Course
Washington, DC APRN Bundle
Course Highlights
- In this Washington DC APRN Renewal Bundle course, we will learn about the disparities LGBTQ patients face within the healthcare system.
- You’ll also learn how to implement patient education taking into consideration different learning styles and individual preferences.
- You’ll leave this course with a broader understanding of uncomplicated and complicated UTI and how to differentiate between the classes of antibiotics and their mechanism of action.
About
Contact Hours Awarded: 24 Including 15 Pharmacology Contact Hours
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
LGBTQ+ Cultural Competence
Introduction
Lesbian, gay, bisexual, transgender, and questioning (LGBTQ+) individuals represent a rapidly growing segment of the U.S. population [1]. This rapid growth brings with it risk for stigmatization [1]. Implicit healthcare provider biases may result in LGBTQ+ patients receiving a lower standard of care or restricted access to services as compared to the general population [2]. Even when institutions and providers make commitments to equitable care explicit and implicit biases operating outside of conscious awareness may undermine that commitment. There is an urgent need to ensure that healthcare providers are prepared to identify and address their own implicit biases to ensure they do not contribute to the health care disparities experienced by LGBTQ+ and other vulnerable populations. Only by addressing their own implicit biases will health care providers be able to provide patient care in accordance with LGBTQ+ cultural competence.
LGBTQ+ individuals face significant disparities in physical and mental health outcomes [3]. Compared to their heterosexual counterparts, LGBTQ+ patients have higher rates of anal cancer [4], asthma, cardiovascular disease [5,7,8], obesity [6], substance abuse [8,9,10], cigarette smoking [11], and suicide [14]. Sexual minority women report fewer lifetime Pap tests [13,15, 16], transgender youth have less access to health care and LGBTQ+ individuals are more likely to delay or avoid necessary medical care [17] compared to heterosexual individuals. These disparities are due, in part, to lower health care utilization by LGBTQ+ individuals [3]. Perceived discrimination from health care providers and denial of health care altogether are common experiences among LGBTQ patients and have been identified as contributing factors to health disparities [19,20,21,22]. Disparities in health care access and outcomes experienced by LGBTQ+ patients are compounded by vulnerabilities linked to racial identity [23,24,25] and geographic location [6].
Biases among health care students and providers toward LGBTQ+ patients are common [27,28] despite commitments to patient care equality. These biases, also known as negative stereotypes, may be either explicit or implicit [29]. These biases contribute to a lack of LGBTQ+ cultural competence in patient care. A large study of heterosexual, first-year medical students demonstrated that about half of students reported having negative attitudes, explicit bias, towards lesbian and gay people and over 80% exhibited increased negative evaluations of lesbian and gay people compared to heterosexual people (implicit bias) [27]. Research in social-cognitive psychology on intergroup processes defines explicit biases as attitudes and beliefs that are consciously-accessible and controlled; these characteristics are typically assessed via self-report measures and are limited by an individual’s awareness of their attitudes, motivation to reveal these attitudes, and ability to accurately report these attitudes [30,31]. In contrast, the term implicit bias refers to attitudes and beliefs that are unconscious (i.e., outside of conscious awareness) and automatic [32,33]. Implicit bias can be assessed with the Implicit Association Test (IAT) [34], which aims to define the relationships between concepts (ex. race, sex, idea), and positive or negative associations and/or stereotypes. Idenitfied biases are then delegated as slight, moderate, or strong [35].
Healthcare provider biases are correlated with poorer access to services, quality of care, and health outcomes [29, 36, 37, 38]. Explicit biases held by health professionals towards racial/ethnic minorities, women, and older adults are known to affect clinical assessments, medical treatment, and quality of care [39]. Importantly, implicit bias measures are more strongly associated with real-world behaviors than explicit bias measures [40] and are linked to intergroup discrimination [43]. Health care provider’s implicit biases towards vulnerable patient groups may persist despite an absence of negative explicit attitudes [36], resulting in preconceived notions about patient adherence, poor doctor-patient communication, and micro-aggressions, all of which can interfere with optimal care. With less time and limited information processing capacity, provider’s decisions are increasingly governed by stereotypes and implicit biases [42]. Medical student and provider biases may contribute to health disparities in vulnerable populations by negatively impacting communication with patients and decisions about patient care [29, 33]. Taken together, these findings suggest that medical students and healthcare providers are likely to underestimate or to be unaware of their implicit biases towards LGBTQ+ patients, particularly when they are rushed or fatigued, which could impact their behavior and judgments in ways that contribute to health disparities experienced by LGBTQ+ populations. By learning about and addressing their implicit biases, health care providers can work towards demonstrating LGBTQ+ cultural competence and providing optimal care(Introduction section courtesy of Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P.- reference 2).

Self-Quiz
Ask Yourself...
- What are some cultural misconceptions regarding the LGBTQ+ community and providing medical care?
- How can you demonstrate LGBTQ+ cultural competence in everyday practice?
Terminology
Understanding the standard terminology utilized is pivotal to treating and interacting with LGBTQ+ patients. Below are listed some of the common terms and how they should be referenced.
Ally– A person not identifying as LGBTQ+, but whom promotes equality and support of LGBTQ+ peoples in a variety of ways.
Androgynous– Identifying as neither masculine nor feminine.
Bisexual – A person who is emotionally, romantically, or sexually attracted to more than one sex, gender, or gender identity.
Cisgender – A person whom identifies with their gender which as assigned at birth. For example, a person assigned female gender at birth who identifies as female.
Gay – A person who is emotionally, romantically and/or sexually attracted to those of the same gender.
Gender-fluid – A person who identifies as a fluid or unfixed gender identity.
Lesbian – A woman who is emotionally, sexually, and/or romantically attracted to other women.
LGBTQ+ – Acronym for “lesbian, gay, bisexual, transgender, and queer.”. The plus sign stands for the innumerable other identities.
Non-binary – Adjective describing person(s) who do not identify exclusively as man nor woman.
Pansexual – A person who has the potential for romantic, emotional, and/or sexual attraction to people of any gender.
Queer – Often used interchangeably with “LGBTQ+”, or to express fluid identities or orientations.
Sexual orientation – An inherent or enduring emotional, romantic, or sexual attraction to other people.
Transgender –Umbrella term for people whose gender identity and/or expression is different from cultural expectations based on the sex they were assigned at birth. It does not imply any specific sexual orientation and transgender persons may identify as straight, gay, lesbian, bisexual, etc.
*Definitions largely derived from (44, 45).

Self-Quiz
Ask Yourself...
- Which of the above definitions have you heard used interchangeably?
Best Practices
Below we will list and discuss the best practices for ensuring a positive, equitable healthcare experience for LGBTQ+ persons, according to the Joint Commission (this is not a comprehensive list, nor inviolable, but rather highlights).
Create a welcoming environment that is inclusive of LGBT patients and demonstrates LGBTQ+ cultural competence.
- Prominently display the hospital nondiscrimination policy and/or patient bill of rights.
- Waiting rooms and common areas should be inclusive of LGBTQ+ patients and families.
- Unisex or single-stall restrooms should be available.
- Ensure that visitation policies are fair and do not discriminate (even inadvertently) against LGBTQ+ patients and families.
- Foster an environment that supports and nurtures all patients and families.
Avoid assumptions about sexual orientation and gender identity.
- Refrain from making assumptions about a person’s sexual orientation and/or gender identity.
- Be cognizant of bias, stereotypes, and other communication barriers.
- Recognize that self-identification and behaviors do not always align.
Facilitate disclosure of sexual orientation and gender identity, but be aware that disclosure is an individual process.
- Honor and respect patient’s decisions to provide or not provide sexual and/or gender information.
- All forms should contain inclusive, gender-neutral language that allows patients to self-identify.
- Use neutral and inclusive language when communicating with patients.
- Listen to and respect patients’ choice of language when they describe their own sexual orientation.
- Conduct confidential patient satisfaction surveys that include questions regarding sexual orientation and gender identity
*Information largely derived from Joint Commission field guide, reference 45.
For more information on best-practices in the workforce, visit the Joint Commission website by clicking here.

Self-Quiz
Ask Yourself...
- Have you ever misused a pronoun, or overheard a co-worker misuse a pronoun in practice? How can you make sure this doesn’t happen again?
Establishing Relationships with LGBTQ+ Patients
When interacting with patients, one should not assume gender or sexuality. Addressing a patient whom identifies as a female as a male can cause grave harm to the relationship. Instead, nurses should use open-ended questions. For example, rather than saying “Hi sir, what brings you to the hospital,” a nurse might say, “Welcome, what brings you to the hospital today (45)?”
If a nurse uses the incorrect pronoun, the best practice is to apologize and ask the patient what pronoun and name they prefer. For example, a nurse may say, “I apologize for assuming your gender. How would you like to be addressed? (45).
In conversation, the nurse should use the name and/or pronoun the patient prefers without drawing special attention to the subject (45). For example, if a patient prefers to be identified as their partner’s wife, you should follow suit.
The core of relationship-building with LGBTQ+ patients is no different than any other patient, fundamentally. If nurses have a basic understanding of best practices and a healthy dose of respect and compassion for LGBTQ+ patients, a positive relationship is likely to develop.

Self-Quiz
Ask Yourself...
- Do you have any biases which may affect the care you provide to LGBTQ+ patients?
- Have you worked for someone who did NOT demonstrate LGBTQ+ cultural competence? In what ways could they improve their practice?
Health Disparities of LGBTQ+ Patients
LGBTQ+ Americans are at higher risk of substance use, sexually transmitted diseases, cancer, cardiovascular disease, obesity, bullying, isolation, anxiety, depression, and suicide when compared to the general population (49). LGBTQ+ youth are frequently bullied at schools (46). In fact, early victimization and subsequent emotional distress accounted for 50% of the disparities between LGBTQ+ youth (46). In other words, LGBTQ+ Americans are discriminated against and disadvantaged from a very young age.
When home life also reflects a lack of LGBTQ+ cultural competence, more problems arise. A major cause of LGBTQ+ distress is family rejection. Disclosure of gender identity or sexuality can cause very significant interpersonal conflicts among family and friends of LGBTQ+ persons (46). This explains some hesitancy and should help nurses understand the importance of respecting privacy, while giving options to patients about disclosing sexuality and gender.

Self-Quiz
Ask Yourself...
- Are there any circumstances in which your current hospital’s policies could discriminate against LGBTQ+ families?
- If so, how would you begin to work with leadership to change those policies so they reflect LGBTQ+ cultural competence?
Providing an Inclusive and Accepting Care Environment
LGBTQ+ patients often experience difficulty in finding healthcare environments in which they feel accepted and understood (45). Past negative experiences, lack of knowledge among healthcare providers, and limited access to healthcare in general may become major barriers for LGBTQ+ persons when seeking care (45).
The core tenant of providing an inclusive environment is understanding the needs of LGBTQ+ patients, and working diligently to create an environment which does not disadvantage or discourage them from seeking care.
Policies and procedures at institutions should be designed to reflect a non-discriminatory environment. For example, many hospital policies dictate that only legal family spouses or partners can visit in specific circumstances. Policies such as this are inherently discriminatory toward LGBTQ+ patients, as they may not have legal spousal status due to social, legal, or personal reasons.

Self-Quiz
Ask Yourself...
- Have you ever had an experience where a colleague made a derogatory remark about a patient, based on sexual orientation or gender status? If this happened to you, how would you handle that situation differently?
Laws Specific to Washington D.C.
1973: Title 34 is passed, which prohibits discrimination based on sexual orientation.
2006: The D.C. Human Rights Act is updated to ensure residents of the district are protected regarding employment, house, and public accommodations.
2016: The Armstrong Amendment is repealed in D.C., which allows religious schools exemptions from complying with anti-discrimination laws.
2016: LGBTQ Cultural Competency CE Act is passed. This requires that all licensed healthcare providers take a 2-credit hour course to increase competency (such as the one you are currently taking!).

Self-Quiz
Ask Yourself...
- Think about the structure of your facility. Does it create an environment which minimizes friction and discrimination of LGBTQ+ patients?
- Do you feel there are any biases among healthcare staff?
- If so, how would begin addressing those?
Exercises on LGBTQ+ Cultural Competence
To help solidify your learning, please complete the following exercises at your own pace. The answers/guidance for each are provided below.
Scenario 1
A patient enters your emergency department and you assume the patient identifies as a female. You introduce yourself and say, “Ma’am, how can we help you? What brings you in today?”
The patient appears dismayed but answers the question. The nurse is confused and does not understand why the patient appears distressed. What is the best course of action?
Answer: The nurse should apologize to the patient and ask the patient how they would like to be addressed. Then, the nurse should update the patient’s records to reflect such, to reduce further confusion.
If the nurse does not address the issue, the patient may feel uncomfortable and develop a negative association with healthcare, which can lead to disparities in the future.
Scenario 2
A patient in your ICU has had a deterioration while his husband was in the room. After a family meeting, a member of the healthcare team makes a derogatory remark about the patient’s sexuality. What is the next best action for the nurse?
Answer: Pre-conceived phobias and stigmatizations can cause significant distress to LGBTQ+ patients, even if not stated directly to them. These type of remarks are abusive and should not be tolerated. The nurse should confront the co-worker (if safe) and consider reporting the comments to the Human Resources department.
Scenario 3
A LGBTQ+ patient is being admitted and prefers not to disclose their sexuality. However, the nurse is unable to proceed with the admission process without this information. What could be done to rectify this system-level issue?
Answer: The nurse should work with administration to ensure that all charting and paperwork allows individuals to self-report sexuality and/or gender if they want. However, healthcare systems should not force patients to “come out” unless it is absolutely medically necessary.

Self-Quiz
Ask Yourself...
- What information from this course can you take to your facility to encourage a positive change of LGBTQ patients, and create an environment for LGBTQ+ cultural competence?
Conclusion
LGBTQ+ cultural competence must be ingrained in our healthcare systems in order to foster excellent relationships between members of the LGBTQ+ community and medical staff. Hospitals and healthcare systems have a great deal of work to do in becoming LGBTQ+ friendly. The efforts must continue until LGBTQ+ patients and families do not feel disadvantaged, anxious, or frustrated when interacting with healthcare systems. As the patient’s ultimate advocate, nurses are at the front-line and should advocate for patients both individually and from a policy perspective. Nurses should work with and spearhead efforts to ensure that healthcare policies reflect best-practice and do not discriminate against LGBTQ+ patients in any way.
Patient Education Strategies
Introduction
As nurses, we wear many hats and take on numerous roles in our careers. The main part of our job is to educate our patients.
Have you ever walked into your patient’s room after the physician leaves, and are bombarded with questions from your patient? They are confused and scared, and this is when you come in.
Patient education is important in every type of nursing: inpatient, outpatient, acute care, long-term care, adults, or pediatrics. No matter the specialty of nursing, at some point in time you must educate your patients and their families.
This course’s goal is to provide resources to improve education for your patients, give strategies to prevent barriers to education and evaluate the effectiveness of the education we provide.
Definition- Patient Education
What does patient education mean exactly?
Education is knowledge that results from the process of being educated [10]. No matter what type of nursing you are in, you are constantly giving patients instruction on a topic.
Whether it is regarding medications, diagnostic testing, or diagnoses we are the patient’s main point of contact. A physician or provider is with a patient for a short amount of time, and it is our job to explain the information that was given to them.
Currently, there is information everywhere. We are almost overloaded with information. With the use of smartphones, we can search for almost anything.
Our patients, for the most part, want to feel in control of their health, and this can come in the form of knowledge. As soon as they hear something, they want to search for information on the subject.
This should not substitute our teaching. A lot of the information published may not be accurate or not pertain to their situation. We must be aware of this and make sure we are providing our patients with resources so they can find accurate information [2].
Who are we educating?
The Healthcare Education Association has shared guidelines on patient education [8]. In some instances, we are educating family members, caregivers, friends, and sometimes an entire family [8].
You might be caring for an elderly patient in an acute care setting and will be discharging this patient home to their adult child. They will now be the caregivers and they will require education. Or you are caring for a five-year-old, just diagnosed with type I diabetes in which multiple members of the family will need to be educated on carbohydrate counting and insulin administration.
During this course, the term patient education may be used but it is meant to encompass anyone that we are providing teaching to.
Importance
At the end of the day, patient safety is our main goal. Patient education is a vital way to promote patient safety.
After a new medication is prescribed, we must educate the patient on why they need to take this medication, how to take the medication appropriately, and the side effects of the medication. Our education can also push the importance of lifestyle changes after a diagnosis.
It is easy to go through the motions of your job and forget why we became nurses. Our patients need their healthcare team to take the time to explain the importance of their treatment plan. Education helps patients be the center of their healthcare [12].
What is health literacy?
Health literacy is described as the knowledge of health information and the ability to understand and find resources related to health information, to make decisions for their healthcare based on this information [1].
This definition was changed in 2020 [1]. The change included being able to use health information and apply it to their life, not just having the ability to understand the information. This new definition also states that organizations need to include health literacy in their mission statement [1].
A study conducted by the National Assessment of Adult Literacy showed that only 12% of adult Americans have the appropriate health literacy to understand their care and make informed decisions [7]. With the average population, there is an extreme deficit of the ability to have the information to make autonomous decisions for their healthcare.
How does health literacy play a role in education?
With understanding what health literacy means, we want to give our patients the most accurate information, so they can make the most informed decisions about their healthcare. As nurses, we should be aware of our patients’ health literacy and want them to have the highest level of information available.
Our goal should be that the patient understands and utilizes the information provided in their healthcare choices. Studies have shown that there is a correlation between low education and poor health status [4].

Self Quiz
Ask yourself...
- How can nurses determine their patient’s health literacy?
- Can patient education cut healthcare spending costs?
- Who is responsible for funding patient education?
Role of Nursing
Whose role is it to provide patient education?
Sometimes education can be thought to fall under the physician’s scope of practice. However, every member of the healthcare team can play a part in educating our patients [8].
As said earlier, nurses usually spend the bulk of their time with patients. It is our duty to reinforce and expand upon the teaching provided by other members of the healthcare team. We also must collaborate with other members of the healthcare team to not leave gaps in the education that is provided [12].
Opportunities for Teaching
How should education be prioritized?
In nursing, we are expected to perform a variety of tasks. It can get overwhelming at times trying to prioritize and complete each task. Adding any other task to that list can be daunting.
Education should be incorporated into our work to place patient safety as the goal. Education should be prioritized over other tasks [13]. Many factors such as time and adequate staffing can result in insufficient education [13]. Simple tasks should be delegated if possible, so that you can focus on educating your patients.
Learning Styles
What are the main learning styles?
- Visual- A visual learner requires seeing what they are learning right in front of them [9]. They benefit from graphs and examples for them to look at. Not only going over the education but also providing them with a copy of the teaching is useful.
- Auditory- An auditory learner thrives on hearing the information [9]. This type of learner would not benefit from just receiving a pamphlet.
- Reading- This example of a learning style would be providing material for the learner to read on their own [9].
- Kinesthetic- This type of learner would be described as a “hands-on” learner [9]. This learner would benefit by tangibly holding material. When providing education about
changing an ostomy bag and giving them an ostomy bag to hold would be useful during the teaching.

How do we as nurses identify a patient’s learning style?
A barrier to education can be that we sometimes treat each patient the same. We build standardized educational pamphlets to provide to our patients, teach group classes, and provide similar, if not identical, resources.
While this can be helpful and save time, it can also be a barrier. Not all people learn the same way. Completing a learning assessment for each patient could help identify their preferred learning style to in turn make the teaching more effective [8].
How can we use learning styles in our teaching?
Each person may not be a single type of learner and may be responsive to a variety of learning styles. Prior to providing the actual education, it is important to determine which learning style the patient would be most receptive to.
Also factoring the subject matter into which style you use can be beneficial in teaching [9]. If you need to educate on how to change a dressing on a wound, a demonstration would be appropriate.
If you need to educate on dietary modifications for a low-cholesterol diet, a handout that can be referenced makes sense. The subject matter should be considered when determining which type of learning style should be used.
Case Study:
A patient is being discharged home with a diagnosis of asthma and a new prescription for an albuterol MDI as needed for wheezing. You are the nurse providing discharge teaching.
Prior to providing education you ask if the patient has a preferred learning style. The patient states they are a hands-on learner and are receptive to reading material.
When providing the teaching you give them a spacer with the inhaler to hold and demonstrate how to attach them together. You demonstrate how to administer the ordered number of puffs. You review and provide them with a printout of triggers that could exacerbate their asthma.

Self Quiz
Ask yourself...
- Can multiple learning styles be utilized in your patient’s education?
- Does age play a role in learning styles?
- Can the patient’s education level be a factor in their learning style?
- What if the patient does not have a preferred learning style?
Teaching Strategies
What to include in your education plan?
Before beginning your education with the patient or family member you must set a plan. In your plan, you should include realistic information [2]. Stick to the need to know and not all the information you would like your patient to know [2].
Information overload can be a barrier to helping the patient understand what you are teaching them. In some specialties, nurses have multiple interactions with their patients, where they can build a rapport with them [12].
Use this to your advantage. It might take several visits with your patients to help them understand a certain topic. While other specialties such as acute care, the emergency department, or outpatient surgery centers need to provide concise information and additional resources so the patient can review the information at a later time [2].
Set an attainable goal for yourself and your patient. If you have a short amount of time, it is not realistic to expect to educate on an entire topic such as COPD and expect the patient to verbalize understanding. With specific attainable goals, this will help in your planning and execution of the teaching.
What to ask patients at the beginning of the teaching?
At the start of your teaching, it is crucial to ask the patient about their concerns [8]. A patient might be more receptive to the education if they feel like they are heard. Patient education should be patient-centered, which means focusing on their needs [8].
This can be useful information so you can include what they are most concerned about in the teaching. The patient will then feel valued and will be open to learning.
How does a learner’s demographic become a factor in their understanding of information?
A review was conducted regarding older adults and their preferred style of information [3]. This review concluded that older adults benefit more from written articles presented by healthcare professionals and were not as receptive to group classes, online apps, or videos [3].
Statistics from the CDC states that by 2030, 71.5 million people will be over the age of 65 living in the United States [6]. Which means, in order for them to lead healthy lives, it is our responsibility as healthcare workers to play our part in providing accurate information for them to implement in their lives [6].
On the other end of the spectrum, you might be educating a patient on the other end of the spectrum, a child. Pediatric nursing requires lots of education for the families and the patients themselves.
Children can learn and understand topics when they are presented with developmentally appropriate material. With pediatric patients props and hands-on learning can be beneficial. Age should be considered when planning education materials for patients or their families.
Language can also be a barrier to communication. It is important to ask a patient their preferred language for healthcare information. A patient may speak English however they might be more comfortable in their first language if it is something other than language.
Prior to teaching, a learning assessment is beneficial for you and the patient [8]. Asking the learner their preferred language should take place first.
A patient’s culture can also impact their learning abilities [5][8]. As health care providers we must not shy away from cultural differences but rather incorporate this in our practice [8]. The information we provide should be standardized with our patients, however the way we communicate can vary.


Self Quiz
Ask yourself...
- How can your own culture become a barrier to patient communication?
- What is the best way to ask about a patient’s culture?
- When providing education to a patient who speaks a different language than your own, can information be lost when utilizing an interpreter?
When is the appropriate time to educate your patient?
The patient may be in the middle of a life-changing event or managing a chronic disease and they may have a hard time focusing. When planning to educate a patient it is important to factor in the time of the education.
Did the patient just get out of surgery? Was the patient up all night? Involving the patient in the education will help the patient be more receptive and give them some control [2].
If the patient is being discharged and requires education set a time with them to go over the information. This can prevent barriers that might occur.
How can technology influence education?
In this day in age, technology has influenced all aspects of our lives. Technology can be incorporated into our education as well [2]. Many hospitals are using programs on patient televisions to provide education.
When planning to teach our patients we should explore these methods to help the patient and ourselves as the educator. Some videos can be used that explain procedures, skills, and medications to our patients [8]. It is also important to know our patients and see how receptive they are to this means of education.
An elderly patient may not be interested in a link for more education regarding dietary changes [3]. A person in their 30s may like education they can look at on their computer at home.

Self Quiz
Ask yourself...
- When is providing a patient with a video for teaching appropriate?
- Can technology inhibit a patient from understanding the education provided?
Evaluating Effectiveness
What does it mean to evaluate your teaching?
Teaching is not complete until it is evaluated. As healthcare professionals, we must gauge if our teaching was understood or if further teaching is indicated [8].
If further teaching is needed, it does not mean we failed at our job. It means that we have our patient’s best interest, and we want them to succeed and need to change our education to fit their needs.
Studies in the past have shown that 40-80% of medical teaching done at an outpatient visit was not remembered by the patient and almost half of the information that was retained was not accurate [11].
What are some strategies to evaluate the patient’s understanding of the education provided?
- Demonstration- Often nurses must teach a patient to perform a skill, for example, check blood pressure with a blood pressure cuff, perform a blood glucose check, and administer a subcutaneous injection.
In this type of instruction, the nurse should begin by stating the objective to the patient, which is the skill that needs to be performed, and explain that the patient should return to demonstrate that skill to the nurse [8]. By stating this at the beginning, the patient will know they need to perform the skill at the end of teaching and not be caught off guard. This is also a way to evaluate the teaching [8].
When the patient returns and demonstrates this skill, the nurse can discuss ways they can improve the skill [8].
- Teach-back method- This is a strategy that includes teaching and then allows the learner/patient to demonstrate what they learned back to you [11].
This is an example of how to evaluate the level of the patient’s understanding [11]. Giving the patient time to verbalize what you are educating is a measurable way to evaluate the education that was provided.
A strategy to use the teach-back method is to teach in sections and then allow the patient to state in their own words what they learned in that section [11]. This helps break up the teaching and allows the patient to process the information [11].
Case Study
You are set to discharge a patient home that was hospitalized due to anaphylactic shock from a food allergy. They are overwhelmed by the amount of information they are receiving.
They are prescribed an Epi-pen in case of future reactions. To implement the teach-back method you can use a training Epi-pen to demonstrate how it works.
Then give the practice Epi-pen to the patient so they can hold the Epi-pen and apply the Epi-pen to themselves. Now the patient can feel more comfortable after practice, and you can evaluate if the teaching was understood.

Self Quiz
Ask yourself...
- How can nurses use the return demonstration method in their practice?
- Is the return demonstration method appropriate for every patient?
- What are the next steps if a patient does not accurately demonstrate the skill you were teaching?
Case Study
A patient is diagnosed with hypertension and high cholesterol. As the nurse at an outpatient clinic, you are responsible for going over some lifestyle changes with the patient. You have listed some changes they should make in their diet.
In the middle of the teaching, you ask, “What are 3 dietary modifications you can implement into your daily life?” This helps the patient process the information and turn it into their own words.

Self Quiz
Ask yourself...
- How can nurses use the teach-back method in their practice?
- What settings can the teach-back method be useful in?
When to allow questions during teaching?
Sometimes it might feel easier for us to instruct the learner to save their questions till the end of the instruction. However, allowing the learner to ask questions throughout the education can help prevent information overload and be helpful for you to evaluate your teaching [8].
Questions can allow you to tailor your education to focus on areas that the patient might need more information on [8]. The patient can emphasize their concerns by asking to hear more information on a certain aspect of what you have taught.
When preparing for education make sure that you insert breaks so the patient or family member can ask questions. This will help with their learning and can help you determine the effectiveness.

Self Quiz
Ask yourself...
- What are signs that the patient is not understanding our education?
- If our patient is not grasping the teaching, does it mean our educational techniques fail?
- What is the next step if the patient does not understand our teaching?
Conclusion
To summarize the content of this course: Patient education should be specific, concise, tailored to your patient’s needs, and measurable.
You should present your patients with objectives at the beginning of your education so they will know what to expect to understand by the end of the teaching. Address any questions that the patient might have and allow the patient to provide you with feedback.
By providing intentional patient-centered education we can give our patients the tools they need to make informed decisions about their healthcare.
Nurse Burnout
Introduction
In May 2022, during Mental Health Awareness Month, the United States Surgeon General Dr. Vivek Murthy issued a new Surgeon General’s Advisory highlighting the urgent need to address the health worker burnout crisis nationwide. Citing existing challenges in the healthcare system and the long-term effects of the coronavirus pandemic, Dr. Murthy prioritized our healthcare workers' mental health to strengthen our nation’s public health infrastructure.
This report stated that “…. up to 54% of nurses and physicians, and up to 60% of medical students and residents, suffering from burnout”. Symptoms of burnout have indeed impacted the current workplace, and ongoing employee mental and physical exhaustion results in a vulnerable, compromised workforce (2).
The lingering effects of post-pandemic burnout have affected every element of our current healthcare system. Healthcare professionals are leaving the profession at an alarming rate (due to illness and scheduled retirement), which translates to increasing shortages of providers. Coupled with additional vacancies due to ongoing mental health conditions (depression, anxiety, post-traumatic stress disorder), our healthcare system is experiencing significant gaps in its ability to provide quality care across the healthcare spectrum.
While the legislature addresses healthcare burnout on a larger scale, nurse professionals owe it to themselves to recognize the signs and symptoms of nurse burnout and take appropriate action to protect themselves, their families, colleagues, and patients.

Self Quiz
Ask yourself...
- Why do you think the coronavirus pandemic caused such large numbers of healthcare worker burnout?
- How do you think the coronavirus pandemic affected your place of employment?
- What difference did the pandemic make in your specific job responsibilities?
Nurse Burnout vs. Compassion Fatigue
Although the terms “nurse burnout” and “compassion fatigue” are often used interchangeably, they do refer to two separate conditions (4). Nurse burnout is the term used to describe emotional and physical exhaustion related to ongoing stressful working environments and associated responsibilities. Burnout has a gradual onset and usually occurs in behaviors such as decreased workplace productivity and persistent feelings of hopelessness, helplessness, and overwhelming exhaustion.
Compassion fatigue, on the other hand, often emerges from some prolonged emotional stress or strain. It may occur after exposure to a traumatized individual more so than a workplace trauma. Signs and symptoms of compassion fatigue may manifest in such behaviors as anger, irritability, increased anxiety, and physical exhaustion. In comparing burnout to compassion fatigue, burnout appears to gradually rise to the surface, while compassion fatigue occurs more suddenly (5).

Self Quiz
Ask yourself...
- Regarding compassion fatigue, what situations could make a healthcare professional “angry, irritable, and exhausted” while on duty?
- Regarding nurse burnout, what situations could make a healthcare professional feel “hopeless and helpless” while on duty?
Life As a Nurse
An average day in the life of a nurse will include varying degrees of stress and long work hours. Both factors are known to affect one’s mental health, yet it is considered “a normal day’s work” when describing a day in the life of a nurse.
In any workplace setting, a nurse's role includes a very demanding set of acceptable stressors (“part of the job”). Upon completing a highly stressful workday, nurses may head home to face additional demands on their time and energy levels (child/elder care, various household responsibilities, and community and church obligations, to name a few). This routine leaves little time for rest and recovery, both mind and body.
All those demands on their time and attention can lead to compassion fatigue. The pandemic is a convincing example of both nurse burnout and compassion fatigue. Nursing professionals were repeatedly exposed to critically ill patients, many of whom did not survive. Staffing patterns were suboptimal, critical care beds and equipment were sorely lacking in some areas, and the daily stressors felt during a single shift seemed to repeat themselves. There was no quality “downtime” for nurses to take a well-deserved break, much less debriefing and regrouping/refocus efforts.
This pandemic, a universal “once in a lifetime” event by any standard, affected everyone at some level. Nurse professionals were witnessing traumatic losses of life every day. Compassion fatigue, understandably so, began to surface. The healthcare community experienced anger, irritability, and increasing levels of anxiety. They took to the news media, voicing feelings of isolation, despair, anger, and devastation. They publicly spoke of sleep difficulties, increased workloads, and lack of appropriate lifesaving supplies, thus becoming more exhausted and cynical with each passing shift. When the pandemic crisis finally came under control, the landscape of nursing looked quite different (6).
Nurses had resigned, transferred, or walked off their shifts. Early retirements and medical leaves of absence were increasing in number. Enrollments in nursing schools were down. The healthcare arena continues to suffer years later, looking for solutions to “heal thyself.”
So, the question remains…. What can we do to reduce the risk of nurse burnout moving forward?

Self Quiz
Ask yourself...
- How would you describe your current workplace?
- Do you feel appreciated for your efforts while at work?
- What is one “major stressor” you wish to change at your workplace?
Burnout Risk Factors
While no single factor causes nurse burnout, there are undoubtedly identifiable risk factors and patterns that heighten the risk. Early identification and intervention of such risk factors lower the chances of nurse professionals suffering personally and professionally.
Increased workloads (due to staff call-ins, lack of patient care equipment, and lack of ancillary help) are a leading causative factor in nurse burnout. In addition, lack of support from senior leadership, unit managers, worksite colleagues, and other members of the organizational healthcare team impacts feelings of helplessness and hopelessness.
Again, there is no single factor to point blame at, but there are often patterns of behavior that warrant further investigation at the workplace. In addition, nurse burnout is very individualized. What is harmful and hurtful to one nurse may not be seen as such to another nurse.
The goal is to make the workplace environment supportive for all employees by creating (and nurturing) a culture that welcomes nursing input. By recognizing the bigger picture of individual and organizational safety, the nurse in crisis feels safe in stepping forward and seeking professional help in a supportive environment.
While nurse burnout can occur in any area of nursing, from hospitals to clinics to home health settings and beyond, some areas are at higher risk for burnout. Nursing professionals in the intensive care and emergency care units are at higher risk for symptoms of burnout.
Studies have shown that many specialty nurses experience anxiety, increasing exhaustion, and mounting frustration while on duty. Combined with a patient population often experiencing high rates of trauma-related mortality and complex illnesses, it is understandable that “typical workdays” may be filled with extremely high levels of workplace stress.

Self Quiz
Ask yourself...
- Think about your current workplace. Are there any factors that could contribute to burnout?
- Have you witnessed anyone in your workplace display signs of being “burned” out?
Causes of Burnout
An article published in the Journal of the American Medical Association identified some causes that directly impact nurse burnout (7). The authors found that nurses who routinely worked longer shifts (extra shifts, mandated overtime shifts) and experienced sleep deprivation exhibited symptoms of burnout. The combination of excessive work hours and inadequate sleep (as often occurred with shortened turnaround times and back-to-back shifts) resulted in increased patient care errors. These occurrences often compounded the feelings of helplessness and hopelessness (8).

Self Quiz
Ask yourself...
- Have you ever picked up extra shifts only to regret it afterward?
- How did you feel after working those extra shifts?
Impact on (Individual) Health
In the early stages of burnout, the nurse professional may feel overworked, underappreciated, and physically tired. While such symptoms may appear benign when occurring sporadically and “chalked up” to “just having a bad day,” repeated shifts like this may manifest into a more profound feeling of despair.
It soon becomes challenging to continue working under such circumstances, further escalating the situation. To distance oneself from these feelings, the nurse professional may become cynical and jaded about their workplace, mentally distancing themselves from colleagues. These efforts only serve to isolate the individual further and exacerbate feelings of hopelessness and isolation while negatively impacting workplace efficacy (9).
Impact on Workplace/Organization Health
The stressed out, overworked, and exhausted nurse professional may unknowingly / unintentionally compromise the quality of care. Feelings of helplessness and hopelessness can negatively affect the nurse’s judgment and critical thinking skills. Critical steps/tasks may be skipped when the nurse is tired and overworked.
Nurse burnout negatively impacts job satisfaction and, in doing so, also negatively impacts patient care. The effect will be poor patient care, increased patient and family complaints, and poorer patient outcomes. Nurse burnout affects not only the individual but the organization. (10)

Self Quiz
Ask yourself...
- How does a nurse unintentionally compromise the care being delivered to a patient?
- How do you think being sleep-deprived could affect your abilities while on duty?
Self-Care Strategies
“I have come to believe that caring for myself is not self-indulgent. Caring for myself is an act of survival.”
— Audre Lorde (3).
What is self-care? (12)
In the most basic definition, self-care refers to doing things that will improve your physical and mental health. It is very subjective, and self-care strategies must focus on your needs, wants, and desires. As stated, nurse burnout is very individualized: what profoundly affects one nurse may not even bother the next nurse.
The strategies discussed here are generic; they must be personalized to fit your specific needs and healing process.
- A good night’s sleep: Limit caffeine intake before bedtime, no electronics 1-2 hours before sleep, lower room temperature to facilitate comfortable sleep, and blackout curtains.
- Physical activity: Light-impact activities such as swimming, yoga, walking, bike riding, and other activities will be physically and mentally beneficial.
- Diet: Maintain a balanced diet. Monitor hydration levels and limit caffeine products. The goal is to nourish your body to offset the adverse effects of stress. Cut down on processed food intake and “junk foods.”
- Mental health: Journaling, podcasts, music, and joyful hobbies and activities (knitting, crafts, painting).
- Homefront Maintenance: Calm surroundings foster the healing process. Keep the environment clean, uncluttered, and welcoming. Empty the sinks and dishwashers, fold the laundry, and make your bed. Aromatherapy, lighted candles, and essential oils are all ways to make your home a place to rest and relax.
The list of “self-care “strategies is endless. Be sure to find an appropriate diet, activity, and behaviors that enable you to focus on building a balanced lifestyle.


Self Quiz
Ask yourself...
- What are some self-care strategies that have worked in your personal life?
- How could you encourage a nursing colleague to “take better care of themselves” through self-care practices?
Organizational Strategies
Healthcare organizations must provide structured support for their nurse professionals to ensure quality patient care. Facility-wide strategies work best to identify and treat nurse stress and burnout early.
- Nursing rounds- routinely meet with nursing staff and listen to their feedback. Ask the difficult questions (staffing patterns, scheduling issues) and be receptive to working on viable solutions.
- Support staff in utilizing earned days off, vacation time/ paid time off.
- Open lines of communication with staff experiencing signs of nurse burnout or compassion fatigue. Offer alternate job duties and work assignments if possible.
- Acknowledge employee organizational loyalty (through retention bonuses, additional days off, gift cards, personalized thank-you letters, and personal development endeavors).
- Encourage critical debriefings for staff members involved in essential/traumatic patient care encounters.
- Openly promote facility resources available to staff, including all Employee Assistance Programs.

Self Quiz
Ask yourself...
- How do you feel your healthcare organization could improve the current workplace?
- What are some employee assistance programs currently offered at your workplace?
- What incentives/ acknowledgments from your nurse leaders would most benefit staff morale?
Case study
Marie is a 35-year-old Registered Nurse working full-time on a 16-bed ICU unit. She has been employed here for three years, beginning her employment at the start of the coronavirus pandemic. Marie works 12-hour shifts (7p-7a) with every other weekend off. Two of Marie’s nurses' coworkers recently resigned, leaving the unit chronically short-staffed.
Marie has been working additional shifts to help her coworkers and has just completed a 50-hour work week. She was once again called into work early and arrived on only 4 hours of sleep the night before. The unit is at total capacity with 2 “ICU holds” in the Emergency Department. Marie has fallen behind on her patient care while intercepting repeated calls from the ED staff.
Marie spent a long overdue break crying in the nurse's lounge. She confided to another staff member (Anne) that she is exhausted and overwhelmed by these work conditions and is considering resigning. Anne told Marie to take a few more minutes for her break and promised to discuss the situation with their charge nurse, Carol. Marie agreed.
Anne discussed the situation with Carol, stating Marie is a great nurse who has been working too many shifts lately. Anne offered to pick up some of Marie’s current patient assignments to lower Marie’s stress level, hopefully. Carol approved and also took some of Marie’s patients. Marie finished her break, apologized to her coworkers for her “moment of weakness,” and promised, “it wouldn’t happen again.”

Self Quiz
Ask yourself...
- What factors did you identify that put Marie at risk for nurse burnout?
- If Marie confided in you, as a colleague, that she was exhausted and overwhelmed, how would you respond?
- Marie apologized for her “moment of weakness” and promised “it wouldn’t happen again.” How would you respond to this employee if you oversaw this shift?
- What resources are available at your current workplace for employees who acknowledge they are “exhausted and stressed out”?
- If you were the Nurse Manager of this ICU, what would you do to support your staff during this time (* significant staffing shortages due to recent resignations)?
Resources
The following links are provided for additional information on nurse burnout surveys.
Conclusion
The healthcare workforce continues to be challenged by large numbers of scheduled retirements, an aging population, and medically complex patients. Nurse leaders must proactively hire and retain a healthy workforce (13). Healthcare organizations must invest in a workplace culture that supports workers' work/life balance. It is the key to ensuring the health and safety of our nation.
Bullying in Nursing
Introduction
In a time when bullying has become one of the most frowned upon behaviors, why is it thriving in the world of nursing? We’ve all heard the saying that “nurses eat their young”. It is a term that has been passed down the nursing ranks as each generation of nurses enters the workplace; unchanged and still true. We, as nurses, cannot permit such unhealthy and detrimental behavior to continue. In this course, we will discuss nurse bullying, why it happens and what we can do to break the curse.
Definitions
To fully understand nurse bullying and the issues that come with it, we must define some terms and phrases so that we are all on the same page.
Nurse Bully
A nurse bully is someone who repeatedly harasses and/or harms other nurses whom they believe they can dominate; they may also see them as less skilled or incompetent (5).
Incivility
Incivility is a type of lower-level bullying that entails more passive types of behavior. This is your mocking, gossiping, alienation, and general rudeness. The difference between incivility and actual bullying is that incivility may not actually harm the victim (6).
Harassment
Harassment is when someone torments or intimidates another person (4).


Self Quiz
Ask yourself...
- What is the difference between incivility and bullying?
- Who is the victim of the nurse bully?
Incidence Rate
The nursing profession has historically been known as the most trusted profession. Nursing is also synonymous with caring and compassion. From the outside looking in, it may be difficult to believe that bullying could exist in such a respected and revered profession. The prevalence of bullying in nursing is staggering. Both new and seasoned nurses; young and old; nurses of every gender; and nurses of every walk of life report that they have been bullied on the job. These instances represent a wide variety of bullying behaviors which include verbal abuse, threatening, scapegoating, sabotage, and physical abuse (5).
Incidence rates of bullying in nursing, as documented in a variety of studies, ranging from 17-85%. This includes incidents of verbal abuse, threatening, belittling, and even physical abuse. With the prevalence of bullying so high among nurses, it is safe to say that virtually every nurse has been touched by bullying, whether victim, perpetrator, or observer (5).

Self Quiz
Ask yourself...
- Does the incident rate of nurse bullying surprise you?
- Have you ever witnessed or been involved in an incident of nurse bullying?
Why Does It Occur?
What drives bullying behaviors? What makes a bully? There are a myriad of factors that come into play when discussing why bullying occurs.
Anger and frustration are two strong emotions that can contribute to bullying behaviors. In today’s nursing work environment, anger and frustration are at the forefront of many nursing units. Nursing shortages have left many units understaffed and the nurses overworked. This frustration leads to anger when the nurses who have remained loyal, full-time staff see travelers come into their areas making higher pay. Lack of resources and the belief that they are unheard of also contribute to feelings of frustration (5).
The belief that another nurse is less competent or altogether incompetent can also lead to bullying. When it is perceived that another nurse can’t do their job and therefore may leave tasks for the oncoming shift, the above-mentioned frustration sets in and bullying may result. Just the feeling of superiority over another nurse can have bullying effects on the nursing environment (1).

Self Quiz
Ask yourself...
- Is there a key risk factor that promotes an environment of nurse bullying?
- Are nurse bullying risk factors real or perceived? Explain.
Risk Factors
There are some circumstances that contribute to the bullying climate. These are not excuses that give permission to the bullies, rather they are risk factors that have been identified as possible catalysts to bullying behaviors.
Seniority
Some nurses may feel that they have “paid their dues” and should have authority over their less-experienced peers. If this authority is not granted, the senior nurse may harbor feelings of underappreciation and lash out by being unhelpful or, to the extreme, harmful. The aim is to show how much this nurse is needed; they will refrain from helping the newer nurse or giving any advice (5).
Insecurity
When new nurses come into the workplace, the existing nurses may feel that they will be replaced. Nursing is an ever-evolving occupation with new technologies and treatments being developed all the time. A new nurse who was taught the most up-to-date trends in nursing may pose a threat to their job. This is when the nurse may start to bully the new nurse joining the team (1).
Protection
Some nurses become very attached to their patients. They may feel that no one else can give the same level of care that they can. As a result, they may see other nurses as incapable of providing care that is up to their standards. Only they can provide the care that their patients require. These perceived inadequacies can quickly turn into bullying behaviors (1).
Education
Differences in levels of education may also contribute to bullying. Nursing has many different levels of education and nurses from all these levels may work together on a single unit. Nurses with higher levels of education may feel superior and lash out at those with less education. RNs may treat LVNs differently than their RN peers (3).

Self Quiz
Ask yourself...
- Name 2 risk factors that contribute to nurse bullying.
- Have these risk factors led to a nurse bullying environment in your organization?
- Does one risk factor stand out to you as a prime contributor to nurse bullying?
- Which one?
Types of Bullying
It is important to note that not every bullying-type behavior can be construed as actual bullying. We all have bad days when things just don’t seem to be going right and we may react inappropriately. One of the key factors that differentiates bullying from a lapse in judgment is that bullying is a repeated or habitual behavior.
This does not excuse the one-time behavior however, we must realize that not all poor behaviors are bullying. Nurse bullying may manifest itself in a variety of different behaviors. Below, we will discuss a few of these types of bullying. This is by no means an exhaustive list of all possible bullying behaviors; they are some of the behaviors that you may commonly see in the healthcare environment (5).
Verbal abuse
This may include being rude, belittling, criticizing, and threatening. We’ve all heard “sticks and stones may break my bones, but words will never hurt me”. This is a false saying as constant verbal abuse plays with our psyche as we rerun the taunts in our heads over and over. If heard enough, we may start to believe the bully’s words.
Controlling
Constantly telling another nurse what to do and how to do it. This is unsolicited advice that if not taken may escalate bullying behaviors. Controlling behaviors may also include certain “looks” and intimidating posturing.
Ignoring/excluding
Ignoring requests for help. Ignoring any suggestions to better provide care to the patients. Excluding that one nurse from lunch plans, work-related activities, or any after-work gatherings.
Assigning heavy workloads
Repeatedly assigning a nurse a heavy workload while everyone else’s load is relatively light. All the other nurses have time to sit and document while the one nurse is overwhelmed.
Physical abuse
Unwanted physical contact is usually violent in nature.
Mobbing
This happens when a group of bullies band together to create an environment to force the victim to resign (2).


Self Quiz
Ask yourself...
- Have you witnessed any of these behaviors at your organization?
- Is there a behavior that is most indicative of nurse bullying?
- What is the key aspect that makes these behaviors acts of bullying?
Characteristics of a Nurse Bully
Nurse bullies come in all shapes and sizes and come from all walks of life. There isn’t necessarily a template for what a nurse bully will look like. However, there are some characteristics that may help identify a nurse bully.
You may encounter a nurse who bullies out of a sense of superiority. They will be condescending and have an entitled attitude. You will also recognize them by their “correcting comments” often spoken where others can hear. Next, we have nurses who bully because they have been offended by something said or done. They bully with an ax to grind. They may hold on to the grudge for a long time. Creating drama with the victim at the center will be their course of action; they will try to pull in other nurses to help ostracize their victim. Other nurse bullies will use rumors and gossip to bully their victim (3)
These bullies love to dish out the put-downs but can’t take any back. They will become offended at the slightest criticism. There are others who will be very friendly at first. Bringing the victim in close to learn details of their lives and then using that information against them. They will weaponize all obtained information to lift themselves up. Another characteristic is envy. There are those bullies who are envious of others. The envy could stem from something totally unrelated to nursing or the workplace. The victim, however, will most likely possess the item or characteristic that the bully is envious of. This bully is very bitter. Finally, there is the bully who plays favorites. They will favor their clique and ignore or exclude the victim (3).

Self Quiz
Ask yourself...
- Do you recognize these characteristics in the nurses you work with?
- Do you see any of these characteristics in you? How will you change?
What Can You Do?
There are many actions that you can take when you are either the witness or victim of nurse bullying. Though some bullies may be intentionally trying to intimidate a fellow nurse, there are those who are oblivious to the fact that they are bullies. They behave like a bully without knowing that they are perceived as such.
The first action that you may want to take is to talk with the bully about the behavior. The bullying may end there. Once it has been brought to the bully’s attention that the behavior is being taken as bullying, change can occur. Communication may be all that is needed (5). Prior to speaking with the bully, try using empathy. Put yourself in the bully’s shoes to figure out what the motive for the behaviors may be. This may aid you in both the tone and direction of the conversation.
Identifying a mentor in the workplace can also help you through a bullying situation. Having someone that you can talk to about the issue and seek their advice about how to handle the situation. Look for those nurses who can’t be bullied. Why do the bullies not prey on them? Why are they not intimidated? Often, these nurses are focused on the patient’s needs above all else and refuse to allow any situation to be about them or the bully (3).
Talking with your manager or director is another prudent course of action. It is possible that these nurse leaders have the best vantage point to deal with and prevent nurse bullying. They work closely with the front-line staff nurses and should have the pulse of the unit. In their position of authority, they are also able to investigate and, if needed, conduct disciplinary actions.
Unless your manager or director is the bully, a meeting with them to discuss any instances of bullying is needed. Contacting the Human Resources department is another step that can be taken. No matter the situation, it is always important to follow your facility’s policies and procedures and chain of command (3).

Self Quiz
Ask yourself...
- What can you do to prevent/stop nurse bullying in your organization?
- What organizational resource should you use to guide your actions?
Solutions to Nurse Bullying
Nurse bullying has repercussions throughout the entire facility. According to a study from 2012, the cost for each individual who is bullied can be from thirty thousand to one hundred thousand dollars (3). This includes the cost of absenteeism, lower work performance, any therapies needed for physical and psychological issues, and increased turnover due to ongoing bullying.
Nurse bullying can also play a big part in the overall feeling of “burnout” among nurses. Nurse bullying can lead to workplace errors which means it is crucial that organizations have strategies to combat any kind of bullying in the workplace. As nursing accounts for the majority of employees at most hospitals, curbing nurse bullying should be in the forefront. Here are some organizational strategies that should be considered:
Culture of Safety
Many organizations have adopted a “Culture of Safety”. The Culture of Safety promotes patient and colleague safety. It is the shared beliefs and values of the organization that influence behaviors and actions. Principles such as non-punitive reporting, communication of policies and expectations, recognition, and leadership modeling of behaviors all come into play in the Culture of Safety. All reports of bullying should be taken seriously (3).
Admit that there is a problem
Like any issue, the first step in fixing it is admitting that the problem exists in the first place. Bullying thrives in the darkness. Once it is brought to light and people are talking about it, it can be addressed. Even if there is no evidence of nurse bullying in your area, talking about and discouraging it may stop it from even starting (3).
Elimination
Try to eliminate factors that promote an environment of bullying.
Commitment
The organization should commit to a zero-tolerance policy when it comes to bullying. The policy on bullying should outline clear expectations along with the consequences that will be enforced if the policy is not followed. The policy should also include the organization’s social and online media sites (3).
Accountability
Nurses should be encouraged to hold each other accountable. You promote what you permit. As there are generally more bullying witnesses than actual bullies, nurses must be empowered to call out bullying. This can lead to a true change in the culture of an organization (3).

Self Quiz
Ask yourself...
- Is your facility currently using any of the above-mentioned strategies?
- How have these strategies mitigated the incidence of nurse bullying in your area?
- Can an organization eliminate nurse bullying?
Conclusion
Nurse bullying is a real problem that can affect any unit in any hospital. It creates a toxic work environment that we, as nurses, can no longer tolerate. In this post-COVID time, nursing shortages and nurse burnout are rapidly depleting the nursing ranks. It is time for nurses to call out bullying when they see it. It is time for nurse leaders to enforce the organizational consequences of nurse bullying.
We must create safe environments for our new nurses (all nurses) to thrive. It is the only way that our profession will survive. Know the signs of nurse bullying and become the change within your organization. Empower your colleagues to do the same. Together, we can see an end to nurse bullying.
Quality Improvement for Nurses
Introduction
Welcome to the world of Quality Improvement (QI) in healthcare, a dedicated field committed to continually enhancing patient care and outcomes. Quality Improvement involves a systematic approach to identify, analyze, and address areas for improvement within healthcare processes, ultimately resulting in improved patient safety, satisfaction, and overall healthcare excellence (13). In this course, we will embark on a journey to explore the fundamental principles and practical applications of QI, explicitly tailored for nurses who aspire to make a positive impact in their healthcare settings.
As a nurse, you know the significance of providing high-quality patient care. However, you may wonder how you can actively contribute to improving the systems and processes in your workplace.
Imagine this scenario: You observe a recurring issue with medication administration, where doses are occasionally missed due to workflow inefficiencies. Through this course, you will acquire the knowledge and skills to apply QI methodologies like Plan-Do-Study-Act (PDSA) cycles to investigate such issues, implement changes, and monitor the impact of your interventions. By understanding QI principles and tools, you will be better equipped to collaborate with your colleagues, drive meaningful improvements, and ensure that your patients receive the best care possible.
Introduction
Welcome to the world of Quality Improvement (QI) in healthcare, a dedicated field committed to continually enhancing patient care and outcomes. Quality Improvement involves a systematic approach to identify, analyze, and address areas for improvement within healthcare processes, ultimately resulting in improved patient safety, satisfaction, and overall healthcare excellence (13). In this course, we will embark on a journey to explore the fundamental principles and practical applications of QI, explicitly tailored for nurses who aspire to make a positive impact in their healthcare settings.
As a nurse, you know the significance of providing high-quality patient care. However, you may wonder how you can actively contribute to improving the systems and processes in your workplace.
Imagine this scenario: You observe a recurring issue with medication administration, where doses are occasionally missed due to workflow inefficiencies. Through this course, you will acquire the knowledge and skills to apply QI methodologies like Plan-Do-Study-Act (PDSA) cycles to investigate such issues, implement changes, and monitor the impact of your interventions. By understanding QI principles and tools, you will be better equipped to collaborate with your colleagues, drive meaningful improvements, and ensure that your patients receive the best care possible.

Self Quiz
Ask yourself...
- How can nurses leverage their unique position at the bedside to identify opportunities for quality improvement in healthcare settings?
- Can you provide an example from your own experience or knowledge where a quality improvement project led to tangible improvements in patient care?
- What potential challenges could a nurse encounter when attempting to implement quality improvement projects?
What is Quality Improvement?
Quality Improvement (QI) in healthcare represents an ongoing, systematic effort to elevate the quality of patient care and healthcare services that involves identifying areas needing improvement, implementing changes, and evaluating the effects of those changes to ensure better patient outcomes (12).
Let’s envision a scenario where a hospital's surgical department grapples with a higher-than-average rate of post-operative infections. Through a QI initiative, the healthcare team can meticulously scrutinize the surgical processes, pinpoint potential sources of infection, and introduce evidence-based practices such as enhanced sterilization techniques or more rigorous antibiotic prophylaxis protocols. Over time, they can gauge the effectiveness of these changes by monitoring infection rates for a reduction.
Commonly used QI methodologies in healthcare include the DMAIC (Define, Measure, Analyze, Improve, Control) process and the Plan-Do-Study-Act (PDSA) cycle. These approaches provide structured frameworks for healthcare professionals to tackle issues systematically and iteratively. For example, imagine a bustling primary care clinic with extended patient wait times.
Here, the PDSA cycle can come into play using the systematic iterative steps below:
- The team defines the problem (lengthy wait times)
- The team proceeds to test a change (for example, adjusting appointment scheduling)
- The team then scrutinizes the results and acts accordingly to refine the process.


Self Quiz
Ask yourself...
- How does the concept of Quality Improvement (QI) align with the goal to provide the best possible care for patients?
- Can you think of a specific healthcare scenario where QI methodologies like DMAIC or PDSA could significantly improve patient care?
- What are the advantages of using structured frameworks like DMAIC and PDSA in QI initiatives?
- How do DMAIC or PDSA contribute to the success of improvement projects?
History and Background of Quality Improvement
The history and background of Quality Improvement (QI) in healthcare have a rich and evolving timeline, dating back to the early 20th Century, with significant developments occurring over the years. One pivotal moment in this journey was the introduction of statistical quality control by Dr. Walter A. Shewhart in the 1920s (24). Dr. Shewhart's pioneering work laid the foundation for using statistical methods to monitor and enhance processes, a concept that would become integral to QI initiatives (24).
In the mid-20th Century, the contributions of Dr. W. Edwards Deming further propelled QI principles forward (7). Dr. Deming emphasized the significance of continuous improvement, active employee engagement, and process variability reduction. His ideas found fertile ground in post-World War II Japan, playing a crucial role in the nation's economic recovery and the emergence of renowned companies like Toyota, famous for its Toyota Production System (TPS), incorporating QI concepts (7).
Until today, QI has become indispensable to healthcare systems worldwide (16). To illustrate, envision a scenario where a hospital grapples with a high readmission rate among heart failure patients. By scrutinizing historical data and implementing evidence-based protocols for post-discharge care, hospitals can effectively lower readmissions, enhance patient outcomes, and potentially evade financial penalties under value-based reimbursement models (16).

