Course
Washington APRN Bundle
Course Highlights
In this course we will cover a variety of nursing topics pertinent in the state of Washington. This course is appropriate for APRNs. Upon completion of this single module you will receive a certificate for 30 contact hours including 16 pharmacology hours.
About
Contact Hours Awarded: 30
Pharmacology Contact Hours Awarded : 16
Course By:
Various authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Washington Suicide Prevention Training
Introduction
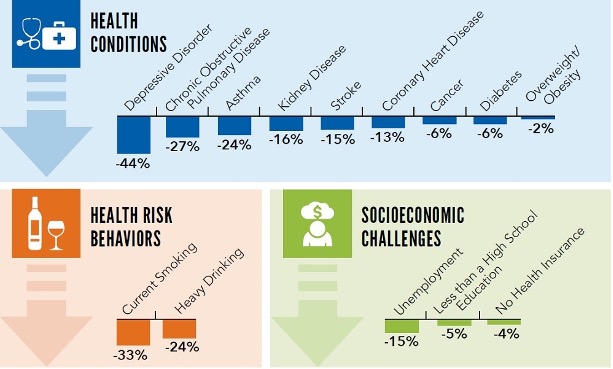
Defined as a harmful act to end one’s own life, suicide is a mental health emergency (25). In 2021, suicide claimed over 48,000 lives in the United States alone. That is approximately 130 individuals daily, and one life every 11 minutes (8). It is reported that in 2021, 12.3 million American adults considered suicide while 3.5 million made a plan, and 1.7 million made an attempt. Of those that complete suicide, 46% had a known or diagnosed mental disorder (23). In comparing this data to other medical conditions, suicide was the 11th cause of death in the United States as reflected in the chart below (5) [See figure 1].
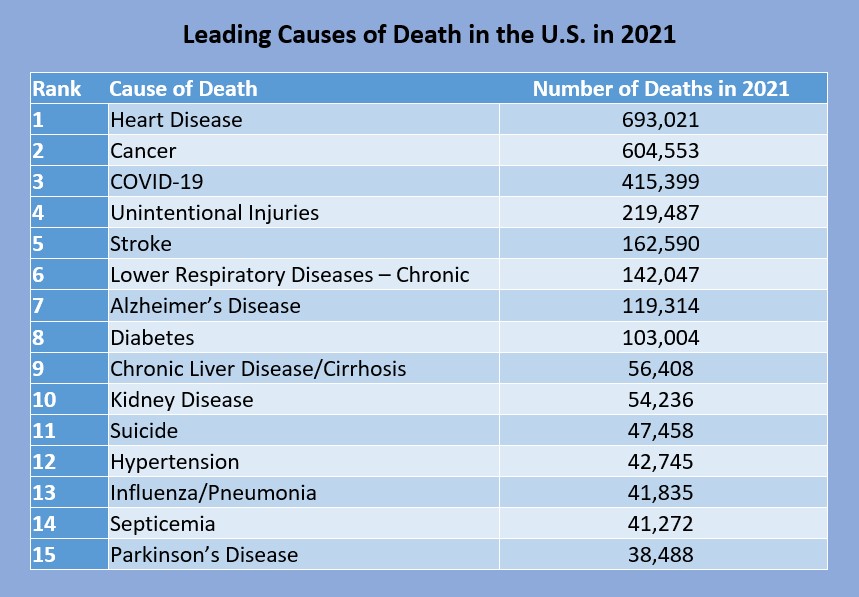
Figure 1: Leading Causes of Death in the U.S. in 2021 (5)
In the United States, Wyoming, Montana, and Alaska all have the highest rates of suicide, over 30 per 100,000 deaths, while New York and New Jersey have the lowest, 7.9 and 7.1 per 100,000 deaths respectively (7). Washington state ranks 27th on this list with 1,229 deaths or 15.3 in the year 2021 (7). Age wise, those 85 years and older had the highest rate of suicide in 2021 at a rate of 22.4 per 100,000. Chart 2 reflects suicide rates among Americans aged 10 to 85+ (7) [See figure 2]. Race and gender must also be considered when discussing suicide. Chart 3 discusses suicide rates based on race [See figure 3], while Chart 4 discusses rates by gender [See figure 4].
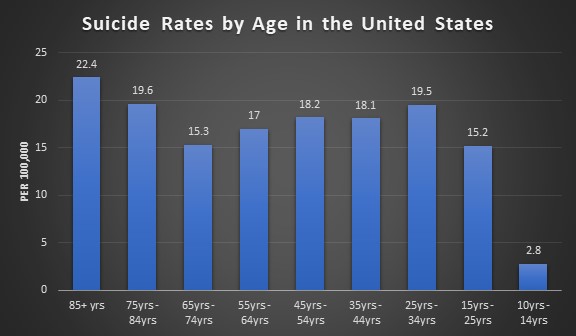
Figure 2: Suicide Rates by Age in the U.S. (7)
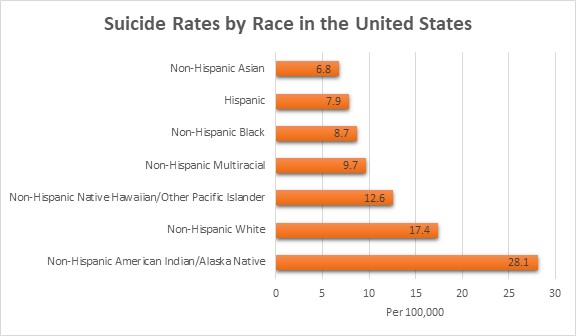
Figure 3: Suicide Rates by Race in the U.S. (7)
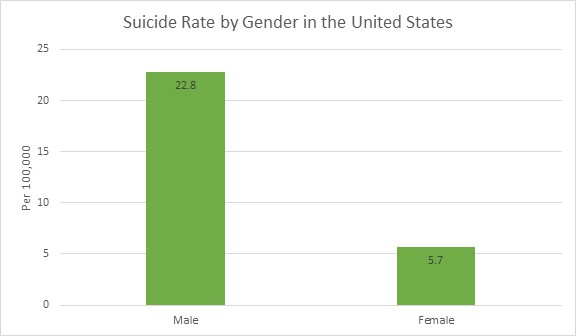
Figure 4: Suicide Rate by Gender in the U.S. (7)
Suicide is a leading cause of death on a global level with more deaths than human immunodeficiency virus (HIV)/ acquired immunodeficiency syndrome (AIDS), breast cancer, war, homicide, or malaria. The World Health Organization reports that an estimated 703,000 individuals die from suicide each year, approximately one in every 100 individuals. However, this number could be higher due to the COVID-19 pandemic and risk factors that were exacerbated during the pandemic: isolation, anxiety, loss of job, and financial stress (40).
Low and middle income countries see higher rates of suicide at approximately 77%. Within the past 45 years, the global suicide rate has increased 60%. For those ages 15 to 29, suicide is the fourth leading cause of death—behind road death, tuberculosis, and interpersonal violence—with it being the third leading cause of death in females and the fourth in males (40).

Self Quiz
Ask yourself...
- Looking at the data above, what can you deduce about suicide and demographics?
- What factors could lead to these numbers being incorrectly reported?
- Was there any information that you did not expect or know? Why was it surprising to you?
- Do you disagree with any of the data above? What is your rationale?
- What countries do you think have the highest rates of suicide based on the information above?
- What other information do you think is important to collect when gathering data on suicide?
Terminology
Using proper definitions to clearly understand what is being discussed is important when discussing suicide. Providers may use certain words or phrases and mean different things. By having clear definitions that are universally used, providers can understand what other providers are conveying and continue care in an appropriate manner. Below is a list of commonly used terms when referring to suicide.
|
Term |
Definition |
|
Suicidal Ideation |
Thoughts regarding killing oneself or ending one’s life. This can include planning. |
|
Suicide Attempt |
Non-fatal self-injurious behavior with the intent to kill oneself. |
|
Suicide Intent |
Intention to kill oneself by acts of suicidal behavior. |
|
Suicide Behaviors |
A spectrum of behaviors that ranges from planning to attempting/preparing to completing suicide. |
|
Suicide |
Fatal self-injurious behavior to end one’s life. |
|
Suicidality |
A spectrum of possible suicidal events. This does not cover if there was suicidal ideation or attempt or if the ideation or attempt is chronic or acute in nature. It is encouraged that when discussing a patient, clearly cover the actual concerns at hand. Does your patient have ideation, or did they attempt to end their life? |
|
Suicide Threat |
Verbalized thoughts of killing oneself through self-injurious behavior. This is to lead others to think the individual making these statements wants to die without the actual intent to do so. “If you breakup with me, I will kill myself.” |
|
Suicide Gestures |
Self-injurious behavior that makes others think that the individual making these gestures wants to kill themselves, despite them having no intent to. |
|
Non-Suicidal Self-Injurious Thoughts |
Thoughts of partaking in self-injurious behavior that includes deliberate damage to body tissue without an intent to die. |
|
Non-Suicidal Self-Injury |
Self-injurious behavior with deliberate damage to body tissue without an intent to die. |
|
Physician-Assisted Death or Suicide; Aid in Dying; Right to Die |
Passive – a provider supplying the patient with medications to take on their own to end their life |
Table 1: Commonly Used Terms When Referring to Suicide (11, 21, 29)
Suicide Assessment
Healthcare providers perform a variety of assessments on their patients: cardiac assessment, respiratory assessments, neurological assessments, etc. Just as those assessments help providers decide what treatment needs to be done, the suicide assessment is utilized to evaluate a variety of factors that can increase an individual’s risk for suicide.
The latest guidelines from the American Psychiatric Association have clear goals of the suicide assessment: (17)
- Identify any psychiatric signs and symptoms
- Assess past suicidal behavior
- Review any available past treatment
- Determine if there is a family history of suicide or mental illness in the family
- Identify the patient’s current psychosocial situation and the cause of the current crisis
- Recognize strengths or coping skills and any opportunities for improvement that the patient has
With the suicide assessment, there are five areas of questions that the American Psychiatric Association discusses with examples as to what is being looked for in each area (17). These areas can be found below:
|
Current Presentation of Suicidality |
|
|
Psychiatric/Mental Illness |
|
|
Patient History |
|
|
Psychosocial Information |
|
|
The Patient’s Strengths and Weaknesses |
|
Table 2: American Psychiatric Association Suicide Assessment (17)

Self Quiz
Ask yourself...
- What goals would you add to the American Psychiatric Association’s list of goals for the suicide assessment?
- Do you think these goals accurately cover suicide assessments? Why or why not?
- Which of the five categories in the suicide assessment do you think is the most important to cover? What is your rationale?
- Are there any questions you would remove or add to the list above?
- If you could create a sixth category, what would it entail?
The Interview: Gathering Information
Conducted in a private place, the suicide assessment is an interview of the patient. Providers must ensure that they ask the right questions based on information provided to them by the patient or those that are accompanying the patient. Empathy, compassion, and trust must be integrated in these interviews. Below is a list of questions that can be used during the interview process. It is important to follow your facility’s specific policies and procedures regarding the suicide assessment and use the proper screening tools. Some common screening tools utilized in healthcare will be discussed later.
|
Open Ended Questions |
In your life, have you ever felt as though your life was not worth living? Have you ever wished to go to sleep and not wake up? |
|
Follow Up Questions |
Have you been thinking about death recently? Has there ever been a point where you have considered harming yourself? |
|
Thoughts on Suicide or Self-Harm |
|
|
Previous Suicide Attempts |
|
|
Repeated Suicide Attempts and Thoughts |
|
|
Psychosis |
|
|
Harm to Other Individuals |
|
Table 3: Suicide Assessment Interview Questions (17)
It is important to keep in mind that the answers to these questions are self-reported, so patients may not be honest for any reason. Providers should pair answers given during the interview with objective data they collect through observation and past medical records. Family, friends, and partners can be a source of information; however, providers should consider collecting information with these individuals separately.

Self Quiz
Ask yourself...
- Does your facility have a policy for suicide screening? If so, do you think the policy is effective? Why or why not?
- What methods have you found to be beneficial to asking the above questions?
- What methods are detrimental to asking the questions above?
- What specific questions do you think could be added to the above list?
- How could you rephrase the questions when talking to a family member or friend about the patient?
- What questions, when given the answer “yes”, would warrant more investigation on your part as a provider?
Columbia-Suicide Severity Rating Scale:
Also known as the Columbia Protocol, the Columbia-Suicide Severity Rating Scale was created by Columbia University, University of Pittsburgh, and University of Pennsylvania to be used during a 2007 National Institute of Mental Health study to decrease the suicide risk in adolescents with depression. The Centers for Disease Control and Prevention began using this protocol and recommending it be used in data collection in 2011. The next year, the Food and Drug Administration stated the Columbia Protocol was the standard for measuring and assessing suicidal behaviors and ideation in clinical trials (33).
The Columbia Protocol is used to assist providers and laypersons in determining if an individual is at risk for suicide. These questions are worded in plain language to ensure this scale can be administered by anyone, regardless of profession. This scale questions individuals about the following information: (33)
- If and when they have had any suicidal ideation or thoughts
- Any action they have taken to prepare for suicide and when they have done so
- If they have attempted suicide or started a suicide attempt that they interrupted or someone else did
The image below [See figure 5] is the six-question Columbia Protocol that can be used by anyone in assessing suicide risk. The far-right column is color coded based on severity if they answer “yes” to the question. Yellow is low-risk, orange is medium-risk, and red is high-risk. The answers the individual gives will guide the interventions needed. If the individual answers “yes” to questions two or three, behavioral healthcare should be sought out. If the individual answers “yes” to questions four, five, or six immediate help is needed. Those asking the questions should call the suicide and crisis lifeline, 911, or take the individual to the nearest emergency department. The individual should not be left alone until an evaluation has been done (33).
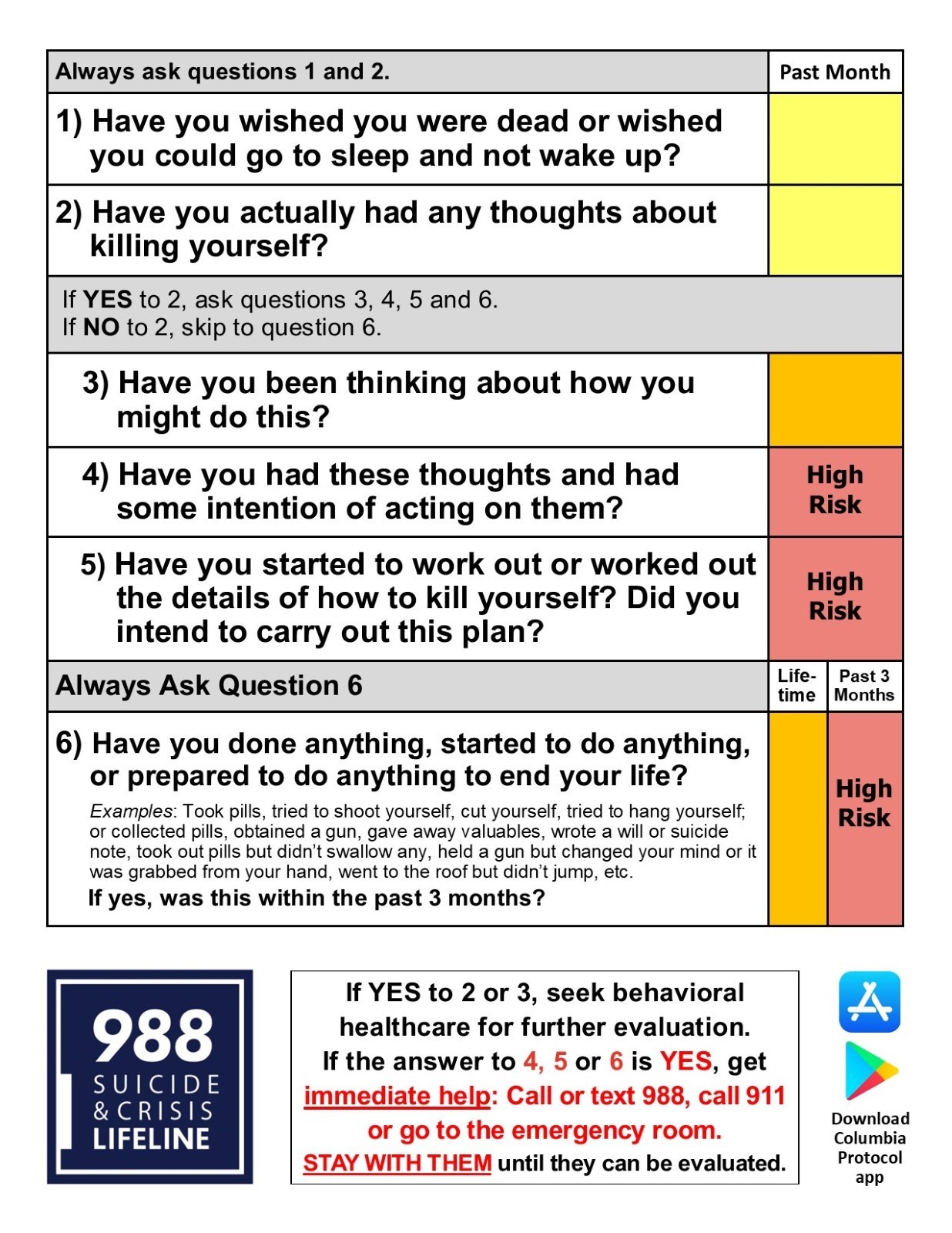
Figure 5: Columbia-Suicide Severity Rating Scale (Columbia Protocol) (33)
Suicide Assessment Five-step Evaluation and Triage:
The Suicide Assessment Five-step Evaluation and Triage consists of five questions that identifies risk and protective factors, risk levels and interventions, suicide inquiry, and documentation of treatment plans. This tool was created by Douglas Jacobs, MD, the physician who assisted in creating the suicide assessment published by the American Psychiatric Association (31). The five questions include:
- Identify risk factors with attention to those that can be modified.
- Identify protective factors and those that can be enhanced.
- Complete a suicide inquiry by asking about thoughts, plans, intent, and behavior.
- Determine risk level and any interventions that are appropriate for the risk level and attempt to reduce risk.
- Document as appropriate to include risk and rationale, interventions, and any follow-up that is needed.
The Suicide Assessment Five-step Evaluation and Triage can be combined with the Columbia Suicide-Severity Rating Scale (C-SSRS) to expand on the benefits of both tools (34).
Questions one through six from the C-SSRS all have an option for “yes” or “no,” If question two is a no, questions three through five can be skipped. After the C-SSRS questions have been asked, further assessment can be directed to precipitating events, clinical status presentation/statements, past treatment history, and any other relevant information. Providers also want to assess for access to lethal means by asking specifically about the presence of firearms in the home or how easy it would be to obtain a firearm (34).
The next step is to identify protective factors the individual has. These can be internal or external factors that the individual has that can provide support. Internal factors can consist of fear of death, or reasons for living while external factors can consist of responsibility to family or friends, supportive social network, or interacting and engaging at work and/or school (34).
Step three is the C-SSRS Suicidal Ideation Intensity screening questions that consists of thoughts, plans, and suicidal intent. Questions focus on frequency of thoughts, duration of how long the individual has had these thoughts, controlling the thoughts, if there is anything that the individual can do to deter the thoughts, and the reason for the suicidal ideation (34).
Ask Suicide-Screening Questions
The Ask Suicide-Screening Questions consists of the Suicide Risk Screening Tool that can be administered in the emergency department, inpatient medical unit, outpatient, primary care, or specialty provider offices as well as schools and juvenile detention centers. All questions are “yes” or “no” with additional open-ended questions if the individual answers “yes” (24) [See figure 6].

Figure 6: Ask Suicide-Screening (24)
The answers provided will guide treatment/interventions. If the individual answers “no” to questions one through four, no intervention is needed. If they answer “yes” to any of the questions, question five must be asked since the individual is said to have a positive screen. If question five has a “yes” response, an imminent risk is identified, or they are an acute positive screen. The patient needs a safety or full mental health evaluation before they are able to leave. Immediate interventions that must be considered are keeping the patient in eyesight at all times, removing items that could be used to harm/kill self or others, notify the provider that is responsible for the individual’s care (24).
You may wonder what to do if the individual answers “yes” to any of questions one through four but does not answer “yes” to question five. This means the individual is a non-acute positive screen and there is a potential risk identified. A brief suicide screen must be done in order to determine if a full mental health evaluation needs to be completed. The individual is not allowed to leave until they have been assessed for safety, and the provider must be notified (24).
Depending on where the individual is when asking these questions, there are some additional questions that need to be asked regarding safety and safety plans. The links below will take you to the safety screening tools based on the location of the individual being assessed (24).
Emergency Department Suicide Safety Assessment
Outpatient, Primary Care Provider, Specialty Provider Office
Patient Health Questionnaire
Since depression is often a risk factor for suicide, the Patient Health Questionnaire (PHQ-9) is used to measure, screen, monitor, and diagnose depression severity. This screening utilizes diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders 4th edition and rates the frequency of the individual’s symptoms. Question nine focuses on the presence and duration of suicidal thoughts while a non-scored question assigns and screens how much depression is affecting the individual’s activities of daily life and function. The minimum score is five while the maximum is 27. Anything greater than 20 has a provisional diagnosis of major/severe depression with a treatment recommendation of antidepressants and psychotherapy (27) [See figure 7]

Figure 7: Patient Health Questionnaire (PHQ-9) Results Interpretation (27)
The screening answer options include: not at all = 0, several days = 1, more than half the days = 2, and nearly every day = 3. The questions are as follows: (27)
- Little pleasure or interest in doing things
- Feeling hopeless, depressed, or down
- Difficulty sleeping, staying asleep, or sleeping too much
- Having too little energy or feeling tired
- Overeating or a poor appetite
- Feeling bad about yourself, or that your family sees you as a failure or that you have let them down
- Having difficulty concentrating on things, like reading a book or watching a movie/television
- Either being too fidgety or restless or moving/speaking slowly that you and/or others notice
- Thoughts that you would be better off dead or thoughts of hurting yourself
- Non-scored question: If you selected any of the above problems, how difficult have those problems made it for you to complete work, get along with family, friends, or manage things at home? (Answers options include: not difficult at all, somewhat difficult, very difficult, extremely difficult).

Self Quiz
Ask yourself...
- What other suicide screening or assessment tools have you seen utilized?
- Is there a specific tool you prefer? Which one and why?
- Have you heard of any up and coming assessment tools that may be more effective than the ones listed here? What is the name of the tool and what does current research show?
- Would you feel comfortable using these assessment tools on friends or family you are concerned about? Why or why not?
- If you did assess a family or friend for suicide and it was positive, how would your reactions vary than if you performed the same assessment on a patient?
Suicide Risk, Protectives Factors, and Warning Signs
Risk factors for suicide can appear in a variety of ways: individual, relationships, community, society. These are factors that increase an individual’s risk for suicide through different means. For example, stay at home orders and quarantining during the initial phases of the COVID-19 pandemic led to isolation, which is a risk factor of suicide. Combining this with other risk factors increases the chance of an individual taking action to end their life (6).
|
Characteristic |
Low Risk |
High Risk |
|
Gender |
Female |
Male |
|
Age |
Less than 45 years old |
Greater than 45 years old |
|
Marital Status |
Married |
Widowed or divorced |
|
Interpersonal Relationships |
Stable |
Unstable/Conflict |
|
Employment |
Employed |
Unemployed |
|
Background of Family |
Low substance use, family feels healthy, they have good health |
Excessive substance use, hypochondriac, chronic illness |
|
Mental Health |
Normal personality, social drinker, neurosis, mild depression, optimistic |
Severe personality disorders, substance abuse, severe depression, hopelessness, or psychosis |
|
Physical Health |
Low substance use, individual feels healthy, has good health |
Excessive substance use, hypochondriac, chronic illness |
|
Suicidal Ideation |
Low intensity, infrequent, transient |
Prolonged, intense, frequent |
|
Suicidal Attempt |
Impulsive, first attempt, wishing for change rather than the wish to die, low lethality method, has external anger, rescue is inevitable |
Multiple attempts, planned out, has a specific wish to die, is self-blaming, done with lethal methods, has a specific wish to die |
|
Personal Resources Available |
Controllable, has good achievement, is insightful |
Has poor achievement, unstable affect, has poor insight |
|
Social Resources Available |
Has good rapport, they are socially integrated, has a concerned/supportive family |
Are socially isolated, family is unsupportive/unresponsive, has a poor rapport |
Table 4: Criteria for Low and High Suicide Risks (3, 4)
Gender
Per research, men are four times as likely to die as a result of suicide as opposed to women. This is regardless of religion, marital status, or race. However, women are three times as likely to have thoughts of suicide and/or attempt suicide than men. Research deducts that this is because the differences in attempt methods between women and men (3). Studies show that 30% of transgender youth in the United States have attempted suicide in their lifetime while 40% of adults who identify as transgender have attempted (15).
Age
Suicide rates increase with age. Individuals who have not gone through puberty are very unlikely to attempt or die by suicide as opposed to those that have gone through puberty. Age 45 is when suicide rates are the highest among men while it is highest in women after 55. Those over the age of 65 or who are considered elderly are less likely to attempt suicide, but they are more successful when they make an attempt. As we pointed out earlier, suicide is increasing among the young population: it is the third leading cause of death among individuals aged 15-24 (3).
Marital Status
Individuals who are married and have children have a lesser likelihood than their single counterparts. Those that are single or never married have a risk two times higher than those that are married (8). Divorce suicide rates in men are three times more than women. Some individuals may attempt or die by suicide on the anniversary of a loved one’s death (3).
Sexual Orientation
Homosexual and heterosexual individuals have differences in suicide rates. Those that identify as homosexual, regardless of marital status, do have higher rates of suicide (3).
Race/Ethnicity
Caucasian individuals, regardless of gender, are three times more likely to die by suicide as opposed to African Americans. Young Alaskan Natives or Native Americans have higher than the national average rates of death by suicide (22). Moving on to immigrants, the rates are much higher than citizens of the United States (40).
Religion
Many religions have negative views on suicide. Despite that, religious groups such as Protestants and Jews have higher rates of suicide than Muslim and Catholics combined. It is important to note that religion alone is not an accurate indicator of suicide, but the inclusion and societal integration and beliefs are better predictive factors (3).
Occupation
Increases in socioeconomic status increase the risk of suicide in any individual. It is noted that being employed is one protective factor, and while true, there are some occupations that increase the risk. Lawyers, healthcare providers, mechanics, artists, and insurance agents are classified as high-risk occupations. On the other hand, unemployment brings an increased risk of suicide in comparison to those that are employed. Providers should be aware that suicide risk increases during economic depressions and decreases during economic booms (3).
Physical Health
Good physical health is vital to good mental health and wellbeing as poor physical health contributes to at least half of all suicides. Thirty percent of those who died by suicide saw a provider within the past six months prior. Physical effects that increase risk factors include disfigurement, loss of mobility, and chronic pain. If these effects impact the individual’s relationships and/or work life, that can increase suicide risk even more (3).
Mental Health
Almost 95% of those who die by suicide have at least one diagnosed mental health disorder. Depressive disorders like major depressive disorder account for 80% of all suicides, and a diagnosis of delusional depression comes with the highest risk of suicide. Those with schizophrenia have a 10% risk, while those with delirium or dementia have a 5% risk of suicide. Alcohol dependency is found in over one fourth of suicide cases (3).
Substance Abuse
As mentioned earlier, alcohol or other substances can play a large factor in suicide. The use of any substance can lead to impairment of judgement, sedation, or manic behavior that can lead to respiratory depression or self-injury (19).
If there is a suspicion of substance abuse, it is important to consider discussing these concerns with patients in a non-threatening, non-judgmental manner (19). Providers should start with questions regarding socially acceptable habits: exercise or dieting, caffeine, and tobacco can help ease the patient into comfort. This is something that should be done as standard procedure for all patients, and providers can even say that to patients. “We ask these questions to everyone.” Providers need to ask questions such as “how many”, “how much”, “how often” to any “yes” answer the patient provides (37). Below are common substances that are abused:
- Alcohol: While alcohol is legal to consume for those over the age of 21 in the United States, patients may still be hesitant to answer truthfully. Providers must take patients at their word but make note of any objective data that they gather through their assessment. Appearances of patients who may have a substance abuse disorder will be discussed later. It is important to ask about specific alcoholic beverages as some cultures may not consider beer or wine to be alcohol (37).
- Over-the-counter medications: These medications can be a source of intentional or unintentional substance abuse, so providers must ensure that they are asking about herbal supplements, cold and cough medications, or diet aids. Prescription medications might be prescribed to the patient or someone else and usually consists of sleeping aids, pain medications, diet medications, or attention deficit (hyperactive) disorder medications (37).
- Cannabis/Marijuana: Cannabis or marijuana use has various levels of legality in states across the United States, so providers should be aware of their state’s rules and regulations regarding its use. Regardless, it is important to screen for usage during any patient interaction as treatments can be affected (37).
- Illicit Drugs: Illicit or street drugs consist of cocaine, heroin, methamphetamine, inhalants, hallucinogens, and more. Asking about use of the substances is important, and again should be done in a non-judgmental manner. Methods include saying the name of each substance as opposed to calling them illegal or street drugs are a great way of doing this. Providers need to assess the amount, method of usage, if patients are doing these substances with someone who they consider safe, if they have access to Narcan, if they are buying from the same person, and if they are sharing needles, or using dirty or clean needles (37).
Knowing the patient’s own view of their substance use can be very helpful. If the patient does not see their usage as a problem or reason for concern, they are less likely to seek out help or accept it. The same goes for consequences (19). Below is a table of tools providers can use to screen for substance abuse in adults and adolescents (32) [See figure 8].

Figure 8: List of Substance Abuse Screening Tools for Adults and Adolescents (32)
As mentioned above, patients may not be completely honest when providing substance use history. Providers need to collect both subjective and objective data to assist them in providing the proper care.
Patients may vocalize thoughts of continuously thinking about the substance they are using. They might forget things or have a hard time focusing or concentrating. If they are aware or know they are abusing a substance, they may be unable to stop regardless of a physical and/or mental challenge that is a result of the substance (19).
There may be reports of strong cravings to use the substance. Patients may report a desire to decrease use of the substance, stop using it all together, or they may take actions to obtain the substance that leaves them feeling guilty or remorseful. Depending on the substance used, the patient may report changes in mood or mood swings (19).
Behaviors may vary from patient to patient, and the type of substance they are using. They may dedicate extensive amounts of time to obtain the substance, neglect important tasks or individuals within their lives, or actively appear intoxicated. They may argue or get in trouble with family, friends, or law enforcement. They may take the substance when it is hazardous to the health and safety of themselves and others. They may also start taking the substance in higher doses for longer than recommended (19).
The physical appearance of the patient can consist of noticeable changes in weight, bloodshot eyes, increased tolerance for a particular substance, constricted or dilated pupils, or irregular sleep patterns. Patients may also have signs of withdrawal that consist of shakiness, sweating, agitation, headaches, nausea and/or vomiting, fatigue, and possibly seizures (19).
Stigma
Stigma is known as negative thoughts that are held towards other individuals, groups, or circumstances (19, 30). Usually stigma stems from differences. Differences can encompass any part of life, ranging from clothing to gender to race to medical or mental health diagnoses. Stigma impacts how society addresses those differences. If most of society sees mental health and suicide as shameful, those that have mental health diagnoses or have attempted/thought of suicide may be less likely to seek help—this is social stigma. Those with mental health diagnoses may have self or perceived stigma. These individuals internalize society’s opinions or their own perception of discrimination (30).
Traumatic Childhood
Traumatic childhood events such as sexual abuse are directly linked to increased risks of suicide or suicide attempts. It is vital that healthcare providers assess children and adults for this history to assist with appropriate treatment and support in order to decrease risks and guide the individual to recovery (19).
Genetics
Recent studies have discovered a locus in the form of a DNA variation on chromosome seven that can increase an individual’s risk for suicide. Other variations in this region can lead to risk-taking behaviors, smoking, and insomnia. This variation was present even after “conditioning on major depressive disorder.” The locus has been deemed to be independent from psychiatric diagnoses as well, meaning that those without a mental health disorder could still be at risk for suicide attempts or suicide if this variation is present (22).
General/Other Risk Factors
There are other general risk factors that can impact an individual and their risk for suicide. The Centers for Disease Control and Prevention rank these risks from individual risk factors to societal risk factors and describes them: (6)
- Individual Risk Factors: serious or chronic illness such as chronic pain, previous attempts of suicide, criminal and/or legal problems, substance use, history of mental illnesses like depression, feelings of hopelessness, job or financial loss or problems, current and/or prior history of adverse childhood experiences, and victim of violence or perpetration.
- Relationship Risk Factors: family or loved one having a history of suicide, social isolation, loss of relationship, bullying, and violent or high-conflict relationships.
- Community Risk Factors: stress of acculturation, historical trauma, violence in the community, discrimination, lack of access to healthcare, and cluster of suicide within the community.
- Society Risk Factors: stigma regarding seeking help for mental health or mental illness, unsafe/inaccurate medical portrayal of suicide/self-harm, and access to lethal means in populations at risk for suicide.
Protective factors are those that improve mental health and provide support to the individual. These can range from individual to societal levels of protection. It is important to know that everyone can participate in preventing suicide within their relationships, communities, or society through equal support (6). Below are some protective factors: (6)
- Individual Protective Factors: strong sense of culture, reasons for living (like friends, family, pets, etc.), effective coping skills, and effective problem-solving skills.
- Relationship Protective Factors: partner, family, and friend support, and having or feeling a connection to others.
- Community Protective Factors: feeling a connection to school, work, or community, and having consistent and high-quality mental and physical healthcare.
- Society Protective Factors: reducing the access and availability of lethal means to those that are at a higher risk of suicide, and religious, moral, or cultural objection to suicide and/or suicide attempts.
Case Study Reflection
Below is a case study divided into three parts. This case study will take you through a scenario and ask questions about what should or should not be done with this patient based on the information that has been covered so far (6).
Case Study Reflection 1
Noelle has lived in your neighborhood for years and is one of your favorite neighbors. She would sometimes watch your children when they were young and worked as a waitress until she retired recently. She mentioned to you once, shortly after her retirement, that her funds are “not what they used to be” as she is relying on her social security’s fixed income. This forces her to budget more than she ever needed to, and she is contemplating finding a job. However, her knee pain has been getting worse, keeping her from moving around and sleeping. You notice she doesn’t garden like she used to. One day when you stop by, you ask her about her children, who you have not seen visit. She tells you they are busy, but she would like to see them because she is lonely. She appears restless and sullen.

Self Quiz
Ask yourself...
- What are some of the factors that put Noelle at an increased risk for suicide?
- What follow-up questions could you ask her?
- Is there anything concerning you at this moment? Why or why not?
- Would you want to use any of the suicide assessment tools listed in the course at this time? What is your rationale?
- What are your next steps to help Noelle and possibly decrease her risk of suicide?
A few days later, you realize you have not seen Noelle outside of her house, nor have you seen her two dogs. Since you know her children, you call the older son to reach out and see if he has spoken with his mother. The son sounds rushed on the phone and says they only talked for a few minutes the day before. Deciding to call Noelle yourself, you are surprised that she answers the phone. She again reiterates that it is hard for her to move and leave the house because of her knees and age. She says that she is lonely. You state you would like to check on her every day for a few days, but she adamantly declines. “I just get irritable around people,” she tells you.

Self Quiz
Ask yourself...
- Would you say that Noelle is better or worse than before? What evidence do you have to support your answer?
- How could you intervene to offer Noelle support?
- Who else could you get involved with when it comes to ensuring Noelle’s safety?
- Would you like to perform a suicide risk assessment on Noelle? Which one would you use?
- Do you think Noelle needs to be assessed by a trained professional? If yes, what provider do you think would be helpful?
The day after your conversation with Noelle, you go to check on her as you are still concerned. When you knock on the door, no one answers, but you know someone is home because of the noises coming from the house. You are able to enter her house through the patio, something she had given you permission to do in the past, and you can now hear her dogs barking continuously. After calling for Noelle and not receiving an answer, you head upstairs to her room. You find Noelle in bed with an empty bottle of prescribed pain medication that she uses for her knees. She seems to be “out of it” but is crying and muttering that she “can’t do this anymore.”

Self Quiz
Ask yourself...
- What is your first priority with providing care for Noelle?
- What information should you provide to first responders when they arrive on scene?
- Looking back on the situation, is there anything that could have been done differently by all parties involved to prevent Noelle from getting to the point where she attempted to take her life?
- What can you and your other neighbors do for Noelle while she is being evaluated?
- Are there any support methods you can offer Noelle when she returns home?
Non-Suicidal Self-Injury
As discussed earlier, self-injury can either be non-suicidal or suicidal in nature. Those who perform non-suicidal self-injury are not looking to end their lives, but instead are trying to escape emotions, thoughts, or other feelings that are causing distress (i.e., not being good enough; feeling anguish, despair, desperate, or depressed; needing a way to relieve stress; believing that people do not care). Physical pain is created through a variety of means, including cutting, burning, biting, scratching, pulling out hair, kicking or punching objects to injure self, or snapping rubber bands on their bodies (19).
To determine if the injury is related to a suicide attempt or not, providers must perform a suicide assessment and discuss actions and behaviors with the patient in a non-judgmental manner. It is important to remember that non-suicidal self-injury is a coping mechanism for individuals, and it may be the last coping mechanism available before an individual makes a suicide attempt. Providers need to refrain from preventing self-injurious behavior until they provide the patient with other coping mechanisms. Always follow facility policy and procedures when addressing non-suicidal self-injury (19).

Self Quiz
Ask yourself...
- What methods of non-suicidal self-injury have you seen individuals use?
- How did you assist these patients in gaining better coping skills?
- What barriers did you face?
- Were there any successes in helping the patient(s) gain better coping skills?
- What recommendations would you give others trying to help their patients refrain from non-suicidal self-injury?
- Are there any reasons you think someone would not want to stop their behavior?
Understanding the Risk of Suicide: Using Assessment Information
As discussed, suicide has many risk factors, one of which is past suicide attempts. Studies have shown this correlation to be more serious than previously thought, with higher rates of a second attempt within the first three months of the first attempt. What does this mean? As providers we should be providing more support during that initial post-attempt phase to ensure patients have better coping skills and resources to decrease the chances of another attempt.
The provider must look at a variety of factors gained during the suicide assessment interview such as any previous self-harming behaviors, suicide attempts, and/or aborted attempts (stopped by themselves or someone else). If you are not the patient’s regular provider, consider consulting their primary care provider or psychiatric provider to assess past history of suicide (3).
Previous hospitalizations for suicide attempts and/or past psychiatric treatment provides important information to the provider that they should be aware of. Consulting with the patient, family, or friends can provide valuable insight into the patient’s history and coping skills (3). Patients may have a history of agitation, anxiety, depression, feelings of hopelessness, changes in mood (which can be severe), insomnia, or substance use (19).
Family history and dynamics can impact a patient and be a factor for suicide, either a risk or preventative. Dysfunctions within the family have a direct link to suicide and self-injurious behaviors. Providers should ask about family history regarding mental health and illnesses as well as family dynamics. Separations, family history of substance abuse, legal or financial trouble, abuse, or domestic violence should be documented and reported as required by law (3).
Assessing the patient’s presentation at the time of the interview is vital and can provide significant objective data on the patient’s psychological status. Providers should ask questions about current stressors in their lives: financial hardships, interpersonal loss, or changes in their economic status. As already discussed, loss of job or residence, family dynamics, religious beliefs, and cultural customs can impact the patient as well (3).
Determining strengths and areas for improvement will guide the provider in providing support, treatment, and referrals as care progresses. These traits may include coping skills, support (from family, friends, religion, or community), personality, and methods of thinking or solving problems. It is important that patients are guided to adjust their thought processes, such as mentalities and self-expectations, that can be detrimental to mental health (3).
Case Study Reflection 2
Marc is a new patient at your organization, who recently relocated to Washington from Wisconsin for a new job. He has moved to your city with his wife and young children. While talking with Marc, you can tell that the move has not been easy on him while his family seems to be settling in well. He makes a comment about “feeling inadequate at work” because everyone has expectations for him despite the fact that he is new to the company and role. He reports that he does not feel a sense of community where he lives, saying that the city he came from was much friendlier and warmer.
You note that Marc does not mention any current coping skills, but you do identify that he used to bike-ride to de-stress after work. The environment is different for him, and he has different work hours with the new position, making it challenging for him to find time or energy to bike. Marc says he thinks that relocating was not the right decision for his family as he has barely any time for them and less time for himself. He says he is a failure.

Self Quiz
Ask yourself...
- What is your priority when assessing Marc? What is your rationale for that decision?
- Are there any additional questions you would like to ask Marc?
- What are some of Marc’s strengths?
- What areas for improvement do you see in Marc?
- What are at least three coping mechanisms that Marc can use or develop to assist him during this transition?
- What are other coping strategies that Marc could develop?
Suicide Risk: Documentation
Documentation of the patient’s suicide assessment is a vital part of the provider’s job. Based on the hospital or facility’s policies, providers might document a suicide risk assessment each time they encounter the patient. Ensure that you are following proper policies and procedures regarding when a suicide risk assessment should be documented. Some best practices include documenting during the first inpatient hospitalization or the initial psychiatric assessment, when there is a significant change, and when there is an occurrence of suicidal ideation or behavior (3).
Providers should consider documenting the following: (3)
- Any changes in treatment
- Risk assessments
- Prescription medications
- Previous treatments, especially regarding past suicide attempts
- Decision making processes
- Conversations with other providers
- The patient’s access to firearms
Actions and Referrals for the Various Levels of Suicide Risk
Patient statements and actions guide the actions and steps a healthcare provider must take. If a patient has attempted suicide, admission to a hospital to treat any medical injuries is the first step, followed by admission to an inpatient behavioral health unit or hospital. Some facilities may have psychiatrists or clinical psychologists see the patient when they are on the medical floor, so both types of treatments can occur simultaneously. Individuals who may benefit from an inpatient psychiatric admission include those who have acute suicidal ideation with previous attempts, previous suicide attempts with no suicidal ideation (but has other psychiatric concerns), or an exacerbation of a mental illness. Individuals who would benefit from outpatient services include those with suicidal ideation or strong support systems (3).
|
Treatment |
Characteristics |
|
Inpatient Treatment – Required |
After an aborted suicide attempt or suicide attempt if:
|
|
Inpatient Treatment – Might be Considered |
If there is a presence of suicidal ideation along with:
|
|
Outpatient Treatment – Recommendation |
Post suicide attempt, or the patient has suicidal ideation or a plan:
|
Table 5: Suicide Attempt Criteria for Recommended Treatment Services (3)
While some patients may agree to inpatient treatment after a suicide attempt, others may not. The state of Washington has an Involuntary Treatment Act that manages the psychiatric hold. For additional information, review Title 71.05 of the Revised Code of Washington (39).
Per Washington legislation, any individual that has firsthand knowledge of an individual they are concerned about can refer them for an evaluation that must be completed by a trained professional such as a psychiatric nurse practitioner or a psychiatrist. The following two points meet the criteria for involuntary admission: (39)
- The individual must have a diagnosed or diagnosable mental health disorder. This is defined as an organic, emotional, or mental impairment that severely impacts the individual’s volitional or cognitive behavior.
- They present with harm to others, property, or self, or the patient is classified as gravely disabled (unable to care for themselves safely).
The trained mental health provider can make a determination if the patient meets the criteria, and if they do, they can initiate a 72-hour involuntary hold. After this hold is initiated, the patient will be transferred to a psychiatric hospital or receiving facility to receive the appropriate treatment. It is important to remember that patients under these holds still maintain their individual rights while in the facility and are presumed competent. This places the patient in a confidential status (39).
Once the 72 hours have passed, the patient can request legal counsel and be evaluated by the court if they continue to refuse voluntary treatment. Psychologists typically evaluate the patients by performing independent exams to determine if the patient still meets the criteria for involuntary placement. The patient and the legal counsel (who is representing the patient) will meet and discuss the patient's desires in a Probable Cause Hearing (39).
In this meeting, the judge will determine if there is probable cause for the patient to continue treatment on an involuntary placement. During the hearing, the following four decisions can be made (39):
- Involuntary petition is dropped, and the patient is released.
- The case is dismissed by the judge, resulting in the patient being released.
- The patient can make the decision to stay voluntarily.
- The patient can be ordered by the judge to continue involuntarily placement and can stay at the facility for 14 additional days.
If a patient is ordered to stay at the facility for 14 additional days and the provider believes that additional treatment longer than 14 days is needed, a 90-day petition can be filed. This will lead to another hearing where the judge can agree or disagree with the petition. An agreement of the petition would lead to the patient being transferred to the Western State Hospital for adults or the Fairfax Hospital for children (39).
Case Study Reflection 3
Jack is a 19-year-old teenager who has just been admitted to your unit following an overdose of prescription medications. It is unclear from the emergency department notes if his actions were accidental or not, and today is your first day speaking with him. He tells you that he was in a car accident last year and has been having a hard time ever since. Past medical history reports depression and feelings of hopelessness. When you ask him about what brought him to your facility, he admits to you that he was trying to end his life. Jake tells you he has seen a provider in the past but does not feel like they listened to him.

Self Quiz
Ask yourself...
- Who should you notify regarding the information that the patient disclosed to you?
- What precautions do you think you should take?
- How can you help Jake during his time on your unit?
- What type of treatment do you think Jake needs after he has been cleared medically?
- Do you think Jake will agree to further treatment? What is the rationale?
- If Jake does not agree to treatment, what would be the next steps? What if he does agree to treatment?
Management and Treatment
Within any healthcare setting, the provider and patient must develop a therapeutic rapport or alliance to ensure that the relationship is productive and respectful. Trust should be a key factor in these relationships. If the patient cannot trust the provider, then they may not wish to disclose personal information that could aid the provider in treatments and care. The opposite can be true as well (17).
Patient safety must be a concern at all times during the provider/patient relationship. If there is concern for the safety of the patient at any time, the proper assessments should be performed, and professional staff should be notified (17).
Together with the patient, the provider needs to create an effective treatment plan for the patient with a focus on the treatment setting, proper education for the patient and their family or other support, and care coordination with other providers. Treatment should be the most beneficial but least restrictive (17).
Non-Pharmacological Interventions and Treatments
Cognitive Behavioral Therapy
The Department of Veteran Affairs recommends the use of suicide-focused cognitive behavioral therapy (CBT) with patients who have a recent history of self-harm or injury (35). Overall, this type of treatment can be beneficial for patients with diagnoses including anxiety disorders, depression, eating disorders, severe mental illness, alcohol and other substance abuse disorders, and even martial problems. The basis for CBT is built on the following three core principles: (2)
- Psychological behaviors can be a result of learned patterns of negative behavior
- Psychological behaviors can be a result of unhelpful ways of thinking
- Those who have psychological diagnoses can learn and develop better coping mechanisms that may help in being more effective in daily life and relieving the symptoms they are experiencing.
Changes in thinking patterns can be attained by training individuals to recognize alterations in their thinking that might create problems in their life. Changes can also occur when the training focuses on reframing an individual’s thinking, which may occur through reevaluating the thoughts realistically rather than based on negativity. Patients can look into obtaining a better understanding of how others are motivated or behave. Problem solving skills can be taught or expanded to help patients cope. Providers can promote role play (to prepare for particular situations), teach patients mind and body relaxation techniques, or encourage patients to face fears rather than avoid them. Patients and providers can work together to come up with the best method to implement CBT (2).
Dialect Behavioral Therapy
Those with recent self-injury or harm as well as borderline personality disorders can benefit from dialect behavior therapy (DBT) (35). It can also be used for those with depression, anxiety, eating disorders, and post-traumatic stress disorder. A type of talk therapy, DBT helps patients accept the reality of their lives and behaviors with the goal to help change the unhelpful behaviors and ultimately change their lives. This is beneficial in many conditions as it focuses on addressing the negative coping skills used to manage negative emotions. Patients may participate one-on-one with the provider, or they may enter DBT group therapy to advance skills gained in one-on-one sessions (10).
Other Psychotherapies
Interpersonal Therapy – helps patients understand interpersonal problems such as conflicts with family or friends, difficulty relating to others, unresolved grief, and changes in work or social roles. This type of therapy assists patients to learn healthier ways to cope and express themselves through effective communication (3).
Psychodynamic Therapy – used with adults to reflect on childhood and other past experiences in order to bring to light some emotions, feelings, thoughts that may have been suppressed. Patients may have developed patterns that can be deemed unhealthy, and this type of therapy can help change those unhealthy coping strategies. Psychoanalysis is a more in-depth form of psychodynamic therapy that is held several times a week (3).
Supportive Therapy – used to support patients in developing their own coping strategies and resources. This process can be used to build self-esteem, improve community and social interactions, and reduce anxiety (3).
Pet, Play, and Creative Art Therapy – can be used in combination with any of the above therapies.
Case Study Reflection 4
Sabrina and her mother come to your outpatient facility for a routine medical visit. Sabrina started high school and wants to join the lacrosse team, so she needs a physical in order to participate. During your assessment you notice that she has lost a significant amount of weight. When her mother steps out of the room, you ask her how she is doing. Sabrina reports that she has been in the nurse’s office more often with stomachaches and nausea. She also reports she fainted in class but was able to convince the school to not call her mother. She tells you that she would like to talk to her mother about all of the stress with school she is experiencing though she is not sure how.

Self Quiz
Ask yourself...
- What would you initially diagnose Sabrina with? Provide your rationale.
- How could you discuss your concerns with Sabrina in a non-judgmental way?
- Are you concerned for Sabrina? Would you screen her for suicide ideation at this time?
- Are you obligated to disclose the information you gathered to her mother? Why or why not?
- Since Sabrina wants to talk to her mother about her worries and stress, how can you facilitate a conversation between them?
- What types of psychotherapy would you recommend to Sabrina?
Medical Treatments and Interventions
Providers need to be aware of medications that can cause or exacerbate depression in patients and increase the risk of suicide. While the list is not all inclusive, some common medications include calcium channel blockers, sedatives, corticosteroids, beta-blockers, H2 blockers, and chemotherapy agents. After a suicide attempt, the provider should assess all medications and diagnoses the patient has. From there, the providers should decide if adjustments should be made (3).
As discussed previously, depression is a major factor in suicide and is present in many other medical and mental health conditions. Anxiety (includes general phobia, specific phobia, generalized anxiety, obsessive compulsive, social anxiety, agoraphobia without panic, and panic disorder), trauma/stress related disorders, bipolar disorder, psychosis, eating disorders, substance use disorders, and non-suicidal self-injury can all have depression as a symptom (19). Medical conditions that co-exist with or exacerbate depression consist of cancer, heart disease, dementia, diabetes, Parkinson’s Disease, and stroke (3).
Medication
The goal of medication administration is to assist the patient to regain balance in their brain’s chemistry and restore it to optimal functioning by controlling the signs and symptoms the patient may have. These medications do not usually result in a cure; instead, they should be taken for extended periods of time, possibly for the patient’s lifetime. These medications can also be combined with other treatment options to give the patient the best possible outcomes (3).
Controversy exists with patients taking antidepressants. In 2004, the Food and Drug Administration made the decision to require that antidepressants have a black box warning addressing increased risks of suicide in young adults. There was a similar claim regarding antiepileptic medications, but the black box warning was not required due to the scientific advisory committee voting against it. Regardless, providers need to stay up to date on medications and warnings, ensuring that they are administering medications in the best interest of their patients. One medication that may work for one patient may not work for another (13).
Antidepressants come in several categories that are based on the type of brain chemical (dopamine, norepinephrine, and serotonin). These categories include serotonin modulators, norepinephrine dopamine reuptake inhibitor, monoamine oxidase inhibitor, tricyclic agents, selective serotonin reuptake inhibitors, and serotonin norepinephrine reuptake inhibitors.

Figure 9: Monoamine Oxidase Inhibitors (28)

Figure 10: Selective Serotonin Reuptake Inhibitors and Serotonin Modulators (9)

Figure 11: Norepinephrine Dopamine Reuptake Inhibitor (16)
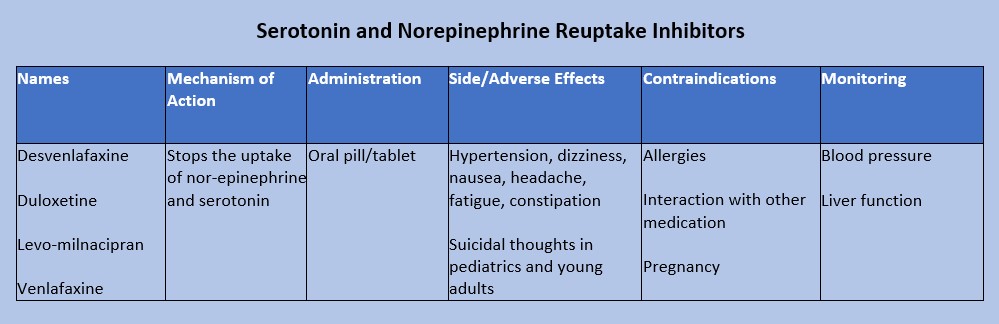
Figure 12: Serotonin and nor-epinephrine reuptake inhibitors (18)
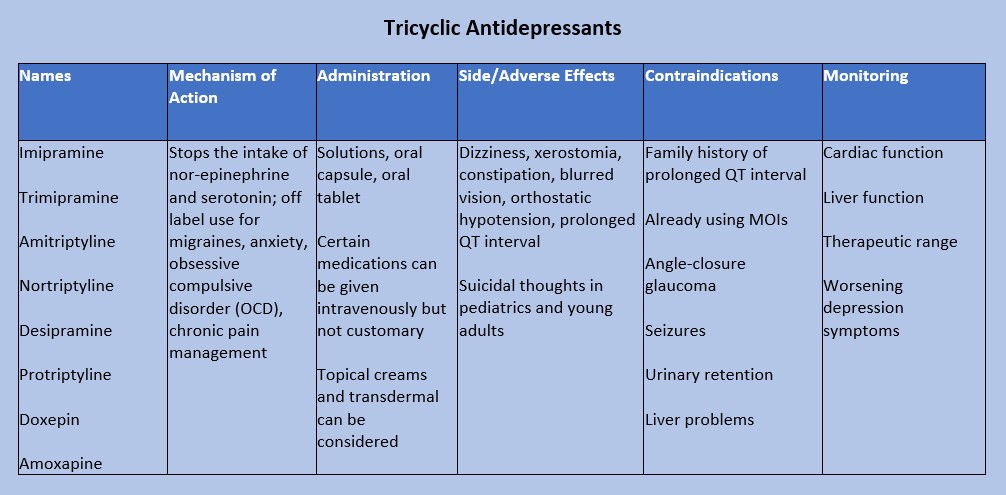
Figure 13: Tricyclic Antidepressants (20)
Case Study Reflection 5
Hope is a 35-year-old who recently moved to your town with her husband, Douglas. She is a teacher at the nearby elementary school while Douglas works in a tech startup, but he was suddenly laid off from his job. After this, Hope brings him to your facility to be evaluated. She tells you that Douglas has become increasingly agitated. He told her that he is a failure and “did not make the right choices in my life.” Douglas admits to drinking heavily with friends since he was laid off.

Self Quiz
Ask yourself...
- What questions do you need to ask Douglas regarding his mental health?
- Is there any medication or medication group that you would recommend prescribed to Douglas?
- If Douglas was prescribed the medication you recommended, what would you teach him about medication administration and adverse effects?
- How would you educate his wife Hope on adverse effects?
- Which adverse effects should prompt Douglas to see a provider?
- If Douglas called your facility with reports of itchiness, a rash, and swelling, what would you instruct him to do?
Substance Abuse Care
Research shows that the longer substance abuse goes on, the harder it is to recover from. Early recognition and treatment can decrease the chance of serious medical conditions or death (19). There are multiple treatment options for patients with substance use disorders, but providers must be aware of each patient’s individual circumstances: time, family and friend support, cost/expenses, and willingness.
All individuals go through the five stages of change when they want to make adjustments in their lives. Those with substance abuse disorders must be willing to make a change for themselves. Even though a person with a substance abuse disorder may want to change for another person or situation (changing for grandchildren, a spouse/romantic partner, children, etc.), they must consider that this person/situation may not remain in their lives. For this reason, they must be willing to make a change for themselves. Sometimes family or friends become too overburdened with the individual’s substance abuse, driving them away. That could inhibit or completely stop the person’s desire to change. The patient may say, “they’re no longer around, what’s the point?” Providers should not deter patients from having support systems as these could be motivation for change. However, patients should also be encouraged to find support within themselves (19). The following are the five stages of change: (19)
- Stage 1: the pre contemplation phase; they do not believe they have a problem. They are not thinking of making changes in their lives or considering how the substance may be harming them.
- Stage 2: the individual begins contemplating the need for change. They begin to realize that the substance is affecting them. This is a great time for providers to encourage them to keep contemplating and consider making a change by identifying the pros and cons of using the substance.
- Stage 3: the preparation phase; the patient has made the decision to change. More encouragement is needed. Healthcare providers should assist patients in planning and providing resources.
- Stage 4: the patient makes the change. They may start decreasing the use of substances or stop using them completely. The best thing to do for the patient is to be as supportive as possible. Patients should develop strategies on how to say “no” to situations regarding the substance.
- Stage 5: the patient is maintaining the change. Patients should focus on the positives of not using the substance and their achievements during this process.
Providers should be honest with patients regarding relapse. Recovery from substance abuse is not a linear path that is 100% successful. Everyone has moments of relapse when it comes to new habits, and it should not be discouraging. Remind patients that there is always help from providers who are non-judgmental.
Treatment strategies can include managing withdrawal symptoms in the acute phase, remaining in treatment, and preventing relapses. Many psychotherapies such as cognitive behavioral therapy can be very beneficial for recovery from substance abuse. Twelve step facilitation programs are twelve weekly sessions done individually that prepare patients for twelve step mutual support programs such as Alcoholics Anonymous and Narcotic Anonymous. While these support programs are not treatments, they are beneficial as additional support to other treatments.
Contingency management programs are similar to a rewards program. Patients, families, friends, or providers may offer rewards or privileges for meeting certain requirements of substance abuse recovery. These requirements might be taking medications as prescribed, participating in sessions, or remaining free of the substance. Rewards can be decided upon by the patient in collaboration with family, friends, and providers (26).

Self Quiz
Ask yourself...
- What services does your facility, organization, city, county provide for substance abuse recovery?
- What services that are offered are beneficial to those that need them?
- Do you believe there are enough resources available? If not, what services do you think are still needed?
- Does your facility have funding for additional services or patients?
- How can you advocate for additional services to be offered?
- Of the five steps of change, which step do you think is the most difficult? Provide your rationale.
- Think back on a patient you had that was in the midst of recovery. What stood out to you about them?
Safety Planning Strategies and Monitoring the Usage of the Safety Plan
Active suicidal ideation and behaviors are considered a medical emergency and should be treated accordingly. Providers in the emergency department setting should focus on medical emergencies and treatments first before moving on to any mental health treatments or consultations (19). Since suicide can be prevented, it is the duty of healthcare providers to ensure the patient is in a safe environment.
Ensuring safety can encompass a variety of methods. One example is searching belongings to remove any weapons or items that can be used to harm the individual or others such as lighters, shoelaces, strings from hoodies, and medications.
Patients may be placed under various observation statuses based on orders made by the physician or a mid-level provider. These observation statuses are also based on facility policies and best practices guided by evidence. Patients withdrawing from substances may need to be closely monitored on a medical floor due to worsening signs and symptoms. Seizures can be life-threatening for these patients.
Restraints and/or seclusion may be required as a last resort for patients. Per Washington law, patients must be under a one-to-one status, meaning there is one staff member always observing the patient. Observation can be done via audio and video equipment, or in-person. There must be documentation discussing the patient’s behavior and condition, attempts for a least restrictive method of treatment, response to seclusion and/or restraints, and the need to continue seclusion and/or restraints. A face-to-face assessment must be performed by a trained professional within one hour of the patient being placed in restraint or seclusion (38).
General regulations for restraints and seclusion include: (38)
- Within one hour of seclusion and/or restraints being initiated, an order from the physician must be entered.
- The nurse must communicate with the family or patient’s legal caregiver regarding the restraints and or/seclusion and the process that will be followed.
- The nurse must discuss with the patient the need for seclusion and/or restraints and attempt to get cooperation from the patient.
- There is to be support from others to assist with the seclusion and/or restraint process.
- Continuous observation is to be maintained while the patient is in seclusion or restraints.
- Physical and psychological needs must be addressed at regular intervals.
- The nurse is responsible for documenting the need for seclusion and/or restraints and patient assessments.
- The nurse is required to maintain education and competence on restraints.

Self Quiz
Ask yourself...
- Do you know what your facilities policies and procedures regarding seclusion and restraints? Do you know where to locate these policies and procedures?
- Some facilities have a no-restraint policy. Does your facility currently have a similar policy, or is that something you think could be advocated for?
- Based on your role, what are your responsibilities when it comes to seclusion and restraints?
- Who in your facility can apply restraints on patients?
- What is your confidence level with applying restraints?
- If you are not confident in applying restraints what are your resources to gain confidence?
- Who are the individuals that are able to monitor patients when they are in seclusion or restraints?
Obtaining Support and Engagement from Third Parties
As reflected in this course, family and friends are vital supportive factors for the individual with suicidal ideation or attempts. If the patient is willing, education should be given to their support system so that everyone understands medications, treatments, follow-up and outpatient treatment, and what to do in another crisis resulting in a suicide attempt or exacerbation of suicidal ideation.
Case Study Reflection 6
Courtney is a 25-year-old female patient who is at your facility with her husband. She was discharged from the hospital a few weeks ago for an aborted suicide attempt. Her friend found her overdosed in the bathroom of her house. She was given follow-up with your facility. Now that she is with you, she reports that she would like resources to help her cope better. After being told she has a history of depression and post-traumatic stress disorder, you begin to think of resources and treatment you can offer her.

