Course
2024 Washington APRN Bundle
Course Highlights
- In this Washington APRN Bundle, we will learn a nurse’s role in caring for patients receiving medication-assisted treatment.
- You’ll also learn the neurobiological and pathophysiological mechanisms underlying migraines.
- You’ll leave this course with a broader understanding of a non-pharmacological treatment for patients with a history of self-harm.
About
Contact Hours Awarded:
Pharmacology Contact Hours Awarded: 17
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Washington Suicide Prevention Training
Introduction
Defined as a harmful act to end one’s own life, suicide is a mental health emergency (25). In 2021, suicide claimed over 48,000 lives in the United States alone. That is approximately 130 individuals daily, and one life every 11 minutes (8). It is reported that in 2021, 12.3 million American adults considered suicide while 3.5 million made a plan, and 1.7 million made an attempt. Of those that complete suicide, 46% had a known or diagnosed mental disorder (23). In comparing this data to other medical conditions, suicide was the 11th cause of death in the United States as reflected in the chart below (5) [See figure 1].
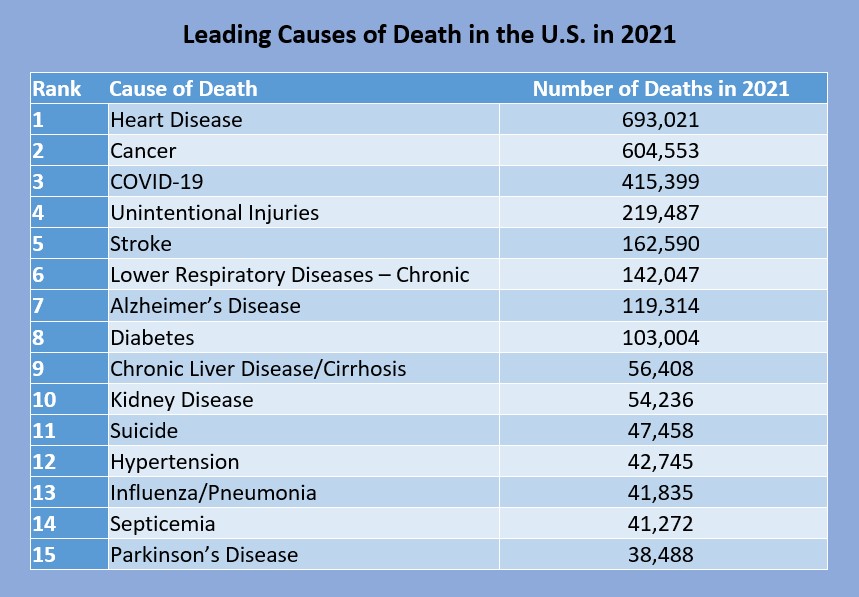
Figure 1: Leading Causes of Death in the U.S. in 2021 (5)
In the United States, Wyoming, Montana, and Alaska all have the highest rates of suicide, over 30 per 100,000 deaths, while New York and New Jersey have the lowest, 7.9 and 7.1 per 100,000 deaths respectively (7). Washington state ranks 27th on this list with 1,229 deaths or 15.3 in the year 2021 (7). Age wise, those 85 years and older had the highest rate of suicide in 2021 at a rate of 22.4 per 100,000. Chart 2 reflects suicide rates among Americans aged 10 to 85+ (7) [See figure 2]. Race and gender must also be considered when discussing suicide. Chart 3 discusses suicide rates based on race [See figure 3], while Chart 4 discusses rates by gender [See figure 4].
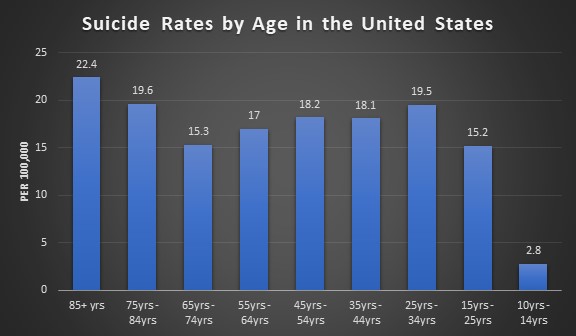
Figure 2: Suicide Rates by Age in the U.S. (7)
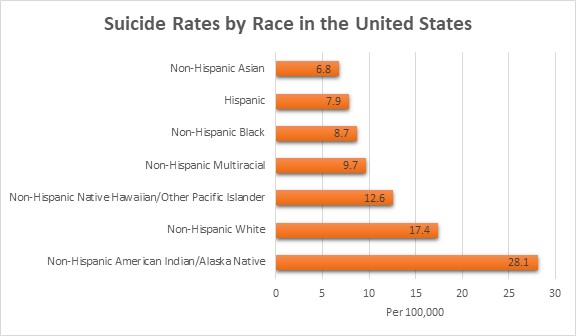
Figure 3: Suicide Rates by Race in the U.S. (7)
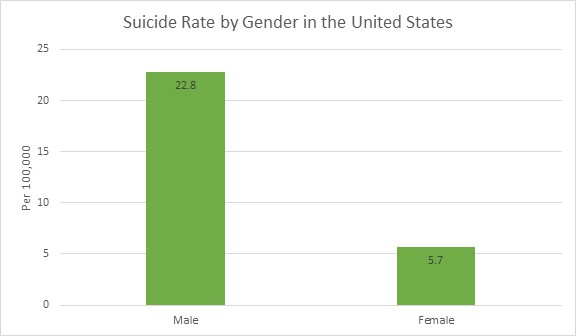
Figure 4: Suicide Rate by Gender in the U.S. (7)
Suicide is a leading cause of death on a global level with more deaths than human immunodeficiency virus (HIV)/ acquired immunodeficiency syndrome (AIDS), breast cancer, war, homicide, or malaria. The World Health Organization reports that an estimated 703,000 individuals die from suicide each year, approximately one in every 100 individuals. However, this number could be higher due to the COVID-19 pandemic and risk factors that were exacerbated during the pandemic: isolation, anxiety, loss of job, and financial stress (40).
Low and middle income countries see higher rates of suicide at approximately 77%. Within the past 45 years, the global suicide rate has increased 60%. For those ages 15 to 29, suicide is the fourth leading cause of death—behind road death, tuberculosis, and interpersonal violence—with it being the third leading cause of death in females and the fourth in males (40).

Self-Quiz
Ask Yourself...
- QUESTION 1
- qUESTION 2
Terminology
Using proper definitions to clearly understand what is being discussed is important when discussing suicide. Providers may use certain words or phrases and mean different things. By having clear definitions that are universally used, providers can understand what other providers are conveying and continue care in an appropriate manner. Below is a list of commonly used terms when referring to suicide.
|
Term |
Definition |
|
Suicidal Ideation |
Thoughts regarding killing oneself or ending one’s life. This can include planning. |
|
Suicide Attempt |
Non-fatal self-injurious behavior with the intent to kill oneself. |
|
Suicide Intent |
Intention to kill oneself by acts of suicidal behavior. |
|
Suicide Behaviors |
A spectrum of behaviors that ranges from planning to attempting/preparing to completing suicide. |
|
Suicide |
Fatal self-injurious behavior to end one’s life. |
|
Suicidality |
A spectrum of possible suicidal events. This does not cover if there was suicidal ideation or attempt or if the ideation or attempt is chronic or acute in nature. It is encouraged that when discussing a patient, clearly cover the actual concerns at hand. Does your patient have ideation, or did they attempt to end their life? |
|
Suicide Threat |
Verbalized thoughts of killing oneself through self-injurious behavior. This is to lead others to think the individual making these statements wants to die without the actual intent to do so. “If you breakup with me, I will kill myself.” |
|
Suicide Gestures |
Self-injurious behavior that makes others think that the individual making these gestures wants to kill themselves, despite them having no intent to. |
|
Non-Suicidal Self-Injurious Thoughts |
Thoughts of partaking in self-injurious behavior that includes deliberate damage to body tissue without an intent to die. |
|
Non-Suicidal Self-Injury |
Self-injurious behavior with deliberate damage to body tissue without an intent to die. |
|
Physician-Assisted Death or Suicide; Aid in Dying; Right to Die |
Passive – a provider supplying the patient with medications to take on their own to end their life |
Table 1: Commonly Used Terms When Referring to Suicide (11, 21, 29)
Suicide Assessment
Healthcare providers perform a variety of assessments on their patients: cardiac assessment, respiratory assessments, neurological assessments, etc. Just as those assessments help providers decide what treatment needs to be done, the suicide assessment is utilized to evaluate a variety of factors that can increase an individual’s risk for suicide.
The latest guidelines from the American Psychiatric Association have clear goals of the suicide assessment: (17)
- Identify any psychiatric signs and symptoms
- Assess past suicidal behavior
- Review any available past treatment
- Determine if there is a family history of suicide or mental illness in the family
- Identify the patient’s current psychosocial situation and the cause of the current crisis
- Recognize strengths or coping skills and any opportunities for improvement that the patient has
With the suicide assessment, there are five areas of questions that the American Psychiatric Association discusses with examples as to what is being looked for in each area (17). These areas can be found below:
|
Current Presentation of Suicidality |
|
|
Psychiatric/Mental Illness |
|
|
Patient History |
|
|
Psychosocial Information |
|
|
The Patient’s Strengths and Weaknesses |
|
Table 2: American Psychiatric Association Suicide Assessment (17)

Self-Quiz
Ask Yourself...
- What goals would you add to the American Psychiatric Association’s list of goals for the suicide assessment?
- Do you think these goals accurately cover suicide assessments? Why or why not?
- Which of the five categories in the suicide assessment do you think is the most important to cover? What is your rationale?
- Are there any questions you would remove or add to the list above?
- If you could create a sixth category, what would it entail?
The Interview: Gathering Information
Conducted in a private place, the suicide assessment is an interview of the patient. Providers must ensure that they ask the right questions based on information provided to them by the patient or those that are accompanying the patient. Empathy, compassion, and trust must be integrated in these interviews. Below is a list of questions that can be used during the interview process. It is important to follow your facility’s specific policies and procedures regarding the suicide assessment and use the proper screening tools. Some common screening tools utilized in healthcare will be discussed later.
|
Open Ended Questions |
In your life, have you ever felt as though your life was not worth living? Have you ever wished to go to sleep and not wake up? |
|
Follow Up Questions |
Have you been thinking about death recently? Has there ever been a point where you have considered harming yourself? |
|
Thoughts on Suicide or Self-Harm |
|
|
Previous Suicide Attempts |
|
|
Repeated Suicide Attempts and Thoughts |
|
|
Psychosis |
|
|
Harm to Other Individuals |
|
Table 3: Suicide Assessment Interview Questions (17)
It is important to keep in mind that the answers to these questions are self-reported, so patients may not be honest for any reason. Providers should pair answers given during the interview with objective data they collect through observation and past medical records. Family, friends, and partners can be a source of information; however, providers should consider collecting information with these individuals separately.

Self-Quiz
Ask Yourself...
- Does your facility have a policy for suicide screening? If so, do you think the policy is effective? Why or why not?
- What methods have you found to be beneficial to asking the above questions?
- What methods are detrimental to asking the questions above?
- What specific questions do you think could be added to the above list?
- How could you rephrase the questions when talking to a family member or friend about the patient?
- What questions, when given the answer “yes”, would warrant more investigation on your part as a provider?
Columbia-Suicide Severity Rating Scale:
Also known as the Columbia Protocol, the Columbia-Suicide Severity Rating Scale was created by Columbia University, University of Pittsburgh, and University of Pennsylvania to be used during a 2007 National Institute of Mental Health study to decrease the suicide risk in adolescents with depression. The Centers for Disease Control and Prevention began using this protocol and recommending it be used in data collection in 2011. The next year, the Food and Drug Administration stated the Columbia Protocol was the standard for measuring and assessing suicidal behaviors and ideation in clinical trials (33).
The Columbia Protocol is used to assist providers and laypersons in determining if an individual is at risk for suicide. These questions are worded in plain language to ensure this scale can be administered by anyone, regardless of profession. This scale questions individuals about the following information: (33)
- If and when they have had any suicidal ideation or thoughts
- Any action they have taken to prepare for suicide and when they have done so
- If they have attempted suicide or started a suicide attempt that they interrupted or someone else did
The image below [See figure 5] is the six-question Columbia Protocol that can be used by anyone in assessing suicide risk. The far-right column is color coded based on severity if they answer “yes” to the question. Yellow is low-risk, orange is medium-risk, and red is high-risk. The answers the individual gives will guide the interventions needed. If the individual answers “yes” to questions two or three, behavioral healthcare should be sought out. If the individual answers “yes” to questions four, five, or six immediate help is needed. Those asking the questions should call the suicide and crisis lifeline, 911, or take the individual to the nearest emergency department. The individual should not be left alone until an evaluation has been done (33).
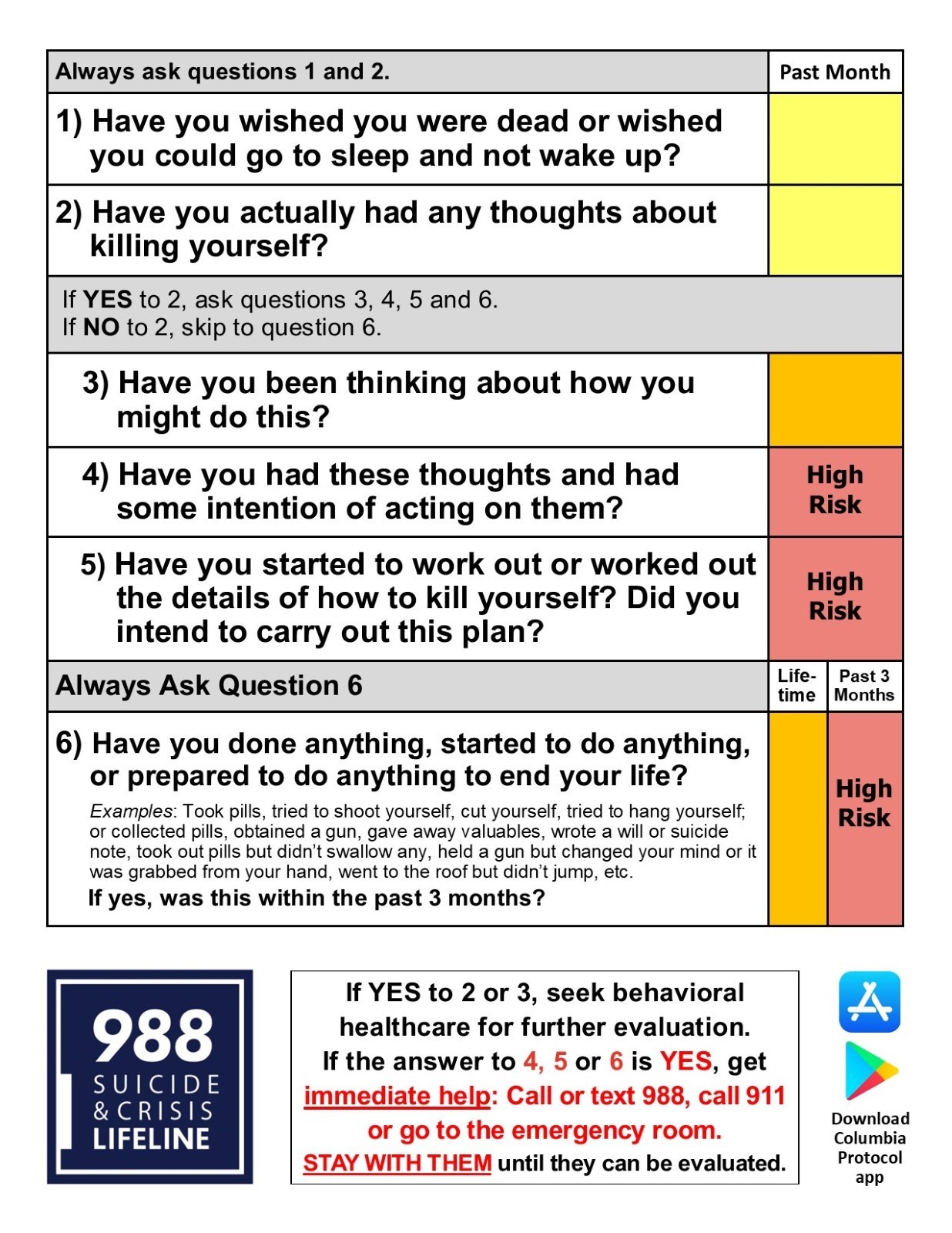
Figure 5: Columbia-Suicide Severity Rating Scale (Columbia Protocol) (33)
Suicide Assessment Five-step Evaluation and Triage:
The Suicide Assessment Five-step Evaluation and Triage consists of five questions that identifies risk and protective factors, risk levels and interventions, suicide inquiry, and documentation of treatment plans. This tool was created by Douglas Jacobs, MD, the physician who assisted in creating the suicide assessment published by the American Psychiatric Association (31). The five questions include:
- Identify risk factors with attention to those that can be modified.
- Identify protective factors and those that can be enhanced.
- Complete a suicide inquiry by asking about thoughts, plans, intent, and behavior.
- Determine risk level and any interventions that are appropriate for the risk level and attempt to reduce risk.
- Document as appropriate to include risk and rationale, interventions, and any follow-up that is needed.
The Suicide Assessment Five-step Evaluation and Triage can be combined with the Columbia Suicide-Severity Rating Scale (C-SSRS) to expand on the benefits of both tools (34).
Questions one through six from the C-SSRS all have an option for “yes” or “no,” If question two is a no, questions three through five can be skipped. After the C-SSRS questions have been asked, further assessment can be directed to precipitating events, clinical status presentation/statements, past treatment history, and any other relevant information. Providers also want to assess for access to lethal means by asking specifically about the presence of firearms in the home or how easy it would be to obtain a firearm (34).
The next step is to identify protective factors the individual has. These can be internal or external factors that the individual has that can provide support. Internal factors can consist of fear of death, or reasons for living while external factors can consist of responsibility to family or friends, supportive social network, or interacting and engaging at work and/or school (34).
Step three is the C-SSRS Suicidal Ideation Intensity screening questions that consists of thoughts, plans, and suicidal intent. Questions focus on frequency of thoughts, duration of how long the individual has had these thoughts, controlling the thoughts, if there is anything that the individual can do to deter the thoughts, and the reason for the suicidal ideation (34).
Ask Suicide-Screening Questions
The Ask Suicide-Screening Questions consists of the Suicide Risk Screening Tool that can be administered in the emergency department, inpatient medical unit, outpatient, primary care, or specialty provider offices as well as schools and juvenile detention centers. All questions are “yes” or “no” with additional open-ended questions if the individual answers “yes” (24) [See figure 6].

Figure 6: Ask Suicide-Screening (24)
The answers provided will guide treatment/interventions. If the individual answers “no” to questions one through four, no intervention is needed. If they answer “yes” to any of the questions, question five must be asked since the individual is said to have a positive screen. If question five has a “yes” response, an imminent risk is identified, or they are an acute positive screen. The patient needs a safety or full mental health evaluation before they are able to leave. Immediate interventions that must be considered are keeping the patient in eyesight at all times, removing items that could be used to harm/kill self or others, notify the provider that is responsible for the individual’s care (24).
You may wonder what to do if the individual answers “yes” to any of questions one through four but does not answer “yes” to question five. This means the individual is a non-acute positive screen and there is a potential risk identified. A brief suicide screen must be done in order to determine if a full mental health evaluation needs to be completed. The individual is not allowed to leave until they have been assessed for safety, and the provider must be notified (24).
Depending on where the individual is when asking these questions, there are some additional questions that need to be asked regarding safety and safety plans. The links below will take you to the safety screening tools based on the location of the individual being assessed (24).
Emergency Department Suicide Safety Assessment
Outpatient, Primary Care Provider, Specialty Provider Office
Patient Health Questionnaire
Since depression is often a risk factor for suicide, the Patient Health Questionnaire (PHQ-9) is used to measure, screen, monitor, and diagnose depression severity. This screening utilizes diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders 4th edition and rates the frequency of the individual’s symptoms. Question nine focuses on the presence and duration of suicidal thoughts while a non-scored question assigns and screens how much depression is affecting the individual’s activities of daily life and function. The minimum score is five while the maximum is 27. Anything greater than 20 has a provisional diagnosis of major/severe depression with a treatment recommendation of antidepressants and psychotherapy (27) [See figure 7]

Figure 7: Patient Health Questionnaire (PHQ-9) Results Interpretation (27)
The screening answer options include: not at all = 0, several days = 1, more than half the days = 2, and nearly every day = 3. The questions are as follows: (27)
- Little pleasure or interest in doing things
- Feeling hopeless, depressed, or down
- Difficulty sleeping, staying asleep, or sleeping too much
- Having too little energy or feeling tired
- Overeating or a poor appetite
- Feeling bad about yourself, or that your family sees you as a failure or that you have let them down
- Having difficulty concentrating on things, like reading a book or watching a movie/television
- Either being too fidgety or restless or moving/speaking slowly that you and/or others notice
- Thoughts that you would be better off dead or thoughts of hurting yourself
- Non-scored question: If you selected any of the above problems, how difficult have those problems made it for you to complete work, get along with family, friends, or manage things at home? (Answers options include: not difficult at all, somewhat difficult, very difficult, extremely difficult).

Self-Quiz
Ask Yourself...
- What other suicide screening or assessment tools have you seen utilized?
- Is there a specific tool you prefer? Which one and why?
- Have you heard of any up and coming assessment tools that may be more effective than the ones listed here? What is the name of the tool and what does current research show?
- Would you feel comfortable using these assessment tools on friends or family you are concerned about? Why or why not?
- If you did assess a family or friend for suicide and it was positive, how would your reactions vary than if you performed the same assessment on a patient?
Suicide Risk, Protectives Factors, and Warning Signs
Risk factors for suicide can appear in a variety of ways: individual, relationships, community, society. These are factors that increase an individual’s risk for suicide through different means. For example, stay at home orders and quarantining during the initial phases of the COVID-19 pandemic led to isolation, which is a risk factor of suicide. Combining this with other risk factors increases the chance of an individual taking action to end their life (6).
|
Characteristic |
Low Risk |
High Risk |
|
Gender |
Female |
Male |
|
Age |
Less than 45 years old |
Greater than 45 years old |
|
Marital Status |
Married |
Widowed or divorced |
|
Interpersonal Relationships |
Stable |
Unstable/Conflict |
|
Employment |
Employed |
Unemployed |
|
Background of Family |
Low substance use, family feels healthy, they have good health |
Excessive substance use, hypochondriac, chronic illness |
|
Mental Health |
Normal personality, social drinker, neurosis, mild depression, optimistic |
Severe personality disorders, substance abuse, severe depression, hopelessness, or psychosis |
|
Physical Health |
Low substance use, individual feels healthy, has good health |
Excessive substance use, hypochondriac, chronic illness |
|
Suicidal Ideation |
Low intensity, infrequent, transient |
Prolonged, intense, frequent |
|
Suicidal Attempt |
Impulsive, first attempt, wishing for change rather than the wish to die, low lethality method, has external anger, rescue is inevitable |
Multiple attempts, planned out, has a specific wish to die, is self-blaming, done with lethal methods, has a specific wish to die |
|
Personal Resources Available |
Controllable, has good achievement, is insightful |
Has poor achievement, unstable affect, has poor insight |
|
Social Resources Available |
Has good rapport, they are socially integrated, has a concerned/supportive family |
Are socially isolated, family is unsupportive/unresponsive, has a poor rapport |
Table 4: Criteria for Low and High Suicide Risks (3, 4)
Gender
Per research, men are four times as likely to die as a result of suicide as opposed to women. This is regardless of religion, marital status, or race. However, women are three times as likely to have thoughts of suicide and/or attempt suicide than men. Research deducts that this is because the differences in attempt methods between women and men (3). Studies show that 30% of transgender youth in the United States have attempted suicide in their lifetime while 40% of adults who identify as transgender have attempted (15).
Age
Suicide rates increase with age. Individuals who have not gone through puberty are very unlikely to attempt or die by suicide as opposed to those that have gone through puberty. Age 45 is when suicide rates are the highest among men while it is highest in women after 55. Those over the age of 65 or who are considered elderly are less likely to attempt suicide, but they are more successful when they make an attempt. As we pointed out earlier, suicide is increasing among the young population: it is the third leading cause of death among individuals aged 15-24 (3).
Marital Status
Individuals who are married and have children have a lesser likelihood than their single counterparts. Those that are single or never married have a risk two times higher than those that are married (8). Divorce suicide rates in men are three times more than women. Some individuals may attempt or die by suicide on the anniversary of a loved one’s death (3).
Sexual Orientation
Homosexual and heterosexual individuals have differences in suicide rates. Those that identify as homosexual, regardless of marital status, do have higher rates of suicide (3).
Race/Ethnicity
Caucasian individuals, regardless of gender, are three times more likely to die by suicide as opposed to African Americans. Young Alaskan Natives or Native Americans have higher than the national average rates of death by suicide (22). Moving on to immigrants, the rates are much higher than citizens of the United States (40).
Religion
Many religions have negative views on suicide. Despite that, religious groups such as Protestants and Jews have higher rates of suicide than Muslim and Catholics combined. It is important to note that religion alone is not an accurate indicator of suicide, but the inclusion and societal integration and beliefs are better predictive factors (3).
Occupation
Increases in socioeconomic status increase the risk of suicide in any individual. It is noted that being employed is one protective factor, and while true, there are some occupations that increase the risk. Lawyers, healthcare providers, mechanics, artists, and insurance agents are classified as high-risk occupations. On the other hand, unemployment brings an increased risk of suicide in comparison to those that are employed. Providers should be aware that suicide risk increases during economic depressions and decreases during economic booms (3).
Physical Health
Good physical health is vital to good mental health and wellbeing as poor physical health contributes to at least half of all suicides. Thirty percent of those who died by suicide saw a provider within the past six months prior. Physical effects that increase risk factors include disfigurement, loss of mobility, and chronic pain. If these effects impact the individual’s relationships and/or work life, that can increase suicide risk even more (3).
Mental Health
Almost 95% of those who die by suicide have at least one diagnosed mental health disorder. Depressive disorders like major depressive disorder account for 80% of all suicides, and a diagnosis of delusional depression comes with the highest risk of suicide. Those with schizophrenia have a 10% risk, while those with delirium or dementia have a 5% risk of suicide. Alcohol dependency is found in over one fourth of suicide cases (3).
Substance Abuse
As mentioned earlier, alcohol or other substances can play a large factor in suicide. The use of any substance can lead to impairment of judgement, sedation, or manic behavior that can lead to respiratory depression or self-injury (19).
If there is a suspicion of substance abuse, it is important to consider discussing these concerns with patients in a non-threatening, non-judgmental manner (19). Providers should start with questions regarding socially acceptable habits: exercise or dieting, caffeine, and tobacco can help ease the patient into comfort. This is something that should be done as standard procedure for all patients, and providers can even say that to patients. “We ask these questions to everyone.” Providers need to ask questions such as “how many”, “how much”, “how often” to any “yes” answer the patient provides (37). Below are common substances that are abused:
- Alcohol: While alcohol is legal to consume for those over the age of 21 in the United States, patients may still be hesitant to answer truthfully. Providers must take patients at their word but make note of any objective data that they gather through their assessment. Appearances of patients who may have a substance abuse disorder will be discussed later. It is important to ask about specific alcoholic beverages as some cultures may not consider beer or wine to be alcohol (37).
- Over-the-counter medications: These medications can be a source of intentional or unintentional substance abuse, so providers must ensure that they are asking about herbal supplements, cold and cough medications, or diet aids. Prescription medications might be prescribed to the patient or someone else and usually consists of sleeping aids, pain medications, diet medications, or attention deficit (hyperactive) disorder medications (37).
- Cannabis/Marijuana: Cannabis or marijuana use has various levels of legality in states across the United States, so providers should be aware of their state’s rules and regulations regarding its use. Regardless, it is important to screen for usage during any patient interaction as treatments can be affected (37).
- Illicit Drugs: Illicit or street drugs consist of cocaine, heroin, methamphetamine, inhalants, hallucinogens, and more. Asking about use of the substances is important, and again should be done in a non-judgmental manner. Methods include saying the name of each substance as opposed to calling them illegal or street drugs are a great way of doing this. Providers need to assess the amount, method of usage, if patients are doing these substances with someone who they consider safe, if they have access to Narcan, if they are buying from the same person, and if they are sharing needles, or using dirty or clean needles (37).
Knowing the patient’s own view of their substance use can be very helpful. If the patient does not see their usage as a problem or reason for concern, they are less likely to seek out help or accept it. The same goes for consequences (19). Below is a table of tools providers can use to screen for substance abuse in adults and adolescents (32) [See figure 8].

Figure 8: List of Substance Abuse Screening Tools for Adults and Adolescents (32)
As mentioned above, patients may not be completely honest when providing substance use history. Providers need to collect both subjective and objective data to assist them in providing the proper care.
Patients may vocalize thoughts of continuously thinking about the substance they are using. They might forget things or have a hard time focusing or concentrating. If they are aware or know they are abusing a substance, they may be unable to stop regardless of a physical and/or mental challenge that is a result of the substance (19).
There may be reports of strong cravings to use the substance. Patients may report a desire to decrease use of the substance, stop using it all together, or they may take actions to obtain the substance that leaves them feeling guilty or remorseful. Depending on the substance used, the patient may report changes in mood or mood swings (19).
Behaviors may vary from patient to patient, and the type of substance they are using. They may dedicate extensive amounts of time to obtain the substance, neglect important tasks or individuals within their lives, or actively appear intoxicated. They may argue or get in trouble with family, friends, or law enforcement. They may take the substance when it is hazardous to the health and safety of themselves and others. They may also start taking the substance in higher doses for longer than recommended (19).
The physical appearance of the patient can consist of noticeable changes in weight, bloodshot eyes, increased tolerance for a particular substance, constricted or dilated pupils, or irregular sleep patterns. Patients may also have signs of withdrawal that consist of shakiness, sweating, agitation, headaches, nausea and/or vomiting, fatigue, and possibly seizures (19).
Stigma
Stigma is known as negative thoughts that are held towards other individuals, groups, or circumstances (19, 30). Usually stigma stems from differences. Differences can encompass any part of life, ranging from clothing to gender to race to medical or mental health diagnoses. Stigma impacts how society addresses those differences. If most of society sees mental health and suicide as shameful, those that have mental health diagnoses or have attempted/thought of suicide may be less likely to seek help—this is social stigma. Those with mental health diagnoses may have self or perceived stigma. These individuals internalize society’s opinions or their own perception of discrimination (30).
Traumatic Childhood
Traumatic childhood events such as sexual abuse are directly linked to increased risks of suicide or suicide attempts. It is vital that healthcare providers assess children and adults for this history to assist with appropriate treatment and support in order to decrease risks and guide the individual to recovery (19).
Genetics
Recent studies have discovered a locus in the form of a DNA variation on chromosome seven that can increase an individual’s risk for suicide. Other variations in this region can lead to risk-taking behaviors, smoking, and insomnia. This variation was present even after “conditioning on major depressive disorder.” The locus has been deemed to be independent from psychiatric diagnoses as well, meaning that those without a mental health disorder could still be at risk for suicide attempts or suicide if this variation is present (22).
General/Other Risk Factors
There are other general risk factors that can impact an individual and their risk for suicide. The Centers for Disease Control and Prevention rank these risks from individual risk factors to societal risk factors and describes them: (6)
- Individual Risk Factors: serious or chronic illness such as chronic pain, previous attempts of suicide, criminal and/or legal problems, substance use, history of mental illnesses like depression, feelings of hopelessness, job or financial loss or problems, current and/or prior history of adverse childhood experiences, and victim of violence or perpetration.
- Relationship Risk Factors: family or loved one having a history of suicide, social isolation, loss of relationship, bullying, and violent or high-conflict relationships.
- Community Risk Factors: stress of acculturation, historical trauma, violence in the community, discrimination, lack of access to healthcare, and cluster of suicide within the community.
- Society Risk Factors: stigma regarding seeking help for mental health or mental illness, unsafe/inaccurate medical portrayal of suicide/self-harm, and access to lethal means in populations at risk for suicide.
Protective factors are those that improve mental health and provide support to the individual. These can range from individual to societal levels of protection. It is important to know that everyone can participate in preventing suicide within their relationships, communities, or society through equal support (6). Below are some protective factors: (6)
- Individual Protective Factors: strong sense of culture, reasons for living (like friends, family, pets, etc.), effective coping skills, and effective problem-solving skills.
- Relationship Protective Factors: partner, family, and friend support, and having or feeling a connection to others.
- Community Protective Factors: feeling a connection to school, work, or community, and having consistent and high-quality mental and physical healthcare.
- Society Protective Factors: reducing the access and availability of lethal means to those that are at a higher risk of suicide, and religious, moral, or cultural objection to suicide and/or suicide attempts.
Case Study Reflection
Below is a case study divided into three parts. This case study will take you through a scenario and ask questions about what should or should not be done with this patient based on the information that has been covered so far (6).
Case Study Reflection 1
Noelle has lived in your neighborhood for years and is one of your favorite neighbors. She would sometimes watch your children when they were young and worked as a waitress until she retired recently. She mentioned to you once, shortly after her retirement, that her funds are “not what they used to be” as she is relying on her social security’s fixed income. This forces her to budget more than she ever needed to, and she is contemplating finding a job. However, her knee pain has been getting worse, keeping her from moving around and sleeping. You notice she doesn’t garden like she used to. One day when you stop by, you ask her about her children, who you have not seen visit. She tells you they are busy, but she would like to see them because she is lonely. She appears restless and sullen.

Self-Quiz
Ask Yourself...
- What are some of the factors that put Noelle at an increased risk for suicide?
- What follow-up questions could you ask her?
- Is there anything concerning you at this moment? Why or why not?
- Would you want to use any of the suicide assessment tools listed in the course at this time? What is your rationale?
- What are your next steps to help Noelle and possibly decrease her risk of suicide?
A few days later, you realize you have not seen Noelle outside of her house, nor have you seen her two dogs. Since you know her children, you call the older son to reach out and see if he has spoken with his mother. The son sounds rushed on the phone and says they only talked for a few minutes the day before. Deciding to call Noelle yourself, you are surprised that she answers the phone. She again reiterates that it is hard for her to move and leave the house because of her knees and age. She says that she is lonely. You state you would like to check on her every day for a few days, but she adamantly declines. “I just get irritable around people,” she tells you.

Self-Quiz
Ask Yourself...
- Would you say that Noelle is better or worse than before? What evidence do you have to support your answer?
- How could you intervene to offer Noelle support?
- Who else could you get involved with when it comes to ensuring Noelle’s safety?
- Would you like to perform a suicide risk assessment on Noelle? Which one would you use?
- Do you think Noelle needs to be assessed by a trained professional? If yes, what provider do you think would be helpful?
The day after your conversation with Noelle, you go to check on her as you are still concerned. When you knock on the door, no one answers, but you know someone is home because of the noises coming from the house. You are able to enter her house through the patio, something she had given you permission to do in the past, and you can now hear her dogs barking continuously. After calling for Noelle and not receiving an answer, you head upstairs to her room. You find Noelle in bed with an empty bottle of prescribed pain medication that she uses for her knees. She seems to be “out of it” but is crying and muttering that she “can’t do this anymore.”

Self-Quiz
Ask Yourself...
- What is your first priority with providing care for Noelle?
- What information should you provide to first responders when they arrive on scene?
- Looking back on the situation, is there anything that could have been done differently by all parties involved to prevent Noelle from getting to the point where she attempted to take her life?
- What can you and your other neighbors do for Noelle while she is being evaluated?
- Are there any support methods you can offer Noelle when she returns home?
Non-Suicidal Self-Injury
As discussed earlier, self-injury can either be non-suicidal or suicidal in nature. Those who perform non-suicidal self-injury are not looking to end their lives, but instead are trying to escape emotions, thoughts, or other feelings that are causing distress (i.e., not being good enough; feeling anguish, despair, desperate, or depressed; needing a way to relieve stress; believing that people do not care). Physical pain is created through a variety of means, including cutting, burning, biting, scratching, pulling out hair, kicking or punching objects to injure self, or snapping rubber bands on their bodies (19).
To determine if the injury is related to a suicide attempt or not, providers must perform a suicide assessment and discuss actions and behaviors with the patient in a non-judgmental manner. It is important to remember that non-suicidal self-injury is a coping mechanism for individuals, and it may be the last coping mechanism available before an individual makes a suicide attempt. Providers need to refrain from preventing self-injurious behavior until they provide the patient with other coping mechanisms. Always follow facility policy and procedures when addressing non-suicidal self-injury (19).

Self-Quiz
Ask Yourself...
- What methods of non-suicidal self-injury have you seen individuals use?
- How did you assist these patients in gaining better coping skills?
- What barriers did you face?
- Were there any successes in helping the patient(s) gain better coping skills?
- What recommendations would you give others trying to help their patients refrain from non-suicidal self-injury?
- Are there any reasons you think someone would not want to stop their behavior?
Understanding the Risk of Suicide: Using Assessment Information
As discussed, suicide has many risk factors, one of which is past suicide attempts. Studies have shown this correlation to be more serious than previously thought, with higher rates of a second attempt within the first three months of the first attempt. What does this mean? As providers we should be providing more support during that initial post-attempt phase to ensure patients have better coping skills and resources to decrease the chances of another attempt.
The provider must look at a variety of factors gained during the suicide assessment interview such as any previous self-harming behaviors, suicide attempts, and/or aborted attempts (stopped by themselves or someone else). If you are not the patient’s regular provider, consider consulting their primary care provider or psychiatric provider to assess past history of suicide (3).
Previous hospitalizations for suicide attempts and/or past psychiatric treatment provides important information to the provider that they should be aware of. Consulting with the patient, family, or friends can provide valuable insight into the patient’s history and coping skills (3). Patients may have a history of agitation, anxiety, depression, feelings of hopelessness, changes in mood (which can be severe), insomnia, or substance use (19).
Family history and dynamics can impact a patient and be a factor for suicide, either a risk or preventative. Dysfunctions within the family have a direct link to suicide and self-injurious behaviors. Providers should ask about family history regarding mental health and illnesses as well as family dynamics. Separations, family history of substance abuse, legal or financial trouble, abuse, or domestic violence should be documented and reported as required by law (3).
Assessing the patient’s presentation at the time of the interview is vital and can provide significant objective data on the patient’s psychological status. Providers should ask questions about current stressors in their lives: financial hardships, interpersonal loss, or changes in their economic status. As already discussed, loss of job or residence, family dynamics, religious beliefs, and cultural customs can impact the patient as well (3).
Determining strengths and areas for improvement will guide the provider in providing support, treatment, and referrals as care progresses. These traits may include coping skills, support (from family, friends, religion, or community), personality, and methods of thinking or solving problems. It is important that patients are guided to adjust their thought processes, such as mentalities and self-expectations, that can be detrimental to mental health (3).
Case Study Reflection 2
Marc is a new patient at your organization, who recently relocated to Washington from Wisconsin for a new job. He has moved to your city with his wife and young children. While talking with Marc, you can tell that the move has not been easy on him while his family seems to be settling in well. He makes a comment about “feeling inadequate at work” because everyone has expectations for him despite the fact that he is new to the company and role. He reports that he does not feel a sense of community where he lives, saying that the city he came from was much friendlier and warmer.
You note that Marc does not mention any current coping skills, but you do identify that he used to bike-ride to de-stress after work. The environment is different for him, and he has different work hours with the new position, making it challenging for him to find time or energy to bike. Marc says he thinks that relocating was not the right decision for his family as he has barely any time for them and less time for himself. He says he is a failure.

Self-Quiz
Ask Yourself...
- What is your priority when assessing Marc? What is your rationale for that decision?
- Are there any additional questions you would like to ask Marc?
- What are some of Marc’s strengths?
- What areas for improvement do you see in Marc?
- What are at least three coping mechanisms that Marc can use or develop to assist him during this transition?
- What are other coping strategies that Marc could develop?
Suicide Risk: Documentation
Documentation of the patient’s suicide assessment is a vital part of the provider’s job. Based on the hospital or facility’s policies, providers might document a suicide risk assessment each time they encounter the patient. Ensure that you are following proper policies and procedures regarding when a suicide risk assessment should be documented. Some best practices include documenting during the first inpatient hospitalization or the initial psychiatric assessment, when there is a significant change, and when there is an occurrence of suicidal ideation or behavior (3).
Providers should consider documenting the following: (3)
- Any changes in treatment
- Risk assessments
- Prescription medications
- Previous treatments, especially regarding past suicide attempts
- Decision making processes
- Conversations with other providers
- The patient’s access to firearms
Actions and Referrals for the Various Levels of Suicide Risk
Patient statements and actions guide the actions and steps a healthcare provider must take. If a patient has attempted suicide, admission to a hospital to treat any medical injuries is the first step, followed by admission to an inpatient behavioral health unit or hospital. Some facilities may have psychiatrists or clinical psychologists see the patient when they are on the medical floor, so both types of treatments can occur simultaneously. Individuals who may benefit from an inpatient psychiatric admission include those who have acute suicidal ideation with previous attempts, previous suicide attempts with no suicidal ideation (but has other psychiatric concerns), or an exacerbation of a mental illness. Individuals who would benefit from outpatient services include those with suicidal ideation or strong support systems (3).
|
Treatment |
Characteristics |
|
Inpatient Treatment – Required |
After an aborted suicide attempt or suicide attempt if:
|
|
Inpatient Treatment – Might be Considered |
If there is a presence of suicidal ideation along with:
|
|
Outpatient Treatment – Recommendation |
Post suicide attempt, or the patient has suicidal ideation or a plan:
|
Table 5: Suicide Attempt Criteria for Recommended Treatment Services (3)
While some patients may agree to inpatient treatment after a suicide attempt, others may not. The state of Washington has an Involuntary Treatment Act that manages the psychiatric hold. For additional information, review Title 71.05 of the Revised Code of Washington (39).
Per Washington legislation, any individual that has firsthand knowledge of an individual they are concerned about can refer them for an evaluation that must be completed by a trained professional such as a psychiatric nurse practitioner or a psychiatrist. The following two points meet the criteria for involuntary admission: (39)
- The individual must have a diagnosed or diagnosable mental health disorder. This is defined as an organic, emotional, or mental impairment that severely impacts the individual’s volitional or cognitive behavior.
- They present with harm to others, property, or self, or the patient is classified as gravely disabled (unable to care for themselves safely).
The trained mental health provider can make a determination if the patient meets the criteria, and if they do, they can initiate a 72-hour involuntary hold. After this hold is initiated, the patient will be transferred to a psychiatric hospital or receiving facility to receive the appropriate treatment. It is important to remember that patients under these holds still maintain their individual rights while in the facility and are presumed competent. This places the patient in a confidential status (39).
Once the 72 hours have passed, the patient can request legal counsel and be evaluated by the court if they continue to refuse voluntary treatment. Psychologists typically evaluate the patients by performing independent exams to determine if the patient still meets the criteria for involuntary placement. The patient and the legal counsel (who is representing the patient) will meet and discuss the patient’s desires in a Probable Cause Hearing (39).
In this meeting, the judge will determine if there is probable cause for the patient to continue treatment on an involuntary placement. During the hearing, the following four decisions can be made (39):
- Involuntary petition is dropped, and the patient is released.
- The case is dismissed by the judge, resulting in the patient being released.
- The patient can make the decision to stay voluntarily.
- The patient can be ordered by the judge to continue involuntarily placement and can stay at the facility for 14 additional days.
If a patient is ordered to stay at the facility for 14 additional days and the provider believes that additional treatment longer than 14 days is needed, a 90-day petition can be filed. This will lead to another hearing where the judge can agree or disagree with the petition. An agreement of the petition would lead to the patient being transferred to the Western State Hospital for adults or the Fairfax Hospital for children (39).
Case Study Reflection 3
Jack is a 19-year-old teenager who has just been admitted to your unit following an overdose of prescription medications. It is unclear from the emergency department notes if his actions were accidental or not, and today is your first day speaking with him. He tells you that he was in a car accident last year and has been having a hard time ever since. Past medical history reports depression and feelings of hopelessness. When you ask him about what brought him to your facility, he admits to you that he was trying to end his life. Jake tells you he has seen a provider in the past but does not feel like they listened to him.

Self-Quiz
Ask Yourself...
- Who should you notify regarding the information that the patient disclosed to you?
- What precautions do you think you should take?
- How can you help Jake during his time on your unit?
- What type of treatment do you think Jake needs after he has been cleared medically?
- Do you think Jake will agree to further treatment? What is the rationale?
- If Jake does not agree to treatment, what would be the next steps? What if he does agree to treatment?
Management and Treatment
Within any healthcare setting, the provider and patient must develop a therapeutic rapport or alliance to ensure that the relationship is productive and respectful. Trust should be a key factor in these relationships. If the patient cannot trust the provider, then they may not wish to disclose personal information that could aid the provider in treatments and care. The opposite can be true as well (17).
Patient safety must be a concern at all times during the provider/patient relationship. If there is concern for the safety of the patient at any time, the proper assessments should be performed, and professional staff should be notified (17).
Together with the patient, the provider needs to create an effective treatment plan for the patient with a focus on the treatment setting, proper education for the patient and their family or other support, and care coordination with other providers. Treatment should be the most beneficial but least restrictive (17).
Non-Pharmacological Interventions and Treatments
Cognitive Behavioral Therapy
The Department of Veteran Affairs recommends the use of suicide-focused cognitive behavioral therapy (CBT) with patients who have a recent history of self-harm or injury (35). Overall, this type of treatment can be beneficial for patients with diagnoses including anxiety disorders, depression, eating disorders, severe mental illness, alcohol and other substance abuse disorders, and even martial problems. The basis for CBT is built on the following three core principles: (2)
- Psychological behaviors can be a result of learned patterns of negative behavior
- Psychological behaviors can be a result of unhelpful ways of thinking
- Those who have psychological diagnoses can learn and develop better coping mechanisms that may help in being more effective in daily life and relieving the symptoms they are experiencing.
Changes in thinking patterns can be attained by training individuals to recognize alterations in their thinking that might create problems in their life. Changes can also occur when the training focuses on reframing an individual’s thinking, which may occur through reevaluating the thoughts realistically rather than based on negativity. Patients can look into obtaining a better understanding of how others are motivated or behave. Problem solving skills can be taught or expanded to help patients cope. Providers can promote role play (to prepare for particular situations), teach patients mind and body relaxation techniques, or encourage patients to face fears rather than avoid them. Patients and providers can work together to come up with the best method to implement CBT (2).
Dialect Behavioral Therapy
Those with recent self-injury or harm as well as borderline personality disorders can benefit from dialect behavior therapy (DBT) (35). It can also be used for those with depression, anxiety, eating disorders, and post-traumatic stress disorder. A type of talk therapy, DBT helps patients accept the reality of their lives and behaviors with the goal to help change the unhelpful behaviors and ultimately change their lives. This is beneficial in many conditions as it focuses on addressing the negative coping skills used to manage negative emotions. Patients may participate one-on-one with the provider, or they may enter DBT group therapy to advance skills gained in one-on-one sessions (10).
Other Psychotherapies
Interpersonal Therapy – helps patients understand interpersonal problems such as conflicts with family or friends, difficulty relating to others, unresolved grief, and changes in work or social roles. This type of therapy assists patients to learn healthier ways to cope and express themselves through effective communication (3).
Psychodynamic Therapy – used with adults to reflect on childhood and other past experiences in order to bring to light some emotions, feelings, thoughts that may have been suppressed. Patients may have developed patterns that can be deemed unhealthy, and this type of therapy can help change those unhealthy coping strategies. Psychoanalysis is a more in-depth form of psychodynamic therapy that is held several times a week (3).
Supportive Therapy – used to support patients in developing their own coping strategies and resources. This process can be used to build self-esteem, improve community and social interactions, and reduce anxiety (3).
Pet, Play, and Creative Art Therapy – can be used in combination with any of the above therapies.
Case Study Reflection 4
Sabrina and her mother come to your outpatient facility for a routine medical visit. Sabrina started high school and wants to join the lacrosse team, so she needs a physical in order to participate. During your assessment you notice that she has lost a significant amount of weight. When her mother steps out of the room, you ask her how she is doing. Sabrina reports that she has been in the nurse’s office more often with stomachaches and nausea. She also reports she fainted in class but was able to convince the school to not call her mother. She tells you that she would like to talk to her mother about all of the stress with school she is experiencing though she is not sure how.

Self-Quiz
Ask Yourself...
- What would you initially diagnose Sabrina with? Provide your rationale.
- How could you discuss your concerns with Sabrina in a non-judgmental way?
- Are you concerned for Sabrina? Would you screen her for suicide ideation at this time?
- Are you obligated to disclose the information you gathered to her mother? Why or why not?
- Since Sabrina wants to talk to her mother about her worries and stress, how can you facilitate a conversation between them?
- What types of psychotherapy would you recommend to Sabrina?
Medical Treatments and Interventions
Providers need to be aware of medications that can cause or exacerbate depression in patients and increase the risk of suicide. While the list is not all inclusive, some common medications include calcium channel blockers, sedatives, corticosteroids, beta-blockers, H2 blockers, and chemotherapy agents. After a suicide attempt, the provider should assess all medications and diagnoses the patient has. From there, the providers should decide if adjustments should be made (3).
As discussed previously, depression is a major factor in suicide and is present in many other medical and mental health conditions. Anxiety (includes general phobia, specific phobia, generalized anxiety, obsessive compulsive, social anxiety, agoraphobia without panic, and panic disorder), trauma/stress related disorders, bipolar disorder, psychosis, eating disorders, substance use disorders, and non-suicidal self-injury can all have depression as a symptom (19). Medical conditions that co-exist with or exacerbate depression consist of cancer, heart disease, dementia, diabetes, Parkinson’s Disease, and stroke (3).
Medication
The goal of medication administration is to assist the patient to regain balance in their brain’s chemistry and restore it to optimal functioning by controlling the signs and symptoms the patient may have. These medications do not usually result in a cure; instead, they should be taken for extended periods of time, possibly for the patient’s lifetime. These medications can also be combined with other treatment options to give the patient the best possible outcomes (3).
Controversy exists with patients taking antidepressants. In 2004, the Food and Drug Administration made the decision to require that antidepressants have a black box warning addressing increased risks of suicide in young adults. There was a similar claim regarding antiepileptic medications, but the black box warning was not required due to the scientific advisory committee voting against it. Regardless, providers need to stay up to date on medications and warnings, ensuring that they are administering medications in the best interest of their patients. One medication that may work for one patient may not work for another (13).
Antidepressants come in several categories that are based on the type of brain chemical (dopamine, norepinephrine, and serotonin). These categories include serotonin modulators, norepinephrine dopamine reuptake inhibitor, monoamine oxidase inhibitor, tricyclic agents, selective serotonin reuptake inhibitors, and serotonin norepinephrine reuptake inhibitors.

Figure 9: Monoamine Oxidase Inhibitors (28)

Figure 10: Selective Serotonin Reuptake Inhibitors and Serotonin Modulators (9)

Figure 11: Norepinephrine Dopamine Reuptake Inhibitor (16)
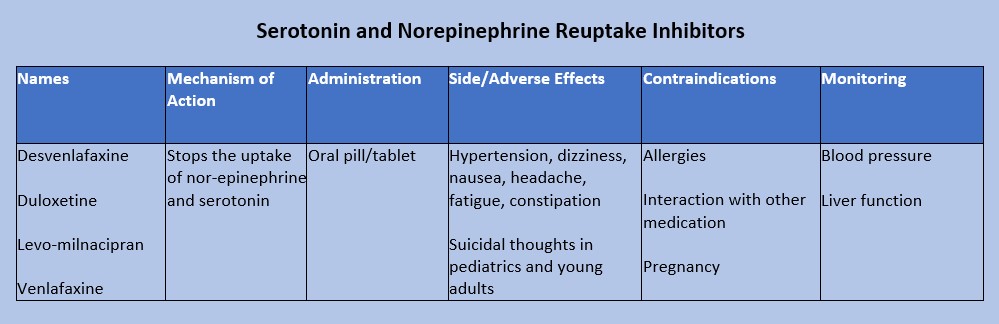
Figure 12: Serotonin and nor-epinephrine reuptake inhibitors (18)
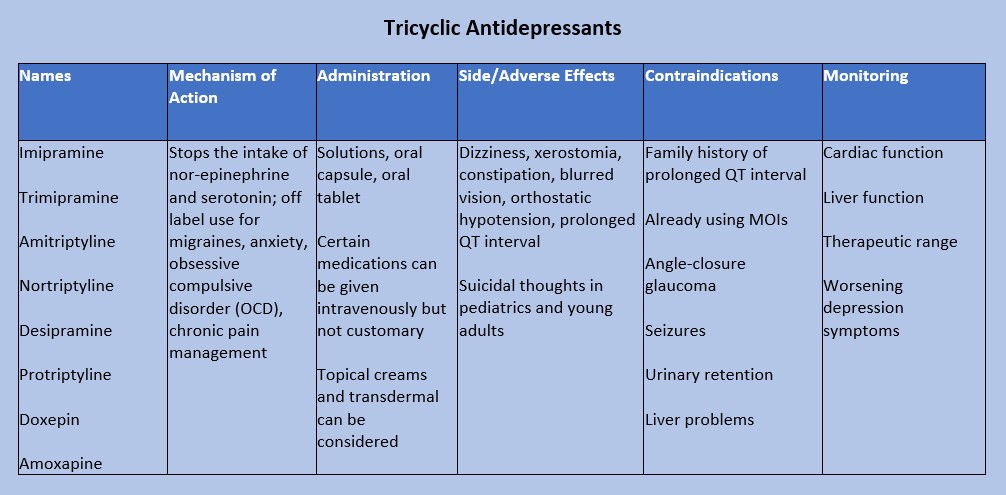
Figure 13: Tricyclic Antidepressants (20)
Case Study Reflection 5
Hope is a 35-year-old who recently moved to your town with her husband, Douglas. She is a teacher at the nearby elementary school while Douglas works in a tech startup, but he was suddenly laid off from his job. After this, Hope brings him to your facility to be evaluated. She tells you that Douglas has become increasingly agitated. He told her that he is a failure and “did not make the right choices in my life.” Douglas admits to drinking heavily with friends since he was laid off.