Self Quiz
Ask yourself...
- How did the work of Dr. Walter A. Shewhart in the early 20th Century contribute to the foundation of QI, and how do statistical methods continue to play a role in healthcare improvement today?
- What fundamental principles were introduced by Dr. W. Edwards Deming, and how did they influence QI practices in healthcare and other industries?
- Can you provide an example of how QI methodologies, inspired by Deming's principles, have been successfully applied in modern healthcare settings to address specific challenges or improve patient care?
- How has continuous improvement evolved, and why is it considered a cornerstone of QI in healthcare?
Models
At the heart of ongoing transformations in healthcare lies various Quality Improvement (QI) models. These models provide structured frameworks for identifying and addressing areas of improvement within healthcare systems (14). These models offer healthcare professionals a systematic approach to instigate meaningful process changes, ultimately resulting in elevated care quality. See some models below.
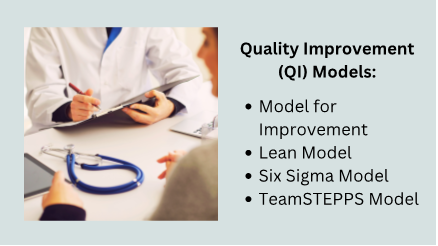
Model for Improvement
The Model for Improvement is a widely recognized and highly effective framework for Quality Improvement (QI) in healthcare. This is because it empowers healthcare professionals to systematically test and fine-tune their ideas for process improvement, ensuring that changes are grounded in evidence and proven effective (17).
The Model for Improvement offers a structured and systematic approach to identifying, testing, and implementing changes to enhance healthcare processes and ultimately elevate patient outcomes.
Developed by Associates in Process Improvement (API), this model revolves around the iterative "Plan-Do-Study-Act" (PDSA) cycle, which forms the foundational structure of QI initiatives (17). The Plan-Do-Study-Act (PDSA) cycle is a systematic approach that guides healthcare teams through quality improvement, and it comprises the four key phases below, each contributing to developing and implementing meaningful changes in healthcare practices (12).
- Plan: In this initial phase, healthcare teams define the specific problem they aim to address, set clear and measurable goals, and craft a comprehensive plan for implementing the proposed change. For instance, if a hospital seeks to reduce patient wait times in the emergency department, the plan may involve adjustments to triage protocols or streamlining documentation processes.
- Do: Once the plan is established, the proposed change is implemented, typically on a small scale or within a controlled or pilot environment. This enables healthcare professionals to assess the feasibility and potential impact of the change without making widespread adjustments.
- Study: The study phase involves rigorous data collection and analysis to evaluate the effects of the change. In our example, the hospital would measure the impact of the new triage protocols on wait times, closely examining whether they have decreased as expected.
- Act: Based on the findings from the study phase, the healthcare team makes informed decisions about the change. They may adopt the change if it has successfully reduced wait times, adapt it further for enhanced effectiveness, or, if necessary, abandon it.
The PDSA cycle's iterative nature means adjustments can be made, and the cycle repeats until the desired improvement is achieved (12).
Lean Model
The Lean model, initially conceived in the manufacturing sector, has found considerable success and applicability in healthcare as a potent tool for process enhancement and waste reduction (22). At its core, Lean thinking revolves around the principles of efficiency and value optimization because it focuses on refining processes to eliminate wasteful elements while simultaneously delivering care of the highest quality (22).
Healthcare organizations have adopted Lean methodologies to tackle many challenges, from reducing patient wait times to improving inventory management and elevating overall patient satisfaction (22). For instance, when a hospital is challenged with prolonged wait times in its outpatient clinic, it can apply Lean principles to systematically analyze the patient flow, pinpoint bottlenecks, and streamline processes.
This might involve reconfiguring furniture to enhance flow, adjusting appointment scheduling, or implementing standardized work procedures. The ultimate objective is to cultivate a patient-centric, efficient environment that ensures timely access to care while meticulously conserving time and resources.
Another integral aspect of Lean thinking is the unwavering commitment to continuous improvement and the pursuit of perfection through the systematic identification and eradication of various forms of waste (19). The forms of waste are often categorized into seven types: overproduction, waiting, unnecessary transportation, overprocessing, excess inventory, motion, and defects (19). By keenly identifying and addressing these forms of waste, healthcare organizations not only enhance the utilization of resources but also curtail costs and elevate the overall quality of care delivery.
Six Sigma model
The Six Sigma model is a robust and widely adopted healthcare method for improving processes and reducing mistakes (9). It was first used in manufacturing but is now used in healthcare to make processes more consistent and improved by finding and fixing mistakes and inefficiencies (9).
An example is when a hospital is concerned about the accuracy of medication dosing for pediatric patients, a Six Sigma team might include: indicating the problem, gathering data on mistakes regarding dosing, and finding out why the mistakes happened. The strategy may encompass the implementation of standardized dosing protocols, refining staff training programs, and closely monitoring the medication administration process to ensure that mistakes are eliminated.
Six Sigma uses a framework called DMAIC (Define, Measure, Analyze, Improve, Control) to make improvements. This framework utilizes data-driven tools to discern problems, quantify their origins, develop practical solutions, and institute control mechanisms to sustain improvements (11). Through this systematic journey, healthcare organizations position themselves to deliver care of elevated quality, curtail costs, and bolster patient safety.
TeamSTEPPS model
TeamSTEPPS, which stands for Team Strategies and Tools to Enhance Performance and Patient Safety, is a teamwork and communication model designed explicitly for healthcare settings (4). Developed by the U.S. Department of Defense and the Agency for Healthcare Research and Quality (AHRQ), TeamSTEPPS focuses on improving patient safety by enhancing team collaboration, communication, and decision-making among healthcare professionals (4).
One key element of TeamSTEPPS is using structured communication techniques to prevent errors and misunderstandings. For instance, during patient handoffs from one healthcare provider to another, TeamSTEPPS emphasizes using a structured tool like SBAR (Situation, Background, Assessment, Recommendation) to convey critical information succinctly and accurately. This ensures that essential patient details are noticed, reducing the risk of adverse events (18).
In a surgical team scenario, TeamSTEPPS principles can be applied to improve teamwork and communication among surgeons, nurses, and anesthesiologists. The model encourages briefings before procedures to set clear objectives, huddles during surgery to address emerging issues, and debriefings afterward to reflect on the process and identify areas for improvement. By fostering a culture of open communication and mutual respect, TeamSTEPPS contributes to safer, more efficient healthcare delivery (4).


Self Quiz
Ask yourself...
- How can healthcare organizations determine which QI model suits their specific challenges or improvement goals?
- How do QI models emphasize data collection and analysis, and why is this critical in healthcare?
- Can you imagine a real-world scenario where the Lean Six Sigma framework can successfully improve healthcare processes and outcomes?
- What are some emerging trends or innovations in QI models and methodologies, and how might they shape the future of healthcare quality improvement?
IOM Six Domains of Patient Care
The Institute of Medicine (IOM), now known as the National Academy of Medicine, introduced the Six Domains of Quality in Healthcare as a framework to assess and improve the quality of patient care (14). These domains, introduced in 2001, encompass various aspects of care delivery and patient experience, helping healthcare organizations and providers identify areas for improvement (14). The domains serve as pillars for assessing the different dimensions of care delivery, ensuring that healthcare organizations and providers address the holistic needs of patients (14).
Definitions
The Six Domains of Patient Care are essential for providing high-quality healthcare. See definitions of each of the IOM's six domains of patient care below.
- Safe: Safety is the foundational domain, emphasizing the importance of reducing the risk of patient harm. This includes preventing medical errors, preventing infections, and ensuring the safe administration of medications. Healthcare organizations implement safety protocols and engage in continuous monitoring to minimize risks (14).
- Effective: Effective care ensures that patients receive evidence-based treatments and interventions that result in the desired outcomes. It involves using the best available scientific knowledge to make informed decisions about patient care avoiding unnecessary or ineffective treatments (14).
- Patient-Centered: Patient-centered care focuses on individualizing healthcare to meet each patient's unique needs and preferences. It involves respecting patients' values and preferences, engaging them in shared decision-making, and delivering care with empathy and compassion (14).
- Timely: Timely care emphasizes reducing delays in healthcare delivery. It includes providing care promptly and avoiding unnecessary waiting times for appointments, tests, and treatments. Timely care is especially critical in emergencies (14).
- Efficient: Efficiency in healthcare means maximizing resource utilization and minimizing waste while providing high-quality care. This domain emphasizes streamlining processes, reducing unnecessary costs, and optimizing healthcare resources (14).
- Equitable: Equitable care underscores the importance of providing healthcare that is fair and just, regardless of a patient's background, socioeconomic status, or other factors. It aims to eliminate healthcare access and outcomes disparities among different patient populations (14).
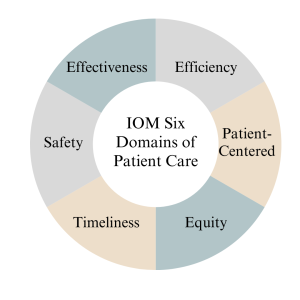
Measures
Measures in the context of the Institute of Medicine (IOM) six domains of patient care refer to the metrics and indicators used to assess and evaluate the quality of care provided in each domain. According to (14), the measures below are essential for monitoring and improving healthcare services. See details below.
- The "Safe" domain measures focus on tracking and reducing adverse events and medical errors. Key indicators include rates of medication errors, hospital-acquired infections, falls, and complications from procedures. Safety measures also assess the implementation of safety protocols, such as hand hygiene compliance and patient identification bracelets.
- Measures in the "Effective" domain assess how evidence-based practices and treatments are utilized. These measures include adherence to clinical guidelines, appropriate use of medications, and the success rates of medical interventions. Additionally, outcomes such as patient recovery, remission, or improvement are indicators of the effectiveness of care.
- The "Patient-Centered" domain focuses on assessing the patient’s experience and satisfaction with care. Patient surveys and feedback are standard measures, evaluating aspects like communication with healthcare providers, involvement in decision-making, and overall satisfaction with the care received. Healthcare organizations also measure shared decision-making and respect for patient preferences.
- Measures related to the "Timely" domain evaluate the efficiency of healthcare delivery. Key metrics include waiting times for appointments, diagnostic tests, and procedures. Additionally, measures track the timely delivery of urgent care and the avoidance of unnecessary delays in treatment.
- Efficiency measures aim to quantify resource utilization and the reduction of waste in healthcare. Metrics may include the cost of care per patient, length of hospital stays, and resource allocation efficiency. Improvement in resource utilization and cost-effectiveness are vital indicators of efficiency.
- Measures within the "Equitable" domain assess disparities in healthcare access and outcomes among different patient populations. Healthcare utilization and outcomes data are stratified by demographics, socioeconomic status, race, and ethnicity to identify and address inequities. Key indicators include access to preventive care, healthcare utilization rates, and health outcomes across various demographic groups.

Self Quiz
Ask yourself...
- How can healthcare providers ensure their care aligns with patients' values, preferences, and cultural backgrounds?
- What challenges might patients face in accessing healthcare services, and how can healthcare organizations improve access for all patients?
- What are the potential consequences of poor care coordination among healthcare providers, and how can interdisciplinary teams work together to enhance coordination?
- Why must healthcare organizations continually assess and improve the quality of care they provide, and what mechanisms can be implemented to support ongoing improvement efforts?
Nursing Quality Indicators
According to (5), nursing quality indicators are essential metrics used to evaluate and improve the quality of nursing care in healthcare settings. These indicators provide valuable insights into nursing practice and patient outcomes, helping healthcare organizations and nursing staff deliver safe, effective, patient-centered care. Let's delve into some key nursing quality indicators and their significance below.
Patient Falls
Patient falls are a critical quality indicator in nursing care since they can result in severe injuries and complications for patients (5). As a result, healthcare organizations measure and monitor the rate of patient falls to identify trends and implement preventive measures.
For example, when a hospital notices an increase in the rate of falls among elderly patients in a particular unit, they may introduce interventions such as nonslip flooring, improved lighting, and patient education as fall prevention strategies to reduce the incidence of falls.

Medication Administration Errors
Ensuring accurate medication administration is crucial in nursing practice because medication errors can lead to adverse events, including patient harm or death (5). Nursing quality indicators related to medication administration errors include the rate of medication errors and adherence to medication reconciliation processes (5). For instance, nurses are encouraged to verify patient allergies and cross-check medication orders to prevent errors. If there is an increase in medication errors in a healthcare facility, it may prompt a review of medication administration protocols and additional staff training.

Pressure Ulcers (Bedsores)
Pressure ulcers are a quality indicator of patient skin integrity since they develop when patients remain immobile for extended periods (5). As a result, healthcare organizations measure the incidence and prevalence of pressure ulcers as an indicator of the quality of nursing care (5).
Patient Satisfaction
Patient satisfaction is a patient-centered nursing quality indicator since it reflects the overall patient experience and perception of care (5). Surveys and feedback mechanisms are used to measure patient satisfaction. For example, a scenario might involve patients receiving post-discharge surveys that assess various aspects of their hospital experience, including nurse responsiveness, communication, and pain management. Healthcare organizations can use this feedback to identify areas for improvement and enhance patient-centered care.
In summary, nursing quality indicators encompass a range of metrics that evaluate nursing care quality, patient safety, and patient experiences. By monitoring and responding to these indicators, healthcare organizations and nursing staff can continuously improve their quality of care, leading to better outcomes and increased patient satisfaction (5).

Self Quiz
Ask yourself...
- Why is data collection critical in nursing quality improvement efforts?
- What types of data should nurses prioritize collecting to assess patient safety?
- How can nurses ensure the accuracy and reliability of the data they collect for quality improvement purposes?
- What challenges might nurse face when collecting patient-related data, and how can these challenges be overcome?
Data Collection
Quality improvement data collection is a critical component of healthcare quality initiatives, providing the necessary information to assess the current state of care, identify areas for improvement, and monitor progress over time (2). Accurate and meaningful data collection enables healthcare organizations to make informed decisions, implement evidence-based interventions, and ultimately enhance patient outcomes. Let's explore the methods of data collection below.
- Clinical Outcome Collection: Clinical outcome data collection is essential for assessing the effectiveness of healthcare interventions (2). For example, consider a scenario where a hospital is implementing a quality improvement project to reduce surgical site infections (SSIs) following orthopedic surgeries. Data collection would involve tracking the number of SSIs occurring over a specific period and collecting information on patient characteristics, surgical techniques, and post-operative care protocols. By analyzing this data, the healthcare team can identify trends, risk factors, and areas for improvement, ultimately leading to targeted interventions to reduce SSIs.
- Patient Satisfaction Survey Data Collection: Patient satisfaction surveys are valuable tools for collecting data on patient experience (2). A primary care clinic that aims to improve patient satisfaction may administer surveys to patients after each visit, asking about aspects of care such as communication with healthcare providers, wait times, and overall experience. The collected data can reveal areas of strength and areas requiring improvement. For instance, if survey results consistently indicate longer-than-desired wait times, the clinic can adjust scheduling practices or implement strategies to reduce wait times and enhance patient satisfaction.
- Process Measures Data Collection: Process measure data collection focuses on evaluating the efficiency and effectiveness of healthcare processes (2). For instance, in a medication reconciliation scenario, a healthcare organization might collect data on the accuracy and completeness of medication lists during care transitions. By tracking the frequency of medication reconciliation discrepancies, they can identify process inefficiencies and implement standardized protocols for reconciliation, leading to safer care transitions and reduced medication errors.
- Adverse Event Reporting Data Collection: Adverse event reporting is a crucial mechanism for collecting data on incidents that result in patient harm or near misses (2). For example, consider a scenario where a nurse administers the wrong medication dose to a patient but catches the error before any harm occurs. Reporting this near-miss event allows the healthcare organization to investigate the root causes, implement preventive measures, and share lessons learned with the care team to prevent similar incidents in the future.
Types of Data
Data types play a crucial role in understanding the current state of care, identifying areas for improvement, and implementing evidence-based interventions (2). Let’s explore the different types of data used in quality improvement below.
- Quantitative Data: Quantitative data involves numerical measurements and is particularly useful for assessing the frequency and extent of specific events or outcomes (2). For instance, in a hospital's quality improvement project focused on reducing hospital-acquired infections, the team collects quantitative data on the number of infections over time, allowing them to track trends and measure the impact of interventions, such as hand hygiene protocols or disinfection practices.
- Qualitative Data: Qualitative data provides insights into the "why" and "how" behind healthcare processes and patient experiences (2). This data type is collected through interviews, focus groups, and open-ended surveys. For example, in a primary care setting aiming to improve patient satisfaction, qualitative data may be collected through patient interviews to gather in-depth information about their perceptions of care. Qualitative data can uncover nuances and provide valuable context to complement quantitative findings (2).
- Patient-Reported Data: Patient-reported data includes information directly provided by patients about their health, symptoms, experiences, and preferences. Patient-reported outcome measures (PROMs) and patient-reported experience measures (PREMs) are standard data collection tools. In a scenario involving chronic disease management, patients with diabetes may be asked to complete a PROM assessing their quality of life and symptom management. This data helps healthcare providers tailor care plans to individual patient needs and preferences (2).
- Process Data: Process data track the steps and activities involved in healthcare delivery to help assess the efficiency and effectiveness of care processes. For example, in a surgical quality improvement initiative, process data may include the time from patient admission to surgery, surgical team checklist completion, and adherence to anesthesia protocols. By collecting and analyzing process data, healthcare organizations can identify bottlenecks and areas for improvement in care delivery processes.
In summary, quality improvement data collection relies on various data types, including quantitative, qualitative, patient-reported, and processed data. Each data type contributes to a comprehensive understanding of healthcare quality and supports evidence-based decision-making to enhance patient care and outcomes.

Identification Stage
The identification stage for quality improvement data collection is a critical initial phase where healthcare organizations and teams define what data to collect, why it is relevant, and how it aligns with their quality improvement goals (23). This stage is essential for ensuring meaningful data collection efforts will lead to actionable insights. Let's explore the identification stage in more detail.
- Defining Objectives and Goals: During this stage, healthcare organizations must clearly define the objectives and goals of their quality improvement initiative (23). For instance, a hospital aiming to reduce readmission rates for heart failure patients may set a specific goal of reducing readmissions by 20% within the following year.
- Selecting Relevant Metrics: Identifying the right metrics and data points is crucial, and organizations should choose metrics that directly relate to their quality improvement goals (23). Continuing with the example of reducing heart failure readmissions, relevant metrics might include the number of heart failure patients readmitted within 30 days, the reasons for readmission, and patient characteristics. By selecting these metrics, the organization ensures that data collection efforts are aligned with their specific improvement goal.
- Determining Data Sources: Healthcare organizations must identify where the necessary data will be sourced (23). This may involve looking at electronic health records, claims data, patient surveys, or other sources. For instance, to collect data on heart failure readmissions, the hospital may extract relevant information from electronic health records, including admission and discharge dates, diagnosis codes, and patient demographics.
- Creating Data Collection Protocols: Establishing clear data collection protocols is essential for consistency and reliability (23). Healthcare teams should define how data will be collected, who will be responsible for data collection, and the frequency of data collection. For example, in a hospital project aiming to improve hand hygiene compliance, data collection protocols might specify that trained observers will monitor hand hygiene practices at random intervals and record their findings on standardized forms.
By carefully navigating the identification stage, healthcare organizations ensure that their quality improvement data collection efforts are purposeful and aligned with their goals. This sets the stage for collecting meaningful data to drive evidence-based decisions and interventions to enhance healthcare quality.
Gathering Stage
The gathering stage of quality improvement data collection is crucial for healthcare organizations to collect the identified data based on their quality improvement objectives and goals (23). This stage involves systematically collecting data from various sources and often requires careful planning and coordination to ensure data accuracy and completeness. Let's delve into the gathering stage in detail below.
- Data Collection Methods: To gather data, healthcare organizations must determine the most suitable methods for collecting the identified data, which may involve a combination of electronic health records, patient surveys, direct observations, and administrative databases (23). For example, in a quality improvement project aimed at reducing hospital readmissions, data may be collected by reviewing electronic health records to track patient outcomes, conducting patient surveys to gather feedback on discharge instructions, and analyzing administrative data to identify trends in readmission rates.
- Ensuring Data Accuracy and Consistency: Data accuracy is critical in the gathering stage, and organizations must implement procedures to collect data consistently and without errors (23). For instance, if a healthcare facility is collecting data on medication administration, nurses may use standardized protocols to accurately record medication administration times and doses. Regular training and quality checks may also be implemented to maintain data accuracy.
- Timely Data Collection: Timeliness is another important aspect of the gathering stage, and data should be collected promptly to ensure it is current and relevant for analysis and decision-making (23). In a scenario involving tracking patient outcomes, healthcare teams may set specific intervals for data collection, such as collecting post-surgical complication data daily or weekly, depending on the project's requirements.
- Data Security and Privacy: Protecting patient data is a paramount concern in healthcare. As a result, healthcare organizations must adhere to strict privacy and security protocols during the gathering stage to ensure that patient information is handled confidentially and complies with applicable laws and regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) (23). For example, when collecting patient-reported data, organizations may anonymize responses to protect patient identities and comply with privacy regulations.
By effectively managing the gathering stage, healthcare organizations can ensure that they collect accurate, timely, and secure data that will serve as the foundation for subsequent analysis and quality improvement efforts.
Analysis stage
The analysis stage for quality improvement data collection is a critical phase where collected data is processed, examined, and transformed into actionable insights. This stage involves various analytical techniques and tools to identify patterns, trends, and areas for improvement (2). Let's explore the analysis stage in detail below.
- Descriptive Analysis: Descriptive analysis is the initial step in data analysis, focusing on summarizing and presenting data meaningfully (2). For example, in a quality improvement project aimed at reducing patient wait times in an emergency department, an analysis may involve calculating and displaying key statistics, such as average wait times, 95th percentile wait times, and the distribution of wait times (2). These descriptive statistics provide an overview of the current situation and help identify areas that need attention.
- Root Cause Analysis (RCA): Root cause analysis is a critical aspect of the analysis stage, as it helps pinpoint the underlying causes of issues or problems (2). In our scenario, if the analysis reveals prolonged wait times in the emergency department, RCA may involve a thorough investigation into the factors contributing to the delays. Potential root causes include staffing shortages, inefficient triage processes, or bottlenecks in diagnostic testing. Identifying these root causes is essential for developing effective interventions.
- Statistical Analysis: Statistical analysis plays a vital role in quality improvement by examining the relationships between variables and testing hypotheses (2). In reducing hospital readmissions, statistical analysis may be used to identify factors associated with readmission risk. For example, healthcare teams can use logistic regression to analyze patient data to determine which variables, such as comorbidities or medication adherence, are statistically significant predictors of readmission risk. This information can guide the development of targeted interventions for at-risk patients.
- Benchmarking: Benchmarking involves comparing an organization's performance data with industry standards or best practices to identify performance gaps (2). When a hospital is looking to improve patient satisfaction, benchmarking may involve comparing its patient satisfaction scores to those of similar hospitals or national averages. Identifying areas where the hospital falls behind benchmarks can inform strategies for improvement, such as implementing best practices from higher-performing institutions.
The analysis stage is critical for transforming raw data into actionable insights and understanding healthcare quality factors (2). Through descriptive analysis, root cause analysis, statistical techniques, and benchmarking, healthcare organizations can gain valuable insights that drive evidence-based decisions and interventions to improve care quality (6).
Benchmarking
The benchmarking stage in quality improvement data collection is a crucial phase where healthcare organizations compare their performance against established benchmarks or best practices (1). This gives healthcare organizations a clear understanding of their position relative to recognized standards and allows them to effectively identify areas for improvement, prioritize, and focus their improvement efforts (5). Let's delve into the benchmarking stage in detail below.
- Defining Benchmarks: In the benchmarking stage, healthcare organizations must define the benchmarks or standards against which they will measure their performance. These benchmarks can be internal (comparing current performance to historical data) or external (comparing to industry standards, best practices, or similar organizations) (1). For example, a primary care clinic seeking to improve appointment scheduling efficiency may choose to benchmark its appointment wait times against industry benchmarks for acceptable wait times.
- Collecting Comparative Data: Gathering data that allows for a meaningful comparison is critical in benchmarking, so healthcare organizations must collect data from relevant sources to measure their performance against the chosen benchmarks (1). Continuing with the appointment scheduling example, the clinic may collect data on the time it takes to schedule an appointment, the number of scheduling errors, and patient feedback. This data is then compared to industry benchmarks or best practices.
- Identifying Performance Gaps: The benchmarking process reveals gaps or disparities between an organization's performance and the benchmarks to highlight improvement areas (1). For instance, if the clinic discovers that its appointment wait times are significantly longer than industry benchmarks, this identifies a performance gap that needs to be addressed to enhance patient access and satisfaction.
- Developing Improvement Strategies: Healthcare organizations can develop targeted improvement strategies once performance gaps are identified. These strategies are based on evidence from the benchmarking process and aim to align performance with or exceed established benchmarks (1). In our scenario, the clinic may implement strategies such as optimizing appointment scheduling processes, enhancing staff training, or using technology to improve scheduling efficiency.


Self Quiz
Ask yourself...
- Why is data collection a crucial step in the quality improvement process?
- What types of data are typically collected during the data collection stage of quality improvement?
- How do you determine which data points are relevant to your quality improvement project?
- What methods and tools can be used to collect data accurately and efficiently?
Change Models in Healthcare
Change models are essential frameworks used in healthcare, including nursing, to guide and manage the effective implementation of quality improvement initiatives (15). These models offer structured approaches to initiate, plan, execute, and sustain changes in healthcare practice (15). Let’s discuss some prominent change models used in nursing quality improvement below.
- Kotter's 8-Step Change Model: Developed by Dr. John Kotter, this model emphasizes the importance of creating a sense of urgency, building a guiding coalition, and sustaining the change (15). For instance, in a nursing scenario focused on reducing hospital-acquired infections, the 8-step model would involve creating urgency by highlighting the impact of infections on patient safety, assembling a coalition of nurses and infection control specialists, and sustaining change by monitoring infection rates over time and continually reinforcing hygiene protocols.
- Lewin's Change Management Model: Lewin's model consists of three stages: unfreezing, changing, and refreezing (15). Let's consider implementing a new electronic health record (EHR) system in nursing. Nurses first "unfreeze" by acknowledging the need for a new system and undergoing training. Then, they "change" by adopting the EHR and adjusting workflows. Finally, they "refreeze" by becoming proficient and maintaining the new system's use as a standard practice.
- PDSA Cycle (Plan-Do-Study-Act): This model emphasizes iterative cycles of planning, implementing, observing, and adjusting (15). For instance, if a nursing unit aims to improve patient handoffs, they might "plan" by identifying handoff best practices, "do" by implementing changes, "study" by assessing the impact on patient outcomes, and "act" by making further refinements based on their findings. This continuous cycle allows for gradual, data-driven improvements.
- ADKAR Model: The ADKAR model focuses on individual change management, and this could apply to a scenario where nurses are adopting new pain management protocols (15). Nurses would first need awareness of the change (A), followed by desire (D) to participate, knowledge (K) of how to implement the new protocols, ability (A) to do so, and reinforcement (R) to sustain the change over time.
In summary, change models provide structured approaches to drive quality improvement initiatives in nursing, and by applying these models, nurses and healthcare organizations can systematically plan, implement, and evaluate changes to enhance patient care, safety, and outcomes (15).

Self Quiz
Ask yourself...
- Why are change models essential in nursing quality improvement initiatives?
- What is the primary purpose of creating a sense of urgency in change models like Kotter's 8-Step model?
- How does Lewin's Change Management Model address the need to "unfreeze" existing practices in nursing before implementing change?
- Why is individual change management crucial in nursing practice, as the ADKAR model emphasizes?
Implementing Change
Implementing changes for quality improvement in nursing is a multifaceted process that requires careful planning, effective communication, and the engagement of healthcare professionals at all levels. According to (15), successful implementation ensures that desired changes are integrated into daily nursing practice, improving patient outcomes. Let’s explore key strategies and considerations for implementing changes in nursing quality improvement below.
- Engage Interdisciplinary Teams: According to (15), collaborative engagement is crucial when implementing changes in nursing practice, and healthcare organizations should assemble interdisciplinary teams that include nurses, physicians, administrators, and other stakeholders. For example, in a scenario involving the adoption of a new pain management protocol, nurses can collaborate with physicians to ensure the consistent application of evidence-based pain management practices. This team approach facilitates a shared understanding of the change and fosters buy-in from all parties.
- Effective Communication: Clear and consistent communication is essential during the implementation phase, so nurses should communicate the rationale behind the change, its expected benefits, and the specific steps involved (15). For example, suppose a hospital is transitioning to a new electronic health record system. In that case, nurses can attend training sessions to understand its features and communicate effectively with patients about how it will enhance their care. This ensures that all stakeholders are informed and can adapt to the change seamlessly.
- Training and Education: Providing adequate training and education is critical to equip nursing staff with the knowledge and skills to implement the change effectively (15). In the case of introducing a new wound care protocol, nurses would require training on the updated practices, wound assessment techniques, and the use of new wound care products. In addition to initial training, ongoing education would ensure that nursing staff stay current with best practices to provide quality care confidently.
- Continuous Monitoring and Feedback: According to (15), implementing change is an ongoing process that requires constant monitoring and feedback since feedback mechanisms allow for adjustments and refinements to the change process. As a result, nursing quality improvement initiatives benefit from the regular collection and analysis of data to assess the impact of the change. For example, suppose a hospital introduces a sepsis screening tool. In that case, nurses can track the number of patients screened, identify missed cases, and evaluate whether early interventions have reduced sepsis-related mortality rates. By engaging interdisciplinary teams, fostering effective communication, providing training and education, and implementing continuous monitoring and feedback mechanisms, nurses can successfully implement changes that improve the quality of patient care and enhance overall healthcare outcomes (8).

Self Quiz
Ask yourself...
- Why is it crucial for nursing teams to engage in interdisciplinary collaboration when implementing changes for quality improvement?
- How can effective communication strategies help nursing staff understand the purpose and benefits of a proposed change in healthcare practice?
- What role does ongoing training and education play in ensuring that nursing staff are well-prepared to implement and sustain changes in their practice?
- What methods can be employed to gather feedback from nursing staff while implementing a new practice or protocol?
Evaluating Change
Evaluating change for quality improvement in nursing is a critical phase that involves assessing the impact and effectiveness of implemented changes on patient care outcomes, safety, and the overall quality of healthcare services. According to (15), rigorous evaluation ensures that improvements are sustained, and necessary adjustments are made. Let’s explore key strategies and considerations for evaluating changes in nursing quality improvement below.
- Establishing Clear Evaluation Metrics: To evaluate change effectively, it is essential to define clear and measurable evaluation metrics, and according to (15), these metrics should align with the specific objectives of the change initiative. For example, suppose a nursing unit has introduced a new hand hygiene protocol to reduce hospital-acquired infections. In that case, evaluation metrics may include the number of infections before and after the change, adherence to hand hygiene guidelines, and patient satisfaction scores related to cleanliness and infection prevention.
- Data Collection and Analysis: Data collection is a fundamental component of the evaluation process, and nursing teams should collect relevant data using standardized methods and tools (15). In our scenario, data on infection rates can be collected regularly, and statistical analysis can be performed to determine whether the change has had a statistically significant impact. Nurses can then use run charts or control charts to visualize trends in infection rates over time, allowing for early detection of any potential issues.
- Patient and Staff Feedback: Patient and nursing staff feedback is invaluable in evaluating change since patients' perspectives on the quality of care and their experiences following the change can provide insights into the initiative's effectiveness (15). Additionally, nursing staff can provide feedback on the practicality and feasibility of the new practices. For instance, nursing staff may suggest further improvements in infection control procedures.
- Sustainability and Continuous Improvement: Evaluating change is not solely about assessing immediate outcomes but also ensuring sustainability and continuous improvement. According to (15), nursing teams should determine whether the positive effects of the change are maintained over time and whether there is room for further refinement. For example, when a nursing unit has reduced infection rates, regular audits and monitoring should continue to ensure sustained compliance with hygiene protocols.

Self Quiz
Ask yourself...
- Why must nursing teams establish clear and measurable evaluation metrics when assessing the impact of change in healthcare practice?
- How can nurses effectively collect and analyze data to evaluate the success of a change in their nursing practice?
- What role does patient feedback play in evaluating the impact of a change on the quality of nursing care, and how can this feedback be gathered and utilized?
- How can nursing staff engage in ongoing self-assessment to determine their practice changes' effectiveness and identify improvement areas?
- What specific infection prevention measures should nurses prioritize in their daily practice to reduce hospital-acquired infections, and why are these measures effective?
- What are the primary goals of a quality improvement project to reduce hospital-acquired infections, and how can nursing staff contribute to achieving these goals?
- Why is continuous monitoring and evaluation crucial in quality improvement projects, and how can nursing staff use data to drive ongoing improvements in patient care quality?

Self Quiz
Ask yourself...
- What specific infection prevention measures should nurses prioritize in their daily practice to reduce hospital-acquired infections, and why are these measures effective?
- What are the primary goals of a quality improvement project to reduce hospital-acquired infections, and how can nursing staff contribute to achieving these goals?
- Why is continuous monitoring and evaluation crucial in quality improvement projects, and how can nursing staff use data to drive ongoing improvements in patient care quality?
- Enhancing Medication Safety: Medication errors can have severe consequences for patients (6). A quality improvement project may target medication safety by introducing barcode scanning systems for medication administration, implementing double-check procedures for high-risk medications, and providing ongoing training to nursing staff. The project's effectiveness can be assessed by monitoring the number of medication errors reported and verifying that the new safety measures reduce the occurrence of such errors. For example, a nursing team could reduce the incidence of wrong-patient medication administration by implementing barcode scanning during medication administration.

Self Quiz
Ask yourself...
- How can nurses ensure that barcode scanning systems and double-check procedures are effectively integrated into their daily workflow in medication safety improvement projects?
- What potential challenges and barriers can nurse units encounter when implementing medication safety improvements, and how can these challenges be addressed?
- Improving Nurse-to-Patient Ratios: Adequate nurse staffing levels are crucial for patient safety and quality of care (6). A quality improvement project may involve adjusting nurse-to-patient ratios based on patient acuity levels, introducing workload management tools, and conducting regular staffing needs assessments. In this case, the project's success can be measured by tracking patient outcomes, nurse workload, and patient satisfaction scores. For example, a nursing unit could reduce nurse burnout and improve patient care by optimizing staffing ratios during peak hours.

Self Quiz
Ask yourself...
- Why is it important to regularly assess and adjust nurse-to-patient ratios in a healthcare setting, and what strategies can nurse leaders employ to optimize staffing levels?
- In a quality improvement project focused on nurse-to-patient ratios, what key factors should nurse leaders consider when determining staffing needs during different shifts and patient acuity levels?
- Enhancing Discharge Planning and Care Transitions: Effective care transitions from the hospital to home or other healthcare settings are essential to preventing readmissions and ensuring continuity of care (6). A quality improvement project may focus on improving the discharge planning process, including patient education, medication reconciliation, and post-discharge follow-up. Success can be assessed by monitoring readmission rates and patient-reported experiences. For example, a nursing team could work on reducing hospital readmissions by ensuring that patients receive thorough discharge instructions and have access to follow-up care.

Self Quiz
Ask yourself...
- What steps can nurse teams take to enhance the discharge planning process and ensure seamless care transitions for patients moving from the hospital to home care?
- What strategies can nurse teams employ to ensure that patient education during discharge planning is effective and leads to better patient outcomes and satisfaction?
The above examples illustrate the diverse range of quality improvement projects in nursing, each addressing specific challenges to enhance patient safety and care quality.

Self Quiz
Ask yourself...
- Why is continuous monitoring and evaluation crucial in quality improvement projects, and how can nursing staff use data to drive ongoing improvements in patient care quality?
- What are the primary goals and objectives of QI models, and how do they contribute to the overall quality of healthcare?
Conclusion
In conclusion, this course provides essential knowledge and skills valuable for nurses aiming to deliver high-quality, safe, patient-centered care. Quality improvement in nursing is not merely a theoretical concept but a practical approach that can be applied to various aspects of healthcare, and one critical aspect to remember is the importance of interdisciplinary collaboration. As frontline caregivers, nurses must collaborate with physicians, administrators, pharmacists, and other healthcare professionals to drive improvements in healthcare delivery.
As nurses continue to play a pivotal role in healthcare delivery, the knowledge and skills gained from this course will empower them to lead and actively participate in quality improvement initiatives. By applying quality improvement principles, nurses can contribute to better patient experiences, patient outcomes, and overall healthcare quality.
Final Reflection Questions
- What have you learned from this course?
- Why is interdisciplinary collaboration essential for nurses to effectively implement quality improvement initiatives in healthcare settings, and how can nurses foster collaboration among healthcare professionals?
- How does the concept of continuous learning and adaptation align with the dynamic nature of healthcare, and what strategies can nurses employ to stay current with evolving best practices and guidelines?
- In what ways does Quality Improvement benefit both healthcare providers and patients?
- What are the potential challenges in implementing QI initiatives in a healthcare organization?
- In what ways has QI in healthcare become intertwined with the broader goals of healthcare reform, such as improving patient outcomes and reducing healthcare costs?
- What role does leadership play in the effective implementation of QI models?
- How can leaders promote a culture of continuous improvement within healthcare organizations?
- How do QI models facilitate interdisciplinary collaboration among healthcare professionals to drive improvements in patient care?
- What challenges might healthcare organizations face when attempting to adopt and sustain QI models, and how can these challenges be overcome?
- How does the "testing and learning" concept in the PDSA cycle align with the principles of evidence-based practice in healthcare?
- In what ways do QI models promote patient-centered care and patient safety, and can you provide examples of tangible improvements in these areas achieved through QI initiatives?
- How can the Six Sigma model contribute to the reliability and consistency of healthcare processes?
- Safe: What steps can healthcare organizations take to minimize the risk of medical errors and adverse events?
- Practical: How do healthcare providers ensure that evidence-based treatments and interventions lead to positive patient outcomes?
- Patient-centered: Why is it important to involve patients in their care decisions, and how can healthcare professionals effectively engage patients in the decision-making process?
- Timely: What are some key factors contributing to delays in healthcare delivery, and how can these delays be reduced to improve timeliness?
- Efficient: How can healthcare processes and workflows be streamlined to enhance efficiency and reduce waste?
- Equitable: What are some barriers to achieving healthcare equity, and how can healthcare organizations address these disparities?
- How can nurses actively involve patients in data collection to enhance patient-centered care?
- What tools or technologies are available to streamline data collection processes in nursing practice?
- How can nurses effectively collaborate with interdisciplinary teams to gather comprehensive data for quality improvement initiatives?
- What strategies can nurses employ to maintain patient privacy and confidentiality while collecting sensitive healthcare data?
- What methods can nurse use to analyze and interpret the data they collect to identify areas for improvement?
- Why must nurses regularly review and assess the data they collect to drive continuous quality improvement in healthcare settings?
- Regarding patient falls, what strategies can healthcare organizations implement to reduce the incidence of patient falls, and how can nursing staff actively contribute to fall prevention efforts?
- How can nurses ensure the accurate and safe administration of medications, and what measures can be taken to minimize medication errors?
- What are the key nursing practices and interventions that can prevent the development of pressure ulcers in hospitalized patients, and how can nursing staff collaborate to achieve this goal?
- Why is patient satisfaction an important nursing quality indicator, and what actions can nurses take to enhance the overall patient experience?
- What impact do nurse-to-patient staffing ratios have on the quality of nursing care, and how can healthcare organizations ensure safe nurse staffing levels?
- How can nurses enhance patient education to promote better understanding and self-management of their health conditions?
- How can you ensure that the data collected is reliable and valid?
- What role does standardization play in data collection for quality improvement?
- How can you establish baseline data for comparison in your quality improvement project?
- What challenges or obstacles might you encounter when collecting data for quality improvement?
- How frequently should data be collected to monitor progress in a quality improvement project?
- How can you involve frontline staff in the data collection to ensure accuracy?
- What measures can be taken to protect patient privacy and confidentiality during data collection?
- How can you analyze the data collected to identify trends or patterns?
- What actions should be taken if the data collected indicates a problem or deviation from the desired outcome?
- What strategies can ensure that data collection remains an ongoing and sustainable practice in healthcare quality improvement efforts?
- What are the potential challenges or resistance nurses might encounter when implementing changes using these models?
- How can a guiding coalition or interdisciplinary team be effectively assembled to support nursing quality improvement efforts?
- What strategies can nurses employ to sustain changes and prevent reverting to previous practices once implemented?
- How can nursing leaders ensure that staff have the necessary knowledge and skills to embrace the changes outlined in these models?
- How can nurses use these change models to promote a culture of continuous improvement in healthcare settings?
- How can nurses ensure their implementation changes align with evidence-based best practices and clinical guidelines?
- What potential challenges or barriers might nurse teams encounter when trying to implement changes for quality improvement?
- What strategies can address resistance to change among nursing staff and promote their active participation in the implementation process?
- How can nursing leaders effectively communicate the expected outcomes and benefits of the change to gain support and commitment from their teams?
- What are the advantages of using data and performance metrics to monitor the progress and impact of change implementation in nursing practice?
- How can nursing staff ensure that changes are sustained and become integral to their daily practice rather than temporary modifications?
- Why is it crucial to consider the sustainability of change when evaluating its long-term impact on nursing quality improvement?
- What challenges or obstacles might nurse teams encounter when collecting and analyzing data for change evaluation, and how can these challenges be addressed?
- How can nursing leaders encourage a culture of continuous improvement among their teams as part of the change evaluation process?
- What strategies can be employed to ensure that the feedback and insights gathered during the evaluation phase are actively used to refine and optimize nursing practices?
- What are the potential consequences of not conducting thorough and systematic evaluations of changes in nursing practice for quality improvement?
- How can nursing staff and healthcare organizations ensure that the lessons learned from change evaluations are applied to future improvement initiatives to enhance patient care outcomes?
Workplace Violence Against Nurses
Introduction
The role of the registered nurse, while fundamentally dedicated to the care and wellbeing of patients, has long been fraught with challenges that extend beyond the complexities of medical care. One such pressing concern is workplace violence, an issue that nurses confront with alarming frequency. Recent statistics show that healthcare workers, particularly nurses, are at a higher risk for workplace violence compared to other professions.
Given the vital role nurses play in patient care and the broader healthcare system, it is imperative to understand the scope, sources, and solutions to this pressing issue. This continuing education course is dedicated to arming nurses with the knowledge, tools, and strategies to recognize, respond to, and prevent incidents of workplace violence, thereby ensuring their safety and the uninterrupted provision of quality care.
Introduction
The role of the registered nurse, while fundamentally dedicated to the care and wellbeing of patients, has long been fraught with challenges that extend beyond the complexities of medical care. One such pressing concern is workplace violence, an issue that nurses confront with alarming frequency. Recent statistics show that healthcare workers, particularly nurses, are at a higher risk for workplace violence compared to other professions.
Given the vital role nurses play in patient care and the broader healthcare system, it is imperative to understand the scope, sources, and solutions to this pressing issue. This continuing education course is dedicated to arming nurses with the knowledge, tools, and strategies to recognize, respond to, and prevent incidents of workplace violence, thereby ensuring their safety and the uninterrupted provision of quality care.
Workplace Violence
Definitions
The Occupational and Safety Health Administration (OSHA) (3) defines workplace violence (WPV for the purpose of this course) as any act or threat of physical violence, harassment, intimidation, or other threatening, disruptive behavior that occurs at the work site. This can also include verbal, written, or acts of sabotage against an individual while they are at work.
Workplace violence crosses all demographic barriers and is indiscriminate in who it can and does affect. Even seeing workplace violence influences morale, attendance, and the overall well-being of employees and their co-workers.
Types of Violence
Currently, there are four categories of workplace violence according to the American Nurses Association (5).
1: Criminal Intent - normally involves theft from the business or employees.
Example: Carol is working on documentation and notices a person lingering in the hallway. Carol doesn’t really think anything of it, assuming they are family members of one of the patients. Several minutes later, the person exits quickly from the supply room and down the stairs. Carol calls security to let them know, but they can’t locate the individual. After looking through the supply room, they find that several containers of wound dressing supplies are missing.
2: Customer/client/patient - the individual becomes violent with employees while receiving services.
Example: David was updating a family on their father’s critical condition. David could tell the family was upset, but the patient’s son seemed more frustrated than the others. During David’s explanation, the son grabbed David’s clipboard and yelled, “You’re not doing anything! You’re just letting him die!” The son then threw the clipboard at David’s head. David blocked the clipboard with his arm, receiving a rather deep cut as a result. Security became involved, and David had to go to the ER for treatment.
3: Worker on worker - an employee bullies, attacks, or threatens another employee.
Example: Emily was rounding when Dr. G. came onto the floor. This doctor was well known for being difficult to work with, and he always required the nurses to stand behind him in the room while he talked with his patients. Emily had one of Dr. G.’s patients today and was in the room, he asked her if the patient had ambulated. Emily told him they had not, but they planned to before and after lunch. The doctor made an audible sigh and while shaking his head at the patient said, “See…this is what I deal with every day. These nurses can’t get anything right. They’re all useless.”
4: Personal relationship - involves a person who has an interpersonal relationship with the nurse, but no association with the nurse’s employer or the business.
Example: Rebecca was walking to her car after work. Halfway to her car, she noticed an individual leaning against the trunk of her vehicle. Rebecca recognized this person as the someone her friend was currently dating. This person approached Rebecca aggressively and began yelling about gossiping and trying to break their relationship. Rebecca started back toward the building, hoping security was nearby, and was pursued by the female. Eventually, Rebecca made it to the building and got inside. Luckily, the door only opened with an employee badge, and Rebecca was safe. She went ahead to security.
Currently, the customer/client type of workplace violence is the most prominent, especially in healthcare and toward nurses. The American Nurses Association (ANA) reports that OSHA does not require employers to implement workplace violence prevention programs, but it supplies voluntary guidelines and may cite employers for not supplying a workplace free from recognized serious hazards.
Some states have legislated that employers develop a program while most states have advanced laws that amend existing statute for assaults of first responders by adding health care providers / nurses and/or increasing the penalty associated with such behavior. (3)
It is worth noting that since there are, in most cases, no actual requirements for employers to provide safe work environments for nurses, preventing and dealing with WPV proves problematic. It falls on nurses to understand what constitutes WPV, how to manage it, how to cope with it, how to report it, and how to ensure action is taken and a resolution is reached when WPV occurs.

Self Quiz
Ask yourself...
- In the scenarios above, should the employees report these incidents to administration at once?
- How would you describe the earlier scenarios on workplace violence?
- Why is it important to ask how you would find and describe workplace violence?
- Can you provide any examples of workplace violence you have experienced or seen?
Epidemiology
Workplace violence can take many forms, and the possible varieties and scenarios are endless. Regardless of how it manifests, the effects of workplace violence are clear and widespread. It can affect productivity of employees, morale, attendance, turnover rates, quality of work, patient outcomes, and much more.
Workplace violence can affect and involve workers, clients, customers, and visitors. WPV ranges from threats and verbal abuse to physical assaults and even homicide. In 2010, the Bureau of Labor Statistics (BLS) data reported healthcare and social aid workers were the victims of approximately 11,370 assaults by persons; a greater than 13% increase over the number of such assaults reported in 2009 (10). Almost 19% of these assaults occurred in nursing and residential care facilities alone. Unfortunately, many more incidents probably go unreported (5).

Impact on Nurses Well-Being
Workplace violence can take a heavy toll on nurses. These tolls can be emotional, mental, and physical as well as short-term or long-term. The seriousness of these injuries can vary widely ranging from minor upset to permanent injury and in worst cases, even death. (13)
This harm doesn’t stop with the nurse. The effects of workplace violence may also include effects spanning the unit the nurse works on or even the entire facility. Low morale, reduced productivity, lack of trust in employers, and fear of going to work can be results of violent events occurring to even a single co-worker.
Workplace violence can also have a financial effect on nurses and their employers related to lost time at work from injury or callouts, costs of care for treatment related to the incident (physical and/or psychological), or even legal fees. (13)
Given that incidents of workplace violence are rapidly increasing, these impacts are expected to increase as well. It is easy to see how this harm is widespread and can potentially ripple outward into the nurse’s professional and personal life. The stress and harm do not stay at work, and can spread to the nurse’s family, social interactions, and more.

Self Quiz
Ask yourself...
- How far reaching do you think workplace violence is?
- Can you give some examples of how workplace violence has affected you or your co-workers?
- What are some examples of how workplace violence against someone else can affect you or the patients on your unit?
Barriers to Reporting
One way to combat workplace violence is knowledge of its existence, its nature, and its frequency. Unfortunately, there are many factors that either prevent or discourage nurses from coming forward with reports when they are the victims of WPV.
A study presented in a Chinese nursing journal surveyed 325 nurses. Of these nurses, 266 were spread across 165 hospitals, and these hospitals were in 72 cities.
A total of 172 nurses (64.7%) experienced violent incidents during the past year. Of these incidents, 45.5% were reported; and the reporting rate of physical assaults (69.0%) was higher than those of verbal abuse (36.9%), threatening behavior (51.7%), and sexual harassment (60.0%). Formal reporting accounted for 25.4% (15.4% in written form and 10.0% through a computer-assisted reporting system.
Almost half of the nurses (49.6%) said that the hospital had no reporting system, or they were uncertain about the reporting system. For reasons of not reporting, 51.9% of the nurses were unaware of how and what types of violence to report, and 50.6% of the nurses believed that the hospital paid greater attention to patients rather than staff. (7)
Interestingly, almost fifty percent of the nurses surveyed had limited knowledge, if any, of a reporting system available to them, while fifty percent felt the hospital favored the patients over their own employees. Combined with an actual or perceived lack of supervisory support, this encourages an environment where nurses feel powerless to protect themselves or to take proper action when threatened or harmed.
The Minnesota Nurses Association, in August of 2022, published a press release with the results of a nursing survey on the topic of workplace violence. In this survey, ninety-seven percent of the nurses surveyed observed WPV or harassment over the previous two years.
The top reasons cited by nurses who did not report workplace violence were lack of time due to overwork and under-staffing, cited by fifty-eight percent of respondents, and lack of action by hospital management, cited by fifty-three percent of nurses in the survey. (4)
It would appear from these studies that many nurses feel it is futile to report incidents of workplace violence they encounter, and even if they realized an incident was reportable, they may not be aware of a way to report it or have time to do it. This perceived powerlessness and sense of futility in the face of abuse and violence will only continue to worsen unless action is taken to remove barriers to reporting and for nurses to have access to aid and support for supervisory staff.

Self Quiz
Ask yourself...
- Can you think of any examples of when you or a co-worker tried to report an incident of workplace violence and were unable to?
- If so, what was the barrier that prevented you from reporting?
- Can you name three alternative ways to report workplace violence at your organization?
Culture of Safety
A commonly used phrase is “Culture of Safety”, but is there a standardized definition of what it is or could be? Many resources point to the safety of patients about medical errors, patient rights, and protecting the patient’s information, but few address the issue facing caregivers and especially nurses. However, there is no agreed-upon or standard definition of what exactly a “culture of safety” is or what it should look like.
The American Nurses Association approaches the concept by saying, “Establishing a culture of safety in health care is essential to the security and well-being of your patients, staff, and organization. Effective nurse leaders embrace safety protocols that ensure their organization delivers a secure, protective environment that prioritizes patients and caregivers.” (12)
Currently, there is only a single federal legislation in place about the issue.
The only federal regulation currently in place is the General Duty Clause of the Occupational Safety and Health Act of 1970. This clause requires employers to supply a work environment free from recognized hazards that are causing or likely to cause death or serious physical harm. However, the general duty clause offers no specific recommendations about management of workplace violence.
The Occupational Safety and Health Administration (OSHA) issued guidelines for workplace violence prevention for health care and social service workers. First issued in 1996 and later updated, the guidelines are only advisory. (1)
It is paramount that nurses and other direct care providers accept the responsibility of creating policies and procedures within their organizations to define and enforce a work environment where violence is not tolerated and dealt with accordingly.
There is currently a small body of research and work of the effects workplace violence has on nurses as human beings. Most of the evidence focuses on how workplace violence increases the risk nurses present to patients in the form of medical errors, staffing issues due to missed work, poor documentation, etc.
The main body of evidence discussing how workplace violence affects nurses is noted in research around nurse burnout. A 2020 study published by the National Health Institute (10) states, “Workplace aggression is a source of extreme socio-emotional stress, which may lead to the experience of psychological strain.
A large body of research shows that exposure to workplace aggression and violence may severely impair healthcare workers’ mental health, including symptoms of post-traumatic stress disorder, depression, and burnout.”
This study also shows an important association with workplace aggression and violence targeting nurses and drastically increased levels of emotional exhaustion, depersonalization, and deep feelings of poor personal accomplishment. Over time, these feelings lead to complete burnout, and even worse, possibly psychological and/or physical conditions in the nurse affected.
Even with this preliminary information and research, we still have a long way to go to show the full and far-reaching effects of workplace violence on nurses. Again, by being proactive and acting now, we as nurses can foster this research and bring to light the issues so they can be addressed.

Self Quiz
Ask yourself...
- How does your organization define a “culture of safety”?
- Do you agree with the definition?
- How would you define a “culture of safety” from your own perspective given your experiences and challenges?
ANA Zero Tolerance Policy
In 2019 the American Nurses Association (ANA) (2) release a brief titled “Reporting Incidents of Workplace Violence”. In it, they discussed several issues surrounding workplace violence, barriers to its reporting, and made recommendations to healthcare organizations on strategies relating to the issues of workplace violence.
They also set forth a “Zero Tolerance Policy on Workplace Violence”, which provided some definitions and several recommendations on how to deal with WPV.
The introduction to the “Culture of Safety” part of this brief is as follows:
By prioritizing, developing, and sustaining an organizational culture focused on safety, we can drive the future of healthcare to a place where patients and those who care for them are free from harm. It is not only one of many priorities but is the overriding ethical imperatives for all leaders. (9)
The ANA also suggested a three-level prevention strategy, each with a part for the employer and the employee. Essentially, the role of the employer is gathering data, providing a “safe” work environment, non-punitive reporting, and development of programs to provide a safe work environment for nurses. The employee’s role is to take part in the implementation and evaluation of said programs.
Unfortunately, these are only suggestions and employers do not have to implement any programs or services to protect employees against workplace violence. Also, healthcare employers do not have to report any incidents to JCAHO who consider events of workplace violence to be “sentinel events”.
In the end, it falls on the nurses and employees directly affected by WPV to assume the charge against workplace violence, hold employers accountable, communicate with local and state legislators, and effect change to protect themselves.

Self Quiz
Ask yourself...
- Considering the recommendations and guidelines set forth by these entities, do you think they are adequate or effective? Why nor why not?
- How has this information changed your perception of the overall reporting process on workplace violence against nurses?
- What generalizations can you make from this information on the reporting process from an employer perspective?
Strategies to Prevent Workplace Violence
To end nurse abuse for good, Boston-Leary says it takes every nurse speaking up and reporting abuse within an organizational culture that has an established process for allowing nurses to report abuse without fear of recrimination and then follows up with a resolution. (8)
There are some suggested actions to help prevent and combat workplace violence in your practice setting. These actions include:
Know the definition of abuse.
The National Institute for Occupational Safety and Health (NIOSH) defines workplace violence as “the act or threat of violence, ranging from verbal abuse to physical assaults directed toward persons at work or on duty.”
Agreeing on this definition is an important first step to achieving widespread acknowledgement of the distinct types of nurse abuse, particularly non-physical abuse, Boston-Leary explains. (8)
Report Abuse
Ask about how your workplace manages abuse reporting, whether it is in your current workplace or when you are applying for a position, Boston-Leary suggests. “Ask about how reporting abuse happens during any shift because there should be a reporting mechanism in place for everyone, even if it’s on a weekend or evening shift with no manager easily accessible to report to.”
If (when) you do experience abuse, it’s essential that you speak up immediately and note any witnesses who could corroborate your description of the incident, she says.
Even after you experience abuse and even if you didn’t report it, it’s important to share your past abuse with others to empower them to report abuse they experience. (8)
Change Your Culture
Join or meet a committee to build or strengthen zero-tolerance abuse policies. Based on ANA’s Zero Tolerance Policy on Workplace Violence, Boston-Leary suggests these crucial elements of a zero-tolerance abuse program:
Stop violence before it starts through education to find risks and reduce vulnerabilities for workplace violence.
Create an effective response to violence immediately after it occurs, including emergency care.
Establish long-term responses that reduce the long-term negative effects of workplace abuse. (8)
Communicate with your Legislator!
Congress was considering legislation to #End Nurse Abuse by passing The Workplace Violence Prevention for Health Care and Social Service Workers Act (H.R 1195). If approved, this law would have required health care and social service industry employers to develop and implement a comprehensive workplace violence prevention plan that protects nurses and other healthcare professionals from on-the-job abuse.
Boston-Leary believes legislators are very attuned to the trusted voice of nurses to share about what is happening in health care today (8).