Self Quiz
Ask yourself...
- Who else can support Courtney during her recovery?
- How can you ask Courtney about her support system and their involvement in her care?
- Thinking back to the beginning of the course, what protective factors can you give Courtney and her support system?
- Would you consider recommending or ordering any medications for Courtney at this time?
- When would you like to follow-up with Courtney? Would you like anyone else to come to the next appointment?
- Are there any goals you can give Courtney that she can work towards prior to your next appointment?
Restricting Access to Lethal Means
Statistics report that 55% of those that attempt suicide use firearms, 26% use suffocation, and 12% use poisoning. The last 8% is classified as “other” (8). Reducing or limiting access to lethal means can be defined as increasing the distance between someone with suicidal ideation and lethal means. An example would be to have the patient give their firearms over to another responsible adult that lives over 30 minutes away (12).
All providers should discuss this information with their patients and their support systems. By reducing access to lethal means, it is possible to decrease rates of suicide. However, providers must be aware that patients may not tell the full truth when it comes to availability of lethal means, and restricting access is only part of treatment and care (12).

Self Quiz
Ask yourself...
- Does your facility, city, county, or state have any requirements for reporting lethal means within the household?
- Are there any states that you know of that report lethal means in the household?
- If not, would you consider “reporting accessibility to lethal means” as a good idea to implement?
- How could you advocate for reporting to your government officials?
Transition of Care: Discharge and Referrals for Continuity of Care
Treatment of the patient who has suicidal ideation or had a suicide attempt does not stop once they leave the hospital setting. Care must be continued outside of the hospital setting through outpatient psychiatric providers such as a psychiatrist or psychiatric nurse practitioner. These providers can prescribe medications, adjust treatments, and provide additional therapy referrals that may be beneficial for the patient. These psychiatric providers should collaborate with the patient’s primary care provider. As discussed previously, certain psychiatric medications can interact with medication for medical diagnoses.
Veteran Populations
Data from 2020 reports that there were over six thousand veteran suicides in the United States, an average of 17 veterans dying by suicide each day. Substance use and mental health prevalence among those using the Veterans Health Administration rose from 27.9% to 41.9% from the years 2001 to 2020 (14). These numbers are staggering as veterans have a 1.5 higher risk of suicide than those in the general population and women Veterans have a suicide rate that is 2.5 times higher than civilian women (36). The chart below shows the suicide rates based on gender as classified by male and female [See figure 14].
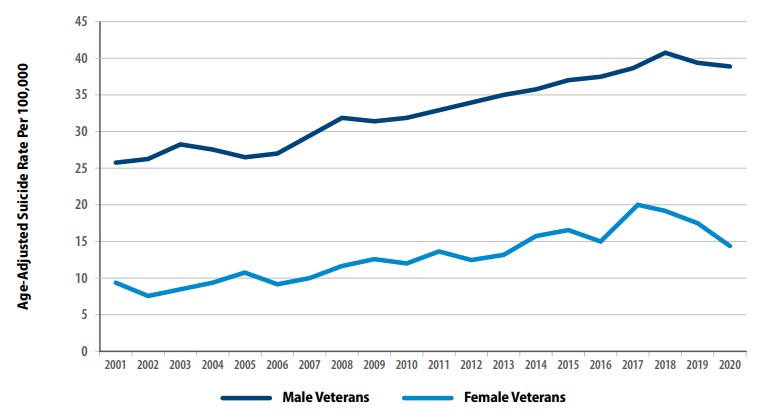
Figure 14: Suicide Rates Among Veterans by Gender From 2001 to 2020 (36)
Rates of suicide were also affected by age. Veterans in the 18- to 34-year age range had a 95.3% increase between 2001 to 2020. Those aged 55 to 74 only rose to 58.2% during that same time period. From 2019 to 2020, older veterans’ suicide rates decreased while those in the 18 to 34 age group increased (14). As with the civilian population, methods of suicide were relatively similar; data was gathered from 2001 to 2020 [See figure 15]. Additionally, rates for suicide are higher among the veteran population in comparison to civilians; the change percentage is based on 2001 data [See figure 16].
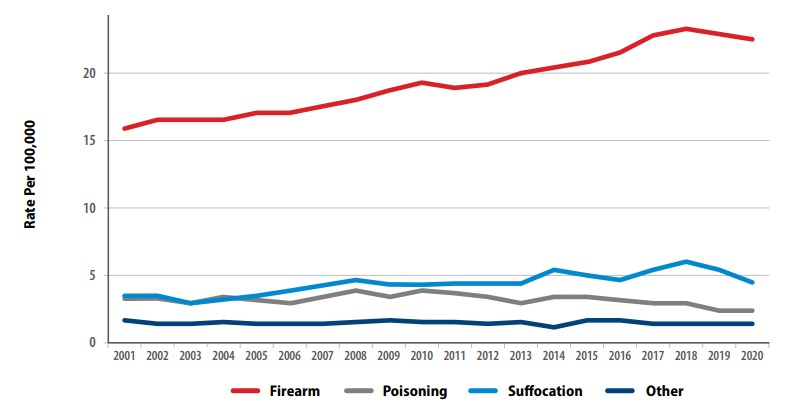
Figure 15: Methods for Suicide Among Veterans from 2001 to 2020 (36)
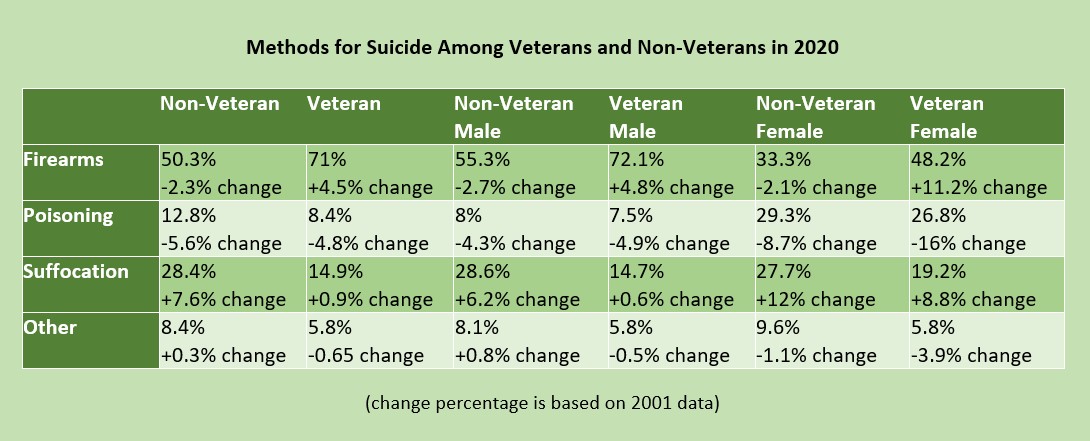
Figure 16: Methods for Suicide among Veterans and Non-Veterans (36)

Self Quiz
Ask yourself...
- Of the statistics listed in the figure above, what surprised you the most?
- Do you agree with this data? Why or why not?
- Have you considered if this data is completely accurate? Do you think the data could be under- or over-reported?
- Does your facility or city have a large veteran population?
- If so, do you provide care to this population often?
Veterans have similar risk factors that have different causes from their civilian counterparts. They have complex mental health conditions such as post-traumatic stress disorder, anxiety, depression, manic-depressive disorder, and traumatic brain injuries as a result of combat exposure. Others have combat wounds that can lead to severe medical diagnoses and possible prescribing of opioid medications for controlling pain. Veterans may have insomnia which can exacerbate any of their other symptoms or diagnoses. These individuals may turn to substance abuse instead of other forms of treatment due to the ease of accessibility. Studies show that over one in 10 veterans are diagnosed with at least one substance use disorder. There is an increased risk of opioid overdose, but this population is more likely to turn to alcohol (36).
The Department of Veteran Affairs has taken steps to provide resources for mental health and suicide prevention to all veterans. Veterans and families are given suicide prevention education upon discharge, and suicide assessments are completed during every visit. Each facility has a Suicide Prevention Coordinator that can be contacted at any time. Veterans, and their families and friends can utilize Veterans Chat, a free, anonymous messaging service that gets them in touch with a Veterans Affairs counselor. If needed, the counselor can transfer the individual to the Veterans Crisis Line for further counseling or referral services (35).
Veteran Resources (All civilian resources are available to veterans):
https://www.veteranscrisisline.net/
https://www.va.gov/health-care/health-needs-conditions/mental-health/suicide-prevention/
https://theactionalliance.org/veteran-and-military-suicide-prevention-resources
Case Study Reflection 7
Cory is a 45-year-old male patient that presents to your emergency department for severe abdominal pain. During your initial assessment, Cory tells you he also feels dehydrated and has been more tired than usual lately. He says he ran out of his sleep medication, “but the providers at the VA are so hard to see. It takes months for an appointment.” When you ask him the standard questions (if he drinks alcohol or uses any other substances), he becomes angry and snaps at you before immediately apologizing. Cory admits that he has been drinking more than usual for the past few months because his chronic leg pain—an injury from when he was in combat—has been bothering him more than normal.

Self Quiz
Ask yourself...
- Would you perform a suicide screening on Cory? What is your rationale?
- If Cory admits to having suicidal ideation, what would be your next steps?
- If Cory denies suicidal ideation, but reports he’s been feeling hopeless or depressed, what would be your next steps?
- Does your facility have any resources to provide Cory while he is in the emergency department?
- Could you consider advocating for a collaboration with the nearest VA to assist veterans like Cory who come to your facility?
Suicide Loss Survivors
As highlighted throughout this course, suicide can happen to anyone, and they leave behind many people. Friends, families, coworkers, and acquaintances can all be affected by the loss. Those who have lost a loved one to suicide are often referred to as suicide loss survivors.
If a healthcare provider encounters a suicide loss survivor, they should always assess the risk for suicide. As discussed previously in this course, some individuals may attempt suicide on the anniversary of their loved one’s passing. In addition, they could attempt on a day of significance to the individual that passed or a major holiday that held special meaning. If the suicide loss survivor is at a high risk for suicide, follow your facility’s protocols for additional assessment or treatment (1).
If there is no significant risk for suicide, provide support and resources. Remember that some individuals have chronic suicidal ideation. Support can be through active listening, having a non-judgmental attitude that is free of bias or criticism. Some individuals may be hesitant to tell their story due to the nature of the loved one’s death. Encourage them to talk to someone they can trust if they do not want to share that information with you. Reassure them that bereavement is not a linear process and that they do not have a time limit to when they should be done grieving. Every person is different, and how they progress through the stages of grieving varies (1).
Resources that can be provided include any of the above options discussed earlier in this course. Psychiatric providers, therapy, and medications may be indicated for survivors of suicide loss. Offer them resources and referrals per your facility’s protocols, but also let them know they are always able to return to your facility if needed, especially emergency departments. Medical providers may need to be involved as well if the patient has any medical concerns (1).

Self Quiz
Ask yourself...
- Have you ever cared for a patient who was a suicide loss survivor?
- How did they present?
- What were their reactions during the initial phase of loss?
- Does your facility have any resources that can be offered to this particular population, for example, a chaplain or spiritual care specialist?
- What behaviors in this patient population would be concerning to you?
- Are there any unique resources you could think of to provide these patients?
Conclusion
Suicide impacts everyone. With the ever-growing need for mental health services and the rise in mental health decline, it is no surprise that suicide rates have increased among all populations. Without proper assessments, knowledge of risk and protective factors, and proper treatment requirements at each level of suicide risk, individuals in need may be missed. It is the job of the healthcare provider to ensure that all individuals are screened and treated appropriately. You may be the last point-of-contact a patient has with a provider prior to taking their own life. Ensure that you ask the questions.

Self Quiz
Ask yourself...
- How often do you screen your patients for suicide risk?
- What suicide screening tool does your facility utilize?
- Do you think the suicide screening tool used at your facility is effective? Why or why not?
- Have you had any family or friends that were going through substance abuse? If you were able to help them, what was challenging for you?
- Are there any nursing groups you are involved in that have position statements or white papers regarding the importance of reporting individuals’ access to lethal means? If so, what do they say?
- In your facility, are the policies and procedures regarding seclusion and restraints effective? Do you think they need to be updated to reflect best practices?
- As a healthcare provider, what can you do to ensure that data reported on suicide is accurate?
➀ Read and Learn
The following course content
LGBTQ+ Cultural Competence
LGBTQ+ patients may experience healthcare disparities due to multiple factors, including lack of provider knowledge. In this course we will discuss how to deliver care, with LGBTQ cultural competence.
Introduction
Lesbian, gay, bisexual, transgender, and questioning (LGBTQ+) individuals represent a rapidly growing segment of the U.S. population [1]. This rapid growth brings with it risk for stigmatization [1]. Implicit healthcare provider biases may result in LGBTQ+ patients receiving a lower standard of care or restricted access to services as compared to the general population [2]. Even when institutions and providers make commitments to equitable care explicit and implicit biases operating outside of conscious awareness may undermine that commitment. There is an urgent need to ensure that healthcare providers are prepared to identify and address their own implicit biases to ensure they do not contribute to the health care disparities experienced by LGBTQ+ and other vulnerable populations. Only by addressing their own implicit biases will health care providers be able to provide patient care in accordance with LGBTQ+ cultural competence.
LGBTQ+ individuals face significant disparities in physical and mental health outcomes [3]. Compared to their heterosexual counterparts, LGBTQ+ patients have higher rates of anal cancer [4], asthma, cardiovascular disease [5,7,8], obesity [6], substance abuse [8,9,10], cigarette smoking [11], and suicide [14]. Sexual minority women report fewer lifetime Pap tests [13,15, 16], transgender youth have less access to health care and LGBTQ+ individuals are more likely to delay or avoid necessary medical care [17] compared to heterosexual individuals. These disparities are due, in part, to lower health care utilization by LGBTQ+ individuals [3]. Perceived discrimination from health care providers and denial of health care altogether are common experiences among LGBTQ patients and have been identified as contributing factors to health disparities [19,20,21,22]. Disparities in health care access and outcomes experienced by LGBTQ+ patients are compounded by vulnerabilities linked to racial identity [23,24,25] and geographic location [6].
Biases among health care students and providers toward LGBTQ+ patients are common [27,28] despite commitments to patient care equality. These biases, also known as negative stereotypes, may be either explicit or implicit [29]. These biases contribute to a lack of LGBTQ+ cultural competence in patient care. A large study of heterosexual, first-year medical students demonstrated that about half of students reported having negative attitudes, explicit bias, towards lesbian and gay people and over 80% exhibited increased negative evaluations of lesbian and gay people compared to heterosexual people (implicit bias) [27]. Research in social-cognitive psychology on intergroup processes defines explicit biases as attitudes and beliefs that are consciously-accessible and controlled; these characteristics are typically assessed via self-report measures and are limited by an individual’s awareness of their attitudes, motivation to reveal these attitudes, and ability to accurately report these attitudes [30,31]. In contrast, the term implicit bias refers to attitudes and beliefs that are unconscious (i.e., outside of conscious awareness) and automatic [32,33]. Implicit bias can be assessed with the Implicit Association Test (IAT) [34], which aims to define the relationships between concepts (ex. race, sex, idea), and positive or negative associations and/or stereotypes. Idenitfied biases are then delegated as slight, moderate, or strong [35].
Healthcare provider biases are correlated with poorer access to services, quality of care, and health outcomes [29, 36, 37, 38]. Explicit biases held by health professionals towards racial/ethnic minorities, women, and older adults are known to affect clinical assessments, medical treatment, and quality of care [39]. Importantly, implicit bias measures are more strongly associated with real-world behaviors than explicit bias measures [40] and are linked to intergroup discrimination [43]. Health care provider’s implicit biases towards vulnerable patient groups may persist despite an absence of negative explicit attitudes [36], resulting in preconceived notions about patient adherence, poor doctor-patient communication, and micro-aggressions, all of which can interfere with optimal care. With less time and limited information processing capacity, provider’s decisions are increasingly governed by stereotypes and implicit biases [42]. Medical student and provider biases may contribute to health disparities in vulnerable populations by negatively impacting communication with patients and decisions about patient care [29, 33]. Taken together, these findings suggest that medical students and healthcare providers are likely to underestimate or to be unaware of their implicit biases towards LGBTQ+ patients, particularly when they are rushed or fatigued, which could impact their behavior and judgments in ways that contribute to health disparities experienced by LGBTQ+ populations. By learning about and addressing their implicit biases, health care providers can work towards demonstrating LGBTQ+ cultural competence and providing optimal care(Introduction section courtesy of Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P.- reference 2).

Self Quiz
Ask yourself...
- What are some cultural misconceptions regarding the LGBTQ+ community and providing medical care?
- How can you demonstrate LGBTQ+ cultural competence in everyday practice?
- What health disparities have you seen in your practice?
- What personal biases have you identified within yourself?
- Have you seen an increase or decrease in understanding of LGBTQ+ people in your facility?
- How have you overcome your personal biases to provide culturally competent care?
- What is implicit bias?
- What do you feel is the definition of cultural competence?
- Have you found difficulties in finding appropriate care for patients in the LGBTQ+ community?
- What is the definition of a health disparity?
Terminology
Understanding the standard terminology utilized is pivotal to treating and interacting with LGBTQ+ patients. Below are listed some of the common terms and how they should be referenced.
Ally- A person not identifying as LGBTQ+, but whom promotes equality and support of LGBTQ+ peoples in a variety of ways.
Androgynous– Identifying as neither masculine nor feminine.
Bisexual – A person who is emotionally, romantically, or sexually attracted to more than one sex, gender, or gender identity.
Cisgender – A person whom identifies with their gender which as assigned at birth. For example, a person assigned female gender at birth who identifies as female.
Gay – A person who is emotionally, romantically and/or sexually attracted to those of the same gender.
Gender-fluid – A person who identifies as a fluid or unfixed gender identity.
Lesbian – A woman who is emotionally, sexually, and/or romantically attracted to other women.
LGBTQ+ – Acronym for “lesbian, gay, bisexual, transgender, and queer.”. The plus sign stands for the innumerable other identities.
Non-binary – Adjective describing person(s) who do not identify exclusively as man nor woman.
Pansexual – A person who has the potential for romantic, emotional, and/or sexual attraction to people of any gender.
Queer – Often used interchangeably with “LGBTQ+”, or to express fluid identities or orientations.
Sexual orientation – An inherent or enduring emotional, romantic, or sexual attraction to other people.
Transgender –Umbrella term for people whose gender identity and/or expression is different from cultural expectations based on the sex they were assigned at birth. It does not imply any specific sexual orientation and transgender persons may identify as straight, gay, lesbian, bisexual, etc.
*Definitions largely derived from (44, 45).

Self Quiz
Ask yourself...
- Which of the above definitions have you heard used interchangeably?
- How does understanding these terms and definitions improve your ability to provide culturally competent care?
- How does using appropriate terminology improve patient care?
- Have you ever encountered a situation where you misused terminology? How was that received, and how did you navigate that conversation/
- Have you used these terms in your patient documentation?
Best Practices
Below we will list and discuss the best practices for ensuring a positive, equitable healthcare experience for LGBTQ+ persons, according to the Joint Commission (this is not a comprehensive list, nor inviolable, but rather highlights).
Create a welcoming environment that is inclusive of LGBT patients and demonstrates LGBTQ+ cultural competence.
- Prominently display the hospital nondiscrimination policy and/or patient bill of rights.
- Waiting rooms and common areas should be inclusive of LGBTQ+ patients and families.
- Unisex or single-stall restrooms should be available.
- Ensure that visitation policies are fair and do not discriminate (even inadvertently) against LGBTQ+ patients and families.
- Foster an environment that supports and nurtures all patients and families.
Avoid assumptions about sexual orientation and gender identity.
- Refrain from making assumptions about a person’s sexual orientation and/or gender identity.
- Be cognizant of bias, stereotypes, and other communication barriers.
- Recognize that self-identification and behaviors do not always align.
Facilitate disclosure of sexual orientation and gender identity, but be aware that disclosure is an individual process.
- Honor and respect patient’s decisions to provide or not provide sexual and/or gender information.
- All forms should contain inclusive, gender-neutral language that allows patients to self-identify.
- Use neutral and inclusive language when communicating with patients.
- Listen to and respect patients’ choice of language when they describe their own sexual orientation.
- Conduct confidential patient satisfaction surveys that include questions regarding sexual orientation and gender identity
*Information largely derived from Joint Commission field guide, reference 45.
For more information on best-practices in the workforce, visit the Joint Commission website by clicking here.

Self Quiz
Ask yourself...
- Have you ever misused a pronoun or overheard a co-worker misuse a pronoun in practice? How can you make sure this doesn't happen again?
- Do you find it getting easier or more difficult to navigate pronouns?
- How does creating a welcoming environment improve patient care?
- Why is it important to avoid assumptions about sexual and gender identity when caring for patients?
- In what ways can the nurse support a patient's desire for privacy?
Establishing Relationships with LGBTQ+ Patients
When interacting with patients, one should not assume gender or sexuality. Addressing a patient whom identifies as a female as a male can cause grave harm to the relationship. Instead, nurses should use open-ended questions. For example, rather than saying “Hi sir, what brings you to the hospital,” a nurse might say, “Welcome, what brings you to the hospital today (45)?”
If a nurse uses the incorrect pronoun, the best practice is to apologize and ask the patient what pronoun and name they prefer. For example, a nurse may say, “I apologize for assuming your gender. How would you like to be addressed? (45).
In conversation, the nurse should use the name and/or pronoun the patient prefers without drawing special attention to the subject (45). For example, if a patient prefers to be identified as their partner’s wife, you should follow suit.
The core of relationship-building with LGBTQ+ patients is no different than any other patient, fundamentally. If nurses have a basic understanding of best practices and a healthy dose of respect and compassion for LGBTQ+ patients, a positive relationship is likely to develop.

Self Quiz
Ask yourself...
- Do you have any biases which may affect the care you provide to LGBTQ+ patients?
- Have you worked for someone who did NOT demonstrate LGBTQ+ cultural competence? In what ways could they improve their practice?
- How does establishing a respectful and welcoming relationship with a patient improve patient care?
- Have you seen other healthcare workers engage negatively with LGBTQ+ patients?
- In what ways can assumptions lead to detrimental interactions with patients?
- Have you dealt with patients who made inappropriate assumptions about you and the care they may receive? How did this impact your care?
- What barriers have you found when establishing a relationship with an LGBTQ+ patient?
Health Disparities of LGBTQ+ Patients
LGBTQ+ Americans are at higher risk of substance use, sexually transmitted diseases, cancer, cardiovascular disease, obesity, bullying, isolation, anxiety, depression, and suicide when compared to the general population (49). LGBTQ+ youth are frequently bullied at schools (46). In fact, early victimization and subsequent emotional distress accounted for 50% of the disparities between LGBTQ+ youth (46). In other words, LGBTQ+ Americans are discriminated against and disadvantaged from a very young age.
When home life also reflects a lack of LGBTQ+ cultural competence, more problems arise. A major cause of LGBTQ+ distress is family rejection. Disclosure of gender identity or sexuality can cause very significant interpersonal conflicts among family and friends of LGBTQ+ persons (46). This explains some hesitancy and should help nurses understand the importance of respecting privacy, while giving options to patients about disclosing sexuality and gender.

Self Quiz
Ask yourself...
- Are there any circumstances in which your current hospital's policies could discriminate against LGBTQ+ families?
- If so, how would you begin to work with leadership to change those policies so they reflect LGBTQ+ cultural competence?
Providing an Inclusive and Accepting Care Environment
LGBTQ+ patients often experience difficulty in finding healthcare environments in which they feel accepted and understood (45). Past negative experiences, lack of knowledge among healthcare providers, and limited access to healthcare in general may become major barriers for LGBTQ+ persons when seeking care (45).
The core tenant of providing an inclusive environment is understanding the needs of LGBTQ+ patients, and working diligently to create an environment which does not disadvantage or discourage them from seeking care.
Policies and procedures at institutions should be designed to reflect a non-discriminatory environment. For example, many hospital policies dictate that only legal family spouses or partners can visit in specific circumstances. Policies such as this are inherently discriminatory toward LGBTQ+ patients, as they may not have legal spousal status due to social, legal, or personal reasons.

Self Quiz
Ask yourself...
- Have you ever had an experience where a colleague made a derogatory remark about a patient based on sexual orientation or gender status? If this happened to you, how would you handle that situation differently?
- How would you address a situation where a colleague handled a patient like that?
- What are examples of an inclusive environment?
- Does your facility have legal policies protecting patients and providing culturally competent care?
- What kinds of continuing education or inservices does your facility incorporate to help ensure culturally competent care?
Laws Specific to Washington D.C.
1973: Title 34 is passed, which prohibits discrimination based on sexual orientation.
2006: The D.C. Human Rights Act is updated to ensure residents of the district are protected regarding employment, house, and public accommodations.
2016: The Armstrong Amendment is repealed in D.C., which allows religious schools exemptions from complying with anti-discrimination laws.
2016: LGBTQ Cultural Competency CE Act is passed. This requires that all licensed healthcare providers take a 2-credit hour course to increase competency (such as the one you are currently taking!).

Self Quiz
Ask yourself...
- Think about the structure of your facility. Does it create an environment which minimizes friction and discrimination of LGBTQ+ patients?
- Do you feel there are any biases among healthcare staff?
- If so, how would begin addressing those?
Exercises on LGBTQ+ Cultural Competence
To help solidify your learning, please complete the following exercises at your own pace. The answers/guidance for each are provided below.
Scenario 1
A patient enters your emergency department and you assume the patient identifies as a female. You introduce yourself and say, “Ma’am, how can we help you? What brings you in today?"
The patient appears dismayed but answers the question. The nurse is confused and does not understand why the patient appears distressed. What is the best course of action?
Answer: The nurse should apologize to the patient and ask the patient how they would like to be addressed. Then, the nurse should update the patient’s records to reflect such, to reduce further confusion.
If the nurse does not address the issue, the patient may feel uncomfortable and develop a negative association with healthcare, which can lead to disparities in the future.
Scenario 2
A patient in your ICU has had a deterioration while his husband was in the room. After a family meeting, a member of the healthcare team makes a derogatory remark about the patient’s sexuality. What is the next best action for the nurse?
Answer: Pre-conceived phobias and stigmatizations can cause significant distress to LGBTQ+ patients, even if not stated directly to them. These type of remarks are abusive and should not be tolerated. The nurse should confront the co-worker (if safe) and consider reporting the comments to the Human Resources department.
Scenario 3
A LGBTQ+ patient is being admitted and prefers not to disclose their sexuality. However, the nurse is unable to proceed with the admission process without this information. What could be done to rectify this system-level issue?
Answer: The nurse should work with administration to ensure that all charting and paperwork allows individuals to self-report sexuality and/or gender if they want. However, healthcare systems should not force patients to “come out” unless it is absolutely medically necessary.

Self Quiz
Ask yourself...
- What information from this course can you take to your facility to encourage a positive change in LGBTQ patients and create an environment for LGBTQ+ cultural competence?
- Do you feel that you are more aware of your biases after reviewing the information in this course?
- What resources do you have access to that can further expand your knowledge and understanding of the LGBTQ+ community?
- How will your patient interaction be changed after completing this course?
- Why is ensuring culturally competent care so important in providing ethical care?
Conclusion
LGBTQ+ cultural competence must be ingrained in our healthcare systems in order to foster excellent relationships between members of the LGBTQ+ community and medical staff. Hospitals and healthcare systems have a great deal of work to do in becoming LGBTQ+ friendly. The efforts must continue until LGBTQ+ patients and families do not feel disadvantaged, anxious, or frustrated when interacting with healthcare systems. As the patient’s ultimate advocate, nurses are at the front-line and should advocate for patients both individually and from a policy perspective. Nurses should work with and spearhead efforts to ensure that healthcare policies reflect best-practice and do not discriminate against LGBTQ+ patients in any way.
➀ Read and Learn
The following course content
Washington State Telemedicine Training
Introduction
Telehealth has become more popular and widespread across the United States. With its widespread use and popularity, more nurses and health care practitioners are required to complete courses like this Washington Telehealth Training. The earliest encounter with telehealth involved Alexander Graham Bell in 1876 when he used his telephone as a means of getting help from his assistant after he had an accident involving spilled acid on his trousers (1). The origin of telehealth officially began in 1959, with clinicians at the University of Nebraska utilizing video communication for medical purposes. These clinicians established a two-way television setup to transmit information to medical students across campus. Five years later, the setup was linked with a state hospital to perform video consultations. Telemedicine first became popular in rural areas, where populations with limited healthcare access could now reach specialists from afar. In the 1960s and 70s, the Public Health Department, NASA, the Department of Defense, and the U.S. Health and Human Services Department all invested time and money into telemedicine research.
In this Washington Telehealth Training course, the following outcomes and objectives will be reviewed:
- Discuss the background, origin, and scope of telehealth practice.
- Explain policies and regulations related to telehealth.
- Describe ways to determine if an organization is ready and prepared for telehealth and the process for the actual telehealth visit.
Telehealth Background
Definition
This Washington Telehealth Training course defines telehealth as the delivery of healthcare services using digital technology and can include services in the behavioral health field, such as substance use disorder treatment, serious mental illness treatment (SMI), and counseling. The clinic is considered the originating site (where the patient is located during the telehealth visit) and the specialist at the other location is the distant site.
In organizations that serve individuals with intellectual and developmental disabilities (IDD), telehealth is the practice of healthcare within a professionally designated scope of practice using electronic communication, information technology, or other means between a licensee in one location and a client in another location with or without an interviewing healthcare provider.
Telehealth allows patients to have better access to a variety of specialists which, in turn, increases the number of people receiving appropriate care. Overall, it can provide cost savings to the patient and increase the quality of care.

Telehealth and its Scope of Practice
The practice of nurses using telehealth is within the legal scope of practice for licensed nurses, registered nurses, licensed practical nurses, and advanced practice registered nurses (2). It can be used among these professionals as needed or when a patient is unable to make an in-person visit.

Self Quiz
Ask yourself...
- What is the history of telehealth and its development?
- How does telehealth apply to everyday life?
Telehealth Policy and Regulations
In-State/Out-of-State Requirements
Most providers are only allowed to see patients located in states where the provider is licensed or certified. However, many states temporarily changed this policy during COVID-19. These in-state restrictions are often due to the nature of the services a clinic provides.
Organizations can choose if they want to provide telehealth services. However, if the topic is suggested, the organization must have team members in place to discuss the options, pros, cons, and feasibility of telehealth within its practice.
Additional Credentialing and Protocols
There are no additional credentialing or privilege protocols in place for those located out-of-state as those individuals are required to seek services within their area and state. The credentialing requirements must abide by the specific guidelines set forth by each organization and these can vary from one place to another.
It is imperative that the right billing codes are used in order for the insurance company to reimburse for services rendered. Typically, there are codes known as the Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS). It is important to pay attention to any changes, as these codes do change from time to time. If ever in doubt, always double-check to ensure that the codes being entered are the correct ones for proper billing and reimbursement.
Reimbursement of In-Person Visits
Telehealth visits are typically reimbursed at an equal rate to in-person visits, but the reimbursement for those with intellectual and developmental disabilities (IDD) relies mostly on Medicaid Home and Community Based Services (HCBS) waivers. The overwhelming majority of waivers permit the temporary use of telehealth services for those individuals with IDD; however, only a small percentage include the use of telehealth on a permanent basis for this population. The limitations that were noted involved those individuals that were not a part of the following services: employment, day, and prevocational services, and in-home residential supports. Controlled substances are also not allowed to be prescribed by using telehealth until an in-person visit takes place.
Ryan Haight Act of 2008
The Ryan Haight Act summarizes that no controlled substance may be delivered, distributed, or dispensed by an electronic method such as the Internet without a valid prescription and requires at least one in-person medical evaluation (3).
This Washington Telehealth Training course asks nurses to consider the following example: if a patient undergoing a telehealth visit needs to be prescribed a controlled substance, the person issuing the prescription must have a doctor-patient relationship with the patient. This may seem reasonable, but the narrow definition in the law indicates that a telehealth visit may be inadequate due to the law specifically requiring an “in-person evaluation”.

Self Quiz
Ask yourself...
- Can an organization willfully choose to participate in telehealth or are they required to do so?
- How can one ensure that services for telehealth are being billed accurately?
- What is an example of the Ryan Haight Act of 2008 in action?
Telehealth Readiness
When an organization begins to consider whether or not telehealth service is right for them, there are four critical factors that must be considered. These four factors include 1) workflow, 2) practitioner availability and acceptance, 3) infrastructure and cost, and 4) sustainability. All of these factors must be considered when attempting to decide if telehealth services would prove beneficial to an organization. An organization must meet as a team to discuss these components in order to assure that these factors can or cannot be met successfully.
Standards of care must be implemented and followed at any given practice and specialty area. The same is true for practices utilizing telehealth. The following serve as standards of care (4):
- Training of staff – staff must be trained in the use of the technology used and must be competent.
- Evaluations and Examinations – diagnosis should be established by establishing the patient’s history, mental evaluation, physical examination, and appropriate laboratory and diagnostic testing.
- Licensee-Patient Relationship – proper identification must be made prior to any telehealth encounter. Failure to verify the patient’s identity may lead to fraudulent activity or disclosure of patient information that is confidential. The location and identity of the patient must be verified. The licensee’s name, professional credentials, and location should be provided to the patient. Appropriate follow-up care and a complete medical record must be available to the patient and other health care providers involved in the treatment plan.
- Prescribing – the concept of “Contact with Patients before Prescribing” must be practiced – other providers must be involved in ongoing care and evaluations of the patient. All federal and state laws must be followed and are expected to participate in the Controlled Substances Reporting System.
- Medical Records – complete records must be maintained and must be consistent with prevailing medical record standards. HIPAA and security related documents must be present and signed appropriately. Confidentiality must be maintained and a copy of the medical records consistent with state and federal laws must be in place.
- Disclaimers – a statement that includes any unique limitations of the electronic model being used should be present, if applicable.
- Licensure – the practice of medicine is deemed to occur in the state in which the patient is located. If the licensee intends to practice telehealth outside of their current state must first check with other state’s licensing board to ensure if this is allowed.
Protocols for the necessity of visits
Typically, most patients can receive an appointment for a telehealth visit without any difficulty as long as the following are not present: conditions causing severe pain or those requiring a detailed in-person examination, prescription and refill of controlled substances, any condition that requires in-person drug administration, highly complex medical conditions, and psychiatric emergencies.
There are certain protocols regarding the type of visit that is appropriate for telehealth and when one should be referred to an in-person visit. The following are some common types of visits that meet the standards of telehealth:
- Lab tests or x-ray results
- Recurring conditions such as migraines or urinary tract infections
- Skin conditions
- Mental health treatment, online therapy, counseling, and medication management
- Prescription management
- Urgent care issues such as colds, coughs, and stomach aches
A patient should be referred to an in-person visit when they require highly specialized care, such as cancer treatments or complex specialty care.
How to Receive a Telehealth Appointment
With most telehealth appointments, it is best and easier if the patient will download the app and initially set up an account. There is also a 1-800 number that can typically be called as well if the patient needs additional help. Each patient will need to complete a brief medical history just as one would at the doctor’s office and once submitted, the telehealth specialist will connect the patient with the right medical professional – doctor, therapist, or a specialist. The telehealth specialist will assist the patient with setting up a date/time for the appointment and the appointment can be completed by phone, video, or app.

General Overview of Telehealth Software
This Washington Telehealth Training course recommends following five things should be considered when looking to choose a platform to implement telehealth services: integration using the same interface which allows everything to be accessed; user-friendly design – all patients should feel comfortable using the platform and not frustrated; specialty care solution – look for a platform that caters to providers that provide specialty services; configuration and customization – the platform needs to be customizable to meet each patient’s unique preferences along with the preferences of the healthcare facility; data analytics – it is important to gain new insights by recoding and logging each patient interaction, which allows the organization to better manage the practice and the experiences of the patients. The collected data assists with identifying issues early and creating resolutions in a timely manner.
In general, the practice of telehealth requires a good source of internet access by all parties, supported by broadband internet connection and mobile communication. The following list includes hardware requirements:
- Desktop
- Computer
- Laptop
- Smartphone with a camera
- Tablet with a camera and microphone
- Telemedicine care
Guide on Approved Software
It is important to ensure that the software platforms used are HIPAA compliant. The list below includes vendors that represent HIPAA-compliant video communication products that are recommended by this Washington Telehealth Training course:
- Skype/Microsoft Teams
- Updox
- VSee
- Zoom for Healthcare
- me
- Google G Suite Hangouts Meet
- Cisco Webex Meetings/Webex Teams
- Amazon Chime

Self Quiz
Ask yourself...
- What are the implications for an organization to implement telehealth?
- Is it difficult for a patient to receive an appointment for telehealth based on their symptoms?
- What are the implications of choosing the correct software for telehealth services?
Obtaining Patient Consent for Telehealth
Once the patient has decided to use telehealth for an appointment, official informed consent may be required. It is important to keep in mind that specific informed consent laws vary by state, but this Washington Telehealth Training course recommends the following actions that are always a good idea to follow (5):
- Explain to the patient what they can expect from the telehealth visit and what their rights consist of.
- Check in with the patient about their responsibilities during online counseling or telehealth visits such as wearing headphones and finding a place to be alone to ensure privacy.
- Inform the patient to get anyone’s consent from the start that may be observing the patient.
- Instruct patients to complete required forms ahead of time and bring them to the telehealth visit.
- Ensure the informed consent form and any other documentation has been done during the check-in process, including verbal consent.
It is important to have your medical intake forms reviewed by the legal team. Obtaining informed consent from each patient is important to have completed before the first appointment.
Verbal consent is where a patient gives their consent to a procedure in a verbal manner and does not sign any written form. This Washington Telehealth Training course provides the following example:
My name is ________________________________ and I am verbally consenting to participate in the study. By signing above, I give permission to be a part of the study and to allow the data collected to be used for the resulting process.

IT Support Services
In order for telehealth to be productive, IT support services must be in place to ensure that all areas are fully functioning and if a problem occurs, the IT department must be available and ready to intervene 24/7/365. If a patient is experiencing problems making an appointment or with any connectivity issues, IT can be notified to assist in these areas.
Practice First
Telehealth is a relatively new technology and as it gains widespread usage it is important for each organization using telehealth to do a practice run first to ensure that all of the elements are working properly. Every platform is used differently, and it is important to understand the requirements for each one. Also, the patient may need to have an app downloaded beforehand to make the entire process smoother.
Emergency Outage Plan
Planning can go a long way to prepare for an emergency situation during a telehealth appointment. If an emergency outage situation occurs, answer the following questions with the patient before or at the beginning of their first appointment:
- What is your current location?
- Confirm the patient’s exact location and obtain their full address.
- What is the information for your emergency contact?
- There should always be more than one number given in case disconnection occurs.
- Do you have an alternate way of contacting the clinic if disconnection occurs?
- If not, this needs to be made known at the beginning of the call.
- Do you have an alternate video platform to use if disconnection occurs?
- If so, this needs to be communicated with the provider at the start of the call.
Patient Information Security/HIPAA Protocols
This Washington Telehealth Training course recommends that all telehealth services provided by insured health-care providers and health plans must comply with the established HIPAA rules according to the Health Insurance Portability and Accountability Act of 1996. The HIPAA rules are in place to ensure that both paper and digital medical histories remain private. During the actual call, the health care provider is required to call the patient from a private setting such as their office or an appointment room. The patient should also be in a private, safe location in which they can freely discuss their health.
There are four important ways to stay compliant with the telehealth HIPAA regulations, 1) check one’s remote communications, 2) double-check the tracking of data, 3) keep all vendor agreements in writing, and 4) protect any and all stored communications.
Connecting Interpreter Services to Telehealth
Many virtual meeting platforms offer an option to connect an interpreter if requested by the patient. Once conencted, a Language Line can be added to the address book that enables the interpreter to be accessed. The service assists in building trust, reducing misunderstandings, and improving the overall patient experience. The patient will be connected to experienced professionals who will securely and patiently assist those with language barriers to make important healthcare decisions. The patient can also access telehealth resources translated from English on the platform that allows the patient to view the information in their own preferred language.
Billing and Documentation Protocols
When submitting documentation for a telehealth visit, the following elements must be included: date of visit; consent for visit from the patient or patient representative (either verbal or written consent); category of office visit, real-time audio with audio/telephone or video only.
In order to ensure that medical records are accurate and supported by telehealth services, the following must be documented in the health record (6):
- Method of telehealth (video connection, phone call, etc.)
- Location of provider (name of clinic, city, home, other)
- Listing of all clinical participants, roles, and actions
- Member location (name of clinic, city, home, other)
- Time actually spent in medical discussion – start/stop times.
- Patient consent – documented confirmation or verbal consent must be documented

Self Quiz
Ask yourself...
- What does verbal consent indicate within telehealth, and can you give an example?
- How does an organization ensure that HIPAA is maintained with telehealth visits?
- How does an organization ensure that accurate billing has been conducted with telehealth visits?
Telehealth Visit
Guidelines
Just as bedside manner encompasses much more superficial appearance, web-side manner transcends how an individual looks on camera, including empathy and understanding for patients regardless of physical distance. The same standards apply for in-person visits, but a patient is likely to observe and evaluate how the telehealth visit goes based on the visual manners given during the visit. The medical professional should be dressed in an appropriate and professional manner. The lighting, angle of the camera, and background are all important factors to consider when doing a telehealth visit. This Washington Telehealth Training course provides the following fundamentals for each telehealth visit:
- Ensure that all professional identification is within clear view for the patient.
- Place yourself in the center of the video frame. You are the focal point – not the background.
- Ask the patient for a contact phone number or alternative communication in case a disconnection occurs.
- If this is the first telehealth visit with the patient, consent must be obtained.
- Ensure that you are HIPAA-compliant by confirming that anyone else in the room and is approved by the patient and that the patient is comfortable performing the visit.
- Position lighting to reduce any glare or spotlights. Uniform lighting is the best and allows the patient to see your face.
- Eliminate background items which may distract the patient.
- Confirm the patient’s location to ensure you have the proper licensure.
- Ask the patient to make any rearrangements regarding furniture, lighting, or body position in order to give you a better view of the patient and a more accurate exam.
Telehealth is not for everyone or for every medical condition. It is important for an individual to discuss the risks, advantages, and disadvantages with one’s healthcare provider.
How to Start a Telehealth Visit
This Washington Telehealth Training course recommends the following four steps will help you successfully conduct a telehealth visit from start to finish:
- Ensure the patient has the resources to schedule a telehealth appointment– patients need to be aware of how to schedule an appointment and how to contact a customer service representative if any problems arise.
- Prepare for the telehealth visit – send the patient a reminder a day before the appointment reminding them to connect 10 minutes prior to the appointment for registration and check-in. The co-payment can also be collected at this time.
- Conduct the telehealth visit – the provider should carefully review the patient’s chart and medical history just as they would for an in-person appointment. Additionally, any messages or information in the patient portal should be reviewed and imported beforehand. The provider should start the visit note, use the appropriate telehealth template, and begin the visit. A proper web-side manner should be implemented the entire time with intentional listening and clear communication. During the evaluation, the provider will document any complaints and symptoms reported by the patient. Note any assessments or treatment plans including the proper diagnosis codes, orders, mediations, and relevant instructions. After ending the telehealth visit, the provider should complete any documentation and sign the note.
- Follow up and complete the telehealth coding and billing – the practice should send a follow-up text message or email the day after the appointment offering contact information for any questions or concerns with a link to a patient survey. The patient can log into the patient portal to review a summary or the visit, education resources, pay a balance, and communicate with the practice if needed.
The following can three diagnostic errors that may create issues during telehealth visits: 1) inadequate history taking due to poor or inadequate communication, 2) limited physical examinations such as the omission of auscultation and accessibility of private areas of the body, and 3 )reliance on patients and their families to accurately measure vital signs, report them, and describe physical findings.

Self Quiz
Ask yourself...
- Do all patients benefit from a telehealth visit?
- What are some potential issues with telehealth that can impact patient safety?
Diabetic Ketoacidosis Management
Introduction
Diabetic ketoacidosis is considered one of the most life-threatening complications of diabetes mellitus. More importantly, it is also one of the most preventable complications of diabetes. Through proper education and empowerment of persons with diabetes to self-manage this chronic medication condition, the overall mortality rates associated with this complication have steadily declined in the United States. An interdisciplinary team approach (including medical providers, social workers, case managers, and community resources) has been proven to reduce recurrences of DKA in vulnerable populations. (2)
Definition
DKA, or diabetic ketoacidosis, is defined as the potentially life-threatening medical condition that occurs in people with diabetes. While it usually occurs in persons with type 1 diabetes mellitus, who are dependent on daily insulin injections, it may also occur in individuals with type 2 diabetes for a variety of reasons (underlying physiologic stress, such as an acute infection or trauma, or uncontrolled blood glucose levels and missed routine diabetic medications).
In an acute case of diabetic ketoacidosis, the body is not producing enough insulin to move glucose into the cell for energy, and the liver then begins to break down fat for fuel instead, producing ketones. This buildup of ketones in the body results in ketoacidosis. Left untreated, diabetic ketoacidosis can lead to a diabetic coma and eventual death. (3)


Self Quiz
Ask yourself...
- As you begin this course, think about the diabetic patients you have cared for in your professional career.
- Do you have family or friends in your life that have been diagnosed with diabetes?
- What are your concerns over their self-management ability of this chronic medical condition?
- What areas of diabetes self-management do you consider the highest priority when you are delivering patient discharge instructions?
Epidemiology
Epidemiology is the study of how often a disease process occurs in different populations. By studying the rates of occurrence, epidemiologists are able to evaluate treatment options and develop long term strategies to lower the risk of ongoing or recurrent disease related episodes.
Diabetic ketoacidosis is currently a leading cause of both morbidity and mortality in children with Type 1 diabetes. It usually occurs at the time of the initial diagnosis in as much as 30-40 percent of the children in the United States alone. In children living with a confirmed Type 1 diabetes condition (previously diagnosed), these percentages decrease to average rates of 6-8 percent annually.
The drastic reduction of such occurrences is believed to be directly related to ongoing patient and family education and medication adherence. Diabetic ketoacidosis is potentially life-threatening, but it is for the most part, also preventable. Throughout this educational offering, key components of patient education in diabetic self-management, including reducing the risk of diabetic ketoacidosis, will be discussed (4) (5).
By comparison, other countries, challenged by annual income, healthcare access, cost management, and food insecurity, do not fare so well. Various studies were funded by the Leona M. and Harry B. Helmsley Charitable Trust, and the Juvenile Diabetes Research Foundation Ltd. Several countries included in these studies were deemed “LLMIC” (low and low middle-income countries). Countries, including Haiti, Ethiopia, Senegal, Nepal, and Tanzania, to name a few were found to have inadequate supplies, medications, and equipment to both initially diagnose, and successfully manage diabetes mellitus long term. Critical items necessary for the treatment and stabilization of acute diabetic ketoacidosis were in even shorter supply. These barriers to treatment resulted in delayed or missed diagnosis, increased overall complication rates and premature deaths.
“Evidence from single-center studies suggest that DKA in new-onset T1D is more common in LLMICs compared to upper and upper-middle income countries, with rates ranging from 62.2 to 77.1% in Nigeria, 69.8% in South Africa, and 92.1% in Sudan. In comparison, in upper and upper-middle income countries in North America and Europe the rates range from 14.7% (Denmark) to 42.0% (France”). (6)
Ongoing education of healthcare professionals and patients/families alike, coupled with availability of and easy access to self-management medications, and monitoring equipment, positively affect DKA related health outcomes and quality of health and well-being.
The development of insulin delivery systems (insulin pumps) has further positively impacted the rate of DKA occurrence. Patient comfort, ongoing education, streamlined medication delivery and enhanced monitoring systems have afforded patients with diabetes a better understanding of their condition and empowered them to successfully self-manage their health conditions. While reported rates of DKA in previously diagnosed persons with T1DM were 6.3% in one study, that number decreased to 2.2% at 3 years out.
Ongoing improvements in closed insulin delivery systems medication continues to improve (lower) DKA occurrence rates, when compared to those previously using multiple daily injection therapy. The development of continuous glucose monitoring (CGM) devices, in addition to insulin delivery systems, provides for early detection and treatment of both hypoglycemia and hyperglycemia. The addition of remote app devices further allows constant monitoring and two-way communication between patients, family members, and even healthcare providers.
Sadly, the population identified as being at highest risk for DKA is that of children who are uninsured/underinsured, lacking the insurance coverage for many closed delivery medication systems as well as specialty care (pediatric endocrinology) provider access.
The acute complications associated with DKA account for a high percentage of premature deaths in T1DM patients under the age of 30 years old. (7) Given these statistics of prevalence and incident rates, DKA is an ever-increasing global concern which is best addressed and managed through ongoing, patient specific disease management education.
The prognosis for DKA worsens in the presence of coma, hypotension and in the presence of severe (chronic and acute) comorbidities. Yet, with early identification, ongoing education, and improved glucose monitoring/treatment options, DKA, often life threatening, is also highly preventable. The goal, therefore, is to ensure all patients with diabetes mellitus are given equal opportunity to access both the education and materials necessary to successfully monitor their health condition. (8)
Pathophysiology
Diabetic ketoacidosis occurs when the body is under stress and responds with an increase in catecholamines, cortisol and growth hormones. The release of such hormones decreases the ability of insulin, further increasing insulin resistance and resulting in serum hyperglycemia. Without cellular glucose for energy the body then begins to break down fat and protein for energy, resulting in increased levels of serum ketones. The combination of hyperglycemia and ketosis, as well as dehydration and various electrolyte imbalances, form the basis of diabetic ketoacidosis. (9)
While it is believed that the omission of insulin (nonadherence/ noncompliance, or mechanical failure of insulin delivery systems) accounts for the largest percentage of DKA admissions, other factors may be responsible for the development of this condition. Any disease process that increases insulin resistance, impairs insulin secretion, or interferes with carbohydrate metabolism may contribute to the onset of acute diabetic ketoacidosis in a vulnerable, health compromised patient.
Clinical Signs and Symptoms
Diabetic ketoacidosis is caused by the underlying presence of hyperglycemia, ketoacidosis and ketonuria. Early signs and symptoms may include any of the following:
- Generalized weakness and fatigue.
- Nausea and vomiting
- Diffuse abdominal pain.
- Decreased appetite and anorexia.
- Decreased/ altered levels of consciousness, such as mild disorientation and confusion.
- Dry skin and mucus membranes and decreased perspiration
- Tachycardia (increased heart rate) and tachypnea (increased respiratory rate)
- Acetone/ketone smell on breath
- Significant weight loss (usually a rapid onset in the newly diagnosed Type 1 diabetes mellitus patients)
- A patient history of noncompliance with prescribed insulin therapy (due to coexisting medical issues in which patient may have intentionally stopped insulin due to decreased food/fluid intake), costs factors (unable to afford prescribed therapy) and missed insulin doses (mechanical failure of the patient’s current insulin delivery system).
Additional signs and symptoms may be present, related to the patient’s age. While an adult patient would be able to verbalize symptoms, a child may not be able to do so, especially in cases where the diagnosis of T1DM is done during their initial presentation to an emergency department for suspected DKA.
In all cases, there may be other factors (illness, injury, medication side effects) that cause DKA to occur; thus, thorough examination and diagnostic testing must be done in all cases prior to initiation of treatment. Likewise, discharge planning and ongoing follow-up care must be patient specific to address behaviors and treatments required for optimal health maintenance.
Teens/Young Adults
In the teenager/ young adult population, the following symptoms may occur: (11)
- Increases in urination, thirst, and appetite.
- Unintentional/ unexplained weight loss despite increases in food and fluid intake.
- Changes in energy level (increased fatigue)
- Vision changes
Please note that normal growth and development stages/patterns in a teenager/young adult will influence glucose metabolism (related to hormone levels).
Young Children
In the young children’s population, symptoms usually strike suddenly and, unlike the adult population, are usually not related to a specific lifestyle or dietary practice. Most children present with the following symptoms:
- Increased urination
- Increased thirst
- Fatigue
- Vision problems (blurred vision)
- Acetone/ketone “fruity smell” on breath
- Unexplained weight loss, often despite appearing to eat (and drink) more.
- Changes in mood and behavior
Infants/Toddlers
In the infant/toddler population, symptoms may present as follows:
- Increased food and fluid intake (always appearing thirsty despite normal fluid intake)
- Frequent urination (in the potty-trained child, this may present as a new onset of bed wetting behaviors)
- Increasing fatigue and changes in normal activity levels
- Unexplained weight loss despite increased food and fluid intake
- Increased occurrences in diaper rashes (suspected increase in yeast infection)
- Fruity/acetone smell to breath
- Unusual behavior (child specific)


Self Quiz
Ask yourself...
- Your patient with DKA appears to be “noncompliant” with his prescribed insulin therapy. What factors may be contributing to his failure to take medication as directed?
- What nursing interventions can be done with/for this patient to increase adherence to his current medication regimen?
- Unexplained weight loss in a young adult may indicate diabetes. What other medical conditions could be causing unexplained weight loss in this age group?
- How would you address these concerns with your patient/ their family members?
Etiology
Etiology: Causes of Diabetic Ketoacidosis
Hyperglycemia and low insulin levels lead to diabetic ketoacidosis. Common causes include the following:
- Acute illness, altering a person’s intake of food or drink, makes glucose management more difficult. This is a two-fold situation. The person with diabetes, recognizing the change in their normal food/fluid intake may also choose to intentionally decrease/skip their routine diabetic medications to avoid episodes of hypoglycemia.
- Insufficient levels of insulin due to the demands of normal growth and development patterns in children and young adults.
- Missed insulin doses (intentional decision to take inadequate doses, inadvertently held doses, inaccurate dose amounts, clogged insulin pump tubing).
Other causes of DKA, unrelated to insulin dose administration, are thought to be related to increased stress levels (inflammation/ infection) and normal hormone disruption, physiologic stressors. Persons with Type 2 diabetes may experience DKA due to prolonged, untreated hyperglycemia. (12), (13)
- Myocardial infarction
- Neurological stroke
- Motor vehicle accident with physical injuries (inflammatory response to blunt force/penetrating trauma)
- Abuse of alcohol and illegal drugs
- Medication side effects (diuretic and corticosteroid *use) see below
- Severe or prolonged illness (such as pneumonia and urinary tract infection/ urosepsis/wound infections)

Self Quiz
Ask yourself...
- Why do you think that the number of diabetes cases continues to rise worldwide, despite advances in medication and related treatment options?
- How do you think the healthcare industry can better address diabetic patient education?
- What factors do you think negatively affect the overall health and well-being of persons with diabetes (lack of care, knowledge deficit, health literacy, access to care, costs of care)?
- What can you do as a healthcare professional to improve the health outcomes of patients with diabetes?
Etiology: Precipitating Factors
Common precipitating factors for diabetic ketoacidosis include the following (14):
- Poor compliance with prescribed insulin therapy (intentional, nonintentional)
- Infections (especially T2DM in the elderly/ adult population)
- Newly diagnosed diabetes (especially T1DM in the pediatric/juvenile population)
- Physiologic based stressors, including coronary syndrome, cerebral vascular accidents, ischemic injuries, shock like states, chronic alcoholism, illicit drug use and certain antipsychotic medications.
Etiology: Diabetic Ketoacidosis and Corticosteroid Use
Diabetic ketoacidosis is related to long term corticosteroid usage. yperglycemia has been reported in a large percentage of patients who are using corticosteroids long term, often as high as “64-71%”. The elevated glucose levels combined with the ongoing physiologic stressors warranting use of these medications, increases the risk of DKA. The benefit/risk of using these medications long term must be assessed, especially in patients with pre-existing metabolic risk factors. Ongoing patient monitoring is essential to lower the risk of long-term complications. (15) (16).
Risk factors that “may” increase the likelihood of developing type 2 diabetes after long term steroid usage include the following:
- Overweight (BMI 25.0 -29.9 percent) / obesity (BMI 30 percent or above)
- History of gestational diabetes
- History of polycystic ovarian syndrome
- History of family members with type 2 diabetes

Self Quiz
Ask yourself...
- Your patient, who is recovering from an acute myocardial infarction, has been started on insulin therapy for hyperglycemia. She is adamant that she is “not diabetic” and refuses to take insulin injections. How would you explain to this patient the connection between physiologic stress and hyperglycemia?
- What patient education, regarding insulin and hyperglycemia, would be appropriate for this patient?
- What follow-up care would be appropriate for this patient?
- Would this patient benefit from a referral to a diabetes education/management program at this time?
Treatment
Emergency Treatment
The initial or emergency treatment of diabetic ketoacidosis may require complex, frequent monitoring, often necessitating an intensive care admission. The following generic guidelines refer to intensive care nursing management. Please refer to your specific organization for nursing protocols related to DKA management. Many facilities have strict admission guidelines to ensure the appropriate use of intensive care resources. With respect to patients with DKA, suitable ICU admissions may include the following:
- A newly diagnosed diabetic during an episode of DKA
- Any infectious disease condition that triggers an episode of DKA
- An episode of DKA occurring concurrently with a physiologic stressor event (acute myocardial infarction, cerebrovascular accident/stroke)
The goals of emergency treatment of diabetic ketoacidosis are multifactorial and listed below. Interventions will include, but not be limited to, insulin intravenous infusions, hourly vital sign monitoring (or more frequent), and hourly glucose checks.
- Treatment/correction of dehydration with IV fluids
- Treatment of hyperglycemia with insulin therapy
- Treatment of electrolyte imbalances
- Treatment/correction of acid-base imbalance
Initial/Emergency treatment of DKA includes (20):
- Initial assessment and stabilization ABC airway, breathing and circulation.
- Aggressive fluid therapy to restore circulating volume.
- Isotonic saline IV infusion
- IV with dextrose component once glucose level 200-250mg/dl

Self Quiz
Ask yourself...
- With regards to your current workplace/unit, are there any specific order sets (“standing orders”) for ICU admissions?
- What “standing orders” are currently in place for a suspected diabetic ketoacidosis patient?
- What additional “order sets” would be initiated if a patient with DKA was found to be febrile (102F) with suspected pneumonia?
Laboratory Findings
The following laboratory ranges provide a generic overview of normal ranges and abnormal findings associated with DKA (17) (18) (19). The confirmation of acute diabetic ketoacidosis is dependent on both laboratory findings as well as patient assessment. Please refer to your specific medical organization (unit specific) for further guidance and treatment parameters.
- Serum potassium levels: Normal range (3.5 to 5.0 mEq/L) hyperkalemia range approximately 5.0 to 5.5mEq/L.
- Serum sodium levels: Normal range (137 to 142 mEq/L) severe hyponatremia range approximately 125mEq/L or lower; severe hypernatremia range above 145mE/L
- Serum Amylase level: Normal range (40 to 140 units per liter) (U/L); may be elevated in cases of pancreatitis/ pancreatic inflammation, which may coexist with DKA
- Serum Lipase level: Normal range (0-160 units per liter) (U/L); may be elevated in cases of pancreatitis/ pancreatic inflammation, which may coexist with DKA
- Serum Osmolality level: Normal range 275-295 mOsm/kg: may be elevated to between 300-320 mOsm/kg in DKA
- Arterial blood gas analysis: Arterial ph below 7.3 (normal range 7.35-7.45)
- Anion Gap: Normal 4-12 mEq/L ; levels above > 10 may indicate existing acidosis in DKA
- Serum glucose level (normal fasting below 100mg/dl). Hyperglycemia range above 250mg/dl
- Serum ketone level (normal negative); serum ketones detected in blood; usually greater than 5mEq/L
- Serum bicarbonate level (normal 22-29 mEq/l); usually less than 18mEq/L
- Anion gap level (normal 4-12mmol/L); usually greater than 12 mmol/L)
| Lab Test | Normal Range | DKA | Comment |
| Potassium | 3.5-5.0 mEq/L | >5-5.5 mEq/L and above | |
| Sodium | 137-142mEq/L |
<125mEq/L hyponatremia >145 mEq/L hypernatremia |
|
| Amylase | 40-140 U/L | >140U/L | Elevated with pancreatitis |
| Lipase | 0-160 U/L | >160U/L | Elevated with pancreatitis |
| Arterial PH | 7.35-7.45 | Below 7.3 | |
| Serum Osmolality | 275-295 mOsm/kg | 300-320 mOsm/kg | |
| Anion Gap | 4-12 mEq/L | >10 mEq/L existing DKA |
|
| Glucose | < 100mg/dl | >250mg/dl | |
| Ketone | Negative | >5mEq/L | |
| Bicarbonate | 22-29mEq/L | <18mEq/L | |
| Anion Gap | 4-12mmol/L | >12mmol/L |
To rule out physiologic stressors associated with the development of DKA (systemic infections, acute myocardial infarction, pneumonia, urosepsis), refer to your medical organization (unit specific) guidelines regarding these additional diagnostics:
- Serial blood and wound cultures
- Serial EKG and Troponin levels
- Sputum cultures and sensitivity
- Urinalysis and culture with sensitivity
- Chest Xray
Fluid Resuscitation Guidelines
The American Diabetes Association (ADA) recommends the following initial fluid resuscitation in the adult population; additional boluses may be required after each hourly reassessment: (21). Please refer to your unit specific guidelines regarding fluid boluses, and fluid resuscitation. Caution in use with patients with preexisting heart failure, kidney failure or other medically indicated “fluid restrictions”.
0.9% SC (Sodium Chloride Solution) initially as a 15–20 mL/Kg bolus for hemodynamic resuscitation
- then 250–500 mL/h of fluid until glucose is normalized (usually faster than DKA resolution)
- then 150–250 mL/h until DKA resolution
- For the replenishment, 0.45% SC (Sodium Chloride Solution) unless hyperglycemia-corrected hyponatremia is present.
In the pediatric population, fluid resuscitation boluses are indicated in children who present with the following symptoms: (22)
- Dry mucus membranes
- Poor skin turgor
- Lethargy; altered level of consciousness.
- Nausea and vomiting
- Tachycardia and tachypnea
- Kussmaul type respirations (deep and labored respiratory breathing patterns)
Fluid recommendation: 10–20 mL/kg bolus of isotonic saline given over 30–60 mins.
Insulin Therapy and Acute Diabetic Ketoacidosis
Intravenous use of insulin is preferred in patients with acute diabetic ketoacidosis, as subcutaneous absorption of insulin would most likely be ineffective in light of dehydration.
Intravenous continuous infusion of insulin at a rate of at 0.14 U/kg/hour or
Insulin bolus of 0.1U/kg, followed by insulin continuous infusion at a rate of 0.1U/kg/hour.
Hourly (or more frequent glucose checks) with a decrease in insulin delivery dose when glucose level is 250mg/dl or less. At this time, insulin dose is further decreased to 0.05 or 0.1U/kg hourly until DKA is resolved.
- Patients, once stabilized and deemed able to eat, can be transitioned to subcutaneous insulin administration and routine glucose monitoring (point of care/ POC glucometers)
Laboratory Tests Guidelines Therapy Goals
- Serum glucose levels below 200mg/dl
- Serum bicarbonate level greater than 15mEq/L
- Serum potassium level 4.0 -5.0 mEq/L
- Venous pH greater than 7.30
- Anion gap equal to/less than 12eEq/l. (23)
Electrolyte Imbalance (Hyperkalemia-> Hypokalemia)
Serum potassium levels are usually high/elevated due to the cellular changes occurring as the result of acidosis and decreased insulin. Electrolyte replacement should be monitored very closely in diabetic ketoacidosis. During the rehydration/ volume restoration phase and insulin administration, extracellular potassium shifts back into the intracellular space (causing hypokalemia). In addition, insufficient insulin levels may deplete various serum electrolytes; thus, frequent serum electrolyte levels with appropriate intravenous replacement ensure proper cellular activity.
Treatment-Related Complications
- Hypoglycemia (blood glucose levels below 70mg/dl); treat; accordingly, patient should be transitioned to subcutaneous insulin injections when serum glucose level 200-250mg/dl, and patient is able to tolerate oral intake.
- Hypokalemia (blood potassium levels below 3-3.4 mmol/L); intravenous therapy to include potassium supplements; oral supplements as tolerated once patient transitions to diabetic diet.
- Cerebral edema
Cerebral Edema
Cerebral edema, or brain swelling, occurs for a variety of conditions (brain tumors, blunt trauma, inflammatory conditions, and even infections). Diabetic ketoacidosis and hyponatremia can cause cerebral edema. (24) Cerebral edema is the leading cause of mortality in children. A normal ICP (intracranial pressure) reading is 7-15mmHG; an increased reading in excess of 20-25mmHG, coupled with the following symptoms, may be indicative of cerebral edema.
Initial symptoms of cerebral edema may include the following:
- Headache
- Visual changes (double vision (diplopia) or blurred vision)
- Changes in speech/ ability to talk/ personality.
- Nausea and vomiting
- Changes in level of consciousness (lethargy-> unresponsiveness)
- Changes in respirations/ difficulty breathing
Symptoms that may indicate worsening of cerebral edema.
- decorticate and decerebrate posturing.
- cranial nerve palsies
- fluctuating level of consciousness
- sustained heart rate deceleration,
- increased vomiting, headache, and lethargy
Confirmation Testing:
- CT (Computerized Tomography) scan
- MRI Magnetic Resonance Imaging
Treatment for DKA Related Cerebral Edema
When cerebral edema is confirmed by radiologic testing, the administration of Mannitol (or hypertonic sodium) is recommended as follows (25) (26):
- 0.5-1 g/kg intravenous mannitol may be given over the course of 20 minutes and repeated if no response is seen in 30-120 minutes.
- If no response to mannitol occurs, hypertonic saline (3%) may be given at 5-10 mg/kg over the course of 30 minutes.
- Additional treatments may be warranted, including diuretics, corticosteroids, and possible surgical intervention (to prevent herniation syndrome).