Self-Quiz
Ask Yourself...
- What questions do you need to ask Douglas regarding his mental health?
- Is there any medication or medication group that you would recommend prescribed to Douglas?
- If Douglas was prescribed the medication you recommended, what would you teach him about medication administration and adverse effects?
- How would you educate his wife Hope on adverse effects?
- Which adverse effects should prompt Douglas to see a provider?
- If Douglas called your facility with reports of itchiness, a rash, and swelling, what would you instruct him to do?
Substance Abuse Care
Research shows that the longer substance abuse goes on, the harder it is to recover from. Early recognition and treatment can decrease the chance of serious medical conditions or death (19). There are multiple treatment options for patients with substance use disorders, but providers must be aware of each patient’s individual circumstances: time, family and friend support, cost/expenses, and willingness.
All individuals go through the five stages of change when they want to make adjustments in their lives. Those with substance abuse disorders must be willing to make a change for themselves. Even though a person with a substance abuse disorder may want to change for another person or situation (changing for grandchildren, a spouse/romantic partner, children, etc.), they must consider that this person/situation may not remain in their lives. For this reason, they must be willing to make a change for themselves. Sometimes family or friends become too overburdened with the individual’s substance abuse, driving them away. That could inhibit or completely stop the person’s desire to change. The patient may say, “they’re no longer around, what’s the point?” Providers should not deter patients from having support systems as these could be motivation for change. However, patients should also be encouraged to find support within themselves (19). The following are the five stages of change: (19)
- Stage 1: the pre contemplation phase; they do not believe they have a problem. They are not thinking of making changes in their lives or considering how the substance may be harming them.
- Stage 2: the individual begins contemplating the need for change. They begin to realize that the substance is affecting them. This is a great time for providers to encourage them to keep contemplating and consider making a change by identifying the pros and cons of using the substance.
- Stage 3: the preparation phase; the patient has made the decision to change. More encouragement is needed. Healthcare providers should assist patients in planning and providing resources.
- Stage 4: the patient makes the change. They may start decreasing the use of substances or stop using them completely. The best thing to do for the patient is to be as supportive as possible. Patients should develop strategies on how to say “no” to situations regarding the substance.
- Stage 5: the patient is maintaining the change. Patients should focus on the positives of not using the substance and their achievements during this process.
Providers should be honest with patients regarding relapse. Recovery from substance abuse is not a linear path that is 100% successful. Everyone has moments of relapse when it comes to new habits, and it should not be discouraging. Remind patients that there is always help from providers who are non-judgmental.
Treatment strategies can include managing withdrawal symptoms in the acute phase, remaining in treatment, and preventing relapses. Many psychotherapies such as cognitive behavioral therapy can be very beneficial for recovery from substance abuse. Twelve step facilitation programs are twelve weekly sessions done individually that prepare patients for twelve step mutual support programs such as Alcoholics Anonymous and Narcotic Anonymous. While these support programs are not treatments, they are beneficial as additional support to other treatments.
Contingency management programs are similar to a rewards program. Patients, families, friends, or providers may offer rewards or privileges for meeting certain requirements of substance abuse recovery. These requirements might be taking medications as prescribed, participating in sessions, or remaining free of the substance. Rewards can be decided upon by the patient in collaboration with family, friends, and providers (26).

Self-Quiz
Ask Yourself...
- What services does your facility, organization, city, county provide for substance abuse recovery?
- What services that are offered are beneficial to those that need them?
- Do you believe there are enough resources available? If not, what services do you think are still needed?
- Does your facility have funding for additional services or patients?
- How can you advocate for additional services to be offered?
- Of the five steps of change, which step do you think is the most difficult? Provide your rationale.
- Think back on a patient you had that was in the midst of recovery. What stood out to you about them?
Safety Planning Strategies and Monitoring the Usage of the Safety Plan
Active suicidal ideation and behaviors are considered a medical emergency and should be treated accordingly. Providers in the emergency department setting should focus on medical emergencies and treatments first before moving on to any mental health treatments or consultations (19). Since suicide can be prevented, it is the duty of healthcare providers to ensure the patient is in a safe environment.
Ensuring safety can encompass a variety of methods. One example is searching belongings to remove any weapons or items that can be used to harm the individual or others such as lighters, shoelaces, strings from hoodies, and medications.
Patients may be placed under various observation statuses based on orders made by the physician or a mid-level provider. These observation statuses are also based on facility policies and best practices guided by evidence. Patients withdrawing from substances may need to be closely monitored on a medical floor due to worsening signs and symptoms. Seizures can be life-threatening for these patients.
Restraints and/or seclusion may be required as a last resort for patients. Per Washington law, patients must be under a one-to-one status, meaning there is one staff member always observing the patient. Observation can be done via audio and video equipment, or in-person. There must be documentation discussing the patient’s behavior and condition, attempts for a least restrictive method of treatment, response to seclusion and/or restraints, and the need to continue seclusion and/or restraints. A face-to-face assessment must be performed by a trained professional within one hour of the patient being placed in restraint or seclusion (38).
General regulations for restraints and seclusion include: (38)
- Within one hour of seclusion and/or restraints being initiated, an order from the physician must be entered.
- The nurse must communicate with the family or patient’s legal caregiver regarding the restraints and or/seclusion and the process that will be followed.
- The nurse must discuss with the patient the need for seclusion and/or restraints and attempt to get cooperation from the patient.
- There is to be support from others to assist with the seclusion and/or restraint process.
- Continuous observation is to be maintained while the patient is in seclusion or restraints.
- Physical and psychological needs must be addressed at regular intervals.
- The nurse is responsible for documenting the need for seclusion and/or restraints and patient assessments.
- The nurse is required to maintain education and competence on restraints.

Self-Quiz
Ask Yourself...
- Do you know what your facilities policies and procedures regarding seclusion and restraints? Do you know where to locate these policies and procedures?
- Some facilities have a no-restraint policy. Does your facility currently have a similar policy, or is that something you think could be advocated for?
- Based on your role, what are your responsibilities when it comes to seclusion and restraints?
- Who in your facility can apply restraints on patients?
- What is your confidence level with applying restraints?
- If you are not confident in applying restraints what are your resources to gain confidence?
- Who are the individuals that are able to monitor patients when they are in seclusion or restraints?
Obtaining Support and Engagement from Third Parties
As reflected in this course, family and friends are vital supportive factors for the individual with suicidal ideation or attempts. If the patient is willing, education should be given to their support system so that everyone understands medications, treatments, follow-up and outpatient treatment, and what to do in another crisis resulting in a suicide attempt or exacerbation of suicidal ideation.
Case Study Reflection 6
Courtney is a 25-year-old female patient who is at your facility with her husband. She was discharged from the hospital a few weeks ago for an aborted suicide attempt. Her friend found her overdosed in the bathroom of her house. She was given follow-up with your facility. Now that she is with you, she reports that she would like resources to help her cope better. After being told she has a history of depression and post-traumatic stress disorder, you begin to think of resources and treatment you can offer her.

Self-Quiz
Ask Yourself...
- Who else can support Courtney during her recovery?
- How can you ask Courtney about her support system and their involvement in her care?
- Thinking back to the beginning of the course, what protective factors can you give Courtney and her support system?
- Would you consider recommending or ordering any medications for Courtney at this time?
- When would you like to follow-up with Courtney? Would you like anyone else to come to the next appointment?
- Are there any goals you can give Courtney that she can work towards prior to your next appointment?
Restricting Access to Lethal Means
Statistics report that 55% of those that attempt suicide use firearms, 26% use suffocation, and 12% use poisoning. The last 8% is classified as “other” (8). Reducing or limiting access to lethal means can be defined as increasing the distance between someone with suicidal ideation and lethal means. An example would be to have the patient give their firearms over to another responsible adult that lives over 30 minutes away (12).
All providers should discuss this information with their patients and their support systems. By reducing access to lethal means, it is possible to decrease rates of suicide. However, providers must be aware that patients may not tell the full truth when it comes to availability of lethal means, and restricting access is only part of treatment and care (12).

Self-Quiz
Ask Yourself...
- Does your facility, city, county, or state have any requirements for reporting lethal means within the household?
- Are there any states that you know of that report lethal means in the household?
- If not, would you consider “reporting accessibility to lethal means” as a good idea to implement?
- How could you advocate for reporting to your government officials?
Transition of Care: Discharge and Referrals for Continuity of Care
Treatment of the patient who has suicidal ideation or had a suicide attempt does not stop once they leave the hospital setting. Care must be continued outside of the hospital setting through outpatient psychiatric providers such as a psychiatrist or psychiatric nurse practitioner. These providers can prescribe medications, adjust treatments, and provide additional therapy referrals that may be beneficial for the patient. These psychiatric providers should collaborate with the patient’s primary care provider. As discussed previously, certain psychiatric medications can interact with medication for medical diagnoses.
Veteran Populations
Data from 2020 reports that there were over six thousand veteran suicides in the United States, an average of 17 veterans dying by suicide each day. Substance use and mental health prevalence among those using the Veterans Health Administration rose from 27.9% to 41.9% from the years 2001 to 2020 (14). These numbers are staggering as veterans have a 1.5 higher risk of suicide than those in the general population and women Veterans have a suicide rate that is 2.5 times higher than civilian women (36). The chart below shows the suicide rates based on gender as classified by male and female [See figure 14].
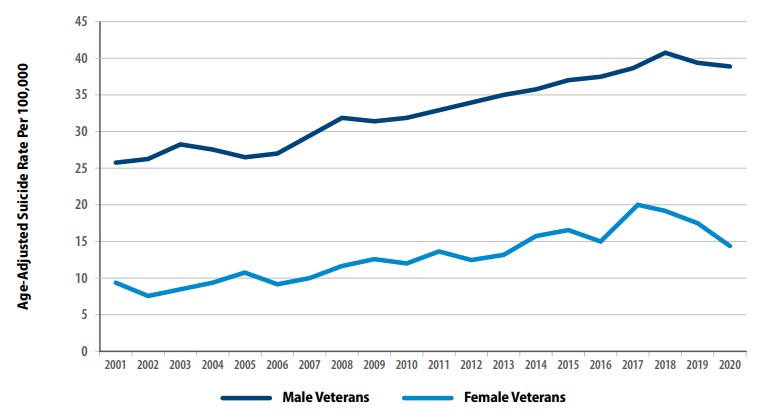
Figure 14: Suicide Rates Among Veterans by Gender From 2001 to 2020 (36)
Rates of suicide were also affected by age. Veterans in the 18- to 34-year age range had a 95.3% increase between 2001 to 2020. Those aged 55 to 74 only rose to 58.2% during that same time period. From 2019 to 2020, older veterans’ suicide rates decreased while those in the 18 to 34 age group increased (14). As with the civilian population, methods of suicide were relatively similar; data was gathered from 2001 to 2020 [See figure 15]. Additionally, rates for suicide are higher among the veteran population in comparison to civilians; the change percentage is based on 2001 data [See figure 16].
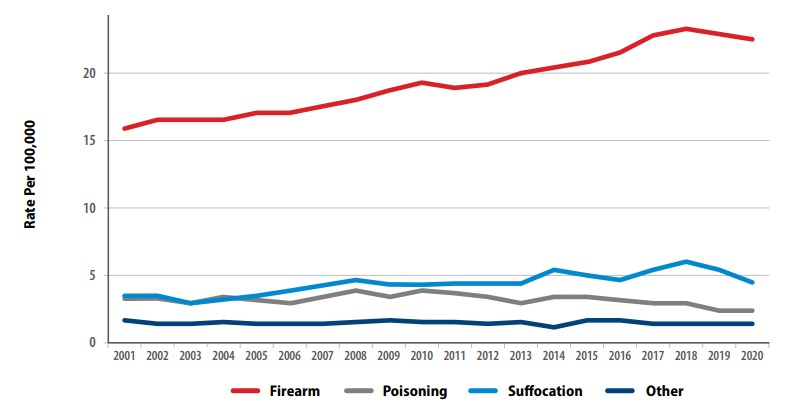
Figure 15: Methods for Suicide Among Veterans from 2001 to 2020 (36)
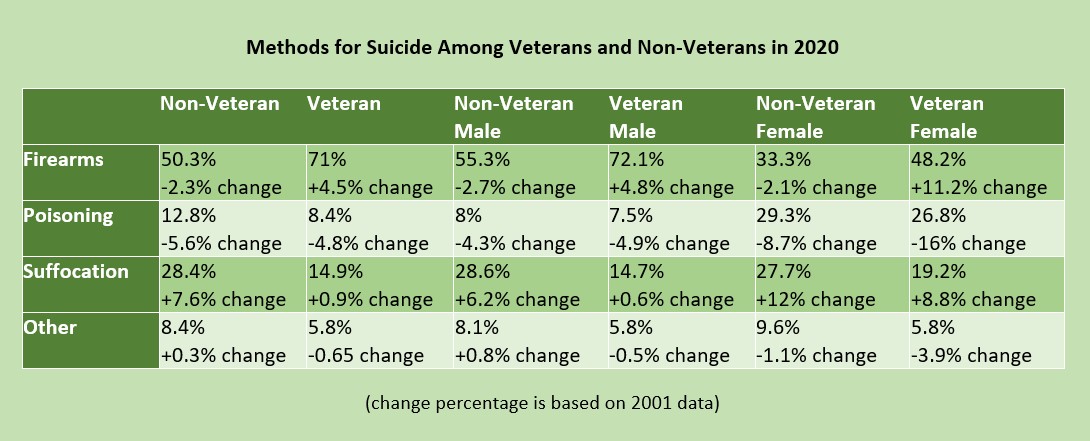
Figure 16: Methods for Suicide among Veterans and Non-Veterans (36)

Self-Quiz
Ask Yourself...
- Of the statistics listed in the figure above, what surprised you the most?
- Do you agree with this data? Why or why not?
- Have you considered if this data is completely accurate? Do you think the data could be under- or over-reported?
- Does your facility or city have a large veteran population?
- If so, do you provide care to this population often?
Veterans have similar risk factors that have different causes from their civilian counterparts. They have complex mental health conditions such as post-traumatic stress disorder, anxiety, depression, manic-depressive disorder, and traumatic brain injuries as a result of combat exposure. Others have combat wounds that can lead to severe medical diagnoses and possible prescribing of opioid medications for controlling pain. Veterans may have insomnia which can exacerbate any of their other symptoms or diagnoses. These individuals may turn to substance abuse instead of other forms of treatment due to the ease of accessibility. Studies show that over one in 10 veterans are diagnosed with at least one substance use disorder. There is an increased risk of opioid overdose, but this population is more likely to turn to alcohol (36).
The Department of Veteran Affairs has taken steps to provide resources for mental health and suicide prevention to all veterans. Veterans and families are given suicide prevention education upon discharge, and suicide assessments are completed during every visit. Each facility has a Suicide Prevention Coordinator that can be contacted at any time. Veterans, and their families and friends can utilize Veterans Chat, a free, anonymous messaging service that gets them in touch with a Veterans Affairs counselor. If needed, the counselor can transfer the individual to the Veterans Crisis Line for further counseling or referral services (35).
Veteran Resources (All civilian resources are available to veterans):
https://www.veteranscrisisline.net/
https://www.va.gov/health-care/health-needs-conditions/mental-health/suicide-prevention/
https://theactionalliance.org/veteran-and-military-suicide-prevention-resources
Case Study Reflection 7
Cory is a 45-year-old male patient that presents to your emergency department for severe abdominal pain. During your initial assessment, Cory tells you he also feels dehydrated and has been more tired than usual lately. He says he ran out of his sleep medication, “but the providers at the VA are so hard to see. It takes months for an appointment.” When you ask him the standard questions (if he drinks alcohol or uses any other substances), he becomes angry and snaps at you before immediately apologizing. Cory admits that he has been drinking more than usual for the past few months because his chronic leg pain—an injury from when he was in combat—has been bothering him more than normal.

Self-Quiz
Ask Yourself...
- Would you perform a suicide screening on Cory? What is your rationale?
- If Cory admits to having suicidal ideation, what would be your next steps?
- If Cory denies suicidal ideation, but reports he’s been feeling hopeless or depressed, what would be your next steps?
- Does your facility have any resources to provide Cory while he is in the emergency department?
- Could you consider advocating for a collaboration with the nearest VA to assist veterans like Cory who come to your facility?
Suicide Loss Survivors
As highlighted throughout this course, suicide can happen to anyone, and they leave behind many people. Friends, families, coworkers, and acquaintances can all be affected by the loss. Those who have lost a loved one to suicide are often referred to as suicide loss survivors.
If a healthcare provider encounters a suicide loss survivor, they should always assess the risk for suicide. As discussed previously in this course, some individuals may attempt suicide on the anniversary of their loved one’s passing. In addition, they could attempt on a day of significance to the individual that passed or a major holiday that held special meaning. If the suicide loss survivor is at a high risk for suicide, follow your facility’s protocols for additional assessment or treatment (1).
If there is no significant risk for suicide, provide support and resources. Remember that some individuals have chronic suicidal ideation. Support can be through active listening, having a non-judgmental attitude that is free of bias or criticism. Some individuals may be hesitant to tell their story due to the nature of the loved one’s death. Encourage them to talk to someone they can trust if they do not want to share that information with you. Reassure them that bereavement is not a linear process and that they do not have a time limit to when they should be done grieving. Every person is different, and how they progress through the stages of grieving varies (1).
Resources that can be provided include any of the above options discussed earlier in this course. Psychiatric providers, therapy, and medications may be indicated for survivors of suicide loss. Offer them resources and referrals per your facility’s protocols, but also let them know they are always able to return to your facility if needed, especially emergency departments. Medical providers may need to be involved as well if the patient has any medical concerns (1).

Self-Quiz
Ask Yourself...
- Have you ever cared for a patient who was a suicide loss survivor?
- How did they present?
- What were their reactions during the initial phase of loss?
- Does your facility have any resources that can be offered to this particular population, for example, a chaplain or spiritual care specialist?
- What behaviors in this patient population would be concerning to you?
- Are there any unique resources you could think of to provide these patients?
Conclusion
Suicide impacts everyone. With the ever-growing need for mental health services and the rise in mental health decline, it is no surprise that suicide rates have increased among all populations. Without proper assessments, knowledge of risk and protective factors, and proper treatment requirements at each level of suicide risk, individuals in need may be missed. It is the job of the healthcare provider to ensure that all individuals are screened and treated appropriately. You may be the last point-of-contact a patient has with a provider prior to taking their own life. Ensure that you ask the questions.

Self-Quiz
Ask Yourself...
- How often do you screen your patients for suicide risk?
- What suicide screening tool does your facility utilize?
- Do you think the suicide screening tool used at your facility is effective? Why or why not?
- Have you had any family or friends that were going through substance abuse? If you were able to help them, what was challenging for you?
- Are there any nursing groups you are involved in that have position statements or white papers regarding the importance of reporting individuals’ access to lethal means? If so, what do they say?
- In your facility, are the policies and procedures regarding seclusion and restraints effective? Do you think they need to be updated to reflect best practices?
- As a healthcare provider, what can you do to ensure that data reported on suicide is accurate?
LGBTQ+ Cultural Competence
LGBTQ+ patients may experience healthcare disparities due to multiple factors, including lack of provider knowledge. In this course we will discuss how to deliver care, with LGBTQ cultural competence.
Introduction
Lesbian, gay, bisexual, transgender, and questioning (LGBTQ+) individuals represent a rapidly growing segment of the U.S. population [1]. This rapid growth brings with it risk for stigmatization [1]. Implicit healthcare provider biases may result in LGBTQ+ patients receiving a lower standard of care or restricted access to services as compared to the general population [2]. Even when institutions and providers make commitments to equitable care explicit and implicit biases operating outside of conscious awareness may undermine that commitment. There is an urgent need to ensure that healthcare providers are prepared to identify and address their own implicit biases to ensure they do not contribute to the health care disparities experienced by LGBTQ+ and other vulnerable populations. Only by addressing their own implicit biases will health care providers be able to provide patient care in accordance with LGBTQ+ cultural competence.
LGBTQ+ individuals face significant disparities in physical and mental health outcomes [3]. Compared to their heterosexual counterparts, LGBTQ+ patients have higher rates of anal cancer [4], asthma, cardiovascular disease [5,7,8], obesity [6], substance abuse [8,9,10], cigarette smoking [11], and suicide [14]. Sexual minority women report fewer lifetime Pap tests [13,15, 16], transgender youth have less access to health care and LGBTQ+ individuals are more likely to delay or avoid necessary medical care [17] compared to heterosexual individuals. These disparities are due, in part, to lower health care utilization by LGBTQ+ individuals [3]. Perceived discrimination from health care providers and denial of health care altogether are common experiences among LGBTQ patients and have been identified as contributing factors to health disparities [19,20,21,22]. Disparities in health care access and outcomes experienced by LGBTQ+ patients are compounded by vulnerabilities linked to racial identity [23,24,25] and geographic location [6].
Biases among health care students and providers toward LGBTQ+ patients are common [27,28] despite commitments to patient care equality. These biases, also known as negative stereotypes, may be either explicit or implicit [29]. These biases contribute to a lack of LGBTQ+ cultural competence in patient care. A large study of heterosexual, first-year medical students demonstrated that about half of students reported having negative attitudes, explicit bias, towards lesbian and gay people and over 80% exhibited increased negative evaluations of lesbian and gay people compared to heterosexual people (implicit bias) [27]. Research in social-cognitive psychology on intergroup processes defines explicit biases as attitudes and beliefs that are consciously-accessible and controlled; these characteristics are typically assessed via self-report measures and are limited by an individual’s awareness of their attitudes, motivation to reveal these attitudes, and ability to accurately report these attitudes [30,31]. In contrast, the term implicit bias refers to attitudes and beliefs that are unconscious (i.e., outside of conscious awareness) and automatic [32,33]. Implicit bias can be assessed with the Implicit Association Test (IAT) [34], which aims to define the relationships between concepts (ex. race, sex, idea), and positive or negative associations and/or stereotypes. Idenitfied biases are then delegated as slight, moderate, or strong [35].
Healthcare provider biases are correlated with poorer access to services, quality of care, and health outcomes [29, 36, 37, 38]. Explicit biases held by health professionals towards racial/ethnic minorities, women, and older adults are known to affect clinical assessments, medical treatment, and quality of care [39]. Importantly, implicit bias measures are more strongly associated with real-world behaviors than explicit bias measures [40] and are linked to intergroup discrimination [43]. Health care provider’s implicit biases towards vulnerable patient groups may persist despite an absence of negative explicit attitudes [36], resulting in preconceived notions about patient adherence, poor doctor-patient communication, and micro-aggressions, all of which can interfere with optimal care. With less time and limited information processing capacity, provider’s decisions are increasingly governed by stereotypes and implicit biases [42]. Medical student and provider biases may contribute to health disparities in vulnerable populations by negatively impacting communication with patients and decisions about patient care [29, 33]. Taken together, these findings suggest that medical students and healthcare providers are likely to underestimate or to be unaware of their implicit biases towards LGBTQ+ patients, particularly when they are rushed or fatigued, which could impact their behavior and judgments in ways that contribute to health disparities experienced by LGBTQ+ populations. By learning about and addressing their implicit biases, health care providers can work towards demonstrating LGBTQ+ cultural competence and providing optimal care(Introduction section courtesy of Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P.- reference 2).

Self-Quiz
Ask Yourself...
- What are some cultural misconceptions regarding the LGBTQ+ community and providing medical care?
- How can you demonstrate LGBTQ+ cultural competence in everyday practice?
Terminology
Understanding the standard terminology utilized is pivotal to treating and interacting with LGBTQ+ patients. Below are listed some of the common terms and how they should be referenced.
Ally– A person not identifying as LGBTQ+, but whom promotes equality and support of LGBTQ+ peoples in a variety of ways.
Androgynous– Identifying as neither masculine nor feminine.
Bisexual – A person who is emotionally, romantically, or sexually attracted to more than one sex, gender, or gender identity.
Cisgender – A person whom identifies with their gender which as assigned at birth. For example, a person assigned female gender at birth who identifies as female.
Gay – A person who is emotionally, romantically and/or sexually attracted to those of the same gender.
Gender-fluid – A person who identifies as a fluid or unfixed gender identity.
Lesbian – A woman who is emotionally, sexually, and/or romantically attracted to other women.
LGBTQ+ – Acronym for “lesbian, gay, bisexual, transgender, and queer.”. The plus sign stands for the innumerable other identities.
Non-binary – Adjective describing person(s) who do not identify exclusively as man nor woman.
Pansexual – A person who has the potential for romantic, emotional, and/or sexual attraction to people of any gender.
Queer – Often used interchangeably with “LGBTQ+”, or to express fluid identities or orientations.
Sexual orientation – An inherent or enduring emotional, romantic, or sexual attraction to other people.
Transgender –Umbrella term for people whose gender identity and/or expression is different from cultural expectations based on the sex they were assigned at birth. It does not imply any specific sexual orientation and transgender persons may identify as straight, gay, lesbian, bisexual, etc.
*Definitions largely derived from (44, 45).

Self-Quiz
Ask Yourself...
- Which of the above definitions have you heard used interchangeably?
Best Practices
Below we will list and discuss the best practices for ensuring a positive, equitable healthcare experience for LGBTQ+ persons, according to the Joint Commission (this is not a comprehensive list, nor inviolable, but rather highlights).
Create a welcoming environment that is inclusive of LGBT patients and demonstrates LGBTQ+ cultural competence.
- Prominently display the hospital nondiscrimination policy and/or patient bill of rights.
- Waiting rooms and common areas should be inclusive of LGBTQ+ patients and families.
- Unisex or single-stall restrooms should be available.
- Ensure that visitation policies are fair and do not discriminate (even inadvertently) against LGBTQ+ patients and families.
- Foster an environment that supports and nurtures all patients and families.
Avoid assumptions about sexual orientation and gender identity.
- Refrain from making assumptions about a person’s sexual orientation and/or gender identity.
- Be cognizant of bias, stereotypes, and other communication barriers.
- Recognize that self-identification and behaviors do not always align.
Facilitate disclosure of sexual orientation and gender identity, but be aware that disclosure is an individual process.
- Honor and respect patient’s decisions to provide or not provide sexual and/or gender information.
- All forms should contain inclusive, gender-neutral language that allows patients to self-identify.
- Use neutral and inclusive language when communicating with patients.
- Listen to and respect patients’ choice of language when they describe their own sexual orientation.
- Conduct confidential patient satisfaction surveys that include questions regarding sexual orientation and gender identity
*Information largely derived from Joint Commission field guide, reference 45.
For more information on best-practices in the workforce, visit the Joint Commission website by clicking here.

Self-Quiz
Ask Yourself...
- Have you ever misused a pronoun, or overheard a co-worker misuse a pronoun in practice? How can you make sure this doesn’t happen again?
Establishing Relationships with LGBTQ+ Patients
When interacting with patients, one should not assume gender or sexuality. Addressing a patient whom identifies as a female as a male can cause grave harm to the relationship. Instead, nurses should use open-ended questions. For example, rather than saying “Hi sir, what brings you to the hospital,” a nurse might say, “Welcome, what brings you to the hospital today (45)?”
If a nurse uses the incorrect pronoun, the best practice is to apologize and ask the patient what pronoun and name they prefer. For example, a nurse may say, “I apologize for assuming your gender. How would you like to be addressed? (45).
In conversation, the nurse should use the name and/or pronoun the patient prefers without drawing special attention to the subject (45). For example, if a patient prefers to be identified as their partner’s wife, you should follow suit.
The core of relationship-building with LGBTQ+ patients is no different than any other patient, fundamentally. If nurses have a basic understanding of best practices and a healthy dose of respect and compassion for LGBTQ+ patients, a positive relationship is likely to develop.

Self-Quiz
Ask Yourself...
- Do you have any biases which may affect the care you provide to LGBTQ+ patients?
- Have you worked for someone who did NOT demonstrate LGBTQ+ cultural competence? In what ways could they improve their practice?
Health Disparities of LGBTQ+ Patients
LGBTQ+ Americans are at higher risk of substance use, sexually transmitted diseases, cancer, cardiovascular disease, obesity, bullying, isolation, anxiety, depression, and suicide when compared to the general population (49). LGBTQ+ youth are frequently bullied at schools (46). In fact, early victimization and subsequent emotional distress accounted for 50% of the disparities between LGBTQ+ youth (46). In other words, LGBTQ+ Americans are discriminated against and disadvantaged from a very young age.
When home life also reflects a lack of LGBTQ+ cultural competence, more problems arise. A major cause of LGBTQ+ distress is family rejection. Disclosure of gender identity or sexuality can cause very significant interpersonal conflicts among family and friends of LGBTQ+ persons (46). This explains some hesitancy and should help nurses understand the importance of respecting privacy, while giving options to patients about disclosing sexuality and gender.

Self-Quiz
Ask Yourself...
- Are there any circumstances in which your current hospital’s policies could discriminate against LGBTQ+ families?
- If so, how would you begin to work with leadership to change those policies so they reflect LGBTQ+ cultural competence?
Providing an Inclusive and Accepting Care Environment
LGBTQ+ patients often experience difficulty in finding healthcare environments in which they feel accepted and understood (45). Past negative experiences, lack of knowledge among healthcare providers, and limited access to healthcare in general may become major barriers for LGBTQ+ persons when seeking care (45).
The core tenant of providing an inclusive environment is understanding the needs of LGBTQ+ patients, and working diligently to create an environment which does not disadvantage or discourage them from seeking care.
Policies and procedures at institutions should be designed to reflect a non-discriminatory environment. For example, many hospital policies dictate that only legal family spouses or partners can visit in specific circumstances. Policies such as this are inherently discriminatory toward LGBTQ+ patients, as they may not have legal spousal status due to social, legal, or personal reasons.

Self-Quiz
Ask Yourself...
- Have you ever had an experience where a colleague made a derogatory remark about a patient, based on sexual orientation or gender status? If this happened to you, how would you handle that situation differently?
Laws Specific to Washington D.C.
1973: Title 34 is passed, which prohibits discrimination based on sexual orientation.
2006: The D.C. Human Rights Act is updated to ensure residents of the district are protected regarding employment, house, and public accommodations.
2016: The Armstrong Amendment is repealed in D.C., which allows religious schools exemptions from complying with anti-discrimination laws.
2016: LGBTQ Cultural Competency CE Act is passed. This requires that all licensed healthcare providers take a 2-credit hour course to increase competency (such as the one you are currently taking!).

Self-Quiz
Ask Yourself...
- Think about the structure of your facility. Does it create an environment which minimizes friction and discrimination of LGBTQ+ patients?
- Do you feel there are any biases among healthcare staff?
- If so, how would begin addressing those?
Exercises on LGBTQ+ Cultural Competence
To help solidify your learning, please complete the following exercises at your own pace. The answers/guidance for each are provided below.
Scenario 1
A patient enters your emergency department and you assume the patient identifies as a female. You introduce yourself and say, “Ma’am, how can we help you? What brings you in today?”
The patient appears dismayed but answers the question. The nurse is confused and does not understand why the patient appears distressed. What is the best course of action?
Answer: The nurse should apologize to the patient and ask the patient how they would like to be addressed. Then, the nurse should update the patient’s records to reflect such, to reduce further confusion.
If the nurse does not address the issue, the patient may feel uncomfortable and develop a negative association with healthcare, which can lead to disparities in the future.
Scenario 2
A patient in your ICU has had a deterioration while his husband was in the room. After a family meeting, a member of the healthcare team makes a derogatory remark about the patient’s sexuality. What is the next best action for the nurse?
Answer: Pre-conceived phobias and stigmatizations can cause significant distress to LGBTQ+ patients, even if not stated directly to them. These type of remarks are abusive and should not be tolerated. The nurse should confront the co-worker (if safe) and consider reporting the comments to the Human Resources department.
Scenario 3
A LGBTQ+ patient is being admitted and prefers not to disclose their sexuality. However, the nurse is unable to proceed with the admission process without this information. What could be done to rectify this system-level issue?
Answer: The nurse should work with administration to ensure that all charting and paperwork allows individuals to self-report sexuality and/or gender if they want. However, healthcare systems should not force patients to “come out” unless it is absolutely medically necessary.

Self-Quiz
Ask Yourself...
- What information from this course can you take to your facility to encourage a positive change of LGBTQ patients, and create an environment for LGBTQ+ cultural competence?
Conclusion
LGBTQ+ cultural competence must be ingrained in our healthcare systems in order to foster excellent relationships between members of the LGBTQ+ community and medical staff. Hospitals and healthcare systems have a great deal of work to do in becoming LGBTQ+ friendly. The efforts must continue until LGBTQ+ patients and families do not feel disadvantaged, anxious, or frustrated when interacting with healthcare systems. As the patient’s ultimate advocate, nurses are at the front-line and should advocate for patients both individually and from a policy perspective. Nurses should work with and spearhead efforts to ensure that healthcare policies reflect best-practice and do not discriminate against LGBTQ+ patients in any way.
Washington State Healthcare Professional Telemedicine Training
Introduction
Telehealth has become more popular and widespread across the United States. With its widespread use and popularity, more nurses and health care practitioners are required to complete courses like this Washington Telehealth Training. The earliest encounter with telehealth involved Alexander Graham Bell in 1876 when he used his telephone as a means of getting help from his assistant after he had an accident involving spilled acid on his trousers (1). The origin of telehealth officially began in 1959, with clinicians at the University of Nebraska utilizing video communication for medical purposes. These clinicians established a two-way television setup to transmit information to medical students across campus. Five years later, the setup was linked with a state hospital to perform video consultations. Telemedicine first became popular in rural areas, where populations with limited healthcare access could now reach specialists from afar. In the 1960s and 70s, the Public Health Department, NASA, the Department of Defense, and the U.S. Health and Human Services Department all invested time and money into telemedicine research.
In this Washington Telehealth Training course, the following outcomes and objectives will be reviewed:
- Discuss the background, origin, and scope of telehealth practice.
- Explain policies and regulations related to telehealth.
- Describe ways to determine if an organization is ready and prepared for telehealth and the process for the actual telehealth visit.
Telehealth Background
Definition
This Washington Telehealth Training course defines telehealth as the delivery of healthcare services using digital technology and can include services in the behavioral health field, such as substance use disorder treatment, serious mental illness treatment (SMI), and counseling. The clinic is considered the originating site (where the patient is located during the telehealth visit) and the specialist at the other location is the distant site.
In organizations that serve individuals with intellectual and developmental disabilities (IDD), telehealth is the practice of healthcare within a professionally designated scope of practice using electronic communication, information technology, or other means between a licensee in one location and a client in another location with or without an interviewing healthcare provider.
Telehealth allows patients to have better access to a variety of specialists which, in turn, increases the number of people receiving appropriate care. Overall, it can provide cost savings to the patient and increase the quality of care.

Telehealth and its Scope of Practice
The practice of nurses using telehealth is within the legal scope of practice for licensed nurses, registered nurses, licensed practical nurses, and advanced practice registered nurses (2). It can be used among these professionals as needed or when a patient is unable to make an in-person visit.

Self-Quiz
Ask Yourself...
- What is the history of telehealth and its development?
- How does telehealth apply to everyday life?
Telehealth Policy and Regulations
In-State/Out-of-State Requirements
Most providers are only allowed to see patients located in states where the provider is licensed or certified. However, many states temporarily changed this policy during COVID-19. These in-state restrictions are often due to the nature of the services a clinic provides.
Organizations can choose if they want to provide telehealth services. However, if the topic is suggested, the organization must have team members in place to discuss the options, pros, cons, and feasibility of telehealth within its practice.
Additional Credentialing and Protocols
There are no additional credentialing or privilege protocols in place for those located out-of-state as those individuals are required to seek services within their area and state. The credentialing requirements must abide by the specific guidelines set forth by each organization and these can vary from one place to another.
It is imperative that the right billing codes are used in order for the insurance company to reimburse for services rendered. Typically, there are codes known as the Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS). It is important to pay attention to any changes, as these codes do change from time to time. If ever in doubt, always double-check to ensure that the codes being entered are the correct ones for proper billing and reimbursement.
Reimbursement of In-Person Visits
Telehealth visits are typically reimbursed at an equal rate to in-person visits, but the reimbursement for those with intellectual and developmental disabilities (IDD) relies mostly on Medicaid Home and Community Based Services (HCBS) waivers. The overwhelming majority of waivers permit the temporary use of telehealth services for those individuals with IDD; however, only a small percentage include the use of telehealth on a permanent basis for this population. The limitations that were noted involved those individuals that were not a part of the following services: employment, day, and prevocational services, and in-home residential supports. Controlled substances are also not allowed to be prescribed by using telehealth until an in-person visit takes place.
Ryan Haight Act of 2008
The Ryan Haight Act summarizes that no controlled substance may be delivered, distributed, or dispensed by an electronic method such as the Internet without a valid prescription and requires at least one in-person medical evaluation (3).
This Washington Telehealth Training course asks nurses to consider the following example: if a patient undergoing a telehealth visit needs to be prescribed a controlled substance, the person issuing the prescription must have a doctor-patient relationship with the patient. This may seem reasonable, but the narrow definition in the law indicates that a telehealth visit may be inadequate due to the law specifically requiring an “in-person evaluation”.

Self-Quiz
Ask Yourself...
- Can an organization willfully choose to participate in telehealth or are they required to do so?
- How can one ensure that services for telehealth are being billed accurately?
- What is an example of the Ryan Haight Act of 2008 in action?
Telehealth Readiness
When an organization begins to consider whether or not telehealth service is right for them, there are four critical factors that must be considered. These four factors include 1) workflow, 2) practitioner availability and acceptance, 3) infrastructure and cost, and 4) sustainability. All of these factors must be considered when attempting to decide if telehealth services would prove beneficial to an organization. An organization must meet as a team to discuss these components in order to assure that these factors can or cannot be met successfully.
Standards of care must be implemented and followed at any given practice and specialty area. The same is true for practices utilizing telehealth. The following serve as standards of care (4):
- Training of staff – staff must be trained in the use of the technology used and must be competent.
- Evaluations and Examinations – diagnosis should be established by establishing the patient’s history, mental evaluation, physical examination, and appropriate laboratory and diagnostic testing.
- Licensee-Patient Relationship – proper identification must be made prior to any telehealth encounter. Failure to verify the patient’s identity may lead to fraudulent activity or disclosure of patient information that is confidential. The location and identity of the patient must be verified. The licensee’s name, professional credentials, and location should be provided to the patient. Appropriate follow-up care and a complete medical record must be available to the patient and other health care providers involved in the treatment plan.
- Prescribing – the concept of “Contact with Patients before Prescribing” must be practiced – other providers must be involved in ongoing care and evaluations of the patient. All federal and state laws must be followed and are expected to participate in the Controlled Substances Reporting System.
- Medical Records – complete records must be maintained and must be consistent with prevailing medical record standards. HIPAA and security related documents must be present and signed appropriately. Confidentiality must be maintained and a copy of the medical records consistent with state and federal laws must be in place.
- Disclaimers – a statement that includes any unique limitations of the electronic model being used should be present, if applicable.
- Licensure – the practice of medicine is deemed to occur in the state in which the patient is located. If the licensee intends to practice telehealth outside of their current state must first check with other state’s licensing board to ensure if this is allowed.
Protocols for the necessity of visits
Typically, most patients can receive an appointment for a telehealth visit without any difficulty as long as the following are not present: conditions causing severe pain or those requiring a detailed in-person examination, prescription and refill of controlled substances, any condition that requires in-person drug administration, highly complex medical conditions, and psychiatric emergencies.
There are certain protocols regarding the type of visit that is appropriate for telehealth and when one should be referred to an in-person visit. The following are some common types of visits that meet the standards of telehealth:
- Lab tests or x-ray results
- Recurring conditions such as migraines or urinary tract infections
- Skin conditions
- Mental health treatment, online therapy, counseling, and medication management
- Prescription management
- Urgent care issues such as colds, coughs, and stomach aches
A patient should be referred to an in-person visit when they require highly specialized care, such as cancer treatments or complex specialty care.
How to Receive a Telehealth Appointment
With most telehealth appointments, it is best and easier if the patient will download the app and initially set up an account. There is also a 1-800 number that can typically be called as well if the patient needs additional help. Each patient will need to complete a brief medical history just as one would at the doctor’s office and once submitted, the telehealth specialist will connect the patient with the right medical professional – doctor, therapist, or a specialist. The telehealth specialist will assist the patient with setting up a date/time for the appointment and the appointment can be completed by phone, video, or app.

General Overview of Telehealth Software
This Washington Telehealth Training course recommends following five things should be considered when looking to choose a platform to implement telehealth services: integration using the same interface which allows everything to be accessed; user-friendly design – all patients should feel comfortable using the platform and not frustrated; specialty care solution – look for a platform that caters to providers that provide specialty services; configuration and customization – the platform needs to be customizable to meet each patient’s unique preferences along with the preferences of the healthcare facility; data analytics – it is important to gain new insights by recoding and logging each patient interaction, which allows the organization to better manage the practice and the experiences of the patients. The collected data assists with identifying issues early and creating resolutions in a timely manner.
In general, the practice of telehealth requires a good source of internet access by all parties, supported by broadband internet connection and mobile communication. The following list includes hardware requirements:
- Desktop
- Computer
- Laptop
- Smartphone with a camera
- Tablet with a camera and microphone
- Telemedicine care
Guide on Approved Software
It is important to ensure that the software platforms used are HIPAA compliant. The list below includes vendors that represent HIPAA-compliant video communication products that are recommended by this Washington Telehealth Training course:
- Skype/Microsoft Teams
- Updox
- VSee
- Zoom for Healthcare
- me
- Google G Suite Hangouts Meet
- Cisco Webex Meetings/Webex Teams
- Amazon Chime

Self-Quiz
Ask Yourself...
- What are the implications for an organization to implement telehealth?
- Is it difficult for a patient to receive an appointment for telehealth based on their symptoms?
- What are the implications of choosing the correct software for telehealth services?
Obtaining Patient Consent for Telehealth
Once the patient has decided to use telehealth for an appointment, official informed consent may be required. It is important to keep in mind that specific informed consent laws vary by state, but this Washington Telehealth Training course recommends the following actions that are always a good idea to follow (5):
- Explain to the patient what they can expect from the telehealth visit and what their rights consist of.
- Check in with the patient about their responsibilities during online counseling or telehealth visits such as wearing headphones and finding a place to be alone to ensure privacy.
- Inform the patient to get anyone’s consent from the start that may be observing the patient.
- Instruct patients to complete required forms ahead of time and bring them to the telehealth visit.
- Ensure the informed consent form and any other documentation has been done during the check-in process, including verbal consent.
It is important to have your medical intake forms reviewed by the legal team. Obtaining informed consent from each patient is important to have completed before the first appointment.
Verbal consent is where a patient gives their consent to a procedure in a verbal manner and does not sign any written form. This Washington Telehealth Training course provides the following example:
My name is ________________________________ and I am verbally consenting to participate in the study. By signing above, I give permission to be a part of the study and to allow the data collected to be used for the resulting process.

IT Support Services
In order for telehealth to be productive, IT support services must be in place to ensure that all areas are fully functioning and if a problem occurs, the IT department must be available and ready to intervene 24/7/365. If a patient is experiencing problems making an appointment or with any connectivity issues, IT can be notified to assist in these areas.
Practice First
Telehealth is a relatively new technology and as it gains widespread usage it is important for each organization using telehealth to do a practice run first to ensure that all of the elements are working properly. Every platform is used differently, and it is important to understand the requirements for each one. Also, the patient may need to have an app downloaded beforehand to make the entire process smoother.
Emergency Outage Plan
Planning can go a long way to prepare for an emergency situation during a telehealth appointment. If an emergency outage situation occurs, answer the following questions with the patient before or at the beginning of their first appointment:
- What is your current location?
- Confirm the patient’s exact location and obtain their full address.
- What is the information for your emergency contact?
- There should always be more than one number given in case disconnection occurs.
- Do you have an alternate way of contacting the clinic if disconnection occurs?
- If not, this needs to be made known at the beginning of the call.
- Do you have an alternate video platform to use if disconnection occurs?
- If so, this needs to be communicated with the provider at the start of the call.
Patient Information Security/HIPAA Protocols
This Washington Telehealth Training course recommends that all telehealth services provided by insured health-care providers and health plans must comply with the established HIPAA rules according to the Health Insurance Portability and Accountability Act of 1996. The HIPAA rules are in place to ensure that both paper and digital medical histories remain private. During the actual call, the health care provider is required to call the patient from a private setting such as their office or an appointment room. The patient should also be in a private, safe location in which they can freely discuss their health.
There are four important ways to stay compliant with the telehealth HIPAA regulations, 1) check one’s remote communications, 2) double-check the tracking of data, 3) keep all vendor agreements in writing, and 4) protect any and all stored communications.
Connecting Interpreter Services to Telehealth
Many virtual meeting platforms offer an option to connect an interpreter if requested by the patient. Once conencted, a Language Line can be added to the address book that enables the interpreter to be accessed. The service assists in building trust, reducing misunderstandings, and improving the overall patient experience. The patient will be connected to experienced professionals who will securely and patiently assist those with language barriers to make important healthcare decisions. The patient can also access telehealth resources translated from English on the platform that allows the patient to view the information in their own preferred language.
Billing and Documentation Protocols
When submitting documentation for a telehealth visit, the following elements must be included: date of visit; consent for visit from the patient or patient representative (either verbal or written consent); category of office visit, real-time audio with audio/telephone or video only.
In order to ensure that medical records are accurate and supported by telehealth services, the following must be documented in the health record (6):
- Method of telehealth (video connection, phone call, etc.)
- Location of provider (name of clinic, city, home, other)
- Listing of all clinical participants, roles, and actions
- Member location (name of clinic, city, home, other)
- Time actually spent in medical discussion – start/stop times.
- Patient consent – documented confirmation or verbal consent must be documented

Self-Quiz
Ask Yourself...
- What does verbal consent indicate within telehealth, and can you give an example?
- How does an organization ensure that HIPAA is maintained with telehealth visits?
- How does an organization ensure that accurate billing has been conducted with telehealth visits?
Telehealth Visit
Guidelines
Just as bedside manner encompasses much more superficial appearance, web-side manner transcends how an individual looks on camera, including empathy and understanding for patients regardless of physical distance. The same standards apply for in-person visits, but a patient is likely to observe and evaluate how the telehealth visit goes based on the visual manners given during the visit. The medical professional should be dressed in an appropriate and professional manner. The lighting, angle of the camera, and background are all important factors to consider when doing a telehealth visit. This Washington Telehealth Training course provides the following fundamentals for each telehealth visit:
- Ensure that all professional identification is within clear view for the patient.
- Place yourself in the center of the video frame. You are the focal point – not the background.
- Ask the patient for a contact phone number or alternative communication in case a disconnection occurs.
- If this is the first telehealth visit with the patient, consent must be obtained.
- Ensure that you are HIPAA-compliant by confirming that anyone else in the room and is approved by the patient and that the patient is comfortable performing the visit.
- Position lighting to reduce any glare or spotlights. Uniform lighting is the best and allows the patient to see your face.
- Eliminate background items which may distract the patient.
- Confirm the patient’s location to ensure you have the proper licensure.
- Ask the patient to make any rearrangements regarding furniture, lighting, or body position in order to give you a better view of the patient and a more accurate exam.
Telehealth is not for everyone or for every medical condition. It is important for an individual to discuss the risks, advantages, and disadvantages with one’s healthcare provider.
How to Start a Telehealth Visit
This Washington Telehealth Training course recommends the following four steps will help you successfully conduct a telehealth visit from start to finish:
- Ensure the patient has the resources to schedule a telehealth appointment– patients need to be aware of how to schedule an appointment and how to contact a customer service representative if any problems arise.
- Prepare for the telehealth visit – send the patient a reminder a day before the appointment reminding them to connect 10 minutes prior to the appointment for registration and check-in. The co-payment can also be collected at this time.
- Conduct the telehealth visit – the provider should carefully review the patient’s chart and medical history just as they would for an in-person appointment. Additionally, any messages or information in the patient portal should be reviewed and imported beforehand. The provider should start the visit note, use the appropriate telehealth template, and begin the visit. A proper web-side manner should be implemented the entire time with intentional listening and clear communication. During the evaluation, the provider will document any complaints and symptoms reported by the patient. Note any assessments or treatment plans including the proper diagnosis codes, orders, mediations, and relevant instructions. After ending the telehealth visit, the provider should complete any documentation and sign the note.
- Follow up and complete the telehealth coding and billing – the practice should send a follow-up text message or email the day after the appointment offering contact information for any questions or concerns with a link to a patient survey. The patient can log into the patient portal to review a summary or the visit, education resources, pay a balance, and communicate with the practice if needed.
The following can three diagnostic errors that may create issues during telehealth visits: 1) inadequate history taking due to poor or inadequate communication, 2) limited physical examinations such as the omission of auscultation and accessibility of private areas of the body, and 3 )reliance on patients and their families to accurately measure vital signs, report them, and describe physical findings.

Self-Quiz
Ask Yourself...
- Do all patients benefit from a telehealth visit?
- What are some potential issues with telehealth that can impact patient safety?
Spinal Cord Injury: Bowel and Bladder Management
Introduction
Imagine one day you are able to walk and take care of your own needs. Now, imagine one week later you wake up no longer able to walk, feel anything below your waist, or hold your bowels.
This is a reality for many people who sustain spinal cord injuries. Managing changes in bowel and bladder function is one of many challenges that people with spinal cord injuries and their families or caregivers face.
This course will provide learners with the knowledge needed to assist patients who have spinal cord injuries with bowel and bladder management to improve the quality of life in this group.

Self Quiz
Ask yourself...
- What are some societal misconceptions or stereotypes about people with spinal cord injuries?
- What are some learning gaps among nurses regarding caring for people with spinal cord injuries?
- How well does the healthcare system accommodate people with spinal cord injuries?
Spinal Cord Injuries: The Basics
Spinal Cord Function
Before defining a spinal cord injury, it is important to understand the function of the spinal cord itself. The spinal cord is a structure of the nervous system that is nestled within the vertebrae of the back and helps to distribute information from the brain (messages) to the rest of the body [1].
These messages result in sensation and other neurological functions. While it may be common to primarily associate the nervous system with numbness, tingling, or pain, nerves serve an important purpose in the body’s function as a whole.
Spinal Cord Injury Definition
When the spinal cord is injured, messages from the brain may be limited or entirely blocked from reaching the rest of the body. Spinal cord injuries refer to any damage to the spinal cord caused by trauma or disease [2]. Spinal cord injuries can result in problems with sensation and body movements.
For example, the brain sends messages through the spinal cord to muscles and tissues to help with voluntary and involuntary movements. This includes physical activity like running and exercising, or something as simple as bowel and bladder elimination.
Spinal Cord Injury Causes
Spinal cord injuries occur when the spinal cord or its vertebrae, ligaments, or disks are damaged [3]. While trauma is the most common cause of spinal cord injuries in the U.S., medical conditions are the primary causes in low-income countries [4] [2].
Trauma
- Vehicle accidents: Accounts for 40% of all cases [2]
- Falls: Accounts for 32% of all cases [2]
- Violence: Includes gun violence and assaults; accounts for 13% of all cases [2] [5]
- Sport-related accidents: Accounts for 8% of all cases [2]
Medical Conditions
- Multiple Sclerosis (MS): Damage to the myelin (or insulating cover) of the nerve fibers [1]
- Amyotrophic Lateral Sclerosis (ALS): Lou Gehrig’s disease, damage to the nerve cells that control voluntary muscle movements [1]
- Post-Polio: Damage to the central nervous system caused by a virus [1]
- Spina Bifida: Congenital defect of the neural tube (structure in utero that eventually forms the central nervous system) [1]
- Transverse Myelitis (TM): Inflammation of the spinal cord caused by viruses and bacteria [1]
- Syringomyelia: Cysts within the spinal cord often caused by a congenital brain abnormality [1]
- Brown-Sequard Syndrome (BSS): Lesions in the spinal cord that causes weakness or paralysis on one side of the body and loss of sensation on the other [1]
- Cauda Equina Syndrome: Compression of the nerves in the lower spinal region [1]
Spinal Cord Injury Statistics
According to the World Health Organization, between 250,000 and 500,000 people worldwide are living with spinal cord injuries [4]. In the U.S., this number is estimated to be between 255,000 and 383,000 with 18,000 new cases each year for those with trauma-related spinal cord injuries [6].
Age/Gender
Globally, young adult males (age 20 to 29) and males over the age of 70 are most at risk. In the U.S., males are also at highest risk, and of this group, 43 is the average age [2].
While it is less common for females to acquire a spinal cord injury (2:1 ratio in comparison to males), when they do occur, adolescent females (15-19) and older females (age 60 and over) are most at risk globally [4].
Race/Ethnicity
In the U.S. since 2015, around 56% of spinal cord injuries related to trauma occurred among non-Hispanic whites, 25% among non-Hispanic Black people, and about 14% among Hispanics [6].
Mortality
People with spinal cord injuries are 2 to 5 times more likely to die prematurely than those without these injuries (WHO, 2013). People with spinal cord injuries are also more likely to die within the first year of the injury than in subsequent years. In the U.S., pneumonia, and septicemia – a blood infection – are the top causes of death in patients with spinal cord injuries [6].
Financial Impact
Spinal cord injuries cost the U.S. healthcare system billions each year [6]. Depending on the type, spinal cord injuries can cost from around $430,000 to $1,300,000 in the first year and between $52,000 and $228,000 each subsequent year [6].
These numbers do not account for the extra costs associated with loss of wages and productivity which can reach approximately $89,000 each year [6].

Self Quiz
Ask yourself...
- What is one function of the spinal cord?
- What is one way to prevent spinal cord injuries in any group?
- Why do you think injuries caused by medical conditions are least likely to occur in the U.S.?
- Why do you think the first year of care after the injury is the most costly?
Think about someone you know (or cared for) who had a spinal cord injury.
- Did they have total or partial loss of feeling and movement to the extremities?
- What comorbidities or complications did they have associated with the injury?
- In what ways did the injury affect their overall quality of life?
Spinal Cord Injuries: Types and Complications
Four Levels of the Spinal Cord
- Cervical (vertebrae C1 – C8): Neck; controls the back of the head down to the arms, hands, and diaphragm
- Thoracic (vertebrae T1 – T12): Upper mid-back; controls the chest muscles, many organs, some back muscles, and parts of the abdomen
- Lumbar (vertebrae L1 – L5): Lower back; controls parts of the lower abdomen, lower back, parts of the leg, buttocks, and some of the external genital organs
- Sacral (vertebrae S1 – S5): Lower back; controls the thighs down to the feet, anus, and most of the external genital organs
Types of Spinal Cord Injuries
Spinal cord injuries may be classified by level and degree of impairment. There are four types of spinal cord injuries [5].
Injury Level
- Tetraplegia or Quadriplegia: Injury at the cervical level; loss of feeling or movement to the head, neck, and down. People with this type of spinal cord injury have the most impairment.
- Paraplegia: Injury at the thoracic level or below; limited or complete loss of feeling or movement to the lower part of the body.
Impairment
- Incomplete spinal cord injury: Some sensation and mobility below the level of injury as the spinal cord can still transmit some messages from the brain.
- Complete spinal cord injury: Total loss of all sensation and mobility below the level of injury. Spinal cord injuries of this type have the greatest functional loss.

Spinal Cord Injury Complications
Complications from spinal cord injuries can be physical, mental, or social, and can impact overall quality of life. There are six common complications of spinal cord injuries [2].
Depression
Studies show that 32.9% of adults with disabilities experience frequent mental distress [7]. Mental distress may be related to functional limitations, chronic disease, and the increased need for healthcare services. Up to 37% of people with spinal cord injuries develop depression [2].
Pressure injuries
People with spinal cord injuries may have problems with circulation and skin sensation– both risk factors for pressure injuries. Some may be bedridden or wheelchair-bound which also places them at risk for pressure injuries. Up to 80% of people with spinal cord injuries will have a pressure injury during their lifetime and 30% will have more than one [2].
Spasticity
Around 65% - 78% of people with spinal cord injuries have spasticity [2]. Spasticity is uncontrolled muscle tightening or contraction. The damage from spinal cord injuries causes misfires in the nervous system leading to twitching, jerking, or stiffening of muscles.
Autonomic dysreflexia
In some people with spinal cord injuries, a full bladder or bowel distention can cause a potentially dangerous condition called autonomic dysreflexia. The full bladder or bowel triggers a sudden exaggerated reflex that causes an increase in blood pressure. This condition is also associated with a severe headache, low heart rate, cold skin, and sweating in the lower body [8].
Respiratory problems
If the diaphragm function is affected, as with cervical spinal cord injuries, there may be breathing difficulties. People with lumbar spinal cord injuries can even have respiratory problems as the abdominal muscles are used to breathe.
Sexual problems
Due to changes in muscle function and depending on the degree of damage, people with spinal cord injuries may have problems with arousal and climax due to altered sensations and changes in sexual reflexes.
Changes in bowel and bladder function
Many people with spinal cord injuries lose bowel control. Bowel problems can include constipation, impaction, and incontinence. They may also have problems with urination, for example, urinary retention.