Self Quiz
Ask yourself...
- What is your organization’s primary method of reporting abuse or violence against employees?
- Do you know who your local and state legislators are and how to contact them?
- Are you aware of any committees or groups within your organization that actively address the issue of workplace violence?
Nurse-led Strategies
You can join these committees or work with your employer to create them. Collaborating with your supervisory staff and HR, you can create workflows, policies, reporting methods, and provide education on prevention of workplace violence and make a difference in your overall work environment.
Regarding Your Legislators
As mentioned before, 2021 Congress was considering federal legislation to end nurse abuse by passing The Workplace Violence Prevention for Health Care and Social Service Workers Act (H.R. 1195). The bill was passed by the House on April 16, 2021, but was never passed by the Senate.
You can find your local and state legislator contact information very easily on the internet. A simple search for “how to find state legislator contact information” is a wonderful place to start. As a voting citizen, you have every right to contact them, and demand laws be created to protect you while you work.
Below are some links to help you find elected officials:
- https://www.usa.gov/elected-officials
- https://www.usa.gov/state-governor
- https://www.senate.gov/senators/senators-contact.htm
- https://www.house.gov/representatives/find-your-representative
Advocate for your own safety the same way you would for your patients!
As nurses we aren’t afraid of stepping up to bat for our patients when they need something, but we are notorious for taking a hit and letting it slide, sometimes even to our own detriment.
We owe it to ourselves to offer that same level of advocacy to ourselves and our co-workers.
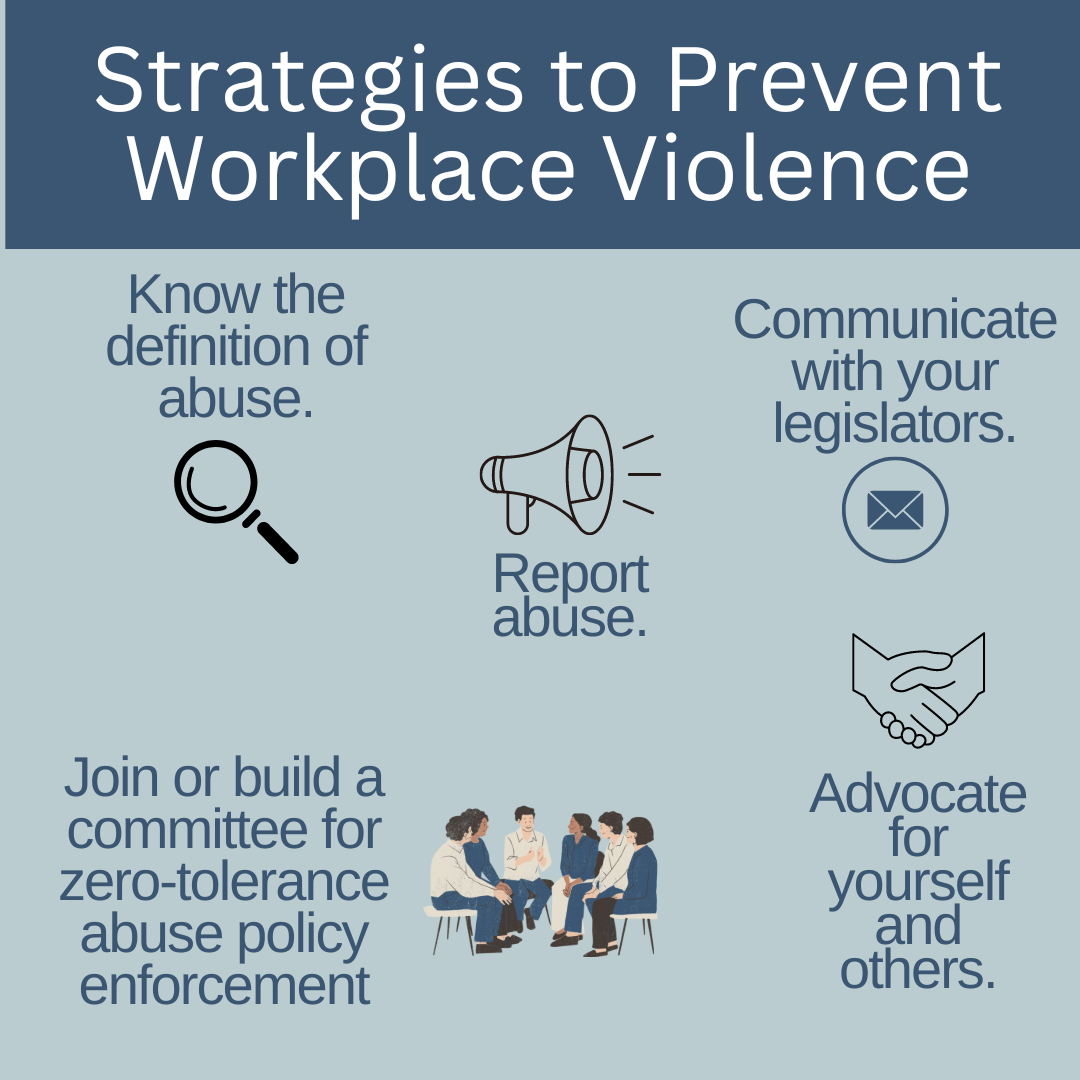

Self Quiz
Ask yourself...
- How can you become an advocate for yourself or your co-workers when it comes to workplace violence?
- Who is the contact in your organization for instances of workplace violence?
Resources
The Joint Commission supplies resources available to report and learn about how to report workplace violence. The links included are for federal, state, professional, and other resources. The direct link to this page is:
The Joint Commission: Workplace Violence Prevention Resources
Local law enforcement
As a private citizen, you are protected by laws about assault, battery, and other attacks on your person. You are within your rights to call the police on events of workplace violence, especially if your life or health are threatened, or you are physically attacked. It is likely your employer will not support you in this situation due to legal implications. It is best to ask your HR department and supervisory staff how these situations should be managed if they occur.
Legal Counsel
Consult with a lawyer about your legal rights in situations on workplace violence and how to best manage them. Be sure to bring scenarios, information on how your employer suggests dealing with these situations, and examples of violence you have seen or have experienced.
Educate and Train Yourself
Learn as much as you can about recognizing and managing workplace violence. Your employer may supply these courses, and if they don’t, it may be prudent to request them. Also, you can seek outside education and training on these topics including self-defense classes and crisis management courses.
Practice Self-Awareness
We all have inherent beliefs, perspectives, and feelings that can prevent us from acting in certain situations. Knowing yourself and understanding possible nuances within yourself that could be a detriment to you appropriately handling a situation of workplace violence could mean the difference between prevention and becoming a victim.

Self Quiz
Ask yourself...
- What training opportunities does your organization provide on management and follow-up for workplace violence?
- What information would you ask local law enforcement or a legal counsel for on workplace violence?
- What might someone who believes abuse against nurses is “just part of the job” do when they find themselves a victim of workplace violence?
- What can you do to help individuals that may simply allow workplace violence to affect their well-being?
Conclusion
Being an agent of change can be intimidating, terrifying, and even force us to deal with feelings and beliefs we didn’t even realize were in our way. Incidents of WPV have been rising sharply over the past several years, and there is no sign of slowing. It’s up to us as front-line workers, nurses, and co-workers to take responsibility for our own safety and work environment.
Through cooperation and consistency, we can create and bring solutions to the workplace and hopefully one day, aid in the creation of laws that make our jobs safer for us to supply the care and support our patients need. We owe it to ourselves to take the necessary steps to show our employers it’s time to address this issue. “Be the change you wish to see in the world.” ~Mahatma Gandhi –
Telemetry Basics - Rhythm Recognition
Introduction
To truly understand telemetry, nurses must have knowledge about the anatomy of the heart and how electricity passes through it, how the electrocardiograph (EKG) works to receive and record the electrical activity, and how this information is transmitted via telemetry to the appropriate receiving device.
Defined as the transmission of instrumental readings by various methods such as radio waves or wires, telemetry gathers and transmits EKG readings to a central or remote monitor for interpretation and storage (71). The ability to read EKG rhythms from a variety of monitors consists of more than looking at a rhythm strip and identifying the rhythm. It consists of knowing the anatomy of the heart, how electricity travels through it and translates into the EKG we know, and what changes can happen based on injury, electrolytes, or other causes.
Introduction
To truly understand telemetry, nurses must have knowledge about the anatomy of the heart and how electricity passes through it, how the electrocardiograph (EKG) works to receive and record the electrical activity, and how this information is transmitted via telemetry to the appropriate receiving device.
Defined as the transmission of instrumental readings by various methods such as radio waves or wires, telemetry gathers and transmits EKG readings to a central or remote monitor for interpretation and storage (71). The ability to read EKG rhythms from a variety of monitors consists of more than looking at a rhythm strip and identifying the rhythm. It consists of knowing the anatomy of the heart, how electricity travels through it and translates into the EKG we know, and what changes can happen based on injury, electrolytes, or other causes.
Heart Anatomy 101
As we know, the heart consists of four chambers, two atria—right atria (RA) and left atria (LA)—and two ventricles—right ventricle (RV) and left ventricle (LV)—working in a cycle to ensure adequate blood flow occurs. The heart receives blood from the inferior and superior vena cava (IVC and SVC) and enters the RA, moves to the RV, passes through the pulmonary artery (PA) and lungs, returns to the LA, enters the LV, and exits the heart through the aorta.
Heart cells, known as myocytes, are negatively charged, or “polarized” at rest. When these muscle cells contract, they become “depolarized” or positively charged. But how do the myocytes know when to contract? Less than 1% of the cells in the heart have a special role and name. These are known as the pacemaker cells and their role is to ensure that the heart beats. This is done through the action potential that is spontaneously created by the pacemaker cells. Some of these pacemaker cells have different speeds in depolarization, meaning that the fastest pacemaker cells are the ones controlling the speed. This will make more sense later when discussing specific cardiac rhythms (69).
Starting in the right atria, the sinoatrial node (SA node) is the primary group of pacemaker cells that determines the heart rhythm. The SA node, as well as the other pacemaker cells within the heart, progress through a rapid depolarization and repolarization process (2).
Pacemaker cells do not have a true resting potential, this means they are always in an “unstable” state to create spontaneous action potential. The action potential is the brief reversal of polarity in the cell; polarity consists of potassium (K+) in the cell with a negative charge, while sodium (Na+) and calcium (Ca++) are outside of the cell with a positive charge (2).
Starting at the beginning of the cardiac cycle the pacemaker cells always have a membrane potential or voltage—the voltage of the cellular membrane as a result of permeability and concentrations of ions inside and outside the cell—of -60 microvolts (mV). From -60mV to -50mV the channels within the cells open, leading to a slow influx of Na+ inside the cell and a slow depolarization of the cell. Once the membrane voltage has reached the minimum threshold of -50mV the Ca++ channels open, causing Ca++ to move into the cell. This is known as the rising depolarization phase. The membrane voltage reaches the peak and the next thing that happens is the falling repolarization phase. This is where the K+ channels open to return the cell to a repolarized state (2).
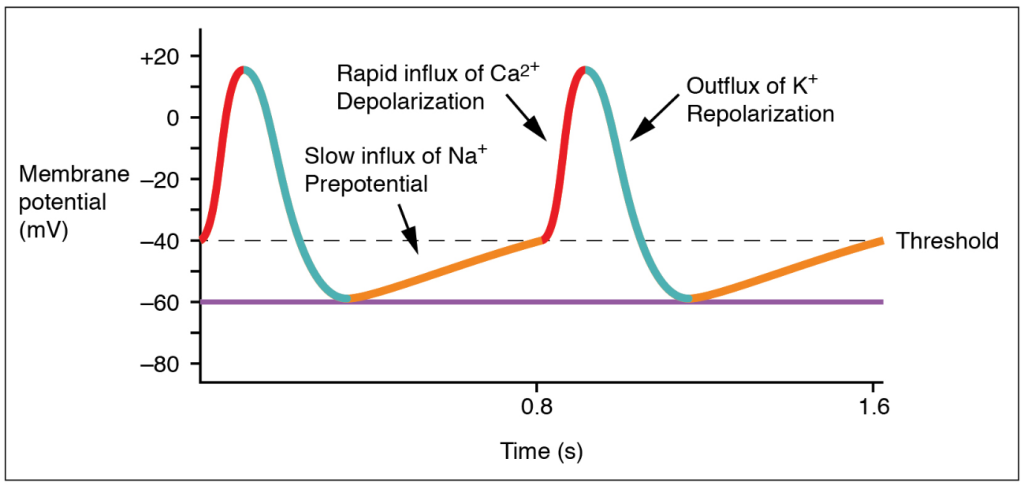
(20)
Once these steps have occurred, the energy is transferred to surrounding cells, and the cardiac cycle continues. However, the action potential in the other myocytes is slightly different. Myocytes have a resting potential, which is different from the pacemaker cells. The resting potential is around -90mV and these cells only start the depolarization process when stimulated by an external force. During the end of the pacemaker cell’s action potential phase, additional Ca++ is passed into the neighboring myocytes through gap junctions. The introduction of Ca++ into the cell causes a sharp rise in the membrane voltage that approaches the threshold which is -70mVs. Once that threshold has been reached, the NA+ fast channels open and a rapid depolarization occurs since Na+ is brought into the cell. The Ca++ slow channels open at -40mVs, further causing depolarization with Ca++ entering the cell (2).
At the peak of cellular depolarization, the Na+ channels close, leading to a slight repolarization through some K+ entering the cell. This is minor as the Ca++ channel is still open and continues to move K+ out of the cell. A plateau is created because of this and allows for the cell to go through two important phases. The first phase starts when the membrane voltage increases from the resting potential and continues until the plateau phase ends. This is known as the absolute refractory period and is where the myocytes relax before they can respond to additional stimuli. It prevents summation and tetanus which could lead to the heart not beating. The second phase is where additional Ca++ is pulled out of the sarcoplasmic reticulum (SR) to further push K+ out of the cell (2).
The phase ends when the Ca++ channel closes, extra Ca++ is sent back to the SR, and K+ is allowed back into the cell. The sodium/potassium pump allows Na+ to exit the cell, returning the cell to its resting potential. This rapid process occurs in every myocyte for the life of the cell. Pacemaker cells are the only cells that can generate a heartbeat. Impulses from the nervous system can increase or decrease the heart rate, but they are influencing the pacemaker cell to generate more beats, not creating them (2).
It is important to note that there are several sets of pacemaker cells within the heart. The SA node starts the process, but there are a few others spaced out along the electricity’s path to ensure that the atria and ventricles of the heart have time to fill and properly contract. The second set of pacemaker cells is the atrioventricular node (AV node) where a slight delay of 0.01-0.05 meters per second (m/s) happens to make sure that the ventricles fill up adequately. The bundle of His takes the electric impulse to the left and right bundle branches and from there, the Purkinje Fibers are triggered. These fibers have a speed of 2-4 m/s to provide enough force to eject the blood from the ventricles (69).
Correlating all of this back to telemetry, scientific development within the medical profession has allowed us to visualize this electrical activity and translate it into an effective method of diagnosing cardiac conditions such as abnormal heart rates or cell death.

Self Quiz
Ask yourself...
- Reflecting on what you know and what you have learned so far, what information would you consider important to know when it comes to reading EKGs or telemetry strips?
- What information, if any, was surprising to you in regard to the action potential of the pacemaker cells?
- Why do you think the pacemaker cells start with a voltage or an action potential?
Types of Telemetry
EKG
There are many ways to view cardiac rhythms now, however, the oldest method is the EKG. During the late 1700s, the Italian physician Luigi Galvani was experimenting with electricity and animal tissue. His experiments spanned at least three decades and inspired other physicians during and after his time. Using legs removed from the bodies of frogs, Galvani theorized that “animal electric fluid” enabled the muscles within the legs to move when touched by metals; according to him, this was “natural” fluid and not created as static electricity or friction is. He went on to theorize that the brain is an essential part of creating the “electric fluid” with nerves as the conductors (6).
Jumping forward to 1842, Doctor Carlo Matteucci made a significant contribution to EKGs. During his time researching electrical detection in animals, he discovered the electrical currents within the heart that accompany each heartbeat. Thirty-five years after Matteucci, Augustus Waller was able to use a capillary electrometer and electrodes to perform the first human EKG. These electrodes were placed on the chest and back of the participant and were vital in demonstrating there was electrical activity that preceded the contraction of the ventricles. William Bayliss and Edward Starling improved upon Waller’s research by using improved capillary electrometers to demonstrate triphasic cardiac electrical activity (1).
The Dutch physician most noted for creating the EKG known today was Doctor Willem Einthoven. He was inspired by Waller and those before him to improve the capillary electrometer, successfully identifying five deflections that were initially named ABCDE. Having to factor for inertia, Einthoven implemented mathematic correlation, resulting in the traditional EKG rhythm strips we use today with the letters PQRST depicted in the image below. Einthoven is also responsible for coining the word electrocardiogram or electrokardiogram in Dutch. This is where providers get the “k” in EKG from (1).
While Waller’s EKG utilized ten electrodes, Einthoven was able to condense that number to three, eliminating the right leg and the mouth electrodes. These three leads created Einthoven’s triangle; an important concept still used today and that will be discussed later. All of Einthoven's work resulted in him being awarded the Nobel Prize in Physiology and Medicine in 1924 (1).

Self Quiz
Ask yourself...
- What do you know of the history of the EKG and telemetry? Was there anything new you learned?
- What process of developing the EKG interested you the most? Why?
- Do you think there is more that can be done to improve EKG? If so, what do you think could be done?
Bedside Monitor
Emergency departments (ED), intensive care units (ICU), and other specialized areas that require continuous monitoring of a patient’s EKG and vital signs utilize various bedside monitors to ensure they are receiving accurate, real-time information on the patient. Cords are used to connect the patient to the monitor. The electrodes to display and document cardiac rhythm and heart rate are applied to patients in the standard 5 lead placement displayed in the below image. The vitals displayed on the monitor can also be displayed outside the room on a screen with multiple patients. Nurses, paramedics, or trained telemetry monitor technicians can watch many of these monitors at a time.
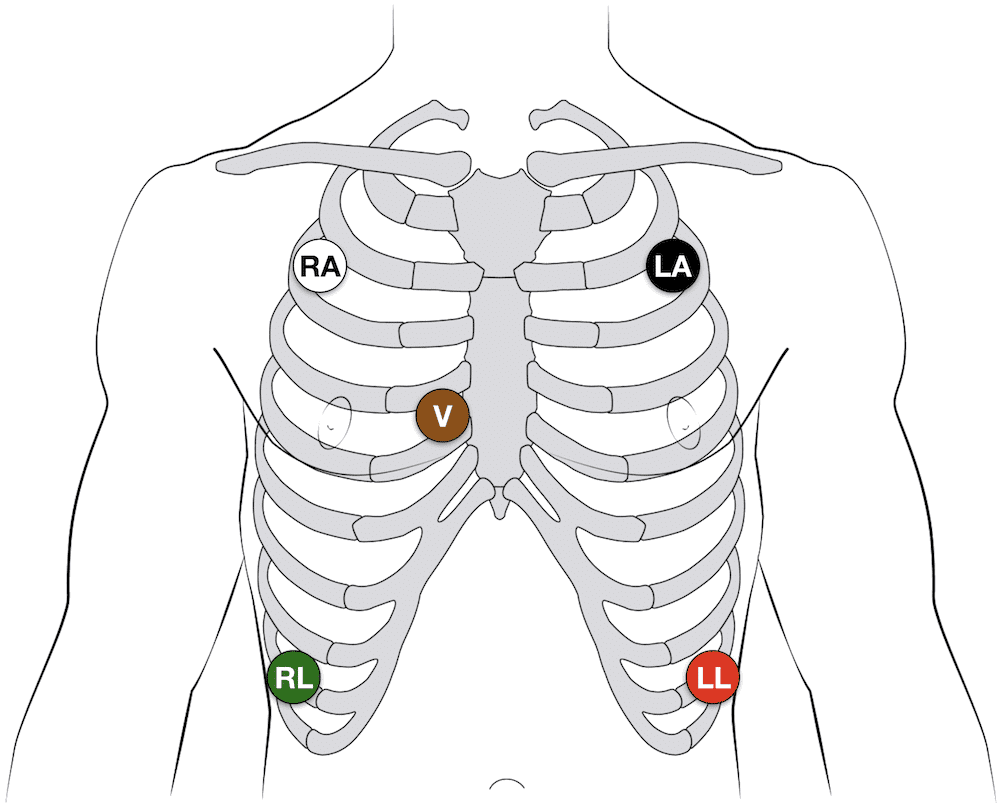
(14)
The placement of the five leads consists of the following:
- RA: 2nd intercostal space, anterior axillary on the right – some providers may put this lead higher on the chest or on the right arm
- LA: 2nd intercostal space, anterior axillary on the left – some providers may put this lead higher on the chest or on the left arm
- RL: 8th intercostal space, anterior axillary on the right – some providers may put this lead lower on the abdomen
- LL: 8th intercostal space, anterior axillary on the left – some providers may put this lead lower on the abdomen
- V: 4th intercostal space, right margin of the sternum
Note: Always follow the manufacturer’s instructions for specific lead placement.
Helpful Tip: Many healthcare providers quickly remember lead placement based on color is smoke (black) over fire (red) and snow (white) over grass (green). This leaves brown (chocolate) in the middle.
These bedside monitors can monitor pulse oximetry, respiratory rate, temperature, capnography, blood pressure, and arterial pressure. Some devices may have other unique monitoring features. These monitors may be portable or have a way to transfer the cords to a transport monitor. They come with alarms that can be adjusted based on the patient’s unique vital signs or hospital policy.
First responders have similar devices they use when transporting patients with the added benefit of having a defibrillator and a real-time feedback device built in (91).
Remote Monitoring
Remote cardiac monitoring is similar to bedside monitoring; however, the EKG rhythm, heart rate, and pulse oximetry are not displayed at the bedside. Instead, they are displayed in a different location, sometimes a monitor room, where a trained professional is watching many patients. When they recognize an abnormal rhythm, they will contact the appropriate staff to assess the patient. They may call for the leads to be removed, a change in rhythm, or a low battery.
The EKG leads are placed the same way as the bedside monitor leads are placed (always be sure to consult the manufacturer’s instructions). The information is transmitted wirelessly via wireless medical telemetry service (WMTS) from the “tele box,” but the leads must be wired to the box. WMTS does not use Wi-Fi and protects transmissions from Wi-Fi interference (48).
Mobile Cardiac Monitor and Event Monitor
A mobile cardiac or event monitor is a device attached to the skin that can perform continuous or event-specific monitoring. This device is attached to the patient’s chest near the heart and records when activated. This device is smaller than other portable cardiac monitoring devices like the Holter Monitor which will be discussed later. Information can be transmitted to the monitoring center to be reviewed by trained staff and/or artificial intelligence. Abnormalities like tachycardia, bradycardia, atrial fibrillation, or cardiac pauses are reported to a physician. The patient may or may not know about the rhythm abnormalities occurring as some patients are asymptomatic (18).
Event monitoring consists of the following methods (23):
- Patch monitor: depending on the manufacturer, the device is stuck to the chest and left on for a designated period of time.
- Loop memory monitor: the sensors always stay on the patient and the patient activates the devices to begin recording when symptoms occur in addition to a few minutes before the event starts and after it ends. There is an implanted option as well.
- Symptom event monitor: Patients place the monitor on them and activate it like a patch monitor, but only when symptoms start.
Insertable Monitor
Insertable or implantable cardiac monitors are just like mobile and event monitors, but they are surgically inserted into the patient. They perform the same actions, but there is an added benefit to these devices. If the patient has worn an external device in the past and has known cardiac arrhythmias, they may have an implanted cardioverter-defibrillator (ICD) inserted to detect and treat the abnormal rhythm. These devices are connected to the heart via wires (they may be placed in the right atria, the right ventricle, or both) and are operated by batteries that do need to be changed per manufacture direction. Patients and providers should be aware of magnets, or electrical signals from other devices that can interfere with the insertable device (61).
Healthcare providers can “interrogate” ICDs or pacemakers with a device created by the monitor’s manufacturer. When interrogated, the device’s information is transmitted to a monitor center who calls the provider to give them a verbal report of what the device has recorded; a paper copy is often faxed to the provider as well. Some newer interrogation devices may display the information of the device on the screen.
Holter Monitor
As mentioned with mobile cardiac monitors, the Holter monitor is another wearable device that can be used to monitor and diagnose cardiac arrhythmias outside of the hospital setting. This device consists of five electrodes and a monitor that the patient can wear or carry on them. It is similar to the remote telemetry devices used in the inpatient hospital setting as shown in the next image. Patients wear this device for a short time, and information is not transmitted to a monitor technician. Instead, information collected is sent to a monitoring center where it is interpreted and sent to the physician (58).
As covered in this section, there are many options for cardiac telemetry monitoring, and providers may encounter many types of them. It is important to know these devices and how they operate.

Self Quiz
Ask yourself...
- What types of telemetry/EKGs are you most familiar with? Which ones would you like to know more about?
- Are there any parts of the devices mentioned above that you have never heard of before?
- Out of all the devices which one do you like best? Which device do you not like?
- What devices do you think could be improved and how would you suggest improving them?
Lead Placement
Now that we have discussed the types of telemetry monitoring devices that are available, it is time to discuss how to properly place the EKG leads on a 12 lead, 15 lead, right-sided EKG, and where to place the V4R lead.
12 Lead EKG
For the 12 lead EKG, providers should start with the four limb leads (14):
- RA: On the upper or lower right arm
- LA: On the upper or lower left arm
- RL: on the upper or lower right leg
- LL: on the upper or lower left leg
From there, the six pericardial leads are placed strategically around the chest to create a partial circle around the heart (14):
- V1: 4th intercostal space, right margin of the sternum (this is lead V on the 5 lead EKG)
- V2: 4th intercostal space, left margin of the sternum
- V3: sits midway between leads V2 and V4 on the left
- V4: 5th intercostal space, mid-clavicular line on the left
- V5: 5th intercostal space, anterior axillary line on the left (aligned horizontally with V4, between V4 and V6) on the left
- V6: 5th intercostal space, mid-axillary line on the left (aligned horizontally with V4)
15 Lead EKG
The 15 lead EKG uses the same leads as the 12 lead EKG, but it adds V7, V8, and V9, known as the posterior leads, to encompass the posterior angles of the heart (14):
- V7: left posterior axillary line (aligned horizontally with V6, across from V5)
- V8: tip of the left scapula (aligned horizontally with V6, across from V4)
- V9: left of the spinal column (aligned horizontally with V6, across from V3)
Right Sided EKG
The right-sided EKG is important to rule out the diagnosis of a right-sided myocardial infarction (MI) or ischemia in or out while treating a patient. Lead placement is the same for the four limb leads, but the 6 precordial leads are flipped (14):
- V1: 4th intercostal space, left margin of the sternum
- V2: 4th intercostal space, right margin of the sternum (this is lead V on the 5 lead EKG)
- V3: sits midway between leads V2 and V4
- V4: 5th intercostal space, mid-clavicular line on the right
- V5: 5th intercostal space, anterior axillary line on the right (aligned horizontally with V4, between V4 and V6)
- V6: 5th intercostal space, mid-axillary line on the right (aligned horizontally with V4)
V4R Lead Placement
A full right-sided EKG is not always needed. Lead V4 on the right side of the heart is the most important lead when it comes to determining an MI on the right side of the heart (14):
- V1, V2, V3, V5, V6: same placement as the 12 and 15 lead EKGs.
- V4 is removed and placed on the right side of the chest
- V4R: 5th intercostal space, mid-clavicular line on the right (Where it is located on a complete right sided EKG)
- The “R” stands for right to ensure that those reading the EKG are aware that lead is on the right while the rest are located on the left side of the chest.
Limb Leads
Now that lead placement has been covered, we can now discuss how lead placement shows different parts of the heart.
Leads I, II, III, AVR, AVL, and AVF are considered limb leads when reading the EKG. It is important to note that the right leg lead is the grounding electrode and does not affect the EKG (83). Leads I, II, and III leads form a triangle over the chest known as Einthoven’s Triangle as reflected in the below image. Lead I always has negative polarity while lead III always has positive polarity. Lead II’s polarity depends on what side of the triangle is being discussed. If we are looking at lead I on the EKG, then lead II is positive, but if we are looking at lead III, then lead II is negative (82).
The importance of what leads are negative and positive comes from how electricity travels through the heart. It starts on the right side and moves to the left, so it would make sense for lead I to have negative polarity while leads II and III are positively charged (82). This is also why the height of a PQRST complex changes based on what lead is being looked at on an EKG as reflected below.
Augmented or unipolar leads AVR, AVL, and AVF have the heart as the negative electrode and the limb leads are the positive electrodes. AVR goes from the heart to the right arm lead, AVL goes from the heart to the left arm lead, and AVF goes from the heart to the left leg lead. Just as discussed with leads I, II, and III, the path of the electricity in the heart determines how the PQRST complex appears on the rhythm strip (82). Lead II is the preferred strip to read by providers due to the best view of the rhythm due to the way electricity travels through the heart and how lead II follows that path by starting at the right shoulder and going to the left leg.
The chest leads, V1 – V9, create a circle around the heart on a horizontal plane. These leads are unipolar as well, with the heart being the negative electrode. Multiple views of the heart are captured because of the many leads placed along the patient’s body. This can give providers valuable knowledge on what areas of the heart may be affected. The next image gives a visual depiction of how the leads display their view of the heart.
 (92)
(92)

Self Quiz
Ask yourself...
- What lead do you think is the most beneficial in reading EKGs? Why do you think that?
- What lead do you prefer to use when reading EKGs? What makes that your “go-to” lead?
- If you could make a policy on EKGs, would you include what type of EKG should be done on patients? Would all patients with chest pain get a 15 lead EKG instead of 12?
- Do you think that one type of EKG is better than the other? Or do they all have their specific uses and benefits?
Reading EKGs: EKG Components
To be able to interpret EKGs successfully, nurses must first have knowledge about the EKG components displayed on the EKG strips and how each part correlates to a part of a single heartbeat.
P wave
The P wave is the first deflection from the isoelectric line or baseline. Correlating this to the heart, this is where the atria depolarize or contract. The contraction of the right atria starts at the beginning of the P wave while the contraction of the left atria begins in the middle and end of it. Normal P waves are apparent between 120 and 200 milliseconds (msec) before the upward deflection of the QRS complex (44)
PR Interval
The next part of the PQRST complex is the PR interval. The interval symbolized the time between the depolarization of the atria and the depolarization of the ventricle. The normal speed is 120 to 200 msec (44).
PR Segment
Next is the PR segment. This is similar to the PR interval but starts at the end of the P wave and ends at the start of the Q wave. This line is important because if there is a deviation from the isoelectric line, it could indicate a cardiac rhythm abnormality like Wolff-Parkinson-White syndrome which will be discussed later. The EKG may have a “slurred” upstroke from the P to R points on the EKG, making the Q wave appear to be on the isoelectric line. This is because the ventricles were stimulated or excited early, leading to a shortened PR interval. The “slurred” area is known as a delta wave (13).
QRS Complex
The QRS complex is where the ventricles depolarize and contract. The first downward deflection of the beat is the Q wave that lasts for < 0.05 seconds. It is present in all leads save for V1 and V3 due to the angle of the vector. The R wave is the upward deflection of the complex. R waves do not have a set height, but severely elevated R waves can be an indicator of ventricular hypertrophy. The second downward deflection is the S wave. Overall, the QRS complex is 0.07 to 0.10 seconds long and variations to this time can be an indicator of abnormal heart rhythms (17).
ST Segment
The ST segment starts when the S wave ends by returning to the isoelectric line and ends when the T wave begins. This period represented the completion of ventricular depolarization (17). The ST segment lasts 0.08 seconds to 0.12 seconds (51).
T Wave
The final wave in the standard EKG components is the T wave. This wave symbolizes the ventricles repolarizing. Inverted T waves can be an indication of past or current infections. A peaked T wave—as opposed to the normal curved T wave—can be caused by hypocalcemia, hyperkalemia, and left ventricular hypertrophy (17). The T wave runs from 0.01 seconds to 0.25 seconds (51).
The image below depicts the components of an EKG with labels to assist with understanding how the waves appear.
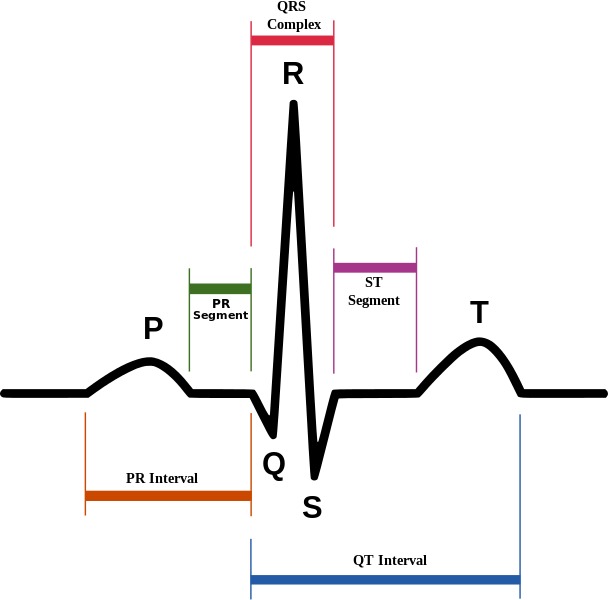
(4)
Reading EKGs: EKG Components
To be able to interpret EKGs successfully, nurses must first have knowledge about the EKG components displayed on the EKG strips and how each part correlates to a part of a single heartbeat.
P wave
The P wave is the first deflection from the isoelectric line or baseline. Correlating this to the heart, this is where the atria depolarize or contract. The contraction of the right atria starts at the beginning of the P wave while the contraction of the left atria begins in the middle and end of it. Normal P waves are apparent between 120 and 200 milliseconds (msec) before the upward deflection of the QRS complex (44)
PR Interval
The next part of the PQRST complex is the PR interval. The interval symbolized the time between the depolarization of the atria and the depolarization of the ventricle. The normal speed is 120 to 200 msec (44).
PR Segment
Next is the PR segment. This is similar to the PR interval but starts at the end of the P wave and ends at the start of the Q wave. This line is important because if there is a deviation from the isoelectric line, it could indicate a cardiac rhythm abnormality like Wolff-Parkinson-White syndrome which will be discussed later. The EKG may have a “slurred” upstroke from the P to R points on the EKG, making the Q wave appear to be on the isoelectric line. This is because the ventricles were stimulated or excited early, leading to a shortened PR interval. The “slurred” area is known as a delta wave (13).
QRS Complex
The QRS complex is where the ventricles depolarize and contract. The first downward deflection of the beat is the Q wave that lasts for < 0.05 seconds. It is present in all leads save for V1 and V3 due to the angle of the vector. The R wave is the upward deflection of the complex. R waves do not have a set height, but severely elevated R waves can be an indicator of ventricular hypertrophy. The second downward deflection is the S wave. Overall, the QRS complex is 0.07 to 0.10 seconds long and variations to this time can be an indicator of abnormal heart rhythms (17).
ST Segment
The ST segment starts when the S wave ends by returning to the isoelectric line and ends when the T wave begins. This period represented the completion of ventricular depolarization (17). The ST segment lasts 0.08 seconds to 0.12 seconds (51).
T Wave
The final wave in the standard EKG components is the T wave. This wave symbolizes the ventricles repolarizing. Inverted T waves can be an indication of past or current infections. A peaked T wave—as opposed to the normal curved T wave—can be caused by hypocalcemia, hyperkalemia, and left ventricular hypertrophy (17). The T wave runs from 0.01 seconds to 0.25 seconds (51).
The image below depicts the components of an EKG with labels to assist with understanding how the waves appear.
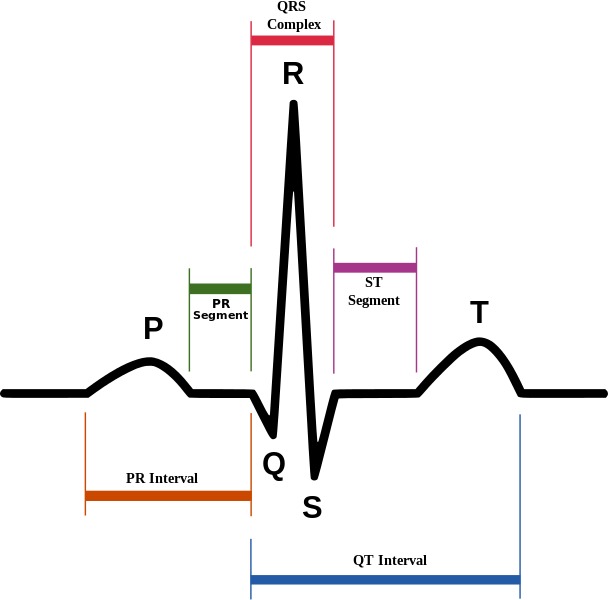
(4)
Reading EKGs: EKG Paper
The EKG paper has sets of squares, 25 little squares within one larger square. The smaller squares symbolize 0.04 seconds making the larger square 0.20 seconds. A single small square is 1mm while the large square is 5mm, this is because the larger square is five small squares tall.

(15)
Some EKG strips are presented in a six second format. To determine if the strip is a six-second, you must count the larger boxes. 30 larger boxes are required for the strip to be six seconds. Some may even have second markers that symbolize one second of time passed.
The 12 lead EKG can be more challenging to read and is often used to make an overall observation about the patient’s heart rate and rhythm. It can provide more information to providers than a single lead strip can.
As discussed previously, the leads are placed along the path of the heart, and providers can determine what part of the heart may be affected by knowing what leads are placed where.
| Lead | Location |
| II, III, AVF | Inferior |
| I, AVL, V5, V6 | Lateral |
| V2, V3, V4 | Anterior |
| V1, AVR | Right atrium, left ventricle |
(51)
Now that we have discussed leads, lead placement, the PQRST complex, and EKG paper, it is time to cover different cardiac rhythms that you may encounter.

Self Quiz
Ask yourself...
- What parts of the PQRST complex may not appear on the EKG strip?
- How do you remember what leads are associated with each part of the heart?
- What are some ways you can quickly determine heart rate using an EKG strip?
- Is there a part of the PQRST complex do you think is important to pay attention to? Why do you think that?
Rhythm Recognition
Normal Sinus (41):
- Rate: 60-100 beats per minute (bpm)
- Conduction:
- PR interval 120-200ms
- QRS width 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic (curves above and then dips below the isoelectric line) in V1
- Duration:
- Less than 0.12 seconds
- Rhythm Strip:
- The maximum height of the P wave is:
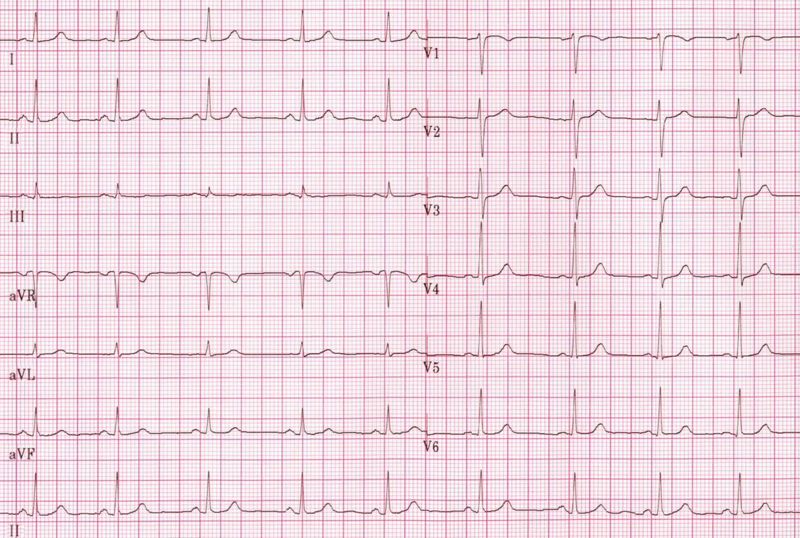
(29)
Sinus Bradycardia (87):
- Rate: less than 60bpm
- Conduction:
- PR interval 120-200ms
- QRS width 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- The maximum height of the P wave is:
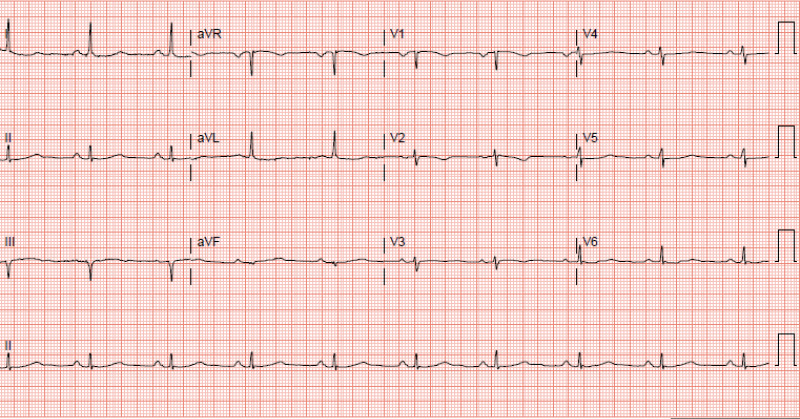
(87)
- Signs and Symptoms:
- None – depending on the patient
- Cyanosis
- Peripheral edema
- Shortness of breath
- Dizziness
- Fatigue
- Syncope or near syncope
- Lightheadedness
- Causes (not limited to):
- Normal physiology in an athlete
- Medications like beta-blockers
- Ischemia
- Heart diseases
- Sick sinus syndrome
- Hypothermia
- Hypothyroidism
- Neuro-mediated bradycardia as caused by a vasovagal reaction
- Pericarditis
- Hypoxia
- Electrolyte imbalances
- Treatment:
- None if asymptomatic, admission for observation may be indicated
- Medications:
- Atropine 0.5mg every 3 to 5 minutes for a maximum dose of 3mg
- Antidotes or reversal agents
- Transcutaneous cardiac pacing or pacemaker
- Return patient to a normothermic state if hypothermic
Sinus Tachycardia (55):
- Rate: greater than 100bpm but less than 150bpm
- Conduction:
- PR interval 120-200ms
- QRS width 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- The maximum height of the P wave is:
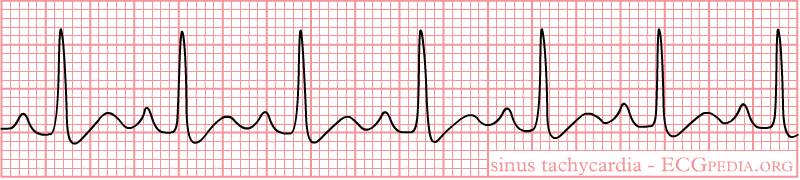
(42)
- Signs and Symptoms:
- Shortness of breath
- Chest pain
- Dizziness
- Syncope or near syncope
- Lightheadedness
- Palpitations
- Causes:
- Infection or sepsis
- Medications
- Withdrawal
- Electrolyte imbalances
- Blood loss or anemia
- Dehydration
- Hypoglycemia
- Pulmonary embolism
- Trauma
- Cardiac tamponade
- Myocarditis
- Pregnancy
- Treatment:
- Medications
- Antibiotics
- Antidotes or reversal agents
- Insulin
- Electrolyte replacement
- Fluids
- Heparin or other anticoagulant medications
- Blood replacement
- Surgery
- Medications

Self Quiz
Ask yourself...
- Looking at the signs and symptoms for sinus bradycardia what other signs and symptoms have you seen with patients who present with that heart rhythm?
- What other causes have you seen as the reason for sinus bradycardia?
- With sinus tachycardia, when would you be concerned with the causes of the rhythm?
- Are there any other treatments you could think of for either sinus bradycardia or tachycardia?
1st Degree AV Block (68):
- Rate: 60-100 beats per minute (bpm)
- Conduction:
- PR interval greater than 0.20 seconds
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- A QRS complex always follows the P wave
- The maximum height of the P wave is:
- Duration:
- Less than 0.12 seconds
- Rhythm Strip:
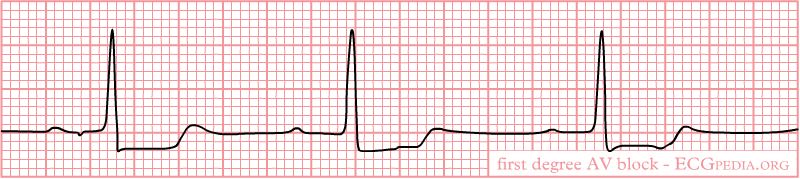
(32)
- Signs and Symptoms:
- None
- Fatigue
- Shortness of breath
- Syncope or near syncope
- Chest pain
- Lightheadedness
- Causes:
- Increased vagal tones in young patients
- Fibrotic changes in the elderly
- Cardiac disease
- Inflammation
- Medications
- Electrolyte abnormalities
- Treatment:
- None if asymptomatic
- Medications
- Antibiotics
- Antidotes or reversal agents
- Electrolyte replacement
2nd Degree Type I AV Block (Mobitz Type 1 or Wenckebach) (60):
- Rate: varies
- Conduction:
- PR interval increases with each beat, eventually “dropping off” and another P wave appears
- “Longer, longer, drop, that’s a Wenckebach.”
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- The maximum height of the P wave is:

(27)
- Signs and Symptoms:
- None
- Fatigue
- Shortness of breath
- Syncope or near syncope
- Chest pain
- Lightheadedness
- Causes:
- Increased vagal tones
- Cardiomyopathy
- Myocardial infarction
- Cardiac surgery
- Electrolyte abnormalities
- Medications
- Treatment:
- None if asymptomatic
- Medications
- Atropine if bradycardic
- Antidotes or reversal agents
- Electrolyte replacement
2nd Degree Type II AV Block (Mobitz II) (60):
- Rate: varies
- Conduction:
- PR interval varies
- QRS width 60-100ms when present
- QRS does not follow all P waves
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- The maximum height of the P wave is:
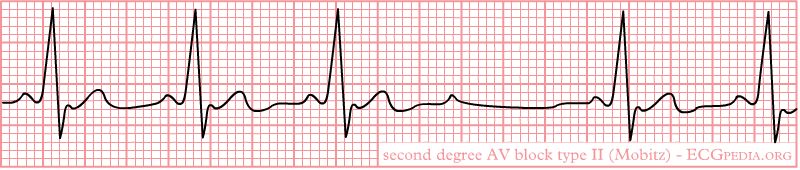
(40)
- Signs and Symptoms:
- Fatigue
- Shortness of breath
- Syncope or near syncope
- Chest pain
- Lightheadedness
- Cardiac arrest
- Causes:
- Structural heart disease
- Amyloidosis
- lymphoma
- Cardiac tumors
- Transcatheter placement of valves
- Myocardial infarction
- Genetics
- Treatment:
- None if asymptomatic
- Medications
- Atropine does not work on these patients
- Antidotes or reversal agents
- Transcutaneous cardiac pacing or pacemaker since this rhythm can progress to a complete heart block or cardiac arrest
3rd Degree AV Block (78):
- Rate: varies, but usually bradycardic
- Conduction:
- PR interval varies
- QRS width 60-100ms when present
- P wave and QRS complex do not communicate (called AV disassociation)
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- The maximum height of the P wave is:

(33)
- Signs and Symptoms:
- Fatigue
- Shortness of breath
- Syncope or near syncope
- Chest pain
- Lightheadedness
- Hemodynamic instability
- Cardiac murmurs
- Cardiac arrest
- Causes:
- Cardiac surgery
- Cardiac disease
- Medications
- Electrolyte imbalances
- Lyme disease
- Transcatheter aortic valve replacement
- Myocardial infarction
- Systemic lupus erythematosus
- Sarcoidosis
- Treatment:
- Medications
- Atropine usually does not work, but can be administered
- Epinephrine
- Dopamine
- Antidotes or reversal agents
- Electrolyte replacement
- Transcutaneous cardiac pacing or pacemaker
- Medications

Self Quiz
Ask yourself...
- 2nd degree Type I and Type II can be mixed up, what are your methods for remembering how each one appears on the EKG strip?
- What type of AV block would lead you to provide quick intervention and why?
- Have you encountered a patient with any of these rhythms? What was the cause? How was it resolved, if it was?
- Are there any causes for these rhythms that were not listed?
Premature Ventricular Contraction (PVC) (88):
- Rate: varies, underlying rhythm is usually normal sinus
- The impulse to beat comes from the ventricles, not from the SA node
- Conduction:
- PR interval varies, but in a regular PQRST complex PR interval is 120-200ms
- PR interval after a PVC is longer due to the PVC and the retrograde concealed conduction goes back into the AV node junction.
- PVC QRS width is at least 120ms but usually 160-200ms
- Regular QRS width is 60-100ms
- PR interval after a PVC is longer due to the PVC and the retrograde concealed conduction goes back into the AV node junction.
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- Monomorphic: All PVCs are shaped the same
- The maximum height of the P wave is:
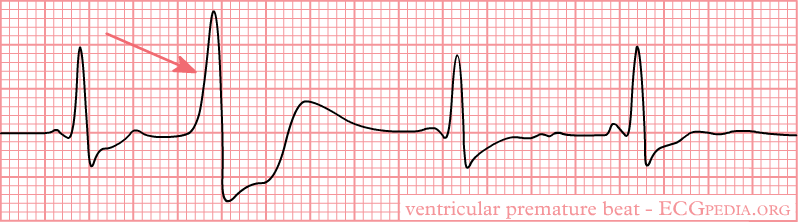
(38)
- Biomorphic: PVCs are shaped differently
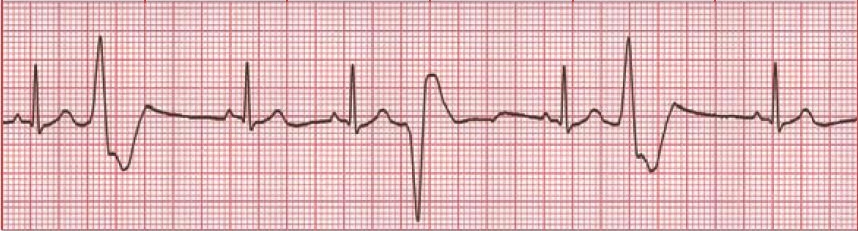
(64)
- Bigeminy: Every PVC is separated by one sinus beat.

(35)
- Trigeminy: Every PVC is separated by two sinus beats.

(9)
- Ventricular Couplet: Two PVC beats in a row.
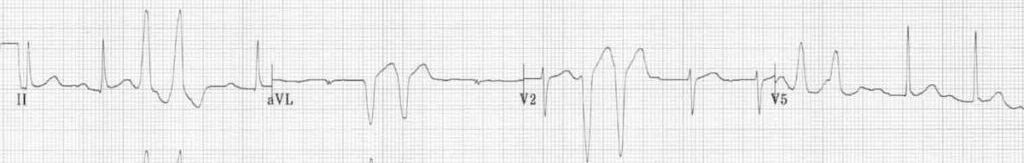
(9)
- Ventricular Triplet: Three PVC beats in a row.