Nursing Care and Management
Nursing Care: Patient Placement
Initial/hourly (or more frequent) assessment to include the following:
Due to the frequency of monitoring and medication administration during the acute phase of DKA, patients are usually placed in the Intensive Care Unit. ICU treatment often includes hourly physical assessments (intake, output, neurological assessment, vital signs; frequent laboratory testing (glucose testing); and rapid identification of complications (cerebral edema, hypoglycemia, hypokalemia).
Transfer to a step-down unit usually occurs when the patient is fully awake, tolerating oral intake (both solid food and liquids), vital signs are stable, and fluid and electrolyte replacements are complete. The average timeline may be 1-2 clinical days. The focus of care now shifts to discharge planning, patient education, and ongoing management.

Self Quiz
Ask yourself...
- What is your current workplace policy of ICU admissions?
- What parameters are used to determine which in-house unit a patient is transferred to?
- Do you feel that patients with acute DKA could be successfully managed on a step-down unit? Why/Why not?
Nursing Care: Acute Phase
- Monitoring of vital signs, level of consciousness/ neurological status, urine output
- Administration of IV fluids as ordered.
- Frequent blood glucose assessment and insulin administration
Nursing Care: Patient Education, Discharge Planning, and Follow-up Care
- Compliance with medications, healthy diet, glucose monitoring, sick day management
- Signs and symptoms of infection
- Importance of follow-up care with primary medical provider/endocrinologist
- Lifestyle behavior changes (smoking cessation, physical activity, healthy diet)
- Medical Alert ID bracelet or wallet insert regarding chronic medical conditions and medication.
- Coordination of follow-up care to ensure ongoing medical support, educational services and financial assistance when appropriate (medical provider, endocrinologist, pharmacist, social worker/ case management services, DSMES classes) (27)
Patient Education
Diabetes Self-Management Education and Support (DSMES)
The Centers for Disease Control and Prevention offer a Diabetes Self-Management Education and Support Toolkit on their website available to the public, designed for various health organizations/ community organizations and others interested in educating persons with diabetes to live a healthier lifestyle. Studies have shown that people who receive such education have better overall health and wellbeing. Despite these studies, a very low percentage of those qualified to receive such services access them. Check out the link below for more information.
- DSMES Program Review: https://www.cdc.gov/diabetes/dsmes/index.html
- DSMES Tooliit: https://www.cdc.gov/diabetes/dsmes-toolkit/index.html
Additional Resources
The following websites are being provided to assist the healthcare professional in accessing appropriate diabetes related information, including insulin coverage, food insecurities, food bank locations, and DSMES information. https://diabetes.org/
The American Diabetes Association provides information on prediabetes, Type 1, and Type 2 diabetes, as well as gestational diabetes. Included on their website are sections on medications, support groups, diet and activity, advocacy efforts, and prevention efforts. https://www.jdrf.org/
The Juvenile Diabetes Research Foundation is a global organization for Type 1 diabetes mellitus. The site offers information on all things T1DM, including sections for those newly diagnosed, those interested in fundraising, research and clinical trials, daily diabetes management, volunteer opportunities, and access to local chapters worldwide. From the healthcare provider perspective, this website offers continuing education programs and pdf downloads for patient specific education. https://getinsulin.org/
The Get Insulin website provides information for persons with diabetes to access affordable insulin coverage. The site also offers information and guidance on health insurance plans, an insulin related newsletter, and external links to food sources (for patients with food insecurity issues) https://www.feedingamerica.org/find-your-local-foodbank
The Feeding America website enables persons with food insecurities to access food banks in their area, according to state location and zip code.

Self Quiz
Ask yourself...
- What community resources are available to your patients, post discharge, regarding access to food and medications?
- If your patient says they simply cannot afford their prescriptions, what is your current facility policy regarding this matter?
- How would you improve your current facility policy regarding patient access to medications for those uninsured/underinsured?
Patient Education and Follow-up Care (DSMES)
DSMES, or Diabetes Self-Management Education and Support, is the gold standard when it comes to patient education on this chronic medical condition. The goal of this education is to educate and empower the patient to successfully manage their medical condition, in efforts to lower the risk of long term, lifetime complications. DSMES is considered an ongoing process, and is recognized as an integral part of patient education at various critical points in their lifetime:
- At time of initial diagnosis
- During all patient medical appointments and routine follow-up care
- At time of onset for newly diagnosed complications
- Anytime a patient expresses concern over current diabetic management challenges.
Medicare and Medicaid
Medicare (Medicare Part B) and Medicaid plans currently offer the following coverage for diabetes related education (28):
- 10 hours of education (combined individual and group training) for an initial diagnosis of diabetes
- 2 hours of follow-up training annually after initial training completion
Qualifying Labs for DSMES
In general, a patient must be diagnosed with type 1, type 2, or gestational diabetes to qualify for DSMES, such as:
- Fasting Blood glucose of 126 mg/dL on 2 separate occasions
- 2-hour Post-Glucose Challenge of ≥200 mg/dL on 2 separate occasions
- Random Glucose Test of >200 mg/dL with symptoms of unmanaged diabetes
DSME Contents Overview
- Diabetes disease process pathophysiology and treatment to increase risk reduction for long term complications.
- Healthy eating includes meal planning, food label reading, carbohydrate counting, and strategies for eating out.
- Physical activity includes the benefits of activity as they related to better weight control, sleep habits and stress reduction.
- Medication usage overview to include medication administration, side effects, storage and cost issues.
- Blood glucose monitoring and management to include proper use of monitoring devices and associated equipment cleaning/repair.
- Prevention of complications (early detection, treatment, acute and chronic complications such as kidney disease and nerve damage; proper foot care)
- Healthy coping strategies to include stress reduction, effective self-management behaviors, and symptom recognition (hypoglycemia/hyperglycemia)
- Sick day management includes intake/output monitoring, over the counter medication usage, carbohydrate counting, ketone assessment, fever control and when to seek emergency services.
- Problem solving to include diabetes management during emergencies (power outages, flooding, tornados, hurricanes)
For more DSMES information visit: https://www.cdc.gov/diabetes/dsmes/dsmes-living-with-diabetes.html


Self Quiz
Ask yourself...
- With respect to DKA, what aspects of DSMES do you think are most important for patient education?
- How do you assess health literacy in your patients?
- What are some nursing interventions that could be done to assess a patient’s ability to correctly use a glucometer (glucose measuring device)?
- What community resources, post hospital discharge, are available for newly diagnosed patients with prediabetes/ type 2 diabetes in your area?
- What aspect of DSMES do you consider most important for ongoing sick day management education for your patients with diabetes?
Safety Considerations (Sick Day Management)
Successful management (prevention) of diabetic ketoacidosis requires patient education and empowerment in managing situations where glucose levels may be elevated and/or insulin levels (doses) are substandard (29).
There are many situations that can put a patient at risk for the development of DKA, including the following (29):
- Illness (acute and chronic), affecting normal food and fluid intake which negatively affects glucose management.
- Missed medication (insulin therapy) due to a clogged insulin pump tubing, a malfunctioning insulin pump, partial doses/skipped doses of insulin (whether related to costs, cognition, or mental health issues {diabetes distress}),
- Medication side effects
- Concurrent use of alcohol or drugs
- Physiologic stress (heart attack, stroke, physical injury)
Patient Education: Sick Day Management
Home treatment/ self-care (30)
The importance of preplanning cannot be understated. All persons with diabetes should have adequate supplies at home, to address an acute illness, including medications to treat basic symptoms before they escalate. These medications may include over the counter medications to treat pain, nausea, vomiting, diarrhea, as well as adequate supplies to manage their diabetes (alcohol prep pads, syringes, prescription medications).
In addition, it is important to stock up on diabetic friendly foods and drinks to maintain nutrition and hydration levels during an acute illness. Such items might include sports drinks, soft drinks, instant cooked cereals, puddings, soups. In the event that a patient cannot eat their regular meals, the goal is to eat or drink 50 grams of carbohydrate every 4 hours to maintain glucose levels.
Sick Day Management Guidelines
- Monitor glucose levels every 4 hours.
- Stay hydrated – 4 to 6 ounces of fluid every ½ hour to prevent dehydration.
- Daily weight
- Temperature checks (rule out underlying infection)
- Current medication compliance- do not stop taking insulin or diabetic oral agents ** notify provider immediately if you choose to stop medications.
Seek emergency care for the following signs/ symptoms:
- Persistent vomiting/diarrhea to the point that you cannot tolerate any food or fluid intake for several hours
- Ongoing glucose levels above 240mg/dl
- The presence of moderate/high levels of ketones in urine
- Unexplained weight loss during an illness
- Any difficulty breathing
- Fruity/acetone smell on breath
- Changes in gait/balance/ vision
Research Findings
Research: Diabetes Distress and Burnout
Diabetes is a 24/7/365 chronic medical condition. Unlike many conditions that are simply managed with lifestyle changes or a single, once a day medication regimen, diabetes mellitus requires lifelong, around the clock commitment. Whether diet, activity, or medication management, a person with diabetes may easily feel overwhelmed by even the basic requirements for self-management. (31)
Ongoing health challenges, comorbid medical conditions, medication and diet cost issues and family dynamics can all affect a person’s ability to successfully manage any health condition. When emotions (sadness, anger, hostility, frustration, and even fear) become overwhelming, diabetic distress (a feeling of defeat) can often occur. Without prompt, patient specific interventions (mental health services, financial assistance, self-management education), these feeling will progress to diabetic burnout, and increase the risk of unhealthy habits (poor medication adherence and overall glycemic control). (32)
Diabetes distress can easily progress to diabetes burnout without appropriate ongoing medical treatment and mental health interventions. When a person with diabetes reaches the point of burnout, they often appear to disconnect from their routine healthcare, exhibiting indifference towards their overall health and well-being. They may become both mentally and physically exhausted from the daily requirements of this chronic medical condition. At this point, it is not uncommon to observe a person’s total disregard for their ongoing medical treatments, daily medications, routine self-care, and more. Missed medications, missed medical appointments, poor dietary intake, and a visible lack of basic hygienic practices are cause for concern.
A multidisciplinary approach to treating suspected diabetic distress and burnout is highly encouraged. From ongoing education, physical and mental health assessments, and enrollment in therapies (individual therapy sessions, and support groups), the person with diabetes needs a supportive environment in which to become empowered in the self-management of their disease progress. In doing so, it is believed that health outcomes are optimal, and the risk of long-term complications is lowered. (33)

Self Quiz
Ask yourself...
- Why do you think diabetes related distress occurs?
- What external factors affect a person’s ability to manage their diabetes successfully?
- What nursing education can you provide to possibly decrease the likelihood of diabetes distress?
- What areas of discharge planning/discharge instructions and follow-up care positively impact a person’s ability to manage their chronic medical condition?
Reserach: Diabulimia
Bulimia nervosa is a potentially life-threatening eating disorder characterized by episodic binge eating of large amounts of food, followed by forced vomiting and possibly laxative use to then “purge” the food. These alternating behaviors are the result of a person fearful of weight gain and willingness to lose weight in unhealthy ways. (34) (35)
Diabulimia is a serious, life threatening eating disorder affecting persons with Type 1 diabetes. Through intentional restricted/ limited use of prescribed insulin, weight loss occurs. This eating disorder is more common in young female adolescents and young adults. (34) (35)
Signs and symptoms may include the following (34) (35):
- Unexplained weight loss
- Hemoglobin A1C > 9
- Multiple episodes of DKA
- Unfilled insulin prescriptions, missed diabetes related medical appointments,
- Expressed fear of insulin related weight gain
- Anxiety related to body image
- Obsessive interest in calories and dieting

Self Quiz
Ask yourself...
- How would you approach patient education with someone you suspect might be suffering from diabulimia?
- What might be some reasons for repeated DKA related incidents, unrelated to intentional restriction of insulin usage?
- How might you encourage a patient to improve compliance with routine medical appointments/ follow-up care?
- How would you respond to a patient’s concerning comment that “insulin is making me gain unwanted weight”?
- What consultations and referrals/resources would be appropriate for discharge planning of patients with suspected diabulimia?

Self Quiz
Ask yourself...
- How would you approach patient education with someone you suspect might be suffering from diabulimia?
- What might be some reasons for repeated DKA related incidents, unrelated to intentional restriction of insulin usage?
- How might you encourage a patient to improve compliance with routine medical appointments/ follow-up care?
- How would you respond to a patient’s concerning comment that “insulin is making me gain unwanted weight”?
- What consultations and referrals/resources would be appropriate for discharge planning of patients with suspected diabulimia?
Research: Insulin Affordability
For many persons with diabetes, the perceived noncompliance with therapy (on behalf of the healthcare professional) is actually that of a cost related issue. Many persons cannot afford ongoing therapies related to management of this chronic medical condition. In attempts to “cut costs”, patients have admitted to skipping certain medications, cutting medications in half, reducing prescribed doses of insulin, and purchasing poorer quality, less expensive foods (that are often lacking in nutritional value). Poorly controlled / uncontrolled diabetes heightens the risk of both acute and chronic complications.
In an attempt to ensure accessibility and affordability of insulin therapy to persons with diabetes, the Inflation Reduction Act of 2022 in part ensures that persons with diabetes on Medicare pay no more than $35 for a month’s supply of insulin product under their prescription drug coverage. Similar drug coverage benefits were also extended to many state-based insurance plans. (36)
In addition, most Medicaid insurance plans, as well as private insurance companies have now enacted reduced insulin costs/ cost sharing programs. Finally, for patients with no insulin costs benefits, many national insurance providers offer free/ reduced cost insulin through their patient assistance program. For a comprehensive list of these resources, please see the following website link (American Diabetes Association): https://diabetes.org/tools-resources/affordable-insulin
Research: Insulin Delivery Systems
With the creation of advanced insulin delivery /monitoring devices (insulin pumps, and continuous glucose monitoring devices), the person with diabetes is afforded a more streamlined process to control their chronic medical condition. Most patients using such devices report better glucose control {“time in range”}, meaning the time their blood glucose levels remained in an acceptable range, ease of portability (of supplies), increased comfort (no more finger sticks), and decreased rates of anxiety, depression and distress.
The following website links represent various insulin delivery devices. Consider making a resource book containing various delivery devices for your specific unit (or hospital organization). Many have 24/7 customer service representatives available if you need to trouble shoot a device suspected of malfunctioning or require additional staff/patient educational resources.
This list contains a variety of websites but is not all inclusive. If you are caring for a patient with an insulin delivery device in place, please contact that specific company for more directions on its usage, removal, replacement parts and more.
Examples of insulin delivery devices:
- Makers of the MiniMed 780G System and the MiniMed 630G system: https://www.medtronic.com/us-en/healthcare-professionals/products/diabetes/insulin-pump-systems.html
- Makers of the Omnipod 5 and the Omnipod DASH Insulin Management System: https://www.omnipod.com/
- Quick overview of various insulin pumps currently on the market: https://consumerguide.diabetes.org/collections/pumps


Self Quiz
Ask yourself...
- What is your facility’s current policy on patient admissions for DKA that want to wear their insulin pumps while in the hospital?
- Would you feel comfortable allowing a Type 1 diabetes patient, admitted for a medical condition unrelated to diabetes, to continue wearing their insulin pump during their hospital stay? Why/Why not?
Case Studies
Case Study #1
A 3-year-old female child is sent, by ambulance, from her local pediatrician’s office with reports of increased lethargy, increased thirst and appetite, and new onset of bedwetting (child had stopped wearing diapers at age 2.5 years). Parents report that the child’s appetite appears increased lately, but pediatrician noted several pounds weight loss since last visit.
- Based on these signs and symptoms alone, what is your initial diagnosis for this child?
- What are your priority nursing interventions for this child?
- How would you assess hydration status on a 3-year-old child?
The child is diagnosed with new onset Type 1 Diabetes and stabilized in the Emergency Department. The parents of this child are visibly distraught over the diagnosis, stating “no one in our family is diabetic; this can’t be happening”.
- What are some of the initial nursing patient/family education areas you could address at this time?
- What are some in hospital consultations that should be considered for this patient and her family?
- What are some community resources you have in your area that you could offer this family?
Case Study #2
A 78-year-old female, with a previous history of CVA, is transferred to your facility from a local nursing home for evaluation of fever and hyperglycemia. The nursing home staff reported the patients’ blood glucose level was 400mg/dl earlier today and her WBC count was 14,500. Upon arrival, the patient is unresponsive, with a temperature 102F , her glucose is 350mg/dl, with +ketones (moderate) and a urinalysis (indwelling catheter) confirms a UTI.
Patient past medical history includes old CVA, T2DM.
- Based on these signs and symptoms alone, what is your initial diagnosis for this patient?
- What diagnostic studies would be warranted in light of hyperglycemia, fever, urinary tract infection, and altered level of consciousness?
- What questions would you ask the nursing home staff, in light of this patient’s initial presentation?
- When this patient is stabilized for transfer back to the nursing home, what information should be included in the discharge instructions/ transfer of care?
Case Study #3
A 60-year-old male present to the Emergency Department with an Acute Myocardial Infarction.
Patient past medical history includes borderline hypertension, and prediabetic HgbA1C 5.8.
The patient was found to have severe coronary artery disease and received Coronary Artery Bypass Graft x 3. During the immediate post operative recovery phase, he receives insulin therapy to control glucose levels >300mg/dl. He is eventually sent home on insulin therapy, pending follow-up with his cardiologist as well as a new consultation for an endocrinologist.
At the time of discharge, the patient is adamant that he was “prediabetic and could easily control my glucose levels with diet alone”; he doesn’t understand how he is now “an insulin diabetic”.
- What are key points in nursing education for this patient, regarding his new “diabetic status”
- How would you explain to the patient the connection between his myocardial infarction, bypass surgery, and currently elevated glucose levels?
- What nursing interventions can you provide PRIOR to discharge to assess his comfort level with insulin injections and glucose monitoring?
- What community resources are available to your patient for a new diagnosis of diabetes?
- The patient wants to know when he can stop the insulin injections. What is your response?
Successful management of acute diabetic ketoacidosis requires resuscitation with intravenous fluids and insulin therapy, replacement of electrolytes and early identification of any events (medical, surgical, and psychological) that contributed to this medical emergency. With the continued increase in diagnosis of diabetes, and ongoing challenges in healthcare costs and coverage, chronic medical conditions will continue to burden the already overwhelmed healthcare arena. By educating and empowering patients to self-manage their disease process, we can lower the risk of long-term complications and improve health outcomes worldwide.
Conclusion
The International Diabetes Federation reports that, in 2021, approximately 10.5 % of the global adult population (ages 20-79 years old) has diabetes, and that nearly 50% of this population are unaware that they are living with this chronic condition. Left untreated, the rates of long-term, nonreversible complications are quite alarming. (37) By the year 2045, it is projected that 1 in every 8 persons (approximately 12.5 %) will be living with diabetes. This will equate to an increase of 46 percent, with nearly 783 million people being affected. This single health condition will represent staggering health expenditures and increased mortality and morbidity associated rates worldwide.
Diabetes ketoacidosis continues to be a potentially life-threatening complication for persons with diabetes. DKA is also, in most cases, a highly preventable condition, with early identification and treatment. The importance of ongoing, patient specific education to address all aspects of diabetes self-management is a key factor in lowering the occurrence of DKA. Dr William Polonsky, a licensed clinical psychologist and certified diabetes educator, is the President of the Behavioral Diabetes Institute in San Diego, California. With regards to the importance of patient education and empowerment, he said the following:
“Well-controlled diabetes is the leading cause of nothing!” Dr William Polonsky. (38)
As healthcare professionals, we have the responsibility to ensure that our patients with diabetes are afforded the education and ongoing support necessary for them to successfully manage their specific disease process. In doing so, we positively impact patient satisfaction, improve medication adherence rates, and lower the risk of long-term complications.

Self Quiz
Ask yourself...
- Why do you think persons with diabetes become “noncompliant” with their diabetes medications?
- What nursing interventions may increase/improve medication compliance rates?
- What community resources are available in your area to assist those who cannot afford their prescribed medications?
- If a patient tells you they simply cannot afford their medications, what resources are available at your place of employment to assist such financial concerns?
- Have you identified any barriers to patient education at your healthcare organization?
- How will your practice change after reading this course?
Nutrition for a Healthy Heart
Introduction
Research indicates that a heart-healthy diet is a powerful tool for the prevention and control of cardiovascular disease [1]. A heart-healthy dietary approach to wellness emphasizes the intake of the appropriate proportions of macronutrients, essential vitamins, minerals, and fiber while minimizing the consumption of saturated fats, trans fats, cholesterol, salt (sodium), and the reduction of processed foods, trans-fats, and added sugars [2] [3]. The cornerstone of the diet includes an abundance of fresh fruits and vegetables, whole grains, lean proteins, and healthy fats [2].
For healthcare providers and patients, the goal of adopting a heart-healthy diet is multifaceted. The diet aims for a reduction in overall cardiometabolic risk, improving blood pressure, lowering cholesterol levels, reducing the risk of developing heart disease and stroke, and preserving the overall health of the circulatory system [3].
Nurses play a pivotal role in patient education and promoting heart-healthy lifestyles by empowering patients with knowledge and skills related to nutrition and dietary choices. This course aims to equip nurses with comprehensive knowledge of heart-healthy eating principles, enabling them to guide and educate their patients.
The adoption of healthy lifestyle choices, with nutrition being the most important behavioral factor, is estimated to reduce the risk of myocardial infarction (MI) by 81–94% [5][6][7]. In comparison, treatment with pharmacotherapies alone results in a 20–30% reduction [8].


Self Quiz
Ask yourself...
- Why is nutrition considered the most important behavioral factor in reducing the risk of myocardial infarction (MI) compared to pharmacotherapies alone?
Heart Disease: A Brief Overview
Heart disease remains one of the leading causes of morbidity and mortality worldwide, with diet and nutrition playing a crucial role in both its development and prevention [4]. Cardiovascular diseases, also known as CVDs, are the primary cause of death worldwide, claiming an estimated 17.9 million lives per year [4].
Cardiovascular disorders affect the heart and blood vessels, manifesting in coronary heart disease, cerebrovascular disease, rheumatic heart disease, and others. More than four out of five CVD fatalities stem from heart attacks and strokes, with one-third of these deaths occurring in individuals under the age of 70 [4].
The term "heart disease" encompasses various conditions affecting the heart's structure and function, many of which are influenced by dietary habits [9]. Cardiovascular risk factors, including malnutrition, tobacco and alcohol use, stress, obesity, sedentary lifestyle, hypertension, diabetes, hyperlipidemia, and genetic predisposition, can increase an individual's likelihood of developing cardiovascular diseases [10] [12].
The modifiable risk factors include sedentary lifestyle, smoking, high blood pressure, diabetes, hypercholesterolemia [12]. Almost three quarters of patients (73%) had at least three risk factors compared to 31% of healthy subjects.
Family history of cardiovascular disease (CVD) is a significant independent risk factor for premature coronary heart disease (CHD). The risk of premature CHD increases in a linear fashion as the number of affected family members grows. [11]. Cardiovascular risk factors, including malnutrition, tobacco and alcohol use, stress, obesity, sedentary lifestyle, hypertension, diabetes, hyperlipidemia, and genetic predisposition, can increase an individual's likelihood of developing cardiovascular diseases [10].
The five modifiable risk factors include sedentary lifestyle, smoking, high blood pressure, diabetes, and hypercholesterolemia [10]. A higher proportion of cardiovascular patients (73%) had at least three risk factors compared to healthy individuals, where less than one-third had three or more risk factors [10].

Self Quiz
Ask yourself...
- What are the key dietary factors that contribute to the development of cardiovascular diseases (CVDs)?
- How do modifiable risk factors, such as sedentary lifestyle, smoking, high blood pressure, diabetes, and hypercholesterolemia, increase an individual's likelihood of developing CVDs?
- Why is a family history of CVD considered a significant independent risk factor for premature coronary heart disease (CHD)?
Types of Heart Disease / Statistics
There are multiple types of heart disease, each with distinct mechanisms and implications for dietary management [13]. Coronary artery disease (CAD), heart failure, hypertensive heart disease, and arrhythmias represent a fraction of these conditions. The four main types of CVD include coronary heart disease, stroke, peripheral arterial disease, and aortic disease [15].
Coronary artery disease (CAD) is the most common type of heart disease [14]. Cerebrovascular disease is the second leading cause of heart disease. Other forms of heart disease include congenital heart disease, heart valve disease, cardiomyopathy, pericardial disease, arrhythmia, and aortic dissection.
Congenital heart disease (CHD) is the most common type of birth defect, affecting about 1 in 100 babies born in the United States [16]. CHDs can range from mild to severe and can affect the heart's structure, function, or both [16].
Heart valve disease is a condition in which one or more of the heart valves are damaged or diseased, which causes blood to flow backward through the valves, damaging the heart and other organs [17]. Heart valve disease affects 2.5% of the U.S population and can be caused by several factors, including infection, injury, and aging [17].
Heart failure is the heart's inability to pump blood, leading to symptoms such as fatigue, shortness of breath, swelling, chest pain, palpitations, weight gain, swelling in the ankles, legs, and abdomen, bloated or hard stomach, dry and hacking cough, and nausea [18] [19]. More than 6 million adults in the United States have heart failure [18].
Cardiomyopathy represents a collection of diverse conditions of the heart which makes it weaker and less able to pump blood. Cardiomyopathy can be caused by several factors, including infection, toxins, and genetic disorders [20]. Due to the potential for underdiagnosis, estimates of cardiomyopathy prevalence can vary. It is estimated that up to 1 in 500 adults may be affected by this condition [21].
Pericardial disease is a condition that affects the pericardium, the sac that surrounds the heart [22]. This can cause inflammation, infection, or scarring of the pericardium, which can interfere with the heart's ability to function. Pericardial disease can manifest as acute pericarditis, pericardial effusion, cardiac tamponade, or constrictive pericarditis [22].
Arrhythmia is a cardiac disorder characterized by an abnormal heart rhythm, manifesting as tachycardia (excessively rapid heartbeat), bradycardia (abnormally slow heartbeat), or irregular heartbeat patterns [23]. These irregularities can induce symptoms such as palpitations, dizziness, and syncope (fainting episodes) and can arise from various etiologies, including underlying heart conditions, electrolyte imbalances, and adverse effects of certain medications [23]. One in 18 people, or 5 percent of the U.S. population has an arrhythmia with a-fib (atrial fibrillation) being the most common [24].
Aortic dissection is a rare, life-threatening condition in which the inner layer of the body’s main artery (aorta), tears [25]. This can cause blood to leak between the layers of the aorta, which can weaken the artery and cause it to rupture. Aortic dissection can be caused by several factors, including high blood pressure, atherosclerosis, and connective tissue disorders [25].
Aortic dissection affects about 30 in 1 million people each year and more than 13,000 die each year [26]. Aortic dissection is most common in those individuals over the age of 60 and if not treated, the tear can worsen, ripping the outer layer of the aorta and allowing blood to escape the artery [25] [26]. As many as 40 percent of individuals who suffer from an aortic dissection die, and the risk of death increases by 3-4 percent every hour the condition is left untreated [26].

Self Quiz
Ask yourself...
- What are the distinct mechanisms and implications for dietary management of different types of heart disease?
- How do the etiologies and clinical manifestations of heart valve disease, cardiomyopathy, and pericardial disease differ from each other?
- What are the potential consequences of untreated arrhythmias, and how can lifestyle modifications and pharmacological interventions contribute to their management?
- Why is aortic dissection considered a life-threatening condition, and what are the critical steps involved in its diagnosis and treatment?
Evidence on Diet and Heart Health / Diet Options
When considering the diet options for heart health, the Mediterranean diet, DASH diet, and plant-based diets are among the most researched and recommended. These diets share common elements such as an emphasis on whole foods, minimal intake of red meat, and a high volume of fruits and vegetables. Extensive research has demonstrated that the DASH dietary pattern lowers the risk of cardiovascular disease [37]. Numerous prospective studies have demonstrated the consistent benefits of the Mediterranean diet on cardiovascular health [30].
There is substantial evidence that most vascular events may be prevented by avoiding smoking, participating in regular physical activity, maintaining normal body mass index, and eating a healthy diet [27].
Observational studies have demonstrated that dietary patterns rich in fruits and vegetables, excluding white potatoes, are linked to a lower risk of CVD [28] [29]. Regular consumption of whole grain foods has been linked to a reduced risk of cardiovascular disease (CVD), coronary heart disease (CHD), stroke, metabolic syndrome, and various cardiometabolic risk factors, as evidenced by robust observational studies and clinical trials [28]. Numerous randomized controlled intervention studies have demonstrated that replacing refined grains with whole grains leads to significant improvements in cardiovascular risk factors [28] [31].
Except for a small trial that demonstrated a reduction in arrhythmia recurrences among regular drinkers with atrial fibrillation upon alcohol abstinence, no other studies have reported favorable outcomes associated with alcohol consumption for cardiovascular health [32].
Dietary fiber, abundant in plant-based foods like fruits, vegetables, whole grains, nuts, seeds, beans, and legumes, have shown an inverse association with a lower risk of metabolic syndrome and cardiometabolic risk factors [33].
A systematic review and meta-analysis provided evidence that substituting saturated fat with unsaturated fat can improve cardiovascular outcomes and reduce the risk of CVD [34]. Plant-based diets rich in foods like whole grains, fruits, vegetables, and nuts, have been linked to a reduced risk of cardiovascular events and intermediate risk factors [36].
Current evidence does not support the widespread use of high-dose vitamin and mineral supplements for the prevention of cardiovascular disease (CVD) [28].


Self Quiz
Ask yourself...
- What are the common elements shared by the Mediterranean diet, DASH diet, and plant-based diets that contribute to their positive impact on heart health?
- How does the evidence from observational studies and clinical trials support the link between regular consumption of whole grains and a reduced risk of cardiovascular diseases?
- What are the potential mechanisms by which dietary fiber from plant-based foods exerts its protective effects against metabolic syndrome and cardiometabolic risk factors?
Role of Sodium and Fats
Sodium and fats hold significant impact over heart health. High sodium intake is associated with hypertension, a risk factor for heart disease, while certain types of saturated and trans fats, are linked to an increase in LDL cholesterol and the development of atherosclerosis [28]. A systematic review and meta-analysis revealed the detrimental effects of saturated fat on cardiovascular disease (CVD) outcomes and risk factors compared to unsaturated fat. [36]
A strong body of evidence has documented the adverse effects of trans fatty acids on cardiometabolic risk factors [37]. Adhering to current recommendations to replace saturated fat from meat and dairy with nontropical plant oils also lowers dietary trans fatty acids [38].

Self Quiz
Ask yourself...
- How does the consumption of sodium and certain types of fats contribute to the development of cardiovascular diseases?
- What dietary strategies can be implemented to reduce sodium intake and limit the consumption of saturated and trans fats, thereby promoting heart health?
Healthy Eating Tips and Strategies
Incorporating a heart-healthy diet into a patient’s lifestyle requires practical tips and strategies. First, make gradual changes instead of overhauling the entire diet. Meal planning can help with healthier choices.
Setting realistic goals and collaborating with the patients to set achievable dietary goals. Controlling portion size, using smaller plates and bowls, prioritizing low-calorie, nutrient-rich foods like fruits and vegetables and limit high-calorie, high-sodium foods like refined, processed, or fast foods [39].
Paying attention to the amount of saturated and trans fats, cholesterol, and sodium. Suggest lean protein sources such as fish, poultry, beans, and lentils and limit the intake of unhealthy fats and instead opt for healthy fats like those found in olive oil, avocados, and nuts [39].
Consume at least five servings of fruit and vegetables daily [41]. Choose whole grains over refined grains and limit the intake of added sugars [28]. To have more control over the ingredients, cook and consume meals at home and make gradual changes to diet habits and build on those habits over time.

Self Quiz
Ask yourself...
- How can healthcare providers collaborate with patients to set achievable dietary goals that align with their lifestyle and preferences?
- What are some practical strategies for making gradual changes to a patient's diet, ensuring adherence and long-term success in adopting heart-healthy eating habits?
Patient Education
Nurses are well positioned to provide patient education and counseling on heart-healthy eating. The core of patient education lies in translating knowledge into practice. Nurses must communicate with consideration of cultural, linguistic, and individual patient dietary preferences. Education should be patient-centered, with actionable steps that patients can integrate into their daily lives [40].
Effective patient education strategies can include establishing a rapport, assessing the patient's knowledge, and understanding, tailoring the educational approach, using plain language, incorporating visual aids, encouraging active participation, providing written materials and ongoing support and follow-up, and addressing any barriers and concerns [42].

Self Quiz
Ask yourself...
- How can nurses tailor their patient education strategies to address individual cultural, linguistic, and dietary preferences, ensuring that the information conveyed is relevant, understandable, and actionable for each patient?
Resources
A wealth of resources is available to support nurses in their role as patient educators, from professional organizations like the American Heart Association to local community programs and online platforms [43]. These resources offer educational materials, dietary guidelines, and support tools that nurses can utilize to enhance their teaching.
A heart-healthy diet is one that is low in saturated and trans fats, cholesterol, and sodium. It is also high in fiber, fruits, vegetables, and whole grains [2][3]. Eating a heart-healthy diet can help to lower your blood pressure, cholesterol levels, and risk of heart disease [2].
The National Heart, Lung, and Blood Institute (NHLBI) has a website with information on heart-healthy eating, including recipes, meal plans, and tips for eating out. The American Heart Association (AHA) has a website with information on heart-healthy eating, including recipes, meal plans, and tips for shopping for heart-healthy foods.
The Dietary Approaches to Stop Hypertension (DASH) diet is a heart-healthy eating plan that has been shown to lower blood pressure [45].
The Mediterranean diet is a heart-healthy eating plan that has been shown to have several health benefits, including reducing the risk of heart disease, stroke, and type 2 diabetes [44]. You can find information about the Mediterranean diet on the Mayo Clinic website.
In addition to these websites, there are many cookbooks and other resources available on heart-healthy eating. Patients can also talk to their doctor or a registered dietitian for personalized advice on how to eat a heart-healthy diet.

Self Quiz
Ask yourself...
- How can nurses utilize the wealth of resources available, such as those from professional organizations and online platforms, to enhance their patient education on heart-healthy eating?
- How can nurses convey the key principles of heart-healthy eating, such as limiting saturated and trans fats, cholesterol, and sodium while emphasizing fiber, fruits, vegetables, and whole grains?
- How can nurses guide patients towards reputable and reliable resources, such as those from the National Heart, Lung, and Blood Institute, the American Heart Association, and the Mayo Clinic, to ensure that they have access to accurate and evidence-based information on heart-healthy eating?
Conclusion
In conclusion, adopting a heart-healthy diet is a crucial step towards maintaining cardiovascular well-being and overall health [30]. The nurse's role as a patient educator in promoting a heart-healthy diet is pivotal. By leveraging a position of trust and frequency of contact with patients, nurses can champion dietary choices that can reduce the risk and impact of heart disease.
Research underscores the importance of a balanced intake of nutrients to support the cardiovascular system's health, emphasizing whole foods, lean proteins, healthy fats, and a reduction in sodium, saturated fats, and sugars [3].
Patients adopting a heart healthy diet require a multifaceted approach, combining knowledge with actionable steps that are practical and sustainable. The role of healthcare professional is instrumental in this dietary transition.
A heart-healthy diet offers a multitude of benefits beyond reducing heart disease risk. It can improve blood pressure control, lower cholesterol levels, promote healthy weight management, and enhance overall energy levels [2][3]. A heart-healthy diet can contribute to a stronger immune system, reduced inflammation, and improved mental clarity [46].

Self Quiz
Ask yourself...
- How can nurses bridge the gap between knowledge and practice when educating patients about heart-healthy eating, ensuring that patients understand the rationale behind dietary recommendations and can translate that knowledge into sustainable dietary changes?
- How can nurses emphasize the broader health benefits of a heart-healthy diet beyond reducing heart disease risk, motivating patients to adopt sustainable dietary changes for their overall well-being?
Adverse Childhood Experiences
Introduction
All children should grow and thrive in a caring, nurturing environment that meets their physical, emotional, and social needs. However, many are not so fortunate. Nearly every two in three Americans (64%) have experienced adverse childhood events (ACEs) (1, 2, 4, 5).
ACEs are highly associated with future chronic health conditions, mental illness, premature death, and more (1). In fact, the more ACEs an individual has had, the higher their risk for having poor health outcomes as adults (13).
Fortunately, there are preventive and protective measures that can be taken with the appropriate resources (1). With better awareness of ACEs and the right support in place, healthcare professionals can help improve the quality of life for a myriad of children and the adults they grow up to be.
Definition
Adverse childhood events, or ACEs, can occur from birth until age 18, and are great determinants of future health (1). These are any potentially traumatic events that happened to a child. ACEs are strongly linked to mental and physical disease in adults, contributing to at least half of the leading causes of death in the United States (1).
The ACE score is a 10-item survey to identify any negative occurrences a person had before their 18th birthday (3). The higher a person’s ACE score, the more risk they have for an unhealthy adulthood (1,2).
ACE was a term coined in a large-scale study published in 1998, describing them as childhood abuse and household dysfunction in seven specific areas (1, 2). In subsequent years, three more areas were added (3, 13). Altogether, the ten ACEs are comprised of the following examples of three broad categories:
- Childhood abuse
-
- Psychological
-
- Physical
-
- Sexual
- Household dysfunction
-
- Substance abuse
-
- Mental illness
-
- Parent treated violently.
-
- Family member incarcerated.
- Neglect
-
- Emotional
-
- Physical

Self Quiz
Ask yourself...
- How would you briefly define adverse childhood experiences (ACEs)?
- Would you add or subtract anything from the list above?
- What other examples of ACEs exist?
- Should one’s community and environment factor into ACEs as well? Why or why not?
Statistics and Demographics
The initial adverse childhood experience (ACE) study, conducted in the late 1990s, included over 17,000 adult participants and revealed the following key demographic data (1, 2, 5):
- Nearly 66% of women and 62% of men reported at least one ACE in their lives.
- More than 1 in 6 people (17.3%) said they had experienced four or more types of ACEs.
- Respondents’ races who reported ACEs were: 74.8% white, 11.2% Hispanic, 7.2% Asian/Pacific Islander, 4.5% black, and 2.3% other.
- About 49% of those with college degrees experienced at least one ACE, compared to 44% without a high school diploma.
- The age group who reported the highest incidence of ACEs was those from 35-49, where almost 70% had experienced at least one ACE. The lowest incidence was reported by those aged 65 and older, at 40%.
- Of all women reporting ACEs, 25% said they endured sexual abuse, 30% witnessed substance abuse in the home, and 25% of the respondents’ parents got divorced.
- Of all men reporting ACEs, 30% went through physical abuse, 24% saw substance abuse at home, and 22% of their parents were divorced.
More recent data shows that at least 50% of the top causes of death in the US are associated with ACEs (6). As there is also a high association between ACES and depression, preventing these experiences could reduce adult depression by 44% (6).

Self Quiz
Ask yourself...
- Did any of the statistics surprise you? Why or why not?
- Reflect on your own life. How many of the 10 ACES might you have had, and how might you be able to manage them as an adult?
- What other data gathering might be useful when it comes to identifying and preventing ACEs?
- What would you identify as some of the highest risk factors for the occurrence of ACEs?
Causes and Risk Factors
The causes of adverse childhood events are varied and multifaceted. They can stem from familial or communal challenges, often referred to as social determinants of health. Many of these determinants can cause ACEs, and may include (8):
- Lack of access to healthcare or other resources
- Financial difficulties
- Homelessness or frequent moving
- Discrimination
- Any type of disrupted living situation
As noted earlier, most of the American population has had some sort of adverse childhood experience. However, there are some factors that make it more likely for these to occur. Societal, communal, and familial cultures all play a role in adverse experiences.
The following situations or conditions increase the likelihood of ACEs (7):
Community Risk Factors:
- High rates of poverty, crime, and violence
- Limited educational, economic, and employment opportunities
- Lack of community activities for youth
- Unstable housing and frequent moves by community residents
- Readily accessible alcohol and drugs
- Frequent experiences of food insecurity
Family and Individual Risk Factors:
- Social or developmental disabilities or delays
- Mental or chronic physical illnesses
- A history of abuse experienced by caregivers themselves.
- Youth dating or engaging in sexual activity early.
- Single-parent families, particularly those with young caregivers
- Low income and/or high economic stress
- Low education levels
- Children with few or no friends, or friends who partake in delinquent or aggressive behaviors
- Caregivers with limited understanding of child development
- Use of spanking or other corporal punishment as a form of discipline
- Inconsistent discipline and/or little parental supervision
- Families isolated from extended family, friends, and/or neighbors

Self Quiz
Ask yourself...
- In the community where you live, what might be some factors that contribute to ACEs in those around you?
- What are some ways your community might be able to mitigate some of the risk factors for ACEs?
- Since nearly two in three people have experienced an ACE in their lives, it is likely that you interact with someone affected by this issue. What resources might you recommend to them, and what else might help?
Cultural Considerations
Though many people experience ACEs, some populations are affected disproportionately. This includes women and those in racial or ethnic minorities, who are at greater risk for experiencing 4 or more ACEs (6, 8). Specifically, African Americans, American Indians, and Alaska Natives (AI/AN) are far more likely to have multiple ACEs than any other race or ethnicity (9,10).
The AI/AN community is a relatively young one, with poverty rates up to four times higher than the national average (10). Furthermore, the AI/AN group is often lumped together as “other” as a race category on surveys, making data harder to come by for this population (10).
AI/AN children, when compared to the total US population, are more likely to have:
- Parents who are divorced (33% versus 21%)
- Lived with someone who abused a substance (24% versus 12%)
- Witnessed domestic violence (15% versus 6%)
- Lived with a parent who ultimately died (4% versus 2%)
Lifespan Impact on the Individual
While adverse childhood experiences affect most Americans, having been through four or more puts a person at significantly higher risk of health problems as an adult (1, 2, 9). In general, the more ACEs an individual has experienced, the more likely they will have poor outcomes later in life, with a specifically high correlation to diabetes, heart disease, obesity, depression, substance abuse, smoking, poor academic achievement, and early death (4).
In fact, ACEs can reduce an individual’s life expectancy by as many as 20 years, compared to someone who has had zero ACEs (8).
The original ACEs study was conducted to determine the link between childhood abuse and adult health risk factors (1). The conclusion was overwhelmingly that in the United States, the main causes of morbidity and mortality are related to many of the health behaviors exhibited by those who have experienced ACEs (1). More recent studies find that ACEs contribute significantly to substance abuse, violence, and self-harming behavior (11).
At least 5 of the top 10 leading causes of death in the United States that are strongly related to ACEs include (9,11, 12):
- Heart disease (#1 cause of death)
- Stroke (#5)
- Chronic lower respiratory diseases (#6)
- Diabetes (#8)
- Chronic liver disease and cirrhosis (#9)
As far as mental health goes, the link with ACEs is clear: The higher one’s ACE score, the more likely they are to be depressed, experience impaired work performance, and have suicidal tendencies (13). Harmful behaviors associated with high ACE scores include smoking, drinking, and drug abuse, as these methods are often used to cope with past traumatic experiences (13).

Self Quiz
Ask yourself...
- In light of the correlation between ACEs and some of the top causes of mortality in the US, what interventions could possibly be made in childhood to prevent these deaths from occurring?
- Though the top 10 causes of death in the US have a variety of causes, the link between ACEs has been well-established for nearly three decades. Why do you think more funding and attention aren’t given to this matter?
- What other physical or mental health concerns not listed above might a person with a high ACE score have?
Societal Implications
Adverse childhood events are preventable and have been shown to contribute to at least half of the leading causes of death in the United States (1, 9, 11). Thus, the impact of ACEs on public health is vast. Since the CDC considers ACEs a public health concern, it is of utmost importance to decrease their incidence (1). Through the reduction and prevention of ACEs, general public health would improve markedly, drastically cutting down on healthcare costs and resources (1, 5, 6, 9).
The societal implications for reducing ACEs are manifold:
- Dramatic reduction of preventable causes of death
- Longer lifespans for the general population
- Better mental health
- More cost-effective physical and mental healthcare
- Lower rates of disease and depression in the general population

Self Quiz
Ask yourself...
- What other societal impacts might ACEs have?
- How could you go about preventing some ACEs in your own life or community?
- What are some local, national, or global resources to which you could introduce those in need?
Ways to Mitigate ACEs
Though ACEs are widely pervasive in American society, they need not be so. With proper resources and support systems, many -if not all- ACEs may be eradicated. The best way to mitigate ACEs would be to prevent them in the first place (4). This requires creating safe, stable, nurturing environments for children and their families (9). Furthermore, as ACEs can occur for a wide array of reasons, they need to be addressed at both the family and communal levels.
With individuals, a first step would be prevention of ACEs in the home. This could involve a vast array of mental health, education, and social work services such as: home visits, parenting classes, therapy sessions, and more (8, 9). Different emotion management techniques and child development concepts could be taught to at-risk families, promoting bonding and trust between children and their caregivers.
High-quality childcare and after-school programs with trusted adults can help mitigate ACEs as well (9). Screening for ACEs at regular intervals would also be helpful. This could include annual check-ups at the doctor’s office, visits with the school nurse or counselor, or a consultation with a home health provider. Medical management of physical and mental health conditions would be made available, including routine health screenings and necessary medications (4, 8, 9).
At the community level, prevention could take the form of free education for family members, food and housing assistance, adequate access to healthcare services, and fostering safe neighborhoods (4, 9). Economic support for families could include family-friendly work policies, earned income tax credits, and so forth. Children could partake in community events like after-school clubs and sports, helping them build bonds with trusted and supportive adults.
Three principles are the most helpful preventing long-term effects of ACEs, (4):
- Reducing stress by ensuring basic needs are met, as well as tending to abusive situations, community crime, substance abuse, discrimination, and poverty.
- Strengthening life skills can strengthen the resilience of children and their family members by practicing planning, focus, and self-control.
- Building responsive relationships by having adults listen to their children and respond adequately to their needs, thereby fostering a safe, trusting relationship.

Self Quiz
Ask yourself...
- What specific local resources are available where you live or work that could help prevent ACEs from occurring in the first place?
- What types of secondary and tertiary prevention resources can you identify for ACEs?
- What are other ways ACEs can be mitigated or prevented at the state or federal level?
Reporting ACEs
Considering there are various types of ACEs, they can be difficult to identify and thus report. However, some are clear-cut. In situations where child abuse or neglect is occurring or suspected, a mandated reporter (e.g., nurse, teacher, counselor) would need to report it as soon as possible. If the child is in imminent danger, take them to a safe place and make a report.
To report child abuse in the United States, call or text 1-800-4-A-CHILD (1-800-422-4453). The website is https://www.childhelphotline.org/.
If there is suspicion that a child is being sexually exploited, the phone number to call is 1-800-THE-LOST (1-800-843-5678), and the website is https://report.cybertip.org/.
To report human trafficking, call 1-888-373-7888, use TTY at 711, text BEFREE (233733), or visit the website at https://humantraffickinghotline.org/.
For anyone experiencing feelings of self-harm or suicide, 988 is the national Suicide and Crisis Lifeline that can be called or texted. The website is https://988lifeline.org/.
Support and Additional Resources
While there is no single way to prevent ACEs from occurring, there is a plethora of resources available to help mitigate the effects and to educate others. Visting a healthcare provider can connect a patient to mental health professionals, support groups, or specialty services like social work and support groups (8).
The Substance Abuse and Mental Health Services Administration (SAMHSA) has an abundance of resources on topics like trauma-informed care, early childhood mental health programs, Native Connections for the AI/AN population, school, and campus health, and much more. More information can be found at https://www.samhsa.gov/programs.
Healthy Outcomes from Positive Experiences (HOPE) is a national resource center offering research, training, and technical assistance in order to better the lives of children and their families. Their website is https://positiveexperience.org/.
The Centers for Disease Control and Prevention (CDC) offers ACE-specific information at this website: https://www.cdc.gov/violenceprevention/aces/resources.html.
Conclusion
Adverse childhood events, or ACES, affect the majority of the American population. Strongly correlated with many leading causes of death, ACEs are preventable and warrant attention from healthcare providers and the general public alike. Fortunately, many resources exist at the individual, community, and national levels to provide care and prevention for these experiences.
Though ACEs tend to lead to negative health outcomes, they need not condemn a person to lifelong problems. Through screening tools, community food and housing programs, mental health assistance, education, and adequate medical care, ACEs can be mitigated, well managed, and prevented.
Despite the misfortune in a child’s life, there is still much hope available when they reach adulthood.
Conclusion
Adverse childhood events, or ACES, affect the majority of the American population. Strongly correlated with many leading causes of death, ACEs are preventable and warrant attention from healthcare providers and the general public alike. Fortunately, many resources exist at the individual, community, and national levels to provide care and prevention for these experiences.
Though ACEs tend to lead to negative health outcomes, they need not condemn a person to lifelong problems. Through screening tools, community food and housing programs, mental health assistance, education, and adequate medical care, ACEs can be mitigated, well managed, and prevented.
Despite the misfortune in a child’s life, there is still much hope available when they reach adulthood.
SSRI Use in Anxiety Disorders
Introduction
Selective Serotonin Reuptake Inhibitors (SSRIs) are a medication class typically used to treat depression. SSRIs are considered first-line treatment for depression and other psychological disorders, including (2):
- Major Depressive Disorder
- Generalized Anxiety Disorder
- Bulimia Nervosa
- Bipolar Depression
- Obsessive-Compulsive Disorder
- Panic Disorder
- Premenstrual Dysphoric Disorder
- Treatment-Resistant Depression
- Pot-traumatic Distress Disorder
- Social Anxiety Disorder
Additional disorders may be treated off-label, including (2):
- Binge Eating Disorder
- Body Dysmorphia Disorder
- Fibromyalgia
- Premature Ejaculation
- Paraphilias
- Autism
- Raynaud’s Phenomenon
- Vasomotor symptoms associated with menopause.
SRRIs remain relatively safe, tolerable, and efficient in treating patients (2).
Fluoxetine
The Fluoxetine drug class includes brand names of Prozac, Rapiflux, Sarafem, and Selfemra
(11).
Indications
Fluoxetine is an FDA-approved medication used to treat major depressive, obsessive-compulsive, binge eating, premenstrual dysphoric, and panic disorders. Fluoxetine is also prescribed for bulimia and bipolar depression.
Off-label uses include social anxiety disorder, adult post-traumatic stress disorder (PTSD), borderline personality disorder, Raynaud phenomenon, and selective mutism (21).
Mechanisms of Action and Pharmacokinetics
Fluoxetine blocks the reuptake of serotonin into the presynaptic serotonin neurons. This is accomplished by blocking the reuptake transporter proteins located in the presynaptic terminal. There have been some indications of mild activity at the 5HT2A and 5HT2C receptors. Conversely, there is minimal activity on noradrenergic reuptake (21).
Fluoxetine produces an activating effect that takes two to four weeks to see antidepressant effects. Fluoxetine actives norfluoxetine, a metabolite produced when cytochrome p450 enzyme acts on it. This indicates that fluoxetine has a high risk for drug-drug interactions that metabolize at the CYP2D6 isoenzyme (21).
Fluoxetine has a half-life of two to four days. Fluoxetine’s active metabolite, norfluoxetine, has a longer half-life of seven to nine days (21).
Contraindications and Precautions
Fluoxetine is contraindicated in patients with (21):
- Hypersensitivity to fluoxetine or its components
- Use of monoamine oxidase inhibitors (MAOIs) to treat psychiatric disorders
- Prescribers should discontinue MAOIs for > 2 weeks before initiation of fluoxetine
- Prescription of:
- Linezolid
- Pimozide
- Thioridazine
- Tamoxifen
- History of seizures
- Elderly patients
- Suicidal thoughts or ideation
- Especially in pediatric patients or those aged 18 to 24 years old
- Monitor closely for the first two months of initiating therapy
- Especially in pediatric patients or those aged 18 to 24 years old
- During pregnancy
- Use in early pregnancy increases the risk of septal heart defects
- After 20 weeks, it is linked with a possible risk for pulmonary hypertension in newborns
- This may increase the risk of gestational hypertension and preeclampsia
- Breastfeeding
- Trace amounts found in breast milk
Precautions should be taken when prescribing Fluoxetine in patients with liver cirrhosis, as this diagnosis reduces clearance of fluoxetine and its active metabolite. This increases the elimination or half-life. Lower or less frequent doses should be considered for these patients (21).
Adverse Effects and Black Box Warnings
Fluoxetine’s most common side effects include (21):
- Insomnia
- Nausea
- Diarrhea
- Anorexia
- Dry mouth
- Headache
- Drowsiness
- Anxiety
- Nervousness
- Yawning
- Decreased libido
- Decrease arousal or lubrication
- Bruising
- Hyperhidrosis
- Weight gain or loss
- Decreased orgasm
- Muscle weakness
- Tremors
- Pharyngitis
Less common adverse effects include (21):
- Bleeding
- Seizures
- Suicidal ideation and behaviors
- Especially in teenagers
Most adverse effects will appear upon initiation of treatment and should fade with time. It is advised to wait for side effects to subside before changing treatment, as most side effects are dose- and time-dependent.
If side effects continue after several weeks, dose adjustment then changing medication is recommended (21).
If insomnia is present, patients should take medication in the early morning (21).
A Black Box Warning is present for Fluoxetine, as this medication increases suicidal thoughts and behaviors. Individuals prescribed this medication should be closely monitored, especially teenagers as they are more prone to experiencing these severe adverse effects (5).
Drug Interactions
Fluoxetine interacts with several medications including (22):
- Monoamine Oxidase inhibitors
- Medications that increase serotonin levels
- Tricyclic antidepressants (TCAs)
- Lithium
- Triptan migraine medications
- Certain opioids
- Other SSRIs
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- St John’s Wort
- Medications that raise the risk of bleeding
- Warfarin
- Apixaban
- Rivaroxaban
- Clopidogrel
- Prasugrel
- Pimozide and thioridazine
- Medications metabolized by certain liver enzymes
- Flecainide
- Propafenone
- TCAs
- Benzodiazepines
- Antipsychotics
- Seizures

Self Quiz
Ask yourself...
- What are the different medication names for Fluoxetine’s class of SSRIs?
- What is the primary use of Fluoxetine?

