17].
In the U.S., there is limited statistical evidence on MS aside from a study by the National MS Society in 2017. The study found there to be one million people living with MS in the U.S.; however, there is minimal evidence of associated demographics or new cases [11]. Before 2017, the only national scientific-based study on the prevalence of MS was in 1975. The study found there to be 400,000 people living with MS at that time [11].
With MS cases more than doubling over the last 50 years or so, the National Multiple Sclerosis Society began fighting for better monitoring and tracking of this disease (as well as other neurological diseases) to bring heightened awareness. In 2016, Congress passed the 21st Century Cures Act, approving the National Neurological Conditions Surveillance System (NNCSS), and in 2018 the Centers for Disease Control and Prevention provided its funding [16]. The NNCSS primarily monitors MS and Parkinson’s disease.
However, the system is still in the early phases of surveillance. Although MS is understudied, there are new advancements in the works which will be discussed later in the course.

Self-Quiz
Ask Yourself...
- In your opinion, what misconceptions does society have about people who have MS?
- How well do you think the healthcare system acknowledges those who have MS?
- Why do you think there is limited data on MS both globally and nationally?
- Do you suspect that MS cases will rise, fall, or remain steady over the next 10 years? What is your reasoning?
Etiology/Pathophysiology
The root cause of MS remains unknown. However, researchers believe that its primary association is autoimmunity, potentially triggered by environmental and/or genetic factors [4, 15]. There is a high probability that MS runs in families. Heritability has been estimated to be between 35% to 75% [4]. Additionally, a person with the Human Leucocyte Antigen-DRB*15:01 gene (HLA-DRB*15:0) has a high risk of developing MS. Other contributing factors include Vitamin D deficiency and the Epstein Barr virus (EBV) [4].
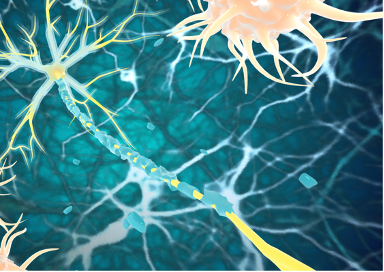
The classification of MS as an autoimmune disease is backed by the discovery of large amounts of T cells present in both spinal fluid and CNS lesions of patients with MS [4]. CNS lesions are typically found on a magnetic resonance imaging (MRI) of the brain. In the immune system, T cells (a type of white blood cell) instruct other immune cells to fight infections. In MS, it is believed that certain T cells are activated by an unknown antigen (a marker in the body that warns the immune system of a foreign invader). T cells then begin to instruct other immune cells to fight the “foreign invader,” which happens to be the body’s nervous system.
As with any immune response, the result is inflammation. In MS, the CNS becomes inflamed leading to the breakdown of myelin – a fatty/protein-rich covering that insulates the tail portion of nerve fibers (axons) [See figure 1]. Myelin protects axons and helps to make electrical impulses transmit quicker. The breakdown of myelin (termed demyelination) eventually leads to the breakdown of the axon itself (neurodegeneration), ultimately causing the deterioration of nerves and subsequent symptoms.
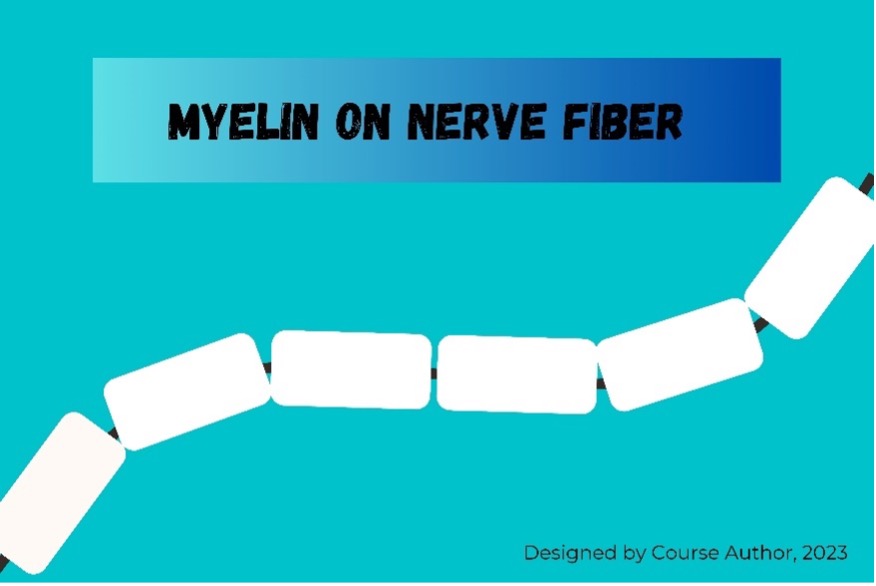
Figure 1: Myelinated Nerve Axon

Self-Quiz
Ask Yourself...
- Can you think of an inflammatory marker for another autoimmune disease?
- Have you ever witnessed a patient receive an initial diagnosis of MS while under your care?
- Do you have familiarity with any other autoimmune diseases that tend to run in families?
- What is your theory on the root cause of autoimmune disease?
Learning Activity: Learn To Play the Game
The nervous system can be likened to a game of football. Imagine that the ball is an electrical impulse/message. To get the ball across the field (transmit the impulse), the team’s players (nerve fibers or “axons”), must work together. Each player must also wear a helmet (myelin sheath) to protect themselves from sustaining a head injury during a tackle (nerve damage). If a player sustains a head injury, they will lose the ability to continue playing in the game. If multiple players lose their helmets, it’s less likely that the ball will ever make it across the field successfully.
- What do you think needs to happen to ensure that electrical impulses are not halted or delayed in people with MS?
Types
MS presents in many ways based on the course of disease progression. In some patients, symptoms start slowly and worsen over time. In others, symptoms come and go in short episodes. There are variations in the categorization of MS types, and currently there is an initiative to move categorizing from a clinical manifestation focus to a biology focus [13]. However, as of now, four primary MS types are outlined by the National Multiple Sclerosis Society. These include Clinically Isolated Syndrome, Relapsing-Remitting MS, Secondary Progressive MS, and Primary Progressive MS [13].
Clinically Isolated Syndrome
Clinically Isolated Syndrome occurs when a patient experiences an initial episode of neurological symptoms related to CNS inflammation and demyelination. This syndrome may or may not progress to MS. Symptoms include vision problems, vertigo, facial sensation loss, unilateral weakness in the extremities, coordination and balance problems, urinary problems, and swallowing and speaking difficulties.
