Understanding Wound Care Dressings
Contact Hours: 1
Author(s):
Kimberlee Emfield Rowett DNP, MSN, MBA, RN
Course Highlights
- In this Understanding Wound Care Dressings course, you can recite the different wound types and healing stages.
- You will learn the various dressing options, their purposes, and be able to describe complications of wounds and wound care dressings.
- You will leave this course with a broad understanding of interventions that can improve the effectiveness of wound care dressings.
Introduction
Wound care dressings are fundamental to effective nursing care across various specialties. The healing and management of wounds can be influenced by numerous medical conditions, requiring nurses to possess the knowledge and skills to select and apply appropriate dressings. Proper wound dressing management promotes faster healing, reduces the risk of infection, and enhances patient comfort and quality of life. This course focuses on the principles of wound care dressings, including their types, uses, and evidence-based strategies for selecting and applying them to optimize wound healing and patient outcomes (1).
Ask yourself...
- Why must nurses stay informed about advancements in wound care dressing technologies and practices?
- What factors should nurses consider when selecting a patient’s most appropriate wound care dressing?
Types of Wounds
There are four main types of wounds: acute, chronic, surgical, and non-surgical. A wound’s classification is crucial in determining the appropriate dressing and treatment approaches. Nurses must understand these types to select the most effective wound care strategies.
An acute wound is typically caused by trauma or injury, such as abrasions, burns, or cuts. These wounds usually follow a predictable healing timeline, normally healing between 4 to 6 weeks without significant complications. The dressing selection is adequate by wound size, location, and exudate. The primary treatment goal would be to promote optimal healing (2).
For acute wounds, the use of the Gustilo-Anderson classification can be helpful. Type 1 wounds are clean, low-energy puncture wounds that are less than 1 centimeter. Type 2 has moderate soft tissue damage and crushing greater than 1 centimeter in size. Type 3 is broken into three subcategories. Type 3A is a high-energy open injury with extensive soft tissue damage. Type 3B is a significantly contaminated wound with extensive soft tissue damage. Type 3C is the same as 3A and 3B but is associated with arterial injuries.
Chronic wounds, on the other hand, fail to progress through normal stages of healing and persist beyond the typical 4 to 6 weeks. Common causes for chronic wounds include diabetes, poor circulation, and conditions such as venous insufficiency or pressure ulcers. Due to the prolonged healing phase, chronic wound healing focuses on utilizing specialized dressings. There are a variety of chronic wounds. Understanding which wound the patient is suffering from will aid in determining which wound care dressing is needed.
Diabetic foot ulcers are often caused by diabetic neuropathy and poor circulation. This leads to reduced blood flow, increasing the risk of trauma to feet and legs. As they sound, pressure ulcers are caused by prolonged skin pressure. This is commonly experienced by bedridden patients or those with limited mobility. Venous ulcers are related to poor venous circulation, typically affecting the lower extremities and exhibiting edema. Similarly, arterial ulcers are related to inadequate blood flow due to peripheral arterial diseases. These wounds are mostly found on the toes, feet, or lower legs.
Surgical wounds, as it sounds, are related to surgical procedures. These wounds are typically acute but can have complications depending on the patient’s health. The surgical site can also impact the timeline of healing. Dressings for surgical wounds will be determined based on the wound type, surgical area, healing stage, and infection prevention needs.
Finally, non-surgical wounds are either acute or chronic wounds that did not develop related to surgery. This can include causes like traumatic injuries, ulcers, or wounds from other health complications. Healing depends on the cause, severity, and current healing phase.
Unfortunately, chronic wounds represent a significant global concern. These are more common among older adults, diabetic patients, or those with poor circulation. Chronic wounds impose a significant economic burden on healthcare systems worldwide.
Hospitalized patients with wounds range from 2-15%, with higher rates in the ICU or long-term care facilities (4). Beyond the causes discussed previously, other considerations include lifestyle choices, such as poor nutrition and smoking. Another consideration is immunocompromised patients, as this can impede wound healing abilities (5).
By understanding the various types of wounds, their causes, and the associated risks, nurses can make informed decisions on dressing selection, wound management, and patient care strategies to ensure adequate healing and minimize complications.
Ask yourself...
- What role do comorbidities play in the development of chronic wounds?