Sertraline
The Sertraline drug class includes the brand name: Zoloft (13).
Indications
Sertraline is FDA-approved to treat the following (20):
- Major depressive disorder
- Obsessive-compulsive disorder (OCD)
- Panic disorder
- Post-traumatic stress disorder (PTSD)
- Premenstrual Dysphoric Disorder (PMDD)
- Social Anxiety Disorder (SAD)
Sertraline may be prescribed off-label for the following disorders (20):
- Binge eating disorder
- Body dysmorphic disorder
- Bulimia Nervosa (BN)
- Generalized Anxiety Disorder (GAD)
- Premature ejaculation
Mechanisms of Action and Pharmacokinetics
Sertraline inhibits serotonin reuptake on the presynaptic terminals. This leads to an accumulation of serotonin, leading to better mood regulation, personality stability, and wakefulness or arousal (20).
Sertraline has a half-life of 24 to 32 hours. Sertraline is metabolized by the liver (7).
Contraindications and Precautions
Sertraline is contraindicated in (20):
- Patients with hypersensitivity to this drug or any of its components
- Coadministration with:
- Thioridazine
- Pimozide
- Monoamine oxidase inhibitors
- Sertraline should not start <2 weeks of discontinuing any monoamine oxidase inhibitors, as this may lead to toxicity with serotonin syndrome.
- Serotonergic medication
- Disulfiram
- may cause an alcohol-disulfiram reaction.
Adverse Effects and Black Box Warnings
Sertraline has multiple adverse effects, including (20):
- Syncope
- Lightheadedness
- Diarrhea
- Nausea
- Sweating
- Dizziness
- Xerostomia
- Confusion
- Hallucinations
- Tremor
- Somnolence
- Impotence
- Disorders of ejaculation
- Fatigue
- Rhinitis
- Female sexual disorder
More serious adverse effects include (20):
- Prolonged QT interval
- Inhibiting platelet aggregation, leading to bleeding risk
- Serotonin syndrome, including symptoms of:
- Myoclonus
- Muscle rigidity
- Diaphoresis
- Tremor
- Hyperreflexia
- Agitated delirium
- hyperthermia
Sertraline has a Black Box Warning related to increased risk of suicidal thoughts and ideation, particularly in pediatric patients and adult patients aged 18 to 24 (20).
Drug Interactions
Due to Sertraline’s interaction with many CYP enzymes, several drug-drug interactions are possible (7). These include:
- Bepridil
- Bromopride
- Cisapride
- Dronedarone
- Eliglustat
- Furazolidone
- Iproniazid
- Isocarboxazid
- Levoketoconazole
- Linezolid
- Mesoridazine
- Methylene Blue
- Metoclopramide
- Ozanimod
- Phenelzine
- Pimozide
- Piperaquine
- Procarbazine
- Rasagiline
- Safinamide
- Saquinavir
- Selegiline
- Sparfloxacin
- Terfenadine
- Thioridazine
- Toloxatone
- Tranylcypromine
- Ziprasidone

Self Quiz
Ask yourself...
- What are the most common side effects of Sertraline?
- What contraindications are present for Sertraline?
Paroxetine
The Paroxetine drug class includes brand names of Brisdelle, Paxil, and Pexeca (19).
Indications
Paroxetine is FDA-approved to treat the following disorders (19):
- Major depressive disorder (MDD)
- Obsessive-compulsive disorder (OCD)
- Social anxiety disorder (SAD)
- Panic disorder
- Post-traumatic stress disorder (PTSD)
- Generalized anxiety disorder (GAD)
- Premenstrual dysphoric disorder (PMDD)
- Vasomotor symptoms associated with menopause
Paroxetine is prescribed off-label for the following disorders (19):
- Obsessive-compulsive disorder (in children and adolescents)
- Social anxiety disorder
- Dysthymia
- Body dysmorphic disorder
- Postpartum depression
- Premature ejaculation
- Malignancy related to pruritus
- unresponsive to standard treatment
Mechanisms of Action and Pharmacokinetics
Paroxetine blocks the serotonin reuptake transports (SERT), increasing the concentration of synaptic serotonin. The diminished serotonin concentration induces the upregulation of serotonergic receptors. Paroxetine induces the downregulation of upregulated serotonin receptors to balance the receptor concentration.
Paroxetine has also shown some affinity for muscarinic, adrenergic (alpha and beta), dopaminergic (D2), serotonergic (5-HT2), and histaminergic (H1) receptors – which assist with antidepressant effects (19).
Paroxetine is metabolized via hepatics CYPP450 2D6 and has a half-life of approximately 21 hours (19).
Contraindications and Precautions
Paroxetine is contraindicated in the following situations (19):
- Concurrent use:
- Monoamine oxidase inhibitors (MAOIs)
- Causes serotonin syndrome
- Thioridazine
- Causes cardiac arrhythmias
- Pimozide
- Causes serotonin syndrome
- Monoamine oxidase inhibitors (MAOIs)
Precautions should be taken when prescribing paroxetine with (19):
- Tricyclic antidepressant (TCA) use
- Inhibits TCA metabolism
- Tamoxifen use
- Inactivates tamoxifen
- Any drugs affecting hepatic metabolism
- Pregnant or breastfeeding patients
- Increased risk of cardiovascular malformations in the first trimester
Adverse Effects and Black Box Warnings
Paroxetine has dose-dependent side effects. The most common side effects include (19):
- Alopecia
- Apathy
- Chest pain
- Constipation
- Diarrhea
- Dizziness
- Drowsiness
- Dry mouth
- Eczema
- Edema
- Headache
- Hypomania
- Hyponatremia
- Loss of appetite
- Mania
- nausea
- Palpitations
- Photosensitivity
- Sexual side effects
- Sleep disturbance
- Sweating
- Tachycardia
- Tremor
- Vasodilation
- Weight gain
Discontinuation syndrome is more severe with Paroxetine versus other SSRIs. Withdrawal may occur, and symptoms include (19):
- Dizziness
- Lethargy
- Nausea
- Vomiting
- Headache
- Fever
- Chills
- Vivid dreams
- Electric shock-like sensations
- Dyskinesia
- Anxiety
- Crying
- Irritability
- Depersonalization
A Black Box Warning is present for Paroxetine related to increased suicidal thoughts and behaviors. Anyone under the age of 24 has a higher risk for these serious adverse effects and should be carefully considered and monitored when prescribed (9).
Drug Interactions
Drug-drug interactions for Paroxetine include (19):
- Monoamine oxidase inhibitors (MAOIs)
- Thioridazine
- Pimozide
- Tricyclic Antidepressant (TCA)
- Tamoxifen use
- Any drugs affecting hepatic metabolism

Self Quiz
Ask yourself...
- What are the different medication names for Paroxetine’s class of SSRIs?
- What are the most common side effects of Paroxetine?
Fluvoxamine
The Fluvoxamine drug class includes the brand names Luvox and Luvox CR (16).
Indications
Fluvoxamine is FDA-approved to treat the following disorders (1):
- Obsessive-compulsive disorder (OCD)
- Depression
- Social anxiety disorder
Fluvoxamine has recently been prescribed off-label for the treatment of COVID-19. However, the COVID-19 Treatment Guidelines Panel recommends against it. There is insufficient evidence for the use of fluvoxamine in combination with inhaled budesonide for non-hospitalized patients.
Conversely, patients with are receiving fluvoxamine for underlying treatments should continue therapy if diagnosed with COVID-19 (16).
Mechanisms of Action and Pharmacokinetics
Fluvoxamine blocks the reuptake of serotonin at the sodium-dependents serotonin reuptake transports (SERT). This enhances the action of serotonin on the 5HT1A auto receptors, leading to an increase in the concentration of synaptic serotonin (16).
Fluvoxamine is metabolized by the liver and has a half-life of 12 to 15 hours (4).
Contraindications and Precautions
Fluvoxamine is contraindicated in the following situations (16):
- Concurrent use of:
- Ethanol
- Tobacco
- Comorbidities, as this medication may impact the illness or medications to treat:
- Bipolar disorder
- Bleeding problems
- Depression
- Glaucoma
- Heart-attack
- Heart disease
- Heart rhythm problems
- Hyponatremia
- Mania
- Mental health problems
- Seizures
- Liver disease
Precautions should be taken when prescribing Fluvoxamine to (16):
- Patients who drink or have a history of alcoholism
- Patients with vocations that include operating heavy machinery
- May cause drowsiness
- Patients with bleeding problems
- This medication may increase the risk for bleeding
- Patients who are expecting or trying to conceive
- There is some link between this medication and infertility
Adverse Effects and Black Box Warnings
Fluvoxamine has the following side effects include (16):
- More common side effects include:
- Sexual side effects
- Decreased libido, erectile dysfunction
- Less common side effects include:
- Changes to behavior or mood
- Decreased orgasm
- Difficulty breathing
- Difficulty urinating
- Twitching
- Rare
- Agitation
- Blurred vision
- Chills
- Clumsiness
- Confusion
- Diarrhea
- Fever
- Inability to move eyes
- Decreased or increased ability to move the body
- Menstrual changes
- Nosebleeds
- Overactive reflexes
- Poor coordination
- Red or irritated eyes
- Skin issues include:
- Redness
- Tenderness
- Itching
- Burning
- Peeling
- Restlessness
- Seizures
- Shivering
- Skin rash
- Sore throat
- Sweating
- Excitement that cannot be controlled
- Trembling or shakiness
- Unusual bruising
- Unusual or sudden body or facial movements
- Unusual secretion of milk in females
- weakness
A Black Box Warning is present for Fluvoxamine related to increased suicidal thoughts and behaviors (6).
Drug Interactions
Drug-drug interactions for Fluvoxamine include (16):
- Alosetron
- Pimozide
- Ramelteon
- Thioridazine
- Tizanidine
- Increase side effects
- Monoamine oxidase inhibitors (MAOIs)
- Should not take until MAOIs are discontinued for > 2 weeks
- Linezolid
- Methylene blue injection
- Phenelzine
- Selegiline
- Tranylcypromine
- Buspirone
- Fentanyl
- Lithium
- Tryptophan
- St John’s Wort
- Amphetamines
- Some pain medications
- Blood thinners

Self Quiz
Ask yourself...
- What is the primary use of Fluvoxamine?
- What contraindications are present for Fluvoxamine?
Citalopram
The Citalopram drug class includes the brand name of Celexa (11).
Indications
Citalopram is FDA-approved to treat the following disorders (11):
- Depression in adults
Citalopram is prescribed off-label to treat:
- Obsessive-compulsive disorder (OCD)
- Panic disorder
- Generalized anxiety disorder (GAD)
- Social anxiety disorder (SAD)
- Premenstrual dysmorphic disorder (PMDD)
- Binge eating disorder
- Posttraumatic stress disorder (PTSD)
- Premature ejaculation
- Poststroke depression
Mechanisms of Action and Pharmacokinetics
Citalopram escalates the brain-derived neurotrophic factor (BDNF) in the hippocampus and preferential cortex, which can be decreased in patients with depression (18).
Citalopram is metabolized by the liver and has a half-life of 24 to 48 hours. This may take longer due to hepatic impairment (18).
Contraindications and Precautions
Citalopram is contraindicated in (18):
- Concomitant use of:
- monoamine oxidase inhibitors (MAOIs)
- Serotonin syndrome, including symptoms of:
- Myoclonus
- Muscle rigidity
- Diaphoresis
- Tremor
- Hyperreflexia
- Agitated delirium
- Hyperthermia
- Urokinase
- Pimozide
- Methylene blue
- Linezolid
- Dapoxetine
- Hypersensitivity to the drug or excipient
- Increases thioridazine concentrations
- Lead to dangerous arrhythmias
- Increases thioridazine concentrations
Adverse Effects and Black Box Warnings
Adverse effects of Citalopram include (18):
- Most common
- Drowsiness
- Insomnia
- Dizziness
- Headache (dose-dependent)
- Diaphoresis
- Nausea
- Vomiting
- Xerostomia
- Constipation
- Diarrhea
- Ejaculation disorder (dose-dependent)
- Less common
- Myocardial infarction
- Prolonged QT interval
- Torsades de pointes
- Hemorrhage
- Cerebrovascular accident
- Suicidal ideation
- Manic
- Serotonin syndrome
Citalopram has a Black Box Warning related to increased risk of suicidal thoughts and ideation, particularly in pediatric patients and adult patients aged 18 to 24 (18).
Drug Interactions
Citalopram interactions significantly with the following medications, and should be monitored closely (18):
- Bupropion
- Omeprazole
- Esomeprazole
- Cimetidine
- Fexinidazole
- Voriconazole
- Fluoxetine
- Fluvoxamine
- Fluconazole


Self Quiz
Ask yourself...
- What are the different medication names for Citalopram’s class of SSRIs?
- What contraindications are present for Citalopram?
Escitalopram
The Escitalopram drug class includes the brand name Lexapro (14).
Indications
Escitalopram is FDA-approved to treat the following disorders (8):
- Depressive disorder in adults and adolescents, ages 12-17
- Generalized anxiety disorder for adults and children, ages7+
Escitalopram is prescribed off-label for (8):
- Social anxiety disorder
- Obsessive-compulsive disorder
- Panic disorder
- Posttraumatic disorder
- Premenstrual dysphoric disorder
- Vasomotor symptoms associated with menopause
Mechanisms of Action and Pharmacokinetics
Escitalopram binds to the sodium-dependent serotonin transporter protein (SERT) in the presynaptic neuron. This inactivates the SERT and causes an elevation in the synaptic serotonin levels (8).
Escitalopram is metabolized by the liver and has a half-life of 27 to 33 hours (8).
Contraindications and Precautions
Escitalopram is contraindicated in the following situations (8):
- Hypersensitivity to the medication or any of its components
- Concurrent use of:
- MAOIs
- pimozide
- QT prolongation
- Or family history
Precautions should be taken when prescribing Escitalopram, including assessment and reduction of risk for serotonin syndrome. Medications that should be avoided to prevent this include (8):
- Other antidepressants
- Triptans
- Fentanyl
- Lithium
- Tramadol
- Tryptophan
- Buspirone
- Amphetamines
- St John’s Wort
- Methylene blue
- Linezolid
- MAOIs
If possible, obtaining genetic testing for patients before prescribing could show an individual’s enzyme activity. If the patient is classified as a poor metabolized of the enzyme, CYP2C19, they are at a greater risk for drug reactions and may want to reduce the dose or consider alternative treatment (8)
Adverse Effects and Black Box Warnings
Escitalopram has the following side effects include (8):
- Insomnia
- Sexual dysfunction
- Reduce libido
- Anorgasmia
- Male ejaculatory delay
- Nausea
- Increased sweating
- Fatigue
- Somnolence
- QT prolongation
- Serotonin syndrome
- Rare but serious
A Black Box Warning is present for Escitalopram for increased risk of suicidal ideation. Patients should be closely monitored for behavioral changes or destructive behaviors, particularly in pediatric and adolescent patients (8).
Drug Interactions
Drug-drug interactions for Escitalopram include (8):
- Rasagiline
- Serotonin syndrome risk
- Antiplatelet agents
- Increased risk for bleeding
- NSAIDS
- Upper GI bleeding risk
- Aspirin or dual antiplatelet therapy
- Risk of bleeding
- Other agents that prolong QTc intervals
- Amiodarone
- Especially in patients with chronic kidney disease
- Amiodarone

Self Quiz
Ask yourself...
- What is the primary use of Escitalopram?
- What are the most common side effects of Escitalopram?
Vilazodone
The Vilazodone drug class includes the brand name Viibryd (3).
Indications
Vilazodone is FDA-approved to treat the following disorders (3):
- Depression
Mechanisms of Action and Pharmacokinetics
Vilazodone binds to the sodium-dependent serotonin transporter protein (SERT) in the presynaptic neuron. This inactivates the SERT and causes an elevation in the synaptic serotonin levels (17).
Vilazodone is metabolized by the liver and has a half-life of 25 hours (17).
Contraindications and Precautions
Vilazodone is contraindicated in the following situations (23):
- Concurrent use of:
- MAOIs
- Methylene blue
- Must be discontinued > 14 days before starting Vilazodone
Precautions should be taken when prescribing Vilazodone for patients at risk for (23):
- Suicidal thoughts
- Bleeding risk
- Fractures
- Ocular issues
- Serotonin syndrome
- Sexual dysfunction
- SIADH and hyponatremia
- Mania/hypomania
- Seizure disorder
This medication also poses a risk of discontinuation syndrome and should only be stopped under the direction of a provider throughout monitored time (23).
Adverse Effects and Black Box Warnings
Vilazodone has the following side effects include (3):
- Allergic reaction
- Bleeding
- Irritability
- Confusion
- Irregular heartbeat
- Muscle stiffness
- Sweating high fever
- Seizures
- Chills
- vomiting
- diarrhea
- fatigue
- dizziness
- headache
- sudden eye pain
- changes in vision
- suicidal ideation
- change in sex drive or performance
- dry mouth
- trouble sleeping
A Black Box Warning is present for Vilazodone
Drug Interactions
Drug-drug interactions for Vilazodone include (3):
- Linezolid
- MAOIs
- Methylene blue
- Amphetamines
- Aspirin
- Buspirone
- Diet medications
- Dexfenfluramine
- Fenfluramine
- Phentermine
- Sibutramine
- Headache medications
- Almotriptan
- Eletriptan
- Frovatriptan
- Naratriptan
- Rizatriptan
- Sumatriptan
- Zolmitriptan
- Blood clots medications
- Warfarin
- Enoxaparin
- Daletparin
- Infection treatment
- Clarithromycin
- Itraconazole
- Voriconazole
- Ketoconazole
- Rifampin
- Seizure medications
- Carbamazepine
- Phenytoin
- Digoxin
- Fentanyl
- Lithium
- NSAIDS
- Other antidepressants
- St John’s Wort
- Tramadol

Self Quiz
Ask yourself...
- What are the most common side effects of Vilazodone?
- What contraindications are present for Vilazodone?
Conclusion
Selective Serotonin Reuptake Inhibitors (SSRIs) are a medication class typically used to treat depression. SSRIs are considered the first-line treatment for depression and other psychological disorders. However, many SSRIs can be used to treat various anxiety disorders.
Some of the SSRIs are FDA-approved for the treatment of anxiety, while others the provider may prescribe off-label if circumstances permit. While SRRIs remain relatively safe, tolerable, and efficient in treating patients. providers should pay special attention to serious or life-threatening side effects of SSRIs including suicidal ideation, discontinuation syndrome, serotonin syndrome, prolonged QTc interval, and increased risk for bleeding (2).
Anticoagulant Therapy
Introduction
Anticoagulants are a class of medications that prevent and treat blood clots, or venous thromboembolism (VTE).
The Centers for Disease Control and Prevention (CDC) estimates that around 900,000 people in the United States are affected by some form of venous thrombosis every year. Furthermore, the CDC estimates around 60,000 to 100,000 Americans die from some form of venous thromboembolism each year.
They further state that sudden death is the first symptom that occurs in about 25% of people who have a pulmonary embolism [4]. Thus, healthcare providers must be knowledgeable of the signs and symptoms of venous thromboembolism and the available anticoagulants for prevention and treatment.
Understanding the different pharmacokinetics of anticoagulant medication is essential during drug selection. This course outlines anticoagulant pharmacology and addresses pharmacokinetics, including mechanism of action, side effects, usage, and contraindications.
Definitions
Anticoagulants - medications used to prevent and treat blood clot formation, commonly referred to as “blood thinners” [5].
Venous Thromboembolism - a condition where a blood clot forms in a vein, including deep vein thrombosis and pulmonary embolism, and appears during periods of hemostasis [5].

Self Quiz
Ask yourself...
- What are anticoagulants?
- What is a venous thromboembolism?
Medications Overview
Anticoagulant medications are used for the prevention and treatment of venous thromboembolism in both inpatient and outpatient settings.
The major anticoagulant medication classes include:
- Unfractionated Heparin
- Low Molecular Weight Heparin
- Vitamin K Dependent Antagonists
- Direct Oral Anticoagulants
- Direct Thrombin Inhibitors
- Direct Factor Xa Inhibitors [14]
Unlike anticoagulants, antiplatelets act on platelet formation. Although commonly mistaken as an anticoagulant, they are not a part of this class [14].
Depending on the type of anticoagulant, they have other indications for use, such as:
- Atrial Fibrillation stroke prevention
- Left Ventricular Thrombus
- Left Ventricular Aneurysm
- Prosthetic Heart Valve
- Venous Thromboembolism treatment
- VTE prevention in people with cancer
- Pulmonary Embolism
- Pregnancy
- Heparin-Induced Thrombocytopenia

Self Quiz
Ask yourself...
- What settings are anticoagulants used in?
- What medical conditions can anticoagulants be used for treatment and prevention?
- What are the different classes of anticoagulant medications?
Pharmacokinetics
Unfractionated Heparin
Unfractionated heparin, also known as heparin, is a medication used to prevent excess blood coagulation. It’s used to prevent and treat thrombotic events like deep vein thrombosis (DVT) and pulmonary embolism (PE).
Heparin is also used in patients with atrial fibrillation to prevent blood clot formation and during medical procedures, like dialysis, continuous renal replacement therapy, extracorporeal circulation, and heart catheterizations and surgeries. It’s also used for various off-label indications and usually in inpatient settings, such as acute coronary syndrome, percutaneous coronary intervention (PCI), or as a bridge medication when converting to oral anticoagulants [15].
Heparin works by binding to an antithrombin that inactivates thrombin and thus, blocks the clotting cascade. More specifically, by inactivating thrombin factor IIa and factor Xa, fibrinogen is not converted to fibrin, and in turn, prevents clot formation [15].
Heparin is available via intravenous (IV) and subcutaneous (SQ) forms. Intravenous heparin is infused via continuous infusion until therapeutic levels are achieved, while the SQ form is administered intermittently for VTE prophylaxis. Starting dosages of IV heparin usually begin with a bolus of 80 units per kilogram (kg), and then a continuous infusion rate of 18 units/kg/hour. However, this is dependent on the underlying medical condition being treated and is titrated to achieve therapeutic levels.
In hospital settings, heparin flushes are available to lock and maintain IV-line patency. Additionally, subcutaneous dosages of heparin are weight-based and dependent on the medical condition [15].
Common side effects of heparin include:
- Bleeding
- Thrombocytopenia
- Injection site reactions
- Hyperkalemia
[15]
As bleeding is a common side effect, nurses and healthcare providers must monitor patients for evidence of bleeding. Some signs or symptoms of bleeding can include petechiae, bruising, nosebleeds, hematuria, and bright red or dark, tarry stools. Moreover, heparin-induced thrombocytopenia (HIT) usually occurs within five days of initiating heparin therapy, causing serious adverse effects, like myocardial infarction, stroke, DVT, PE, and even death [15].
Before ordering this medication, healthcare providers should be aware of this anticoagulant’s contraindications. Heparin is contraindicated in individuals who have a platelet count of less than 100,000/mm or they have an active, uncontrolled bleed except if they have disseminated intravascular coagulation (DIC). It should also be avoided in patients with a history of HIT or who cannot have routine blood monitoring of heparin therapeutic levels.
Monitoring the patient’s hemoglobin, hematocrit, and vital signs is also essential to detecting a possible hemorrhage [15].
As heparin affects clotting time, healthcare providers must order therapeutic monitoring for activated partial thromboplastin time (aPTT) and activated clotting time (ACT). Prior to patients being initiated on a heparin infusion, a baseline aPTT level is drawn and then subsequently monitored every 6 hours until a therapeutic aPTT level is achieved. After there are two or more aPTT therapeutic results, then an aPTT is drawn every 24 hours.
The therapeutic range of heparin is typically 1.5 to 2 times the normal range, and titration algorithms are dependent on the healthcare facility’s protocols. ACT monitoring is less specific than aPTT and is typically reserved for PCI or cardiac bypass [15].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of unfractionated heparin?
- What are common side effects and contraindications for unfractionated heparin?
- Which lab value(s) require routine monitoring when administering this medication?

Low Molecular Weight Heparin
Another medication used to prevent excess blood coagulation is low molecular weight heparin (LMWH). This medication is used to prevent venous thromboembolic disease in hospitalized patients and is also used to treat DVT and PE. Low molecular weight heparin is also approved for use and treatment of medical conditions such as ST-elevation myocardial infarction (STEMI), unstable angina, and extracorporeal clot prevention.
Common names of LMWH include enoxaparin and dalteparin [13].
Low molecular weight heparin’s mechanism of action works on the body’s clotting cascade by activating antithrombin III. Once antithrombin III is activated, it binds to factor Xa, which inhibits thrombin activation. Therefore, clot formation is prevented since fibrinogen is not converted to fibrin. This medication’s mechanism of action slightly differs from heparin, as LMWH inhibits factor Xa only, while heparin acts on factor IIa and factor Xa [13].
Low molecular weight heparin is available via subcutaneous injection. Dosages of this medication are typically calculated by body weight and are dependent on whether it’s being used for prevention or treatment. LMWH is typically administered once or twice daily and is safe to administer during pregnancy.
Some adverse effects of LMWH include:
- Bleeding
- Heparin-induced Thrombocytopenia
- Injection site reactions
- Osteoporosis [13].
Some other side effects are spontaneous fracture, hyperaldosteronism, and hypersensitivity reactions. Before prescribing this medication, healthcare providers must be knowledgeable of LMWH contraindications. It’s contraindicated in patients with hemorrhagic disorders, peptic ulcer disease, cerebral hemorrhage, trauma, and recent eye or nervous system surgeries.
Additionally, healthcare providers should caution when prescribing LMWH to patients with chronic kidney disease, as it increases the risk of accumulation in their system. Lower doses may be required for these individuals. A benefit of low molecular weight heparin when compared to unfractionated heparin is that the patient’s aPTT blood levels do not need to be monitored [13].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of low molecular weight heparin?
- What are the common side effects and contraindications of low molecular weight heparin?
Vitamin K Dependent Antagonists
Vitamin K antagonists (VKAs) are a class of anticoagulant medications used in the prevention and treatment of blood clots. Warfarin is a commonly prescribed VKA and other less common VKAs are acenocoumarol, fluindione, and phenprocoumon [7].
Warfarin is approved for the treatment and prevention of pulmonary embolism, venous thrombosis, and thromboembolic complications of heart valve replacement and atrial fibrillation. It’s also used to reduce mortality risk after a myocardial infarction or stroke. Prevention of transient ischemic attack and stroke are additional off-label indications [11].
Vitamin K antagonists act by inhibiting the liver’s vitamin K epoxide reductase complex 1 (VKORC1). This reduces the amount of vitamin K reserves and therefore reduces the production of the body’s clotting factors that require vitamin K. Some clotting factors that are reduced include factors II, VII, IX, and X [7].
Vitamin K antagonists are available in oral form and are typically taken once daily in the afternoon or evening. Warfarin is rapidly absorbed, and onset of action is about 24 to 72 hours. The medication’s therapeutic effects aren’t normally seen until five to seven days after taking the medication. The typical starting dosage is 5 mg but might be less (2.5 mg) in patients who are elderly or who have liver disease [11].
Some common side effects of this class of medications include:
- Bleeding or bruising
- Nausea
- Vomiting
- Abdominal pain
- Altered sense of taste [11].
As VKAs alter the body’s ability to clot, it can cause more serious adverse effects, such as:
- Significant bleeding or hemorrhage
- Purple toe syndrome
- Warfarin-induced skin necrosis
- Calciphylaxis [11].
Warfarin and other VKAs have several contraindications such as gastrointestinal bleeding, cerebral aneurysm, dissecting aortic aneurysm, or other hemorrhagic conditions. Additionally, if the patient has had a recent nervous system, eye, or trauma surgery, then this medication should not be prescribed. Threatened abortion, malignant hypertension, and regional or lumbar anesthesia blocks are contraindications as well [11].
When prescribing VKAs, healthcare providers must order therapeutic monitoring and assess the patient’s prothrombin (PT) or international normalized ratio (INR). INR is usually the preferred method where a baseline level is initially drawn, and then subsequent levels are drawn within a week. The therapeutic range is dependent on the underlying medication condition, where the goal can range from an INR of 2 to 3 for most patients or from 2.5 to 3 for patients with a mechanical mitral valve.
Once the patient has reached their therapeutic goal, levels are typically drawn every four weeks unless there have been changes in their medications. Additionally, patients who take VKAs should have their hemoglobin and hematocrit levels and liver and kidney function checked at least every 6 months [11].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of vitamin K dependent antagonists?
- What are common side effects and contraindications of vitamin K dependent antagonists?
- Which lab value(s) require routine monitoring when administering vitamin K antagonists?
Direct Oral Anticoagulants
Direct oral anticoagulants (DOACs) are a class of anticoagulant medications mainly used to prevent thrombosis formation. There are two main classes of DOACs, which include direction thrombin inhibitors and direct factor Xa inhibitors [6].
Direct Thrombin Inhibitors
Direct thrombin inhibitors (DTIs) are used to treat and prevent thrombosis in patients with heparin-induced thrombocytopenia, acute coronary syndrome, or during percutaneous coronary intervention. Common names of direct thrombin inhibitors include argatroban, bivalirudin, fondaparinux, and dabigatran [9]. Additional off label uses may include anticoagulation during dialysis or renal replacement therapy, and it can be used as an alternative anticoagulant for patients who are resistant to heparin [10].
Direct thrombin inhibitors block coagulation activities that are involved in fibrin clot formation. There are two types of direct thrombin inhibitors, which are univalent DTIs that act by binding to the active site of thrombin, and bivalent DTIs that bind to two sites, the active thrombin site and exosite I.
As the thrombin pathways are blocked and cleavage of fibrinogen to fibrin is prevented, this ultimately inhibits clot formation and coagulation [9]. Some DTIs, like argatroban, are metabolized primarily via the cytochrome P450 enzyme [10].
This class of anticoagulant medications is typically available in intravenous form. However, it is also available in oral form, but dabigatran is the only available oral form. Starting dosages for DTIs depend on the medical condition being treated [9].
Some side effects of DTIs may include:
- Bleeding
- Gastrointestinal symptoms and bleeding
- Hypotension
- Dyspnea
- Fever
- Sepsis
[10]
When DTIs are used during PCI, some potential side effects are back pain, nausea, chest pain, and headache. Contraindications include increased bleeding, a history of medication hypersensitivity, lumbar puncture, and spinal anesthesia [10].
As most patients who are treated with DTIs have HIT, aPTT monitoring is common and the goal is 1.5 to 3 times the patient’s baseline. For patients who undergo PCI, ACT is used, and levels are obtained according to the hospital’s protocol or policy [10].
Direct Factor Xa Inhibitors
Direct factor Xa inhibitors are used to prevent and treat several blood clotting disorders. Examples of direct factor Xa inhibitors include apixaban, rivaroxaban, and edoxaban and they are only available in oral form [9].
These medications are often used to reduce the risk of stroke in patients with atrial fibrillation or other cardiac arrhythmias. Direct Xa inhibitors are also used to prevent and treat conditions like DVT or PE [1]. Rivaroxaban is approved for secondary prevention and adjunct therapy after acute coronary syndrome and peripheral artery disease [12].
Direct factor Xa inhibitors directly bind to factor Xa, preventing it from cleaving prothrombin to thrombin. This results in blocking the propagation phase of the coagulation cascade [9]. It is metabolized via the liver and by the CYP3A4/5 and CYP2J2 mechanisms [12].
Starting dosages of direct factor Xa inhibitors depend on the underlying medical condition. Rivaroxaban usually is started at 20mg daily for atrial fibrillation stroke prevention or 10mg daily for VTE prevention [12].
Some side effects of direct factor Xa inhibitors may include:
- Dizziness
- Hemorrhage
- Abdominal Pain
- Pruritis
- Nausea
[1] [12]
Direct factor Xa inhibitors have several drug interactions and thus, the healthcare provider must review any potential interactions before initiating this medication. Common drugs that have potential interactions are aspirin, ketoconazole, phenytoin, rifampin, and carbamazepine [1].
They are also contraindicated in patients with hepatic and renal impairment, antiphospholipid syndrome, and increased bleeding risk. Most have black box warnings of increased risk of thrombotic adverse events and spinal or epidural hematoma. They should also be avoided in patients who are pregnant or breastfeeding [12].
Although this class of medications does not require routine blood monitoring, the healthcare provider should consider obtaining baseline aPTT, PT, and kidney and liver function.
If the patient is scheduled for surgery with a moderately high risk of bleeding, direct factor Xa inhibitors should be held for at least 48 hours before the procedure [1].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of direct thrombin inhibitors?
- What are common side effects and contraindications of direct thrombin inhibitors?
- What is the pharmacokinetics of direct factor Xa inhibitors?
- What are the common side effects and contraindications of direct factor Xa inhibitors?
Considerations for Prescribers
This section reviews potential considerations when prescribing anticoagulants.
When prescribing anticoagulant medications, healthcare providers must consider and review several factors. First, the route and dosage are typically determined by the setting, inpatient versus outpatient, if it’s being used for prevention or treatment, and the underlying medical condition.
Additionally, healthcare providers should strive to follow current guidelines, approved uses, and hospital protocols when initiating or adjusting these medications. Healthcare providers must review the patient’s medical history, baseline lab values, contraindications, and recommended therapeutic medication range as discussed above.
Low molecular weight heparin is often considered safe during pregnancy [13]. Certain anticoagulants, especially warfarin, should be avoided in patients who are elderly, prone to falls, or have reduced kidney function [11]. Oftentimes, anticoagulants are combined with antiplatelet medications to produce better therapeutic results in certain medical conditions [8].
Healthcare providers should also review the potential common and adverse side effects of anticoagulants with patients. Additionally, as bleeding is a serious adverse effect, they should review potential signs of bleeding, such as dizziness, uncontrolled bleeding to the skin, blood in the stool or urine, and other symptoms [15]. Patients should be instructed to seek immediate medical treatment if they experience any of these symptoms, fall at home, or have another traumatic injury.
In addition, they should be instructed on how to control bleeding when cuts occur to the skin [11]. A common side effect of LMWH is pain and bruising around the injection site. Therefore, patients should understand the importance of rotating injection sites and if side effects become a concern, then an oral alternative should be considered [13].
As periodic blood monitoring is required for many anticoagulants, such as INR, PT, or aPPT, the healthcare provider must review the importance of completing these labs and coming to their scheduled visits [15, 11]. If the patient is non-compliant with laboratory monitoring, then the healthcare provider should consider other alternatives, such are direct oral anticoagulants that do not require routine bloodwork or DTIs that have a wider therapeutic range [6] [9].
In addition, the healthcare provider must be knowledgeable about the potential drug interactions for each medication and dietary concern. For example, patients on vitamin K antagonists should reduce their intake of foods high in vitamin K since it counteracts the therapeutic effects of the medication. They should avoid foods rich in vitamin K, such as spinach, kale, and broccoli [7]. Co-administration of other anticoagulants, aspirin, and non-steroidal anti-inflammatory medications also increases bleeding risk [11].
Most anticoagulant medications can potentially cause toxicity and patients should seek emergency medical treatment. Therefore, healthcare providers must be aware of the signs and symptoms of toxicity and the reversal agent, or antidote, for each medication.
Protamine sulfate is the reversal agent for heparin and low molecular weight heparin. Protamine sulfate is administered via IV push and if administered too rapidly can lead to pulmonary edema, vasoconstriction, and pulmonary hypertension [15]. Vitamin K is the antidote for vitamin K antagonists [11]. Andexanet alfa is the reversal agent for direct factor Xa inhibitors and idarucizumab is approved for the reversal of dabigatran specifically [12].


Self Quiz
Ask yourself...
- What factors should healthcare providers consider when prescribing anticoagulants?
- What are the reversal agents for each anticoagulant class?
- Which anticoagulant medication is often prescribed during pregnancy?
- What health conditions and lab values are important when selecting anticoagulants?
Upcoming Research
This section reviews upcoming research and medications for anticoagulant treatment.
There have been many new anticoagulant medications introduced over the past several years and research continues to evolve for this type of medication. More recently, a newer class of anticoagulant medications called anti-factor XI and Xia inhibitors, affect the factor XI pathway for clot formation. However, it’s still being researched and there are ongoing clinical trials [3].
Moreover, in November 2023, the American Heart Association released promising information about abelacimab, a monoclonal antibody that acts as a factor XI inhibitor, which has been shown to reduce stroke risk in patients with atrial fibrillation. The same report stated that bleeding risk was reduced by more than 60% while taking this medication [2].
Potential factor VII and VIII inhibitors are also being researched [16].

Self Quiz
Ask yourself...
- What new research is there about anticoagulants?
- Which new class of medications has shown promise in reducing bleeding risk in patients with atrial fibrillation?
Conclusion
Anticoagulants are typically indicated for the prevention and treatment of blood clotting conditions, including deep vein thrombosis and pulmonary embolism. However, they have several additional approved and off-label uses. Healthcare providers should understand the pharmacokinetics, potential side effects, and contraindications when selecting an anticoagulant. They should also follow current clinical guidelines and their facility’s protocols for a more evidence-based approach.

Self Quiz
Ask yourself...
- What new research is there about anticoagulants?
- Which new class of medications has shown promise in reducing bleeding risk in patients with atrial fibrillation?
SNRIs for Depression
Introduction
Depression can significantly interfere with daily activities and diminish quality of life among patients who experience it. Major depressive disorder (MDD) is one of the leading causes of the burden for worldwide diseases (5). At the present stage, the first-line treatment of MDD is selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs). Research has found that SNRIs showed faster antidepressant effects than SSRIs (5).
The serotonin norepinephrine reuptake inhibitors (SNRIs) are a family of antidepressants that inhibit the reuptake of both serotonin and norepinephrine; however, it is important to recognize the differences among each specific drug in this class. In this course, we will examine pharmacological properties, clinical indications, mechanism of action, metabolism and excretion, dosing schedules, side effects, and warnings of each SNRI currently approved by the United States Food and Drug Administration (FDA) for the treatment of depression.
Forms and Symptoms of Depression
Depression can have crippling effects. Research suggests that genetic, biological, environmental, and psychological factors play a role in depression (7). Depression can be present with other comorbidities, such as mental disorders, diabetes, cancer, heart disease, and chronic pain. Depression can make these conditions worse, and vice versa. Certain medications have been shown to increase depressive symptoms.
Common forms of depression are: (7)
- Major depression - which includes symptoms of depression most of the time for at least two weeks that regularly interfere with work, sleep, eating, and quality of life.
- Persistent depressive disorder (dysthymia), which often includes less severe symptoms of depression that last much longer, typically for at least two years.
- Perinatal depression - occurs when a woman experiences major depression during pregnancy or after delivery (postpartum depression).
- Seasonal affective disorder – impacted by change in seasons, typically starting in late fall and early winter and improving during spring and summer.
- Depression with symptoms of psychosis - a severe form of depression in which the patient experiences psychosis symptoms, such as delusions or hallucinations
Common symptoms of depression include:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness
- Irritability, frustration‚ or restlessness
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies or activities once enjoyed
- Fatigue or lack of energy
- Aches, musculoskeletal pain, or headaches without injury or obvious causation, and do not improve with medication.
- Gastrointestinal issues
- Difficulty concentrating, remembering, or making decisions
- Poor sleeping patterns
- Changes in appetite
- Suicide attempts or thoughts of death or suicide


Self Quiz
Ask yourself...
- Are you aware of certain biological, environmental, or psychological factors that play a role in depression?
- How would you describe the difference between occasional sadness and depression?
- Can you name common symptoms of depression?
- Which drug class has shown faster antidepressant effects in studies, SSRIs or SNRIs?
Pharmacokinetics of SNRIs
The major mechanism of action of SNRIs is the inhibition of presynaptic neuronal uptake of 5-HT (serotonin) and norepinephrine after release from the synaptic cleft (3). Blocking the reuptake prolongs the presence of monoamines in the synaptic cleft within the central nervous system (CNS). This causes an increase in postsynaptic receptor stimulation and additional post synaptic neuronal transmission (3).
Serotonin
Serotonin, or 5-hydroxytryptamine (5-HT), is a neurotransmitter that has an important role in regulating various activities, including behavior, mood, memory, and gastrointestinal homeostasis (1). It is often referred to as the “feel good hormone” and delivers messages between brain cells, contributing to well-being, mood, appetite, social behavior, as well as helping to regulate the body’s sleep-wake cycle.
Serotonin is synthesized in the raphe nuclei of the brainstem and the enterochromaffin cells of the intestinal mucosa (1). Serotonin is a primary treatment target for major depressive disorder (MDD), post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), and anxiety disorders.
Norepinephrine
Norepinephrine, also known as noradrenaline, is a neurotransmitter in the brain that plays an essential role in the regulation of arousal, attention, cognitive function, and stress reactions. It also functions as a hormone peripherally as part of the sympathetic nervous system in the “fight or flight” response.
During states of stress or anxiety, norepinephrine and epinephrine are released and bind to adrenergic receptors throughout the body which exert effects such as dilating pupils and bronchioles, increasing heart rate and constricting blood vessels, increasing renin secretion from the kidneys, and inhibiting peristalsis.
It works closely with dopamine and serotonin systems and is thought to help mobilize the brain for action, increasing alertness, focus, and the retrieval of memory (4).
The increased availability of serotonin and norepinephrine in the nerve synapse means that information can be transmitted easier from one nerve to another.
There are currently five SNRIs approved by the FDA for use in the U.S.:
- Venlafaxine (Effexor XR)
- Duloxetine (Cymbalta, Irenka)
- Desvenlafaxine (Pristiq, Khedezla)
- Levomilnacipran (Fetzima)
- Milnacipran (Savella)
- Milnacipran (Savella TM) is not approved by the FDA to treat depression, but rather only fibromyalgia. For this reason, this course will not review this SNRI.
As mentioned, all SNRIs regulate serotonin and norepinephrine, but there are subtle differences in how much absorption they prevent and the side effects of each type.

Self Quiz
Ask yourself...
- Do all SNRIs have the same uses?
- Can you define serotonin and norepinephrine in your own words?
- Are you familiar with these SNRIs? If so, have you known patients who have benefited from use?
- How would you describe the relationship between sleep cycles, nutrition, and mood?
Venlafaxine
Venlafaxine (Effexor ™) is approved by the FDA and was the first SNRI approved in the U.S. It is available in an extended-release formula and works by regulating levels of serotonin and norepinephrine.
Uses
- Major depressive disorder
- Generalized anxiety disorder
- Social anxiety disorder
- Panic disorder
Mechanism of Action
Venlafaxine increases serotonin, norepinephrine, and dopamine in the brain by blocking transport proteins and preventing their reuptake at the presynaptic terminal (10). This action leads to more neurotransmitters available at the synapse, which ultimately increases the stimulation of postsynaptic receptors.
Venlafaxine is a bicyclic phenylethylamine compound; it is a more potent inhibitor of serotonin reuptake than norepinephrine reuptake (8). Venlafaxine acts as a selective serotonin reuptake inhibitor at 75 mg, but when a higher dose is given, such as 225 mg/day, it has significant effects on the norepinephrine transporter as well (10). Venlafaxine does not have MAO-inhibitory properties.
Pharmacodynamics
The pharmacodynamics of venlafaxine is as follows: (9)
Absorption: 92-100% absorbed after oral administration.
Distribution: Extensive distribution into body tissues.
Metabolism and Excretion: Extensively metabolized in first pass through the liver. 5% of venlafaxine is excreted unchanged in urine; 30% of the active metabolite is excreted in urine.
Half-life: 3-5 hr.; ODV: 9-11 hr.
Contraindications
- Hypersensitivity
- Precaution advised for use in patients with:
- Cardiovascular disease
- Hepatic or renal impairment
- History of seizures or neurologic impairment
- History of mania
- History of drug abuse
- Angle-closure glaucoma
Obstetrics (OB): Use during pregnancy only if risks are closely examined. There is a potential for discontinuation syndrome or toxicity in the neonate when venlafaxine is taken during the 3rd trimester (9). Venlafaxine is a category C pregnancy drug and can potentially pass into breast milk (8).
Venlafaxine is contraindicated if it causes worsening suicidal ideation, depression, anxiety, and psychosis. Precaution is needed for patients with heart failure patients, hyperthyroidism, and those with recent myocardial infarctions, as it can raise blood pressure and increase heart rate. Venlafaxine raises the risk of seizures, and prescribers should avoid the drug in patients with a seizure disorder (8).
Adverse Reactions / Side Effects
Adverse reactions / side effects of venlafaxine include: (10)
CV: Chest pain, hypertension, palpitations, tachycardia.
Neuro: Abnormal dreams, anxiety, dizziness, headache, insomnia, nervousness, paresthesia.
Dermatology: ecchymoses, itching, photosensitivity, skin rash.
EENT: rhinitis, visual disturbances.
GI: abdominal pain, altered taste, anorexia, constipation, diarrhea, dry mouth, dyspepsia, nausea, vomiting, weight loss.
GU: Decreased libido, erectile dysfunction, urinary frequency, urinary retention.
Hematological: Bleeding.
Serotonin syndrome – a condition of building up high levels of serotonin in the body due to medication use. Although rare, serotonin syndrome is a very serious condition that has a high mortality rate (5). Signs of serotonin syndrome include tachycardia, sialorrhea (excessive saliva production), hyperactive bowel sounds, mydriasis (sustained dilated pupils), hyperthermia, and diaphoresis (6). This condition is caused by combining monoamine oxidase inhibitors, tricyclic antidepressants, triptans, additional serotonin receptor modulators, or over-the-counter drugs such as St. John's Wort (6).
If a clinician is suspecting serotonin syndrome, the Sternbach and Hunter criteria can be useful to help arrive at a definitive diagnosis.
Drug-Drug Interactions
- Concurrent use with MAO inhibitors or serotonergic neurotransmitter systems, including tricyclic antidepressants, fentanyl, buspirone, tramadol, amphetamines, and triptans, may increase the risk of serotonin syndrome (9).
- Concurrent use of NSAIDs, aspirin, warfarin or other drugs that affect coagulation may increase the risk of bleeding.
- Concurrent use of other medications that may increase risk of hypertension.
- Concurrent use with alcohol may cause a rapid release of drug and should be avoided.
- Monitor closely for any changes in behavior that could indicate the emergence or worsening of suicidal thoughts or behavior or depression.
Route and Dosage in Depression
PO (Adults): Tablets: 75 mg/day in 2-3 divided doses; may increase by up to 75 mg per day every 4 days, up to 225 mg/day. Do not exceed 375 mg per day in 3 divided doses.
Extended-release capsules: 75 mg once daily (some patients may be started at 37.5 mg once daily) for 4-7 days; may increase by up to 75 mg/day at intervals for no less than 4 days (not to exceed 225 mg/day).
ALERT: US Boxed Warning
Antidepressants increased the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders (10). Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults older than 24 years old (10).
Venlafaxine is not approved for use in pediatric patients.

Self Quiz
Ask yourself...
- What are the major mechanisms of action for Venlafaxine?
- Can you explain the side effects and contraindications of Venlafaxine?
- Are SNRIs currently recommended for pediatric patients?
- Does an increased dosage of Venlafaxine result in different neurotransmitter activity?
Duloxetine
Duloxetine (Cymbalta ™) has the most FDA-approved uses of any SNRI, and, unlike Venlafaxine, is proven to be effective in the treatment of other conditions, such as neuropathy, fibromyalgia, and osteoarthritis (9).
Drug Class
Selective Serotonin/Norepinephrine Reuptake Inhibitors
Uses
Duloxetine is used for the following conditions: (9)
- Major depressive disorder
- Diabetic peripheral neuropathic pain
- Generalized anxiety disorder
- Chronic musculoskeletal pain (including chronic lower back pain and chronic pain from osteoarthritis)
- Fibromyalgia
Mechanism of Action
Duloxetine inhibits serotonin and norepinephrine reuptake, and also enhances dopamine levels within the prefrontal cortex. This increase in dopamine levels involve the inhibition of norepinephrine transporters, which are particularly attracted to dopamine, making it effective in transporting dopamine and norepinephrine (2). Essentially, inhibition of norepinephrine transporters can cause an increase in dopamine.
The secondary mechanisms of action, in increasing dopamine, is helpful in pain reduction. This occurs due to increased activity of noradrenergic and serotonergic neurons in the descending spinal pathway on the dorsal horn and suppression of excessive input from reaching the brain (2). The perception of pain can be reduced as these signals are interrupted.
Pharmacokinetics
Absorption: Well-absorbed following oral administration.
Distribution: Unknown.
Protein Binding: >90%.
Metabolism and Excretion: Primarily metabolized in the liver via the CYP2D6 and CYP1A2 isoenzymes. Excretion: Fecal is 20%; renal is 70% as metabolites.
Half-life: 12 hr.
Time/Action Profile (Plasma Concentrations):
| ROUTE | ONSET | PEAK | DURATION |
| PO | Unknown | 6 hr. | 12 hr. |
Contraindications:
Contraindications in the use of duloxetine include: (9)
- Hypersensitivity
- Concurrent use of MAO inhibitors or MAO-like drugs (linezolid or methylene blue).
- Severe renal impairment (CCr <30 mL/min).
- Hepatic impairment or substantial alcohol use (increased risk of hepatitis).
Use cautiously in:
- History of suicide attempt or ideation.
- History of mania (may activate mania/hypomania).
- History of seizure disorder.
- Diabetes (may worsen glycemic control).
- Angle-closure glaucoma.
OB/ Lactation: Use while pregnant or breastfeeding only if potential maternal benefit justifies potential risk to infant.
Geriatric Precaution: Appears on Beers list. May worsen or cause syndrome of inappropriate antidiuretic hormone (SIADH) secretion and/or hyponatremia in older adults; closely monitor sodium concentrations.
Adverse Reactions / Side Effects
CV: Hypertension, orthostatic hypotension.
EENT: Increased intraocular pressure, blurred vision.
Endocrine: SIADH.
Fluids and Electrolytes: Hyponatremia.
GI: Decreased appetite, constipation, dry mouth, nausea.
GU: Dysuria.
Neurological: Drowsiness, fatigue, insomnia.
Drug-Drug Interactions
- Concurrent use with MAO inhibitors is contraindicated; wait at least 14 days following discontinuation of MAO inhibitor before initiation of levomilnacipran (9). Concurrent use with MAO-inhibitor like drugs, serotonergic neurotransmitter systems, including tricyclic antidepressants, SNRIs, fentanyl, buspirone, tramadol, amphetamines, and triptans may increase the risk of serotonin syndrome (9).
- Increased risk of hepatotoxicity in patients who abuse alcohol or have alcohol use disorder (9).
- Increased risk of serious arrhythmias when used with thioridazine; avoid concurrent use (9).
- Concurrent use of NSAIDs, aspirin, warfarin or other drugs that affect coagulation may increase the risk of bleeding.
- Concurrent use of other medications that may increase risk of hypertension.
- Concurrent use with alcohol may cause a rapid release of drug and should be avoided.
- Monitor closely for any changes in behavior that could indicate the emergence or worsening of suicidal thoughts or behavior or depression.
Route and Dosage in Depression
PO (Adults): 40-60 mg/day (as 20 mg or 30 mg twice daily or as 60 mg once daily) as initial therapy, then 60 mg once daily as maintenance therapy (9).


Self Quiz
Ask yourself...
- What are the major mechanisms of action for Duloxetine?
- Can you explain the side effects and contraindications of Duloxetine?
- Which of these patient symptoms do you think should be a priority: mild drowsiness or tachycardia?
- Does an increased dosage of Venlafaxine result in different neurotransmitter activity?
Desvenlafaxine
Desvenlafaxine (Pristiq ™) received approval from the FDA in 2008. The drug is similar to Venlafaxine structurally and 10 times more potent in inhibiting serotonin reabsorbing than norepinephrine (6). It has been observed weakly blocking dopamine reuptake, similar to Venlafaxine and Duloxetine.
Uses
Desvenlafaxine is an antidepressant that is an FDA-approved drug to treat major depressive disorder in adults. For healthy women who have contraindications to estrogen, desvenlafaxine has an off-label use to treat hot flashes during menopause (6).
Mechanisms of Actions
Desvenlafaxine is the primary active metabolite of venlafaxine. Therefore, the two agents are structurally similar in that they both contain two chemical rings that are not next to each other. In vitro studies have shown that desvenlafaxine is ten times more selective for serotonin than for norepinephrine, making it similar to the drug duloxetine (6).
Pharmacokinetics
Absorption: 80% absorbed following oral administration.
Distribution: Widely distributed to tissues.
Metabolism and Excretion: 55% metabolized by the liver, 45% excreted unchanged in urine.
Half-life: 10 hr.
Time / Action Profile (Plasma Concentrations):
|
ROUTE |
ONSET |
PEAK |
DURATION |
|
PO |
Unknown |
7.5 hr. |
24 hr. |
Contraindications/Precautions
- Hypersensitivity to venlafaxine or desvenlafaxine.
- Concurrent use of MAO inhibitors or MAO-like drugs (linezolid or methylene blue).
- Should not be used concurrently with venlafaxine.
Use cautiously in:
- Untreated cerebrovascular or cardiovascular disease, including untreated hypertension (control BP before initiating therapy).
- Bipolar disorder (may activate mania/hypomania).
- Moderate or severe renal impairment.
- History of seizures or neurologic impairment.
- Moderate or severe hepatic impairment.
- Angle-closure glaucoma.
OB: Safety is not established in pregnancy. Desvenlafaxine is excreted into breast milk, with one study reporting that peak levels are 3.3 hours after a dose (6).
Adverse Reactions / Side Effects
There is a broad range of general adverse effects that patients have reported with desvenlafaxine. A study comparing desvenlafaxine to a placebo in treating major depressive disorder in adolescents noted the most common side effects to be abdominal pain, decreased appetite, headache, and nausea (6).
Less common side effects were diarrhea, dizziness, and cough.
Abruptly stopping the use of desvenlafaxine can cause irritability, nausea, and headaches (6). Gradually tapering the medication is recommended to avoid such side effects.
Drug-Drug Interactions
- The concurrent use of all SNRIs and MAO inhibitors may result in serious and potentially fatal reactions (it may increase the risk of serotonin syndrome) (9). A period of at least two weeks is recommended between stopping MAO inhibitors and initiating venlafaxine (9).
- Concurrent use of NSAIDs, aspirin, warfarin or other drugs that affect coagulation may increase the risk of bleeding.
- Concurrent use of other medications that may increase the risk of hypertension.
- Concurrent use with alcohol may cause a rapid release of drug and should be avoided.
- Monitor closely for any changes in behavior that could indicate the emergence or worsening of suicidal thoughts or behavior or depression.
Increased risk of hepatotoxicity in patients who abuse alcohol or have alcohol use disorder (9).
Increased risk of serious arrhythmias when used with thioridazine; avoid concurrent use (9).
Route and Dosage in Depression
PO (Adults): 50 mg once daily (range = 50-400 mg/day).
Renal Impairment:
PO (Adults): CCr 30-50 mL/min: 50 mg once daily; CCr <30 mL/min: 50 mg every other day or 25 mg once daily.
Hepatic Impairment:
PO (Adults): 50 mg once daily (not to exceed 100 mg/day).

Self Quiz
Ask yourself...
- What are adverse effects for desvenlafaxine?
- Can you explain why SNRI and MAO inhibitors are contraindicated to use together?
Levomilnacipran
Levomilnacipran (Fetzima ™) is the most recent medication approved for treating major depression.
Levomilnacipran is different from other SNRIs because it has greater inhibition of norepinephrine than serotonin; essentially, it has twice the potency of norepinephrine reuptake inhibition compared to serotonin (3). The more recent FDA approval and relatively lower number of prescriptions may be contributing factors to an overall low volume of research and evidence on this drug.
Levomilnacipran has a one-a-day extended-release form, which makes it easier for patients to stick to its regimen. The drug has no effect on dopamine and affects reuptake inhibition of serotonin and norepinephrine steadily at any dose (3).
Uses
- Major Depressive Disorder
Mechanisms of Actions
Levomilnacipran enhances the amount of serotonin (5-HT) and norepinephrine (NE) activity in the central nervous system by inhibition of reuptake at 5-HT and NE transporters (9). Levomilnacipran has shown to be a more potent inhibitor of NE versus 5-HT transporter (9).
Pharmacokinetics
Absorption: Well-absorbed (92%) following oral administration.
Metabolism and Excretion: Primarily metabolized in the liver via the CYP3A4 isoenzyme. 58% eliminated unchanged in urine; 42% metabolized; metabolites are renally eliminated.
Half-life: 12 hr.
Time/Action Profile (Plasma Concentrations):
|
ROUTE |
ONSET |
PEAK |
DURATION |
|
PO |
unknown |
6-8 hr. |
unknown |
Contraindications/Precautions
- Hypersensitivity to Levomilnacipran or milnacipran.
- Uncontrolled narrow-angle glaucoma.
- Use Cautiously in:
- Hypertension, cardiovascular or cerebrovascular disease (blood pressure should be controlled prior to treatment).
- Bipolar disorder (may activate mania/hypomania).
- Renal impairment.
OB: Use only if potential maternal benefit justifies potential fetal risk.
Geriatric: Consider age-related decrease in renal function, chronic disease state and concurrent drug therapy in older adults; increased risk of hyponatremia.
Adverse Reactions/Side Effects
CV: Hypertension, hypotension, palpitations, tachycardia.
Dermatology: Hyperhidrosis (excessive sweating), rash.
EENT: Mydriasis.
Fluids and Electrolytes: Hyponatremia (in association with syndrome of inappropriate antidiuretic hormone [SIADH]).
GI: Nausea, constipation, decreased appetite, vomiting.
GU: Sexual dysfunction, testicular pain, urinary hesitation, and retention.
Drug-Drug Interactions
- Concurrent use with MAO inhibitors is contraindicated; wait at least 14 days following discontinuation of MAO inhibitor before initiation of levomilnacipran (9). Concurrent use with MAO-inhibitor like drugs, serotonergic neurotransmitter systems, including tricyclic antidepressants, SNRIs, fentanyl, buspirone, tramadol, amphetamines, and triptans may increase the risk of serotonin syndrome (9).
- Concurrent use of NSAIDs, aspirin, warfarin or other drugs that affect coagulation may increase the risk of bleeding.
- Concurrent use of other medications that may increase the risk of hypertension.
- Concurrent use with alcohol may cause a rapid release of drug and should be avoided.
- Monitor closely for any changes in behavior that could indicate the emergence or worsening of suicidal thoughts or behavior or depression.

Self Quiz
Ask yourself...
- What are the major mechanisms of action for Levomilnacipran?
- Does an increased dosage of Levomilnacipran result in different neurotransmitter activity?
Review of SNRI Pharmacokinetics
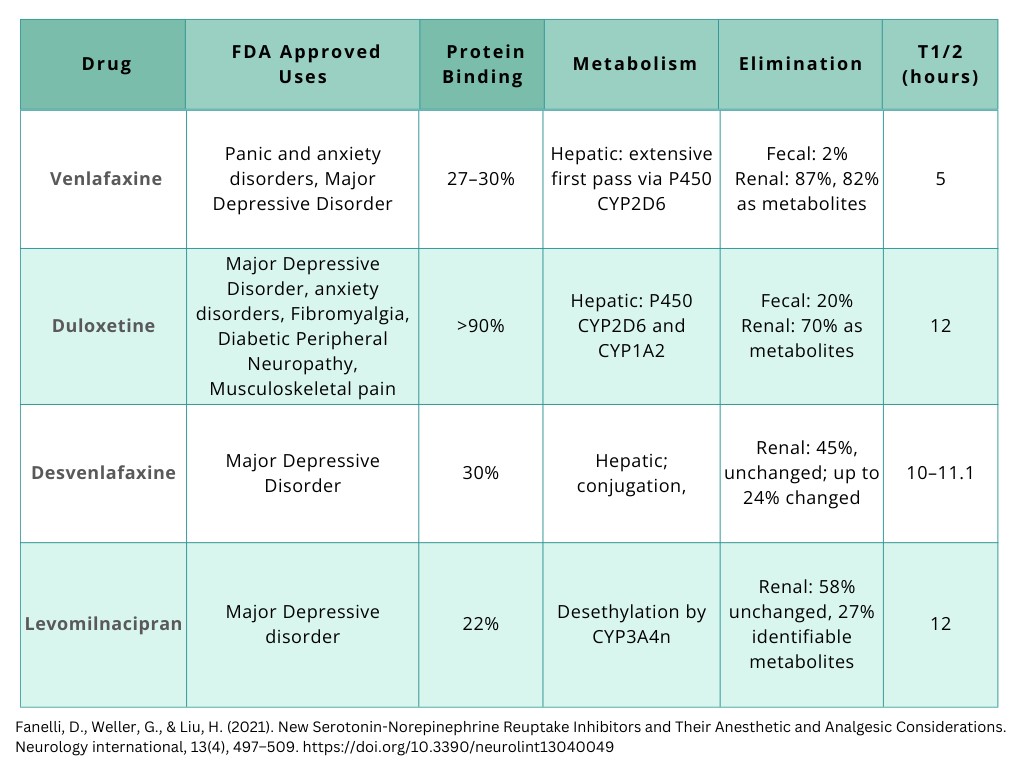
Figure 1. Pharmacokinetics of SNRIs [Created by course author].
Nursing Considerations
It is vital to recognize how each patient is unique and different in their journey of depression treatment. Nurses play a key role in assessing and providing advocacy for these patients.
The following are important nursing considerations:
- Thorough and focused mental status assessment
- Assess level of consciousness and orientation, appearance and general behavior, speech, motor activity, affect and mood, thought and perception, attitude and insight, and cognitive abilities.
- Assess status and mood changes.
- Assess suicidal tendencies, especially in early beginning of SNRI (9).
- Monitor BP before and periodically during therapy. Sustained hypertension may be dose-related; decrease dose or discontinue therapy if this occurs.
- Assess for serotonin syndrome.
- Provide patient education on medication use, dosage, and side effects. Provide patient education on support and resources available.
Nursing Diagnosis: Disturbed Thought Processes
Nursing Diagnosis: Ineffective Coping
Lab Assessments
Monitor CBC with differential and platelet count periodically during SNRI therapy. These medications can cause anemia, leukocytosis, leukopenia, thrombocytopenia, basophilia, and eosinophilia (9).
May cause an increase in serum alkaline phosphatase, bilirubin, AST, ALT, BUN, and creatinine, and serum cholesterol.
SNRIs can also cause electrolyte abnormalities (hyperglycemia or hypoglycemia, hyperkalemia or hypokalemia, hyperuricemia, hyperphosphatemia or hypophosphatemia, and hyponatremia).
Conclusion
SNRIs are an effective method of treatment for those suffering from depression. The effectiveness of SNRIs is dependent on a variety of factors like dosage and time spent in the body. Although the mechanisms of actions and makeup of SNRIs are consistent, each drug has differences on how much reuptake they prevent and the side effects of each type. Prescribers must be aware of these differences, the uses, mechanisms of action, side effects, and warnings.
Conclusion
SNRIs are an effective method of treatment for those suffering from depression. The effectiveness of SNRIs is dependent on a variety of factors like dosage and time spent in the body. Although the mechanisms of actions and makeup of SNRIs are consistent, each drug has differences on how much reuptake they prevent and the side effects of each type. Prescribers must be aware of these differences, the uses, mechanisms of action, side effects, and warnings.
Corticosteroid Therapy
Introduction
When many people hear of steroids, they may think of athletes. However, the steroids that some athletes misuse to enhance their strength and training abilities are not the same as those administered for allergic reactions and some inflammatory conditions. The steroids used by some athletes are called anabolic steroids. The steroids used for the treatment of disease are called corticosteroids.
Steroids are hormones naturally produced in the body (made from cholesterol) to regulate the function of various bodily systems [2]. Some steroid hormones are produced by the adrenal glands of the endocrine system (a set of two glands that rest atop the kidneys). The adrenal glands produce the hormone types: glucocorticoids, mineralocorticoids, and adrenal androgens [2]. Corticosteroid medication mimics glucocorticoids, more specifically a glucocorticoid called “cortisol.”
The Immune System
Corticosteroids are well-known for increasing a patient’s risk for infection. This is due to the medication’s effect on the immune system, particularly its anti-inflammatory properties. It is important to have a clear understanding of how the immune system works as well as the inflammatory process that takes place when a foreign pathogen enters the body.
How Does the Immune System Work?
In a typical immune system the immune system is triggered by an antigen – a marker in the body that alerts cells of the immune system that there’s a foreign invader present, like a pathogen or foreign object. Subsequently, a series of events follows. Like in a war, the body rounds up the first line of defense soldiers to fight the pathogen.
These include [11]:
- Proteins (called “the inflammasome”) to active inflammatory responses.
- Macrophages to engulf and digest pathogens.
- Neutrophils to help kill pathogens and rid of the leftover debris.
- Endothelial cells to help rid of the dead pathogens/debris.
The influx of these cells to the site of injury or infection is the beginning of inflammation.
What is Inflammation?
Inflammation is more than just “swelling.” Inflammation is a process in which a cascade of events occurs to help the immune system fight against pathogens and foreign bodies. The inflammatory process encompasses a variety of signs/symptoms including redness, warmth, swelling, and drainage [11].
For example, when a person sustains a traumatic injury to the skin causing an open wound, the accompanying redness (or erythema) is caused by a rush of red blood cells through the site [5]. The dilation of the blood vessels is what causes this “rush” of cells. The increased blood flow also causes the localized warmth that typically occurs. Blood vessel dilation is responsible for the associated swelling as well. The pus that forms is a combination of fluid, dead immune/pathogen cells, and debris from the fight, essentially, the “casualties at war” that must be removed from the body [5].
As with fever, inflammation aids in the fight against pathogens and therefore should not be inhibited unless it is likely to be damaging or fatal in and of itself. [11]. This inflammatory process is acute in nature, and typically goes away on its own or with the help of medication. While acute inflammation from a normal immune response is natural and beneficial, chronic inflammation is harmful and can lead to permanent damage of tissues and body systems.
Chronic inflammation can be seen in conditions including inflammatory bowel disease, cancer, heart disease, and autoimmune disorders like rheumatoid arthritis, multiple sclerosis, and systemic lupus erythematosus [11]. Chronic inflammation is typically caused by an overactive immune system or autoimmune disease (when the immune system mistakenly attacks normal tissues). In cases like these, inhibiting the inflammatory process by suppressing the immune system is most beneficial. This is where corticosteroids come into play.