(9)
- Signs and Symptoms:
- None
- Fatigue
- Shortness of breath
- Syncope or near syncope
- Chest pain
- Palpitations
- Lightheadedness
- Abnormal neck pulsation
- Hemodynamic instability with frequent PVCs
- Cardiac arrest
- Causes:
- Hypoxia
- Illicit drug use
- Amphetamines
- Alcohol
- Cocaine
- Electrolyte imbalances
- Myocarditis
- Mitral valve prolapse
- Hypercarbia
- Cardiomyopathies
- Myocardial infarction
- Medications
- Treatment:
- None if asymptomatic
- Medications
- Beta-blockers
- Calcium channel blockers
- Amiodarone is for those with preexisting coronary artery diseases, but used with caution and close observation and monitoring
- Antidotes or reversal agents
- Electrolyte replacement
- Cardiac ablation
- Defibrillation if cardiac arrest occurs
Premature Atrial Contractions (PAC) (54):
- Rate: varies, underlying rhythm is usually normal sinus
- Conduction:
- PR interval varies, but in a regular PQRST complex PR interval is 120-200ms
- PAC
- Regular QRS width is 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave:
- Can be inverted
- May be hidden in the T wave creating a hump or peaked T wave
- These rhythms can come in the same variations as PVCs:
- Bigeminy
- Trigeminy
- Couplet
- Triplet
- Rhythm Strip:
- The maximum height of the P wave is:
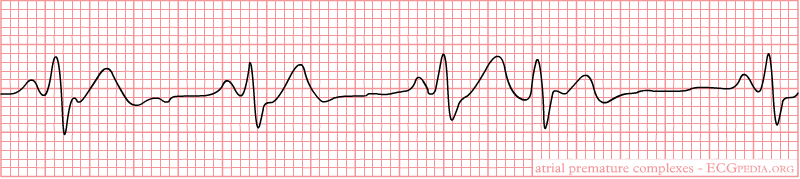
(37)
- Signs and Symptoms:
- None
- Palpitations
- Shortness of breath
- Anxiety
- Signs and symptoms of heart failure
- Early or additional heart sounds
- Pauses in rhythm
- Causes:
- Coronary artery disease
- Left ventricular hypertrophy
- Septal defects
- Congenital heart deformities
- Medications
- Beta-blockers
- Chemotherapeutic agents
- Congestive heart failure
- Diabetes mellitus
- Hypertension
- Chronic obstructive pulmonary disorder
- Anxiety
- Treatment:
- None if asymptomatic
- Avoiding triggers
- Medications
- Beta-adrenergic blockers
- Antiarrhythmic agents are used with caution and close observation and monitoring
- Antidotes or reversal agents
- Cardiac ablation

Self Quiz
Ask yourself...
- Between PACs and PVCs, which one would you be more concerned about? Why did you pick that rhythm?
- Have you encountered a patient with either of these rhythms? What treatments were ordered if any?
Ventricular Tachycardia (V Tach) (45):
- Rate: greater than 100bpm
- Conduction:
- PR interval none
- QRS width greater than 140ms
- P wave morphology:
- Not present
- Non-sustained V-Tach: three or more ventricular beats over a maximum of 30 seconds.
- Sustained V-Tach: a run of V Tach for more than 30 seconds or less is treated by cardioversion
- Monomorphic V-Tach: all ventricular beats look the same
- Polymorphic V-Tach: the ventricular beats look different.
- Biphasic V Teach: where the QRS complexes alternate with each beat.
- Digoxin intoxication
- Long QT syndrome
- Rhythm Strip:
- Monomorphic V-Tach
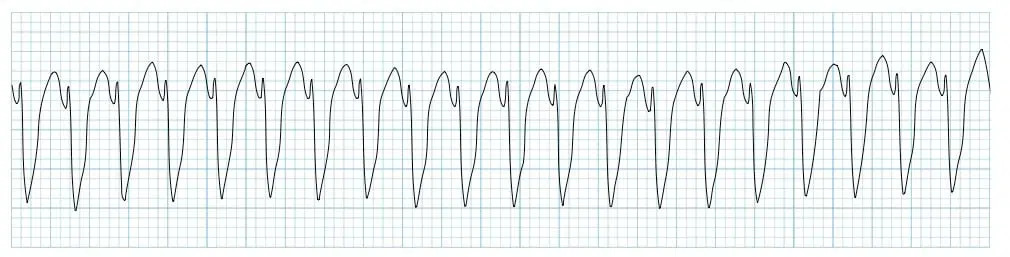
(11)
- Signs and Symptoms:
- Palpitations
- Shortness of breath
- Chest pain
- Syncope or near syncope
- Signs of heart failure
- Hemodynamic instability
- ICD shocks if the patient has one
- Cardiac arrest
- Also known as pulseless V-Tach
- Causes:
- Ischemic heart disease
- Acute coronary artery disease
- Myocardial scar-related reentry
- Congenital heart deformities
- Cardiomyopathy
- Illicit drugs
- Cocaine
- Digitalis toxicity
- Methamphetamine
- Medications
- Beta-blockers
- Chemotherapeutic agents
- Electrolyte imbalances
- Sepsis
- Metabolic acidosis
- Inherited cardiac channelopathies
- Treatment:
- Cardiopulmonary resuscitation (CPR) and defibrillation if no pulse present
- Cardioversion if hemodynamically unstable and has a pulse
- Treatment for myocardial infarction
- Medications
- Amiodarone, procainamide, sotalol
- Antidotes or reversal agents
- ICD
- Cardiac ablation

Self Quiz
Ask yourself...
- What would be the priorities when providing care to a patient with V-Tach with a pulse?
- If you were the only one in the room with the patient what would be your first action?
- Have you ever cardioverted a patient with this rhythm? What do you remember from the event?
- Do you think the patient should sign consent before cardioversion? Why or why not?
Torsades de Pointes (V Fib) (25):
- Rate: none
- Conduction:
- Polymorphic V-Tach with a prolonged QR interval
- P wave morphology:
- Not present
- Rhythm Strip:
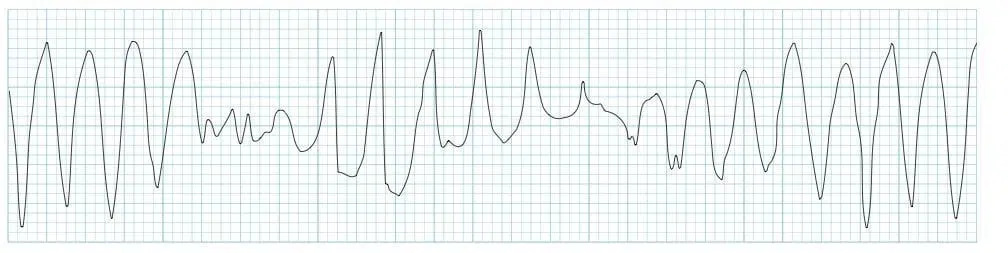
(12)
- Signs and Symptoms:
- None
- Syncope or near syncope
- Dizziness
- Lightheadedness
- Hypotension
- Rapid pulse
- Cardiac arrest
- No pulse
- Not breathing or only gasping for air
- Loss of consciousness
- Causes:
- Electrolyte imbalances
- Medications
- Zofran causes a long QT interval (19)
- Congenital prolonged QT:
- Jervell and Lange-Nielsen
- Romano-Ward syndrome
- Bradycardia
- Diuretic use
- Female gender
- Age
- Treatment:
- Electrolyte replacement
- CPR and defibrillation
- Medications
- Epinephrine
- Atropine
- Cardioversion
- Treatment of the underlying cause
Supraventricular Tachycardia (SVT) (72):
- Rate: Greater than 160bpm
- Conduction:
- PR interval not present
- QRS width less than 120 milliseconds = narrow complex, regular SVT
- QRS width greater than 120 milliseconds = wide complex, regular SVT
- P wave morphology:
- Not present
- Rhythm Strip:
- Narrow complex, regular SVT

(30)
- Wide complex, regular SVT

(79)
- Signs and Symptoms:
- None
- Hypotension
- Shortness of breath
- Lightheadedness
- Signs and symptoms of heart failure
- Shock
- Causes:
- Narrow complex, regular SVT - Orthodromic reentry phenomenon (56):
- Accessory pathway that connects the atria and ventricles without passing through the AV node
- A pulse goes through the AV node, down into the ventricles via the Bundle of His, up through the accessory pathway, and back into the AV node
- Wide complex, regular SVT - Atrioventricular reentry phenomenon (57):
- Signals from the SA node travel through the accessory pathway down the ventricles via the Bundle of His and up to the AV node, creating a backward cycle.
- This is slower than the orthodromic SVT because it is traveling against the regular path of conduction, leaving to a wide QRS complex
- Medications
- Caffeine
- Smoking
- Stress
- Alcohol
- Narrow complex, regular SVT - Orthodromic reentry phenomenon (56):
- Treatment:
- None if asymptomatic
- Vagal maneuvers
- Bearing down
- Blowing into a straw
- Medications
- Adenosine: 1st dose 6mg, 2nd dose 12mg
- Ensure rapid saline flush after pushing medication as it has an extremely short half-life
- Cardizem
- Antidotes or reversal agents
- Adenosine: 1st dose 6mg, 2nd dose 12mg
- Cardioversion
- Cardiac ablation

Self Quiz
Ask yourself...
- If you have encountered a patient in SVT, what vagal maneuvers have you seen used? Were they successful or not?
- If you have not encountered a patient with SVT, what vagal maneuvers could you think of that might be utilized?
- Would a patient’s age impact the vagal maneuvers used? Why or why not?
- Do you know the half-life of Adenosine? If not, will you look it up after this course?
Ventricular Fibrillation (V-Fib) (3):
- Rate: none
- Conduction:
- PR interval not present
- QRS width not present
- P wave morphology:
- Not present
- Rhythm Strip:
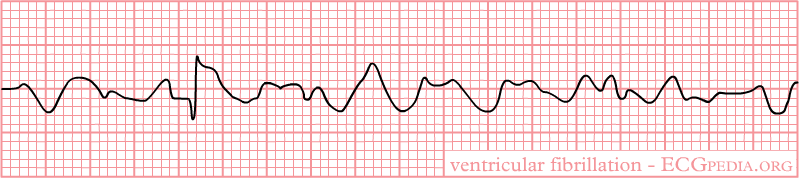
(39)
- Signs and Symptoms:
- Cardiac arrest
- No pulse
- Not breathing or only gasping for air
- Loss of consciousness
- Causes:
- Electrolyte imbalances
- Myocardial infarction
- Congenital heart defects
- Sudden blow to the chest right over the heart
- Medications
- Anemia
- Cardiomyopathy
- Electrocution
- Thoracic trauma
- Heart surgery
- Treatment:
- CPR and defibrillation
- Medications
- Epinephrine
- Atropine
- Electrolytes
- Surgery
- Coronary perfusion
- Treatment of the underlying cause
- Cardiac arrest
Asystole (59):
- Rate: none
- Conduction:
- PR interval not present
- QRS width not present
- P wave morphology:
- May or may not be present
- Rhythm Strip:

(21)
- Signs and Symptoms:
- Cardiac arrest
- No pulse
- Not breathing or only gasping for air
- Loss of consciousness
- Causes:
- Electrolyte imbalances
- Myocardial infarction
- Congenital heart defects
- Medications or illicit drugs
- Blood loss
- Cardiomyopathy
- Electrocution
- Trauma
- Treatment:
- CPR
- Since there is no electrical activity with this rhythm, defibrillation cannot be used
- Medications
- Epinephrine
- Atropine
- Electrolytes
- Surgery
- Coronary perfusion
- Treatment of the underlying cause
- CPR
- Cardiac arrest
Pulseless Electrical Activity (PEA) (22):
- Rate: varies
- There is no pulse with this rhythm despite the fact that it may appear as an organized rhythm
- Conduction:
- PR interval none
- QRS width greater than 110ms
- P wave morphology:
- Not present
- The P wave is:
- Not present
- Rhythm Strip:
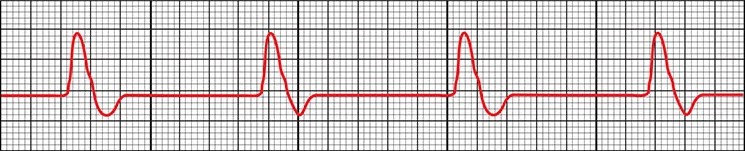
(22)
- Signs and Symptoms:
- Cardiac arrest
- No pulse
- Not breathing or only gasping for air
- Loss of consciousness
- Causes:
- Electrolyte imbalances
- Myocardial infarction
- Congenital heart defects
- Medications or illicit drugs
- Blood loss
- Cardiomyopathy
- Electrocution
- Trauma
- Hypothermia
- Pneumothorax or hemothorax
- Treatment:
- CPR
- Since there is no electrical activity with this rhythm, defibrillation cannot be used
- Medications
- Epinephrine
- Atropine
- Electrolytes
- Surgery
- Coronary perfusion
- Treatment of the underlying cause
- CPR
- Cardiac arrest

Self Quiz
Ask yourself...
- What are some misconceptions about V-Fib, asystole, and PEA?
- How do you educate other staff members and family members on these misconceptions?
- What treatments have you seen work on V Fib? What treatments did not work?
- Have you ever seen a patient’s rhythm change from asystole to another rhythm?
- What is the most prominent cause of cardiac arrest in your area?
Atrial Flutter (73):
- Rate: varies
- Depends on how many QRS complexes there are
- Atrial rate 250-350 bpm
- Ventricular rate 75-150bpm
- P waves can come in blocks
- 2 P waves per 1 QRS (2:1)
- 3 P waves per 1 QRS (3:1)
- 4 P waves per 1 QRS (4:1)
- Intervals of P waves per 1 QRS (2:1 then 3: 1 then 2:1 then 4:1)
- Conduction:
- PR interval varies
- QRS width 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- Sawtooth pattern
- Rhythm Strip:
- The maximum height of the P wave is:
- Depends on how many QRS complexes there are
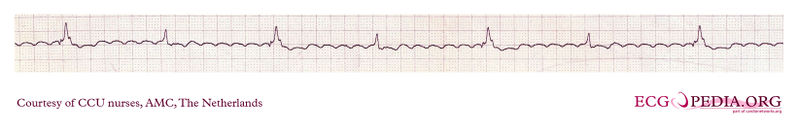
(31)
- Signs and Symptoms:
- None
- Palpitations
- Fatigue
- Syncope or near syncope
- Shortness of breath
- Regular or irregularly regular pulse
- Causes:
- COPD
- Heart failure
- Atrial size abnormalities
- Hypertension
- Diabetes mellitus
- Age
- Male gender
- Treatment:
- None if asymptomatic
- Medications
- Amiodarone
- Cardizem
- Metoprolol
- Anticoagulation to prevent stroke
- Catheter ablation
- Treatment of the underlying cause
Atrial Fibrillation (AFib) (89):
- Rate: varies
- Atrial rate 400-600 bpm
- Ventricular rate 75-175 bpm
- Anything over 100 is considered A Fib with rapid ventricular response (RVR)
- Conduction:
- PR interval varies
- QRS width 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- Rhythm Strip:
- A Fib
- The maximum height of the P wave is:
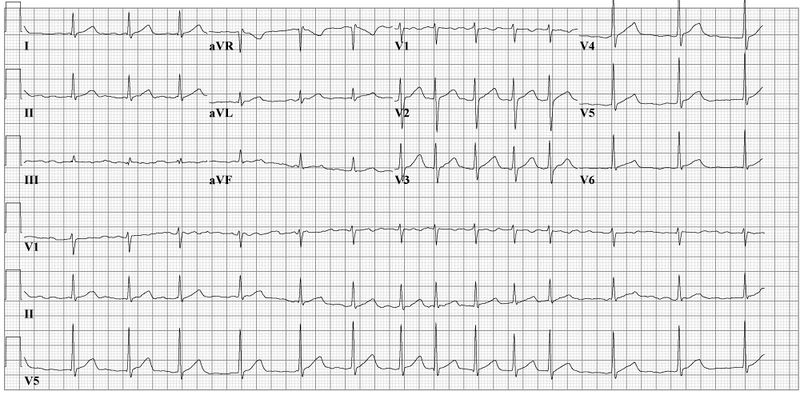
(28)
- A Fib RVR

(34)
- Signs and Symptoms:
- None
- Palpitations
- Fatigue
- Syncope or near syncope
- Shortness of breath
- Regular or irregular pulse
- Patients can go in and out of A Fib or it can be permanent,
- They can go in and out of RVR
- Causes:
- Heart disease
- Genetics
- Pulmonary embolism or other hemodynamic stressors
- Obstructive sleep apnea
- Heart failure
- Pericarditis
- Myocarditis
- Myocardial infarction
- Hypertension
- Diabetes mellitus
- Age
- Treatment:
- None if asymptomatic
- Medications
- Cardizem
- Metoprolol
- Amiodarone
- Anticoagulation to prevent stroke
- Catheter ablation
- Treatment of the underlying cause
Idioventricular Rhythms (47):
- Rate: varies
- Idioventricular rate 35-40bpm
- Accelerated rate 60-120bpm
- Conduction:
- PR interval not present
- QRS width greater than 120ms but can be greater than 160ms
- The normal conduction system does not transmit the signal to beat, the vertical signal is transmitted from cell to cell
- P wave morphology:
- Not present
- Rhythm Strip:
- Idioventricular rate

(36)
- Signs and Symptoms:
- None
- Palpitations
- Fatigue
- Lightheadedness
- Syncope or near syncope
- Cardiac arrest
- Causes:
- Electrolyte imbalances
- Reperfusion of cardiac cells after a myocardial infarction
- Medications
- Digoxin
- Beta-adrenoreceptor agonists
- Illicit drug use like cocaine
- Cardiomyopathies
- Congenital cardiac defects
- Athletes
- Treatment:
- None if asymptomatic
- Medications
- Atropine
- Amiodarone or lidocaine
- Reversal agents
- Rarely cardiac pacing
- Treatment of the underlying cause
Junctional Rhythms (52):
- Rate: varies
- Junctional bradycardia less than 40bpm
- Junctional escape rhythm 40-60bpm
- Accelerated junctional rhythm 60-100bpm
- Junctional tachycardia greater than 100bpm
- Conduction:
- PR interval not present
- QRS width 60-100ms
- P wave morphology:
- Not present
- Rhythm Strip:
- Accelerated Junctional Rhythm
- Rhythms look the same but have more beats depending on the type of rhythm
- Accelerated Junctional Rhythm

(52)
- Signs and Symptoms:
- None
- Shortness of breath
- Palpitations, intermittent or continuous
- Fatigue
- Lightheadedness
- Syncope or near syncope
- Causes:
- Electrolyte imbalances
- Can be caused by anorexia nervosa
- Thoracic trauma
- Myocarditis
- Reperfusion of cardiac cells after a myocardial infarction
- Medications
- Adenosine
- Clonidine
- Antiarrhythmics
- Lithium
- Digoxin
- Sleep apnea
- Hypoxia
- Coronary artery disease
- Congenital cardiac defects and repairs of these defects
- Electrolyte imbalances
- Treatment:
- None if asymptomatic
- Medications
- Atropine
- Reversal agents
- Transcutaneous pacing
- Permanent pacemaker
- Treatment of the underlying cause
Bundle Branch Blocks (BBB) (43, 53, 70):
- Rate: varies
- Conduction:
- Right BBB (RBBB):
- QRS interval greater than 120ms
- Septal depolarization that leads to a:
- Small R wave being present in V1
- Q wave in V6
- The left ventricle’s contraction leads to and:
-
- S wave in V1
- R wave in V6
-
- The right ventricle’s contraction leads to an:
- R wave in V1
- Deep S wave in V6
- Left BBB (LBBB):
- QRS interval greater than 120ms
- T wave inversion is due to abnormal repolarization
- From first principles:
- Septal depolarization that leads to a:
- Q wave in V1
- R wave in V6
- Right BBB (RBBB):
-
-
- The right ventricle’s contraction leads to an:
- R wave in V1
- S wave in V6
- The left ventricle’s contraction leads to and:
- S wave in V1
- R wave in V6
- The right ventricle’s contraction leads to an:
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- Rhythm Strip:
- RBBB
- The maximum height of the P wave is:
-
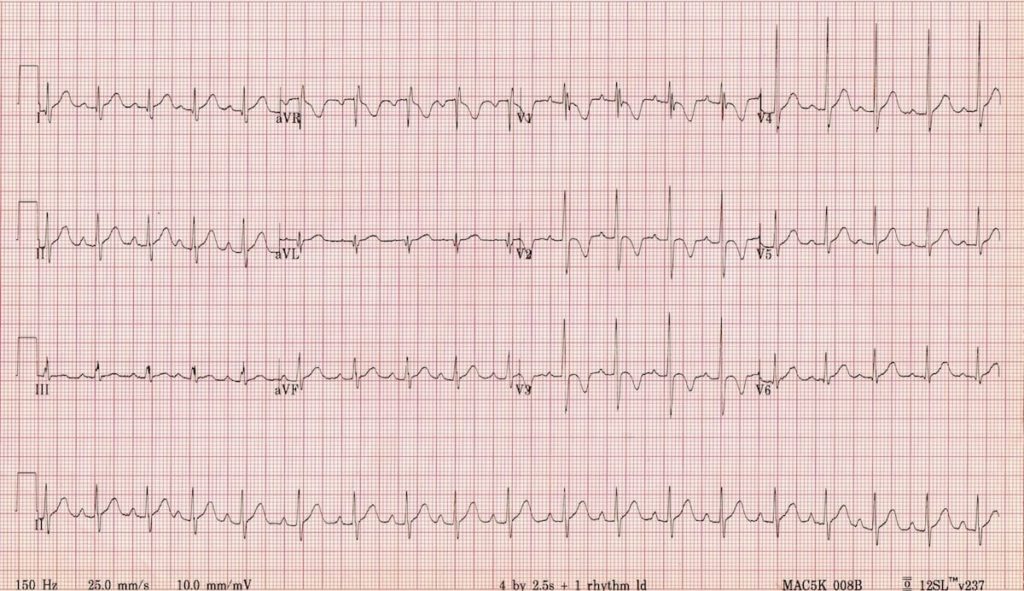
(71)
-
-
-
- LBBB
-
-
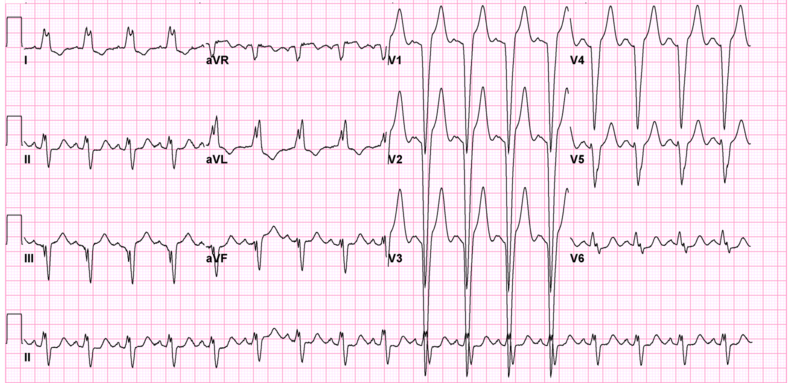
(71)
- Signs and Symptoms:
- None
- Lightheadedness
- Syncope or near syncope
- Causes:
- RBBB:
- Myocardial infarction
- Congenital cardiac defects
- Pulmonary embolism
- Myocarditis
- Pulmonary hypertension
- LBBB:
- Myocardial infarction
- Hypertension
- Cardiomyopathy
- Myocarditis
- Treatment:
- None if asymptomatic
- Treatment of the underlying cause
- RBBB:
Identifying Ischemia and Infarction
Known as coronary artery disease (CAD), acute myocardial ischemia is the decrease of blood flow to the heart by atherosclerosis or plaque. The atherosclerosis starts as a plaque streak within the large arteries and continues to build up. After the plaque has grown to a significant size, occlusion begins and blood flow to areas below the growing occlusion suffers a decrease in blood flow. This is what is known as ischemia (81).
When resting, patients may not experience any signs or symptoms. Upon exertion, however, patients may experience stable angina—chest pain, discomfort, pressure, etc.—as activity requires increased blood flow and the arteries constrict to pump blood through the body faster. This pain is relieved at rest and can be further treated by nitrates. The routine is what makes this stable angina (81).
Unstable angina begins once the artery has become occluded enough to create a significant obstruction of blood flow. Signs and symptoms can include chest pain or other discomfort that is challenging to relieve, even when at rest. Patients may be woken from sleep due to the pain and report that it takes longer for the pain to decrease or resolve completely. These signs and symptoms symbolize that the plaque within the artery is unstable and could potentially rupture (90).
Infarction is when the blood flow is completely obstructed and the cells below the obstruction begin to die off. This often occurs when the plaque within the artery ruptures, leading to the body’s natural clotting processing in an attempt to repair the rupture, and a complete occlusion of the artery occurs (46).
Now that we have discussed ischemia and infarction, it is time to discuss how a myocardial infarction (MI) appears on an EKG and how to identify it. You may also hear them referred to as STEMIs or ST-elevation myocardial infarction.
The progression of PQRST complex changes during an MI can start with hyperacute T waves. The T wave will increase with amplitude and become wider, while some ST elevation may be noted. This elevation begins to occur as injury to the heart muscle begins. From there, the ST elevation increases and creates the image often associated with an MI. Pathological Q wave may develop as the MI progresses. As discussed earlier, the Q wave is the first downward deflection of the QRS complex and is normally 1mm or less in depth. Pathological Q waves are measured by greater than 1mm wide or greater than 25% of the R wave’s amplitude (84).
T wave inversion occurs when the cells have become necrotized and begin to form fibrosis. Once all necrotized cells have become fibrotic, the Q waves will remain, but the T waves will become upright again (84).
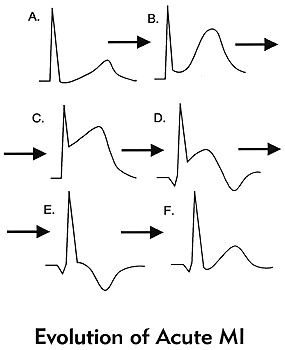
(84)
These changes should be present in at least 2 contiguous leads or leads that are side by side. To discuss this more, we will refer to the 12 lead EKG photo we used earlier. It is important to know that there will be leads with ST elevation and there will be leads with reciprocal ST depression based on the type of MI and how these leads are placed in relation to the area of the heart that is being affected.
| Type of MI | Leads with ST Elevation | Reciprocal ST Depression |
| Inferior | I, II, AVF | I, AVL |
| Lateral | V5, V6 | III, AVR |
| Anterior | I, AVL, V5, V6 | II, III, AVF |
| Posterior | V7, V8, V9 | V1, V2, V3 |
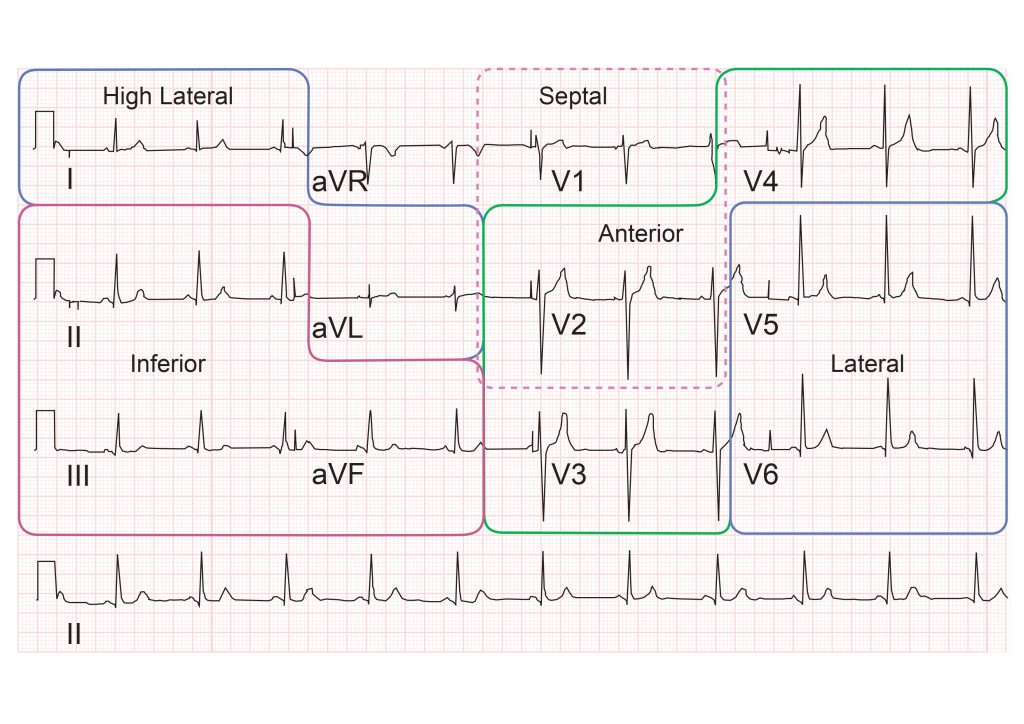
(82)
With posterior MIs the elevation must be at least 0.5mm, there will be tall, broad R waves of at least 30ms long, and the T wave will be upright. When looking at an EKG for a posterior MI, the ST depression is what will be observed in leads V1, V2, and V3. If a posterior MI is suspected, look at the EKG from the back of the paper by flipping it over and holding it to light. This will display the ST depression as ST elevation, prompting you to consider a posterior EKG. It is advised that a posterior EKG with leads V7, V8, and V9 be done. A quick method to do this is by removing leads V4, V5, and V6; placing them in the posterior lead positions; and relabeling them on the EKG. (77).
Right ventricular MIs can occur, and it is important to assess and treat them appropriately. To assess for a right-sided MI, first look at the standard EKG. If ST elevation is noted in leads II and III, but the ST elevation is greater in lead III than lead II, consider right ventricular involvement. As discussed previously, one method is to do a right-sided EKG, with lead placement along the right side of the chest. The second, quicker way to do this is to take lead V4 and place it on the right side of the chest and mark it as V4R on the EKG (77).
Another rhythm that can be an indicator of an MI is a bundle branch block. New or suspected new BBBs are to be treated as a MI by providers. But what if you have a copy of an old EKG and the BBB isn’t new, can the patient still be having an MI? The answer is yes. However, it can be challenging to determine what is a change from the MI and what is from the BBB. The Sgarbossa criteria is useful in making these determinations and can also be used for patients who have a pacemaker (77)
Sgarbossa criteria (77):
- Concordant ST elevation that is greater than 1mm
- Concordant ST depression that is greater than 1mm
- Excess discordant ST elevation that is greater than 5mm in leads with negative QRS complexes – these are complexes below the isoelectric line
For reference, concordance means that the ST segment and QRS complex go in the same direction, either both deflecting upwards or downwards. Discordance is what should be seen in a BBB or paced rhythm. This is where the ST segment and the QRS complex go in different directions. Smith et al. created a modification to the Sgarbossa criteria to include a greater than 1mm ST elevation to an S-wave amplitude ratio of greater than 0.25mm (7).
Another method that has been created, but not validated is the Barcelona criteria. This criterion has greater than 1mm ST deviation concordance or discordance with QRS polarity in any EKG lead. Discordant ST deviation is greater than 1mm in any lead where the R or S points of the QRS complex are less than 6mm (7).
There is an EKG rhythm that can indicate a future MI which is known as Wellens syndrome. This EKG has a deeply inverted or biphasic T wave in leads V2 and V3. The patient is often pain-free when the rhythm is present, ischemic chest pain can obscure the rhythm by creating a false normal appearance of the T waves in the affected leads. Their cardiac enzymes may not even be elevated. Any patient presenting with chest pain should have serial EKGs done for this reason, since they may be pain-free at a later time. These EKG changes symbolize the critical stenosis of the proximal left anterior descending artery (LAD). This is the artery that provides the left ventricle with blood (65).

Self Quiz
Ask yourself...
- Do you remember the first patient that you had that was experiencing an MI? What stood out about that patient in your mind?
- Patients have a variety of symptoms that can be experienced during an MI, what was the most interesting symptom a patient had during an MI?
- Have you ever encountered a patient with Wellens Syndrome? Do you know if they ended up having an MI later?
Cardiac Assessment:
A traditional cardiac assessment focuses on more than just the heart; it encompasses aspects of both the neurological and respiratory systems. However, we will begin our focus with the heart.
Pain may not be a word patients use to describe what they are feeling. As mentioned, they may vocalize discomfort, pressure, cramping, burning, or tightness. Women may have jaw or arm pain as opposed to the traditional chest pain that men may experience. Ask them to rate their pain on a scale of one to ten, looking for changes in the value. An EKG based on pain, discomfort, pressure, cramping, or tightness should be completed within the time frame set by hospital policy.
The PQRST pneumonic can assist providers in remembering the specific information they need to collect (90).
P: What provokes, precipitates, or palliates/alleviates the pain or discomfort the patient is feeling? Does it get worse or better when you do certain things, i.e., walk or rest?
Q: What is the quality of pain or discomfort you are feeling?
R: Does this pain or discomfort radiate anywhere else in your body? Jaw, arm, back?
S: Are there associated symptoms with the pain or discomfort? Shortness of breath, dizziness, heartburn?
T: What time elements are involved? When did it start? Did it stop and come back? Are you currently feeling it now? Was it gradual or did it occur suddenly? Did it wake you up?
Patients should be asked about palpitations or any experienced abnormal heart rhythms detected on monitoring devices. Many individuals have smartwatches that can detect heart rates and some rhythms. If the patient is wearing one, determine if the device has recorded anything.
Edema in the legs can be a sign of acute heart failure while pain in the calf can indicate a blood clot that could have traveled from another part of the body (85). In A Fib, the blood can clot in the ventricles due to poor circulation of blood. It will pool until it clots or is ejected from the heart. Once expelled, the clot will travel until it can no longer pass through the veins (63). Ensure a thorough assessment of the patient’s distal pulses is done as well to determine circulation. The further pulse locations can be an indicator of poor circulation (85).
Moving on to the respiratory system, we will reflect on the many arrhythmias that have shortness of breath as a sign or symptom. Providers should assess lung sounds to determine if there is any fluid buildup, a sign of acute heart failure. Determine if the shortness of breath is all the time, upon exertion, or at rest. Also, it is important to ask if the patient has been woken from sleep due to a shortness of breath. Sometimes arrhythmias occur at unexpected moments, even in the middle of the night (85).
Syncope was another common sign or symptom of cardiac arrhythmias due to decreased perfusion to the brain. Providers should determine if the patient currently feels lightheaded or dizzy, if they felt that way in the past, or if they have fainted. They should ask when this feeling happens—at rest, while moving, or both—and if they get any warning signs or auras beforehand. Always ensure you ask the patient to describe what happened so it can be added to the assessment (85).
A full medical history should be obtained, with a special focus on any past cardiac medical history the patient or their family has. Providers may consider asking the following questions:
- Have you been diagnosed with coronary artery disease, high blood pressure, peripheral vascular disease, valve problems, heart failure, high cholesterol, or other heart conditions?
- Have you had a heart attack or stroke in the past?
- Have you had any surgical procedures to help with your heart function? This may include things like ablation or stent placement.
Asking about medications can assist providers in determining any missed diagnoses with the patient while asking about social history can provide information about smoking, illicit drug use, alcohol consumption, and exercise habits (85).
Conclusion
Thanks to advancements within the medical profession, cardiac telemetry can be greatly beneficial to patients in and outside of the hospital setting. From devices you can carry, to devices implanted inside someone, patient outcomes have improved for identifying, treating, and managing cardiac arrhythmias that had once been deemed unmanageable. With proper knowledge of EKG rhythms, nurses can confidently provide the proper care for their patients by being an advocate for those they care for.

Self Quiz
Ask yourself...
- Have you seen changes in the patients admitted to your facilities that you could correlate to these indications?
- Do you agree with this list? Is there anything you feel should be added or removed? Why?
- Are there any time frames (how long a patient is on a telemetry monitor) that you think should be adjusted?
- Do you think sending patients home with wearable monitors could be used in the future to prevent admission in some of the patients who meet the criteria for admission with telemetry?
Conclusion
Thanks to advancements within the medical profession, cardiac telemetry can be greatly beneficial to patients in and outside of the hospital setting. From devices you can carry, to devices implanted inside someone, patient outcomes have improved for identifying, treating, and managing cardiac arrhythmias that had once been deemed unmanageable. With proper knowledge of EKG rhythms, nurses can confidently provide the proper care for their patients by being an advocate for those they care for.
Tirzepatide for Type 2 Diabetes and Weight Management
Introduction
The emergence of the drug tirzepatide is becoming more popular and widespread and is being utilized among those with diabetes and also those who desire to lose weight. It is one of the newest diabetic drugs given by injection that also triggers dramatic weight loss in those who use the injections.
The U.S. Food and Drug Administration (FDA) approved tirzepatide in 2022 for individuals with diabetes, particularly Type 2 Diabetes. The FDA officials have not approved tirzepatide yet for weight loss, but they are currently tracking the medication and may have a recommendation for its approval by the end of this year. Clinical trials have shown that individuals with an elevated body mass index (BMI) and who did not have diabetes lost a considerable amount of weight when they received tirzepatide (1).
Advanced Practice Registered Nurses (APRNs) need to understand how to safely prescribe tirzepatide and the reasoning as to why it causes weight loss for specific individuals.
Drug Classification
Tirzepatide is part of a class of medications called glucose-dependent insulin tropic polypeptide (GIP) receptor and glucagon-like peptide-1 (GLP-1) receptor agonists. It comprises a 39 amino acid linear synthetic peptide conjugate to selective receptor agonists in preclinical and clinical trials.
Tirzepatide is used for treating Type II diabetes in adults as an adjunct to diet and exercise. It is also used for weight loss in some individuals and has gained increased attention as a new therapeutic agent for glycemic and weight control.
Social media has had a significant influence and increased the desire to use tirzepatide, and while individual results vary, the weight loss in adults ranged from 12 – 25 pounds.
Online pharmacies, diet clinics, and medical spas are implementing thousands of ads on social media to capitalize on a surge of interest in the drug.

Self-Quiz
Ask Yourself...
- Why has there seemed to be an increase in patients requesting this medication? What other medicines intended for type 2 diabetes are also being used for weight loss management?
- What are the ethical considerations regarding marketing this drug for weight loss when its primary use is for type 2 diabetes? Could this impact supply and costs?
Indications of Usage
The use of tirzepatide is being used for both Type II diabetes and weight control in certain patients. It has been a game changer for people living with Type II diabetes. The drug’s primary use is as an adjunct to diet and exercise to improve glycemic control in adults with diabetes.
The drug has also proven beneficial for weight loss in patients experiencing obesity, and those who are taking the highest dosage have shared a body weight reduction of 15.7% (2). Tirzepatide is an injectable prescription medication used together with diet and exercise, and it is not yet known if it can be used safely with patients who have had pancreatitis.
It is important to remember that it is not to be used for patients with Type I diabetes, but it is safe for Type II diabetic patients. Also, the safety of tirzepatide has yet to be discovered for children and those under 18; therefore, the medication should not be used for this age group.
In studies conducted with or without diabetic medicines, 75% – 90% of patients taking tirzepatide reached an overall A1C of less than 7% with an average starting A1C of 7.9 – 8.6% across the following dosages – 5mg, 10mg, and 15mg. The study results were measured at weeks 40 and 52 (3).

Self-Quiz
Ask Yourself...
- What dietary and activity recommendations can you provide to patients using tirzepatide for weight loss?
- Is this drug intended for those who want to lose 5-10 pounds?
Use of Tirzepatide with Diabetic Patients
Tirzepatide can be used for patients with Type II diabetes in combination with a diabetic-friendly diet and exercise. The drug works by lowering the patient’s overall blood sugar and also improves the A1C results of patients over some time. The injection has been approved by the FDA to treat Type II diabetes and is administered once weekly (4).
It is considered the first in a new class of medications – a dual glucose-dependent insulin tropic polypeptide (GIP) and glucagon-like-peptide-1 (GLP-1) receptor antagonist. The mechanism of how it works mimics two gut hormones (GIP and GLP-1). These hormones are essential in how patients digest food and regulate blood glucose after meals. The hormones also play a role in making individuals feel fuller and curb specific food cravings.
The provider can prescribe tirzepatide before attempting other diabetic medications if a patient has a BMI of 30 or greater or 27 or greater with weight-related conditions and if the drug is combined with a personalized weight loss plan that addresses physical activity, nutrition, and lifestyle changes.
However, due to the cost and some insurance companies not covering the injection unless the patient has both diabetes and obesity, the provider must carefully consider prescribing this medication.

Case Study
The patient states this ‘miracle drug’ is worth paying for out of pocket!
Jeff Capron, a 53-year-old Boonville, New York, web developer, started taking tirzepatide in December 2022. His friend had reported good results with the medication, so Jeff looked into the research studies behind it and then spoke with his primary physician.
The physician said, “Yeah, let’s give it a shot,” even though he did not have much experience with it. The physician did not have an opinion one way or the other than looking at the data set and seeing no reason why they could not try it.
Jeff’s hemoglobin A1C went from 10.1% to 6% in 3 months, which was very promising. “I never had that kind of experience with any medication for diabetes.” There is a range in how much A1C reduction people experience with tirzepatide, but many people taking it can get their A1C under 7% — an ideal goal for people with Type 2 diabetes.
Jeff experienced constipation and a little trouble sleeping early, but both issues disappeared quickly. He says, “I wake up in the morning, and my fasting blood sugars are normal.”
The medication took effect, he says, within 12 hours. He compared the feeling to having a gastric bypass.
“You cannot overeat food. As soon as you overeat, you almost feel ill.” While it generally takes a few months to notice effects like A1C reduction and significant weight loss, side effects such as lower appetite may be felt immediately.
Weight loss was not his primary goal, but he lost about 35 pounds on the medication in the first five months. He also lost his sweet tooth. “I can maybe count three sweet things I have eaten since December.”
Jeff found that his appetite slowly recovered days after taking tirzepatide. “You take the shot every Sunday, and by Saturday, you start to get a lot of appetite,” he says. “It does not seem to affect your weight. If I eat a little bit more on Saturday night, on Sunday, the scale will not move one way or the other.”
Jeff is allergic to hornets, so he already carries an auto-injector. He was not worried about using another drug delivered through a needle. “It’s just a push button,” he says. It also helped that his wife is a nurse. “So, I had her with me the first time to ensure I was doing it right. I didn’t even feel it.”
When Jeff was first prescribed tirzepatide, his insurance covered it. The company has since removed that benefit. He has filed an appeal but pays about $1,000 monthly out of pocket for his weekly injections. He plans to keep paying as long as necessary.
He considers the financial burden well worth it. “I have never had a medication that worked as well before for chronic conditions,” Jeff says. “I’ve been blown away by it. For me, it’s a miracle drug. It got rid of my diabetes” (4).

Self Quiz
Ask yourself…
- Can a provider willfully choose to prescribe tirzepatide before other diabetic medications are attempted?
- Would that impact his insurance coverage if Jeff did not meet the clinical criteria for using tirzepatide?
Use of Tirzepatide for Weight Loss Management
As mentioned, this medication is indicated for patients with a BMI of >30 or a BMI of >27 with qualifying comorbidities. Obesity can become a chronic lifetime disease, and for conditions such as these, the patient needs to implement therapy for the lifetime of the disease.
In a study conducted for tirzepatide, there was a dramatic increase in effectiveness compared to traditional nonsurgical interventions such as diet, exercise, and lifestyle changes. However, it has been noted that taking tirzepatide on an ongoing basis is recommended and necessary to maintain any weight loss achieved from the medication.
If a patient stops taking the drug, likely, it will no longer work (5).
Public health officials have expressed concerns about using the drug long-term. Still, data is currently lacking regarding long-term effectiveness, treatment duration, and maintaining weight reduction once the therapy is discontinued.
A recent trial consisted of 783 participants with a BMI greater than 30, and these participants agreed to take either a 10mg or 15mg dose of tirzepatide over 36 weeks. The injection is given once weekly, so this would equal a total of 36 injections.
By the end of 36 weeks, participants lost more than 21% of their body weight. After 36 weeks, participants continued on tirzepatide or received placebo treatment for the following year. The patients needed to be made aware of which treatment they were receiving.
Those still taking tirzepatide injections weekly after 88 weeks lost an additional 7% of their body weight, and those taking the placebo regained 15% at the end of 88 weeks (5).

Self Quiz
Ask yourself…
- What is the minimum BMI needed to qualify to receive this drug for weight loss management?
- Is this medication indicated for long-term use for patients with a high BMI?
Common Side Effects and Contraindications
Side Effects
Patients vary immensely with different experiences and side effects related to tirzepatide; however, the following are the most common side effects experienced by those taking the medication:
- Nausea
- Decreased appetite
- Vomiting
- Diarrhea
- Indigestion
- Constipation
- Stomach Pain
Tirzepatide usually does not cause fatigue, leaving one feeling weak, tired, and low energy. However, fatigue can be a common side effect of Type II diabetes.
It is important to note that most individuals who experience nausea, vomiting, and diarrhea episodes do so while the dosage increases, and typically, the symptoms decrease over time. G.I. effects were more prominent in those taking tirzepatide than those taking the placebo. The individuals not in the placebo group were more likely to stop treatment due to the unpleasant side effects (3).


Self Quiz
Ask yourself...
- Does tirzepatide cause fatigue in patients who use it?
Contraindications
Tirzepatide may cause thyroid tumors, including thyroid cancer, and it is essential to watch for possible symptoms, such as swelling or a lump in the neck, hoarseness, shortness of breath, or trouble swallowing.
Tirzepatide should also not be prescribed to any patient with Type 1 Diabetes.
One of the main ways that tirzepatide works is by stimulating the release of insulin from the pancreas, and due to this fact, there have not been many studies and clinical trials that include those with Type I diabetes.
However, this is not to say that prescribers have never ordered tirzepatide for those with Type I diabetes. Still, it is essential to note that if prescribed, it would be in addition to traditional insulin therapy.
- Personal or family history of a type of thyroid cancer known as medullary thyroid carcinoma (MTC).
- Any history of Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
- Patients who are allergic to the actual medication or any of its ingredients.
- Younger than 18 years of age


Self Quiz
Ask yourself...
- What is the reason that tripeptide is contraindicated in those with Type I diabetes?
- Why is there a risk with patients who have a thyroid disorder?
Safe Prescribing Practices, Guidelines, and Considerations for Providers
Safe Prescribing Practices
As with all prescribed medications, safe standards of care must be implemented and followed to ensure patient safety is maintained. The same applies to providers considering prescribing tirzepatide, and specific criteria must be met beforehand. The following information discusses guidelines involving exclusion and inclusion criteria for providers to prescribe tirzepatide (6) accurately.
Guidelines
Exclusion Criteria – If present, the following indicates that the patient should not receive tirzepatide:
- Diagnosis of Type I diabetes
- Personal or family history of medullary thyroid carcinoma or with Multiple Endocrine Neoplasia syndrome type 2
- Severe gastrointestinal dysmotility
- History of pancreatitis
- Pregnancy
- Proliferative Diabetic Retinopathy (PDR), severe Nonproliferative Diabetic Retinopathy (NDR), clinically significant myalgic encephalomyelitis (M.E.), or diabetic macular edema (DME) unless the risks/benefits have been discussed with the patient and are documented in the patient's health record along with monitoring plans and follow-up with an eye specialist who is informed at the time of initiation.
Inclusion Criteria – All of the following must be met for tirzepatide to be prescribed:
- Diagnosis of Type II diabetes
- A BMI of 25 or greater
- Inadequate glycemic control on at least 1mg of semaglutide injection plus two or more glucose-lowering drugs
- Change needed to achieve goal A1C is less than 1%.
- Goal A1C should be based on those recommended in the Diabetic Guidelines.
- Adherence to current diabetic medications as evidenced by a review of the prescription refill history during the six months.
Additional Inclusion Criteria – All of the following must be met for tirzepatide to be prescribed:
- Patients with atherosclerotic cardiovascular disease or chronic kidney disease
- Patients of childbearing potential who are using oral contraceptives
Inclusion Criteria for Weight Loss
- BMI of >30 or >27 with patient weight conditions.

Self Quiz
Ask yourself...
- Would a patient with a BMI of 23 with no comorbidities qualify to use tirzepatide to lose 5-10% of their body weight? Why not?
- What impact can tirzepatide have on a person with a healthy weight and BMI of <25?
Considerations for Providers
There are specific considerations that prescribers must be aware of when contemplating if a patient should receive the medication tirzepatide. The following is imperative and must be considered each time the medication is prescribed to a patient:
- Clinical Indications – indicated for treating adults with insufficiently controlled diabetes mellitus as an add-on therapy to diet and exercise; as monotherapy when metformin is considered inappropriate due to contraindications or intolerance; and other medicinal products for treating Type II diabetes.
- Monitoring of medication – routine monitoring of serum calcitonin or thyroid ultrasound is of uncertain value but is recommended for early detection of Medullary Thyroid Cancer (MTC).
- Cost – the average price for tirzepatide ranges from $1,071-$1,351 without any coupons or insurance. Savings Card – manufacturer provided; patients can pay as little as $25 monthly for up to 12 injections. Savings Card – manufacturer provided; patients can pay as little as $25 monthly for up to 12 injections.
- Benefits and Risks – One must evaluate the effectiveness of diabetes and the weight loss experienced. Some of the risks must be evaluated, such as increased cost of medication, unpleasant gastrointestinal side effects, poor insurance coverage, and drug shortages. The FDA has warned that the medicine can cause thyroid C-cell tumors in rats, and it is not sure whether tirzepatide causes similar tumors.
How long does it take for tirzepatide to begin working?
Tirzepatide will start to lower one's blood sugar levels immediately, but it can take 8 to 12 weeks to reach one's target A1C goal.
Compared to other diabetic treatments, studies have shown that it can take eight weeks to reach an A1C target of less than or equal to 7% and 12 weeks to get an A1C of less than or equal to 6.5%. Significant weight loss can occur as early as 28 weeks.
Safe Administration
It is essential to follow the correct steps for safe administration of tirzepatide as listed below:
- The recommended starting dosage is 2.5mg, injected subcutaneously once weekly. The 2.5mg dosage is for treatment initiation and not for glycemic control.
- After four weeks, increase the dosage to 5mg, injected subcutaneously once weekly.
- If additional glycemic control is needed, increase the dosage in 2.5mg increments after at least four weeks on the current dose.
- The maximum dosage is 15mg, injected subcutaneously once weekly.
- If a dose is missed, instruct patients to administer it as soon as possible, within four days (96 hours) after the missed dose. If more than four days have passed, skip the missed dose, and administer the next dose on the regularly scheduled day. In each case, patients can then resume their regular once-weekly dosing schedule.
- The day of weekly Administration can be changed, if necessary, as long as the time between the two doses is at least three days (72 hours).
- Before initiation, train patients and caregivers on proper injection techniques.
- Instruct patients using the single-dose vial to use a syringe appropriate for dose administration (e.g., a 1ml syringe capable of measuring a 0.5 mL dose).
- Administer the medication once weekly, any time of day.
- Inject the medication subcutaneously in the abdomen, thigh, or upper arm.
- Rotate injection sites with each dose.
- Inspect the medication visually before use. It should appear clear and colorless to slightly yellow. Do not use the medicine if particulate matter or discoloration is seen.
- When using the medication with insulin, administer it as separate injections and never mix. It is acceptable to inject tirzepatide and insulin in the same body region, but the injections should not be adjacent.
Does the tirzepatide injection hurt when administered?
Pain from the injection site has not been reported as a common side effect, but it may occur.
Due to the injection being given subcutaneously, slight pain or discomfort can occur.


Self Quiz
Ask yourself...
- The patient asks you," How long will this take to work?" How will you respond?
- The patient reports they have never used an injection before; what methods can you use to teach your patient how to administer this medication safely?
Alternatives to Tirzepatide for Weight Loss Management
In some instances, patients need to be aware of alternatives to tirzepatide in case they cannot take the actual injection for whatever reason. In cases such as these, there are alternative supplements that can be purchased over the counter, and they include the following (7):
- PhenQ – top OTC choice – comprehensive weight loss solution that targets specific body regions, facilitates prompt fat loss, and expedites the weight loss journey.
- PhenGold – the most potent OTC weight loss alternative – one of the top weight loss supplements that boost metabolism, making one less hungry, less tired, and an overall improved feeling.
- Capsiplex BURN – the best choice for men – helps to burn fat faster and keep blood sugar levels in check. It helps to keep one's muscles, curbs hunger, gives one more energy, and torches stubborn fats.
- Trimtone – the best choice for women – helps women to lose weight, eat less, increase metabolism, burn extra calories, and boost energy.
- Prime Shred – best fat burner for men – boosts metabolism, keeps muscles intact, increases energy, and helps maintain focus.
The advanced practicing nurse or prescriber needs to inform patients about alternative options such as these in an effort for individuals to understand that other choices are available and can be used. Many individuals need to be more knowledgeable about alternatives besides tirzepatide due to the extra hype from social media sources that promote advertisements related to tirzepatide only but do not mention the other options.
Why does social media influence and encourage patients to take tirzepatide?
Social media trends can be helpful but can also become harmful by setting unrealistic expectations and promoting a diet culture mentality. They can create an unhealthy obsession with "clean" eating, especially in the younger populations.
Due to this, many individuals take the medication despite any occurrence or history of Type II diabetes, and the drug can ultimately become misused.
It has been noted that there is an influx of patients requesting this medication for weight loss instead of the intended purpose, which is to help control Type II diabetes.
Tirzepatide represents one of the most recent non-medical treatments aimed at managing the symptoms of Type II diabetes. While it is not indicated for weight management, diabetic patients who receive it frequently report a significant reduction in body weight.
Empirical evidence suggests the efficacy of tirzepatide in weight management, and certain physicians currently endorse the Administration of the medication as a therapeutic and effective means to overcome obesity.
What are some severe side effects of tirzepatide that can impact patient safety?
The Administration of tirzepatide can benefit many individuals, but some severe side effects must be mentioned.
These include thyroid tumors, thyroid cancer, pancreatitis, hypoglycemia, serious allergic reactions, kidney issues, severe stomach problems, vision changes, and gallbladder issues. All these side effects must be taken seriously and reported, as they can lead to life-threatening

Self Quiz
Ask yourself...
- With what you have learned in this course, what education will you provide to patients requesting this medication for weight loss?
- Have you seen increased demand for this medication in your current practice?
- If you Google tirzepatide, your results will likely include links to telehealth services promoting this weight-loss medication. To determine eligibility, what special considerations need to be taken to assess a telehealth patient?
Conclusion
Medications like tirzepatide are game changers for those patients with type 2 diabetes that have failed other medications. Unfortunately, several companies seek to profit from its weight-loss benefits through aggressive marketing campaigns that limit the available supply and increase the costs for those who need it. As healthcare providers, we need to use sound clinical judgment and follow the exclusion/inclusion criteria and other guidelines before prescribing this medication, so we do not unintentionally cause harm while looking to appease our patients who request this.
Semaglutide and Type 2 Diabetes
Introduction
In 2017, the FDA approved the semaglutide injectable (Ozempic) for treating type 2 diabetes. The drug has experienced widespread acceptance due to its positive effects on weight loss and lowering of chronic health risks. The drug has risen in popularity over the past few years, as many well-known actors/actresses/songwriters, and more came forward, publicly sharing their weight loss journey.
This rise in popularity has also resulted in significant shortages of this medication, negatively impacting the lives of the diabetic community, local pharmacies, and healthcare providers. The goal of this continuing education course is to educate and empower the healthcare provider in all aspects of this drug regimen: clinical indications, patient education, cost options, and benefit/risk analysis.
Diabetes Overview
Diabetes is a chronic medical condition. Despite advances in diet, medications, and monitoring devices, diabetes diagnoses continue to grow at staggering rates. The Institute for Health Metrics and Evaluation (IHME) reports that over 529 million people worldwide are currently living with diabetes, and that number is expected to grow to 1.3 billion in only 30 years. While the risk factors for diabetes are vast in number (poor diet, inadequate activity, obesity, sedentary lifestyles, daily stressors, and more), the sad reality is that this chronic medical condition will most likely linger on for generations to come despite our efforts to contain this health epidemic (1).
According to the latest research on diabetes, there are over 37 million people in the United States alone with diabetes as of 2022. Statistically, approximately 28 million of them have a confirmed diagnosis, while another estimated 8 million are experiencing symptoms, without an official diagnosis. Diabetes currently ranks as the 7th leading cause of death in the United States (2).

Self Quiz
Ask yourself...
- As a healthcare provider, what has been your experience with treating chronic medical conditions?
- Why do you think there is a continued increase in diabetes, despite advances in medication and monitoring devices to treat this condition?
- Are you currently offering comprehensive care to your patients, including medication, diet, and activity counseling for their chronic health conditions?
Types of Diabetes
In basic terms, diabetes is an impairment in one’s ability to either adequately produce or utilize insulin, which results in elevated levels of circulating glucose. Chronically elevated glucose levels affect blood vessels at every level, causing chronic inflammation and raising the risk of heart disease, stroke, blindness, and atraumatic amputations.
There are three main types of diabetes:
Type 1 diabetes is thought to be an autoimmune disease. Approximately 5-10 percent of people with diabetes are diagnosed with type 1 diabetes. The diagnosis usually occurs in early childhood, and results in a lifetime use of insulin to regulate blood glucose levels.
Type 2 diabetes is thought to be related to dietary and lifestyle choices. It accounts for nearly 90-95 percent of diabetes diagnoses. Usually occurring later in life (adult-elderly population), it is believed to be related to factors such as diet, activity, weight gain, and related factors. Type 2 diabetes is usually controlled by diet and exercise, in addition to oral medications, although injectable insulin may be included in the treatment plan.
Gestational diabetes refers to elevated glucose levels occurring during pregnancy for patients who are not diabetic at the onset of pregnancy. This version of diabetes usually resolves itself post-partum, although a woman may develop type 2 diabetes later in life, unrelated to pregnancy.
Type 2 diabetes in children: no longer a “later in life diagnosis”
Children are now being diagnosed with type 2 diabetes at an alarming rate. Despite widespread education and an increased awareness of diabetes, our up-and-coming generation is unhealthier than ever. Many families lack access to healthy food for their families, due to both general socioeconomic challenges and an increased rate of food insecurity. (19)
The CDC recommends care providers have resources for diabetic patients and their families, such as food and nutrition programs, budget-friendly diabetes meal plans, how to save money on diabetes care, and coping strategies for diabetes. (19)


Self Quiz
Ask yourself...
- Are you able to articulate the different types of diabetes to patients?
- What resources can you offer to the families of children with type 2 diabetes?
Diabetes Signs and Symptoms, Diagnostic Testing
There are various ways to test for diabetes. The fasting blood sugar (FBS)/ fasting glucose level is a simple way to test for diabetes.
The normal fasting glucose level is below 100mg/dl. The fasting glucose result of 100-125mg/dl indicates prediabetes and results above 126mg/dl indicate diabetes.
The hemoglobin A1C blood test is another test used to confirm the diagnosis of diabetes. The patient does not need to be fasting for this test; thus, it is easier to order this test regardless of the time of day. This blood test reflects the average glucose level over the period of 2-3 months.
The normal A1C level is below 5.7%. Test results between 5.7%- 6.4% indicate prediabetes. Test results above 6.5% indicate diabetes.
A random glucose reading above 200mg/dl, done at any time of day, indicates diabetes.
The diagnosis of diabetes is by blood tests, and for improved accuracy, should be based on two separate readings, done (at least) a day apart. In the case of fasting and random blood tests, dietary intake (large amounts of carbohydrates in a single meal) may adversely affect test results. This is not the case when using A1C testing for a confirmation diagnosis, as the results are the average of a 2–3-month span.
Target blood levels for a person with diabetes (3).
Target blood glucose levels for people with diabetes are as follows:
- Fasting glucose 80-130mg/dl.
- Postprandial blood glucose level- less than 180mg/dl
- A1C level 7-8%.
These target ranges are general guidelines. Patient-specific ranges will be dependent on a variety of factors, including preexisting comorbidities, overall health status, age, and activity levels.

The hallmark signs/symptoms of diabetes
- Polyuria- increased urination
- Polydipsia- increased thirst
- Polyphagia-increased hunger/appetite
The truth is, as healthcare providers, you will have patients who have no hallmark signs and symptoms of diabetes; the diagnosis will be found during annual preventive examinations often unrelated to any chronic disease. For this reason, many insurance companies now cover numerous preventive screenings, including diabetes screenings, as part of their wellness and prevention initiatives. These tests are often approved based on a patient's age, or preexisting conditions, rather than outright signs and symptoms.

Self Quiz
Ask yourself...
- What are the typical glucose levels for non-diabetic versus diabetic patients?
- What are the hallmark symptoms you can identify when treating a potentially diabetic patient?
Lifestyle Interventions and the Diabetes Prevention Program
The initial diagnosis of diabetes can be managed in a variety of ways, depending on the severity of the illness at the time of diagnosis. Lifestyle interventions (behavior modification education) are of utmost importance in the care and management of people with diabetes. Research over the past few decades has consistently shown that such interventions have immense positive effects on the successful long-term management of diabetes.
The official Diabetes Prevention Program was created in 2010 (4) and confirmed the effects of lifestyle interventions in the management of diabetes: Lifestyle interventions decreased the incidence of type 2 diabetes by 58% compared with 31% in the metformin-treated group. Thus, these findings now serve as the blueprint, if you will, for all-inclusive, patient-specific disease management guidelines. These lifestyle interventions will be discussed in detail later in the program.
Additional Resources on Diabetes Prevention

Self Quiz
Ask yourself...
- How do lifestyle interventions compare to other kinds of treatment for patients with type 2 diabetes?
Semaglutide
Semaglutide is an injectable drug used in the treatment of type 2 diabetes. It was approved by the FDA in May of 2017.
It is a once-a-week injectable and belongs to the drug class known as glucagon-like peptide-1 receptor agonists (GLP-1RAs) (5). It has been referred to as a “miracle weight loss drug” among those who are living with obesity, despite frequent side effects, unusually high out-of-pocket costs, drug shortages, and weight regain when attempting to stop using the medication.
GLP-1 receptor agonist: Hormone Review
GLP-1 RAs are a class of medications used to treat Type 2 diabetes, and in some cases, obesity treatment. They are also known as GLP-1 receptor agonists, incretin mimetics, and GLP-1 analogs.
Ghrelin and Leptin (6)
Ghrelin and Leptin are two hormones that greatly influence appetite and the sensation of fullness. Often referred to as the “hunger hormone.” Ghrelin is responsible for many functions, including playing a key role in metabolism through glucose and insulin regulation.
Ghrelin, produced in your stomach, signals your brain when you are hungry, and results in increased food intake.
Leptin, conversely, is produced in your fat cells, and signals to the brain when you have eaten enough (by a decrease in appetite).
Glucagon-like peptide-1 receptors
Known as GLP1 receptors, Glucagon-like peptide-1 receptor proteins are located in the beta cells of the pancreas as well as in the neurons in the brain. GLP-1 receptors are involved in the regulation of blood glucose levels and affect the secretion of insulin. These cells encourage the release of insulin from the pancreas, increase the volume of beta cells, and reduce the release of glucagon. In doing so, they increase the feeling of fullness during and between meals, suppressing the appetite and slowing gastric emptying.