- How does understanding the underlying causes of chronic wounds help develop a more targeted treatment plan?
Stages of Wound Healing
When preparing for wound care, nurses must review the provider’s orders and understand the approach required for effective management. Understanding key definitions and principles of wound dressings is essential to selecting the proper intervention. A wound is defined as a skin or tissue integrity disruption caused by physical damage.
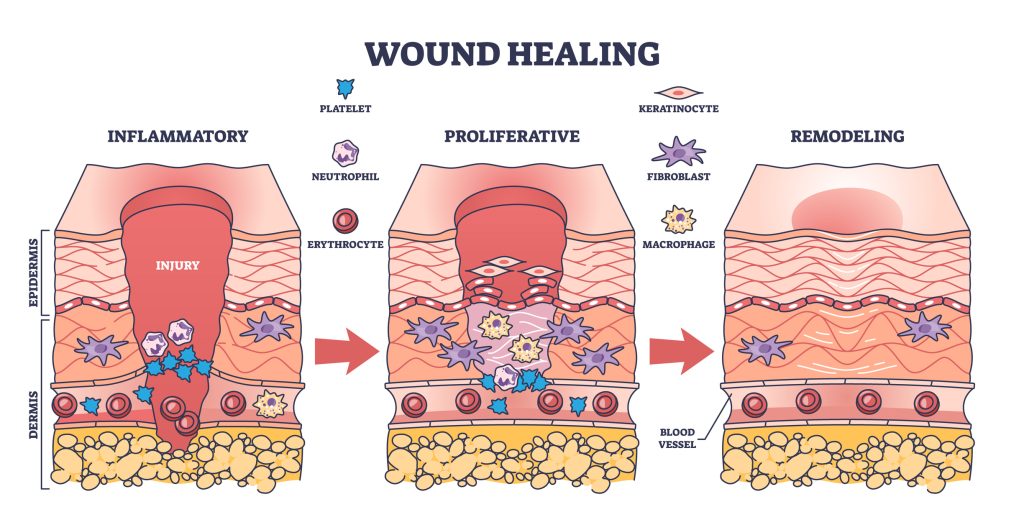
Wound healing progresses through four stages: hemostasis, inflammation, proliferation, and remodeling. Each stage has unique characteristics, requiring careful consideration of dressing type to meet the wound’s evolving needs (3).
During hemostasis, blood vessels constrict immediately after the wound develops to stop bleeding, and a clot forms to prevent further loss. Dressings in this phase focus on maintaining pressure, absorbing exudate, and preventing contamination (3).
The inflammation stage spans from day zero to day four. During this phase, neutrophils and macrophages clear debris and prevent infection, often causing redness and swelling (7). Dressings used here should manage exudate, reduce inflammation, and create a protective barrier against infection (3)
The proliferation stage involves rebuilding the wound with connective tissue, promoting granulation, and facilitating repair. Dressings that maintain moisture, support granulation, and prevent disruption of new tissue are critical in this phase (3).
Finally, the remodeling stage, which can last from day 24 up to a year, focuses on strengthening and reorganizing the newly formed tissue. Dressings in this stage should protect the fragile epithelial tissue and support continued healing in a moist environment (3).
Ask yourself...
- How can understanding the properties of various wound dressings improve nursing interventions across different wound types?
- Why must nurses align dressing selection with the specific stage of wound healing?
Clinical Signs and Symptoms of Wounds
Clinical signs and symptoms of wounds include redness, swelling, persistent pain, warm wound site, put or draining, delayed healing, increased red streak, fever, chills, or swollen lymph nodes (7). Acute wounds may exhibit redness, swelling, pain, and scab formation (2). Chronic wounds, on the other hand, may show different symptoms based on the wound type (7).
Odor and exudate are indicators of wound health and possible complications. The odor may range from mild to malodorous, signaling an infection. Exudate types include serous, purulent, sanguineous, or combination. These provide insight into the wound’s healing stage and possible infection. Assessing these factors helps personalize care plans, select appropriate dressings, and allow early interventions when needed (2).
Exudate, the discharge exhibited from wounds, is another clinical sign that should be examined. Exudate can provide insight into the healing process and expected complications. There are three types of exudates: serous, purulent, and sanguineous. Serous exudate is a clear, watery fluid seen in the early stages of healing. It suggests the wound is in an inflammatory state (6).