Self Quiz
Ask yourself...
- How often do you encounter patients with autoimmune disease or chronic inflammatory diseases?
- Have you ever cared for a patient who was on long-term corticosteroid therapy?
- Have you ever cared for a patient who developed an infection after corticosteroid use?
- How comfortable are you with the idea of immunosuppression?
Corticosteroids: The Basics
Corticosteroids are a group of steroidal therapy medications that are often the go-to for reducing inflammation in the body. Once referred to as “a miracle drug,” these medications are helpful in the treatment of acute and chronic inflammatory conditions and autoimmune diseases.
Corticosteroids are also useful in emergency situations, for example during asthma attacks or allergic reactions – when the inflammation is life-threatening. Corticosteroids are synthetically formulated to mimic the hormone cortisol.
What is Cortisol?
As mentioned earlier, the adrenal glands of the endocrine system produce three different types of steroid hormones, one of which is glucocorticoids. Cortisol is a major glucocorticoid hormone.
There are two major structures of the adrenal glands – the outer layer (cortex) and inner portion (medulla) – each producing its own hormones. The outer layer (cortex) produces cortisol, hence the name “corticosteroid” [6].
Cortisol levels in the body rise when a person is stressed [2]. This hormone helps to regulate metabolism, growth, reproduction, and the immune system [2]. Cortisol also aids in cardiovascular function by making blood vessels more sensitive to natural vasoconstrictors in the body (like adrenaline) [2].
How Do Corticosteroids Work?
Corticosteroids work by suppressing the immune system which in turn reduces inflammation. In patients with an overactive immune system or acute flareups from a triggering agent, the inflammation can cause troubling symptoms, become prolonged, and spread to other areas within the body. If left untreated, inflammation can lead to tissue scarring (or damage to affected structures) and loss of bodily functions [11].
The challenge with administering corticosteroids to suppress an overactive immune system is balancing the benefits of inflammatory symptom relief and the risks of infection due to the resulting underactivity of the immune system. In this case, clinicians are encouraged to start with the lowest therapeutic dose possible, carefully monitor its use in patients with infections, and ensure that the benefits exceed the risks [6].
Corticosteroids also stop the body from producing its own natural cortisol. In a sense, a course of corticosteroids gives the adrenal glands a break. In a short course of corticosteroids, once the medication is discontinued, the adrenal glands can start back releasing cortisol. However, the adrenal glands do not resume releasing cortisol right away and need time to start working again.
This is why corticosteroids (oral and parenteral forms) should not be stopped abruptly when taken for more than about two weeks [6]. If stopped abruptly, patients may develop adrenal insufficiency during this period, which can be life-threatening.


Self Quiz
Ask yourself...
- What do you think is the biggest concern of nurses and clinicians when prescribing/administering corticosteroids?
- Have you encountered patients with permanent bodily dysfunction caused by prolonged inflammation?
- How challenging is it to balance infection risk and therapeutic benefit when prescribing/administering corticosteroids?
- How do you determine what to begin with when initiating a new corticosteroid treatment? Or have you ever discussed dosing safety with a provider?
Corticosteroid Pharmacology
Common corticosteroid formulations include intravenous (IV), intramuscular (IM), intra-articular (injected directly into a joint), oral, inhaled, intranasal (nasal spray), topical, ophthalmic (eye drops), and otic (ear canal). The increased risk of infection is most associated with systemic formulations (oral and parenteral).
The following sections will cover the pharmacology of systemic corticosteroids, including indications, mechanisms of action, pharmacokinetics, precautions, adverse effects, drug interactions, and warnings [7].
Indications
Corticosteroids are useful in the treatment of many medical conditions. Some indications for corticosteroids among adults include the following diseases, conditions, and situations (maybe drug- or route-specific) [6][7].
Allergic Reactions
Corticosteroids are well-known for treating mild to severe allergic reactions. These include anaphylaxis, angioedema, and laryngeal edema (non-infectious). Others include hypersensitivity reactions to medications or food, severe seasonal allergies (like allergic rhinitis), contact dermatitis (or rash), and itching.
Autoimmune Diseases
Corticosteroids are used to treat autoimmune disorders including systemic lupus erythematosus, Crohn’s disease, rheumatoid arthritis, and plaque psoriasis. Others include autoimmune hepatitis, hemolytic anemia, celiac disease (gluten intolerance), sarcoidosis (marked by lumps of inflammatory cells throughout the body) and myasthenia gravis (marked by weakness in voluntary muscles).
Pulmonary Exacerbations
Corticosteroids are useful in the treatment of exacerbations from asthma and chronic obstructive pulmonary disease (COPD).
Adrenal Insufficiency
Corticosteroids may be used to treat both primary and secondary adrenocortical insufficiency. This includes Addison’s disease, congenital adrenal hyperplasia, and adrenogenital syndrome.
Inflammatory Bowel Disease
Inflammatory bowel disease, such as the aforementioned Crohn’s disease, and ulcerative colitis may be treated with corticosteroids.
Neuro/Musculoskeletal Disorders
Corticosteroids are used in the treatment of ankylosing spondylitis (chronic inflammation of spinal joints), bursitis, polymyalgia rheumatica (marked by muscle pain and stiffness), osteoarthritis, and psoriatic arthritis. Corticosteroids can also treat neurological conditions like multiple sclerosis and Bell’s palsy (facial paralysis, often temporary).
Inflammatory Eye Conditions
Corticosteroids are useful in the systemic treatment of inflammatory ophthalmic conditions including optic neuritis, allergic conjunctivitis, and other conditions that cause inflammation of various structures of the eye.
Organ Transplant Rejection Prophylaxis
Renal transplant guidelines recommend corticosteroids in combination with other medications to prevent kidney rejection after transplantation (called induction therapy or immunosuppressant therapy). Corticosteroids are also indicated for heart and liver transplant rejection prophylaxis.
Cancer
Corticosteroids may be used for the palliative treatment of cancers including multiple myeloma and chronic lymphocytic leukemia (CLL). They may also be used to treat Hodgkin lymphoma (in conjunction with cancer medications), aggressive non-Hodgkin lymphoma, peripheral T-cell lymphoma, and neoplastic-associated hypercalcemia.
COVID-19
Although still in the investigative stages, the World Health Organization (WHO) recommends systemic corticosteroids as an adjunctive treatment for severe COVID-19 [6][13].

Self Quiz
Ask yourself...
- Do you prescribe/administer corticosteroids most frequently for acute or chronic conditions?
- What is the most common indication for corticosteroid therapy you have witnessed in your practice?
- Have you ever prescribed/administered corticosteroids for prophylaxis treatment alone?
- Can you think of ways to minimize the severity of adverse effects of corticosteroid therapy among patients most at risk?
Mechanism of Action
As already mentioned, corticosteroids suppress the immune system. This is done by preventing protein synthesis in certain cells of the immune system (like macrophages and neutrophils), ultimately inhibiting their fighting potential [6][11]. More specifically, corticosteroids repress the activity of DNA within the immune cell – an activity that would otherwise serve as the beginning of protein synthesis.
Within immune cells, DNA sends messages to protein-making structures within the cell that prompts them to start making protein. However, the message must be “translated” or “decoded” (transcription) first before the structures can “understand” what to do [6][12]. Messenger RNA (mRNA) is the transcribed version of DNA. Corticosteroids work by making it difficult for DNA to be transcribed into mRNA.
Pharmacokinetics
The pharmacokinetics of corticosteroids differ based on drug type and route. The following is the pharmacokinetics of three common systemic corticosteroid drugs: prednisone, methylprednisolone, and dexamethasone [6].
Prednisone
Prednisone comes in oral forms, both immediate-release (IR) and delayed-release. Prednisone IR is quickly absorbed in the gastrointestinal (GI) tract with a peak effect after one to two hours. Delayed-release tablets are released four hours after ingestion and peak after about six hours. Prednisone is metabolized by the liver and excreted by the kidneys.
Methylprednisolone
Methylprednisolone is rapidly absorbed orally and peaks within one to two hours. After IV administration, effects can occur within one hour with nearly complete excretion in 12 hours. When given as an injection in the joint, methylprednisolone absorption can occur over several days. This medication is distributed into various organs and body structures including the kidneys, intestines, skin, liver, and muscle. Methylprednisolone is metabolized by the liver and excreted by the kidneys.
Dexamethasone
Oral dexamethasone peaks in one to two hours. Absorption times for parenteral forms depends on the dosage and indication. For example, in patients with cerebral edema, treatment response from an IV dose of dexamethasone followed by an IM dose occurs in 12 to 24 hours [1]. Dexamethasone is rapidly distributed into the skin, intestines, liver, muscle, and kidneys. As with prednisone and methylprednisolone, this medication is metabolized by the liver and excreted by the kidneys.


Self Quiz
Ask yourself...
- What is the most common corticosteroid you have prescribed/administered?
- Why do you think it is important to know the mechanism of action of corticosteroids?
- What is the main determining factor in prescribing/administering an oral corticosteroid as opposed to a parenteral form?
Contraindications and Precautions
Clinicians should not prescribe/administer prednisone to patients with an allergy to the drug or any components of its formulation. Precautions should be taken in patients with an allergy to other corticosteroids as cross-sensitivity can occur. Clinicians should also be aware that high-dose systemic corticosteroids place patients at risk for immunosuppression, especially when prescribed/administered with other immunosuppressant medications.
Although carrying a lower risk, moderate-dose and low-dose corticosteroid preparations should be monitored as well. Clinicians should avoid prescribing/administering these medications to patients with fungal or bacterial infections that are not well controlled with anti-infective medications.
Pregnancy and Breastfeeding Precautions
While corticosteroids are not contraindicated for pregnant or breastfeeding patients, clinicians have reason to be cautious when prescribing/administering these medications [6]. The following are precautions for pregnant and breastfeeding patients.
Pregnancy
If corticosteroids must be prescribed/administered during pregnancy, precaution should be taken as these medications cross the placenta and may be harmful to the fetus/infant (may cause adrenal insufficiency in the infant). Although the risks are small and inconsistent, oral or facial clefts (like cleft palate) may occur if systemic corticosteroids are prescribed/administered during the first trimester.
Breastfeeding
Corticosteroids are distributed into breastmilk. While no reported side effects have been reported in breast-fed infants, lower doses are recommended as high doses may cause problems with the infant’s growth and development. Corticosteroids can interfere with the infant’s ability to produce their own glucocorticoid hormones. With prednisone in particular, peak concentrations in breastmilk occur in about one hour after the dose is taken and it is recommended for patients to avoid breastfeeding during this time. However, the total daily dose of prednisone reaching the infant has been shown to be approximately 0.1% of the mother’s total daily dose [6].

Self Quiz
Ask yourself...
- How comfortable are you prescribing/administering corticosteroids to patients who already take immunosuppressive medications?
- Have you ever witnessed a patient have a severe allergic reaction to a corticosteroid? If so, what was the treatment/anecdote?
- Have you ever been in a situation in which you had no choice but to prescribe/administer corticosteroids to a patient who was pregnant?
Adverse Effects
Corticosteroids given systemically can affect multiple body systems, particularly with prolonged use. Short-term use in high doses typically does not cause adverse effects [6]. Adverse effects of corticosteroids can be as mild as a rash to as severe as psychosis or a ruptured heart wall.
The following are adverse effects categorized by body systems [6].
Neurological
Corticosteroids may increase intracranial and intraocular pressure which can lead to optic nerve damage and visual impairments. These medications can also lower seizure thresholds. Other neurological findings include headache, vertigo, and peripheral neuropathy.
Pulmonary
Corticosteroids can reactivate tuberculosis (TB) in patients who have a history of active TB.
Cardiovascular
Sodium retention, edema, and low potassium may occur in patients with high blood pressure or congestive heart failure (can also occur with renal failure/insufficiency). Left ventricular free-wall rupture can occur in patients with a recent myocardial infarction. Corticosteroids may also exacerbate arrhythmias and cause blood clots which may lead to a stroke.
Endocrine
Corticosteroids are known to decrease glucose tolerance and raise blood glucose levels. This can aggravate existing diabetes mellitus. Hypothalamic-pituitary-adrenal (HPA) suppression or signs/symptoms of Cushing’s syndrome (marked by high cortisol levels) can also occur with prolonged systemic use.
Gastrointestinal/Genitourinary
Corticosteroids can increase the risk of GI perforation and should therefore be monitored in patients with peptic ulcer disease, diverticulitis, or GI abscess. Additionally, esophageal ulcers and GI bleed may occur with use. Corticosteroids may cause weight loss, but can stimulate the appetite as well, leading to weight gain conversely. Menstrual irregularity may occur as well.
Musculoskeletal
Osteopenia (loss of bone density) and osteoporosis (more severe bone loss) can occur due to decreased bone formation, increased bone resorption, and inhibition of osteoblast function. Bone fractures (primarily in elderly patients) can occur as well. Acute generalized myopathy leading to quadriparesis (weakness in all extremities) may occur in patients with neuromuscular disease or those receiving neuroblocking medications. Muscle pain and waste can also occur due to protein depletion.
Skin
Corticosteroids may cause impaired wound healing due to protein depletion. Sweating, abnormal hair growth, and striae (stretch marks) can also occur with use. While corticosteroids may be useful in the treatment of rashes and itching, they can cause these symptoms as well.
Psychiatric
Psychiatric problems can occur with corticosteroid use, including euphoria, severe depression, anxiety, hallucinations, psychosis, personality changes, and withdrawn behavior. Patients may also experience insomnia, impaired cognition, mood swings, irritability, and restlessness.
Laboratory Changes
A common lab finding with corticosteroid use is leukocytosis (without an infectious or inflammatory cause). It is important for clinicians to differentiate between infectious and corticosteroid-related leukocytosis. Other lab findings may include low neutrophil count and abnormal electrolyte levels (high sodium, low calcium, and low potassium).

Self Quiz
Ask yourself...
- What are the most common adverse effects of corticosteroid therapy you have witnessed in your practice?
- Considering the severity of some adverse effects of corticosteroids, what is your strategy for safe dosing/administration?
- Has a patient under your care ever reported a serious adverse effect from a short-term course of corticosteroids?
- How often do you consult another provider in prescribing corticosteroid therapy for patients with multiple comorbidities? Or how often do witness providers doing so?
Black Box Warning
Black box warnings are issued by the U.S Food and Drug Administration (FDA) to warn the public about the serious adverse effects of some medications. The most recent black box warning for corticosteroids was issued in 2014. The FDA warned against administering corticosteroid injections into the epidural space of the spine for the treatment of neck/back pain and radiating pain in the extremities [4]. When administered in this way, serious (although rare) adverse effects can occur including vision loss, stroke, paralysis, and death.
Drug Interactions
The therapeutic effect of corticosteroids may be counteracted or enhanced when administered with certain medications. Clinicians should perform an accurate medication reconciliation when prescribing/administering corticosteroids to ensure effective and safe treatment.
The following are medications that interact with corticosteroids categorized by a decreased or increased therapeutic effect [1]. Corticosteroid doses should be adjusted accordingly.
Decreased Therapeutic Effect
Medications that can decrease the level of corticosteroids in the blood when administered together include:
- Barbiturates
- Carbamazepine
- Ephedrine
- Phenytoin
- Rifampin
- Cholestyramine (affects oral corticosteroids in particular)
Increased Therapeutic Effect
Medications that can increase the level of corticosteroids in the blood when administered together include:
- Ketoconazole
- Macrolide antibiotics

Self Quiz
Ask yourself...
- How often do you prescribe/administer corticosteroid injections (in any area of the body)?
- How comfortable are you prescribing/administering corticosteroids in conjunction with antibiotics?
- Have you ever had to increase a corticosteroid dose due to inadequate therapeutic levels (evidenced by persistent symptoms)?
- How often do you rely on pharmacists to check drug interactions for you?
Clinical Guidelines on Corticosteroid Use in the Critically Ill
Clinical practice guidelines for corticosteroid therapy were developed to assist clinicians and providers in ensuring optimal prescribing and administration practices. Currently, guidelines are in place for corticosteroid use in critical illness. The most recent 2024 guidelines were reestablished for the treatment of septic shock, acute respiratory distress syndrome, and community-acquired bacterial pneumonia, particularly in adult patients.
In the following sections, these guidelines are compared with prior 2017 recommendations [3]. Clinicians practicing in acute care settings can use the following guidelines when prescribing/administering corticosteroids to patients who are critically ill.
Sepsis and Septic Shock
Previously, the guidelines recommend against administering corticosteroids in adult patients with sepsis without shock. Instead, corticosteroids were recommended in patients with septic shock not responsive to fluid and moderate- to high-dose vasopressor therapy.
Current Recommendation: Administer corticosteroids to adult patients with septic shock. Do not administer high dose/short duration corticosteroids for adult patients with septic shock (no more than 400 mg per day of a hydrocortisone equivalent for no more than three days).
Acute Respiratory Distress Syndrome
Previously, the guidelines recommended corticosteroid use in patients with early moderate to severe acute respiratory distress syndrome (PaO2/FIO2 of less than 200 and within 14 days of onset).
Current Recommendation: Administer to adult hospitalized patients with acute respiratory distress syndrome.
Community-Acquired Bacterial Pneumonia
Previously, the guidelines recommended corticosteroid use for five to seven days at a daily dose of less than 400 mg IV hydrocortisone (or equivalent) in hospitalized patients with community-acquired pneumonia.
Current Recommendation: Administer to adult patients hospitalized with severe bacterial community-acquired pneumonia. There is no recommendation for adult patients hospitalized with less severe bacterial community-acquired pneumonia.

Clinical Guidelines on Corticosteroid Use for COVID-19
While data is limited and still developing, both the World Health Organization (WHO) and the National Institutes of Health (NIH) developed clinical practice guidelines for the use of corticosteroids as a treatment for COVID-19.
Clinicians practicing in acute care settings can use the following guidelines when prescribing/administering corticosteroids to patients with COVID-19.
Global Guidelines for Corticosteroid Use for COVID-19
As mentioned earlier, the WHO recommends corticosteroids for the treatment of severe COVID-19 [6]. The 2020 “Corticosteroids for COVID-19: Living Guidance” recommendations are as follows [13]:
- The WHO recommends systemic corticosteroids rather than no corticosteroids for the treatment of patients with severe and critical COVID-19.
- The WHO suggests not to use corticosteroids in the treatment of patients with non-severe COVID-19.
National Guidelines for Corticosteroid Use for COVID-19
The National Institutes of Health (NIH) developed the 2023 “Therapeutic Management of Hospitalized Adults with COVID-19” guidelines outlining various drug therapy recommendations for patients with COVID-19, including corticosteroids. Recommendations are as follows [9][10]:
- The panel recommends against the use of dexamethasone (or other systemic corticosteroids) for the treatment of COVID-19 in patients who do not require supplemental oxygen.
- The panel recommends against the use of dexamethasone (or other systemic corticosteroids) in nonhospitalized patients in the absence of another indication.
- The panel recommends patients with COVID-19 receiving dexamethasone (or another corticosteroid) for an underlying condition to continue this therapy as directed by their health care provider.

Self Quiz
Ask yourself...
- How does your facility/organization inform nursing staff of new clinical practice recommendations?
- How comfortable are you with the idea of using corticosteroids in the treatment of septic shock and COVID-19?
- How often do you review clinical practice guidelines on your own time?
- Are there any other practice recommendations your facility has shared with nursing staff about corticosteroid safety?
Patient Education
Therapeutic and safe corticosteroid use is dependent on safe prescribing and administration practices, as well as patient compliance. Optimal patient education is vital for successful treatment with corticosteroids.
The following are teaching points to share with patients about corticosteroid use [1][6][7].
- Adverse Effects: Patients should be informed of common adverse effects, particularly elevated blood sugar, mood changes, appetite changes, and weight gain.
- Vaccine Safety: Patients should be encouraged to check with their health provider before receiving vaccines (Corticosteroids should not be given with live vaccines)
- Infection Risk: Patients should be informed of the risk for developing an infection when corticosteroid doses are high or used to suppress the immune system, and to therefore avoid exposure to chickenpox or measles.
- Administration: Patients should be instructed to avoid abruptly stopping corticosteroids to prevent adrenal insufficiency and potentially death. They should also be made aware that stress on the body (for example, when having surgery) may require additional doses of corticosteroids.


Self Quiz
Ask yourself...
- What do you think is the most important teaching point for patients about corticosteroids?
- Have you ever had to adjust a patient’s corticosteroid dose due to a stressful event (like surgery)? Or have you witnessed a provider doing so?
- What is the protocol in your facility/organization for educating patients about corticosteroid therapy?
- Have you ever encountered a patient who abruptly stopped corticosteroid treatment? If so, did the patient develop any symptoms?
Future Implications
Corticosteroid use may be on the rise. As aforementioned, corticosteroids are useful in the treatment of autoimmune disease. In the U.S., researchers anticipate a rise in autoimmune diseases in the future.
In a 2020 study in Arthritis and Rheumatology, researchers noted that the prevalence of antinuclear antibodies (ANA) (markers of autoimmune disease) is increasing in the U.S. [8]. The study analyzed the antibodies of over 14,000 participants (age 12 and older) over the course of three time periods. Results revealed the following:
- From 1988 – 1991, 22 million people had antibodies.
- From 1999 – 2004, 27 million people had antibodies.
- From 2011 – 2012, 41 million people had antibodies.
The study also found that antibody prevalence is highest among males, non-Hispanic whites, adults over age 50, and adolescents. Young people age12 to 19 had the highest antibody prevalence. While it is unclear why this is the case among the youth, the study findings may suggest an increase in the use of corticosteroids in the future. Further, clinicians might anticipate changes in clinical guidelines for safe prescribing/administration practices.

Self Quiz
Ask yourself...
- How often do you encounter patients on long-term corticosteroid therapy for autoimmune disease?
- Have you noticed a rise in corticosteroid prescribing/use in your facility/organization?
- Why do you think antibody prevalence is on the rise in the adolescent population?
Conclusion
Corticosteroids are helpful in the treatment of many medical conditions and diseases. While the use of these medications is common, there are equally associated risks, many of which can be life-threatening. Safe prescribing/administration practices are imperative. Clinicians can ensure that treatments are safe and effective through the gathering of accurate health histories, careful evaluation of each patient’s situation, weighing of risks and benefits, and provision of effective education to patients.


Self Quiz
Ask yourself...
- In your opinion, what is the biggest public misconception about corticosteroid use?
- Do you feel that corticosteroids are over-prescribed/used?
- How can nurses enhance teaching for patients to ensure compliance with corticosteroid treatments?
- How can nurses advocate in the workplace for safer prescribing/administration of corticosteroids?
- What future clinical practice changes do you anticipate with regards to corticosteroid use in the U.S.?
Anti-arrhythmics
Introduction
Cardiac arrhythmias continue to present significant clinical challenges and remain a cause common of death and disability [5]. Arrhythmias encompass a wide array of heart rate and rhythm disturbances; they are classified into broad terms as bradyarrhythmia’s (heart rates below 60 beats per minute) and tachyarrhythmias (heart rates exceeding 100 beats per minute) [10].
The defining feature of cardiac arrhythmias is an irregular heartbeat, or a symptom of abnormal heart rhythm linked to irregular initiation of electrical impulses, or a combination of both factors.
The mechanisms underlying cardiac arrhythmias are complex. The management of these conditions often involves the administration of antiarrhythmic drugs. It is vital that prescribers are aware of the pharmacokinetics of this drug class.
Overview of Cardiac Arrhythmias
Arrhythmias impact an estimated 17 million individuals across the planet, they rank among the most prevalent forms of heart disease [8]. The clinical manifestations of arrhythmias vary from asymptomatic individuals to sudden cardiac death (SCD), contributing to 10–15% of all mortality cases [10].
The only pattern considered to be a normal heart rhythm is the normal sinus rhythm. In this state, an electrical impulse originates in the sinoatrial (SA) node and travels through the heart [1]. This delayed impulse occurs in the atrioventricular (AV) node, then it proceeds through the His-Purkinje network, which encompasses the bundle of HIS, the left and right bundle branches, and the Purkinje fibers [1]. These reactions essentially coordinate each beat of the heart.
Despite the notable limitations associated with existing antiarrhythmic medications, pharmacological intervention remains a fundamental aspect of managing cardiac arrhythmias [5]. Research suggests that arrhythmias occur in 1.5% to 5% of the general population, with atrial fibrillation being the most prevalent form [1, 10].
Arrhythmia refers to any deviation from the heart's normal rhythm, with the normal sinus rhythm being the baseline for a healthy heart rhythm [1]. The categorization of arrhythmias occurs through various criteria, with the most prevalent method being the heart rate of conduction. This includes bradyarrhythmia’s, where the heart beats slower than 60 beats per minute (bpm), and tachyarrhythmias, where the heart rate exceeds 100 bpm [1].
Atrial fibrillation (AF) is the most frequent occurring sustained cardiac arrhythmia and linked to heightened morbidity and mortality rates, in addition to increased healthcare costs [2][3].
Arrhythmias may originate from congenital anomalies (present from birth) or can develop due to irritation or damage to the myocardial tissue, causing disruptions or ‘short circuits’ in the heart's electrical system [13].
Basics of Antiarrhythmic Drugs (AADs)
Antiarrhythmic drugs (AADs) continue to be fundamental in the management of cardiac arrhythmias and classified based on the cardiac action potential [4]. The action of these drugs works toward the immediate cessation of atrial and ventricular arrhythmias (acute cardioversion) and for the long-term prevention of arrhythmia recurrence to maintain normal sinus rhythm [5].
A limited number of new AADs have reached the market despite the growing incidence of cardiac arrhythmias [5].
Two key objectives define the rationale for treating arrhythmias: (1) to mitigate significant clinical symptoms, including weakness, syncope, or the onset or worsening of congestive heart failure caused by an arrhythmia, and (2) to extend the patient's lifespan [8].
In the initial stages of antiarrhythmic drug (AAD) development, the primary focus was on controlling ventricular arrhythmias [6]. The direction of treatment changed following the adverse outcomes highlighted by the Cardiac Arrhythmia Suppression Trial (CAST) and the Survival with Oral D-Sotalol (SWORD) trial, which demonstrated that patients receiving AADs (encainide or flecainide) fared worse than those on placebo [6].
The primary criterion of antiarrhythmic drugs is safety. In the last decade antiarrhythmic drugs have been subject to intense reevaluation, prompted by the outcomes of large-scale human research studies that highlighted various risks and limitations associated with pharmacological treatments for arrhythmias [7].
In the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study, the trial demonstrated that although achieving rhythm control was associated with improved survival the adverse effects negated survival benefits [8].

Self Quiz
Ask yourself...
- How would you describe the range from asymptomatic cases to life-threatening conditions?
- How can healthcare professionals balance the immediate need for rhythm control with the long-term goal of minimizing adverse effects and mortality?
Definition
Antiarrhythmic agents, often referred to as cardiac dysrhythmia medications, constitute a category of pharmaceuticals designed to moderate the heart’s electrical impulse and mitigate rapid heart rhythms; these rhythms include atrial fibrillation (AF), supraventricular tachycardia (SVT), and ventricular tachycardia (VT) [11].
This class of drugs influence cardiac ionic channels or receptors, modifying the cardiac action potential, or its creation and transmission [11]. These alterations affect the activation spread or repolarization pattern, suppressing cardiac arrhythmias [12].
Common symptoms of arrhythmias include heart fluttering, abnormal or rapid heart rhythms, lightheadedness, fainting spells, chest pain, and breathlessness. Individuals may also experience heart palpitations, dizziness or feeling faint, chest pain or discomfort, weakness, and fatigue [12].

[10]

Self Quiz
Ask yourself...
- How do antiarrhythmic agents contribute to the suppression of arrhythmias and the alleviation of associated symptoms such as heart fluttering, lightheadedness, and chest pain?
- Do you have experience administering antiarrhythmic medications to patients?
Classification of Antiarrhythmic Medications
The categorization of arrhythmias is based on the location within the conduction pathway where they originate.
There are two main groups:
- Supraventricular - originating from the atria or the atrioventricular (AV) node.
- Ventricular - occur distal to the AV node.
[23]
Prior to 2018, the categorization of antiarrhythmic drugs was based on the Vaughan-Williams (VW) classification system, which organized these medications by their principal mechanism of action [4, 14]. The initial Vaughan-Williams classification had limitations. When introduced in the 1970s, the range of antiarrhythmic drugs focused on altering the function of Na+, K+, and Ca2+ channels, as well as targeting intracellular processes governed by adrenergic activity [15].
Today, there is a broader range of advanced antiarrhythmics, many possessing overlapping interactions with drugs in other classes. For example, amiodarone, categorized under Class III (Potassium channels blockers), also exhibits sodium and calcium-channel blocking properties (Class IV).

Self Quiz
Ask yourself...
- How do the limitations of the initial Vaughan-Williams classification system highlight the importance of continuous research and development in the field of cardiac pharmacology?
- Can you think of an example of a drug that contains overlapping drug actions?
Class 0: HCN Channel Blockers
Ivabradine
Ivabradine is designed to lower heart rate. It is used in the management of stable angina pectoris and chronic heart failure with heart rate ≥70 bpm across various clinical scenarios, including those with either preserved or compromised left ventricular (LV) function.
Ivabradine is effective by decreasing heart rate while preserving myocardial contractility and coronary vasomotor responsiveness, thereby reducing oxygen consumption, and extending diastolic duration [16] [17].

Self Quiz
Ask yourself...
- How does Ivabradine's mechanism of action contribute to its therapeutic benefits in patients with stable angina pectoris and chronic heart failure?
Class I: Voltage-gated Na+ Channel Blockers
Class IA
Class IA medications block fast sodium channels and include agents such as quinidine, procainamide, and disopyramide [11]. Quinidine, disopyramide, and procainamide are used in the management of supraventricular tachyarrhythmias, recurrent atrial fibrillation, ventricular tachycardia, ventricular fibrillation, Brugada syndrome, and Short QT Syndrome (SQTS) [4].
These drugs are associated with the highest risk of proarrhythmic among sodium channel blockers due to their capacity to prolong the QTc interval, which restricts their use because of their proarrhythmic potential [11].
For patients with Brugada syndrome, Quinidine is an alternative to implantable cardioverter-defibrillator (ICD) placement [66].
This class has also shown utility in individuals with short QT syndrome experiencing recurrent ventricular arrhythmias (VAs), reducing the frequency of ICD shocks in these patients [66].
Disopyramide is employed in cases of hypertrophic obstructive cardiomyopathy (HOCM), when combined with a beta-blocker or verapamil to alleviate symptoms like angina or dyspnea in patients unresponsive to beta-blockers or verapamil alone [67].
Procainamide is useful for exposing and diagnosing Brugada syndrome in individuals suspected of the condition but without a confirmed diagnosis [68]. Procainamide has shown to reestablish sinus rhythm in patients with Wolff-Parkinson-White (WPW) syndrome who experience atrial fibrillation (AF) without hemodynamic instability, which is marked by a wide QRS complex or a rapid pre-excited ventricular response [69]. Procainamide may also assist in terminating ventricular tachycardia and other arrhythmias [69].

Self Quiz
Ask yourself...
- How might the proarrhythmic potential of these drugs and their ability to prolong the QTc interval influence the decision-making process in selecting an appropriate treatment strategy for patients with conditions like Brugada syndrome, Short QT Syndrome (SQTS), or Wolff-Parkinson-White (WPW) syndrome?
Class IB
Lidocaine and Mexiletine treat ventricular tachycardia and ventricular fibrillation after a myocardial infarction by inducing a mild blockade of sodium channels [4]. These are not effective for treating atrial arrhythmias [4].
In the context of long QT syndrome, mexiletine is capable of reducing the QTc interval and has been employed to decrease the incidence of recurrent arrhythmias and the need for interventions by implantable cardioverter-defibrillators (ICDs) [70].
The effectiveness of Lidocaine diminishes in instances of hypokalemia, necessitating the correction of potassium levels [80].

Self Quiz
Ask yourself...
- How does the mechanism of sodium channel blockade by Lidocaine and Mexiletine contribute to their differential effectiveness in treating ventricular?
- What implications does this have for their use in managing long QT syndrome and conditions of electrolyte imbalance such as hypokalemia?
Top of Form
Class IC
Research recommends Encainide (Enkaid), flecainide (Tambocor), and propafenone (Rythmol SR) for managing supraventricular and ventricular tachyarrhythmias that do not respond to standard treatments, in the absence of underlying structural heart disease. [72].
Propafenone increases the effects of cyclosporin, desipramine, and theophylline [81].
Class IC is used to treat premature ventricular contractions and catecholaminergic polymorphic ventricular tachycardia [18]. These drugs block sodium channels without altering the QT interval and suit ongoing management in individuals with symptomatic supraventricular tachycardia (SVT) who have no structural or ischemic heart disease, and either are unsuitable for or opt against catheter ablation. [11].
In addition, these agents are effective for the pharmacological cardioversion of atrial fibrillation (AF). The “pill in the pocket” strategy involves patients with paroxysmal AF carrying a loading dose of medication to take at the onset of an AF episode. This approach aims for chemical cardioversion to restore normal rhythm, rather than adhering to a regular maintenance dose regime [71].
The Cardiac Arrhythmia Suppression Trials (CAST I and II) showed that patients with a history of myocardial infarction, treated with class IC agents (flecainide, encainide, moricizine) to reduce premature ventricular contractions (PVCs), faced a higher mortality risk compared to those receiving placebo [72].

Self Quiz
Ask yourself...
- How does the balance between the therapeutic benefits in the absence of structural heart disease and the increased mortality risk with a history of myocardial infarction guide clinical decision-making?
- How would you describe the 'pill in the pocket' strategy versus traditional maintenance dosing?
Class ID
Ranolazine presents a potential therapeutic option for managing tachyarrhythmias and ventricular tachycardia [19].

Class II: Autonomic Inhibitors/Activators
The literature recommends beta-blockers (BB) for managing the heart rate in individuals with paroxysmal, persistent, or permanent atrial fibrillation (AF) and atrial flutter [73]. Beta-blockers (BB) are also beneficial for long-term management in patients with symptomatic supraventricular tachycardia (SVT) [73].
Due to their favorable safety profile and efficacy, healthcare professionals can consider beta-blockers as the first-choice therapy for ventricular arrhythmias [39]. Their use is associated with a reduction in adverse cardiac events in conditions such as long QT syndrome and catecholaminergic polymorphic ventricular tachycardia [74].
For patients exhibiting symptomatic premature ventricular contractions (PVCs) in the absence of underlying heart disease, beta-blocker therapy can help decrease the frequency of recurrent arrhythmias and alleviate symptoms [75].

Self Quiz
Ask yourself...
- How does the mechanism of action of beta-blockers contribute to their effectiveness across a spectrum of arrhythmias?
- What factors influence the decision to prioritize beta-blockers as a first-choice therapy in these conditions, considering their impact on reducing adverse cardiac events in long QT syndrome and catecholaminergic polymorphic ventricular tachycardia?
IIa: Inhibitors including pindolol, carvedilol, timolol, nadolol (non-selective beta-blockers), and bisoprolol, atenolol, metoprolol, esmolol (selective beta-1 blockers) treat rate control in atrial fibrillation, atrial flutter, and ventricular tachyarrhythmia [4].
IIb: Activators: The use of Isoproterenol can manage ventricular escape rhythm in cases of complete AV block before pacemaker implantation [4][20].
IIc: Inhibitors: Atropine treats symptomatic sinus bradycardia and conduction block [4][21].
IId: Activators: For the management of supraventricular tachyarrhythmias, Carbachol, methacholine, and digoxin [4].
IIe: Activators: Adenosine for the cessation of paroxysmal supraventricular tachycardia (PSVT) [22].
Class III: K+ Channel Blockers/Openers
Potassium channel blockers decrease potassium efflux out of the cell and prolong the QTc interval [4] Amiodarone displays sympatholytic effects as well as sodium and calcium channel blocking properties, leading to reduced conduction through the AV and sinus nodes [4].
Amiodarone helps maintain sinus rhythm in patients with atrial fibrillation (AF) and those suffering from left ventricular systolic dysfunction [4].
Amiodarone also stands as a viable choice for pharmacological cardioversion and can help manage ventricular rate in critical patients without pre-excitation, though it is less effective than non-dihydropyridine calcium channel blockers [4] [49].
Amiodarone is the preferred antiarrhythmic medication for suppressing ventricular arrhythmias (VA) [4]. Administration of intravenous amiodarone may achieve rhythm stabilization in cases of unstable persistent ventricular arrhythmias (VA) following defibrillation [49]. Administering intravenous amiodarone stabilizes rhythm in cases of unstable persistent ventricular arrhythmias (VA) following defibrillation.
In addition, amiodarone controls ventricular arrhythmias (VA) in patients with ischemic heart disease who are also receiving beta-blocker treatment [4].
Observations show that Dronedarone reduces hospital admissions for atrial fibrillation (AF) in individuals with a history of non-permanent AF who are in sinus rhythm. However, for patients with permanent AF that cannot convert back to normal sinus rhythm, it is contraindicated due to FDA reviews indicating a significant increase in the risk of cardiovascular death, stroke, and heart failure in these cases [76].
Dofetilide is employed in the treatment of atrial arrhythmias and for the acute pharmacological cardioversion of atrial fibrillation or flutter [77].
Sotalol, combining class II beta-blocker properties and class III potassium channel blocker effects, manages both ventricular and supraventricular arrhythmias. [78].
Ibutilide (Corvert) targets the treatment of atrial fibrillation or flutter, underlining its specialized use in managing these specific arrhythmias [79].

Self Quiz
Ask yourself...
- How do these drug mechanisms contribute to its efficacy in managing both atrial and ventricular arrhythmias
- What considerations should be made when choosing Amiodarone for patients with left ventricular systolic dysfunction or those undergoing pharmacological cardioversion?
- How should clinicians navigate the decision-making process for employing Dronedarone in treating AF, considering the patient's AF status and the potential benefits and risks?
IIIA: Voltage-dependent K+ channels
Amiodarone and dronedarone are notable for their role as non-selective potassium (K+) channel blockers, which are crucial in the treatment of unstable ventricular tachycardia and life-threatening recurrent ventricular fibrillation [4].
Kv11.1 (rapid K+ current) blockers: Dofetilide, almokalant, ibutilide, sematilide, and sotalol manage ventricular tachycardia in patients without prior myocardial infarction or underlying structural heart disease. They also treat Wolff-Parkinson-White (WPW) syndrome when associated with atrial fibrillation [4].
Kv1.5 (ultra-rapid K+ current) blockers: Vernakalant serves to convert recent onset atrial fibrillation in patients without structural or ischemic heart disease. It is important to note that the FDA does not approve this specific use of vernakalant [24].
IIIb: Metabolically dependent K+ channels blockers: Nicorandil and pinacidil are employed as second-line treatments for stable angina [25].
Class IV: Ca2+ handling modulators
Non-dihydropyridine calcium channel blockers, such as diltiazem and verapamil, reduce conduction speed and decelerate signal transmission through the AV node [82]. These medications are effective for controlling the ventricular rate in both acute and chronic cases of atrial fibrillation (AF) and atrial flutter [82].
In the acute management of stable patients with supraventricular tachycardia (SVT), including focal and multifocal atrial tachycardias, diltiazem and verapamil serve as viable treatment options [4] [39].

Self Quiz
Ask yourself...
- Given the mechanism by which non-dihydropyridine calcium channel blockers like diltiazem and verapamil slow conduction and decelerate signal transmission through the AV node, why are these medications suited for controlling the ventricular rate in atrial fibrillation and atrial flutter?
- How does this mechanism influence their effectiveness in the acute management of various forms of supraventricular tachycardia?
IVa: Bepridil and falipamil, which block non-selective surface membrane calcium (Ca2+) channels, may manage supraventricular tachyarrhythmias [4]. Verapamil and diltiazem, which block surface membrane L-type calcium (Ca2+) channels, treat supraventricular arrhythmias, and control the rate of atrial fibrillation [4].
IVb: Propafenone and flecainide serve as intracellular calcium channel blockers utilized in addressing catecholaminergic polymorphic ventricular tachycardia (CPVT) [4].
Class V Mechanosensitive channel blockers
Inhibitors: N-(p-amylcinnamoyl) Anthranilic Acid: Under Research and Not Approved by the FDA [26].
Class VI: Gap junction channel blockers
Inhibitors: carbenoxolone (under investigation- not FDA approved) [27].
Class VII: Upstream target modulators
Omega-3 fatty acids: Eicosapentaenoic Acid and Docosahexaenoic Acid: Reduction in Cardiac Death Risk Post-Myocardial Infarction [28].
Statins: Potential for use in atrial fibrillation
ACE inhibitors: Captopril, Enalapril, Ramipril, Lisinopril (ACE Inhibitors), and ARBs (Losartan, Telmisartan): Potential Use in Atrial Fibrillation Associated with Heart Failure [29].
Clinical Prescribing Criteria
Antiarrhythmic medications are pivotal in managing symptoms and safeguarding against the decline of cardiac function caused by conditions such as tachycardia, irregular rhythms, or desynchrony [4]. The primary objective is to reestablish normal cardiac rhythm and conduction, averting the onset of more severe and fatal arrhythmias.
Antiarrhythmics have a narrow therapeutic index, indicating a minimal margin between the effective dosage and the onset of toxicity [4]. There is a tenuous balance between suboptimal treatment and the risk of toxic or proarrhythmic effects, underscoring the importance of precise dosing and monitoring. Clinical attention focuses on the patient's clinical status, underlying structural and functional conditions, and the mechanisms of arrhythmia at both cellular and molecular levels.
The use of antiarrhythmic drugs in therapy seeks to alter conduction velocity, by either slowing down or speeding it up, modify the excitability of cardiac cells via changes in the length of the effective refractory period, and suppress unusual spontaneous activity [14].
Numerous variables influence the effectiveness of antiarrhythmic drugs, such as race, sex, genetics, environmental temperature, drug interactions, precipitating factors, changes in neurohormones, the disease's present condition and severity, and disease-driven structural changes in the body [30]. The complexity increases with some antiarrhythmic drugs (AADs) displaying diverse electrophysiological and pharmacological effects that depend on the administration route, plasma concentration, and the existence of active metabolites.
A variety of factors can influence the efficacy of medications, including racial background, gender, genetic makeup, ambient temperature, interactions between different drugs, initiating triggers, neurohormonal fluctuations, the current state and intensity of the disease, and alterations in the body's structure caused by the disease itself [31].
Complicating the pharmacology, certain antiarrhythmic drugs (AADs) exhibit a wide range of electrophysiological and pharmacological actions, which can vary based on the method of administration, concentration levels in the plasma, and the presence of active metabolites [4] [5].

Self Quiz
Ask yourself...
- Considering the narrow therapeutic index of antiarrhythmic drugs, how does precise dosing and monitoring contribute to optimizing treatment outcomes while minimizing the risk of adverse effects?
- What role do patient-specific factors play in this process?
- Given the complex interplay of factors such as race, sex, genetics, and environmental conditions on the effectiveness of antiarrhythmic drugs, how should clinicians integrate this knowledge into personalized treatment plans?
- With some antiarrhythmic drugs displaying varied electrophysiological and pharmacological effects based on administration route, plasma concentration, and the presence of active metabolites, how do these variables complicate the management of arrhythmias?
The Cardiac Electrical Cycle (Electrical Cascade)
The cardiac action potential represents the sequence of ion exchanges that result in the successive depolarization and repolarization of the cardiac myocyte, culminating in muscle contraction [4]. During its resting phase, a cardiac myocyte maintains a baseline resting membrane potential ranging from negative 80 to negative 90 millivolts [32].
Antiarrhythmic drugs slow down ion movement during various stages of the cardiac action potential [32].
- Phase 0: The “depolarization” phase of the action potential occurs due to the influx of sodium ions (Na+) into the cell, following an electrochemical gradient, leading to a membrane potential of around positive 30 millivolts [33].
- Phase 1: “The notch,” or the early repolarization phase of the action potential, features potassium (K+) ions flowing out. [4] [33].
- Phase 2: “The plateau” phase occurs when the inward movement of calcium ions (Ca2+) balances the outward movement of potassium (K+) ions [4] [34].
- Phase 3: “The repolarization” phase of the action potential occurs through the efflux of potassium (K+) ions along their electrochemical gradient out of the cell. This movement removes the positive charge of the K+ ion from the cell, reinstating the cardiac myocyte's negative potential [33][34].
- Phase 4: Reactivation of the Na/K-ATPase pump, which re-establishes the resting membrane potential in the cardiac myocyte [4][35].

Self Quiz
Ask yourself...
- How do antiarrhythmic drugs alter the ion movement during the different phases of the cardiac action potential to correct arrhythmias?
- What are the potential consequences of these modifications on the overall function of the cardiac myocyte and the heart's rhythm?
Pharmacokinetics of Anti-Arrhythmic Medications
Pharmacokinetics involves the study of drug absorption, distribution, metabolism, and excretion. All antiarrhythmic drugs affect the conductance of membranes and ions, modifying cardiac action potential dynamics either via direct or indirect action.
For example, some medications inhibit fast sodium channels, essential for controlling the rate of membrane depolarization (phase 0) during an action potential [33]. Electrical conduction velocity links to membrane depolarization and blocking sodium channels slows this velocity down [32][33]. Slowing conduction velocity is advantageous for eradicating tachyarrhythmias resulting from reentry circuits [36].
Various antiarrhythmic drug classes affect the duration of action potentials and the effective refractory period [37]. Extending the effective refractory period often eradicates reentry tachyarrhythmias [38]. This effect occurs by inhibiting potassium channels and postponing the repolarization phase (phase 3) of action potentials [38].
Medications that inhibit the slow inward calcium channels aim to diminish pacemaker activity by decelerating the depolarizing pacemaker potential’s rate of rise (phase 4 depolarization) [14].
These drugs also decrease the speed of electrical signal transmission through the atrioventricular (AV) node [14][38]. Similar to sinoatrial (SA) node cells, AV nodal cells rely on the influx of calcium ions for depolarization [34]. Due to the potential for sympathetic nervous system activity to cause arrhythmias, beta1-adrenoceptor blockers are employed to diminish the sympathetic impact on the heart [39]. These beta-adrenoceptors connect to ion channels through specific signal transduction pathways, indicating that beta-blockers modify ion conductance across the membrane, influencing calcium and potassium conductance [39].
In instances of AV block, doctors sometimes use drugs like atropine, a muscarinic receptor antagonist, to counteract vagal effects [40]. AV block can emerge as an adverse effect of beta-blocker medication, and stopping the beta-blocker in such cases may return AV conduction to normal [41].
An increased ventricular rate can be a consequence of atrial flutter or fibrillation [42].
In response, medications that slow down conduction through the atrioventricular (AV) node regulate the ventricular rate. Calcium channel blockers and beta-blockers are particularly effective for this purpose [4].
Digoxin proves advantageous for patients with systolic heart failure, also referred to as heart failure with reduced ejection fraction (HFrEF), characterized by an ejection fraction of less than 40% [43]. Nonetheless, it does not contribute to a reduction in mortality [43]. When standard treatments do not achieve heart rate objectives in atrial fibrillation or atrial flutter, clinicians can deploy Digoxin for heart rate management [44].
Administration of digoxin is contraindicated in instances of pre-excitation due to accessory pathways since it promotes AV blockade and could precipitate ventricular tachyarrhythmias [44]. In conditions of elevated sympathetic activity, digoxin is ineffective, and beta-blockers are the preferred treatment option [44].
Healthcare providers favor oral drug formulations for their improved patient compliance, ease of use, and scalability, which offer economic advantages [45]. However, the oral bioavailability of drugs can vary, influenced by differences in physicochemical characteristics and metabolic activities that impact pharmacokinetics [46]. Challenges such as intestinal metabolism, efflux mechanisms in the gastrointestinal tract, and the hepatic first-pass effect hinder the bioavailability of drugs administered orally [46] [47].
The first-pass effect describes a pharmacokinetic process in which a drug undergoes metabolism at a specific site in the body before reaching the systemic circulation or its intended site of action, which reduces the concentration of the active drug available [47]. The liver, a primary location for drug metabolism, has a direct link to the first-pass effect. This effect can also occur in other active metabolic areas of the body, such as the lungs, blood vessels, gastrointestinal tract, and various tissues [47].

Self Quiz
Ask yourself...
- How do the pharmacokinetic processes of absorption, distribution, metabolism, and excretion influence the clinical efficacy and safety of antiarrhythmic drugs?
- What strategies can healthcare providers employ to mitigate potential adverse effects, including those related to the first-pass effect?
- Given the varied mechanisms by which antiarrhythmic drugs modify cardiac action potentials and conduction velocities to treat arrhythmias, how do these mechanisms align with the selection of specific antiarrhythmic medications for conditions such as atrial flutter, atrial fibrillation, and AV block, considering both the intended therapeutic outcomes and the potential for adverse effects?
Absorption
Antiarrhythmic medications exhibit quick absorption, but the pronounced first-pass effect often reduces their bioavailability [47]. They achieve peak plasma concentrations within 1–3 hours, except for digoxin and dronedarone, which reach their peak in 3–6 hours, and amiodarone, which takes 6–8 hours to peak [11]. In elderly individuals and patients with liver dysfunction, the oral bioavailability of medications tends to be higher [11].
Intestinal bacteria transform digoxin into inactive compounds; antibiotics such as tetracycline and erythromycin eliminate these bacteria, leading to elevated levels of digoxin in the bloodstream [44]. The antiarrhythmic effect of digoxin starts within 2–5 minutes after its intravenous administration [44].
The absorption of drugs through the gastrointestinal tract is crucial for their bioavailability, with meals playing a role that can either enhance or impede this process [46]. For instance, a high-fat meal can increase the oral absorption of dronedarone by fourfold [11].

Self Quiz
Ask yourself...
- How do factors such as age, liver function, intestinal flora, and dietary habits influence the therapeutic levels and efficacy of these drugs in the bloodstream?
Distribution
With the exception of sotalol, antiarrhythmic drugs (AADs) exhibit some degree of binding to plasma proteins [11]. Amiodarone, digoxin, flecainide, and propafenone build up in the heart at concentrations higher than those in plasma and dialysis cannot remove them [11].
The concurrent administration of flecainide and amiodarone increases flecainide plasma concentrations by 50% [48].
Disopyramide, mexiletine, sotalol, and verapamil can cross the placenta and appear in breast milk. High concentrations of Procainamide also occur in breast milk and eliminated by newborns [11].
Oral administration of amiodarone reaches steady-state plasma concentrations after an extended period, except when administered in substantial loading doses; delivering it via intravenous form also delays its maximal effect [49]. This delay is indicative of its distribution across multiple compartments, including the intravascular compartment, which a standard loading dose saturates, a peripheral compartment encompassing various tissues, and a deep compartment represented by adipose tissue, serving as a reservoir for the drug [49].
Amiodarone is known for its distinctive side effects, with a 15% prevalence rate in the first year of use, which can escalate to up to 50% with prolonged treatment [87]. Side effects include pulmonary fibrosis, thyroid dysfunction, photosensitivity, blue-grey skin discoloration, corneal microdeposits, peripheral neuropathy, and elevated liver enzymes [87]. Providers must weigh the potential benefits of amiodarone against its long-term risks [94].

Self Quiz
Ask yourself...
- How does the differential binding of antiarrhythmic drugs to plasma proteins and their accumulation in various body compartments (heart and adipose tissue) affect their pharmacodynamics and pharmacokinetics?
Biotransformation
Antiarrhythmic drugs (AADs) undergo metabolism in the liver through CYP450 isoenzymes, resulting in active metabolites that either block sodium (Na+) channels (such as mexiletine and propafenone), extend action potential duration (APD) [for instance, N-acetylprocainamide (NAPA)], or cause central nervous system (CNS) toxicity (as seen with lidocaine) [11].
Genetics influence the metabolism of CYP2D6 resulting in higher plasma concentrations and extended half-lives (t½) of metoprolol and propafenone in individuals with poor metabolizing capabilities (6% of Caucasians) compared to those who are rapid metabolizers [50]. In similar fashion, the conversion of procainamide to N-acetylprocainamide (NAPA) varies, with 15–20% metabolized in individuals classified as 'slow-acetylators' and 25–33% in 'fast-acetylators' [11].
These metabolic phenotypes are determined by genetics. There are no standard tests available to identify a patient's metabolic phenotype prior to treatment initiation, with the exception of measuring the procainamide/NAPA concentration ratio. It is advisable to decrease dosages for poor or slow metabolizers to two-thirds or less of the standard maintenance dose [11] [51].
Lipophilic beta-blockers, such as bisoprolol, carvedilol, metoprolol, and propranolol, undergo metabolism via CYP2D6, and their bioavailability and half-life (t½) are prolonged in cases of liver dysfunction [11]. The body excretes hydrophilic beta-blockers, including atenolol and sotalol, in their unchanged form through the urine [11].
Following an intravenous loading dose, lidocaine undergoes metabolism with a half-life (t½) of 1.5–2 hours. In patients with liver impairment or decreased hepatic blood flow — including the elderly, those experiencing cardiogenic shock, heart failure, myocardial infarction, or those taking cimetidine and beta-blockers — lidocaine's plasma levels increase, and its half-life extends [51]. In these cases, one should lower both the loading and maintenance doses.
Due to its brief half-life, an initial loading dose of lidocaine requires supplementation with a continuous infusion or repeated administrations to achieve and maintain a consistent plasma concentration [53].
Intravenous Esmolol undergoes rapid hydrolysis in red blood cells, with a half-life of ∼ 9 minutes, and achieves complete reversal of beta-blockade 20–30 minutes after drug cessation [11]. Intravenous adenosine acts within 15–30 seconds, with erythrocytes and vascular endothelial cells absorbing and metabolizing it through adenosine deaminase (ADA), leading to a short half-life (t½) of less than 10 seconds [11].

Self Quiz
Ask yourself...
- How do genetic variations in CYP450 isoenzymes (CYP2D6) affect the metabolism, efficacy, and safety of antiarrhythmic drugs?
Elimination
Antiarrhythmic drugs (AADs) vary in their extent of excretion through urine and feces [11]. The half-life (t½) of these drugs extends in elderly individuals and patients with renal impairment (such as digoxin, disopyramide, dofetilide, flecainide, procainamide, and sotalol) or liver dysfunction (including amiodarone, diltiazem, flecainide, lidocaine, metoprolol, mexiletine, propafenone, propranolol, quinidine, and verapamil) [11]. This prolongation also occurs in congestive heart failure (seen with amiodarone, flecainide, lidocaine, mexiletine, procainamide, and quinidine) or after a myocardial infarction (noted with disopyramide, lidocaine, and mexiletine) [11][54].
For these patients, it is advisable to lower the dosages and to conduct regular ECG monitoring. Amiodarone is subject to extensive metabolism in the liver, excreted through the bile, and has a prolonged half-life (t½) ranging from 25 to 110 days. This extended half-life accounts for the persistence of its effects for weeks or even months following cessation of the drug [11][55].
Due to their short half-life (t½), manufacturers dispense certain antiarrhythmic drugs, including beta-blockers, diltiazem, propafenone, and verapamil, in modified-release formulations [11].
Amiodarone, cimetidine, diltiazem, ketoconazole, procainamide, propranolol, and verapamil elevate plasma concentrations of quinidine [11]. Quinidine acts as a strong inhibitor of CYP2D6 and P-glycoprotein (P-gp), raising the plasma levels of drugs metabolized by this enzyme; it also reduces digoxin clearance, necessitating a 50% reduction in digoxin dosage [11]. Beta-blockers, cimetidine, and halothane cause an increase in plasma concentrations of lidocaine, thereby requiring a reduction in lidocaine dosage [11]. In addition, mexiletine elevates the plasma levels of theophylline, while amiodarone increases the levels of mexiletine [56].
Flecainide and propafenone lead to higher plasma concentrations of digoxin and propranolol. Propafenone (Rythmol) raises the plasma levels of digoxin, metoprolol, propranolol, and warfarin [48]. Mexiletine and quinidine amplify the effects of warfarin; thus, it is advisable to decrease the dosage of warfarin and monitor the prothrombin time/international normalized ratio (INR) [11] [48].
Amiodarone inhibits P-glycoprotein (P-gp) and several cytochrome P450 isoenzymes, such as CYP1A2, CYP2C9, CYP2D6, and CYP3A4, thus increasing the plasma concentrations of drugs metabolized by these pathways or that are substrates of P-gp [94]. Dosage modifications are necessary for medications such as digoxin, flecainide, and warfarin; it is also important to monitor digoxin concentrations and the international normalized ratio (INR) [57][58].
Cholestyramine may decrease the absorption of amiodarone [59]. Since diltiazem and verapamil inhibit both CYP3A4 and P-glycoprotein (P-gp), adjusting the dosages of drugs metabolized by CYP3A4 or are substrates of P-gp becomes necessary [59]. Furthermore, verapamil has the capacity to suppress the liver's metabolism of lipophilic beta-blockers, resulting in elevated plasma concentrations of these medications [60].
There is a significant pharmacokinetic interaction between certain antiarrhythmic/rate controlling medications (such as amiodarone, quinidine, dronedarone, verapamil, digoxin, and diltiazem) and non-vitamin K antagonist oral anticoagulants (NOACs) due to competition for P-glycoprotein (P-gp) or inhibition of CYP3A4 (notably by diltiazem, dronedarone, and verapamil) [61] [62].
Due to these interactions leading to elevated plasma levels of NOACs, experts advise against combining dronedarone with dabigatran and recommend reducing the dose of edoxaban by 50% [62] [63]. Consider reducing the dose of all non-vitamin K antagonist oral anticoagulants (NOACs) when administering amiodarone alongside other P-gp competing substances [64].
Prescribers recommend reducing the dose of dabigatran (Pradaxa) when used with verapamil. Combining edoxaban with verapamil, especially when other P-gp competitors are present, may also necessitate a dose reduction [65].


Self Quiz
Ask yourself...
- Considering the extensive metabolism of antiarrhythmic drugs in the liver and their excretion through bile or urine, how do renal and liver dysfunctions affect the pharmacokinetics of these drugs?
- What principles should guide the adjustment of dosages in patients with such conditions to maintain therapeutic efficacy while minimizing toxicity?
Other Antiarrhythmic Drugs
- Adenosine is effective for both diagnosing and halting supraventricular tachycardia (SVT) arising from atrioventricular nodal reentrant tachycardia (AVNRT) or orthodromic atrioventricular reentrant tachycardia (AVRT) [83]. Adenosine serves as a diagnostic aid by revealing underlying atrial flutter or atrial tachycardia (AT) [83]. Adenosine can also terminate focal AT caused by a triggered mechanism and distinguish focal AT from AVNRT and AVRT [83]. Adenosine, a purine nucleoside, results from the breakdown of adenosine triphosphate [86]. Within cardiomyocytes, it interacts with Gi-protein type 1 receptors, facilitating swift potassium efflux and hyperpolarization, while also inhibiting calcium influx [86]. These actions decrease the heart rate and slow down conduction velocity by targeting the AV node.
- Digoxin is not a first-line therapy for ventricular rate control in patients with AF, a combination of digoxin and beta-blocker/or non-dihydropyridine calcium channel blockers is a reasonable rate control option in patients with AF and heart failure [84].
Treatment of Overdose
In instances of antiarrhythmic drug overdose, medical professionals must ensure the patient has a clear airway, adequate breathing, and support for circulation [4] [87]. Managing cardiac arrest and severe toxicity from poisoning involves the use of specialized interventions, including antidotes and venoarterial extracorporeal membrane oxygenation (VA-ECMO), alongside fundamental and advanced life support techniques [87].
Symptoms such as nausea, vomiting, neurological manifestations, and lethal arrhythmias characterize Digoxin toxicity [88]. To treat ventricular tachyarrhythmias from digoxin toxicity, clinicians can use lidocaine, and atropine serves as an option for bradyarrhythmia’s. In addition, digoxin-specific antibody fragments prove effective in severe toxicity cases [89].
Therapeutic and excessive dosages of dofetilide may induce Torsades de Pointes (TdP), which clinicians manage by reducing or stopping the drug's dosage [90]. If the arrhythmia persists, initial treatment involves activated charcoal if ingestion occurred within the last 15 minutes, followed by intravenous magnesium and correction of any electrolyte imbalances [90].
For persistent arrhythmias, administering isoproterenol/dopamine may serve as a temporary measure until initiating pacing [90].
In cases of beta-blocker poisoning, treatments involve administering catecholamines, applying high-dose insulin euglycemic therapy, and using vasopressors, noting glucagon for its positive effects on hemodynamics [91].
Treating calcium channel blocker (CCB) overdoses involves administering intravenous calcium, dopamine, and norepinephrine. High-dose insulin therapy can reduce mortality in cases of calcium channel blocker poisoning [60]. For severe shock or cardiac arrest resulting from these overdoses, extracorporeal life support is employed [60]. Case reports indicate that clinicians use lipid emulsion therapy to treat overdoses of amiodarone and flecainide [4] [92].