To be considered Clinically Isolated Syndrome, the episode must last at least 24 hours. While this syndrome is not MS, it will likely progress to MS if the patient has brain lesions similar to those present in MS. In this case, patients with this syndrome might receive treatments that can delay the onset of MS.
Relapsing-Remitting
The most common of all types, Relapsing-Remitting MS is the “intermittent” type of MS. This type occurs when patients are generally stable but experience relapse (or exacerbation) of neurological symptoms on occasion. During remission periods, there may be little to no symptoms. In some patients, residual symptoms may accumulate over time with each relapse, leading to long-term disability after about 10 to 15 years [15]. Relapsing-remitting MS can be characterized in three ways:
- Active: relapses and/or MRI activity
- Not Active
- Worsening: increased disability after a relapse
Secondary Progressive
Secondary Progressive MS is a “gradual” type of MS. Patients with this type of MS start to experience a gradual worsening of symptoms/disability after an initial course of Relapsing-Remitting MS. A patient with Secondary Progressive MS may or may not experience relapses on top of an already worsening progressive course of disease. Secondary Progressive MS can be characterized in four ways:
- Active: relapses and/or MRI activity
- Not Active
- With progression: increased disability over time, with or without relapses/MRI activity
- Without progression
Primary Progressive
Primary Progressive MS is also a “gradual” type of MS. However, patients with this type of MS experience a gradual worsening of disability from the moment the disease starts (once initial symptoms begin). Symptoms include cognitive difficulties, vision problems, and myelopathy (neurological deficits related to a damaged spinal cord) [15]. Primary Progressive MS can be characterized in four ways:
- Active: occasional relapses and/or MRI activity
- Not Active
- With progression: increased disability over time, with or without relapses/MRI activity
- Without progression
Other Types/Conditions
- Radiographically Isolated Syndrome: lesions found on MRI that are similar to those seen in MS, but without the presence of symptoms
- Fulminant MS: severe MS with multiple relapses and rapid progression towards disability [15]
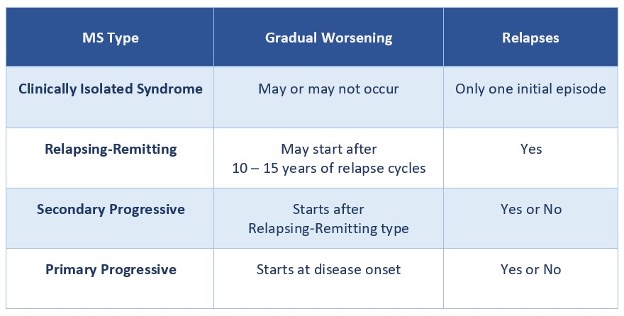
Figure 2: Types of Multiple Sclerosis [4, 13, 15]

Self-Quiz
Ask Yourself...
- Have you ever observed MS lesions/plaques on a brain MRI?
- Do your patients with MS typically have the “gradual” or “intermittent” type?
- Have you ever cared for a patient who was in the remission phase of MS?
- For your patients with MS, how long have they had the disease?
Learning Activity: Why the Personal Attack?
With the analogy of the football game, we can now understand how the neurological system functions. If a nerve is damaged due to its cells losing their myelin sheath, it will no longer function properly within the nervous system, and messages will be either lost or misconstrued. Remember the strange football game you encountered at the beginning of the course? The players in your favorite team suddenly removed their helmets for no apparent reason, which they have never done before. They have always been a strong winning team.
- How do you explain the “removing of helmets” phenomenon concerning MS? Why is this happening?
Clinical Manifestations
MS can be stable and chronic, or rapidly progressive and debilitating [15]. Symptoms can be different in each patient based on the number and location of lesions within the CNS, and according to the degree of damage. The following are some clinical manifestations of MS [13, 15]
Visual Impairments
Vision problems are one of the first symptoms of MS in many people. Double vision (diplopia), rapid eye movement (nystagmus), and inflammation of the optic nerve (optic neuritis) are common. Double vision occurs as the result of damage to the nerve that controls eye movements. With rapid eye movement, the eyes move uncontrollably and can move from side to side, up and down, or in a rotating fashion.
Both double vision and rapid eye movement can be persistent or intermittent and may resolve on their own. Typically occurring in one eye, optic neuritis is a painful MS symptom that can cause blurred vision, color blindness, and temporary or permanent impaired vision.
Fatigue
About 80% of people who have MS report fatigue [13]. Fatigue may be disease-associated or related to MS symptoms. MS lassitude is a type of fatigue that occurs as a direct result of the disease itself. People with lassitude may experience a higher-than-normal level of fatigue daily irrespective of sleep satisfaction. The fatigue typically begins suddenly, worsens as the day progresses, and is triggered by heat and humidity.
Indirect fatigue can result from MS symptoms or complications. For example, people with MS may experience sleep loss due to pain or frequent urination during the night. Sleep deprivation can cause fatigue. People with MS may also experience exhaustion from performing basic daily tasks due to activity intolerance and mobility issues, ultimately resulting in fatigue.
Pain
In patients with MS, pain may be neuropathic or musculoskeletal. Pain may be either directly related to the disease, associated with damaged nerves, or related to body changes. Musculoskeletal pain may be associated with stiffness and mobility problems. Neuropathic pain (from damaged nerves) can present as sharp, burning, stabbing, or squeezing. Examples of neuropathic pain that may occur in patients with MS include:
- Trigeminal neuralgia: stabbing intermittent pain in the jaw or face caused by damage to the trigeminal nerve.
- L’hermitte’s Sign: electric-shock-like sensation that radiates down the back and into the extremities when flexing the neck, caused by damage to the cervical area.
- MS Hug: squeezing sensation around the torso.
- Muscle spasms: sudden painful tightening of muscles occurring at any time of the day or night.
Cognitive Difficulties
People with MS may struggle with memory and concentration problems. These may include trouble finding the right words, difficulty remembering daily routines or job tasks, difficulty with making decisions, poor judgment, or trouble keeping up with conversations [13].
Cognitive dysfunction often occurs later in the disease process and is more likely with progressive MS. The dysfunction may also occur during relapse episodes. The cause of cognitive dysfunction is related to the brain atrophy that can occur in patients with MS. The number and location of lesions in the brain may also play a role.
Sensory Impairments
Numbness and tingling are common symptoms of MS. Sensory impairments may be evident in various parts of the body, including the face, arms, and legs. The impairments may be so severe that they interact with a person’s daily functioning and walking (ataxia). Numbness in the face can lead to problems with chewing or swallowing, and the inability to sense safe food temperatures.
Coordination Problems
MS can cause damage to the nerve pathways responsible for coordination and movement. This may be evidenced by ataxia, tremors that can occur at rest or with movement, and difficulty swallowing or speaking (speech can be slow or slurred).
Muscle Tightening
Though MS can cause muscle weakness, it often causes muscle tightening. Muscle spasms (spasticity) are a common symptom of MS. Spasms are involuntary and sudden and can be mild or severe. Spasms can be triggered by sudden movements, position changes, temperature extremes, or tight clothing. In people with MS, spasticity typically occurs in the lower extremities and can fall under two categories:
- Flexor spasticity: spasms cause the extremities to remain bent and difficult to straighten.
- Extensor spasticity: spasms cause the extremities to remain straight and difficult to bend.
Bladder and Bowel Dysfunction
Bladder dysfunction occurs in at least 80% of people who have MS. The dysfunction is caused by damage to the nerves that control the muscles of the bladder. In people with MS, spasms of the bladder (overactive bladder) may cause symptoms like frequency and urgency, hesitancy in starting urination, and frequent urination at night. On the oppositive end, MS can cause the bladder muscles to weaken, leading to urinary retention and incontinence. Bladder dysfunction can also be triggered by the bowel symptoms of MS. Bowel dysfunction may include constipation, diarrhea, and incontinence.
Emotional Problems
Due to the difficult challenges faced as the disease progresses, people with MS may struggle with emotional problems. These may encompass grief/loss related to independence, mood changes, anxiety, stress, moodiness, and irritability. Many people with MS may struggle with coping with their illness. Mood changes may be driven by worry and fear about how MS will impact their future. The changes may also stem from the grief and sadness associated with the loss of independence.
People with MS may experience irritability due to feeling frustrated by the functional limitations they face. They may also have high levels of stress due to the unpredictability of symptoms. Waiting for the next relapse may cause significant stress which can exacerbate even more symptoms.
Mental Illness
Emotional difficulties can lead to depression. Depression is a common symptom of MS that can occur at any point during the disease course. Research shows that the most severe form of depression – clinical depression – is more common in patients with MS than in the general population or with other chronic conditions [13].
Depression in patients with MS may be related to the emotional difficulties they may face as well as the disease itself. MS may damage the area of the brain that controls emotional regulation. Further, medications frequently administered for MS may trigger mood changes which may lead to depression. Depression can worsen during MS relapses or when there is a change in the person’s ability to care for themselves.
Other Symptoms
- Vertigo and dizziness
- Hearing loss (up to 6% of people with MS)
- Loss of taste (25% of people with MS)
- Breathing difficulties (due to weakness in the muscles of the chest)
- Seizures (2% to 5% of people with MS; caused by abnormal electrical discharges in damaged areas of the brain)
- Sexual problems (difficulty reaching orgasm for both men and women)

Self-Quiz
Ask Yourself...
- What is the most common symptom of MS you see among patients?
- Have you ever cared for a patient who had MS-like symptoms that never progressed to MS?
- In your experience, what symptoms are the most bothersome/troubling to patients who have MS?
- What are some other MS signs or symptoms you have encountered during your practice?
Complications
Due to the progressive nature of the disease, MS can cause many complications over time. Although MS only targets one body system (the CNS), the nervous system is responsible for several functions within the body. For this reason, MS complications can occur across multiple body systems.
The following are complications of MS that can lead to disability [15].
- Permanent cognitive dysfunction
- Worsening mood disorders (can lead to morbidity as suicide risk is 7.5 times higher in people with MS compared to the general population) [13]
- Unilateral blindness (related to optic neuritis)
- Chronic aspiration (due to swallowing problems)
- Transverse myelitis (inflammation of the spinal cord; can cause sensation and mobility problems below the level of spinal cord damage) [10]
- Impaired mobility (may be caused by loss of motor control or gait issues)
- Urinary tract infections and kidney stones (due to bladder dysfunction)
- Skin breakdown due to incontinence
- Erectile dysfunction

Self-Quiz
Ask Yourself...
- What is the most common complication of MS you have encountered?
- Does your facility use a standardized suicide screening tool?
- In your opinion, how can nurses help to maintain or improve a patient’s mobility status?
Prognosis
MS is a progressive disease, typically worsening over time. Various factors may lead to a better (or worse) prognosis. These factors are mostly related to the type of MS, gender, size of lesions, and frequency and intensity of relapses, among others. The following are factors that are associated with both favorable and non-favorable prognoses: [15]
Factors that suggest a more favorable prognosis:
- Female gender
- Remitting-Relapsing type of MS
- Relapses are mild
- Good recovery in between relapses
- Symptoms are mostly sensory-related
- Minimal number of lesions on MRI
Factors that suggest a less favorable prognosis:
- Male gender
- Progressive type of MS
- Frequent relapses
- Minimal recovery between relapses
- A larger number of lesions on MRI
- Brain atrophy on MRI

Self-Quiz
Ask Yourself...
- Do you witness more men or women with MS?
- How often do you care for patients with MS who primarily experience sensory deficits over other symptoms?
- What clinical signs do you think would indicate that a patient may have brain atrophy?
Impact on Quality of Life
MS is a chronic disease that can be debilitating and its impact on a person’s quality of life can be substantial. In a 2020 global survey of over 1,000 adult participants with MS, people living with the Relapsing-Remitting type of MS were questioned about the impact that MS had on their overall quality of life [2]. Participants were recruited from the U.S., United Kingdom, Spain, Italy, France, Canada, and Australia. Approximately 18% had been diagnosed with MS within 15 to 20 years of the study, 22% within 10 to 14 years, 26% within five to nine years, and 22% within less than five years. The study found that MS had a negative impact on functionality, emotional and social health, work and other life roles.
- Activities of Daily Living: Over 40% reported a worsened ability to perform activities of daily living over two years. Over half reported limitations related to fatigue, weakness, balance/coordination problems, heat/cold sensitivity, numbness/tingling, and muscle stiffness. Nearly 40% reported urinary problems as a consideration before planning to leave the house. Almost half listed trouble multitasking as a limiting factor.