Purulent exudate is thick, yellow, or green and contains pus. This can indicate infection is present and should be assessed further. Sanguineous exudate often contains blood and is commonly observed in the initial stages of wound healing. It can also be present after a significant trauma. Unfortunately, this can indicate a disruption in the healing process.
Granulation and epithelialization are other things the nurse should be mindful of, as these can indicate progress or lack thereof. Granulation is the presence of new, pink tissue that is formed from capillaries and fibroblasts. Epithelialization is when skin cells migrate across the wound bed to cover it. A thin layer of epithelial cells will begin to form over the wound as the healing progresses, typically in the later stages of healing (3).
Identifying complications of wounds will be necessary when completing wound care dressings. Some complications that may be present include necrosis, delayed healing, and infection. Necrosis is dead tissue that appears black or brown (6). This can prevent healing and requires debridement (8).
Delayed healing occurs when the wound fails to progress through the expected stage of healing. This can indicate infection, insufficient circulation, or underlying health issues (7). Finally, signs of disease may be present in or around the wound. Increased redness, warmth, swelling, pain, foul odor, or increased exudate (especially purulent exudate) can indicate wound infection (3).
Ask yourself...
- What clinical signs and symptoms should nurses watch to detect infection or complication in chronic wounds?
- How can nurses differentiate between typical signs of healing and indications that a wound may be worsening or infected?
Types of Wound Care Dressings
Wound care treatment is primarily focused on the use of dressings. These are selected based on the wound type, the exudate level, and the stage of healing. The dressing protects the wound, promotes healing, and manages exudate.
There are two dressing types: primary and secondary dressings. Primary dressings are placed directly on the wound bed to maintain moisture, promote autolytic debridement, and protect from external contaminants. These also absorb drainage and rude additional trauma. Secondary dressings are applied over the primary dressing to provide additional absorption, support, or protection (8). These dressings maintain the overall integrity of the wound care plan, as they further support the function of the primary dressing.
Several dressing categories may be prescribed for primary or secondary dressing purposes. First, gauze dressings may be ordered, as they are particularly low cost and can aid in wounds with low exudate. Gauze is available in woven and non-woven forms (1). Next, foam dressings are used for absorbency and maintaining a moist healing environment. Foam dressings can be used for moderate to heavy exudate wounds and reduce the risk of maceration around the wound (1).
Hydrocolloid dressings maintain moisture, promote autolytic debridement, and provide a barrier against bacterial invasion. Hydrocolloid dressings are helpful for wounds with low to moderate exudate and are often used for partial-thickness wounds or burns (1). Hydrogel is another dressing category used to hydrate dry or necrotic tissue. This dressing is appropriate for partial-thickness wounds and burns because of the moisture it can provide, supporting granulation (1).
Alginate dressings are highly absorbent and ideal for moderate to heavy exudate. They are made from seaweed and are commonly prescribed for venous ulcers and surgical wounds (1). Antimicrobial dressings contain silver or iodine to manage infected wounds (1). This reduces the bacterial load and prevents infection.
Silver-infused dressings are beneficial for chronic or infected wounds. Lastly, transparent film dressings are thin, flexible, and waterproof (1). This allows for easy visual access and monitoring while maintaining the barrier. This dressing category is often used for surgical wounds with minimal exudate. It can also be utilized as a securement device for other dressing types, such as gauze.
Regardless of the dressing chosen, debridement is a necessary step to promote healing. Debridement removes non-viable tissue and prepares the wound bed for granulation. Methods include enzymatic, autolytic, and surgical debridement. Nurses must identify the most suitable technique based on wound conditions. This also requires collaboration with the care team to address complex cases (2).
Two other treatment considerations are negative pressure wound therapy (NPWT) and bioengineered skin substitutes. NPWT uses a vacuum-assisted closure device to help draw out excessive fluid from the wound bed (8). This promotes tissue growth and accelerates healing. This treatment is often utilized for more extensive or chronic wounds, such as diabetic foot ulcers (1).
Bioengineered skin substations are used in severe or non-healing wounds. Synthetics or cultured skin grafts provide an essential barrier and promote wound healing (8). This approach aids tissue regeneration and is often prescribed for full-thickness wounds or burns (1).
Ask yourself...