Self Quiz
Ask yourself...
- How do the principles of emergency management in the treatment of severe toxicity from antiarrhythmic drug overdose?
- What factors determine the choice of specific treatments for complications such as lethal arrhythmias, digoxin toxicity, Torsades de Pointes, beta-blocker poisoning, and calcium channel blocker overdoses?
Conclusion
Arrhythmias encompass a broad spectrum of heart rate and rhythm disturbances and present significant clinical challenges. Atrial fibrillation (AF) is the most prevalent arrhythmia, associated with increased morbidity, mortality, and healthcare costs [2][3]. Management involves antiarrhythmic drugs (AADs), which play a fundamental role despite their limitations and the potential for adverse effects.
Antiarrhythmic agents, classified by their primary action mechanism on the cardiac action potential, impact ionic channels or receptors, aiming to suppress arrhythmias [4]. The management objectives for arrhythmias include alleviating significant clinical symptoms and extending life.
Pharmacokinetic aspects, such as drug absorption, distribution, metabolism, and excretion, play crucial roles in the effectiveness and safety of AADs. Pharmacodynamics involves modifying the cardiac action potential and conduction velocity to prevent or terminate arrhythmias. Factors influencing drug efficacy include genetics, environmental conditions, and the patient's specific clinical profile.
Treatment of overdose with antiarrhythmic drugs requires immediate medical intervention, including antidotes and supportive measures like venoarterial extracorporeal membrane oxygenation (VA-ECMO) for severe cases. The management of specific drug toxicities, such as digoxin and beta-blockers, involves targeted therapies and supportive care to mitigate adverse effects and stabilize the patient's condition.
Conclusion
Arrhythmias encompass a broad spectrum of heart rate and rhythm disturbances and present significant clinical challenges. Atrial fibrillation (AF) is the most prevalent arrhythmia, associated with increased morbidity, mortality, and healthcare costs [2][3]. Management involves antiarrhythmic drugs (AADs), which play a fundamental role despite their limitations and the potential for adverse effects.
Antiarrhythmic agents, classified by their primary action mechanism on the cardiac action potential, impact ionic channels or receptors, aiming to suppress arrhythmias [4]. The management objectives for arrhythmias include alleviating significant clinical symptoms and extending life.
Pharmacokinetic aspects, such as drug absorption, distribution, metabolism, and excretion, play crucial roles in the effectiveness and safety of AADs. Pharmacodynamics involves modifying the cardiac action potential and conduction velocity to prevent or terminate arrhythmias. Factors influencing drug efficacy include genetics, environmental conditions, and the patient’s specific clinical profile.
Treatment of overdose with antiarrhythmic drugs requires immediate medical intervention, including antidotes and supportive measures like venoarterial extracorporeal membrane oxygenation (VA-ECMO) for severe cases. The management of specific drug toxicities, such as digoxin and beta-blockers, involves targeted therapies and supportive care to mitigate adverse effects and stabilize the patient’s condition.
Antipsychotic Prescribing
Introduction
There are many intricacies surrounding mental health conditions, notably psychosis. Can you imagine being placed into an anti-gravity machine without holding on to any sort of anchor? I imagine this loss of control would be terrifying. Similarly, psychosis can disorient and destabilize patients, as they have lost their grip on reality and their perceptions are no longer reliable. Psychosis is characterized by hallucinations, delusions, disorganized thinking, and impaired social functioning.
The use of antipsychotics has resulted in decreased mortality and improved patient’s quality-of-life; however, adverse drug reactions from these drugs are major challenges in treating patients with psychotic disorders (2).
In this course, we will review conditions associated with psychosis and explore the crucial role of antipsychotic medications in restoring stability and fostering recovery. Through a comprehensive understanding of antipsychotics and their uses, mechanisms of action, adverse reactions, and contraindications, prescribers can play a pivotal role in administering these treatments with precision and compassion. The ultimate goal is to empower patients to regain their footing and take back control over their lives.
Case Study
Lilly, age 36, presents to the urgent care clinic with complaints of a large and bleeding laceration on her tongue, which she got from biting her tongue while eating earlier this evening. She reports, “I guess you have to take the good with the bad”, which puzzles you, but you decide not to further question what this means right now. While reviewing her chart, you note a diagnosis of schizoaffective disorder.
Medical History: Lilly's medical history is significant for a family history of mental illness. Her paternal grandmother was diagnosed with schizophrenia. Lilly has been on antipsychotic medication since her diagnosis 10 years ago, with varying degrees of success in managing her symptoms. Lilly has struggled with medication adherence, often discontinuing the medication due to side effects or a belief that she no longer needed treatment.
Current Presentation: At present, Lilly reports strict adherence to her medication regimen with exacerbation of her symptoms for four years, and grateful that her paranoia and auditory hallucinations have reduced in frequency. She also states, “I cannot remember what the physician told me about the medication side effects, but it cannot be as frightening as my life had become.” She has a history of delusions and hallucinations, accompanied by long-term depression and anxiety.

Overview of Psychosis
Instead of reviewing all mental health conditions, we will examine psychosis, as treatment of this symptom is one of the main goals for antipsychotics. Psychosis can be described as a burden of interruption to an individual’s thoughts and perceptions that make it difficult for them to recognize what is real and what isn’t. Most people who have experienced psychosis describe it as frightening and confusing.
Psychosis is actually a symptom, not an illness. As many as 3 in 100 people will have an episode of psychosis at some point in their lives (8). This symptom can be present in different conditions.
Early or first-episode psychosis (FEP) refers to the initial occurrence of the symptom of distortion of reality.
Psychopathology
Mental health professionals need the ability to carefully assess and precisely describe signs and symptoms in a qualified manner. Psychopathology is a discipline that applies systematic methods to study abnormal functioning of psychic activity, with the intent to elaborate subdivisions, classifications, and theories, to identify the causes of mental illnesses.
Psychopathology applies direct observation of the clinical manifestations of mental illnesses to diagnostic systems (e.g., Diagnostic and Statistical Manual of Mental Disorders-5) which outlines signs, symptoms, and features that are required to establish a diagnosis.
Psychopathology can be broadly divided into two main subgroups (3):
- Descriptive psychopathology - involves the description and denomination of mental states and abnormal behaviors of the patient, carefully removing theoretical assumptions and personal interpretations.
- Interpretative psychopathology - the understanding of a human subjective experiences and attempting to explain these features using theoretical models.
Early Warning Signs Before Psychosis
Early psychosis or FEP rarely has a sudden onset. Typically, an individual has gradual, non-specific changes in thoughts and perceptions.
Early warning signs include the following (8):
- Difficulty concentrating
- Suspiciousness or uneasiness with others
- Poor self-care or personal hygiene
- Isolation
- A worrisome change in job performance completion of typical duties
- Strong, inappropriate emotions or the absence of response or emotions at all
Signs Of Early or First-Episode Psychosis
It can be difficult to pinpoint the initial episode of psychosis, but these signs and symptoms strongly indicate an episode of psychosis:
- Hearing, seeing, tasting, or believing things that others don’t
- Persistent, unusual thoughts or beliefs that can’t be set aside regardless of what others believe
- Strong and inappropriate emotions or no emotions at all
- Withdrawing from family or friends
- A sudden decline in self-care
- Trouble thinking clearly or concentrating
Such warning signs often point to a person’s deteriorating health, and a physical and neurological evaluation can help find the problem. A mental health professional performing a psychological evaluation can determine if a mental health condition is involved and discuss next steps. If the psychosis is a symptom of a mental health condition, early action helps to keep lives on track.
Psychosis
Psychosis includes a range of symptoms but typically involves one of these two major experiences (6):
Hallucinations - seeing, hearing, or feeling things that aren’t there, such as the following:
- Hearing voices (auditory hallucinations)
- Seeing glimpses of objects or people that are not there or distortions
Delusions - strong beliefs that are not consistent and unlikely to be true, and may seem irrational to others, such as the following (6):
- Believing external forces are controlling thoughts, feelings, and behaviors
- Believing that trivial remarks, events, objects have personal meaning or significance
- Thinking you have special powers or even that you are God
Causes of Psychosis
The medical and research community is still learning about how and why psychosis develops, but several factors are thought to be involved.
Several factors that can contribute to psychosis:
- Genetics
- Many genes can contribute to the development of psychosis, but just because a person has a gene doesn’t mean they will experience psychosis. Ongoing studies will help us better understand which genes play a role in psychosis.
- Trauma
- A traumatic event such as a death, war, or sexual assault can trigger a psychotic episode. The type of trauma—and a person’s age—affects whether a traumatic event will result in psychosis.
- Substance use
- The use of marijuana, LSD, amphetamines, and other substances can increase the risk of psychosis in people who are already vulnerable.
- Physical illness or injury
- Traumatic brain injuries, brain tumors, strokes, HIV, and some brain diseases such as Parkinson’s, Alzheimer’s and dementia can sometimes cause psychosis.
- Mental health conditions
- Sometimes psychosis is a symptom of a condition like schizophrenia, schizoaffective disorder, bipolar disorder, or depression.
These mental health problems have catastrophic effects on an individual’s life. Schizophrenia (SCZ) and bipolar disorder (BPD) are two of the most relevant mental disorders when focusing on functional impairment (3). There are significant implications for poor long-term functional outcomes, such as lower rates of employment, difficulties in living independently, and harming or preventing stable relationships. The World Psychiatry Association explains that cognition is highly related to functional outcome.

Self Quiz
Ask yourself...
- Have you ever cared for a patient experiencing psychosis?
- Can you name some factors that can contribute to the development of psychosis?
- What are some possible long-term outcomes that untreated psychosis can lead to?
- How would you describe signs of early or first-episode psychosis?
Types of Antipsychotics
Antipsychotic drugs tend to fall into one of two categories:
- First Generation Antipsychotics
-
- Referred to as “Typical” antipsychotics
- Older
- Second Generation Antipsychotics
- Referred to as “Atypical” antipsychotics.
- Newer
- In general, they cause less severe neuromuscular side effects than first generation antipsychotics.
- Second generation antipsychotics may be more likely to cause serious metabolic side effects such as rapid weight gain and changes to blood sugar levels.
Both types can potentially work for different people. Remember, the different types of antipsychotics have different side effects.
Indications for Antipsychotic Prescribing
Schizophrenia is the primary indication for antipsychotic agents (2). However, the use of antipsychotics in the treatment of mood disorders such as type 1 bipolar disorder (BD-1), depression with psychosis, and treatment-resistant depression have become widely used in the last decade. The following are descriptions of the indications for antipsychotic use.
Schizophrenia and Schizoaffective disorders
Schizophrenia is a chronic disorder that affects less than one percent of the U.S. population (1). When schizophrenia is active, symptoms can include delusions, hallucinations, disorganized speech, difficulty thinking and lack of motivation. Antipsychotic drugs are the mainstay of treatment for this condition.
Antipsychotic drugs are also indicated for schizoaffective disorders, which show characteristics of both schizophrenia and affective disorders. The psychotic aspects of the illness require treatment with antipsychotic drugs, along with other drugs such as antidepressants, lithium, or valproic acid (2).
Acute Mania
The manic phase in bipolar affective disorder often requires treatment with antipsychotic agents. First-generation antipsychotics are effective in the treatment of acute mania with psychotic symptoms and all second-generation antipsychotics (except clozapine) can also be used as a treatment of symptoms of acute mania.
Major Depressive Disorder with Psychotic features
First or second-generation antipsychotics, along with an antidepressant, is typically the treatment of choice for depression with psychotic features.
Personality Disorders
First-generation antipsychotics are indicated in the treatment of paranoia and delusions associated with personality disorders. Borderline personality disorder is a type of personality disorder that can have symptoms of psychosis and paranoia; both first and second-generation antipsychotics are used for the treatment of these symptoms.
Dementia and Delirium
A low dose of high potency first-generation antipsychotics like haloperidol is recommended for the treatment of agitation in delirium and dementia. It is essential to use caution in elderly patients as the antimuscarinic effects can cause significant adverse effects in this population. Second-generation antipsychotics can also be used for treating behavioral disturbances in dementia. Off-Label use of second-generation antipsychotics is acquired immunodeficiency syndrome-related dementia.
Substance-Induced Psychotic Disorder
In cases of severe psychosis secondary to substance use, antipsychotics can be used to control agitation symptoms. Caution is necessary when using first-generation antipsychotics in alcohol withdrawal and phencyclidine intoxication.
Non-Psychiatric Indications
- Antiemetic effect: Older first-generation antipsychotic drugs (with the exception of thioridazine).
-
- This action is due to dopamine-receptor blockade
- Some drugs, such as prochlorperazine and benzquinamide, are used solely as antiemetics.
- H1-receptor-blocking
-
- Phenothiazines have been used for relief of pruritus or, in the case of promethazine, as preoperative sedatives.

Figure 1. Indications for Antipsychotics (Designed by course author, 2024)

Self Quiz
Ask yourself...
- Can you describe the symptoms of schizophrenia?
- What are some conditions that antipsychotic drugs may be used for?
- What are some precautions needed when using antipsychotic drugs to treat substance-induced psychotic disorders?
- Can you describe the antiemetic effect of these drugs?
How Do Antipsychotics Work on the Brain?
There are several researched reasons why antipsychotic drugs may help to reduce psychotic symptoms, these include:
Blocking the Action of Dopamine
It is a common perception that many psychotic experiences are caused by the brain producing too much dopamine. Dopamine is a neurotransmitter, which means that it passes messages around in your brain. Most antipsychotic drugs are known to block some of the dopamine receptors in the brain. This reduces the flow of these messages and ultimately helps to reduce your psychotic symptoms.
Dopamine is an important central nervous system neurotransmitter in the body. It belongs to the catecholamine family, which includes dopamine, norepinephrine, and epinephrine. Dopamine is the first catecholamine made in the biosynthetic pathway, produced by the decarboxylation of L-3, 4-dihydroxyphenylalanine (dopa) by aromatic amino acid decarboxylase (15).
Dopamine is stored in vesicles that are released into the synaptic cleft; dopamine binds to dopamine receptors at the synapse (15). There are five different types of dopamine receptors (D1, D2, D3, D4, and D5), all receptors have different pharmacological, biochemical, and physiological functions.
These receptors are divided into two receptor families (15):
- D1-like receptor family: D1 and D5 receptors
- D2-like receptor family: D2, D3, and D4 receptors
Dopamine pathways are neuronal connections in which dopamine travels to areas of the brain and body to relay messages such as executive thinking, cognition, feelings of reward and pleasure, and voluntary motor movements. Dopamine is responsible for many functions in the brain, including actions and perceptions, voluntary movements, motivation, punishment and reward, sleep, mood, attention, memory, and learning (15).
Affecting Other Brain Chemicals
Most antipsychotics are known to affect other brain chemicals too. This may include the neurotransmitters serotonin, noradrenaline, and glutamate. These chemicals are thought to be involved in regulating your mood.
Parkinsonism
Some of the medical and research community believe that certain antipsychotics work by causing Parkinsonism, which is a movement disorder. This means they can induce the physical symptoms of Parkinsonism as side effects; they are also known to produce psychological symptoms of Parkinsonism, such as lacking appropriate emotions or losing interest in activities. These effects are more common with first-generation, or 'typical' antipsychotics.

Self Quiz
Ask yourself...
- How would you describe the role of dopamine in the central nervous system?
- Can you name examples of messages that dopamine transports within the brain?
- Do all dopamine receptors have the same physiological functions?
- Do you think elevated levels of dopamine could negatively impact mood, attention, sleep, and voluntary movements?
Case Study (Continued)
Following the treatment for Lilly’s oral laceration, she asks if this report will be sent to her primary care provider (PCP). She states she is not followed by a psychiatrist, but she gets her routine prescription for Chlorpromazine from her PCP.
Previous medical history:
- Schizoaffective disorder, diagnosed 2013
- Hypothyroidism, diagnosed 2010
Her medication list includes the following:
- Chlorpromazine 400mg, PO, Twice Daily
- Synthroid 75mcg, PO, Daily
Lilly reports taking Benadryl every night to help her sleep (which is not on her medication list), as she struggles with ongoing insomnia.
Pharmacokinetics of First-Generation Antipsychotics: Dopamine Receptor Antagonists (DRA)
First-generation antipsychotics are dopamine receptor antagonists (DRA). They are known as typical antipsychotics. The first-generation antipsychotics work by inhibiting dopaminergic neurotransmission, with the peak effectiveness when 72% of the D2 dopamine receptors in the brain are blocked (4). They also have noradrenergic, cholinergic, and histaminergic blocking action.
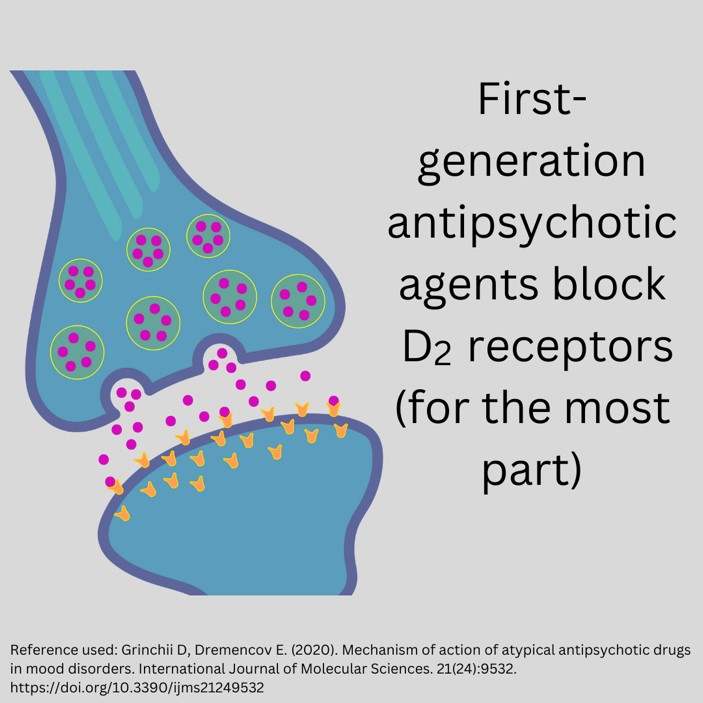
Figure 2. Blocking Action of First-Generation Antipsychotics (Designed by course author, 2024)
First-generation antipsychotics have the following approved uses:
- Psychotic disorders
- Schizophrenia
- Sedation for psychosis
- Acute agitation
- Behavioral disorders
- Schizophrenia and bipolar I agitation
- Non-psychotic anxiety
- Tourette syndrome (a nervous system disorder involving repetitive movements or unwanted sounds)
- Nausea and vomiting
It is important to note that adverse reactions of first-generation antipsychotics are highly prevalent in a significant number of patients. This warrants prescribers to perform risk minimization strategies including staff training on identification, management, and prevention, revision of treatment guidelines and algorithms, and laboratory protocol set-up to enable therapeutic and adverse event monitoring (2).
Examples of dopamine receptor antagonists (DRA) include (4):
- Butyrophenones (haloperidol)
- Phenothiazines (trifluoperazine, perphenazine, prochlorperazine, acetophenazine, triflupromazine, mesoridazine)
- Thioxanthenes (thiothixene, chlorprothixene),
- Dibenzoxazepines (loxapine)
- Dihydroindoles (molindone)
- Diphenylbutylpiperidines (pimozide)
Mechanism of Action of Dopamine Receptor Antagonists (DRA)
There are five dopaminergic pathways that are important for understanding schizophrenia and the mechanism of action of antipsychotic drugs.
- Mesolimbic-mesocortical pathway
-
- Projects from cell bodies in the ventral tegmentum in separate bundles of axons to the limbic system and neocortex
-
- The most closely related to behavior and psychosis.
- Nigrostriatal pathway
-
- Neurons that project from the substantia nigra to the dorsal striatum
- Involved in the coordination of voluntary movement
- Tuberoinfundibular system
-
- Occurs in the arcuate nuclei and periventricular neurons and releases dopamine into the pituitary portal circulation.
- Dopamine released by these neurons inhibits prolactin secretion from the anterior pituitary.
- Medullary-periventricular pathway
-
- Consists of neurons in the motor nucleus of the vagus
- This system is thought to be involved in eating patterns and behavior.
- Incertohypothalamic pathway
-
- Connections from the medial zona incerta to the hypothalamus and the amygdala
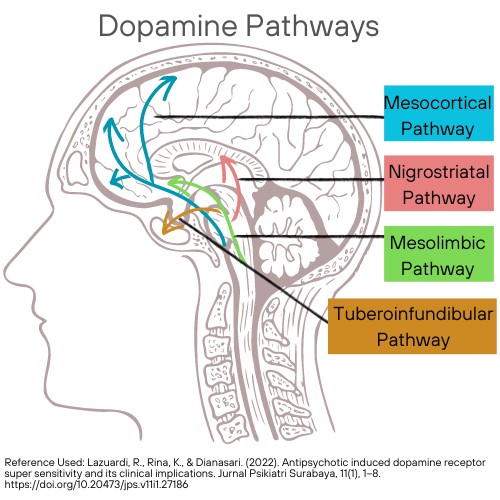
Figure 3. Dopamine Pathways. (This design is copyrighted by Abbie Schmitt, RN, MSN, 2024, and may not be reproduced without permission from Nursing CE Central)
At present, five dopamine receptors have been described, consisting of two separate families, the D1-like (D1, D5) and D2-like (D2, D3, D4) receptor groups.
The antipsychotic action is thought to be mostly produced by their ability to block the effect of dopamine; D2 receptors inhibit the activity of adenylyl cyclase in the mesolimbic system (4).
The D1-like receptor is coded by a gene on chromosome 5, increases cAMP by Gs-coupled activation of adenylyl cyclase, and is located mainly in the putamen, nucleus accumbens, and olfactory tubercle and cortex (2). D5, is coded by a gene on chromosome 4, also increases cAMP, and is found in the hippocampus and hypothalamus.
The D2 decreases cAMP (by Gi-coupled inhibition of adenylyl cyclase), and inhibits calcium channels, but opens potassium channels (2). It is found both pre- and postsynaptically on neurons in the caudate-putamen, nucleus accumbens, and olfactory tubercle. A second member of this family, the D3 receptor is thought to also decrease cAMP and is located in the frontal cortex, medulla, and midbrain. D4 receptors also decrease cAMP and are concentrated in the cortex (2).
The first-generation antipsychotic agents block D2 receptors for the most part, and their binding affinity is correlated with clinical antipsychotic and extrapyramidal potency. The degree of this blockade in D2 receptors and relation to other actions varies considerably among drugs (2).
The first-generation antipsychotics also depress the release of hormones by the hypothalamus and pituitary gland. Loxapine, in addition to D2 receptors, blocks the activity of serotonin 5-HT2A receptors (4).

Self Quiz
Ask yourself...
- Can you describe the five dopaminergic pathways?
- Does the degree D2 receptor blocking vary among first-generation antipsychotic drugs?
- Are there commonly known side effects of these drugs?
- What are some risk minimization strategies that prescribers can use?
Case Study (Continued)
You ask Lilly to describe what happened when she bit her tongue. You note scars from deep lacerations in the mucosa of her tongue, gums, and lips at varying degrees of healing.
Lilly states, “my face and mouth stiffen and jerk for several minutes at a time”. When you ask about the frequency, she reports “almost daily.” She explains that her family gets aggravated at her when she “smacks her lips” or “sticks out her tongue,” but she cannot control these movements. Her elderly mother tells her she is possessed by a demon, which Lilly says causes her significant emotional distress and embarrassment.
- What other assessment data would you collect from Lilly?
- How would you assess psychosocial factors, such as coping and support systems?
Drug-Specific Pharmacokinetics of First-Generation Antipsychotics
Butyrophenones (Haloperidol)
The following are pharmacokinetics of butyrophenones (10):
Class: Antipsychotic, neuroleptic
Black Box Warning: Risk for death in dementia-related psychosis
Uses: Psychotic disorders, control of vocal utterances in Gilles de la Tourette’s syndrome, short-term treatment of hyperactive children showing excessive motor activity, prolonged parenteral therapy in chronic schizophrenia, organic mental syndrome with psychotic features, emergency sedation of severely agitated or delirious patients.
- Metabolized by liver
- Excreted in urine, bile
- Crosses placenta; enters breast milk
- Protein binding: 92%
- Terminal half-life 12-36 hr. (metabolites)
- PO: Onset erratic, peak 2-6 hr.; half-life 24 hr.
- IM: Onset 15-30 min, peak 15-20 min; half-life: 21 hr.
- IM (Decanoate): Peak 4-11 days; half-life: 3 weeks
Contraindications: Hypersensitivity, coma, Parkinson’s disease
Precautions: Pregnancy, breastfeeding, geriatric patients, seizure disorders, hypertension, pulmonary or cardiac conditions, hepatic disease, QT prolongation, torsades de pointes, prostatic hypertrophy, hyperthyroidism, thyrotoxicosis, pediatrics, blood dyscrasias, neurological injury, bone marrow depression, alcohol and barbiturate withdrawal states, angina, epilepsy, urinary retention, closed-angle glaucoma, and CNS depression.
Phenothiazines
The following are pharmacokinetics of phenothiazines (7):
Group: Nitrogen and sulfur-containing heterocyclic compounds
Uses: Treatment of schizophrenia, bipolar disorders, control nausea and vomiting, and other psychotic disorders with delusional manifestations.
Examples of phenothiazines (10):
- Chlorpromazine
- Black Box Warning: Beers Criteria: Avoid in older adults (except in schizophrenia, bipolar disorder, or short-term use as antiemetic in chemotherapy); increased risk for stroke and cognitive decline and mortality if used in dementia (10).
- Metabolized by liver, excreted in urine (metabolites)
- Crosses placenta; Enters breast milk
- 95% bound to plasma proteins
- Elimination half-life: 23-37 hr.
- PO: Absorption variable, widely distributed, onset erratic 30-60 min, duration 4-6 hr.
- PO/extended release (ER): Onset 30-60 min, peak unknown, duration 10-12 hr
- IM: Well absorbed, peak 15-20 min, duration 4-8 hr. IV: Onset 5 min
- Fluphenazine
- Black Box Warning: Increased mortality reported with dementia-related psychosis.
- Metabolized by liver
- Excreted in urine (metabolites)
- Crosses placenta; Enters breast milk
- Protein binding >90%, not dialyzable
- PO/IM (HCl): Onset 1 hr, peak 90-120 min, duration 6-8 hr, half-life 15 hr
- IM/SUBCUT (decanoate): Onset 1-3 days; peak 1-2 days, duration over 4 wk, single-dose half-life 7-10 days, multiple dose 14.3 days
Phenothiazines produce the most optimal results when combined with non-pharmacological psychotherapeutic therapy, such as narrative, meta-cognitive, and mindfulness therapy (7)
Thioxanthenes (thiothixene, chlorprothixene)
The following are pharmacokinetics of thioxanthenes:
Thioxanthenes reduce antipsychotic activity by postsynaptic blocking of central nervous system (CNS) dopamine receptors, resulting in inhibition of dopamine-mediated effects; also has alpha-adrenergic blocking activity.
Example of thioxanthenes:
- Thiothixene
- Thiothixene is not approved for the treatment of patients with dementia-related psychosis (13).
- Absorption: Erratic; high lipophilicity
- Protein binding: 90%
- Metabolism: Hepatic; substrate of CYP1A2
- Half-life elimination: 34 hours
Dibenzoxazepines (Loxapine)
The following are pharmacokinetics of dibenzoxazepines (10):
Uses: Schizophrenia, bipolar disorder, Unlabeled uses: Anxiety
Black Box Warning: Acute bronchospasm, asthma, chronic obstructive pulmonary disease (COPD), emphysema
Loxapine inhalation must be administered only in a health care facility (14).
- Loxapine
- Onset of action: Oral, IM: Within 30 minutes; Inhalation: 2 minutes
- Peak effect: Oral, IM: 1.5 to 3 hours
- Duration: Oral, IM: ~12 hours
- Absorption: Oral, inhalation, IM: Rapid and complete
- Protein binding: Inhalation: ~97%
- Metabolism: Hepatic to glucuronide conjugates
- Bioavailability: Inhalation: 91% (de Berardis 2017)
- Half-life elimination: Oral: Biphasic: Initial: 5 hours; Terminal: 19 hours; Inhalation: 6 to 8 hours
- Excretion: Urine (as metabolites); feces (as metabolites)
Diphenylbutylpiperidines (Pimozide)
- Pimozide
- Onset of action: Within 1 week; Maximum effect: 4 to 6 weeks
- Duration of action: Variable
- Absorption: ≥50%
- Protein binding: 99%
- Metabolism: Hepatic
- Half-life elimination: Children 6 to 13 years (n=4): Mean ± SD: 66 ± 49 hours; Adults 23 to 39 years (n=7): Mean ± SD: 111 ± 57 hours
- Time to peak, serum: 6 to 8 hours; Range: 4 to 12 hours
- Excretion: Urine

Self Quiz
Ask yourself...
- What are the black box warnings for these drugs?
- How do the onset of action and elimination differ among these drugs?
- Are these drugs considered older or newer agents?
- What are some populations that are contraindicated for use of first-generation antipsychotics?
Adverse Effects of First-Generation Antipsychotics
Possible side effects and adverse effects of first-generation antipsychotics include (1, 2, 5, 6, 7, 8):
- Extrapyramidal symptoms, which are drug-induced movement disorders such as:
- Akathisia
- Dystonia
- Dyskinesia
- Akinesia
- Muscle stiffness
- Tardive dyskinesia
- Anticholinergic effects such as:
- Constipation
- Urinary retention
- Blurred vision
- Sedation
- Confusion
- Drowsiness
- Dizziness
- Headache
- Agitation
- Seizure
- Cerebral edema
- Peripheral edema
- Impaired regulation of body temperature
- Hypotension
- Orthostatic hypotension
- Abnormal ECG results or cardiac abnormalities
- Retinal disorders such as:
- Pigmentary retinopathy
- Retinitis pigmentosa
- Nausea
- Diarrhea
- Hypersensitivity reactions such as:
- Rash
- Pruritus (itching)
- Light sensitivity
- Abnormal liver function test results
- Sexual disfunction
Neurological Effects
First-generation antipsychotics are associated with significant extrapyramidal (EPS) side effects. The mild to severe EPS, including akathisia, sleepiness, restlessness, and autonomic effects, are unlike any associated sedatives or hypnotics. It is important that prescribers recognize this possibility and educate patients on these effects.
Tardive dyskinesia, as the name implies, is a late-occurring syndrome of abnormal choreoathetoid movements and is the most important unwanted effect of antipsychotic drugs (2). It is suspected to be caused by cholinergic deficiency secondary to sensitivity of dopamine receptors in the caudate-putamen (2). Tardive dyskinesia is estimated to have occurred in 20–40% of chronically treated patients before the introduction of the newer atypical antipsychotics, which caused the prevalence to vary greatly (11).
The majority of the medical community agree that the first step after tardive dyskinesia is noted should be to discontinue or slowly reduce the dose of the current antipsychotic agent or switch to one of the newer atypical agents, followed by elimination of all drugs with central anticholinergic action (2)
Neuroleptic malignant syndrome is a life-threatening disorder that occurs in patients who are extremely sensitive to the extrapyramidal effects of antipsychotic agents. This syndrome is believed to result from an excessively rapid blockade of postsynaptic dopamine receptors. The initial symptom is marked muscle rigidity, then fever may ensue and often reaches dangerous levels (2). The leukocytosis and high fever that is present with this syndrome may erroneously be considered as infectious process.
Altered blood pressure and pulse rate are also common (2). Muscle-type creatine kinase levels are usually elevated, which reflects the muscle damage.
Switching to an atypical antipsychotic drug following recovery is indicated.
Anticholinergic Effects
Anticholinergic adverse effects like dry mouth, constipation, and urinary retention are common with dopamine receptor antagonists like chlorpromazine and thioridazine (4). The action of H1 histamine blocking causes sedation; chlorpromazine is the most sedating, while fluphenazine, haloperidol, and pimozide are less sedating (4).
Cardiac Effects
Haloperidol can cause abnormal heart rhythm, ventricular arrhythmia, torsades de pointes, and even sudden death if injected intravenously (2). Other adverse effects include prolongation of QTc interval, prolonged atrial and ventricular contraction, and other cardiac conduction abnormalities (2).
Thioridazine has an FDA-backed warning for sudden cardiac death. Low-potency first-generation antipsychotics, like chlorpromazine or thioridazine, commonly cause orthostatic hypotension (2).
Additional Effects
First-generation antipsychotics can also lower the seizure threshold, and chlorpromazine and thioridazine are more epileptogenic than others (2).
Increased serum prolactin concentrations, with breast enlargement, amenorrhea, changes in sexual function are known adverse effects due to the action of the dopamine receptor block in the tuberoinfundibular tract (2).
Use In Pregnancy
Although antipsychotic drugs appear to be relatively safe in pregnancy, there is a small increase in teratogenic risk. If a pregnant woman could manage to be free of antipsychotic drugs during pregnancy, this would be desirable because of their effects on the neurotransmitters involved in neurodevelopment.
Drug Interactions for Antipsychotic Drugs
Antipsychotics are contraindicated in combination with other drugs that have sedative effects, including α-adrenoceptor-blocking action, anticholinergic effects, and—for thioridazine and ziprasidone—quinidine-like action (2).
Parenteral Preparations
There are parenteral forms of haloperidol and fluphenazine that are available for rapid initiation of treatment, as well as for maintenance treatment in noncompliant patients (2). It is important for prescribers to closely follow the manufacturer’s literature because the parenterally administered drugs may have much greater bioavailability (2). Fluphenazine decanoate and haloperidol decanoate are appropriate for long-term therapy in patients who cannot or will not take oral medication.
Dosage Schedules
Antipsychotic drugs are often given in divided daily doses, titrating to an effective dosage (2). The low end of the dosage range is recommended for at least several weeks. After an effective daily dosage has been defined for an individual patient, doses can be given less frequently. Once-daily doses (usually given at night) are feasible for many patients during chronic maintenance treatment. Research shows that simplification of dosage schedules often leads to better compliance.

Self Quiz
Ask yourself...
- Can you describe common adverse effects of these drugs?
- Have you ever witnessed extrapyramidal (EPS) side effects in a patient?
- Are extrapyramidal (EPS) side effects more common in first- or second-generation antipsychotics?
- What are some of the cardiac abnormalities reported with specific first-generation antipsychotic agents?
Pharmacokinetics of Second-Generation Antipsychotics
Second-generation antipsychotics are serotonin-dopamine antagonists and are also known as atypical antipsychotics.
Typical antipsychotics act almost exclusively on the dopamine system; these atypical drugs, however, regulate serotonin (5-HT), norepinephrine, and/or histamine neurotransmission as well (5).
The Food and Drug Administration (FDA) has approved the following atypical antipsychotics:
(* indicates the pharmacokinetics will be discussed in the next section)
- Aripiprazole (marketed as Abilify)*
- Asenapine Maleate (marketed as Saphris)
- Clozapine (marketed as Clozaril)*
- Risperidone (marketed as Risperdal)*
- Quetiapine (marketed as Seroquel)*
- Olanzapine (marketed as Zyprexa)
- Olanzapine/Fluoxetine (marketed as Symbyax)
- Iloperidone (marketed as Fanapt)
- Lurasidone (marketed as Latuda)
- Paliperidone (marketed as Invega)
- Ziprasidone (marketed as Geodon)
Second-generation antipsychotics are approved for treatment of the following:
| Generic Name | Indications |
| Aripiprazole |
|
| Asenapine |
|
| Clozapine |
|
| Iloperidone |
|
| Olanzapine |
|
| Paliperidone |
|
| Quetiapine |
|
| Risperidone |
|
| Ziprasidone |
|
Mechanism of Action of Second-Generation Antipsychotics: Serotonin-Dopamine Antagonists (SDA)
Typical antipsychotics act almost exclusively as blockers of dopamine-2 (D2) receptors. In contrast, second-generation atypical antipsychotic drugs are characterized by serotonin-2A (5-HT2A) antagonistic property (5). Targeting these receptors can lead to altering the excitability of 5-HT neurons.
Some atypical antipsychotics are also potent serotonin-1A (5-HT1A; aripiprazole), serotonin-1C (5-HT1C; clozapine, olanzapine, risperidone), histamine-1 (H1; olanzapine, quetiapine) and α1-(aripiprazole, clozapine, olanzapine, paliperidone, quetiapine) and α2-adrenergic (clozapine, olanzapine, paliperidone, quetiapine, risperidone) receptor blockers (5).
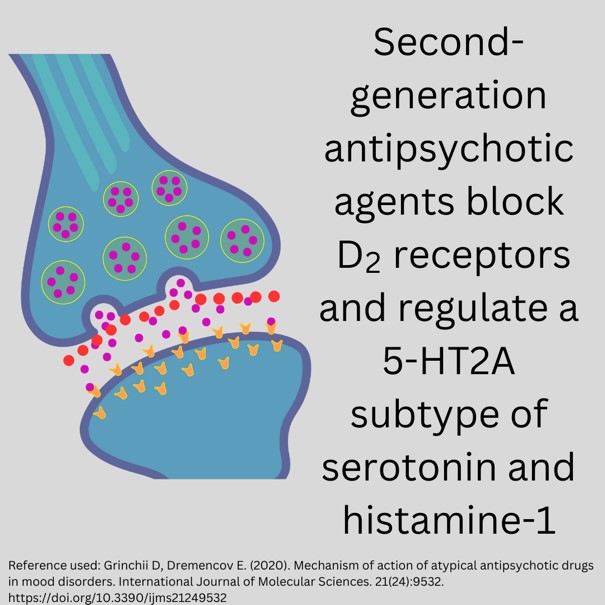
Figure 4. Blocking Action of Second-Generation Antipsychotics (Designed by course author, 2024)

Self Quiz
Ask yourself...
- Can you explain the difference in mechanism of action between first- and second-generation antipsychotic medications?
- Are you familiar with any atypical antipsychotics?
- What would be an overall benefit of targeting more than one specific neurotransmitter receptor?
- Can you name some uses for second-generation antipsychotics?
Drug-Specific Pharmacokinetics of Second-Generation Antipsychotics
These antipsychotics are identified in the Beers Criteria as potentially inappropriate medications to be avoided in patients 65 years and older due to an increased risk of cerebrovascular accidents (stroke) and a greater rate of cognitive decline and mortality in patients with dementia (12).
Aripiprazole
The following are pharmacokinetics of aripriprazole (12):
- Onset of action: Initial: 1 to 3 weeks.
- Absorption:
- IM: Extended-release: Slow, prolonged.
- Oral: Well absorbed.
- Distribution: Vd: 4.9 L/kg.
- Protein binding: ≥99%, primarily to albumin.
- Metabolism: Hepatic dehydrogenation, hydroxylation and N-dealkylation via CYP2D6, CYP3A4
- Bioavailability: Tablet: 87%
- Half-life elimination:
- Aripiprazole: 75 hours; dehydro-aripiprazole: 94 hours
- IM, extended release (terminal): ~30 to 47 days (dose-dependent).
- Time to peak, plasma:
- IM: Extended release (after multiple doses): 4 days (deltoid administration); 5 to 7 days (gluteal administration).
- Tablet: 3 to 5 hours; high-fat meals delay time to peak by 3 hours for aripiprazole and 12 hours for dehydro-aripiprazole.
- Excretion: Feces (55%; 18% of the total dose as unchanged drug; 37% of the total dose as changed drug); urine (25%)
Risperidone
The following are pharmacokinetics of risperidone (10):
- Black Box Warning: Increased mortality in elderly patients with dementia-related psychosis (10).
- PO: Extensively metabolized by liver
- Plasma protein binding: 90%
- Peak 1-2 hr.
- Excreted 90% in urine
- Terminal half-life 3-24 hr.
Quetiapine
The following are pharmacokinetics of quetiapine (10):
- Black Box Warning: Increased risk for mortality in elderly patients with dementia-related psychosis; Increased suicidal ideation in pediatric patients (10)
- Extensively metabolized by liver
- Half-life: ≥ 6 hr.
- Peak: 1.5 hr.
- Protein binding: 83%
- Excretion: <1% unchanged urine
Clozapine
The following are pharmacokinetics of clozapine (10):
- Black Box Warning: Bone marrow suppression, hypotension, myocarditis, orthostatic hypotension, geriatric patients with dementia-related psychosis, seizures, syncope (10).
- Patient-specific registration required before administration
- If WBC <3500 cells/mm 3 or ANC <2000 cells/mm 3, therapy should not be initiated
- Prescribers can only dispense 7-, 14-, 28-day supply upon receipt of lab report that is within appropriate levels.
- Completely metabolized by liver enzymes
- Bioavailability 27%-47%
- Protein binding: 97%
- Excreted in urine (50%), feces (30%) (metabolites)
- Half-life 8-12 hr.
- Clozapine can cause the following adverse effects:
- Hypersalivation
- Tachycardia
- Hypotension
- Anticholinergic side effects
- Agranulocytosis and leukopenia; therefore, requires monitoring of white blood cells and absolute neutrophil count. The FDA guidelines indicate monitoring absolute neutrophil count weekly for the first six months and, if normal, can be monitored every two weeks after that (10). Clozapine should be discontinued if absolute neutrophil count is below 1000 cells per cubic millimeter or below 500 cells per cubic millimeter in those with benign ethnic neutropenia.

Self Quiz
Ask yourself...
- Can you describe common pharmacokinetics of these second-generation antipsychotic drugs?
- What is a major adverse effect of Clozapine that must be closely monitored before prescribing?
- Can you name the black box warnings for Clozapine?
- How would you compare the pharmacokinetics of these drugs to the first-generation antipsychotics?
Adverse Effects of Second-Generation Antipsychotics
Second-generation antipsychotics (SGAs) have a decreased risk of extrapyramidal side effects as compared to first-generation antipsychotics. However, SGAs are associated with significant weight gain and the development of metabolic syndrome (2).
The FDA recommends that prescribers closely consider the following:
- Diabetes mellitus (personal and family history)
- Dyslipidemia
- BMI
- Blood pressure
- Fasting plasma glucose
- Fasting lipid profile
Risperidone is associated with dizziness, anxiety, sedation, and extrapyramidal side effects.
Paliperidone can cause temperature sensitivity to hot or cold temperatures and QTc prolongation (QTc = corrected QT interval).
Olanzapine has been associated most frequently with weight gain, increased appetite, and somnolence.
Quetiapine is the least likely to cause extrapyramidal side effects. The most common side effects of quetiapine are somnolence, orthostatic hypotension, and dizziness.
Ziprasidone has almost no weight gain but can cause prolongation of QTc. Aripiprazole is the most common side effect of agitation, headache, and akathisia-like restlessness.
Asenapine can cause an increase in serum prolactin concentrations, weight gain, and prolongation of QTc.

Self Quiz
Ask yourself...
- What does the FDA recommend to closely monitor when prescribing second-generation antipsychotics?
- What are some adverse effects of Risperidone?
- What is the most common adverse effect of Quetiapine?
- What lab work would be helpful in monitoring metabolic alterations in patients taking these drugs?
Drug Choice
Choice among antipsychotic drugs is based mainly on differences in adverse effects and possible differences in efficacy. In addition, cost and the availability of a given agent on drug formularies also influence the choice of a specific antipsychotic.
For approximately 70% of patients with psychotic features, first- and second-generation antipsychotic drugs have similar efficacy for treating positive symptoms; however, evidence shows that second-generation drugs may have fewer negative symptoms, poor cognition, risk of tardive dyskinesia, and lesser increases in prolactin levels (2).
Some of the second-generation antipsychotic drugs cause increased weight gain and increased lipid levels compared to some first-generation drugs, and a small percentage of patients develop diabetes mellitus, most often seen with clozapine and olanzapine (2). Thus, these drugs should be considered as second-line drugs unless there is a specific indication.
Uncontrollable behavior may respond equally well to all potent antipsychotics but is still frequently treated with older drugs that offer intramuscular formulations for acute and chronic treatment. The low cost of the older first-generation antipsychotic drugs contributes to their widespread use despite their risk of adverse EPS effects (2).
The best guide for selecting a drug for an individual patient is the patient history of past responses to drugs.
At present, clozapine is limited to patients who have failed to respond to substantial doses of conventional antipsychotic drugs (2). Aripiprazole is one of the most commonly prescribed second-generation antipsychotics in the U.S. due to lower side effect profile and aggressive marketing (2).


Self Quiz
Ask yourself...
- Do both types of antipsychotics (typical and atypical) have similar efficacy for treating positive symptoms?
- Which type of antipsychotics (first or second generation) are more likely to cause tardive dyskinesia?
- Which types of antipsychotics (first or second generation) are more likely to cause an increase in lipid levels?
- How would you explain the benefits and risks of each antipsychotic to a patient who has recently been prescribed one of these drugs?
Case Study (Continued)
After providing education to Lilly on the side effects of the first-generation antipsychotic medications, you note that Lilly appears anxious. However, you quickly explain that research supports that changing to a second-generation antipsychotic agent can lead to less of these involuntary muscle movements. Lilly seems relieved and hopeful.
She agrees to the mental health referral for psychiatry establishment, verbalizes understanding of the gradual taper instructions from the psychologist that consulted while at your facility, and is thankful for the counseling, outpatient therapy, and community resources. All lab work is normal at this time. The social worker at the hospital is also consulted and begins case management for Lilly, making sure she has support for areas such as housing, financial resources, and employment stability.

Self Quiz
Ask yourself...
- What type of antipsychotic agent was Lilly taking?
- What condition do her symptoms align with?
- What resources and referrals would you incorporate if you were involved in her care?
- Do you think the muscle movements and facial twitching is chronic and incurable for Lilly?
Psychosocial Treatment & Cognitive Remediation
Patients with schizophrenia need psychosocial support based around activities of daily living, including housing, social activities, returning to school, obtaining the optimal level of work they may be capable of, and restoring social interactions.
Case management and therapy services are a vital part of the treatment program that should be provided to patients with schizophrenia. First-episode patients may be particularly needful of this support because they may be more likely to deny their illness and display noncompliance with medication.

Self Quiz
Ask yourself...
- Why is it important that a case manager be involved with patients experiencing symptoms of psychosis?
- Are you familiar with social determinants of health (SDOH)?
- How can psychosis interfere with an individual’s daily activities?
- Do you think there is a stigma attached to mental health conditions?
Research
Considering that most second-generation and some first-generation antipsychotic agents are at least as potent in inhibiting 5-HT2 receptors as they are in inhibiting D2 receptors, current research is directed toward developing antipsychotic compounds that are more selective for the mesolimbic system (2). This increased selectivity would reduce their effects on the extrapyramidal system and hopefully decrease undesirable side effects.
The differences in receptor effects of various antipsychotics can explain many of their toxicities and are shown to be consistently associated with high D2 potency (2). Essentially, a significant goal of research is to find more effective blockage of dopamine activity with less involuntary movement or toxic effects.
There is also research on non-pharmacological therapies such as psychotherapy, cognitive behavioral therapy, and physical activity in improving these conditions.

Self Quiz
Ask yourself...
- What is a major goal of research when considering involuntary movement or toxic effects?
- What are non-pharmacological areas of research for treatment of psychosis?
Conclusion
As we have discussed, the use of antipsychotics has resulted in improved quality-of-life for many patients; however, prescribers must be aware of the adverse drug reactions from these drugs. Treating patients with psychotic disorders requires a holistic care plan for each patient. The pharmacokinetics of each drug, specifically the mechanism of action and side effects, can be used as an effective tool for designing a holistic care plan.
Oral STI Medications
Introduction
When hearing the phrase sexually transmitted infections, what comes to mind? If you're an advanced practice registered nurse (APRN) with prescriptive authority, you've definitely heard of sexually transmitted infections (STIs) before. Even as a nurse or maybe before nursing school, conversations about prescription drug use and sexual health existed every so often.
Presently, patients seek guidance and information on various health topics from APRNs, including medication management and sexual health. The information in this course will serve as a valuable resource for APRNs with prescriptive authority of all specialties, education levels, and backgrounds to learn more about oral medications that can treat and manage STIs.
Defining Sexually Transmitted Infections (STIs)
What Are STIs?
Sexually transmitted infections (STIs) are infections that transmitted via sexual activity, such as oral sex, vaginal sex, anal sex, and sexual skin-to-skin contact. STIs can be bacterial, viral, and parasitic in nature and infect millions of people in the USA and around the world every year. STIs can be stigmatized as only common among those who are poor or unhoused, but it is important to note that anyone who is engaging in sexual activity is at risk for a STI (1).
What Are Bacterial STIs?
Bacterial STIs include chlamydia, gonorrhea, syphilis, bacterial vaginosis, chancroid, and mycoplasma genitalium.
Chlamydia is the most common bacterial STI in the United States and a leading cause of infection-related vision loss worldwide. Chlamydia is a bacterial infection as a result of exposure to the Chlamydia trachomatis bacterium via sexual contact.
Gonorrhea is another common bacterial STI in the United States and is a bacterial infection as a result of exposure to the Neisseria gonorrhoeae bacterium via sexual contact.
In addition, syphilis is another bacterial infection as a result of exposure to the spirochete Treponema pallidum bacteria via sexual contact (4). Syphilis rates in the United States were once very minimal but have increased significantly over the past few years (4).
Bacterial vaginosis is a vaginal condition in which there is an imbalance of bacteria in the vaginal microbiome (5). Several cases of bacterial vaginosis can be related to vaginal sexual activity; however, people can have bacterial vaginosis anytime there is an imbalance of bacteria in the vaginal microbiome (5).
Chancroid is a bacterial infection that is a result of exposure to the H. ducreyi bacterium via sexual contact (6). Chancroid prevalence in the United States has decreased over the past several years but is still a bacterial STI of concern (6).
The final bacterial STI for this course is mycoplasma genitalium, in which someone is exposed to this bacterium via sexual contact.
What Are Viral STIs?
Viral STIs include herpes simplex virus (HSV), human papillomavirus (HPV), and human immunodeficiency virus (HIV). HSV, also known as herpes, is a chronic viral infection that is transmitted via sexual skin-to-skin contact and sexual activity (8). HPV is the world's most common sexually transmitted infection, a chronic viral infection, and is transmitted via sexual skin-to-skin contact and sexual activity (9).
HIV is a chronic viral infection transmitted via blood, semen, vaginal secretion, or breastmilk that can progress to acquired immunodeficiency syndrome (AIDS) if left untreated and unmanaged (10).
What Are Parasitic STIs?
Trichomoniasis is a parasitic STI that is a result of being exposed to the Trichomonas vaginalis protozoan parasite via sexual activity (11).
What If STIs Are Left Untreated?
Depending on the STI, STIs can cause several long-term complications if left untreated. If HIV is not properly managed, several complications, such as AIDS and immune-related deficiencies, can emerge (10). Untreated or repeated chlamydia and gonorrhea infections can lead to chronic pelvic pain, genital pain, genital discharge, and infertility (2,3).
If syphilis is left untreated, neurological, cardiac, and musculoskeletal complications can occur (4). While the most common STI symptom is no symptom, it is important to offer routine STI screening and be able to assess and manage positive STI results if they occur.
Defining Oral STI Medications
Oral STI medications depend on the type of infection being treated or managed. Bacterial STIs are treated with antibiotics, and some viral STIs are managed with antiviral medications. The most common oral STI medications are azithromycin, metronidazole, acyclovir, and doxycycline.
Oral STI medications are used in various clinical settings, such as hospitals, outpatient clinical settings, public health departments, correction facilities, and more. Oral STI medications are prescribed and then taken by mouth. Depending on the dosage and type of STI, someone might take only one pill of an antibiotic to cure chlamydia or take a series of pills to manage their HIV viral load.
What are the Clinical Criteria for Prescribing Oral STI Medication?
Clinical criteria for prescribing oral STI medications can vary depending on the STI itself. First, a health care provider would order and perform testing to detect STIs, such as a Pap smear, urine sample, visual examination, blood sample, or genital swab (1,2,3,4,9).
If any of these tests show a positive result for an STI, clinical guidelines from reputable organizations, such as the Centers for Disease Control and Prevention (CDC) or the National Institutes of Health (NIH), are followed to manage these conditions (1, 2). In addition, local laws and health departments might have reporting requirements if a patient tests positive for an STI, so be sure to check with your local boards of nursing or health department on any reporting requirements.
What Is the Average Cost for Oral STI Medications?
Cost for oral STI medications can significantly vary depending on the type of medication, insurance, dosage, frequency, and other factors. Cost is among a leading reason why many patients cannot maintain their medication regime (12). If cost is a concern for your patient, consider reaching out to your local pharmacies or patient care teams to find cost effective solutions for your patients.

Self Quiz
Ask yourself...
- What are some common STIs?
- What are some common medications that can be prescribed to manage STIs?

Antibiotic Pharmacokinetics
Drug Class – Oral Antibiotics for STIs
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient’s medication history and health history prior to prescribing oral medications for STIs.
Bacterial STIs include chlamydia, gonorrhea, syphilis, bacterial vaginosis, chancroid, and mycoplasma genitalium.
Oral Antibiotics Method of Action
The method of action for oral antibiotics for STI treatment depends on the antibiotic and the type of bacterium present.
Chlamydia infections are a result of exposure to the chlamydia trachomatis bacteria. A chlamydia infection can be treated with a course of doxycycline 100mg pills twice a day for seven days. Alternative treatment options include azithromycin 1 g pill as a single dose or levofloxacin 500mg pill once a day for seven days (1,2).
Doxycycline is an antibiotic that is part of the tetracycline drug class and works by preventing the growth of gram-negative and gram-positive bacteria, such as chlamydia trachomatis, Neisseria gonorrhoeae, and spirochete Treponema pallidum (13). Doxycycline works to eliminate the chlamydia trachomatis bacteria by binding to the 30S prokaryotic ribosomal unit during the protein synthesis, thus slowing down and eliminating the growth of bacteria (13).
Azithromycin and erythromycin are antibiotics that are part of the macrolide drug class and work by preventing the growth of many gram-negative and gram-positive bacteria (14). Azithromycin and erythromycin work to eliminate the chlamydia trachomatis bacteria and Hemophilus ducreyi by binding to the 50S subunit of bacterial ribosomes and leading to decreased bacterial synthesis (14).
Levofloxacin is an antibiotic that is part of the fluoroquinolone drug class and works by directly stopping bacterial DNA synthesis, as levofloxacin is considered to have the strongest activity against gram-positive, penicillin-sensitive, and resistant bacterium (15). Levofloxacin works to eliminate the chlamydia trachomatis bacteria by breaking the DNA strands through DNA-gyrase inhibition (15).
Gonorrhea infections are a result of exposure to the Neisseria gonorrhoeae bacteria. Gonorrhea infection treatment guidelines include a single injection of ceftriaxone depending on the patient’s weight (16). If ceftriaxone is a contraindication for the patient’s condition or unavailable, gonorrhea can be treated with a course of doxycycline 100mg pills twice a day for seven days (16).
Syphilis infection is a result of exposure to the spirochete Treponema pallidum bacteria (4). Syphilis infection treatment guidelines include benzathine penicillin injections, where the dosage and frequency depend on the stage of syphilis, patient age, and other co-existing health conditions. Some guidelines also recommend doxycycline 100mg pills twice a day for 14 days; however, penicillin injections appear to be more effective at syphilis management and treatment (4).
Bacterial vaginosis is not always STI, as bacterial vaginosis is the result of an imbalance of bacteria in the vaginal microbiome. However, regardless of the cause of bacterial vaginosis, current guidelines for bacterial vaginosis treatment includes metronidazole pills at 500mg twice a day for seven days with possible intravaginal application of metronidazole or clindamycin as well (5).
Metronidazole is a medication that is part of the nitroimidazole antimicrobial and antiprotozoal drug class, where its method of action involves protein synthesis inhibition (17). Metronidazole works to eliminate bacteria and Trichomonas vaginalis protozoan by causing the destruction of helical DNA structure and strand breakage, causing bacterial death (17). Tinidazole is another medication part of the nitroimidazole drug class, has a similar pharmacokinetic profile to metronidazole, and a higher cure rate for parasitic infections (17).
Chancroid is a result of exposure to the Haemophilus ducreyi (H. ducreyi) bacteria via sexual contact. Current guidelines for chancroid treatment include either a single dose of azithromycin 1g pill, a single ceftriaxone 250 mg injection, ciprofloxacin 500mg pills twice a day for three days, or erythromycin 500mg pills three times a day for seven days.
Ciprofloxacin is an antibiotic that is part of the fluoroquinolone drug class, where it works to eliminate the H. ducreyi bacteria by breaking the DNA strands through DNA-gyrase inhibition (18).
Having Mycoplasma Genitalium as an STI is a result of exposure to this bacterium. Current guidelines for mycoplasma Genitalium treatment depend on the macrolide sensitivity of the bacteria and patient condition. If the mycoplasma Genitalium is macrolide sensitive, the recommendations include doxycycline 100mg pills twice a day for 7 days followed by a single azithromycin 1mg pill, then followed by one 500mg pill once a day for three additional days (7). If the mycoplasma Genitalium is macrolide resistant or if resistance testing is not available, recommendations include doxycycline 100mg pills twice a day for 7 days followed by a single azithromycin 1mg pill, followed by moxifloxacin one 400 mg pill daily for seven days (7).
Trichomoniasis is a parasitic STI that is a result of being exposed to the Trichomonas vaginalis protozoan parasite via sexual activity (11). Current guidelines for trichomoniasis treatment include metronidazole one 500mg pill twice a day for 7 days for women or a single metronidazole 2g pill for men. An alternative treatment option for both men and women include a single tinidazole 2g pill (11).
Oral Antibiotic Side Effects
Every medication has the possibility of side effects, and oral antibiotics are no exception. Possible side effects of doxycycline include photosensitivity, GI upset, headaches, tooth discoloration, and a skin rash (13). More severe side effects of doxycycline include chest pain, leukopenia, changes in heart rate, and hepatoxicity.
Doxycycline is also contraindicated for pregnant people and children under 12 because of the teratogenic properties and risk of teeth discoloration. Doxycycline is also contraindicated for people who are allergic to tetracycline medications or penicillin (13).
Possible side effects of azithromycin and erythromycin include hepatotoxicity, GI upset, QT interval prolongation, and cardiac complications. Azithromycin and erythromycin are contraindicated in people who are allergic to macrolides (14).
Possible side effects of levofloxacin and moxifloxacin include photosensitivity, GI upset, headache, tendon rupture, changes in glucose levels, seizures, QT interval prolongation, and peripheral neuropathy. Levofloxacin and moxifloxacin are contraindicated in pregnancy and breastfeeding patients (15). Levofloxacin has FDA-issued box warnings for side effects related to tendinitis and tendon rupture, peripheral neuropathy, and central nervous system effects (15).
Possible side effects of metronidazole include peripheral neuropathy, metallic taste, GI upset, and confusion (17). Consuming alcohol and being in the first trimester of pregnancy are contraindications for metronidazole usage (17).
Possible side effects of ciprofloxacin include GI upset, QT interval prolongation, glucose level changes, and photosensitivity. FDA-issued box warnings for side effects related to ciprofloxacin include tendinitis and tendon rupture, peripheral neuropathy, and central nervous system effects (18).
Oral Antibiotics Alternatives
Given the nature of bacterial STIs, the only evidence-based method of treating bacterial STIs is with antibiotic medications (1). Condom use can help prevent the transmissions of STIs1.

Self Quiz
Ask yourself...
- What are some common STIs?
- What are some common medications that can be prescribed to manage STIs?