- Mental Well-Being: Over 70% reported a negative impact of MS on their energy level. Over 45% reported problems with memory and concentration, mood swings, and depression/anxiety. More than 70% reported concerns about disease progression and possible future disability, which may have contributed to the anxiety they had.
- Sleep: Over half reported trouble sleeping.
- Emotional Wellbeing: Almost half reported a negative impact on their future outlook, 40% on their ability to cope with stress, and 35% on self-esteem.
- Social Life: One-fourth of all participants reported a negative impact on relationships with friends and 16% on family. Almost 45% were concerned about matters relating to sexual attractiveness. A fourth worried their partner would leave them. Nearly 35% reported MS affected their roles related to family, friends, and work. More than a third reported that they go out of their way to keep their MS hidden from others.
- Job/Career: Nearly 65% reported that MS affected their ability to keep a job, and 50% reported that MS affected their career progression.

Self-Quiz
Ask Yourself...
- In your opinion, what are some MS symptoms that might contribute to sleep loss?
- What strategies would you recommend that might help patients with MS conserve energy?
- What do you think are some contributing factors to self-esteem issues in people with MS?
- What are some changes that family or friends can make to help people with MS feel comfortable sharing their diagnosis?
Learning Activity: The Damage Has Been Done
Back to football’s correlation to MS. The “removing of helmets” phenomenon can be likened to the autoimmunity of MS. The body works against itself by attacking its own myelin.
The story continues…After the strange behavior at the game, all team players (axons) were treated for their injuries. However, some developed permanent injuries (permanent nerve damage). The coach arranged for the team to be evaluated to determine the cause of the strange behavior. All findings came back inconclusive.
Due to the injuries and sudden behavior change, the team is at risk for lost contracts, money, and notoriety (the body is at risk for complications of MS). The coach begins to devise a plan to finish out the football season with the players who can still play. Although the team is already at a disadvantage, the coach’s goal is to prevent further injuries during the next game. A cure for MS has not been found. The damage has been done.
- What would you say is the primary goal in the care of patients with MS?
Nursing Assessment
MS is a disease characterized by classic neurological symptoms. An accurate history and physical are key in the care of patients with actual or suspected MS. Collecting information about symptom onset, frequency, and intensity helps to guide the diagnosis and eventual treatment of MS. While a general head-to-toe assessment is appropriate as symptoms vary, a focused assessment on body systems that are typically affected by MS may be most beneficial. Nurses caring for patients with actual or suspected MS should perform the following focused assessments [15].
General Presentation
Begin by observing the overall presentation of the patient. Observe for tremors and twitching as these may be present with MS. Assess the patient’s gait. Ataxia can be a sign of MS. Observe the patient’s overall mood and inquire about mental illnesses such as mood disorders, depression, and anxiety may be present with MS.
Depression screening tools may be beneficial. Pay attention to the rate, quality, and clarity of the patient’s speech as slow or slurred speech can indicate MS. Ask if the patient has had problems concentrating or remembering people or events. Take note of the level of concentration the patient has during the assessment. Patients with MS can experience memory loss and difficulty concentrating.
Pain Assessment
Depending on the patient’s cognitive abilities, pain may be assessed with various methods including verbal pain scores, visual analog scales (faces pain scale), or physical signs of pain. If appropriate, ask the patient to describe the pain’s characteristics, intensity, duration, and precipitating factors. Sharp pains or shock-like sensations may be present with MS, for example, L’hermittes sign as mentioned earlier (electrical sensation down the back when the neck is flexed).
Neurological Assessment
Begin by assessing the patient’s hearing. Ask if they have been having difficulty hearing and perform a hearing exam. Some patients with MS may experience hearing loss. Next, ask the patient if they have experienced numbness, tingling, prickling, coldness, or any odd sensations anywhere on the body. It may also be helpful to ask the patient to close their eyes, then gently tap (or place a cotton ball) to various locations on the skin while asking if they feel anything. Impaired sensations are common in patients with MS and may also be associated with transverse myelitis.
Begin an eye exam. Ask if the patient has noticed any visual changes or disturbances and when the change began. Perform a vision test, pupillary response test, and ocular movement test (extraocular muscle function). Vision loss and pain with eye movements may indicate the presence of optic neuritis. Rapid eye movements and double vision may also be present with MS. Adduction difficulties may also be present with MS (when one or both of the patient’s eyes do not move when they look to the side).
Neuromuscular Assessment
Many MS symptoms are associated with muscle strength which is dependent on nerve function. Ask the patient if they have experienced any general, unilateral, or extremity-specific weakness. Inquire if the weakness was sudden or progressive as these may give clues on the type of MS. Ask the patient if they have had difficulty with speaking or swallowing as these may be present with MS. Begin assessing the rest of the body. Assess muscle tone and strength. Ask the patient if they have experienced muscle spasms and in what areas of the body. Patients with MS may experience poor muscle tone, paralysis, and muscle spasms.
Genitourinary/Gastrointestinal Assessment:
Patients with MS may experience many complications associated with bowel and bladder function. Therefore, a detailed elimination assessment is vital. Start by asking the patient if they have experienced any changes in bowel or bladder function. Inquire if they void or pass stool on their own. Assess the pelvic region for bladder distention and check residual bladder volume if indicated.
Urinary and bowel incontinence and urinary retention may be present in patients with MS. Assess urine for color, consistency, clarity, and odor as urinary tract infections are a complication of MS. Ask when the last bowel movement was made and inquire about stool characteristics and elimination patterns as constipation and/or diarrhea may be present with MS.

Self-Quiz
Ask Yourself...
- What are some additional questions you might ask a patient with MS to better understand their disease course?
- How have patients with MS described their pain to you? Burning? Itching? Sharp?
- Have you ever had a patient with MS experience an exacerbation of a symptom during your assessment/care? For example, while repositioning the patient?
- Does your facility use a standardized depression screening tool?
Nursing Management
After obtaining an accurate history and performing both general and focused assessments, nurses must devise a plan of care for patients with MS that focuses on managing symptoms and maintaining the quality of life. As mentioned earlier in the course, MS can significantly impact a person’s functioning, sleep, mental/emotional health, and social/work life.
The plan of care should address each debilitating symptom, empowering the patient with the knowledge, skills, and resources needed to effectively manage their own lives. The following are ways in which nurses can help patients cope with their disease [13].
Cognitive Rehabilitation
Early recognition of cognitive problems is ideal in caring for a patient with MS. After performing a neurological assessment, report abnormal findings to the physician and arrange for cognitive screening tests as ordered. Interdisciplinary team members like neuropsychologists and speech or language pathologists may perform the tests. The screening will address various levels of cognitive functioning and results will help to determine what type of services or therapies are needed to help the patient manage the symptoms.
Cognitive rehabilitation is a group of restorative and compensatory activities that help patients become stronger mentally and make up for cognitive losses [13]. Assist by encouraging the patient to participate in activities led by members of the interdisciplinary team. Recommending the following activities may be helpful:
- Create checklists and calendars
- Set alarms and timers
- Dictate to-do-lists on a digital recorder
- Eliminate background noises when speaking to others (i.e. turning off the television)
- Take breaks
- Do one thing at a time
Physical, Occupational, and Speech Rehabilitation
Symptoms including fatigue, muscle weakness, spasticity, and tremors can make it difficult for patients with MS to walk and perform daily tasks safely. Muscle weakness and numbness in the face can lead to difficulties with speaking and swallowing. Physical, occupational, and speech rehabilitation can help patients maintain quality of life through various techniques.
Encourage patients to participate in these rehabilitative activities by providing education on the benefits of each service. Eliminate any barriers to participation, which may include ensuring that the patient’s pain is properly managed and involving the patient’s support system (family, caregivers, etc.).
Physical therapists can teach patients better ways of moving or walking to help conserve energy and avoid falls and other injuries. Occupational therapists can help patients discover ways to perform activities of daily living most effectively, using assistive devices as needed. Speech-language pathologists can teach patients techniques to enhance communication and swallow safely.
Bladder and Bowel Care
While patients with MS may benefit from prescribed medications for elimination, lifestyle modifications can help promote optimal bladder and bowel care. This can include tips for how to manage symptoms when in public (i.e., wearing easily removable clothing), fluid intake adjustments (like avoiding drinking water right before bedtime), and bladder/bowel training.
Bladder and bowel training involves helping patients understand their elimination patterns and create an elimination schedule. Intermittent urinary catheterization may be beneficial for some patients who have difficulty emptying the bladder. To further assist with urination, consider teaching patients how to perform pelvic floor exercises to target the muscles responsible for bladder muscle contraction. The exercises can strengthen weakened muscles, help with muscle control, and relax spasmodic muscles.
Support Healthy Coping
When addressing the emotional health of patients with MS, first create a supportive safe environment for the patient to express their concerns. The nurse’s primary role in this case is to determine the patient’s supportive needs based on the history that was obtained and the assessment performed. Patients with MS may greatly benefit from counseling and education on stress management. Provide both verbal and written education and make referrals as needed. It may also be beneficial to refer patients to national and community organizations/groups in which they can find support groups and other supportive and educational resources for themselves and their families.
Although emotional problems can be attributed to brain changes that are unavoidable in some MS cases, many emotional difficulties result from unmet physical/functional needs. Part of helping patients cope involves ensuring that basic needs are met, for example, effectively managing pain, and arranging for caregiver services or physical/occupational therapies as needed.
Other Interventions
- Sleep Care: Promote sleep health to help with fatigue by addressing problems that can interfere with sleep. These may include limiting environmental distractions, managing pain, and following elimination schedules. Encourage the patient’s family/caregiver to avoid unnecessary sleep interruptions.
- Heat Regulation: Avoid triggering fatigue and muscle spasms by keeping the patient at a comfortable temperature. Teach the patient and their family/caregiver heat management strategies that can be used in the home.
- Fall Prevention: Prevent falls by maintaining safety precautions as patients with MS can be at risk for falls related to balance/coordination issues, muscle spasticity, fatigue, and weakness. Teach the patient and their family/caregiver how to prevent falls in the home.
- Skin Care: Perform skin care to avoid skin breakdown related to incontinence and limited mobility. Teach the patient and their family/caregiver how to maintain skin integrity while at home.
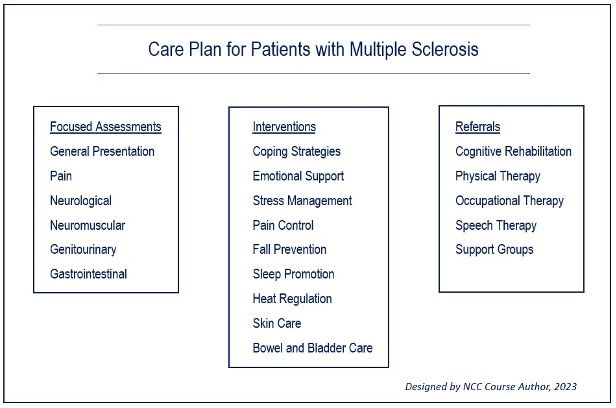
Figure 3: Care Plan for Patients with Multiple Sclerosis

Self-Quiz
Ask Yourself...
- In what ways does your facility ensure that interdisciplinary team members collaborate effectively?
- When was the last time you assisted a patient with a bowel or bladder program?
- In your opinion, what are some ways that people with MS can be prepared for incontinence episodes when away from home?
- In what ways do you promote sleep for the patients in your facility?
Treatment
Treatment for MS is difficult due to the chronic inflammatory degenerative nature of the disease. Treatment is primarily aimed at reversing the damage and protecting axons from future damage [5]. MS treatments can also include those focused on symptom management. MS may be treated with medications and various therapies. The following are some treatment options for patients with MS.
Medications
Medications for MS may target three areas of MS management: modifying the disease course, addressing relapses/exacerbations, and managing symptoms. MS medications may be administered intravenously (IV), intramuscularly (IM), subcutaneously (SQ), intradermally, and orally. Some may be administered directly into the detrusor muscle (bladder muscle) to help with bladder dysfunction.
The following tables include common medications for the treatment of MS, routes, doses, adverse effects, and precautions for nurses when administering the drug [13].
|
Infusion Medications to Treat Multiple Sclerosis
|
|||
|
Drug |
Route/Dose |
Adverse Effects |
Precautions |
|
Ublituximab-Xiiy (Briumvi) |
Initial dose: 150mg IV, Second dose: 450mg IV two weeks later and every 24 weeks subsequently |
Headache, diarrhea, nausea, alopecia |
Can reduce immunoglobulin; Monitor immunoglobulin levels |
|
Alemtuzumab (Lemtrada) |
Initial dose: 5mg IV/day for five days, Subsequent doses: 5mg IV/day for three days 12 months after prior doses. |
Headache, fever, nasopharyngitis, nausea |
Can cause lymphopenia; Monitor complete blood count Monitor for suicidal ideation |
|
Mitoxantrone (Novantrone) |
12 mg/m2 IV every three months (m2 is a calculation of body surface area based on height and weight) |
Urinary tract infection, nausea, diarrhea |
Can cause leukemia, anemia, and cardiac function changes; Monitor complete blood count and cardiac status |
|
Ocrelizumab (Ocrevus) |
First dose: 300mg IV, Second dose: 300mg IV two weeks later, Subsequent doses: 600mg IV every six months |
Headache, diarrhea, cough, sinusitis, back pain |
Can increase blood pressure; Monitor blood pressure Monitor for bradycardia with first dose. |
|
Natalizumab (Tysabri) |
300mg IV every four weeks |
Headache, fatigue, muscle ache, urinary tract infection, lower respiratory tract infection |
Can cause thrombocytopenia; Monitor complete blood count
|
Table 1: Infusion Medications for Multiple Sclerosis [13]
|
Injection Medications to Treat Multiple Sclerosis
|
|||
|
Drug |
Route/Dose |
Adverse Effects |
Precautions |
|
Interferon Beta-1A (Avonex) |
30mcg IM once weekly |
Flu-like symptoms |
Can cause reduced blood counts; Monitor complete blood count |
|
Interferon Beta-1A (Rebif) |
22mg or 44 mg SQ three times a week |
Flu-like symptoms, abdominal pain, depression |
Can cause reduced blood counts; Monitor complete blood count |
|
Interferon Beta-1B (Betaseron, Extavia) |
0.25mg SQ every other day |
Flu-like symptoms, headache, insomnia |
Can cause decreased white blood cell count; Monitor complete blood count |
|
Glatiramer Acetate (Copaxone)
|
20mg SQ daily |
Vasodilation, dyspnea |
Monitor for sudden flushing, tachycardia, and anxiety post-injection |
|
Onabotulinumtoxin A (Botox) |
100- or 200-units IM, intradermal, or intradetrusor |
Urinary tract infection (when given in detrusor muscle), extremity pain (when given in extremity) |
Watch for swallowing and breathing difficulties |
|
Peginterferon Beta-1A (Plegridy) |
125mg SQ or IM every 14 days |
Flu-like illness, fever, headache |
Can cause reduced blood counts; Monitor complete blood count |
|
Ofatumumab (Kesimpta) |
20mg SQ weekly x3, then monthly |
Upper respiratory infection, headache |
Contraindicated if patient has hepatitis B |
Table 2: Injection Medications for Multiple Sclerosis [13]
|
Oral Medications to Treat Multiple Sclerosis
|
|||
|
Drug |
Route/Dose |
Adverse Effects |
Precautions |
|
Teriflunomide (Aubagio)
|
7 to 14mg oral once daily |
Headache, diarrhea, nausea, alopecia |
Can increase blood pressure; Monitor blood pressure |
|
Monomethyl Fumarate (Bafiertam) |
95mg oral twice daily for 7 days, then 190mg twice daily |
Flushing, abdominal pain, diarrhea, nausea |
Can cause lymphopenia; Monitor complete blood count |
|
Dimethyl Fumarate (Tecfidera) |
120mg oral twice daily for 7 days, then 240mg twice daily |
Flushing, abdominal pain, diarrhea, nausea |
Can cause lymphopenia; Monitor complete blood count |
|
Fingolimod (Gilenya) |
0.5mg oral once daily |
Headache, diarrhea, cough, sinusitis, back pain |
Can increase blood pressure; Monitor blood pressure Monitor for bradycardia with first dose. |
|
Cladribine (Mavenclad) |
1.75mg/kg oral per treatment course (max 2 courses) |
Upper respiratory tract infection, headache |
Can cause lymphopenia; Monitor complete blood count Do not give within three hours of any other oral medication |
|
Siponimod (Mayzent) |
Titrate initial doses for 5 days starting at 0.25mg oral daily; then 2mg daily |
Headache |
Can increase blood pressure; Monitor blood pressure Monitor for bradycardia and arrythmias |
|
Ponesimod (Ponvory) |
Titrate initial doses for 14 days starting at 2mg oral daily; then 20mg daily |
Upper respiratory tract infection |
Can increase blood pressure; Monitor blood pressure Monitor for bradycardia and arrythmias |
|
Diroximel Fumarate (Vumerity) |
231mg oral twice daily for 7 days, then 462mg twice daily |
Flushing, abdominal pain, diarrhea, nausea |
Can cause lymphopenia; Monitor complete blood count |
|
Ozanimod (Zeposia) |
0.23mg oral daily for 7 days, then 0.92mg daily |
Upper respiratory tract infection, urinary tract infection, back pain |
Can increase blood pressure and/or orthostatic hypotension; Monitor blood pressure Monitor for bradycardia and arrythmias |
Table 3: Oral Medications for Multiple Sclerosis [13]
Medications for Pain: antidepressants and anticonvulsants are used to manage pain in patients with MS [13].
- Duloxetine (Cymbalta)
- Venlafaxine (Effexor)
- Amitriptyline (Elavil)
- Lamotrigine (Lamictal)
- Pregabalin (Lyrica)
- Gabapentin (Neurontin)
- Nortriptyline (Pamelor; Aventyl)
- Carbamazepine (Tegetrol)
- Oxcarbazepine (Trileptal)
Medication for Fatigue: CNS stimulants, wakefulness-promoting agents, some antivirals, and antidepressants are used to manage fatigue in patients with MS [13].
- Dextroamphetamine and amphetamine (Adderall)
- Amantadine
- Modafinil (Provigil)
- Fluoxetine (Prozac)
- Methylphenidate (Ritalin)
Medications for Spasticity: muscle relaxants and CNS depressants are used to manage muscle spasticity in patients with MS [13].
- Baclofen
- Onabotulinumtoxin A (Botox)
- Dantrolene (Dantrium)
- Clonazepam (Klonopin)
- Diazepam (Valium)
- Tizanidine (Zanaflex)
Medications for Bladder Dysfunction: antimuscarinics/anticholinergics, antispasmodics, bladder muscle relaxants, some antihypertensives, and tricyclic antidepressants are used to manage bladder dysfunction in patients with MS [13].
- Onabotulinumtoxin A (Botox)
- Desmopressin (DDAVP Nasal Spray)
- Tolterodine (Detrol)
- Oxybutynin, (Ditropan; Oxytrol)
- Darifenacin (Enablex)
- Tamsulosin (Flomax)
- Prazosin
- Mirabegron (Myrbetriq)
- Imipramine (Tofranil)
- Solifenacin Succinate (Vesicare)
Medications for Bowel Dysfunction: stool softeners, laxatives, suppositories, and enemas are used to manage bowel dysfunction in patients with MS [13].
- Docusate (Colace)
- Bisacodyl (Dulcolax)
- Fleet enema
- Mineral oil
- Psyllium hydrophilic musilloid (Metamucil)
- Magnesium hydroxide (Milk of Magnesia)
- Glycerin suppository
Procedures
Aside from medications, procedural therapies may help patients with MS to manage their illness better. The following are three optional procedures for MS symptom management [13].
- Sacral Neuromodulation (SNM): SNM is a minimally invasive therapy in which a neurostimulator is surgically implanted under the skin to stimulate nerves of the sacral region (those that control bladder and pelvic muscles). SNM is indicated to help regulate elimination for patients with urinary frequency, urgency, and incontinence. Globally, more than 300,000 people have sacral neuromodulation implants [3]. While SNM is also used in other countries for bowel incontinence, the Food and Drug Administration has not approved it for this purpose in the U.S. [3].
- Percutaneous Tibial Nerve Stimulation (PTNS): PTNS is another form of neuromodulation that targets the tibial nerve. This procedure is used to help patients with an overactive bladder. During the procedure, an electrode is placed in the ankle and transmits a signal starting at the tibial nerve extending to the nerves in the sacral region. PTNS has been shown to reduce urinary frequency, urgency, incontinence, and nocturnal urination in 60% – 80% of people who have had it done [3].
- Suprapubic Cystostomy: Surgically placed suprapubic catheter to help manage bladder dysfunction.

Self-Quiz
Ask Yourself...
- What medications for MS are you most familiar with?
- What is your experience administering IV medications for MS?
- Have you experienced difficulty controlling pain in patients who have MS?
- How often do you care for patients who have suprapubic catheters?
Learning Activity: “Remain in the Game”
Remember the football players? Some of the players who had removed their helmets sustained injuries that led to permanent disability. They were no longer useful to the team. The coach’s goal was to prevent the remaining players (who could still play in the game) from further injuries in the next game. With MS, the goal is to prevent further nerve damage and manage the symptoms that will occur in the next relapse (or “next game”).
The coach ultimately arranged for the remaining players to participate in a rehabilitation and counseling program, so that the team could finish the season. With MS, damaged axons – or nerve damage – may lead to permanent disabilities. For example, with optic neuritis, a patient may develop permanent vision loss in one eye. However, if the optic nerve is treated/rehabilitated early enough, vision may be partially or fully restored, and the nerve can “remain in the game.”
- Can you think of another treatment or intervention that can help CNS nerves “remain in the game”?
New Research
No cure has been found for MS. However, researchers are attempting to better understand the disease process and find new treatment strategies. This includes studying risk factors, drugs and other therapies, and ways to improve accuracy in diagnosis [9].
The following are MS topics that are currently under study by researchers [9].
Topics of Research
- Role of genetics and the environment as risk factors for MS
- Diagnosis and monitoring of MS through biomarkers (signs that might show MS risk or help to monitor disease progression)
- Strategies to improve MRI testing in people with MS
- The role diet and gut biome play in MS
- Reason for gender differences in how MS presents
- Disparities in the care of people with MS, particularly African American and Hispanic populations
- Function of the immune system in the CNS of people with MS
- Basics of myelination and demyelination, and strategies to limit myelin and axonal loss
Current Updates
While there are many topics of study surrounding MS, scientists have already made grand discoveries that have proven to be effective in the management of MS. Many studies are conducted by the National Institute of Neurological Diseases and Stroke and sponsored and funded by groups like the National Institute of Health and the National Institute of Allergy and Infectious Diseases.
The following are research updates on MS [9].
- Genetic Testing: There are genes associated with an increased risk for MS, for example, the earlier mentioned HLA-DRB*15:0 gene. Scientists are studying the function of these genes in the nervous system and the role they play in MS development.
- Diagnostic Studies: The body naturally attempts to repair itself, and with MS, the body’s repair mechanisms may obscure evidence of active lesions on MRIs (lesions may appear to come and go) [15]. For this reason, symptoms may not be reflective of MRI results as they might with many other diseases and conditions. Scientists are studying ways to develop more powerful MRI methods to diagnose and monitor MS and assess the effectiveness of MS treatments. To do this, scientists are conducting years-long studies comparing MRIs of over 100 patients with MS with MRIs of those without MS. Scientists are also studying how detection of a “central vein” passing through brain lesions/plaques on MRIs can help differentiate between MS and other neurological disorders that might mimic MS (to prevent misdiagnosis).
- Blood Tests: Scientists are studying a blood test that measures neurofilaments (proteins derived from nerve cells) to determine MS severity and effectiveness of treatments.
- New Medications: Through clinical trials, scientists tested a drug called “Ibudilast” for neuroprotective properties in progressive MS. The trials found that the drug slowed down the rate of brain atrophy.
- Stem Cell Treatment: Scientists are testing a stem cell treatment called “autologous hematopoietic stem cell transplantation” (AHSCT) for severe forms of relapsing MS. The treatment involves removing some of a person’s immune cells and replacing them with their own stem cells as a way to “reset” the immune system.

Self-Quiz
Ask Yourself...
- What types of laboratory or diagnostic tests do you see ordered for patients with MS?
- In your opinion, what are societal barriers to adequate MS research?
- Have you heard of any other new treatments for MS?
- Do you know of any other medical conditions in which stem cell therapy has been effective?
Patient Resources
Nurses can provide support to patients with MS and their families by providing them with community resources from various groups and organizations. These groups provide educational materials on autoimmune disease and MS for better disease management. These groups also serve as a great resource for disability support.
Multiple Sclerosis Association of America
Founded in 1970, the Multiple Sclerosis Association of America (MSAA) is an organization that aims to improve the lives of people living with MS and their families. The organization has a national Board of Directors, a Chief Medical Officer for medical consultation and review, and Advisory boards for diverse populations, including African Americans and Hispanics/Latinx. Aside from leading educational programs on MS, the organization hosts a helpline, online forum, blog, and podcast [6].
National Multiple Sclerosis Society
The National Multiple Sclerosis Society (NMSS) is an organization that aims to find a cure for MS. The organization is a great resource for people with MS, their families, and health professionals, including providers, nurses, rehabilitation professionals, mental health workers, and health and wellness professionals. The group provides statistical data on MS and is a source for detailed and extensive education on the disease. The organization also provides resources for advocacy, volunteering, fundraising, and support groups [12]
Autoimmune Association
The Autoimmune Association is a group that advocates for patients with autoimmune diseases and supports research that aims to find a cure. The group raises awareness about autoimmune diseases and advocates for federal and state-level changes that improve the lives of patients living with the disease. The group also educates, supports, and empowers patients starting with diagnosis and access to care, to disease management and quality of life improvement [1].
National Ataxia Foundation
Founded in 1957, the National Ataxia Foundation (NAF) is an organization that supports people living with ataxia, and their families. The organization funds research on ataxia with hopes of developing new treatments and finding a cure. People with MS may benefit from involvement with the NAF as the organization is a great resource for education and finding support groups and events [7].
Paralyzed Veterans of America
While the Paralyzed Veterans of America (PVA) is primarily focused on helping veterans with spinal cord injuries, people with spinal dysfunction (which may occur with MS) are also welcomed. The organization was started by a group of World War II veterans who returned home with spinal cord injuries. Today, the PVA advocates for quality health care, education, benefits, and civil rights for affected veterans [14].

Self-Quiz
Ask Yourself...
- Have you ever referred a patient or family member to a community support group?
- In your opinion, how can nurses help people with MS gain better access to healthcare?
- What community resources might you anticipate a person with MS might need?
- What do you think are some learning needs of patients with autoimmune diseases?
Learning Activity: “Damage Control”
The next football game is approaching, and the coach makes one final move – designing a helmet that is more difficult to remove. The coach knows that the players will likely still try to remove their helmets in the game, but now the process of doing so will be more challenging. In MS, progressive CNS damage is inevitable. However, many MS medications work by slowing down the demyelination process, ultimately protecting the axons from future damage (in a sense, doing “damage control”).
While the football team may win fewer plays, they are still able to stay in the game. While MS is progressive, it is not a death sentence. Patients can still function in the “game of life” and nurses can help to make it easier.
- In your opinion, how can nurses encourage patients who have MS?
Conclusion
An MS diagnosis can be life-altering, but it does not have to be life-limiting. There are many therapies, treatments, and resources available to help patients maintain the quality of their lives. Although the population of people with MS has more than doubled over the last 50 years or so, new and innovative developments are underway. Nurses can contribute by performing thorough assessments, asking the right questions, arranging appropriate referrals, and educating patients on disease management. These strategies and more can make a big impact on the lives of patients with MS and their families.

Self-Quiz
Ask Yourself...
- What do you think is the highest nursing priority when caring for patients who have MS?
- What do you think is the greatest learning need for families of patients who have MS?
- How can nurses challenge their perceptions about people who have MS and other autoimmune diseases?
- What are ways nurses can contribute to MS research?
- How can you advocate for patients with MS in your facility?
- What is one way you can change your practice to better care for patients with MS?
- How can you bring more awareness to MS in your community?
- How can society help people with MS continue to live productive lives?
References + Disclaimer
- Autoimmune Association. (2023). Four pillars of the autoimmune association. https://autoimmune.org/
- Bass, A. D., Van Wijmeersch, B., Mayer, L., Mäurer, M., Boster, A., Mandel, M., Mitchell, C., Sharrock, K., & Singer, B. (2020). Effect of multiple sclerosis on daily activities, emotional well-being, and relationships. International Journal of MS Care, 22(4), 158–164. https://doi.org/10.7224/1537-2073.2018-087
- Feloney, M.P., Stauss, K., Leslie, & S.W. Sacral neuromodulation. (2023). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK567751/
- Kunkl, M., Frascolla, S., Amormino, C., Volpe, E., & Tuosto, L. (2020). T helper cells: The modulators of inflammation in multiple sclerosis. Cells, 9(2), 482. https://doi.org/10.3390/cells9020482
- Mey, G. M., Mahajan, K. R., & DeSilva, T. M. (2023). Neurodegeneration in multiple sclerosis. WIREs Mechanisms of Disease, 15(1), e1583. https://doi.org/10.1002/wsbm.1583
- Multiple Sclerosis Association of America. (2023). Who we are. https://mymsaa.org/about-msaa/who-we-are-mission-overview/
- National Ataxia Foundation. (n.d.). About NAF. https://www.ataxia.org/about-naf/
- National Institute of Allergy and Infectious Disease. (2022). Autoimmune diseases. https://www.niaid.nih.gov/diseases-conditions/autoimmune-diseases
- National Institute of Neurological Disorders and Stroke. (2023). Multiple sclerosis. https://www.ninds.nih.gov/health-information/disorders/multiple-sclerosis#toc-what-are-the-latest-updates-on-multiple-sclerosis-
- National Institute of Neurological Disorders and Stroke. (2023). Transverse myelitis. https://www.ninds.nih.gov/health-information/disorders/transverse-myelitis
- National Multiple Sclerosis Society. (2019). Landmark study estimates nearly 1 million in the U.S. have multiple sclerosis. https://www.nationalmssociety.org/About-the-Society/News/Landmark-Study-Estimates-Nearly%C2%A01-Million-in-the-U
- National Multiple Sclerosis Society. (2023). [Homepage]. https://www.nationalmssociety.org/
- National Multiple Sclerosis Society. (2023). What is MS? https://www.nationalmssociety.org/What-is-MS
- Paralyzed Veterans of America. (n.d.). Mission statement. Retrieved from https://pva.org/about-us/mission-statement/
- Tafti, D., Ehsan, M., Xixis, K.L. (2022). Multiple sclerosis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK499849/
- U.S. Centers for Disease Control and Prevention, Office of Public Health Data, Surveillance, and Technology. (2023). National Neurological Conditions Surveillance System (NNCSS): Progress to date. https://www.cdc.gov/surveillance/neurology/progress_to_date.html
- World Health Organization. (2023). Multiple sclerosis. https://www.who.int/news-room/fact-sheets/detail/multiple-sclerosis
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