Self Quiz
Ask yourself...
- Why might a person with a disability experience mental distress?
- In what type of spinal cord injury does a person lose all sensation and mobility below the waist?
- Why are people with spinal cord injuries at risk for pressure injuries?
- How can spinal cord injuries affect a person’s personal relationships?
Bowel and Bladder Dysfunction in Spinal Cord Injuries
This section will cover the normal function of the bowel and bladder, and the types of bowel and bladder dysfunction that occurs in patients with spinal cord injuries.


Self Quiz
Ask yourself...
Think about a time you assisted with bowel or bladder management in someone with a spinal cord injury.
- What types of activities were included in their bowel or bladder regimen?
- What challenges did you encounter during bowel or bladder care?
- What difficulties did they express to you about managing their bowel or bladder program?
- In what ways did you assist them in managing their own bowel or bladder program?
Normal Bowel and Bladder Function
In normal bowel and bladder function, when the rectum or bladder fills with stool/urine and presses on area nerves (stimulation), the message is sent to the spinal cord which sends it to the brain. The brain gives the person the “urge” feeling, allowing an option to control the elimination or not.
Whatever decision the person makes, the brain sends the message back to the spinal cord, which in turn sends a message to the elimination muscles (anal and bladder sphincters) to either relax or stay closed until the person is ready. In people with spinal cord injuries, the messages are limited or blocked, leading to problems with bowel and bladder control [9] [10].
Bowel Dysfunction with Spinal Cord Injuries
Reflex hypertonic neurogenic bowel occurs when a rectum full of stool presses against area nerves sending a message to the spinal cord, but it stops there. The message never makes it to the brain, so the person never gets the urge.
As a result, a reflex is set off, prompting the spinal cord to send a message to the anal muscle (sphincter) instead, causing it to relax and release the stool. This condition leads to bowel incontinence and usually occurs in spinal injuries at the cervical and thoracic levels [9] [10].
Flaccid hypotonic bowel occurs when area nerves are also stimulated by a full rectum, but the message does not even reach the spinal cord, so there is no reflex. The anal sphincter is always in a relaxed state.
As a result, the bowels simply empty when they are full, and this can occur at any time without the person having the ability to control it. This condition results in bowel incontinence and can lead to constipation as the patient does not have the urge and may not have the ability to push. This condition usually occurs in spinal injuries at the lumbar level [9] [10].
Bladder Dysfunction with Spinal Cord Injuries
Reflex neurogenic bladder occurs when the bladder automatically starts to contract after filling with a certain amount of urine. The person has no urge to go as the messages are either limited or blocked from reaching the brain, therefore leading to loss of bladder control. Similar to reflex hypertonic neurogenic bowel, the full bladder triggers are nerves that set off a reflex, prompting the spinal cord to send messages to the bladder releasing urine outside of the person’s control [9] [10].
Acontractile bladder occurs when the bladder loses muscle tone after a spinal cord injury, lessening its ability to contract, leading to bladder distention, and dribbling of urine. People with this condition need to use urinary catheters to help empty the bladder [9].


Self Quiz
Ask yourself...
- What is one role of the brain in bowel and bladder function?
- Which type of bowel dysfunction occurs in thoracic-level spinal cord injuries?
- In which type of bowel dysfunction might a suppository be most effective?
- In which type of bladder dysfunction does the bladder lose muscle tone?
The Nurse’s Role in Bowel and Bladder Management
This section will cover how nurses can assess, intervene, and teach when caring for patients with spinal cord injuries who have bowel and bladder dysfunction.

Self Quiz
Ask yourself...
Think about your experiences with patients with spinal cord injuries and their family or caregivers.
-
- How knowledgeable was the patient about their bowel or bladder care?
- In what ways were the family or caregiver involved in the plan of care?
- Did the family or caregiver have any learning gaps that needed to be addressed?
- What difficulties did the family or caregiver express to you about their role?
Nurse Assessments
When caring for patients with spinal cord injuries, nurses should obtain a detailed bowel and bladder history including diet, fluid intake, medications, and elimination patterns/habits [11]. Many of these patients may already manage their own bowel and bladder care at home.
If so, the nurse should obtain the patient’s current regimen and communicate the information to the physician. The physician may choose to continue the regimen or adjust as needed based on the patient’s current illness/condition.
Questions the nurse can ask the patient:
- What does your typical diet consist of?
- How much fluid do you drink on a daily basis?
- How often do you have a bowel movement or urinate?
- Do you schedule your bowel movements with assistance from medications?
- Are there certain body positions or things you do to help you pass stool more easily?
- How often do you use an intermittent urinary catheter for bladder relief?
- How much time do you spend on your bowel and bladder regimens?
- Do you care for all of your elimination needs or does someone help you?
- How does your bowel and bladder dysfunction affect your quality of life?
Some assessments may be observed. For example, nurses may notice that the patient has a surgically placed permanent suprapubic urinary catheter or colostomy (when the bowel is cut somewhere above the level of the rectum and diverted to the outside of the abdomen).
Nurse Interventions
Since many patients with spinal cord injuries have problems with bowel and bladder function, elimination must be scheduled. Nurses can help by implementing bowel and bladder programs and providing education and support to patients, families, or caregivers.
Regimens
Follow the patient’s home bowel and bladder regimen (as ordered). This may include maintaining intermittent catheterization every few hours or administering suppositories daily.
For patients who do not have a regimen already or wish to modify their current one, encourage them to pay attention to how often they urinate and pass stools, elimination problems, foods that alleviate or worsen the problem, and medications or other things that help. This can be done through a diary.
Dietary Considerations
Educate patients on the importance of a fiber-rich diet to avoid constipation. Patients should also be made aware that high-fat foods, spicy foods, and caffeine can alter gut dynamics and lead to bowel incontinence episodes [12].
Fluid Intake
Some patients may avoid drinking enough water to avoid bladder complications (e.g., frequent incontinent episodes) [12]. However, nurses should educate patients on the importance of adequate fluid intake to prevent constipation. Patients should be made aware that bladder and bowel elimination regimens go hand in hand.
Bladder Elimination
For bladder dysfunction, help patients perform intermittent urinary catheterization as needed or place a temporary urinary catheter (as ordered).
Bowel Elimination
For bowel dysfunction, administer ordered suppositories and laxatives to help the bowels move (use suppositories in conjunction with the level of sensation the patient has near the anus/rectum) [9]. Changes in body position may help as well.
While many of these interventions may not work in some patients with spinal cord injuries, bowel irrigation (water enemas) may be helpful [11]. Surgical placement of a colostomy may be indicated if all other measures have failed [11].
Emotional Support
Ensure privacy and sensitivity during all elimination care as patients may experience embarrassment or frustration.
Education for Families or Caregivers
Provide education to families or caregivers on the importance of helping patients stay consistent with their elimination regimen, follow diet and fluid intake recommendations, and comply with medication orders.
Referrals
Inform the physician if interventions are not effective or if the patient, family, or caregiver has a special need (e.g., counselor or dietician). Refer patients and families or caregivers to support groups as needed.
Support Groups and Resources
Christopher and Dana Reeve Foundation
Christopher Reeve – an actor who was left paralyzed after an equestrian accident – and his wife Dana’s legacy lives on through their foundation, an organization that advocates for people living with paralysis [13].
Miami Project to Cure Paralysis
In response to his son, who acquired a spinal cord injury during college football, NFL Hall of Famer Nick Buoniconti and world-renowned neurosurgeon Barth A. Green, M.D. started a research program aimed at finding a cure for paralysis and discovering new treatments for many other neurological injuries and disorders [14].
National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR)
The National Institute on Disability, Independent Living, and Rehabilitation Research, a part of the U.S. Department of Health and Human Services’ Administration for Community Living, helps people with disabilities integrate into society, employment, and independent living [15].
Paralyzed Veterans of America (PVA)
A group of World War II veterans who returned home with spinal cord injuries, started this organization to support those with spinal cord injuries and dysfunction. Today, the organization focuses on quality health care, research and education, benefits, and civil rights to affected veterans [16].
The United Spinal Association supports people with spinal cord injuries and those in wheelchairs. The organization advocates for disability rights like access to healthcare, mobility equipment, public transportation, and community support. Support groups can be found on their website [17).

Self Quiz
Ask yourself...
- What is one question a nurse can ask a patient to obtain a bowel and bladder history?
- How can nurses help patients with spinal cord injuries start or modify a bowel or bladder regimen?
- When might a colostomy be indicated for a patient with a spinal cord injury?
- What type of referral might be ordered for a patient with a spinal cord injury who has bowel or bladder dysfunction?
Conclusion
Spinal cord injuries can have devastating effects on patients and their families. Management of basic bodily functions like bowel and bladder elimination should be made as easy as possible for these patients.
When nurses learn how to effectively help patients with spinal cord injuries better manage their own bowel and bladder regimens, quality of life and health outcomes may be improved for this group.
Pressure Injury Prevention, Staging and Treatment
Introduction
When hearing the term HAPI, what comes to mind? The fact is, HAPI may not necessarily generate happy thoughts. Hospital-acquired pressure injuries (HAPIs) are a significant problem in the U.S. today. In fact, pressure injuries in general – whether acquired in a hospital or not – are a global problem.
Many articles have noted that staging and differentiating pressure injuries can be overwhelming for nurses [9]. The purpose of this course is to equip learners with the knowledge needed to reduce pressure injuries, resulting complications, financial risk, and associated death. The information in this course will serve as a valuable resource to nurses from all specialties and backgrounds.
What is a pressure injury?
The National Pressure Injury Advisory Panel (NPIAH) defines pressure injuries as “localized damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device” [17]. Pressure injuries can present as intact or opened skin and can be shallow or deep. Pressure injuries can be quite painful for patients and may require extensive treatment.
Prior to 2016, pressure injuries were termed “pressure ulcers.” However, since ulcer implies “open skin,” the NPIAH changed it to “pressure injury” as the skin is not always open with some of these injuries [22][25].
What causes a pressure injury to develop?
Pressure
Intense and/or prolonged pressure on the patient’s skin and/or tissue can cause compromised blood flow and decreased sensation [7]. This can occur when patients lay or sit on a bony prominence for an extended period of time [16].
Bony prominences are areas where you can easily feel a bone underneath the skin or tissue when palpating. These can include the heels, hips, elbows, and tailbone. Approximately two-thirds of all pressure injuries occur on the hip and buttocks area [7].
Friction and Shear
Friction and shear often happen when patients slide down in bed, for example, when the head of the bed is raised. Although “friction and shear” are often used together, there is actually a difference between the two.
While friction occurs when skin is dragged across a coarse surface (leading to surface-level injuries), shearing occurs when internal bodily structures and skin tissue move in opposite directions (leading to deep-level injuries) [10]. Shearing is often associated with a type of pressure injury called deep tissue injury (occurring in the deeper tissue layers rather than on the skin’s surface) [10].

[24]
What are risk factors for developing a pressure injury?
There are numerous risk factors for pressure injuries – some of which may not be directly related to the skin. These risk factors can be categorized as either intrinsic factors (occurring from within the body) or extrinsic (occurring from outside of the body) [2][13].
Intrinsic Risk Factors
- Poor skin perfusion (e.g., peripheral vascular disease or smoking)
- Sensation deficits (e.g., diabetic neuropathy or spinal cord injuries)
- Moist skin (e.g., urinary incontinence or excessive sweating)
- Inadequate nutrition (particularly poor protein intake)
- Poor skin elasticity (e.g., normal age-related skin changes)
- End of life/palliative (leads to organ failure including the skin)
- Limited mobility (i.e., bedridden, or wheelchair-bound)
Extrinsic Risk Factors
- Physical and chemical restraints (leads to limited mobility)
- Undergoing a procedure (laying down for extended periods of time)
- Length of hospital stay (for HAPIs)
- Medical devices (can lead to medical device-related pressure injuries)

Self Quiz
Ask yourself...
- What are the most common areas for pressure injuries to develop?
- What is the major difference between friction and shear?
- What is one reason why elderly adults are at an increased risk for developing a pressure injury?
Statistical Evidence
This section will cover pressure injury statistics both globally and nationally. This section will also cover the impact pressure injuries have on healthcare.
What is happening on a global scale?
In a global study, researchers found that the prevalence (all cases) and incidence (new cases) of pressure injuries in 2019 were 0.85 million and 3.17 million, respectively – numbers that have decreased over time [23][25]. Numbers were disproportionately high in high-income North America, Central Latin America, and Tropic Latin America [25]. Numbers were lowest in Central Asia and Southeast Asia. The report revealed that although numbers are high overall, they are much lower than what they were predicted to be, which may be attributed to better prevention and treatment initiatives.
What is happening nationally?
In the U.S., 2.5 million people develop pressure injuries each year [1]. This number does not account for the many people trying to manage pressure injuries on their own at home (i.e., when family acts as the caregiver).
HAPIs in particular are a growing problem. The most recent data on hospital-acquired conditions in the U.S. shows that from 2014 to 2017, HAPIs increased by 6% (647,000 cases in 2014 to 683,000 in 2017) [6]. Each year 60,000 patients in the U.S. die as a direct result of pressure injuries [1].
How do pressure injuries impact healthcare?
Pressure injuries can be quite costly to the healthcare system. These injuries can lead to persistent pain, prolonged infections, long-term disability, increased healthcare costs, and increased mortality [1].
In the U.S., pressure injuries cost between $9.1 - $11.6 billion per year [1]. These injuries are complex and can be difficult to treat [7]. Often requiring an interdisciplinary approach to care, the costs of one pressure injury admission can be substantial. Individual care for patients with pressure injuries ranges from $20,900 to $151,700 per injury [1]. Not to mention, more than 17,000 lawsuits are related to pressure injuries every year [1].
Due to the significant impact that these injuries have on healthcare, prevention and accurate diagnosis is imperative.

Self Quiz
Ask yourself...
- What are possible contributing factors to the increase in HAPIs in the U.S.?
- What are some factors that may contribute to the high costs of pressure injuries in healthcare settings?
Staging and Diagnosis
The section will cover the staging, varying types, and diagnosis of pressure injuries.
What is the difference between wound assessment and staging?
Pressure injury staging is more than a basic wound assessment. Wound assessment includes visualizing the wound, measuring the size of the wound, paying attention to odors coming from the wound, and lightly palpating the area on and/or around the wound for abnormalities. Pressure injury staging, however, involves determining the specific cause of injury, depth of skin or tissue damage, and progression of the disease.
What are the six stages of pressure injuries?
According to NPIAP guidelines, there are six types of pressure injuries – four of which are stageable [14].

[16]
Stage 1
In Stage 1 pressure injuries, there is intact skin with a localized area of non-blanchable erythema (pink or red in color), which may appear differently in darkly pigmented skin. Before visual changes are noted, there may be the presence of blanchable erythema or changes in sensation, temperature, or firmness. Stage 1 pressure injuries do not have a purple or maroon discoloration (this can indicate a deep tissue pressure injury).
Stage 2
In Stage 2 pressure injuries, there is partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist, and may represent an intact or opened serum-filled blister. Fat (adipose) and deeper tissues are not visible. Granulation tissue, slough (soft moist material, typically yellow or white), and eschar (hard necrotic tissue, typically black in color) are not present. Stage 2 injuries cannot be used to describe wounds associated with moisture-only, skin chaffing, medical adhesives, or trauma.
Stage 3
In Stage 3 pressure injuries, there is full-thickness loss of skin, in which fat is visible in the injury, and granulation tissue and rolled wound edges are often present. Slough and/or eschar may be noted. The depth of tissue damage is dependent on the area of the wound. Areas with a significant amount of fat can develop deep wounds.
Undermining (burrowing in one or more directions, may be wide) and tunneling (burrowing in one direction) may be present. Fascia, muscle, tendon, ligament, cartilage, and/or bone are not exposed. If slough or eschar covers the extent of tissue loss, this would be considered an unstageable pressure injury, not a Stage 3.
Stage 4
In Stage 4 pressure injuries, there is full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage, or bone in the wound. Slough and/or eschar may be visible. Rolled wound edges, undermining, and/or tunneling are often present. The area where the wound is present will determine the depth. As with stage 3 pressure injuries, if slough or eschar covers the extent of tissue loss, this would be considered an unstageable pressure injury.
Unstageable
In unstageable pressure injuries, there is full-thickness skin and tissue loss in which the extent of tissue damage within the wound cannot be confirmed because it is covered by slough or eschar. If the slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar (i.e., dry, adherent, intact without erythema or fluctuance) on an ischemic limb or the heel(s) should not be removed.
Deep Tissue Injury
In deep tissue pressure injuries (also termed: deep tissue injuries or DTIs), there is intact or non-intact skin with localized area or persistent non-blanchable deep red, maroon, purple discoloration, or epidermal separation revealing a dark wound bed or blood-filled blister.
Pain and temperature changes often precede skin color changes. Discoloration may appear differently in darker-pigmented skin. The injury may resolve without tissue loss or may worsen quickly and open up, revealing the actual extent of tissue injury. Deep tissue pressure injuries should not be used to describe vascular, traumatic, neuropathic, or dermatologic conditions.

Self Quiz
Ask yourself...
- How do basic wound assessments differ from pressure injury staging?
- What is the main difference between a Stage 1 pressure injury and deep tissue injury?
- What is one structure you might see in a Stage 4 pressure injury wound bed that you would not see in any other pressure injury?
What are other types of pressure injuries?
Mucosal Membrane Pressure Injury
Mucosal membrane pressure injuries are found on mucous membranes with a history of a medical device in use at the location of the injury. For example, a wound on the inside of a nostril from a nasogastric tube would be considered a mucosal membrane pressure injury. Due to the anatomy of the tissue, mucosal membrane pressure injuries cannot be staged [18].
Medical Device-Related Pressure Injury
Medical device-related pressure injuries, often associated with healthcare facilities, resulting from the use of devices designed and applied for diagnostic or therapeutic purposes [15]. The resulting pressure injury typically conforms to the pattern or shape of the device which makes identification easier. The injury should be staged using the staging system.
Hospital Acquired Pressure Injury (HAPI)
While the general hospital setting places patients at a 5% to 15% increased risk of developing a pressure injury (HAPI), patients in the intensive (or critical) care unit in particular have an even higher risk [17]. Critical care patients typically have serious illnesses and conditions that may cause temporary or permanent functional decline. There is also evidence that pressure injuries in this setting can actually be unavoidable.
The NPIAP defines “unavoidable” pressure injuries as those that still develop after several measures by the health provider have been taken. These measures include when the provider has (a) evaluated the patient’s condition and pressure injury risk factors, (b) defined and implemented interventions consistent with standards of practice and the patient’s needs and goals, and (c) monitored and evaluated the impact of interventions [20]. There are certain situations in which a critical care patient may have a higher risk of developing unavoidable pressure injuries.
In one study of 154 critical care patients, researchers found that 41% of HAPIs were unavoidable and those who had a pressure injury in the past were five times more likely to develop an unavoidable pressure injury during their stay [20]. The study also found that the chance of developing an unavoidable HAPI increased the longer patients stayed in the hospital – a 4% risk increase each day.

Self Quiz
Ask yourself...
- What type of pressure injury can be caused by nasogastric tube use?
- What is it about critical care patients that places them at a high risk for HAPIs?
- In what situation is a pressure injury considered unavoidable?
How are pressure injuries diagnosed?
Diagnosing a pressure injury is done by simply staging the injury. The health provider may stage the injury or rely on the nurse’s staging assessment before giving the final diagnosis and initiating treatment. There are tests that may be ordered to help identify the early stages of a developing injury.
For example, subepidermal moisture assessment (SEM) scanners may help to identify tissue changes early on in patients with darker skin tones [8]. Tests may also be ordered to determine the extent of the damage, disease, or infection caused by a pressure injury. A magnetic resonance imaging test (MRI) can be used to determine if the infection in a stage 4 pressure injury has spread to the bone.

Self Quiz
Ask yourself...
- What are some problems that can occur if a pressure injury is not staged correctly?
- What is one reason a provider would order an MRI of a pressure injury?
Prevention and Treatment
This section will cover various strategies that can be used to prevent and treat pressure injuries.
What are some ways to prevent pressure injuries?
Preventing pressure injuries takes more than just one nurse repositioning a patient every two hours. It involves a combination of strategies, protocols, and guidelines that facilities can implement across various departments, specialties, and care team members. The NIAPH recommends the following prevention strategies [19].
Risk assessment
Facilities should use a standardized risk assessment tool to help identify patients at risk for pressure injuries (i.e., the Braden or Norton Scale). Rather than using the tool as the only risk assessment strategy, risk factors should be identified by other means (for example, by gathering a detailed patient history).
Risk assessments should be performed on a regular basis and updated as needed based on changes in the patient’s condition. Care plans should include risk assessment findings to address needs.
Skin Care
Monitoring and protecting the patient’s skin is vital for pressure injury prevention. Stage 1 pressure injuries should be identified early to prevent the progress of disease. These include looking at pressure points, temperature, and the skin beneath medical devices.
The frequency of assessments may change depending on the department. Ideally, assessments should be performed upon admission and at least once daily. Skin should also be cleaned promptly after incontinence episodes.
Nutritional Care
Tools should be used that help to identify patients at risk for malnutrition. Patients at risk should be referred to a registered dietician or nutritionist. Patients at risk should be weighed daily and monitored for any barriers to adequate nutritional intake. These may include swallowing difficulties, clogged feeding tubes, or delays in intravenous nutrition infusions.
Positioning and mobilization
Immobility can be related to age, general poor health, sedation, and more. Using offloading pressure activities and keeping patients mobile overall can prevent pressure injuries. Patients at risk should be assisted in turning and repositioning on a schedule. Pressure-relieving devices may be used as well. Patients should not be positioned on an area of previous pressure injury.
Monitoring, training, and leadership
Current and new cases of pressure injuries should be documented appropriately and reported. All care team members should be educated on pressure injury prevention and the importance of up-to-date care plans and documentation.
All care team members should be provided with appropriate resources to carry out all strategies outlined. Leadership should be available to all care team members for support (this may include a specialized wound care nurse or wound care provider).


Self Quiz
Ask yourself...
- What is one reason why a patient at risk for pressure injuries would be weighed daily?
- What are two ways to prevent pressure injuries in a patient with limited mobility?
How are pressure injuries treated?
There is no one way to treat a pressure injury. Management of pressure injuries involves a specialized team of care providers and a combination of therapies that aim to target underlying factors and prevent complications [7]. Depending on the stage of the wound and skin risk factors, providers may order specific types of treatments.
Some pressure injury treatments may include the following [7].
- Wound debridement – a procedure in which necrotic tissue is removed from a wound bed to prevent the growth of pathogens in the wound, allowing for healing
- Antibiotic therapy (topical or systemic)
- Medicated ointments applied to the wound bed (e.g., hydrogels, hydrocolloids, or saline-moistened gauze to enable granulation tissue to grow and the wound to heal)
- Nutritional therapies (e.g., referrals to dieticians)
- Disease management (e.g., controlling blood sugar in diabetes)
- Pain medications
- Physical therapy (to keep the patient active)

Self Quiz
Ask yourself...
- In what way does debridement help to heal a pressure injury?
- What non-nursing care team member may be consulted for a patient with a pressure injury?
The Nurse’s Role
The section will cover the nurse’s role in preventing pressure injuries and the progression of disease.
What is the nurse’s role in pressure injury prevention?
Based on NPIAH guidelines, the Agency for Healthcare Research and Quality (AHRQ) – an agency that monitors pressure injury data for the U.S. – breaks down quality initiatives for preventing pressure injuries in a three-component care bundle [2].
A care bundle is a combination of best practices that when used together, can lead to better patient outcomes [2]. The care bundle includes skin assessments, risk assessments, and care planning. Nurses should follow the guidelines listed under each component.
Standardized pressure injury risk assessment
- Use risk assessment tools and processes to identify patients at risk
- Do not rely on tools only, use your own judgment as well (tools are meant to guide the assessment)
- Update risk scores at least once daily and if patient’s condition changes
- Document findings in the medical record
- Communicate findings to other staff involved for continuity of care (e.g., informing another nurse during patient handoff reporting)
Comprehensive skin assessment
- Identify any pressure injuries that may be present
- Determine whether there are other areas of skin breakdown or factors that may predispose the patient to develop a pressure injury (e.g., moist skin)
- Identify other skin issues
- Perform assessments at regular intervals
- Document findings in the medical record
- Communicate findings to other staff involved in care so that appropriate changes can be reported (e.g., informing the nursing assistant)
- Ask colleague to confirm findings for accuracy (i.e., two-nurse skin checks)
Care planning and implementation to address areas of risk
- Create care plans that include each skin risk factor (e.g., nutrition, mobility, and moisture)
- Update care plans as often as needed if there are any changes in the patient’s condition
- Evaluate whether care plan was effective by assessing patient response to interventions
- Individualize care plans for each patient based on risk assessment scores and other observed risks
- Identify patient learning needs and implement teaching as needed
- Document care plan in the medical record
- Communicate care plan to other staff involved for continuity of care (e.g., informing another nurse during patient handoff reporting)

Self Quiz
Ask yourself...
- Why should nurses avoid relying solely on standardized assessment tools?
- Why is documentation important when performing a skin assessment?
- What pressure injury information should nurses communicate during handoff report?
How can nurses prevent medical device-related pressure injuries?
The NPIAP outlined best practices to prevent medical device-related pressure injuries in various settings including general care, long-term care, critical care, and pediatric care [20]. The following strategies apply across all settings.
- Choose the correct size of medical device for the individual.
- Cushion and protect the skin with dressings in high-risk areas (e.g., nasal bridge).
- Inspect the skin under and around the device at least daily (if not medically contraindicated).
- Rotate sites of oximetry probes.
- Rotate between O2 mask and prongs (if feasible).
- Reposition devices (if feasible).
- Avoid placement of device over sites of prior or existing pressure injury OR directly under the patient.
- Be aware of edema under the device and the potential for skin breakdown.
- Change rigid C-collar to softer collar when medically cleared (for critical care settings).

Self Quiz
Ask yourself...
- How can nurses prevent a pressure injury from developing on the ear of a patient who wears a nasal cannula?
How can nurses identify pressure injuries in patients with darker skin tones?
Research suggests that it may be difficult to note early changes that can lead to the development of a pressure injury in patients with darker skin tones – for one, blanching may not be as visible [8]. This places the patient at a greater risk for the advancement of disease as early identification may be challenging.
In order to appropriately identify pressure injuries in patients with darker skin tones, nurses should use unique strategies. The NIPAH offers these recommendations for nurses to help accurately identify pressure injuries in this group [8].
Identification tips
- Clean the suspected area beforehand
- Compare the area to surrounding unaffected areas
- Compare the area to the opposite laterality if possible (i.e., right versus left elbow)
- Compare the area to unaffected areas in a different location (i.e., upper back versus chest)
- Look for differences in skin tautness
- Look for shining skin changes
- Palpate for changes in skin temperature

Self Quiz
Ask yourself...
- What is one way to identify pressure injuries in patients with darker skin tones?
How can nurses quickly differentiate between pressure injury stages?
Correct staging of pressure injuries is vital as treatment is determined by the extent of damage, disease, or infection. First and foremost, wounds should be gently cleaned prior to staging as drainage or debris can be mistaken for fat or bone within the wound bed [14].
Nurses can quickly differentiate between stages by asking these simple easy-to-understand starter questions. A more detailed assessment should follow.
- Stage 1 versus Stage 2: Is the skin intact?
Rationale: The skin is always intact in Stage 1. The skin is always open in Stage 2 (or there may be an intact blister present).
- Stage 2 versus Stage 3: Is the wound bed pink or beefy red?
Rationale: The wound bed is pink or beefy red in Stage 2. In Stage 3, the wound bed has structures within that may be discolored.
- Stage 3 versus Stage 4: Does the wound bed contain soft or firm structures?
Rationale: The wound bed contains softer structures in Stage 3. The wound bed contains firmer structures in Stage 4.*
- Unstageable versus Stageable: Is any part of the wound bed hidden?
Rationale: The wound bed is not entirely exposed in an unstageable. The wound bed is exposed in a stageable that is open.
- Intact DTI versus Stage 1: Is the discoloration light or dark?
Rationale: The discoloration is dark in a DTI. The discoloration is much lighter in Stage 1.
- Open DTI versus Stage 2: Is the discoloration in or around the wound bed dark?
Rationale: There is dark discoloration in or around the wound bed in an open DTI. In stage 2, the discoloration is much lighter (if even present).
*Nurses should familiarize themselves with the appearance of the various structures that may be present in a wound like fat, fascia, bone, tendon, ligament, etc. Most importantly, nurses should consult the wound care team or health provider if a stage cannot be determined.

Self Quiz
Ask yourself...
- Why should nurses clean a wound prior to staging?
- What should nurses do if unsure how to stage a pressure injury?
What should patients know?
Facilities can use the NIAPH prevention strategies to devise teaching plans for patients [19]. Nurses should educate patients and families/caregivers on risk factors, signs and symptoms, prevention tips, and the importance of following through with treatment.
Nurses should also teach patients to advocate for their own health in order to avoid progression of disease. Here are important tips to teach at any point during the patient’s stay. These tips can apply to nurses working in a variety of settings.
- Tell the nurse or provider of your medical conditions (needed to identify risk factors)
- Tell the nurse or provider if you notice any numbness or tingling in your body (potential risk for sensory deficits)
- Tell the nurse or provider if you have a loss of appetite or trouble eating (potential risk for malnutrition)
- Clean yourself well after using the restroom (maintains skin integrity)
- Tell the nurse or provider if you need to use the restroom or need help with cleaning yourself (maintains skin integrity)
- Tell the nurse right away if you have an incontinence episode (maintains skin integrity)
- Take all prescribed medications (may include necessary antibiotics or wound-healing medications)
- Reposition yourself in bed often or tell the nurse if you need help doing so (reduces immobility risk)
- Tell the nurse or provider if you notice a new discolored area on your skin, or an open area (potential new or worsening pressure injury)
- Tell the nurse or provider if you notice any changes to your wound (potential worsening pressure injury)

Self Quiz
Ask yourself...
- What is one pressure injury prevention tip nurses can teach hospitalized patients?
- What signs or symptoms should nurses teach the patient to report?
Quality Improvement
This section will cover the quality improvement measures in place to reduce pressure injuries.
What is a pressure injury quality improvement initiative?
Quality improvement involves setting goals (or initiatives) and standards of care. The goal of quality improvement is to improve patient outcomes at a systematic level where everyone involved is on the same page.
Although possibly unaware, all care team members are involved in quality improvement. Nursing leaders design, manage, and evaluate program initiatives. Staff nurses and other care team members follow protocols that are often developed from these initiatives.
The Pressure Injury Prevention Program is a guide designed by the AHRQ to help health facilities implement a structured pressure injury prevention initiative based on quality improvement [12]. Facilities can use the guide as a training toolkit to implement a new quality improvement program [5].
Initiative Goals:
- Reduced pressure injury rates
- Reduced adverse events related to pressure injuries
- Reduced costs associated with pressure injuries
- Reduced lawsuits related to pressure injuries
Ways facilities can implement a prevention program:
- Address the overall objectives of the prevention program
- Identify the needs for change and how to redesign practice
- Develop goals and plans for change
- Use the NIAPH pressure injury prevention recommended practices
- Establish comprehensive skin assessment protocols
- Standardize assessments of pressure injury risk factors
- Incorporate risk factors into individualized care planning
- Establish clear staff and leadership roles

Self Quiz
Ask yourself...
- What is one reason why a health facility would start or update a pressure injury prevention program?
- When pressure injury rates are reduced, what else can health facilities expect to improve as well?
What are some pressure injury quality measures?
Quality measures are tools that measure a system’s healthcare goals and/or ability to provide high-quality care [11]. In simple terms, quality measures are specific ways that systems (governments, states, organizations, etc.) can show how they are making progress in meeting goals. The AHRQ highlights the following three ways the U.S. measures its progress.
Number of HAPIs
The AHRQ measures the number of HAPIs per year. The most recent data is from 2014 to 2017 [6].
| Year | Number of HAPIs |
| 2014 | 647,000 |
| 2015 | 700,000 |
| 2016 | 677,000 |
| 2017 | 683,000 |
Rate of HAPIs per admission
The AHRQ measures the number of HAPIs per admission related to age groups. The number is measured as a “rate,” meaning the number of HAPIs per 1,000 hospital admissions. The most recent evidence is from 2017 [4].
| Age group | Number of HAPIs per 1,000 admissions |
| 18 – 39 | 0.38 |
| 40 – 64 | 0.63 |
| 65 – 74 | 0.74 |
| 75 and over | 0.71 |
Costs of HAPIs
Another quality measure is HAPI costs. While the AHRQ does not measure costs of HAPIs every single year, the most recent data is from 2017 [3].
| Year | Cost of HAPIs per patient |
| 2017 | $8,573 – $21,075 |
Deaths related to HAPIs
Patient mortality rates related to HAPIs are a quality measure (calculated per 1,000 pressure injury cases). The most recent data is from 2017 [6].
| Year | Number of deaths per 1,000 pressure injury cases |
| 2017 | 2.42 – 5.06 |

Self Quiz
Ask yourself...
- What is one way a health facility can show its progress in preventing pressure injuries?
- What patient age range do you think has the most pressure injury rates? Age 65 to 74 or age 75 and over?
Conclusion
Pressure injuries are complex conditions that can lead to poor patient outcomes and a burdened healthcare system. The best strategy in the care of patients with pressure injuries or those at risk is prevention.
However, preventing these injuries involves more than individual nurses taking specific steps. Prevention of pressure injuries involves a team effort from all members of the care team and a systemic plan for improvement.
Controlled Substances
Introduction
Pain is complex and subjective. The experience of pain can significantly impact an individual’s quality of life. According to the National Institute of Health (NIH) (40), pain is the most common complaint in a primary care office, with 20% of all patients reporting pain. Chronic pain is the leading cause of disability, and effective pain management is crucial to health and well-being, particularly when it improves functional ability. Effective pain treatment starts with a comprehensive, empathic assessment and a desire to listen and understand. Nurse Practitioners are well-positioned to fill a vital role in providing comprehensive and empathic patient care, including pain management (23).
While the incidence of chronic pain has remained a significant problem, how clinicians manage pain has significantly changed in the last decade, primarily due to the opioid epidemic. This education aims to discuss pain and the assessment of pain, federal guidelines for prescribing, the opioid epidemic, addiction and diversion, and recommendations for managing pain.
Definition of Pain
Understanding the definition of pain, differentiating between various types of pain, and recognizing the descriptors patients use to communicate their pain experiences are essential for Nurse practitioners involved in pain management. By understanding the medical definition of pain and how individuals may communicate it, nurse practitioners can differentiate varying types of pain to target assessment.
According to the International Association for the Study of Pain (27), pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or terms of described such in damage.” The IASP, in July 2020, expanded its definition of pain to include context further.
Their expansion is summarized below:
- Pain is a personal experience influenced by biological, psychological, and social factors.
- Pain cannot be inferred solely from activity in sensory neurons.
- Individuals learn the concept of pain through their life experiences.
- A person’s report of an experience in pain should be respected.
- Pain usually serves an adaptive role but may adversely affect function and social and psychological well-being.
- The inability to communicate does not negate the possibility of the experience of pain.


Self Quiz
Ask yourself...
- Analyze how changes to the definition of pain may affect your practice.
- Discuss how you manage appointment times, knowing that 20% of your scheduled patients may seek pain treatment.
- How does the approach to pain management change in the presence of a person with a disability?
Types of Pain
Pain originates from different mechanisms, causes, and areas of the body. As a nurse practitioner, understanding the type of pain a patient is experiencing is essential for several reasons (23).
- Determining an accurate diagnosis. This kind of pain can provide valuable clues to the underlying cause or condition.
- Creating a treatment plan. Different types of pain respond better to specific treatments or interventions.
- Developing patient education. A nurse practitioner can provide targeted education to patients about their condition, why they may experience the pain as they do, its causes, and treatment options. Improving the patient's knowledge and control over their condition improves outcomes.
Acute Pain
Acute pain is typically short-lived and is a protective response to an injury or illness. Patients are usually able to identify the cause. This type of pain resolves as the underlying condition improves or heals (12).
Chronic Pain
Chronic pain is diagnosed when it continues beyond the expected healing time. Pain is defined as chronic when it persists for longer than three months. It may result from an underlying disease or injury or develop without a clear cause. Chronic pain often significantly impacts a person's physical and emotional well-being, requiring long-term management strategies. The prolonged experience of chronic pain usually indicates a central nervous system component of pain that may require additional treatment. Patients with centralized pain often experience allodynia or hyperalgesia (12).
Allodynia is pain evoked by a stimulus that usually does not cause pain, such as a light touch. Hyperalgesia is the effect of a heightened pain response to a stimulus that usually evokes pain (12).
Nociceptive Pain
Nociceptive pain arises from activating peripheral nociceptors, specialized nerve endings that respond to noxious stimuli. This type of pain is typically associated with tissue damage or inflammation and is further classified into somatic and visceral pain subtypes.
Somatic pain is most common and occurs in muscles, skin, or bones; patients may describe it as sharp, aching, stiffness, or throbbing.
Visceral pain occurs in the internal organs, such as indigestion or bowel spasms. It is more vague than somatic pain; patients may describe it as deep, gnawing, twisting, or dull (12).
Neuropathic pain
Neuropathic pain is a lesion or disease of the somatosensory nervous system. Examples include trigeminal neuralgia, painful polyneuropathy, postherpetic neuralgia, and central poststroke pain (10).
Neuropathic pain may be ongoing, intermittent, or spontaneous pain. Patients often describe neuropathic pain as burning, prickling, or squeezing quality. Neuropathic pain is a common chronic pain. Patients commonly describe allodynia and hyperalgesia as part of their chronic pain experience (10).
Affective pain
Affective descriptors reflect the emotional aspects of pain and include terms like distressing, unbearable, depressing, or frightening. These descriptors provide insights into the emotional impact of pain on an individual's well-being (12).

Self Quiz
Ask yourself...
- How can nurse practitioners effectively elicit patient descriptors to accurately assess the type of pain the patient is experiencing?
- Expand on how pain descriptors can guide interventions even if the cause is not yet determined.
- What strategies ensure patients feel comfortable describing their pain, particularly regarding subjective elements such as quality and location?
Case Study
Mary Adams is a licensed practical nurse who has just relocated to town. Mary will be the utilization review nurse at a local long-term care facility. Mary was diagnosed with Postherpetic Neuralgia last year, and she is happy that her new job will have her mostly doing desk work and not providing direct patient care as she had been before the relocation. Mary was having difficulty at work at her previous employer due to pain. She called into work several times, and before leaving, Mary's supervisor had counseled her because of her absences.
Mary wants to establish primary care immediately because she needs ongoing pain treatment. She is hopeful that, with her new job and pain under control, she will be able to continue a successful career in nursing. When Mary called the primary care office, she specifically requested a nurse practitioner as her primary care provider because she believes that nurse practitioners tend to spend more time with their patients.
Assessment
The assessment effectively determines the type of treatment needed, the options for treatment, and whether the patient may be at risk for opioid dependence. Since we know that chronic pain can lead to disability and pain has a high potential to negatively affect the patient's ability to work or otherwise, be productive, perform self-care, and potentially impact family or caregivers, it is imperative to approach the assessment with curiosity and empathy. This approach will ensure a thorough review of pain and research on pain management options. Compassion and support alone can improve patient outcomes related to pain management (23).
Record Review
Regardless of familiarity with the patient, reviewing the patient's treatment records is essential, as the ability to recall details is unreliable. Reviewing the records can help identify subtle changes in pain description and site, the patient's story around pain, failed modalities, side effects, and the need for education, all impacting further treatment (23).
Research beforehand the patient's current prescription and whether or not the patient has achieved the maximum dosage of the medication. Analysis of the patient's past prescription could reveal a documented failed therapy even though the patient did not receive the maximum dose (23).
A review of documented allergens may indicate an allergy to pain medication. Discuss with the patient the specific response to the drug to determine if it is a true allergy, such as hives or anaphylaxis, or if the response may have been a side effect, such as nausea and vomiting.
Research whether the patient tried any non-medication modalities for pain, such as physical therapy (PT), occupational therapy (OT), or Cognitive Behavioral Therapy (CBT). Note any non-medication modalities documented as failed therapies. The presence of any failed therapies should prompt further discussion with the patient, family, or caregiver about the experience. The incompletion of therapy should not be considered failed therapy. Explore further if the patient abandoned appointments.
Case Study
You review the schedule for the week, and there are three new patient appointments. One is Mary Adams. The interdisciplinary team requested and received Mary's treatment records from her previous primary care provider. You make 15 minutes available to review Mary's records and the questionnaire Mary filled out for her upcoming appointment. You see that Mary has been diagnosed with Postherpetic Neuralgia and note her current treatment regimen, which she stated was ineffective. You write down questions you will want to ask Mary. You do not see evidence of non-medication modalities or allergies to pain medication.

Self Quiz
Ask yourself...
- What potential risks or complications can arise from neglecting to conduct a thorough chart review before initiating a pain management assessment?
- In your experience, what evidence supports reviewing known patient records?
- What is an alternative to reviewing past treatment if records are not available?
Pain Assessment
To physically assess pain, several acronyms help explore all the aspects of the patient's experience. Acronyms commonly used to assess pain are SOCRATES, OLDCARTS, and COLDERAS. These pain assessment acronyms are also helpful in determining treatment since they include a character and duration of pain assessment (23).
| O-Onset | S-Site | C-Character |
| L-Location | O-Onset | O-Onset |
| D-Duration | C-Character | L-Location |
| C-Character | R-Radiate | D-Duration |
| A-Alleviating | A-Associated symptoms | E-Exacerbating symptoms |
| R-Radiating, relieving | T-Time/Duration | R-Relieving, radiating |
| T-Temporal patterns (frequency) | E-Exacerbating | A-Associated symptoms |
| S-Symptoms | S-Severity | S-Severity of illness |
Inquire where the patient is feeling pain. The patient may have multiple areas and types of pain. Each type and location must be explored and assessed. Unless the pain is from a localized injury, a body diagram map, as seen below, is helpful to document, inform, and communicate locations and types of pain. In cases of Fibromyalgia, rheumatoid arthritis, or other centralized or widespread pain, it is vital to inquire about radiating pain. The patient with chronic pain could be experiencing acute pain or a new pain site, such as osteoarthritis, that may need further evaluation and treatment (23).
Inquire with the patient how long their pain has been present and any associated or known causative factors. Pain experienced longer than three months defines chronic versus acute pain. Chronic pain means that the pain is centralized or a function of the Central Nervous system, which should guide treatment decisions.
To help guide treatment, ask the patient to describe their pain. The description helps identify what type of pain the patient is experiencing: Allodynia and hyperalgesia indicate centralized pain; sharp, shooting pain could indicate neuropathic pain. Have the patient rate their pain. There are various tools, as shown below, for pain rating depending on the patient's ability to communicate. Not using the pain rating number alone is imperative. Ask the patient to compare the severity of pain to a previous experience. For example, a 1/10 may be experienced as a bumped knee or bruise, whereas a 10/10 is experienced on the level of a kidney stone or childbirth (23).
Besides the 0-10 rating scale and depending on the patient's needs, several pain rating scales are appropriate. They are listed below.
The 0-5 and Faces scales may be used for all adult patients and are especially effective for patients experiencing confusion.
The Defense and Veterans Pain Rating Scale (DVPRS) is a five-item tool that assesses the impact of pain on sleep, mood, stress, and activity levels (20).
For patients unable to self-report pain, such as those intubated in the ICU or late-stage neurological diseases, the FLACC scale is practical. The FLACC scale was initially created to assess pain in infants. Note: The patient need not cry to be rated 10/10.
| Behavior | 0 | 1 | 2 |
| Face | No particular expression or smile | Occasional grimace or frown, withdrawn, disinterested | Frequent or constant quivering chin, clenched jaw |
| Legs | Normal position or relaxed | Uneasy, restless, tense | Kicking or legs drawn |
| Activity | Lying quietly, in a normal position, or relaxed | Squirming, shifting back and forth, tense | Arched, rigid, or jerking |
| Cry | No cry wake or asleep | Moans or whimpers: occasional complaints | Crying steadily, screams, sobs, frequent complaints |
| Consolability | Content, relaxed | Distractable, reassured by touching, hugging, or being talked to | Difficult to console or comfort |
(21).
Assess contributors to pain such as insomnia, stress, exercise, diet, and any comorbid conditions. Limited access to care, socioeconomic status, and local culture also contribute to the patient's experience of pain (23). Most patients have limited opportunity to discuss these issues, and though challenging to bring up, it is compassionate and supportive care. A referral to social work or another agency may be helpful if you cannot explore it fully.
Assess for substance abuse disorders, especially among male, younger, less educated, or unemployed adults. Substance abuse disorders increase the likelihood of misuse disorder and include alcohol, tobacco, cannabis, cocaine, and heroin (29).
Inquire as to what changes in function the pain has caused. One question to ask is, "Were it not for pain, what would you be doing?" As seen below, a Pain, Enjoyment, and General Activity (PEG) three-question scale, which focuses on function and quality of life, may help determine the severity of pain and the effect of treatment over time.
| What number best describes your pain on average in the past week? 0-10 |
| What number best describes how, in the past week, pain has interfered with your enjoyment of life? 0-10 |
| What number determines how, in the past week, pain has interfered with your general activity? 0-10 |
(21).
Assess family history, mental health disorders, chronic pain, or substance abuse disorders. Each familial aspect puts patients at higher risk for developing chronic pain (23).
Evaluate for mental health disorders the patient may be experiencing, particularly anxiety and depression. The Patient Health Questionnaire (PHQ4) is a four-question tool for assessing depression and anxiety.
In some cases, functional MRI or imaging studies effectively determine the cause of pain and the treatment. If further assessment is needed to diagnose and treat pain, consult Neurology, Orthopedics, Palliative care, and pain specialists (23).
Case Study
You used OLDCARTS to evaluate Mary's pain and completed a body diagram. Mary is experiencing allodynia in her back and shoulders, described as burning and tingling. It is exacerbated when she lifts, such as moving patients at the long-term care facility and, more recently, boxes from her move to the new house. Mary has also been experiencing anxiety due to fear of losing her job, the move, and her new role. She has moved closer to her family to help care for her children since she often experiences fatigue. Mary has experienced a tumultuous divorce in the last five years and feels she is still undergoing some trauma.
You saw in the chart that Mary had tried Gabapentin 300 mg BID for her pain and inquired what happened. Mary explained that her pain improved from 8/10 to 7/10 and had no side effects. Her previous care provider discontinued the medication and documented it as a failed therapy. You reviewed the minimum and maximum dosages of Gabapentin and know Mary can take up to 1800mg/day.
During the assessment, Mary also described stiffness and aching in her left knee. She gets a sharp pain when she walks more than 500 steps, and her knee is throbbing by the end of the day. Mary rated the pain a 10/10, but when she compared 10/10 to childbirth, Mary said her pain was closer to 6/10. Her moderate knee pain has reduced Mary's ability to exercise. She used to like to take walks. Mary stated she has had knee pain for six months and has been taking Ibuprofen 3 – 4 times daily.
Since Mary's pain is moderate, you evaluate your options of drugs for moderate to severe pain.


Self Quiz
Ask yourself...
- How do you assess and evaluate a patient's pain level?
- What are the different types of pain and their management strategies?
- How do you determine the appropriate dosage of pain medications for a patient?
- How do you assess the effectiveness of pain medications in your patients?
- How do you adjust medication dosages for elderly patients with pain or addiction?
- How do you address the unique challenges in pain management for pediatric patients?
- What is the role of non-pharmacological interventions in pain management?
- How do you incorporate non-pharmacological interventions into your treatment plans?
Opioid Classifications and Drug Schedules
A comprehensive understanding of drug schedules and opioid classifications is essential for nurse practitioners to ensure patient safety, prevent drug misuse, and adhere to legal and regulatory requirements. Nurse practitioners with a comprehensive understanding of drug schedules and opioid classifications can effectively communicate with colleagues, ensuring accurate medication reconciliation and facilitating interdisciplinary care. Nurse practitioners’ knowledge in facilitating discussions with pharmacists regarding opioid dosing, potential interactions, and patient education is essential (49).
Drug scheduling became mandated under the Controlled Substance Act. The Drug Enforcement Agency (DEA) Schedule of Controlled Drugs and the criteria and common drugs are listed below.
|
Schedule |
Criteria | Examples |
|
I |
No medical use; high addiction potential |
Heroin, marijuana, PCP |
|
II |
Medical use; high addiction potential |
Morphine, oxycodone, Methadone, Fentanyl, amphetamines |
|
III |
Medical use; high addiction potential |
Hydrocodone, codeine, anabolic steroids |
|
IV |
Medical use, low abuse potential |
Benzodiazepines, meprobamate, butorphanol, pentazocine, propoxyphene |
| V | Medical use; low abuse potential |
Buprex, Phenergan with codeine |
(Pain Physician, 2008)
Listed below are drugs classified by their schedule and mechanism of action. "Agonist" indicates a drug that binds to the opioid receptor, causing pain relief and also euphoria. An agonist-antagonist indicates the drug binds to some opioid receptors but blocks others. Mixed antagonist-agonist drugs control pain but have a lower potential for abuse and dependence than agonists (7).
| Schedule I | Schedule II | Schedule III | Schedule IV | Schedule V | |
| Opioid agonists |
BenzomorphineDihydromor-phone, Ketobemidine, Levomoramide, Morphine-methylsulfate, Nicocodeine, Nicomorphine, Racemoramide |
Codeine, Fentanyl, Sublimaze, Hydrocodone, Hydromorphone, Dilaudid, Meperidine, Demerol, Methadone, Morphine, Oxycodone, Endocet, Oxycontin, Percocet, Oxymorphone, Numorphan |
Buprenorphine Buprenex, Subutex, Codeine compounds, Tylenol #3, Hydrocodone compounds, Lortab, Lorcet, Tussionex, Vicodin |
Propoxyphene, Darvon, Darvocet | Opium, Donnagel, Kapectolin |
| Mixed Agonist -Antagonist | BuprenorphineNaloxone, Suboxone |
Pentazocine, Naloxone, Talwin-Nx |
|||
| Stimulants | N-methylampheta-mine 3, 4-methylenedioxy amphetamine, MDMA, Ecstacy | Amphetamine, Adderal, Cocaine, Dextroamphetamine, Dexedrine, Methamphetamine, Desoxyn, Methylphenidate, Concerta, Metadate, Ritalin, Phenmetrazine, Fastin, Preludin | Benapheta-mine, Didrex, Pemolin, Cylert, Phendimetra-zine, Plegine | Diethylpropion, Tenuate, Fenfluramine, Phentermine Fastin | 1-dioxy-ephedrine-Vicks Inhaler |
| Hallucinogen-gens, other | Lysergic Acid Diamine LSD, marijuana, Mescaline, Peyote, Phencyclidine PCP, Psilocybin, Tetrahydro-cannabinol | Dronabinol, Marinol | |||
| Sedative Hypnotics |
Methylqualine, Quaalude, Gamma-hydroxy butyrate, GHB
|
Amobarbitol, Amytal, Glutethamide, Doriden, Pentobarbital, Nembutal, Secobarbital, Seconal |
Butibarbital. Butisol, Butilbital, Florecet, Florinal, Methylprylon, Noludar |
Alprazolam, Xanax, Chlordiazepoxide, Librium, Chloral betaine, Chloral hydrate, Noctec, Chlorazepam, Clonazepam, Klonopin, Clorazopate, Tranxene, Diazepam, Valium, Estazolam, Prosom, Ethchlorvynol, Placidyl, Ethinamate, Flurazepam, Dalmane, Halazepam, Paxipam, Lorazepam, Ativan, Mazindol, Sanorex, Mephobarbital, Mebaral, Meprobamate, Equanil, Methohexital, Brevital Sodium, Methyl-phenobarbital, Midazolam, Versed, Oxazepam, Serax, Paraldehyde, Paral, Phenobarbital, Luminal, Prazepam, Centrax, Temazepam, Restoril, Triazolam, Halcion, Sonata, Zolpidem, Ambien |
Diphenoxylate preparations, Lomotil |
(41).

Self Quiz
Ask yourself...
- What are the potential risks and benefits of using opioids for pain management?
- How can nurse practitioners effectively monitor patients on long-term opioid therapy?
- What are the potential risks and benefits of using long-acting opioids for chronic pain?
- How do you monitor patients on long-acting opioids for safety and efficacy?
Commonly Prescribed Opioids, Indications for Use, and Typical Side Effects
Opioid medications are widely used for managing moderate to severe pain. Referencing NIDA (2023), this section aims to give healthcare professionals an overview of the indications and typical side effects of commonly prescribed Schedule II opioid medications, including hydrocodone, oxycodone, morphine, Fentanyl, and hydromorphone.
Opioids are derived and manufactured in several ways. Naturally occurring opioids come directly from the opium poppy plant. Synthetic opioids are manufactured by chemically synthesizing compounds that mimic the effects of a natural opioid. Semi-synthetic is a mix of naturally occurring and man-made (35).
Understanding the variations in how an opioid is derived and manufactured is crucial in deciding the type of opioid prescribed, as potency and analgesic effects differ. Synthetic opioids are often more potent than naturally occurring opioids. Synthetic opioids have a longer half-life and slower elimination, affecting the duration of action and timing for dose adjustments. They are also associated with a higher risk of abuse and addiction (38).
Hydrocodone
Mechanism of Action and Metabolism
Hydrocodone is a Schedule II medication. It is an opioid agonist and works as an analgesic by activating mu and kappa opioid receptors located in the central nervous system and the enteric plexus of the bowel. Agonist stimulation of the opioid receptors inhibits nociceptive neurotransmitters' release and reduces neuronal excitability (17).
- Produces analgesia.
- Suppresses the cough reflex at the medulla.
- Causes respiratory depression at higher doses.
Hydrocodone is indicated for treating severe pain after nonopioid therapy has failed. It is also indicated as an antitussive for nonproductive cough in adults over 18.
Available Forms
Hydrocodone immediate release (IR) reaches maximum serum concentrations in one hour with a half-life of 4 hours. Extended-release (ER) Hydrocodone reaches peak concentration at 14-16 hours and a half-life of 7 to 9 hours. Hydrocodone is metabolized to an inactive metabolite in the liver by cytochrome P450 enzymes CYP2D6 and CYP3A4. Hydrocodone is converted to hydromorphone and is excreted renally. Plasma concentrations of hydromorphone are correlated with analgesic effects rather than hydrocodone.
Hydrocodone is formulated for oral administration into tablets, capsules, and oral solutions. Capsules and tablets should never be crushed, chewed, or dissolved. These actions convert the extended-release dose into immediate release, resulting in uncontrolled and rapid release of opioids and possible overdose.
Dosing and Monitoring
Hydrocodone IR is combined with acetaminophen or ibuprofen. The dosage range is 2.5mg to 10mg every 4 to 6 hours. If formulated with acetaminophen, the dosage is limited to 4gm/day.
Hydrocodone ER is available as tablets and capsules. Depending on the product, the dose of hydrocodone ER formulations in opioid-naïve patients is 10 to 20 mg every 12 to 24 hours.
Nurse practitioners should ensure patients discontinue all other opioids when starting the extended-release formula.
Side Effects and Contraindications
Because mu and kappa opioid receptors are in the central nervous system and enteric plexus of the bowel, the most common side effects of hydrocodone are constipation and nausea (>10%).
Other adverse effects of hydrocodone include:
- Respiratory: severe respiratory depression, shortness of breath
- Cardiovascular: hypotension, bradycardia, peripheral edema
- Neurologic: Headache, chills, anxiety, sedation, insomnia, dizziness, drowsiness, fatigue
- Dermatologic: Pruritus, diaphoresis, rash
- Gastrointestinal: Vomiting, dyspepsia, gastroenteritis, abdominal pain
- Genitourinary: Urinary tract infection, urinary retention
- Otic: Tinnitus, sensorineural hearing loss
- Endocrine: Secondary adrenal insufficiency (17)
Hydrocodone, being an agonist, must not be taken with other central nervous system depressants as sedation and respiratory depression can result. In formulations combined with acetaminophen, hydrocodone can increase the international normalized ratio (INR) and cause bleeding. Medications that induce or inhibit cytochrome enzymes can lead to wide variations in absorption.
The most common drug interactions are listed below:
- Alcohol
- Benzodiazepines
- Barbiturates
- other opioids
- rifampin
- phenytoin
- carbamazepine
- cimetidine,
- fluoxetine
- ritonavir
- erythromycin
- diltiazem
- ketoconazole
- verapamil
- Phenytoin
- John’s Wort
- Glucocorticoids
Considerations
Use with caution in the following:
- Patients with Hepatic Impairment: Initiate 50% of the usual dose
- Patients with Renal Impairment: Initiate 50% of the usual dose
- Pregnancy: While not contraindicated, the FDA issued a black-boxed warning since opioids cross the placenta, and prolonged use during pregnancy may cause neonatal opioid withdrawal syndrome (NOWS).
- Breastfeeding: Infants are susceptible to low dosages of opioids. Non-opioid analgesics are preferred.
Pharmacogenomic: Genetic variants in hydrocodone metabolism include ultra-rapid, extensive, and poor metabolizer phenotypes. After administration of hydrocodone, hydromorphone levels in rapid metabolizers are significantly higher than in poor metabolizers.
Oxycodone
Mechanism of Action and Metabolism
Oxycodone has been in use since 1917 and is derived from Thebaine. It is a semi-synthetic opioid analgesic that works by binding to mu-opioid receptors in the central nervous system. It primarily acts as an agonist, producing analgesic effects by inhibiting the transmission of pain signals (Altman, Clark, Huddart, & Klein, 2018).
Oxycodone is primarily metabolized in the liver by CYP3A4/5. It is metabolized in the liver to noroxycodone and oxymorphone. The metabolite oxymorphone also has an analgesic effect and does not inhibit CYP3A4/5. Because of this metabolite, oxycodone is more potent than morphine, with fewer side effects and less drug interactions. Approximately 72% of oxycodone is excreted in urine (Altman, Clark, Huddart, & Klein, 2018).
Available Forms
Oxycodone can be administered orally, rectally, intravenously, and as an epidural. For this sake, we will focus on immediate-release and extended-release oral formulations.
- Immediate-release (IR) tablets
- IR capsules
- IR oral solutions
- Extended-release (ER) tablets
Dosing and Monitoring
The dosing of oxycodone should be individualized based on the patient's pain severity, previous opioid exposure, and response. Initial dosages for opioid naïve patients range from 5-15 mg for immediate-release formulations, while extended-release formulations are usually initiated at 10-20 mg. Dosage adjustments may be necessary based on the patient's response, but caution should be exercised. IR and ER formulations reach a steady state at 24 hours and titrating before 24 hours may lead to overdose.
Regular monitoring is essential to assess the patient's response to treatment, including pain relief, side effects, and signs of opioid misuse or addiction. Monitoring should include periodic reassessment of pain intensity, functional status, and adverse effects (Altman, Clark, Huddart, & Klein, 2018).
Side Effects and Contraindications
Common side effects of oxycodone include:
- constipation
- nausea
- sedation
- dizziness
- respiratory depression
- respiratory arrest
- hypotension
- fatal overdose
Oxycodone is contraindicated in patients with known hypersensitivity to opioids, severe respiratory depression, paralytic ileus, or acute or severe bronchial asthma. It should be used cautiously in patients with a history of substance abuse, respiratory conditions, liver or kidney impairment, and those taking other medications that may interact with opioids, such as alcohol (4).
It is also contraindicated with the following medications and classes:
- Antifungal agents
- Antibiotics
- Rifampin
- Carbamazepine
- Fluoxetine
- Paroxetine
Considerations
- Nurse practitioners should consider the variations in the mechanism of action for the following:
- Metabolism differs between males and females: females have been shown to have less concentration of oxymorphone and more CYP3A4/5 metabolites.
- Infants have reduced clearance of oxycodone, increasing side effects.
- Pediatrics have 20-40% increased clearance over adults.
- Reduced clearance with age increases the half-life of oxycodone.
- Pregnant women have a greater clearance and reduced half-life.
- Impairment of the liver reduces clearance.
- Cancer patients with cachexia have increased exposure to oxycodone and its metabolite.
- Maternal and neonate concentrations are similar, indicating placenta crossing (4)
Morphine

Mechanism of Action and Metabolism
Morphine is a naturally occurring opioid alkaloid extracted from the opium poppy. It was isolated in 1805 and is the opioid against which all others are compared. Morphine binds to mu-opioid receptors in the brain and spinal cord, inhibiting the transmission of pain signals and producing analgesia. It is a first-line choice of opioid for moderate to severe acute, postoperative, and cancer-related pain (8).
Morphine undergoes first-pass metabolism in the liver and gut. It is well absorbed and distributed throughout the body. Its main metabolites are morphine-3-glucuronide and morphine-6-glucuronide. Its mean plasma elimination half-life after intravenous administration is about 2 hours. Approximately 90% of morphine is excreted in the urine within 24 hours (8).
Available Forms
Morphine is available in various forms, including.
- immediate-release tablets
- extended release tablets
- oral IR solutions
- injectable solutions
- transdermal patches
Dosing and Monitoring
Morphine is hydrophilic and, as such, has a slow onset time. The advantage of this is that it is unlikely to cause acute respiratory depression even when injected. However, because of the slow onset time, there is more likelihood of morphine overdose due to the ability to “stack” doses in patients experiencing severe pain (Bistas, Lopez-Ojeda, & Ramos-Matos, 2023).
The dosing of morphine depends on the patient's pain severity, previous opioid exposure, and other factors. It is usually initiated at a low dose and titrated upwards as needed. Monitoring pain relief, adverse effects, and signs of opioid toxicity is crucial. Reevaluate benefits and harms with patients within 1 to 4 weeks of starting opioid therapy or of dose escalation. General recommendations for initiating morphine (Bistas, Lopez-Ojeda, & Ramos-Matos, 2023).
Prescribe IR opioids instead of ER opioids.
Prescribe the lowest effective dosage, below 50 Morphine Milligram Equivalents (MME) /day.
Side Effects and Contraindications
Because morphine binds to opioid receptors in the brain and spinal cord, is metabolized in the liver and gut, and has a slow onset, the following side effects are common:
- Constipation
- Nausea
- Vomiting
- Sedation
- Dizziness
- Respiratory depression
- Pruritis
- Sweating
- Dysphoria/Euphoria
- Dry mouth
- Anorexia
- Spasms of urinary and biliary tract
Contraindications of morphine are:
- Known hypersensitivity or allergy to morphine.
- Bronchial asthma or upper airway obstruction
- Respiratory depression in the absence of resuscitative equipment
- Paralytic ileus
- Risk of choking in patients with dysphagia, including infants, children, and the elderly (8)
Concurrent use with other sedating medications: Amitriptyline, diazepam, haloperidol, chlorpromazine
Morphine interacts with the following medications:
- Ciprofloxacin
- Metoclopramide
- Ritonavir
Considerations for Nurse Practitioners
Assess for medical conditions that may pose serious and life-threatening risks with opioid use, such as the following:
- Sleep-disordered breathing, such as sleep apnea.
- Pregnancy
- Renal or hepatic insufficiency
- Age >= 65
- Certain mental health conditions
- Substance use disorder
- Previous nonfatal overdose
Fentanyl
Mechanism of Action and Metabolism
Fentanyl is a synthetic opioid more potent than morphine and was approved in 1968. Fentanyl is an agonist that works by binding to the mu-opioid receptors in the central nervous system. This binding inhibits the transmission of pain signals, resulting in analgesia. Fentanyl is often used for severe pain management, particularly in the perioperative and palliative care settings, or for severe pain in patients with Hepatic failure (8).
It is a mu-selective opioid agonist. However, it can activate other opioid receptors in the body, such as the delta and kappa receptors, producing analgesia. It also activates the Dopamine center of the brain, stimulating relaxation and exhilaration, which is responsible for its high potential for addiction (8).
Indications for fentanyl are as follows:
- Preoperative analgesia
- Anesthesia adjunct
- Regional anesthesia adjunct
- General anesthesia
- Postoperative pain control
- Moderate to severe acute pain (off-label)
Available Forms
- Fentanyl is available in various forms, including:
- transdermal patches
- injectable solutions
- lozenges
- nasal sprays
- oral tablets (8)
Dosing and Monitoring
Fentanyl is metabolized via the CYP3A4 enzyme in the liver. It has a half-life of 3 to 7 hours, and 75% of Fentanyl is excreted in the urine and 9% in feces.
The dosing of fentanyl depends on the route of administration and the patient's needs. For example, transdermal patches are typically applied every 72 hours, while injectable solutions are titrated to achieve the desired analgesic effect. Monitoring should include assessing pain levels, respiratory rate, blood pressure, and sedation scores (8).
Fentanyl is most dosed as follows:
- Post-operative pain control
- 50 to 100 mcg IV/IM every 1 to 2 hours as needed; alternately 0.5 to 1.5 mcg/kg/hour IV as needed. Consider lower dosing in patients 65 and older.
PCA (patient-controlled analgesia): 10 to 20 mcg IV every 6 to 20 minutes as needed; start at the lowest effective dose for the shortest effective duration - refer to institutional protocols (8).
Moderate to severe acute pain (off-label) 1 to 2 mcg/kg/dose intranasally each hour as needed; the maximum dose is 100 mcg. Use the lowest effective dose for the shortest effective duration (8).
Side Effects and Contraindications
Common side effects of fentanyl include:
- respiratory depression
- sedation
- constipation
- nausea
- vomiting
- euphoria
- confusion
- respiratory depression/arrest
- visual disturbances
- dyskinesia
- hallucinations
- delirium
- narcotic ileus
- muscle rigidity
- addiction
- loss of consciousness
- hypotension
- coma
- death (8).
The use of fentanyl is contraindicated in patients in the following situations:
- After operative interventions in the biliary tract, these may slow hepatic elimination of the drug.
- With respiratory depression or obstructive airway diseases (i.e., asthma, COPD, obstructive sleep apnea, obesity hyperventilation, also known as Pickwickian syndrome)
- With liver failure
- With known intolerance to fentanyl or other morphine-like drugs, including codeine or any components in the formulation.
- With known hypersensitivity (i.e., anaphylaxis) or any common drug delivery excipients (i.e., sodium chloride, sodium hydroxide) (8).
Considerations for Nurse Practitioners
Nurse practitioners prescribing fentanyl should thoroughly assess the patient's pain, medical history, and potential risk factors for opioid misuse. They should also educate patients about the proper use, storage, and disposal of fentanyl. It should be used cautiously in patients with respiratory disorders, liver or kidney impairment, or a history of substance abuse. Fentanyl is contraindicated in patients with known hypersensitivity to opioids and those without exposure to opioids.
Alcohol and other drugs, legal or illegal, can exacerbate fentanyl's side effects, creating multi-layered clinical scenarios that can be complex to manage. These substances, taken together, generate undesirable conditions that complicate the patient's prognosis (8).
Hydromorphone
Mechanism of Action and Metabolism
Hydromorphone is a semi-synthetic opioid derived from morphine. It binds to the mu-opioid receptors in the central nervous system. It primarily exerts its analgesic effects by inhibiting the release of neurotransmitters involved in pain transmission, thereby reducing pain perception. Hydromorphone also exerts its effects centrally at the medulla level, leading to respiratory depression and cough suppression (1).
Hydromorphone is indicated for:
- moderate to severe acute pain
- severe chronic pain
- refractory cough suppression (off-label) (1)
Available Forms
Hydromorphone is available in various forms, depending on the patient’s needs and severity of pain.
- immediate-release tablet
- extended release tablets
- oral liquid
- injectable solution
- rectal suppositories
Dosing and Monitoring
The immediate-release oral formulations of hydromorphone have an onset of action within 15 to 30 minutes. Peak levels are typically between 30 and 60 minutes with a half-life of 2 to 3 hours. Hydromorphone is primarily excreted through the urine.
The dosing of hydromorphone should be individualized based on the patient's pain intensity, initiated at the lowest effective dose, and adjusted gradually as needed. Close monitoring of pain relief, adverse effects, and signs of opioid toxicity is essential. Patients should be assessed regularly to ensure they receive adequate pain control without experiencing excessive sedation or respiratory depression.
The following are standard dosages that should only be administered when other opioid and non-opioid options fail.
- Immediate-release oral solutions dosage: 1 mg/1 mLoral tablets are available in 2 mg, 4 mg, and 8 mg.
- Extended-release oral tablets are available in dosages of 8 mg, 12 mg, 16 mg, and 32 mg.
- Injection solutions are available in concentrations of 1 mg/mL, 2 mg/mL, 4 mg/mL, and 10 mg/mL.
- Intravenous solutions are available in strengths of 2 mg/1 mL, 2500 mg/250 mL, ten mg/1 mL, and 500 mg/50 mL.
- Suppositories are formulated at a strength of 3 mg (1).
Side Effects and Contraindications
Hydromorphone has potential adverse effects on several organ systems, including the integumentary, gastrointestinal, neurologic, cardiovascular, endocrine, and respiratory.
Common side effects of hydromorphone include:
- Constipation
- Nausea
- Vomiting
- Dizziness
- Sedation
- respiratory depression
- pruritus
- headache
- Somnolence
- Severe adverse effects of hydromorphone include:
- Hypotension
- Syncope
- adrenal insufficiency
- coma
- raised intracranial pressure.
- seizure
- suicidal thoughts
- apnea
- respiratory depression or arrest
- drug dependence or withdrawal
- neonatal drug withdrawal syndrome
- Hydromorphone is contraindicated in patients with:
- known allergies to the drug, sulfites, or other components of the formulation.
- known hypersensitivity to opioids.
- severe respiratory depression
- paralytic ileus
- acute or severe bronchial asthma (1).
Caution should be exercised in patients with:
- respiratory insufficiency
- head injuries
- increased intracranial pressure.
- liver or kidney impairment.
Considerations for Nurse Practitioners
As nurse practitioners, it is crucial to assess the patient's pain intensity and overall health status before initiating Hydromorphone. Start with the lowest effective dose and titrate carefully for optimal pain control. Regular monitoring for adverse effects, signs of opioid toxicity, and therapeutic response is essential. Educate patients about the potential side effects, proper dosing, and the importance of not exceeding prescribed doses. Additionally, nurse practitioners should be familiar with local regulations and guidelines regarding opioid prescribing and follow appropriate documentation and monitoring practices.
Additional Considerations
In terminal cancer patients, clinicians should not restrain opioid therapy even if signs of respiratory depression become apparent.
Hydromorphone requires careful administration in cases of concurrent psychiatric illness.
Specific Patient Considerations:
- Hepatic impairment and Renal Impairment: Initiate hydromorphone treatment at one-fourth to one-half of the standard starting dosage, depending on the degree of impairment.
- Pregnancy considerations: Hydromorphone can traverse the placental barrier and induce NOWS.
- Breastfeeding considerations: Nonopioid analgesic agents are preferable for breastfeeding women.
- Older patients: hydromorphone is categorized as a potentially inappropriate medication for older adults (1).
Tramadol

Mechanism of Action and Metabolism
Tramadol is a Schedule IV opioid medication with a higher potential for dependency and misuse than non-opioid medications. It binds to opioid receptors in the central nervous system, inhibiting the reuptake of norepinephrine and serotonin. It also has weak mu-opioid receptor agonist activity.
The liver metabolizes tramadol mediated by the cytochrome P450 pathways (particularly CYP2D6) and is mainly excreted through the kidneys.
Tramadol is used for moderate to severe pain.
Available Forms of Tramadol include:
- Immediate-release-typically used for acute pain management.
- Extended-release-used for chronic pain.
Dosing and Monitoring
Tramadol has an oral bioavailability of 68% after a single dose and 90–100% after multiple doses and reaches peak concentrations within 2 hours. Approximately 75% of an oral dose is absorbed, and the half-life of tramadol is 9 hours (18).
Tramadol dosing should be individualized based on the patient's pain severity and response.
The initial dose for adults is usually 50-100 mg orally every 4-6 hours for pain relief. The maximum daily dose is 400 mg for immediate-release formulations and 300 mg for extended-release formulations (18).
It is essential to monitor the patient's pain intensity, response to treatment, and any adverse effects. Regular reassessment and adjustment of the dosage may be necessary.
Side Effects and Contraindications
Tramadol is responsible for severe intoxications leading to consciousness disorder (30%), seizures (15%), agitation (10%), and respiratory depression (5%). The reactions to Tramadol suggest that the decision to prescribe should be carefully considered.
Common Side Effects of Tramadol Include:
- Nausea
- Vomiting
- Dizziness
- Constipation
- Sedation
- Headache
- CNS depression
- Seizure
- Agitation
- Tachycardia
- Hypertension
- reduced appetite
- pruritus and rash
- gastric irritation
Serious side effects include:
- respiratory depression
- serotonin syndrome
- seizures
Contraindications
Tramadol is contraindicated in patients with:
- history of hypersensitivity to opioids
- acute intoxication with alcohol
- opioids, or other psychoactive substances
- Patients who have recently received monoamine oxidase inhibitors (MAOIs)
Additionally, the following can be observed in tramadol intoxication:
- miosis
- respiratory depression
- decreased level of consciousness
- hypertension
- tremor
- irritability
- increased deep tendon reflexes
Poisoning leads to:
- multiple organ failure
- coma
- cardiopulmonary arrest
- death
Considerations for Nurse Practitioners
Tramadol has been increasingly misused with intentional overdoses or intoxications. Suicide attempts were the most common cause of intoxication (52–80%), followed by abuse (18–31%), and unintentional intoxication (1–11%). Chronic tramadol or opioid abuse was reported in 20% of tramadol poisoning cases. Fatal tramadol intoxications are uncommon except when ingested concurrent with depressants, most commonly benzodiazepines and alcohol (18).
Tramadol poisoning can affect multiple organ systems:
- gastrointestinal
- central nervous system: seizure, CNS depression, low-grade coma, anxiety, and over time anoxic brain damage
- Cardiovascular system: palpitation, mild hypertension to life-threatening complications such as cardiopulmonary arrest
- respiratory system
- renal system: renal failure with higher doses of tramadol intoxication
- musculoskeletal system: rhabdomyolysis
- endocrine system: hypoglycemia, serotonin syndrome (18)
Cannabis
Mechanism of Action and Metabolism
Cannabis is classified as a Schedule I status. It contains various cannabinoids, with delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) being the most studied. THC primarily acts on cannabinoid receptors in the brain, producing psychoactive effects, while CBD has more diverse effects on the nervous system. These cannabinoids interact with the endocannabinoid system, modulating neurotransmitter release and influencing various physiological processes (32).
Similar to opioids, cannabinoids are synthesized and released in the body by synapses that act on the cannabinoid receptors present in presynaptic endings (32). They perform the following actions related to analgesia:
- Decrease the release of neurotransmitters.
- Activate descending inhibitory pain pathways.
- Reduce postsynaptic sensitivity and alleviate neural inflammation.
- Modulate CB1 receptors within central nociception processing areas and the spinal cord, resulting in analgesic effects.
- Attenuate inflammation by activating CB2 receptors (32).
- Emerging research shows cannabis is indicated for:
- Migraines
- chronic pain
- back pain
- arthritic pain
- pain associated with cancer and surgery.
- neuropathic pain
- diabetic neuropathic pain when administered early in the disease progression.
- sickle cell disease
- cancer
- inflammatory bowel disease (32)
Available Forms
Cannabis refers to products sourced from the Cannabis sativa plant. There are differences between cannabis, cannabinoids, and cannabidiol (CBD). Cannabinoids are extracted from the cannabis plants. Cannabinoid-based treatments, such as dronabinol and CBD, are typically approved medical interventions for specific indications. THC (9-tetrahydrocannabinol) is the psychoactive component of the cannabis plant. CBD is a non-psychoactive component (32).
Cannabis can be consumed in different forms, each with a different onset and duration. Patients may have individual preferences, including:
- smoking/vaporizing dried flowers.
- consuming edibles
- tinctures or oils
- applying topicals (32)
Dosing and Monitoring
Inhaling marijuana via the lungs by smoking or vaping causes maximum plasma concentration within minutes. Psychiatric effects begin within seconds to a few minutes after inhalation and peak after 15 to 30 minutes. The effect diminishes throughout 2 to 3 hours (32).
Oral ingestion of marijuana causes psychiatric effects that typically occur between 30 and 90 minutes and reach maximum effect after 2 to 3 hours. Ingested marijuana effects last about 4 to 12 hours (32).
Dosing cannabis is challenging due to variations in potency and individual responses. Start with low doses and titrate slowly to achieve the desired effect while minimizing side effects. Regular monitoring is crucial, including assessing symptom relief, adverse effects, and potential drug interactions. Encourage patients to keep a diary to track their cannabis use and its effects (32).
Side Effects and Contraindications
Cannabis can exacerbate mental health conditions such as anxiety and psychosis. Common side effects of cannabis include (32):
- Dizziness
- dry mouth
- increased heart rate
- impaired memory
- psychoactive effects
Contraindications include:
- Pregnancy
- Breastfeeding
- heart disease
- respiratory conditions
- history of substance abuse
- mental health disorders

Self Quiz
Ask yourself...
- How do you address patients' misconceptions about pain medications?
- What are the mechanisms of action for commonly prescribed pain medications?
- How do these mechanisms of action contribute to pain relief?
- What are the potential side effects and risks associated with commonly prescribed pain medications?
- How do you educate patients about the risks and benefits of pain medications?
- How do you manage patients who require high-dose opioids for pain management?
- Is medical cannabis legal in your State? If yes, are you familiar with the prescribing guidelines?
- Do you have any personal biases against the use of medical cannabis? Why or why not?
Case Study
Mary is agreeable to trying an increased dose of Gabapentin. Mary would also like to see a counselor to discuss her past and get help with her anxiety. You made an appointment for Mary to see a Licensed Clinical Social Worker in your clinic.
You read the side effects and warnings for Gabapentin, and it is unsafe to use Gabapentin and Tramadol together since they are both depressants. You order a non-steroidal drug for Mary's somatic knee pain and make a consult for imaging studies on her left knee. You also make a referral to Orthopedics.
You educated Mary about the side effects of Gabapentin and scheduled a follow-up appointment. The day after Mary began her treatment with the increased Gabapentin, you called Mary to follow up on its effect. Mary still has pain, but she is not having any untoward side effects. Gabapentin may not work immediately so you will schedule a follow-up call in 3 days.


Self Quiz
Ask yourself...
- In this case study, Mary has insurance. How might your practice be different were Mary not insured?
- In your experience, what are the possible reasons for Mary's knee pain not being a part of her previous treatment record?
- Consider how your assessment of Mary's needs differs from the above-mentioned case study.
- Explain the rationale for decisions made by the nurse practitioner in the case study mentioned above and if your decisions would differ.
Opioid Use, the Opioid Epidemic, and Statistics
The use and misuse of opioids has become a pressing public health concern, leading to a global epidemic. The history of opioid use, the opioid epidemic, and associated statistics provide essential context for healthcare professionals in addressing this public health crisis. More importantly, it is estimated that 1 in 4 patients receiving prescription opioids in primary care settings will misuse them. In addition, 50% of opioid prescriptions are written by primary care providers, including nurse practitioners (22). Understanding the factors contributing to the epidemic and the magnitude of its impact is crucial for effective prevention, intervention, and treatment strategies.
History of Opioid Use
Opioids have a long history of medicinal use, dating back to ancient civilizations. They have been a drug of choice for pain relief for thousands of years. The introduction of synthetic opioids in the 19th century, such as morphine and later heroin, revolutionized pain management. However, their potential for addiction and misuse soon became apparent (16).
The Opioid Epidemic
The opioid epidemic refers to the surge in opioid misuse, addiction, and overdose deaths. The epidemic gained momentum in the late 1990s with increased prescribing of opioids for chronic pain (43).
No doubt, increased prescribing put opioids in the hands of consumers, but increased prescribing resulted from a multifactorial influence. One of the main influences was aggressive marketing by pharmaceutical companies, which has been well publicized. However, due to the long history of underprescribing pain medications for fear of misuse and addiction, the medical community was primed to expand its opioid prescribing practices (31).
A historical event that increased comfort with prescribing opioids, in the writer's opinion, was the introduction of the Medicare Hospice Benefit in 1986. Medical directors must be contracted or employed by hospices, and these medical directors had or soon gained pain management expertise. To further promote hospice and effective pain management, the hospice medical directors, with newly acquired skills, provided education throughout medical communities about pain management and specifically to decrease the fear of using opioids. Pharmacies and attending physicians grew accustomed to giving opioids for home use. Hospice care is for terminally ill patients, defined as a life expectancy of 6 months or less. Still, the reality is that hospice discharges 12 to 40% of patients for ineligibility and other reasons.
A more prominent factor in increasing opioid prescribing was the 1996 American Pain Society's introduction of pain as "the 5th Vital sign." Soon after, The Joint Commission promoted pain as "the 5th Vital Sign" and began compliance surveys in healthcare organizations requiring pain assessment details to be as prominent as blood pressure and heart rate. The Joint Commission cited a quote from 1968 by a nurse from the University of California Los Angeles, Margo McCaffrey, who defined pain as "…Whatever the experiencing person says it is, existing whenever s/he says it does." The Joint Commission accreditation programs pursued pain management as part of the accreditation process throughout its healthcare accreditation programs, including hospice accreditation by 1989 per TJC Timeline (48).
The National Institute of Health published an article about the Joint Commission's role in the opioid epidemic, particularly regarding the definition of pain, "This definition emphasizes that pain is a subjective experience with no objective measures. It also stresses that the patient, not the clinician, is the authority on the pain and that their self-report is the most reliable indicator of pain. This set the tone for clinicians: Patients are always to be trusted to report pain accurately” (45).
Statistics on the Opioid Epidemic
In the United States alone, over 500,000 people died from opioid overdoses between 1999 and 2017. The number of opioid-related overdose deaths continues to increase, with synthetic opioids, mainly illicitly manufactured Fentanyl, playing a significant role in recent years (46). Fentanyl-laced drugs, such as marijuana, are increasingly sold knowing and unknowingly to introduce medications with a high addiction rate, thus creating new consumers. This practice can potentially increase deaths due to the imprecise nature of manufacturing (16).
Opioid-related hospitalizations have also risen substantially. In 2014, there were approximately 1.27 million hospitalizations related to opioids in the United States. These hospitalizations not only place a burden on healthcare systems but also reflect the severe consequences of opioid misuse (3).


Self Quiz
Ask yourself...
- Have you experienced changes to your practice because of the opioid epidemic? If so, what are the changes?
- What is your opinion on the validity of Margo McCaffrey's definition of pain?
- What factors influence your willingness or unwillingness to prescribe opioids?
Federal Regulations on Opioid Prescribing
The history of substance use disorder prevention that promotes opioid recovery and treatment for patients and communities can be traced back to the early 20th century. However, the current approach to addressing opioid addiction and promoting healing has evolved significantly in recent times (36).
In the early 1900s, health professionals treated opioid addiction with punitive measures, including incarceration and moralistic approaches. The focus was on punishing individuals rather than providing effective treatment. This approach persisted for several decades until the mid-20th century when the medical community started recognizing addiction as a medical condition rather than a moral failing (36).
The Controlled Substances Act (CSA), introduced in 1970, was a response to increasing drug abuse and illicit drug trafficking in the United States. The CSA is a federal law regulating the manufacture, possession, distribution, and use of certain substances, including drugs and medications, that can potentially cause abuse and dependence. Its primary purpose is to combat drug abuse, reduce drug-related crimes, and protect public health and safety. The Drug Enforcement Agency (DEA) plays a crucial role in enforcing the CSA by monitoring and controlling controlled substance production, distribution, and use (31).
In the 1990s, the significant increase in opioid prescribing, leading to a surge in opioid addiction and overdose deaths, prompted a shift in focus toward prevention. Efforts were made to educate healthcare providers about the risks of overprescribing opioids and to implement prescription drug monitoring programs to track and prevent abuse (36).
The Comprehensive Addiction and Recovery Act (CARA) was signed into law in 2016 to expand access to treatment and recovery services for opioid addiction. This legislation allocated funding for prevention, treatment, recovery, and support services while promoting evidence-based practices and programs (36).
The Centers for Disease Control and Prevention (CDC) published guidelines in 2016 for prescribing opioids for chronic pain, which was updated in 2022. These guidelines emphasize the importance of non-opioid alternatives, using the lowest effective dose for the shortest duration, and assessing the benefits and risks of continued opioid therapy (13).
Furthermore, the Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT) was signed into law in 2018, providing additional resources to address the opioid crisis. This legislation expanded access to medication-assisted treatment (MAT), increased the availability of naloxone, a medication used to reverse opioid overdose, and enhanced support for recovery housing (36).
In recent years, there has been a growing recognition of the importance of a comprehensive approach to opioid addiction, including harm reduction strategies, increased access to naloxone, and the integration of mental health services. Communities and organizations have been working together to address the underlying issues contributing to addiction, such as poverty, trauma, and social determinants of health (50).
Overall, the history of substance use disorder prevention that promotes opioid recovery and treatment has evolved from a punitive approach to a more compassionate and evidence-based model. Efforts are now focused on prevention, early intervention, and expanding access to comprehensive treatment and support services for individuals and communities affected by opioid addiction (36).
The most current federal regulations on opioid prescribing for healthcare providers are the amendments to the CSA in 2018, which added new rules to limit the quantity and duration of opioid prescriptions for acute pain to seven days. In 2022, the CDC updated recommendations to the Clinical Practice Guidelines for Prescribing Opioids for Pain.
The 2022 CDC guidelines are summarized below (13):
- Non-opioid therapies should be considered the first-line treatment for chronic pain.
- Establish clear treatment goals with patients, including realistic pain management and functional improvement expectations.
- Conduct a thorough risk assessment for potential harms before initiating opioid therapy.
- When opioids are used, start with the lowest effective dose and consider immediate-release opioids instead of extended-release or long-acting opioids.
- Prescribe the lowest effective dose for the shortest duration possible, typically three days or less and rarely exceeding seven days.
- Reassess benefits and risks within one day after prescribing opioids, including checking the prescription drug monitoring database.
- Avoid prescribing opioids and benzodiazepines concurrently whenever possible due to the increased risk of overdose and death.
- Offer naloxone to patients at increased risk of opioid overdose, including those with a history of overdose, substance use disorder, or concurrent benzodiazepine use.
- When opioids are no longer needed, taper the dose gradually to minimize withdrawal symptoms.
- Arrange an evidence-based treatment for patients with opioid use disorder, including medication-assisted treatment (Naltrexone, Buprenorphine, or Methadone).

Self Quiz
Ask yourself...
- What are the guidelines general for prescribing opioids for acute pain?
- How do these guidelines differ for chronic pain management?
- Discuss how federal regulations impact the practice of nurse practitioners in terms of opioid prescribing.
- Describe the potential benefits and challenges nurse practitioners face when adhering to federal regulations on opioid prescribing.
- How can nurse practitioners navigate and stay updated with evolving federal regulations surrounding opioid prescribing to ensure safe and effective care?
- How do you ensure appropriate documentation when prescribing controlled substances?
Safe Prescribing and Prescription Monitoring Program
Prescription Drug Monitoring Programs (PDMP) are state-run electronic databases that track.
the prescribing and dispensing of controlled substances. PDMPs are designed to improve patients.
care and safety by giving clinicians access to patients' prescription histories, allowing them to make informed decisions when prescribing controlled substances. PDMPs help identify patients at risk of substance misuse or prescription drug overdose. They also enable clinicians to identify potential drug interactions and prevent opioid diversion (14).
PDMPs collect and store data from pharmacies and prescribers in a centralized database. Clinicians can access this database to review a patient's prescription history, including the types of medications prescribed, the prescribers involved, and the dispensing pharmacies (14).
In many states, PDMP use is mandated by law, and nurse practitioners may be required to register and use the system. It is essential to understand state-specific laws and regulations regarding PDMP use.
PDMPs have some limitations, such as incomplete data or delays in reporting. The CDC emphasizes that clinicians should use PDMP data for their clinical assessment and other relevant information to make informed decisions about prescribing controlled substances. Still, PDMP cannot be used as the sole basis for denying or providing treatment (14).
Case Study
After five days on Gabapentin, Mary was doing well, and her neuropathic pain had decreased to 3/10. However, Mary suffered a fall after her knee "gave out" and injured her knee and back. She was in severe pain, and her family drove her to the ER. The ER doctors saw Mary, and orthopedics were consulted. Mary has surgery scheduled for a knee replacement a week from now.
Mary was prescribed Vicodin because she was in excruciating pain, but her prescription only allowed enough medication for two days. Mary has made an appointment with you to renew her prescription.
You evaluate Mary because you know that concomitant use of Gabapentin and opioids puts Mary at risk for respiratory depression and possible side effects, including accidental overdose.
Mary stated she has been more alert the past 24 hours and is afraid her functional status will continue to decline if she does not have more Vicodin because the pain in her back and knee makes it difficult to stand. You assess Mary. Mary stated she occasionally drinks alcohol but has not had a drink since she moved. She has no familial history of substance abuse or mental health disorders.
Mary's mother stayed at her house to help her for the first 24 hours after Mary's return from the ER, but Mary is providing her care now.
You check the PDMP database and see that Mary was prescribed eight pills she has taken over the last 48 hours.
Since the Vicodin has been effective without untoward side effects, and Mary's function is improving, you decide to refill the prescription of Vicodin. You will taper the dose to three Vicodin daily for two days and two for one day. Mary will be near her appointment for a knee replacement as well.


Self Quiz
Ask yourself...
- What are the potential benefits and drawbacks of using PDMPs in your practice?
- How can PDMPs help you identify potential drug abuse or diversion cases among your patients? Can you provide examples from your own experience?
- In what ways do PDMPs impact your decision-making process when prescribing controlled substances?
- What are the key considerations when prescribing controlled substances?
- How do you ensure responsible prescribing practices for controlled substances?
Preventing Opioid Use Disorder
As previously discussed, opioid addiction is a growing concern worldwide, affecting individuals from all walks of life. According to the CDC, "Anyone who takes prescription opioids can become addicted to them" (14).
As frontline healthcare professionals, nurse practitioners must recognize the signs of opioid addiction to provide timely intervention and support. This section will outline the key indicators of opioid addiction.
Physical Symptoms
Physical symptoms are often the first noticeable signs of opioid addiction. These symptoms may include constricted pupils, drowsiness, slurred speech, impaired coordination, and increased sensitivity to pain. Additionally, individuals struggling with opioid addiction may exhibit frequent flu-like symptoms, such as a runny nose, sweating, itching, or gastrointestinal issues.
Behavioral Changes
Opioid addiction can significantly impact an individual's behavior. These may include increased secrecy, frequent requests for early prescription refills, doctor shopping (seeking prescriptions from multiple healthcare providers), neglecting personal hygiene, and experiencing financial difficulties due to excessive spending on opioids (37).

Social Isolation
Opioid addiction often leads to social withdrawal and isolation. Individuals struggling with opioid addiction may distance themselves from family, friends, and social activities they once enjoyed. They may exhibit erratic mood swings, become defensive or hostile when confronted about their drug use, and display a general lack of interest in previously important activities (30).
Psychological Changes
The psychological impact of opioid addiction is significant. Individuals with opioid addiction may exhibit increased anxiety, depression, irritability, and restlessness. They may also experience cognitive impairments, memory lapses, and difficulties in decision-making. Healthcare professionals should be attentive to these changes, as they can indicate opioid addiction (51).
Tolerance and Withdrawal Symptoms
The development of tolerance and withdrawal symptoms are critical signs of opioid addiction. Individuals may require increased dosages of opioids to achieve the desired effect, indicating a growing tolerance. Furthermore, withdrawal symptoms such as muscle aches, nausea, vomiting, insomnia, and intense cravings for opioids may occur when the drug is discontinued or reduced abruptly (51).

Self Quiz
Ask yourself...
- Discuss how nurse practitioners can contribute to preventing opioid use disorder.
- Explain how nurse practitioners effectively communicate the risks and signs of opioid misuse without stigmatizing or alienating patients.
- What are the signs of opioid addiction or misuse in patients?
- How do you approach patients who may be at risk for opioid addiction?
- How do you ensure appropriate documentation when prescribing controlled substances?
Opioid Overdose
The management of opioid overdose, withdrawal, and addiction requires a comprehensive approach that combines pharmacological interventions with psychosocial support. Naloxone remains a vital tool for reversing opioid overdose, while medications such as Methadone, buprenorphine, and naltrexone play crucial roles in withdrawal and addiction treatment (National Institute of Health, 2023). Nurse practitioners must stay vigilant and informed about the evolving landscape of medications. This section aims to provide a comprehensive review of medications and treatment strategies for opioid overdose, withdrawal, and addiction and is excerpted from the NIH (40).
Naloxone
Mechanism of Action and Metabolism
Naloxone is an opioid receptor antagonist. It works by binding to opioid receptors and displacing any opioids present, thereby reversing the effects of opioid overdose. It has a higher affinity for opioid receptors than most opioids, effectively blocking their action.
Naloxone is indicated for emergency intervention of opioid overdose. It effectively reverses respiratory depression and other life-threatening effects. Studies suggest the potential benefits of combining naloxone with other medications, such as buprenorphine (see below), to improve outcomes. Initiatives promoting community-based naloxone distribution programs have shown promising results in reducing opioid-related deaths.
Available Forms
Naloxone is available in various formulations:
- Intranasal
- Intramuscular
- Intravenous
- auto-injectors.
The most used form is the intranasal spray, which is easy to administer and requires no specialized training. Intranasal naloxone formulations have gained popularity due to their ease of use and increased availability. A recent study showed that the non-FDA-approved compound spray was far less effective than either FDA compound (15).
Dosing and Monitoring
The recommended initial dose of naloxone for opioid overdose is 2mg intranasally or 0.4mg to 2mg intramuscularly or intravenously. If the patient does not respond within 23- minutes, additional doses may be administered every 2-3 minutes. Continuous monitoring of the patient's respiratory status is essential, as repeat doses may be required due to the short half-life of naloxone.
Side Effects and Contraindications
Naloxone has been shown not to affect individuals without opioids in their system.
Common side effects of naloxone include
- Withdrawal symptoms: increased heart rate, sweating, and agitation
- nausea
- vomiting
- headache
Contraindications include known hypersensitivity to naloxone and situations where the use of naloxone may be unsafe or not feasible.
Considerations for Nurse Practitioners
Fentanyl and other opioids have a rapid onset, and the need to act quickly is paramount. As mentioned previously, the ease of use and higher plasma concentrations using the FDA-approved 4-mg FDANxSpray device compared with the locally compounded nasal sprays should be considered when ordering Naloxone (15).
Fentanyl and other potent synthetic opioids may require multiple administrations of naloxone to achieve reversal of an overdose (Chiang, Gyaw, & Krieter, 2019). As a nurse practitioner prescribing naloxone, it is crucial to assess the patient's risk factors for opioid overdose, such as a history of substance use disorder or chronic pain management. Education regarding the proper administration of naloxone should be provided to the patients and their caregivers. Additionally, it is essential to provide resources for follow-up care, including addiction treatment and ongoing support.
Methadone
Mechanism of Action and Metabolism
Methadone is a long-acting opioid agonist that effectively suppresses withdrawal symptoms and reduces cravings. It binds to the same opioid receptors in the brain as other opioids. It relieves withdrawal symptoms and reduces cravings by blocking the euphoric effects of opioids, thus helping individuals with opioid dependence to achieve stability (33).
Available Forms
Methadone is available in oral tablets and liquid formulations. The oral tablet is the most used form and is typically administered once daily (33).
Dosing and Monitoring
Methadone dosing is individualized based on the patient's response and needs. Initially, the dose often started low and gradually increased until the patient reached a stable dose. Dosing may need to be adjusted based on the patient's response, adherence, and any changes in their overall health. Regularly monitoring the patient's vital signs, urine drug screens, and assessment of their withdrawal symptoms and cravings is essential.
Side Effects and Contraindications
Common side effects of methadone include:
- Constipation
- dry mouth
- drowsiness
- sweating
- weight gain
- respiratory depression
Contraindications include:
- known hypersensitivity to methadone
- severe asthma
- respiratory depression
- certain heart conditions (33).
Considerations for Nurse Practitioners
As a nurse practitioner prescribing methadone, conducting a comprehensive assessment of the patient's medical history, current medications, and substance use history is crucial. Opioid treatment programs or specialized clinics are often involved in methadone treatment, so collaboration and coordination of care with these programs are essential. Regularly monitoring the patient's progress, adherence, and potential side effects or drug interactions is essential. Additionally, providing education on the risks and benefits of methadone and the importance of adherence to the prescribed regimen is crucial for successful treatment outcomes.
Buprenorphine
Mechanism of Action and Metabolism
Buprenorphine is a partial opioid agonist with a ceiling effect that minimizes the risk of overdose while reducing withdrawal symptoms. Buprenorphine is a partial opioid agonist that binds to the same receptors as other opioids but produces a weaker response. It has a high affinity for the mu-opioid receptors, which helps reduce cravings and withdrawal symptoms in individuals with opioid dependence.
Available Forms
Buprenorphine is available in different formulations, including sublingual tablets, buccal films, and extended-release injections. The sublingual tablets have different strengths, such as 2mg, 4mg, 8mg, and 12mg. Buprenorphine is taken as a daily tablet or weekly or monthly injection.
Dosing and Monitoring
The dosing of buprenorphine varies depending on the individual's opioid dependence severity and treatment phase. Initially, a low dose (e.g., 2-4mg) is given, and it may gradually increase to a maintenance dose of 8-24 mg daily. Regular monitoring is essential to assess the patient's response, adherence, and potential side effects.
Side Effects and Contraindications
Common side effects of buprenorphine include:
- Constipation
- Nausea
- Headache
- Insomnia
- Sweating
Serious side effects are rare but can include:
- Respiratory depression
- Allergic reactions
Buprenorphine is contraindicated in individuals with:
- Severe respiratory insufficiency
- Acute intoxication with opioids
- Known hypersensitivity
Considerations for Nurse Practitioners
Nurse practitioners can prescribe buprenorphine for opioid dependence treatment under the Drug Addiction Treatment Act (DATA). To become eligible, they must complete specific training requirements and obtain a waiver from the Substance Abuse and Mental Health Services Administration (SAMHSA). Nurse practitioners should assess patients thoroughly, including their opioid use history, comorbidities, and medication compatibility, while ensuring appropriate counseling and referral for comprehensive treatment (40).
Clonidine + Lofexidine
Mechanism of Action and Metabolism:
Both Clonidine and Lofexidine are alpha-2 adrenergic agonists. They work by stimulating alpha-2 receptors in the brain, which reduces sympathetic outflow and norepinephrine release. This results in decreased sympathetic activity, leading to various effects such as reduced blood pressure, decreased heart rate, and alleviated withdrawal symptoms (28).
Available Forms
Clonidine is available in oral tablets and patches. Lofexidine is available in oral tablets and is taken as needed (40).
Dosing and Monitoring
For opioid withdrawal, the Clonidine dose ranges from 0.1-0.3 mg every 4-6 hours. Lofexidine is usually initiated at 0.53 mg three times daily, and the dose can be increased to 2.88 mg daily. Monitoring blood pressure and heart rate is essential during treatment (40).
Side Effects and Contraindications:
Common side effects of both medications include:
- dry mouth
- sedation
- dizziness
- constipation
- orthostatic hypotension (40).
Both medications are contraindicated in patients with:
- Hypotension
- Bradycardia
- heart block
- history of hypersensitivity to the drugs (40).
Considerations for Nurse Practitioners:
An early study of lofexidine vs. clonidine for withdrawal symptoms showed that treatment with lofexidine resulted in lower withdrawal symptoms, fewer mood problems, less sedation, and hypotension. There were no significant differences in craving levels, morphine metabolites in urine, or dropout rates when both were compared.
Lofexidine can be a safe option for outpatient treatment as it does not lead to hypotension. However, nurse practitioners must closely monitor patients' blood pressure and heart rate during treatment and educate them about possible side effects. If patients experience any concerning symptoms, they should inform their nurse practitioner immediately.
Gradual dose reduction of Clonidine is crucial to prevent rebound hypertension. Before prescribing either medication, nurse practitioners should assess for any contraindications or potential drug interactions (19).
Emerging Therapies for Withdrawal
Extended-release naltrexone: Naltrexone is an opioid receptor antagonist that blocks the effects of opioids, reducing the risk of relapse. It is taken as a monthly injection.
Alpha-2 adrenergic agonists: Emerging evidence suggests the potential use of dexmedetomidine and guanfacine for managing opioid withdrawal symptoms.
Medication-Assisted Treatment (MAT):
Methadone was introduced in the 1960s and marked a significant turning point in opioid addiction treatment or MAT. Along with counseling and behavioral therapies, MAT became the cornerstone of opioid addiction recovery.
Examples of medications used:
- Methadone
- Buprenorphine:
- Naltrexone:
Adjunctive Pharmacotherapies:
Antidepressants: Selective serotonin reuptake inhibitors and tricyclic antidepressants may help manage co-occurring depression and anxiety.
Anticonvulsants:
Medications like Gabapentin and pregabalin show promise in reducing opioid cravings and improving treatment outcomes.


Self Quiz
Ask yourself...
- What are the mechanisms of action for commonly prescribed addiction medications?
- What are the potential risks and benefits of using benzodiazepines for pain management?
- How do you assess and manage patients with co-occurring pain and substance use disorders?
- What are the guidelines for prescribing addiction medications like buprenorphine or methadone?
- How do these medications work in the treatment of opioid use disorder?
- What are the potential side effects and risks associated with addiction medications?
- How do you support patients in their recovery from opioid use disorder?
- How do you address patients' concerns and fears about addiction medications?
- What are the federal guidelines around prescribing addiction medications for nurse practitioners?
- How do these guidelines influence your prescribing practices?
Other Substance Use Disorders
Patients in pain may struggle with Substance Use Disorders other than Opioid Use Disorder. Substance use disorders may often occur with mental health conditions such as anxiety, depression, and bipolar disorder. In addition, many individuals engage in polydrug use. Understanding the most common Substance Use Disorders aids in a comprehensive assessment of the patient and the development of appropriate treatment plans (28).
Alcohol Use Disorder (AUD):
The prevalence of AUD worldwide was estimated to be 9.8% in men and 5.5% in women in 2016 (28).
Cannabis Use Disorder (CUD):
the prevalence of CUD in the United States increased from 2.18% in 2001-2002 to 2.89% in 2012-2013. (28).
Cocaine Use Disorder:
According to the National Survey on Drug Use and Health (NSDUH), in 2019, approximately 1.9 million Americans aged 12 or older had cocaine use disorder in the past year (44).
Methamphetamine Use Disorder:
A study published in Drug and Alcohol Dependence reported that the prevalence of methamphetamine use disorder in the United States was estimated to be 0.2% in 2015-2016 (6).

Self Quiz
Ask yourself...
- What are the options available for managing opioid addiction and withdrawal?
- How can nurse practitioners support patients in their recovery from opioid addiction?
- What strategies can nurse practitioners employ to effectively engage and build trust with patients reluctant to disclose or seek help for substance abuse disorders?
- How can nurse practitioners collaborate with other healthcare professionals and community resources to provide comprehensive care and support for patients with substance abuse disorders?
- What techniques or tools can nurse practitioners employ to start these sensitive conversations with new patients?
- How do you assess and manage patients experiencing opioid withdrawal symptoms?
- What are the non-pharmacological interventions for managing opioid withdrawal?
- How do you educate patients about the risks and benefits of addiction medications?
- How do you monitor patients on addiction medications for adherence and progress?
- What are the drug potential interactions with commonly prescribed addiction medications?
Drug Diversion and Illegal opioids
Misuse of opioids is facilitated by diversion and is defined as "the transfer of drugs from lawful to unlawful use" (24). Most commonly, this occurs when family and friends share prescribed opioids with other family and friends. Opioids and other controlled drugs are also diverted from healthcare facilities. Statistics show that healthcare facility diversion has increased since 2015 (24)
Diversion affects patients, healthcare workers, healthcare facilities, and public health. Patients experience substandard care due to ineffective pain management and impaired healthcare workers. In addition, affected patients are at risk of infections from compromised syringes (24).
Healthcare employees who divert are at risk of overdose and death. If caught, they face criminal prosecution and malpractice suits. Healthcare facilities also bear the cost of diverted drugs via internal investigations, follow-up care for affected patients, regulatory fines for inadequate safeguards, and declining public trust (24).
Despite the enormous consequences of drug diversion, healthcare facilities have implemented few processes to detect and deter the diversion of controlled substances (24).

Self Quiz
Ask yourself...
- What protocols can nurse practitioners implement to prevent drug diversion within their healthcare setting?
Patient Teachings and Considerations
Opioids have significant side effects and carry a risk of addiction and overdose. Nurse practitioners can decrease the risks of misuse and addiction by educating patients on appropriate disposal, safe storage, and potential signs of addiction. Taking additional time to provide teaching nurse practitioners can promote patient safety, informed decision-making, and responsible opioid use.
Safe Storage and Disposal:
- Teach patients to store opioids securely, out of reach of children, pets, visitors, and non-caregiver family members, to prevent accidental ingestion or misuse (13). Only the caregiver, if applicable, or the patient should have access to pain medications.
- Instruct patients on proper disposal methods, such as using drug take-back programs or mixing opioids with undesirable substances (e.g., coffee grounds) before throwing them away (11) (13).
Medication Adherence:
- Emphasize the importance of taking opioids as prescribed, at the correct dose and frequency, to achieve optimal pain relief.
- Encourage patients to notify their healthcare provider if they experience inadequate pain control or side effects (35).
Potential Side Effects:
- Educate patients about common side effects of opioids, including constipation, nausea, sedation, and respiratory depression.
- Discuss strategies to manage side effects, such as maintaining adequate hydration, consuming a fiber-rich diet, and using over-the-counter laxatives as needed (11).
Risk of Dependence and Addiction:
- Explain the potential for opioid dependence and addiction, especially with long-term use or a history of substance abuse.
- Encourage patients to promptly report signs of opioid misuse, such as craving, loss of control, or continued use despite negative consequences (51).

Avoiding Alcohol and Other Central Nervous System Depressants:
- Instruct patients to avoid consuming alcohol or other medications that can enhance the sedative effects of opioids, increasing the risk of respiratory depression.
- Advise patients to contact the Nurse Practitioner before starting new medications, including over-the-counter drugs or herbal supplements (2).
Driving and Operating Machinery:
- Inform patients about the potential impairment caused by opioids, including reduced alertness, reaction time, and coordination.
- Advise patients to avoid driving or operating heavy machinery while taking opioids until they know how the medication affects them (14).

Self Quiz
Ask yourself...
- What strategies can nurse practitioners employ to effectively communicate the risks and benefits of opioid use while ensuring they clearly understand the potential side effects and the importance of adhering to the prescribed regimen?
- How can nurse practitioners promote patient engagement and shared decision-making regarding opioid pain management, considering the potential for dependence and addiction?
- How can nurse practitioners assess a patient's knowledge and understand the safe storage and disposal of opioids?
Case Study
You take some extra time with Mary to educate her on the taper dose of Vicodin, the potential for harm, and the risk of opioids, especially when used concomitantly with Gabapentin. You let Mary know it is unsafe to use alcohol, not only with Vicodin but also with Gabapentin. You let Mary know that Vicodin has a risk of dependency and misuse and, therefore, she will be monitored carefully. You also educate that Mary should store the Vicodin away from visibility by anyone but herself since she can self-administer her medication. You let Mary know that Vicodin can cause constipation and that she should increase her water intake and take a stool softener.
You ask Mary to call you if her pain is not adequately relieved or if her medications run out before the three days.
You let Mary know that if she does stop taking the Vicodin before she has completed all the medication, she should dispose of it by mixing the pills with liquid and coffee grounds to make them unpalatable to animals and others.
Mary complied with your education, completed her course of Vicodin, and was scheduled for surgery. Mary's social worker helped her communicate with her new employer and delayed her start date until after her recovery.
During her recovery, Mary received physical therapy and a short course of pain medication managed by her orthopedist.
Mary returned to the clinic for a follow-up visit after completing her therapy and before starting work. Mary's pain level in her knee is 3/10, and she already feels like she can walk further than pre-surgery. Gabapentin has continued to help Mary's neuropathic pain in her back, and she reports 2/10. Mary looks forward to beginning her new job and is optimistic about the future.
Conclusion
Pain management is the leading cause of primary care appointments and chronic pain is the leading cause of disability. Yet, prescribing opioids for primary care patients is also a factor in drug misuse and the opioid epidemic. Nurse practitioners are challenged to appropriately treat pain and effectively control diversion, addiction, and death from overdose.
It is imperative that nurse practitioners use evidence-based practices to assess, appropriately intervene, and educate about the benefits and potential harm caused by treatment with opioids. Nurse practitioners must stay up to date with the current federal regulations regarding PDMPs, clinical prescribing guidelines, and emerging treatments for pain and opioid abuse disorders.
Tirzepatide for Type 2 Diabetes and Weight Management
Introduction
The emergence of the drug tirzepatide is becoming more popular and widespread and is being utilized among those with diabetes and also those who desire to lose weight. It is one of the newest diabetic drugs given by injection that also triggers dramatic weight loss in those who use the injections.
The U.S. Food and Drug Administration (FDA) approved tirzepatide in 2022 for individuals with diabetes, particularly Type 2 Diabetes. The FDA officials have not approved tirzepatide yet for weight loss, but they are currently tracking the medication and may have a recommendation for its approval by the end of this year. Clinical trials have shown that individuals with an elevated body mass index (BMI) and who did not have diabetes lost a considerable amount of weight when they received tirzepatide (1).
Advanced Practice Registered Nurses (APRNs) need to understand how to safely prescribe tirzepatide and the reasoning as to why it causes weight loss for specific individuals.
Drug Classification
Tirzepatide is part of a class of medications called glucose-dependent insulin tropic polypeptide (GIP) receptor and glucagon-like peptide-1 (GLP-1) receptor agonists. It comprises a 39 amino acid linear synthetic peptide conjugate to selective receptor agonists in preclinical and clinical trials.
Tirzepatide is used for treating Type II diabetes in adults as an adjunct to diet and exercise. It is also used for weight loss in some individuals and has gained increased attention as a new therapeutic agent for glycemic and weight control.
Social media has had a significant influence and increased the desire to use tirzepatide, and while individual results vary, the weight loss in adults ranged from 12 – 25 pounds.
Online pharmacies, diet clinics, and medical spas are implementing thousands of ads on social media to capitalize on a surge of interest in the drug.

Self-Quiz
Ask Yourself...
- Why has there seemed to be an increase in patients requesting this medication? What other medicines intended for type 2 diabetes are also being used for weight loss management?
- What are the ethical considerations regarding marketing this drug for weight loss when its primary use is for type 2 diabetes? Could this impact supply and costs?
Indications of Usage
The use of tirzepatide is being used for both Type II diabetes and weight control in certain patients. It has been a game changer for people living with Type II diabetes. The drug’s primary use is as an adjunct to diet and exercise to improve glycemic control in adults with diabetes.
The drug has also proven beneficial for weight loss in patients experiencing obesity, and those who are taking the highest dosage have shared a body weight reduction of 15.7% (2). Tirzepatide is an injectable prescription medication used together with diet and exercise, and it is not yet known if it can be used safely with patients who have had pancreatitis.
It is important to remember that it is not to be used for patients with Type I diabetes, but it is safe for Type II diabetic patients. Also, the safety of tirzepatide has yet to be discovered for children and those under 18; therefore, the medication should not be used for this age group.
In studies conducted with or without diabetic medicines, 75% – 90% of patients taking tirzepatide reached an overall A1C of less than 7% with an average starting A1C of 7.9 – 8.6% across the following dosages – 5mg, 10mg, and 15mg. The study results were measured at weeks 40 and 52 (3).

Self-Quiz
Ask Yourself...
- What dietary and activity recommendations can you provide to patients using tirzepatide for weight loss?
- Is this drug intended for those who want to lose 5-10 pounds?
Use of Tirzepatide with Diabetic Patients
Tirzepatide can be used for patients with Type II diabetes in combination with a diabetic-friendly diet and exercise. The drug works by lowering the patient’s overall blood sugar and also improves the A1C results of patients over some time. The injection has been approved by the FDA to treat Type II diabetes and is administered once weekly (4).
It is considered the first in a new class of medications – a dual glucose-dependent insulin tropic polypeptide (GIP) and glucagon-like-peptide-1 (GLP-1) receptor antagonist. The mechanism of how it works mimics two gut hormones (GIP and GLP-1). These hormones are essential in how patients digest food and regulate blood glucose after meals. The hormones also play a role in making individuals feel fuller and curb specific food cravings.
The provider can prescribe tirzepatide before attempting other diabetic medications if a patient has a BMI of 30 or greater or 27 or greater with weight-related conditions and if the drug is combined with a personalized weight loss plan that addresses physical activity, nutrition, and lifestyle changes.
However, due to the cost and some insurance companies not covering the injection unless the patient has both diabetes and obesity, the provider must carefully consider prescribing this medication.

Case Study
The patient states this ‘miracle drug’ is worth paying for out of pocket!
Jeff Capron, a 53-year-old Boonville, New York, web developer, started taking tirzepatide in December 2022. His friend had reported good results with the medication, so Jeff looked into the research studies behind it and then spoke with his primary physician.
The physician said, “Yeah, let’s give it a shot,” even though he did not have much experience with it. The physician did not have an opinion one way or the other than looking at the data set and seeing no reason why they could not try it.
Jeff’s hemoglobin A1C went from 10.1% to 6% in 3 months, which was very promising. “I never had that kind of experience with any medication for diabetes.” There is a range in how much A1C reduction people experience with tirzepatide, but many people taking it can get their A1C under 7% — an ideal goal for people with Type 2 diabetes.
Jeff experienced constipation and a little trouble sleeping early, but both issues disappeared quickly. He says, “I wake up in the morning, and my fasting blood sugars are normal.”
The medication took effect, he says, within 12 hours. He compared the feeling to having a gastric bypass.
“You cannot overeat food. As soon as you overeat, you almost feel ill.” While it generally takes a few months to notice effects like A1C reduction and significant weight loss, side effects such as lower appetite may be felt immediately.
Weight loss was not his primary goal, but he lost about 35 pounds on the medication in the first five months. He also lost his sweet tooth. “I can maybe count three sweet things I have eaten since December.”
Jeff found that his appetite slowly recovered days after taking tirzepatide. “You take the shot every Sunday, and by Saturday, you start to get a lot of appetite,” he says. “It does not seem to affect your weight. If I eat a little bit more on Saturday night, on Sunday, the scale will not move one way or the other.”
Jeff is allergic to hornets, so he already carries an auto-injector. He was not worried about using another drug delivered through a needle. “It’s just a push button,” he says. It also helped that his wife is a nurse. “So, I had her with me the first time to ensure I was doing it right. I didn’t even feel it.”
When Jeff was first prescribed tirzepatide, his insurance covered it. The company has since removed that benefit. He has filed an appeal but pays about $1,000 monthly out of pocket for his weekly injections. He plans to keep paying as long as necessary.
He considers the financial burden well worth it. “I have never had a medication that worked as well before for chronic conditions,” Jeff says. “I’ve been blown away by it. For me, it’s a miracle drug. It got rid of my diabetes” (4).

Self Quiz
Ask yourself…
- Can a provider willfully choose to prescribe tirzepatide before other diabetic medications are attempted?
- Would that impact his insurance coverage if Jeff did not meet the clinical criteria for using tirzepatide?
Use of Tirzepatide for Weight Loss Management
As mentioned, this medication is indicated for patients with a BMI of >30 or a BMI of >27 with qualifying comorbidities. Obesity can become a chronic lifetime disease, and for conditions such as these, the patient needs to implement therapy for the lifetime of the disease.
In a study conducted for tirzepatide, there was a dramatic increase in effectiveness compared to traditional nonsurgical interventions such as diet, exercise, and lifestyle changes. However, it has been noted that taking tirzepatide on an ongoing basis is recommended and necessary to maintain any weight loss achieved from the medication.
If a patient stops taking the drug, likely, it will no longer work (5).
Public health officials have expressed concerns about using the drug long-term. Still, data is currently lacking regarding long-term effectiveness, treatment duration, and maintaining weight reduction once the therapy is discontinued.
A recent trial consisted of 783 participants with a BMI greater than 30, and these participants agreed to take either a 10mg or 15mg dose of tirzepatide over 36 weeks. The injection is given once weekly, so this would equal a total of 36 injections.
By the end of 36 weeks, participants lost more than 21% of their body weight. After 36 weeks, participants continued on tirzepatide or received placebo treatment for the following year. The patients needed to be made aware of which treatment they were receiving.
Those still taking tirzepatide injections weekly after 88 weeks lost an additional 7% of their body weight, and those taking the placebo regained 15% at the end of 88 weeks (5).

Self Quiz
Ask yourself…
- What is the minimum BMI needed to qualify to receive this drug for weight loss management?
- Is this medication indicated for long-term use for patients with a high BMI?
Common Side Effects and Contraindications
Side Effects
Patients vary immensely with different experiences and side effects related to tirzepatide; however, the following are the most common side effects experienced by those taking the medication:
- Nausea
- Decreased appetite
- Vomiting
- Diarrhea
- Indigestion
- Constipation
- Stomach Pain
Tirzepatide usually does not cause fatigue, leaving one feeling weak, tired, and low energy. However, fatigue can be a common side effect of Type II diabetes.
It is important to note that most individuals who experience nausea, vomiting, and diarrhea episodes do so while the dosage increases, and typically, the symptoms decrease over time. G.I. effects were more prominent in those taking tirzepatide than those taking the placebo. The individuals not in the placebo group were more likely to stop treatment due to the unpleasant side effects (3).


Self Quiz
Ask yourself...
- Does tirzepatide cause fatigue in patients who use it?
Contraindications
Tirzepatide may cause thyroid tumors, including thyroid cancer, and it is essential to watch for possible symptoms, such as swelling or a lump in the neck, hoarseness, shortness of breath, or trouble swallowing.
Tirzepatide should also not be prescribed to any patient with Type 1 Diabetes.
One of the main ways that tirzepatide works is by stimulating the release of insulin from the pancreas, and due to this fact, there have not been many studies and clinical trials that include those with Type I diabetes.
However, this is not to say that prescribers have never ordered tirzepatide for those with Type I diabetes. Still, it is essential to note that if prescribed, it would be in addition to traditional insulin therapy.
- Personal or family history of a type of thyroid cancer known as medullary thyroid carcinoma (MTC).
- Any history of Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
- Patients who are allergic to the actual medication or any of its ingredients.
- Younger than 18 years of age


Self Quiz
Ask yourself...
- What is the reason that tripeptide is contraindicated in those with Type I diabetes?
- Why is there a risk with patients who have a thyroid disorder?
Safe Prescribing Practices, Guidelines, and Considerations for Providers
Safe Prescribing Practices
As with all prescribed medications, safe standards of care must be implemented and followed to ensure patient safety is maintained. The same applies to providers considering prescribing tirzepatide, and specific criteria must be met beforehand. The following information discusses guidelines involving exclusion and inclusion criteria for providers to prescribe tirzepatide (6) accurately.
Guidelines
Exclusion Criteria – If present, the following indicates that the patient should not receive tirzepatide:
- Diagnosis of Type I diabetes
- Personal or family history of medullary thyroid carcinoma or with Multiple Endocrine Neoplasia syndrome type 2
- Severe gastrointestinal dysmotility
- History of pancreatitis
- Pregnancy
- Proliferative Diabetic Retinopathy (PDR), severe Nonproliferative Diabetic Retinopathy (NDR), clinically significant myalgic encephalomyelitis (M.E.), or diabetic macular edema (DME) unless the risks/benefits have been discussed with the patient and are documented in the patient's health record along with monitoring plans and follow-up with an eye specialist who is informed at the time of initiation.
Inclusion Criteria – All of the following must be met for tirzepatide to be prescribed:
- Diagnosis of Type II diabetes
- A BMI of 25 or greater
- Inadequate glycemic control on at least 1mg of semaglutide injection plus two or more glucose-lowering drugs
- Change needed to achieve goal A1C is less than 1%.
- Goal A1C should be based on those recommended in the Diabetic Guidelines.
- Adherence to current diabetic medications as evidenced by a review of the prescription refill history during the six months.
Additional Inclusion Criteria – All of the following must be met for tirzepatide to be prescribed:
- Patients with atherosclerotic cardiovascular disease or chronic kidney disease
- Patients of childbearing potential who are using oral contraceptives
Inclusion Criteria for Weight Loss
- BMI of >30 or >27 with patient weight conditions.

Self Quiz
Ask yourself...
- Would a patient with a BMI of 23 with no comorbidities qualify to use tirzepatide to lose 5-10% of their body weight? Why not?
- What impact can tirzepatide have on a person with a healthy weight and BMI of <25?
Considerations for Providers
There are specific considerations that prescribers must be aware of when contemplating if a patient should receive the medication tirzepatide. The following is imperative and must be considered each time the medication is prescribed to a patient:
- Clinical Indications – indicated for treating adults with insufficiently controlled diabetes mellitus as an add-on therapy to diet and exercise; as monotherapy when metformin is considered inappropriate due to contraindications or intolerance; and other medicinal products for treating Type II diabetes.
- Monitoring of medication – routine monitoring of serum calcitonin or thyroid ultrasound is of uncertain value but is recommended for early detection of Medullary Thyroid Cancer (MTC).
- Cost – the average price for tirzepatide ranges from $1,071-$1,351 without any coupons or insurance. Savings Card – manufacturer provided; patients can pay as little as $25 monthly for up to 12 injections. Savings Card – manufacturer provided; patients can pay as little as $25 monthly for up to 12 injections.
- Benefits and Risks – One must evaluate the effectiveness of diabetes and the weight loss experienced. Some of the risks must be evaluated, such as increased cost of medication, unpleasant gastrointestinal side effects, poor insurance coverage, and drug shortages. The FDA has warned that the medicine can cause thyroid C-cell tumors in rats, and it is not sure whether tirzepatide causes similar tumors.
How long does it take for tirzepatide to begin working?
Tirzepatide will start to lower one's blood sugar levels immediately, but it can take 8 to 12 weeks to reach one's target A1C goal.
Compared to other diabetic treatments, studies have shown that it can take eight weeks to reach an A1C target of less than or equal to 7% and 12 weeks to get an A1C of less than or equal to 6.5%. Significant weight loss can occur as early as 28 weeks.
Safe Administration
It is essential to follow the correct steps for safe administration of tirzepatide as listed below:
- The recommended starting dosage is 2.5mg, injected subcutaneously once weekly. The 2.5mg dosage is for treatment initiation and not for glycemic control.
- After four weeks, increase the dosage to 5mg, injected subcutaneously once weekly.
- If additional glycemic control is needed, increase the dosage in 2.5mg increments after at least four weeks on the current dose.
- The maximum dosage is 15mg, injected subcutaneously once weekly.
- If a dose is missed, instruct patients to administer it as soon as possible, within four days (96 hours) after the missed dose. If more than four days have passed, skip the missed dose, and administer the next dose on the regularly scheduled day. In each case, patients can then resume their regular once-weekly dosing schedule.
- The day of weekly Administration can be changed, if necessary, as long as the time between the two doses is at least three days (72 hours).
- Before initiation, train patients and caregivers on proper injection techniques.
- Instruct patients using the single-dose vial to use a syringe appropriate for dose administration (e.g., a 1ml syringe capable of measuring a 0.5 mL dose).
- Administer the medication once weekly, any time of day.
- Inject the medication subcutaneously in the abdomen, thigh, or upper arm.
- Rotate injection sites with each dose.
- Inspect the medication visually before use. It should appear clear and colorless to slightly yellow. Do not use the medicine if particulate matter or discoloration is seen.
- When using the medication with insulin, administer it as separate injections and never mix. It is acceptable to inject tirzepatide and insulin in the same body region, but the injections should not be adjacent.
Does the tirzepatide injection hurt when administered?
Pain from the injection site has not been reported as a common side effect, but it may occur.
Due to the injection being given subcutaneously, slight pain or discomfort can occur.


Self Quiz
Ask yourself...
- The patient asks you," How long will this take to work?" How will you respond?
- The patient reports they have never used an injection before; what methods can you use to teach your patient how to administer this medication safely?
Alternatives to Tirzepatide for Weight Loss Management
In some instances, patients need to be aware of alternatives to tirzepatide in case they cannot take the actual injection for whatever reason. In cases such as these, there are alternative supplements that can be purchased over the counter, and they include the following (7):
- PhenQ – top OTC choice – comprehensive weight loss solution that targets specific body regions, facilitates prompt fat loss, and expedites the weight loss journey.
- PhenGold – the most potent OTC weight loss alternative – one of the top weight loss supplements that boost metabolism, making one less hungry, less tired, and an overall improved feeling.
- Capsiplex BURN – the best choice for men – helps to burn fat faster and keep blood sugar levels in check. It helps to keep one's muscles, curbs hunger, gives one more energy, and torches stubborn fats.
- Trimtone – the best choice for women – helps women to lose weight, eat less, increase metabolism, burn extra calories, and boost energy.
- Prime Shred – best fat burner for men – boosts metabolism, keeps muscles intact, increases energy, and helps maintain focus.
The advanced practicing nurse or prescriber needs to inform patients about alternative options such as these in an effort for individuals to understand that other choices are available and can be used. Many individuals need to be more knowledgeable about alternatives besides tirzepatide due to the extra hype from social media sources that promote advertisements related to tirzepatide only but do not mention the other options.
Why does social media influence and encourage patients to take tirzepatide?
Social media trends can be helpful but can also become harmful by setting unrealistic expectations and promoting a diet culture mentality. They can create an unhealthy obsession with "clean" eating, especially in the younger populations.
Due to this, many individuals take the medication despite any occurrence or history of Type II diabetes, and the drug can ultimately become misused.
It has been noted that there is an influx of patients requesting this medication for weight loss instead of the intended purpose, which is to help control Type II diabetes.
Tirzepatide represents one of the most recent non-medical treatments aimed at managing the symptoms of Type II diabetes. While it is not indicated for weight management, diabetic patients who receive it frequently report a significant reduction in body weight.
Empirical evidence suggests the efficacy of tirzepatide in weight management, and certain physicians currently endorse the Administration of the medication as a therapeutic and effective means to overcome obesity.
What are some severe side effects of tirzepatide that can impact patient safety?
The Administration of tirzepatide can benefit many individuals, but some severe side effects must be mentioned.
These include thyroid tumors, thyroid cancer, pancreatitis, hypoglycemia, serious allergic reactions, kidney issues, severe stomach problems, vision changes, and gallbladder issues. All these side effects must be taken seriously and reported, as they can lead to life-threatening

Self Quiz
Ask yourself...
- With what you have learned in this course, what education will you provide to patients requesting this medication for weight loss?
- Have you seen increased demand for this medication in your current practice?
- If you Google tirzepatide, your results will likely include links to telehealth services promoting this weight-loss medication. To determine eligibility, what special considerations need to be taken to assess a telehealth patient?
Conclusion
Medications like tirzepatide are game changers for those patients with type 2 diabetes that have failed other medications. Unfortunately, several companies seek to profit from its weight-loss benefits through aggressive marketing campaigns that limit the available supply and increase the costs for those who need it. As healthcare providers, we need to use sound clinical judgment and follow the exclusion/inclusion criteria and other guidelines before prescribing this medication, so we do not unintentionally cause harm while looking to appease our patients who request this.
Semaglutide and Type 2 Diabetes
Introduction
In 2017, the FDA approved the semaglutide injectable (Ozempic) for treating type 2 diabetes. The drug has experienced widespread acceptance due to its positive effects on weight loss and lowering of chronic health risks. The drug has risen in popularity over the past few years, as many well-known actors/actresses/songwriters, and more came forward, publicly sharing their weight loss journey.
This rise in popularity has also resulted in significant shortages of this medication, negatively impacting the lives of the diabetic community, local pharmacies, and healthcare providers. The goal of this continuing education course is to educate and empower the healthcare provider in all aspects of this drug regimen: clinical indications, patient education, cost options, and benefit/risk analysis.
Diabetes Overview
Diabetes is a chronic medical condition. Despite advances in diet, medications, and monitoring devices, diabetes diagnoses continue to grow at staggering rates. The Institute for Health Metrics and Evaluation (IHME) reports that over 529 million people worldwide are currently living with diabetes, and that number is expected to grow to 1.3 billion in only 30 years. While the risk factors for diabetes are vast in number (poor diet, inadequate activity, obesity, sedentary lifestyles, daily stressors, and more), the sad reality is that this chronic medical condition will most likely linger on for generations to come despite our efforts to contain this health epidemic (1).
According to the latest research on diabetes, there are over 37 million people in the United States alone with diabetes as of 2022. Statistically, approximately 28 million of them have a confirmed diagnosis, while another estimated 8 million are experiencing symptoms, without an official diagnosis. Diabetes currently ranks as the 7th leading cause of death in the United States (2).

Self Quiz
Ask yourself...
- As a healthcare provider, what has been your experience with treating chronic medical conditions?
- Why do you think there is a continued increase in diabetes, despite advances in medication and monitoring devices to treat this condition?
- Are you currently offering comprehensive care to your patients, including medication, diet, and activity counseling for their chronic health conditions?
Types of Diabetes
In basic terms, diabetes is an impairment in one’s ability to either adequately produce or utilize insulin, which results in elevated levels of circulating glucose. Chronically elevated glucose levels affect blood vessels at every level, causing chronic inflammation and raising the risk of heart disease, stroke, blindness, and atraumatic amputations.
There are three main types of diabetes:
Type 1 diabetes is thought to be an autoimmune disease. Approximately 5-10 percent of people with diabetes are diagnosed with type 1 diabetes. The diagnosis usually occurs in early childhood, and results in a lifetime use of insulin to regulate blood glucose levels.
Type 2 diabetes is thought to be related to dietary and lifestyle choices. It accounts for nearly 90-95 percent of diabetes diagnoses. Usually occurring later in life (adult-elderly population), it is believed to be related to factors such as diet, activity, weight gain, and related factors. Type 2 diabetes is usually controlled by diet and exercise, in addition to oral medications, although injectable insulin may be included in the treatment plan.
Gestational diabetes refers to elevated glucose levels occurring during pregnancy for patients who are not diabetic at the onset of pregnancy. This version of diabetes usually resolves itself post-partum, although a woman may develop type 2 diabetes later in life, unrelated to pregnancy.
Type 2 diabetes in children: no longer a “later in life diagnosis”
Children are now being diagnosed with type 2 diabetes at an alarming rate. Despite widespread education and an increased awareness of diabetes, our up-and-coming generation is unhealthier than ever. Many families lack access to healthy food for their families, due to both general socioeconomic challenges and an increased rate of food insecurity. (19)
The CDC recommends care providers have resources for diabetic patients and their families, such as food and nutrition programs, budget-friendly diabetes meal plans, how to save money on diabetes care, and coping strategies for diabetes. (19)


Self Quiz
Ask yourself...
- Are you able to articulate the different types of diabetes to patients?
- What resources can you offer to the families of children with type 2 diabetes?
Diabetes Signs and Symptoms, Diagnostic Testing
There are various ways to test for diabetes. The fasting blood sugar (FBS)/ fasting glucose level is a simple way to test for diabetes.
The normal fasting glucose level is below 100mg/dl. The fasting glucose result of 100-125mg/dl indicates prediabetes and results above 126mg/dl indicate diabetes.
The hemoglobin A1C blood test is another test used to confirm the diagnosis of diabetes. The patient does not need to be fasting for this test; thus, it is easier to order this test regardless of the time of day. This blood test reflects the average glucose level over the period of 2-3 months.
The normal A1C level is below 5.7%. Test results between 5.7%- 6.4% indicate prediabetes. Test results above 6.5% indicate diabetes.
A random glucose reading above 200mg/dl, done at any time of day, indicates diabetes.
The diagnosis of diabetes is by blood tests, and for improved accuracy, should be based on two separate readings, done (at least) a day apart. In the case of fasting and random blood tests, dietary intake (large amounts of carbohydrates in a single meal) may adversely affect test results. This is not the case when using A1C testing for a confirmation diagnosis, as the results are the average of a 2–3-month span.
Target blood levels for a person with diabetes (3).
Target blood glucose levels for people with diabetes are as follows:
- Fasting glucose 80-130mg/dl.
- Postprandial blood glucose level- less than 180mg/dl
- A1C level 7-8%.
These target ranges are general guidelines. Patient-specific ranges will be dependent on a variety of factors, including preexisting comorbidities, overall health status, age, and activity levels.

The hallmark signs/symptoms of diabetes
- Polyuria- increased urination
- Polydipsia- increased thirst
- Polyphagia-increased hunger/appetite
The truth is, as healthcare providers, you will have patients who have no hallmark signs and symptoms of diabetes; the diagnosis will be found during annual preventive examinations often unrelated to any chronic disease. For this reason, many insurance companies now cover numerous preventive screenings, including diabetes screenings, as part of their wellness and prevention initiatives. These tests are often approved based on a patient's age, or preexisting conditions, rather than outright signs and symptoms.

Self Quiz
Ask yourself...
- What are the typical glucose levels for non-diabetic versus diabetic patients?
- What are the hallmark symptoms you can identify when treating a potentially diabetic patient?
Lifestyle Interventions and the Diabetes Prevention Program
The initial diagnosis of diabetes can be managed in a variety of ways, depending on the severity of the illness at the time of diagnosis. Lifestyle interventions (behavior modification education) are of utmost importance in the care and management of people with diabetes. Research over the past few decades has consistently shown that such interventions have immense positive effects on the successful long-term management of diabetes.
The official Diabetes Prevention Program was created in 2010 (4) and confirmed the effects of lifestyle interventions in the management of diabetes: Lifestyle interventions decreased the incidence of type 2 diabetes by 58% compared with 31% in the metformin-treated group. Thus, these findings now serve as the blueprint, if you will, for all-inclusive, patient-specific disease management guidelines. These lifestyle interventions will be discussed in detail later in the program.
Additional Resources on Diabetes Prevention

Self Quiz
Ask yourself...
- How do lifestyle interventions compare to other kinds of treatment for patients with type 2 diabetes?
Semaglutide
Semaglutide is an injectable drug used in the treatment of type 2 diabetes. It was approved by the FDA in May of 2017.
It is a once-a-week injectable and belongs to the drug class known as glucagon-like peptide-1 receptor agonists (GLP-1RAs) (5). It has been referred to as a “miracle weight loss drug” among those who are living with obesity, despite frequent side effects, unusually high out-of-pocket costs, drug shortages, and weight regain when attempting to stop using the medication.
GLP-1 receptor agonist: Hormone Review
GLP-1 RAs are a class of medications used to treat Type 2 diabetes, and in some cases, obesity treatment. They are also known as GLP-1 receptor agonists, incretin mimetics, and GLP-1 analogs.
Ghrelin and Leptin (6)
Ghrelin and Leptin are two hormones that greatly influence appetite and the sensation of fullness. Often referred to as the “hunger hormone.” Ghrelin is responsible for many functions, including playing a key role in metabolism through glucose and insulin regulation.
Ghrelin, produced in your stomach, signals your brain when you are hungry, and results in increased food intake.
Leptin, conversely, is produced in your fat cells, and signals to the brain when you have eaten enough (by a decrease in appetite).
Glucagon-like peptide-1 receptors
Known as GLP1 receptors, Glucagon-like peptide-1 receptor proteins are located in the beta cells of the pancreas as well as in the neurons in the brain. GLP-1 receptors are involved in the regulation of blood glucose levels and affect the secretion of insulin. These cells encourage the release of insulin from the pancreas, increase the volume of beta cells, and reduce the release of glucagon. In doing so, they increase the feeling of fullness during and between meals, suppressing the appetite and slowing gastric emptying.

Self Quiz
Ask yourself...
- What are some problems patients might face if they choose to take semaglutide?
- How do Ghrelin and Leptin relate to a patient's appetite?
What is meant by receptor agonist and antagonist?
The term agonist refers to any substance that mimics the actions of a hormone in producing a specific response: a receptor antagonist blocks a response from occurring.
Opioids are examples of receptor agonists in that they produce responses such as analgesia.
Naloxone/Narcan is an example of a receptor antagonist, in that it binds to a receptor site and decreases/blocks a response from occurring.
Semaglutide mechanism of action (7)
GLP-1 agonists work in several ways to positively affect glucose levels. Their mechanism of action includes the following:
- Increasing (stimulating) insulin secretion by the pancreatic beta cells.
- Decreasing the production of glucagon, a hormone that raises blood glucose levels
- Decreasing (slowing) gastric emptying
- Decreasing appetite (and thereby reducing food intake) by creating a sensation of stomach fullness
Through these mechanisms of action, semaglutide results in a lowering of serum glucose/A1C levels, which lowers the risk of cardiovascular events. Studies have also shown that semaglutide resulted in weight loss (approximately 8-14 pounds on average {dose dependent results}.

Self Quiz
Ask yourself...
- What is the difference between an agonist and antagonist substance?
- How much weight do patients lose, on average, when taking semaglutide?
Side Effects of Semaglutide
Common side effects of semaglutide (8)
Common side effects may include any of the following:
- Nausea and vomiting
- Headache
- Diarrhea and stomach pain
- Upset stomach, indigestion, constipation, flatulence
These side effects usually subside within a few weeks, as the patient becomes acclimated to the medication.
Serious side effects of semaglutide
- Hypoglycemia- enhanced/worsened when used in combination with other diabetes medication. Symptoms may include drowsiness, confusion, weakness, irritability, and headache.
- Symptoms may include abdominal pain and distension, nausea and vomiting, fever, and back pain.
- Diabetic retinopathy. Symptoms may include blurred vision, vision loss, and diminished night vision.
- Kidney damage/injury/failure. Symptoms may include fatigue, nausea, diminished urine output, confusion, and edema of extremities.
- Gallbladder disease. Symptoms may include gallstones, abdominal pain, nausea and vomiting, and poor appetite.
Black Box Warning (9)
Semaglutide has a Black Box Warning for thyroid cancer. This is the most serious warning from the Food and Drug Administration (FDA) and is intended to alert consumers to the potential risks of a medication. This black box warning was issued when research found that the drug increased the risk of thyroid tumors in animals.
It is not known if semaglutide actually causes tumors in humans.
Contraindications
- Semaglutide is contraindicated in people with a personal or family history of MTC (medullary thyroid cancer) or in patients with multiple endocrine neoplasia syndrome type 2.
- Known hypersensitivity to semaglutide or any of the product components
Cautions
As noted under “serious side effects”, there have been reports of new illnesses or worsening of existing health conditions occurring “post-marketing”. Thus, healthcare providers are strongly encouraged to continue ongoing surveillance of any patients on semaglutide therapy. In addition, there is insufficient data available regarding the use of semaglutide by pregnant women. Women are therefore highly encouraged to stop any treatment with semaglutide for at least 2 months prior to a planned pregnancy.

Self Quiz
Ask yourself...
- Can you name the 4 common side effects of semaglutide?
- What is the most severe warning associated with semaglutide?
Dosing
Semaglutide is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus (T2DM). It is looked upon favorably to reduce the risk of cardiovascular events in adults with T2DM and a preexisting history of cardiovascular disease. This drug is FDA-approved for use in people with diabetes, with a BMI of 27% or higher (a BMI of 25-29.9% is considered overweight).
Semaglutide (Ozempic) is available as an injectable prescription medication. Doses include 0.5mg, 1mg, or 2 mg, once weekly.
The injection should be administered subcutaneously to the abdomen, thigh, or upper arm. Injection sites should be rotated, and given as a single injection.
Start at 0.25 mg once weekly. After 4 weeks, increase the dose to 0.5 mg once weekly.
- If additional glycemic control is needed, increase the dose to 1 mg once weekly after at least 4 weeks on the 0.5 mg dose.
- If additional glycemic control is needed, increase the dose to 2 mg once weekly after at least 4 weeks on the 1 mg dose
Administer once weekly at any time of day, with or without meals. The maximum dose recommendation is 2mg/weekly once weekly.
Note: The initial 0.25-mg dose is intended for treatment initiation and is not effective for glycemic control
Missing Dose Guidelines
- If the missed dose is ≤5 days: Administer dose as soon as possible
- If missed dose >5 days: Skip the missed dose and administer the next dose on the regularly scheduled day; patients can then resume their regular once-weekly dosing schedule
Administration Day Guidelines (10).
The administration day each week can be changed, if necessary, as long as the time between 2 doses is at least 2 days (>48 hours)
Dose Availability (packaging)
- 2mg/1.5mL (1.34mg/mL); delivers doses of 0.25mg or 0.5mg per injection or four to eight doses per injection pen
- 4mg/3mL (1.34mg/mL); delivers 1mg per injection or 4 doses per injection pen
- 8mg/3mL (2.68 mg/mL); delivers 2mg per injection or 4 doses per injection pen
Treatment Goals- Effects on A1C and Weight (11)
A majority of adults who were placed on injectable semaglutide for diabetes management achieved a target A1C under 7% and were able to maintain it.
- Dose specific effects on A1C were as follows:
- 0.5mg dose injection yielded a 1.4% decrease
- 1.0mg dose injection yielded a 1.6% decrease
- 2.0 mg dose injection, in combination with diabetes pills, yielded a 2.1% decrease in A1C.
Adults taking semifluid injectables for diabetes management also noted weight loss.
- 8-pound weight loss reported with 0.5mg dose injection
- 10 pounds weight loss reported with 1.0mg dose injection
- Up to 14 pounds of weight loss reported with a 2.0mg dose injection


Self Quiz
Ask yourself...
- What should you tell a patient if they miss their injection by more than 5 days? What if it has been less than five days?
Prescribing insights: Long-Term therapy for a chronic condition?
Semaglutide is viewed favorably as a treatment option for Type 2 diabetes. It appears to lower A1C levels and body weight in the majority of patients, lowering their risk of future cardiovascular events.
The question of long-term medication use, for a chronic health condition, is being heavily discussed in the media. While a percentage of people can decrease or eliminate the need for chronic medications through significant lifestyle changes, there have been reports of weight gain in those who stopped taking this injectable medication.
Without intense lifestyle behavior modification education, there is a heightened risk of weight regain in the absence of such medications. Leaders in the treatment of obesity and related illnesses have commented that this drug is intended for long-term use.
Examples of this include the following:
“GLP-1 medications [like Ozempic] are designed to be taken long-term... They are chronic medications for the treatment of chronic conditions (both diabetes and obesity) (12)". - Christopher McGowan, M.D., a gastroenterologist specializing in obesity medicine and endobariatrics
“As with many chronic conditions, most people who use the drugs for diabetes or weight loss will need to keep taking them to keep benefiting from them. Depending on your individual situation, and without sustained lifestyle changes, it is likely you would need to be on these medications indefinitely to maintain weight loss (13)." - Dr. Cecilia Low Wang, a UCHealth expert in endocrinology, diabetes and metabolism.

Self Quiz
Ask yourself...
- Is semaglutide considered to be a long-term treatment for type 2 diabetes?
Cost Concerns
At this time, injectable semaglutide, FDA-approved for the treatment of Type 2 diabetes, has a self-pay price tag of $935.77 per month (4 injections). With FDA approval, many people with diabetes, insured under commercial plans, receive the drug for the cost of their copay. Those patients without coverage may use pharmacy discount cards that reduce the price, on average, to $814.55/month.
The following links are available to familiarize yourself with patient assistance programs related to semaglutide injectables.
Semaglutide Cost Savings Programs
The following links are provided to explore various semaglutide cost savings programs.

Self Quiz
Ask yourself...
- What resources can you offer patients who are struggling to pay for semaglutide?
Emerging Concerns: Semaglutide and gastroparesis
In August 2023, a first-of-its-kind lawsuit was filed in Louisiana, against the makers of semaglutide. The lawsuit states the makers of this injectable drug did not adequately warn patients about the risk of severe gastrointestinal issues/possible gastroparesis.
The plaintiff in this case had used both Ozempic and Mounjaro and experienced repeated episodes of severe gastrointestinal events, warranting trips to the emergency room and additional medications to alleviate her symptoms (14). While this lawsuit is in the developing stages, it bears mentioning in terms of concerns over long-term usage of the drug and possible complications.
While the drug labeling for semaglutide (Ozempic) does not specifically mention gastroparesis, the semaglutide/Mounjaro drug label does state that the drug has not been studied in patients with severe gastrointestinal disease and is therefore not recommended in these patients.
Up to 50% of people with diabetes have some degree of delayed gastric emptying, but most have no digestive symptoms or have only mild symptoms. For some people with diabetes, problems managing blood glucose levels may be a sign of delayed gastric emptying (15).
Healthcare providers should evaluate all patients with diabetes for possible symptoms of underlying gastroparesis, such as the feeling of fullness shortly after beginning a meal, or the inability to finish a regular meal. Other symptoms of gastroparesis may include abdominal pain, nausea, bloating, vomiting, and anorexia.
Diabetes and gastroparesis
Uncontrolled or poorly controlled diabetes can affect nerve endings systemwide. Diabetes is a very common cause of gastroparesis. Although the condition is rare it occurs more often in people with chronic conditions such as diabetes, autoimmune diseases, and nervous system disorders. Nerve endings are injured or damaged, cease to function properly, and result in delayed gastric emptying. The delay in gastric emptying can cause various symptoms, such as nausea, vomiting, bloating and distension, abdominal pain, and poor appetite.
In addition to underlying medical conditions, some medications may cause symptoms of gastroparesis (delays in gastric emptying and overall gastric motility. These medications include narcotics, antidepressants, and anticholinergics.
Left untreated, diabetic gastroparesis may lead to malnutrition, electrolyte imbalances, and poor glucose management and control.

Self Quiz
Ask yourself...
- Why should nurses prescribing semaglutide watch out for symptoms of gastroparesis?
- What do you think are some ethical issues with semaglutide use for weight loss?
Diabetes Lifestyle changes: Patient education (16)
- Weight Management
- Healthy Eating
- Physical Activity
- Smoking Cessation
- Stress Management
The importance of patient education regarding lifestyle changes is a priority. As with any chronic medication condition, the patient and their family/support system must be given every opportunity to educate and empower themselves on self-management of their disease process. Patients must be given the benefit of the doubt that they can indeed embrace their health and well-being and work with their healthcare provider in maximizing their health outcomes.
For diabetes mellitus, numerous lifestyle behaviors should be addressed and actively worked on, so that the patient receives the maximum health benefits. The following lifestyle behaviors are in no particular order; they all warrant discussion at every office visit.
Diet
A person with diabetes should be educated on the effects of food and nutrition on their glucose level. Referrals to a dietitian/nutritionist or Certified Diabetes Care Education Specialist (CDCES) should be considered a top priority. Well-balanced nutritional intake, appropriate carbohydrate awareness, calorie monitoring if weight loss is appropriate to your specific patient) and medication/food interactions are all essential aspects of dietary lifestyle education. Many commercial insurance plans, as well as hospital community outreach programs, offer diabetes self-management classes.

Activity (17)
The CDC recommends a target goal of 150 minutes weekly, Patients should be educated on the positive effects of daily activity on overall health and well-being, stress management, and metabolism. Patients should find activities they are genuinely interested in, involve family and friends, and slowly build greater endurance through increased intervals of longer duration.
Sleep hygiene (18)
Patients should be educated on the positive effects of a good night’s sleep. The aim should be approximately 7-8 hours of restful sleep. Electronics should be powered down and (optimally) removed from the bedroom. A dark, well-vented, cool room temperature is encouraged, and large meals and late-evening caffeine should be avoided.
Medication adherence/ literacy
Medication education is critical to the health and well-being of a patient. Routine education of the patient, and family members or support systems when available, should be supportive and patient-specific. Patients should be assessed on language barriers, literacy issues, and related comprehension concerns. Medication education should include effects, side effects, treatment goals, and sick day management. Emergency care issues should also be discussed. Any monitoring equipment (continuous glucose monitors, accuchecks, lancets) should be reviewed with patients and confirmed with return verbalization and demonstration.
As discussed in this course, patients with chronic diseases must learn self-management techniques to optimize their health and well-being. They must become confident in their understanding of their disease process and take ownership of their health. In doing so, they minimize the risk of long-term complications, improve their self-worth, and actively invest (both time and money) in their future.

Self Quiz
Ask yourself...
- How does sleep, diet, and activity level affect the treatment of type 2 diabetes?
Ozempic Case Study
- 52-year-old female
- Height 67 inches
- Weight 225 pounds
- B/P 138/84, Heart rate 76 NSR
- BMI 35.2%
- Nonsmoker, occasional social drinker
- Multiple attempts at dieting without success.
- Diagnosed T2DM approx. 6 months ago current A1C 7.5%; initial medication Metformin 500mg BID tablets; tolerated well. No GI upsets.
Today’s appointment is for evaluation and additional medication consideration (the patient requested this appointment)
The patient was diagnosed with T2DM approximately 6 months ago. Initial A1C 8.0%. Current A1C 7.7%
Despite an improved diet and adherence to the medication regimen, the patient voiced frustration at the lack of weight loss. Requesting additional medication. Has a neighbor friend who began injectable Ozempic and is having “really great results with it. I want to start on it as well”.
- What are your thoughts on prescribing semaglutide injectable for this patient?
- What objective health data points should be taken into consideration regarding prescribing semaglutide for this patient?
The patient has expressed frustration that despite taking her medications and adjusting her diet, she has not lost any weight in the past 6 months. She has “heard from her neighbor friend that the weight just melts off immediately” and she is ready to start this medication.
- What concerns do you know about this patient's understanding of weight loss as it relates to semaglutide?
- What prescribing information, specific to semaglutide and weight loss, could you share with your patient regarding realistic weight loss targets?
- In addition to teaching your patient proper injection technique for the use of semaglutide, what other lifestyle education behaviors should you discuss at this point?
- What information should you share with your patient regarding the long-term use of semaglutide and the potential risks of stopping this medication (as it relates to weight regain)?
Your patient decides to go ahead with the semaglutide regimen.
- What are some patient education guidelines regarding common side effects of this medication?
- How often is the dose increased? What is the maximum dose this patient can receive weekly?
Your patient wants to know how long she will be taking this medication.
- What talking points will you cover regarding the long-term use of this medication?
- How do you best prepare this patient for long-term success with this medication?
- What lifestyle behavior modification education would you discuss with your patient, to give her the best chance at successfully managing her diabetes?
Medication Assisted Treatment
Introduction
Medication Assisted Treatment (MAT) is a treatment modality for substance use disorders. It combines counseling and behavioral therapies for addiction with medications used carefully to reduce the physical symptoms of cravings and withdrawal and assist clients in the recovery process. With half of people 12 and older reporting use of an illicit substance at least once and 21 million Americans experiencing addiction, this is an important and relevant topic (4).
Historically, an intense stigma is attached to both addiction and some of the medications used to treat addiction. A thorough understanding of substance use disorders, available MAT therapies, and care of affecting clients are essential topics for nurses to be familiar with, particularly those working in psychiatry, pain management, or addiction medicine.
Overview of Addiction and Substance Abuse:
Drug and alcohol abuse and addiction are chronic, complicated issues involving persistent changes to the brain. There is a stigma or misunderstanding that people with substance abuse disorders can stop any time they want to or lack the willpower or moral fortitude to stop using. This is entirely untrue, and even people who are "recovering" and have not had any drugs or alcohol in years can easily relapse into addiction once those brain changes have occurred (5).
When a person uses drugs or alcohol, the brain's reward center is flooded with dopamine. This provides a "buzz" or pleasurable sensation that may create the desire to use more of the same substance. Over time, and with regular use of the substance, the brain becomes accustomed to the flooding of dopamine and reduces the reward response, a process known as tolerance.
It will now take the same person a more significant amount of the substance to achieve the same "buzz" or "high" they used to feel. This process can also dull the pleasure response to activities not involving substance use, such as food, socialization, or sexual activity. Over time, the chemical changes in the brain can progress to include decreased functioning of learning, decision-making, judgment, response to stress, memory, and behavior (5).
To understand substance abuse disorders, it is first essential to understand some basic definitions. These terms are sometimes used interchangeably, but they mean different things and represent different stages of disease.
Definitions
Substance Use: Substance use is any consumption of drugs or alcohol, regardless of frequency or amount. An occasional glass of wine or taking an edible at a party is an example of substance use. Substance use does not cause problems or dependency in many people (5).
Substance Abuse: Substance abuse is the continued use of drugs or alcohol, even when they do cause problems. Conflict or problems at home, school, work, or legal issues related to the use of drugs or alcohol are signs of abuse. For example, being sent home from school for smoking in the bathroom or failing a drug test at work (5).
Substance Dependence or Addiction: Dependence and addiction can be used interchangeably or is sometimes called substance use disorder. Addiction occurs when a person cannot stop drinking or using drugs despite creating problems in their life. People who are addicted may experience cravings until they use a specific substance, or they may experience uncomfortable physical symptoms, known as withdrawal if they do stop (5).
The American Psychiatric Association (APA) utilizes the following criteria to diagnose clients who suffer from addiction. The more criteria a client answers yes to, the greater their problem with substance use.
Six or more positive criteria are indicative of addiction.
- Using substance in more significant amounts or for more extended periods than intended
- Trying to stop using but being unable to
- Increased amounts of time getting, using, or recovering from use of the substance
- Experiencing cravings or urges to use.
- Continuing to use the substance despite problems with relationships or social situations.
- Missing work, social, or recreational obligations or activities because of substance use
- Participating in risky behavior because of substance use
- Continuing to use the substance despite psychological or physical health problems.
- Needing to use more substance over time to achieve the desired effect.
- Experiencing withdrawal symptoms when stopping the substance (1).


Self Quiz
Ask yourself...
- Do you know anyone who suffers from a substance use disorder?
- Think about your biases (thoughts, opinions, attitudes) about addiction. Does any of the information above conflict with those biases?
Substance Abuse Statistics
Many factors go into gathering data on substance abuse disorders, from underreporting, the nuance between use, abuse, and addiction, and the large variety of substances available, with the legality of some substances varying by state or age.
The statistics below from 2020 are not meant to be an exhaustive list of substance use disorders in this country but rather an overview of some of the more prevalent addiction-related issues.
- 50% of people 12 years and older have used an illicit substance at least once.
- 5% of Americans 12 years and older have used drugs within the last month.
- This is a 3.8% increase from the previous year.
- About 50% of Americans 12 and over drink alcohol
- 4% of those people have an alcohol use disorder.
- About 20% of Americans use tobacco products or vape
- 18% of Americans over 18 used marijuana in the last 12 months
- 30% of those have some level of misuse or addiction.
- Marijuana is commonly involved in polysubstance use, paired with alcohol or other drugs.
- 7% of Americans over 12 misused opioids in the last 12 months
- 96% of those used prescription pain relievers
- Opioid prescriptions peaked in 2012, with 81.3 prescriptions per 100 people.
- The rate has declined recently due to increased attention to this crisis.
- In 2018, the rate was down to 51 prescriptions for every 100 people
- Fentanyl is now rising as a new and deadly concern.
- 5 million prescriptions were written for fentanyl in 2015.
- Fentanyl is involved in 53% of overdose deaths.
- 7% of all Americans misuse a prescription drug.
- 1% of those misuse stimulants
- 2% of those misuse sedatives
- 5% misuse painkillers
- Over 70,000 drug overdose deaths occur annually in the United States (4)
Risk Factors
A combination of factors is involved in the risk of addiction, and no one factor can determine if someone will develop addiction or after how many uses this will occur.
The addiction process does occur more easily or progresses more rapidly for people with certain risk factors, including:
Genetics
There is a strong genetic correlation with addiction, indicating that biology plays a significant role in the disorder. Family history of addiction, gender, ethnicity, and comorbid mental health conditions can all influence the risk of addiction. (5)
- Children of addicts are eight times more likely to develop an addiction at some point.
- In 2020, among those using illicit or misusing prescription drugs, 22% were male and 17% female.
- Only 20% of users in drug treatment programs are women.
- 9% of people with substance abuse disorders also have at least one mental health disorder (4)
Environment/Non-Genetic Demographics
The attitudes about drugs and alcohol from those in a person's network and life experiences play a role in the risk of addiction. Substance use among friends, family, or coworkers increases the risk that a person will also use substances. Exposure to substance use from a young age relaxed parental attitudes about substance use, and peer pressure from friends can increase the risk. Certain stressful life circumstances such as veteran status, history of sexual or physical assault, or being part of the LGBTQ community can also increase risk. (5)
- 20% of people in urban areas used illegal drugs in 2020 compared to 5% in rural locations.
- 51% of Americans with an illegal pain relief medication obtained it from a friend or relative.
- 7% of LGBTQ Americans abuse illicit drugs.
- 2% of LGBTQ Americans abuse alcohol.
- 7% of Veterans abuse illicit drugs.
- 80% of Veterans abuse alcohol (4)
Developmental Stage
Substance use at any age can lead to addiction, but children and teens are at particular risk due to their underdeveloped brains. The parts of the brain responsible for decision-making, risk assessment, and self-control do not fully develop until the early 20's, putting teenagers at increased risk of dangerous behaviors. In addition, the effects of drugs and alcohol on the developing brain may mean that those parts of the brain never fully develop at all for teens with substance abuse disorders. (5)
- 70% of users who try an illegal substance before age 13 will develop a substance use disorder within the next seven years.
- This is for only 27% of people who first try an illegal substance after age 17.
- 47% of youths report trying an illegal substance by the time they graduate high school (4)

Self Quiz
Ask yourself...
- Why do you think medication alone is not an adequate treatment for substance abuse disorders?
- Is MAT something you have heard of before? Why do you think it is relatively uncommon despite being around for decades?
Overview of Medication Assisted Treatment (MAT)
Treatment of substance abuse disorders is a complex and often tumultuous process. The nature of the brain changes that occur during addiction means that a person is never entirely "cured" but will always be considered "recovering" as the risk for relapse is always present. Effective treatment must be multifaceted and often involves removing triggers (such as people, places, and stressors) that may prompt a person to use again behavioral therapy, and medications to curb withdrawal symptoms and reduce cravings.
Medication Assisted Treatment (MAT) is a treatment that involves FDA-approved medications, in combination with behavioral therapy, in the recovery process for substance abuse disorders. Several medications are available for MAT, and evidence continues to emerge that the treatment is highly effective if used correctly.
However, it is a vastly underused and understudied treatment modality. MAT has been available in some form for over 50 years but is just starting to gain traction among the medical community (and policymakers) in recent years, with the federal government calling for more research and increased accessibility for the treatment (8).
The height of the opioid crisis in the last several years has highlighted the magnitude of drug addiction and deaths in the United States, bringing renewed attention to MAT as a treatment option. So, how does MAT work? Prescription medication is given to both stimulate the receptors seeking the abused substance and block the drug's euphoric effects.
Over time, this normalizes brain chemistry and helps the person break the habit of using without the discomfort of cravings and withdrawal symptoms. Gradually, the prescription medication dosage is reduced, all the while in conjunction with behavioral therapy and lifestyle changes, and eventually, the client should be able to stop the medication altogether, often within 1-3 months (8).
MAT does require close supervision by a trained medical professional and an appropriate facility for treatment. It can be done on an inpatient, partial inpatient, or outpatient basis. There may be side effects to the medication, and there is a risk of misusing or developing addiction to the new drug, though the successful outcomes often outweigh this risk. Clients must also participate in behavioral therapy for a comprehensive and effective treatment plan. As with any treatment regimen, careful consideration of the client's history and circumstances is essential (8).


Self Quiz
Ask yourself...
- Why do you think medication alone is not an adequate treatment for substance abuse disorders?
- Is Medication Assisted Treatment (MAT) something you have heard of before? Why do you think it is relatively uncommon despite being around for decades?
Pharmacokinetics
Currently, there are three medications with FDA approval for MAT: buprenorphine, methadone, and naltrexone. Each will be discussed in depth below.
Buprenorphine
Mechanism of Action and Metabolism
Buprenorphine is an opioid partial agonist, acting on the same receptors as other opioids but with weaker effects. It can be used for the treatment of misuse of opioids, including:
- Heroin
- Fentanyl
- Oxycodone
- Hydrocodone
- Morphine
- Methadone (3)
Opiate receptors are G-protein coupled receptors (GPCRs) with four major types: Mu, Delta, Kappa, and opioid receptor like-1 (ORL1). Stimulation of these receptors results in varying levels of the following effects:
- Euphoria
- Relaxation
- Pain relief
- Sleepiness
- Sweating
- Constipation
- Impaired concentration
- Reduced sex drive (3)
Buprenorphine has a high affinity to the Mu-opioid receptor and is a partial agonist at this site, causing reduced opioid effects with a plateau or ceiling at higher doses. This limits dangerous effects and makes overdose unlikely. It also has slow dissociation from the site, allowing milder and more easily tolerated withdrawal effects compared to full agonists like morphine and fentanyl. Buprenorphine is also a weak kappa receptor antagonist and delta receptor agonist, reducing the craving sensation and improving tolerance to stress (3).
Buprenorphine has poor bioavailability when given orally due to the first-pass effect, where most of the drug is broken down in the liver and intestines. Because of this, sublingual or buccal are the preferred routes of administration and the most common forms in which the drug is manufactured. Transdermal patches and IV and IM forms exist, though not for use in MAT (3).
CYP34A enzymes break down buprenorphine, so other drugs, such as ketoconazole, may inhibit metabolism and increase available levels of buprenorphine. CYP34A inducers such as carbamazepine, topiramate, phenytoin, and barbiturates may speed metabolism and lower available levels. Once broken down, the med takes the form of norbuprenorphine and is excreted in the feces (3).
Available Forms
Buprenorphine is available by itself and with naloxone (in a 4 to 1 ratio). However, in oral form, naloxone is not readily absorbed, and buprenorphine is the only genuinely active ingredient. This combination is beneficial should clients try to inject their buprenorphine to get high; naloxone is a fast-acting opioid antagonist that is active when used intravenously and would block the opioid effect of buprenorphine, rendering it useless for recreational use and ensuring it has no street value.
The currently available preparations of buprenorphine for MAT include:
- Generic Buprenorphine/naloxone sublingual tablets
- Subutex - Buprenorphine sublingual tablets
- Suboxone - Buprenorphine/naloxone sublingual films
- Zubsolv - Buprenorphine/naloxone sublingual tablets
- Bunavail - Buprenorphine/naloxone buccal film (3)
Sublingual products dissolve within 2-10 minutes. Bloodstream absorption begins quickly, bypassing the first pass effect. Buprenorphine has a slow onset of action, peaking about 3-4 hours later. Metabolism is also slow, with the half-life lasting anywhere from 25 to 70 hours (an average of about 38 hours). This long half-life means the drug can be spaced out to every other day administration once weaning begins (3).
Dosing and Monitoring
Clients prescribed buprenorphine must stop using opioids for at least 12 to 24 hours before the first dose; this varies depending on which opioid they are stopping. For short-acting opioids like heroin and oxycodone, buprenorphine may be started 6-12 hours after the last dose. With longer-acting opioids such as morphine or extended-release preparations of oxycodone, buprenorphine should be delayed for about 24 hours. For the longest action opioids, fentanyl patch, 48 -72 hours must be between the last dose and buprenorphine initiation (3).
This initiation schedule means clients will be in the early stages of discomfort and withdrawal. Administration of buprenorphine when clients still have opioids in their bloodstream will lead to competition for receptor sites, rapidly replacing the opioid with buprenorphine and causing acute and more severe withdrawal symptoms.
Depending on the severity of a client's addiction, they may complete the first step of abstaining and withdrawal in an inpatient setting. Once the initial withdrawal symptoms have passed and the initial dose of buprenorphine has been given, the client may be discharged home to continue buprenorphine initiation on an outpatient basis (3).
Initial doses are typically 2-4mg, with up to 4mg given to clients used to higher potency or larger doses of opioids. The dose is gradually increased to meet the client's individual needs, with a maximum dosage of 24mg per day. The average client requires 8-12 mg per day and can reach this dose within the first 2-4 days. It is recommended that doses be supervised by a pharmacist at the dispensing pharmacy for the first two months of treatment to ensure compliance and clients are less likely to relapse (3).
The length of treatment with buprenorphine depends on each client's case and, for some, may be indefinite. Clients who do wish to wean off buprenorphine can begin the process once they are stable and experiencing few or no cravings, and a minimum of 8 weeks from treatment initiation. Doses are moved to alternating days and eventually discontinued altogether (3).
Side Effects and Contraindications:
As with any medication, there are potential side effects, including:
Common Side Effects
- Nausea
- Vomiting
- Drowsiness
- Dizziness
- Headache
- Memory loss
- Sweating
- Dry mouth
- Miosis
- Postural hypotension
- Sexual dysfunction
- Urinary retention
Serious side effects
- CNS depression
- QT prolongation
- Reduced seizure threshold
- Potential for abuse or overdose (3)
Buprenorphine is contraindicated for clients with a past hypersensitive reaction to it. It should be used cautiously for clients with respiratory suppression, older adults, or for those with liver pathologies. Regular monitoring of liver enzymes via lab work is essential (3).
It is a Category C medication for pregnancy, and the risks versus benefits should be carefully weighed. Buprenorphine does cross the placenta and increases the risk of withdrawal symptoms and neonatal abstinence syndrome (NAS) after delivery. However, for pregnant clients with the highest risk of relapse and abuse of opioids, evidence does support that continuation of buprenorphine during pregnancy may improve maternal and fetal outcomes (3).
Buprenorphine may be abused by crushing tablets, snorting the powder, or dissolving it into an injectable solution. Safety measures against this include supervised administration by a pharmacist and the addition of naloxone, which blocks the buprenorphine effects. While the effect ceiling of buprenorphine makes overdose difficult, combining the drug with benzodiazepines, alcohol, or other drugs can compound the CNS depressant effects and increase the risk of overdose (3).
Clinicians need to have a comprehensive health history of clients before initiating buprenorphine so that all risks and potential interactions can be addressed appropriately.
Role of the Pharmacist
Pharmacists play a significant role in the success of MAT involving buprenorphine. Outpatient doses are monitored by the dispensing pharmacist daily, with at-home quantities being allowed on a limited basis (such as weekends or travel) and only for the most motivated and compliant clients. Vital signs are collected before each dosage, with careful monitoring for hypotension or bradypnea. The dose may be skipped for clients who experience excessive side effects, and the client can return the next day for their dose.
Clients presenting with signs of overdose (usually to the ED) may receive naloxone, which will reverse overdose symptoms within 1 hour. Overdose symptoms include dizziness, pinpoint pupils, hypotension, bradypnea, hallucinations, seizure, or unconscious state.
If a client misses a dose, does not show up for it, or is experiencing significant side effects from buprenorphine, the prescribing clinician should be notified so that the treatment plan can be revisited and revised if needed (3).
Considerations for the Prescriber
When considering which medication to prescribe for MAT, prescribers should understand that buprenorphine offers advantages over methadone.
- Lower risk of abuse
- Safer, including at higher doses.
- Therapeutic dose achieved quickly.
- Easier to taper.
- Can be obtained from any provider rather than a methadone clinic.
- Less stigma
The cost of a 30-day supply is around $300. Buprenorphine/naloxone combinations are a little more expensive at $400/month. While prior authorization is usually required, most commercial insurance and state Medicaid programs will cover the medication.
Buprenorphine is a Schedule III Controlled Substance; however, recent federal regulations have been aimed at approving access to MAT, and any provider with an active DEA license may prescribe buprenorphine as allowed by state regulations. Specialized clinics are not required (as they are with methadone), and it is dispensed at regular pharmacies.
Prescribers are encouraged to participate in additional training about MAT with buprenorphine, but it is not required. Detailed documentation must be completed, including the reason for prescribing, start and end dates of treatment, the pharmacy used, the credentials of who will supervise administration, and frequency of follow-up and compliance monitoring. The sublingual and buccal routes are the only forms of medication used for MAT; patches, IM, and IV preparations are not routinely used for MAT.
The success of buprenorphine treatment depends on the client's education. Addiction potential, risk of combination with other CNS depressants, and side effects vs. signs of overdose should all be discussed with clients and their support system (3).

Self Quiz
Ask yourself...
- Given the nature of substance abuse disorders, why do you think including an opioid antagonist like naloxone in preparations of buprenorphine is necessary for safety and compliance?
- What challenges do you see with a medication needing to be administered daily with pharmacist supervision?
- What are the risks of buprenorphine being given without this supervision?
- Consider the possible pros and cons of taking a medication like buprenorphine during pregnancy. Also, consider the risks of NOT taking the drug during pregnancy when a substance use disorder is present.
Methadone
Mechanism of Action and Metabolism
Methadone is a synthetic opioid and a full agonist of the Mu-receptor site, stimulating the same effects as opioids.
- Euphoria
- Analgesia
- Sedation
It can be used as a potent analgesic for pain not responding to traditional medications, such as in clients with cancer or terminal illness, as well as for MAT and neonatal abstinence syndrome (NAS).
For this course, it will be discussed as a MAT agent, used in treatment for clients addicted to opioids such as:
- Heroin
- Fentanyl
- Oxycodone
- Hydrocodone
- Morphine
- Hydromorphone (2)
Methadone is a full agonist at the Mu-receptor, meaning it is a more potent and more easily addictive medication than partial agonists like buprenorphine. Methadone has a long half-life (8-60 hours), occupying the Mu-receptors and blocking short-acting opioids from making a client high. The longer half-life also leads to less severe cravings and withdrawal symptoms. Methadone is also an antagonist to the N-methyl-d-aspartate (NMDA) receptor, which adds to its pain relief action (2).
It has high oral bioavailability, is active in the bloodstream within 30 minutes of ingestion and remains elevated for around 24 hours. It is broken down via CYP3A4 and CYP2B6 enzymes and metabolized through the liver, making it a good option for clients with renal problems.
Medications such as ciprofloxacin, benzodiazepines, fluconazole, cimetidine, and fluoxetine may slow methadone metabolism, increasing the available drug and the side effects of overdose risk. Other medications may speed metabolism and decrease the effects of methadone, including phenobarbital, phenytoin, rifampin, ritonavir, and carbamazepine (2).
Available Forms
Methadone is available in many forms, including oral, IM, subcutaneous, IV, and intrathecal, though only the oral is typically used for MAT.
- Methadone - tablets
- DISKETS - dispersible/dissolvable tablet
- Methadone HCL Intensol - 10mg/ml suspension
- Methadone - dispersible tablet (2)
Dosing and Monitoring
Oral dosing is initiated at 30-40 mg/day with a slow titration of 10-20 mg/week until the optimal dosage is reached. The optimal dosage varies by client and depends on the drug they are replacing, tolerance to opioids, and side effects experienced. A dosage between 80- 150 mg/day is the typical goal. (2)
If parenteral methadone is given, it is usually 50%-80% of the oral dosage.
Blood sugar, EKG, and methadone blood levels should be checked regularly, every week for higher-risk patients, and every 3-6 months for those in good health and compliance. The target methadone blood level is around 400 ug/ml (2).
Side Effects and Contraindications
Potential side effects are directly related to stimulation of the opioid receptors and include:
- Diaphoresis
- Flushing
- Pruritus
- Nausea
- Dry mouth
- Constipation
- Sedation
- Lethargy
- Respiratory Depression
- QT prolongation
- Hypoglycemia (2)
Methadone should be considered with a comprehensive view of a client's health history and other medications. Clients with CNS-related disease processes (trauma, increased ICP, dementia, or delirium) must be monitored closely or have other medication considered.
Methadone should not be used simultaneously as other opioids, benzodiazepines, alcohol, or antipsychotics due to increased CNS effects. Methadone is a Pregnancy Category C medication, and risks versus benefits should be weighed carefully. Infants exposed to methadone in utero are at increased risk of NAS after delivery (2).
Overdose can occur, and clients and support systems should be educated on signs of overdose.
- Lethargy
- Somnolence
- Stupor
- Coma
- Miosis
- Bradycardia
- Hypotension
- Respiratory sedation
- Cardiac arrest
Naloxone is used to reverse overdose (2).
Considerations for Prescribers and Clinics
Methadone is a Schedule II Controlled Substance, meaning it has a high abuse potential and must be carefully monitored. The Prescription Drug Monitoring Program (PDMP) is an electronic database used nationwide to register the distribution of controlled substances so that clients do not seek care at multiple clinics or pharmacies to obtain more of a controlled substance.
When prescribing methadone, providers should check the PDMP for both methadone and other prescription opioids so that they are fully aware of other medications clients may be receiving from other places. Regular urine drug screening should be performed to make sure clients are not using other substances not obtained by prescription and that they are testing positive for methadone, meaning they are genuinely taking it if administration is not observed (2).
At the beginning of treatment, methadone is given in the office under a nurse's supervision, and then clients are monitored for adverse effects. Some take-home doses (up to 7 in the first two weeks) may be arranged for weekends or during travel, but this possibility is limited during the first few weeks of treatment. As treatment progresses and compliance is demonstrated, clients may self-administer more doses at home (up to 28 doses per month) and go longer between visits to the clinic. The total length of treatment varies but is often 1-2 years and can even be indefinite (7).
There are methadone clinics that work entirely in the scope of addiction management, but primary care providers may prescribe methadone as well. Prescribers must have an active DEA license and comply with state-based controlled substance regulations (2).


Self Quiz
Ask yourself...
- Why do you think methadone is a Schedule II Controlled Substance while buprenorphine is only a Schedule III?
- What are the benefits of checking the serum level of methadone?
- What might the clinical presentation be for someone overdosing on methadone?
- Have you ever used the PDMP database before? What are the benefits of accessing this database?
Naltrexone
Mechanism of Action and Metabolism
Naltrexone has been in use since the 1960s and is an opioid antagonist. It competes primarily with the mu-receptor but also serves as an antagonist at the kappa and delta receptors. As an antagonist, it competes with agonists such as opioids and alcohol and blocks the effects of agonists at those sites.
- Prevents euphoria.
- Prevents intoxication.
- Reduces tolerance (6)
Naltrexone also acts on the hypothalamic-pituitary-adrenal axis, modifying it to reduce cravings and suppress alcohol consumption.
It is FDA-approved for use in clinical practice for the treatment of:
- Alcohol use disorder
- Opioid use disorder (prescription and non)
Naltrexone is absorbed orally and undergoes extensive metabolism via the first-pass effect. However, this does not affect its potency as naltrexone's active metabolite, 6β-naltrexone, acts as a potent opioid antagonist. The medication's half-life is around 4 hours but can last up to 24 hours. If administered parenterally, it bypasses the first pass and is even longer acting, with a half-life of 5-10 days. Naltrexone is excreted by the kidneys (6).
Available Forms
Naltrexone is available in an oral tablet and IM injection. Available preparations include:
- Generic naltrexone tablets
- Revia (oral tablet)
- Depade (oral tablet)
- Vivitrol (solution for IM injection, extended-release) (6)
Dosing and Monitoring
Since naltrexone will compete for and block all opioid receptor sites, the risk for withdrawal symptoms is high, and clients must stop the use of alcohol or opioids for 7-10 days before beginning treatment to lessen the risk of withdrawal symptoms. A naltrexone challenge is recommended at the start of therapy.
This consists of administering small amounts of naltrexone subcutaneously or via IV and monitoring the client and their vital signs for signs of withdrawal, such as:
- Nausea
- Vomiting
- Diaphoresis
- BP changes
- Tachycardia
- Rhinorrhea
- Agitation
- Tremors
- Abdominal pain
- Pupillary dilation (6)
If a client fails the naltrexone challenge and has not been long enough since their last use of alcohol or opioids, the naltrexone initiation should be delayed, and the test should be repeated in 24 hours. If clients tolerate the naltrexone test and the negative result, they may begin naltrexone treatment (6).
For oral tablets, dosing usually starts at 25 mg for the first dose. Clients are observed for withdrawal symptoms and side effects; an additional 25 mg is given 1 hour later. After that, clients take 50 mg per day. Clients may continue with 50mg daily or take 100 mg every other day or 150 mg every 3rd day (6).
Alternatively, naltrexone may be given via IM injection for more extended action, improving compliance and reducing relapse. Particularly for alcohol or heroin dependence, data indicates that the IM route has much higher success rates than the oral route. If a client receives the IM injection, 380 mg is given to the gluteal muscle every four weeks (6).
Side Effects and Contraindications
Most common side effects of naltrexone include:
- GI irritation
- Diarrhea
- Abdominal cramps
- Nausea
- Vomiting
- Hypertension
- Headache
- Anxiety
- Low energy
- Joint or muscle pain
- Nervousness
- Sleep disruption
Less commonly, clients report:
- Loss of appetite
- Constipation
- Dizziness
- Irritability
- Depression
- Rash
- Chills (6)
Caution should be used for clients with liver function issues and renal impairment. It is Category C for use during pregnancy, and the risks versus benefits of use in pregnancy must be carefully considered. It also crosses into breast milk and must be considered carefully.
There is limited data about the overdose of naltrexone, and there may be very few symptoms if an overdose occurs. Clients should be monitored for signs of liver dysfunction, seizures, depression, and suicidal ideations. No antidote for naltrexone is currently available.
Naltrexone is contraindicated for clients who failed a naltrexone challenge, test positive for opioids or alcohol on drug screening, have a history of seizures, or have experienced a past hypersensitivity reaction to naltrexone.
Clients may switch from buprenorphine or methadone to naltrexone at some point in treatment. Both medications are agonists at the opioid receptor sites, so changing to naltrexone (an antagonist) may increase the risk of withdrawal symptoms for the first two weeks of treatment (6).
Considerations for Prescribers
Because naltrexone does not cause any euphoria or "high," the abuse potential is non-existent. It is not a controlled substance and can be prescribed by any clinician with prescriptive authority. However, its use is typically only by those who work in mental health or addiction medicine. Clients can take the medication at home or go to the clinic for IM injections.
Many considerations for naltrexone use center around monitoring for side effects and treatment compliance. Baseline and periodic drug screening and liver function tests are prudent. Clients' support persons should be educated on compliance and signs of relapse. The IM formulation should be considered for those with poor compliance or most at risk for relapse (6).

Self Quiz
Ask yourself...
- Why might a client benefit from the IM formulation of naltrexone instead of the oral preparation?
- Why might compliance with an opioid antagonist be more complex than an opioid agonist like methadone or buprenorphine?
- How do side effects differ between naltrexone and the agonist medications like methadone?
- What does it mean if a client fails a "naltrexone challenge," and how does this delay their care?
Nursing Considerations
Nurses will encounter clients with addiction and even those receiving MAT in a variety of settings, including:
- Outpatient clinics for routine care of any health issues
- ED admission for acute problems not related to addiction.
- Inpatient hospitalization related to other health problems.
- Outpatient setting for participation in MAT or addiction management.
- ED admission for acute problems related to substance abuse or toxicity of MAT medication.
- Inpatient mental health admission for mental health and addiction issues
Regardless of the setting and if the client is being seen for an addiction issue or something else, it is crucial for nurses to be familiar with MAT medications and how they work to provide safe and competent care. Nurses may need to:
- Administer medication.
- Monitor lab results.
- Observe for side effects, toxicity, or withdrawal symptoms.
- Coordinate care within a multidisciplinary team
- Communicate with therapeutic and nonjudgmental techniques.


Self Quiz
Ask yourself...
- Have you ever cared for a client in a non-addiction setting who had a MAT medication on their drug list?
- Did you have any biases or preconceived ideas about what this medication meant?
- Is there anything you have learned throughout this course that will change your care the next time you encounter a client receiving MAT?
Case Study
Justin is a 32-year-old male who presents to the ED with nausea, lethargy, and confusion worsening over the last 24 hours. Upon exam, the nurse notes diaphoresis, slurred speech, and pinpoint pupils. His vitals are RR 10, HR 54, BP 82/58, SPO2 97%, Temp 99.0.
He reports taking Wellbutrin 150mg daily for depression and smoking cessation, methadone 100mg daily for history of oxycodone abuse, and was started on ciprofloxacin 250mg BID for a UTI 2 days ago at urgent care.
His labs are significant for a WBC of 15,000 but otherwise regular. He tests positive for methadone, which is expected, but not for other substances. He reports being compliant with MAT and avoiding opioid use for nine months.
It is determined that Justin is experiencing methadone toxicity due to the slowed metabolism of the drug from the combination of methadone and ciprofloxacin. He is given naloxone in the ED, and within an hour, his symptoms have improved significantly, and his vital signs are typical. His antibiotic is switched to cefdinir, and he is discharged home in stable condition with instructions to follow up with his PCP within 1-2 days.

Self Quiz
Ask yourself...
- Given Justin's presentation, how could you differentiate between methadone toxicity and relapse?
- How might Justin's condition have progressed if he had not sought emergency care?
- How would Justin's case have been different if he had not tested positive for methadone?
- In what ways could Justin's care before his ED visit have been improved to avoid this complication?
Conclusion
Substance use disorders are a long-standing and dangerous pathology experienced by millions of people each year. At the same time, the stigma of seeking help for such disorders has been eroding in recent years; there has also been a renewed push by the federal government to address the issue in evidence-based and meaningful ways, with access to effective treatment being at the top of the priority list.
Addiction treatment programs utilizing MAT will likely become much more popular in the coming years, and nurses will be on the front lines of this therapy. For nurses to provide competent and comprehensive care to this client population, up-to-date and accurate knowledge is necessary.
Hypertensive Agents
Definitions
Hypertension – high blood pressure above normal. Normal is considered anything less than 120/80 mmHg [7].
Antihypertensives – medications used to control hypertension and lower blood pressure [7].
Hypertensive crisis – severely elevated blood pressure of either:
- Systolic greater than 180 mmHg
- Diastolic greater than 120 mmHg [19].
Hypertensive emergency – acutely elevated blood pressure with signs of target organ damage [2].
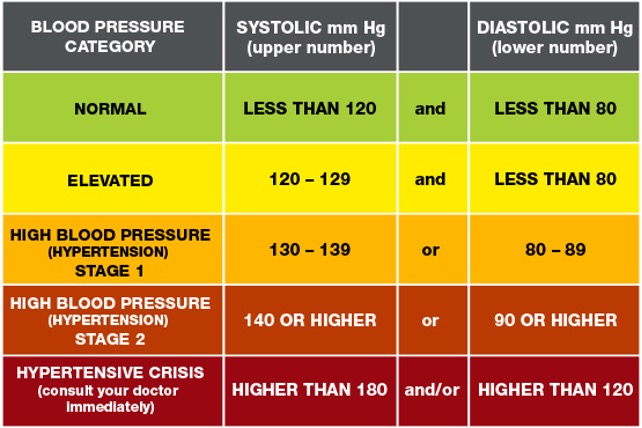

Self-Quiz
Ask Yourself...
- What is hypertension?
- What are antihypertensives?
- What is a hypertensive crisis?
- What is a hypertensive emergency?
Medications Overview
Antihypertensive medications are used for the treatment of hypertension and are used in both inpatient, outpatient, and emergency settings.
Some of the major antihypertensive medication classes include:
- Diuretics
- Beta-blockers
- Angiotensin-converting enzyme inhibitors
- Angiotensin II receptor blockers
- Calcium channel blockers
- Selective alpha-1 blockers
- Alpha-2 Receptor Agonists
- Vasodilators [3].
Different medical organizations have varying recommendations and hypertension treatment guidelines. Hypertension treatment clinical practice guidelines are available from organizations like the American Heart Association, the American College of Cardiology, and the European Society of Cardiology to name a few [21]. Healthcare providers should be aware of their healthcare institution’s recommendations for clinical practice guidelines and organizations.
All organizational guidelines share the same recommended treatment of starting antihypertensives immediately when:
- Blood pressure is greater than 140/90 mmHg for patients with a history of ischemic heart disease, heart failure, or cerebrovascular disease.
- Blood pressure is greater than 160/100 mmHg regardless of underlying medical conditions [21].
Again, healthcare providers should follow current and evidence-based clinical guidelines for initiating or titrating antihypertensive medications.
While most antihypertensives are prescribed in an outpatient setting, certain antihypertensives are indicated during hypertensive or medical emergencies. For example, intravenous (IV) vasodilators, like nitroprusside and nitroglycerin, and calcium channel blockers, like nicardipine, are used during hypertensive emergencies and crises.


Self-Quiz
Ask Yourself...
- In what settings are antihypertensives used?
- What are the clinical guidelines for initiating hypertensive medications?
- Which medications are commonly used to treat hypertensive emergencies?
Pharmacokinetics
Diuretics
Diuretics are a class of drugs that help control blood pressure by removing excess sodium and water from the body through the kidneys. There are several varying types of diuretics, some including thiazide, potassium-sparing, and loop, and all work to lower blood pressure differently [3].
Thiazide Diuretics
Thiazide diuretics remove excess sodium and water from the body by blocking the sodium-chloride (Na-Cl) channels in the kidneys’ distal convoluted tubule. As the Na-Cl channel becomes blocked, this inhibits the reabsorption of sodium and water into the kidneys. Concurrently, this causes a loss of potassium and calcium ions through the sodium-calcium channels and sodium-potassium pump [1].
Thiazide diuretics are approved by the Food and Drug Administration (FDA) for controlling primary hypertension and are available via oral route. Some common thiazide diuretics are hydrochlorothiazide, chlorthalidone, and metolazone [3].
When initiating this medication, the healthcare provider should start with the lowest dose, which is usually 25mg daily, and then increase accordingly to aid with blood pressure control or if the patient has excess fluid retention, usually as evidenced by leg swelling or edema [1].
Common side effects of thiazide diuretics include:
- Increased urination
- Diarrhea
- Headache
- Stomach and muscle aches [16].
As thiazide diuretics interfere with Na-Cl, Na-Ca, and Na-K channels, there is an increased potential for adverse effects, including:
- Hypotension
- Hypokalemia
- Hyponatremia
- Hypercalcemia
- Hyperglycemia
- Hyperlipidemia
- Hyperuricemia
- Acute pancreatitis
When prescribing thiazide diuretics, healthcare providers should avoid prescribing thiazide diuretics to patients with a sulfonamide allergy, since thiazides are sulfa-containing medications. Also, they should avoid prescribing these to patients with a history of gout [1].
Additionally, patients can experience a thiazide overdose if they take more than the amount prescribed. Patients with a suspected overdose may experience confusion, dizziness, hypotension, and other symptoms. These patients must seek emergency care and poison control must be alerted [16].
Potassium-Sparing Diuretics
Potassium-sparing diuretics remove excess sodium and water from the body without causing loss of potassium. Depending on the type, they interrupt sodium reabsorption by either binding to epithelial sodium channels or inhibiting aldosterone receptors. When catatonic sodium is reabsorbed, this creates a negative gradient causing the reabsorption of potassium ions through the mineralocorticoid receptor [5].
Potassium-sparing diuretics are approved for controlling hypertension and are usually combined with other diuretics, like thiazide or loop diuretics since they have a weak antihypertensive effect.
Common names of potassium-sparing diuretics are amiloride, triamterene, and spironolactone. These medications are available by either intravenous or oral routes. Spironolactone is commonly used for treating primary aldosteronism and heart failure [5]. Patients should be started on the lowest dose when first prescribing this class of medications.
Common side effects can include:
- Increased urination
- Hyperkalemia
- Metabolic acidosis
- Nausea
[4]
Healthcare providers should avoid prescribing this class of medications to patients with hyperkalemia or chronic kidney disease. They should also be avoided during pregnancy or in patients who are taking digoxin. Since potassium-sparing medications can cause hyperkalemia, periodic monitoring for electrolyte imbalances and potassium levels is necessary [4].
Loop Diuretics
Loop diuretics inhibit sodium and chloride reabsorption by competing with chloride binding in the Na-K-2Cl (NKCC2) cotransporter. Potassium is not reabsorbed by the kidney, which causes additional calcium and magnesium ion loss.
Loop diuretics are FDA-approved for the treatment of hypertension but are not considered first-line treatment. They can also be used for treating fluid overload in conditions like heart failure or nephrotic syndrome [12].
Loop diuretics are available via oral or IV routes and furosemide, torsemide, and bumetanide are common forms [3].
Bioavailability and dosage differ for each type and route of loop diuretics. The bioavailability of furosemide is 50%, with a half-life of around 2 hours for patients with normal kidney function, and dosages start at 8mg for oral medication. Torsemide has a bioavailability of about 80%, a half-life of about 3 to 4 hours, and oral dosages start at 5mg [12].
Common side effects can include:
- Dizziness
- Increased urination
- Headache
- Stomach upset
- Hyponatremia
- Hypokalemia [13].
Loop diuretics can lead to several adverse effects, including toxicity, electrolyte imbalances, hyperglycemia, and ototoxicity. They have a black box warning stating that high dosages can cause severe diuresis. Therefore, electrolytes, BUN, and creatinine values should be monitored closely by a healthcare provider.
People with a sulfonamide allergy may also be allergic to loop diuretics, so this should be avoided if the patient is allergic. Loop diuretics also interfere with digoxin and therefore should be avoided. Other contraindications include anuria, hepatic impairments, and use during severe electrolyte disturbances [12].


Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of thiazide diuretics?
- What is the pharmacokinetics of loop diuretics?
- What is the pharmacokinetics of potassium-sparing diuretics?
- What are common side effects and contraindications for each type of diuretic?
Beta-Blockers
Beta-blockers work by reducing the body’s heart rate and thus, lowering cardiac output resulting in lowered blood pressure [3]. The mechanism of action for beta-blockers varies, depending on the receptor type it blocks, and are classified as either non-selective or beta-1 (B1) selective.
Non-selective beta-blockers bind to the B1 and B2 receptors, blocking epinephrine and norepinephrine, causing a slowed heart rate. Propranolol, labetalol, and carvedilol are common non-selective beta-blockers.
Alternatively, beta-1 selective blockers only bind to the B1 receptors of the heart, so they are considered cardio-selective. Some examples include atenolol, metoprolol, and bisoprolol. Sotalol is a type of beta-blocker that also blocks potassium channels and is, therefore, a class III antiarrhythmic [8].
Beta-blockers are not primarily used for the initial treatment of hypertension but can be prescribed for conditions like tachycardia, myocardial infarction, congestive heart failure, and cardiac arrhythmias. It’s also approved for use in conditions such as essential tremors, hyperthyroidism, glaucoma, and prevention of migraines.
Beta-blockers are available in many forms, including oral, IV, intramuscular injection, and ophthalmic drops. Starting dosage and route are determined by the health condition being treated [8].
Common side effects of beta-blockers include:
- Bradycardia
- Hypotension
- Dizziness
- Feeling tired
- Nausea
- Dry mouth
- Sexual Dysfunction
[17]
This class of medications can also lead to more severe adverse effects such as orthostatic hypotension, bronchospasm, shortness of breath, hyperglycemia, and increased risk of QT prolongation, torsades de pointes, and heart block [8]. Healthcare providers should avoid prescribing non-selective beta-blockers to patients with asthma. Instead, they can prescribe cardio-selective beta-blockers for patients with asthma.
Additionally, the use of beta-blockers is contraindicated in patients with a history of bradycardia, hypotension, Raynaud disease, QT prolongation, or torsades de pointes. Healthcare providers must encourage patients to monitor their heart rate and blood pressure and follow administration parameters before taking beta-blockers daily since it decreases their heart rate.
Overdose of beta-blockers is life-threatening and healthcare providers must discuss the symptoms of an overdose and the need for emergency care [8].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of beta-blockers?
- What are the common side effects and contraindications of beta-blockers?
Angiotensin-converting Enzyme Inhibitors
Angiotensin-converting enzyme (ACE) inhibitors prevent the body from producing angiotensin, a hormone that causes vasoconstriction. As angiotensin production is reduced, this allows the blood vessels to dilate and therefore lowers blood pressure [3].
Moreover, ACE inhibitors act specifically on the renin-angiotensin-aldosterone system (RAAS) by preventing the conversion of angiotensin I to angiotensin II. It also works to decrease aldosterone, which in turn, decreases sodium and water reabsorption [9].
ACE inhibitors usually end in the suffix -pril and some common examples include lisinopril, benazepril, enalapril, and captopril, and they usually end in the suffix [3].
While ACE inhibitors are approved for treating hypertension, they are also FDA-approved for other uses or combination therapies for medical conditions such as:
- Systolic heart failure
- Chronic kidney disease
- ST-elevated myocardial infarction
One non-approved FDA use is treatment of diabetic nephropathy [9]. This class of medication is available in oral, and IV forms, and dosages are dependent on clinical guidelines, underlying medical conditions, and route.
ACE inhibitors have common side effects, with some including:
- Dry cough
- Dizziness
- Hypotension [9].
This medication can also lead to adverse effects, such as syncope, angioedema, and hyperkalemia [9]. As angioedema is an adverse effect, healthcare providers should understand this class of medications is contraindicated in patients with a history of hypersensitivity to ACE inhibitors.
Additionally, ACE inhibitors are contraindicated in patients with aortic valve stenosis, hypovolemia, and during pregnancy. Individuals with abnormal kidney function should have renal function and electrolyte values monitored. If a patient develops a chronic dry cough, then the healthcare provider should consider another antihypertensive medication class by following current guidelines [9].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of angiotensin-converting enzyme inhibitors?
- What are common side effects and contraindications of angiotensin-converting enzyme inhibitors?
Angiotensin II Receptor Blockers
Similar to ACE inhibitors, Angiotensin II Receptor Blockers (ARBs) act on the RAAS by binding to angiotensin II receptors and thus block and reduce the action of angiotensin II. Again, this reduces blood pressure by causing blood vessel dilation and decreasing sodium and water reabsorption [11]. ARBs typically end in the suffix -artan and common names are losartan, valsartan, and Olmesartan [3]. Oral and IV routes of the medication are available and again, dosages are dependent on the medication specifically and form [11].
All ARBs are FDA-approved for the treatment of hypertension, but a select few are approved for treating other medical conditions, such as:
- Candesartan for heart failure
- Irbesartan for diabetic nephropathy
- Losartan for proteinuria and diabetic nephropathy
- Telmisartan for stroke and myocardial infarction prevention
- Valsartan for heart failure and reduction of mortality in patients with left ventricular dysfunction [11].
Although not as common as ACE inhibitors, two side effects of ARBs are dry cough and angioedema.
Other common side effects include:
- Dizziness
- Hypotension
- Hyperkalemia
[11]
Contraindications for use are if the patient is pregnant or has renal impairment or failure. If a patient is on an ARB, the healthcare provider should closely monitor lab values for electrolyte imbalances and kidney function.
Additionally, if a patient is taking lithium, ARBs can increase lithium concentration and therefore, lithium blood concentration should be frequently checked [11].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of angiotensin II receptor blockers?
- What are common side effects and contraindications of angiotensin II receptor blockers?
Calcium Channel Blockers
Calcium channel blockers (CCBs), also known as calcium channel antagonists, act by preventing calcium from entering the smooth vascular and heart muscles. In turn, this reduces heart rate and causes vasodilation [3].
They are further divided into two major categories, non-dihydropyridines and dihydropyridines, where there are differences in the mechanism of action. Non-dihydropyridines inhibit calcium from entering the heart’s sinoatrial and atrioventricular nodes and thus cause a cardiac conduction delay and reduce cardiac contractility.
Alternatively, dihydropyridines do not directly affect the heart but do act as a peripheral vasodilator leading to lowered blood pressure. Both categories are metabolized by the CYP3A4 pathway [15].
Names of non-dihydropyridine CCBs are verapamil and diltiazem. Dihydropyridine CCBs typically end in the suffix -pine and common names are amlodipine and nicardipine. Both categories are available via oral and IV routes for administration. Oral dosages of non-dihydropyridine CCBs start at 30mg daily and dihydropyridine CCBs start at 30mg daily for immediate release [15].
Calcium channel blockers can be used to treat other medical conditions in addition to hypertension and include:
- Coronary spasm
- Angina pectoris
- Supraventricular dysrhythmias
- Pulmonary hypertension
- Hypertrophic cardiomyopathy
Non-dihydropyridine CCBs can cause side effects like bradycardia, and constipation, while dihydropyridine CCBs can cause:
- Headaches
- Feeling lightheaded
- Leg swelling [15].
Both categories pose the risk of potential hypotension and bradycardia, so healthcare providers should closely monitor the patient’s blood pressure and heart rate when initiating or titrating the dosage.
Also, an overdose of this medication can lead to cardiac conduction delays, complete heart block, and cardiovascular collapse. Patients with possible symptoms of overdose should be sent to the emergency room immediately.
Additionally, healthcare providers should avoid prescribing CCBs to people with heart failure and sick sinus syndrome [15].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of calcium channel blockers?
- What are the common side effects and contraindications of calcium channel blockers?
Selective Alpha-1 Blockers
Selective alpha-1 blockers act on the body’s sympathetic nervous system to lower blood pressure. They prevent norepinephrine from binding to the alpha-1 receptors of the sympathetic nervous system, causing smooth muscle relaxation and vasodilation which leads to lowered blood pressure [18].
Selective alpha-1 blockers are available via the oral route, end in the suffix -osin and examples are doxazosin, terazosin, and prazosin [3]. They are FDA-approved for the treatment of hypertension but are not considered first-line therapy. Additionally, this class of medications may be used to treat benign prostatic hyperplasia. Dosages can start as low as 1mg daily depending on the drug selected.
Common side effects include:
- Hypotension
- Tachycardia
- Dizziness
- Headache
- Weakness [18].
As selective alpha-1 blockers can lead to orthostatic hypotension, the healthcare provider should instruct the patient to take this medication at night. They should also avoid prescribing to the elderly population when able because of hypotension and increased fall risk [18].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of alpha-1 blockers?
- What are the common side effects and contraindications of alpha-1 blockers?
Alpha-2 Receptor Agonists
Alpha-2 receptor agonists work by decreasing the activity of the sympathetic nervous system to lower blood pressure. It inhibits adenylyl cyclase and decreases the formation of cyclic adenosine monophosphate (cAMP). Alpha-2 agonists also cause vasodilation by reducing the amount of available cytoplasmic calcium [20].
This class of medications is typically administered via oral route but is also available in intravenous and transdermal forms. Two FDA-approved alpha-2 agonists for hypertension treatment are methyldopa and clonidine and dosages are dependent on the name and route.
Methyldopa is commonly prescribed to patients with hypertension and who are pregnant since it’s safe [20].
Common side effects of alpha-2 receptor agonists are:
- Dry mouth
- Drowsiness
- Fatigue
- Headache
- Sexual dysfunction [3].
Contraindications for use are orthostatic hypotension and autonomic disorders. Healthcare providers must avoid prescribing alpha-2 receptor agonists to individuals taking phosphodiesterase inhibitors [20].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of alpha-2 receptor agonists?
- What are common side effects and contraindications of alpha-2 receptor agonists?
Vasodilators
Vasodilators lower blood pressure by dilating the body’s blood vessels. It binds to the receptors of the blood vessel’s endothelial cells, releasing calcium. Calcium stimulates nitric oxide synthase (NO synthase), eventually converting to L-arginine to nitric oxide. As nitric oxide is available, this allows for GTP to convert to cGMP, and causes dephosphorylation of the myosin and actin filaments. As this occurs, the blood vessels’ smooth muscles relax, leading to vasodilation and lowered blood pressure.
Common vasodilators that act via this pathway are nitrates and minoxidil. Hydralazine is another vasodilator, but the mechanism of action is unknown [10].
Available forms of vasodilators are sublingual, oral, and intravenous. Similar to other classes of antihypertensives, vasodilator dosages depend on the form and treatment setting [10].
Nitrovasodilators like nitroprusside and nitroglycerin are used during hypertensive emergencies. Hydralazine is used for severe hypertension for the prevention of eclampsia or intracranial hemorrhage and minoxidil for resistant hypertension [10] [3].
Side effects for each will vary, but nitrates commonly cause:
- Reflex tachycardia
- Headache
- Orthostatic hypotension
[10]
Common side effects of hydralazine are headaches, heart palpitations, and myalgias. Minoxidil causes excessive hair growth, weight gain, and fluid retention [3]. Additionally, nitroprusside can potentially cause cyanide toxicity.
Vasodilators have varying degrees of contraindications, such as nitrates are avoided in patients with an inferior myocardial infarction. Hydralazine should not be given to patients with coronary artery disease, angina, or rheumatic heart disease. Healthcare providers should be aware of contraindications and monitor patients’ blood pressure and potential side effects [10].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of vasodilators?
- What are the common side effects and contraindications of vasodilators?
Combination Antihypertensives
Many antihypertensive medications come in combined forms, such as ACE inhibitors and thiazide diuretics, beta-blockers and diuretics, or calcium channel blockers and ACE inhibitors. The mechanism of action for combination antihypertensives depends on the blend of medications [3].
Considerations for Prescribers
This section reviews potential considerations when prescribing antihypertensives.
When prescribing antihypertensive medications, there are several factors that healthcare providers must consider. The route is typically determined by the healthcare setting and dosage by the underlying treatment goals. Again, healthcare providers should follow current guidelines when initiating or titrating antihypertensive medications.
Healthcare providers must complete a thorough health history, and review lab values, and contraindications as mentioned above. Monitoring kidney function and electrolyte values is imperative while any patient is taking antihypertensive medications.
While a single antihypertensive medication is recommended for initial treatment, there are some scenarios where combination therapy or combination antihypertensives are recommended [14].
Healthcare providers should also discuss the potential side effects of antihypertensives with patients and what to do if they are experiencing symptoms. For instance, if a patient reports syncope, they should be advised to go to the emergency room or be seen immediately for further evaluation. Also, healthcare providers must encourage patients to monitor their heart rate and blood pressure at home and abide by administration parameters.
For example, instruct patients who are taking beta-blockers to measure their blood pressure and heart rate before taking their medication. If their heart rate is below 60 beats per minute, then they should not take the medication [14].
If a patient is experiencing side effects from an antihypertensive medication, then another alternative should be selected.


Self-Quiz
Ask Yourself...
- What factors should healthcare providers consider when prescribing antihypertensives?
Upcoming Research
This section reviews upcoming research and medications for hypertension treatment.
Research on antihypertensive medications has slowed throughout the years. Some clinical trials were performed on the potential of endothelin receptor antagonists to reduce hypertension. However, some studies found several unwanted side effects, and thus clinical use was stopped for safety reasons.
An endothelin-A and endothelin-B receptor blocker, called aprocinentan, has shown promise for the treatment of resistant hypertension by lowering blood pressure and decreasing vascular resistance.
Research on sodium-glucose transport protein (SGLT2) inhibitors, which are typically used for the treatment of type II diabetes mellitus, is also ongoing. SGLT2 inhibitors may promote blood pressure reduction through diuresis and reduce sympathetic tone [21].

Self-Quiz
Ask Yourself...
- What new research is there about antihypertensives?
Conclusion
If hypertension is left untreated, it can lead to serious health complications, including death. When selecting antihypertensive treatment, healthcare providers should understand the pharmacokinetics of each drug class along with potential side effects and contraindications. They should also follow current clinical guidelines for an evidence-based approach.
Final Reflection Questions
- Which antihypertensive medication is often prescribed during pregnancy?
- Which lab values are important when monitoring patients on each antihypertensive medication?
- Which antihypertensive medications cause hypokalemia?
- Which antihypertensive medications cause hyperkalemia?
Migraine Management

Self Quiz
Ask yourself...
- How might a comprehensive knowledge of migraine medications, including their mechanisms of action, enhance the ability of healthcare professionals to address the specific needs of patients experiencing migraines?
- In what ways can recognizing warnings related to migraine medications contribute to ensuring patient safety?
Definition
Migraines are recurrent, pulsating headaches often accompanied by other symptoms such as nausea, sensitivity to light, and sensitivity to sound. According to recent studies by (17), migraines are recognized as a complex neurological disorder involving abnormal brain activity and a cascade of events leading to pain and associated symptoms.
The impact of migraines extends beyond physical pain, influencing various aspects of life, and recent literature by (14) highlights the profound effect on the quality of life, with disruptions in daily activities, work, and social interactions. For example, a professional experiencing frequent migraines might struggle to meet work deadlines and engage in social events. Recent advancements in diagnostic criteria by (15) emphasize the importance of a precise definition to ensure appropriate treatment strategies. Therefore, understanding the definition is crucial for accurate diagnosis and effective communication between healthcare providers and patients.


Self Quiz
Ask yourself...
- What distinguishes migraines from common headaches, and how does understanding this difference impact the approach to their management?
- In what ways do migraines extend beyond physical pain, and how might this impact influence an individual's overall quality of life?
- How can a precise definition of migraines contribute to accurate diagnosis, and why is accurate diagnosis essential for effective treatment planning?
- How does understanding the definition of migraines facilitate effective communication between healthcare professionals and patients?
Migraine Medications
Understanding the various classes of migraine medications is like having a diverse toolkit to address the complexities of this neurological disorder. By exploring the different classes of medications, healthcare professionals can tailor their approach and make informed decisions based on individual patient profiles and specific migraine characteristics (20).
It is crucial to recognize that migraine medications are not one-size-fits-all. Each patient is unique, and their response to medications may vary. Recent literature by (12) emphasizes the importance of an individualized approach when considering the best medication for each patient. Here’s a list of migraine medications in addition to important details to consider:
Triptans
Triptans are a class of medications specifically designed for the acute treatment of migraines. According to (39), they are not meant for preventive use but are highly effective in providing relief during an ongoing migraine attack. They work by narrowing blood vessels and inhibiting the release of certain chemicals in the brain associated with migraine symptoms (39). Let’s see more details below as described by (7), (39), (29).
Drug Class
Belonging to the serotonin (5-HT) receptor agonists class, Triptans modulate the effects of serotonin receptors in the brain. The various types of Triptans include Sumatriptan, Rizatriptan, Eletriptan, and others. Each Triptan has unique characteristics, such as the onset of action and duration, allowing healthcare professionals to tailor prescriptions based on individual patient needs.
Benefits
Triptans offer several benefits in the management of migraines. One of the primary advantages is their ability to provide rapid and effective relief from migraine symptoms, including headache pain, nausea, and sensitivity to light and sound. The prompt onset of action is particularly valuable for individuals aiming to resume their daily activities quickly. Triptans are available in various formulations, including oral tablets, nasal sprays, and injectables, allowing for flexibility in administration.
Side Effects
While generally well-tolerated, Triptans may cause side effects. Common side effects include mild sensations of warmth or tingling, dizziness, and tightness or pressure in the chest. It is crucial for healthcare professionals to consider the patient's medical history and potential contraindications, such as cardiovascular issues, before prescribing Triptans. In rare cases, more severe side effects like chest pain and changes in heart rate may occur, necessitating immediate medical attention.
Clinical Effects
The clinical effects of Triptans are profound, offering relief to individuals experiencing acute migraine attacks. The primary outcomes include:
- Pain Relief: Triptans are highly effective in reducing the intensity of migraine-associated pain. By targeting the vascular and neuronal components of migraines, these drugs provide rapid relief, allowing patients to resume their normal activities.
- Relief of Associated Symptoms: Beyond pain relief, Triptans address accompanying symptoms such as nausea, photophobia, and phonophobia. This comprehensive effect enhances the overall patient experience during a migraine episode.
- Prevention of Migraine Progression: Triptans, when administered early in the migraine attack, can prevent the progression of the headache phase to more severe stages. This early intervention is crucial for optimizing outcomes and minimizing the impact of migraines on daily life.
- Improvement in Functional Impairment: Migraines often result in functional impairment, limiting individuals' ability to perform daily tasks. Triptans restore functional capacity, allowing patients to regain control over their activities.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDSs)
Nonsteroidal anti-inflammatory drugs, commonly known as NSAIDs, constitute a class of medications used in the treatment of migraines. According to (6), these drugs are characterized by their anti-inflammatory, analgesic, and antipyretic properties. NSAIDs are versatile, as they are not exclusively used for migraines but are also used for various other pain and inflammatory conditions (6). Let’s see more details below as described by (25), (40), (6) and (28).
Drug Class
NSAIDs encompass a broad class of medications, including well-known examples such as ibuprofen, naproxen, and aspirin. They function by inhibiting enzymes called cyclooxygenases (COX), thereby reducing the production of inflammatory prostaglandins. This mechanism provides relief from pain and mitigates inflammation associated with migraines.
Benefits
The primary benefit of NSAIDs in migraine management lies in their ability to alleviate pain and reduce inflammation. They are particularly effective for individuals experiencing mild to moderate migraines. NSAIDs offer a rapid onset of action, making them suitable for individuals seeking prompt relief. Additionally, these medications are available over-the-counter in many formulations, providing accessibility for patients.
Side Effects
While NSAIDs are generally well-tolerated, they may cause side effects, especially with prolonged or excessive use. Common side effects include gastrointestinal issues such as stomach upset or ulcers. Healthcare professionals need to consider a patient's medical history, including conditions like gastric ulcers, before prescribing NSAIDs. In rare cases, more severe side effects like cardiovascular events may occur, emphasizing the importance of cautious use.
Clinical Effects
The clinical effects of NSAIDs in migraine management encompass various aspects. Here’s a list of some of them.
- Pain Relief: NSAIDs are effective in providing pain relief during acute migraine attacks. By reducing prostaglandin levels, they alleviate headache symptoms and contribute to the overall comfort of individuals experiencing migraines.
- Inhibition of Inflammatory Responses: The anti-inflammatory properties of NSAIDs are particularly beneficial when migraines are associated with inflammatory processes. NSAIDs help mitigate inflammation, reducing the severity and duration of migraine attacks.
- Improvement in Associated Symptoms: Beyond pain relief, NSAIDs address associated symptoms such as nausea and photophobia, enhancing the overall patient experience during a migraine episode.
- Prevention of Migraine Progression: When administered early in the migraine attack, NSAIDs can prevent the progression of headaches to more severe stages. This early intervention is critical for optimizing outcomes and minimizing the impact of migraines on daily life.
Calcitonin Gene-Related Peptide (CGRP) Inhibitors
Calcitonin gene-related peptide (CGRP) inhibitors represent a modern class of medications revolutionizing the landscape of migraine management. According to (11), these drugs specifically target CGRP, a neuropeptide involved in dilating blood vessels and transmitting pain signals. By inhibiting CGRP, these inhibitors aim to modulate migraine pathways and reduce the frequency and severity of attacks (11). Let’s see more details below as described by (23) and (11).
Drug Class
CGRP inhibitors belong to a unique drug class designed explicitly for migraine prevention. Examples of CGRP inhibitors include Erenumab, Fremanezumab, and Galcanezumab. These medications are administered via subcutaneous injections, typically monthly or quarterly. The focus on preventive therapy distinguishes CGRP inhibitors from acute treatment options like Triptans.
Benefits
The primary benefit of CGRP inhibitors lies in their efficacy in preventing migraines. Clinical trials have demonstrated a significant reduction in the frequency of monthly migraine attacks among individuals using CGRP inhibitors. This preventive approach is especially valuable for those with frequent and debilitating migraines, offering a chance to enhance their quality of life.
Moreover, CGRP inhibitors are well-tolerated with fewer side effects than other preventive medications. They provide a targeted and specific intervention, addressing the underlying mechanisms of migraines without causing widespread effects on other bodily functions.
Side Effects
While generally well-tolerated, CGRP inhibitors may have some side effects. Local injection site reactions, such as redness or swelling, are common but typically mild. It is crucial for healthcare professionals to monitor and address any adverse effects promptly. Additionally, ongoing research is essential to further understand the long-term safety profile of these medications.
Clinical Effects
The clinical effects of CGRP inhibitors are transformative in the realm of migraine management, offering a novel approach to prevention. Primary clinical effects include the following:
- Reduction in Migraine Frequency: One of the hallmark effects of CGRP inhibitors is a significant reduction in the frequency of migraine attacks. By consistently blocking CGRP receptors, these medications disrupt the migraine cascade, leading to a sustained preventive effect.
- Improvement in Migraine Severity: CGRP inhibitors not only reduce the frequency but also contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall quality of life for individuals suffering from chronic migraines.
- Enhanced Functional Capacity: Migraines often result in functional impairment, limiting individuals' ability to perform daily tasks. CGRP inhibitors restore functional capacity, allowing patients to regain control over their activities and participate more fully in their daily lives.
- Well-Tolerated Profile: CGRP inhibitors are generally well-tolerated, with a favorable side effect profile. This characteristic enhances patient adherence to preventive treatment, a critical factor in long-term migraine management.
Beta-Blockers
Beta-blockers are a class of medications that have found a significant place in migraine management. Initially developed for cardiovascular conditions, beta-blockers have demonstrated efficacy in preventing migraines by reducing the frequency and severity of attacks (32). According to (32), these medications work by blocking the effects of adrenaline, leading to reduced heart rate and blood pressure. Let’s see more details below as described by (32) and (27).
Drug Class
Beta-blockers encompass various medications, with examples such as propranolol, metoprolol, and timolol commonly prescribed for migraine prevention. These drugs fall into the broader category of antihypertensive medications but are repurposed for their preventive benefits in migraine care. Unlike acute treatments, which provide relief during an ongoing attack, beta-blockers are taken regularly to reduce the overall occurrence of migraines.
Benefits
The primary benefit of beta-blockers in migraine management is their preventive action. Clinical studies have shown that beta-blockers can significantly reduce the frequency of migraines, making them particularly suitable for individuals with chronic or frequent attacks. This preventive approach aims to enhance the overall quality of life for those who experience migraines regularly.
Beta-blockers are especially beneficial for individuals with comorbid conditions such as hypertension or heart disease. By addressing both cardiovascular concerns and migraines, these medications offer a comprehensive therapeutic approach.
Side Effects
While generally well-tolerated, beta-blockers may cause side effects that individuals need to be aware of. Common side effects include fatigue, dizziness, and changes in sleep patterns. Healthcare professionals need to monitor patients regularly and adjust the dosage or consider alternative medications if side effects become problematic. Beta-blockers are typically avoided in individuals with certain heart conditions, emphasizing the importance of an individualized approach.
Clinical Effects
The clinical effects of beta-blockers in migraine management encompass various dimensions. See some examples below:
- Reduction in Migraine Frequency: Beta-blockers are known for their ability to reduce the frequency of migraine attacks significantly. This preventive effect is especially valuable for individuals experiencing chronic migraines, enhancing their overall quality of life.
- Alleviation of Migraine Severity: Beyond frequency reduction, beta-blockers contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall comfort of individuals during migraine episodes.
- Improvement in Associated Symptoms: Beta-blockers have been shown to address associated symptoms such as nausea and sensitivity to light. By modulating the autonomic nervous system, these medications offer a holistic approach to migraine management.
- Cardiovascular Benefits: Beta-blockers provide additional benefits for individuals with comorbidities due to their primary use in cardiovascular conditions. This dual action allows for comprehensive management of both migraine and cardiovascular health.
Anticonvulsants
Anticonvulsants, originally developed to control seizures in epilepsy, have emerged as a valuable class of medications in the preventive management of migraines (9). According to (9), these drugs, also known as antiepileptic drugs (AEDs), work by stabilizing electrical activity in the brain and reducing the frequency and severity of migraine attacks. Let’s see more details below as described by (32) and (9).
Drug Class
Anticonvulsants comprise a diverse class of medications, including Topiramate, Valproic acid, and Gabapentin. While their primary use may be in epilepsy, the preventive benefits of certain anticonvulsants extend to migraines. These medications are taken regularly to provide ongoing protection against migraines.
Benefits
The primary benefit of anticonvulsants in migraine management is their preventive action. Clinical trials have demonstrated the efficacy of certain anticonvulsants, such as topiramate, in significantly reducing the frequency of migraines. This preventative approach is particularly suitable for individuals with chronic or frequent attacks, aiming to improve overall quality of life.
Anticonvulsants are especially valuable for individuals who may not find relief or experience intolerable side effects with other preventive medications. The versatility of this drug class allows healthcare professionals to tailor treatment plans based on individual patient characteristics and responses.
Side Effects
While generally well-tolerated, anticonvulsants may cause side effects that individuals need to be aware of. Common side effects include drowsiness, dizziness, and gastrointestinal disturbances. It is crucial for healthcare professionals to monitor patients regularly and adjust the dosage or consider alternative medications if side effects become problematic. Additionally, certain anticonvulsants may have specific considerations, such as the need to regularly monitor liver function in individuals taking Valproic acid.
Clinical Effects
The clinical effects of anticonvulsants in migraine management encompass the following dimensions:
- Reduction in Migraine Frequency: Anticonvulsants are known for their ability to significantly reduce the frequency of migraine attacks. This preventive effect is particularly valuable for individuals experiencing chronic migraines, substantially improving their overall quality of life.
- Alleviation of Migraine Severity: Beyond frequency reduction, anticonvulsants contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall comfort of individuals during migraine episodes.
- Improvement in Associated Symptoms: By modulating neurotransmission and neuronal excitability, Anticonvulsants address associated symptoms such as nausea and sensitivity to light. This holistic approach contributes to a more comprehensive management of migraines.
- Beneficial in Comorbid Conditions: Anticonvulsants, due to their broader neurological effects, can be helpful for individuals with comorbid conditions such as epilepsy or mood disorders. This dual benefit allows for comprehensive management and improves overall well-being.

Self Quiz
Ask yourself...
- How do Triptans contribute to migraine management, and in what scenarios might healthcare professionals prioritize their use during acute migraine attacks?
- Can you differentiate the mechanisms of action between NSAIDs and Triptans in migraine management, and how might this understanding influence the choice of medication for a specific patient?
- What roles do CGRP inhibitors play in migraine pharmacotherapy?
- Consider a scenario where a patient experiences migraines with comorbid cardiovascular issues. How might the choice of medication be influenced by the need to prioritize both migraine relief and cardiovascular safety?
Clinical Criteria for Prescribing
In migraine management, prescribing medications involves a comprehensive understanding of clinical criteria to tailor interventions effectively. This section explores the clinical factors guiding the prescription of migraine medications and the decision-making process for healthcare providers. Here are some of the factors.
Frequency and Severity of Migraine Attacks
An essential consideration in prescribing migraine medications is the frequency and severity of migraine attacks experienced by the patient. For instance, a patient suffering from frequent and severe attacks may benefit from preventive medications to reduce the overall frequency and intensity of migraines (31).
Individual Response to Pain and Associated Symptoms
The subjective experience of pain and associated symptoms during migraines varies among individuals. A patient who experiences intense nausea and vomiting may require medications with rapid onset and alternative formulations, such as nasal sprays or injectables, to address these specific symptoms effectively (8).
Impact on Daily Functioning and Quality of Life
Prescribing migraine medications involves considering the impact of migraines on a patient's daily functioning and overall quality of life (24). For example, a working professional with migraines that significantly impede productivity may require acute medications with fast-acting formulations for quick relief during work hours.
Comorbid Conditions and Patient Preferences
Comorbid conditions and patient preferences are pivotal factors in prescribing migraine medications. A patient with comorbid cardiovascular issues may require careful consideration of medication options to mitigate potential risks (2).

Self Quiz
Ask yourself...
- How does a patient's medical history, especially factors like cardiovascular health, influence the clinical criteria for prescribing migraine medications?
- Why is it essential for healthcare professionals to assess the frequency and severity of migraine attacks when determining the clinical criteria for prescribing medications?
- How do patient preferences contribute to the clinical criteria for prescribing migraine medications?
Pharmacokinetics
Understanding the pharmacokinetics of migraine management medications enables healthcare professionals to tailor treatment plans based on individual patient characteristics, ensuring maximum therapeutic benefit. Let’s get into more details for each of the medications listed above:
Triptans
Absorption
Triptans exhibit distinct pharmacokinetic properties that influence their efficacy and onset of action. Following oral administration, Triptans are absorbed through the gastrointestinal tract and the rate of absorption varies among different Triptans, contributing to differences in their clinical profiles. (39)
Distribution
Upon absorption, Triptans undergo distribution to reach target sites in the body, primarily the central nervous system. Their lipophilic nature allows them to penetrate the blood-brain barrier, enabling interaction with serotonin receptors implicated in migraine pathophysiology. The distribution of Triptans influences their ability to exert effects centrally and peripherally. (39)
Metabolism
Metabolism is a crucial aspect of triptan pharmacokinetics, occurring predominantly in the liver. The enzyme responsible for triptan metabolism is monoamine oxidase-A (MAO-A). (39)
Excretion
The final phase in the pharmacokinetic journey of Triptans is excretion, primarily through renal and biliary routes. Renal excretion eliminates the unchanged drug and its metabolites, while biliary excretion expels metabolites via the bile into the gastrointestinal tract. The interplay between metabolism and excretion contributes to the overall pharmacokinetic profile of Triptans. Variations in renal function may influence the elimination of the half-life of certain Triptans, impacting the duration of their therapeutic effect. (39)
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Absorption
Following oral administration, NSAIDs are absorbed in the gastrointestinal tract, with the rate and extent varying among different agents. For instance, ibuprofen exhibits rapid absorption, making it suitable for prompt relief during acute migraine attacks. On the other hand, naproxen has a longer duration of action due to slower absorption, making it well-suited for sustained pain relief. (28)
Distribution
Upon absorption, NSAIDs embark on a journey of distribution throughout the body. Their lipophilic nature allows for penetration into various tissues, including inflamed areas. The distribution influences the drug's ability to reach target sites, such as the central nervous system, where NSAIDs exert their analgesic and anti-inflammatory effects. This property is particularly relevant in the context of migraines, where the inflammatory component contributes to pain. (28)
Metabolism
Metabolism plays a role in shaping the pharmacokinetic profile of NSAIDs, occurring primarily in the liver. Enzymes such as cytochrome P450 contribute to the biotransformation of NSAIDs into metabolites. The metabolism of NSAIDs can vary among individuals, impacting factors such as drug efficacy and potential side effects. For example, the metabolism of certain NSAIDs, like diclofenac, can be influenced by genetic polymorphisms, contributing to interindividual variability in drug response. (21)
Excretion
The final phase of the NSAID journey involves excretion, predominantly through the kidneys. Unchanged NSAIDs and their metabolites are eliminated via urine. Considerations of renal function are crucial in the context of NSAID use, as impaired kidney function can lead to prolonged drug half-life and increased risk of adverse effects. Regular monitoring of renal function is essential, especially in individuals with conditions that may affect kidney health. (21)
Calcitonin Gene-Related Peptide (CGRP)
Absorption
Administered via subcutaneous injections, CGRP inhibitors such as Erenumab and Fremanezumab enter the bloodstream directly, allowing for precise control over drug levels. This mode of administration ensures a reliable and consistent absorption rate, contributing to the predictability of therapeutic outcomes. (11)
Distribution
Following absorption, CGRP inhibitors are distributed throughout the body, focusing on target sites implicated in migraine pathophysiology, like the central nervous system. (11)
Metabolism
Unlike many traditional medications, CGRP inhibitors follow a different path in terms of metabolism. Due to their biotechnological origin as monoclonal antibodies, these drugs do not undergo significant hepatic metabolism. Instead, proteolytic enzymes break them down into smaller peptides and amino acids, which occur systemically. This unique metabolic pathway aligns with the specificity of CGRP inhibitors, minimizing interactions with hepatic enzymes and potential drug-drug interactions. (37)
Excretion
The final phase of the CGRP inhibitor journey involves excretion, primarily through the kidneys via renal clearance. This aspect is particularly relevant when considering individual patient factors such as renal function, as impaired kidney function can affect the clearance of CGRP inhibitors and influence their duration of action. (37)
Beta-Blockers
Absorption
Administered orally, beta-blockers like propranolol and metoprolol are absorbed through the gastrointestinal tract. Depending on the condition of the gastrointestinal tract, the rate and extent of absorption can vary, impacting the time it takes for these medications to reach therapeutic levels in the bloodstream. (27)
Distribution
Once absorbed, beta-blockers embark on distribution throughout the body. Their lipophilic nature enables penetration through cell membranes, allowing them to reach target tissues, including the heart and blood vessels. In the context of migraine management, the distribution properties of beta-blockers are crucial for their ability to modulate the autonomic nervous system centrally and peripherally, leading to the desired preventive effects against migraines. (27)
Metabolism
The metabolism of beta-blockers occurs primarily in the liver, where enzymes play a role in their biotransformation. Genetic polymorphisms in these enzymes can contribute to interindividual variability in drug metabolism. (27)
Excretion
The final phase of the beta-blocker journey involves excretion, predominantly through the kidneys, where unchanged beta-blockers and their metabolites are eliminated via urine. The renal excretion of these drugs is relevant when considering individual patient factors, such as renal function, as impaired kidney function can affect the clearance of beta-blockers and influence their duration of action. (27)
Anticonvulsants
Absorption
Typically administered orally, anticonvulsants like topiramate and valproic acid are absorbed through the gastrointestinal tract. The rate and extent of absorption play a crucial role in determining the onset of action and overall effectiveness. (9)
Distribution
Following absorption, anticonvulsants undergo distribution throughout the body. Their lipophilic nature allows them to penetrate the blood-brain barrier, reaching target sites in the central nervous system relevant to migraine pathophysiology. The distribution properties of anticonvulsants contribute to their ability to modulate neuronal excitability centrally and exert preventive effects against migraines. (9)
Metabolism
Metabolism is a crucial aspect of anticonvulsant pharmacokinetics. This occurs predominantly in the liver and enzymes play an important role in the biotransformation of anticonvulsants into metabolites. The metabolism of anticonvulsants can vary among individuals, impacting factors such as drug efficacy and potential side effects. For example, valproic acid undergoes extensive hepatic metabolism, and variations in enzyme activity can lead to interindividual variability in drug response. (30)
Excretion
The final phase in the anticonvulsant journey involves excretion, primarily through the kidneys. Unchanged anticonvulsants and their metabolites are eliminated via urine. This renal excretion is relevant when considering individual patient factors such as renal function, as impaired kidney function can affect the clearance of anticonvulsants and influence their duration of action. (30)

Self Quiz
Ask yourself...
- How do the pharmacokinetics of Triptans, specifically their absorption and distribution, contribute to their efficacy in managing acute migraine attacks?
- Can you explain the key pharmacokinetic parameters of nonsteroidal anti-inflammatory drugs (NSAIDs) used in migraine management and how they influence drug effectiveness?
- What role do pharmacokinetic factors play in the onset and duration of action of calcitonin gene-related peptide (CGRP) inhibitors?
- In the context of migraine medications, how does the pharmacokinetics of beta-blockers influence their absorption, distribution, metabolism, and excretion in the body?
Warnings Related to Migraine Medications
Understanding potential warnings related to migraine medications is essential for healthcare professionals to ensure safe and effective treatment. Here are some factors to consider.
Medication Safety
Migraine medications, whether preventive or acute, come with specific warnings that need careful attention. For instance, some medications may have contraindications for individuals with certain medical conditions or those taking specific medications concurrently. According to (34), healthcare providers must be vigilant in assessing patient medical histories to identify potential contraindications.
Addressing Cardiovascular Risks
Certain migraine medications, such as Triptans, may pose cardiovascular risks, especially in individuals with pre-existing cardiovascular conditions (35). Therefore, it is crucial for healthcare providers to assess patients' cardiovascular health and consider alternative medications or dose adjustments for those at higher risk. For example, a patient with a history of myocardial infarction may be advised to avoid Triptans, and a different class of medication, like NSAIDs, may be recommended.
Pregnancy and Lactation Considerations
Warnings related to pregnancy and lactation are paramount. Some migraine medications may have potential risks during pregnancy, and healthcare providers must carefully weigh the benefits and risks when prescribing for pregnant or lactating individuals. For instance, valproic acid is associated with an increased risk of congenital disabilities, and alternative medications with a safer profile may be preferred for pregnant individuals seeking migraine relief (1).
Managing Medication Overuse Headaches (MOH)
A significant warning associated with migraine medications is the risk of medication overuse headaches (34). To prevent this problem, healthcare providers need to educate patients about the importance of adhering to prescribed dosages and avoiding excessive use of acute medications. Offering alternative strategies, such as lifestyle modifications and preventive medications, can be crucial in managing and preventing MOH.


Self Quiz
Ask yourself...
- What are some common warnings associated with the use of Triptans in migraine management, and how should healthcare providers address these warnings?
- Can you identify specific cardiovascular risks associated with certain migraine medications, and what should be considered when prescribing these medications to patients with pre-existing cardiovascular conditions?
- What warnings are typically associated with the use of valproic acid in migraine management, particularly concerning specific patient populations such as pregnant individuals?
- How do healthcare providers manage and educate patients about the risk of medication overuse headaches associated with certain migraine medications, and what preventive measures can be implemented to minimize this risk?
Alternatives to Migraine Medications
According to (5), integrating alternative methods provides additional tools for healthcare professionals and empowers individuals seeking a more comprehensive and personalized approach to migraine care. Here are some alternative approaches:
Holistic Lifestyle Modifications
Holistic management of migraines involves lifestyle modifications that can significantly impact the frequency and severity of attacks. For instance, incorporating regular physical activity, maintaining a consistent sleep schedule, and managing stress through practices like mindfulness and yoga have shown promise in reducing migraine occurrence (5). Educating patients about these lifestyle changes empowers them to actively participate in their migraine management.
Biofeedback and Relaxation Techniques
Biofeedback and relaxation techniques offer non-pharmacological interventions that enhance self-awareness and control over physiological responses (22). These approaches teach individuals to recognize and manage stress triggers, ultimately reducing the frequency of migraines. For example, biofeedback training that monitors muscle tension and provides real-time feedback can effectively prevent migraines (22).
Acupuncture and Acupressure
According to (22), traditional Chinese medicine practices like acupuncture and acupressure have gained recognition for their potential in migraine management. Acupuncture involves the insertion of thin needles into specific points on the body, while acupressure applies pressure to these points. Research suggests that these methods reduce the frequency and intensity of migraines, providing an alternative avenue for individuals seeking non-pharmacological options (22).
Nutritional Approaches
Dietary modifications and nutritional approaches also play a role in holistic migraine management. For example, identifying and avoiding potential trigger foods, such as those containing tyramine or artificial additives, can be beneficial (10). Additionally, ensuring adequate hydration and incorporating anti-inflammatory foods into the diet may contribute to overall well-being and migraine prevention (10).

Self Quiz
Ask yourself...
- What benefits do biofeedback and relaxation techniques offer in reducing the frequency and intensity of migraines?
- How can biofeedback and relaxation techniques be integrated into a comprehensive migraine management plan?
- What role do dietary modifications and nutritional approaches play in the holistic management of migraines?
- How can healthcare professionals guide patients in identifying trigger foods and making informed nutritional choices?
Nursing Considerations
Nurses play a pivotal role in the holistic care of individuals with migraines, contributing to both the preventive and acute aspects of management through various considerations. Here are some important considerations.
Assessment and Patient Education
A thorough assessment includes evaluating the frequency, duration, and severity of migraines and identifying triggers and associated symptoms (3). Additionally, nurses play a key role in patient education, ensuring individuals clearly understand their migraine condition, the prescribed medications, and potential side effects. For instance, educating a patient about the importance of early intervention with acute medications during a migraine attack empowers them to take timely action.
Monitoring and Adverse Event Management
Nurses actively monitor individuals undergoing migraine treatment, monitoring the response to medications and any potential adverse events. Regular monitoring includes assessing the effectiveness of preventive measures, tracking the frequency of migraine attacks, and identifying patterns that may require adjustments in the treatment plan (34). If adverse events or side effects occur, nurses are instrumental in managing them promptly, collaborating with healthcare providers to ensure the safety and well-being of individuals.
Supportive Care and Holistic Approach
Nursing considerations extend beyond medication management to supportive care and a holistic approach. Nurses provide emotional support, helping individuals cope with the impact of migraines on their daily lives. Moreover, they collaborate with other healthcare professionals to integrate holistic approaches such as lifestyle modifications, stress management, and alternative therapies into the overall care plan. According to (34), this collaborative and patient-centered approach enhances the effectiveness of migraine management.
Documentation and Communication
Accurate and thorough documentation of relevant patient information, medication administration details, and responses to treatment is a fundamental nursing responsibility in migraine management (34). In addition to that, clear and concise communication between nursing staff, healthcare providers, and other healthcare team members ensures continuity of care (34).

Self Quiz
Ask yourself...
- How can a thorough patient assessment contribute to the safe and effective administration of migraine medications?
- How do nursing responsibilities extend beyond medication administration to encompass patient education?
- When monitoring individuals undergoing migraine treatment, what are the essential aspects that nurses should observe?
- How does the collaborative communication between nursing staff, healthcare providers, and other team members contribute to the continuity of care in migraine management?
Upcoming Research
Staying ahead of the curve is essential for healthcare professionals to provide cutting-edge care and optimize outcomes for individuals with migraines. Upcoming research include the following:
Advancements in Targeted Therapies
Recent research has unveiled promising advancements in targeted therapies for migraine management. For example, research about monoclonal antibodies targeting the calcitonin gene-related peptide (CGRP) pathway is proving to be effective in preventing migraines (12).
Digital Health and Telemedicine in Migraine Care
Integrating digital health technologies and telemedicine is a burgeoning trend in migraine management research. Smartphone applications for tracking migraine patterns, wearable devices for monitoring physiological parameters, and virtual consultations enable a more comprehensive and patient-centric approach (12). This shift toward digital solutions enhances data collection and facilitates remote monitoring and timely interventions, particularly in scenarios where in-person visits may be challenging (12).
Genetic and Personalized Medicine Approaches
Advancements in genetic research are paving the way for personalized medicine in migraine care. Understanding the genetic underpinnings of migraines can guide the development of targeted interventions tailored to an individual's unique genetic profile. This personalized approach could revolutionize treatment strategies, allowing for more precise and effective interventions based on the genetic factors contributing to a person's migraines (13).
Exploration of Lifestyle and Environmental Influences
Upcoming research increasingly focuses on the intricate interplay between lifestyle, environmental factors, and migraines; and studies examining the impact of factors such as diet, sleep patterns, and environmental triggers contribute valuable insights (13). For instance, research may reveal specific dietary components that act as triggers or protective factors for migraines, allowing healthcare professionals to offer targeted lifestyle recommendations.

Self Quiz
Ask yourself...
- What recent research findings have emerged regarding migraine prevention?
- How are digital health technologies and telemedicine being incorporated into upcoming research on migraine management?
- In personalized medicine, how is genetic research influencing upcoming approaches to migraine care?
- How can consideration of lifestyle factors and environmental influences contribute to a more holistic approach of migraine management?
Conclusion
In conclusion, this course focused on empowering learners not only with knowledge about migraine management, but with the practical insights and skills crucial for excellence in migraine care. The journey doesn’t end here; it extends into the realm of compassionate practice, where the combination of scientific understanding and safety measures transforms care providers into formidable advocates for those navigating the complexities of migraines.
Asthma Treatment and Monitoring
Introduction
When hearing the phrase asthma, what comes to mind? If you're an advanced practice registered nurse (APRN) with prescriptive authority, you've definitely heard of asthma before. Even as a nurse or maybe before nursing school, conversations about prescription drug use and respiratory health existed every so often.
Presently, patients seek guidance and information on various health topics from APRNs, including medication management and respiratory health. The information in this course will serve as a valuable resource for APRNs with prescriptive authority of all specialties, education levels, and backgrounds, to learn more about medications that can treat and manage asthma.
Defining Asthma
What Is Asthma?
Asthma is a non-communicable chronic health condition that affects the airways of the lungs and affects millions of people nationwide. Asthma is often diagnosed in childhood and can resolve in adulthood or continue for the rest of a patient's life. Several studies postulate the cause of asthma, but there is no definitive cause.
Genetics, age, environmental exposures, smoking, and a history of allergies are thought to play a role in asthma severity and development. Clinical presentation of asthma often includes trouble breathing, chronic airway inflammation, and airway hyperresponsiveness. Assessment for asthma often includes patient history, clinical presentation, spirometry testing, and pulmonary function tests (PFTs).
What Are the Stages of Asthma?
Since asthma is a chronic condition, several established guidelines can be used to determine the severity of asthma and explore possible medication options. Depending on the stage of asthma and patient response to existing therapy, treatment and management vary.
The four stages of asthma include intermittent, mild, moderate, and severe. Based on the 2020 National Asthma Education and Prevention Program (NAEPP) guidelines, here is the standard criteria for what constitutes each stage of asthma (2).
Intermittent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness <2 times a week
- Asthmatic flare-ups are short-lived with varying intensity
- Symptoms at night are <2 a month
- No asthmatic symptoms between flare-ups
- Lung function test FEV 1 at >80% above normal values
- Peak flow has <20% variability am-to-am or am-to-pm, day-to-day
Mild persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness 3-6 times a week
- Asthmatic flare-ups may affect activity level and can vary in intensity
- Symptoms at night are 3-4 times a month
- Lung function test FEV1 is >80% above normal values
- Peak flow has less than 20-30% variability
Moderate persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness daily
- Asthmatic flare-ups may affect activity level and can vary in intensity
- Symptoms at night are >5 times a month
- Lung function test FEV1 is 60%-80% of normal values
- Peak flow has more than 30% variability
Severe persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness continuously
- Asthmatic flare-ups affect activity level and often vary in intensity
- Asthmatic symptoms at night are constant
- Lung function test FEV1 is <60% of normal values
- Peak flow has more than 30% variability
Based on patient history, clinical presentation, and these criteria, treatment can be administered to decrease the symptoms of the patient. If a patient presents with symptoms that are outside of your scope of work or understanding, you can always refer patients to a pulmonologist or asthma specialist.
Often times, more severe cases of asthma and asthma emergencies require increased frequency and dosing of asthma-related medications. Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history, pulmonary function, and health history prior to prescribing asthma medications (1).
What Are Asthmatic Emergencies?
Asthmatic emergencies are if a patient has asthma symptoms that are beyond what they typically experience and are unable to function without immediate medical intervention. Asthma emergencies can occur as a result of a patient being unable to access their asthmatic medications, being exposed to a possible allergen, or being under increased stress on the body.
Asthmatic emergencies often require collaborative medical intervention, increased dosages of medications discussed below, and patient education to prevent future asthmatic emergencies (1).
What If Asthma Is Left Untreated?
Depending on the clinical presentation and severity of asthma, asthma can cause several long-term complications if left untreated. If asthma is not properly managed, several complications, such as chronic obstructive pulmonary disease (COPD), decreased lung function, permanent changes to the lungs' airways, and death can occur (1, 2).
Defining Asthma Medications
What Are Commonly Used Medications to Manage Asthma?
Commonly used medications to manage asthma include inhaled corticosteroids, oral corticosteroids, short-acting beta agonists (SABAs), long-acting beta agonists (LABAs), long-acting muscarinic antagonists (LABAs), adenosine receptor antagonists, leukotriene modifiers, mast cell stabilizers, and monoclonal antibodies. The dosage, frequency, amount of asthma management medications, and medication administration route can all vary depending on clinical presentation, patient health history, and more.
How and Where are Asthma Medications Used?
Asthma medications can be used routinely or as needed for management of asthma symptoms depending on the patient. Asthma medications can be used at home, in public, and in health care facilities. Depending on the specific asthma medication and dosage, these medications can be taken by mouth, by an external device, such as an inhaler, via subcutaneous injection, or via intravenous solution (1).
What Are the Clinical Criteria for Prescribing Asthma Medication?
Clinical criteria for prescribing asthma medication can depend on the clinical presentation of a patient. Assessment of lung health and patient history are essential to determining the dosage and medications needed for adequate asthmatic symptom control.
Clinical guidelines from reputable organizations, such as the National Asthma Education and Prevention Program (NAEPP), the National Institutes of Health (NIH), the Global Initiative for Asthma (GINA), and the American Academy of Family Physicians (AAFP) can provide insight into the latest recommendations for asthma management (1, 2). In addition, local laws or health departments might have recommendations for asthma medication guidelines.
What Is the Average Cost for Asthma Medications?
Cost for asthma medications can significantly vary depending on the type of medication, insurance, dosage, frequency, medication administration route, and other factors. Cost is among a leading reason why many patients cannot maintain their medication regime (3). If cost is a concern for your patient, consider reaching out to your local pharmacies or patient care teams to find cost effective solutions for your patients.


Self Quiz
Ask yourself...
- What are some common signs of asthma?
- What are some common medications that can be prescribed to manage asthma?
- What are some factors that can influence asthma development and severity?
Inhaled Corticosteroids Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Inhaled Corticosteroids
Commercially available inhaled corticosteroids include: ciclesonide (Alvesco HFA), fluticasone propionate (Flovent Diskus, Flovent HFA, Armon Digihaler), budesonide (Pulmicort Flexhaler), beclomethasone dipropionate (QVAR RediHaler), fluticasone furoate (Arnuity Ellipta), and mometasone furoate (Asmanex HFA, Asmanex Twisthaler).
Clinical criteria for prescribing an inhaled corticosteroid includes adherence to the latest clinical guidelines, patient medical history, patient clinical presentation, and drug availability (4).
Inhaled Corticosteroids Method of Action
Inhaled corticosteroids have an intricate mechanism of action involving several responses to the immune system. Inhaled corticosteroids decrease the existing initial inflammatory response by decreasing the creation and slowing the release of inflammatory mediators. Common inflammatory mediators include histamine, cytokines, eicosanoids, and leukotrienes. Inhaled corticosteroids can also induce vasoconstrictive mechanisms, which, as a result, can lead to less blood flow, resulting in less discomfort and edema (4).
In addition to anti-inflammatory properties, inhaled corticosteroids can create a localized immunosuppressive state that limits the airways' hypersensitivity reaction, which is thought to reduce bronchospasms and other asthma-associated symptoms. It is important to note that inhaled corticosteroids often do not produce therapeutic effects immediately, as many patients may not see a change in their asthma symptoms for at least a week after beginning inhaled corticosteroid therapy (4).
Inhaled Corticosteroids Side Effects
Every medication has the possibility of side effects, and inhaled corticosteroids are no exception. Common side effects of inhaled corticosteroids include oral candidiasis (thrush), throat irritation, headache, and cough.
Patient education about rinsing their mouth and oral hygiene after use is essential to avoid the possibility of thrush and other oral infections and irritations. More severe side effects can include prolonged immunosuppression, reduction in bone density, and adrenal dysfunction (4).
Inhaled Corticosteroids Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with inhaled corticosteroids, so additional medication, increased dosage, a change in frequency, or a new medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of inhaled corticosteroids?
- What are some patient considerations to keep in mind when prescribing inhaled corticosteroids?
Oral Corticosteroids Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Oral Corticosteroids
Commercially available oral corticosteroids include methylprednisolone, prednisolone, and prednisone. Clinical criteria for prescribing an oral corticosteroid includes adherence to the latest clinical guidelines, patient medical history, patient clinical presentation, and drug availability (4).
Oral Corticosteroids Method of Action
Methylprednisolone and prednisolone have a method of action as intermediate, long-lasting, synthetic glucocorticoids, have COX-2 inhibitory properties, and inhibit the creation of inflammatory cytokines (5).
Prednisone is a prodrug to prednisolone and has anti-inflammatory and immunomodulating glucocorticoid properties. Prednisone has a method of decreasing inflammation by reversing increased capillary permeability and suppressing the movement of certain leukocytes (6).
Oral Corticosteroids Side Effects
Every medication has the possibility of side effects, and oral corticosteroids are no exception. Methylprednisolone and prednisolone have possible side effects of skin changes, weight gain, increased intraocular pressure, neuropsychiatric events, neutrophilia, immunocompromised state, fluid retention, and GI upset.
Consider monitoring symptoms and overall health of patients on systemic corticosteroids to assess for long-term side effects (5). Prednisone has possible side effects of changes in blood glucose, changes in sleep habits, changes in appetite, increased bone loss, an immunocompromised state, changes in adrenal function, and changes in blood pressure (6).
Oral Corticosteroids Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with oral corticosteroids, so additional medication, increased dosage, a change in frequency, or a new medication class might need to be considered (6).

Self Quiz
Ask yourself...
- What are some possible side effects of oral corticosteroids?
- What are some patient considerations to keep in mind when prescribing oral corticosteroids versus inhaled corticosteroids?
Short-Acting Beta Agonists (SABAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – SABAs
Common commercially available SABAs include albuterol sulfate (ProAir HFA, Proventil HFA, Ventolin HFA), albuterol sulfate inhalation powder (ProAir RespiClick, ProAir Digihaler), levalbuterol tartrate (Xopenex HFA), and levalbuterol hydrochloride (Xopenex) (4).
SABAs Method of Action
Short-acting beta-agonists (SABAs) have a rapid onset as broncho-dilating medications. SABAs, especially albuterol in emergent situations, are used often to quickly relax bronchial smooth muscle from the trachea to the bronchioles through action on the β2-receptors.
While SABAs are effective bronchodilators in the short term for asthma symptoms, SABAs do not affect the underlying mechanism of inflammation. As a result, SABAs are often used for short-acting intervals, such as few hours, and have limited capabilities to prevent asthma exacerbations alone (4). SABAs can be administered via meter-dosed inhalers, intravenous, dry powder inhalers, orally, subcutaneously, or via nebulizer.
SABAs Side Effects
Every medication has the possibility of side effects, and SABAs are no exception. Because of the beta receptor agonisms, possible SABA side effects include increased heart rate, chest pain, chest palpitations, body tremors, and nervousness (4). Because of the short half-life of SABAs, chronic side effects are not typically observed.
SABAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with SABAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of short-acting beta agonists?
- What are some patient considerations to keep in mind when prescribing SABAs?
Long-Acting Beta Agonists (LABAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – LABAs
Common commercially available LABAs are salmeterol and formoterol (7).
LABAs Method of Action
Long-acting beta-agonists (LABAs) have a rapid onset like SABAs, but also have a longer half-life. LABAs are used often as asthma maintenance medications to relax bronchial smooth muscle from the trachea to the bronchioles through action on the β2-receptors. While SABAs are effective bronchodilators in the short term for asthma symptoms, LABAs are effective bronchodilators in the long term for asthma symptoms.
Like SABAs, LABAs do not affect the underlying mechanism of inflammation. LABAs can be administered via meter-dosed inhalers, intravenous, dry powder inhalers, orally, subcutaneously, or via nebulizer. LABAs are often effective for 12-hour durations (7).
LABAs Side Effects
Every medication has the possibility of side effects, and LABAs are no exception. Like SABAs, because of the beta receptor agonisms, possible LABA side effects include increased heart rate, chest pain, chest palpitations, body tremors, and nervousness (7). Other more prolonged side effects can include changes in blood glucose levels and changes in potassium levels with prolonged LABA use (7).
LABAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with LABAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).
In addition, there are combination inhaled corticosteroid/LABA medications that can be considered, such as fluticasone propionate and salmeterol (Advair Diskus, Advair HFA, AirDuo Digihaler, AirDuo RespiClick, Wixela Inhub), fluticasone furoate and vilanterol (Breo Ellipta), mometasone furoate and formoterol fumarate dihydrate (Dulera), and budesonide and formoterol fumarate dihydrate (Symbicort) (4).

Self Quiz
Ask yourself...
- What are some possible side effects of LABAs?
- What are some patient considerations to keep in mind when prescribing SABAs compared to LABAs?
Long-Acting Muscarinic Antagonists (LAMAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – LAMAs
Common commercially available LAMAs include two inhalation powders via inhalers known as tiotropium bromide (Spiriva Respimat) and fluticasone furoate, umeclidinium, and vilanterol (Trelegy Ellipta) (4).
LAMAs Method of Action
Both drugs mentioned above are long-acting muscarinic antagonists (LAMAs). LAMAs work to alleviate asthmatic symptoms by antagonizing the type 3 muscarinic receptors in bronchial smooth muscles, resulting in relaxation of muscles in the airway (4). Because LAMAs are long-acting, they are not recommended for cases of acute asthma exacerbations or asthmatic emergencies (4).
LAMAs Side Effects
Possible LAMA side effects include urinary retention, dry mouth, constipation, and glaucoma (4).
LAMAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with LAMAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of LAMAs?
- What are some patient considerations to keep in mind when prescribing LAMAs?
Adenosine Receptor Antagonists Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Adenosine Receptor Antagonists
The commercially available adenosine receptor antagonist for asthma management is theophylline as a pill or intravenous (8).
Adenosine Receptor Antagonists Method of Action
The method of action for theophylline is acting as a nonselective adenosine receptor antagonist, acting as a competitive, nonselective phosphodiesterase inhibitor, and reducing airway responsiveness to histamine, allergens, and methacholine (8).
Adenosine Receptor Antagonists Side Effects
Common side effects of theophylline include GI upset, headache, dizziness, irritability, and arrythmias (8).
Adenosine Receptor Antagonists Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with theophylline, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of adenosine receptor antagonists?
- What are some patient considerations to keep in mind when prescribing adenosine receptor antagonists?

Leukotriene Modifiers Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Leukotriene Modifiers
Commercially available leukotriene modifiers include montelukast (Singular) and zafirlukast (Accolate) as oral pills taken once a day. Zileuton (Zyflo CR) is a 5-lipoxygenase inhibitor that also modifies leukotriene activity (4).
Leukotriene Modifiers Method of Action
Montelukast and zafirlukast work to control asthma-related symptoms by targeting leukotrienes, which are eicosanoid inflammatory markers. Montelukast works in particular by blocking leukotriene D4 receptors in the lungs, thus allowing decreased inflammation in the lungs and increased relaxation of lung smooth muscle (9).
Zafirlukast works by being a competitive antagonist at the cysteinyl leukotriene-1 receptor (CYSLTR1) (10). Zileuton is a 5-lipoxygenase inhibitor, in which 5-lipoxygenase is needed for leukotriene creation. Blocking 5-lipoxygenase decreases the formation of leukotrienes at several receptors. As a result of decreased leukotriene production, there is decreased inflammation, decreased mucus secretion, decreased bronchoconstriction (11).
Leukotriene Modifiers Side Effects
Possible side effects of montelukast include headaches, GI upset, and upset. Neuropsychiatric events, such as nightmares, changes in sleep, depression, and suicidal ideation are more severe side effects associated with montelukast.
Possible side effects of zafirlukast include headache, GI upset, and hepatic dysfunction (9).
Possible side effects of zileuton include hepatic dysfunction, changes in sleep, changes in mood, headaches, and GI upset. When the leukotriene modifiers, neuropsychiatric side effects are to be monitored for in particular, especially for suicidal ideation (9,10,11).
Leukotriene Modifiers Alternatives
Some patients might not report their symptoms alleviating with leukotriene modifiers, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of leukotriene modifiers?
- What are some patient considerations to keep in mind when prescribing leukotriene modifiers?
Mast Cell Stabilizer Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Mast Cell Stabilizer
A commercially available mast cell stabilizer is cromolyn available via metered-dose inhaler and nebulizer solution (12).
Mast Cell Stabilizer Method of Action
Cromolyn has a method of action in which it inhibits the release of inflammatory mediators from cells, such as the release of histamine and leukotrienes (12).
Mast Cell Stabilizer Side Effects
Every medication has the possibility of side effects, and cromolyn is no exception. Common side effects of cromolyn include dry throat, throat irritation, drowsiness, dizziness, cough, headache, and GI upset (12).
Mast Cell Stabilizer Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with mast cell stabilizers, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of mast cell stabilizers?
- What are some patient considerations to keep in mind when prescribing mast cell stabilizers?
Monoclonal Antibody Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Monoclonal Antibody
Commercially available monoclonal antibodies include Omalizumab (Xolair), mepolizumab (Nucala), reslizumab (Cinqair), benralizumab (Fasenra), dupilumab (Dupixent), and tezepelumab-ekko (Tezspire). Omalizumab, mepolizumab, benralizumab, dupilumab, and texepelumab-ekko are available via subcutaneous injection. Reslizumab is available via intravenous solution (4).
Monoclonal Antibody Method of Action
Omalizumab is an anti-IgE monoclonal antibody that works by inhibiting the binding of IgE to mast cells and basophils. As a result of decreased bound IgE, activation and release of mediators, such as histamine, in the allergic response are decreased (13).
Mepolizumab, reslizumab, and benralizumab are interleukin (IL)-5 antagonists. These IL-5 antagonists inhibit IL-5 signaling, allowing for a decrease in the creation and survival of eosinophils. However, the full method of action for IL-5 antagonists is still unknown, as more evidence-based research is needed (4, 15).
Dupilumab is an IgG4 antibody that inhibits IL-4 and IL-13 signaling by binding to the IL-4Rα subunit. This inhibition of the IL-4Rα subunit allows for the decrease of IL-4 and IL-13 cytokine-induced inflammatory responses (14).
Tezepelumab-ekko is an IgG antibody that binds to the thymic stromal lymphopoietin (TSLP) and prevents TSLP from interacting with the TSLP receptor. Blocking TSLP decreases biomarkers and cytokines associated with inflammation. Knowing this, the full method of action for Tezepelumab-ekko is still unknown, as more evidence-based research is needed4,15.
Monoclonal Antibody Side Effects
Possible side effects of omalizumab include injection site reactions, fracture, anaphylaxis, headache, and sore throat (13). Possible side effects of mepolizumab, reslizumab, and benralizumab include injection site reactions, headache, and hypersensitivity reactions (4). Possible side effects of dupilumab include joint aches, injection site reactions, and headache (14). Possible side effects of tezepelumab-ekko include injection site reactions and headache (14).
Monoclonal Antibody Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with monoclonal antibodies, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of monoclonal antibodies?
- What are some patient considerations to keep in mind when prescribing monoclonal antibodies?
Nursing Considerations
Nurses remain the most trusted profession for a reason, and APRNs are often pillars of patient care in several health care settings. Patients turn to nurses for guidance, education, and support. While there is no specific guideline for the nurses' role in asthma education and management, here are some suggestions to provide quality care for patients currently taking medications to manage asthma or concerned about possibly having asthma.
- Take a detailed health history. Often times, respiratory symptoms, such as a cough or trouble breathing, are often dismissed in health care settings, or seen as "common symptoms with everyone." If a patient is complaining of symptoms that could be related to asthma, inquire more about that complaint.
Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient's complaint is not being taken seriously by other health care professionals, advocate for that patient to the best of your abilities.
- Review medication history at every encounter. Often times, in busy clinical settings, reviewing health records can be overwhelming. Millions of people take asthma medications at varying dosages, frequencies, and times of day. Many people with asthma take more than one medication to manage their symptoms.
Ask patients how they are feeling on the medication, if their symptoms are improving, and if there are any changes to medication history.
- Be willing to answer questions about asthma, respiratory health, and medication options. Society stigmatizes open discussions of prescription medication and can minimize symptoms of asthma, such as a chronic cough.
There are many people who do not know about medication options or the long-term effects of undiagnosed or poorly managed asthma. Be willing to be honest with yourself about your comfort level discussing topics and providing education on asthma medications and asthma clinical assessment options.
- Inquire about a patient's life outside of medications, such as their occupation, living situation, and smoking habits. Household exposures, such as carpets or pets, can trigger asthma. Occupations with high exposure to smoke can also trigger asthmatic symptoms. Smoking, living with someone who smokes, or residing in an area with high levels of pollution can also influence asthma symptoms.
Discuss possible solutions to help with symptoms, such as improving ventilation, increasing air quality, and mask wearing when possible.
- Communicate the care plan to other staff involved for continuity of care. For several patients, especially for patients with severe asthma, care often involves a team of nurses, specialists, pharmacies, and more. Ensure that patients' records are up to date for ease in record sharing and continuity of care.
- Stay up to date on continuing education related to asthma medications, as evidence-based information is always evolving and changing. You can then present your new learnings and findings to other health care professionals and educate your patients with the latest information. You can learn more about the latest research on asthma and asthma-related medications by following updates from evidence-based organizations.
How can nurses identify if someone has asthma?
Unfortunately, it is not always possible to look at someone with the naked eye and determine if they have asthma. While some people might have visible asthmatic symptoms, such as wheezing or trouble breathing, asthmatic clinical presentation can significantly vary from person to person.
APRNs can identify and diagnose if someone has asthma by taking a complete health history, listening to patient's concerns, and offering pulmonary function testing.
What should patients know about asthma medications?
Patients should know that anyone has the possibility of experiencing side effects medications for asthma management, just like any other medication. Patients should be aware that if they notice any changes in their mood, experience any sharp headaches, or feel like something is a concern, they should seek medical care.
Nurses should also teach patients to advocate for their own health in order to avoid untreated or undetected asthma and possible chronic complications from asthma or asthma-related medications.
Here are important tips for patient education in the inpatient or outpatient setting:
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors).
- Tell the health care provider of any existing lifestyle concerns, such as tobacco use, other drug use, sleeping habits, occupation, diet, menstrual cycle changes (need to identify lifestyle factors that can influence asthmatic medication use, asthma severity, and asthma management).
- Tell the health care provider if you have any changes in your breathing, such as pain with deep breathing or persistent coughing (potential asthma exacerbation symptoms or possibility of asthma medications not being as effective for treatment).
- Tell the nurse of health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life.
- Keep track of your health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes).
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality is a possible side effect for montelukast use).
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries.
- Tell the health care provider if you notice any changes while taking medications or on other treatments to manage asthma (potential worsening or improving health situation).

Self Quiz
Ask yourself...
- What are some problems that can occur if medications are not asthma properly?
- What are some possible ways you can obtain a detailed, patient centric health history?
- What are some possible ways APRNs can educate patients on asthma and air quality?
Research Findings
What Research on Asthma Medication Exists Presently?
There is extensive publicly available literature on asthma and asthma-related medications via the National Institutes of Health and other evidence-based journals (1,2,4).
What are some ways for people who take asthma medications to become a part of research?
If a patient is interested in participating in clinical trial research, they can seek more information on clinical trials from local universities and health care organizations.

Self Quiz
Ask yourself...
- What are some reasons someone would want to enroll in clinical trials?
Conclusion
Asthma is a chronic condition that affects many people from their childhood to their aging years. As more medications for asthma come onto the market and more evidence-based approaches to asthma and lung care emerge, APRNs will be at the forefront of primary care and asthma care across the lifespan.
Case Study #1
Susie is a mom to a 15-year-old named Jill. She arrives at the pediatric asthma and allergy specialist practice for a new patient visit. Susie reports that she notices Jill is having trouble sleeping at night and coughing more during the day for the past month. Jill plays soccer with her school, but her mom is concerned about coughing and trouble sleeping interfering with her sports.
Susie knows that her dad has asthma, and Jill spends a lot of time with her aunt who smokes cigarettes. Jill has a history of generalized anxiety disorder and reports no smoking, no drinking, and no recreational drugs. Jill also wants to learn more about her lung health, as she wants to play soccer professionally one day.
- What are some specific questions you’d want to ask about Jill’s coughing and respiratory health?
- What are health history questions you would want to highlight?
- What are some tests or lab work would you suggest performing?

Case Study #2 (Continued)
Susie also shares that she is dating a new partner who vapes in the home, and they recently got a pet puppy in the home. She states that Jill had trouble sleeping at night and coughing a lot when she was younger, but Susie thought Jill grew out of it. Susie wants to learn more about if Jill has asthma like her grandfather, if there are any ways to manage this cough, and if there are any tests that can determine Jill’s lung health in the office today.
- What sort of tests can be done in-office to assess pulmonary function?
- What sort of environmental exposures can trigger respiratory conditions?
Susie agrees to have Jill do allergy testing and to do an in-office pulmonary function test for teenagers. Jill also wants to learn more about spirometry that you mentioned earlier and how to monitor her health outside of the office since she’s busy with school and soccer and doesn’t want to come to the office every time there’s a problem.
Susie is open to medication options for Jill but doesn’t want anything that will interfere too much with Jill’s social time with her friends. Susie and Jill also want to know if this is a health condition that Jill will have forever or if Jill will grow out of this.
- Knowing Susie’s concerns and Jill’s age, what are some talking points about reducing possible asthma triggers?
- How would you explain asthma as a chronic health condition to an adolescent patient?
- Given Jill and Susie’s concerns about medications, what would be some possible medication options to consider after reviewing Jill’s pulmonary function test results and patient history?
SSRI Use in Major Depressive Disorder
Introduction
When hearing the phrase selective serotonin reuptake inhibitors, what comes to mind? If you're an advanced practice registered nurse (APRN) with prescriptive authority, you've heard of SSRIs before. Even as a nurse or maybe before nursing school, conversations about prescription drug use and mental health existed every so often.
Presently, patients seek guidance and information on various health topics from APRNs, including medication management, women's health, and mental health. The information in this course will serve as a valuable resource for APRNs with prescriptive authority of all specialties, education levels, and backgrounds to learn more about SSRIs and major depressive disorder (MDD).
Defining SSRIs
What Are SSRIs?
Selective serotonin reuptake inhibitors, known as SSRIs, are a type of pharmacological drug class. SSRIs have existed for the past several decades as a class of prescription medications that can manage major depressive disorder (MDD) and other mental health conditions (1).
While this course focuses explicitly on SSRI use in MDD management, SSRIs are also Food and Drug Administration (FDA) approved to manage obsessive-compulsive disorder (OCD), panic disorder (PD), post-traumatic stress disorder (PTSD), and social anxiety disorder (SAD). In addition, several off-label uses for SSRI include management for binge eating disorder and menopausal vasomotor symptoms.
How and Where Are SSRIs Used?
SSRIs are commonly prescribed to manage MDD and other mood disorders in the U.S. and around the world in pediatric, adult, and geriatric populations (1, 2). SSRIs can be taken by mouth as a pill, capsule, or liquid oral solution. Presently, SSRIs cannot be offered via intravenous, rectal, buccal, or injection routes.
What Is the Clinical Criteria for Prescribing SSRIs?
Clinical criteria for prescribing SSRIs can vary depending on the intention for the SSRI. In the case of MDD, several factors can play a role in the clinical criteria for prescribing SSRIs. A patient's adherence to swallowing a pill daily, dosage given the patient's weight, medical history, and MDD concerns, and prior experience with other medications can influence prescribing SSRIs. When considering prescribing SSRIs for MDD management, consider assessing the patient for MDD first, taking a detailed health history, and discussing the risk versus benefits of starting SSRIs for this patient (1, 3).
What Is the Average Cost for SSRIs?
Cost for SSRIs can significantly vary depending on the type of SSRI, insurance, dosage, frequency, and other factors. Cost is among leading reasons why many patients cannot maintain their medication regime (4). If cost is a concern for your patient, consider reaching out to your local pharmacies or patient care teams to find cost-effective solutions for your patients.
What Is Major Depressive Disorder (MDD)?
Major depressive disorder (MDD) is a mental health condition in which a person has consistent appetite changes, sleep changes, psychomotor changes, decreased interest in activities, negative thoughts, suicidal thoughts, and depressed mood that interfere with a person's quality of life (5). According to the Diagnostic and Statistical Manual of Mental Health Disorders, a patient must have at least five persistent mood related symptoms, including depression or anhedonia (loss of interest in activities once enjoyed), that interferes with a person's quality of life to be formally diagnosed with MDD. Note that MDD does not include a history of manic episodes, and pediatric populations can present with more variable MDD symptoms (5). As an APRN, you can assess for MDD by doing a detailed patient health history or having a patient complete the Patient Health Questionnaire-9 (PHQ-9) - a depression assessment tool (5).


Self Quiz
Ask yourself...
- What are some medication administration options for SSRIs?
- What populations can be prescribed SSRIs?
SSRI Pharmacokinetics
Drug Class SSRIs
Selective serotonin reuptake inhibitors, known as SSRIs, are a type of pharmacological drug class part of the antidepressant drug class. They can be prescribed at various dosages depending on the patient history, severity of major depressive disorder (MDD), other medication use, and other factors based on patient-centered decision making. Currently, SSRIs that are FDA approved for MDD management include paroxetine, sertraline, citalopram, escitalopram, vilazodone, and fluoxetine. SSRIs can be prescribed for the oral route and are available via capsule, tablet, or liquid suspension/solution. SSRIs can be taken at any time of day. They can be taken with or without food, though vilazodone in particular is recommended with food. SSRIs are often prescribed to be taken once a day, sometimes twice a day, depending on the severity of MDD. Health care provider professional discretion and patient condition should guide therapy (1).
SSRIs are metabolized by and known to affect the cytochrome P450 system. CYP2D6 inhibitors include escitalopram, citalopram, sertraline, paroxetine, and fluoxetine. Fluoxetine and fluvoxamine are inhibitors of CYP2C19. Fluvoxamine is an inhibitor of CYP1A2. Consider reviewing a patient's medication history and health history prior to prescribing SSRIs (1).
SSRIs Method of Action
SSRI method of action has been subject to several studies, especially in the last few years. Serotonin is a neurotransmitter that plays a role in mood and other bodily functions. It can be measured in plasma, blood, urine, and CSF (6). It is important to note that serotonin is rapidly metabolized to 5-hydroxyindoleacetic acid (5-HIAA) (6). SSRIs work by inhibiting the reuptake of serotonin at certain chemical receptors, thereby increasing serotonin activity and concentration (1). SSRIs inhibit the serotonin transporter (SERT) at the presynaptic axon terminal.
By obstructing the SERT, a higher amount of serotonin (5-hydroxytryptamine or 5HT) remains in synaptic clefts. This higher amount of serotonin can then stimulate postsynaptic receptors for a more extended period (1). While SSRIs can increase serotonin activity, there is some evidence that suggests the possibility of long-term SSRI use reducing serotonin concentration (6). In addition, the clinical response to SSRIs in patients with MDD can take anywhere from a few to several weeks to emerge (7). While some research suggests that there are initial improvements in mood, evidence remains inconclusive as to the exact time SSRIs can take to provide a therapeutic response for patients (7). Also, while research suggests that SSRIs can increase serotonin levels, there is still mixed evidence on the exact method of action for SSRIs (7).
As a result, it is important to counsel patients that SSRIs can take a few weeks to provide a therapeutic response and to monitor mood and symptoms while taking SSRIs.
SSRI Side Effects
Every medication has the possibility of side effects, and SSRIs are no exception. Fortunately, SSRIs are known to have less side effects than other drug classes of antidepressants, such as monoamine oxidase inhibitors (MAOIs) or tricyclic antidepressants (TCAs). The most commonly known side effects of SSRIs include weight gain, sleep changes, headache, gastrointestinal issues, drowsiness, orthostatic hypotension, and sexual function changes (1).
Sleep changes can include an increased desire to sleep, increase in the amount of time sleeping, or insomnia. Gastrointestinal issues can include an upset stomach, nausea, or dry mouth. Mood changes, such as anxiety, are possible side effects as well. Sexual function changes can include erectile dysfunction, libido changes, impaired orgasmic response, and vaginal dryness (1, 8).
There are more serious possible side effects of SSRIs as well. For instance, SSRIs have the possible side effect of QT prolongation, which if left untreated or undiagnosed, can lead to fatal cardiac arrythmias (1, 8). In particular, the SSRI citalopram has been shown to have more of a risk for QT prolongation compared to other SSRIs. Also, like any other medication that can possibly increase levels of serotonin in the body, there is a possibility of serotonin syndrome as a complication of SSRI use. Possible serotonin syndrome clinical manifestations include increased blood pressure, increased sweating, increased reflex ability, and increased dry eyes (8). Due to the wide varied range of side effects, patient counseling, monitoring, and education is essential when prescribing SSRIs.
SSRI Black Box Warning
In 2004, the FDA issued a black box warning for SSRIs and other antidepressant medications due to the possible increased risk of suicidality in pediatric and young adult populations (up to age 25). When considering SSRI use in patients under 25 and knowing MDD is a risk factor for suicidality, having a conversation with the patient about risks versus benefits must be considered. However, in the past several years since the FDA's warning, there is no clear evidence showing a correlation between SSRIs and the increased risk of suicidality (1, 8). Health care provider professional discretion and patient condition should guide therapy.
SSRI Alternatives
MDD can be a complex, chronic condition to manage with varying clinical presentation and influence on a patient's quality of life. There are several alternatives to SSRI use, such as: (1, 9)
- Other prescription drugs
- Serotonin-norepinephrine reuptake inhibitors (SNRIs). Commonly known SNRIs include milnacipran, venlafaxine, desvenlafaxine, duloxetine, and levomilnacipran.
- Atypical antidepressants. Commonly known atypical antidepressants include bupropion and mirtazapine.
- Tricyclic antidepressants (TCAs). Commonly known TCAs include amitriptyline, desipramine, imipramine, clomipramine, doxepin, and nortriptyline.
- Monoamine oxidase inhibitors (MAOIs). Commonly known MAOIs include phenelzine, tranylcypromine, isocarboxazid, and selegiline.
- Psychotherapy, such as cognitive behavioral therapy (CBT) or interpersonal therapy
- Electroconvulsive therapy (ECT)
- Vagus Nerve Stimulation (VNS)
- Transcranial Magnetic Stimulation (TMS)

Self Quiz
Ask yourself...
- What are some possible side effects of SSRIs?
- What are some pharmacological alternatives to SSRIs?
Nursing Considerations
Nurse’s Role
What Is the Nurses' Role in SSRI Patient Education and Management?
Nurses remain the most trusted profession for a reason, and APRNs are often pillars of patient care in several health care settings. Patients turn to nurses for guidance, education, and support. While there is no specific guideline for the nurses' role in SSRI education and management, here are some suggestions to provide quality care for patients interested in or currently taking SSRIs to manage current or suspected major depressive disorder (MDD).
- Take a detailed health history. Often times, mental health symptoms, such as depressive thoughts or anxiety, are often dismissed in health care settings, even in mental health settings. If a patient is complaining of symptoms that could be related to major depressive disorder, inquire more about that complaint. Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient's complaint is not being taken seriously by other health care professionals, advocate for that patient to the best of your abilities.
- Review medication history at every encounter. Often times, in busy clinical settings, reviewing health records can be overwhelming. While a vast number of people take SSRIs, many are no longer benefiting from the medication. Ask patients how they are feeling on the medication, if their symptoms are improving, and if there are any changes to medication history.
- Ask about family history. If someone is complaining of symptoms that could be related to MDD, ask if anyone in their immediate family, such as their parent or sibling, experienced similar conditions.
- Be willing to answer questions about mental health and SSRIs. Society can often stigmatize open discussions of prescription medication and mental health. SSRIs are no exception. There are many people who do not know about the benefits and risks of SSRIs, the long-term effects of unmanaged MDD, or possible treatment options. Be willing to be honest with yourself about your comfort level discussing topics and providing education on SSRIs and MDD.
- Communicate the care plan to other staff involved for continuity of care. For several patients, MDD management often involves a team of mental health professionals, nurses, primary care specialists, pharmacies, and more. Ensure that patients' records are up to date for ease in record sharing and continuity of care.
- Stay up to date on continuing education related to SSRIs and mental health conditions, as evidence-based information is always evolving and changing. You can then present your new findings to other health care professionals and educate your patients with the latest information. You can learn more about the latest research on SSRIs and mental health by following updates from evidence-based organizations.
Identifying Major Depressive Disorder
How can nurses identify if someone has major depressive disorder?
Unfortunately, it is not possible to look at someone with the naked eye and determine if they have MDD. APRNs can identify and diagnose if someone has MDD by taking a complete health history, listening to patient's concerns, having patients complete the PHQ-9 questionnaire and communicating any concerns to other health care professionals (9).
Patient Education
What should patients know about SSRIs?
Patients should know that anyone has the possibility of experiencing side effects of SSRIs, just like any other medication. Patients should be aware that if they notice any changes in their mood, experience any sharp headaches, or feel like something is a concern, they should seek medical care. Due to social stigma associated with mental health and SSRI use, people may be hesitant to seek medical care for fear of being dismissed by health care professionals (1, 6). In addition, side effects (that interfere with the quality of life) are often normalized (1, 6). However, as more research and social movements discuss mental health and SSRI use more openly, there is more space and awareness for SSRI use and mental health.
Nurses should also teach patients to advocate for their own health in order to avoid progression of MDD and possible unwanted side effects of SSRIs. Here are important tips for patient education in the inpatient or outpatient setting.
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors)
- Tell the health care provider of any existing lifestyle concerns, such as alcohol use, other drug use, sleeping habits, diet, menstrual cycle changes (need to identify lifestyle factors that can influence SSRI use and MDD)
- Tell the health care provider if you notice any changes in your mood, behavior, sleep, sexual health (including vaginal dryness or erectile dysfunction), or weight (possible changes that could hint at more chronic side effects of SSRIs)
- Tell the health care provider if you have any changes in urinary or bowel habits, such as increased or decreased urination or defecation (potential risk for SSRI malabsorption or possible unwanted side effects)
- Tell the nurse of health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life
- Keep track of your mental health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes)
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality is a possible side effect for SSRI use)
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries
- Tell the health care provider if you notice any changes while taking medications or on other treatments to manage your MDD (potential worsening or improving mental health situation)


Self Quiz
Ask yourself...
- What are some possible ways you can obtain a detailed, patient centric health history?
- What are some possible ways APRNs can educate patients on SSRIs and major depressive disorder?
Research Findings
What Research on SSRIs exists presently?
There is extensive publicly available literature on SSRIs via the National Institutes of Health and other evidence-based journals.
What are some ways for people who take SSRIs to become a part of research?
If a patient is interested in participating in clinical trial research, they can seek more information on clinical trials from local universities and health care organizations.

Self Quiz
Ask yourself...
- What are some problems that can occur if SSRIs are not managing major depressive disorder symptoms adequately?
- What are some reasons someone might want to enroll in SSRI clinical trials?
Case Study
Case Study Part 1
Susan is a 22-year-old Black woman working as a teacher. She arrives for her annual exam at the local health department next to her place of work. She reports nothing new in her health, but she says she's been feeling more tired over the past few months. Susan reports having some trouble sleeping and trouble eating but doesn't feel too stressed overall. She heard one of her friends talking about SSRIs and wants to try them, but she's never taken prescription medications long-term before. She also thinks she might have some depression because she looked at some forums online and resonated with a lot of people's comments.

Self Quiz
Ask yourself...
- What are some specific questions you'd want to ask about her mental health?
- What are some health history questions you'd want to highlight?
- What lab work would you suggest performing?
Case Study Part 2
Susan agrees to complete bloodwork later this week and thinks she might have a family history of depression. She said that no one in her family talks about mental health, but she heard about depression from her friends recently and family a long time ago. She's back in the office a few weeks later, and her labs are within normal limits. Susan states she's still feeling fatigued and feeling a bit more hopeless these days. She denies thinking about hurting herself or others.

Self Quiz
Ask yourself...
- How would you discuss Susan's mental health concerns?
- How would you explain to Susan the influence of lifestyle, such as sleep, diet, and environment, on mood?
Case Study Part 3
Susan completed the PHQ-9 questionnaire and had a high score. After discussing her responses with her, you diagnose her with MDD. Susan admits that she is open to trying SSRIs. She is also open to seeing a therapist, as she states that she's never been to therapy. She would like resources on any therapy services, medication options, and non-pharmacological options to help her manage her condition.

Self Quiz
Ask yourself...
- Knowing Susan's concerns, what are some possible non-pharmacological management options for her MDD?
- What are some major SSRI side effects to educate Susan on?
References + Disclaimer
- American Association of Suicidology. (2019, July 17). Suicide loss survivors. American Association of Suicidology. https://suicidology.org/resources/suicide-loss-survivors/
- American Psychological Association. (2017). What is cognitive behavioral therapy? American Psychological Association. https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
- Boland, R., Verduin, M., & Ruiz, P. (2021). Kaplan & Sadock’s synopsis of psychiatry (12th ed.). Wolters Kluwer Medical.
- Bostwick, J. M., Pabbati, C., Geske, J. R., & McKean, A. J. (2016). Suicide attempt as a risk factor for completed suicide: Even more lethal than we knew. American Journal of Psychiatry, 173(11), 1094–1100. https://doi.org/10.1176/appi.ajp.2016.15070854
- Centers for Disease Control and Prevention. (2022a, April 12). Provisional count of deaths by leading causes of death – United States, 2021. Www.cdc.gov. https://www.cdc.gov/nchs/data/health_policy/provisional-leading-causes-of-death-for-2021.pdf
- Centers for Disease Control and Prevention. (2022b, November 2). Risk and protective factors. Www.cdc.gov. https://www.cdc.gov/suicide/factors/index.html
- Centers for Disease Control and Prevention. (2023a, May 1). Suicide rates by state. Www.cdc.gov. https://www.cdc.gov/suicide/suicide-rates-by-state.html
- Centers for Disease Control and Prevention. (2023b, August 10). Suicide Data and Statistics | Suicide | CDC. Www.cdc.gov; CDC. https://www.cdc.gov/suicide/suicide-data-statistics.html
- Chu, A., & Wadhwa, R. (2023, May 1). Selective serotonin reuptake inhibitors. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK554406/
- Cleveland Clinic. (2022, April 19). Dialectical behavior therapy (DBT). Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/22838-dialectical-behavior-therapy-dbt
- Cornell Law School. (2020, July). Physician-assisted suicide. LII / Legal Information Institute. https://www.law.cornell.edu/wex/physician-assisted_suicide
- Department of Veterans Affairs. (2021, December 3). Lethal means safety & suicide prevention. Www.mirecc.va.gov. https://www.mirecc.va.gov/visn19/lethalmeanssafety/
- Fornaro, M., Anastasia, A., Valchera, A., Carano, A., Orsolini, L., Vellante, F., Rapini, G., Olivieri, L., Di Natale, S., Perna, G., Martinotti, G., Di Giannantonio, M., & De Berardis, D. (2019). The FDA “black box” warning on antidepressant suicide risk in young adults: More harm than benefits?. Frontiers in Psychiatry, 10(294). https://doi.org/10.3389/fpsyt.2019.00294
- Hardey, S. (2021, July 28). Suicide among veterans – why are veterans at a higher risk of suicide? American Addiction Centers. https://americanaddictioncenters.org/veterans/suicide-among-veterans
- Herman, J., & O’Neill, K. (2021). Suicide risk and prevention for transgender people: Summary of research findings. https://williamsinstitute.law.ucla.edu/wp-content/uploads/Trans-Suicide-Summary-Sep-2021.pdf
- Huecker, M. R., Smiley, A., & Saadabadi, A. (2020). Bupropion. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470212/
- Jacobs, D., Baldessarini, R., Conwell, Y., Fawcett, J., Horton, L., Meltzer, H., Pfeffer, C., & Simon, R. (2009). Assessment and treatment of patients with suicidal behaviors. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/suicide.pdf
- Mayo Clinic. (2019, October 5). Serotonin and norepinephrine reuptake inhibitors (SNRIs). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/depression/in-depth/antidepressants/art-20044970
- Mental Health First Aid USA. (2020). Mental health first aid USA for adults assisting adults. National Council for Behavioral Health.
- Moraczewski, J., & Aedma, K. K. (2020). Tricyclic antidepressants. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557791/
- Moutier, C. (2023, July). Suicidal behavior – psychiatric disorders. MSD Manual Professional Edition. https://www.msdmanuals.com/professional/psychiatric-disorders/suicidal-behavior-and-self-injury/suicidal-behavior?query=Suicidal%20Behavior
- Mullins, N., Kang, J., Campos, A. I., Coleman, J. R. I., Edwards, A. C., Galfalvy, H., Levey, D. F., Lori, A., Shabalin, A., Starnawska, A., Su, M.-H., Watson, H. J., Adams, M., Awasthi, S., Gandal, M., Hafferty, J. D., Hishimoto, A., Kim, M., Okazaki, S., & Otsuka, I. (2022). Dissecting the shared genetic architecture of suicide attempt, psychiatric disorders, and known risk factors. Biological Psychiatry, 91(3), 313–327. https://doi.org/10.1016/j.biopsych.2021.05.029
- National Alliance on Mental Illness. (2022, August). Risk of suicide. Nami.org. https://nami.org/About-Mental-Illness/Common-with-Mental-Illness/Risk-of-Suicide
- National Institute of Mental Health. (2020). Suicide risk screening tool. https://www.nimh.nih.gov/sites/default/files/documents/research/research-conducted-at-nimh/asq-toolkit-materials/asq-tool/screening_tool_asq_nimh_toolkit.pdf
- National Institute of Mental Health. (2023). Frequently asked questions about suicide. Www.nimh.nih.gov. https://www.nimh.nih.gov/health/publications/suicide-faq
- National Institute on Drug Abuse. (2020, July 10). Treatment and recovery. National Institute on Drug Abuse. https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery
- Pfizer Inc. (n.d.). The patient health questionnaire (PHQ-9). https://coepes.nih.gov/sites/default/files/2020-12/PHQ-9%20depression%20scale.pdf
- Sabri, M. A., & Saber-Ayad, M. M. (2020). MAO inhibitors. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557395/
- Schreiber, J., & Culpepper, L. (2023, October). Suicidal ideation and behavior in adults. Www.uptodate.com. https://www.uptodate.com/contents/suicidal-ideation-and-behavior-in-adults#H2534680824
- Seattle University. (n.d.). Breaking the stigma about suicide. Www.seattleu.edu. https://www.seattleu.edu/wellness/mental/stigma/
- Substance Abuse and Mental Health Services Administration. (2009). SAFE-T pocket card: Suicide assessment five-step evaluation and triage for clinicians. Samhsa.gov. https://store.samhsa.gov/product/SAFE-T-Pocket-Card-Suicide-Assessment-Five-Step-Evaluation-and-Triage-for-Clinicians/sma09-4432
- Substance Abuse and Mental Health Services Administration. (2016, November 1). Table 4.1, evidence-based screening tools for substance use. Www.ncbi.nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK424859/table/ch4.t1/?report=objectonly
- The Columbia Lighthouse Project. (2016a). About the protocol the Columbia lighthouse project. The Columbia Lighthouse Project. https://cssrs.columbia.edu/the-columbia-scale-c-ssrs/about-the-scale/
- The Columbia Lighthouse Project. (2016b). SAFE-T with C-SSRS. The Columbia Lighthouse Project. https://cssrs.columbia.edu/documents/safe-t-c-ssrs/
- U.S. Department of Veteran Affairs. (2020, November 1). Suicide prevention program guide . Www.va.gov. https://www.mirecc.va.gov/suicideprevention/documents/suicidepreventionprogramguide_06222022.pdf
- U.S. Department of Veterans Affairs. (2022). National veteran suicide prevention annual report. https://www.mentalhealth.va.gov/docs/data-sheets/2022/2022-National-Veteran-Suicide-Prevention-Annual-Report-FINAL-508.pdf
- University of Washington. (2021, February 8). How to ask about substance use. Https://Psychiatry.uw.edu/; Department of Psychiatry and Behavioral Sciences. https://pcl.psychiatry.uw.edu/how-to-ask-about-substance-use/
- Washington State Legislature. (n.d.). WAC 246-337-110: Use of restraint and seclusion. Apps.leg.wa.gov. Retrieved November 12, 2023, from https://apps.leg.wa.gov/WAC/default.aspx?cite=246-337-110
- Washington State Legislature. (2015). Chapter 71.05 RCW: Behavioral health disorders. Wa.gov. https://app.leg.wa.gov/RCW/default.aspx?cite=71.05
- World Health Organization. (2021). Suicide worldwide in 2019. World Health Organization. https://iris.who.int/bitstream/handle/10665/341728/9789240026643-eng.pdf?sequence=1
- Yu H, Flores DD, Bonett S, Bauermeister, JA. LGBTQ+ cultural competency training for health professionals: a systematic review. BMC Medical Education. 2023;23:558:1-83.
- Morris, M., Cooper, R.L., Ramesh, A. et al. Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC Med Educ 19, 325 (2019). https://doi.org/10.1186/s12909-019-1727-3
- Waisel DB. Vulnerable populations in healthcare. Curr Opin Anesthesiol. 2013;26(2):186–92.
- Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: Trends over the past 10 years. NCHS Data Brief. 2012;2012(100):1–8.
- Institute of Medicine. Collecting sexual orientation and gender identity data in electronic health records: workshop summary. Washington DC: National Academy of Sciences; 2013.
- Quinn GP, Sanchez JA, Sutton SK, Vadaparampil ST, Nguyen GT, Green BL, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA-Cancer J Clin. 2015;65(5):384–400
- Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–60.
- Dilley JA, Simmons KW, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific northwest. Am J Public Health. 2010;100(3):460–7.
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health. 2013;103(10):1802–9.
- Bauermeister J, Eaton L, Stephenson R. A multilevel analysis of neighborhood socioeconomic disadvantage and transactional sex with casual partners among Young men who have sex with men living in metro Detroit. Behav Med. 2016;42(3):197–204.
- Smalley KB, Warren JC, Barefoot KN. Differences in health risk behaviors across understudied LGBT subgroups. Health Psychol. 2016;35(2):103–14.
- Staats C, Capatosto K, Wright RA, Jackson VW. State of the science: Implicit bias review 2016. Columbus: Kirwan Institute.
- Cochran SD, Bandiera FC, Mays VM. Sexual orientation-related differences in tobacco use and secondhand smoke exposure among US adults aged 20 to 59 years: 2003-2010 National Health and nutrition examination surveys. Am J Public Health. 2013;103(10):1837–44.
- Ramchand, R., Schuler, M. S., Schoenbaum, M., Colpe, L., & Ayer, L. (2021). Suicidality among sexual minority adults: Gender, age, and race/ethnicity differences. American Journal of Preventive Medicine. https://doi.org/10.1016/j.amepre.2021.07.012
- Charlton BM, Corliss HL, Missmer SA, Frazier AL, Rosario M, Kahn JA, et al. Reproductive health screening disparities and sexual orientation in a cohort study of U.S. adolescent and Young adult females. J Adolesc Health. 2011;49(5):505–10.
- Agénor M, Krieger N, Austin SB, et al. Sexual Orientation Disparities in Papanicolaou Test Use Among US Women: The Role of Sexual and Reproductive Health Services. Am J Public Health. 2014;104(2):e68-72
- Tracy JK, Lydecker AD, Ireland L. Barriers to cervical Cancer screening among lesbians. J Women’s Health. 2010;19(2):229–37.
- Safer JD, Coleman E, Feldman J, Garofalo R, Hembree W, Radix A, Sevelius J. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016 Apr;23(2):168-71. doi: 10.1097/MED.0000000000000227. PMID: 26910276; PMCID: PMC4802845.
- Heck JE, Sell RL, Gorin SS. Health care access among individuals involved in same-sex relationships. Am J Public Health. 2006;96(6):1111–8.
- Kamen C, Palesh O, Gerry AA, Andrykowski MA, Heckler C, Mohile S, et al. Disparities in health risk behavior and psychological distress among gay versus heterosexual male Cancer survivors. LGBT Health. 2014;1(2):86–U103.
- Legal L. When health care Isn’t caring: lambda Legal’s survey of discrimination against LGBT people and people with HIV. New York: Lamba Legal; 2010.
- Grant JM, Mottet LA, Tanis J. National Transgender Discrimination Survey Report on health and health care. Washington DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2010.
- Shires DA, Jaffee K. Factors associated with health care discrimination experiences among a National Sample of female-to-male transgender individuals. Health Soc Work. 2015;40(2):134–41.
- Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians’ experiences in the workplace. J Homosex. 2011;58(10):1355–71.
- Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54.
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
- Mereish EH, Bradford JB. Intersecting identities and substance use problems: sexual orientation, gender, race, and lifetime substance use problems. J Stud Alcohol Drugs. 2014;75(1):179–88.
- Torres CG, Renfrew M, Kenst K, Tan-McGrory A, Betancourt JR, Lopez L. Improving transgender health by building safe clinical environments that promote existing resilience: results from a qualitative analysis of providers. BMC Pediatr. 2015;15:187.
- Burke SE, Dovidio JF, Przedworski JM, Hardeman RR, Perry SP, Phelan SM, et al. Do contact and empathy mitigate Bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. 2015;90(5):645–51.
- Sabin JA, Riskind RG, Nosek BA. Health care Providers’ implicit and explicit attitudes toward lesbian women and gay men. Am J Public Health. 2015;105(9):1831–41.
- Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–7.
- Wilson TD, Brekke N. Mental contamination and mental correction: unwanted influences on judgments and evaluation. Psychol Bull. 1994;116(1):117–42.
- Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit Bias in health care: a narrative review. Group Proccess Interg. 2016;19(4):528–42.
- Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102(1):4–27.
- Van Ryn M, Saha S. Exploring unconscious bias in disparities research and medical education. JAMA. 2011;306(9):995–6.
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41.
- Nosek BA, Riskind RG. Policy implications of implicit social cognition. Soc Issue Policy Rev. 2012;6(1):113–47.
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
- Shavers VL, Fagan P, Jones D, Klein WMP, Boyington J, Moten C, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953–66.
- Chapman EN, Kaatz A, Carnes M. Physicians and implicit Bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–10.
- Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: Confronting racial and ethnic disparities in health care. Brian D. Smedley, Adrienne Y. Stith, and Alan R. Nelson, Editors; Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Board on Health Sciences Policy; Institute of Medicine. Washington, DC; 2003.
- Greenwald AG, Banaji MR, Nosek BA. Statistically small effects of the implicit association test can have societally large effects. J Pers Soc Psychol. 2015;108(4):553–61.
- Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P. (2019). Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC medical education, 19(1), 325. https://doi.org/10.1186/s12909-019-1727-3
- Human rights campaigns. Glossary of terms. Retrieved from https://www.hrc.org/resources/glossary-of-terms
- Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community, a field guide. Joint Commission. Retrieved from https://www.jointcommission.org/ /media/enterprise/tjc/imported-resource assets/documents/lgbtfieldguide_web_linked_verpdf.pdf?db=web hash=1EC363A65C710BCD1D4E14ED120CB2
- Delivering culturally sensitive care to LGBTQI Patients. The Journal for nurse practitioners. Volume 13, issue 5 p342-347.
- (2023, July 25). Telehealth. Www.Telehealth.HHS.gov. Retrieved July 26, 2023, from https://en.m.wikipedia.org/wiki/Telehealth
- Skill Creations, Inc. (2022). Skill Creations Intranet. Retrieved July 24, 2023, from www.skillcreations.com.
- (2008, June 24). H.R. 6353 – Ryan Haight Online Pharmacy Consumer Protection Act of 2008. Www.Congress.gov. Retrieved July 24, 2023, from https://www.congress.gov/bill/110th-congress/house-bill/6353#:~:text=The%20summary%20of%20that%20version,Internet%20without%20a%20valid%20prescription
- (2019, March 1). North Carolina Medical Board – www.Ncmedboard.org. Retrieved July 25, 2023, from https://www.ncmedboard.org/resources-information/professional-resources/laws-rules-position-statements/position-statements/telemedicine
- (2022, June 29). Obtaining Informed Consent – www.Telehealth.HHS.gov. Retrieved July 26, 2023, from https://telehealth.hhs.gov/providers/preparing-patients-for-telehealth/obtaining-informed-consent
- (2022, January 12). Telehealth Documentation Requirements – www.Securityhealth.org. Retrieved July 29, 2023, from securityhealth.org/providers/provider-manual/shared-content/documentation-requirements/telehealth-documentation-requirements?documentation-requirements-group–direct-pay
- United Spinal Association. (n.d.). What is spinal cord injury/disorder? Retrieved from https://unitedspinal.org/what-is-spinal-cord-injury-disorder-scid/
- United Spinal Association. (2022). Spinal cord injuries facts and stats. Retrieved from https://unitedspinal.org/spinal-cord-injury-facts-and-stats/
- U.S. Department of Health and Human Services, National Institutes of Health. (2022). What causes spinal cord injury (SCI) and how does it affect your body? Retrieved from https://www.nichd.nih.gov/health/topics/spinalinjury/conditioninfo/causes
- World Health Organization. (2013). Spinal cord injury. Retrieved from https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury
- National Institute of Neurological Disorders and Stroke. (2023). Spinal cord injury. Retrieved from https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury
- National Spinal Cord Injury Statistical Center. (2023). Traumatic spinal cord injury statistics: Facts and figures at a glance. Retrieved from https://www.nscisc.uab.edu/public/Facts%20and%20Figures%202023%20-%20Final.pdf
- Centers for Disease Control and Prevention. (2020). Many adults with disabilities report frequent mental distress. Retrieved from https://www.cdc.gov/ncbddd/disabilityandhealth/features/adults-with-disabilities-mental-distress.html
- Allen K. J. & Leslie S. W. (2023). Autonomic dysreflexia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482434/
- Bowel and Bladder Community. (n.d.). Spinal injuries. Retrieved from https://www.bladderandbowel.org/help-information/spinal-injuries/
- Shepherd Center. (n.d.). Bowel function after SCI. Retrieved from https://www.myshepherdconnection.org/sci/bowel-care/function-after-sci
- Emmanuel A. (2019). Neurogenic bowel dysfunction. F1000Research, 8, F1000 Faculty Rev-1800. https://doi.org/10.12688/f1000research.20529.1
- Gater, D. R., Bauman, C., & Cowan, R. (2020). A primary care provider’s guide to diet and nutrition after spinal cord injury. Topics in spinal cord injury rehabilitation, 26(3):197–202. https://doi.org/10.46292/sci2603-197
- Christopher & Dana Reeve Foundation. (2023). Our mission. Retrieved from https://www.christopherreeve.org/community/about-us/history-of-the-reeve-foundation/
- University of Miami, Miller School of Medicine. (n.d.). About us. Retrieved from https://www.themiamiproject.org/about-us/
- U.S. Department of Health and Human Services, Administration for Community Living. (n.d.) Advancing independence, integration, and inclusion throughout life. Retrieved from https://acl.gov/
- Paralyzed Veterans of America. (n.d.). Mission statement. Retrieved from https://pva.org/about-us/mission-statement/
- United Spinal Association. (2023). About us. Retrieved from https://unitedspinal.org/our-story/
- Agency for Healthcare Research and Quality. (2014). Preventing pressure ulcers in hospitals: Are we ready for this change? Retrieved from https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu1.html
- Agency for Healthcare Research and Quality. (2014). Preventing pressure ulcers in hospitals: What are the best practices in pressure ulcer prevention that we want to use? Retrieved from https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu3.html
- Agency for Healthcare Research and Quality. (2017). Estimating the additional hospital inpatient cost and mortality associated with selected hospital-acquired conditions. Retrieved from https://www.ahrq.gov/hai/pfp/haccost2017-results.html
- Agency for Healthcare Research and Quality. (2017). Patient safety indicators™ v2020 benchmark data tables. Retrieved https://qualityindicators.ahrq.gov/Downloads/Modules/PSI/V2020/Version_2020_Benchmark_Tables_PSI.pdf
- Agency for Healthcare Research and Quality. (2017). Pressure injury prevention program implementation guide. Retrieved https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureinjury/guide/intro.html#Program
- Agency for Healthcare Research and Quality. (2020). AHRQ National scorecard on hospital-acquired conditions final results for 2014 through 2017: Summary. Retrieved from https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/pfp/Updated-hacreportFInal2017data.pdf
- Al Aboud, A. M. & Manna, B. (2023). Wound pressure injury management. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532897/
- Black, J. et al. (2023). Current perspectives on pressure injuries in persons with dark skin tones from the National Pressure Injury Advisory Panel. Advances in Skin & Wound Care, 36(9):470-480. Retrieved from https://journals.lww.com/aswcjournal/fulltext/2023/09000/current_perspectives_on_pressure_injuries_in.5.aspx
- Brennan, M. (2022). Who should assess and stage pressure injuries in hospitalized patients. Advances in Skin & Wound Care 35(9):473-476. Retrieved from https://journals.lww.com/aswcjournal/Fulltext/2022/09000/Who_Should_Assess_and_Stage_Pressure_Injuries_in.2.aspx
- Broderick, V. V. & Cowan, L. J. (2021). Pressure injury related to friction and shearing forces in older adults. Journal of Dermatology and Skin Science. Retrieved from https://www.dermatoljournal.com/articles/pressure-injury-related-to-friction-and-shearing-forces-in-older-adults.html
- Centers for Medicare and Medicaid Services. (2023). Quality measures. Retrieved from https://www.cms.gov/medicare/quality/measures
- Centers for Medicare and Medicaid Services. (2023). Quality measurement and quality improvement. Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/Quality-Measure-and-Quality-Improvement-
- Cox, J. & Schallom, M. (2021). Pressure injuries in critical care patients: a conceptual schema. Advances in Skin & Wound Care 34(3):124-131. Retrieved from https://journals.lww.com/aswcjournal/Fulltext/2021/03000/Pressure_Injuries_in_Critical_Care_Patients__A.4.aspx
- Edsberg, L. E. et al. (2016). Revised National Pressure Ulcer Advisory Panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound Ostomy Continence Nursing, 43(6):585-597. Retrieved from https://journals.lww.com/jwocnonline/fulltext/2016/11000/revised_national_pressure_ulcer_advisory_panel.3.aspx
- The Joint Commission. (2022). Quick Safety 25: Preventing pressure injuries (Updated March 2022). Retrieved from https://www.jointcommission.org/resources/news-and-multimedia/newsletters/newsletters/quick-safety/quick-safety-issue-25-preventing-pressure-injuries/preventing-pressure-injuries/
- Kottner, J.; Cuddigan, J.; Carville, K.; Balzer, K.; Berlowitz, D.; Law, S.; Litchford, M.; Mitchell, P.; Moore, Z.; Pittman, J.; et al. Prevention and Treatment of Pressure Ulcers/Injuries: The Protocol for the Second Update of the International Clinical Practice Guideline 2019. J. Tissue Viability 2019, 28, 51–58.
- Mondragon, N. & Zito, P. M. (2022). Pressure injury. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557868/
- National Pressure Injury Advisory Panel. (2016). Pressure injury and stages. Retrieved from https://cdn.ymaws.com/npiap.com/resource/resmgr/NPIAP-Staging-Poster.pdf
- National Pressure Injury Advisory Panel. (2016). Pressure injury prevention points. Retrieved from https://npiap.com/page/PreventionPoints
- National Pressure Injury Advisory Panel. (2020). Best practices for prevention of medical device-related pressure injuries. Retrieved from https://npiap.com/page/MDRPI-Posters
- Nursing Times (2020). Pressure Ulcer Education 5: Keeping Patients Moving. Retrieved on September 12th, 2023, from https://www.nursingtimes.net/clinical-archive/tissue-viability/pressure-ulcer-education-5-keeping-patients-moving-13-01-2020/
- Pitman, J. et al. (2019). Hospital-acquired pressure injuries in critical and progressive care: Avoidable versus unavoidable. American Journal of Critical Care, 28(5):338-350. Retrieved from https://doi.org/10.4037/ajcc2019264
- Salcido, R. (2016). From pressure ulcers to “pressure injury”: Disambiguation and anthropology. Advances in Skin & Wound Care, 29(7):295. Retrieved from https://journals.lww.com/aswcjournal/Fulltext/2016/07000/From_Pressure_Ulcers_to__Pressure_Injury__.1.aspx
- Shear Force” and “Shear Force Closeup” by Meredith Pomietlo at Chippewa Valley Technical College are licensed under CC BY 4.0
- Tenny, S. & Hoffman, M. R. (2023). Prevalence. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430867/
- Zhang, X. et al. (2021). The global burden of decubitus ulcers from 1990 to 2019. Scientific Reports 11(21750). Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8571371/
- Abi-Aad, K., & Derain, A. (2023, August 17). Hydromorphone. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK470393/
- Adler, J., Ballantyne, J., Chou, R., Davies, P., Fanciullo, G., & Fine, P. (2009). Clinical Guidelines for the Use of Chronic Opioid Therapy in Chronic NonCancer Pain. The Journal of Pain, 113-130.
- Ahmad, F., Rossen, L., Sutton, P., & & Talih, M. (2018). Provisional drug overdose. National Vital Statistics Reports, pp. 1-12.
- Altman, R., Clark, M., Huddart, R., & Klein, T. (2018, October 28). Pharm GKB Summary: Oxycodone Pathway, Pharmacokinetics. Retrieved from Pharmacogenet Genomics: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6602093/#:~:text=Approximately%2072%25%20of%20an%20oxycodone,oxycodone%20is%20unconjugated%20%5B70%5D
- Atrux-Tallau, N., naimi, Z., & Jaudinot, E. (2022, November 4). Pharmocokinetics of Morphine Sulfate Orodispersible tablets and Bioequivalence with Immediate-Release Oral Morphine Sulfate Formulations in Healthy Adult SubjectsUnder fastin Conditions. Retrieved from Clinical Drig Investigation: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9705466/
- Baldwin, G., Compton, W. M., Han, B., Houry, D., Jones, C. M., & Vivolo-Kantor, A. (2021, September 24). Methamphetamine use in the United States: epidemiological update and implocations for prevention, treatment and harm reduction. Annual New York Academy of Science. New York: National Institute of Health.
- Berg, K. A., & Clarke, W. P. (2018). Making Sense of Pharmacology: Inverse Agonism and Functional Selectivtiy. International Journal of Neuropsychopharmacology, 962-977.
- Bistas, K., Lopez-Ojeda, W., & Ramos-Matos, C. (2023, May 29). Fentanyl. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK459275/
- Blyth, F., Briggs, A., Hoy, D. G., March, L. M., & Schneider, C. H. (2019). The Global Burden of Musculoskeletal Pain-Where to From Here? American Journal of Public Health, 35-40.
- Bramanti, P., Cavalli, E., Mammana, S., Mazzon, E., & Nicoletti, F. (2019). The neuropathic pain: An Overview of the current treatment and future therapeutic approaches. International Journal of Immunopathology and Pharmacology, 33.
- Brennan, F., Carr, D., Cousins, M., & Pain, D. (2013). Pain Management: A Fundamental Human Right. Anesthesia and Analgesia, 224-227.
- Carver, A. C., & Foley, K. (2003). Types of Pain. In D. Kufke, & R. W. Pollock, Cancer Medicine. Hamilton: Holland Frei Cancer Medicine.
- Centers for Disease Control and Prevention. (2022). CDCs Clinical Practice Guidelines for Prescribing Opioids. Retrieved from Opioids: https://www.cdc.gov/opioids/healthcare-professionals/prescribing/guideline/index.html?s_cid=DOP_Clinician_Search_Paid_001&gclid=CjwKCAjwrranBhAEEiwAzbhNtVKOCMzLLnwhfj7B2D_aBCZM_SryNcEyXl0GRigmorFhKve2ekCVrhoCNYQQAvD_BwE
- Centers for Disease Control and Prevention. (2023, August 8). Opioids. Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/opioids/basics/epidemic.html#print
- Chiang, N., Gyaw, S., & Krieter, P. A. (2019). Comparison of the Pharmacokinetic Properties of Naloxone Following the Use of FDA-Approved Intranasal and Intramuscular Devices Versus a Common Improvised Nasal Naloxone Device. Journal of Clinical Pharmacology, 1078-1084.
- Cicero, T., & Ellis, M. &. (2017). The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA, 673-681.
- Cofano, S., & Yellon, R. (2022, October 24). Stat Pearls: Hydrocodone. Retrieved from National Institutes of Health: https://www.ncbi.nlm.nih.gov/books/NBK537288/
- Dart, R., Hoyte, C., & Nakhee, S. (2021). A Review on Tramadol Toxicity: Mechanism of Action, Clinical Presentation, and Treatment. Forensic Toxicology, 293-310. Retrieved from Forensic Toxicology: https://link.springer.com/article/10.1007/s11419-020-00569-0
- Delsignor, R. e. (2001). Lofexidine versus clonidine in rapid opiate detoxification. Journal of Substance Abuse Treatment, 11-17.
- Department of Defense Veterans Association. (2023). Defense and Veterans Pain Rating Scale. Retrieved from VA.gov: https://www.va.gov/PAINMANAGEMENT/docs/DVPRS_2slides_and_references.pdf
- Department of Health and Aged Care. (2013, January 20). FLACC Pain Scale. Retrieved from health.gov: https://www1.health.gov.au/internet/publications/publishing.nsf/Content/triageqrg~triageqrg-pain~triageqrg-FLACC
- Donaldson, S. L. (2017). Provider-Based Interventions to Mitigate Risk for Opioid Pain Medication Abuse Among Adult Patients in a Primary Care Setting.
- Dydyk, A. M., & Grandhe, S. (2023, January 29). Pain Assessment. Retrieved from STAT PEARLS: https://www.ncbi.nlm.nih.gov/books/NBK556098/#:~:text=Pain%20is%20the%20most%20common,pain%20in%20the%20United%20States.
- Fan, M., Hamilton, M., Hyland, B., & Tscheng, D. (2019). Diversion of Controlled Drugs in Hospitals: A Scoping review of Contributors and Safeguards. Journal of Hospital Medicine.
- GeriatricPain.org. (2022, January). Fast Facts: Selected Pain Assessment Tools. Retrieved from Geriatricpain.org: Geriatricpain.org https://geriatricpain.org/selected-pain-assessment-tools-fc
- Haffajee, R., Jena, A., Weiner, S., & & Kesselheim, A. (2019). Mandatory use of prescription drug monitoring programs. Journal of the American Medical Association, 1667-1668.
- International Association for the Study of Pain . (2020, July 16). IASP Announces Revised Definition of Pain. Retrieved from International Association for the Study of Pain: https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
- JAMA. (2023). Substance Use and Addiction Medicine. Retrieved from JAMA Network: https://jamanetwork.com/collections/5921/substance-use-and-addiction-medicine
- John, W. S., Schwartz, R. P., Subramanian, G., & Wu, L.-T. (2018). Prevalence, Patterns and correlates of multiple substance use disorders among adults. Drug and Alcohol Dependency, 79-87.
- Jones, C., Einstein, E., & Compton, W. (2018). Changes in synthetic opioid involvement in drug overdose deaths in the United States. JAMA, 1819-1821.
- Kalava, A., King, K. C., & Preuss, C. V. (2023, April 29). Perscription of Controlled Substances: Benefits and Risks. Retrieved from STAT PEARLS: https://www.ncbi.nlm.nih.gov/books/NBK537318/
- Khalid, N., Patel, P., & Singh, A. (2023, January). Cannabis Versus Opioids for Pain. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK573080/
- Kreutzwiser, D., & Tawfic, Q. (2020). Mathadone for Pain Management. A Pharmacotherapeutic Review, 827-839.
- Kroenke, K., Spiter, R., Williams, J., & Lowe, B. (2011, Nov). An ultra-brief screening scale for anxiety and depression: the PHQ-4. From Principles of Neuropathic Pain Assessment and Management, 613-21. Psychosomatics 2009.
- Manchikanti, L., Kaye, A., Knezevic, N., McAnally, H., Slavin, K., Trescot, A., & Hirsch, J. (2018). Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians guidelines. Pain Physician, S3-S92.
- Marquez, C. B. (2020). Changing the outlook toward the problem of opioid addiction: From “War on Drug” to “Public Health Emergency”. Seton Hall: Law Student Scholarship.
- Marsch, L., Borodovsky, J., & Dallery, J. (2019). Advances in the psychosocial treatment of addiction: The role of technology in the delivery of evidence-based psychosocial treatment. The Psyciatric Clinics of North America, 585-596.
- McLellan, T., & Volkow, N. (2016). Opioid Abuse in Chronic Pain-Misconceptions and Mitigation Strategies. New England Journal of Medicine, 1253-1263.
- National Institute of Drug Abuse (NIDA). (2023, August 30). Prescription Opioid Drug Facts. Retrieved from National Institute on Drug Abuse: https://nida.nih.gov/publications/drugfacts/prescription-opioids
- National Institute of Health. (2023, August 25). Medications for Opioid Overdose, Withdrawal, & Addiction. Retrieved from National Institute of Drug Addiction: https://nida.nih.gov/research-topics/opioids/medications-opioid-overdose-withdrawal-addiction-infographic
- Pain Physician. (2008). Opioid Special Issue. Pain Physician, S133-S153.
- Ransford, e. a. (2019, February 08). The Ransford Pain Drawing . Retrieved from compassionandsupport.org: https://compassionandsupport.org/wp-content/uploads/sites/2/2019/08/PainScaleRansford.pdf
- Rudd, R. A., Zibbell, J., & Gladden, M. (2016). Increases in drug and opioid overdose deaths-Untied States. Morbidity and Mortlity Weekly Report, 1378-1382.
- SAMHSA. (2020). Key Substance Use and Mental Health Indicators in the United States: Ressults from the 2019 National Survey on Drug Use and Health. SAMHSA.
- Scalpel, S. (2016, November). The Joint Commission Deserves Some Blame for the Opioid Crisis. Retrieved from Missouri Medicine: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6139759/
- Scholl, L., Seth, P., Kariisa, M., Wilson, N., & Baldwin, G. (2019). Drug and opioid-involved overdose deaths-Unioted States, 2013-2017. Morbidity and Mortatlity Weekly Report 67, 1419-1427.
- Stauffer, L., & Gibson, S. (2017). The Nurse’s Role in Identifying and Educating Patients At Risk for Opioid Abuse. AAACN Viewpoint, 1.
- The Joint Commission. (2023, January). The Joint Commission History Timeline. Retrieved from JointCommission.org: https://www.jointcommission.org/-/media/tjc/documents/tjc-history-timeline-through-2022.pdf
- Toombs, K., Kral, L., Colleran, C., & & Varney, S. (2018). Nurse practitioner-pharmacist collaboration in pain management: Strategies for success. . Journal of the American Association of Nurse Practitioners, 141-148.
- U.S. Food and Drug Administration. (2023, May 23). FDA. Retrieved from Information about Medication Assisted Treatment (MAT): https://www.fda.gov/drugs/information-drug-class/information-about-medication-assisted-treatment-mat
- Volkow, N., Jones, E., Einstein, E., & Wargo, E. (2019). Prevention and Treatment of Opioid mIsuse and Addiction: A Review. JAMA Psychiatry, 208-216.
- Katie Kerwin McCrimmon, Uch. (2023, May 15). What is Mounjaro? and does it work better for weight loss than Ozempic and Wegovy?. UCHealth Today. https://www.uchealth.org/today/what-is-mounjaro-and-how-does-it-work-for-weight-loss/
- National Institutes of Health. (2023, July 28). DailyMed – mounjaro- tirzepatide injection, solution. U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d2d7da5d-ad07-4228-955f-cf7e355c8cc0
- Type 2 Diabetes Treatment to Lower A1C | Mounjaro® (tirzepatide). (2023). https://www.mounjaro.com/?utm_id=go_cmp-16966473997_adg-133042365262_ad-626584063672_kwd-1651326559888_dev-c_ext-_prd-_mca-_sig-EAIaIQobChMIxcXZqYeHgQMVhDjUAR2Lvw5CEAAYASAAEgIMkfD_BwE&utm_source=google&utm_medium=ppc&campaign=16966473997&adgroup=133042365262&ad=626584063672&utm_keyword=kwd-1651326559888&gclid=EAIaIQobChMIxcXZqYeHgQMVhDjUAR2Lvw5CEAAYASAAEgIMkfD_BwE
- GoodRX – error. (2023, July 14). https://www.goodrx.com/mounjaro/how-make-you-feel
- Chen, S. (2023, July 28). Diabetes drug Mounjaro shown to have extraordinary weight loss for people without diabetes. diaTribe. https://diatribe.org/diabetes-drug-mounjaro-shown-have-extraordinary-weight-loss-people-without-diabetes
- VA Pharmacy Benefits Management Services. (2022, August). Tirzepatide Injection Criteria for Use. https://www.va.gov/formularyadvisor/DOC_PDF/CFU_Tirzepatide_MOUNJARO_Criteria_Aug_2022.pdf.
- Allied PR. (2023 B.C.E., May 6). Mounjaro Weight Loss: Newly Launch Over The Counter Alternative Pills To Tirzepatide & Mounjaro Weight Loss. https://newsdirect.com/news/mounjaro-weight-loss-newly-launch-over-the-counter-alternative-pills-to-tirzepatide-and-mounjaro-weight-loss-300908569. Retrieved August 30, 2023, from https://newsdirect.com/news/mounjaro-weight-loss-newly-launch-over-the-counter-alternative-pills-to-tirzepatide-and-mounjaro-weight-loss-300908569
- Mounjaro (2023). Savings and support for Mounjaro. Retrieved on August 31st 2023 from https://www.mounjaro.com/savings-resources?gclid=Cj0KCQjw9MCnBhCYARIsAB1WQVWAcINPKFwiHl4SbZQiGC8E_o9wHVOkDJDDUuphW3OlsKBagVTF1rQaApLJEALw_wcB
- Global diabetes cases to soar from 529 million to 1.3 billion by 2050. (n.d.). The Institute for Health Metrics and Evaluation. https://www.healthdata.org/news-events/newsroom/news-releases/global-diabetes-cases-soar-529-million-13-billion-2050.
- Diabetes Research Institute Foundation. (2023, March 31). Diabetes Statistics – DRIF. DRIF. https://diabetesresearch.org/diabetes-statistics/#:~:text=37.3%20million%20people%2C%20or%2011.3,yet%20been%20diagnosed%20(2022)
- Manage blood sugar. (2021, April 28). Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/managing/manage-blood-sugar.html
- About the National Diabetes Prevention Program | CDC. (n.d.). https://www.cdc.gov/diabetes/prevention/about.htm#:~:text=The%20National%20Diabetes%20Prevention%20Program%E2%80%94or%20National%20DPP%E2%80%94was%20created,diabetes%20in%20
- Ms, M. G. R. (2023, February 16). All about Ozempic. Healthline. https://www.healthline.com/health/drugs/ozempic#_noHeaderPrefixedContent
- Professional, C. C. M. (n.d.). Ghrelin. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22804-ghrelin#:~:text=Ghrelin%20and%20leptin%20are%20two,brain%20when%20you’re%20hungry
- Prelipcean, M., MD. (2020, June 22). Behind the counter: Glucagon-like peptide-1 receptor agonists for type 2 diabetes. https://www.medicalnewstoday.com/articles/glp-1-receptor-agonists-type-2-diabetes
- Mba, A. B. P. (2023, May 1). Ozempic side effects: What you should know. https://www.medicalnewstoday.com/articles/drugs-ozempic-side-effects
- Delong, C. (2023, February 11). Black box warning. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538521/
- MNT Medical Network. (2023, February 16). Ozempic (semaglutide). https://www.medicalnewstoday.com/articles/326252
- Ozempic® vs. Other Type 2 Diabetes Treatments | Ozempic® (semaglutide) injection 0.5 mg or 1 mg. (n.d.). https://www.ozempic.com/why-ozempic/diabetes-medicines-comparison.html
- Northrop, A. (2023, August 3). Ozempic For Weight Loss: Side Effects, Risks And More. Forbes Health. https://www.forbes.com/health/body/ozempic-for-weight-loss/%20)
- Kerwin McCrimmon, UCHealth, K. (2023, April 5). Wegovy vs. Ozempic: The truth about new ‘weight-loss’ drugs. Uchealth. https://www.uchealth.org/today/wegovy-vs-ozempic-the-truth-about-new-weight-loss-drugs/#:~:text=If%20you%20take%20Wegovy%20or,to%20keep%20benefiting%20from%20them
- Stott, R. (2023, August 4). Lawsuit claims Ozempic, Mounjaro labels ‘downplayed severity’ of gastroparesis. Healio Gastroenterology. Retrieved August 11, 2023, from https://www.healio.com/news/gastroenterology/20230804/lawsuit-claims-ozempic-mounjaro-labels-downplayed-severity-of-gastroparesis#:~:text=While%20the%20drug%20label%20for,not%20recommended%20in%20these%20patients.%E2%80%9D
- How Does Gastroparesis Affect People with Diabetes? (2022, August 30). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/professionals/diabetes-discoveries-practice/how-gastroparesis-affect-people-with-diabetes
- Living Healthy with Diabetes. (2023, March 29). www.heart.org. https://www.heart.org/en/health-topics/diabetes/prevention–treatment-of-diabetes/living-healthy-with-diabetes
- Move more; sit less. (2023, June 22). Centers for Disease Control and Prevention. https://www.cdc.gov/physicalactivity/basics/adults/index.htm#:~:text=Each%20week%20adults%20need%20150,Physical%20Activity%20Guidelines%20for%20Americans.&text=We%20know%20150%20minutes%20of,do%20it%20all%20at%20once
- Good sleep habits. (2022, September 13). Centers for Disease Control and Prevention. https://www.cdc.gov/sleep/about_sleep/sleep_hygiene.html
- Centers for Disease Control and Prevention. (2022, August 1). Food and nutrition insecurity and diabetes. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes-and-food-insecurity.htm
- American Psychiatric Association. (2020, December). What is a substance use disorder? https://www.psychiatry.org/patients-families/addiction-substance-use-disorders/what-is-a-substance-use-disorder
- Durrani M, Bansal K. Methadone. [Updated 2023 Apr 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562216/
- Kumar R, Viswanath O, Saadabadi A. Buprenorphine. [Updated 2023 Apr 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459126/
- National Center for Drug Abuse Statistics. (2023). Drug abuse statistics. https://drugabusestatistics.org/
- National Institute of Health. (2018, June). Understanding drug use and addiction. https://nida.nih.gov/publications/drugfacts/understanding-drug-use-addiction
- Singh D, Saadabadi A. Naltrexone. [Updated 2023 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534811/
- Substance Abuse and Mental Health Services Administration. (2023, August). Methadone take-home flexibilities extension guidance. https://www.samhsa.gov/medications-substance-use-disorders/statutes-regulations-guidelines/methadone-guidance#:~:text=In%20treatment%200%2D14%20days,be%20provided%20to%20the%20patient
- S. Food and Drug Administration. (2023, May). Information about medication assisted treatment (MAT). https://www.fda.gov/drugs/information-drug-class/information-about-medication-assisted-treatment-mat
- Akbari, P., Khorasani-Zadeh, A. (Updated 2023, January 23). Thiazide Diuretics. In Stat Pearls. Stat Pearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532918/
- Alley, W.D., & Schick, M.A. (Updated 2023, July 24). Hypertensive Emergency. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470371/
- American Heart Association. (2023 June 7). Types of Blood Pressure Medications. Retrieved from https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications
- Arumugham, V.B., & Shahin, M.H. (Updated 2023, May 29). Therapeutic Uses of Diuretic Agents. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557838/
- Brater, D.C., & Ellison, D.H. (Updated 2022, November 30). Mechanism of action of diuretics. UpToDate. Retrieved from https://www.uptodate.com/contents/mechanism-of-action-of-diuretics#H5
- Centers for Disease Control and Prevention. (2023, July 6). Facts about Hypertension. Retrieved from https://www.cdc.gov/bloodpressure/facts.htm
- Centers for Disease Control and Prevention. (2021, May 18). High Blood Pressure Symptoms and Causes. Retrieved from https://www.cdc.gov/bloodpressure/about.htm
- Farzam, K., & Jan, A. (Updated 2023, August 22). Beta Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532906/
- Goyal, A., Cusick, A.S., & Thielemier, B. (Updated 2023, June 26). ACE Inhibitors. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430896/
- Hariri, L., & Patel, J.B. (Updated 2023, August 14). Vasodilators. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554423
- Hill, R.D., & Vaidya, P. (Updated 2023, March 27). Angiotensin II Receptors Blockers (ARBs). In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK537027/
- Huxel, C., Raja, A., Ollivierre-Lawrence, M.D. (Updated 2023, May 22). Loop Diuretics. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK546656/
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Loop Diuretics. [Updated 2021 Oct 13]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548619/
- Mann, J.F.E, &Flack, J.M. (Updated 2023, June 22). Choice of Drug Therapy in Primary (Essential) Hypertension. UpToDate. Retrieved from https://www.uptodate.com/contents/choice-of-drug-therapy-in-primary-essential-hypertension
- McKeever, R.G., & Hamilton, R.J. (Updated 2022, August 5). Calcium Channel Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482473/
- MedlinePlus. (2023). Hydrochlorothiazide. National Institutes of Health. Retrieved from https://medlineplus.gov/druginfo/meds/a682571.html
- MedlinePlus. (2023). Metoprolol. National Institutes of Health. Retrieved from https://medlineplus.gov/druginfo/meds/a682864.html
- Nachawati D, Patel JB. (Updated 2023, July 3). Alpha-Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK556066/
- Naranjo, M., Chauhan, S., & Paul, M. (Updated 2023, June 19). Malignant Hypertension. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507701
- Taylor, B.N., & Cassagnol, M. (Updated 2023, July 10). Alpha-Adrenergic Receptors. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539830/
- Verdecchia, P., Cavallini, C., & Angeli, F. (2022). Advances in the Treatment Strategies in Hypertension: Present and Future. Journal of cardiovascular development and disease, 9(3), 72. https://doi.org/10.3390/jcdd9030072
- American Academy of Neurology. (2019). AAN Updates Guideline on Valproate for Women with Epilepsy. Neurology Today, 19(5), 46-47.
- American Headache Society. (2020). The American Headache Society position statement on integrating new migraine treatments into clinical practice. Headache: The Journal of Head and Face Pain, 60(3), 415-423.
- American Nurses Association. (2017). Nursing: Scope and standards of practice (3rd ed.). Silver Spring, MD: American Nurses Association.
- Ashina, M., Goadsby, P. J., Reuter, U., Silberstein, S., Dodick, D. W., Xue, F., … & Trugman, J. M. (2020). Long-term efficacy and safety of erenumab in migraine prevention: Results from a 5-year, open-label treatment phase of a randomized clinical trial. European Journal of Neurology, 27(6), 1058-1067.
- Buse, D. C., Silberstein, S. D., Manack, A. N., Papapetropoulos, S., & Lipton, R. B. (2019). Psychiatric comorbidities of episodic and chronic migraine. Journal of Neurology, 266(3), 634-646.
- Davies, N. M., & Anderson, K. E. (2020). Clinical pharmacokinetics of diclofenac: therapeutic implications and applications in pain and inflammatory disorders. Clinical Pharmacokinetics, 59(2), 153-162.
- Dodick, D. W. (2018). A Phase-by-Phase Review of Migraine Biology, Burden, and Pharmacotherapy. Headache: The Journal of Head and Face Pain, 58(S1), 4-16.
- Dodick, D. W., Lipton, R. B., Ailani, J., Lu, K., Finnegan, M., Trugman, J. M., & Szegedi, A. (2019). Ubrogepant for the treatment of migraine. New England Journal of Medicine, 381(23), 2230-2241.
- Dodgson, S. J., Shank, R. P., & Maryanoff, B. E. (2018). Topiramate as an inhibitor of carbonic anhydrase isoenzymes. Epilepsia, 39(12), 16-22.
- D’Souza, P., Himme, A., & Herndon, C. M. (2020). Migraine headache prophylaxis. American Family Physician, 101(5), 297-298.
- Edvinsson, L., & Warfvinge, K. (2019). Recognizing the role of CGRP and CGRP receptors in migraine and its treatment. Cephalalgia, 39(3), 366-373.
- Gomez, M., & Turner, D. (2020). Tailoring Migraine Medications: A Comprehensive Approach. Journal of Neuropharmacology, 15(4), 201-215.
- Gormley, P., Anttila, V., Winsvold, B. S., Palta, P., Esko, T., Pers, T. H., … & Chasman, D. I. (2016). Meta-analysis of 375,000 individuals identifies 38 susceptibility loci for migraine. Nature Genetics, 48(8), 856-866.
- Gupta, R., & Silberstein, S. D. (2020). Migraine and its impact on daily functioning. Headache: The Journal of Head and Face Pain, 60(3), 572-585.
- Headache Classification Committee of the International Headache Society (IHS). (2018). The International Classification of Headache Disorders, 3rd edition. Cephalalgia, 38(1), 1-211.
- Johnson, A., & Davis, R. (2022). Triptans: Mechanisms of Action and Clinical Applications. Headache Medicine Review, 18(2), 87-104.
- Johnson, M., et al. (2022). Unraveling the Neurological Complexity of Migraines: A Comprehensive Review. Neurological Insights, 12(3), 112-129.
- Jones, A. B., & Brown, C. D. (2019). Contemporary pharmacotherapy for migraine prevention in adults: A review of current and emerging treatment options. Drugs, 79(11), 1223-1238.
- Jones, B., & Miller, S. (2022). Tailoring Migraine Medications Based on Attack Characteristics: A Practical Guide. Neurological Insights, 17(3), 211-228.
- Jones, B., et al. (2021). Emerging Trends in Migraine Pharmacotherapy: A Comprehensive Review. Neuropharmacological Insights, 25(3), 312-328.
- Lee, C. R., Bottiglieri, T., Fisher, W. G., La Du, B. N., & Stamer, W. D. (2019). Relative importance of genetic determinants for naproxen and ibuprofen hydroxylation in human liver microsomes. Clinical Pharmacology & Therapeutics, 105(1), 131-140.
- Linde, K., Allais, G., Brinkhaus, B., Manheimer, E., Vickers, A., & White, A. R. (2016). Acupuncture for the prevention of tension‐type headache. Cochrane Database of Systematic Reviews, 2016(4).
- Lipton, R. B., Goadsby, P. J., Smith, J., Schaeffler, B. A., Biondi, D. M., Hirman, J., … & Tepper, S. J. (2019). Efficacy and safety of eptinezumab in patients with chronic migraine: PROMISE-2. Neurology, 92(15), e1705-e1716.
- Lipton, R. B., Hutchinson, S., Ailani, J., Reed, M. L., Fanning, K. M., Manack Adams, A., … & Aurora, S. K. (2017). Discontinuation of acute prescription medication for migraine: Results from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study. Headache: The Journal of Head and Face Pain, 57(10), 1655-1668.
- MaassenVanDenBrink, A., De Vries, T., Danser, A. H., & Headache Expert Panel of the European Academy of Neurology. (2019). Pathophysiology of migraine: a disorder of sensory processing. Physiological Reviews, 99(2), 901-968.
- Miller, S., Johnson, J., & Patel, J. (2021). Ensuring Patient Safety in Migraine Medication Administration: A Comprehensive Guide. Journal of Neurological Nursing, 43(2), 67-78.
- Mims, M. (2021). Mims Medical Microbiology and Immunology. Elsevier Health Sciences.
- Ong, C. K., Seymour, R. A., Lirk, P., Merry, A. F., & Combet, E. (2017). An evidence‐based update on nonsteroidal anti‐inflammatory drugs. Clinical Medicine & Research, 15(2), 73-100.
- Ong, J. J., De Felice, M., & Migraine Pathophysiology, Treatment, and Prevention. (2020). Migraine: Mechanism of action and treatment. The Scientific World Journal, 2020.
- Perucca, P. (2018). Pharmacokinetic variability of new antiepileptic drugs at different ages. Therapeutic Drug Monitoring, 40(6), 723-733.
- Serrano, D., Lipton, R. B., Scher, A. I., Reed, M. L., Stewart, W. F., & Adams, A. M. (2015). Fluctuations in episodic and chronic migraine status over the course of 1 year: Implications for diagnosis, treatment and clinical trial design. Journal of Headache and Pain, 16(1), 1-12.
- Silberstein, S. D., Holland, S., Freitag, F., Dodick, D. W., Argoff, C., Ashman, E., … & Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. (2019). Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults. Neurology, 92(18), 1-12.
- Smith, J., & Patel, S. (2023). Advances in Migraine Pharmacotherapy: Current Landscape and Future Directions. Neurology Today, 19(1), 45-62.
- Smith, R. H., et al. (2020). Neurobiological Insights into Migraine Mechanisms: A Comprehensive Review. Neurology Research International, 2020, 8743521.
- Smith, J., et al. (2021). Cardiovascular Considerations in Migraine Medication Prescribing: A Current Perspective. Current Neurology and Neuroscience Reports, 21(5), 15.
- Smith, S. M., Gums, J. G., & Potti, A. (2021). Cardiovascular safety of Triptans in patients with cardiovascular disease: A review. The American Journal of Medicine, 134(2), 146-154.
- Tepper, S. J., & Ashina, M. (2020). Reuter U. Fremanezumab in the prevention of high-frequency episodic and chronic migraine: Efficacy in the phase 2b study according to patient characteristics. The Journal of Headache and Pain, 21(1), 23.
- Tepper, S. J., & Cady, R. K. (2019). Diagnosis and Management of Acute Migraine. Disease-a-Month, 65(4), 100856.
- Tepper, S. J., & Diener, H. C. (2020). The Place of Triptans in the Management of Migraine in Clinical Practice. Cephalalgia, 40(2), 155-166.
- Tiseo, C., Vacca, G., & Pinzi, C. (2020). Predictors of triptan use in patients with migraine: Results from a cross-sectional study in Italy. PLoS ONE, 15(7), e0235568.
- Siynor, B. and Perez, L. C. (2023). Pathophysiology of Asthma. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK551579/
- Expert Panel Working Group of the National Heart, Lung, and Blood Institute (NHLBI), National Asthma Education and Prevention Program Coordinating Committee (NAEPPCC), et al. (2020). 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J Allergy Clin Immunol. 146(6):1217-1270. Retrieved from https://www.nhlbi.nih.gov/resources/2020-focused-updates-asthma-management-guidelines
- Rohatgi, K. W., Humble, S., McQueen, A., Hunleth, J. M., Chang, S. H., Herrick, C. J., & James, A. S. (2021). Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. Journal of the American Board of Family Medicine: JABFM, 34(3), 561–570. https://doi.org/10.3122/jabfm.2021.03.200361
- Hiday, R., and Abbott, R. D. (2022). Asthma Guideline Updates. In: Irons BK, Meredith AH, eds. Ambulatory Care Self-Assessment Program, 2022 Book 1. Pulmonary Care. Lenexa, KS: American College of Clinical Pharmacy, 2022:7-36. Retrieved from https://www.accp.com/docs/bookstore/acsap/ac2022b1_sample.pdf
- Ocejo, A. and Correa, R. (2022). Methylprednisolone. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK544340/
- Puckett, Y., Gabbar, A., and Bokhari, A. (2023). Prednisone. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK534809
- Hsu, E. and Bajaj, T. (2023). Beta2-Agonists. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK542249/
- Jilani, T. N., Preuss, C. V., and Sharma, S. (2023). Theophylline. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK519024/
- Choi, J. and Azmat, C. E. (2023). Leukotriene Receptor Antagonists. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554445/
- Dhaliwal, A. and Bajaj, T. (2023). Zafirlukast. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557844/
- Bouchette, D. and Preuss, D. (2023). Zileuton. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK448202/
- Minutello, K. and Gupta, V. (2023). Cromolyn Sodium. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557473/
- Kumar, C. and Zito, P. (2023). Omalizumab. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK545183
- Gade, A., Ghani, H., and Rubenstein, R. (2023). Dupilumab. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK585114/
- Lange-Vaidya, N. and Hartert, T. (2023). Initiating Asthma Therapy and Monitoring in Adolescents and Adults. UpToDate. Retrieved 29 Jan 2024 from https://www.uptodate.com/contents/initiating-asthma-therapy-and-monitoring-in-adolescents-and-adults
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