Antiviral Pharmacokinetics
Drug Class – Oral Antivirals for STIs
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing SSRIs.
Viral STIs include herpes simplex virus (HSV), human papillomavirus (HPV), and human immunodeficiency virus (HIV).
Oral Antivirals Method of Action
HSV, also known as herpes, is a chronic viral infection that is transmitted via sexual skin-to-skin contact and sexual activity (8). Current guidelines for HSV antiviral medication management include one acyclovir 400mg pill twice a day, one valacyclovir 500mg or 1g pill a day, or one famciclovir 250mg twice a day with a duration depending on the severity of the HSV outbreak, patient health history, and clinical presentation. Since HSV is a chronic viral health condition, dosage and frequency can vary from patient to patient.
Acyclovir and valacyclovir are an antiviral medication part of the antiviral drug class that works by incorporating into viral DNA, thus reducing further HSV synthesis (19). Valacyclovir is the prodrug to acyclovir (19). Famciclovir is a prodrug antiviral medication part of the nucleoside analog antiviral drug class, where its method of action involves inhibiting DNA polymerase, leading to decreased viral replication (20).
HPV is the world's most common sexually transmitted infection, a chronic viral infection, and is transmitted via sexual skin-to-skin contact and sexual activity (9). There are no oral STI medication options to manage HPV (9).
HIV is a chronic viral infection transmitted via blood, semen, vaginal secretion, or breastmilk that can progress to acquired immunodeficiency syndrome (AIDS) if left untreated and unmanaged (10). Given the complex pharmacological properties of HIV antiviral medications and HIV clinical manifestations, refer to specialty care for HIV for chronic management or seek additional training if possible (10).
There are several antiviral medications that can be used to manage HIV depending on the patient's health history, severity of HIV status, and clinical presentation. Oral antiviral drug classes for HIV medications include capsid inhibitors, entry inhibitors, nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), integrase strand transfer inhibitors (ISTIs), and protease inhibitors (PIs) (10).
Lenacapavir is a capsid inhibitor often prescribed at 600 mg once a day that works to distort HIV capsid protein function, thus reducing the influence of HIV in the body. Similar to HSV medications, dosage, frequency, and co-administration of other HIV-related antivirals will depend on patient response to the medication, patient health history, and patient condition (10).
Entry inhibitors work to reduce the HIV viral load by blocking HIV from entering CD4 cells. There are three main types of entry inhibitors: CCR5 antagonists, fusion inhibitors, and attachment inhibitors.
Maraviroc is an entry inhibitor pill often prescribed at 150, 300, or 600 mg, depending on patient health history and severity of HIV. Maraviroc acts as a CCR5 antagonist, where the method of action is blocking HIV from binding to the chemokine coreceptor 5 (CCR5) (10).
Enfuvirtide is an injection medication and acts as an entry inhibitor by preventing HIV from fusing to CD4 cells walls. Fostemsavir is another entry inhibitor pill often prescribed at 600mg twice daily, where the method of action is binding to the HIV glycoprotein GP120 to inhibit HIV attachment to host T cells (10).
NRTIs include abacavir, emtricitabine, lamivudine, tenofovir alafenamide, tenofovir disoproxil fumarate, zidovudine, didanosine, and stavudine. NRTIs are often given in pairs, where the most commonly prescribed pairs are tenofovir alafenamide-emtricitabine, tenofovir disoproxil fumarate-emtricitabine, and abacavir-lamivudine. Clinical management of HIV with NRTIs can depend on severity of HIV, co-existing health conditions, and patient health history. NRTIs' method of action involves undergoing intracellular phosphorylation mediated by host enzymes, allowing HIV's DNA chains to be depleted over time (10).
NNRTIs work to suppress the HIV viral load by preventing HIV-1 reverse transcriptase from creating new nucleotides to the HIV DNA chain. Common NNRTI medications include efavirenz, nevirapine, doravirine, etavirine, and rilpivirine (10).
INSTIs work to suppress the HIV viral load by targeting the strand transfer step of HIV DNA replication, thus reducing the rate in which the HIV DNA replicates. Common INSTI medications include raltegravir, elvitegravir, dolutegravir, and bictregravir (10).
Protease inhibitors work to suppress the HIV viral load by suppressing the cleaving of Gag-Pol polyproteins in HIV-infected cells, thus having cells that are not mature enough to be infectious in the body. Protease inhibitors include atazanavir, darunavir, lopinavir, indinavir, fosamprenavir, nelfinavir, saquinavir, and tipranavir (10).
Oral Antiviral Side Effects
Every medication has the possibility of side effects, and oral antivirals are no exception.
- The most common side effects of acyclovir and valacyclovir include fatigue, GI upset, confusion, headache, and neurotoxicity (19). Most common side effects of famciclovir include GI upset, headache, and hepatoxicity (20).
- Common side effects of lenacapavir include GI upset, changes in blood sugar, changes in urine, and hepatic dysfunction (10).
- Side effects commonly noted in maraviroc include skin rash, GI upset, sexual dysfunction, and anemia. There is an FDA boxed warning for maraviroc and hepatoxicity (10).
- The most common side effects of fostemsavir include increased serum creatine, prolonged QT elongation, changes in cholesterol levels, changes in glucose levels, changes in liver, and confusion (10).
- Common side effects of NRTIs include mitochondrial toxicity, which can have a significant range of clinical presentations, such as hepatic dysfunction, peripheral neuropathy, changes in cholesterol levels, or changes in pancreatic function. Zidovudine, in particular, has an FDA boxed warning for hematological toxicity, myopathy, and severe hepatomegaly (10).
- Common side effects of NNRTIs include GI upset, headache, skin rash, changes in cholesterol levels, and changes in glucose levels. The most commonly prescribed NNRTIs rilpivirine and etavirine have possible side effects of prolonged QT interval and neuropsychological effects (10).
- Side effects commonly reported with INSTIs include changes in weight, headache, and GI upset. Dolutegravir and raltegravir in particular have possible side effects of myopathy, elevations in creatine phosphokinase (CPK), and rhabdomyolysis (10).
- Common side effects of protesase inhibitors include changes in blood glucose, changes in cholesterol levels, hepatotoxicity, PR interval prolongation, GI upset, and headache (10).
Oral Antiviral Alternatives
HIV and HSV are complex, chronic conditions that are often managed with antiviral medications and require patient monitoring to observe patient response to the medications and clinical presentation.
While antiviral medications are considered the standard for evidence-based care for HSV and HIV, lifestyle modifications to strengthen one's immune system, such as increased sleep, decreased stress, and a healthy diet are thought to play a role in HIV and HSV management (10). Condom use can help prevent the transmissions of STIs (1).

Self Quiz
Ask yourself...
- What are some possible side effects of oral antiviral medications?
- What are some ways patients can maintain a healthier immune system?
Nursing Considerations
Nurses remain the most trusted profession for a reason, and APRNs are often pillars of patient care in several health care settings. Patients turn to nurses for guidance, education, and support.
While there is no specific guideline for the nurses' role in STI education and management, here are some suggestions to provide quality care for patients currently taking oral medications to manage STIs or concerned about possibly having a STI.
- Take a detailed health history. Often times, sexual health, such as pain during sex or bleeding after sex, are often dismissed in health care settings. If a patient is complaining of symptoms that could be related to a STI, inquire more about that complaint.
Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient's complaint is not being taken seriously by other health care professionals, advocate for that patient to the best of your abilities.
- Review medication history at every encounter. Often times, in busy clinical settings, reviewing health records can be overwhelming. Millions of people take antibiotics and antiviral medications for various infections. Ask patients how they are feeling on the medication, if their symptoms are improving, and if there are any changes to medication history.
- Be willing to answer questions about sexual health and oral STI medication options. Society stigmatizes open discussions of prescription medication and sexual health. There are many people who do not know about safe sexual practices, the long-term effects of undiagnosed or repeat STIs, or possible STI treatment options.
Be willing to be honest with yourself about your comfort level discussing topics and providing education on oral STI medications and STI prevention.
- Communicate the care plan to other staff involved for continuity of care. For several patients, especially for patients with viral STI infections or re-current STIs, care often involves a team of mental health professionals, nurses, specialists, pharmacies, and more. Ensure that patients' records are up to date for ease in record sharing and continuity of care.
- Stay up to date on continuing education related to oral STI medications and STIS. This is essential, as evidence-based information is always evolving and changing. You can then present your new learnings and findings to other health care professionals and educate your patients with the latest information.
You can learn more about the latest research on oral STI medications and STIs by following updates from evidence-based organizations.
How can nurses identify if someone has a STI?
Unfortunately, it is not possible to look at someone with the naked eye and determine if they have an STI. While some people might have visible STI symptoms, such as a wart or discharge, the most common STI symptom is no symptom.
APRNs can identify and diagnose if someone has a STI by taking a complete health history, listening to patient's concerns, and offering STI testing.
What should patients know about oral STI medication?
Patients should know that anyone has the possibility of experiencing side effects on antiviral or antibiotic medications for STIs, just like any other medication. Patients should be aware that if they notice any changes in their vision, experience any sharp headaches, or feel like something is a concern, they should seek medical care.
Because of social stigma associated with sexual health, people are hesitant to seek medical care because of fear, shame, and embarrassment. However, as more research and social movements discuss sexual health more openly, there is more space and awareness for STI prevention and management.
Nurses should also teach patients to advocate for their own health in order to avoid untreated or undetected STIs and possible unwanted side effects of oral STI medication.
Here are important tips for patient education in the inpatient or outpatient setting:
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors)
- Tell the health care provider of any existing lifestyle concerns, such as alcohol use, other drug use, sleeping habits, diet, menstrual cycle changes (need to identify lifestyle factors that can influence SSRI use and major depressive disorder management)
- Tell the health care provider if you have any changes in your pelvis, such as pain with urination, pain during sex, or bleeding during or after sex (potential STI symptoms)
- Tell the nurse of health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life
- Keep track of your sexual health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes)
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality is a possible side effect for ____ use)
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries
- Tell the health care provider if you notice any changes while taking medications or on other treatments to manage STIs (potential worsening or improving health situation)

Self Quiz
Ask yourself...
- What are some problems that can occur if oral medications are not managing STIs adequately?
- What are some possible ways you can obtain a detailed, patient centric health history?
- What are some possible ways APRNs can educate patients on STIs and oral STI medication options?
Research Findings
There is extensive publicly available literature on antibiotics and antiviral medications via the National Institutes of Health and other evidence-based journals.
If a patient is interested in participating in clinical trial research, they can seek more information on clinical trials from local universities and health care organizations.


Self Quiz
Ask yourself...
- What are some reasons someone would want to enroll in clinical trials?
Conclusion
STIs affect millions of people nationwide and can affect anyone who is having sex. Oral STI medication is often a first-line pharmacological option for managing several STIs. However, clinical presentation and symptom management for STIs can vary widely. Education and awareness of different STIs and different oral STI medications can influence the lives of many people in a healthy way.
Case Study #1
Sabrina is a 26-year-old Latina woman working as a teacher. She arrives for her annual exam at the local health department next to her place of work. She reports nothing new in her health, but she says she's been having some pain when she has sex and sometimes bleeds after sex.
Sabrina said she's never felt this way before, and she denies having any major changes in her life that could be affecting her pelvic health. She heard one of her friends talk about STIs, but she doesn't think she has any because she tested negative for STIs a few years ago. She wants to know if she could have an STI and what else could be causing pain and bleeding during sex.

Self Quiz
Ask yourself...
- What are some specific questions you would ask about her sexual health?
- What are some questions on health history you would want to highlight?
- What lab work would you suggest performing?
Case Study (Continued)
Sabrina agrees to provide a urine sample, complete a Pap smear, and complete bloodwork later this week. She said that no health care provider talked to her about sexual health, but she heard about different STI symptoms from her friends recently.
She's back in the office a few weeks later to discuss her lab results. Her Pap smear shows that she is HPV negative, her bloodwork is unremarkable, and her urine culture is positive for trichomoniasis and chlamydia. Sabrina states that she is shocked about the results since she is in a monogamous relationship with her boyfriend. She would like to know how she contracted two STIs.

Self Quiz
Ask yourself...
- How would you discuss Susan's sexual health concerns and her diagnosis?
- How would you discuss STI transmission routes?
Case Study (Continued)
Sabrina is willing to take antibiotics for her STI infections. She has questions about how to take these medications since she read online that antibiotics can interfere with the birth control pill. She reports taking a birth control pill called Sprintec. She also wants to know if there is a way to have treatment for her boyfriend as well and if he can get tested for STIs. Sabrina also wants to be pregnant in the future, and she would like to know if these STIs can affect her fertility.

Self Quiz
Ask yourself...
- Knowing Susan's concerns, how can you check for drug-drug interactions between her antibiotics and Sprintec?
- What patient education talking points would you discuss with Sabrina about STIs and future fertility concerns?
- What are some side effects of antibiotics to educate Susan on?
Antibiotic Use for UTI
Introduction
A urinary tract infection (UTI) can develop in anyone but is more common in females than males. Approximately 40% of American women will develop a urinary tract infection in their lives [2]. Many UTIs can lead to serious health complications, including sepsis and sometimes patient mortality.
Thus, healthcare providers must be knowledgeable of the signs and symptoms of UTIs, the available antibiotics, and UTI treatment guidelines. Understanding the different pharmacokinetics of antibiotics used to treat UTIs is essential during drug selection. This course outlines UTI antibiotic pharmacology and addresses pharmacokinetics, including mechanism of action, side effects, usage, and contraindications.
Definitions
This section covers the definitions related to UTI treatment and management.
Urinary Tract Infection
Bacterial infection of the lower urinary tract (usually confined to the bladder). This is also sometimes called cystitis and is primarily caused by the bacteria E. coli [2].
Asymptomatic Bacteremia
A urine specimen is collected on a patient and shows the presence of bacteria, but they do not have any UTI symptoms [5].
Pyelonephritis
Bacterial infection of the upper urinary tract (i.e. kidneys) [6].
Urosepsis
When a urinary tract infection causes a systemic infection, also known as sepsis [6].

Self-Quiz
Ask Yourself...
- What is a urinary tract infection?
- What is asymptomatic bacteremia?
- What is pyelonephritis?
- What is urosepsis?
Medications Overview
This section briefly reviews UTI antibiotic classes and medical indications.
Certain antibiotics are used to prevent or treat urinary tract infections and are used in both inpatient and outpatient settings. Healthcare providers should follow current guidelines regarding UTI treatment, which depends on the patient and type of urinary tract infection. UTI treatment algorithms are further divided into:
- Uncomplicated UTIs
- Complicated UTIs
- Prophylactic treatment for recurrent UTIs [6]
What constitutes uncomplicated UTIs are patients who have urinary symptoms, but do not have signs of systemic infections, like fever, flank pain, costovertebral angle (CVA) tenderness, etc. Patients can be male or female, unlike previous guidelines that categorized all males as complicated UTIs. Also, patients with uncomplicated UTIs usually have no underlying health conditions or risk factors that may affect treatment [6].
Conversely, complicated UTIs occur when patients have systemic symptoms. Patients who are pregnant, have a history of UTIs, or who are considered elderly also fall under complicated UTIs. Patients with pyelonephritis are automatically considered as having complicated UTIs as well. Patients with recurrent UTIs may be prescribed certain low-dose antibiotics for prevention [6].
Regardless of the UTI type, below are some of the common antibiotics prescribed:
- Trimethoprim-sulfamethoxazole
- Nitrofurantoin
- Fluoroquinolones
- Ciprofloxacin
- Levofloxacin
- Beta-lactams
- Cephalexin
- Amoxicillin-clavulanate
- Ceftriaxone
- Cefdinir
- Piperacillin-tazobactam
- Meropenem
- Fosfomycin
- Pivmecillinam


Self-Quiz
Ask Yourself...
- What are some factors that classify an uncomplicated UTI?
- What are some factors that classify a complicated UTI?
- What are the different names and types of antibiotics used to treat UTI?
Pharmacokinetics
This section discusses the pharmacokinetics of each antibiotic medication used to treat UTIs.
Trimethoprim-sulfamethoxazole
Sulfonamides, also called sulfa drugs, are a class of medications commonly used to treat bacterial infections, including UTIs. A common sulfonamide medication used to treat UTIs is sulfamethoxazole formulated with trimethoprim which is sometimes abbreviated as TMP-SMX, TMP-sulfa, or TMP-SMZ [22]. Trimethoprim-sulfamethoxazole is also approved by the Federal Drug Administration (FDA) to treat chronic bronchitis exacerbations, otitis media in children, and shigellosis.
This medication is also used for prevention and treatment of traveler’s diarrhea, toxoplasmosis, and Pneumocystis jirovecci and Pneumocystis carinii pneumonia. Some other off-label or non-FDA-approved uses are tuberculosis, malaria, listeria, pertussis, and community-acquired pneumonia [10].
Since this a combination medication, TMP-SMX works by two different mechanisms of action. Trimethoprim competes with the enzyme dihydrofolate reductase and subsequently stops the production of tetrahydrofolate from converting to folate.
Sulfamethoxazole, a CYP2CP inhibitor, competes with p-aminobenzoic acid during dihydrofolate synthesis. These two medications combined work against folate production and block bacterial biosynthesis of nucleic acids and proteins. Both medications are metabolized by the liver [10].
TMP-SMX is available via oral and intravenous (IV) forms. Adult TMP-SMX oral dosages are typically 160mg/800mg for the treatment of UTI, respectively, and dosages for children under 40 kilograms are weight-based. This medicaiton is best absorbed orally when taken with at least eight ounces of water. Intravenous TMP-SMX is given to hospitalized patients and dosages will vary. Some common side effects of trimethoprim-sulfamethoxazole include:
- Nausea and/or vomiting
- Rash and photosensitivity
- Dizziness
- Fatigue
- Loss of appetite and anorexia [10]
As this medication’s mechanism of action interferes with folate production, folate deficiency is also common. More severe side effects may include Stevens-Johnson syndrome, anemia, and Clostridioides difficile (C. diff) diarrhea. This medication should not be prescribed to patients with a sulfa allergy since it can cause anaphylaxis [10].
Before prescribing this medication, healthcare providers should also be aware of the precautions and contraindications. Healthcare providers should be cautious when prescribing this medication to patients with decreased kidney function, as it can lead to toxicity and high potassium levels. Therefore, baseline and frequent monitoring of blood urea nitrogen (BUN), creatinine, and potassium levels are helpful.
Other contraindications include patients with liver failure, hematological disorders, or who are pregnant. TMP-SMX interferes with several medications, including phenytoin, digoxin, diuretics, and rifampin. Many of these medication interactions increase the risk for potential hyperkalemia, medication toxicity, and QT prolongation [10].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of trimethoprim-sulfamethoxazole?
- What are the common side effects of trimethoprim-sulfamethoxazole?
- What are some contraindications of trimethoprim-sulfamethoxazole?
Nitrofurantoin
Nitrofurantoin is another antibiotic commonly prescribed to treat urinary tract infections. This medication has been FDA-approved since 1953 to treat and prevent lower UTIs and is commonly considered a first-line treatment. Currently, nitrofurantoin has no other approved or off-label uses. It comes in two different forms, which are monohydrate and macrocrystalline [16].
The mechanism of action for nitrofurantoin is not completely understood. However, it is thought to be absorbed by bacterial flavoproteins in the gastrointestinal tract and then further prevents bacterial enzymes from synthesizing DNA, RNA, and cell wall proteins [16].
Nitrofurantoin is only available via the oral route. The dosage is usually 100 mg twice daily for UTI treatment and for UTI prophylaxis is 50mg to 100mg once daily. Common medication side effects include:
- Nausea and/or vomiting
- Diarrhea
- Loss of appetite [16]
Severe reactions, although rare, are pulmonary toxicity where patients may present with fever, chills, cough, and dyspnea. It may also cause liver toxicity, liver failure, and peripheral neuropathy. This medication is contraindicated in patients with a creatinine clearance of less than 60 mL/minute, hemolysis, or who have glucose-6-phosphate dehydrogenase (G6PD) deficiency [16].
Healthcare providers should also be aware of considerations when prescribing nitrofurantoin. They must understand that nitrofurantoin should not be prescribed to patients with suspected or confirmed pyelonephritis, since it is only used to treat lower UTIs.
Nitrofurantoin should not be prescribed to people who are pregnant, especially between 38 to 42 weeks gestation, and neonates. It is also not recommended to give to patients who are 65 years or older due to increased potential adverse effects. For patients who take nitrofurantoin long-term for prophylactic use, liver function tests should be routinely completed and monitoring of pulmonary function [16].


Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of nitrofurantoin?
- What are the common side effects of nitrofurantoin?
- What are some contraindications of nitrofurantoin?
Fluoroquinolones
Fluoroquinolones are a class of antibiotics used to treat UTIs and other bacterial conditions. Examples of common fluoroquinolones include ciprofloxacin, moxifloxacin, and levofloxacin. However, ciprofloxacin is more commonly used to treat UTIs than the others and therefore, will be the medication reviewed in this section [19].
In addition to urinary tract infections, ciprofloxacin is FDA-approved to treat various health conditions. Some common health conditions treated are gonorrhea, chancroids, joint infections, prostatitis, and some gastrointestinal infections. Ophthalmic forms are used to treat corneal ulcers and conjunctivitis, while otic forms may be used in otitis externa [17].
Ciprofloxacin’s mechanism of action is considered bactericidal since it works by inhibiting bacterial DNA replication. It acts against DNA topoisomerase and DNA gyrase to hinder DNA replication. Ciprofloxacin is most effective against gram-negative bacteria, but also some gram-positive bacteria. Due to mutations in the DNA gyrase, ciprofloxacin and other fluoroquinolones have begun to show bacterial resistance over the past several years [17].
Ciprofloxacin comes in many forms, including oral, IV, ophthalmic, and otic. For the treatment of UTI, this medication is available via oral and IV forms. Recommended dosages are dependent on the severity of UTI and route. Oral dosages for UTI treatment range from 250mg to 500mg twice daily, while IV dosages can range from 200mg to 400mg twice daily to upwards of 400mg every eight hours. Regardless of the administration route, common side effects are nausea and diarrhea. Some serious adverse effects include:
- QT prolongation
- Hypoglycemia
- Hyperglycemia
- Photosensitivity [17]
Ciprofloxacin has an FDA black box warning of tendinitis and tendon rupture, peripheral neuropathy, and myasthenia gravis exacerbation. Due to the effects this medication has on tendons, Achilles tendon rupture, aortic aneurysm, and aortic dissection are also serious adverse effects. If the healthcare provider suspects any adverse effects, including mild tendonitis, the medication should be discontinued immediately.
Furthermore, when prescribing ciprofloxacin, there are additional considerations and contraindications. As with all medications, ciprofloxacin should not be prescribed to patients with a known allergy to this medication.
Ciprofloxacin should not be prescribed along with tizanidine, theophylline, or cyclosporine due to interactions. Antacids can also interfere with the absorption of ciprofloxacin and ciprofloxacin toxicity is more likely in older adults. Healthcare providers should encourage patients with diabetes to closely monitor their blood glucose levels at home since this medication can cause hypo- or hyperglycemia [17].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of ciprofloxacin?
- What are the common side effects of ciprofloxacin?
- What are some contraindications of ciprofloxacin?
- What is the black box warning of ciprofloxacin?
Beta-lactams
Beta-lactams are a class of antibiotics used to treat various bacterial conditions, including UTIs. The three main beta-lactams covered below are those commonly used to treat UTI and include cephalexin, amoxicillin-clavulanate, and ceftriaxone. Other beta-lactams that are approved for UTI treatment are cefpodoxime, cefdinir, and cefadroxil, and work similarly to others in this medication family.
Cephalexin
Cephalexin is a beta-lactam antibiotic that is classified as a first-generation cephalosporin. It was initially approved by the FDA in 1970 and is widely used throughout healthcare settings. In addition to acute and chronic UTIs, cephalexin is approved to treat upper and lower respiratory infections, bone infections, and otitis media. It is also used to treat surgical site, skin, and soft tissue infections [8].
Cephalexin falls under the beta-lactam class since its structure has a beta-lactam ring. This ring inhibits the synthesis of peptidoglycan which further disrupts the bacterial cell wall. More specifically, the beta-lactam ring binds to the penicillin-binding proteins during peptidoglycan synthesis, causing the disruption of the bacterial cell wall and viability [8].
Cephalexin is only available via oral route and can be prescribed in tablet, capsule, and suspension forms. Daily dosages from 1000mg to 4000mg for adults and for children, are weight-based and range from 25mg to 100mg per kilogram per day. Some side effects of cephalexin include:
- Abdominal pain
- Diarrhea
- Nausea and/or vomiting
- Rash
- Candidiasis [8]
Other reactions may include increased liver enzymes, C. diff colitis, and hemolytic anemia. Although cross-reactivity with penicillin is somewhat uncommon, healthcare providers should use caution when prescribing this medication to patients who are allergic to penicillin. Furthermore, it should not be prescribed to patients with a cephalosporin allergy. Cephalexin also interacts with metformin, causing decreased clearance of metformin from the body.
If a patient is taking metformin, they should be advised to closely monitor their blood glucose levels since the risk for hypoglycemia is increased. Healthcare providers should also be cautious when prescribing this medication to patients who are taking probenecid. Cephalexin can also increase prothrombin time, which typically requires monitoring, especially for those undergoing anticoagulant treatment [8].


Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of cephalexin?
- What are the common side effects of cephalexin?
- What are some contraindications of cephalexin?
Amoxicillin-clavulanate
As its name implies, amoxicillin-clavulanate is a combination medication of amoxicillin and clavulanic acid. In addition to treating UTIs, this medication is FDA-approved to treat rhinosinusitis, acute otitis media, skin infections, and aspiration and community-acquired pneumonia. Other non FDA-approved uses are impetigo, chronic obstructive pulmonary disease exacerbations, diabetic foot infections, and human and animal bites [4].
Amoxicillin-clavulanate works via two different mechanisms of action since it is a combination medication. The amoxicillin component is a beta-lactam antibiotic and works via the same mechanism as cephalexin described above. Clavulanic acid is a beta-lactamase inhibitor, which prevents bacteria from destroying beta-lactam antibiotics. Thus, the reason why clavulanic acid is often combined with amoxicillin [4].
This medication is only available via oral forms, such as suspensions, chewable, immediate-release, or extended-release tablets. Dosages are dependent on the underlying condition being treated, medication form (i.e. immediate- versus extended-release), and the patient’s age. Regardless of dosage, amoxicillin-clavulanate can lead to common gastrointestinal side effects, such as:
- Diarrhea
- Nausea
- Vomiting
- Loose stools [4]
Vaginal candidiasis is another common side effect of amoxicillin-clavulanate. For patients who are breastfeeding, this medication may cause hypersensitivity reactions in infants since it is excreted in breast milk. Additionally, amoxicillin-clavulanate has several drug interactions with medications, including probenecid, oral anticoagulants, allopurinol, and oral contraceptives. For patients on hemodialysis or with severe renal impairment, usually where their creatinine clearance is less than 30 mL/min, dose adjustments are recommended.
Healthcare providers should monitor patients’ liver enzymes for possible hepatic impairment, and if hepatic injury occurs, stop the medication immediately and follow treatment recommendations accordingly. Since amoxicillin is a penicillin derivative, it should not be prescribed to individuals with a penicillin allergy [4].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of amoxicillin-clavulanate?
- What are the common side effects of amoxicillin-clavulanate?
- What are some contraindications of amoxicillin-clavulanate?
Ceftriaxone
Ceftriaxone is another beta-lactam antibiotic used to treat UTIs and is usually an adjunct medication. It is a third-generation cephalosporin that is also used to treat gonorrhea, pelvic inflammatory disease, meningitis, and certain abdominal, respiratory, and joint infections. Additionally, ceftriaxone treats bacteremia, sepsis, and infective endocarditis. Since ceftriaxone belongs to the beta-lactam class, its mechanism of action is the same as previously described cephalexin [18].
Ceftriaxone comes in both intravenous and intramuscular (IM) forms since it is not absorbed through the gastrointestinal tract. For UTI treatment, the dosage for adults is 1 to 2 grams IV or IM every 24 hours. In an outpatient setting, ceftriaxone is often given as a single IM dose to patients with pyelonephritis who are not hospitalized. Again, this medication is used as an adjunct medication, so it is given as a single IM dose, followed by another oral antibiotic for UTI treatment. Dosages for children range from 50mg to 75mg per kilogram per day for both IM and IV forms [18]. Some common side effects of ceftriaxone are:
- Diarrhea
- Nausea
- Vomiting
- Dysgeusia (metallic or foul taste in the mouth)
- Injection site reaction, especially for IM [18]
Other adverse effects associated with ceftriaxone are hemolytic anemias, neutropenia, and thrombocytosis. It should also be noted that this medication can cause neurological symptoms, cholelithiasis, jaundice, elevated liver enzymes, and pancreatitis [18].
Healthcare providers should also review ceftriaxone’s precautions and contraindications. This medication is cross-reactive with penicillin and can cause a hypersensitivity reaction. Furthermore, it should not be prescribed to patients with a cephalosporin allergy. If ceftriaxone is administered through an IV, it must not be mixed with calcium-containing IV solutions or products. Other possible medication interactions are estradiol, cyclosporine, and bumetanide. For patients with liver or kidney impairment, dosages must be adjusted and should not exceed 2 grams per day [18].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of ceftriaxone?
- What are the common side effects of ceftriaxone?
- What are some contraindications of ceftriaxone?
Cefdinir
Cefdinir is another beta-lactam antibiotic used to treat UTIs and is also a third-generation cephalosporin. In addition to UTI treatment, cefdinir is approved for the treatment of pneumonia, bacterial infections involving the skin, and respiratory infections of the ears, throat, and sinuses. As cefdinir is a third-generation cephalosporin, its mechanism of action is the same as previously described ceftriaxone. Thus, it interferes with bacterial cell wall synthesis [13].
Cefdinir is only available via oral route by either capsule or liquid suspension. Treatment dosages and duration are dependent on the underlying condition it is being used to treat [13]. For UTI, this medication is usually prescribed at 300mg twice daily for 5 to 7 days. However, this course may be extended for patients with pyelonephritis or complicated UTIs. Some common side effects of this medication include:
- Nausea and vomiting
- Diarrhea
- Vaginal itching
- Red-tinged stools [13]
Other more serious side effects may include rash, hives, facial swelling, and difficulty breathing or swallowing. As with all medications, healthcare providers should be aware of this medication’s precautions and contraindications. Cefdinir should not be prescribed to patients with a cephalosporin allergy or who are taking probenecid. It should also be avoided in patients with gastrointestinal diseases, like colitis, and kidney disease. This medication should be taken at least two hours apart from any aluminum, magnesium, or iron supplement. Additionally, healthcare providers should avoid prescribing the oral suspension form to patients with diabetes, since it contains high amounts of sucrose and can potentially raise blood sugar levels [13].


Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of cefdinir?
- What are the common side effects of cefdinir?
- What are some contraindications of cefdinir?
Other Antibiotics Used to Treat UTI
This section reviews other antibiotics used to treat urinary tract infections. Two common additional antibiotics administered in an inpatient setting include piperacillin-tazobactam and antipseudomonal carbapenems, such as imipenem or meropenem. These are usually reserved for patients with at least one risk factor for multidrug-resistant gram-negative organisms [7]. Drug information about meropenem will be discussed in greater detail below. Other less common antibiotics available in the outpatient are fosfomycin and pivmecillinam. Although these medicatios are used less commonly, it is still important to understand their pharmacokinetics.
Piperacillin-tazobactam
As mentioned, piperacillin-tazobactam is used to treat multidrug-resistant gram-negative UTIs in an inpatient setting. In addition to treating UTIs, it is approved for the treatment of skin, gynecological, and certain abdominal infections. This medication is a combination of piperacillin (a penicillin antibiotic) and tazobactam (a beta-lactamase inhibitor). Therefore, its mechanism of action is that of both the penicillin and beta-lactam classes as previously described [15].
Piperacillin-tazobactam is available in IV form and the dosage is usually 3.375 grams every six hours [7]. Like many antibiotics, some common side effects include:
- Diarrhea
- Nausea and/or vomiting
- Stomach pain [15]
This medication can also cause mouth sores, sleeping difficulties, and in more severe cases, itching, difficulty swallowing, and wheezing. Piperacillin-tazobactam should not be prescribed to patients who are taking other penicillin or beta-lactam antibiotics or who have an allergy. It interferes with certain medications including, aminoglycosides, anticoagulants, methotrexate, and vancomycin. Additionally, for patients with diabetes, this medication can cause false results with certain glucose tests [15].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of piperacillin-tazobactam?
- What are common side effects of piperacillin-tazobactam?
- What are some contraindications of piperacillin-tazobactam?
Meropenem
An antipseudomonal carbapenem, meropenem, is used to treat inpatient multidrug-resistant gram-negative UTIs. Meropenem is also approved for the treatment of pneumonia, intra-abdominal infections, peritonitis, and meningitis [21].
This medication’s mechanism of action is similar to beta-lactams, as it falls under the same family of antibiotics. It binds to penicillin-binding proteins and inhibits bacterial cell wall synthesis by inhibiting peptidoglycan [21].
Meropenem is only available in IV form and dosages are dependent on the condition being treated. For UTIs, 1 gram is administered every 8 hours. Gastrointestinal side effects are common for this medication and include symptoms like diarrhea, nausea, vomiting, and constipation. Additional adverse effects may include:
- Drowsiness
- Headache
- Insomnia
- Depression [21]
Seizures are also a potential adverse effect, and therefore, healthcare providers must monitor patients for neurological symptoms. Agranulocytosis, thrombocytopenia, gastrointestinal bleeding, and hemolytic anemia are other conditions which have been reported when taking this medication. For patients with renal impairment, the dosage will need to be adjusted. Meropenem also has many medication interactions, with some major ones including afatinib, atogepant, cariprazine, and colchicine [21].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of meropenem?
- What are the common side effects of meropenem?
- What are some contraindications of meropenem?
Fosfomycin
Fosfomycin is an antibiotic that is FDA-approved to treat uncomplicated urinary tract infections and is considered a first-line treatment option. In the United States, fosfomycin is only available in oral, powder which is mixed and dissolved in liquid. Furthermore, although this medication is a first-line UTI treatment option, it is not widely available in the United States [20].
This medication’s mechanism of action works by interfering with the formation of peptidoglycan precursor UDP N-acetylmuramic acid, also known as UDP-MurNAc. As it acts one step prior to the beta-lactam antibiotic family, Fosfomycin enters the bacteria through the transporter systems L-alpha-glycerophosphate and hexose-6-phosphate. This medication also reduces the ability of bacteria to adhere to the epithelial cells of the urinary tract [9].
To treat UTI, a single dose of 3 grams of fosfomycin is given, which is added to about 3 to 4 ounces of cold water to dissolve the medication. Common side effects may include:
- Nausea
- Diarrhea
- Headache
- Back pain [14]
Other serious side effects are joint pain, rash, facial or oral swelling, and jaundice. Healthcare providers should review this medication’s interactions and contraindications. Fosfomycin interacts with medications like cisapride, metoclopramide, and certain vitamins. Healthcare providers should use caution when prescribing to patients with a history of asthma, liver disease, or who are pregnant or breastfeeding [14].

Self-Quiz
Ask Yourself...
- What is the mechanism of action for fosfomycin?
- What are some common side effects of fosfomycin?
- What are some contraindications of fosfomycin?
Pivmecillinam
Pivmecillinam is another antibiotic used to treat lower urinary tract infections and is part of the UTI treatment algorithm. However, the FDA has not approved this medication for use in the United States [11]. Therefore, most of the specific drug information is not available.

Considerations for Prescribers
This section reviews potential considerations when prescribing antibiotics for UTIs.
Healthcare providers must consider and review several factors when prescribing antibiotics for UTI treatment. First, the medication’s route, dosage, and treatment duration are usually determined by the setting (inpatient versus outpatient), the type of UTI (e.g. empirical, asymptomatic bacteremia, uncomplicated, complicated, or prophylaxis), and the patient’s underlying medical conditions and risk factors. Furthermore, healthcare providers should strive to follow current treatment guidelines, approved uses, and their organization’s protocols when initiating or adjusting these medications. Healthcare providers must review the patient’s medical history, recent lab values, contraindications, and potential side effects.
Patient Population
Certain classes of antibiotics should be avoided in specific individuals or patient populations, and thus, healthcare providers must be aware of these precautions, contraindications, and black box warnings. Ciprofloxacin can lead to medication toxicity and hypoglycemia in older adults and must be avoided in this patient population when able [17]. Additionally, prescribing medications, such as TMP-SMZ and cephalexin, should be cautioned in patients with renal impairment [8, 10]. Prescribing nitrofurantoin, TMP-SMZ, cephalexin, and ceftriaxone should be cautioned in patients with liver failure or elevated liver enzymes. Healthcare providers should routinely monitor the patient’s liver enzymes and function tests [8, 10, 16, 18].
The patient’s gender at birth plays another large factor in antibiotic selection since treatment for males is considered a complicated UTI and antibiotic duration is extended. Furthermore, in patients who are pregnant or breastfeeding, certain antibiotics should not be prescribed, with some including TMP-SMZ and fluoroquinolones. Alternative treatments for patients who are pregnant are amoxicillin-clavulanate or [6]. For patients with chronic UTIs, initial prophylactic treatment should be started for 3 months and then reevaluated thereafter for prevention. Typical low-dose prophylactic antibiotics are TMP-SMX and nitrofurantoin. However, the healthcare provider should strongly consider medication compliance and potential antibiotic resistance [1].
Allergies
Healthcare providers should also review the patient’s allergies and cross-reactivity of certain antibiotics. Trimethoprim-sulfamethoxazole should not be prescribed to individuals with a sulfa allergy. Furthermore, healthcare providers should not prescribe patients with a penicillin allergy amoxicillin-clavulanate and should use caution when prescribing these individuals beta-lactams or cephalosporins due to their potential cross-reactivity, although the percentage is low [8, 10].
Medication History
As discussed, certain antibiotics interact with specific medications. Healthcare providers must review the patient’s medication list prior to prescribing antibiotics. For instance, amoxicillin-clavulanate interacts with allopurinol and lessens the effectiveness of oral contraceptives. Patients on oral contraceptives should be instructed to use backup birth control methods while on the antibiotic [4]. Additionally, while interactions may exist medication timing plays an important role. For example, medications such as ciprofloxacin and TMP-SMZ interact with antacids. However, if the antibiotic is taken two hours before or six hours after the antacid, a potential medication interaction is less likely [17]. Cephalexin is better absorbed on an empty stomach while other antibiotics are recommended to be taken with food [8].
Bacterial Sensitivity
Some antibiotics do not treat certain strains of bacteria and thus, healthcare providers must be judicious about initial antibiotic selection and following up with the patient about their urine culture results. For example, bacterial growth on the urine culture might not be sensitive to the initial antibiotic prescribed and may be resistant. Therefore, the antibiotic may need to be changed or dual therapy may be needed.
Also, patients with recurrent UTIs sometimes develop antibiotic resistance to first-line medications for the treatment of UTI, so an alternative medication should be initially prescribed, and a urine culture sent. If the patient is treated frequently for UTIs, then a referral to urology is warranted for further evaluation [6]. In some patients, asymptomatic bacteremia is found on a routine urinalysis completed during an annual comprehensive exam. Healthcare providers should review the current screening and treatment guidelines on asymptomatic bacteria in adults. For most patients, a urine culture should be sent for further evaluation, and antibiotic administration delayed until the culture has resulted [5].
Patient Education
Patients should be instructed on potential medication side effects and signs of adverse reactions. In an outpatient setting, healthcare providers must instruct patients on worsening symptoms and when to seek immediate or emergent treatment. Oftentimes, urinary tract infections move upstream into the kidneys and cause pyelonephritis or urosepsis [6].

Self-Quiz
Ask Yourself...
- What factors should healthcare providers consider when prescribing antibiotics?
- Which antibiotic can be prescribed during pregnancy?
- Which steps should be taken for patients with recurrent UTIs?
- What health conditions and lab values are important when selecting UTI antibiotics?
Upcoming Research
This section reviews upcoming research and medications for UTI treatment.
The bacteria strain, E. coli, is typically responsible for urinary tract infections. However, this is not the case for all UTIs, and some patients have developed multiple drug-resistant organisms due to recurrent infections. Therefore, there is much research needed on UTI antibiotic treatment to eradicate these organisms. Recent development of immunomodulatory therapy has been considered as well as medications that inhibit bacterial adhesions to the epithelial cells of the urinary tract. Vaccinations against UTI have also shown recent promise, but further research is still needed [3]. Other non-antibiotic therapies are also being researched, like Lactobacillus-containing products (i.e. probiotics) and cranberry supplements [12].


Self-Quiz
Ask Yourself...
- Which bacteria commonly causes urinary tract infections?
- What new research is there about antibiotics for UTI treatment?
- Which types of new products are being researched about UTI treatment?
Conclusion
As discussed, antibiotic selection for the treatment of urinary tract infections depends on a variety of factors. Healthcare providers should understand the pharmacokinetics, potential side effects, interactions, and contraindications when selecting an antibiotic. They should also follow current clinical guidelines and their facility’s protocols for a more evidence-based approach. Furthermore, ordering a urine culture or referring a patient to a urologist is warranted for patients with recurrent urinary tract infections.