- How can nurses ensure they are selecting the most appropriate wound care dressing for a particular patient’s wound?
- What are the advantages and limitations of advanced wound care therapies?
Factors Influencing Dressing Selection
Choosing the appropriate wound dressing is a critical component of successful healing. Wound characteristics, patient-specific considerations, resource availability, and effectiveness influence selection. Wound characteristics include the size, depth, exudate, and infection status (3).
Of these factors, the primary consideration when choosing a wound care dressing is the wound’s characteristics. For example, a large and deep wound may require an absorbent dressing to manage the expected exudate. Infection status is also a crucial consideration. If the wound is infected, an antimicrobial dressing may be necessary to prevent further complications.
Patient factors may include comorbidities, mobility, and skin sensitivity. While not the primary consideration, comorbidities such as diabetes, peripheral vascular disease, or immunocompromised patients may impact the choice of dressing needed (5). Mobility is another important consideration, as patients who are bedridden or have limited movement may require more secure dressings. Hydrocolloids or foam dressings can withstand friction and shear.
Intrinsic factors like nutrition, chronic illness, and age, as well as extrinsic factors like wound location, mechanical stress, and moisture imbalance, significantly influence wound healing. Addressing these factors through individualized care plans, such as optimizing nutrition or repositioning immobile patients, promotes faster healing and reduces complications. Nurses must consider these items when choosing dressings and planning interventions (2).
Cost and availability of care should be considered when making decisions regarding dressings. Particularly in healthcare settings with budget constraints or regions where certain supplies are limited, cost-effective dressings may be more readily available. The care setting may also impact dressing selection. When a patient is being treated as an inpatient, there is excellent access to dressings and the appropriate personnel to monitor them.
Finding a balance between effectiveness and comfort is a final consideration when determining what to proceed with. A dressing should promote health, but it needs to be comfortable enough for the patient to tolerate it during the healing process. If it is irritating, the patient will be less likely to maintain compliance with wearing the identified dressing.

Ask yourself...
- How does size and depth impact the choice of dressing?
- In what way might a patient’s comorbidities impact the wound care plan?
Evidence-Based Practices for Wound Care
Evidence-based practices (EBPs) are necessary for effective wound care. To improve patient outcomes, a nurse should be aware of various key principles. First, aseptic techniques and infection prevention are crucial in reducing infection risk. This can be accomplished through proper hand hygiene, sterile equipment, and regular wound site cleaning. Antimicrobial dressings and topical agents can be prescribed for high-risk wounds (8).
Maintaining moisture has been proven to improve wound care outcomes, as optimal moisture balance promotes cell migration, reduces pain, and prevents infections (8). Hydrocolloid, hydrogel, and alginate dressings are all designed to maintain this moisture balance. Dressing changes and monitoring help reduce infection and track healing progress. The healthcare team can use proper documentation to align care plan efforts and optimize patient outcomes (3).
Similarly, effective dressing changes require preparation to minimize discomfort and promote healing. Nurses should ensure the environment is clean, the equipment is sterile, and the patient is positioned comfortably. Aseptic technique, appropriate cleaning solutions, and pain management should all be considered. Clear communication with the patient about the procedure can help reduce fear or uncertainty during the wound care dressing change (2).
Ask yourself...
- How does maintaining optimal moisture balance contribute to the wound-healing process?
- Why is it important to use evidence-based guidelines for dressing changes and wound monitoring?
Nursing Interventions
Nursing interventions are vital for wound care. Nursing interventions for this patient population include thorough assessments, tailored treatment, and ongoing monitoring. A comprehensive wound assessment should be completed. This assessment should include size, depth, exudate, infection signs, and progress toward healing. This must be documented accurately and regularly to ensure progression in the patient care plan (9).
The nurse should be prepared to document all the findings from the physical examination. This should include the location of the wound, the cause, the stage of the wound, the depth, length, and width of the wound, the measurements of undermining and tunneling, if present if the wound bed exposure includes bone, vessels, hardware, or subcutaneous fat, the type and amount of exudate, the surrounding skin for integrity, the status of the wound edges, signs of infection, pain, and any other unexpected findings (9).
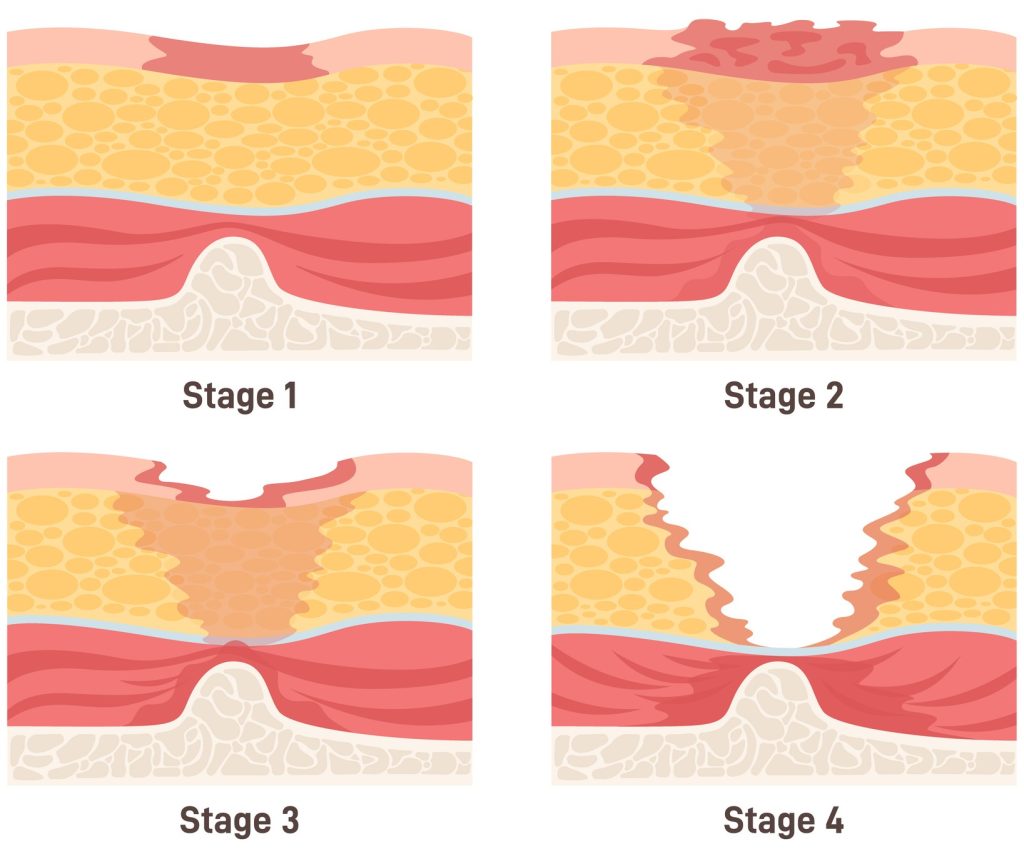
To properly document the stage of the wound, the nurse must understand that a stage 1 wound is considered superficial with intact, non-blanchable skin. Stage 2 is a partial thickness wound that affects the epidermis and may extend into the dermis. Stage 3 is a full-thickness wound that extends through the dermis and into the adipose tissue. Stage 4 is a full-thickness wound that extends through the dermis and adipose and either exposes or extends into the muscle, bone, fascia, and tendon. While not a stage, a fifth option is available: unstageable. This is reserved for full-thickness skin and tissue loss that is obscured by slough or eschar (9).
The nurse can use the acronym TIME to recall what essential aspects must be documented. TIME stands for the tissue, infection or inflammation, moisture balance, and edges. The nurse should identify which type of tissue is present, such as necrotic or granulating, and signs of infection or inflammation, such as warmth and redness. The nurse should also document the level of moisture present, including exudate level and type, and the edge healing stage. Through the TIME acronym, the nurse can accurately document necessary information to track the progression of the patient’s healing goal and support improved patient outcomes (2).
The patient’s care plan should be personalized for their unique needs, underlying conditions, nutrition, and mobility. The nurse must also complete infection control. This includes following strict aseptic techniques, proper hand hygiene, and monitoring the patient for signs of infection. If any signs of illness are present, the nurse should initiate antibiotic treatment and diligent sterilization (9).
Another vital nursing intervention is patient and caregiver education. For patients who are not hospitalized, the patient and caregivers will have the most significant exposure to the wound care dressing. Because of this, dressing basics, the role of nutrition in wound healing, regular movement, and managing conditions. Finally, the interdisciplinary care team approach ensures that all aspects of the wound care plan are addressed. Regular and effective communication ensures comprehensive, adaptive care that enhances the patient’s healing and reduces complications (9).
Lastly, pain is a critical aspect of wound care that influences patient comfort and adherence. Accurate pain assessments before, during, and after dressing changes provide essential information for selecting dressing types and planning interventions. Nurses can use non-pharmacological and pharmacological interventions to minimize pain, ensuring more tolerable and effective care (2).
Ask yourself...
- How can regular wound assessments improve healing and prevent complications?
- What role do patient education and behavioral interventions play in ensuring the success of wound care?
Current and Upcoming Trends in Wound Care
Current research indicates various treatment options are on the rise, including tissue engineering, advanced wound care products, stem cell therapies, and genetic research. Tissue engineering utilizes lab-grown tissues and bioengineered skin to treat severe or non-healing wounds. Advanced wound care products, such as antimicrobial dressings and innovative dressings that change color to indicate infection, are also being developed and researched (9).
Stem cell therapies are on the rise, and use for wound care is no different. Investigating the use of stem cells to promote wound healing and tissue regeneration. Finally, genetic research is also promising for this patient population. Genetics’ role in wound healing rates can aid in personalized treatment for chronic wounds (10).
Advanced wound care technologies like Negative Pressure Wound Therapy (NPWT) and bioengineered skin substitutes have transformed wound management. NPWT accelerates healing by reducing exudate and enhancing blood flow, while bioengineered skin promotes tissue regeneration in severe and non-healing wounds. Incorporating these therapies into care plans enhances patient outcomes, particularly for complex and chronic wounds (2).
Ask yourself...
- How might developing new technologies change the future of wound care practices?
- What ethical considerations should a nurse be aware of?
Conclusion
Wound care is a dynamic and essential part of nursing care. It requires knowledge of various dressings, treatments, and techniques. Nurses play a crucial role in managing wounds, selecting the appropriate dressings, and supporting patients through the healing process. By staying informed about current research and evidence-based practices, nurses can improve patient outcomes and reduce the burden of chronic wounds. Proper wound care promotes faster healing, reduces complications, and enhances patient comfort.
References + Disclaimer
- Labib, A. (2023, July 4). Complex Wound Management. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK576385/
- Armstrong, D. G., & Meyr, A. J. (2024, October 28). Principles of acute wound management. UpToDate. https://www.uptodate.com/contents/principles-of-acute-wound-management
- The Royal Children’s Hospital Melbourne. (2023, February). The Royal Children’s hospital Melbourne. https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Wound_assessment_and_management/#definition-of-terms
- Sen, C. K. (2021, May). Human wound and its burden: Updated 2020 compendium of estimates. Advances in wound care. https://pmc.ncbi.nlm.nih.gov/articles/PMC8024242/
- Nova Scotia Health. (2024, October 29). Libguides: Skin and wound care: Basics of wound healing. Basics of Wound Healing. https://library.nshealth.ca/WoundCare/HealingBasics
- Wilkinson, H. N., & Hardman, M. J. (2020). Wound healing: Cellular mechanisms and pathological outcomes. Open Biology, 10(9). https://doi.org/10.1098/rsob.200223
- Glencoe Regional Health. (2023, August 8). Spot the 8 Signs of A Wound Infection. https://grhsonline.org/touching-lives/spot-the-8-signs-of-a-wound-infection/
- Eriksson, E., Liu, P. Y., Schultz, G. S., Martins‐Green, M. M., Tanaka, R., Weir, D., Gould, L. J., Armstrong, D. G., Gibbons, G. W., Wolcott, R., Olutoye, O. O., Kirsner, R. S., & Gurtner, G. C. (2022). Chronic wounds: Treatment consensus. Wound Repair and Regeneration, 30(2), 156–171. https://doi.org/10.1111/wrr.12994
- Nagle, S. M. (2023, June 26). Wound assessment. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482198/
- Kolimi, P., Narala, S., Nyavanandi, D., Youssef, A. A., & Dudhipala, N. (2022). Innovative treatment strategies to accelerate wound healing: Trajectory and recent advancements. Cells, 11(15), 2439. https://doi.org/10.3390/cells11152439
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