Self Quiz
Ask yourself...
- What are some problems patients might face if they choose to take semaglutide?
- How do Ghrelin and Leptin relate to a patient's appetite?
What is meant by receptor agonist and antagonist?
The term agonist refers to any substance that mimics the actions of a hormone in producing a specific response: a receptor antagonist blocks a response from occurring.
Opioids are examples of receptor agonists in that they produce responses such as analgesia.
Naloxone/Narcan is an example of a receptor antagonist, in that it binds to a receptor site and decreases/blocks a response from occurring.
Semaglutide mechanism of action (7)
GLP-1 agonists work in several ways to positively affect glucose levels. Their mechanism of action includes the following:
- Increasing (stimulating) insulin secretion by the pancreatic beta cells.
- Decreasing the production of glucagon, a hormone that raises blood glucose levels
- Decreasing (slowing) gastric emptying
- Decreasing appetite (and thereby reducing food intake) by creating a sensation of stomach fullness
Through these mechanisms of action, semaglutide results in a lowering of serum glucose/A1C levels, which lowers the risk of cardiovascular events. Studies have also shown that semaglutide resulted in weight loss (approximately 8-14 pounds on average {dose dependent results}.

Self Quiz
Ask yourself...
- What is the difference between an agonist and antagonist substance?
- How much weight do patients lose, on average, when taking semaglutide?
Side Effects of Semaglutide
Common side effects of semaglutide (8)
Common side effects may include any of the following:
- Nausea and vomiting
- Headache
- Diarrhea and stomach pain
- Upset stomach, indigestion, constipation, flatulence
These side effects usually subside within a few weeks, as the patient becomes acclimated to the medication.
Serious side effects of semaglutide
- Hypoglycemia- enhanced/worsened when used in combination with other diabetes medication. Symptoms may include drowsiness, confusion, weakness, irritability, and headache.
- Symptoms may include abdominal pain and distension, nausea and vomiting, fever, and back pain.
- Diabetic retinopathy. Symptoms may include blurred vision, vision loss, and diminished night vision.
- Kidney damage/injury/failure. Symptoms may include fatigue, nausea, diminished urine output, confusion, and edema of extremities.
- Gallbladder disease. Symptoms may include gallstones, abdominal pain, nausea and vomiting, and poor appetite.
Black Box Warning (9)
Semaglutide has a Black Box Warning for thyroid cancer. This is the most serious warning from the Food and Drug Administration (FDA) and is intended to alert consumers to the potential risks of a medication. This black box warning was issued when research found that the drug increased the risk of thyroid tumors in animals.
It is not known if semaglutide actually causes tumors in humans.
Contraindications
- Semaglutide is contraindicated in people with a personal or family history of MTC (medullary thyroid cancer) or in patients with multiple endocrine neoplasia syndrome type 2.
- Known hypersensitivity to semaglutide or any of the product components
Cautions
As noted under “serious side effects”, there have been reports of new illnesses or worsening of existing health conditions occurring “post-marketing”. Thus, healthcare providers are strongly encouraged to continue ongoing surveillance of any patients on semaglutide therapy. In addition, there is insufficient data available regarding the use of semaglutide by pregnant women. Women are therefore highly encouraged to stop any treatment with semaglutide for at least 2 months prior to a planned pregnancy.

Self Quiz
Ask yourself...
- Can you name the 4 common side effects of semaglutide?
- What is the most severe warning associated with semaglutide?
Dosing
Semaglutide is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus (T2DM). It is looked upon favorably to reduce the risk of cardiovascular events in adults with T2DM and a preexisting history of cardiovascular disease. This drug is FDA-approved for use in people with diabetes, with a BMI of 27% or higher (a BMI of 25-29.9% is considered overweight).
Semaglutide (Ozempic) is available as an injectable prescription medication. Doses include 0.5mg, 1mg, or 2 mg, once weekly.
The injection should be administered subcutaneously to the abdomen, thigh, or upper arm. Injection sites should be rotated, and given as a single injection.
Start at 0.25 mg once weekly. After 4 weeks, increase the dose to 0.5 mg once weekly.
- If additional glycemic control is needed, increase the dose to 1 mg once weekly after at least 4 weeks on the 0.5 mg dose.
- If additional glycemic control is needed, increase the dose to 2 mg once weekly after at least 4 weeks on the 1 mg dose
Administer once weekly at any time of day, with or without meals. The maximum dose recommendation is 2mg/weekly once weekly.
Note: The initial 0.25-mg dose is intended for treatment initiation and is not effective for glycemic control
Missing Dose Guidelines
- If the missed dose is ≤5 days: Administer dose as soon as possible
- If missed dose >5 days: Skip the missed dose and administer the next dose on the regularly scheduled day; patients can then resume their regular once-weekly dosing schedule
Administration Day Guidelines (10).
The administration day each week can be changed, if necessary, as long as the time between 2 doses is at least 2 days (>48 hours)
Dose Availability (packaging)
- 2mg/1.5mL (1.34mg/mL); delivers doses of 0.25mg or 0.5mg per injection or four to eight doses per injection pen
- 4mg/3mL (1.34mg/mL); delivers 1mg per injection or 4 doses per injection pen
- 8mg/3mL (2.68 mg/mL); delivers 2mg per injection or 4 doses per injection pen
Treatment Goals- Effects on A1C and Weight (11)
A majority of adults who were placed on injectable semaglutide for diabetes management achieved a target A1C under 7% and were able to maintain it.
- Dose specific effects on A1C were as follows:
- 0.5mg dose injection yielded a 1.4% decrease
- 1.0mg dose injection yielded a 1.6% decrease
- 2.0 mg dose injection, in combination with diabetes pills, yielded a 2.1% decrease in A1C.
Adults taking semifluid injectables for diabetes management also noted weight loss.
- 8-pound weight loss reported with 0.5mg dose injection
- 10 pounds weight loss reported with 1.0mg dose injection
- Up to 14 pounds of weight loss reported with a 2.0mg dose injection


Self Quiz
Ask yourself...
- What should you tell a patient if they miss their injection by more than 5 days? What if it has been less than five days?
Prescribing insights: Long-Term therapy for a chronic condition?
Semaglutide is viewed favorably as a treatment option for Type 2 diabetes. It appears to lower A1C levels and body weight in the majority of patients, lowering their risk of future cardiovascular events.
The question of long-term medication use, for a chronic health condition, is being heavily discussed in the media. While a percentage of people can decrease or eliminate the need for chronic medications through significant lifestyle changes, there have been reports of weight gain in those who stopped taking this injectable medication.
Without intense lifestyle behavior modification education, there is a heightened risk of weight regain in the absence of such medications. Leaders in the treatment of obesity and related illnesses have commented that this drug is intended for long-term use.
Examples of this include the following:
“GLP-1 medications [like Ozempic] are designed to be taken long-term... They are chronic medications for the treatment of chronic conditions (both diabetes and obesity) (12)". - Christopher McGowan, M.D., a gastroenterologist specializing in obesity medicine and endobariatrics
“As with many chronic conditions, most people who use the drugs for diabetes or weight loss will need to keep taking them to keep benefiting from them. Depending on your individual situation, and without sustained lifestyle changes, it is likely you would need to be on these medications indefinitely to maintain weight loss (13)." - Dr. Cecilia Low Wang, a UCHealth expert in endocrinology, diabetes and metabolism.

Self Quiz
Ask yourself...
- Is semaglutide considered to be a long-term treatment for type 2 diabetes?
Cost Concerns
At this time, injectable semaglutide, FDA-approved for the treatment of Type 2 diabetes, has a self-pay price tag of $935.77 per month (4 injections). With FDA approval, many people with diabetes, insured under commercial plans, receive the drug for the cost of their copay. Those patients without coverage may use pharmacy discount cards that reduce the price, on average, to $814.55/month.
The following links are available to familiarize yourself with patient assistance programs related to semaglutide injectables.
Semaglutide Cost Savings Programs
The following links are provided to explore various semaglutide cost savings programs.

Self Quiz
Ask yourself...
- What resources can you offer patients who are struggling to pay for semaglutide?
Emerging Concerns: Semaglutide and gastroparesis
In August 2023, a first-of-its-kind lawsuit was filed in Louisiana, against the makers of semaglutide. The lawsuit states the makers of this injectable drug did not adequately warn patients about the risk of severe gastrointestinal issues/possible gastroparesis.
The plaintiff in this case had used both Ozempic and Mounjaro and experienced repeated episodes of severe gastrointestinal events, warranting trips to the emergency room and additional medications to alleviate her symptoms (14). While this lawsuit is in the developing stages, it bears mentioning in terms of concerns over long-term usage of the drug and possible complications.
While the drug labeling for semaglutide (Ozempic) does not specifically mention gastroparesis, the semaglutide/Mounjaro drug label does state that the drug has not been studied in patients with severe gastrointestinal disease and is therefore not recommended in these patients.
Up to 50% of people with diabetes have some degree of delayed gastric emptying, but most have no digestive symptoms or have only mild symptoms. For some people with diabetes, problems managing blood glucose levels may be a sign of delayed gastric emptying (15).
Healthcare providers should evaluate all patients with diabetes for possible symptoms of underlying gastroparesis, such as the feeling of fullness shortly after beginning a meal, or the inability to finish a regular meal. Other symptoms of gastroparesis may include abdominal pain, nausea, bloating, vomiting, and anorexia.
Diabetes and gastroparesis
Uncontrolled or poorly controlled diabetes can affect nerve endings systemwide. Diabetes is a very common cause of gastroparesis. Although the condition is rare it occurs more often in people with chronic conditions such as diabetes, autoimmune diseases, and nervous system disorders. Nerve endings are injured or damaged, cease to function properly, and result in delayed gastric emptying. The delay in gastric emptying can cause various symptoms, such as nausea, vomiting, bloating and distension, abdominal pain, and poor appetite.
In addition to underlying medical conditions, some medications may cause symptoms of gastroparesis (delays in gastric emptying and overall gastric motility. These medications include narcotics, antidepressants, and anticholinergics.
Left untreated, diabetic gastroparesis may lead to malnutrition, electrolyte imbalances, and poor glucose management and control.

Self Quiz
Ask yourself...
- Why should nurses prescribing semaglutide watch out for symptoms of gastroparesis?
- What do you think are some ethical issues with semaglutide use for weight loss?
Diabetes Lifestyle changes: Patient education (16)
- Weight Management
- Healthy Eating
- Physical Activity
- Smoking Cessation
- Stress Management
The importance of patient education regarding lifestyle changes is a priority. As with any chronic medication condition, the patient and their family/support system must be given every opportunity to educate and empower themselves on self-management of their disease process. Patients must be given the benefit of the doubt that they can indeed embrace their health and well-being and work with their healthcare provider in maximizing their health outcomes.
For diabetes mellitus, numerous lifestyle behaviors should be addressed and actively worked on, so that the patient receives the maximum health benefits. The following lifestyle behaviors are in no particular order; they all warrant discussion at every office visit.
Diet
A person with diabetes should be educated on the effects of food and nutrition on their glucose level. Referrals to a dietitian/nutritionist or Certified Diabetes Care Education Specialist (CDCES) should be considered a top priority. Well-balanced nutritional intake, appropriate carbohydrate awareness, calorie monitoring if weight loss is appropriate to your specific patient) and medication/food interactions are all essential aspects of dietary lifestyle education. Many commercial insurance plans, as well as hospital community outreach programs, offer diabetes self-management classes.

Activity (17)
The CDC recommends a target goal of 150 minutes weekly, Patients should be educated on the positive effects of daily activity on overall health and well-being, stress management, and metabolism. Patients should find activities they are genuinely interested in, involve family and friends, and slowly build greater endurance through increased intervals of longer duration.
Sleep hygiene (18)
Patients should be educated on the positive effects of a good night’s sleep. The aim should be approximately 7-8 hours of restful sleep. Electronics should be powered down and (optimally) removed from the bedroom. A dark, well-vented, cool room temperature is encouraged, and large meals and late-evening caffeine should be avoided.
Medication adherence/ literacy
Medication education is critical to the health and well-being of a patient. Routine education of the patient, and family members or support systems when available, should be supportive and patient-specific. Patients should be assessed on language barriers, literacy issues, and related comprehension concerns. Medication education should include effects, side effects, treatment goals, and sick day management. Emergency care issues should also be discussed. Any monitoring equipment (continuous glucose monitors, accuchecks, lancets) should be reviewed with patients and confirmed with return verbalization and demonstration.
As discussed in this course, patients with chronic diseases must learn self-management techniques to optimize their health and well-being. They must become confident in their understanding of their disease process and take ownership of their health. In doing so, they minimize the risk of long-term complications, improve their self-worth, and actively invest (both time and money) in their future.

Self Quiz
Ask yourself...
- How does sleep, diet, and activity level affect the treatment of type 2 diabetes?
Ozempic Case Study
- 52-year-old female
- Height 67 inches
- Weight 225 pounds
- B/P 138/84, Heart rate 76 NSR
- BMI 35.2%
- Nonsmoker, occasional social drinker
- Multiple attempts at dieting without success.
- Diagnosed T2DM approx. 6 months ago current A1C 7.5%; initial medication Metformin 500mg BID tablets; tolerated well. No GI upsets.
Today’s appointment is for evaluation and additional medication consideration (the patient requested this appointment)
The patient was diagnosed with T2DM approximately 6 months ago. Initial A1C 8.0%. Current A1C 7.7%
Despite an improved diet and adherence to the medication regimen, the patient voiced frustration at the lack of weight loss. Requesting additional medication. Has a neighbor friend who began injectable Ozempic and is having “really great results with it. I want to start on it as well”.
- What are your thoughts on prescribing semaglutide injectable for this patient?
- What objective health data points should be taken into consideration regarding prescribing semaglutide for this patient?
The patient has expressed frustration that despite taking her medications and adjusting her diet, she has not lost any weight in the past 6 months. She has “heard from her neighbor friend that the weight just melts off immediately” and she is ready to start this medication.
- What concerns do you know about this patient's understanding of weight loss as it relates to semaglutide?
- What prescribing information, specific to semaglutide and weight loss, could you share with your patient regarding realistic weight loss targets?
- In addition to teaching your patient proper injection technique for the use of semaglutide, what other lifestyle education behaviors should you discuss at this point?
- What information should you share with your patient regarding the long-term use of semaglutide and the potential risks of stopping this medication (as it relates to weight regain)?
Your patient decides to go ahead with the semaglutide regimen.
- What are some patient education guidelines regarding common side effects of this medication?
- How often is the dose increased? What is the maximum dose this patient can receive weekly?
Your patient wants to know how long she will be taking this medication.
- What talking points will you cover regarding the long-term use of this medication?
- How do you best prepare this patient for long-term success with this medication?
- What lifestyle behavior modification education would you discuss with your patient, to give her the best chance at successfully managing her diabetes?
Medication Assisted Treatment (MAT)
Introduction
Medication Assisted Treatment (MAT) is a treatment modality for substance use disorders. It combines counseling and behavioral therapies for addiction with medications used carefully to reduce the physical symptoms of cravings and withdrawal and assist clients in the recovery process. With half of people 12 and older reporting use of an illicit substance at least once and 21 million Americans experiencing addiction, this is an important and relevant topic (4).
Historically, an intense stigma is attached to both addiction and some of the medications used to treat addiction. A thorough understanding of substance use disorders, available MAT therapies, and care of affecting clients are essential topics for nurses to be familiar with, particularly those working in psychiatry, pain management, or addiction medicine.
Overview of Addiction and Substance Abuse:
Drug and alcohol abuse and addiction are chronic, complicated issues involving persistent changes to the brain. There is a stigma or misunderstanding that people with substance abuse disorders can stop any time they want to or lack the willpower or moral fortitude to stop using. This is entirely untrue, and even people who are "recovering" and have not had any drugs or alcohol in years can easily relapse into addiction once those brain changes have occurred (5).
When a person uses drugs or alcohol, the brain's reward center is flooded with dopamine. This provides a "buzz" or pleasurable sensation that may create the desire to use more of the same substance. Over time, and with regular use of the substance, the brain becomes accustomed to the flooding of dopamine and reduces the reward response, a process known as tolerance.
It will now take the same person a more significant amount of the substance to achieve the same "buzz" or "high" they used to feel. This process can also dull the pleasure response to activities not involving substance use, such as food, socialization, or sexual activity. Over time, the chemical changes in the brain can progress to include decreased functioning of learning, decision-making, judgment, response to stress, memory, and behavior (5).
To understand substance abuse disorders, it is first essential to understand some basic definitions. These terms are sometimes used interchangeably, but they mean different things and represent different stages of disease.
Definitions
Substance Use: Substance use is any consumption of drugs or alcohol, regardless of frequency or amount. An occasional glass of wine or taking an edible at a party is an example of substance use. Substance use does not cause problems or dependency in many people (5).
Substance Abuse: Substance abuse is the continued use of drugs or alcohol, even when they do cause problems. Conflict or problems at home, school, work, or legal issues related to the use of drugs or alcohol are signs of abuse. For example, being sent home from school for smoking in the bathroom or failing a drug test at work (5).
Substance Dependence or Addiction: Dependence and addiction can be used interchangeably or is sometimes called substance use disorder. Addiction occurs when a person cannot stop drinking or using drugs despite creating problems in their life. People who are addicted may experience cravings until they use a specific substance, or they may experience uncomfortable physical symptoms, known as withdrawal if they do stop (5).
The American Psychiatric Association (APA) utilizes the following criteria to diagnose clients who suffer from addiction. The more criteria a client answers yes to, the greater their problem with substance use.
Six or more positive criteria are indicative of addiction.
- Using substance in more significant amounts or for more extended periods than intended
- Trying to stop using but being unable to
- Increased amounts of time getting, using, or recovering from use of the substance
- Experiencing cravings or urges to use.
- Continuing to use the substance despite problems with relationships or social situations.
- Missing work, social, or recreational obligations or activities because of substance use
- Participating in risky behavior because of substance use
- Continuing to use the substance despite psychological or physical health problems.
- Needing to use more substance over time to achieve the desired effect.
- Experiencing withdrawal symptoms when stopping the substance (1).


Self Quiz
Ask yourself...
- Do you know anyone who suffers from a substance use disorder?
- Think about your biases (thoughts, opinions, attitudes) about addiction. Does any of the information above conflict with those biases?
Substance Abuse Statistics
Many factors go into gathering data on substance abuse disorders, from underreporting, the nuance between use, abuse, and addiction, and the large variety of substances available, with the legality of some substances varying by state or age.
The statistics below from 2020 are not meant to be an exhaustive list of substance use disorders in this country but rather an overview of some of the more prevalent addiction-related issues.
- 50% of people 12 years and older have used an illicit substance at least once.
- 5% of Americans 12 years and older have used drugs within the last month.
- This is a 3.8% increase from the previous year.
- About 50% of Americans 12 and over drink alcohol
- 4% of those people have an alcohol use disorder.
- About 20% of Americans use tobacco products or vape
- 18% of Americans over 18 used marijuana in the last 12 months
- 30% of those have some level of misuse or addiction.
- Marijuana is commonly involved in polysubstance use, paired with alcohol or other drugs.
- 7% of Americans over 12 misused opioids in the last 12 months
- 96% of those used prescription pain relievers
- Opioid prescriptions peaked in 2012, with 81.3 prescriptions per 100 people.
- The rate has declined recently due to increased attention to this crisis.
- In 2018, the rate was down to 51 prescriptions for every 100 people
- Fentanyl is now rising as a new and deadly concern.
- 5 million prescriptions were written for fentanyl in 2015.
- Fentanyl is involved in 53% of overdose deaths.
- 7% of all Americans misuse a prescription drug.
- 1% of those misuse stimulants
- 2% of those misuse sedatives
- 5% misuse painkillers
- Over 70,000 drug overdose deaths occur annually in the United States (4)
Risk Factors
A combination of factors is involved in the risk of addiction, and no one factor can determine if someone will develop addiction or after how many uses this will occur.
The addiction process does occur more easily or progresses more rapidly for people with certain risk factors, including:
Genetics
There is a strong genetic correlation with addiction, indicating that biology plays a significant role in the disorder. Family history of addiction, gender, ethnicity, and comorbid mental health conditions can all influence the risk of addiction. (5)
- Children of addicts are eight times more likely to develop an addiction at some point.
- In 2020, among those using illicit or misusing prescription drugs, 22% were male and 17% female.
- Only 20% of users in drug treatment programs are women.
- 9% of people with substance abuse disorders also have at least one mental health disorder (4)
Environment/Non-Genetic Demographics
The attitudes about drugs and alcohol from those in a person's network and life experiences play a role in the risk of addiction. Substance use among friends, family, or coworkers increases the risk that a person will also use substances. Exposure to substance use from a young age relaxed parental attitudes about substance use, and peer pressure from friends can increase the risk. Certain stressful life circumstances such as veteran status, history of sexual or physical assault, or being part of the LGBTQ community can also increase risk. (5)
- 20% of people in urban areas used illegal drugs in 2020 compared to 5% in rural locations.
- 51% of Americans with an illegal pain relief medication obtained it from a friend or relative.
- 7% of LGBTQ Americans abuse illicit drugs.
- 2% of LGBTQ Americans abuse alcohol.
- 7% of Veterans abuse illicit drugs.
- 80% of Veterans abuse alcohol (4)
Developmental Stage
Substance use at any age can lead to addiction, but children and teens are at particular risk due to their underdeveloped brains. The parts of the brain responsible for decision-making, risk assessment, and self-control do not fully develop until the early 20's, putting teenagers at increased risk of dangerous behaviors. In addition, the effects of drugs and alcohol on the developing brain may mean that those parts of the brain never fully develop at all for teens with substance abuse disorders. (5)
- 70% of users who try an illegal substance before age 13 will develop a substance use disorder within the next seven years.
- This is for only 27% of people who first try an illegal substance after age 17.
- 47% of youths report trying an illegal substance by the time they graduate high school (4)

Self Quiz
Ask yourself...
- Why do you think medication alone is not an adequate treatment for substance abuse disorders?
- Is MAT something you have heard of before? Why do you think it is relatively uncommon despite being around for decades?
Overview of Medication Assisted Treatment (MAT)
Treatment of substance abuse disorders is a complex and often tumultuous process. The nature of the brain changes that occur during addiction means that a person is never entirely "cured" but will always be considered "recovering" as the risk for relapse is always present. Effective treatment must be multifaceted and often involves removing triggers (such as people, places, and stressors) that may prompt a person to use again behavioral therapy, and medications to curb withdrawal symptoms and reduce cravings.
Medication Assisted Treatment (MAT) is a treatment that involves FDA-approved medications, in combination with behavioral therapy, in the recovery process for substance abuse disorders. Several medications are available for MAT, and evidence continues to emerge that the treatment is highly effective if used correctly.
However, it is a vastly underused and understudied treatment modality. MAT has been available in some form for over 50 years but is just starting to gain traction among the medical community (and policymakers) in recent years, with the federal government calling for more research and increased accessibility for the treatment (8).
The height of the opioid crisis in the last several years has highlighted the magnitude of drug addiction and deaths in the United States, bringing renewed attention to MAT as a treatment option. So, how does MAT work? Prescription medication is given to both stimulate the receptors seeking the abused substance and block the drug's euphoric effects.
Over time, this normalizes brain chemistry and helps the person break the habit of using without the discomfort of cravings and withdrawal symptoms. Gradually, the prescription medication dosage is reduced, all the while in conjunction with behavioral therapy and lifestyle changes, and eventually, the client should be able to stop the medication altogether, often within 1-3 months (8).
MAT does require close supervision by a trained medical professional and an appropriate facility for treatment. It can be done on an inpatient, partial inpatient, or outpatient basis. There may be side effects to the medication, and there is a risk of misusing or developing addiction to the new drug, though the successful outcomes often outweigh this risk. Clients must also participate in behavioral therapy for a comprehensive and effective treatment plan. As with any treatment regimen, careful consideration of the client's history and circumstances is essential (8).


Self Quiz
Ask yourself...
- Why do you think medication alone is not an adequate treatment for substance abuse disorders?
- Is Medication Assisted Treatment (MAT) something you have heard of before? Why do you think it is relatively uncommon despite being around for decades?
Pharmacokinetics
Currently, there are three medications with FDA approval for MAT: buprenorphine, methadone, and naltrexone. Each will be discussed in depth below.
Buprenorphine
Mechanism of Action and Metabolism
Buprenorphine is an opioid partial agonist, acting on the same receptors as other opioids but with weaker effects. It can be used for the treatment of misuse of opioids, including:
- Heroin
- Fentanyl
- Oxycodone
- Hydrocodone
- Morphine
- Methadone (3)
Opiate receptors are G-protein coupled receptors (GPCRs) with four major types: Mu, Delta, Kappa, and opioid receptor like-1 (ORL1). Stimulation of these receptors results in varying levels of the following effects:
- Euphoria
- Relaxation
- Pain relief
- Sleepiness
- Sweating
- Constipation
- Impaired concentration
- Reduced sex drive (3)
Buprenorphine has a high affinity to the Mu-opioid receptor and is a partial agonist at this site, causing reduced opioid effects with a plateau or ceiling at higher doses. This limits dangerous effects and makes overdose unlikely. It also has slow dissociation from the site, allowing milder and more easily tolerated withdrawal effects compared to full agonists like morphine and fentanyl. Buprenorphine is also a weak kappa receptor antagonist and delta receptor agonist, reducing the craving sensation and improving tolerance to stress (3).
Buprenorphine has poor bioavailability when given orally due to the first-pass effect, where most of the drug is broken down in the liver and intestines. Because of this, sublingual or buccal are the preferred routes of administration and the most common forms in which the drug is manufactured. Transdermal patches and IV and IM forms exist, though not for use in MAT (3).
CYP34A enzymes break down buprenorphine, so other drugs, such as ketoconazole, may inhibit metabolism and increase available levels of buprenorphine. CYP34A inducers such as carbamazepine, topiramate, phenytoin, and barbiturates may speed metabolism and lower available levels. Once broken down, the med takes the form of norbuprenorphine and is excreted in the feces (3).
Available Forms
Buprenorphine is available by itself and with naloxone (in a 4 to 1 ratio). However, in oral form, naloxone is not readily absorbed, and buprenorphine is the only genuinely active ingredient. This combination is beneficial should clients try to inject their buprenorphine to get high; naloxone is a fast-acting opioid antagonist that is active when used intravenously and would block the opioid effect of buprenorphine, rendering it useless for recreational use and ensuring it has no street value.
The currently available preparations of buprenorphine for MAT include:
- Generic Buprenorphine/naloxone sublingual tablets
- Subutex - Buprenorphine sublingual tablets
- Suboxone - Buprenorphine/naloxone sublingual films
- Zubsolv - Buprenorphine/naloxone sublingual tablets
- Bunavail - Buprenorphine/naloxone buccal film (3)
Sublingual products dissolve within 2-10 minutes. Bloodstream absorption begins quickly, bypassing the first pass effect. Buprenorphine has a slow onset of action, peaking about 3-4 hours later. Metabolism is also slow, with the half-life lasting anywhere from 25 to 70 hours (an average of about 38 hours). This long half-life means the drug can be spaced out to every other day administration once weaning begins (3).
Dosing and Monitoring
Clients prescribed buprenorphine must stop using opioids for at least 12 to 24 hours before the first dose; this varies depending on which opioid they are stopping. For short-acting opioids like heroin and oxycodone, buprenorphine may be started 6-12 hours after the last dose. With longer-acting opioids such as morphine or extended-release preparations of oxycodone, buprenorphine should be delayed for about 24 hours. For the longest action opioids, fentanyl patch, 48 -72 hours must be between the last dose and buprenorphine initiation (3).
This initiation schedule means clients will be in the early stages of discomfort and withdrawal. Administration of buprenorphine when clients still have opioids in their bloodstream will lead to competition for receptor sites, rapidly replacing the opioid with buprenorphine and causing acute and more severe withdrawal symptoms.
Depending on the severity of a client's addiction, they may complete the first step of abstaining and withdrawal in an inpatient setting. Once the initial withdrawal symptoms have passed and the initial dose of buprenorphine has been given, the client may be discharged home to continue buprenorphine initiation on an outpatient basis (3).
Initial doses are typically 2-4mg, with up to 4mg given to clients used to higher potency or larger doses of opioids. The dose is gradually increased to meet the client's individual needs, with a maximum dosage of 24mg per day. The average client requires 8-12 mg per day and can reach this dose within the first 2-4 days. It is recommended that doses be supervised by a pharmacist at the dispensing pharmacy for the first two months of treatment to ensure compliance and clients are less likely to relapse (3).
The length of treatment with buprenorphine depends on each client's case and, for some, may be indefinite. Clients who do wish to wean off buprenorphine can begin the process once they are stable and experiencing few or no cravings, and a minimum of 8 weeks from treatment initiation. Doses are moved to alternating days and eventually discontinued altogether (3).
Side Effects and Contraindications:
As with any medication, there are potential side effects, including:
Common Side Effects
- Nausea
- Vomiting
- Drowsiness
- Dizziness
- Headache
- Memory loss
- Sweating
- Dry mouth
- Miosis
- Postural hypotension
- Sexual dysfunction
- Urinary retention
Serious side effects
- CNS depression
- QT prolongation
- Reduced seizure threshold
- Potential for abuse or overdose (3)
Buprenorphine is contraindicated for clients with a past hypersensitive reaction to it. It should be used cautiously for clients with respiratory suppression, older adults, or for those with liver pathologies. Regular monitoring of liver enzymes via lab work is essential (3).
It is a Category C medication for pregnancy, and the risks versus benefits should be carefully weighed. Buprenorphine does cross the placenta and increases the risk of withdrawal symptoms and neonatal abstinence syndrome (NAS) after delivery. However, for pregnant clients with the highest risk of relapse and abuse of opioids, evidence does support that continuation of buprenorphine during pregnancy may improve maternal and fetal outcomes (3).
Buprenorphine may be abused by crushing tablets, snorting the powder, or dissolving it into an injectable solution. Safety measures against this include supervised administration by a pharmacist and the addition of naloxone, which blocks the buprenorphine effects. While the effect ceiling of buprenorphine makes overdose difficult, combining the drug with benzodiazepines, alcohol, or other drugs can compound the CNS depressant effects and increase the risk of overdose (3).
Clinicians need to have a comprehensive health history of clients before initiating buprenorphine so that all risks and potential interactions can be addressed appropriately.
Role of the Pharmacist
Pharmacists play a significant role in the success of MAT involving buprenorphine. Outpatient doses are monitored by the dispensing pharmacist daily, with at-home quantities being allowed on a limited basis (such as weekends or travel) and only for the most motivated and compliant clients. Vital signs are collected before each dosage, with careful monitoring for hypotension or bradypnea. The dose may be skipped for clients who experience excessive side effects, and the client can return the next day for their dose.
Clients presenting with signs of overdose (usually to the ED) may receive naloxone, which will reverse overdose symptoms within 1 hour. Overdose symptoms include dizziness, pinpoint pupils, hypotension, bradypnea, hallucinations, seizure, or unconscious state.
If a client misses a dose, does not show up for it, or is experiencing significant side effects from buprenorphine, the prescribing clinician should be notified so that the treatment plan can be revisited and revised if needed (3).
Considerations for the Prescriber
When considering which medication to prescribe for MAT, prescribers should understand that buprenorphine offers advantages over methadone.
- Lower risk of abuse
- Safer, including at higher doses.
- Therapeutic dose achieved quickly.
- Easier to taper.
- Can be obtained from any provider rather than a methadone clinic.
- Less stigma
The cost of a 30-day supply is around $300. Buprenorphine/naloxone combinations are a little more expensive at $400/month. While prior authorization is usually required, most commercial insurance and state Medicaid programs will cover the medication.
Buprenorphine is a Schedule III Controlled Substance; however, recent federal regulations have been aimed at approving access to MAT, and any provider with an active DEA license may prescribe buprenorphine as allowed by state regulations. Specialized clinics are not required (as they are with methadone), and it is dispensed at regular pharmacies.
Prescribers are encouraged to participate in additional training about MAT with buprenorphine, but it is not required. Detailed documentation must be completed, including the reason for prescribing, start and end dates of treatment, the pharmacy used, the credentials of who will supervise administration, and frequency of follow-up and compliance monitoring. The sublingual and buccal routes are the only forms of medication used for MAT; patches, IM, and IV preparations are not routinely used for MAT.
The success of buprenorphine treatment depends on the client's education. Addiction potential, risk of combination with other CNS depressants, and side effects vs. signs of overdose should all be discussed with clients and their support system (3).

Self Quiz
Ask yourself...
- Given the nature of substance abuse disorders, why do you think including an opioid antagonist like naloxone in preparations of buprenorphine is necessary for safety and compliance?
- What challenges do you see with a medication needing to be administered daily with pharmacist supervision?
- What are the risks of buprenorphine being given without this supervision?
- Consider the possible pros and cons of taking a medication like buprenorphine during pregnancy. Also, consider the risks of NOT taking the drug during pregnancy when a substance use disorder is present.
Methadone
Mechanism of Action and Metabolism
Methadone is a synthetic opioid and a full agonist of the Mu-receptor site, stimulating the same effects as opioids.
- Euphoria
- Analgesia
- Sedation
It can be used as a potent analgesic for pain not responding to traditional medications, such as in clients with cancer or terminal illness, as well as for MAT and neonatal abstinence syndrome (NAS).
For this course, it will be discussed as a MAT agent, used in treatment for clients addicted to opioids such as:
- Heroin
- Fentanyl
- Oxycodone
- Hydrocodone
- Morphine
- Hydromorphone (2)
Methadone is a full agonist at the Mu-receptor, meaning it is a more potent and more easily addictive medication than partial agonists like buprenorphine. Methadone has a long half-life (8-60 hours), occupying the Mu-receptors and blocking short-acting opioids from making a client high. The longer half-life also leads to less severe cravings and withdrawal symptoms. Methadone is also an antagonist to the N-methyl-d-aspartate (NMDA) receptor, which adds to its pain relief action (2).
It has high oral bioavailability, is active in the bloodstream within 30 minutes of ingestion and remains elevated for around 24 hours. It is broken down via CYP3A4 and CYP2B6 enzymes and metabolized through the liver, making it a good option for clients with renal problems.
Medications such as ciprofloxacin, benzodiazepines, fluconazole, cimetidine, and fluoxetine may slow methadone metabolism, increasing the available drug and the side effects of overdose risk. Other medications may speed metabolism and decrease the effects of methadone, including phenobarbital, phenytoin, rifampin, ritonavir, and carbamazepine (2).
Available Forms
Methadone is available in many forms, including oral, IM, subcutaneous, IV, and intrathecal, though only the oral is typically used for MAT.
- Methadone - tablets
- DISKETS - dispersible/dissolvable tablet
- Methadone HCL Intensol - 10mg/ml suspension
- Methadone - dispersible tablet (2)
Dosing and Monitoring
Oral dosing is initiated at 30-40 mg/day with a slow titration of 10-20 mg/week until the optimal dosage is reached. The optimal dosage varies by client and depends on the drug they are replacing, tolerance to opioids, and side effects experienced. A dosage between 80- 150 mg/day is the typical goal. (2)
If parenteral methadone is given, it is usually 50%-80% of the oral dosage.
Blood sugar, EKG, and methadone blood levels should be checked regularly, every week for higher-risk patients, and every 3-6 months for those in good health and compliance. The target methadone blood level is around 400 ug/ml (2).
Side Effects and Contraindications
Potential side effects are directly related to stimulation of the opioid receptors and include:
- Diaphoresis
- Flushing
- Pruritus
- Nausea
- Dry mouth
- Constipation
- Sedation
- Lethargy
- Respiratory Depression
- QT prolongation
- Hypoglycemia (2)
Methadone should be considered with a comprehensive view of a client's health history and other medications. Clients with CNS-related disease processes (trauma, increased ICP, dementia, or delirium) must be monitored closely or have other medication considered.
Methadone should not be used simultaneously as other opioids, benzodiazepines, alcohol, or antipsychotics due to increased CNS effects. Methadone is a Pregnancy Category C medication, and risks versus benefits should be weighed carefully. Infants exposed to methadone in utero are at increased risk of NAS after delivery (2).
Overdose can occur, and clients and support systems should be educated on signs of overdose.
- Lethargy
- Somnolence
- Stupor
- Coma
- Miosis
- Bradycardia
- Hypotension
- Respiratory sedation
- Cardiac arrest
Naloxone is used to reverse overdose (2).
Considerations for Prescribers and Clinics
Methadone is a Schedule II Controlled Substance, meaning it has a high abuse potential and must be carefully monitored. The Prescription Drug Monitoring Program (PDMP) is an electronic database used nationwide to register the distribution of controlled substances so that clients do not seek care at multiple clinics or pharmacies to obtain more of a controlled substance.
When prescribing methadone, providers should check the PDMP for both methadone and other prescription opioids so that they are fully aware of other medications clients may be receiving from other places. Regular urine drug screening should be performed to make sure clients are not using other substances not obtained by prescription and that they are testing positive for methadone, meaning they are genuinely taking it if administration is not observed (2).
At the beginning of treatment, methadone is given in the office under a nurse's supervision, and then clients are monitored for adverse effects. Some take-home doses (up to 7 in the first two weeks) may be arranged for weekends or during travel, but this possibility is limited during the first few weeks of treatment. As treatment progresses and compliance is demonstrated, clients may self-administer more doses at home (up to 28 doses per month) and go longer between visits to the clinic. The total length of treatment varies but is often 1-2 years and can even be indefinite (7).
There are methadone clinics that work entirely in the scope of addiction management, but primary care providers may prescribe methadone as well. Prescribers must have an active DEA license and comply with state-based controlled substance regulations (2).


Self Quiz
Ask yourself...
- Why do you think methadone is a Schedule II Controlled Substance while buprenorphine is only a Schedule III?
- What are the benefits of checking the serum level of methadone?
- What might the clinical presentation be for someone overdosing on methadone?
- Have you ever used the PDMP database before? What are the benefits of accessing this database?
Naltrexone
Mechanism of Action and Metabolism
Naltrexone has been in use since the 1960s and is an opioid antagonist. It competes primarily with the mu-receptor but also serves as an antagonist at the kappa and delta receptors. As an antagonist, it competes with agonists such as opioids and alcohol and blocks the effects of agonists at those sites.
- Prevents euphoria.
- Prevents intoxication.
- Reduces tolerance (6)
Naltrexone also acts on the hypothalamic-pituitary-adrenal axis, modifying it to reduce cravings and suppress alcohol consumption.
It is FDA-approved for use in clinical practice for the treatment of:
- Alcohol use disorder
- Opioid use disorder (prescription and non)
Naltrexone is absorbed orally and undergoes extensive metabolism via the first-pass effect. However, this does not affect its potency as naltrexone's active metabolite, 6β-naltrexone, acts as a potent opioid antagonist. The medication's half-life is around 4 hours but can last up to 24 hours. If administered parenterally, it bypasses the first pass and is even longer acting, with a half-life of 5-10 days. Naltrexone is excreted by the kidneys (6).
Available Forms
Naltrexone is available in an oral tablet and IM injection. Available preparations include:
- Generic naltrexone tablets
- Revia (oral tablet)
- Depade (oral tablet)
- Vivitrol (solution for IM injection, extended-release) (6)
Dosing and Monitoring
Since naltrexone will compete for and block all opioid receptor sites, the risk for withdrawal symptoms is high, and clients must stop the use of alcohol or opioids for 7-10 days before beginning treatment to lessen the risk of withdrawal symptoms. A naltrexone challenge is recommended at the start of therapy.
This consists of administering small amounts of naltrexone subcutaneously or via IV and monitoring the client and their vital signs for signs of withdrawal, such as:
- Nausea
- Vomiting
- Diaphoresis
- BP changes
- Tachycardia
- Rhinorrhea
- Agitation
- Tremors
- Abdominal pain
- Pupillary dilation (6)
If a client fails the naltrexone challenge and has not been long enough since their last use of alcohol or opioids, the naltrexone initiation should be delayed, and the test should be repeated in 24 hours. If clients tolerate the naltrexone test and the negative result, they may begin naltrexone treatment (6).
For oral tablets, dosing usually starts at 25 mg for the first dose. Clients are observed for withdrawal symptoms and side effects; an additional 25 mg is given 1 hour later. After that, clients take 50 mg per day. Clients may continue with 50mg daily or take 100 mg every other day or 150 mg every 3rd day (6).
Alternatively, naltrexone may be given via IM injection for more extended action, improving compliance and reducing relapse. Particularly for alcohol or heroin dependence, data indicates that the IM route has much higher success rates than the oral route. If a client receives the IM injection, 380 mg is given to the gluteal muscle every four weeks (6).
Side Effects and Contraindications
Most common side effects of naltrexone include:
- GI irritation
- Diarrhea
- Abdominal cramps
- Nausea
- Vomiting
- Hypertension
- Headache
- Anxiety
- Low energy
- Joint or muscle pain
- Nervousness
- Sleep disruption
Less commonly, clients report:
- Loss of appetite
- Constipation
- Dizziness
- Irritability
- Depression
- Rash
- Chills (6)
Caution should be used for clients with liver function issues and renal impairment. It is Category C for use during pregnancy, and the risks versus benefits of use in pregnancy must be carefully considered. It also crosses into breast milk and must be considered carefully.
There is limited data about the overdose of naltrexone, and there may be very few symptoms if an overdose occurs. Clients should be monitored for signs of liver dysfunction, seizures, depression, and suicidal ideations. No antidote for naltrexone is currently available.
Naltrexone is contraindicated for clients who failed a naltrexone challenge, test positive for opioids or alcohol on drug screening, have a history of seizures, or have experienced a past hypersensitivity reaction to naltrexone.
Clients may switch from buprenorphine or methadone to naltrexone at some point in treatment. Both medications are agonists at the opioid receptor sites, so changing to naltrexone (an antagonist) may increase the risk of withdrawal symptoms for the first two weeks of treatment (6).
Considerations for Prescribers
Because naltrexone does not cause any euphoria or "high," the abuse potential is non-existent. It is not a controlled substance and can be prescribed by any clinician with prescriptive authority. However, its use is typically only by those who work in mental health or addiction medicine. Clients can take the medication at home or go to the clinic for IM injections.
Many considerations for naltrexone use center around monitoring for side effects and treatment compliance. Baseline and periodic drug screening and liver function tests are prudent. Clients' support persons should be educated on compliance and signs of relapse. The IM formulation should be considered for those with poor compliance or most at risk for relapse (6).

Self Quiz
Ask yourself...
- Why might a client benefit from the IM formulation of naltrexone instead of the oral preparation?
- Why might compliance with an opioid antagonist be more complex than an opioid agonist like methadone or buprenorphine?
- How do side effects differ between naltrexone and the agonist medications like methadone?
- What does it mean if a client fails a "naltrexone challenge," and how does this delay their care?
Nursing Considerations
Nurses will encounter clients with addiction and even those receiving MAT in a variety of settings, including:
- Outpatient clinics for routine care of any health issues
- ED admission for acute problems not related to addiction.
- Inpatient hospitalization related to other health problems.
- Outpatient setting for participation in MAT or addiction management.
- ED admission for acute problems related to substance abuse or toxicity of MAT medication.
- Inpatient mental health admission for mental health and addiction issues
Regardless of the setting and if the client is being seen for an addiction issue or something else, it is crucial for nurses to be familiar with MAT medications and how they work to provide safe and competent care. Nurses may need to:
- Administer medication.
- Monitor lab results.
- Observe for side effects, toxicity, or withdrawal symptoms.
- Coordinate care within a multidisciplinary team
- Communicate with therapeutic and nonjudgmental techniques.


Self Quiz
Ask yourself...
- Have you ever cared for a client in a non-addiction setting who had a MAT medication on their drug list?
- Did you have any biases or preconceived ideas about what this medication meant?
- Is there anything you have learned throughout this course that will change your care the next time you encounter a client receiving MAT?
Case Study
Justin is a 32-year-old male who presents to the ED with nausea, lethargy, and confusion worsening over the last 24 hours. Upon exam, the nurse notes diaphoresis, slurred speech, and pinpoint pupils. His vitals are RR 10, HR 54, BP 82/58, SPO2 97%, Temp 99.0.
He reports taking Wellbutrin 150mg daily for depression and smoking cessation, methadone 100mg daily for history of oxycodone abuse, and was started on ciprofloxacin 250mg BID for a UTI 2 days ago at urgent care.
His labs are significant for a WBC of 15,000 but otherwise regular. He tests positive for methadone, which is expected, but not for other substances. He reports being compliant with MAT and avoiding opioid use for nine months.
It is determined that Justin is experiencing methadone toxicity due to the slowed metabolism of the drug from the combination of methadone and ciprofloxacin. He is given naloxone in the ED, and within an hour, his symptoms have improved significantly, and his vital signs are typical. His antibiotic is switched to cefdinir, and he is discharged home in stable condition with instructions to follow up with his PCP within 1-2 days.

Self Quiz
Ask yourself...
- Given Justin's presentation, how could you differentiate between methadone toxicity and relapse?
- How might Justin's condition have progressed if he had not sought emergency care?
- How would Justin's case have been different if he had not tested positive for methadone?
- In what ways could Justin's care before his ED visit have been improved to avoid this complication?
Conclusion
Substance use disorders are a long-standing and dangerous pathology experienced by millions of people each year. At the same time, the stigma of seeking help for such disorders has been eroding in recent years; there has also been a renewed push by the federal government to address the issue in evidence-based and meaningful ways, with access to effective treatment being at the top of the priority list.
Addiction treatment programs utilizing MAT will likely become much more popular in the coming years, and nurses will be on the front lines of this therapy. For nurses to provide competent and comprehensive care to this client population, up-to-date and accurate knowledge is necessary.
Hypertensive Agents
Introduction
Hypertension, or high blood pressure, is a common medical condition diagnosed and treated by healthcare professionals. According to the Centers for Disease Control and Prevention, around 34 million Americans are prescribed antihypertensive medications. Additionally, hypertension was a primary or contributing cause of more than 690,000 deaths in the United States in 2021 [6].
Healthcare providers must be knowledgeable of and follow current hypertension clinical practice guidelines. Understanding the different pharmacokinetics of antihypertensive medications is essential. This course outlines antihypertensive pharmacology and addresses pharmacokinetics, including mechanism of action, side effects, usage, and contraindications.
Definitions
Hypertension – high blood pressure above normal. Normal is considered anything less than 120/80 mmHg [7].
Antihypertensives – medications used to control hypertension and lower blood pressure [7].
Hypertensive crisis – severely elevated blood pressure of either:
- Systolic greater than 180 mmHg
- Diastolic greater than 120 mmHg [19].
Hypertensive emergency – acutely elevated blood pressure with signs of target organ damage [2].
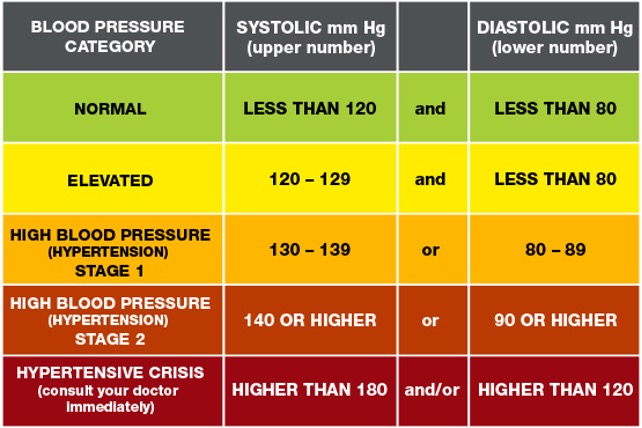

Self-Quiz
Ask Yourself...
- What is hypertension?
- What are antihypertensives?
- What is a hypertensive crisis?
- What is a hypertensive emergency?
Medications Overview
Antihypertensive medications are used for the treatment of hypertension and are used in both inpatient, outpatient, and emergency settings.
Some of the major antihypertensive medication classes include:
- Diuretics
- Beta-blockers
- Angiotensin-converting enzyme inhibitors
- Angiotensin II receptor blockers
- Calcium channel blockers
- Selective alpha-1 blockers
- Alpha-2 Receptor Agonists
- Vasodilators [3].
Different medical organizations have varying recommendations and hypertension treatment guidelines. Hypertension treatment clinical practice guidelines are available from organizations like the American Heart Association, the American College of Cardiology, and the European Society of Cardiology to name a few [21]. Healthcare providers should be aware of their healthcare institution’s recommendations for clinical practice guidelines and organizations.
All organizational guidelines share the same recommended treatment of starting antihypertensives immediately when:
- Blood pressure is greater than 140/90 mmHg for patients with a history of ischemic heart disease, heart failure, or cerebrovascular disease.
- Blood pressure is greater than 160/100 mmHg regardless of underlying medical conditions [21].
Again, healthcare providers should follow current and evidence-based clinical guidelines for initiating or titrating antihypertensive medications.
While most antihypertensives are prescribed in an outpatient setting, certain antihypertensives are indicated during hypertensive or medical emergencies. For example, intravenous (IV) vasodilators, like nitroprusside and nitroglycerin, and calcium channel blockers, like nicardipine, are used during hypertensive emergencies and crises.


Self-Quiz
Ask Yourself...
- In what settings are antihypertensives used?
- What are the clinical guidelines for initiating hypertensive medications?
- Which medications are commonly used to treat hypertensive emergencies?
Pharmacokinetics
Diuretics
Diuretics are a class of drugs that help control blood pressure by removing excess sodium and water from the body through the kidneys. There are several varying types of diuretics, some including thiazide, potassium-sparing, and loop, and all work to lower blood pressure differently [3].
Thiazide Diuretics
Thiazide diuretics remove excess sodium and water from the body by blocking the sodium-chloride (Na-Cl) channels in the kidneys’ distal convoluted tubule. As the Na-Cl channel becomes blocked, this inhibits the reabsorption of sodium and water into the kidneys. Concurrently, this causes a loss of potassium and calcium ions through the sodium-calcium channels and sodium-potassium pump [1].
Thiazide diuretics are approved by the Food and Drug Administration (FDA) for controlling primary hypertension and are available via oral route. Some common thiazide diuretics are hydrochlorothiazide, chlorthalidone, and metolazone [3].
When initiating this medication, the healthcare provider should start with the lowest dose, which is usually 25mg daily, and then increase accordingly to aid with blood pressure control or if the patient has excess fluid retention, usually as evidenced by leg swelling or edema [1].
Common side effects of thiazide diuretics include:
- Increased urination
- Diarrhea
- Headache
- Stomach and muscle aches [16].
As thiazide diuretics interfere with Na-Cl, Na-Ca, and Na-K channels, there is an increased potential for adverse effects, including:
- Hypotension
- Hypokalemia
- Hyponatremia
- Hypercalcemia
- Hyperglycemia
- Hyperlipidemia
- Hyperuricemia
- Acute pancreatitis
When prescribing thiazide diuretics, healthcare providers should avoid prescribing thiazide diuretics to patients with a sulfonamide allergy, since thiazides are sulfa-containing medications. Also, they should avoid prescribing these to patients with a history of gout [1].
Additionally, patients can experience a thiazide overdose if they take more than the amount prescribed. Patients with a suspected overdose may experience confusion, dizziness, hypotension, and other symptoms. These patients must seek emergency care and poison control must be alerted [16].
Potassium-Sparing Diuretics
Potassium-sparing diuretics remove excess sodium and water from the body without causing loss of potassium. Depending on the type, they interrupt sodium reabsorption by either binding to epithelial sodium channels or inhibiting aldosterone receptors. When catatonic sodium is reabsorbed, this creates a negative gradient causing the reabsorption of potassium ions through the mineralocorticoid receptor [5].
Potassium-sparing diuretics are approved for controlling hypertension and are usually combined with other diuretics, like thiazide or loop diuretics since they have a weak antihypertensive effect.
Common names of potassium-sparing diuretics are amiloride, triamterene, and spironolactone. These medications are available by either intravenous or oral routes. Spironolactone is commonly used for treating primary aldosteronism and heart failure [5]. Patients should be started on the lowest dose when first prescribing this class of medications.
Common side effects can include:
- Increased urination
- Hyperkalemia
- Metabolic acidosis
- Nausea
[4]
Healthcare providers should avoid prescribing this class of medications to patients with hyperkalemia or chronic kidney disease. They should also be avoided during pregnancy or in patients who are taking digoxin. Since potassium-sparing medications can cause hyperkalemia, periodic monitoring for electrolyte imbalances and potassium levels is necessary [4].
Loop Diuretics
Loop diuretics inhibit sodium and chloride reabsorption by competing with chloride binding in the Na-K-2Cl (NKCC2) cotransporter. Potassium is not reabsorbed by the kidney, which causes additional calcium and magnesium ion loss.
Loop diuretics are FDA-approved for the treatment of hypertension but are not considered first-line treatment. They can also be used for treating fluid overload in conditions like heart failure or nephrotic syndrome [12].
Loop diuretics are available via oral or IV routes and furosemide, torsemide, and bumetanide are common forms [3].
Bioavailability and dosage differ for each type and route of loop diuretics. The bioavailability of furosemide is 50%, with a half-life of around 2 hours for patients with normal kidney function, and dosages start at 8mg for oral medication. Torsemide has a bioavailability of about 80%, a half-life of about 3 to 4 hours, and oral dosages start at 5mg [12].
Common side effects can include:
- Dizziness
- Increased urination
- Headache
- Stomach upset
- Hyponatremia
- Hypokalemia [13].
Loop diuretics can lead to several adverse effects, including toxicity, electrolyte imbalances, hyperglycemia, and ototoxicity. They have a black box warning stating that high dosages can cause severe diuresis. Therefore, electrolytes, BUN, and creatinine values should be monitored closely by a healthcare provider.
People with a sulfonamide allergy may also be allergic to loop diuretics, so this should be avoided if the patient is allergic. Loop diuretics also interfere with digoxin and therefore should be avoided. Other contraindications include anuria, hepatic impairments, and use during severe electrolyte disturbances [12].


Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of thiazide diuretics?
- What is the pharmacokinetics of loop diuretics?
- What is the pharmacokinetics of potassium-sparing diuretics?
- What are common side effects and contraindications for each type of diuretic?
Beta-Blockers
Beta-blockers work by reducing the body’s heart rate and thus, lowering cardiac output resulting in lowered blood pressure [3]. The mechanism of action for beta-blockers varies, depending on the receptor type it blocks, and are classified as either non-selective or beta-1 (B1) selective.
Non-selective beta-blockers bind to the B1 and B2 receptors, blocking epinephrine and norepinephrine, causing a slowed heart rate. Propranolol, labetalol, and carvedilol are common non-selective beta-blockers.
Alternatively, beta-1 selective blockers only bind to the B1 receptors of the heart, so they are considered cardio-selective. Some examples include atenolol, metoprolol, and bisoprolol. Sotalol is a type of beta-blocker that also blocks potassium channels and is, therefore, a class III antiarrhythmic [8].
Beta-blockers are not primarily used for the initial treatment of hypertension but can be prescribed for conditions like tachycardia, myocardial infarction, congestive heart failure, and cardiac arrhythmias. It’s also approved for use in conditions such as essential tremors, hyperthyroidism, glaucoma, and prevention of migraines.
Beta-blockers are available in many forms, including oral, IV, intramuscular injection, and ophthalmic drops. Starting dosage and route are determined by the health condition being treated [8].
Common side effects of beta-blockers include:
- Bradycardia
- Hypotension
- Dizziness
- Feeling tired
- Nausea
- Dry mouth
- Sexual Dysfunction
[17]
This class of medications can also lead to more severe adverse effects such as orthostatic hypotension, bronchospasm, shortness of breath, hyperglycemia, and increased risk of QT prolongation, torsades de pointes, and heart block [8]. Healthcare providers should avoid prescribing non-selective beta-blockers to patients with asthma. Instead, they can prescribe cardio-selective beta-blockers for patients with asthma.
Additionally, the use of beta-blockers is contraindicated in patients with a history of bradycardia, hypotension, Raynaud disease, QT prolongation, or torsades de pointes. Healthcare providers must encourage patients to monitor their heart rate and blood pressure and follow administration parameters before taking beta-blockers daily since it decreases their heart rate.
Overdose of beta-blockers is life-threatening and healthcare providers must discuss the symptoms of an overdose and the need for emergency care [8].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of beta-blockers?
- What are the common side effects and contraindications of beta-blockers?
Angiotensin-converting Enzyme Inhibitors
Angiotensin-converting enzyme (ACE) inhibitors prevent the body from producing angiotensin, a hormone that causes vasoconstriction. As angiotensin production is reduced, this allows the blood vessels to dilate and therefore lowers blood pressure [3].
Moreover, ACE inhibitors act specifically on the renin-angiotensin-aldosterone system (RAAS) by preventing the conversion of angiotensin I to angiotensin II. It also works to decrease aldosterone, which in turn, decreases sodium and water reabsorption [9].
ACE inhibitors usually end in the suffix -pril and some common examples include lisinopril, benazepril, enalapril, and captopril, and they usually end in the suffix [3].
While ACE inhibitors are approved for treating hypertension, they are also FDA-approved for other uses or combination therapies for medical conditions such as:
- Systolic heart failure
- Chronic kidney disease
- ST-elevated myocardial infarction
One non-approved FDA use is treatment of diabetic nephropathy [9]. This class of medication is available in oral, and IV forms, and dosages are dependent on clinical guidelines, underlying medical conditions, and route.
ACE inhibitors have common side effects, with some including:
- Dry cough
- Dizziness
- Hypotension [9].
This medication can also lead to adverse effects, such as syncope, angioedema, and hyperkalemia [9]. As angioedema is an adverse effect, healthcare providers should understand this class of medications is contraindicated in patients with a history of hypersensitivity to ACE inhibitors.
Additionally, ACE inhibitors are contraindicated in patients with aortic valve stenosis, hypovolemia, and during pregnancy. Individuals with abnormal kidney function should have renal function and electrolyte values monitored. If a patient develops a chronic dry cough, then the healthcare provider should consider another antihypertensive medication class by following current guidelines [9].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of angiotensin-converting enzyme inhibitors?
- What are common side effects and contraindications of angiotensin-converting enzyme inhibitors?
Angiotensin II Receptor Blockers
Similar to ACE inhibitors, Angiotensin II Receptor Blockers (ARBs) act on the RAAS by binding to angiotensin II receptors and thus block and reduce the action of angiotensin II. Again, this reduces blood pressure by causing blood vessel dilation and decreasing sodium and water reabsorption [11]. ARBs typically end in the suffix -artan and common names are losartan, valsartan, and Olmesartan [3]. Oral and IV routes of the medication are available and again, dosages are dependent on the medication specifically and form [11].
All ARBs are FDA-approved for the treatment of hypertension, but a select few are approved for treating other medical conditions, such as:
- Candesartan for heart failure
- Irbesartan for diabetic nephropathy
- Losartan for proteinuria and diabetic nephropathy
- Telmisartan for stroke and myocardial infarction prevention
- Valsartan for heart failure and reduction of mortality in patients with left ventricular dysfunction [11].
Although not as common as ACE inhibitors, two side effects of ARBs are dry cough and angioedema.
Other common side effects include:
- Dizziness
- Hypotension
- Hyperkalemia
[11]
Contraindications for use are if the patient is pregnant or has renal impairment or failure. If a patient is on an ARB, the healthcare provider should closely monitor lab values for electrolyte imbalances and kidney function.
Additionally, if a patient is taking lithium, ARBs can increase lithium concentration and therefore, lithium blood concentration should be frequently checked [11].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of angiotensin II receptor blockers?
- What are common side effects and contraindications of angiotensin II receptor blockers?
Calcium Channel Blockers
Calcium channel blockers (CCBs), also known as calcium channel antagonists, act by preventing calcium from entering the smooth vascular and heart muscles. In turn, this reduces heart rate and causes vasodilation [3].
They are further divided into two major categories, non-dihydropyridines and dihydropyridines, where there are differences in the mechanism of action. Non-dihydropyridines inhibit calcium from entering the heart’s sinoatrial and atrioventricular nodes and thus cause a cardiac conduction delay and reduce cardiac contractility.
Alternatively, dihydropyridines do not directly affect the heart but do act as a peripheral vasodilator leading to lowered blood pressure. Both categories are metabolized by the CYP3A4 pathway [15].
Names of non-dihydropyridine CCBs are verapamil and diltiazem. Dihydropyridine CCBs typically end in the suffix -pine and common names are amlodipine and nicardipine. Both categories are available via oral and IV routes for administration. Oral dosages of non-dihydropyridine CCBs start at 30mg daily and dihydropyridine CCBs start at 30mg daily for immediate release [15].
Calcium channel blockers can be used to treat other medical conditions in addition to hypertension and include:
- Coronary spasm
- Angina pectoris
- Supraventricular dysrhythmias
- Pulmonary hypertension
- Hypertrophic cardiomyopathy
Non-dihydropyridine CCBs can cause side effects like bradycardia, and constipation, while dihydropyridine CCBs can cause:
- Headaches
- Feeling lightheaded
- Leg swelling [15].
Both categories pose the risk of potential hypotension and bradycardia, so healthcare providers should closely monitor the patient’s blood pressure and heart rate when initiating or titrating the dosage.
Also, an overdose of this medication can lead to cardiac conduction delays, complete heart block, and cardiovascular collapse. Patients with possible symptoms of overdose should be sent to the emergency room immediately.
Additionally, healthcare providers should avoid prescribing CCBs to people with heart failure and sick sinus syndrome [15].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of calcium channel blockers?
- What are the common side effects and contraindications of calcium channel blockers?
Selective Alpha-1 Blockers
Selective alpha-1 blockers act on the body’s sympathetic nervous system to lower blood pressure. They prevent norepinephrine from binding to the alpha-1 receptors of the sympathetic nervous system, causing smooth muscle relaxation and vasodilation which leads to lowered blood pressure [18].
Selective alpha-1 blockers are available via the oral route, end in the suffix -osin and examples are doxazosin, terazosin, and prazosin [3]. They are FDA-approved for the treatment of hypertension but are not considered first-line therapy. Additionally, this class of medications may be used to treat benign prostatic hyperplasia. Dosages can start as low as 1mg daily depending on the drug selected.
Common side effects include:
- Hypotension
- Tachycardia
- Dizziness
- Headache
- Weakness [18].
As selective alpha-1 blockers can lead to orthostatic hypotension, the healthcare provider should instruct the patient to take this medication at night. They should also avoid prescribing to the elderly population when able because of hypotension and increased fall risk [18].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of alpha-1 blockers?
- What are the common side effects and contraindications of alpha-1 blockers?
Alpha-2 Receptor Agonists
Alpha-2 receptor agonists work by decreasing the activity of the sympathetic nervous system to lower blood pressure. It inhibits adenylyl cyclase and decreases the formation of cyclic adenosine monophosphate (cAMP). Alpha-2 agonists also cause vasodilation by reducing the amount of available cytoplasmic calcium [20].
This class of medications is typically administered via oral route but is also available in intravenous and transdermal forms. Two FDA-approved alpha-2 agonists for hypertension treatment are methyldopa and clonidine and dosages are dependent on the name and route.
Methyldopa is commonly prescribed to patients with hypertension and who are pregnant since it’s safe [20].
Common side effects of alpha-2 receptor agonists are:
- Dry mouth
- Drowsiness
- Fatigue
- Headache
- Sexual dysfunction [3].
Contraindications for use are orthostatic hypotension and autonomic disorders. Healthcare providers must avoid prescribing alpha-2 receptor agonists to individuals taking phosphodiesterase inhibitors [20].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of alpha-2 receptor agonists?
- What are common side effects and contraindications of alpha-2 receptor agonists?
Vasodilators
Vasodilators lower blood pressure by dilating the body’s blood vessels. It binds to the receptors of the blood vessel’s endothelial cells, releasing calcium. Calcium stimulates nitric oxide synthase (NO synthase), eventually converting to L-arginine to nitric oxide. As nitric oxide is available, this allows for GTP to convert to cGMP, and causes dephosphorylation of the myosin and actin filaments. As this occurs, the blood vessels’ smooth muscles relax, leading to vasodilation and lowered blood pressure.
Common vasodilators that act via this pathway are nitrates and minoxidil. Hydralazine is another vasodilator, but the mechanism of action is unknown [10].
Available forms of vasodilators are sublingual, oral, and intravenous. Similar to other classes of antihypertensives, vasodilator dosages depend on the form and treatment setting [10].
Nitrovasodilators like nitroprusside and nitroglycerin are used during hypertensive emergencies. Hydralazine is used for severe hypertension for the prevention of eclampsia or intracranial hemorrhage and minoxidil for resistant hypertension [10] [3].
Side effects for each will vary, but nitrates commonly cause:
- Reflex tachycardia
- Headache
- Orthostatic hypotension
[10]
Common side effects of hydralazine are headaches, heart palpitations, and myalgias. Minoxidil causes excessive hair growth, weight gain, and fluid retention [3]. Additionally, nitroprusside can potentially cause cyanide toxicity.
Vasodilators have varying degrees of contraindications, such as nitrates are avoided in patients with an inferior myocardial infarction. Hydralazine should not be given to patients with coronary artery disease, angina, or rheumatic heart disease. Healthcare providers should be aware of contraindications and monitor patients’ blood pressure and potential side effects [10].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of vasodilators?
- What are the common side effects and contraindications of vasodilators?
Combination Antihypertensives
Many antihypertensive medications come in combined forms, such as ACE inhibitors and thiazide diuretics, beta-blockers and diuretics, or calcium channel blockers and ACE inhibitors. The mechanism of action for combination antihypertensives depends on the blend of medications [3].
Considerations for Prescribers
This section reviews potential considerations when prescribing antihypertensives.
When prescribing antihypertensive medications, there are several factors that healthcare providers must consider. The route is typically determined by the healthcare setting and dosage by the underlying treatment goals. Again, healthcare providers should follow current guidelines when initiating or titrating antihypertensive medications.
Healthcare providers must complete a thorough health history, and review lab values, and contraindications as mentioned above. Monitoring kidney function and electrolyte values is imperative while any patient is taking antihypertensive medications.
While a single antihypertensive medication is recommended for initial treatment, there are some scenarios where combination therapy or combination antihypertensives are recommended [14].
Healthcare providers should also discuss the potential side effects of antihypertensives with patients and what to do if they are experiencing symptoms. For instance, if a patient reports syncope, they should be advised to go to the emergency room or be seen immediately for further evaluation. Also, healthcare providers must encourage patients to monitor their heart rate and blood pressure at home and abide by administration parameters.
For example, instruct patients who are taking beta-blockers to measure their blood pressure and heart rate before taking their medication. If their heart rate is below 60 beats per minute, then they should not take the medication [14].
If a patient is experiencing side effects from an antihypertensive medication, then another alternative should be selected.


Self-Quiz
Ask Yourself...
- What factors should healthcare providers consider when prescribing antihypertensives?
Upcoming Research
This section reviews upcoming research and medications for hypertension treatment.
Research on antihypertensive medications has slowed throughout the years. Some clinical trials were performed on the potential of endothelin receptor antagonists to reduce hypertension. However, some studies found several unwanted side effects, and thus clinical use was stopped for safety reasons.
An endothelin-A and endothelin-B receptor blocker, called aprocinentan, has shown promise for the treatment of resistant hypertension by lowering blood pressure and decreasing vascular resistance.
Research on sodium-glucose transport protein (SGLT2) inhibitors, which are typically used for the treatment of type II diabetes mellitus, is also ongoing. SGLT2 inhibitors may promote blood pressure reduction through diuresis and reduce sympathetic tone [21].

Self-Quiz
Ask Yourself...
- What new research is there about antihypertensives?
Migraine Management
Introduction
This course will guide you on a journey to unravel the complexities of migraines and empower you with the knowledge and skills needed for effective pharmaceutical interventions.
According to recent studies by (34), migraines involve changes in brain activity, neurotransmitter levels, and vascular function, resulting in throbbing headaches accompanied by sensitivity to light and sound. Diverse classes of migraine medications are available, such as Triptans and calcitonin gene-related peptide (CGRP) inhibitors and understanding their mechanisms of action enables healthcare professionals to make informed decisions in prescribing and administering treatments (18).
Furthermore, recent research by (26) emphasizes the importance of recognizing warnings related to migraine medications. In this course, we will learn the details of medications for effective management of migraines and delve into ways of ensuring patient safety when dealing with them.

Self-Quiz
Ask Yourself...
- How might a comprehensive knowledge of migraine medications, including their mechanisms of action, enhance the ability of healthcare professionals to address the specific needs of patients experiencing migraines?
- In what ways can recognizing warnings related to migraine medications contribute to ensuring patient safety?
Definition
Migraines are recurrent, pulsating headaches often accompanied by other symptoms such as nausea, sensitivity to light, and sensitivity to sound. According to recent studies by (17), migraines are recognized as a complex neurological disorder involving abnormal brain activity and a cascade of events leading to pain and associated symptoms.
The impact of migraines extends beyond physical pain, influencing various aspects of life, and recent literature by (14) highlights the profound effect on the quality of life, with disruptions in daily activities, work, and social interactions. For example, a professional experiencing frequent migraines might struggle to meet work deadlines and engage in social events. Recent advancements in diagnostic criteria by (15) emphasize the importance of a precise definition to ensure appropriate treatment strategies. Therefore, understanding the definition is crucial for accurate diagnosis and effective communication between healthcare providers and patients.


Self-Quiz
Ask Yourself...
- What distinguishes migraines from common headaches, and how does understanding this difference impact the approach to their management?
- In what ways do migraines extend beyond physical pain, and how might this impact influence an individual’s overall quality of life?
- How can a precise definition of migraines contribute to accurate diagnosis, and why is accurate diagnosis essential for effective treatment planning?
- How does understanding the definition of migraines facilitate effective communication between healthcare professionals and patients?
Migraine Medications
Understanding the various classes of migraine medications is like having a diverse toolkit to address the complexities of this neurological disorder. By exploring the different classes of medications, healthcare professionals can tailor their approach and make informed decisions based on individual patient profiles and specific migraine characteristics (20).
It is crucial to recognize that migraine medications are not one-size-fits-all. Each patient is unique, and their response to medications may vary. Recent literature by (12) emphasizes the importance of an individualized approach when considering the best medication for each patient. Here’s a list of migraine medications in addition to important details to consider:
Triptans
Triptans are a class of medications specifically designed for the acute treatment of migraines. According to (39), they are not meant for preventive use but are highly effective in providing relief during an ongoing migraine attack. They work by narrowing blood vessels and inhibiting the release of certain chemicals in the brain associated with migraine symptoms (39). Let’s see more details below as described by (7), (39), (29).
Drug Class
Belonging to the serotonin (5-HT) receptor agonists class, Triptans modulate the effects of serotonin receptors in the brain. The various types of Triptans include Sumatriptan, Rizatriptan, Eletriptan, and others. Each Triptan has unique characteristics, such as the onset of action and duration, allowing healthcare professionals to tailor prescriptions based on individual patient needs.
Benefits
Triptans offer several benefits in the management of migraines. One of the primary advantages is their ability to provide rapid and effective relief from migraine symptoms, including headache pain, nausea, and sensitivity to light and sound. The prompt onset of action is particularly valuable for individuals aiming to resume their daily activities quickly. Triptans are available in various formulations, including oral tablets, nasal sprays, and injectables, allowing for flexibility in administration.
Side Effects
While generally well-tolerated, Triptans may cause side effects. Common side effects include mild sensations of warmth or tingling, dizziness, and tightness or pressure in the chest. It is crucial for healthcare professionals to consider the patient’s medical history and potential contraindications, such as cardiovascular issues, before prescribing Triptans. In rare cases, more severe side effects like chest pain and changes in heart rate may occur, necessitating immediate medical attention.
Clinical Effects
The clinical effects of Triptans are profound, offering relief to individuals experiencing acute migraine attacks. The primary outcomes include:
- Pain Relief: Triptans are highly effective in reducing the intensity of migraine-associated pain. By targeting the vascular and neuronal components of migraines, these drugs provide rapid relief, allowing patients to resume their normal activities.
- Relief of Associated Symptoms: Beyond pain relief, Triptans address accompanying symptoms such as nausea, photophobia, and phonophobia. This comprehensive effect enhances the overall patient experience during a migraine episode.
- Prevention of Migraine Progression: Triptans, when administered early in the migraine attack, can prevent the progression of the headache phase to more severe stages. This early intervention is crucial for optimizing outcomes and minimizing the impact of migraines on daily life.
- Improvement in Functional Impairment: Migraines often result in functional impairment, limiting individuals’ ability to perform daily tasks. Triptans restore functional capacity, allowing patients to regain control over their activities.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDSs)
Nonsteroidal anti-inflammatory drugs, commonly known as NSAIDs, constitute a class of medications used in the treatment of migraines. According to (6), these drugs are characterized by their anti-inflammatory, analgesic, and antipyretic properties. NSAIDs are versatile, as they are not exclusively used for migraines but are also used for various other pain and inflammatory conditions (6). Let’s see more details below as described by (25), (40), (6) and (28).
Drug Class
NSAIDs encompass a broad class of medications, including well-known examples such as ibuprofen, naproxen, and aspirin. They function by inhibiting enzymes called cyclooxygenases (COX), thereby reducing the production of inflammatory prostaglandins. This mechanism provides relief from pain and mitigates inflammation associated with migraines.
Benefits
The primary benefit of NSAIDs in migraine management lies in their ability to alleviate pain and reduce inflammation. They are particularly effective for individuals experiencing mild to moderate migraines. NSAIDs offer a rapid onset of action, making them suitable for individuals seeking prompt relief. Additionally, these medications are available over-the-counter in many formulations, providing accessibility for patients.
Side Effects
While NSAIDs are generally well-tolerated, they may cause side effects, especially with prolonged or excessive use. Common side effects include gastrointestinal issues such as stomach upset or ulcers. Healthcare professionals need to consider a patient’s medical history, including conditions like gastric ulcers, before prescribing NSAIDs. In rare cases, more severe side effects like cardiovascular events may occur, emphasizing the importance of cautious use.
Clinical Effects
The clinical effects of NSAIDs in migraine management encompass various aspects. Here’s a list of some of them.
- Pain Relief: NSAIDs are effective in providing pain relief during acute migraine attacks. By reducing prostaglandin levels, they alleviate headache symptoms and contribute to the overall comfort of individuals experiencing migraines.
- Inhibition of Inflammatory Responses: The anti-inflammatory properties of NSAIDs are particularly beneficial when migraines are associated with inflammatory processes. NSAIDs help mitigate inflammation, reducing the severity and duration of migraine attacks.
- Improvement in Associated Symptoms: Beyond pain relief, NSAIDs address associated symptoms such as nausea and photophobia, enhancing the overall patient experience during a migraine episode.
- Prevention of Migraine Progression: When administered early in the migraine attack, NSAIDs can prevent the progression of headaches to more severe stages. This early intervention is critical for optimizing outcomes and minimizing the impact of migraines on daily life.
Calcitonin Gene-Related Peptide (CGRP) Inhibitors
Calcitonin gene-related peptide (CGRP) inhibitors represent a modern class of medications revolutionizing the landscape of migraine management. According to (11), these drugs specifically target CGRP, a neuropeptide involved in dilating blood vessels and transmitting pain signals. By inhibiting CGRP, these inhibitors aim to modulate migraine pathways and reduce the frequency and severity of attacks (11). Let’s see more details below as described by (23) and (11).
Drug Class
CGRP inhibitors belong to a unique drug class designed explicitly for migraine prevention. Examples of CGRP inhibitors include Erenumab, Fremanezumab, and Galcanezumab. These medications are administered via subcutaneous injections, typically monthly or quarterly. The focus on preventive therapy distinguishes CGRP inhibitors from acute treatment options like Triptans.
Benefits
The primary benefit of CGRP inhibitors lies in their efficacy in preventing migraines. Clinical trials have demonstrated a significant reduction in the frequency of monthly migraine attacks among individuals using CGRP inhibitors. This preventive approach is especially valuable for those with frequent and debilitating migraines, offering a chance to enhance their quality of life.
Moreover, CGRP inhibitors are well-tolerated with fewer side effects than other preventive medications. They provide a targeted and specific intervention, addressing the underlying mechanisms of migraines without causing widespread effects on other bodily functions.
Side Effects
While generally well-tolerated, CGRP inhibitors may have some side effects. Local injection site reactions, such as redness or swelling, are common but typically mild. It is crucial for healthcare professionals to monitor and address any adverse effects promptly. Additionally, ongoing research is essential to further understand the long-term safety profile of these medications.
Clinical Effects
The clinical effects of CGRP inhibitors are transformative in the realm of migraine management, offering a novel approach to prevention. Primary clinical effects include the following:
- Reduction in Migraine Frequency: One of the hallmark effects of CGRP inhibitors is a significant reduction in the frequency of migraine attacks. By consistently blocking CGRP receptors, these medications disrupt the migraine cascade, leading to a sustained preventive effect.
- Improvement in Migraine Severity: CGRP inhibitors not only reduce the frequency but also contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall quality of life for individuals suffering from chronic migraines.
- Enhanced Functional Capacity: Migraines often result in functional impairment, limiting individuals’ ability to perform daily tasks. CGRP inhibitors restore functional capacity, allowing patients to regain control over their activities and participate more fully in their daily lives.
- Well-Tolerated Profile: CGRP inhibitors are generally well-tolerated, with a favorable side effect profile. This characteristic enhances patient adherence to preventive treatment, a critical factor in long-term migraine management.
Beta-Blockers
Beta-blockers are a class of medications that have found a significant place in migraine management. Initially developed for cardiovascular conditions, beta-blockers have demonstrated efficacy in preventing migraines by reducing the frequency and severity of attacks (32). According to (32), these medications work by blocking the effects of adrenaline, leading to reduced heart rate and blood pressure. Let’s see more details below as described by (32) and (27).
Drug Class
Beta-blockers encompass various medications, with examples such as propranolol, metoprolol, and timolol commonly prescribed for migraine prevention. These drugs fall into the broader category of antihypertensive medications but are repurposed for their preventive benefits in migraine care. Unlike acute treatments, which provide relief during an ongoing attack, beta-blockers are taken regularly to reduce the overall occurrence of migraines.
Benefits
The primary benefit of beta-blockers in migraine management is their preventive action. Clinical studies have shown that beta-blockers can significantly reduce the frequency of migraines, making them particularly suitable for individuals with chronic or frequent attacks. This preventive approach aims to enhance the overall quality of life for those who experience migraines regularly.
Beta-blockers are especially beneficial for individuals with comorbid conditions such as hypertension or heart disease. By addressing both cardiovascular concerns and migraines, these medications offer a comprehensive therapeutic approach.
Side Effects
While generally well-tolerated, beta-blockers may cause side effects that individuals need to be aware of. Common side effects include fatigue, dizziness, and changes in sleep patterns. Healthcare professionals need to monitor patients regularly and adjust the dosage or consider alternative medications if side effects become problematic. Beta-blockers are typically avoided in individuals with certain heart conditions, emphasizing the importance of an individualized approach.
Clinical Effects
The clinical effects of beta-blockers in migraine management encompass various dimensions. See some examples below:
- Reduction in Migraine Frequency: Beta-blockers are known for their ability to reduce the frequency of migraine attacks significantly. This preventive effect is especially valuable for individuals experiencing chronic migraines, enhancing their overall quality of life.
- Alleviation of Migraine Severity: Beyond frequency reduction, beta-blockers contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall comfort of individuals during migraine episodes.
- Improvement in Associated Symptoms: Beta-blockers have been shown to address associated symptoms such as nausea and sensitivity to light. By modulating the autonomic nervous system, these medications offer a holistic approach to migraine management.
- Cardiovascular Benefits: Beta-blockers provide additional benefits for individuals with comorbidities due to their primary use in cardiovascular conditions. This dual action allows for comprehensive management of both migraine and cardiovascular health.
Anticonvulsants
Anticonvulsants, originally developed to control seizures in epilepsy, have emerged as a valuable class of medications in the preventive management of migraines (9). According to (9), these drugs, also known as antiepileptic drugs (AEDs), work by stabilizing electrical activity in the brain and reducing the frequency and severity of migraine attacks. Let’s see more details below as described by (32) and (9).
Drug Class
Anticonvulsants comprise a diverse class of medications, including Topiramate, Valproic acid, and Gabapentin. While their primary use may be in epilepsy, the preventive benefits of certain anticonvulsants extend to migraines. These medications are taken regularly to provide ongoing protection against migraines.
Benefits
The primary benefit of anticonvulsants in migraine management is their preventive action. Clinical trials have demonstrated the efficacy of certain anticonvulsants, such as topiramate, in significantly reducing the frequency of migraines. This preventative approach is particularly suitable for individuals with chronic or frequent attacks, aiming to improve overall quality of life.
Anticonvulsants are especially valuable for individuals who may not find relief or experience intolerable side effects with other preventive medications. The versatility of this drug class allows healthcare professionals to tailor treatment plans based on individual patient characteristics and responses.
Side Effects
While generally well-tolerated, anticonvulsants may cause side effects that individuals need to be aware of. Common side effects include drowsiness, dizziness, and gastrointestinal disturbances. It is crucial for healthcare professionals to monitor patients regularly and adjust the dosage or consider alternative medications if side effects become problematic. Additionally, certain anticonvulsants may have specific considerations, such as the need to regularly monitor liver function in individuals taking Valproic acid.
Clinical Effects
The clinical effects of anticonvulsants in migraine management encompass the following dimensions:
- Reduction in Migraine Frequency: Anticonvulsants are known for their ability to significantly reduce the frequency of migraine attacks. This preventive effect is particularly valuable for individuals experiencing chronic migraines, substantially improving their overall quality of life.
- Alleviation of Migraine Severity: Beyond frequency reduction, anticonvulsants contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall comfort of individuals during migraine episodes.
- Improvement in Associated Symptoms: By modulating neurotransmission and neuronal excitability, Anticonvulsants address associated symptoms such as nausea and sensitivity to light. This holistic approach contributes to a more comprehensive management of migraines.
- Beneficial in Comorbid Conditions: Anticonvulsants, due to their broader neurological effects, can be helpful for individuals with comorbid conditions such as epilepsy or mood disorders. This dual benefit allows for comprehensive management and improves overall well-being.

Self-Quiz
Ask Yourself...
- How do Triptans contribute to migraine management, and in what scenarios might healthcare professionals prioritize their use during acute migraine attacks?
- Can you differentiate the mechanisms of action between NSAIDs and Triptans in migraine management, and how might this understanding influence the choice of medication for a specific patient?
- What roles do CGRP inhibitors play in migraine pharmacotherapy?
- Consider a scenario where a patient experiences migraines with comorbid cardiovascular issues. How might the choice of medication be influenced by the need to prioritize both migraine relief and cardiovascular safety?
Clinical Criteria for Prescribing
In migraine management, prescribing medications involves a comprehensive understanding of clinical criteria to tailor interventions effectively. This section explores the clinical factors guiding the prescription of migraine medications and the decision-making process for healthcare providers. Here are some of the factors.
Frequency and Severity of Migraine Attacks
An essential consideration in prescribing migraine medications is the frequency and severity of migraine attacks experienced by the patient. For instance, a patient suffering from frequent and severe attacks may benefit from preventive medications to reduce the overall frequency and intensity of migraines (31).
Individual Response to Pain and Associated Symptoms
The subjective experience of pain and associated symptoms during migraines varies among individuals. A patient who experiences intense nausea and vomiting may require medications with rapid onset and alternative formulations, such as nasal sprays or injectables, to address these specific symptoms effectively (8).
Impact on Daily Functioning and Quality of Life
Prescribing migraine medications involves considering the impact of migraines on a patient’s daily functioning and overall quality of life (24). For example, a working professional with migraines that significantly impede productivity may require acute medications with fast-acting formulations for quick relief during work hours.
Comorbid Conditions and Patient Preferences
Comorbid conditions and patient preferences are pivotal factors in prescribing migraine medications. A patient with comorbid cardiovascular issues may require careful consideration of medication options to mitigate potential risks (2).

Self-Quiz
Ask Yourself...
- How does a patient’s medical history, especially factors like cardiovascular health, influence the clinical criteria for prescribing migraine medications?
- Why is it essential for healthcare professionals to assess the frequency and severity of migraine attacks when determining the clinical criteria for prescribing medications?
- How do patient preferences contribute to the clinical criteria for prescribing migraine medications?
Pharmacokinetics
Understanding the pharmacokinetics of migraine management medications enables healthcare professionals to tailor treatment plans based on individual patient characteristics, ensuring maximum therapeutic benefit. Let’s get into more details for each of the medications listed above:
Triptans
Absorption
Triptans exhibit distinct pharmacokinetic properties that influence their efficacy and onset of action. Following oral administration, Triptans are absorbed through the gastrointestinal tract and the rate of absorption varies among different Triptans, contributing to differences in their clinical profiles. (39)
Distribution
Upon absorption, Triptans undergo distribution to reach target sites in the body, primarily the central nervous system. Their lipophilic nature allows them to penetrate the blood-brain barrier, enabling interaction with serotonin receptors implicated in migraine pathophysiology. The distribution of Triptans influences their ability to exert effects centrally and peripherally. (39)
Metabolism
Metabolism is a crucial aspect of triptan pharmacokinetics, occurring predominantly in the liver. The enzyme responsible for triptan metabolism is monoamine oxidase-A (MAO-A). (39)
Excretion
The final phase in the pharmacokinetic journey of Triptans is excretion, primarily through renal and biliary routes. Renal excretion eliminates the unchanged drug and its metabolites, while biliary excretion expels metabolites via the bile into the gastrointestinal tract. The interplay between metabolism and excretion contributes to the overall pharmacokinetic profile of Triptans. Variations in renal function may influence the elimination of the half-life of certain Triptans, impacting the duration of their therapeutic effect. (39)
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Absorption
Following oral administration, NSAIDs are absorbed in the gastrointestinal tract, with the rate and extent varying among different agents. For instance, ibuprofen exhibits rapid absorption, making it suitable for prompt relief during acute migraine attacks. On the other hand, naproxen has a longer duration of action due to slower absorption, making it well-suited for sustained pain relief. (28)
Distribution
Upon absorption, NSAIDs embark on a journey of distribution throughout the body. Their lipophilic nature allows for penetration into various tissues, including inflamed areas. The distribution influences the drug’s ability to reach target sites, such as the central nervous system, where NSAIDs exert their analgesic and anti-inflammatory effects. This property is particularly relevant in the context of migraines, where the inflammatory component contributes to pain. (28)
Metabolism
Metabolism plays a role in shaping the pharmacokinetic profile of NSAIDs, occurring primarily in the liver. Enzymes such as cytochrome P450 contribute to the biotransformation of NSAIDs into metabolites. The metabolism of NSAIDs can vary among individuals, impacting factors such as drug efficacy and potential side effects. For example, the metabolism of certain NSAIDs, like diclofenac, can be influenced by genetic polymorphisms, contributing to interindividual variability in drug response. (21)
Excretion
The final phase of the NSAID journey involves excretion, predominantly through the kidneys. Unchanged NSAIDs and their metabolites are eliminated via urine. Considerations of renal function are crucial in the context of NSAID use, as impaired kidney function can lead to prolonged drug half-life and increased risk of adverse effects. Regular monitoring of renal function is essential, especially in individuals with conditions that may affect kidney health. (21)
Calcitonin Gene-Related Peptide (CGRP)
Absorption
Administered via subcutaneous injections, CGRP inhibitors such as Erenumab and Fremanezumab enter the bloodstream directly, allowing for precise control over drug levels. This mode of administration ensures a reliable and consistent absorption rate, contributing to the predictability of therapeutic outcomes. (11)
Distribution
Following absorption, CGRP inhibitors are distributed throughout the body, focusing on target sites implicated in migraine pathophysiology, like the central nervous system. (11)
Metabolism
Unlike many traditional medications, CGRP inhibitors follow a different path in terms of metabolism. Due to their biotechnological origin as monoclonal antibodies, these drugs do not undergo significant hepatic metabolism. Instead, proteolytic enzymes break them down into smaller peptides and amino acids, which occur systemically. This unique metabolic pathway aligns with the specificity of CGRP inhibitors, minimizing interactions with hepatic enzymes and potential drug-drug interactions. (37)
Excretion
The final phase of the CGRP inhibitor journey involves excretion, primarily through the kidneys via renal clearance. This aspect is particularly relevant when considering individual patient factors such as renal function, as impaired kidney function can affect the clearance of CGRP inhibitors and influence their duration of action. (37)
Beta-Blockers
Absorption
Administered orally, beta-blockers like propranolol and metoprolol are absorbed through the gastrointestinal tract. Depending on the condition of the gastrointestinal tract, the rate and extent of absorption can vary, impacting the time it takes for these medications to reach therapeutic levels in the bloodstream. (27)
Distribution
Once absorbed, beta-blockers embark on distribution throughout the body. Their lipophilic nature enables penetration through cell membranes, allowing them to reach target tissues, including the heart and blood vessels. In the context of migraine management, the distribution properties of beta-blockers are crucial for their ability to modulate the autonomic nervous system centrally and peripherally, leading to the desired preventive effects against migraines. (27)
Metabolism
The metabolism of beta-blockers occurs primarily in the liver, where enzymes play a role in their biotransformation. Genetic polymorphisms in these enzymes can contribute to interindividual variability in drug metabolism. (27)
Excretion
The final phase of the beta-blocker journey involves excretion, predominantly through the kidneys, where unchanged beta-blockers and their metabolites are eliminated via urine. The renal excretion of these drugs is relevant when considering individual patient factors, such as renal function, as impaired kidney function can affect the clearance of beta-blockers and influence their duration of action. (27)
Anticonvulsants
Absorption
Typically administered orally, anticonvulsants like topiramate and valproic acid are absorbed through the gastrointestinal tract. The rate and extent of absorption play a crucial role in determining the onset of action and overall effectiveness. (9)
Distribution
Following absorption, anticonvulsants undergo distribution throughout the body. Their lipophilic nature allows them to penetrate the blood-brain barrier, reaching target sites in the central nervous system relevant to migraine pathophysiology. The distribution properties of anticonvulsants contribute to their ability to modulate neuronal excitability centrally and exert preventive effects against migraines. (9)
Metabolism
Metabolism is a crucial aspect of anticonvulsant pharmacokinetics. This occurs predominantly in the liver and enzymes play an important role in the biotransformation of anticonvulsants into metabolites. The metabolism of anticonvulsants can vary among individuals, impacting factors such as drug efficacy and potential side effects. For example, valproic acid undergoes extensive hepatic metabolism, and variations in enzyme activity can lead to interindividual variability in drug response. (30)
Excretion
The final phase in the anticonvulsant journey involves excretion, primarily through the kidneys. Unchanged anticonvulsants and their metabolites are eliminated via urine. This renal excretion is relevant when considering individual patient factors such as renal function, as impaired kidney function can affect the clearance of anticonvulsants and influence their duration of action. (30)

Self-Quiz
Ask Yourself...
- How do the pharmacokinetics of Triptans, specifically their absorption and distribution, contribute to their efficacy in managing acute migraine attacks?
- Can you explain the key pharmacokinetic parameters of nonsteroidal anti-inflammatory drugs (NSAIDs) used in migraine management and how they influence drug effectiveness?
- What role do pharmacokinetic factors play in the onset and duration of action of calcitonin gene-related peptide (CGRP) inhibitors?
- In the context of migraine medications, how does the pharmacokinetics of beta-blockers influence their absorption, distribution, metabolism, and excretion in the body?
Warnings Related to Migraine Medications
Understanding potential warnings related to migraine medications is essential for healthcare professionals to ensure safe and effective treatment. Here are some factors to consider.
Medication Safety
Migraine medications, whether preventive or acute, come with specific warnings that need careful attention. For instance, some medications may have contraindications for individuals with certain medical conditions or those taking specific medications concurrently. According to (34), healthcare providers must be vigilant in assessing patient medical histories to identify potential contraindications.
Addressing Cardiovascular Risks
Certain migraine medications, such as Triptans, may pose cardiovascular risks, especially in individuals with pre-existing cardiovascular conditions (35). Therefore, it is crucial for healthcare providers to assess patients’ cardiovascular health and consider alternative medications or dose adjustments for those at higher risk. For example, a patient with a history of myocardial infarction may be advised to avoid Triptans, and a different class of medication, like NSAIDs, may be recommended.
Pregnancy and Lactation Considerations
Warnings related to pregnancy and lactation are paramount. Some migraine medications may have potential risks during pregnancy, and healthcare providers must carefully weigh the benefits and risks when prescribing for pregnant or lactating individuals. For instance, valproic acid is associated with an increased risk of congenital disabilities, and alternative medications with a safer profile may be preferred for pregnant individuals seeking migraine relief (1).
Managing Medication Overuse Headaches (MOH)
A significant warning associated with migraine medications is the risk of medication overuse headaches (34). To prevent this problem, healthcare providers need to educate patients about the importance of adhering to prescribed dosages and avoiding excessive use of acute medications. Offering alternative strategies, such as lifestyle modifications and preventive medications, can be crucial in managing and preventing MOH.


Self-Quiz
Ask Yourself...
- What are some common warnings associated with the use of Triptans in migraine management, and how should healthcare providers address these warnings?
- Can you identify specific cardiovascular risks associated with certain migraine medications, and what should be considered when prescribing these medications to patients with pre-existing cardiovascular conditions?
- What warnings are typically associated with the use of valproic acid in migraine management, particularly concerning specific patient populations such as pregnant individuals?
- How do healthcare providers manage and educate patients about the risk of medication overuse headaches associated with certain migraine medications, and what preventive measures can be implemented to minimize this risk?
Alternatives to Migraine Medications
According to (5), integrating alternative methods provides additional tools for healthcare professionals and empowers individuals seeking a more comprehensive and personalized approach to migraine care. Here are some alternative approaches:
Holistic Lifestyle Modifications
Holistic management of migraines involves lifestyle modifications that can significantly impact the frequency and severity of attacks. For instance, incorporating regular physical activity, maintaining a consistent sleep schedule, and managing stress through practices like mindfulness and yoga have shown promise in reducing migraine occurrence (5). Educating patients about these lifestyle changes empowers them to actively participate in their migraine management.
Biofeedback and Relaxation Techniques
Biofeedback and relaxation techniques offer non-pharmacological interventions that enhance self-awareness and control over physiological responses (22). These approaches teach individuals to recognize and manage stress triggers, ultimately reducing the frequency of migraines. For example, biofeedback training that monitors muscle tension and provides real-time feedback can effectively prevent migraines (22).
Acupuncture and Acupressure
According to (22), traditional Chinese medicine practices like acupuncture and acupressure have gained recognition for their potential in migraine management. Acupuncture involves the insertion of thin needles into specific points on the body, while acupressure applies pressure to these points. Research suggests that these methods reduce the frequency and intensity of migraines, providing an alternative avenue for individuals seeking non-pharmacological options (22).
Nutritional Approaches
Dietary modifications and nutritional approaches also play a role in holistic migraine management. For example, identifying and avoiding potential trigger foods, such as those containing tyramine or artificial additives, can be beneficial (10). Additionally, ensuring adequate hydration and incorporating anti-inflammatory foods into the diet may contribute to overall well-being and migraine prevention (10).

Self-Quiz
Ask Yourself...
- What benefits do biofeedback and relaxation techniques offer in reducing the frequency and intensity of migraines?
- How can biofeedback and relaxation techniques be integrated into a comprehensive migraine management plan?
- What role do dietary modifications and nutritional approaches play in the holistic management of migraines?
- How can healthcare professionals guide patients in identifying trigger foods and making informed nutritional choices?
Nursing Considerations
Nurses play a pivotal role in the holistic care of individuals with migraines, contributing to both the preventive and acute aspects of management through various considerations. Here are some important considerations.
Assessment and Patient Education
A thorough assessment includes evaluating the frequency, duration, and severity of migraines and identifying triggers and associated symptoms (3). Additionally, nurses play a key role in patient education, ensuring individuals clearly understand their migraine condition, the prescribed medications, and potential side effects. For instance, educating a patient about the importance of early intervention with acute medications during a migraine attack empowers them to take timely action.
Monitoring and Adverse Event Management
Nurses actively monitor individuals undergoing migraine treatment, monitoring the response to medications and any potential adverse events. Regular monitoring includes assessing the effectiveness of preventive measures, tracking the frequency of migraine attacks, and identifying patterns that may require adjustments in the treatment plan (34). If adverse events or side effects occur, nurses are instrumental in managing them promptly, collaborating with healthcare providers to ensure the safety and well-being of individuals.
Supportive Care and Holistic Approach
Nursing considerations extend beyond medication management to supportive care and a holistic approach. Nurses provide emotional support, helping individuals cope with the impact of migraines on their daily lives. Moreover, they collaborate with other healthcare professionals to integrate holistic approaches such as lifestyle modifications, stress management, and alternative therapies into the overall care plan. According to (34), this collaborative and patient-centered approach enhances the effectiveness of migraine management.
Documentation and Communication
Accurate and thorough documentation of relevant patient information, medication administration details, and responses to treatment is a fundamental nursing responsibility in migraine management (34). In addition to that, clear and concise communication between nursing staff, healthcare providers, and other healthcare team members ensures continuity of care (34).

Self-Quiz
Ask Yourself...
- How can a thorough patient assessment contribute to the safe and effective administration of migraine medications?
- How do nursing responsibilities extend beyond medication administration to encompass patient education?
- When monitoring individuals undergoing migraine treatment, what are the essential aspects that nurses should observe?
- How does the collaborative communication between nursing staff, healthcare providers, and other team members contribute to the continuity of care in migraine management?
Upcoming Research
Staying ahead of the curve is essential for healthcare professionals to provide cutting-edge care and optimize outcomes for individuals with migraines. Upcoming research include the following:
Advancements in Targeted Therapies
Recent research has unveiled promising advancements in targeted therapies for migraine management. For example, research about monoclonal antibodies targeting the calcitonin gene-related peptide (CGRP) pathway is proving to be effective in preventing migraines (12).
Digital Health and Telemedicine in Migraine Care
Integrating digital health technologies and telemedicine is a burgeoning trend in migraine management research. Smartphone applications for tracking migraine patterns, wearable devices for monitoring physiological parameters, and virtual consultations enable a more comprehensive and patient-centric approach (12). This shift toward digital solutions enhances data collection and facilitates remote monitoring and timely interventions, particularly in scenarios where in-person visits may be challenging (12).
Genetic and Personalized Medicine Approaches
Advancements in genetic research are paving the way for personalized medicine in migraine care. Understanding the genetic underpinnings of migraines can guide the development of targeted interventions tailored to an individual’s unique genetic profile. This personalized approach could revolutionize treatment strategies, allowing for more precise and effective interventions based on the genetic factors contributing to a person’s migraines (13).
Exploration of Lifestyle and Environmental Influences
Upcoming research increasingly focuses on the intricate interplay between lifestyle, environmental factors, and migraines; and studies examining the impact of factors such as diet, sleep patterns, and environmental triggers contribute valuable insights (13). For instance, research may reveal specific dietary components that act as triggers or protective factors for migraines, allowing healthcare professionals to offer targeted lifestyle recommendations.

Self-Quiz
Ask Yourself...
- What recent research findings have emerged regarding migraine prevention?
- How are digital health technologies and telemedicine being incorporated into upcoming research on migraine management?
- In personalized medicine, how is genetic research influencing upcoming approaches to migraine care?
- How can consideration of lifestyle factors and environmental influences contribute to a more holistic approach of migraine management?
Asthma Treatment and Monitoring
Introduction
When hearing the phrase asthma, what comes to mind? If you’re an advanced practice registered nurse (APRN) with prescriptive authority, you’ve definitely heard of asthma before. Even as a nurse or maybe before nursing school, conversations about prescription drug use and respiratory health existed every so often.
Presently, patients seek guidance and information on various health topics from APRNs, including medication management and respiratory health. The information in this course will serve as a valuable resource for APRNs with prescriptive authority of all specialties, education levels, and backgrounds, to learn more about medications that can treat and manage asthma.
Defining Asthma
What Is Asthma?
Asthma is a non-communicable chronic health condition that affects the airways of the lungs and affects millions of people nationwide. Asthma is often diagnosed in childhood and can resolve in adulthood or continue for the rest of a patient’s life. Several studies postulate the cause of asthma, but there is no definitive cause.
Genetics, age, environmental exposures, smoking, and a history of allergies are thought to play a role in asthma severity and development. Clinical presentation of asthma often includes trouble breathing, chronic airway inflammation, and airway hyperresponsiveness. Assessment for asthma often includes patient history, clinical presentation, spirometry testing, and pulmonary function tests (PFTs).
What Are the Stages of Asthma?
Since asthma is a chronic condition, several established guidelines can be used to determine the severity of asthma and explore possible medication options. Depending on the stage of asthma and patient response to existing therapy, treatment and management vary.
The four stages of asthma include intermittent, mild, moderate, and severe. Based on the 2020 National Asthma Education and Prevention Program (NAEPP) guidelines, here is the standard criteria for what constitutes each stage of asthma (2).
Intermittent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness <2 times a week
- Asthmatic flare-ups are short-lived with varying intensity
- Symptoms at night are <2 a month
- No asthmatic symptoms between flare-ups
- Lung function test FEV 1 at >80% above normal values
- Peak flow has <20% variability am-to-am or am-to-pm, day-to-day
Mild persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness 3-6 times a week
- Asthmatic flare-ups may affect activity level and can vary in intensity
- Symptoms at night are 3-4 times a month
- Lung function test FEV1 is >80% above normal values
- Peak flow has less than 20-30% variability
Moderate persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness daily
- Asthmatic flare-ups may affect activity level and can vary in intensity
- Symptoms at night are >5 times a month
- Lung function test FEV1 is 60%-80% of normal values
- Peak flow has more than 30% variability
Severe persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness continuously
- Asthmatic flare-ups affect activity level and often vary in intensity
- Asthmatic symptoms at night are constant
- Lung function test FEV1 is <60% of normal values
- Peak flow has more than 30% variability
Based on patient history, clinical presentation, and these criteria, treatment can be administered to decrease the symptoms of the patient. If a patient presents with symptoms that are outside of your scope of work or understanding, you can always refer patients to a pulmonologist or asthma specialist.
Often times, more severe cases of asthma and asthma emergencies require increased frequency and dosing of asthma-related medications. Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient’s medication history, pulmonary function, and health history prior to prescribing asthma medications (1).
What Are Asthmatic Emergencies?
Asthmatic emergencies are if a patient has asthma symptoms that are beyond what they typically experience and are unable to function without immediate medical intervention. Asthma emergencies can occur as a result of a patient being unable to access their asthmatic medications, being exposed to a possible allergen, or being under increased stress on the body.
Asthmatic emergencies often require collaborative medical intervention, increased dosages of medications discussed below, and patient education to prevent future asthmatic emergencies (1).
What If Asthma Is Left Untreated?
Depending on the clinical presentation and severity of asthma, asthma can cause several long-term complications if left untreated. If asthma is not properly managed, several complications, such as chronic obstructive pulmonary disease (COPD), decreased lung function, permanent changes to the lungs’ airways, and death can occur (1, 2).
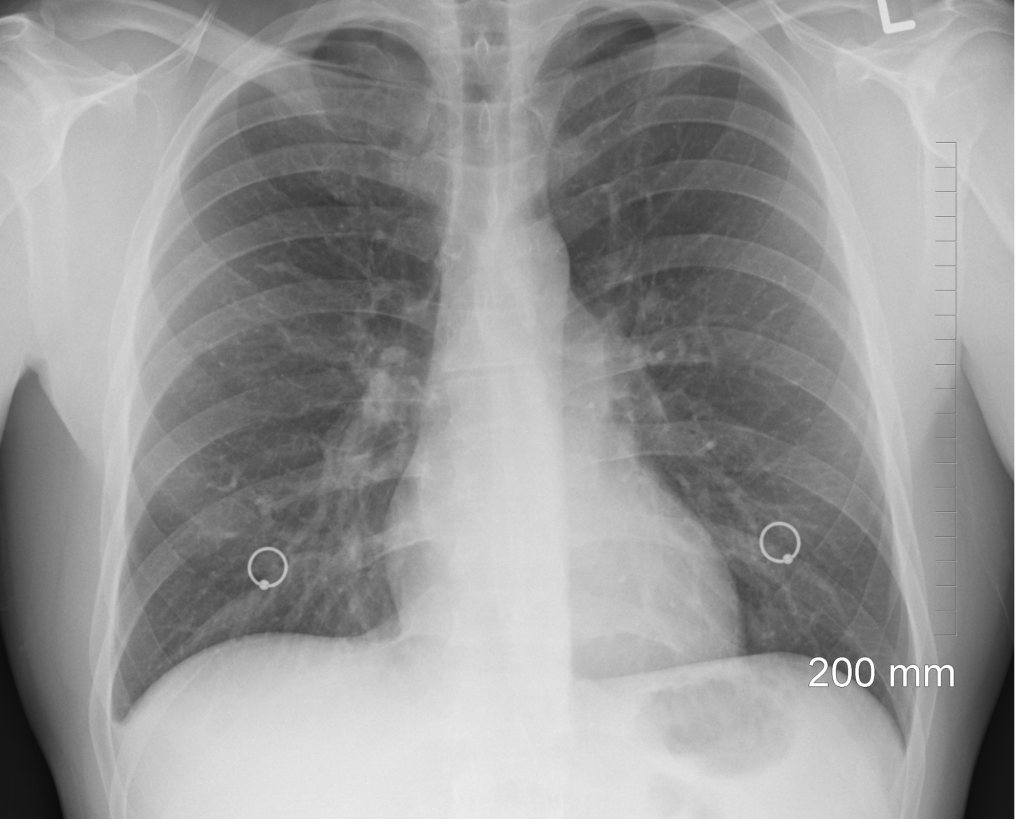
Defining Asthma Medications
What Are Commonly Used Medications to Manage Asthma?
Commonly used medications to manage asthma include inhaled corticosteroids, oral corticosteroids, short-acting beta agonists (SABAs), long-acting beta agonists (LABAs), long-acting muscarinic antagonists (LABAs), adenosine receptor antagonists, leukotriene modifiers, mast cell stabilizers, and monoclonal antibodies. The dosage, frequency, amount of asthma management medications, and medication administration route can all vary depending on clinical presentation, patient health history, and more.
How and Where are Asthma Medications Used?
Asthma medications can be used routinely or as needed for management of asthma symptoms depending on the patient. Asthma medications can be used at home, in public, and in health care facilities. Depending on the specific asthma medication and dosage, these medications can be taken by mouth, by an external device, such as an inhaler, via subcutaneous injection, or via intravenous solution (1).
What Are the Clinical Criteria for Prescribing Asthma Medication?
Clinical criteria for prescribing asthma medication can depend on the clinical presentation of a patient. Assessment of lung health and patient history are essential to determining the dosage and medications needed for adequate asthmatic symptom control.
Clinical guidelines from reputable organizations, such as the National Asthma Education and Prevention Program (NAEPP), the National Institutes of Health (NIH), the Global Initiative for Asthma (GINA), and the American Academy of Family Physicians (AAFP) can provide insight into the latest recommendations for asthma management (1, 2). In addition, local laws or health departments might have recommendations for asthma medication guidelines.
What Is the Average Cost for Asthma Medications?
Cost for asthma medications can significantly vary depending on the type of medication, insurance, dosage, frequency, medication administration route, and other factors. Cost is among a leading reason why many patients cannot maintain their medication regime (3). If cost is a concern for your patient, consider reaching out to your local pharmacies or patient care teams to find cost effective solutions for your patients.


Self-Quiz
Ask Yourself...
- What are some common signs of asthma?
- What are some common medications that can be prescribed to manage asthma?
- What are some factors that can influence asthma development and severity?
Inhaled Corticosteroids Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient’s medication history and health history prior to prescribing asthma medications.
Drug Class – Inhaled Corticosteroids
Commercially available inhaled corticosteroids include: ciclesonide (Alvesco HFA), fluticasone propionate (Flovent Diskus, Flovent HFA, Armon Digihaler), budesonide (Pulmicort Flexhaler), beclomethasone dipropionate (QVAR RediHaler), fluticasone furoate (Arnuity Ellipta), and mometasone furoate (Asmanex HFA, Asmanex Twisthaler).
Clinical criteria for prescribing an inhaled corticosteroid includes adherence to the latest clinical guidelines, patient medical history, patient clinical presentation, and drug availability (4).
Inhaled Corticosteroids Method of Action
Inhaled corticosteroids have an intricate mechanism of action involving several responses to the immune system. Inhaled corticosteroids decrease the existing initial inflammatory response by decreasing the creation and slowing the release of inflammatory mediators. Common inflammatory mediators include histamine, cytokines, eicosanoids, and leukotrienes. Inhaled corticosteroids can also induce vasoconstrictive mechanisms, which, as a result, can lead to less blood flow, resulting in less discomfort and edema (4).
In addition to anti-inflammatory properties, inhaled corticosteroids can create a localized immunosuppressive state that limits the airways’ hypersensitivity reaction, which is thought to reduce bronchospasms and other asthma-associated symptoms. It is important to note that inhaled corticosteroids often do not produce therapeutic effects immediately, as many patients may not see a change in their asthma symptoms for at least a week after beginning inhaled corticosteroid therapy (4).
Inhaled Corticosteroids Side Effects
Every medication has the possibility of side effects, and inhaled corticosteroids are no exception. Common side effects of inhaled corticosteroids include oral candidiasis (thrush), throat irritation, headache, and cough.
Patient education about rinsing their mouth and oral hygiene after use is essential to avoid the possibility of thrush and other oral infections and irritations. More severe side effects can include prolonged immunosuppression, reduction in bone density, and adrenal dysfunction (4).
Inhaled Corticosteroids Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with inhaled corticosteroids, so additional medication, increased dosage, a change in frequency, or a new medication class might need to be considered (4).

Self-Quiz
Ask Yourself...
- What are some possible side effects of inhaled corticosteroids?
- What are some patient considerations to keep in mind when prescribing inhaled corticosteroids?
Oral Corticosteroids Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient’s medication history and health history prior to prescribing asthma medications.
Drug Class – Oral Corticosteroids
Commercially available oral corticosteroids include methylprednisolone, prednisolone, and prednisone. Clinical criteria for prescribing an oral corticosteroid includes adherence to the latest clinical guidelines, patient medical history, patient clinical presentation, and drug availability (4).
Oral Corticosteroids Method of Action
Methylprednisolone and prednisolone have a method of action as intermediate, long-lasting, synthetic glucocorticoids, have COX-2 inhibitory properties, and inhibit the creation of inflammatory cytokines (5).
Prednisone is a prodrug to prednisolone and has anti-inflammatory and immunomodulating glucocorticoid properties. Prednisone has a method of decreasing inflammation by reversing increased capillary permeability and suppressing the movement of certain leukocytes (6).
Oral Corticosteroids Side Effects
Every medication has the possibility of side effects, and oral corticosteroids are no exception. Methylprednisolone and prednisolone have possible side effects of skin changes, weight gain, increased intraocular pressure, neuropsychiatric events, neutrophilia, immunocompromised state, fluid retention, and GI upset.
Consider monitoring symptoms and overall health of patients on systemic corticosteroids to assess for long-term side effects (5). Prednisone has possible side effects of changes in blood glucose, changes in sleep habits, changes in appetite, increased bone loss, an immunocompromised state, changes in adrenal function, and changes in blood pressure (6).
Oral Corticosteroids Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with oral corticosteroids, so additional medication, increased dosage, a change in frequency, or a new medication class might need to be considered (6).

Self-Quiz
Ask Yourself...
- What are some possible side effects of oral corticosteroids?
- What are some patient considerations to keep in mind when prescribing oral corticosteroids versus inhaled corticosteroids?
Short-Acting Beta Agonists (SABAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient’s medication history and health history prior to prescribing asthma medications.
Drug Class – SABAs
Common commercially available SABAs include albuterol sulfate (ProAir HFA, Proventil HFA, Ventolin HFA), albuterol sulfate inhalation powder (ProAir RespiClick, ProAir Digihaler), levalbuterol tartrate (Xopenex HFA), and levalbuterol hydrochloride (Xopenex) (4).
SABAs Method of Action
Short-acting beta-agonists (SABAs) have a rapid onset as broncho-dilating medications. SABAs, especially albuterol in emergent situations, are used often to quickly relax bronchial smooth muscle from the trachea to the bronchioles through action on the β2-receptors.
While SABAs are effective bronchodilators in the short term for asthma symptoms, SABAs do not affect the underlying mechanism of inflammation. As a result, SABAs are often used for short-acting intervals, such as few hours, and have limited capabilities to prevent asthma exacerbations alone (4). SABAs can be administered via meter-dosed inhalers, intravenous, dry powder inhalers, orally, subcutaneously, or via nebulizer.
SABAs Side Effects
Every medication has the possibility of side effects, and SABAs are no exception. Because of the beta receptor agonisms, possible SABA side effects include increased heart rate, chest pain, chest palpitations, body tremors, and nervousness (4). Because of the short half-life of SABAs, chronic side effects are not typically observed.
SABAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with SABAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self-Quiz
Ask Yourself...
- What are some possible side effects of short-acting beta agonists?
- What are some patient considerations to keep in mind when prescribing SABAs?
Long-Acting Beta Agonists (LABAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient’s medication history and health history prior to prescribing asthma medications.
Drug Class – LABAs
Common commercially available LABAs are salmeterol and formoterol (7).
LABAs Method of Action
Long-acting beta-agonists (LABAs) have a rapid onset like SABAs, but also have a longer half-life. LABAs are used often as asthma maintenance medications to relax bronchial smooth muscle from the trachea to the bronchioles through action on the β2-receptors. While SABAs are effective bronchodilators in the short term for asthma symptoms, LABAs are effective bronchodilators in the long term for asthma symptoms.
Like SABAs, LABAs do not affect the underlying mechanism of inflammation. LABAs can be administered via meter-dosed inhalers, intravenous, dry powder inhalers, orally, subcutaneously, or via nebulizer. LABAs are often effective for 12-hour durations (7).
LABAs Side Effects
Every medication has the possibility of side effects, and LABAs are no exception. Like SABAs, because of the beta receptor agonisms, possible LABA side effects include increased heart rate, chest pain, chest palpitations, body tremors, and nervousness (7). Other more prolonged side effects can include changes in blood glucose levels and changes in potassium levels with prolonged LABA use (7).
LABAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with LABAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).
In addition, there are combination inhaled corticosteroid/LABA medications that can be considered, such as fluticasone propionate and salmeterol (Advair Diskus, Advair HFA, AirDuo Digihaler, AirDuo RespiClick, Wixela Inhub), fluticasone furoate and vilanterol (Breo Ellipta), mometasone furoate and formoterol fumarate dihydrate (Dulera), and budesonide and formoterol fumarate dihydrate (Symbicort) (4).

Self-Quiz
Ask Yourself...
- What are some possible side effects of LABAs?
- What are some patient considerations to keep in mind when prescribing SABAs compared to LABAs?
Long-Acting Muscarinic Antagonists (LAMAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient’s medication history and health history prior to prescribing asthma medications.
Drug Class – LAMAs
Common commercially available LAMAs include two inhalation powders via inhalers known as tiotropium bromide (Spiriva Respimat) and fluticasone furoate, umeclidinium, and vilanterol (Trelegy Ellipta) (4).
LAMAs Method of Action
Both drugs mentioned above are long-acting muscarinic antagonists (LAMAs). LAMAs work to alleviate asthmatic symptoms by antagonizing the type 3 muscarinic receptors in bronchial smooth muscles, resulting in relaxation of muscles in the airway (4). Because LAMAs are long-acting, they are not recommended for cases of acute asthma exacerbations or asthmatic emergencies (4).
LAMAs Side Effects
Possible LAMA side effects include urinary retention, dry mouth, constipation, and glaucoma (4).
LAMAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with LAMAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self-Quiz
Ask Yourself...
- What are some possible side effects of LAMAs?
- What are some patient considerations to keep in mind when prescribing LAMAs?
Adenosine Receptor Antagonists Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient’s medication history and health history prior to prescribing asthma medications.
Drug Class – Adenosine Receptor Antagonists
The commercially available adenosine receptor antagonist for asthma management is theophylline as a pill or intravenous (8).
Adenosine Receptor Antagonists Method of Action
The method of action for theophylline is acting as a nonselective adenosine receptor antagonist, acting as a competitive, nonselective phosphodiesterase inhibitor, and reducing airway responsiveness to histamine, allergens, and methacholine (8).
Adenosine Receptor Antagonists Side Effects
Common side effects of theophylline include GI upset, headache, dizziness, irritability, and arrythmias (8).
Adenosine Receptor Antagonists Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with theophylline, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self-Quiz
Ask Yourself...
- What are some possible side effects of adenosine receptor antagonists?
- What are some patient considerations to keep in mind when prescribing adenosine receptor antagonists?

Leukotriene Modifiers Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient’s medication history and health history prior to prescribing asthma medications.
Drug Class – Leukotriene Modifiers
Commercially available leukotriene modifiers include montelukast (Singular) and zafirlukast (Accolate) as oral pills taken once a day. Zileuton (Zyflo CR) is a 5-lipoxygenase inhibitor that also modifies leukotriene activity (4).
Leukotriene Modifiers Method of Action
Montelukast and zafirlukast work to control asthma-related symptoms by targeting leukotrienes, which are eicosanoid inflammatory markers. Montelukast works in particular by blocking leukotriene D4 receptors in the lungs, thus allowing decreased inflammation in the lungs and increased relaxation of lung smooth muscle (9).
Zafirlukast works by being a competitive antagonist at the cysteinyl leukotriene-1 receptor (CYSLTR1) (10). Zileuton is a 5-lipoxygenase inhibitor, in which 5-lipoxygenase is needed for leukotriene creation. Blocking 5-lipoxygenase decreases the formation of leukotrienes at several receptors. As a result of decreased leukotriene production, there is decreased inflammation, decreased mucus secretion, decreased bronchoconstriction (11).
Leukotriene Modifiers Side Effects
Possible side effects of montelukast include headaches, GI upset, and upset. Neuropsychiatric events, such as nightmares, changes in sleep, depression, and suicidal ideation are more severe side effects associated with montelukast.
Possible side effects of zafirlukast include headache, GI upset, and hepatic dysfunction (9).
Possible side effects of zileuton include hepatic dysfunction, changes in sleep, changes in mood, headaches, and GI upset. When the leukotriene modifiers, neuropsychiatric side effects are to be monitored for in particular, especially for suicidal ideation (9,10,11).
Leukotriene Modifiers Alternatives
Some patients might not report their symptoms alleviating with leukotriene modifiers, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self-Quiz
Ask Yourself...
- What are some possible side effects of leukotriene modifiers?
- What are some patient considerations to keep in mind when prescribing leukotriene modifiers?
Mast Cell Stabilizer Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient’s medication history and health history prior to prescribing asthma medications.
Drug Class – Mast Cell Stabilizer
A commercially available mast cell stabilizer is cromolyn available via metered-dose inhaler and nebulizer solution (12).
Mast Cell Stabilizer Method of Action
Cromolyn has a method of action in which it inhibits the release of inflammatory mediators from cells, such as the release of histamine and leukotrienes (12).
Mast Cell Stabilizer Side Effects
Every medication has the possibility of side effects, and cromolyn is no exception. Common side effects of cromolyn include dry throat, throat irritation, drowsiness, dizziness, cough, headache, and GI upset (12).
Mast Cell Stabilizer Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with mast cell stabilizers, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self-Quiz
Ask Yourself...
- What are some possible side effects of mast cell stabilizers?
- What are some patient considerations to keep in mind when prescribing mast cell stabilizers?
Monoclonal Antibody Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient’s medication history and health history prior to prescribing asthma medications.
Drug Class – Monoclonal Antibody
Commercially available monoclonal antibodies include Omalizumab (Xolair), mepolizumab (Nucala), reslizumab (Cinqair), benralizumab (Fasenra), dupilumab (Dupixent), and tezepelumab-ekko (Tezspire). Omalizumab, mepolizumab, benralizumab, dupilumab, and texepelumab-ekko are available via subcutaneous injection. Reslizumab is available via intravenous solution (4).
Monoclonal Antibody Method of Action
Omalizumab is an anti-IgE monoclonal antibody that works by inhibiting the binding of IgE to mast cells and basophils. As a result of decreased bound IgE, activation and release of mediators, such as histamine, in the allergic response are decreased (13).
Mepolizumab, reslizumab, and benralizumab are interleukin (IL)-5 antagonists. These IL-5 antagonists inhibit IL-5 signaling, allowing for a decrease in the creation and survival of eosinophils. However, the full method of action for IL-5 antagonists is still unknown, as more evidence-based research is needed (4, 15).
Dupilumab is an IgG4 antibody that inhibits IL-4 and IL-13 signaling by binding to the IL-4Rα subunit. This inhibition of the IL-4Rα subunit allows for the decrease of IL-4 and IL-13 cytokine-induced inflammatory responses (14).
Tezepelumab-ekko is an IgG antibody that binds to the thymic stromal lymphopoietin (TSLP) and prevents TSLP from interacting with the TSLP receptor. Blocking TSLP decreases biomarkers and cytokines associated with inflammation. Knowing this, the full method of action for Tezepelumab-ekko is still unknown, as more evidence-based research is needed4,15.
Monoclonal Antibody Side Effects
Possible side effects of omalizumab include injection site reactions, fracture, anaphylaxis, headache, and sore throat (13). Possible side effects of mepolizumab, reslizumab, and benralizumab include injection site reactions, headache, and hypersensitivity reactions (4). Possible side effects of dupilumab include joint aches, injection site reactions, and headache (14). Possible side effects of tezepelumab-ekko include injection site reactions and headache (14).
Monoclonal Antibody Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with monoclonal antibodies, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self-Quiz
Ask Yourself...
- What are some possible side effects of monoclonal antibodies?
- What are some patient considerations to keep in mind when prescribing monoclonal antibodies?
Nursing Considerations
Nurses remain the most trusted profession for a reason, and APRNs are often pillars of patient care in several health care settings. Patients turn to nurses for guidance, education, and support. While there is no specific guideline for the nurses’ role in asthma education and management, here are some suggestions to provide quality care for patients currently taking medications to manage asthma or concerned about possibly having asthma.
- Take a detailed health history. Often times, respiratory symptoms, such as a cough or trouble breathing, are often dismissed in health care settings, or seen as “common symptoms with everyone.” If a patient is complaining of symptoms that could be related to asthma, inquire more about that complaint.
Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient’s complaint is not being taken seriously by other health care professionals, advocate for that patient to the best of your abilities.
- Review medication history at every encounter. Often times, in busy clinical settings, reviewing health records can be overwhelming. Millions of people take asthma medications at varying dosages, frequencies, and times of day. Many people with asthma take more than one medication to manage their symptoms.
Ask patients how they are feeling on the medication, if their symptoms are improving, and if there are any changes to medication history.
- Be willing to answer questions about asthma, respiratory health, and medication options. Society stigmatizes open discussions of prescription medication and can minimize symptoms of asthma, such as a chronic cough.
There are many people who do not know about medication options or the long-term effects of undiagnosed or poorly managed asthma. Be willing to be honest with yourself about your comfort level discussing topics and providing education on asthma medications and asthma clinical assessment options.
- Inquire about a patient’s life outside of medications, such as their occupation, living situation, and smoking habits. Household exposures, such as carpets or pets, can trigger asthma. Occupations with high exposure to smoke can also trigger asthmatic symptoms. Smoking, living with someone who smokes, or residing in an area with high levels of pollution can also influence asthma symptoms.
Discuss possible solutions to help with symptoms, such as improving ventilation, increasing air quality, and mask wearing when possible.
- Communicate the care plan to other staff involved for continuity of care. For several patients, especially for patients with severe asthma, care often involves a team of nurses, specialists, pharmacies, and more. Ensure that patients’ records are up to date for ease in record sharing and continuity of care.
- Stay up to date on continuing education related to asthma medications, as evidence-based information is always evolving and changing. You can then present your new learnings and findings to other health care professionals and educate your patients with the latest information. You can learn more about the latest research on asthma and asthma-related medications by following updates from evidence-based organizations.
How can nurses identify if someone has asthma?
Unfortunately, it is not always possible to look at someone with the naked eye and determine if they have asthma. While some people might have visible asthmatic symptoms, such as wheezing or trouble breathing, asthmatic clinical presentation can significantly vary from person to person.
APRNs can identify and diagnose if someone has asthma by taking a complete health history, listening to patient’s concerns, and offering pulmonary function testing.
What should patients know about asthma medications?
Patients should know that anyone has the possibility of experiencing side effects medications for asthma management, just like any other medication. Patients should be aware that if they notice any changes in their mood, experience any sharp headaches, or feel like something is a concern, they should seek medical care.
Nurses should also teach patients to advocate for their own health in order to avoid untreated or undetected asthma and possible chronic complications from asthma or asthma-related medications.
Here are important tips for patient education in the inpatient or outpatient setting:
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors).
- Tell the health care provider of any existing lifestyle concerns, such as tobacco use, other drug use, sleeping habits, occupation, diet, menstrual cycle changes (need to identify lifestyle factors that can influence asthmatic medication use, asthma severity, and asthma management).
- Tell the health care provider if you have any changes in your breathing, such as pain with deep breathing or persistent coughing (potential asthma exacerbation symptoms or possibility of asthma medications not being as effective for treatment).
- Tell the nurse of health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life.
- Keep track of your health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes).
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality is a possible side effect for montelukast use).
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries.
- Tell the health care provider if you notice any changes while taking medications or on other treatments to manage asthma (potential worsening or improving health situation).

Self-Quiz
Ask Yourself...
- What are some problems that can occur if medications are not asthma properly?
- What are some possible ways you can obtain a detailed, patient centric health history?
- What are some possible ways APRNs can educate patients on asthma and air quality?
Research Findings
What Research on Asthma Medication Exists Presently?
There is extensive publicly available literature on asthma and asthma-related medications via the National Institutes of Health and other evidence-based journals (1,2,4).
What are some ways for people who take asthma medications to become a part of research?
If a patient is interested in participating in clinical trial research, they can seek more information on clinical trials from local universities and health care organizations.

Self-Quiz
Ask Yourself...
- What are some reasons someone would want to enroll in clinical trials?
SSRI Use in Major Depressive Disorder
Introduction
When hearing the phrase selective serotonin reuptake inhibitors, what comes to mind? If you’re an advanced practice registered nurse (APRN) with prescriptive authority, you’ve heard of SSRIs before. Even as a nurse or maybe before nursing school, conversations about prescription drug use and mental health existed every so often.
Presently, patients seek guidance and information on various health topics from APRNs, including medication management, women’s health, and mental health. The information in this course will serve as a valuable resource for APRNs with prescriptive authority of all specialties, education levels, and backgrounds to learn more about SSRIs and major depressive disorder (MDD).
Defining SSRIs
What Are SSRIs?
Selective serotonin reuptake inhibitors, known as SSRIs, are a type of pharmacological drug class. SSRIs have existed for the past several decades as a class of prescription medications that can manage major depressive disorder (MDD) and other mental health conditions (1).
While this course focuses explicitly on SSRI use in MDD management, SSRIs are also Food and Drug Administration (FDA) approved to manage obsessive-compulsive disorder (OCD), panic disorder (PD), post-traumatic stress disorder (PTSD), and social anxiety disorder (SAD). In addition, several off-label uses for SSRI include management for binge eating disorder and menopausal vasomotor symptoms.
How and Where Are SSRIs Used?
SSRIs are commonly prescribed to manage MDD and other mood disorders in the U.S. and around the world in pediatric, adult, and geriatric populations (1, 2). SSRIs can be taken by mouth as a pill, capsule, or liquid oral solution. Presently, SSRIs cannot be offered via intravenous, rectal, buccal, or injection routes.
What Is the Clinical Criteria for Prescribing SSRIs?
Clinical criteria for prescribing SSRIs can vary depending on the intention for the SSRI. In the case of MDD, several factors can play a role in the clinical criteria for prescribing SSRIs. A patient’s adherence to swallowing a pill daily, dosage given the patient’s weight, medical history, and MDD concerns, and prior experience with other medications can influence prescribing SSRIs. When considering prescribing SSRIs for MDD management, consider assessing the patient for MDD first, taking a detailed health history, and discussing the risk versus benefits of starting SSRIs for this patient (1, 3).
What Is the Average Cost for SSRIs?
Cost for SSRIs can significantly vary depending on the type of SSRI, insurance, dosage, frequency, and other factors. Cost is among leading reasons why many patients cannot maintain their medication regime (4). If cost is a concern for your patient, consider reaching out to your local pharmacies or patient care teams to find cost-effective solutions for your patients.
What Is Major Depressive Disorder (MDD)?
Major depressive disorder (MDD) is a mental health condition in which a person has consistent appetite changes, sleep changes, psychomotor changes, decreased interest in activities, negative thoughts, suicidal thoughts, and depressed mood that interfere with a person’s quality of life (5). According to the Diagnostic and Statistical Manual of Mental Health Disorders, a patient must have at least five persistent mood related symptoms, including depression or anhedonia (loss of interest in activities once enjoyed), that interferes with a person’s quality of life to be formally diagnosed with MDD. Note that MDD does not include a history of manic episodes, and pediatric populations can present with more variable MDD symptoms (5). As an APRN, you can assess for MDD by doing a detailed patient health history or having a patient complete the Patient Health Questionnaire-9 (PHQ-9) – a depression assessment tool (5).


Self-Quiz
Ask Yourself...
- What are some medication administration options for SSRIs?
- What populations can be prescribed SSRIs?
SSRI Pharmacokinetics
Drug Class SSRIs
Selective serotonin reuptake inhibitors, known as SSRIs, are a type of pharmacological drug class part of the antidepressant drug class. They can be prescribed at various dosages depending on the patient history, severity of major depressive disorder (MDD), other medication use, and other factors based on patient-centered decision making. Currently, SSRIs that are FDA approved for MDD management include paroxetine, sertraline, citalopram, escitalopram, vilazodone, and fluoxetine. SSRIs can be prescribed for the oral route and are available via capsule, tablet, or liquid suspension/solution. SSRIs can be taken at any time of day. They can be taken with or without food, though vilazodone in particular is recommended with food. SSRIs are often prescribed to be taken once a day, sometimes twice a day, depending on the severity of MDD. Health care provider professional discretion and patient condition should guide therapy (1).
SSRIs are metabolized by and known to affect the cytochrome P450 system. CYP2D6 inhibitors include escitalopram, citalopram, sertraline, paroxetine, and fluoxetine. Fluoxetine and fluvoxamine are inhibitors of CYP2C19. Fluvoxamine is an inhibitor of CYP1A2. Consider reviewing a patient’s medication history and health history prior to prescribing SSRIs (1).
SSRIs Method of Action
SSRI method of action has been subject to several studies, especially in the last few years. Serotonin is a neurotransmitter that plays a role in mood and other bodily functions. It can be measured in plasma, blood, urine, and CSF (6). It is important to note that serotonin is rapidly metabolized to 5-hydroxyindoleacetic acid (5-HIAA) (6). SSRIs work by inhibiting the reuptake of serotonin at certain chemical receptors, thereby increasing serotonin activity and concentration (1). SSRIs inhibit the serotonin transporter (SERT) at the presynaptic axon terminal.
By obstructing the SERT, a higher amount of serotonin (5-hydroxytryptamine or 5HT) remains in synaptic clefts. This higher amount of serotonin can then stimulate postsynaptic receptors for a more extended period (1). While SSRIs can increase serotonin activity, there is some evidence that suggests the possibility of long-term SSRI use reducing serotonin concentration (6). In addition, the clinical response to SSRIs in patients with MDD can take anywhere from a few to several weeks to emerge (7). While some research suggests that there are initial improvements in mood, evidence remains inconclusive as to the exact time SSRIs can take to provide a therapeutic response for patients (7). Also, while research suggests that SSRIs can increase serotonin levels, there is still mixed evidence on the exact method of action for SSRIs (7).
As a result, it is important to counsel patients that SSRIs can take a few weeks to provide a therapeutic response and to monitor mood and symptoms while taking SSRIs.
SSRI Side Effects
Every medication has the possibility of side effects, and SSRIs are no exception. Fortunately, SSRIs are known to have less side effects than other drug classes of antidepressants, such as monoamine oxidase inhibitors (MAOIs) or tricyclic antidepressants (TCAs). The most commonly known side effects of SSRIs include weight gain, sleep changes, headache, gastrointestinal issues, drowsiness, orthostatic hypotension, and sexual function changes (1).
Sleep changes can include an increased desire to sleep, increase in the amount of time sleeping, or insomnia. Gastrointestinal issues can include an upset stomach, nausea, or dry mouth. Mood changes, such as anxiety, are possible side effects as well. Sexual function changes can include erectile dysfunction, libido changes, impaired orgasmic response, and vaginal dryness (1, 8).
There are more serious possible side effects of SSRIs as well. For instance, SSRIs have the possible side effect of QT prolongation, which if left untreated or undiagnosed, can lead to fatal cardiac arrythmias (1, 8). In particular, the SSRI citalopram has been shown to have more of a risk for QT prolongation compared to other SSRIs. Also, like any other medication that can possibly increase levels of serotonin in the body, there is a possibility of serotonin syndrome as a complication of SSRI use. Possible serotonin syndrome clinical manifestations include increased blood pressure, increased sweating, increased reflex ability, and increased dry eyes (8). Due to the wide varied range of side effects, patient counseling, monitoring, and education is essential when prescribing SSRIs.
SSRI Black Box Warning
In 2004, the FDA issued a black box warning for SSRIs and other antidepressant medications due to the possible increased risk of suicidality in pediatric and young adult populations (up to age 25). When considering SSRI use in patients under 25 and knowing MDD is a risk factor for suicidality, having a conversation with the patient about risks versus benefits must be considered. However, in the past several years since the FDA’s warning, there is no clear evidence showing a correlation between SSRIs and the increased risk of suicidality (1, 8). Health care provider professional discretion and patient condition should guide therapy.
SSRI Alternatives
MDD can be a complex, chronic condition to manage with varying clinical presentation and influence on a patient’s quality of life. There are several alternatives to SSRI use, such as: (1, 9)
- Other prescription drugs
- Serotonin-norepinephrine reuptake inhibitors (SNRIs). Commonly known SNRIs include milnacipran, venlafaxine, desvenlafaxine, duloxetine, and levomilnacipran.
- Atypical antidepressants. Commonly known atypical antidepressants include bupropion and mirtazapine.
- Tricyclic antidepressants (TCAs). Commonly known TCAs include amitriptyline, desipramine, imipramine, clomipramine, doxepin, and nortriptyline.
- Monoamine oxidase inhibitors (MAOIs). Commonly known MAOIs include phenelzine, tranylcypromine, isocarboxazid, and selegiline.
- Psychotherapy, such as cognitive behavioral therapy (CBT) or interpersonal therapy
- Electroconvulsive therapy (ECT)
- Vagus Nerve Stimulation (VNS)
- Transcranial Magnetic Stimulation (TMS)

Self-Quiz
Ask Yourself...
- What are some possible side effects of SSRIs?
- What are some pharmacological alternatives to SSRIs?
Nursing Considerations
Nurse’s Role
What Is the Nurses’ Role in SSRI Patient Education and Management?
Nurses remain the most trusted profession for a reason, and APRNs are often pillars of patient care in several health care settings. Patients turn to nurses for guidance, education, and support. While there is no specific guideline for the nurses’ role in SSRI education and management, here are some suggestions to provide quality care for patients interested in or currently taking SSRIs to manage current or suspected major depressive disorder (MDD).
- Take a detailed health history. Often times, mental health symptoms, such as depressive thoughts or anxiety, are often dismissed in health care settings, even in mental health settings. If a patient is complaining of symptoms that could be related to major depressive disorder, inquire more about that complaint. Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient’s complaint is not being taken seriously by other health care professionals, advocate for that patient to the best of your abilities.
- Review medication history at every encounter. Often times, in busy clinical settings, reviewing health records can be overwhelming. While a vast number of people take SSRIs, many are no longer benefiting from the medication. Ask patients how they are feeling on the medication, if their symptoms are improving, and if there are any changes to medication history.
- Ask about family history. If someone is complaining of symptoms that could be related to MDD, ask if anyone in their immediate family, such as their parent or sibling, experienced similar conditions.
- Be willing to answer questions about mental health and SSRIs. Society can often stigmatize open discussions of prescription medication and mental health. SSRIs are no exception. There are many people who do not know about the benefits and risks of SSRIs, the long-term effects of unmanaged MDD, or possible treatment options. Be willing to be honest with yourself about your comfort level discussing topics and providing education on SSRIs and MDD.
- Communicate the care plan to other staff involved for continuity of care. For several patients, MDD management often involves a team of mental health professionals, nurses, primary care specialists, pharmacies, and more. Ensure that patients’ records are up to date for ease in record sharing and continuity of care.
- Stay up to date on continuing education related to SSRIs and mental health conditions, as evidence-based information is always evolving and changing. You can then present your new findings to other health care professionals and educate your patients with the latest information. You can learn more about the latest research on SSRIs and mental health by following updates from evidence-based organizations.
Identifying Major Depressive Disorder
How can nurses identify if someone has major depressive disorder?
Unfortunately, it is not possible to look at someone with the naked eye and determine if they have MDD. APRNs can identify and diagnose if someone has MDD by taking a complete health history, listening to patient’s concerns, having patients complete the PHQ-9 questionnaire and communicating any concerns to other health care professionals (9).
Patient Education
What should patients know about SSRIs?
Patients should know that anyone has the possibility of experiencing side effects of SSRIs, just like any other medication. Patients should be aware that if they notice any changes in their mood, experience any sharp headaches, or feel like something is a concern, they should seek medical care. Due to social stigma associated with mental health and SSRI use, people may be hesitant to seek medical care for fear of being dismissed by health care professionals (1, 6). In addition, side effects (that interfere with the quality of life) are often normalized (1, 6). However, as more research and social movements discuss mental health and SSRI use more openly, there is more space and awareness for SSRI use and mental health.
Nurses should also teach patients to advocate for their own health in order to avoid progression of MDD and possible unwanted side effects of SSRIs. Here are important tips for patient education in the inpatient or outpatient setting.
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors)
- Tell the health care provider of any existing lifestyle concerns, such as alcohol use, other drug use, sleeping habits, diet, menstrual cycle changes (need to identify lifestyle factors that can influence SSRI use and MDD)
- Tell the health care provider if you notice any changes in your mood, behavior, sleep, sexual health (including vaginal dryness or erectile dysfunction), or weight (possible changes that could hint at more chronic side effects of SSRIs)
- Tell the health care provider if you have any changes in urinary or bowel habits, such as increased or decreased urination or defecation (potential risk for SSRI malabsorption or possible unwanted side effects)
- Tell the nurse of health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life
- Keep track of your mental health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes)
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality is a possible side effect for SSRI use)
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries
- Tell the health care provider if you notice any changes while taking medications or on other treatments to manage your MDD (potential worsening or improving mental health situation)


Self-Quiz
Ask Yourself...
- What are some possible ways you can obtain a detailed, patient centric health history?
- What are some possible ways APRNs can educate patients on SSRIs and major depressive disorder?
Research Findings
What Research on SSRIs exists presently?
There is extensive publicly available literature on SSRIs via the National Institutes of Health and other evidence-based journals.
What are some ways for people who take SSRIs to become a part of research?
If a patient is interested in participating in clinical trial research, they can seek more information on clinical trials from local universities and health care organizations.

Self-Quiz
Ask Yourself...
- What are some problems that can occur if SSRIs are not managing major depressive disorder symptoms adequately?
- What are some reasons someone might want to enroll in SSRI clinical trials?
Case Study
Case Study Part 1
Susan is a 22-year-old Black woman working as a teacher. She arrives for her annual exam at the local health department next to her place of work. She reports nothing new in her health, but she says she’s been feeling more tired over the past few months. Susan reports having some trouble sleeping and trouble eating but doesn’t feel too stressed overall. She heard one of her friends talking about SSRIs and wants to try them, but she’s never taken prescription medications long-term before. She also thinks she might have some depression because she looked at some forums online and resonated with a lot of people’s comments.

Self-Quiz
Ask Yourself...
- What are some specific questions you’d want to ask about her mental health?
- What are some health history questions you’d want to highlight?
- What lab work would you suggest performing?
Case Study Part 2
Susan agrees to complete bloodwork later this week and thinks she might have a family history of depression. She said that no one in her family talks about mental health, but she heard about depression from her friends recently and family a long time ago. She’s back in the office a few weeks later, and her labs are within normal limits. Susan states she’s still feeling fatigued and feeling a bit more hopeless these days. She denies thinking about hurting herself or others.

Self-Quiz
Ask Yourself...
- How would you discuss Susan’s mental health concerns?
- How would you explain to Susan the influence of lifestyle, such as sleep, diet, and environment, on mood?
Case Study Part 3
Susan completed the PHQ-9 questionnaire and had a high score. After discussing her responses with her, you diagnose her with MDD. Susan admits that she is open to trying SSRIs. She is also open to seeing a therapist, as she states that she’s never been to therapy. She would like resources on any therapy services, medication options, and non-pharmacological options to help her manage her condition.

Self-Quiz
Ask Yourself...
- Knowing Susan’s concerns, what are some possible non-pharmacological management options for her MDD?
- What are some major SSRI side effects to educate Susan on?
Conclusion
Major depressive disorder is a complex chronic health condition that affects many people nationwide. SSRIs are often a first-line pharmacological option for MDD management. However, clinical presentation and symptom management with SSRIs can vary widely. While some patients would prefer a low-dose SSRI, others will need a higher dose and possible extra medication management. Education and awareness of SSRIs can influence the lives of many people.
Antibiotic Use in UTI
Definitions
This section covers the definitions related to UTI treatment and management.
Urinary Tract Infection
Bacterial infection of the lower urinary tract (usually confined to the bladder). This is also sometimes called cystitis and is primarily caused by the bacteria E. coli [2].
Asymptomatic Bacteremia
A urine specimen is collected on a patient and shows the presence of bacteria, but they do not have any UTI symptoms [5].
Pyelonephritis
Bacterial infection of the upper urinary tract (i.e. kidneys) [6].
Urosepsis
When a urinary tract infection causes a systemic infection, also known as sepsis [6].

Self-Quiz
Ask Yourself...
- What is a urinary tract infection?
- What is asymptomatic bacteremia?
- What is pyelonephritis?
- What is urosepsis?
Medications Overview
This section briefly reviews UTI antibiotic classes and medical indications.
Certain antibiotics are used to prevent or treat urinary tract infections and are used in both inpatient and outpatient settings. Healthcare providers should follow current guidelines regarding UTI treatment, which depends on the patient and type of urinary tract infection. UTI treatment algorithms are further divided into:
- Uncomplicated UTIs
- Complicated UTIs
- Prophylactic treatment for recurrent UTIs [6]
What constitutes uncomplicated UTIs are patients who have urinary symptoms, but do not have signs of systemic infections, like fever, flank pain, costovertebral angle (CVA) tenderness, etc. Patients can be male or female, unlike previous guidelines that categorized all males as complicated UTIs. Also, patients with uncomplicated UTIs usually have no underlying health conditions or risk factors that may affect treatment [6].
Conversely, complicated UTIs occur when patients have systemic symptoms. Patients who are pregnant, have a history of UTIs, or who are considered elderly also fall under complicated UTIs. Patients with pyelonephritis are automatically considered as having complicated UTIs as well. Patients with recurrent UTIs may be prescribed certain low-dose antibiotics for prevention [6].
Regardless of the UTI type, below are some of the common antibiotics prescribed:
- Trimethoprim-sulfamethoxazole
- Nitrofurantoin
- Fluoroquinolones
- Ciprofloxacin
- Levofloxacin
- Beta-lactams
- Cephalexin
- Amoxicillin-clavulanate
- Ceftriaxone
- Cefdinir
- Piperacillin-tazobactam
- Meropenem
- Fosfomycin
- Pivmecillinam


Self-Quiz
Ask Yourself...
- What are some factors that classify an uncomplicated UTI?
- What are some factors that classify a complicated UTI?
- What are the different names and types of antibiotics used to treat UTI?
Pharmacokinetics
This section discusses the pharmacokinetics of each antibiotic medication used to treat UTIs.
Trimethoprim-sulfamethoxazole
Sulfonamides, also called sulfa drugs, are a class of medications commonly used to treat bacterial infections, including UTIs. A common sulfonamide medication used to treat UTIs is sulfamethoxazole formulated with trimethoprim which is sometimes abbreviated as TMP-SMX, TMP-sulfa, or TMP-SMZ [22]. Trimethoprim-sulfamethoxazole is also approved by the Federal Drug Administration (FDA) to treat chronic bronchitis exacerbations, otitis media in children, and shigellosis.
This medication is also used for prevention and treatment of traveler’s diarrhea, toxoplasmosis, and Pneumocystis jirovecci and Pneumocystis carinii pneumonia. Some other off-label or non-FDA-approved uses are tuberculosis, malaria, listeria, pertussis, and community-acquired pneumonia [10].
Since this a combination medication, TMP-SMX works by two different mechanisms of action. Trimethoprim competes with the enzyme dihydrofolate reductase and subsequently stops the production of tetrahydrofolate from converting to folate.
Sulfamethoxazole, a CYP2CP inhibitor, competes with p-aminobenzoic acid during dihydrofolate synthesis. These two medications combined work against folate production and block bacterial biosynthesis of nucleic acids and proteins. Both medications are metabolized by the liver [10].
TMP-SMX is available via oral and intravenous (IV) forms. Adult TMP-SMX oral dosages are typically 160mg/800mg for the treatment of UTI, respectively, and dosages for children under 40 kilograms are weight-based. This medicaiton is best absorbed orally when taken with at least eight ounces of water. Intravenous TMP-SMX is given to hospitalized patients and dosages will vary. Some common side effects of trimethoprim-sulfamethoxazole include:
- Nausea and/or vomiting
- Rash and photosensitivity
- Dizziness
- Fatigue
- Loss of appetite and anorexia [10]
As this medication’s mechanism of action interferes with folate production, folate deficiency is also common. More severe side effects may include Stevens-Johnson syndrome, anemia, and Clostridioides difficile (C. diff) diarrhea. This medication should not be prescribed to patients with a sulfa allergy since it can cause anaphylaxis [10].
Before prescribing this medication, healthcare providers should also be aware of the precautions and contraindications. Healthcare providers should be cautious when prescribing this medication to patients with decreased kidney function, as it can lead to toxicity and high potassium levels. Therefore, baseline and frequent monitoring of blood urea nitrogen (BUN), creatinine, and potassium levels are helpful.
Other contraindications include patients with liver failure, hematological disorders, or who are pregnant. TMP-SMX interferes with several medications, including phenytoin, digoxin, diuretics, and rifampin. Many of these medication interactions increase the risk for potential hyperkalemia, medication toxicity, and QT prolongation [10].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of trimethoprim-sulfamethoxazole?
- What are the common side effects of trimethoprim-sulfamethoxazole?
- What are some contraindications of trimethoprim-sulfamethoxazole?
Nitrofurantoin
Nitrofurantoin is another antibiotic commonly prescribed to treat urinary tract infections. This medication has been FDA-approved since 1953 to treat and prevent lower UTIs and is commonly considered a first-line treatment. Currently, nitrofurantoin has no other approved or off-label uses. It comes in two different forms, which are monohydrate and macrocrystalline [16].
The mechanism of action for nitrofurantoin is not completely understood. However, it is thought to be absorbed by bacterial flavoproteins in the gastrointestinal tract and then further prevents bacterial enzymes from synthesizing DNA, RNA, and cell wall proteins [16].
Nitrofurantoin is only available via the oral route. The dosage is usually 100 mg twice daily for UTI treatment and for UTI prophylaxis is 50mg to 100mg once daily. Common medication side effects include:
- Nausea and/or vomiting
- Diarrhea
- Loss of appetite [16]
Severe reactions, although rare, are pulmonary toxicity where patients may present with fever, chills, cough, and dyspnea. It may also cause liver toxicity, liver failure, and peripheral neuropathy. This medication is contraindicated in patients with a creatinine clearance of less than 60 mL/minute, hemolysis, or who have glucose-6-phosphate dehydrogenase (G6PD) deficiency [16].
Healthcare providers should also be aware of considerations when prescribing nitrofurantoin. They must understand that nitrofurantoin should not be prescribed to patients with suspected or confirmed pyelonephritis, since it is only used to treat lower UTIs.
Nitrofurantoin should not be prescribed to people who are pregnant, especially between 38 to 42 weeks gestation, and neonates. It is also not recommended to give to patients who are 65 years or older due to increased potential adverse effects. For patients who take nitrofurantoin long-term for prophylactic use, liver function tests should be routinely completed and monitoring of pulmonary function [16].


Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of nitrofurantoin?
- What are the common side effects of nitrofurantoin?
- What are some contraindications of nitrofurantoin?
Fluoroquinolones
Fluoroquinolones are a class of antibiotics used to treat UTIs and other bacterial conditions. Examples of common fluoroquinolones include ciprofloxacin, moxifloxacin, and levofloxacin. However, ciprofloxacin is more commonly used to treat UTIs than the others and therefore, will be the medication reviewed in this section [19].
In addition to urinary tract infections, ciprofloxacin is FDA-approved to treat various health conditions. Some common health conditions treated are gonorrhea, chancroids, joint infections, prostatitis, and some gastrointestinal infections. Ophthalmic forms are used to treat corneal ulcers and conjunctivitis, while otic forms may be used in otitis externa [17].
Ciprofloxacin’s mechanism of action is considered bactericidal since it works by inhibiting bacterial DNA replication. It acts against DNA topoisomerase and DNA gyrase to hinder DNA replication. Ciprofloxacin is most effective against gram-negative bacteria, but also some gram-positive bacteria. Due to mutations in the DNA gyrase, ciprofloxacin and other fluoroquinolones have begun to show bacterial resistance over the past several years [17].
Ciprofloxacin comes in many forms, including oral, IV, ophthalmic, and otic. For the treatment of UTI, this medication is available via oral and IV forms. Recommended dosages are dependent on the severity of UTI and route. Oral dosages for UTI treatment range from 250mg to 500mg twice daily, while IV dosages can range from 200mg to 400mg twice daily to upwards of 400mg every eight hours. Regardless of the administration route, common side effects are nausea and diarrhea. Some serious adverse effects include:
- QT prolongation
- Hypoglycemia
- Hyperglycemia
- Photosensitivity [17]
Ciprofloxacin has an FDA black box warning of tendinitis and tendon rupture, peripheral neuropathy, and myasthenia gravis exacerbation. Due to the effects this medication has on tendons, Achilles tendon rupture, aortic aneurysm, and aortic dissection are also serious adverse effects. If the healthcare provider suspects any adverse effects, including mild tendonitis, the medication should be discontinued immediately.
Furthermore, when prescribing ciprofloxacin, there are additional considerations and contraindications. As with all medications, ciprofloxacin should not be prescribed to patients with a known allergy to this medication.
Ciprofloxacin should not be prescribed along with tizanidine, theophylline, or cyclosporine due to interactions. Antacids can also interfere with the absorption of ciprofloxacin and ciprofloxacin toxicity is more likely in older adults. Healthcare providers should encourage patients with diabetes to closely monitor their blood glucose levels at home since this medication can cause hypo- or hyperglycemia [17].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of ciprofloxacin?
- What are the common side effects of ciprofloxacin?
- What are some contraindications of ciprofloxacin?
- What is the black box warning of ciprofloxacin?
Beta-lactams
Beta-lactams are a class of antibiotics used to treat various bacterial conditions, including UTIs. The three main beta-lactams covered below are those commonly used to treat UTI and include cephalexin, amoxicillin-clavulanate, and ceftriaxone. Other beta-lactams that are approved for UTI treatment are cefpodoxime, cefdinir, and cefadroxil, and work similarly to others in this medication family.
Cephalexin
Cephalexin is a beta-lactam antibiotic that is classified as a first-generation cephalosporin. It was initially approved by the FDA in 1970 and is widely used throughout healthcare settings. In addition to acute and chronic UTIs, cephalexin is approved to treat upper and lower respiratory infections, bone infections, and otitis media. It is also used to treat surgical site, skin, and soft tissue infections [8].
Cephalexin falls under the beta-lactam class since its structure has a beta-lactam ring. This ring inhibits the synthesis of peptidoglycan which further disrupts the bacterial cell wall. More specifically, the beta-lactam ring binds to the penicillin-binding proteins during peptidoglycan synthesis, causing the disruption of the bacterial cell wall and viability [8].
Cephalexin is only available via oral route and can be prescribed in tablet, capsule, and suspension forms. Daily dosages from 1000mg to 4000mg for adults and for children, are weight-based and range from 25mg to 100mg per kilogram per day. Some side effects of cephalexin include:
- Abdominal pain
- Diarrhea
- Nausea and/or vomiting
- Rash
- Candidiasis [8]
Other reactions may include increased liver enzymes, C. diff colitis, and hemolytic anemia. Although cross-reactivity with penicillin is somewhat uncommon, healthcare providers should use caution when prescribing this medication to patients who are allergic to penicillin. Furthermore, it should not be prescribed to patients with a cephalosporin allergy. Cephalexin also interacts with metformin, causing decreased clearance of metformin from the body.
If a patient is taking metformin, they should be advised to closely monitor their blood glucose levels since the risk for hypoglycemia is increased. Healthcare providers should also be cautious when prescribing this medication to patients who are taking probenecid. Cephalexin can also increase prothrombin time, which typically requires monitoring, especially for those undergoing anticoagulant treatment [8].


Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of cephalexin?
- What are the common side effects of cephalexin?
- What are some contraindications of cephalexin?
Amoxicillin-clavulanate
As its name implies, amoxicillin-clavulanate is a combination medication of amoxicillin and clavulanic acid. In addition to treating UTIs, this medication is FDA-approved to treat rhinosinusitis, acute otitis media, skin infections, and aspiration and community-acquired pneumonia. Other non FDA-approved uses are impetigo, chronic obstructive pulmonary disease exacerbations, diabetic foot infections, and human and animal bites [4].
Amoxicillin-clavulanate works via two different mechanisms of action since it is a combination medication. The amoxicillin component is a beta-lactam antibiotic and works via the same mechanism as cephalexin described above. Clavulanic acid is a beta-lactamase inhibitor, which prevents bacteria from destroying beta-lactam antibiotics. Thus, the reason why clavulanic acid is often combined with amoxicillin [4].
This medication is only available via oral forms, such as suspensions, chewable, immediate-release, or extended-release tablets. Dosages are dependent on the underlying condition being treated, medication form (i.e. immediate- versus extended-release), and the patient’s age. Regardless of dosage, amoxicillin-clavulanate can lead to common gastrointestinal side effects, such as:
- Diarrhea
- Nausea
- Vomiting
- Loose stools [4]
Vaginal candidiasis is another common side effect of amoxicillin-clavulanate. For patients who are breastfeeding, this medication may cause hypersensitivity reactions in infants since it is excreted in breast milk. Additionally, amoxicillin-clavulanate has several drug interactions with medications, including probenecid, oral anticoagulants, allopurinol, and oral contraceptives. For patients on hemodialysis or with severe renal impairment, usually where their creatinine clearance is less than 30 mL/min, dose adjustments are recommended.
Healthcare providers should monitor patients’ liver enzymes for possible hepatic impairment, and if hepatic injury occurs, stop the medication immediately and follow treatment recommendations accordingly. Since amoxicillin is a penicillin derivative, it should not be prescribed to individuals with a penicillin allergy [4].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of amoxicillin-clavulanate?
- What are the common side effects of amoxicillin-clavulanate?
- What are some contraindications of amoxicillin-clavulanate?
Ceftriaxone
Ceftriaxone is another beta-lactam antibiotic used to treat UTIs and is usually an adjunct medication. It is a third-generation cephalosporin that is also used to treat gonorrhea, pelvic inflammatory disease, meningitis, and certain abdominal, respiratory, and joint infections. Additionally, ceftriaxone treats bacteremia, sepsis, and infective endocarditis. Since ceftriaxone belongs to the beta-lactam class, its mechanism of action is the same as previously described cephalexin [18].
Ceftriaxone comes in both intravenous and intramuscular (IM) forms since it is not absorbed through the gastrointestinal tract. For UTI treatment, the dosage for adults is 1 to 2 grams IV or IM every 24 hours. In an outpatient setting, ceftriaxone is often given as a single IM dose to patients with pyelonephritis who are not hospitalized. Again, this medication is used as an adjunct medication, so it is given as a single IM dose, followed by another oral antibiotic for UTI treatment. Dosages for children range from 50mg to 75mg per kilogram per day for both IM and IV forms [18]. Some common side effects of ceftriaxone are:
- Diarrhea
- Nausea
- Vomiting
- Dysgeusia (metallic or foul taste in the mouth)
- Injection site reaction, especially for IM [18]
Other adverse effects associated with ceftriaxone are hemolytic anemias, neutropenia, and thrombocytosis. It should also be noted that this medication can cause neurological symptoms, cholelithiasis, jaundice, elevated liver enzymes, and pancreatitis [18].
Healthcare providers should also review ceftriaxone’s precautions and contraindications. This medication is cross-reactive with penicillin and can cause a hypersensitivity reaction. Furthermore, it should not be prescribed to patients with a cephalosporin allergy. If ceftriaxone is administered through an IV, it must not be mixed with calcium-containing IV solutions or products. Other possible medication interactions are estradiol, cyclosporine, and bumetanide. For patients with liver or kidney impairment, dosages must be adjusted and should not exceed 2 grams per day [18].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of ceftriaxone?
- What are the common side effects of ceftriaxone?
- What are some contraindications of ceftriaxone?
Cefdinir
Cefdinir is another beta-lactam antibiotic used to treat UTIs and is also a third-generation cephalosporin. In addition to UTI treatment, cefdinir is approved for the treatment of pneumonia, bacterial infections involving the skin, and respiratory infections of the ears, throat, and sinuses. As cefdinir is a third-generation cephalosporin, its mechanism of action is the same as previously described ceftriaxone. Thus, it interferes with bacterial cell wall synthesis [13].
Cefdinir is only available via oral route by either capsule or liquid suspension. Treatment dosages and duration are dependent on the underlying condition it is being used to treat [13]. For UTI, this medication is usually prescribed at 300mg twice daily for 5 to 7 days. However, this course may be extended for patients with pyelonephritis or complicated UTIs. Some common side effects of this medication include:
- Nausea and vomiting
- Diarrhea
- Vaginal itching
- Red-tinged stools [13]
Other more serious side effects may include rash, hives, facial swelling, and difficulty breathing or swallowing. As with all medications, healthcare providers should be aware of this medication’s precautions and contraindications. Cefdinir should not be prescribed to patients with a cephalosporin allergy or who are taking probenecid. It should also be avoided in patients with gastrointestinal diseases, like colitis, and kidney disease. This medication should be taken at least two hours apart from any aluminum, magnesium, or iron supplement. Additionally, healthcare providers should avoid prescribing the oral suspension form to patients with diabetes, since it contains high amounts of sucrose and can potentially raise blood sugar levels [13].


Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of cefdinir?
- What are the common side effects of cefdinir?
- What are some contraindications of cefdinir?
Other Antibiotics Used to Treat UTI
This section reviews other antibiotics used to treat urinary tract infections. Two common additional antibiotics administered in an inpatient setting include piperacillin-tazobactam and antipseudomonal carbapenems, such as imipenem or meropenem. These are usually reserved for patients with at least one risk factor for multidrug-resistant gram-negative organisms [7]. Drug information about meropenem will be discussed in greater detail below. Other less common antibiotics available in the outpatient are fosfomycin and pivmecillinam. Although these medicatios are used less commonly, it is still important to understand their pharmacokinetics.
Piperacillin-tazobactam
As mentioned, piperacillin-tazobactam is used to treat multidrug-resistant gram-negative UTIs in an inpatient setting. In addition to treating UTIs, it is approved for the treatment of skin, gynecological, and certain abdominal infections. This medication is a combination of piperacillin (a penicillin antibiotic) and tazobactam (a beta-lactamase inhibitor). Therefore, its mechanism of action is that of both the penicillin and beta-lactam classes as previously described [15].
Piperacillin-tazobactam is available in IV form and the dosage is usually 3.375 grams every six hours [7]. Like many antibiotics, some common side effects include:
- Diarrhea
- Nausea and/or vomiting
- Stomach pain [15]
This medication can also cause mouth sores, sleeping difficulties, and in more severe cases, itching, difficulty swallowing, and wheezing. Piperacillin-tazobactam should not be prescribed to patients who are taking other penicillin or beta-lactam antibiotics or who have an allergy. It interferes with certain medications including, aminoglycosides, anticoagulants, methotrexate, and vancomycin. Additionally, for patients with diabetes, this medication can cause false results with certain glucose tests [15].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of piperacillin-tazobactam?
- What are common side effects of piperacillin-tazobactam?
- What are some contraindications of piperacillin-tazobactam?
Meropenem
An antipseudomonal carbapenem, meropenem, is used to treat inpatient multidrug-resistant gram-negative UTIs. Meropenem is also approved for the treatment of pneumonia, intra-abdominal infections, peritonitis, and meningitis [21].
This medication’s mechanism of action is similar to beta-lactams, as it falls under the same family of antibiotics. It binds to penicillin-binding proteins and inhibits bacterial cell wall synthesis by inhibiting peptidoglycan [21].
Meropenem is only available in IV form and dosages are dependent on the condition being treated. For UTIs, 1 gram is administered every 8 hours. Gastrointestinal side effects are common for this medication and include symptoms like diarrhea, nausea, vomiting, and constipation. Additional adverse effects may include:
- Drowsiness
- Headache
- Insomnia
- Depression [21]
Seizures are also a potential adverse effect, and therefore, healthcare providers must monitor patients for neurological symptoms. Agranulocytosis, thrombocytopenia, gastrointestinal bleeding, and hemolytic anemia are other conditions which have been reported when taking this medication. For patients with renal impairment, the dosage will need to be adjusted. Meropenem also has many medication interactions, with some major ones including afatinib, atogepant, cariprazine, and colchicine [21].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of meropenem?
- What are the common side effects of meropenem?
- What are some contraindications of meropenem?
Fosfomycin
Fosfomycin is an antibiotic that is FDA-approved to treat uncomplicated urinary tract infections and is considered a first-line treatment option. In the United States, fosfomycin is only available in oral, powder which is mixed and dissolved in liquid. Furthermore, although this medication is a first-line UTI treatment option, it is not widely available in the United States [20].
This medication’s mechanism of action works by interfering with the formation of peptidoglycan precursor UDP N-acetylmuramic acid, also known as UDP-MurNAc. As it acts one step prior to the beta-lactam antibiotic family, Fosfomycin enters the bacteria through the transporter systems L-alpha-glycerophosphate and hexose-6-phosphate. This medication also reduces the ability of bacteria to adhere to the epithelial cells of the urinary tract [9].
To treat UTI, a single dose of 3 grams of fosfomycin is given, which is added to about 3 to 4 ounces of cold water to dissolve the medication. Common side effects may include:
- Nausea
- Diarrhea
- Headache
- Back pain [14]
Other serious side effects are joint pain, rash, facial or oral swelling, and jaundice. Healthcare providers should review this medication’s interactions and contraindications. Fosfomycin interacts with medications like cisapride, metoclopramide, and certain vitamins. Healthcare providers should use caution when prescribing to patients with a history of asthma, liver disease, or who are pregnant or breastfeeding [14].

Self-Quiz
Ask Yourself...
- What is the mechanism of action for fosfomycin?
- What are some common side effects of fosfomycin?
- What are some contraindications of fosfomycin?
Pivmecillinam
Pivmecillinam is another antibiotic used to treat lower urinary tract infections and is part of the UTI treatment algorithm. However, the FDA has not approved this medication for use in the United States [11]. Therefore, most of the specific drug information is not available.

Considerations for Prescribers
This section reviews potential considerations when prescribing antibiotics for UTIs.
Healthcare providers must consider and review several factors when prescribing antibiotics for UTI treatment. First, the medication’s route, dosage, and treatment duration are usually determined by the setting (inpatient versus outpatient), the type of UTI (e.g. empirical, asymptomatic bacteremia, uncomplicated, complicated, or prophylaxis), and the patient’s underlying medical conditions and risk factors. Furthermore, healthcare providers should strive to follow current treatment guidelines, approved uses, and their organization’s protocols when initiating or adjusting these medications. Healthcare providers must review the patient’s medical history, recent lab values, contraindications, and potential side effects.
Patient Population
Certain classes of antibiotics should be avoided in specific individuals or patient populations, and thus, healthcare providers must be aware of these precautions, contraindications, and black box warnings. Ciprofloxacin can lead to medication toxicity and hypoglycemia in older adults and must be avoided in this patient population when able [17]. Additionally, prescribing medications, such as TMP-SMZ and cephalexin, should be cautioned in patients with renal impairment [8, 10]. Prescribing nitrofurantoin, TMP-SMZ, cephalexin, and ceftriaxone should be cautioned in patients with liver failure or elevated liver enzymes. Healthcare providers should routinely monitor the patient’s liver enzymes and function tests [8, 10, 16, 18].
The patient’s gender at birth plays another large factor in antibiotic selection since treatment for males is considered a complicated UTI and antibiotic duration is extended. Furthermore, in patients who are pregnant or breastfeeding, certain antibiotics should not be prescribed, with some including TMP-SMZ and fluoroquinolones. Alternative treatments for patients who are pregnant are amoxicillin-clavulanate or [6]. For patients with chronic UTIs, initial prophylactic treatment should be started for 3 months and then reevaluated thereafter for prevention. Typical low-dose prophylactic antibiotics are TMP-SMX and nitrofurantoin. However, the healthcare provider should strongly consider medication compliance and potential antibiotic resistance [1].
Allergies
Healthcare providers should also review the patient’s allergies and cross-reactivity of certain antibiotics. Trimethoprim-sulfamethoxazole should not be prescribed to individuals with a sulfa allergy. Furthermore, healthcare providers should not prescribe patients with a penicillin allergy amoxicillin-clavulanate and should use caution when prescribing these individuals beta-lactams or cephalosporins due to their potential cross-reactivity, although the percentage is low [8, 10].
Medication History
As discussed, certain antibiotics interact with specific medications. Healthcare providers must review the patient’s medication list prior to prescribing antibiotics. For instance, amoxicillin-clavulanate interacts with allopurinol and lessens the effectiveness of oral contraceptives. Patients on oral contraceptives should be instructed to use backup birth control methods while on the antibiotic [4]. Additionally, while interactions may exist medication timing plays an important role. For example, medications such as ciprofloxacin and TMP-SMZ interact with antacids. However, if the antibiotic is taken two hours before or six hours after the antacid, a potential medication interaction is less likely [17]. Cephalexin is better absorbed on an empty stomach while other antibiotics are recommended to be taken with food [8].
Bacterial Sensitivity
Some antibiotics do not treat certain strains of bacteria and thus, healthcare providers must be judicious about initial antibiotic selection and following up with the patient about their urine culture results. For example, bacterial growth on the urine culture might not be sensitive to the initial antibiotic prescribed and may be resistant. Therefore, the antibiotic may need to be changed or dual therapy may be needed.
Also, patients with recurrent UTIs sometimes develop antibiotic resistance to first-line medications for the treatment of UTI, so an alternative medication should be initially prescribed, and a urine culture sent. If the patient is treated frequently for UTIs, then a referral to urology is warranted for further evaluation [6]. In some patients, asymptomatic bacteremia is found on a routine urinalysis completed during an annual comprehensive exam. Healthcare providers should review the current screening and treatment guidelines on asymptomatic bacteria in adults. For most patients, a urine culture should be sent for further evaluation, and antibiotic administration delayed until the culture has resulted [5].
Patient Education
Patients should be instructed on potential medication side effects and signs of adverse reactions. In an outpatient setting, healthcare providers must instruct patients on worsening symptoms and when to seek immediate or emergent treatment. Oftentimes, urinary tract infections move upstream into the kidneys and cause pyelonephritis or urosepsis [6].

Self-Quiz
Ask Yourself...
- What factors should healthcare providers consider when prescribing antibiotics?
- Which antibiotic can be prescribed during pregnancy?
- Which steps should be taken for patients with recurrent UTIs?
- What health conditions and lab values are important when selecting UTI antibiotics?
Upcoming Research
This section reviews upcoming research and medications for UTI treatment.
The bacteria strain, E. coli, is typically responsible for urinary tract infections. However, this is not the case for all UTIs, and some patients have developed multiple drug-resistant organisms due to recurrent infections. Therefore, there is much research needed on UTI antibiotic treatment to eradicate these organisms. Recent development of immunomodulatory therapy has been considered as well as medications that inhibit bacterial adhesions to the epithelial cells of the urinary tract. Vaccinations against UTI have also shown recent promise, but further research is still needed [3]. Other non-antibiotic therapies are also being researched, like Lactobacillus-containing products (i.e. probiotics) and cranberry supplements [12].


Self-Quiz
Ask Yourself...
- Which bacteria commonly causes urinary tract infections?
- What new research is there about antibiotics for UTI treatment?
- Which types of new products are being researched about UTI treatment?
Conclusion
As discussed, antibiotic selection for the treatment of urinary tract infections depends on a variety of factors. Healthcare providers should understand the pharmacokinetics, potential side effects, interactions, and contraindications when selecting an antibiotic. They should also follow current clinical guidelines and their facility’s protocols for a more evidence-based approach. Furthermore, ordering a urine culture or referring a patient to a urologist is warranted for patients with recurrent urinary tract infections.

Self-Quiz
Ask Yourself...
Final Reflection Questions
- What differentiates a lower versus upper UTI?
- What are the different names of beta-lactam antibiotics used to treat UTIs?
- Which antibiotics are commonly prescribed for UTI prophylaxis?
- Which antibiotics are not commonly prescribed or available in the United States?
- Which antibiotics are commonly used to treat multi-drug resistant organisms?
- Which antibiotics can be used in outpatient versus inpatient settings?
- What are the two types of fluoroquinolones used to treat UTIs?
- What are some other antibiotics used to treat UTIs?
References + Disclaimer
- Waisel DB. Vulnerable populations in healthcare. Curr Opin Anesthesiol. 2013;26(2):186–92.
- Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: Trends over the past 10 years. NCHS Data Brief. 2012;2012(100):1–8.
- Institute of Medicine. Collecting sexual orientation and gender identity data in electronic health records: workshop summary. Washington DC: National Academy of Sciences; 2013.
- Quinn GP, Sanchez JA, Sutton SK, Vadaparampil ST, Nguyen GT, Green BL, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA-Cancer J Clin. 2015;65(5):384–400
- Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–60.
- Dilley JA, Simmons KW, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific northwest. Am J Public Health. 2010;100(3):460–7.
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health. 2013;103(10):1802–9.
- Bauermeister J, Eaton L, Stephenson R. A multilevel analysis of neighborhood socioeconomic disadvantage and transactional sex with casual partners among Young men who have sex with men living in metro Detroit. Behav Med. 2016;42(3):197–204.
- Smalley KB, Warren JC, Barefoot KN. Differences in health risk behaviors across understudied LGBT subgroups. Health Psychol. 2016;35(2):103–14.
- Staats C, Capatosto K, Wright RA, Jackson VW. State of the science: Implicit bias review 2016. Columbus: Kirwan Institute.
- Cochran SD, Bandiera FC, Mays VM. Sexual orientation-related differences in tobacco use and secondhand smoke exposure among US adults aged 20 to 59 years: 2003-2010 National Health and nutrition examination surveys. Am J Public Health. 2013;103(10):1837–44.
- Remafedi G, French S, Story M, Resnick MD, Blum R. The relationship between suicide risk and sexual orientation: results of a population-based study. Am J Public Health. 1998;88(1):57–60.
- Charlton BM, Corliss HL, Missmer SA, Frazier AL, Rosario M, Kahn JA, et al. Reproductive health screening disparities and sexual orientation in a cohort study of U.S. adolescent and Young adult females. J Adolesc Health. 2011;49(5):505–10.
- Matthews AK, Brandenburg DL, Johnson TP, Hughes TL. Correlates of underutilization of gynecological cancer screening among lesbian and heterosexual women. Prev Med. 2004;38(1):105–13.
- Tracy JK, Lydecker AD, Ireland L. Barriers to cervical Cancer screening among lesbians. J Women’s Health. 2010;19(2):229–37.
- Grossman AH, D’Augelli AR. Transgender youth: invisible and vulnerable. J Homosex. 2006;51(1):111–28.
- Krehely J. How to close the LGBT health disparities gap. Center for American Progress; 2009. p. 1–9.
- Buchmueller T, Carpenter CS. Disparities in health insurance coverage, access, and outcomes for individuals in same-sex versus different-sex relationships, 2000-2007. Am J Public Health. 2010;100(3):489–95.
- Heck JE, Sell RL, Gorin SS. Health care access among individuals involved in same-sex relationships. Am J Public Health. 2006;96(6):1111–8.
- Kamen C, Palesh O, Gerry AA, Andrykowski MA, Heckler C, Mohile S, et al. Disparities in health risk behavior and psychological distress among gay versus heterosexual male Cancer survivors. LGBT Health. 2014;1(2):86–U103.
- Legal L. When health care Isn’t caring: lambda Legal’s survey of discrimination against LGBT people and people with HIV. New York: Lamba Legal; 2010.
- Grant JM, Mottet LA, Tanis J. National Transgender Discrimination Survey Report on health and health care. Washington DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2010.
- Shires DA, Jaffee K. Factors associated with health care discrimination experiences among a National Sample of female-to-male transgender individuals. Health Soc Work. 2015;40(2):134–41.
- Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians’ experiences in the workplace. J Homosex. 2011;58(10):1355–71.
- Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54.
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
- Mereish EH, Bradford JB. Intersecting identities and substance use problems: sexual orientation, gender, race, and lifetime substance use problems. J Stud Alcohol Drugs. 2014;75(1):179–88.
- Torres CG, Renfrew M, Kenst K, Tan-McGrory A, Betancourt JR, Lopez L. Improving transgender health by building safe clinical environments that promote existing resilience: results from a qualitative analysis of providers. BMC Pediatr. 2015;15:187.
- Burke SE, Dovidio JF, Przedworski JM, Hardeman RR, Perry SP, Phelan SM, et al. Do contact and empathy mitigate Bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. 2015;90(5):645–51.
- Sabin JA, Riskind RG, Nosek BA. Health care Providers’ implicit and explicit attitudes toward lesbian women and gay men. Am J Public Health. 2015;105(9):1831–41.
- Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–7.
- Wilson TD, Brekke N. Mental contamination and mental correction: unwanted influences on judgments and evaluation. Psychol Bull. 1994;116(1):117–42.
- Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit Bias in health care: a narrative review. Group Proccess Interg. 2016;19(4):528–42.
- Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102(1):4–27.
- Van Ryn M, Saha S. Exploring unconscious bias in disparities research and medical education. JAMA. 2011;306(9):995–6.
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74(6):1464–80.
- Nosek BA, Riskind RG. Policy implications of implicit social cognition. Soc Issue Policy Rev. 2012;6(1):113–47.
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
- Shavers VL, Fagan P, Jones D, Klein WMP, Boyington J, Moten C, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953–66.
- Chapman EN, Kaatz A, Carnes M. Physicians and implicit Bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–10.
- Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: Confronting racial and ethnic disparities in health care. Brian D. Smedley, Adrienne Y. Stith, and Alan R. Nelson, Editors; Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Board on Health Sciences Policy; Institute of Medicine. Washington, DC; 2003.
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41.
- Greenwald AG, Banaji MR, Nosek BA. Statistically small effects of the implicit association test can have societally large effects. J Pers Soc Psychol. 2015;108(4):553–61.
- Khan A, Plummer D, Hussain R, Minichiello V. Does physician bias affect the quality of care they deliver? Evidence in the care of sexually transmitted infections. Sex Transm Infect. 2008;84(2):150–1.
- Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P. (2019). Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC medical education, 19(1), 325. https://doi.org/10.1186/s12909-019-1727-3
- Human rights campaigns. Glossary of terms. Retrieved from https://www.hrc.org/resources/glossary-of-terms
- Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community, a field guide. Joint Commission. Retrieved from https://www.jointcommission.org/ /media/enterprise/tjc/imported-resource assets/documents/lgbtfieldguide_web_linked_verpdf.pdf?db=web hash=1EC363A65C710BCD1D4E14ED120CB2
- Delivering culturally sensitive care to LGBTQI Patients. The Journal for nurse practitioners. Volume 13, issue 5 p342-347.
- Centers for Disease Control and Prevention (2023). What is health Literacy? Retrieved on September 15, 2023 from https://www.cdc.gov/healthliteracy/learn/index.html
- MedlinePlus [Internet] National Library of Medicine. Choosing effective patient education materials; Reviewed 2021 October 17] Retrieved on September 15, 2023, from https://medlineplus.gov/ency/patientinstructions/000455.htm
- Goodman, C., Lambert., (2022). Scoping review of the preferences of older adults for patient education materials. Patient Education and Counseling, Volume 108, March 2023, 107591. Retrieved on September 15, 2023, from https://doi.org/10.1016/j.pec.2022.107591
- Zajacova, A., & Lawrence, M., (2018). The relationship between education and health: reducing disparities through a contextual approach. Annual Review of Public Health. 2018 April 1; Vol 39: pp 273-289. Retrieved on September 15, 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5880718/
- Betancourt, J., Green, A., & Carrillo, E., (2021). The patient’s culture and effective communication. UpToDate. Retrieved on September 14th, 2023 from https://www.uptodate.com/contents/the-patients-culture-and-effective-communication/print
- Centers for Disease Control and Prevention (2021). Importance of Health Literacy. Retrieved on September 13, 2023 ,from https://www.cdc.gov/healthliteracy/developmaterials/audiences/olderadults/importance.html#:~:text=The%20National%20Assessment%20of%20Adult,interpreting%20numbers%20and%20doing%20calculations
- U.S. Department of Health and Human Services. (2019). Health Literacy Reports and Publications. Retrieved on September 15, 2023 from https://www.hhs.gov/surgeongeneral/reports-and-publications/health-literacy/index.html#:~:text=Health%20literacy%20is%20key%20to,have%20proficient%20health%20literacy%20skills
- Health Care Education Association. (2021). Patient Education Guidelines for Health Care Professionals. Retrieved on September 14, 2023, from https://www.hcea-info.org/assets/hcea%20guidelines%20color%201-25-2021.pdf
- Chick, N (2010). Learning Styles. Vanderbilt University Center for Teaching. Retrieved September 15, 2023, from https://cft.vanderbilt.edu/guides-sub-pages/learning-styles-preferences/
- Merriam-Webster. (n.d). Education. In Merriam-Webster.com dictionary. Retrieved September 15, 2023, from https://www.merriam-webster.com/dictionary/education
- Use the Teach-back Method: Tool #5. Content last reviewed September 2020. Agency for Healthcare Research and Quality, Rockville, MD. Retrieved on September 15, 2023, from https://www.ahrq.gov/health-literacy/improve/precautions/tool5.html
- Medline Plus. [Internet]. National Library of Medicine. (2021). Communicating with patients. Retrieved on September 17, 2023 from https://medlineplus.gov/ency/patientinstructions/000456.htm
- Marcum, J., Ridenour, M., Shaff, G., Hammons, M., & Taylor,M. (2021). A Study of Professional Nurses’ Perceptions of Patient Education. The Journal of Continuing Education in Nursing. 2013;33(3): pp 112-118. Retrieved on September 18, 2023 from https://doi.org/10.3928/0022-0124-20020501-05
- Nurses are Still Stressed, Frustrated, and Overwhelmed Almost 2 Years into COVID-19. (2021, October 26). ANA. https://www.nursingworld.org/news/news-releases/2021/new-survey-data-thousands-of-nurses-are-still-stressed-frustrated-and-overwhelmed-almost-2-years-into-the-pandemic/
- General, O. O. T. S. (2022, May 23). New Surgeon General Advisory sounds alarm on health worker burnout and resignation. HHS.gov. https://www.hhs.gov/about/news/2022/05/23/new-surgeon-general-advisory-sounds-alarm-on-health-worker-burnout-and-resignation.html
- Harvey, B. (2022) 98 Best self-care quotes to remind you what matters. Retrieved from https://www.goodgoodgood.co/articles/self-care-quotes
- Writers, S. (2023, March 23). What is nurse burnout? | nursejournal.org. NurseJournal. https://nursejournal.org/resources/nurse-burnout/
- Wolotira, E. A. (2023). Trauma, compassion fatigue, and burnout in nurses. Nurse Leader, 21(2), 202–206. https://doi.org/10.1016/j.mnl.2022.04.009
- Vaughn, N. (2023). Nursing Compassion Fatigue and Burnout vs. Moral Injury. Nurse.com Blog. https://www.nurse.com/blog/nursing-compassion-fatigue-and-burnout-vs-moral-injury/
- Shah, M., Gandrakota, N., Cimiotti, J. P., Ghose, N., Moore, M., & Ali, M. K. (2021). Prevalence of and factors associated with nurse burnout in the US. JAMA Network Open, 4(2), e2036469. https://doi.org/10.1001/jamanetworkopen.2020.36469
- National Academies Press (US). (2019, October 23). Introduction. Taking Action Against Clinician Burnout – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK552613/#:~:text=Extensive%20research%20has%20found%20that,and%2060%20percent%20for%20medical
- Nurse burnout: What is it & how to prevent it | ANA. (2023, February 17). ANA. https://www.nursingworld.org/practice-policy/work-environment/health-safety/nurse-burnout-and-how-to-prevent-it/
- Burnout. (2022, September 27). PSNet. https://psnet.ahrq.gov/primer/burnout#:~:text=The%20emotional%20exhaustion%20and%20depersonalization,compromises%20the%20quality%20of%20care
- Shift. (2021, June 22). On the Verge of Burnout? Three Proactive Steps You Can Take Today – SHIFT. SHIFT. https://www.shiftnursing.com/articles/on-the-verge-of-burnout-three-proactive-steps-you-can-take-today
- Caring for your mental health. (n.d.). National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/topics/caring-for-your-mental-health
- Tribe-Scott, BSN, RN, RAC-MT, RAC-MTA, QCP, M. (2022). Burnout: How can nurse leadership help? AAPACN. https://www.aapacn.org/blog/burnout-how-can-nurse-leadership-help
- Anusiewicz, C. V., Ivankova, N. V., Swiger, P. A., Gillespie, G. L., Li, P., & Patrician, P. A. (2020). How does workplace bullying influence nurses’ abilities to provide patient care? a nurse perspective. Journal of Clinical Nursing, 29(21-22), 4148–4160. https://doi.org/10.1111/jocn.15443
- Collins, B. (2022). Mobbing and workplace bullying among registered nurses in Mississippi. ABNFF Journal, 1(2), 20–28.
- Edmonson, C., & Zelonka, C. (2019). Our own worst enemies. Nursing Administration Quarterly, 43(3), 274–279. https://doi.org/10.1097/naq.0000000000000353
- Harassment definition & meaning. (n.d.). Dictionary.com. https://www.dictionary.com/browse/harassment
- Meires, J. (2018). Workplace incivility – the essentials: Here’s what you need to know about bullying in nursing. Urologic Nursing, 38(2), 95. https://doi.org/10.7257/1053-816x.2018.38.2.95
- Thompson, R. (Feb 2022). Getting Clear on Bullying Versus Incivility. Florida Nurse, 70(1), 19–19.
- Arnetz, J. E. (2022, April). The Joint Commission’s new and revised Workplace violence prevention standards for hospitals: A major step forward toward improved quality and safety. Joint Commission journal on quality and patient safety. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8816837/
- American Nurses Association. (2019, January). Reporting incidents of Workplace Violence – Ana Enterprise. Reporting Incidents of Workplace Violence. https://www.nursingworld.org/~495349/globalassets/docs/ana/ethics/endabuse-issue-brief-final.pdf
- Occupational Safety and Health Administration. (n.d.). Healthcare – workplace violence. https://www.osha.gov/healthcare/workplace-violence/
- Minnesota Nurses Association. (2022, August 10). Hennepin Healthcare Nurses report rising violence against nurses and patients, cite under-staffing, unresponsive management as barriers in new survey. Minnesota Nurses Association. https://mnnurses.org/hennepin-healthcare-nurses-report-rising-violence-against-nurses-and-patients-cite-under-staffing-unresponsive-management-as-barriers-in-new-survey/
- ANA) Workplace violence. (2017). https://www.nursingworld.org/practice-policy/advocacy/state/workplace-violence2/
- Sahebi, A., Golitaleb, M., Moayedi, S., Torres, M., & Sheikhbardsiri, H. (2022, August 8). Prevalence of workplace violence against health care workers in hospital and pre-hospital settings: An umbrella review of meta-analyses. Frontiers in public health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9393420/#:~:text=The%20overall%20prevalence%20of%20WPV,%2C%20and%2010.5%25%20(95%25
- Song, C., Wang, G., & Wu, H. (2020, December 3). Frequency and barriers of reporting workplace violence in nurses: An online survey in China. International Journal of Nursing Sciences. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7859538/
- Staff, A. (2022, November 4). End Nurse Abuse: 4 Actions You Can Take Today. Aorn.org. https://www.aorn.org/article/2021-12-03-End-Nurse-Abuse
- Fountain, D., Zankowski, D., & Arriola, J. (n.d.). Reporting incidents of Workplace Violence – Ana Enterprise. Reporting incidents of Workplace Violence. https://www.nursingworld.org/~495349/globalassets/docs/ana/ethics/endabuse-issue-brief-final.pdf
- U.S. Bureau of Labor Statistics. (n.d.). Workplace violence in healthcare, 2018. U.S. Bureau of Labor Statistics. https://www.bls.gov/iif/factsheets/workplace-violence-healthcare-2018.htm
- Vincent-Höper, S., Stein, M., Nienhaus, A., & Schablon, A. (2020, May 1). Workplace aggression and burnout in nursing-the moderating role of follow-up counseling. International journal of environmental research and public health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7246829/
- Creating a culture of safety in nursing. ANA. (2023, September 12). https://www.nursingworld.org/resources/individual/nurse-managers/safety-in-nursing/
- AlGhatrif, M., & Lindsay, J. (2012). A brief review: History to understand fundamentals of electrocardiography. Journal of Community Hospital Internal Medicine Perspectives, 2(1), 14383. https://doi.org/10.3402/jchimp.v2i1.14383
- Alila Medical Media. (2017). Cardiac action potential, animation. [YouTube Video]. In YouTube. https://www.youtube.com/watch?v=v7Q9BrNfIpQ
- American Heart Association. (2016). Ventricular fibrillation. Www.heart.org. https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia/ventricular-fibrillation
- Atkielski, A. (2023). PQRST segment. In StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK551635/figure/article-20939.image.f1/?report=objectonly
- Benzoni, T., & Cascella, M. (2021). Procedural sedation. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551685/
- Bern Dibner. (2018). Luigi Galvani | Italian physician and physicist. In Encyclopædia Britannica. https://www.britannica.com/biography/Luigi-Galvani
- Birnbaum, Y., Ye, Y., Smith, S. W., & Jneid, H. (2021). Rapid diagnosis of STEMI equivalent in patients with left bundle‐branch block: Is it feasible? Journal of the American Heart Association, 10(18). https://doi.org/10.1161/jaha.121.023275
- Bracey, A. (2023). Posterior MI. In ncbi.nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK553168/figure/article-698.image.f1/?report=objectonly
- Burns, E., & Buttner, R. (2021). PVCs. In litfl.com. https://litfl.com/premature-ventricular-complex-pvc-ecg-library/
- Burns, E., & Buttner, R. (2023a). Anterior MI. In litfl.com. https://litfl.com/anterior-myocardial-infarction-ecg-library/)
- Burns, E., & Buttner, R. (2023b). Monomorphic vtach. In litfl.com. https://litfl.com/ventricular-tachycardia-monomorphic-ecg-library/
- Burns, E., & Buttner, R. (2023c). Torsades de Pointes. In litfl.com. https://litfl.com/polymorphic-vt-and-torsades-de-pointes-tdp/
- Cadogan, M. (2018, August 1). Delta wave. Life in the Fast Lane. https://litfl.com/delta-wave-ecg-library/
- Cadogan, M. (2022). Lead positioning. In litfl.com. https://litfl.com/ecg-lead-positioning/
- Cardiac Science. (2021). ECG graph paper. In cardiacsciencesmb.ca. https://cardiacsciencesmb.ca/ecg-graph-paper/
- Cardogan, M., & Buttner, R. (2021). Sgarbossa criteria. In litfl.com. https://litfl.com/sgarbossa-criteria-ecg-library
- Cascino, T., & Shea, M. (2022, September). Electrocardiography – cardiovascular disorders. MSD Manual Professional Edition. https://www.msdmanuals.com/professional/cardiovascular-disorders/cardiovascular-tests-and-procedures/electrocardiography
- Center for Advanced Cardiac and Vascular Interventions. (2023). Mobile cardiac telemetry (MCT). Center for Advanced Cardiac and Vascular Interventions. https://cacvi.org/services/diagnostic-procedures/mobile-cardiac-telemetry/
- Center for Drug Evaluation and Research. (2021, January 8). FDA drug safety communication: New information regarding QT prolongation with ondansetron (zofran). FDA. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-new-information-regarding-qt-prolongation-ondansetron-zofran
- Chruścik, A., Kauter, K., Windus, L., & Whiteside, E. (2021). 6.2 cardiac muscle and electrical activity. In usq.pressbooks.pub. University of Southern Queensland. https://usq.pressbooks.pub/anatomy/chapter/6-2-cardiac-muscle-and-electrical-activity/
- Cleveland Clinic. (2022a). Asystole. In my.clevelandclinic.org. https://my.clevelandclinic.org/health/symptoms/22920-asystole
- Cleveland Clinic. (2022b, June 3). Pulseless electrical activity (PEA): Causes and treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/23213-pulseless-electrical-activity
- Cleveland Clinic. (2022c, June 11). Cardiac event monitor: Types and uses. Cleveland Clinic. https://my.clevelandclinic.org/health/diagnostics/23272-cardiac-event-monitor
- Clip Art Library. (2023). EKG machine. In https://clipart-library.com/clipart/2049261.htm.
- Cohagan, B., & Dov Brandis. (2019, February 17). Torsade de Pointes. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459388/
- Costa, C. (2016). Figure 2.1: A) basic cardiac anatomy and blood circulation through the… In ResearchGate. ResearchGate. https://www.researchgate.net/figure/A-Basic-cardiac-anatomy-and-blood-circulation-through-the-hearts-cavities-and-valves_fig20_320411039
- de Jong, J. (2007a). 2nd AV block. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Wenckebach2.png
- de Jong, J. (2007b). A fib. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Afib_ecg.jpg
- de Jong, J. (2007c). Normal sinus rhythm. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Nsr.jpg
- de Jong, J. (2008). SVT. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Avrt_small.svg
- de Jong, J. (2009). A flutter. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:ECG000011.jpg
- de Jong, J. (2010a). 1st AV block. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Rhythm_1stAVblock.png
- de Jong, J. (2010b). 3rd AV block. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Rhythm_3rdAVblock.png
- de Jong, J. (2010c). A fib RVR. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Afib_f_VR_ecg.jpg
- de Jong, J. (2010d). Bigeminy PVC. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Rhythm_bigemini.png
- de Jong, J. (2010e). Idioventricular rhythm. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Rhythm_idioventricular.png
- de Jong, J. (2010f). PAC. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Rhythm_premature.png
- de Jong, J. (2010g). PVCs. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Rhythm_ventricular_premature.png
- de Jong, J. (2010h). Ventricular fibrillation. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Rhythm_ventricular_fibrillation.png
- de Jong, J. (2011a). Mobitz. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Rhythm_Mobitz.png
- de Jong, J. (2011b, December 13). Normal tracing. En.ecgpedia.org. https://en.ecgpedia.org/index.php?title=Normal_Tracing
- de Jong, J. (2011c). Sinus tachycardia. In ecgpedia.org. https://en.ecgpedia.org/index.php?title=File:Rhythm_tachycardia.png
- Dmitriy Scherbak, & Hicks, G. J. (2019, April 7). Left bundle branch block (LBBB). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482167/
- Douedi, S., & Douedi, H. (2020). P wave. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551635/
- Foth, C., Manesh Kumar Gangwani, & Alvey, H. (2020, January 13). Ventricular Tachycardia (VT, V Tach). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532954/
- Foth, C., & Mountfort, S. (2022). Acute myocardial infarction ST elevation (STEMI). National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532281/
- Gangwani, M. K., & Nagalli, S. (2020). Idioventricular rhythm. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK554520/
- GE HealthCare. (2023a). Apexpro ch telemetry system patient monitors. Www.gehealthcare.com. https://www.gehealthcare.com/products/patient-monitoring/patient-monitors/apexpro-ch-telemetry-system
- GE HealthCare. (2023b). Cardiac beside monitor. In gehealthcare.com. https://www.gehealthcare.com/products/patient-monitoring/patient-monitors/carescape-monitor-b650
- Glenlarson . (2023). Inferior MI. In ncbi.nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK470572/figure/article-23500.image.f1/?report=objectonly
- Gray, D. (2016). How to read an electrocardiogram (EKG/ECG) (K. Gaines , Ed.). Nurse.org. https://nurse.org/articles/how-to-read-an-ECG-or-EKG-electrocardiogram/
- Hafeez, Y., & Grossman, S. A. (2020). Junctional rhythm. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507715/
- Harkness, W. T., & Hicks, M. (2019, June 3). Right bundle branch block (RBBB). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507872/
- Heaton, J., & Yandrapalli, S. (2021). Premature atrial contractions. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559204/
- Henning, A., & Krawiec, C. (2022, August 8). Sinus tachycardia. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK553128/
- Ibrahim, H. (2022a, May 19). ECG tip 20. what about “orthodromic” SVT? Www.youtube.com. https://www.youtube.com/watch?v=XcnU7mGKdis
- Ibrahim, H. (2022b, May 24). ECG tip 21. what about “antidromic” SVT? Www.youtube.com. https://www.youtube.com/watch?v=qTaNeoGEKJc
- Johns Hopkins Medicine. (2019). Holter monitor. John Hopkins Medicine. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/holter-monitor
- Jordan, M. R., Lopez, R. A., & Morrisonponce, D. (2020). Asystole. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430866/
- Mangi, M. A., Jones, W. M., & Napier, L. (2019, November 6). Atrioventricular block second-degree. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482359/
- Mayo Clinic. (2017). Implantable cardioverter-defibrillators (ICDs). Mayoclinic.org. https://www.mayoclinic.org/tests-procedures/implantable-cardioverter-defibrillators/about/pac-20384692
- Mayo Clinic. (2019). Acute coronary syndrome – symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/acute-coronary-syndrome/symptoms-causes/syc-20352136
- Mayo Clinic. (2023, July 26). Atrial fibrillation – symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/atrial-fibrillation/symptoms-causes/syc-20350624
- McMurray, P. (2018). PVCs multiform. In bossrn.com. https://bossrn.com/pvc
- Miner, B., Grigg, W. S., & Hart, E. H. (2020a). Wellens syndrome. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482490/
- Mountfort, S. (2023). Lateral MI. In ncbi.nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK537228/figure/article-24110.image.f2/?report=objectonly
- National Heart, Lung, and Blood Institute. (2022). Atherosclerosis . In nhlbi.nih.gov. https://www.nhlbi.nih.gov/health/atherosclerosis
- Oldroyd, S. H., & Makaryus, A. N. (2020). First degree heart block. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448164/
- Osmosis by Elsevier. (2023). Cardiac electrophysiology notes: Diagrams & illustrations. Www.osmosis.org. https://www.osmosis.org/notes/Cardiac_Electrophysiology#page-1
- Oxford Medical Education. (n.d.). ECG (EKG) – bundle branch block. Oxford Medical Education. https://oxfordmedicaleducation.com/ecgs/bundle-branch-block/
- Parker, S. (n.d.). Telemetry – MeSH – NCBI. Www.ncbi.nlm.nih.gov. Retrieved September 8, 2023, from https://www.ncbi.nlm.nih.gov/mesh/?term=telemetry
- Patti, L., & Ashurst, J. V. (2019, June 4). Supraventricular tachycardia (SVT). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441972/
- Rodriguez Ziccardi, M., Goyal, A., & Maani, C. V. (2020). Atrial flutter. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK540985/
- RWJ Barnabas Health. (2023). Telemetry monitor technician. In rwjbh.org. https://www.rwjbh.org/community-medical-center/treatment-care/heart-and-vascular-care/programs-and-specialties/centralized-cardiac-telemetry-monitoring-program/
- Sandau, K. E., Funk, M., Auerbach, A., Barsness, G. W., Blum, K., Cvach, M., Lampert, R., May, J. L., McDaniel, G. M., Perez, M. V., Sendelbach, S., Sommargren, C. E., & Wang, P. J. (2017). Update to practice standards for electrocardiographic monitoring in hospital settings: A scientific statement from the American Heart Association. Circulation, 136(19). https://doi.org/10.1161/cir.0000000000000527
- Sattar, Y. (2023). Lead placement. In StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK549803/figure/article-20969.image.f1/?report=objectonly
- Sklavos, T. (2020, November 3). ECG interpretation: Myocardial ischaemia and infarction. LITFL. https://litfl.com/ecg-interpretation-myocardial-ischaemia-and-infarction/
- Slane, M., Knabben, V., & Chhabra, L. (2019). Third-Degree atrioventricular block. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK545199/
- Smith, S. (2014). Wide complex SVT. In hqmeded-ecg.blogspot.com. https://hqmeded-ecg.blogspot.com/2014/12/wide-complex-tachycardia-lewis-leads-do.html
- St. Vincent’s Hospital. (n.d.). Holter monitor. In svhhearthealth.com.au. https://www.svhhearthealth.com.au/Images/UserUploadedImages/976/10_HolterMonitor.jpg
- Thanassoulis, G., & Aziz, H. (2018). Atherosclerosis. Merck Manuals Professional Edition; Merck Manuals. https://www.merckmanuals.com/professional/cardiovascular-disorders/arteriosclerosis/atherosclerosis
- The Univeristy of Nottingham. (n.d.-a). Bipolar Leads. Www.nottingham.ac.uk. https://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/bipolar_leads.php
- The University of Nottingham. (n.d.-b). Limb leads. Www.nottingham.ac.uk. https://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/limb_leads.php
- University of Utah Health. (n.d.). ECG learning center – an introduction to clinical electrocardiography. Utah.edu. https://ecg.utah.edu/lesson/9
- Wisconsin Technical College System. (2021). 9.3 cardiovascular assessment. Wtcs.pressbooks.pub. https://wtcs.pressbooks.pub/nursingskills/chapter/9-3-cardiovascular-assessment/
- Wong, E. (2013). Action potential of cardiac muscles. In Pathophys.org. http://www.pathophys.org/physiology-of-cardiac-conduction-and-contractility/actionpotential/
- Yamama Hafeez, & Grossman, S. A. (2019, November 18). Sinus bradycardia. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK493201/
- Yasar Sattar, & Hashmi, M. F. (2019, December 3). Ventricular premature complexes. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK547713/
- Zeid Nesheiwat, Amandeep Goyal, & Mandar Jagtap. (2022). Atrial fibrillation . Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK526072/
- Zimmermann, P., & Hammond, B. (2023). Sheehy’s manual of emergency care. (8th ed.). Elsevier Health Sciences.
- ZOLL Medical Corporation. (2023). X series cardiac monitor/defibrillator for EMS – ZOLL medical. Www.zoll.com. https://www.zoll.com/products/defibrillators/x-series-for-ems
- Katie Kerwin McCrimmon, Uch. (2023, May 15). What is Mounjaro? and does it work better for weight loss than Ozempic and Wegovy?. UCHealth Today. https://www.uchealth.org/today/what-is-mounjaro-and-how-does-it-work-for-weight-loss/
- National Institutes of Health. (2023, July 28). DailyMed – mounjaro- tirzepatide injection, solution. U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d2d7da5d-ad07-4228-955f-cf7e355c8cc0
- Type 2 Diabetes Treatment to Lower A1C | Mounjaro® (tirzepatide). (2023). https://www.mounjaro.com/?utm_id=go_cmp-16966473997_adg-133042365262_ad-626584063672_kwd-1651326559888_dev-c_ext-_prd-_mca-_sig-EAIaIQobChMIxcXZqYeHgQMVhDjUAR2Lvw5CEAAYASAAEgIMkfD_BwE&utm_source=google&utm_medium=ppc&campaign=16966473997&adgroup=133042365262&ad=626584063672&utm_keyword=kwd-1651326559888&gclid=EAIaIQobChMIxcXZqYeHgQMVhDjUAR2Lvw5CEAAYASAAEgIMkfD_BwE
- GoodRX – error. (2023, July 14). https://www.goodrx.com/mounjaro/how-make-you-feel
- Chen, S. (2023, July 28). Diabetes drug Mounjaro shown to have extraordinary weight loss for people without diabetes. diaTribe. https://diatribe.org/diabetes-drug-mounjaro-shown-have-extraordinary-weight-loss-people-without-diabetes
- VA Pharmacy Benefits Management Services. (2022, August). Tirzepatide Injection Criteria for Use. https://www.va.gov/formularyadvisor/DOC_PDF/CFU_Tirzepatide_MOUNJARO_Criteria_Aug_2022.pdf.
- Allied PR. (2023 B.C.E., May 6). Mounjaro Weight Loss: Newly Launch Over The Counter Alternative Pills To Tirzepatide & Mounjaro Weight Loss. https://newsdirect.com/news/mounjaro-weight-loss-newly-launch-over-the-counter-alternative-pills-to-tirzepatide-and-mounjaro-weight-loss-300908569. Retrieved August 30, 2023, from https://newsdirect.com/news/mounjaro-weight-loss-newly-launch-over-the-counter-alternative-pills-to-tirzepatide-and-mounjaro-weight-loss-300908569
- Mounjaro (2023). Savings and support for Mounjaro. Retrieved on August 31st 2023 from https://www.mounjaro.com/savings-resources?gclid=Cj0KCQjw9MCnBhCYARIsAB1WQVWAcINPKFwiHl4SbZQiGC8E_o9wHVOkDJDDUuphW3OlsKBagVTF1rQaApLJEALw_wcB
- Global diabetes cases to soar from 529 million to 1.3 billion by 2050. (n.d.). The Institute for Health Metrics and Evaluation. https://www.healthdata.org/news-events/newsroom/news-releases/global-diabetes-cases-soar-529-million-13-billion-2050.
- Diabetes Research Institute Foundation. (2023, March 31). Diabetes Statistics – DRIF. DRIF. https://diabetesresearch.org/diabetes-statistics/#:~:text=37.3%20million%20people%2C%20or%2011.3,yet%20been%20diagnosed%20(2022)
- Manage blood sugar. (2021, April 28). Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/managing/manage-blood-sugar.html
- About the National Diabetes Prevention Program | CDC. (n.d.). https://www.cdc.gov/diabetes/prevention/about.htm#:~:text=The%20National%20Diabetes%20Prevention%20Program%E2%80%94or%20National%20DPP%E2%80%94was%20created,diabetes%20in%20
- Ms, M. G. R. (2023, February 16). All about Ozempic. Healthline. https://www.healthline.com/health/drugs/ozempic#_noHeaderPrefixedContent
- Professional, C. C. M. (n.d.). Ghrelin. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22804-ghrelin#:~:text=Ghrelin%20and%20leptin%20are%20two,brain%20when%20you’re%20hungry
- Prelipcean, M., MD. (2020, June 22). Behind the counter: Glucagon-like peptide-1 receptor agonists for type 2 diabetes. https://www.medicalnewstoday.com/articles/glp-1-receptor-agonists-type-2-diabetes
- Mba, A. B. P. (2023, May 1). Ozempic side effects: What you should know. https://www.medicalnewstoday.com/articles/drugs-ozempic-side-effects
- Delong, C. (2023, February 11). Black box warning. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538521/
- MNT Medical Network. (2023, February 16). Ozempic (semaglutide). https://www.medicalnewstoday.com/articles/326252
- Ozempic® vs. Other Type 2 Diabetes Treatments | Ozempic® (semaglutide) injection 0.5 mg or 1 mg. (n.d.). https://www.ozempic.com/why-ozempic/diabetes-medicines-comparison.html
- Northrop, A. (2023, August 3). Ozempic For Weight Loss: Side Effects, Risks And More. Forbes Health. https://www.forbes.com/health/body/ozempic-for-weight-loss/%20)
- Kerwin McCrimmon, UCHealth, K. (2023, April 5). Wegovy vs. Ozempic: The truth about new ‘weight-loss’ drugs. Uchealth. https://www.uchealth.org/today/wegovy-vs-ozempic-the-truth-about-new-weight-loss-drugs/#:~:text=If%20you%20take%20Wegovy%20or,to%20keep%20benefiting%20from%20them
- Stott, R. (2023, August 4). Lawsuit claims Ozempic, Mounjaro labels ‘downplayed severity’ of gastroparesis. Healio Gastroenterology. Retrieved August 11, 2023, from https://www.healio.com/news/gastroenterology/20230804/lawsuit-claims-ozempic-mounjaro-labels-downplayed-severity-of-gastroparesis#:~:text=While%20the%20drug%20label%20for,not%20recommended%20in%20these%20patients.%E2%80%9D
- How Does Gastroparesis Affect People with Diabetes? (2022, August 30). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/professionals/diabetes-discoveries-practice/how-gastroparesis-affect-people-with-diabetes
- Living Healthy with Diabetes. (2023, March 29). www.heart.org. https://www.heart.org/en/health-topics/diabetes/prevention–treatment-of-diabetes/living-healthy-with-diabetes
- Move more; sit less. (2023, June 22). Centers for Disease Control and Prevention. https://www.cdc.gov/physicalactivity/basics/adults/index.htm#:~:text=Each%20week%20adults%20need%20150,Physical%20Activity%20Guidelines%20for%20Americans.&text=We%20know%20150%20minutes%20of,do%20it%20all%20at%20once
- Good sleep habits. (2022, September 13). Centers for Disease Control and Prevention. https://www.cdc.gov/sleep/about_sleep/sleep_hygiene.html
- Centers for Disease Control and Prevention. (2022, August 1). Food and nutrition insecurity and diabetes. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes-and-food-insecurity.htm
- American Psychiatric Association. (2020, December). What is a substance use disorder? https://www.psychiatry.org/patients-families/addiction-substance-use-disorders/what-is-a-substance-use-disorder
- Durrani M, Bansal K. Methadone. [Updated 2023 Apr 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562216/
- Kumar R, Viswanath O, Saadabadi A. Buprenorphine. [Updated 2023 Apr 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459126/
- National Center for Drug Abuse Statistics. (2023). Drug abuse statistics. https://drugabusestatistics.org/
- National Institute of Health. (2018, June). Understanding drug use and addiction. https://nida.nih.gov/publications/drugfacts/understanding-drug-use-addiction
- Singh D, Saadabadi A. Naltrexone. [Updated 2023 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534811/
- Substance Abuse and Mental Health Services Administration. (2023, August). Methadone take-home flexibilities extension guidance. https://www.samhsa.gov/medications-substance-use-disorders/statutes-regulations-guidelines/methadone-guidance#:~:text=In%20treatment%200%2D14%20days,be%20provided%20to%20the%20patient
- U.S. Food and Drug Administration. (2023, May). Information about medication assisted treatment (MAT). https://www.fda.gov/drugs/information-drug-class/information-about-medication-assisted-treatment-mat
- Akbari, P., Khorasani-Zadeh, A. (Updated 2023, January 23). Thiazide Diuretics. In Stat Pearls. Stat Pearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532918/
- Alley, W.D., & Schick, M.A. (Updated 2023, July 24). Hypertensive Emergency. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470371/
- American Heart Association. (2023 June 7). Types of Blood Pressure Medications. Retrieved from https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications
- Arumugham, V.B., & Shahin, M.H. (Updated 2023, May 29). Therapeutic Uses of Diuretic Agents. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557838/
- Brater, D.C., & Ellison, D.H. (Updated 2022, November 30). Mechanism of action of diuretics. UpToDate. Retrieved from https://www.uptodate.com/contents/mechanism-of-action-of-diuretics#H5
- Centers for Disease Control and Prevention. (2023, July 6). Facts about Hypertension. Retrieved from https://www.cdc.gov/bloodpressure/facts.htm
- Centers for Disease Control and Prevention. (2021, May 18). High Blood Pressure Symptoms and Causes. Retrieved from https://www.cdc.gov/bloodpressure/about.htm
- Farzam, K., & Jan, A. (Updated 2023, August 22). Beta Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532906/
- Goyal, A., Cusick, A.S., & Thielemier, B. (Updated 2023, June 26). ACE Inhibitors. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430896/
- Hariri, L., & Patel, J.B. (Updated 2023, August 14). Vasodilators. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554423
- Hill, R.D., & Vaidya, P. (Updated 2023, March 27). Angiotensin II Receptors Blockers (ARBs). In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK537027/
- Huxel, C., Raja, A., Ollivierre-Lawrence, M.D. (Updated 2023, May 22). Loop Diuretics. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK546656/
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Loop Diuretics. [Updated 2021 Oct 13]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548619/
- Mann, J.F.E, &Flack, J.M. (Updated 2023, June 22). Choice of Drug Therapy in Primary (Essential) Hypertension. UpToDate. Retrieved from https://www.uptodate.com/contents/choice-of-drug-therapy-in-primary-essential-hypertension
- McKeever, R.G., & Hamilton, R.J. (Updated 2022, August 5). Calcium Channel Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482473/
- MedlinePlus. (2023). Hydrochlorothiazide. National Institutes of Health. Retrieved from https://medlineplus.gov/druginfo/meds/a682571.html
- MedlinePlus. (2023). Metoprolol. National Institutes of Health. Retrieved from https://medlineplus.gov/druginfo/meds/a682864.html
- Nachawati D, Patel JB. (Updated 2023, July 3). Alpha-Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK556066/
- Naranjo, M., Chauhan, S., & Paul, M. (Updated 2023, June 19). Malignant Hypertension. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507701
- Taylor, B.N., & Cassagnol, M. (Updated 2023, July 10). Alpha-Adrenergic Receptors. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539830/
- Verdecchia, P., Cavallini, C., & Angeli, F. (2022). Advances in the Treatment Strategies in Hypertension: Present and Future. Journal of cardiovascular development and disease, 9(3), 72. https://doi.org/10.3390/jcdd9030072
- American Academy of Neurology. (2019). AAN Updates Guideline on Valproate for Women with Epilepsy. Neurology Today, 19(5), 46-47.
- American Headache Society. (2020). The American Headache Society position statement on integrating new migraine treatments into clinical practice. Headache: The Journal of Head and Face Pain, 60(3), 415-423.
- American Nurses Association. (2017). Nursing: Scope and standards of practice (3rd ed.). Silver Spring, MD: American Nurses Association.
- Ashina, M., Goadsby, P. J., Reuter, U., Silberstein, S., Dodick, D. W., Xue, F., … & Trugman, J. M. (2020). Long-term efficacy and safety of erenumab in migraine prevention: Results from a 5-year, open-label treatment phase of a randomized clinical trial. European Journal of Neurology, 27(6), 1058-1067.
- Buse, D. C., Silberstein, S. D., Manack, A. N., Papapetropoulos, S., & Lipton, R. B. (2019). Psychiatric comorbidities of episodic and chronic migraine. Journal of Neurology, 266(3), 634-646.
- Davies, N. M., & Anderson, K. E. (2020). Clinical pharmacokinetics of diclofenac: therapeutic implications and applications in pain and inflammatory disorders. Clinical Pharmacokinetics, 59(2), 153-162.
- Dodick, D. W. (2018). A Phase-by-Phase Review of Migraine Biology, Burden, and Pharmacotherapy. Headache: The Journal of Head and Face Pain, 58(S1), 4-16.
- Dodick, D. W., Lipton, R. B., Ailani, J., Lu, K., Finnegan, M., Trugman, J. M., & Szegedi, A. (2019). Ubrogepant for the treatment of migraine. New England Journal of Medicine, 381(23), 2230-2241.
- Dodgson, S. J., Shank, R. P., & Maryanoff, B. E. (2018). Topiramate as an inhibitor of carbonic anhydrase isoenzymes. Epilepsia, 39(12), 16-22.
- D’Souza, P., Himme, A., & Herndon, C. M. (2020). Migraine headache prophylaxis. American Family Physician, 101(5), 297-298.
- Edvinsson, L., & Warfvinge, K. (2019). Recognizing the role of CGRP and CGRP receptors in migraine and its treatment. Cephalalgia, 39(3), 366-373.
- Gomez, M., & Turner, D. (2020). Tailoring Migraine Medications: A Comprehensive Approach. Journal of Neuropharmacology, 15(4), 201-215.
- Gormley, P., Anttila, V., Winsvold, B. S., Palta, P., Esko, T., Pers, T. H., … & Chasman, D. I. (2016). Meta-analysis of 375,000 individuals identifies 38 susceptibility loci for migraine. Nature Genetics, 48(8), 856-866.
- Gupta, R., & Silberstein, S. D. (2020). Migraine and its impact on daily functioning. Headache: The Journal of Head and Face Pain, 60(3), 572-585.
- Headache Classification Committee of the International Headache Society (IHS). (2018). The International Classification of Headache Disorders, 3rd edition. Cephalalgia, 38(1), 1-211.
- Johnson, A., & Davis, R. (2022). Triptans: Mechanisms of Action and Clinical Applications. Headache Medicine Review, 18(2), 87-104.
- Johnson, M., et al. (2022). Unraveling the Neurological Complexity of Migraines: A Comprehensive Review. Neurological Insights, 12(3), 112-129.
- Jones, A. B., & Brown, C. D. (2019). Contemporary pharmacotherapy for migraine prevention in adults: A review of current and emerging treatment options. Drugs, 79(11), 1223-1238.
- Jones, B., & Miller, S. (2022). Tailoring Migraine Medications Based on Attack Characteristics: A Practical Guide. Neurological Insights, 17(3), 211-228.
- Jones, B., et al. (2021). Emerging Trends in Migraine Pharmacotherapy: A Comprehensive Review. Neuropharmacological Insights, 25(3), 312-328.
- Lee, C. R., Bottiglieri, T., Fisher, W. G., La Du, B. N., & Stamer, W. D. (2019). Relative importance of genetic determinants for naproxen and ibuprofen hydroxylation in human liver microsomes. Clinical Pharmacology & Therapeutics, 105(1), 131-140.
- Linde, K., Allais, G., Brinkhaus, B., Manheimer, E., Vickers, A., & White, A. R. (2016). Acupuncture for the prevention of tension‐type headache. Cochrane Database of Systematic Reviews, 2016(4).
- Lipton, R. B., Goadsby, P. J., Smith, J., Schaeffler, B. A., Biondi, D. M., Hirman, J., … & Tepper, S. J. (2019). Efficacy and safety of eptinezumab in patients with chronic migraine: PROMISE-2. Neurology, 92(15), e1705-e1716.
- Lipton, R. B., Hutchinson, S., Ailani, J., Reed, M. L., Fanning, K. M., Manack Adams, A., … & Aurora, S. K. (2017). Discontinuation of acute prescription medication for migraine: Results from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study. Headache: The Journal of Head and Face Pain, 57(10), 1655-1668.
- MaassenVanDenBrink, A., De Vries, T., Danser, A. H., & Headache Expert Panel of the European Academy of Neurology. (2019). Pathophysiology of migraine: a disorder of sensory processing. Physiological Reviews, 99(2), 901-968.
- Miller, S., Johnson, J., & Patel, J. (2021). Ensuring Patient Safety in Migraine Medication Administration: A Comprehensive Guide. Journal of Neurological Nursing, 43(2), 67-78.
- Mims, M. (2021). Mims Medical Microbiology and Immunology. Elsevier Health Sciences.
- Ong, C. K., Seymour, R. A., Lirk, P., Merry, A. F., & Combet, E. (2017). An evidence‐based update on nonsteroidal anti‐inflammatory drugs. Clinical Medicine & Research, 15(2), 73-100.
- Ong, J. J., De Felice, M., & Migraine Pathophysiology, Treatment, and Prevention. (2020). Migraine: Mechanism of action and treatment. The Scientific World Journal, 2020.
- Perucca, P. (2018). Pharmacokinetic variability of new antiepileptic drugs at different ages. Therapeutic Drug Monitoring, 40(6), 723-733.
- Serrano, D., Lipton, R. B., Scher, A. I., Reed, M. L., Stewart, W. F., & Adams, A. M. (2015). Fluctuations in episodic and chronic migraine status over the course of 1 year: Implications for diagnosis, treatment and clinical trial design. Journal of Headache and Pain, 16(1), 1-12.
- Silberstein, S. D., Holland, S., Freitag, F., Dodick, D. W., Argoff, C., Ashman, E., … & Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. (2019). Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults. Neurology, 92(18), 1-12.
- Smith, J., & Patel, S. (2023). Advances in Migraine Pharmacotherapy: Current Landscape and Future Directions. Neurology Today, 19(1), 45-62.
- Smith, R. H., et al. (2020). Neurobiological Insights into Migraine Mechanisms: A Comprehensive Review. Neurology Research International, 2020, 8743521.
- Smith, J., et al. (2021). Cardiovascular Considerations in Migraine Medication Prescribing: A Current Perspective. Current Neurology and Neuroscience Reports, 21(5), 15.
- Smith, S. M., Gums, J. G., & Potti, A. (2021). Cardiovascular safety of Triptans in patients with cardiovascular disease: A review. The American Journal of Medicine, 134(2), 146-154.
- Tepper, S. J., & Ashina, M. (2020). Reuter U. Fremanezumab in the prevention of high-frequency episodic and chronic migraine: Efficacy in the phase 2b study according to patient characteristics. The Journal of Headache and Pain, 21(1), 23.
- Tepper, S. J., & Cady, R. K. (2019). Diagnosis and Management of Acute Migraine. Disease-a-Month, 65(4), 100856.
- Tepper, S. J., & Diener, H. C. (2020). The Place of Triptans in the Management of Migraine in Clinical Practice. Cephalalgia, 40(2), 155-166.
- Tiseo, C., Vacca, G., & Pinzi, C. (2020). Predictors of triptan use in patients with migraine: Results from a cross-sectional study in Italy. PLoS ONE, 15(7), e0235568.
- Siynor, B. and Perez, L. C. (2023). Pathophysiology of Asthma. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK551579/
- Expert Panel Working Group of the National Heart, Lung, and Blood Institute (NHLBI), National Asthma Education and Prevention Program Coordinating Committee (NAEPPCC), et al. (2020). 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J Allergy Clin Immunol. 146(6):1217-1270. Retrieved from https://www.nhlbi.nih.gov/resources/2020-focused-updates-asthma-management-guidelines
- Rohatgi, K. W., Humble, S., McQueen, A., Hunleth, J. M., Chang, S. H., Herrick, C. J., & James, A. S. (2021). Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. Journal of the American Board of Family Medicine: JABFM, 34(3), 561–570. https://doi.org/10.3122/jabfm.2021.03.200361
- Hiday, R., and Abbott, R. D. (2022). Asthma Guideline Updates. In: Irons BK, Meredith AH, eds. Ambulatory Care Self-Assessment Program, 2022 Book 1. Pulmonary Care. Lenexa, KS: American College of Clinical Pharmacy, 2022:7-36. Retrieved from https://www.accp.com/docs/bookstore/acsap/ac2022b1_sample.pdf
- Ocejo, A. and Correa, R. (2022). Methylprednisolone. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK544340/
- Puckett, Y., Gabbar, A., and Bokhari, A. (2023). Prednisone. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK534809
- Hsu, E. and Bajaj, T. (2023). Beta2-Agonists. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK542249/
- Jilani, T. N., Preuss, C. V., and Sharma, S. (2023). Theophylline. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK519024/
- Choi, J. and Azmat, C. E. (2023). Leukotriene Receptor Antagonists. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554445/
- Dhaliwal, A. and Bajaj, T. (2023). Zafirlukast. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557844/
- Bouchette, D. and Preuss, D. (2023). Zileuton. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK448202/
- Minutello, K. and Gupta, V. (2023). Cromolyn Sodium. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557473/
- Kumar, C. and Zito, P. (2023). Omalizumab. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK545183
- Gade, A., Ghani, H., and Rubenstein, R. (2023). Dupilumab. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK585114/
- Lange-Vaidya, N. and Hartert, T. (2023). Initiating Asthma Therapy and Monitoring in Adolescents and Adults. UpToDate. Retrieved 29 Jan 2024 from https://www.uptodate.com/contents/initiating-asthma-therapy-and-monitoring-in-adolescents-and-adults
- Chu A. and Wadhwa R. Selective Serotonin Reuptake Inhibitors. (2023). In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK55440
- Woodall, A. and Walker, L. (2022). A guide to prescribing antidepressants in primary care. Prescriber, 33: 11-18. https://doi.org/10.1002/psb.2006
- Bains N. and Abdijadid S. Major Depressive Disorder. (2023). In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559078/
- Rohatgi, K. W., Humble, S., McQueen, A., Hunleth, J. M., Chang, S. H., Herrick, C. J., & James, A. S. (2021). Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. Journal of the American Board of Family Medicine: JABFM, 34(3), 561–570. https://doi.org/10.3122/jabfm.2021.03.200361
- Lam, M. K., Lam, L. T., Butler-Henderson, K., King, J., Clark, T., Slocombe, P., Dimarco, K., & Cockshaw, W. (2022). Prescribing behavior of antidepressants for depressive disorders: A systematic review. Frontiers in Psychiatry, 13, 918040. https://doi.org/10.3389/fpsyt.2022.918040
- Moncrieff, J., Cooper, R. E., Stockmann, T., Amendola, S., Hengartner, M. P., & Horowitz, M. A. (2023). The serotonin theory of depression: a systemic umbrella review of the evidence. Molecular Psychiatry, 28, 3243-3256. https://doi.org/10.1038/s41380-022-01661-0
- Boschloo, L., Hieronymus, F., Lisinski, A., Cuijpers, P., & Erikkson, E. (2023). The complex clinical response to selective serotonin reuptake inhibitors in depression: a network perspective. Translational Psychiatry, 13, 2-25. https://doi.org/10.1038/s41398-022-02285-2
- Hirsch, M., Birnbaum, R. J. (2023). Selective serotonin reuptake inhibitors: Pharmacology, administration, and side effects. UptoDate. Retrieved 12 Jan 2024 from https://www.uptodate.com/contents/selective-serotonin-reuptake-inhibitors-pharmacology-administration-and-side-effects
- Bains, N. & Abdijadid, S. (2023). Major Depressive Disorder. In: StatPearls: Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559078/
- Aggarwal, N., Leslie, S.W., & Lotfollhzadeh, S. (Updated 2024, January 11). Recurrent Urinary Tract Infections. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557479
- Bono, M.J., Leslie, S.W., & Reygaert, W.C. (Updated 2023, November 13). Uncomplicated Urinary Tract Infections. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470195
- Butler, D., Ambite, I., Wan, M. L. Y., Tran, T. H., Wullt, B., & Svanborg, C. (2022). Immunomodulation therapy offers new molecular strategies to treat UTIs. Nature reviews. Urology, 19(7), 419–437. https://doi.org/10.1038/s41585-022-00602-4
- Evans, J., Hanoodi, M., & Wittler, M. (Updated 2023, August 16). Amoxicillin Clavulanate. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538164/
- Fekete, T. (Last reviewed 2024, January). Asymptomatic bacteriuria in adults. UpToDate. Retrieved from https://www.uptodate.com/contents/asymptomatic-bacteriuria-in-adults
- Gupta, K. (Last reviewed 2024, January). Acute simple cystitis in adult and adolescent females. UpToDate. Retrieved from https://www.uptodate.com/contents/acute-simple-cystitis-in-adult-and-adolescent-females#H207461713
- Gupta, K. (Last reviewed 2024, January). Acute Complicated Urinary Tract Infection (including pyelonephritis) in Adults and Adolescents. UpToDate. Retrieved from https://www.uptodate.com/contents/acute-complicated-urinary-tract-infection-including-pyelonephritis-in-adults-and-adolescents
- Herman, T.F., & Hashmi, M.F. (Updated 2023, August 17). Cephalexin. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK549780
- Kaye, K. S., Rice, L. B., Dane, A. L., Stus, V., Sagan, O., Fedosiuk, E., Das, A. F., Skarinsky, D., Eckburg, P. B., & Ellis-Grosse, E. J. (2019). Fosfomycin for Injection (ZTI-01) Versus Piperacillin-tazobactam for the Treatment of Complicated Urinary Tract Infection Including Acute Pyelonephritis: ZEUS, A Phase 2/3 Randomized Trial. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America, 69(12), 2045–2056. https://doi.org/10.1093/cid/ciz181
- Kemnic, T.R., & Coleman, M. (Updated 2022, November 28). Trimethoprim Sulfamethoxazole. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK513232/
- Lodise, T. P., Henriksen, A. S., Hadley, T., & Patel, N. (2021). US-Focused Conceptual Health Care Decision-Analytic Models Examining the Value of Pivmecillinam Relative to Current Standard-of-Care Agents Among Adult Patients With Uncomplicated Urinary Tract Infections due to Enterobacterales. Open forum infectious diseases, 8(10), ofab380. https://doi.org/10.1093/ofid/ofab380
- Loubet, P., Ranfaing, J., Dinh, A., Dunyach-Remy, C., Bernard, L., Bruyère, F., Lavigne, J. P., & Sotto, A. (2020). Alternative Therapeutic Options to Antibiotics for the Treatment of Urinary Tract Infections. Frontiers in microbiology, 11, 1509. https://doi.org/10.3389/fmicb.2020.01509
- MedlinePlus. (2024). Cefdinir. MedlinePlus. Retrieved from https://medlineplus.gov/druginfo/meds/a698001.html
- MedlinePlus. (2024). Fosfomycin. MedlinePlus. Retrieved from https://medlineplus.gov/druginfo/meds/a697008.html
- MedlinePlus. (2024). Piperacillin and Tazobactam Injection. MedlinePlus. Retrieved from https://medlineplus.gov/druginfo/meds/a694003.html
- Squadrito, F.J., & del Portal, D. (Updated 2023, May 29). Nitrofurantoin. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470526
- Thai, T., Salisbury, B.H., & Zito, P.M. (Updated 2023, August 28). Ciprofloxacin. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK535454/
- Werth, B.J. (Last revised 2022, September). Cephalosporins. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/cephalosporins
- Werth, B.J. (Last revised 2022, September). Fluoroquinolones. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/fluoroquinolones
- Werth, B.J. (Last revised 2022, September). Fosfomycin. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/fosfomycin
- Werth, B.J. (Last revised 2022, September). Meropenem. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/carbapenems
- Werth, B.J. (Last revised 2022, September). Sulfonamides. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/sulfonamides
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