Self-Quiz
Ask Yourself...
Final Reflection Questions
- What differentiates a lower versus upper UTI?
- What are the different names of beta-lactam antibiotics used to treat UTIs?
- Which antibiotics are commonly prescribed for UTI prophylaxis?
- Which antibiotics are not commonly prescribed or available in the United States?
- Which antibiotics are commonly used to treat multi-drug resistant organisms?
- Which antibiotics can be used in outpatient versus inpatient settings?
- What are the two types of fluoroquinolones used to treat UTIs?
- What are some other antibiotics used to treat UTIs?
References + Disclaimer
- American Association of Suicidology. (2019, July 17). Suicide loss survivors. American Association of Suicidology. https://suicidology.org/resources/suicide-loss-survivors/
- American Psychological Association. (2017). What is cognitive behavioral therapy? American Psychological Association. https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
- Boland, R., Verduin, M., & Ruiz, P. (2021). Kaplan & Sadock’s synopsis of psychiatry (12th ed.). Wolters Kluwer Medical.
- Bostwick, J. M., Pabbati, C., Geske, J. R., & McKean, A. J. (2016). Suicide attempt as a risk factor for completed suicide: Even more lethal than we knew. American Journal of Psychiatry, 173(11), 1094–1100. https://doi.org/10.1176/appi.ajp.2016.15070854
- Centers for Disease Control and Prevention. (2022a, April 12). Provisional count of deaths by leading causes of death – United States, 2021. Www.cdc.gov. https://www.cdc.gov/nchs/data/health_policy/provisional-leading-causes-of-death-for-2021.pdf
- Centers for Disease Control and Prevention. (2022b, November 2). Risk and protective factors. Www.cdc.gov. https://www.cdc.gov/suicide/factors/index.html
- Centers for Disease Control and Prevention. (2023a, May 1). Suicide rates by state. Www.cdc.gov. https://www.cdc.gov/suicide/suicide-rates-by-state.html
- Centers for Disease Control and Prevention. (2023b, August 10). Suicide Data and Statistics | Suicide | CDC. Www.cdc.gov; CDC. https://www.cdc.gov/suicide/suicide-data-statistics.html
- Chu, A., & Wadhwa, R. (2023, May 1). Selective serotonin reuptake inhibitors. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK554406/
- Cleveland Clinic. (2022, April 19). Dialectical behavior therapy (DBT). Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/22838-dialectical-behavior-therapy-dbt
- Cornell Law School. (2020, July). Physician-assisted suicide. LII / Legal Information Institute. https://www.law.cornell.edu/wex/physician-assisted_suicide
- Department of Veterans Affairs. (2021, December 3). Lethal means safety & suicide prevention. Www.mirecc.va.gov. https://www.mirecc.va.gov/visn19/lethalmeanssafety/
- Fornaro, M., Anastasia, A., Valchera, A., Carano, A., Orsolini, L., Vellante, F., Rapini, G., Olivieri, L., Di Natale, S., Perna, G., Martinotti, G., Di Giannantonio, M., & De Berardis, D. (2019). The FDA “black box” warning on antidepressant suicide risk in young adults: More harm than benefits?. Frontiers in Psychiatry, 10(294). https://doi.org/10.3389/fpsyt.2019.00294
- Hardey, S. (2021, July 28). Suicide among veterans – why are veterans at a higher risk of suicide? American Addiction Centers. https://americanaddictioncenters.org/veterans/suicide-among-veterans
- Herman, J., & O’Neill, K. (2021). Suicide risk and prevention for transgender people: Summary of research findings. https://williamsinstitute.law.ucla.edu/wp-content/uploads/Trans-Suicide-Summary-Sep-2021.pdf
- Huecker, M. R., Smiley, A., & Saadabadi, A. (2020). Bupropion. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470212/
- Jacobs, D., Baldessarini, R., Conwell, Y., Fawcett, J., Horton, L., Meltzer, H., Pfeffer, C., & Simon, R. (2009). Assessment and treatment of patients with suicidal behaviors. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/suicide.pdf
- Mayo Clinic. (2019, October 5). Serotonin and norepinephrine reuptake inhibitors (SNRIs). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/depression/in-depth/antidepressants/art-20044970
- Mental Health First Aid USA. (2020). Mental health first aid USA for adults assisting adults. National Council for Behavioral Health.
- Moraczewski, J., & Aedma, K. K. (2020). Tricyclic antidepressants. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557791/
- Moutier, C. (2023, July). Suicidal behavior – psychiatric disorders. MSD Manual Professional Edition. https://www.msdmanuals.com/professional/psychiatric-disorders/suicidal-behavior-and-self-injury/suicidal-behavior?query=Suicidal%20Behavior
- Mullins, N., Kang, J., Campos, A. I., Coleman, J. R. I., Edwards, A. C., Galfalvy, H., Levey, D. F., Lori, A., Shabalin, A., Starnawska, A., Su, M.-H., Watson, H. J., Adams, M., Awasthi, S., Gandal, M., Hafferty, J. D., Hishimoto, A., Kim, M., Okazaki, S., & Otsuka, I. (2022). Dissecting the shared genetic architecture of suicide attempt, psychiatric disorders, and known risk factors. Biological Psychiatry, 91(3), 313–327. https://doi.org/10.1016/j.biopsych.2021.05.029
- National Alliance on Mental Illness. (2022, August). Risk of suicide. Nami.org. https://nami.org/About-Mental-Illness/Common-with-Mental-Illness/Risk-of-Suicide
- National Institute of Mental Health. (2020). Suicide risk screening tool. https://www.nimh.nih.gov/sites/default/files/documents/research/research-conducted-at-nimh/asq-toolkit-materials/asq-tool/screening_tool_asq_nimh_toolkit.pdf
- National Institute of Mental Health. (2023). Frequently asked questions about suicide. Www.nimh.nih.gov. https://www.nimh.nih.gov/health/publications/suicide-faq
- National Institute on Drug Abuse. (2020, July 10). Treatment and recovery. National Institute on Drug Abuse. https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery
- Pfizer Inc. (n.d.). The patient health questionnaire (PHQ-9). https://coepes.nih.gov/sites/default/files/2020-12/PHQ-9%20depression%20scale.pdf
- Sabri, M. A., & Saber-Ayad, M. M. (2020). MAO inhibitors. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557395/
- Schreiber, J., & Culpepper, L. (2023, October). Suicidal ideation and behavior in adults. Www.uptodate.com. https://www.uptodate.com/contents/suicidal-ideation-and-behavior-in-adults#H2534680824
- Seattle University. (n.d.). Breaking the stigma about suicide. Www.seattleu.edu. https://www.seattleu.edu/wellness/mental/stigma/
- Substance Abuse and Mental Health Services Administration. (2009). SAFE-T pocket card: Suicide assessment five-step evaluation and triage for clinicians. Samhsa.gov. https://store.samhsa.gov/product/SAFE-T-Pocket-Card-Suicide-Assessment-Five-Step-Evaluation-and-Triage-for-Clinicians/sma09-4432
- Substance Abuse and Mental Health Services Administration. (2016, November 1). Table 4.1, evidence-based screening tools for substance use. Www.ncbi.nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK424859/table/ch4.t1/?report=objectonly
- The Columbia Lighthouse Project. (2016a). About the protocol the Columbia lighthouse project. The Columbia Lighthouse Project. https://cssrs.columbia.edu/the-columbia-scale-c-ssrs/about-the-scale/
- The Columbia Lighthouse Project. (2016b). SAFE-T with C-SSRS. The Columbia Lighthouse Project. https://cssrs.columbia.edu/documents/safe-t-c-ssrs/
- U.S. Department of Veteran Affairs. (2020, November 1). Suicide prevention program guide . Www.va.gov. https://www.mirecc.va.gov/suicideprevention/documents/suicidepreventionprogramguide_06222022.pdf
- U.S. Department of Veterans Affairs. (2022). National veteran suicide prevention annual report. https://www.mentalhealth.va.gov/docs/data-sheets/2022/2022-National-Veteran-Suicide-Prevention-Annual-Report-FINAL-508.pdf
- University of Washington. (2021, February 8). How to ask about substance use. Https://Psychiatry.uw.edu/; Department of Psychiatry and Behavioral Sciences. https://pcl.psychiatry.uw.edu/how-to-ask-about-substance-use/
- Washington State Legislature. (n.d.). WAC 246-337-110: Use of restraint and seclusion. Apps.leg.wa.gov. Retrieved November 12, 2023, from https://apps.leg.wa.gov/WAC/default.aspx?cite=246-337-110
- Washington State Legislature. (2015). Chapter 71.05 RCW: Behavioral health disorders. Wa.gov. https://app.leg.wa.gov/RCW/default.aspx?cite=71.05
- World Health Organization. (2021). Suicide worldwide in 2019. World Health Organization. https://iris.who.int/bitstream/handle/10665/341728/9789240026643-eng.pdf?sequence=1
- Yu H, Flores DD, Bonett S, Bauermeister, JA. LGBTQ+ cultural competency training for health professionals: a systematic review. BMC Medical Education. 2023;23:558:1-83.
- Morris, M., Cooper, R.L., Ramesh, A. et al. Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC Med Educ 19, 325 (2019). https://doi.org/10.1186/s12909-019-1727-3
- Waisel DB. Vulnerable populations in healthcare. Curr Opin Anesthesiol. 2013;26(2):186–92.
- Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: Trends over the past 10 years. NCHS Data Brief. 2012;2012(100):1–8.
- Institute of Medicine. Collecting sexual orientation and gender identity data in electronic health records: workshop summary. Washington DC: National Academy of Sciences; 2013.
- Quinn GP, Sanchez JA, Sutton SK, Vadaparampil ST, Nguyen GT, Green BL, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA-Cancer J Clin. 2015;65(5):384–400
- Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–60.
- Dilley JA, Simmons KW, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific northwest. Am J Public Health. 2010;100(3):460–7.
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health. 2013;103(10):1802–9.
- Bauermeister J, Eaton L, Stephenson R. A multilevel analysis of neighborhood socioeconomic disadvantage and transactional sex with casual partners among Young men who have sex with men living in metro Detroit. Behav Med. 2016;42(3):197–204.
- Smalley KB, Warren JC, Barefoot KN. Differences in health risk behaviors across understudied LGBT subgroups. Health Psychol. 2016;35(2):103–14.
- Staats C, Capatosto K, Wright RA, Jackson VW. State of the science: Implicit bias review 2016. Columbus: Kirwan Institute.
- Cochran SD, Bandiera FC, Mays VM. Sexual orientation-related differences in tobacco use and secondhand smoke exposure among US adults aged 20 to 59 years: 2003-2010 National Health and nutrition examination surveys. Am J Public Health. 2013;103(10):1837–44.
- Ramchand, R., Schuler, M. S., Schoenbaum, M., Colpe, L., & Ayer, L. (2021). Suicidality among sexual minority adults: Gender, age, and race/ethnicity differences. American Journal of Preventive Medicine. https://doi.org/10.1016/j.amepre.2021.07.012
- Charlton BM, Corliss HL, Missmer SA, Frazier AL, Rosario M, Kahn JA, et al. Reproductive health screening disparities and sexual orientation in a cohort study of U.S. adolescent and Young adult females. J Adolesc Health. 2011;49(5):505–10.
- Agénor M, Krieger N, Austin SB, et al. Sexual Orientation Disparities in Papanicolaou Test Use Among US Women: The Role of Sexual and Reproductive Health Services. Am J Public Health. 2014;104(2):e68-72
- Tracy JK, Lydecker AD, Ireland L. Barriers to cervical Cancer screening among lesbians. J Women’s Health. 2010;19(2):229–37.
- Safer JD, Coleman E, Feldman J, Garofalo R, Hembree W, Radix A, Sevelius J. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016 Apr;23(2):168-71. doi: 10.1097/MED.0000000000000227. PMID: 26910276; PMCID: PMC4802845.
- Heck JE, Sell RL, Gorin SS. Health care access among individuals involved in same-sex relationships. Am J Public Health. 2006;96(6):1111–8.
- Kamen C, Palesh O, Gerry AA, Andrykowski MA, Heckler C, Mohile S, et al. Disparities in health risk behavior and psychological distress among gay versus heterosexual male Cancer survivors. LGBT Health. 2014;1(2):86–U103.
- Legal L. When health care Isn’t caring: lambda Legal’s survey of discrimination against LGBT people and people with HIV. New York: Lamba Legal; 2010.
- Grant JM, Mottet LA, Tanis J. National Transgender Discrimination Survey Report on health and health care. Washington DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2010.
- Shires DA, Jaffee K. Factors associated with health care discrimination experiences among a National Sample of female-to-male transgender individuals. Health Soc Work. 2015;40(2):134–41.
- Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians’ experiences in the workplace. J Homosex. 2011;58(10):1355–71.
- Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54.
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
- Mereish EH, Bradford JB. Intersecting identities and substance use problems: sexual orientation, gender, race, and lifetime substance use problems. J Stud Alcohol Drugs. 2014;75(1):179–88.
- Torres CG, Renfrew M, Kenst K, Tan-McGrory A, Betancourt JR, Lopez L. Improving transgender health by building safe clinical environments that promote existing resilience: results from a qualitative analysis of providers. BMC Pediatr. 2015;15:187.
- Burke SE, Dovidio JF, Przedworski JM, Hardeman RR, Perry SP, Phelan SM, et al. Do contact and empathy mitigate Bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. 2015;90(5):645–51.
- Sabin JA, Riskind RG, Nosek BA. Health care Providers’ implicit and explicit attitudes toward lesbian women and gay men. Am J Public Health. 2015;105(9):1831–41.
- Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–7.
- Wilson TD, Brekke N. Mental contamination and mental correction: unwanted influences on judgments and evaluation. Psychol Bull. 1994;116(1):117–42.
- Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit Bias in health care: a narrative review. Group Proccess Interg. 2016;19(4):528–42.
- Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102(1):4–27.
- Van Ryn M, Saha S. Exploring unconscious bias in disparities research and medical education. JAMA. 2011;306(9):995–6.
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41.
- Nosek BA, Riskind RG. Policy implications of implicit social cognition. Soc Issue Policy Rev. 2012;6(1):113–47.
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
- Shavers VL, Fagan P, Jones D, Klein WMP, Boyington J, Moten C, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953–66.
- Chapman EN, Kaatz A, Carnes M. Physicians and implicit Bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–10.
- Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: Confronting racial and ethnic disparities in health care. Brian D. Smedley, Adrienne Y. Stith, and Alan R. Nelson, Editors; Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Board on Health Sciences Policy; Institute of Medicine. Washington, DC; 2003.
- Greenwald AG, Banaji MR, Nosek BA. Statistically small effects of the implicit association test can have societally large effects. J Pers Soc Psychol. 2015;108(4):553–61.
- Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P. (2019). Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC medical education, 19(1), 325. https://doi.org/10.1186/s12909-019-1727-3
- Human rights campaigns. Glossary of terms. Retrieved from https://www.hrc.org/resources/glossary-of-terms
- Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community, a field guide. Joint Commission. Retrieved from https://www.jointcommission.org/ /media/enterprise/tjc/imported-resource assets/documents/lgbtfieldguide_web_linked_verpdf.pdf?db=web hash=1EC363A65C710BCD1D4E14ED120CB2
- Delivering culturally sensitive care to LGBTQI Patients. The Journal for nurse practitioners. Volume 13, issue 5 p342-347.
- (2023, July 25). Telehealth. Www.Telehealth.HHS.gov. Retrieved July 26, 2023, from https://en.m.wikipedia.org/wiki/Telehealth
- Skill Creations, Inc. (2022). Skill Creations Intranet. Retrieved July 24, 2023, from www.skillcreations.com.
- (2008, June 24). H.R. 6353 – Ryan Haight Online Pharmacy Consumer Protection Act of 2008. Www.Congress.gov. Retrieved July 24, 2023, from https://www.congress.gov/bill/110th-congress/house-bill/6353#:~:text=The%20summary%20of%20that%20version,Internet%20without%20a%20valid%20prescription
- (2019, March 1). North Carolina Medical Board – www.Ncmedboard.org. Retrieved July 25, 2023, from https://www.ncmedboard.org/resources-information/professional-resources/laws-rules-position-statements/position-statements/telemedicine
- (2022, June 29). Obtaining Informed Consent – www.Telehealth.HHS.gov. Retrieved July 26, 2023, from https://telehealth.hhs.gov/providers/preparing-patients-for-telehealth/obtaining-informed-consent
- (2022, January 12). Telehealth Documentation Requirements – www.Securityhealth.org. Retrieved July 29, 2023, from securityhealth.org/providers/provider-manual/shared-content/documentation-requirements/telehealth-documentation-requirements?documentation-requirements-group–direct-pay
- World Health Organization: WHO. (2019, May 13). Diabetes. https://www.who.int/health-topics/diabetes#tab=tab_
- Lizzo, J. M., Goyal, A., & Gupta, V. (2023, July 10). Adult diabetic ketoacidosis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560723/
- Diabetic ketoacidosis: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/000320.htm
- UpToDate. (n.d.). UpToDate. https://www.uptodate.com/contents/diabetic-ketoacidosis-in-children-clinical-features-and-diagnosis/print
- Virdi, N., Poon, Y., Abaniel, R., & Bergenstal, R. M. (2023). Prevalence, cost, and burden of diabetic ketoacidosis. Diabetes Technology & Therapeutics, 25(S3), S-84. https://doi.org/10.1089/dia.2023.0149
- Matthews, S., Coates, M. M., Bukhman, A., & Trujillo, C. (2023). Health system capacity to manage diabetic ketoacidosis in nine low-income and lower-middle income countries: a cross-sectional analysis of nationally representative survey data. eClinical Medicine, 55(101759). https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(22)00488-6/fulltext#%20
- Virdi, N., Poon, Y., Abaniel, R., & Bergenstal, R. M. (2023b). Prevalence, cost, and burden of diabetic ketoacidosis. Diabetes Technology & Therapeutics, 25(S3), S-84. https://doi.org/10.1089/dia.2023.0149
- Lizzo, J. M., Goyal, A., & Gupta, V. (2023b, July 10). Adult diabetic ketoacidosis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560723/
- Ghimire, P., & Dhamoon, A. S. (2023, August 8). Ketoacidosis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK534848/#:~:text=Introduction-,Ketoacidosis%20is%20a%20metabolic%20state%20associated%20with%20pathologically%20high%20serum,individual%20cells%20in%20the%20body
- Hamdy, O., MD PhD. (n.d.). Diabetic Ketoacidosis (DKA): practice essentials, background, pathophysiology. https://emedicine.medscape.com/article/118361-overview?form=fpf
- JDRF. (2023, February 24). Signs and symptoms of Type 1 diabetes in Children – JDRF. https://www.jdrf.org/t1d-resources/about/symptoms/children/
- Diabetic ketoacidosis: MedlinePlus Medical Encyclopedia. (n.d.-b). https://medlineplus.gov/ency/article/000320.htm#:~:text=People%20with%20type%202%20diabetes,a%20severe%20illness%20or%20infection.
- Diabetic ketoacidosis – Symptoms & causes – Mayo Clinic. (2022, October 6). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/diabetic-ketoacidosis/symptoms-causes/syc-20371551
- Chukwuka, E., Johnson, D., Udoyen, A.-O., Egbunu, E. O., & Ogbuiyi-Chima, I. C. (2023). Comprehensive Review of Diabetic Ketoacidosis: An update. PMC PubMed Central, 85(6), 2802–2807. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10289692/
- Cavataio, M. M., & Packer, C. D. (2022). Steroid-Induced Diabetic Ketoacidosis: A case Report and Review of the literature. Cureus, 14(4), e24372. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9124452/#:~:text=Mechanisms%20for%20steroid%2Dinduced%20diabetes,translocation%20%5B9%2D10%5D.
- Mfa, J. H. M. M. (2021, August 18). What to know about Steroid-Induced Diabetes. Healthline. https://www.healthline.com/health/diabetes/steroid-induced-diabetes
- Professional, C. C. M. (n.d.). Hyperosmolar hyperglycemic state (HHS). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21147-hyperosmolar-hyperglycemic-state
- Ghimire, P., Dhamoon, A. S., & Doerr, C. (2023, August 8). Ketoacidosis (Nursing). StatPearls – NCBI Bookshelf. Retrieved March 22, 2024, from https://www.ncbi.nlm.nih.gov/books/NBK568717/
- Anion gap blood test. (n.d.). https://medlineplus.gov/lab-tests/anion-gap-blood-test/#:~:text=A%20high%20anion%20gap%20test,Dehydration
- Ghimire, P., Dhamoon, A. S., & Doerr, C. (2023b, August 8). Ketoacidosis (Nursing). StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK568717/
- Besen, B. a. M. P., Boer, W., & Honoré, P. M. (2021). Fluid management in diabetic ketoacidosis: new tricks for old dogs? Intensive Care Medicine, 47(11), 1312–1314. https://doi.org/10.1007/s00134-021-06527-7
- Jayashree, M., Williams, V., & Iyer, R. (2019). Fluid therapy for pediatric patients with diabetic ketoacidosis: current perspectives. PMC PubMed Central, 12, 2355–2361. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6858801/
- Lizzo, J. M., Goyal, A., & Gupta, V. (2023c, July 10). Adult diabetic ketoacidosis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560723/
- Professional, C. C. M. (n.d.-a). Cerebral edema (Brain swelling). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/cerebral-edema-brain-swelling
- Hamdy, O., MD PhD. (n.d.-b). Diabetic Ketoacidosis (DKA) treatment & management: approach considerations, correction of fluid loss, insulin therapy. https://emedicine.medscape.com/article/118361-treatment#d13
- Intracranial pressure monitoring. (2024, January 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/31194438/#:~:text=Excerpt,20%20to%2025%20mm%20Hg
- Ahmad, F., & Joshi, S. H. (2023). Self-Care practices and their Role in the control of Diabetes: A Narrative review. PubMed Central Cureus, 15 (7), e41409. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10402910/#:~:text=To%20reduce%20the%20burden%20of,glucose%20levels%20in%20the%20patients.
- Diabetes self-management training. (n.d.). Medicare. https://www.medicare.gov/coverage/diabetes-self-management-training
- Diabetic ketoacidosis. (2021, March 25). Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/basics/diabetic-ketoacidosis.html
- Managing sick days | Diabetes | CDC. (n.d.). https://www.cdc.gov/diabetes/managing/flu-sick-days.html
- Mental Health and Diabetes | ADA. (n.d.). https://diabetes.org/health-wellness/mental-health
- Diabetes Distress Assessment & Resource Center. (n.d.). https://diabetesdistress.org/learn-about-dd/
- Dealing with diabetes burnout. (2022, June 20). Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/spotlights/diabetes-burnout.html
- Professional, C. C. M. (n.d.-b). Diabulimia. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22658-diabulimia
- Bulimia nervosa – Symptoms and causes – Mayo Clinic. (2024, February 29). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/bulimia/symptoms-causes/syc-20353615
- Anniversary of the Inflation Reduction Act: Update on CMS Implementation | CMS. (2023, August 16). https://www.cms.gov/newsroom/fact-sheets/anniversary-inflation-reduction-act-update-cms-implementation#:~:text=Specifically%2C%20the%20Inflation%20Reduction%20Act,Traditional%20Medicare%2C%20or%20Medicare%20Advantage.
- International Diabetes Federation. (2024, February 7). Diabetes Facets and Figures | International Diabetes Federation. https://idf.org/about-diabetes/diabetes-facts-figures/
- Brown, A. (2021, August 14). Diabetes distress: why it’s common and what we can do about it! diaTribe. https://diatribe.org/diabetes-distress-why-it%E2%80%99s-common-and-what-we-can-do-about-it
- Diab, A., Dastmalchi, L. N., Gulati, M., & Michos, E. D. (2023). A Heart-Healthy Diet for cardiovascular Disease Prevention: Where are we now? Vascular Health and Risk Management, Volume 19, 237–253. https://doi.org/10.2147/vhrm.s379874
- Cena, H., & Calder, P. C. (2020). Defining a Healthy Diet: Evidence for the role of contemporary dietary patterns in Health and disease. Nutrients, 12(2), 334. https://doi.org/10.3390/nu12020334
- Diab, A., Dastmalchi, L. N., Gulati, M., & Michos, E. D. (2023). A Heart-Healthy Diet for cardiovascular Disease Prevention: Where are we now? Vascular Health and Risk Management, Volume 19, 237–253. https://doi.org/10.2147/vhrm.s379874
- World Health Organization: WHO. (2019, June 11). Cardiovascular diseases. https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1
- Yusuf S., Hawken S., Ounpuu S., Dans T., Avezum A., Lanas F., McQueen M., Budaj A., Pais P., Varigos J., et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004; 364:937–952. doi: 10.1016/S0140-6736(04)17018-9.
- Akesson A., Weismayer C., Newby P.K., Wolk A. Combined effect of low-risk dietary and lifestyle behaviors in primary prevention of myocardial infarction in women. Arch. Intern. Med. 2007; 167:2122–2127. doi: 10.1001/archinte.167.19.2122
- Ford E.S., Bergmann M.M., Kröger J., Schienkiewitz A., Weikert C., Boeing H. Healthy living is the best revenge: Findings from the European Perspective Investigation into Cancer and Nutrition-Potsdam study. Arch. Intern. Med. 2009; 169:1355–1362. doi: 10.1001/archinternmed.2009.237.
- Chiuve S.E., McCullough M.L., Sacks F.M., Rimm E.B. Healthy lifestyle factors in the primary prevention of coronary heart disease among men: Benefits among users and nonusers of lipid-lowering and antihypertensive medications. Circulation. 2006; 114:160–167. doi: 10.1161/CIRCULATIONAHA.106.621417
- National Library of Medicine. (2022). Heart diseases. https://medlineplus.gov/heartdiseases.html
- Sharifi‐Rad, J., Rodrigues, C. F., Sharopov, F., Docea, A. O., Karaça, A. C., Sharifi‐Rad, M., Karıncaoglu, D. K., Gülseren, G., Şenol, E., Demircan, E., Taheri, Y., Suleria, H. a. R., Özçelik, B., Kasapoğlu, K. N., Gültekin-Özgüven, M., Daşkaya-Dikmen, C., Cho, W. C., Martins, N., & Calina, D. (2020). Diet, Lifestyle and Cardiovascular Diseases: Linking pathophysiology to cardioprotective effects of natural bioactive compounds. International Journal of Environmental Research and Public Health, 17(7), 2326. https://doi.org/10.3390/ijerph17072326
- Chacko, M., Sarma, P. S., Harikrishnan, S., Zachariah, G., & Jeemon, P. (2020). Family history of cardiovascular disease and risk of premature coronary heart disease: A matched case-control study. Welcome Open Research, 5, 70. https://doi.org/10.12688/wellcomeopenres.15829.2
- Holvoet P. Stress in obesity and associated metabolic and cardiovascular disorders. Scientifica. 2012; 2012:205027. doi: 10.6064/2012/205027
- Casas, R., Castro‐Barquero, S., Estruch, R., & Sacanella, E. (2018). Nutrition and cardiovascular health. International Journal of Molecular Sciences, 19(12), 3988. https://doi.org/10.3390/ijms19123988
- Coronary artery disease – Symptoms and causes – Mayo Clinic. (2022, May 25). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/symptoms-causes/syc-20350613
- NHS inform. (2023, November 9). Cardiovascular disease – Illnesses & conditions | NHS inform. NHS Inform. https://www.nhsinform.scot/illnesses-and-conditions/heart-and-blood-vessels/conditions/cardiovascular-disease/
- Data and Statistics on Congenital Heart Defects | CDC. (2023, September 19). Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/heartdefects/data.html
- Valvular heart Disease | Cdc.gov. (2019, December 9). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/valvular_disease.htm
- What is heart failure? | NHLBI, NIH. (2022, March 24). NHLBI, NIH. https://www.nhlbi.nih.gov/health/heart-failure
- Heart failure signs and symptoms. (2023, October 18). www.heart.org. https://www.heart.org/en/health-topics/heart-failure/warning-signs-of-heart-failure
- What is cardiomyopathy? | NHLBI, NIH. (2022, April 19). NHLBI, NIH. https://www.nhlbi.nih.gov/health/cardiomyopathy
- Cardiomyopathy | cdc.gov. (2023, February 21). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/cardiomyopathy.htm
- Khandaker, M. H., Espinosa, R. E., Nishimura, R. A., Sinak, L. J., Hayes, S. N., Melduni, R. M., & Oh, J. K. (2010). Pericardial Disease: Diagnosis and management. Mayo Clinic Proceedings, 85(6), 572–593. https://doi.org/10.4065/mcp.2010.0046
- What is an arrhythmia? | NHLBI, NIH. (2022, March 24). NHLBI, NIH. https://www.nhlbi.nih.gov/health/arrhythmias
- Atrial fibrillation | Cdc.gov. (2022, October 14). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
- Harris, C., Croce, B., & Cao, C. (2016). ACS Patient Page Type A aortic dissection. Annals of Cardiothoracic Surgery, 5(4), 256. https://doi.org/10.21037/acs.2016.05.04
- Milner, R., MD. (2022, January 25). What is aortic dissection: What you need to know about the causes, types and more. UChicago Medicine. https://www.uchicagomedicine.org/forefront/heart-and-vascular-articles/silent-killer-everything-you-need-to-know-about-aortic-dissection
- Yu, E., Rimm, E. B., Qi, L., Rexrode, K. M., Chen, A., Sun, Q., Willett, W. C., Hu, F. B., & Manson, J. E. (2016). Diet, lifestyle, biomarkers, genetic factors, and risk of cardiovascular disease in the nurses’ health studies. American Journal of Public Health, 106(9), 1616–1623. https://doi.org/10.2105/ajph.2016.303316
- Lichtenstein, A. H., Appel, L. J., Vadiveloo, M., Hu, F. B., Kris‐Etherton, P. M., Rebholz, C. M., Sacks, F. M., Thorndike, A. N., Van Horn, L., Wylie‐Rosett, J., & Biology, V. (2021). 2021 Dietary Guidance to Improve Cardiovascular Health: A scientific statement from the American Heart Association. Circulation, 144(23). https://doi.org/10.1161/cir.0000000000001031
- Schwingshackl L, Schwedhelm C, Hoffmann G, Boeing H. Potatoes, and risk of chronic disease: a systematic review and dose-response meta-analysis. Eur J Nutr. 2019; 58:2243–2251. doi: 10.1007/s00394-018-1774-2
- Preventing heart disease. (2023, February 2). The Nutrition Source. https://www.hsph.harvard.edu/nutritionsource/disease-prevention/cardiovascular-disease/preventing-cvd/
- Tosh SM, Bordenave N. Emerging science on benefits of whole grain oat and barley and their soluble dietary fibers for heart health, glycemic response, and gut microbiota. Nutr Rev. 2020; 78(suppl 1):13–20. doi: 10.1093/nutrit/nuz085
- Voskoboinik A, Kalman JM, De Silva A, Nicholls T, Costello B, Nanayakkara S, Prabhu S, Stub D, Azzopardi S, Vizi D, et al. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med. 2020; 382:20–28. doi: 10.1056/NEJMoa1817591
- Hardy DS, Garvin JT, Xu H. Carbohydrate quality, glycemic index, glycemic load and cardiometabolic risks in the US, Europe, and Asia: a dose-response meta-analysis. Nutr Metab Cardiovasc Dis. 2020; 30:853–871. doi: 10.1016/j.numecd.2019.12.050
- Sacks FM, Lichtenstein AH, Wu JHY, Appel LJ, Creager MA, Kris-Etherton PM, Miller M, Rimm EB, Rudel LL, Robinson JG, et al; American Heart Association. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. 2017; 136: e1–e23. doi: 10.1161/CIR.0000000000000510
- Chiavaroli, L., Viguiliouk, E., Nishi, S. K., Mejía, S. B., Rahelić, D., Kahleová, H., Salas‐Salvadó, J., Kendall, C. W., & Sievenpiper, J. L. (2019). DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients, 11(2), 338. https://doi.org/10.3390/nu11020338
- Satija, A., & Hu, F. B. (2018). Plant-based diets and cardiovascular health. Trends in Cardiovascular Medicine, 28(7), 437–441. https://doi.org/10.1016/j.tcm.2018.02.004
- Wang DD, Hu FB. Dietary fat and risk of cardiovascular disease: recent controversies and advances. Annu Rev Nutr. 2017; 37:423–446. doi: 10.1146/annurev-nutr-071816-064614
- Eckel RH, Borra S, Lichtenstein AH, Yin-Piazza SY; Trans Fat Conference Planning Group. Understanding the complexity of trans fatty acid reduction in the American diet: American Heart Association Trans Fat Conference 2006: report of the Trans Fat Conference Planning Group. Circulation. 2007; 115:2231–2246. doi: 10.1161/CIRCULATIONAHA.106.181947
- Heart-healthy diet: 8 steps to prevent heart disease. (2022, April 28). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/heart-disease/in-depth/heart-healthy-diet/art-20047702
- Bhattad, P. B., & Pacifico, L. (2022). Empowering patients: Promoting patient education and health literacy. Cureus. https://doi.org/10.7759/cureus.27336
- Pem, D. (2015, October 1). Fruit and Vegetable Intake: Benefits and Progress of Nutrition Education Interventions- Narrative Review article. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4644575/
- Marcus, C. (2014). Strategies for improving the quality of verbal patient and family education: a review of the literature and creation of the EDUCATE model. Health Psychology and Behavioral Medicine, 2(1), 482–495. https://doi.org/10.1080/21642850.2014.900450
- Woodgate, R. L., & Sigurdson, C. (2015). Building school-based cardiovascular health promotion capacity in youth: a mixed methods study. BMC Public Health, 15(1). https://doi.org/10.1186/s12889-015-1759-5
- Trichopoulou, A., Martínez‐González, M. A., Tong, T. Y., Forouhi, N. G., Khandelwal, S., Prabhakaran, D., Mozaffarian, D., & De Lorgeril, M. (2014). Definitions and potential health benefits of the Mediterranean diet: views from experts around the world. BMC Medicine, 12(1). https://doi.org/10.1186/1741-7015-12-112
- Challa, H. J. (2023, January 23). DASH Diet to Stop Hypertension. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482514/
- Childs, C. E., Calder, P. C., & Miles, E. A. (2019). Diet and immune function. Nutrients, 11(8), 1933. https://doi.org/10.3390/nu11081933
- Centers for Disease Control and Prevention (CDC) (2023). Fast Facts: Preventing Adverse Childhood Experiences. https://www.cdc.gov/violenceprevention/aces/fastfact.html
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. https://doi.org/10.1016/S0749-3797(98)00017-8.
- Starecheski, L. (2015). Take the ACE quiz—And learn what it does and doesn’t mean. NPR. https://www.npr.org/sections/health-shots/2015/03/02/387007941/take-the-ace-quiz-and-learn-what-it-does-and-doesnt-mean
- Center on the Developing Child at Harvard University (n.d.). What are ACEs? And how do they relate to toxic stress? https://developingchild.harvard.edu/resources/aces-and-toxic-stress-frequently-asked-questions/
- CDC, (2022). About the CDC-Kaiser ACE study. https://www.cdc.gov/violenceprevention/aces/about.html
- CDC. (2021). Preventing adverse childhood experiences. https://www.cdc.gov/vitalsigns/aces/index.html
- CDC (2023). Risk and protective factors. https://www.cdc.gov/violenceprevention/aces/riskprotectivefactors.html
- Cleveland Clinic (2023). Adverse childhood experiences (ACEs) & childhood trauma. (2023). https://my.clevelandclinic.org/health/symptoms/24875-adverse-childhood-experiences-ace
- Merrick, M. T. (2019). Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention — 25 States, 2015–2017. Morbidity and Mortality Weekly Report, 68. https://doi.org/10.15585/mmwr.mm6844e1
- Child Trends. (2018). American Indians and Alaska Natives must be included in research on adverse childhood experiences. https://www.childtrends.org/blog/american-indians-alaska-natives-adverse-childhood-experiences
- Hughes, K., Bellis, M.A., Hardcastle, K.A., Sethi, D., Butchart, A., Mikton, C., Jones, L., Dunne, M.P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health; 2(8): e356-e366. doi: 10.1016/S2468-2667(17)30118-4.
- CDC (2023). Leading causes of death. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
- Merrick, M. T., Ports, K. A., Ford, D. C., Afifi, T. O., Gershoff, E. T., & Grogan-Kaylor, A. (2017). Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse & Neglect, 69, 10–19. https://doi.org/10.1016/j.chiabu.2017.03.016
- Center on the Developing Child at Harvard University (n.d.). Take the ACE quiz – And learn what it does and doesn’t mean. https://developingchild.harvard.edu/media-coverage/take-the-ace-quiz-and-learn-what-it-does-and-doesnt-mean/
- National Conference of State Legislatures (2022). Adverse Childhood Experiences. https://www.ncsl.org/health/adverse-childhood-experience
- National Center for Missing & Exploited Children (2023). CyberTipline http://www.missingkids.org/content/ncmec/en/gethelpnow/cybertipline.html
- American Society of Health-System Pharmacists. (2022, January 1). Fluvoxamine: Medlineplus drug information. MedlinePlus. https://medlineplus.gov/druginfo/meds/a695004.html#:~:text=Fluvoxamine%20is%20used%20to%20treat,that%20interferes%20with%20normal%20life).
- Chu, A. (2023, May 1). Selective serotonin reuptake inhibitors. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK554406/
- Cleveland Clinic. (2024). Vilazodone (Viibryd®): Uses & Side effects. https://my.clevelandclinic.org/health/drugs/20831-vilazodone-tablets
- DrugBank. (2024, March 6). Fluvoxamine. Uses, Interactions, Mechanism of Action | DrugBank Online. https://go.drugbank.com/drugs/DB00176
- Fornaro, M., Anastasia, A., Valchera, A., Carano, A., Orsolini, L., Vellante, F., Rapini, G., Olivieri, L., Di Natale, S., Perna, G., Martinotti, G., Di Giannantonio, M., & De Berardis, D. (2019). The FDA “black box” warning on antidepressant suicide risk in young adults: More harm than benefits? Frontiers in Psychiatry, 10. https://doi.org/10.3389/fpsyt.2019.00294
- Gasanli, E. (2023, December 12). Luvox (fluvoxamine): Uses, side effects, dosage, & more. Choosing Therapy. https://www.choosingtherapy.com/luvox-fluvoxamine/
- Huddart, R., Hicks, J. K., Ramsey, L. B., Strawn, J. R., Smith, D. M., Bobonis Babilonia, M., Altman, R. B., & Klein, T. E. (2020, February). PharmGKB summary: Sertraline pathway, pharmacokinetics. Pharmacogenetics and genomics. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7008964/
- Landy, K. (2023, November 10). Escitalopram. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK557734/#article-60.s5
- Mauney, M. (2023, September 5). Paxil: Uses, black box warning, Recall & Alternatives. Drugwatch.com. https://www.drugwatch.com/ssri/paxil/#:~:text=The%20FDA%20issued%20a%20black,risks%20with%20the%20clinical%20need
- Mayo Clinic. (2024a, February 1). Fluoxetine (oral route) description and brand names. https://www.mayoclinic.org/drugs-supplements/fluoxetine-oral-route/description/drg-20063952
- Mayo Clinic. (2024b, February 1). Citalopram (oral route) description and brand names. https://www.mayoclinic.org/drugs-supplements/citalopram-oral-route/description/drg-20062980
- Mayo Clinic. (2024c, March 1). Paroxetine (oral route) description and brand names. https://www.mayoclinic.org/drugs-supplements/paroxetine-oral-route/description/drg-20067632
- Mayo Clinic. (2024d, March 1). Sertraline (oral route) precautions. https://www.mayoclinic.org/drugs-supplements/sertraline-oral-route/precautions/drg-20065940?p=1
- Mayo Clinic. (2024e, March 1). Escitalopram (oral route) description and brand names. https://www.mayoclinic.org/drugs-supplements/escitalopram-oral-route/description/drg-20063707
- Mayo Clinic. (2024f, March 1). Fluvoxamine (oral route) precautions. https://www.mayoclinic.org/drugs-supplements/fluvoxamine-oral-route/precautions/drg-20066874?p=1
- National Institutes of Health. (2023, December 20). Fluvoxamine. National Institutes of Health. https://www.covid19treatmentguidelines.nih.gov/therapies/miscellaneous-drugs/fluvoxamine/#:~:text=Fluvoxamine%20is%20a%20selective%20serotonin,for%20other%20conditions%2C%20including%20depression.
- Plenge, P., Yang, D., Salomon, K., Laursen, L., Kalenderoglou, I. E., Newman, A. H., Gouaux, E., Coleman, J. A., & Loland, C. J. (2021, August 20). The Antidepressant Drug Vilazodone is an allosteric inhibitor of the serotonin transporter. Nature News. https://www.nature.com/articles/s41467-021-25363-3
- Shoar, N. S. (2023, November 7). Citalopram. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482222/
- Shrestha, P. (2023, July 17). Paroxetine. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK526022/
- Singh, H. K. (2023, February 13). Sertraline. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK547689/
- Sohel, A. J. (2022, July 4). Fluoxetine. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459223/
- Ulrich, A. (2022, December 13). 7 fluoxetine (Prozac) interactions to watch out for. GoodRx. https://www.goodrx.com/fluoxetine/interactions
- UpToDate. (2024). Vilazodone: Drug information. Vilazodone: Drug Information. https://medilib.ir/uptodate/show/16102
- Agrawal, A., Kerndt, C.C., & Manna, B. (Updated 2023, April 19). Apixaban. In Stat Pearls. Stat Pearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507910/
- American Heart Association. (2023, November 12). New Anti-clotting Medication Reduces Bleeding Among People with Atrial Fibrillation. Retrieved from https://newsroom.heart.org/news/new-anti-clotting-medication-reduces-bleeding-among-people-with-atrial-fibrillation
- Bentounes, N. K., Melicine, S., Martin, A. C., Smadja, D. M., & Gendron, N. (2023). Development of new anticoagulant in 2023: Prime time for anti-factor XI and XIa inhibitors. Journal de medecine vasculaire, 48(2), 69–80. https://doi.org/10.1016/j.jdmv.2023.04.002
- Centers for Disease Control and Prevention. (2023, June 28). Data and Statistics on Venous Thromboembolism. Retrieved from https://www.cdc.gov/ncbddd/dvt/data.html
- Centers for Disease Control and Prevention. (2023, June 28). Diagnosis and Treatment of Venous Thromboembolism. Retrieved from https://www.cdc.gov/ncbddd/diagnosis-treatment.html
- Chen, A., Stecker, E., & A Warden, B. (2020). Direct Oral Anticoagulant Use: A Practical Guide to Common Clinical Challenges. Journal of the American Heart Association, 9(13), e017559. https://doi.org/10.1161/JAHA.120.017559
- Hull, R.D., Garcia, D.A., Vazquez, S.R. (Updated 2023, January 24). Biology of Warfarin and Modulators of INR Control. UpToDate. Retrieved from https://www.uptodate.com/contents/biology-of-warfarin-and-modulators-of-inr-control
- Iqbal, A.M., Lopez, R.A., & Hai, O. (Updated 2022, November 7). Antiplatelet Medications. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK537062/
- Leung, L.LK. (Updated 2023, July 27). Direct oral anticoagulants (DOACs) and parenteral direct-acting anticoagulants: Dosing and adverse effects. UpToDate. Retrieved from https://www.uptodate.com/contents/direct-oral-anticoagulants-doacs-and-parenteral-direct-acting-anticoagulants-dosing-and-adverse-effects/print
- Mahat, K.C., Sedhair, Y.R., Krishnan, P. (Updated 2023, August 4). Argatroban. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK555971/
- Patel, S., Singh, R., Preuss, C.V., and Patel, N. (Updated 2023, March 24). Warfarin. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470313/
- Singh, R., & Emmady, P.D. (Updated 2023, April 17). Rivaroxaban. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557502/
- Solari, F., & Varacallo, M. (Updated 2023, August 4). Low-Molecular-Weight Heparin (LMWH). In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK525957/
- Umerah, C.O., & Momodu, I.I. (Updated 2023, July 17). Anticoagulation. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560651/
- Warnock, L.B., & Huang, D. (Updated 2023, July 10). Heparin. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538247/
- Weitz, J.I. (Updated 2023, August 17). Investigational Anticoagulants. UpToDate. Retrieved from https://www.uptodate.com/contents/investigational-anticoagulants
- Bamalan, O.A., Moore, M.J., Al Khalili Y. (2024). Physiology, serotonin. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK545168/
- Dhaliwal JS, Spurling BC, Molla M. (2023). Duloxetine. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK549806/
- Fanelli, D., Weller, G., & Liu, H. (2021). New Serotonin-Norepinephrine Reuptake Inhibitors and Their Anesthetic and Analgesic Considerations. Neurology international, 13(4), 497–509. https://doi.org/10.3390/neurolint13040049
- Hussain LS, Reddy V, Maani CV. (2023) Physiology, Noradrenergic Synapse. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK540977/
- Li, J., Lu, C., Gao, Z, Feng, Y., Luo, H., Lu, T., Sun, X., Hu, J., & Luo, Y. (2020). SNRIs achieve faster antidepressant effects than SSRIs by elevating the concentrations of dopamine in the forebrain. Neuropharmacology, 177, 108237, ISSN 0028-3908. https://doi.org/10.1016/j.neuropharm.2020.108237.
- Naseeruddin, R., Rosani, A., & Marwaha, R. (2023). Desvenlafaxine. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534829/
- National Institute of Mental Health (NIH). (2022). Depression. Retrieved from https://www.nimh.nih.gov/health/publications/depression.
- Singh, D., & Saadabadi, A. (2022). Venlafaxine. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK535363/
- Vallerand, A. H., & Sanoski, C. A. (2023). Davis’s drug guide for nurses (Eighteenth edition.). Philadelphia, PA. F. A. Davis Company. ISBN-10: 1-7196-4640-6. eISBN-10: 1-7196-4811-5.
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Venlafaxine. Access Pharmacy. Retrieved from https://accesspharmacy.mhmedical.com/drugs.aspx?gbosID=426975.
- American Society of Health-System Pharmacists (ASHP). (2023). Dexamethasone (monograph). https://www.drugs.com/monograph/dexamethasone.html
- Dutt, M., Wehrle, C.J., & Jialal, I. (2024). Physiology, adrenal gland. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing https://www.ncbi.nlm.nih.gov/books/NBK537260/
- Chaudhuri, D., Nei, A. M., Rochwerg, B. et at. (2024). 2024 Focused update: Guidelines on use of corticosteroids in sepsis, acute respiratory distress syndrome, and community-acquired pneumonia. Critical Care Medicine ():10.1097/CCM.0000000000006172 https://journals.lww.com/ccmjournal/fulltext/9900/2024_focused_update__guidelines_on_use_of.275.aspx
- U.S. Food and Drug Administration. (2016). FDA drug safety communication: FDA requires label changes to warn of rare but serious neurologic problems after epidural corticosteroid injections for pain. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-requires-label-changes-warn-rare-serious-neurologic-problems-after
- Hannoodee, S., & Nasuruddin, D.N. (2024). Acute inflammatory response. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK556083/
- Merck Manual. (2024). Drug information. Elsevier. https://www.merckmanuals.com/professional/drug-names-generic-and-brand
- Merck Manual. (2024). Corticosteroids: Uses and side effects. Elsevier. https://www.merckmanuals.com/home/multimedia/table/corticosteroids-uses-and-side-effects
- National Institutes of Health, U.S. Department of Health and Human Services. (2020). Autoimmunity may be rising in the United States. https://www.nih.gov/news-events/news-releases/autoimmunity-may-be-rising-united-states
- National Institutes of Health, U.S. Department of Health and Human Services. (2023). Therapeutic management of hospitalized adults with COVID-19. https://www.covid19treatmentguidelines.nih.gov/management/clinical-management-of-adults/hospitalized-adults–therapeutic-management/
- National Institutes of Health, U.S. Department of Health and Human Services. (2023). Therapeutic management of nonhospitalized adults with COVID-19. https://www.covid19treatmentguidelines.nih.gov/management/clinical-management-of-adults/nonhospitalized-adults–therapeutic-management/
- Oronsky, B., Caroen, S., & Reid, T. (2022). What exactly is inflammation (and what is it not?). International Journal of Molecular Sciences, 23(23), 14905. https://doi.org/10.3390/ijms232314905
- Sen, S. K. (2024). Messenger RNA (MRNA). National Human Genome Research Institute. https://www.genome.gov/genetics-glossary/messenger-rna
- World Health Organization. (2020). Corticosteroids for COVID-19: Living guidance. https://iris.who.int/bitstream/handle/10665/334125/WHO-2019-nCoV-Corticosteroids-2020.1-eng.pdf?sequence=1%26isAllowed=y
- Desai, D. S. (2023, June 5). Arrhythmias. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK558923/
- Benjamin, E. J., Wolf, P. A., D’Agostino, R. B., Silbershatz, H., Kannel, W. B., & Levy, D. (1998). Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation, 98(10), 946-952.
- Atrial fibrillation | Cdc.gov. (2022, October 14). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
- King, G. S. (2023, February 19). Antiarrhythmic medications. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482322/
- Saljic, A., Heijman, J., & Dobrev, D. (2023). Recent Advances in Antiarrhythmic Drug Therapy. Drugs, 83(13), 1147–1160. https://doi.org/10.1007/s40265-023-01923-3
- Kowey, P. R., & Robinson, V. M. (2020). The relentless pursuit of new drugs to treat cardiac arrhythmias. Circulation, 141(19), 1507–1509. https://doi.org/10.1161/circulationaha.119.045149
- Wright, K. N. (2009). Antiarrhythmic agents. In Elsevier eBooks (pp. 807–810). https://doi.org/10.1016/b978-1-4160-2591-7.10190-0
- Geng, M., Lin, A., & Nguyen, T. P. (2020). Revisiting Antiarrhythmic Drug Therapy for Atrial Fibrillation: Reviewing Lessons Learned and Redefining Therapeutic Paradigms. Frontiers in pharmacology, 11, 581837. https://doi.org/10.3389/fphar.2020.581837
- Sharma, A.K., Singh, S., Bhat, M. et al. new drug discovery of cardiac anti-arrhythmic drugs: insights in animal models. Sci Rep 13, 16420 (2023). https://doi.org/10.1038/s41598-023-41942-4
- Heart arrhythmias. (2024). Physiopedia. https://www.physio-pedia.com/Heart_Arrhythmias
- Dan, G., Martínez‐Rubio, A., Agewall, S., Boriani, G., Borggrefe, M., Gaïta, F., Van Gelder, I. C., Görenek, B., Kaski, J. C., Kjeldsen, K., Lip, G. Y., Merkely, B., Okumura, K., Piccini, J. P., Potpara, T., Poulsen, B. K., Saba, M., Savelieva, I., Tamargo, J., & Wolpert, C. (2018). Antiarrhythmic drugs–clinical use and clinical decision making: a consensus document from the European Heart Rhythm Association (EHRA) and European Society of Cardiology (ESC) Working Group on Cardiovascular Pharmacology, endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS) and International Society of Cardiovascular Pharmacotherapy (ISCP). Europace, 20(5), 731–732an. https://doi.org/10.1093/europace/eux373
- Heart arrhythmia – Symptoms and causes – Mayo Clinic. (2023, October 13). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/heart-arrhythmia/symptoms-causes/syc-20350668
- Arrhythmias and congenital defects. (2023, June 15). www.heart.org. https://www.heart.org/en/health-topics/congenital-heart-defects/the-impact-of-congenital-heart-defects/arrhythmias-and-congenital-defects
- CV Pharmacology | Vaughan-Williams Classification of Antiarrhythmic Drugs. (2024). https://cvpharmacology.com/antiarrhy/vaughan-williams
- Lei, M., Wu, L., Terrar, D. A., & Huang, C. L. (2018). Modernized classification of cardiac antiarrhythmic drugs. Circulation, 138(17), 1879–1896. https://doi.org/10.1161/circulationaha.118.035455
- Custodis F, Schirmer SH, Baumhäkel M, et al. Vascular pathophysiology in response to increased heart rate. J Am Coll Cardiol 2010; 56:1973–83. 10.1016/j.jacc.2010.09.014
- Kaski, J. C., Gloekler, S., Ferrari, R., Fox, K., Lévy, B., Komajda, M., Vardas, P., & Camici, P. G. (2018). Role of ivabradine in management of stable angina in patients with different clinical profiles. Open Heart, 5(1), e000725. https://doi.org/10.1136/openhrt-2017-000725
- Salvage, S. C., Chandrasekharan, K. H., Jeevaratnam, K., Dulhunty, A. F., Thompson, A. J., Jackson, A. P., & Huang, C. L. (2018). Multiple targets for flecainide action: implications for cardiac arrhythmogenesis. British journal of pharmacology, 175(8), 1260–1278. https://doi.org/10.1111/bph.13807
- Bazoukis, G., Tse, G., Letsas, K. P., Thomopoulos, C., Naka, K. K., Korantzopoulos, P., Bazoukis, X., Michelongona, P., Papadatos, S. S., Vlachos, K., Liu, T., Efremidis, M., Baranchuk, A., Stavrakis, S., & Tsioufis, C. (2018). Impact of ranolazine on ventricular arrhythmias – A systematic review. Journal of arrhythmia, 34(2), 124–128. https://doi.org/10.1002/joa3.12031
- Rahman, M. F. F. (2023, July 24). Atrioventricular dissociation. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK563205/
- Perera, R. K., Fischer, T. H., Wagner, M., Dewenter, M., Vettel, C., Bork, N. I., Maier, L. S., Conti, M., Wess, J., El-Armouche, A., Hasenfuß, G., & Nikolaev, V. O. (2017). Atropine augments cardiac contractility by inhibiting cAMP-specific phosphodiesterase type 4. Scientific reports, 7(1), 15222. https://doi.org/10.1038/s41598-017-15632-x
- Singh, S. (2023, August 28). Adenosine. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK519049/
- Patti, L. (2023, August 7). Supraventricular tachycardia. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK441972/
- McIntyre, W. F., Healey, J. S., Bhatnagar, A. K., Wang, P., Gordon, J. A., Baranchuk, A., Deif, B., Whitlock, R. P., & Belley-Côté, É. P. (2019). Vernakalant for cardioversion of recent-onset atrial fibrillation: a systematic review and meta-analysis. Europace: European pacing, arrhythmias, and cardiac electrophysiology: journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology, 21(8), 1159–1166. https://doi.org/10.1093/europace/euz175
- Ahmed L. A. (2019). Nicorandil: A drug with ongoing benefits and different mechanisms in various diseased conditions. Indian journal of pharmacology, 51(5), 296–301. https://doi.org/10.4103/ijp.IJP_298_19
- PubChem. (2024). N-(p-Amylcinnamoyl) anthranilic acid. PubChem. https://pubchem.ncbi.nlm.nih.gov/compound/N-_p-Amylcinnamoyl_anthranilic-acid
- Salcher, S., Spoden, G. A., Hagenbuchner, J., Führer, S., Kaserer, T., Tollinger, M., Huber-Cantonati, P., Gruber, T., Schuster, D., Gust, R., Zwierzina, H., Müller, T., Kiechl‐Kohlendorfer, U., Ausserlechner, M. J., & Obexer, P. (2019). A drug library screen identifies Carbenoxolone as novel FOXO inhibitor that overcomes FOXO3-mediated chemoprotection in high-stage neuroblastoma. Oncogene, 39(5), 1080–1097. https://doi.org/10.1038/s41388-019-1044-7
- Le, V. T., Knight, S., Watrous, J. D., Najhawan, M., Dao, K., McCubrey, R. O., Bair, T. L., Horne, B. D., May, H. T., Muhlestein, J. B., Nelson, J. R., Carlquist, J. F., Knowlton, K. U., Jain, M., & Anderson, J. L. (2023). Higher docosahexaenoic acid levels lower the protective impact of eicosapentaenoic acid on long-term major cardiovascular events. Frontiers in cardiovascular medicine, 10, 1229130. https://doi.org/10.3389/fcvm.2023.1229130
- Alcocer, L., Bryce, A., Brasil, D. P., Terán, J. L., Cortés, J. E., Quesada, D., & Rodríguez, P. (2023). The pivotal role of Angiotensin-Converting enzyme inhibitors and Angiotensin II receptor blockers in hypertension management and cardiovascular and renal Protection: A Critical appraisal and comparison of international guidelines. American Journal of Cardiovascular Drugs, 23(6), 663–682. https://doi.org/10.1007/s40256-023-00605-5
- Kornej, J., Börschel, C. S., Benjamin, E. J., & Schnabel, R. B. (2020). Epidemiology of Atrial fibrillation in the 21st century. Circulation Research, 127(1), 4–20. https://doi.org/10.1161/circresaha.120.316340
- O’Brien, T. J., Fenton, K., Sidahmed, A., Barbour, A., & Harralson, A. F. (2021). Race and Drug Toxicity: A Study of Three Cardiovascular Drugs with Strong Pharmacogenetic Recommendations. Journal of Personalized Medicine, 11(11), 1226. https://doi.org/10.3390/jpm11111226
- Joukar S. (2021). A comparative review on heart ion channels, action potentials and electrocardiogram in rodents and humans: extrapolation of experimental insights to clinic. Laboratory animal research, 37(1), 25. https://doi.org/10.1186/s42826-021-00102-3
- Chrysafides, S. M. (2023, April 10). Physiology, resting potential. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538338/
- Wei, X. (2023, April 17). Physiology, cardiac repolarization dispersion and reserve. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537194/
- Pirahanchi, Y. (2023, March 13). Physiology, Sodium potassium pump. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537088/
- Goyal, A. (2023, July 4). Reentry arrhythmia. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537089/
- An, Z., Yang, G., Liu, X., Zhang, Z., & Liu, G. (2018). New progress in understanding the cellular mechanisms of anti-arrhythmic drugs. Central European Journal of Biology, 13(1), 335–339. https://doi.org/10.1515/biol-2018-0041
- Osadchii, O. E. (2017). Effects of Na+ channel blockers on the restitution of refractory period, conduction time, and excitation wavelength in perfused guinea-pig heart. PLOS ONE, 12(2), e0172683. https://doi.org/10.1371/journal.pone.0172683
- Wołowiec, Ł., Grześk, G., Osiak, J., Wijata, A., Mędlewska, M., Gaborek, P., Banach, J., Wołowiec, A., & Głowacka, M. (2023). Beta-blockers in cardiac arrhythmias–Clinical pharmacologist’s point of view. Frontiers in Pharmacology, 13. https://doi.org/10.3389/fphar.2022.1043714
- Naji, A. (2023, May 8). Muscarinic antagonists. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK557541/
- Marcu, D., Adam, C. A., Dorobantu, D. M., Șalaru, D. L., Sascău, R. A., Balasanian, M., Macovei, L., Arsenescu-Georgescu, C., & Stătescu, C. (2022). Beta-Blocker-Related Atrioventricular Conduction Disorders—A single tertiary referral Center experience. Medicina-lithuania, 58(2), 320. https://doi.org/10.3390/medicina58020320
- Westergaard, L. M., Alhakak, A., Rørth, R., Fosbøl, E. L., Kristensen, S. L., Svendsen, J. H., Graff, C., Jb, N., Gislason, G., Køber, L., Torp‐Pedersen, C., Lee, C. J., & Weeke, P. (2023). Ventricular rate in atrial fibrillation and the risk of heart failure and death. Europace, 25(5). https://doi.org/10.1093/europace/euad088
- Grubb A, Mentz RJ. Pharmacological management of atrial fibrillation in patients with heart failure with reduced ejection fraction: review of current knowledge and future directions. Expert Rev Cardiovasc Ther. 2020 Feb;18(2):85-101
- David, M. N. V. (2023, January 19). Digoxin. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK556025/
- Alqahtani, M. S., Kazi, M., Alsenaidy, M. A., & Ahmad, M. Z. (2021). Advances in oral drug delivery. Frontiers in Pharmacology, 12. https://doi.org/10.3389/fphar.2021.618411
- Cheng, L., & Wong, H. (2020). Food effects on oral drug absorption: Application of Physiologically Based Pharmacokinetic Modeling as a predictive tool. Pharmaceutics, 12(7), 672. https://doi.org/10.3390/pharmaceutics12070672
- Herman, T. F. (2023, November 3). First-Pass effect. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK551679/
- Mar, P. L., Horbal, P., Chung, M. K., Dukes, J. W., Ezekowitz, M. D., Lakkireddy, D., Lip, G. Y. H., Miletello, M., Noseworthy, P. A., Reiffel, J. A., Tisdale, J. E., Olshansky, B., & Gopinathannair, R. (2022). Drug interactions affecting antiarrhythmic drug use. Circulation: Arrhythmia and Electrophysiology, 15(5). https://doi.org/10.1161/circep.121.007955
- Florek, J. B. (2023, November 12). Amiodarone. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482154/
- Dean, L. (2017, April 4). Propafenone therapy and CYP2D6 genotype. Medical Genetics Summaries – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK425391/
- Rollason, V., Lloret‐Linares, C., Lorenzini, K. I., Daali, Y., Gex‐Fabry, M., Piguet, V., Besson, M., Samer, C. F., & Desmeules, J. A. (2020). Evaluation of phenotypic and genotypic variations of drug metabolizing enzymes and transporters in chronic pain patients facing adverse drug reactions or Non-Response to analgesics: a retrospective study. Journal of Personalized Medicine, 10(4), 198. https://doi.org/10.3390/jpm10040198
- Chu, R. (2020, October 10). Intravenous lidocaine infusion for the management of early postoperative pain: A Comprehensive review of controlled trials. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7901134/
- Weibel, S., Jelting, Y., Pace, N. L., Helf, A., Eberhart, L., Hahnenkamp, K., Hollmann, M. W., Poepping, D., Schnabel, A., & Kranke, P. (2018). Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery in adults. The Cochrane Library, 2018(6). https://doi.org/10.1002/14651858.cd009642.pub3
- Larson, J., Rich, L., Deshmukh, A., Judge, E. C., & Liang, J. J. (2022). Pharmacologic Management for Ventricular arrhythmias: Overview of Anti-Arrhythmic Drugs. Journal of Clinical Medicine, 11(11), 3233. https://doi.org/10.3390/jcm11113233
- Tun, M. M., Pandey, S., Adhikari, S., Mainali, A., Thapa, A., Bisural, R., Bista, P. B., Htet, S. Y., Chhetri, B., & Panigrahi, K. (2023). Amiodarone-Induced liver attenuation on CT scan: alarming signal for toxicity and prompt discontinuation. Cureus. https://doi.org/10.7759/cureus.39844
- Sasi, N., MD. (2024). Medscape Registration. https://emedicine.medscape.com/article/813046-overview?form=fpf
- Ohyama, K., Nakajima, M., Suzuki, M., Shimada, N., Yamazaki, H., & Yokoi, T. (2000). Inhibitory effects of amiodarone and its N‐deethylated metabolite on human cytochrome P450 activities: Prediction of in vivo drug interactions. British Journal of Clinical Pharmacology, 49(3), 244–253. https://doi.org/10.1046/j.1365-2125.2000.00134.x
- Beavers, C. J., Rodgers, J. E., Bagnola, A., Beckie, T. M., Campia, U., Di Palo, K. E., Okwuosa, T. M., Przespolewski, E., & Dent, S. (2022). Cardio-Oncology Drug Interactions: A scientific statement from the American Heart Association. Circulation, 145(15). https://doi.org/10.1161/cir.0000000000001056
- Kamaraju, S., Mohan, M., Zaharova, S., Wallace, B., McGraw, J., Lokken, J., Tierney, J. F., Weil, E., Fatunde, O., & Brown, S. (2021). Interactions between cardiology and oncology drugs in precision cardio-oncology. Clinical Science, 135(11), 1333–1351. https://doi.org/10.1042/cs20200309
- Chakraborty, R. K. (2023, July 28). Calcium channel blocker toxicity. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537147/
- Konieczny, K. M., & Dorian, P. (2019). Clinically important Drug–Drug interactions between antiarrhythmic drugs and anticoagulants. The Journal of Innovations in Cardiac Rhythm Management, 0(3), 3552–3559. https://doi.org/10.19102/icrm.2019.100304
- Ferri, N., Colombo, E., Tenconi, M., Baldessin, L., & Corsini, A. (2022). Drug-Drug interactions of direct oral anticoagulants (DOACs): From pharmacological to clinical practice. Pharmaceutics, 14(6), 1120. https://doi.org/10.3390/pharmaceutics14061120
- Hügl, B., Horlitz, M., Fischer, K., & Kreutz, R. (2023). Clinical significance of the rivaroxaban–dronedarone interaction: insights from physiologically based pharmacokinetic modelling. European Heart Journal Open, 3(1). https://doi.org/10.1093/ehjopen/oead004
- Lucà, F., Oliva, F., Abrignani, M. G., Di Fusco, S. A., Parrini, I., Canale, M. L., Giubilato, S., Cornara, S., Nesti, M., Rao, C. M., Pozzi, A., Binaghi, G., Maloberti, A., Ceravolo, R., Bisceglia, I., Rossini, R., Temporelli, P. L., Amico, A., Calvanese, R., . . . Gulizia, M. M. (2023). Management of Patients Treated with Direct Oral Anticoagulants in Clinical Practice and Challenging Scenarios. Journal of Clinical Medicine, 12(18), 5955. https://doi.org/10.3390/jcm12185955
- Wiggins, B. S., Dixon, D. L., Neyens, R., Page, R. L., & Gluckman, T. J. (2020). Select Drug-Drug interactions with direct oral anticoagulants. Journal of the American College of Cardiology, 75(11), 1341–1350. https://doi.org/10.1016/j.jacc.2019.12.068
- Tovia-Brodie, O. (2020). Pharmacological therapy in Brugada syndrome. Radcliffe Cardiology. https://www.aerjournal.com/articles/pharmacological-therapy-brugada-syndrome
- Sanchez‐Nadales, A., Anampa-Guzmán, A., & Khan, A. (2019). Disopyramide for hypertrophic cardiomyopathy. Cureus. https://doi.org/10.7759/cureus.4526
- Blotner, M., Betageri, O., Miles, W. M., & Kong, X. (2022). WorkUp for Suspected Brugada Syndrome: Two case reports for the general practitioner. Cureus. https://doi.org/10.7759/cureus.21921
- Chhabra, L. (2023, August 7). Wolff-Parkinson-White Syndrome. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK554437/
- Bohnen, M. S., Peng, G., Robey, S., Terrenoire, C., Iyer, V., Sampson, K. J., & Kass, R. S. (2017). Molecular Pathophysiology of Congenital Long QT Syndrome. Physiological Reviews, 97(1), 89–134. https://doi.org/10.1152/physrev.00008.2016
- Narayanan, K. (2020). Strategies for rhythm control in Atrial fibrillation. Indian Journal of Clinical Cardiology, 1(2), 94–107. https://doi.org/10.1177/2632463620936018
- Arunachalam, K. (2023, August 8). Flecainide. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK542291/
- Sreenivas, S. (2021, March 3). Beta-Blocker Medications for AFIB. WebMD. https://www.webmd.com/heart-disease/atrial-fibrillation/beta-blocker-medications-afib
- Viskin, S., Chorin, E., Viskin, D., Hochstadt, A., Schwartz, A. L., & Rosso, R. (2021). Polymorphic Ventricular Tachycardia: Terminology, mechanism, diagnosis, and emergency therapy. Circulation, 144(10), 823–839. https://doi.org/10.1161/circulationaha.121.055783
- Muser, D., Tritto, M., Mariani, M. V., Di Monaco, A., Compagnucci, P., Accogli, M., De Ponti, R., & Guarracini, F. (2021). Diagnosis and treatment of idiopathic Premature ventricular contractions: A stepwise approach based on the site of origin. Diagnostics, 11(10), 1840. https://doi.org/10.3390/diagnostics11101840
- Khachatryan, A., Merino, J. L., De Abajo, F. J., Botto, G. L., Kirchhof, P., Breithardt, G., Stambler, B. S., Abenhaim, L., & Grimaldi-Bensouda, L. (2021). International cohort study on the effectiveness of dronedarone and other antiarrhythmic drugs for atrial fibrillation in real-world practice (EFFECT-AF). Europace, 24(6), 899–909. https://doi.org/10.1093/europace/euab262
- Clinical use of dofetilide – UpToDate. (2024). UpToDate. https://www.uptodate.com/contents/clinical-use-of-dofetilide
- Mubarik, A. (2022, June 10). Sotalol. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK534832/
- Szymanski, M. W. (2023, April 3). Ibutilide. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK526021/
- Phillips, C. T., Wang, J., Celi, L. A., Zhang, Z., & Feng, M. (2019). Association of hypokalemia with an increased risk for medically treated arrhythmias. PLOS ONE, 14(6), e0217432. https://doi.org/10.1371/journal.pone.0217432
- PROPAFENONE HYDROCHLORIDE TABLETS. (2024). https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=a7c8f090-c48c-44f7-9973-2cf4b491e35c&type=display
- Intro_to_antiarrhythmics [TUSOM | Pharmwiki]. (2024). https://tmedweb.tulane.edu/pharmwiki/doku.php/intro_to_antiarrhythmics
- Singh, S. (2023, August 28). Adenosine. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK519049/
- Alobaida, M., & Alrumayh, A. (2021). Rate control strategies for atrial fibrillation. Annals of Medicine, 53(1), 682–692. https://doi.org/10.1080/07853890.2021.1930137
- Fatima, N., Mandava, K., Khatoon, F., Badar, J., Begum, S. F., Narasimhan, C., Daljeet, K., & Mohammed, W. (2022). CLInical Profile and Side Effects of chronic use of oral Amiodarone in cardiology outpatient department (CLIPSE-A Study)- A prospective observational study. Annals of Medicine and Surgery, 80. https://doi.org/10.1016/j.amsu.2022.104167
- Dunn, J. (2023, February 13). Physiology, adenosine triphosphate. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK553175/
- Lavonas, E. J., Akpunonu, P., Arens, A. M., Babu, K. M., Cao, D., Hoffman, R. S., Hoyte, C., Mazer‐Amirshahi, M., Stolbach, A., St‐Onge, M., Thompson, T. M., Wang, G. S., Hoover, A. V., & Drennan, I. R. (2023). 2023 American Heart Association Focused Update on the Management of Patients with Cardiac Arrest or Life-Threatening Toxicity Due to Poisoning: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 148(16). https://doi.org/10.1161/cir.0000000000001161
- Rehman, R. (2023, May 1). Digitalis toxicity. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK459165/
- Pincus M. (2016). Management of digoxin toxicity. Australian prescriber, 39(1), 18–20. https://doi.org/10.18773/austprescr.2016.006
- Crosby, J., Bhopalwala, H., Kharawala, A., Dewaswala, N., Ganti, S. S., & Bhopalwala, A. (2021). Refractory Torsades de Pointes Due to Dofetilide Overdose. Journal of Investigative Medicine High Impact Case Reports, 9, 232470962110564. https://doi.org/10.1177/23247096211056492
- Khalid, M. M. (2023, July 28). Beta-Blocker toxicity. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK448097/
- Bologa, C., Lionte, C., Popescu, A., Sorodoc, V., & Sorodoc, L. (2021). First Case of Acute Poisoning with Amiodarone and Flecainide in Attempted Suicide Successfully Managed with Lipid Emulsion Therapy in the Emergency Department: Case Report and Literature Review. Healthcare (Basel, Switzerland), 9(6), 671. https://doi.org/10.3390/healthcare9060671
- Lei, M., Wu, L., Terrar, D. A., & Huang, C. L. (2018). Modernized Classification of Cardiac Antiarrhythmic Drugs. Circulation, 138(17), 1879–1896. https://doi.org/10.1161/CIRCULATIONAHA.118.035455
- Hakkola, J., Hukkanen, J., Turpeinen, M., & Pelkonen, O. (2020). Inhibition and induction of CYP enzymes in humans: an update. Archives of Toxicology, 94(11), 3671–3722. https://doi.org/10.1007/s00204-020-02936-7
- American Psychiatric Association. (2020). What is schizophrenia? Retrieved from https://www.psychiatry.org/patients-families/schizophrenia/what-is-schizophrenia/
- Bahta, M., Berhe, T., Russom, M., Tesfamariam, E. H., & Ogbaghebriel, A. (2020). Magnitude, nature, and risk factors of adverse drug reactions associated with first generation antipsychotics in outpatients with schizophrenia: a cross-sectional study. Integrated pharmacy research & practice, 9, 205–217. https://doi.org/10.2147/IPRP.S271814
- Cavallaro, R., & Colombo, C. (Eds.). (2022). Fundamentals of psychiatry for health care professionals. Springer. https://doi.org/10.1007/978-3-031-07715-9
- Chokhawala K, Stevens L. Antipsychotic Medications. [Updated 2023 Feb 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519503/
- Grinchii D, Dremencov E. (2020). Mechanism of action of atypical antipsychotic drugs in mood disorders. International Journal of Molecular Sciences. 21(24):9532. https://doi.org/10.3390/ijms21249532
- Katzung B.G., Kruidering-Hall M, Tuan R, Vanderah T.W., & Trevor A.J.(Eds.). (2021) Antipsychotic & bipolar disorder agents. Katzung & Trevor’s Pharmacology: Examination & Board Review, 13e. McGraw-Hill Education. https://accesspharmacy.mhmedical.com/content.aspx?bookid=3058§ionid=255305897
- Kidron A, Nguyen H. Phenothiazine. [Updated 2023 May 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556113/
- National Alliance on Mental Illnesses (NAMI). (2023). Psychosis. Retrieved from https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Psychosis?gad_source=1&gclid=Cj0KCQiAw6yuBhDrARIsACf94RUVJ9RgZl6u71jk32H1dD9N67XFuivUjDnIwTqS7TRiyowwk_90kt0aAlwBEALw_wcB
- Rocca, P., & Bellino, S. (Eds.). (2022). Psychosis and personality disorders: unmet needs in early diagnosis and treatment. Springer. https://doi.org/10.1007/978-3-031-09058-5
- Skidmore-Roth, Linda. Mosby’s 2020 Nursing Drug Reference E-Book : Mosby’s 2020 Nursing Drug Reference E-Book, Mosby, 2019. ProQuest Ebook Central, http://ebookcentral.proquest.com/lib/liberty/detail.action?docID=5978994.
- Vasan S, Padhy RK. Tardive Dyskinesia. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448207/
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Aripiprazole. McGraw Hill
Retrieved from https://accesspharmacy.mhmedical.com/drugs.aspx?gbosID=426473#monoNumber=426473§ionID=243193191&tab=tab0 - Wolters Kluwer Clinical Drug Information, Inc. (2024). Thiothixene. McGraw Hill
Retrieved from https://accesspharmacy.mhmedical.com/drugs.aspx?gbosID=426942#monoNumber=426942§ionID=243275754&tab=tab0 - Wolters Kluwer Clinical Drug Information, Inc. (2024). Loxapine. McGraw Hill; Access Pharmacy.
- Yang S, Boudier-Revéret M, Choo YJ, Chang MC. Association between Chronic Pain, and Alterations in the Mesolimbic Dopaminergic System. Brain Sciences. 2020; 10(10):701. https://doi.org/10.3390/brainsci10100701
- How You Can Prevent Sexually Transmitted Diseases. (2023). Centers for Disease Control and Prevention (CDC). Retrieved from https://www.cdc.gov/std/prevention/default.htm
- Mohseni, M., Sung, S., & Takov V. (2023). Chlamydia. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK537286/
- Springer, C. and Salen, P. (2023). Gonorrhea. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK558903/
- Tudor, M. E., Al-Aboud, A. M., Leslie, S. W., & Gossman, W. (2023). Syphilis. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK534780/
- Bacterial Vaginosis (2021). The Centers for Disease Control and Prevention (CDC). Retrieved from https://www.cdc.gov/std/treatment-guidelines/bv.htm
- Chancroid (2021). The Centers for Disease Control and Prevention (CDC). Retrieved from https://www.cdc.gov/std/treatment-guidelines/chancroid.htm
- Mycoplasma Genitalium. (2021). The Centers for Disease Control and Prevention (CDC). Retrieved from https://www.cdc.gov/std/treatment-guidelines/mycoplasmagenitalium.htm
- Genital Herpes. (2021). The Centers for Disease Control and Prevention (CDC). Retrieved from https://www.cdc.gov/std/treatment-guidelines/herpes.htm
- Kombe Kombe, A. J., Li, B., Zahid, A., Mengist, H. M., Bounda, G. A., Zhou, Y., & Jin, T. (2021). Epidemiology and Burden of Human Papillomavirus and Related Diseases, Molecular Pathogenesis, and Vaccine Evaluation. Frontiers in public health, 8, 552028. https://doi.org/10.3389/fpubh.2020.552028
- Fletcher, C. V., Sax, P. E., & Mitty, J. (2023). Overview of antiretroviral agents used to treat HIV. UptoDate. Retrieved 22 Jan 2024 from https://www.uptodate.com/contents/overview-of-antiretroviral-agents-used-to-treat-hiv
- Trichomoniasis (2023). The Centers for Disease Control and Prevention (CDC). Retrieved from https://www.cdc.gov/std/trichomonas/default.htm
- Rohatgi, K. W., Humble, S., McQueen, A., Hunleth, J. M., Chang, S. H., Herrick, C. J., & James, A. S. (2021). Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. Journal of the American Board of Family Medicine: JABFM, 34(3), 561–570. https://doi.org/10.3122/jabfm.2021.03.200361
- Patel, R.M. and Parmar, M. (2023). Doxycycline Hyclate. In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK555888
- Graziani, A. L., Hooper, D. C., and Bogorodskaya, M. (2023). Azithromycin and clarithromycin. UptoDate. Retrieved 22 Jan 2024 from https://www.uptodate.com/contents/azithromycin-and-clarithromycin
- Podder, V. and Sadiq, N. M. (2022). Levofloxacin. In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK545180/
- Gonorrhea (2023). The Centers for Disease Control and Prevention (CDC). Retrieved from https://www.cdc.gov/std/gonorrhea/treatment.htm
- Weir, C. B. and Le, J. K. (2023). Metronidazole. In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539728/
- Thai, T., Salisbury, B. H., & Zito, P. M (2023). Ciprofloxacin. In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK535454
- Taylor, M. and Gerriets, V. (2023). Acyclovir. In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK542180
- Semaan, J. R. and Parmar, M. (2023). Famciclovir. In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557563
- Aggarwal, N., Leslie, S.W., & Lotfollhzadeh, S. (Updated 2024, January 11). Recurrent Urinary Tract Infections. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557479
- Bono, M.J., Leslie, S.W., & Reygaert, W.C. (Updated 2023, November 13). Uncomplicated Urinary Tract Infections. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470195
- Butler, D., Ambite, I., Wan, M. L. Y., Tran, T. H., Wullt, B., & Svanborg, C. (2022). Immunomodulation therapy offers new molecular strategies to treat UTIs. Nature reviews. Urology, 19(7), 419–437. https://doi.org/10.1038/s41585-022-00602-4
- Evans, J., Hanoodi, M., & Wittler, M. (Updated 2023, August 16). Amoxicillin Clavulanate. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538164/
- Fekete, T. (Last reviewed 2024, January). Asymptomatic bacteriuria in adults. UpToDate. Retrieved from https://www.uptodate.com/contents/asymptomatic-bacteriuria-in-adults
- Gupta, K. (Last reviewed 2024, January). Acute simple cystitis in adult and adolescent females. UpToDate. Retrieved from https://www.uptodate.com/contents/acute-simple-cystitis-in-adult-and-adolescent-females#H207461713
- Gupta, K. (Last reviewed 2024, January). Acute Complicated Urinary Tract Infection (including pyelonephritis) in Adults and Adolescents. UpToDate. Retrieved from https://www.uptodate.com/contents/acute-complicated-urinary-tract-infection-including-pyelonephritis-in-adults-and-adolescents
- Herman, T.F., & Hashmi, M.F. (Updated 2023, August 17). Cephalexin. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK549780
- Kaye, K. S., Rice, L. B., Dane, A. L., Stus, V., Sagan, O., Fedosiuk, E., Das, A. F., Skarinsky, D., Eckburg, P. B., & Ellis-Grosse, E. J. (2019). Fosfomycin for Injection (ZTI-01) Versus Piperacillin-tazobactam for the Treatment of Complicated Urinary Tract Infection Including Acute Pyelonephritis: ZEUS, A Phase 2/3 Randomized Trial. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America, 69(12), 2045–2056. https://doi.org/10.1093/cid/ciz181
- Kemnic, T.R., & Coleman, M. (Updated 2022, November 28). Trimethoprim Sulfamethoxazole. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK513232/
- Lodise, T. P., Henriksen, A. S., Hadley, T., & Patel, N. (2021). US-Focused Conceptual Health Care Decision-Analytic Models Examining the Value of Pivmecillinam Relative to Current Standard-of-Care Agents Among Adult Patients With Uncomplicated Urinary Tract Infections due to Enterobacterales. Open forum infectious diseases, 8(10), ofab380. https://doi.org/10.1093/ofid/ofab380
- Loubet, P., Ranfaing, J., Dinh, A., Dunyach-Remy, C., Bernard, L., Bruyère, F., Lavigne, J. P., & Sotto, A. (2020). Alternative Therapeutic Options to Antibiotics for the Treatment of Urinary Tract Infections. Frontiers in microbiology, 11, 1509. https://doi.org/10.3389/fmicb.2020.01509
- MedlinePlus. (2024). Cefdinir. MedlinePlus. Retrieved from https://medlineplus.gov/druginfo/meds/a698001.html
- MedlinePlus. (2024). Fosfomycin. MedlinePlus. Retrieved from https://medlineplus.gov/druginfo/meds/a697008.html
- MedlinePlus. (2024). Piperacillin and Tazobactam Injection. MedlinePlus. Retrieved from https://medlineplus.gov/druginfo/meds/a694003.html
- Squadrito, F.J., & del Portal, D. (Updated 2023, May 29). Nitrofurantoin. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470526
- Thai, T., Salisbury, B.H., & Zito, P.M. (Updated 2023, August 28). Ciprofloxacin. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK535454/
- Werth, B.J. (Last revised 2022, September). Cephalosporins. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/cephalosporins
- Werth, B.J. (Last revised 2022, September). Fluoroquinolones. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/fluoroquinolones
- Werth, B.J. (Last revised 2022, September). Fosfomycin. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/fosfomycin
- Werth, B.J. (Last revised 2022, September). Meropenem. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/carbapenems
- Werth, B.J. (Last revised 2022, September). Sulfonamides. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/sulfonamides
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate