Course
Washington DC LPN Renewal Bundle
Course Highlights
In this Washington DC LPN Bundle, we will learn about various topics applicable to LPNs in the District of Columbia (Washington DC).
About
Contact Hours Awarded: 18
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
LGBTQ+ Cultural Competence
Introduction
Lesbian, gay, bisexual, transgender, and questioning (LGBTQ+) individuals represent a rapidly growing segment of the U.S. population [1]. This rapid growth brings with it risk for stigmatization [1]. Implicit healthcare provider biases may result in LGBTQ+ patients receiving a lower standard of care or restricted access to services as compared to the general population [2]. Even when institutions and providers make commitments to equitable care explicit and implicit biases operating outside of conscious awareness may undermine that commitment. There is an urgent need to ensure that healthcare providers are prepared to identify and address their own implicit biases to ensure they do not contribute to the health care disparities experienced by LGBTQ+ and other vulnerable populations. Only by addressing their own implicit biases will health care providers be able to provide patient care in accordance with LGBTQ+ cultural competence.
LGBTQ+ individuals face significant disparities in physical and mental health outcomes [3]. Compared to their heterosexual counterparts, LGBTQ+ patients have higher rates of anal cancer [4], asthma, cardiovascular disease [5,7,8], obesity [6], substance abuse [8,9,10], cigarette smoking [11], and suicide [14]. Sexual minority women report fewer lifetime Pap tests [13,15, 16], transgender youth have less access to health care and LGBTQ+ individuals are more likely to delay or avoid necessary medical care [17] compared to heterosexual individuals. These disparities are due, in part, to lower health care utilization by LGBTQ+ individuals [3]. Perceived discrimination from health care providers and denial of health care altogether are common experiences among LGBTQ patients and have been identified as contributing factors to health disparities [19,20,21,22]. Disparities in health care access and outcomes experienced by LGBTQ+ patients are compounded by vulnerabilities linked to racial identity [23,24,25] and geographic location [6].
Biases among health care students and providers toward LGBTQ+ patients are common [27,28] despite commitments to patient care equality. These biases, also known as negative stereotypes, may be either explicit or implicit [29]. These biases contribute to a lack of LGBTQ+ cultural competence in patient care. A large study of heterosexual, first-year medical students demonstrated that about half of students reported having negative attitudes, explicit bias, towards lesbian and gay people and over 80% exhibited increased negative evaluations of lesbian and gay people compared to heterosexual people (implicit bias) [27]. Research in social-cognitive psychology on intergroup processes defines explicit biases as attitudes and beliefs that are consciously-accessible and controlled; these characteristics are typically assessed via self-report measures and are limited by an individual’s awareness of their attitudes, motivation to reveal these attitudes, and ability to accurately report these attitudes [30,31]. In contrast, the term implicit bias refers to attitudes and beliefs that are unconscious (i.e., outside of conscious awareness) and automatic [32,33]. Implicit bias can be assessed with the Implicit Association Test (IAT) [34], which aims to define the relationships between concepts (ex. race, sex, idea), and positive or negative associations and/or stereotypes. Idenitfied biases are then delegated as slight, moderate, or strong [35].
Healthcare provider biases are correlated with poorer access to services, quality of care, and health outcomes [29, 36, 37, 38]. Explicit biases held by health professionals towards racial/ethnic minorities, women, and older adults are known to affect clinical assessments, medical treatment, and quality of care [39]. Importantly, implicit bias measures are more strongly associated with real-world behaviors than explicit bias measures [40] and are linked to intergroup discrimination [43]. Health care provider’s implicit biases towards vulnerable patient groups may persist despite an absence of negative explicit attitudes [36], resulting in preconceived notions about patient adherence, poor doctor-patient communication, and micro-aggressions, all of which can interfere with optimal care. With less time and limited information processing capacity, provider’s decisions are increasingly governed by stereotypes and implicit biases [42]. Medical student and provider biases may contribute to health disparities in vulnerable populations by negatively impacting communication with patients and decisions about patient care [29, 33]. Taken together, these findings suggest that medical students and healthcare providers are likely to underestimate or to be unaware of their implicit biases towards LGBTQ+ patients, particularly when they are rushed or fatigued, which could impact their behavior and judgments in ways that contribute to health disparities experienced by LGBTQ+ populations. By learning about and addressing their implicit biases, health care providers can work towards demonstrating LGBTQ+ cultural competence and providing optimal care(Introduction section courtesy of Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P.- reference 2).

Self Quiz
Ask yourself...
- What are some cultural misconceptions regarding the LGBTQ+ community and providing medical care?
- How can you demonstrate LGBTQ+ cultural competence in everyday practice?
- What health disparities have you seen in your practice?
- What personal biases have you identified within yourself?
- Have you seen an increase or decrease in understanding of LGBTQ+ people in your facility?
- How have you overcome your personal biases to provide culturally competent care?
- What is implicit bias?
- What do you feel is the definition of cultural competence?
- Have you found difficulties in finding appropriate care for patients in the LGBTQ+ community?
- What is the definition of a health disparity?
Terminology
Understanding the standard terminology utilized is pivotal to treating and interacting with LGBTQ+ patients. Below are listed some of the common terms and how they should be referenced.
Ally- A person not identifying as LGBTQ+, but whom promotes equality and support of LGBTQ+ peoples in a variety of ways.
Androgynous– Identifying as neither masculine nor feminine.
Bisexual – A person who is emotionally, romantically, or sexually attracted to more than one sex, gender, or gender identity.
Cisgender – A person whom identifies with their gender which as assigned at birth. For example, a person assigned female gender at birth who identifies as female.
Gay – A person who is emotionally, romantically and/or sexually attracted to those of the same gender.
Gender-fluid – A person who identifies as a fluid or unfixed gender identity.
Lesbian – A woman who is emotionally, sexually, and/or romantically attracted to other women.
LGBTQ+ – Acronym for “lesbian, gay, bisexual, transgender, and queer.”. The plus sign stands for the innumerable other identities.
Non-binary – Adjective describing person(s) who do not identify exclusively as man nor woman.
Pansexual – A person who has the potential for romantic, emotional, and/or sexual attraction to people of any gender.
Queer – Often used interchangeably with “LGBTQ+”, or to express fluid identities or orientations.
Sexual orientation – An inherent or enduring emotional, romantic, or sexual attraction to other people.
Transgender –Umbrella term for people whose gender identity and/or expression is different from cultural expectations based on the sex they were assigned at birth. It does not imply any specific sexual orientation and transgender persons may identify as straight, gay, lesbian, bisexual, etc.
*Definitions largely derived from (44, 45).

Self Quiz
Ask yourself...
- Which of the above definitions have you heard used interchangeably?
- How does understanding these terms and definitions improve your ability to provide culturally competent care?
- How does using appropriate terminology improve patient care?
- Have you ever encountered a situation where you misused terminology? How was that received, and how did you navigate that conversation/
- Have you used these terms in your patient documentation?
Best Practices
Below we will list and discuss the best practices for ensuring a positive, equitable healthcare experience for LGBTQ+ persons, according to the Joint Commission (this is not a comprehensive list, nor inviolable, but rather highlights).
Create a welcoming environment that is inclusive of LGBT patients and demonstrates LGBTQ+ cultural competence.
- Prominently display the hospital nondiscrimination policy and/or patient bill of rights.
- Waiting rooms and common areas should be inclusive of LGBTQ+ patients and families.
- Unisex or single-stall restrooms should be available.
- Ensure that visitation policies are fair and do not discriminate (even inadvertently) against LGBTQ+ patients and families.
- Foster an environment that supports and nurtures all patients and families.
Avoid assumptions about sexual orientation and gender identity.
- Refrain from making assumptions about a person’s sexual orientation and/or gender identity.
- Be cognizant of bias, stereotypes, and other communication barriers.
- Recognize that self-identification and behaviors do not always align.
Facilitate disclosure of sexual orientation and gender identity, but be aware that disclosure is an individual process.
- Honor and respect patient’s decisions to provide or not provide sexual and/or gender information.
- All forms should contain inclusive, gender-neutral language that allows patients to self-identify.
- Use neutral and inclusive language when communicating with patients.
- Listen to and respect patients’ choice of language when they describe their own sexual orientation.
- Conduct confidential patient satisfaction surveys that include questions regarding sexual orientation and gender identity
*Information largely derived from Joint Commission field guide, reference 45.
For more information on best-practices in the workforce, visit the Joint Commission website by clicking here.

Self Quiz
Ask yourself...
- Have you ever misused a pronoun or overheard a co-worker misuse a pronoun in practice? How can you make sure this doesn't happen again?
- Do you find it getting easier or more difficult to navigate pronouns?
- How does creating a welcoming environment improve patient care?
- Why is it important to avoid assumptions about sexual and gender identity when caring for patients?
- In what ways can the nurse support a patient's desire for privacy?
Establishing Relationships with LGBTQ+ Patients
When interacting with patients, one should not assume gender or sexuality. Addressing a patient whom identifies as a female as a male can cause grave harm to the relationship. Instead, nurses should use open-ended questions. For example, rather than saying “Hi sir, what brings you to the hospital,” a nurse might say, “Welcome, what brings you to the hospital today (45)?”
If a nurse uses the incorrect pronoun, the best practice is to apologize and ask the patient what pronoun and name they prefer. For example, a nurse may say, “I apologize for assuming your gender. How would you like to be addressed? (45).
In conversation, the nurse should use the name and/or pronoun the patient prefers without drawing special attention to the subject (45). For example, if a patient prefers to be identified as their partner’s wife, you should follow suit.
The core of relationship-building with LGBTQ+ patients is no different than any other patient, fundamentally. If nurses have a basic understanding of best practices and a healthy dose of respect and compassion for LGBTQ+ patients, a positive relationship is likely to develop.

Self Quiz
Ask yourself...
- Do you have any biases which may affect the care you provide to LGBTQ+ patients?
- Have you worked for someone who did NOT demonstrate LGBTQ+ cultural competence? In what ways could they improve their practice?
- How does establishing a respectful and welcoming relationship with a patient improve patient care?
- Have you seen other healthcare workers engage negatively with LGBTQ+ patients?
- In what ways can assumptions lead to detrimental interactions with patients?
- Have you dealt with patients who made inappropriate assumptions about you and the care they may receive? How did this impact your care?
- What barriers have you found when establishing a relationship with an LGBTQ+ patient?
Health Disparities of LGBTQ+ Patients
LGBTQ+ Americans are at higher risk of substance use, sexually transmitted diseases, cancer, cardiovascular disease, obesity, bullying, isolation, anxiety, depression, and suicide when compared to the general population (49). LGBTQ+ youth are frequently bullied at schools (46). In fact, early victimization and subsequent emotional distress accounted for 50% of the disparities between LGBTQ+ youth (46). In other words, LGBTQ+ Americans are discriminated against and disadvantaged from a very young age.
When home life also reflects a lack of LGBTQ+ cultural competence, more problems arise. A major cause of LGBTQ+ distress is family rejection. Disclosure of gender identity or sexuality can cause very significant interpersonal conflicts among family and friends of LGBTQ+ persons (46). This explains some hesitancy and should help nurses understand the importance of respecting privacy, while giving options to patients about disclosing sexuality and gender.

Self Quiz
Ask yourself...
- Are there any circumstances in which your current hospital's policies could discriminate against LGBTQ+ families?
- If so, how would you begin to work with leadership to change those policies so they reflect LGBTQ+ cultural competence?
Providing an Inclusive and Accepting Care Environment
LGBTQ+ patients often experience difficulty in finding healthcare environments in which they feel accepted and understood (45). Past negative experiences, lack of knowledge among healthcare providers, and limited access to healthcare in general may become major barriers for LGBTQ+ persons when seeking care (45).
The core tenant of providing an inclusive environment is understanding the needs of LGBTQ+ patients, and working diligently to create an environment which does not disadvantage or discourage them from seeking care.
Policies and procedures at institutions should be designed to reflect a non-discriminatory environment. For example, many hospital policies dictate that only legal family spouses or partners can visit in specific circumstances. Policies such as this are inherently discriminatory toward LGBTQ+ patients, as they may not have legal spousal status due to social, legal, or personal reasons.

Self Quiz
Ask yourself...
- Have you ever had an experience where a colleague made a derogatory remark about a patient based on sexual orientation or gender status? If this happened to you, how would you handle that situation differently?
- How would you address a situation where a colleague handled a patient like that?
- What are examples of an inclusive environment?
- Does your facility have legal policies protecting patients and providing culturally competent care?
- What kinds of continuing education or inservices does your facility incorporate to help ensure culturally competent care?
Laws Specific to Washington D.C.
1973: Title 34 is passed, which prohibits discrimination based on sexual orientation.
2006: The D.C. Human Rights Act is updated to ensure residents of the district are protected regarding employment, house, and public accommodations.
2016: The Armstrong Amendment is repealed in D.C., which allows religious schools exemptions from complying with anti-discrimination laws.
2016: LGBTQ Cultural Competency CE Act is passed. This requires that all licensed healthcare providers take a 2-credit hour course to increase competency (such as the one you are currently taking!).

Self Quiz
Ask yourself...
- Think about the structure of your facility. Does it create an environment which minimizes friction and discrimination of LGBTQ+ patients?
- Do you feel there are any biases among healthcare staff?
- If so, how would begin addressing those?
Exercises on LGBTQ+ Cultural Competence
To help solidify your learning, please complete the following exercises at your own pace. The answers/guidance for each are provided below.
Scenario 1
A patient enters your emergency department and you assume the patient identifies as a female. You introduce yourself and say, “Ma’am, how can we help you? What brings you in today?"
The patient appears dismayed but answers the question. The nurse is confused and does not understand why the patient appears distressed. What is the best course of action?
Answer: The nurse should apologize to the patient and ask the patient how they would like to be addressed. Then, the nurse should update the patient’s records to reflect such, to reduce further confusion.
If the nurse does not address the issue, the patient may feel uncomfortable and develop a negative association with healthcare, which can lead to disparities in the future.
Scenario 2
A patient in your ICU has had a deterioration while his husband was in the room. After a family meeting, a member of the healthcare team makes a derogatory remark about the patient’s sexuality. What is the next best action for the nurse?
Answer: Pre-conceived phobias and stigmatizations can cause significant distress to LGBTQ+ patients, even if not stated directly to them. These type of remarks are abusive and should not be tolerated. The nurse should confront the co-worker (if safe) and consider reporting the comments to the Human Resources department.
Scenario 3
A LGBTQ+ patient is being admitted and prefers not to disclose their sexuality. However, the nurse is unable to proceed with the admission process without this information. What could be done to rectify this system-level issue?
Answer: The nurse should work with administration to ensure that all charting and paperwork allows individuals to self-report sexuality and/or gender if they want. However, healthcare systems should not force patients to “come out” unless it is absolutely medically necessary.

Self Quiz
Ask yourself...
- What information from this course can you take to your facility to encourage a positive change in LGBTQ patients and create an environment for LGBTQ+ cultural competence?
- Do you feel that you are more aware of your biases after reviewing the information in this course?
- What resources do you have access to that can further expand your knowledge and understanding of the LGBTQ+ community?
- How will your patient interaction be changed after completing this course?
- Why is ensuring culturally competent care so important in providing ethical care?
Conclusion
LGBTQ+ cultural competence must be ingrained in our healthcare systems in order to foster excellent relationships between members of the LGBTQ+ community and medical staff. Hospitals and healthcare systems have a great deal of work to do in becoming LGBTQ+ friendly. The efforts must continue until LGBTQ+ patients and families do not feel disadvantaged, anxious, or frustrated when interacting with healthcare systems. As the patient’s ultimate advocate, nurses are at the front-line and should advocate for patients both individually and from a policy perspective. Nurses should work with and spearhead efforts to ensure that healthcare policies reflect best-practice and do not discriminate against LGBTQ+ patients in any way.
HIV / AIDS
Introduction and Objectives
An estimated 1.2 million Americans are living with HIV. As many as 1 in 7 of them do not even know they are infected. The others utilize the healthcare system in a variety of ways, from testing and treatment regimens to hospitalizations for symptoms and opportunistic infections. Healthcare professionals in nearly every setting have the potential to encounter patients with HIV as the disease can affect patients of any age or stage of life (4). Proper understanding of HIV is important in order to provide high–quality and holistic care to these patients.
Upon completion of this course, the learner will:
- Have an increased understanding of the history of HIV and how stigma around the disease developed and is being combated today.
- Demonstrate an understanding of how a person is infected with HIV and the various stages of the disease.
- Demonstrate understanding of transmission modalities and appropriate infection control measures.
- Have a basic knowledge of treatment approaches, common side effects, and barriers to proper treatment.
- Understand comorbidities and coinfections common with HIV.
- Understand ethical issues and confidentiality surrounding the care of HIV patients.
Epidemiology
In the early 1980s, a series of unusual and aggressive illnesses began popping up in clusters across the United States, affecting previously healthy men. Illnesses such as pneumocystis pneumonia, Kaposi‘s sarcoma, and severe wasting, all related to unexplained immunodeficiency, were suddenly rapidly increasing in prevalence, and the only common link seemed to be that it was occurring in gay men. By 1982, the term Acquired Immune Deficiency Syndrome (AIDS) was being used to describe a “moderately predictive…defect in cell–mediated immunity,“ but the details of disease trajectory and how men were contracting it were still foggy (2).
Over the next several years, cases continued to rise, and women and children began presenting with the disease, bringing scientists to the realization that it could be contracted through more ways than just homosexual sex. Amid the social panic, the retrovirus responsible was identified and named Human Immunodeficiency Virus, more reliable testing developed, and various other modes of transmission (like needle sharing, contaminated blood products, childbirth, and breastfeeding) were recognized. By 1989, less than a decade after the first cases were garnering attention, 142,000 cases were reported by 145 countries worldwide (2).
Over the next several decades, more and more information was discovered about HIV and AIDS, and scientists and legislators worked hard to understand and reduce transmission, increase quality and duration of life for those already infected, and fight the stigma and discrimination that had developed during the 1980s (2).
Today, approximately 1.2 million people in the United States are living with HIV, though 1 in 7 people don‘t know it. Rates of infection are not equal across demographic groups, and certain factors may increase a person‘s risk (10). Patient information to consider when determining someone‘s risk includes:
- Age: As of 2018, the age group with the highest incidence of new HIV diagnoses is 25-34 years or approximately 36% of new infections. Ages 13-24 are next, though the numbers in this age range are coming down in recent years. From there, the risk seems to decrease as people age, with the 55 years and older group accounting for only around 10% of new diagnoses each year (10).
- Race/Ethnicity: Currently, the highest rate of new infections is in African Americans, at approximately 45%. This is incredibly high when you consider that African Americans only make up 13% of the general population. This is followed by Hispanic/Latinos at 22% of new infections and people of multiple races at 19% (7).
- Gender: Men are disproportionately affected by HIV, accounting for five times the amount of new infections as females each year. This data refers to the sex of someone at birth. When looking at the transgender population, there is a nearly equal rate of new infections among those who have transitioned male-to-female and female-to-male. Together, transgender people account for 2% of new cases in 2018 (7).
- Sexual orientation: Gay and bisexual men remain the population most at risk of HIV, accounting for around 69% of all new infections in 2018 and 86% of all males diagnosed. Similar racial and ethnic disparities affecting all people with HIV still existed among gay and bisexual men (7).
- Location: Different areas of the country are affected at different rates for a variety of factors, including population density, racial distribution, and access to healthcare. The southern states are unmistakably more affected than other regions, with anywhere from 13-45 people per 100,000 having a diagnosis of HIV. California, Nevada, New York, and D.C. all having similar rates of infection as the southern states and are among the highest in the country. The Midwest and Pacific Northwest are next most affected, with 9-13 people per 100,000. The Northeast and Northwest have the lowest rates nationally at just up to 5 people per 100,000 (7).
While the effects of HIV and AIDS have resulted in a staggering 32 million deaths worldwide since the start of the epidemic, global and national numbers indicate that it peaked around 2005. Numbers of infections and deaths have been on a slow decline since then, mostly due to earlier and more accurate diagnosis, increased knowledge of how to prevent transmission, and effective and accessible treatments. An estimated 65% of Americans currently diagnosed with HIV are considered “virally suppressed,“ demonstrating that adherence to treatment guidelines means most infected people have virtually no risk of transmitting the virus to their partners and have a life expectancy nearly the same as non-infected people (6).
HIV/AIDS’s financial impact is also significant, with an estimated $380,000 spent throughout an individual‘s lifetime with the disease. In 2009, it was estimated that $16.6 billion was spent on HIV treatment in the U.S. alone. However, federal prevention programs do more than improve health outcomes and decrease the number of new infections; they also claim financial benefits and saved approximately $129 billion in the last two decades by averting new infections.
The Ryan White Program is notable and has been in place since 1990. It is a significant source of expanded coverage and funding for patients living with HIV who cannot afford health insurance or proper treatment. This safety net program is federally funded and named after a teenager who died from AIDS after receiving an HIV–contaminated blood transfusion. Ryan‘s story was also a turning point in the public perception of the disease, and the program helps fight the stigma surrounding HIV today (5).

Self-Quiz
Ask Yourself...
- Has the info about HIV/AIDs changed since you first learned it?
- Think about nurses who are from a different generation. How does their experience with this disease differ?
- How might your patients’ experiences or views of this illness be different from yours?
- Why is understanding the complicated history of this illness and its social stigma an important part of providing compassionate care?
- Is access to health insurance and quality healthcare more difficult for those with higher risk to obtain?
- What factors might make one area of the country more at risk than another?
Etiology and Pathogenesis
So just what is this virus that can cause so much devastation but took scientists years to understand? HIV is a type of retrovirus known as lentiviruses; these viruses have long incubation periods and lead to chronic and deadly infections in mammals. Studies indicate that the virus may have first infected humans hunting and eating the meat of infected chimpanzees in central Africa as early as the late 1800s. Once the virus jumped to humans, it spread slowly over many decades and across countries before picking up steam and attracting attention in the United States in the 1980s (7).
Once a host has been infected, the virus seeks out, attaches to, and enters CD4-T cells, immune cells largely responsible for attacking and clearing pathogens in the body. Once inside the cell, viral mRNA (or genetic code) directs the cell to become a factory of more HIV virions, which are then released through a process known as budding. Those virions travel through the body, enter other CD4-T cells, and produce more viruses in a slow but deadly cascade. As part of the body‘s defense against such pathogens, CD4-T cells are programmed for apoptosis (cell death) upon being taken over by a host. Others will experience cell death due to close proximity to infected cells. Still, others will be killed by other types of immune cells. While HIV ravages the body and continues to rise in viral load, the number of CD4-T cells will drop lower and lower until, eventually, the body‘s cell-mediated immunity is no longer viable. Without cell-mediated immunity, opportunistic infections and cancers can take over, and the infected person progresses from HIV infection to full–fledged AIDS (12).
Typically, the disease progresses in 3 stages.
- Stage 1 is acute HIV infection. The virus is reproducing rapidly, and affected individuals may experience flu–like symptoms, including fever, chills, headache, and fatigue. Not everyone experiences symptoms during Stage 1, but all are highly contagious during this period.
- Stage 2 is Chronic HIV infection; viral replication slows, and this stage can last for many years. A person in this stage is still contagious, but they may have no symptoms. Proper use of medication treatment may mean an infected person never moves past this stage.
- And finally, if the viral load continues to increase and the CD4-T cell count gets below 200 cells/mm, the illness transitions to Stage 3, AIDS. In this stage, even minor opportunistic pathogens can make a person very ill due to the lack of a properly functioning immune system. Symptoms and infections such as thrush, pneumonia, peripheral neuropathy, and Kaposi sarcoma are common. Stage 3 is very contagious and life expectancy is about 3 years if left untreated (7).

Self-Quiz
Ask Yourself...
- HIV is unique in that it primarily targets CD4-T cells inside the host. How does this directly contribute to symptoms and affect the trajectory of the disease?
- How does the body‘s natural defenses against such an invasion affect disease trajectory?
- Which stage do you think a person is most likely to be unknowingly transmitting the virus to others?
- Which stage do you think someone not undergoing routine testing is most likely to find out about their illness?
- What about someone who gets routine or yearly testing?
Transmissibility
Perhaps the most elusive part of this virus for many years was how it spreads. We now know that HIV is spread only through certain bodily fluids. An accurate understanding of HIV transmission is important for healthcare professionals to provide proper education to their patients, reduce misconceptions and stigmas, and prevent transmission and protect themselves and other patients (11).
Bodily fluids that can transmit the virus include:
- Blood
- Semen and pre-seminal fluid
- Rectal fluid
- Vaginal fluid
- Breastmilk
- Fluids that may contain blood such as amniotic fluid, pleural fluid, pericardial fluid, and cerebrospinal fluid
If one of these fluids comes in contact with a mucous membrane such as the mouth, vagina, rectum, etc., or damaged tissue such as open wounds, or is directly injected into the bloodstream, then transmission of HIV is possible (11).
Scenarios where transmission is possible include:
- Vaginal or anal sex with someone who has HIV (condoms and appropriate treatment with antivirals reduce this risk)
- Sharing needles or syringes with someone who has HIV
- Mother-to-child transmission during pregnancy, delivery, or breastfeeding (appropriate treatment during pregnancy, c-section delivery, and alternative feeding methods reduce this risk)
- Receiving a transfusion of infected blood or blood products (this is very rare now because of screening processes for blood donations)
- Oral sex with someone who has HIV (though this is very rare)
- A healthcare worker receiving a needle stick with a dirty sharp (risk of transmission is very low in this scenario)
HIV cannot be transmitted via:
- Saliva
- Sputum
- Feces
- Urine
- Vomit
- Sweat
- Mucous
- Kissing
- Sharing food or drink

Self-Quiz
Ask Yourself...
- What sort of PPE do you need to wear when helping an HIV+ patient use a bedpan?
- What about assisting with a procedure where blood splatter may occur?
- What factors about childbirth make this event particularly risky for transmission?
- What interventions might help reduce that risk?
- Think about the population you work with. What methods of transmission are they most at risk from?
- How might this differ among different populations or work settings?
Reducing Transmission
Patient education about risk and protection against HIV, testing, and what to do if exposed should be standard practice for healthcare professionals in nearly all healthcare settings. Primary care should include risk screenings and patient education routinely to ideally help prevent infections from even occurring or catch those that have occurred early on in the disease process (11).
Strategies include:
- Identifying those most at risk, incredibly gay or bisexual men, minority patients, and those using drugs by injection
- Ensure patients are aware of and have access to protective measures such as condoms and clean needle exchange programs
- Provide routine screening blood work for anyone with risk factors or desiring testing
- Providing access to PrEP medications where indicated (discussed further below)
- Staying up to date on current CDC recommendations and HIV developments
- Maintaining a nonjudgmental demeanor when discussing HIV with patients to welcome open discussion (11)
For patients with a repeated or frequent high risk of HIV exposure, such as those with an HIV+ partner or those routinely using IV drugs, pre-exposure prophylaxis (PrEP) may be a good choice to reduce the risk of them contracting the virus. When used correctly, PrEP is 99% effective at preventing infection from high–risk sexual activity and 74% effective at preventing infection from injectable drug use. Depending on the type of exposure risk (anal sex, vaginal sex, needle sharing, etc.), PrEP needs to be taken anywhere from 7-21 days before it reaches its maximum effectiveness. Most insurances, including Medicaid programs, cover PrEP at least in part. There are also federal and state assistance programs available to make PrEP available to as many people who need it as possible. Some side effects are commonly reported, primarily G.I. symptoms, headaches, and fatigue (11).
For those who have a confirmed diagnosis of HIV/AIDS, the focus should be promoting interventions that will prevent further transmission. One of the biggest determinants for transmission is the infected person’s viral load. Individuals being treated for HIV can have their viral load measured to ensure viral replication is being controlled as intended. A viral load lower than 20-40 copies per milliliter of blood is considered undetectable, meaning the virus is not transmissible to others. Even for those not receiving treatment, there are methods to reduce transmission (11).
Important considerations for transmission in patients who are HIV+ include:
- Referral for treatment and educating on the importance of treatment compliance in order to keep the viral load as low as possible
- Education on the importance (and possible legal consequences) of proper disclosure to any sexual or needle–sharing partners who may be at risk of exposure
- Encouraging and assisting with access to condom use and clean needle programs
- Providing information to HIV+ pregnant women about how interventions such as proper treatment during pregnancy, c-section delivery, and formula feeding can keep the risk of transmission as low as 1% (11)
Methods of infection control for healthcare professionals include:
- Universal precautions when handling any bodily fluids
- Eyewear when at risk for fluid splashing
- Careful and proper handling of sharps
- Facilities having a standard plan in place for potential exposures
If exposure or needlestick do occur for healthcare professionals, the patient would ideally submit to testing for HIV to determine if the staff member is even at any risk. If the HIV status of the patient is unknown or confirmed to be positive, four weeks of post–exposure prophylaxis (PEP) may be advised within 72 hours of exposure (11).
PEP is meant for emergency use only, such as for healthcare workers with a potential exposure or patients with an exposure that is not expected to become routine. PEP is not meant to replace the use of PrEP or other preventative measures. In order to be effective, PEP must be started within 72 hours of the potential exposure and must be taken for a 28–day course of treatment. When used correctly, it is highly effective and typically well–tolerated, with nausea being the most common side effect. For healthcare professionals taking it due to workplace exposure, your facility should cover the cost. For patients in the general population, insurance will usually cover it, or there are assistance programs available to make it affordable for everyone (11).

Self-Quiz
Ask Yourself...
- What screening questions or protocols are in place where you work to detect those most at risk of contracting HIV?
- In what ways, if any, could your facility improve its screening protocol to identify more at–risk patients?
- What information should be given to a pregnant woman with HIV who is asking about different infant feeding methods?
- Do you know what your facility‘s blood–borne pathogen protocol is?
- What steps are in place to help you if you get a dirty needle stick?
- Think about the population you work with. Are there any patients that might benefit from routine use of PrEP?
- What sorts of scenarios might indicate the need for the use of PEP?
Treatment Considerations
When HIV is appropriately treated, advancement from HIV to AIDS can be significantly reduced, and quality and longevity of life maximized. In 2018, the CDC estimated around 65% of all U.S. citizens living with HIV were virally suppressed, and 85% of those receiving regular HIV–related care were considered virally suppressed. However, an estimated13% of all HIV cases do not know they are infected. Appropriate medical care and keeping viral loads undetectable is one of the single most effective methods of preventing transmission (4, 6).
For those receiving treatment, a multifaceted and individualized approach can reduce a person‘s viral load, reduce the risk of transmission, reduce the likelihood of developing AIDS, and preserve the immune system. Regardless of how early someone receives treatment, there is no cure for HIV, and an infected person will be infected for life. All individuals diagnosed with HIV (even asymptomatic people, infants, and children) should receive antiretroviral therapy or ART as quickly as possible after a diagnosis of HIV is made. There are seven different classes of antiretroviral medications that disrupt various points in the viral replication process. Most treatment regimens use several of these medications combined with the most effective results; some combination pills are also available for administration ease. Medication regimens are chosen based on a patient‘s health status and history, tolerance or sensitivity to medication, and stage and severity of HIV infection. Patient condition and viral load should be monitored closely, and changes or inadequate response to treatment may indicate the need for a change in medication regimen at any time (1).
The classes and available medications for ART include (1):
Nucleoside reverse transcriptase inhibitors (NRTIs): these inhibit the transcription of viral RNA to DNA
- Abacavir (Ziagen)
- Emtricitabine (Emtriva)
- Lamivudine (Epivir)
- Tenofovir disoproxil fumerate (Viread)
- Zidovudine (Retrovir)
Non-nucleoside reverse transcriptase inhibitors (NNRTIs): these inhibit the transcription of viral RNA to DNA
- Doravirine (Pifeltro)
- Efavirenz (Sustiva)
- Etravirine (Intelence)
- Nevirapine (Viramune, Viramune XR)
- Rilpivirine (Edurant)
Protease inhibitors: inhibit the final step of viral budding
- Atazanavir (Reyataz)
- Darunavir (Prezista)
- Fosamprenavir (Lexiva)
- Ritonavir (Norvir)
- Saquinavir (Invirase)
- Tipranavir (Apitvus)
Fusion inhibitors: prevent the virus from fusing with CD4-T cells
- Enfuvirtide (Fuzeon)
Integrase strand transfer inhibitors (INSTIs): these stop HIV from inserting its DNA into cells
- Dolutegravir (Tivicay)
- Raltegravir (Isentress, Isentress HD)
Chemokine receptor antagonists (CCR5 antagonists): prevent the virus from binding to CD4-T cells
- Maraviroc (Selzentry)
Entry inhibitors: prevent the virus from binding to and entering cells
- Ibalizumab-uiyk (Trogarzo) (1)
These types of medication do not come without side effects or complications. Most side effects fit into a few major groups and may be bothersome but are not life–threatening or serious. More Serious or worrisome adverse effects may occur, and a patient‘s current health status, as well as medical history or existing conditions, should be carefully considered (3). The common categories of adverse medication reactions include:
- Gastrointestinal: Nausea, vomiting, diarrhea, decrease in appetite, reflux, constipation, damage to liver or pancreas
- CNS: Headache, dizziness, sleep disturbance, neuropathy, memory problems, hearing impairment or tinnitus
- Hematological: Anemia, hematuria, hyperbilirubinemia
- Psychological: Mood swings, anxiety, depression, confusion, nightmares/vivid dreams
- Dermatological: Rash, face discoloration, pruritus
- Musculoskeletal: Body aches, abnormal fat distribution
- GU: Menstrual cycle disruption
Due to the need to take medications for the rest of one‘s life and the long list of potentially bothersome side effects, medication adherence is a common issue in treating HIV appropriately (3).
There are several scenarios that increase the likelihood of poor compliance, including:
- Asymptomatic patients, since side effects of medications, maybe unpleasant and they are in a latent phase of disease without symptoms
- Young patients, including children or teenagers who may not understand the necessity of taking daily medications and face a lifetime of treatment
- Patients with substance abuse or mental health issues, as they may be in and out of cognitive and psychiatric crises
- Poor literacy or education level, as these patients may be easily confused by a complicated medication regimen or simply not understand the importance of lifelong therapy, especially if they are feeling well
- Social stigma, which may lead people to try and hide medications or not want their diagnosis to be discovered (3)

Self-Quiz
Ask Yourself...
- Why might it be important to take several medications that interrupt the viral replication process at different points?
- Think about the population you work with. What potential barriers to proper treatment are there?
- Think about the potential side effects of medications for HIV. How difficult do you think it would be to keep taking a medication like that, even if you understood why you needed it?
- Do you think it would be difficult to take daily medication if you had no symptoms and felt well?
Care Considerations for Comorbidities and Coinfections
Caring for patients with HIV or AIDS is a complicated task requiring compassion, patience, and understanding the many potential complications and ways that various body systems are affected. Many infections and comorbidities commonly present alongside HIV/AIDS, particularly as patients age, immune function declines, and effects of long-term medication use develop. The social stigma and psychological impact of such a devastating disease must also be considered to provide holistic care to these patients (9). Common coinfections/comorbidities include:
Tuberculosis
T.B. is a highly contagious airborne illness that affects the respiratory system. It is an opportunistic infection that frequently affects people with weakened immune systems, like those with AIDS. The bacteria can live in the body without causing symptoms in a latent phase for long periods. As the immune system in HIV weakens, a latent T.B. infection may become active, causing symptoms and deteriorating health. Most common symptoms include cough, hemoptysis, fever, fatigue, night sweats, or poor appetite, and weight loss. Seriously immunocompromised people may even experience disseminated T.B. where the infection affects more than the lungs and can even lead to septic shock and death. Annual PPD tests for T.B., or chest X-ray for anyone with a history of positive PPD, should be conducted on patients with HIV (9).
Hepatitis
About 1 in 10 people affected by HIV will also have viral hepatitis, as the diseases are spread in much the same way, particularly needle sharing and sexually and vertically (mother to fetus). Hepatitis infections progress quickly in immunocompromised patients and can greatly reduce liver function, which complicates the use of ART medications and can result in poor clearance from the body. All new HIV diagnoses should be screened for Hepatitis A, B, and C, and Hep A and B vaccines should be encouraged in unvaccinated patients (9).
STIs
Because HIV can be acquired via high–risk sexual activity, infection with other STIs is common. Sometimes, other STIs may even increase the risk of contracting HIV as they result in open sores or breaks in the skin where HIV can more easily enter. Bacterial STIs can typically be cured with antibiotics, but other viral STIs like Herpes and HPV do not have a cure. Routine screening for patients engaging in high–risk sexual activity or those already infected with HIV should be a typical part of care (9).
Cardiovascular Disease
Studies show that patients with HIV also increase inflammation of the arteries and plaque formations throughout the body due to a complicated effect on macrophages. Some of the ART medications also increase the risk of heart attack or stroke. Concurrent infection with hepatitis can increase cholesterol, which further deteriorates cardiovascular health and increases MI or stroke risk. Patients with HIV should be screened for family history and current heart health, and their plan of care should incorporate ways to reduce risks, including a focus on diet and activity level (9)l.
Osteoporosis
Bone density has been shown to decrease faster than normal in patients receiving ART medications, and it is recommended that patients over age 50 have annual bone density scans to estimate fracture risk. Treatment for osteoporosis should be added to the plan of care as needed (9).
Cancer
As science has become better equipped to detect and treat HIV and concomitant infection, cancer has remained a leading cause of death for HIV patients and is a considerable risk for those living with the disease. Most commonly, cancers of the head and neck, anus, lungs, liver, and lymph system occur. Smoking cessation, regular pap tests for women, HPV vaccines, and routine screenings like colonoscopies after a certain age should be heavily counseled in HIV patients to reduce their risk further. Earlier and consistent ART has been shown to reduce the risk of developing cancer (9).
Mental Health Issues
When considering the long–term and eventually fatal nature of this disease, along with the social stigma and complicated and expensive treatment regimens, it is no surprise that mental health disorders such as anxiety and depression are common for patients with HIV. Upwards of 22% of patients with HIV will suffer from depression, likely higher when you account for substance abuse disorders. In addition to assessing and treating body systems affected by the virus, it is important to screen patients for psychiatric disorders and be aware of the negative effects the diagnosis may be having on mental health. Medication treatment and therapy should be included in care where appropriate (9).

Self-Quiz
Ask Yourself...
- Think of the common health concerns in the population you work with, particularly when age and family history are factored in. How would a diagnosis of HIV affect those risks and health considerations?
- Consider what it would feel like to have a diagnosis of HIV and then be given a diagnosis of cancer or T.B. How do you think you would feel?
- How do you think your mental health would be affected?
- What other potential screenings or lifestyle changes would be a good idea for someone with HIV?
Ethical Concerns
Maintaining confidentiality under HIPAA laws is essential in the care of patients with any diagnosis, but the social stigma attached to HIV infection–in addition to the frequency and intensity of medical care needed and the responsibility to notify partners and prevent further spread–makes confidentiality particularly challenging with many ethical considerations to navigate.
The first issue with maintaining confidentiality occurs with testing itself. HIV is considered a reportable disease. Any positive results must be reported to a local health department and then on to the CDC for local and national statistics and to initiate follow–up with the positive person and provide education on the next steps. Patient names and identifying information are included with the positive result when reported to local and state health departments but is removed before it is reported to the CDC. There is an option for anonymous testing where patients are given a special identification number, and their names and identifying information are not included. These are often self–administered tests and are not available everywhere (8).
Testing for HIV requires informed consent, meaning healthcare professionals must discuss the risks, benefits, and potential consequences of testing for HIV and cannot test someone for HIV without their consent. Minors’ ability to get testing and treatment for HIV without a parent or guardian’s consent varies from state to state (8).
Once someone tests positive for HIV, the issue of disclosure presents itself. Patients need to inform their past and future sexual partners or anyone they share needles with of their HIV status. Health departments will help contact tracing and notifying past partners and help those potentially exposed with their testing and prophylactic treatment options. In some states, it is considered a criminal offense to withhold a positive infection status when a person may be exposing others. However, the responsibility to disclose falls on the patient, and healthcare professionals may not notify potential contacts without a patient‘s consent. Infected persons are not required to inform friends, family, employers, or others who are not at risk of contracting the disease (8).
Employers who provide health insurance for their employees may be given information about the costs and benefits of disclosing an HIV diagnosis indirectly. So while insurance companies cannot directly tell an employer about an HIV diagnosis, employees should be aware the information may come out indirectly. However, all workers with HIV are protected under the Americans with Disabilities Act. As long as they can complete their job duties, employers may not discriminate against them (8).
Finally, and of particular importance for healthcare professionals, is navigating the stigma or negative stereotypes that often accompany an HIV diagnosis. There are some societal misconceptions that HIV infections only occur as a result of immoral or taboo behavior or that those infected should be treated differently or avoided. People with HIV may have internalized these harmful stereotypes and feel a sense of shame around their diagnosis. It is important for healthcare professionals to understand that these stereotypes are untrue and harmful, but to provide non–judgemental and compassion that preserves dignity and views the patient as more than their diagnosis.

Self-Quiz
Ask Yourself...
- Why do you think there are laws in place requiring people to disclose their HIV status to potential sexual partners?
- Can you think of any other illnesses where your disclosure is as important as with this disease? Why or why not?
- Why is reporting data about new HIV infections to the CDC important?
- Think about your own internalized thoughts on HIV. Do you have any stereotypes or other negative views that might subconsciously affect your ability to provide non-judgmental care?
Conclusion
Professionals in any healthcare setting may encounter patients with HIV or AIDS. A basic understanding of this disease’s many considerations is fundamental to ensure that quality and compassionate care is being provided. Understanding the disease, treatments, and the unique struggles of these patients can significantly impact their healthcare experiences and promote quality of life.
Nutrition for a Healthy Heart
Introduction
Research indicates that a heart-healthy diet is a powerful tool for the prevention and control of cardiovascular disease [1]. A heart-healthy dietary approach to wellness emphasizes the intake of the appropriate proportions of macronutrients, essential vitamins, minerals, and fiber while minimizing the consumption of saturated fats, trans fats, cholesterol, salt (sodium), and the reduction of processed foods, trans-fats, and added sugars [2] [3]. The cornerstone of the diet includes an abundance of fresh fruits and vegetables, whole grains, lean proteins, and healthy fats [2].
For healthcare providers and patients, the goal of adopting a heart-healthy diet is multifaceted. The diet aims for a reduction in overall cardiometabolic risk, improving blood pressure, lowering cholesterol levels, reducing the risk of developing heart disease and stroke, and preserving the overall health of the circulatory system [3].
Nurses play a pivotal role in patient education and promoting heart-healthy lifestyles by empowering patients with knowledge and skills related to nutrition and dietary choices. This course aims to equip nurses with comprehensive knowledge of heart-healthy eating principles, enabling them to guide and educate their patients.
The adoption of healthy lifestyle choices, with nutrition being the most important behavioral factor, is estimated to reduce the risk of myocardial infarction (MI) by 81–94% [5][6][7]. In comparison, treatment with pharmacotherapies alone results in a 20–30% reduction [8].


Self Quiz
Ask yourself...
- Why is nutrition considered the most important behavioral factor in reducing the risk of myocardial infarction (MI) compared to pharmacotherapies alone?
Heart Disease: A Brief Overview
Heart disease remains one of the leading causes of morbidity and mortality worldwide, with diet and nutrition playing a crucial role in both its development and prevention [4]. Cardiovascular diseases, also known as CVDs, are the primary cause of death worldwide, claiming an estimated 17.9 million lives per year [4].
Cardiovascular disorders affect the heart and blood vessels, manifesting in coronary heart disease, cerebrovascular disease, rheumatic heart disease, and others. More than four out of five CVD fatalities stem from heart attacks and strokes, with one-third of these deaths occurring in individuals under the age of 70 [4].
The term "heart disease" encompasses various conditions affecting the heart's structure and function, many of which are influenced by dietary habits [9]. Cardiovascular risk factors, including malnutrition, tobacco and alcohol use, stress, obesity, sedentary lifestyle, hypertension, diabetes, hyperlipidemia, and genetic predisposition, can increase an individual's likelihood of developing cardiovascular diseases [10] [12].
The modifiable risk factors include sedentary lifestyle, smoking, high blood pressure, diabetes, hypercholesterolemia [12]. Almost three quarters of patients (73%) had at least three risk factors compared to 31% of healthy subjects.
Family history of cardiovascular disease (CVD) is a significant independent risk factor for premature coronary heart disease (CHD). The risk of premature CHD increases in a linear fashion as the number of affected family members grows. [11]. Cardiovascular risk factors, including malnutrition, tobacco and alcohol use, stress, obesity, sedentary lifestyle, hypertension, diabetes, hyperlipidemia, and genetic predisposition, can increase an individual's likelihood of developing cardiovascular diseases [10].
The five modifiable risk factors include sedentary lifestyle, smoking, high blood pressure, diabetes, and hypercholesterolemia [10]. A higher proportion of cardiovascular patients (73%) had at least three risk factors compared to healthy individuals, where less than one-third had three or more risk factors [10].

Self Quiz
Ask yourself...
- What are the key dietary factors that contribute to the development of cardiovascular diseases (CVDs)?
- How do modifiable risk factors, such as sedentary lifestyle, smoking, high blood pressure, diabetes, and hypercholesterolemia, increase an individual's likelihood of developing CVDs?
- Why is a family history of CVD considered a significant independent risk factor for premature coronary heart disease (CHD)?
Types of Heart Disease / Statistics
There are multiple types of heart disease, each with distinct mechanisms and implications for dietary management [13]. Coronary artery disease (CAD), heart failure, hypertensive heart disease, and arrhythmias represent a fraction of these conditions. The four main types of CVD include coronary heart disease, stroke, peripheral arterial disease, and aortic disease [15].
Coronary artery disease (CAD) is the most common type of heart disease [14]. Cerebrovascular disease is the second leading cause of heart disease. Other forms of heart disease include congenital heart disease, heart valve disease, cardiomyopathy, pericardial disease, arrhythmia, and aortic dissection.
Congenital heart disease (CHD) is the most common type of birth defect, affecting about 1 in 100 babies born in the United States [16]. CHDs can range from mild to severe and can affect the heart's structure, function, or both [16].
Heart valve disease is a condition in which one or more of the heart valves are damaged or diseased, which causes blood to flow backward through the valves, damaging the heart and other organs [17]. Heart valve disease affects 2.5% of the U.S population and can be caused by several factors, including infection, injury, and aging [17].
Heart failure is the heart's inability to pump blood, leading to symptoms such as fatigue, shortness of breath, swelling, chest pain, palpitations, weight gain, swelling in the ankles, legs, and abdomen, bloated or hard stomach, dry and hacking cough, and nausea [18] [19]. More than 6 million adults in the United States have heart failure [18].
Cardiomyopathy represents a collection of diverse conditions of the heart which makes it weaker and less able to pump blood. Cardiomyopathy can be caused by several factors, including infection, toxins, and genetic disorders [20]. Due to the potential for underdiagnosis, estimates of cardiomyopathy prevalence can vary. It is estimated that up to 1 in 500 adults may be affected by this condition [21].
Pericardial disease is a condition that affects the pericardium, the sac that surrounds the heart [22]. This can cause inflammation, infection, or scarring of the pericardium, which can interfere with the heart's ability to function. Pericardial disease can manifest as acute pericarditis, pericardial effusion, cardiac tamponade, or constrictive pericarditis [22].
Arrhythmia is a cardiac disorder characterized by an abnormal heart rhythm, manifesting as tachycardia (excessively rapid heartbeat), bradycardia (abnormally slow heartbeat), or irregular heartbeat patterns [23]. These irregularities can induce symptoms such as palpitations, dizziness, and syncope (fainting episodes) and can arise from various etiologies, including underlying heart conditions, electrolyte imbalances, and adverse effects of certain medications [23]. One in 18 people, or 5 percent of the U.S. population has an arrhythmia with a-fib (atrial fibrillation) being the most common [24].
Aortic dissection is a rare, life-threatening condition in which the inner layer of the body’s main artery (aorta), tears [25]. This can cause blood to leak between the layers of the aorta, which can weaken the artery and cause it to rupture. Aortic dissection can be caused by several factors, including high blood pressure, atherosclerosis, and connective tissue disorders [25].
Aortic dissection affects about 30 in 1 million people each year and more than 13,000 die each year [26]. Aortic dissection is most common in those individuals over the age of 60 and if not treated, the tear can worsen, ripping the outer layer of the aorta and allowing blood to escape the artery [25] [26]. As many as 40 percent of individuals who suffer from an aortic dissection die, and the risk of death increases by 3-4 percent every hour the condition is left untreated [26].

Self Quiz
Ask yourself...
- What are the distinct mechanisms and implications for dietary management of different types of heart disease?
- How do the etiologies and clinical manifestations of heart valve disease, cardiomyopathy, and pericardial disease differ from each other?
- What are the potential consequences of untreated arrhythmias, and how can lifestyle modifications and pharmacological interventions contribute to their management?
- Why is aortic dissection considered a life-threatening condition, and what are the critical steps involved in its diagnosis and treatment?
Evidence on Diet and Heart Health / Diet Options
When considering the diet options for heart health, the Mediterranean diet, DASH diet, and plant-based diets are among the most researched and recommended. These diets share common elements such as an emphasis on whole foods, minimal intake of red meat, and a high volume of fruits and vegetables. Extensive research has demonstrated that the DASH dietary pattern lowers the risk of cardiovascular disease [37]. Numerous prospective studies have demonstrated the consistent benefits of the Mediterranean diet on cardiovascular health [30].
There is substantial evidence that most vascular events may be prevented by avoiding smoking, participating in regular physical activity, maintaining normal body mass index, and eating a healthy diet [27].
Observational studies have demonstrated that dietary patterns rich in fruits and vegetables, excluding white potatoes, are linked to a lower risk of CVD [28] [29]. Regular consumption of whole grain foods has been linked to a reduced risk of cardiovascular disease (CVD), coronary heart disease (CHD), stroke, metabolic syndrome, and various cardiometabolic risk factors, as evidenced by robust observational studies and clinical trials [28]. Numerous randomized controlled intervention studies have demonstrated that replacing refined grains with whole grains leads to significant improvements in cardiovascular risk factors [28] [31].
Except for a small trial that demonstrated a reduction in arrhythmia recurrences among regular drinkers with atrial fibrillation upon alcohol abstinence, no other studies have reported favorable outcomes associated with alcohol consumption for cardiovascular health [32].
Dietary fiber, abundant in plant-based foods like fruits, vegetables, whole grains, nuts, seeds, beans, and legumes, have shown an inverse association with a lower risk of metabolic syndrome and cardiometabolic risk factors [33].
A systematic review and meta-analysis provided evidence that substituting saturated fat with unsaturated fat can improve cardiovascular outcomes and reduce the risk of CVD [34]. Plant-based diets rich in foods like whole grains, fruits, vegetables, and nuts, have been linked to a reduced risk of cardiovascular events and intermediate risk factors [36].
Current evidence does not support the widespread use of high-dose vitamin and mineral supplements for the prevention of cardiovascular disease (CVD) [28].


Self Quiz
Ask yourself...
- What are the common elements shared by the Mediterranean diet, DASH diet, and plant-based diets that contribute to their positive impact on heart health?
- How does the evidence from observational studies and clinical trials support the link between regular consumption of whole grains and a reduced risk of cardiovascular diseases?
- What are the potential mechanisms by which dietary fiber from plant-based foods exerts its protective effects against metabolic syndrome and cardiometabolic risk factors?
Role of Sodium and Fats
Sodium and fats hold significant impact over heart health. High sodium intake is associated with hypertension, a risk factor for heart disease, while certain types of saturated and trans fats, are linked to an increase in LDL cholesterol and the development of atherosclerosis [28]. A systematic review and meta-analysis revealed the detrimental effects of saturated fat on cardiovascular disease (CVD) outcomes and risk factors compared to unsaturated fat. [36]
A strong body of evidence has documented the adverse effects of trans fatty acids on cardiometabolic risk factors [37]. Adhering to current recommendations to replace saturated fat from meat and dairy with nontropical plant oils also lowers dietary trans fatty acids [38].

Self Quiz
Ask yourself...
- How does the consumption of sodium and certain types of fats contribute to the development of cardiovascular diseases?
- What dietary strategies can be implemented to reduce sodium intake and limit the consumption of saturated and trans fats, thereby promoting heart health?
Healthy Eating Tips and Strategies
Incorporating a heart-healthy diet into a patient’s lifestyle requires practical tips and strategies. First, make gradual changes instead of overhauling the entire diet. Meal planning can help with healthier choices.
Setting realistic goals and collaborating with the patients to set achievable dietary goals. Controlling portion size, using smaller plates and bowls, prioritizing low-calorie, nutrient-rich foods like fruits and vegetables and limit high-calorie, high-sodium foods like refined, processed, or fast foods [39].
Paying attention to the amount of saturated and trans fats, cholesterol, and sodium. Suggest lean protein sources such as fish, poultry, beans, and lentils and limit the intake of unhealthy fats and instead opt for healthy fats like those found in olive oil, avocados, and nuts [39].
Consume at least five servings of fruit and vegetables daily [41]. Choose whole grains over refined grains and limit the intake of added sugars [28]. To have more control over the ingredients, cook and consume meals at home and make gradual changes to diet habits and build on those habits over time.

Self Quiz
Ask yourself...
- How can healthcare providers collaborate with patients to set achievable dietary goals that align with their lifestyle and preferences?
- What are some practical strategies for making gradual changes to a patient's diet, ensuring adherence and long-term success in adopting heart-healthy eating habits?
Patient Education
Nurses are well positioned to provide patient education and counseling on heart-healthy eating. The core of patient education lies in translating knowledge into practice. Nurses must communicate with consideration of cultural, linguistic, and individual patient dietary preferences. Education should be patient-centered, with actionable steps that patients can integrate into their daily lives [40].
Effective patient education strategies can include establishing a rapport, assessing the patient's knowledge, and understanding, tailoring the educational approach, using plain language, incorporating visual aids, encouraging active participation, providing written materials and ongoing support and follow-up, and addressing any barriers and concerns [42].

Self Quiz
Ask yourself...
- How can nurses tailor their patient education strategies to address individual cultural, linguistic, and dietary preferences, ensuring that the information conveyed is relevant, understandable, and actionable for each patient?
Resources
A wealth of resources is available to support nurses in their role as patient educators, from professional organizations like the American Heart Association to local community programs and online platforms [43]. These resources offer educational materials, dietary guidelines, and support tools that nurses can utilize to enhance their teaching.
A heart-healthy diet is one that is low in saturated and trans fats, cholesterol, and sodium. It is also high in fiber, fruits, vegetables, and whole grains [2][3]. Eating a heart-healthy diet can help to lower your blood pressure, cholesterol levels, and risk of heart disease [2].
The National Heart, Lung, and Blood Institute (NHLBI) has a website with information on heart-healthy eating, including recipes, meal plans, and tips for eating out. The American Heart Association (AHA) has a website with information on heart-healthy eating, including recipes, meal plans, and tips for shopping for heart-healthy foods.
The Dietary Approaches to Stop Hypertension (DASH) diet is a heart-healthy eating plan that has been shown to lower blood pressure [45].
The Mediterranean diet is a heart-healthy eating plan that has been shown to have several health benefits, including reducing the risk of heart disease, stroke, and type 2 diabetes [44]. You can find information about the Mediterranean diet on the Mayo Clinic website.
In addition to these websites, there are many cookbooks and other resources available on heart-healthy eating. Patients can also talk to their doctor or a registered dietitian for personalized advice on how to eat a heart-healthy diet.

Self Quiz
Ask yourself...
- How can nurses utilize the wealth of resources available, such as those from professional organizations and online platforms, to enhance their patient education on heart-healthy eating?
- How can nurses convey the key principles of heart-healthy eating, such as limiting saturated and trans fats, cholesterol, and sodium while emphasizing fiber, fruits, vegetables, and whole grains?
- How can nurses guide patients towards reputable and reliable resources, such as those from the National Heart, Lung, and Blood Institute, the American Heart Association, and the Mayo Clinic, to ensure that they have access to accurate and evidence-based information on heart-healthy eating?
Conclusion
In conclusion, adopting a heart-healthy diet is a crucial step towards maintaining cardiovascular well-being and overall health [30]. The nurse's role as a patient educator in promoting a heart-healthy diet is pivotal. By leveraging a position of trust and frequency of contact with patients, nurses can champion dietary choices that can reduce the risk and impact of heart disease.
Research underscores the importance of a balanced intake of nutrients to support the cardiovascular system's health, emphasizing whole foods, lean proteins, healthy fats, and a reduction in sodium, saturated fats, and sugars [3].
Patients adopting a heart healthy diet require a multifaceted approach, combining knowledge with actionable steps that are practical and sustainable. The role of healthcare professional is instrumental in this dietary transition.
A heart-healthy diet offers a multitude of benefits beyond reducing heart disease risk. It can improve blood pressure control, lower cholesterol levels, promote healthy weight management, and enhance overall energy levels [2][3]. A heart-healthy diet can contribute to a stronger immune system, reduced inflammation, and improved mental clarity [46].

Self Quiz
Ask yourself...
- How can nurses bridge the gap between knowledge and practice when educating patients about heart-healthy eating, ensuring that patients understand the rationale behind dietary recommendations and can translate that knowledge into sustainable dietary changes?
- How can nurses emphasize the broader health benefits of a heart-healthy diet beyond reducing heart disease risk, motivating patients to adopt sustainable dietary changes for their overall well-being?
Adverse Childhood Experiences
Introduction
All children should grow and thrive in a caring, nurturing environment that meets their physical, emotional, and social needs. However, many are not so fortunate. Nearly every two in three Americans (64%) have experienced adverse childhood events (ACEs) (1, 2, 4, 5).
ACEs are highly associated with future chronic health conditions, mental illness, premature death, and more (1). In fact, the more ACEs an individual has had, the higher their risk for having poor health outcomes as adults (13).
Fortunately, there are preventive and protective measures that can be taken with the appropriate resources (1). With better awareness of ACEs and the right support in place, healthcare professionals can help improve the quality of life for a myriad of children and the adults they grow up to be.
Definition
Adverse childhood events, or ACEs, can occur from birth until age 18, and are great determinants of future health (1). These are any potentially traumatic events that happened to a child. ACEs are strongly linked to mental and physical disease in adults, contributing to at least half of the leading causes of death in the United States (1).
The ACE score is a 10-item survey to identify any negative occurrences a person had before their 18th birthday (3). The higher a person’s ACE score, the more risk they have for an unhealthy adulthood (1,2).
ACE was a term coined in a large-scale study published in 1998, describing them as childhood abuse and household dysfunction in seven specific areas (1, 2). In subsequent years, three more areas were added (3, 13). Altogether, the ten ACEs are comprised of the following examples of three broad categories:
- Childhood abuse
-
- Psychological
-
- Physical
-
- Sexual
- Household dysfunction
-
- Substance abuse
-
- Mental illness
-
- Parent treated violently.
-
- Family member incarcerated.
- Neglect
-
- Emotional
-
- Physical

Self Quiz
Ask yourself...
- How would you briefly define adverse childhood experiences (ACEs)?
- Would you add or subtract anything from the list above?
- What other examples of ACEs exist?
- Should one’s community and environment factor into ACEs as well? Why or why not?
Statistics and Demographics
The initial adverse childhood experience (ACE) study, conducted in the late 1990s, included over 17,000 adult participants and revealed the following key demographic data (1, 2, 5):
- Nearly 66% of women and 62% of men reported at least one ACE in their lives.
- More than 1 in 6 people (17.3%) said they had experienced four or more types of ACEs.
- Respondents’ races who reported ACEs were: 74.8% white, 11.2% Hispanic, 7.2% Asian/Pacific Islander, 4.5% black, and 2.3% other.
- About 49% of those with college degrees experienced at least one ACE, compared to 44% without a high school diploma.
- The age group who reported the highest incidence of ACEs was those from 35-49, where almost 70% had experienced at least one ACE. The lowest incidence was reported by those aged 65 and older, at 40%.
- Of all women reporting ACEs, 25% said they endured sexual abuse, 30% witnessed substance abuse in the home, and 25% of the respondents’ parents got divorced.
- Of all men reporting ACEs, 30% went through physical abuse, 24% saw substance abuse at home, and 22% of their parents were divorced.
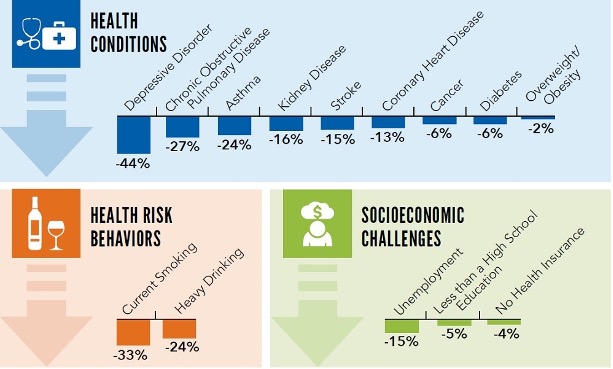
More recent data shows that at least 50% of the top causes of death in the US are associated with ACEs (6). As there is also a high association between ACES and depression, preventing these experiences could reduce adult depression by 44% (6).

Self Quiz
Ask yourself...
- Did any of the statistics surprise you? Why or why not?
- Reflect on your own life. How many of the 10 ACES might you have had, and how might you be able to manage them as an adult?
- What other data gathering might be useful when it comes to identifying and preventing ACEs?
- What would you identify as some of the highest risk factors for the occurrence of ACEs?
Causes and Risk Factors
The causes of adverse childhood events are varied and multifaceted. They can stem from familial or communal challenges, often referred to as social determinants of health. Many of these determinants can cause ACEs, and may include (8):
- Lack of access to healthcare or other resources
- Financial difficulties
- Homelessness or frequent moving
- Discrimination
- Any type of disrupted living situation
As noted earlier, most of the American population has had some sort of adverse childhood experience. However, there are some factors that make it more likely for these to occur. Societal, communal, and familial cultures all play a role in adverse experiences.
The following situations or conditions increase the likelihood of ACEs (7):
Community Risk Factors:
- High rates of poverty, crime, and violence
- Limited educational, economic, and employment opportunities
- Lack of community activities for youth
- Unstable housing and frequent moves by community residents
- Readily accessible alcohol and drugs
- Frequent experiences of food insecurity
Family and Individual Risk Factors:
- Social or developmental disabilities or delays
- Mental or chronic physical illnesses
- A history of abuse experienced by caregivers themselves.
- Youth dating or engaging in sexual activity early.
- Single-parent families, particularly those with young caregivers
- Low income and/or high economic stress
- Low education levels
- Children with few or no friends, or friends who partake in delinquent or aggressive behaviors
- Caregivers with limited understanding of child development
- Use of spanking or other corporal punishment as a form of discipline
- Inconsistent discipline and/or little parental supervision
- Families isolated from extended family, friends, and/or neighbors

Self Quiz
Ask yourself...
- In the community where you live, what might be some factors that contribute to ACEs in those around you?
- What are some ways your community might be able to mitigate some of the risk factors for ACEs?
- Since nearly two in three people have experienced an ACE in their lives, it is likely that you interact with someone affected by this issue. What resources might you recommend to them, and what else might help?
Cultural Considerations
Though many people experience ACEs, some populations are affected disproportionately. This includes women and those in racial or ethnic minorities, who are at greater risk for experiencing 4 or more ACEs (6, 8). Specifically, African Americans, American Indians, and Alaska Natives (AI/AN) are far more likely to have multiple ACEs than any other race or ethnicity (9,10).
The AI/AN community is a relatively young one, with poverty rates up to four times higher than the national average (10). Furthermore, the AI/AN group is often lumped together as “other” as a race category on surveys, making data harder to come by for this population (10).
AI/AN children, when compared to the total US population, are more likely to have:
- Parents who are divorced (33% versus 21%)
- Lived with someone who abused a substance (24% versus 12%)
- Witnessed domestic violence (15% versus 6%)
- Lived with a parent who ultimately died (4% versus 2%)
Lifespan Impact on the Individual
While adverse childhood experiences affect most Americans, having been through four or more puts a person at significantly higher risk of health problems as an adult (1, 2, 9). In general, the more ACEs an individual has experienced, the more likely they will have poor outcomes later in life, with a specifically high correlation to diabetes, heart disease, obesity, depression, substance abuse, smoking, poor academic achievement, and early death (4).
In fact, ACEs can reduce an individual’s life expectancy by as many as 20 years, compared to someone who has had zero ACEs (8).
The original ACEs study was conducted to determine the link between childhood abuse and adult health risk factors (1). The conclusion was overwhelmingly that in the United States, the main causes of morbidity and mortality are related to many of the health behaviors exhibited by those who have experienced ACEs (1). More recent studies find that ACEs contribute significantly to substance abuse, violence, and self-harming behavior (11).
At least 5 of the top 10 leading causes of death in the United States that are strongly related to ACEs include (9,11, 12):
- Heart disease (#1 cause of death)
- Stroke (#5)
- Chronic lower respiratory diseases (#6)
- Diabetes (#8)
- Chronic liver disease and cirrhosis (#9)
As far as mental health goes, the link with ACEs is clear: The higher one’s ACE score, the more likely they are to be depressed, experience impaired work performance, and have suicidal tendencies (13). Harmful behaviors associated with high ACE scores include smoking, drinking, and drug abuse, as these methods are often used to cope with past traumatic experiences (13).

Self Quiz
Ask yourself...
- In light of the correlation between ACEs and some of the top causes of mortality in the US, what interventions could possibly be made in childhood to prevent these deaths from occurring?
- Though the top 10 causes of death in the US have a variety of causes, the link between ACEs has been well-established for nearly three decades. Why do you think more funding and attention aren’t given to this matter?
- What other physical or mental health concerns not listed above might a person with a high ACE score have?
Societal Implications
Adverse childhood events are preventable and have been shown to contribute to at least half of the leading causes of death in the United States (1, 9, 11). Thus, the impact of ACEs on public health is vast. Since the CDC considers ACEs a public health concern, it is of utmost importance to decrease their incidence (1). Through the reduction and prevention of ACEs, general public health would improve markedly, drastically cutting down on healthcare costs and resources (1, 5, 6, 9).
The societal implications for reducing ACEs are manifold:
- Dramatic reduction of preventable causes of death
- Longer lifespans for the general population
- Better mental health
- More cost-effective physical and mental healthcare
- Lower rates of disease and depression in the general population

Self Quiz
Ask yourself...
- What other societal impacts might ACEs have?
- How could you go about preventing some ACEs in your own life or community?
- What are some local, national, or global resources to which you could introduce those in need?
Ways to Mitigate ACEs
Though ACEs are widely pervasive in American society, they need not be so. With proper resources and support systems, many -if not all- ACEs may be eradicated. The best way to mitigate ACEs would be to prevent them in the first place (4). This requires creating safe, stable, nurturing environments for children and their families (9). Furthermore, as ACEs can occur for a wide array of reasons, they need to be addressed at both the family and communal levels.
With individuals, a first step would be prevention of ACEs in the home. This could involve a vast array of mental health, education, and social work services such as: home visits, parenting classes, therapy sessions, and more (8, 9). Different emotion management techniques and child development concepts could be taught to at-risk families, promoting bonding and trust between children and their caregivers.
High-quality childcare and after-school programs with trusted adults can help mitigate ACEs as well (9). Screening for ACEs at regular intervals would also be helpful. This could include annual check-ups at the doctor’s office, visits with the school nurse or counselor, or a consultation with a home health provider. Medical management of physical and mental health conditions would be made available, including routine health screenings and necessary medications (4, 8, 9).
At the community level, prevention could take the form of free education for family members, food and housing assistance, adequate access to healthcare services, and fostering safe neighborhoods (4, 9). Economic support for families could include family-friendly work policies, earned income tax credits, and so forth. Children could partake in community events like after-school clubs and sports, helping them build bonds with trusted and supportive adults.
Three principles are the most helpful preventing long-term effects of ACEs, (4):
- Reducing stress by ensuring basic needs are met, as well as tending to abusive situations, community crime, substance abuse, discrimination, and poverty.
- Strengthening life skills can strengthen the resilience of children and their family members by practicing planning, focus, and self-control.
- Building responsive relationships by having adults listen to their children and respond adequately to their needs, thereby fostering a safe, trusting relationship.

Self Quiz
Ask yourself...
- What specific local resources are available where you live or work that could help prevent ACEs from occurring in the first place?
- What types of secondary and tertiary prevention resources can you identify for ACEs?
- What are other ways ACEs can be mitigated or prevented at the state or federal level?
Reporting ACEs
Considering there are various types of ACEs, they can be difficult to identify and thus report. However, some are clear-cut. In situations where child abuse or neglect is occurring or suspected, a mandated reporter (e.g., nurse, teacher, counselor) would need to report it as soon as possible. If the child is in imminent danger, take them to a safe place and make a report.
To report child abuse in the United States, call or text 1-800-4-A-CHILD (1-800-422-4453). The website is https://www.childhelphotline.org/.
If there is suspicion that a child is being sexually exploited, the phone number to call is 1-800-THE-LOST (1-800-843-5678), and the website is https://report.cybertip.org/.
To report human trafficking, call 1-888-373-7888, use TTY at 711, text BEFREE (233733), or visit the website at https://humantraffickinghotline.org/.
For anyone experiencing feelings of self-harm or suicide, 988 is the national Suicide and Crisis Lifeline that can be called or texted. The website is https://988lifeline.org/.
Support and Additional Resources
While there is no single way to prevent ACEs from occurring, there is a plethora of resources available to help mitigate the effects and to educate others. Visting a healthcare provider can connect a patient to mental health professionals, support groups, or specialty services like social work and support groups (8).
The Substance Abuse and Mental Health Services Administration (SAMHSA) has an abundance of resources on topics like trauma-informed care, early childhood mental health programs, Native Connections for the AI/AN population, school, and campus health, and much more. More information can be found at https://www.samhsa.gov/programs.
Healthy Outcomes from Positive Experiences (HOPE) is a national resource center offering research, training, and technical assistance in order to better the lives of children and their families. Their website is https://positiveexperience.org/.
The Centers for Disease Control and Prevention (CDC) offers ACE-specific information at this website: https://www.cdc.gov/violenceprevention/aces/resources.html.
Conclusion
Adverse childhood events, or ACES, affect the majority of the American population. Strongly correlated with many leading causes of death, ACEs are preventable and warrant attention from healthcare providers and the general public alike. Fortunately, many resources exist at the individual, community, and national levels to provide care and prevention for these experiences.
Though ACEs tend to lead to negative health outcomes, they need not condemn a person to lifelong problems. Through screening tools, community food and housing programs, mental health assistance, education, and adequate medical care, ACEs can be mitigated, well managed, and prevented.
Despite the misfortune in a child’s life, there is still much hope available when they reach adulthood.
Conclusion
Adverse childhood events, or ACES, affect the majority of the American population. Strongly correlated with many leading causes of death, ACEs are preventable and warrant attention from healthcare providers and the general public alike. Fortunately, many resources exist at the individual, community, and national levels to provide care and prevention for these experiences.
Though ACEs tend to lead to negative health outcomes, they need not condemn a person to lifelong problems. Through screening tools, community food and housing programs, mental health assistance, education, and adequate medical care, ACEs can be mitigated, well managed, and prevented.
Despite the misfortune in a child’s life, there is still much hope available when they reach adulthood.
Trauma Informed Care in Nursing
Introduction
As nurses, we have been trained to perform ongoing assessments on patients with every encounter. Many patients have gone through traumatic events that often go undiscovered by the healthcare team.
A trauma informed care approach will help healthcare providers uncover past trauma. This will allow them to tailor a plan of care that helps alleviate patient suffering by decreasing overall stress and anxiety. When the healthcare team is aware of past trauma, they can avoid conversations and situations that could potentially re-traumatize the patient.
Trauma Informed Care
Trauma is a human experience that can affect people from all different backgrounds and walks of life. There is no race, gender, sexual orientation, or social class that is immune to the far-reaching clutches of trauma. A traumatic event is an event that is marked by sexual violence, severe injury and/or death. These events can be first-hand accounts where the people themselves were the victims of the event.
They can also be indirectly experienced by witnessing the event take place on another person. The event can also produce vicarious trauma when it happens to a close friend or loved one. No matter how traumatic an event was experienced, it can have severe and long-lasting effects (1).
Despite the rising accounts of traumatic events, trauma informed care is an underused skill in the healthcare field. Those who support and use trauma informed care understand that there is a large population of people seeking healthcare services who have had past traumatic experiences. They are also aware that just by seeking out care, they have the potential of being re-traumatized.
Empowering the patient to have control over their care through collaboration will help decrease the chances of re-traumatization.
There are six principles of trauma informed care:
- Safety
- Trustworthiness and transparency
- Peer support
- Collaboration and mutual support
- Cultural and historical sensitivity
- Empowerment of voice and choice
Trauma informed care runs parallel to ethics in the healthcare setting. It endeavors to ease the patient’s suffering by preventing re-traumatization and empowering the patient. (3)

Self Quiz
Ask yourself...
- What are two principles of trauma informed care?
- What is a past traumatic event?
- Who is affected by trauma?
Principles of Trauma Informed Care
It is meaningful to explore each of the six principles of trauma informed care
Safety
In trauma informed care, safety pertains to both the psychological and physical safety of the patient and their family throughout their encounter with the healthcare organization. The goal is to prevent any form of re-traumatization. This is accomplished by creating safe spaces, access to services, and engagement between the patient and the healthcare team.
One of the greatest aspects of safety in trauma informed care is environmental. This demands that the healthcare teams create an environment that is both welcoming and accommodating to all patients regardless of their diverse backgrounds. We must understand that patients who have undergone traumatic events can be hypersensitive to their environmental safety.
The trauma informed care plan must be individually tailored and include communication initiatives that promote the patient’s self-identity and how they would like to be addressed (1).

Self Quiz
Ask yourself...
- In trauma informed care, what kind of safety is discussed?
- How does the environment play a part in safety?
Trustworthiness and Transparency
Nursing has long been recognized as the nation’s most trusted profession. This has been accomplished through the intentional focus of patient advocacy. Nation-wide policies and safety goals have promoted diversity, equity, and inclusion. Initiatives to make sure that the patient understands and agrees with their plan of care, such as using their preferred language in plain and clear terms, is an example of how nurses build that trust.
Using the concept of patient-centered care helps demonstrate transparency, which is a way nurses further build trust. True transparency can be accomplished through encouraging patients to be involved in their care. Asking patients if it is acceptable that we document their experiences and even share our notes or computer screens to demonstrate our desire to be transparent.
Educating patients using the teach-back method also indicates our transparency as our knowledge becomes theirs (1).

Self Quiz
Ask yourself...
- How can the healthcare team build trust using trauma informed care?
- How can transparency be accomplished?
Peer Support
Contrary to popular beliefs, the goal of peer support in trauma informed care is not fixing the individual. Rather, the goal is to assist the individual to empower themselves by connecting them with supportive groups of peers that have similar experiences, culture, beliefs, and religion. Empowerment of the patient should be the goal of peer support. Traumatic stress is often accompanied by a re-traumatization cycle that can be interrupted and ultimately stopped through individual empowerment of the patient.
These peer support groups often contain members who themselves have survived traumatic events. To have the best probability of success, the patient should leave behind former friends who enable the re-traumatization cycle and gravitate to the peer support group members. This can leave the patient with further feelings of loss and grief. This has to be considered when developing the plan of care for the patient (1).
Identifying Past Trauma
Trauma informed care does not mean that the care is tailored to a patient’s specific trauma. Nor does it mean that the team endeavors to heal or even address past trauma. Rather, in simple terms, trauma informed care recognizes that the patient has been through a traumatic ordeal and that the plan of care must take that trauma into account in order to properly care for the patient.
The patient’s reaction and compliance may be affected by their past trauma. Past trauma needs to be identified and acknowledged. Past trauma can affect all aspects of a patient’s life. Identifying and acknowledging the trauma and how the patients then needed coping mechanisms may now have become detrimental to their health is important for the overall well-being of the patient.
Through the identification of past trauma, the team can take the opportunity to ensure that the patient does not feel responsible for the life-altering trauma and understands that the trauma was not their fault. Identifying the trauma can lead to the revelation that there is a connection between past trauma and the patient’s current coping and functioning; this can change their overall perspective, thus changing their lives (4).

Self Quiz
Ask yourself...
- What is the goal of peer support in trauma informed care?
- Who is often involved in peer past trauma support groups?
Collaboration and Mutual Support
Collaboration and mutual support demand that the entire healthcare team see the patient as both an equal partner and the expert in their own personal experiences. The patient should be allowed to both identify and prioritize their goals, then the healthcare team can work with the patient to for the plan of care with these goals at the forefront.
Collaboration takes more time than the traditional healthcare “do as I say” method. It helps in the trust-building process and when done properly, it helps the patient to succeed as the goals have come from them. This is something that can also interrupt the re-traumatization cycle. It also increases the probability that the patient will be compliant with the plan of care and any after-care appointments and follow-ups (1,4).


Self Quiz
Ask yourself...
- How is the patient seen through the collaboration lens?
- What destructive cycle can collaboration and peer support interrupt?
Cultural and Historical Sensitivity
The entirety of the patient’s identity is surrounded in cultural and historical sensitivity. Not only does this encompass aspects such as race, gender, age, etc. but it also includes life experiences and relationships right down to the base familial associations.
It also includes beliefs, core values and experiences in open spaces. When seeking healthcare, no matter the reason, all of these aspects of the patient’s identity are brought to the facility and laid in front of the healthcare team (1).
Empowerment of Voice and Choice
As discussed earlier in the peer support principle, empowerment is paramount in trauma informed care. Empowerment of voice and choice is perhaps the chief cornerstone and is present in all the other principles of trauma informed care. Trauma informed care empowers patients by making them feel heard and that their voice is important for their overall well-being.
Though the healthcare team may not always agree, trauma informed care also enforces the concept that the patient’s choices are to be respected. Through the trauma informed care journey, the patient develops their ability to navigate the healthcare setting and becomes familiar with the language of the medical community.
This further empowers the patient as they can understand the plan of care and become an active participant in that plan, as they were involved in both the planning and implementation. Further, trauma informed care creates a safe and supportive environment where the patient is allowed to grow and mature in their knowledge and understanding of themselves and their health (1).

Self Quiz
Ask yourself...
- In what ways does trauma informed care empower patients?
Effects of Traumatic Stress
Traumatic stress has shown to increase chronic illness, mental health issues and early death. When left alone, traumatic stress can morph into enduring stress. Some forms of enduring stress include:
- Chronic stress – this happens when trauma is continuous over a long period of time.
- Toxic stress – this is found in children who experience long-standing and/or frequent trauma such as emotional and physical abuse, neglect, and exposure to violence.
Traumatic stress can have altering effects on multiple brain processes. This includes the neurologic, immunologic, endocrinologic, metabolic, inflammatory, and autonomic processes. Depending on which phase of brain development the patient is in when the trauma occurs, it determines the long-lasting effects.
Repeated trauma can cause a hormonal cascade which can result in the allostatic load phenomenon. This phenomenon distorts the normal stress mediating processes.
Traumatic stress often leads to self-destructive behavior. Drug and alcohol use/addiction, violence and risky behavior often follows those who have had traumatic stress events. There is a fear among traumatic stress victims that they may be judged for their choices and lifestyle (1).


Self Quiz
Ask yourself...
- Can you name a type of enduring stress?
- What is the phenomenon that distorts the normal stress mediating processes of the brain?
- What can traumatic stress lead to?

Self Quiz
Ask yourself...
- What are two things that trauma informed care is not?
- What can be accomplished through identifying trauma?
- What does the healthcare team need to do in connection with the patient’s trauma?
Adverse Childhood Experiences
Nearly 40% of people have been exposed to adverse childhood experiences. Of course, adverse childhood experiences harm the overall health and well-being of the child; they also have a potential great impact on the physical and mental health of the person as they transition into adulthood.
Adverse childhood experiences and childhood trauma have shown to leave the patient with an increased risk for developing leading causes of death and disability. These conditions include heart disease, stroke, cancer, and depression with suicidal ideation. Also, childhood trauma can lead to symptoms of chronic headache and pain as an adult (2).
As most childhood trauma is perpetrated by someone known and close to the child such as a parent, relative or close family friend, the child is often left with an altered expectation of interpersonal relationships. This may lead to severe insecurity and distrust where negative personal perception especially in relation to others may develop.
People who develop physical symptoms of past childhood trauma are often unable to adjust and move on post-trauma. On the other hand, those who are able to form positive relationships tend to have fewer physical symptoms and are more liable to have adjusted to childhood trauma. Childhood trauma can have long-reaching effects on the ability of the adult to form positive relationships and have normal responses to stressful situations (2).

Self Quiz
Ask yourself...
- What percentage of people have had adverse childhood experiences?
- What type of conditions are victims of adverse childhood experiences in danger of developing?
- Can you discuss what adverse childhood experiences can lead to?
Trauma Informed Approach
The trauma informed approach was born out of the research on adverse childhood experiences. The research showed that the more adverse childhood experiences that took place in the patient’s life, the more it affected their mental and physical health; even leading to early death.
Trauma informed approach begins at the organizational level, where the culture must adapt to prevent re-traumatization. There are a few aspects that need to be incorporated into the organization’s training to accomplish the changes needed.
The organization must put on trauma glasses and view the healthcare team through the trauma lens. There is a direct correlation between trauma and mental health; this needs to be acknowledged, accepted, and viewed as part of the care plan.
In order for the trauma informed approach to be effective, the organization must realize that trauma expands beyond Post Traumatic Stress Disorder (PTSD). Rather, trauma incorporates a multitude of differing issues that can include mental, emotional, physical, and other multiple trauma sources.
The healthcare professional who is assessing the patient should be trained in recognizing the signs of trauma and, if disclosed, be able to respond appropriately in the moment. Training needs to be done with all front-line staff who the patient may confide in.
The healthcare team should be aware of resources that are available in the community and be able to refer the patient to those organizations. Being as trauma specific as possible so that the patient can connect in a meaningful way with this new support system. The organization should partner with these support groups to ensure easy transitioning from the institution to the community.
The team should also prioritize the principles of trauma informed care. For instance, to promote trustworthiness and transparency, the team could limit the number of healthcare providers who will ask the patient to repeat the story of their traumatic experience. Turning to more collaborative communication and relationships between the team and the patient; allowing the patient to be actively involved in their plan of care also promotes the trauma informed care principles.
Promoting safety within the organization for both the patient and the healthcare team also helps to change the culture to one of a trauma informed approach. Trauma survivors could be approached and asked to help design, implement, and evaluate the trauma informed approach to be used. What better way to get to know your community resources than to actively partner with them to help meet the needs of the organization’s patients.
It needs to be recognized that not all patients who show similar symptoms to those of past trauma have gone through a traumatic event. There is no cookie-cutter plan of care, and all patients must be properly assessed to determine what their plan of care will be (6).

Self Quiz
Ask yourself...
- How was the trauma informed approach born?
- What must change to prevent patient re-traumatization?
- What are two ways that an organization can change to a trauma informed care culture?
- Should all past trauma survivors be cared for in the same manner?
Impact of Trauma Informed Care
The impact of trauma-informed care on the patient and on the healthcare system as a whole cannot be overstated. By understanding that a great deal of the patients who seek out healthcare services have undergone a traumatic event and tailoring the assessment with that in mind, an organization can minimize the occurrence of re-traumatization.
When we understand how trauma has affected our patients’ lives, how they perceive the healthcare system and what their previous experiences within that system have been like, steps can be taken to ensure better outcomes within this population (1).

Self Quiz
Ask yourself...
- What are healthcare institutions trying to prevent through trauma informed care?
- How can healthcare facilities ensure better outcomes within the past trauma patient?
- What are two ways that nurses can help minimize re-traumatization?
Nursing Implications
In order for trauma informed care to be properly accepted and put into use in the healthcare setting, the culture must be transformed to be a trauma-informed culture. Nursing is with the patient around the clock and nurses have the ability to touch patient’s lives in the most impactful way.
Here are a few considerations that pertain to the healthcare team but when used by nurses have the ability to transform the patient’s environment into a true trauma informed care setting.
Introductions
Even if the nurse believes that the patient knows who they are, it is important for the nurse to reintroduce themselves with every interaction. The patient generally has many different members of the healthcare team entering their space throughout their stay. Team members tend to meld into one anonymous face to the patient; the nurse by introducing and reintroducing themselves and their role to the patient will not only foster an understanding of who does what, but they will empower the patient to be engaged and involved in their plan of care.
Body Language
Body language is important when caring for any patient. When caring for a patient who has experienced trauma, this becomes even more impactful. Open body language sets the stage for trust.
Trauma survivors may often feel a sense of being trapped or confined which may lead to an overall sense of powerlessness. Unintentional threatening body language magnifies these feelings and could bring on a re-traumatization episode. By contrast, non-threatening body language decreases the trauma center and leaves the patient calm and non-triggered.
Trauma informed care body language includes being at the patient’s level; commit to sit or raising the bed so that both patient and nurse are at the same level. Knowing the environment and deescalating trauma by the nurse positioning themselves properly in relation to the patient and the door; allowing for both to access so that the patient does not feel confined.
Anticipatory Guidance
Past trauma may have been unpredictable or an outright surprise. Verbally telling a patient what will be expected during their stay will reassure them even if the coming procedure or test may cause pain. Sharing who will be part of their care during their stay will also set them at ease. Knowing and understanding the expectation further empowers the patient to be involved in their plan of care.
The expectation, when known, decreases those feelings of surprise which could bring them back to that time of trauma.

Self Quiz
Ask yourself...
- Why should the nurse introduce themselves by name and role?
- How can the nurse’s body language affect the past trauma patient?
- What is incorporated in anticipatory guidance?
Permission
Touch can have an incredible impact on the patient who has experienced past trauma. Unwanted or inappropriate touch quite likely may have been a part of their traumatic experience. It can activate those traumatic memories and activate the re-traumatization cycle. Touch is also inevitable when it comes to the nurse/patient relationship.
What the nurse can control is when the touch occurs. Touch should always be preceded by the nurse explaining what they are going to do and asking for the patient’s permission to touch them. Asking permission puts the ball in the patient’s court and empowers them as they are now given a choice and are in control of their body and space.
Permission to touch the patient should never be assumed; permission should be asked every time the nurse needs to touch the patient.
Protect
In many cases, patients who have experienced trauma experienced it at the hand of someone that they know. Many times, the patient will not be alone in their room; family and friends are often present. Patient advocacy has always been the primary role of the nurse.
As part of being an advocate for the patient, the nurse should protect the privacy and safety of the patient. Asking those present in the room to leave prior to discussing the patient’s plan of care is a way to protect both privacy and safety. The patient may not feel safe asking visitors to leave their room especially if they may have been involved in the prior traumatic episode.
By asking visitors to leave, the nurse gives control back to the patient. In private, the nurse can ask who the patient is comfortable with remaining in the room. Once again, the patient is empowered.
Clear and Consistent
Realistic expectations are understood when given in clear and consistent language. This will also foster trust especially if the entire healthcare team is on the same page and vocalizing the same message, consistency. Using language that the patient understands is also paramount. Avoiding medical terminology and acronyms also builds trust as the patient knows that the nurse has made it their priority that the patient understands their plan of care.
Universal Precaution
Finally, trauma informed care needs to be a universal precaution regardless of if the patient’s past trauma history is known or not. By treating all patients as if they had experienced past trauma, those who have will be more apt to share the experience.
Also, nurses will be less likely to start the re-traumatization cycle by inadvertently triggering an episode. It will help treat the patient without relying on the patient to disclose something that they may not yet feel comfortable sharing. (3)

Self Quiz
Ask yourself...
- Why should the nurse ask permission to touch the patient?
- When should the nurse ask permission to touch the patient?
- What does universal precaution in terms of trauma informed care mean?
Resources
It is not easy to become a center where trauma informed care is practiced, it does not happen overnight. Trauma informed care is an intentional shift in culture at the facility and/or system level. Trauma informed training should be implemented, and the staff need to understand the “why” behind the training in order to buy-in.
Trauma informed care not only helps the patient to be empowered and prevent re-traumatization, but staff that have undergone past traumatic experiences can also be helped once a facility adopts this culture. This culture should be at the forefront of both staff and leadership minds. Staff meetings, unit huddles and any other opportunity where leadership actively communicates with staff should incorporate the messaging of trauma informed care.
Facilities should actively be hiring a trauma informed workforce. People from wide varieties of racial and cultural backgrounds should be on the interview panel. Questions pertaining to trauma informed care can and should be asked to pick up on skills and traits that will promote this culture.

A few environmental factors to create the trauma informed culture include keeping doors and common areas well-lit, keeping noise levels low and having warm, cozy colors as decoration in common areas.
Below are some websites that can be visited in order to help kickstart the culture of trauma informed care:
- https://TraumaInformedCare.chcs.org
- https://www.creatingpresence.net/
- https://www.chcs.org/resource/key-ingredients-for-successful-trauma-informed-care-implementation/
- https://store.samhsa.gov/product/SAMHSA-s-Concept-of-Trauma-and-Guidance-for-a-Trauma-Informed-Approach/SMA14-4884
(5)

Self Quiz
Ask yourself...
- What do staff need to understand to be participants in patient informed care?
- When should trauma informed care concepts be communicated to staff?
- How can facilities ensure that new hires are on board with trauma informed care?
- What are some environmental elements that facilities can apply to promote trauma informed care?
Conclusion
Though not a new concept, trauma informed care is essential to help patients who have had traumatic experiences navigate through the healthcare system. Trauma informed care empowers patients to take control of their care in collaboration with the healthcare team. Ultimately, the goal of trauma informed care is to prevent re-traumatization of the patient at the hands of the healthcare team.
The trauma background of any given patient is unknown when they arrive at the facility. It is the responsibility of the nurse to use trauma informed care to both assess the patient and create trust so that they will disclose the trauma. Once known, the team will be able to work together with the patient to prevent further trauma and have positive outcomes.
Conclusion
Though not a new concept, trauma informed care is essential to help patients who have had traumatic experiences navigate through the healthcare system. Trauma informed care empowers patients to take control of their care in collaboration with the healthcare team. Ultimately, the goal of trauma informed care is to prevent re-traumatization of the patient at the hands of the healthcare team.
The trauma background of any given patient is unknown when they arrive at the facility. It is the responsibility of the nurse to use trauma informed care to both assess the patient and create trust so that they will disclose the trauma. Once known, the team will be able to work together with the patient to prevent further trauma and have positive outcomes.
Nursing Care in Lewy Body Dementia
Introduction
Lewy body dementia is one of the more common causes of dementia. Currently it is the second most common dementia disorder following Alzheimer’s disease [2]. This condition is shown to affect more than 1.4 million people in the United States [1] [2]. Of dementia cases in older adults, Lewy body dementia is said to make up 5% of people with dementia [2]. Lewy body dementia is a disorder that progresses over time [1]. The progression of the disease differs between individuals and the severity of the symptoms [1].
On average an individual lives between five to eight years after diagnosis [1]. Currently there is not a cure for this disease [1]. This course will examine the causes of this disease, signs and symptoms patients might experience, diagnostic tests, types of management, and educational resources for family members. This course is designed to inform nurses about this common disease and to use this information in their daily practice to care for their patients.

Self Quiz
Ask yourself...
- What do you think is the most common form of dementia in the United States?
- How common is Lewy body dementia in other parts of the world?
- Is there currently a cure for Lewy body dementia?
- Why do you think Alzheimer’s disease is more common than Lewy body dementia?
Definition
Lewy body is an umbrella term that includes two separate diagnoses: Dementia with Lewy bodies and Parkinson’s disease dementia [5]. As these diseases progress, they develop together and are seen as one entity, not two separate conditions [4]. Lewy body dementia is a condition that involves neurocognitive disorders that include hallucinations, memory loss, behavior changes, and parkinsonism features [2]. This disease can also affect intellectual abilities and cause individuals to act out dreams during REM (rapid eye movement) sleep [2]. REM sleep behavior disorder sometimes may be experienced before any other symptoms are exhibited [2].
Lewy body dementia is known for a buildup of deposits of alpha- synuclein proteins called Lewy bodies [1]. Diagnosing this condition can be difficult because many neurological disorders have similar symptoms. Lewy body dementia and Parkinson disease dementia are very similar. For a diagnosis of Lewy body dementia, there must be a cognitive impairment with motor symptoms occuring in less than 12 months [3]. Parkinson’s disease dementia affects an individual’s movements; cognitive symptoms appear later (greater than one year) [5].
Lewy body dementia is known to affect older adults generally between the ages of 50 and 85 [2]. This disease is said to be underdiagnosed due to a large number of diagnoses occuring post-death during autopsies [4]. Several medications used to treat neurocognitive and behavioral symptoms in other conditions can worsen the symptoms of Lewy body dementia [4]. Therefore, an accurate diagnosis can impact an individual’s quality of life.

Self Quiz
Ask yourself...
- What are the two forms of Lewy body dementia?
- What are the differences between dementia with Lewy bodies and Parkinson’s disease dementia?
- Why is it difficult to diagnose Lewy body dementia?
Epidemiology
Lewy body dementia affects a significant number of individuals in the United States. This condition is found more often in men than women [4]. Age is thought to be the greatest risk factor for an individual developing this disease [4]. An individual who has a family history of Lewy body dementia and Parkinson’s disease is at a higher risk for developing this condition [3].
Lewy Body dementia is more widespread in European, Asian, and African ethnic groups [3]. In individuals with Parkinson’s disease, the incidence of Parkinson’s disease dementia is said to be around 25-30% [4]. The incidence of individuals with Parkinson disease developing this type of dementia after having Parkinson’s for more than 20 years increases to around 83% [4].


Self Quiz
Ask yourself...
- What is the greatest risk factor for developing Lewy body dementia?
- Are there certain ethnic groups that have a higher rate of Lewy body dementia?
- Which gender is Lewy body dementia prominent in?
Pathophysiology
There is a buildup of alpha- synuclein proteins that causes neurons to die in Lewy body dementia [2] [5]. As mentioned above in this course, this buildup of proteins is called Lewy bodies. The death of neurons that produce dopamine result in problems with movement, cognitive impairment, a decline in cognition, and sleep disturbances [4]. In Lewy body dementia there is a deficiency of acetylcholine [3]. There is also a decrease in acetylcholine with Alzheimer’s disease, but the deficiency is greater with Lewy body dementia [3]. The decrease in neurons that produce acetylcholine causes memory loss and learning impairment [4].
The mutation of synuclein alpha and synuclein beta genes can cause dementia with Lewy bodies [2]. Mutations in apolipoprotein E and GBA genes are potential risk factors for developing the disease [2]. There have been cases where a buildup of alpha-synuclein was found during an autopsy, but the individual did not show any clinical signs of Lewy Body dementia when alive [4]. The function of these proteins in this condition is still undetermined [5].

Self Quiz
Ask yourself...
- What are considered Lewy bodies?
- What other disease besides Lewy body dementia has a decrease in acetylcholine?
- What symptoms are a result of destruction of neurons that produce dopamine?
Etiology
The exact cause of Lewy body dementia is still unknown. While research is ongoing and new developments are occuring, the specific cause has not been determined. The accumulation of Lewy bodies cause cell death which causes symptoms, however, the reason for the buildup of Lewy bodies is still under research [5]. As mentioned earlier, there are specific gene mutations that have been shown to increase the likelihood of producing altered alpha- synuclein proteins, in turn causing them to clump together (forming the Lewy bodies) [2].
The mutation of the GBA gene interferes with the function of lysosomes, which can affect the breakdown of the alpha- synuclein proteins, causing the proteins to accumulate [2]. The e4 allele type of the APOE gene has been shown to increase the risk of developing Lewy body dementia [2]. These clumps of Lewy bodies form inside and outside of neurons in different areas of the brain, where they can alter the function of the cell and can cause the cell to die [2].
The neurons that develop the neurotransmitter dopamine are especially impacted by these clumps of Lewy bodies, which was addressed earlier in this course [2]. Further research is required to find out why these Lewy bodies develop in certain individuals. Currently, age, genetics, and environmental factors are some of the greatest risk factors [3].

Self Quiz
Ask yourself...
- What is the cause of Lewy body dementia?
- Why is age a risk factor for developing this disease?
- What does the buildup of Lewy bodies do to cells?
Clinical Signs and Symptoms
Lewy body dementia is a progressive disorder - the signs and symptoms worsen over time. The symptoms that are more common are sleep changes, impaired behavior, movement, and cognition [5]. Research shows that the location of Lewy body accumulation impacts the clinical signs and symptoms the individual experiences [3]. If Lewy bodies develop in the brainstem and cerebral cortex first, the condition is called dementia with Lewy bodies, and the onset of the dementia is early [3]. If Lewy bodies accumulate in the brain stem and then develop into the cerebral cortex as time passes, the onset of dementia appears later, and this condition is called Parkinson’s disease dementia [3].
Rapid Eye Movement Sleep Behavior Disorder
Rapid eye movement (REM) sleep behavior disorder is sometimes the first clinical sign of dementia with Lewy bodies [2]. Individuals with this disorder move and talk while dreaming in their sleep [2]. The movements can be violent and cause the individual to fall out of bed [5]. Individuals may kick, punch, and scream in REM sleep (the second half of their sleep) [4]. REM sleep behavior disorder is seen in 76% of patients with dementia with Lewy bodies [4].
This disorder can cause fractures and contusions in some individuals resulting from falling out of bed [4]. This can not only affect the individual, but also the sleep partner of the patient [4]. In some cases, separate sleeping arrangements are needed for the safety of the individual and their sleeping partner. A questionnaire by the patient and sleep partner is part of the diagnosis of REM sleep behavior disorder [14]. If the individual does sleep next to someone, this questionnaire can be helpful as most of the time the patient cannot recall the events while asleep [14]. Video polysomnography is required for a complete diagnosis of this disorder [14]. These events while asleep must be repeated to meet the diagnostic criteria [14].
Other Sleep Disorders
Other disorders of sleep include sleepiness in the daytime, restless leg syndrome, confusion when awakened, and obstructive sleep apnea [4].
Visual Hallucinations
Visual hallucinations are present in about 80% of individuals with Lewy body dementia [1]. Visual hallucinations are a core clinical symptom of dementia with Lewy bodies [4]. They are more common in women than in men [4]. Individuals are aware of these hallucinations and can tell others what they experienced [4]. Visual hallucinations are vivid to individuals and have been said to range from people walking around the house to seeing people that have died sitting next to them [6]. During the beginning stages of the disease, the hallucinations do not seem to affect the patient as much as when the disease progresses [6]. Patients are said to be afraid of these hallucinations in the later stages of the disease [6]. Nonvisual hallucinations are less common, however can occur in some patients [1]. These hallucinations include smelling or hearing something that is not in their surroundings [1].
Fluctuation in Cognition
Fluctuation in cognition is also a clinical sign that is associated with dementia with Lewy bodies [4]. This symptom includes changes in attention, concentration, and alertness [5]. These changes are random and can differ day-to-day [1]. Symptoms can include delirium, and mimic symptoms that are caused by metabolic diseases, which can further the difficulty with identifying the correct diagnosis [4]. To diagnose dementia with Lewy bodies, one of the episodes must be confirmed [4]. These fluctuations can be present in other forms of dementia in their later stages but when present in earlier stages, they point to dementia with Lewy bodies [4].
Memory loss that impacts activities of daily living can be found in later stages of Lewy body dementia [1]. Memory loss early on is more often a characteristic sign of Alzheimer’s dementia [1]. Confusion about the individual’s whereabouts, and inability to multitask can also occur in dementia with Lewy bodies [4].
Problems with Movement
Problems with movement are signs of Lewy body dementia. Bradykinesia (slow movements) and rigidity occur in about 85% of individuals with dementia with Lewy bodies [4]. Tremor at rest is less common in individuals with this condition [4]. Loss of coordination and difficultly swallowing can occur [1]. Problems with movement greatly increase the risk of falls for these individuals [4]. This can place strain on the individual’s caregivers [4].
Autonomic Dysfunction
Autonomic dysfunction can be present in dementia with Lewy bodies and Parkinson’s disease dementia. This symptom is seen in about 90% of patients with Lewy body dementia [4]. The symptoms that result from autonomic dysfunction can be constipation, urinary incontinence, orthostatic hypotension, erectile dysfunction, and dizziness [1] [4]. Orthostatic hypotension appears as early as five years prior to the diagnosis of Lewy body dementia [4]. Syncope and falls are usually the result of orthostatic hypotension [4]. Constipation can also occur earlier in the disease process [4].


Self Quiz
Ask yourself...
- What is REM sleep behavior disorder?
- Are visual hallucinations common in Lewy body dementia?
- What does cognitive fluctuation mean?
- What are symptoms of autonomic dysfunction seen in dementia with Lewy bodies?
Diagnostic Tests and Evaluations
Throughout this course, it has been mentioned that Lewy body dementia is significantly underdiagnosed. Individuals are usually diagnosed as the disease progresses due to the symptoms that overlap with other forms of dementia and other neurological and psychiatric disorders [3]. An autopsy of the brain after death is one of the only ways to have a conclusive diagnosis of Lewy body dementia [16]. There are certain diagnostic criteria and diagnostic tests that are used to diagnose an individual with Lewy body dementia.
Diagnosis by Symptoms
Lewy body dementia is probable when an individual experiences dementia and two main features of the disease. Lewy body dementia is a potential diagnosis if the individual experiences progressive dementia and one main feature of the disease [3]. As discussed in the clinical signs and symptoms section of this course, key features of Lewy body dementia are cognitive fluctuations, dementia that progresses, problems with movement (signs of parkinsonism), REM sleep behavior disorder, and visual hallucinations [3] [16].
Timing of symptoms is relevant for distinguishing between the two forms of Lewy body dementia [3]. Currently healthcare providers use the time span of one year to distinguish the two forms [3]. If dementia occurs within one year of the appearance of movement problems, then a diagnosis of dementia with Lewy bodies is used [3]. If an individual is diagnosed with Parkinson’s disease and starts experiencing symptoms of dementia more than one year after their Parkinson’s diagnosis, then Parkinson’s disease dementia is used [3]. Some indicative biomarkers in addition to clinical symptoms are used in diagnosis [4]. Some of these biomarkers can be found in cerebral spinal fluid (CSF) and are still under research [4].
Cognitive Tests
Cognitive testing can be used to show the cognitive impairment of patients with Lewy body dementia [3]. The Mini-Mental State Examination can be used as an initial screening test [4]. This exam tests cognitive function by focusing on concentration, orientation, and memory [15]. This test can be limited since symptoms of these patients can fluctuate day to day [3]. Another cognitive function test is the Montreal Cognitive Assessment (MoCA) [15]. Providers do not usually diagnose based on a single test; instead, they use the results to look for other signs and symptoms of Lewy body dementia [4].
Imaging Tests
There are certain imaging tests that can help with diagnosis and distinguishing between other dementia disorders. A single-photon emission computerized tomography (SPECT) scan can help support a diagnosis [16]. This is a nuclear scan that can sense radioactivity [16]. If the SPECT scan shows a reduced dopamine transporter uptake in the basal ganglia, this can be a sign of Lewy body dementia [16]. This will separate the diagnosis between Lewy body dementia and Alzheimer’s disease [4]. Performing this scan alone will not lead to a possible diagnosis of Lewy body dementia; however, in combination with other diagnostic tests, the scan can lead to a more certain diagnosis [4]. Results from these scans can appear normal initially, and the scan may need to be repeated [4].
An iodine- MIBG myocardial scintigraphy can be performed to support Lewy body dementia [16]. This would show decreased communication of cardiac nerves [16]. The results may be skewed by heart disease or certain drugs [4]. A CT or MRI may be used but these imaging tests can present mixed results [4]. With Alzheimer’s disease, significant atrophy is seen in the medial temporal lobes [4]. There is normally minimal atrophy in Lewy body dementia [4].
As mentioned earlier in the course, video polysomnography is needed for the diagnosis of REM sleep behavior disorder [14]. This sleep study without the loss of muscle tone can also point towards a diagnosis of Lewy body dementia as REM sleep behavior disorder has now moved to a key feature of this disease [14].

Self Quiz
Ask yourself...
- What types of imaging tests can be used in the diagnosis of Lewy body dementia?
- Why are cognitive tests used in diagnosis of this disease?
- What criteria are needed for a probable diagnosis of Lewy body dementia?
- Can the cost of diagnostic imaging lead to a reduction in diagnosing Lewy body dementia?
Case Studies
Case Study #1
A 74-year-old male presents to his primary care provider after his wife reports abnormal behavior over the past several months. His wife reports the patient kicks and screams during sleep. The patient reports seeing little people walking around the living room during the day. The wife states the patient some days will fall asleep throughout the day while completing activities. The patient states difficulty walking and muscle stiffness.
The wife states last week the patient was supposed to go to the local grocery store to buy milk. After two hours passed, the wife called her husband as she was worried about him. He states he got lost finding the grocery store and did not know where he was. The wife said she had to drive to find her husband and bring him home. The patient also reports dizziness when standing. After the nurse obtained an orthostatic blood pressure, the patient was positive for orthostatic hypotension.
- Which form of dementia is the patient most likely experiencing?
- What type of symptoms is the patient experiencing that would point to that diagnosis?
- What diagnostic tests or evaluations should the patient undergo?
- What types of supportive treatment should the healthcare provider include in the treatment plan for this patient?
Case Study #2
A 70-year-old female presents to the emergency department via EMS after falling at home. The patient’s daughter called 911 after finding her on the floor when going to visit her. Upon arrival at the emergency department the patient is oriented to self. The patient does not know where she is or what happened to precipitate the fall. The patient has a past medical history of hypertension, diabetes type II, and Parkinson’s disease.
The patient was diagnosed with Parkinson’s disease two years prior. The daughter states the patient has been forgetful lately and not acting like herself. The daughter reports that her mom’s behavior is different from day-to-day. An MRI and the National Institutes of Health Stroke Scale (NIHSS) are used to rule out a cerebrovascular accident. A complete blood count (CBC), a complete metabolic count (CMP), and urinalysis are obtained. The patient suffered a contusion to her right cheek and a right radius fracture. The patient states that she sees figures dancing in the room and smells popcorn. The patient appears to be frightened by the hallucinations. The patient’s daughter states for the last six months the patient has had difficulty swallowing and a reduced appetite.
- Which form of dementia is the patient most likely experiencing?
- What would the MRI of the patient most likely show?
- What clinical signs of dementia is the patient exhibiting?
Management
Currently there is not a cure for Lewy body dementia, only supportive treatment. The management of this disease involves a multifaceted approach, including therapies, pharmacological treatments, and family support.
Therapies
Specific therapies can help with symptom management and help improve the individual’s quality of life. Occupational therapy can help improve a patient’s ability to complete activities of daily living. Speech therapy can help with swallowing coordination and improve the clarity and volume of speech [5]. Physical therapy can aid patients with problems with movement [5]. Mental health counseling can help individuals and their families with managing behaviors and their emotions [5].
Medications
Pharmacotherapy can help with supportive treatment but can also worsen symptoms if certain medications are taken. Below are some examples of medications that are used by patients with Lewy body dementia.
- Cholinesterase Inhibitors are used to help cholinergic activity to improve cognitive function [6].
- Rivastigmine was one of the first of these drugs to be tested [6]. Patients were noted to have improved on their cognitive exams [6]. It is also shown to reduce hallucinations and lessen anxiety [6]. This class of drugs has been said to improve the quality of life for some patients [4].
- Donepezil and Galantamine are also used to reduce dementia symptoms of hallucinations [6]. These drugs were initially targeted for patients with Alzheimer dementia, however, they are effective for individuals with Lewy body dementia as well [3]. A study was done stating even if there is not a sign of cognitive improvement, this should not be the criteria to stop the medication as this medication has been proven to protect the individual from further impairment of cognition [4].
- Atypical Antipsychotics are prescribed to patients that are not seeing a reduction of symptoms while on cholinesterase inhibitors [3]. These types of drugs are seen as controversial due to the many adverse effects that have been seen in patients [4]. Drugs such as haloperidol and olanzapine should be avoided in patients with Lewy body dementia as they can cause neuroleptic malignant syndrome (a life-threatening condition) [5]. Quetiapine, clozapine, pimavanserin, and aripiprazole are atypical antipsychotic drugs that can be used to improve agitation and help prevent cognitive fluctuations [5].
- Carbidopa-Levodopa can be used in patients to manage problems with movement [3]. This medication can cause side effects and can result in hallucinations, delusions, and increase confusion [3]. Providers should begin with low doses of this medication [3].
- Clonazepam is a benzodiazepine that can lessen the REM sleep behavior disorder that patients with dementia with Lewy bodies can experience [5]. Between 33-65% of patients with REM sleep behavior disorder can experience an injury while sleeping [5]. This medication has been proven to decrease injuries that occur during sleep [5]. Clonazepam can adversely affect individuals with gait disorders or sleep apnea [5].
- Melatonin is a hormone that can be used for patients that are affected by REM sleep behavior disorder (5). Studies have shown that the use of melatonin lessened the frequency and the severity of symptoms associated with REM sleep behavior disorder [5]. Melatonin can have side effects such as headaches in the morning, sleepiness during the day, and hallucinations [5].
- Memantine is used to treat dementia symptoms [5]. This medication is an NMDA receptor antagonist that stops effects of glutamate in the brain [5]. Memantine has been shown to improve symptoms of patients early in the disease [5].


Self Quiz
Ask yourself...
- What type of therapies are used in management of Lewy body dementia?
- What class of drugs are used to help improve cognitive function?
- What are some medications that should be avoided in patients with Lewy body dementia?
- Why is melatonin used in patients with Lewy body dementia?
Nursing Care
As mentioned before, there is not a cure for Lewy body dementia. Caring for patients with Lewy body dementia includes supportive treatment. Nurses can play a significant role in caring for these patients and providing the family with support. Home health nurses can help with frequent assessment of the patient and their environment [3]. Environmental changes may be needed to protect the patient from falls and other accidents. Home health nurses can assess the type of assistance the patient would benefit from.
Nurses can aid the family by providing education to assist in how to care for the patient. Family members and caregivers must be aware of the changes in behavior, fluctuations in cognition, and hallucinations that the individual might experience [3]. Nurses must also provide education to the caregiver of the patient on the side effects of certain medications, as they can affect an individual with this disease [7].

Self Quiz
Ask yourself...
- Are there any modifications that nurses must apply to care for patients with Lewy body dementia?
- Whose role is it to educate patients and their family members?
Family Support
Lewy body dementia is growing in recognition; however, many people might not be aware of this condition and the disease process. Family members need support from health care professionals to better care for their loved ones. Support can come in the form of education and preparing the family for the symptoms the individual may experience. The cognitive function of patients with this disease can be very limited [3]. Family members must be educated on monitoring the individual closely to promote safety [3]. These individuals are at a high risk for falling and developing aspiration pneumonia (due to swallowing difficulties) [3]. Family members should be educated in preparing for an emergency.
Individuals with Lewy body dementia may need care and the family needs to know how to inform health care providers of their specific needs. It is important to educate family members that their roles in their past relationship with the patient will likely change due to the disease process. To prevent caregiver burnout, family members must be aware of their limitations and know when they need help [7]. Modifying the patient’s home may be needed for patient safety [3]. Each patient may have specific needs and family members should know what modifications may be necessary [3].

Self Quiz
Ask yourself...
- What type of support do you feel is important to give family members of loved ones with this disease?
- What should nurses include in education for fall risk safety for family members while the individual is at home?
- Can nurses help to prevent caregiver burnout?
Prognosis
The prognosis of Lewy body dementia can be viewed as poor. As mentioned briefly earlier in this course, this disease is progressive and after diagnosis, the life expectancy is five to eight years [3]. The range of expectancy has also been attributed to delay in diagnosis, which can further delay supportive treatment to improve quality of life for the individual [3]. Patients can die from complications from the disease. Complications can include cardiac complications, falls, adverse effects from medications, pneumonia, and suicide [3].
Compared to Alzheimer’s dementia, the risk of hospitalization or death due to respiratory infections is higher in patients with Lewy body dementia [8]. The median age at death is said to be similar between patients with Alzheimer’s dementia and Lewy body dementia [8]. The life expectancy from diagnosis to death is shorter in patients with Lewy body dementia [8]. The patient’s environment has been shown to play a role in the increased risk of mortality [8]. Patients in nursing homes have been shown to have a higher risk of mortality [8]. Caregivers can decrease the risk of complications by educating themselves on this disease and keeping their loved ones safe.

Self Quiz
Ask yourself...
- What are some complications of Lewy body dementia?
- How can the patient’s environment increase the risk of mortality with this disease?
- Why do you think there is delay in diagnosis with Lewy body dementia?
Resources for Family Support
Lewy body dementia is a diagnosis that can affect all aspects of an individual’s life and their family members lives. As nurses we must provide support for family members so they can better care for their loved ones and improve their quality of life. As recognition of this condition grows, family support resources are increasing. The Lewy Body Dementia Association is a nonprofit organization that raises awareness and provides support for families with individuals that suffer from Lewy body dementia [10]. Support groups can be found on their website to help families across the country in their local area [10].
The Lewy Body Dementia Association was started by caregivers of individuals with this condition. They also focus on education and research into the disease. This association is a resource for family members [10].
Another resource for family members is The Lewy Body Dementia Resource Center. This is a nonprofit charitable organization that gives assistance and support to those who care for someone with Lewy body dementia [9]. This organization was founded by caregivers of individuals with Lewy body dementia. They have a support phone line that is available seven days a week to answer questions [9]. They also promote research and early diagnosis of this disease [9].

Self Quiz
Ask yourself...
- How can support of family members improve the quality of life of a patient with Lewy body dementia?
- What are some examples of resources for caregivers of individuals with Lewy body dementia?
- Can providing resources to the community help with early diagnosis of this disease?
Research Programs
Lewy body dementia is the second most common form of dementia in the United States [4]. This illness is thought to be underdiagnosed and commonly mistaken for other neurological disorders [3]. Research on Lewy body dementia can decrease the time it takes to diagnose a patient, and can help with management of the condition.
The National Institute of Neurological Disorders and Stroke provides support for a variety of research endeavors for Lewy body dementia [11]. In 2021 The National Institute of Health spent $93 million dollars on Lewy Body dementia research [11]. One program is the Biomarkers for Lew body dementias program. This program aims to increase clinical data collection from patients with this condition, find biomarkers to expand further research, and allow access to the science community to help with further studies [11]. Another program is the Parkinson’s Disease Biomarkers Program. This program’s purpose is to collectively research with healthcare professionals, patients and family members, and technology professionals to increase biomarker research [11].
Biomarker research has been increasing in Lewy body dementia. A biomarker is a feature that can specifically indicate a certain disease [12]. For quite some time there were not any identified biomarkers for Lewy body dementia. There are certain biomarkers that aid in distinguishing Alzheimer’s disease from Lewy Body dementia [13]. These biomarkers can be assessed through imaging or in cerebral spinal fluid [13]. Currently these biomarkers are only helpful if another disease is doubtful [13].
New biomarkers are needed to separate Alzheimer’s dementia from Lewy Body dementia and other neurological disorders [13]. Biomarkers that can help with early diagnosis would be beneficial for early treatment [13].


Self Quiz
Ask yourself...
- Why is researching biomarkers important for early diagnosis of Lewy body dementia?
- Is there more research conducted on Alzheimer dementia than on Lewy body dementia?
- What are some organizations that promote research for this disease?
Conclusion
Lewy Body dementia affects 1.4 million Americans [2]. The disease is underdiagnosed and often diagnosed incorrectly. Incorrect diagnoses can lead to worsening of symptoms and the administration of drugs that can lead to adverse effects.
Educating healthcare providers and the community about Lewy body dementia can improve quality of life for individuals with the disease. As nurses, we must be informed about this disease to better educate our patients and their caregivers, and to know how to advocate for our patients.
Understanding Lupus Nephritis
Introduction
A lupus diagnosis and the complications that arise can be devastating for patients. Nurses are often looked to for support and answers, so it is important to educate ourselves on these serious conditions. Lupus nephritis (LN) is considered one of the most severe organ manifestations of the autoimmune disease systemic lupus erythematosus (SLE). Essential knowledge on lupus nephritis includes the defining features, epidemiology, pathophysiology of normal kidney function and lupus nephritis, clinical presentation, and treatments.
Lupus Nephritis
Lupus nephritis (LN) is an organ manifestation of the autoimmune disease systemic lupus erythematosus (SLE). The cause of lupus erythematosus is not known. Researchers suggest a genetic predisposition, but a genetic link has not been identified (2). This is a difficult reality, as patients and healthcare providers usually hope for a why. We will discuss the definition, prevalence, pathophysiology, manifestations, clinical diagnosis guidelines, and treatment regimens for LN.
Definition
Lupus nephritis (LN) is considered a condition and a manifestation. LN is one of the most severe organ manifestations of the autoimmune disease systemic lupus erythematosus (SLE). LN is a form of glomerulonephritis, which is inflammation of the glomeruli (the tiny filters within the kidneys). This inflammation causes significant imbalances within the body due to impaired kidney function.
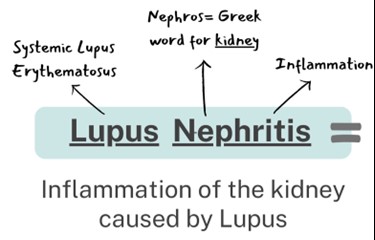
Overview of Systemic Lupus Erythematosus (SLE)
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by a loss of immune tolerance of endogenous nuclear material, which leads to systemic autoimmunity that may cause damage to various tissues and organs (1). Essentially, the damage to DNA structures causes the body’s immune system to be incidentally programmed to attack its own tissue. There are two types of lupus: systemic lupus erythematosus and “discoid” lupus erythematosus. SLE is systemic, meaning it can affect almost any organ system or tissue and presents in different manifestations impacting the skin, joints, kidneys, and brain (2). “Discoid” lupus erythematosus only affects the skin tissue. Our focus will be on systemic lupus erythematosus (SLE) as we gain a deeper understanding of lupus nephritis.
The causes of SLE are unknown but many attribute it to genetic, environmental, and hormonal factors. SLE is hard to diagnose because the symptoms are often mistaken for those of other conditions. There is no cure for SLE, but symptoms can be managed. SLE presentation and prognosis are highly variable, with symptoms ranging from minimal to life-threatening. Patients with lupus may experience periods of exacerbation of symptoms, sometimes called 'flares', as well as periods of remission. SLE is associated with substantial morbidity and mortality, particularly caused by renal and cardiovascular disease and infections. LN is considered one of the most severe manifestations of SLE.
SLE can be compared to a guard dog intended to protect your home. The guard dog (immune system) protects you from unwanted intruders (infection), but also bites friends, family, and the mailman (your own organ tissue)!

Self Quiz
Ask yourself...
- Have you cared for a patient with autoimmune disorders impacting the skin or joints?
- Are you familiar with other autoimmune conditions?
- How are systemic and focal conditions different?
- Can you list the two types of lupus?
Epidemiology and Statistical Evidence of Lupus Nephritis
Systemic lupus erythematosus has an estimated prevalence of about 10–150 per 100,000 persons (2). However, a large number of people could be undiagnosed due to being asymptomatic or the symptoms mistaken for other diseases. An average of 40% of SLE patients develop lupus nephritis (LN). Those diagnosed with SLE at a younger age are at a higher risk of developing LN and other complications (1).
SLE in general is more prevalent in women, especially women of reproductive age, than in men; the ratio is 9:1 (1). Therefore, 90% of SLE cases are women. However, men who have been diagnosed with SLE more commonly develop LN than women with SLE. Numerous studies have also found that the prevalence of LN in patients with SLE is higher in African American, Hispanic, and Asian populations (1). The impact of SLE disproportionately affects children and adults living in poorer geographic areas (8).
Within 10 years of the initial SLE diagnosis, 5–20% of patients with LN develop end-stage kidney disease and the multiple comorbidities associated with immunosuppressive treatment (1). Mortality in LN is quite variable ranging in between 15% and 25% (6). It is important to remember that the treatments are also very risky because it is difficult to balance the risks and benefits of suppressing the immune system. LN is a topic of significant research, so nurses can have a meaningful impact in raising awareness and encouraging hope for more advanced treatment development.

Self Quiz
Ask yourself...
- Can you name the population at greatest risk for developing SLE?
- Do you think all ethnicities are impacted equally?
- Do you think men and women are impacted equally when developing SLE and LN?
- Have you ever cared for a patient with systemic lupus erythematosus? If so, what were specific problems they faced?
Normal Kidney Function
The kidneys have several life-sustaining functions. The kidney serves to maintain fluid and chemical homeostasis and to contribute to hemodynamic stability (3). The renal tubules of the kidneys have unique and vital roles. Daily urine output is about 1–2 L, and over 98% of the glomerular filtrate is reabsorbed by the renal tubules (3).
There is a delicate balance and interdependency between the kidneys and other organs. For example, the kidneys produce hormones that help regulate blood pressure and control calcium metabolism, the kidneys also release a hormone that stimulates red blood cell production. A simple and fun mnemonic formula to help you remember the vital functions: A WET BED.
A WET BED: Functions of the Kidneys
A - controlling ACID-base balance
W - controlling WATER balance
E - maintaining ELECTROLYTE balance
T - removing TOXINS and waste products from the body
B - controlling BLOOD PRESSURE
E - producing the hormone ERYTHROPOIETIN
D - activating vitamin D
Controlling acid-base balance
- Our bodies always have a state of delicate equilibrium among the acids and bases, which has a parameter known as pH.
- The kidneys excrete or retain acids and bases when there is an excess or lack of them.
- The normal pH of the blood is 7.35 to 7.45.
Controlling water balance
The kidneys regulate the volume of urine produced and adapt to one’s hydration level to maintain water balance.
Maintaining electrolyte balance
The kidneys filter specific electrolytes from the blood, return them back into circulation, and excrete excess electrolytes into the urine. Kidneys maintain electrolyte balances like sodium and phosphate.
Removing toxins and waste products from the body
The kidneys remove water-soluble waste products and toxins and excrete them in urine.
Controlling blood pressure
The kidneys produce an enzyme called renin, which converts the angiotensinogen produced in the liver into angiotensin I, that is later converted in the lungs into angiotensin II. Angiotensin II constricts the blood vessels and increases blood pressure. Another way the kidneys help reduce elevated blood pressure is they produce more urine to reduce the volume of liquid circulating in the body to compensate.
Producing the hormone erythropoietin
The kidneys produce a hormone called erythropoietin, which aids in the creation of more red blood cells (erythrocytes), which are vital for the transport of oxygen throughout all the tissues and organs.
Activating vitamin D
The kidneys transform calcifediol into calcitriol, the active form of vitamin D.

Self Quiz
Ask yourself...
- What are ways to help remember the major functions of the kidneys?
- How do the kidneys regulate and maintain electrolyte balance?
- Can you list examples of how electrolyte imbalances affect various organ functions? (example: cardiovascular system)
- What are some ways the kidneys help to regulate blood pressure?
Anatomy and Physiology of the Kidneys
It is important to review the anatomy and physiology of the kidneys. The urinary system as a whole is composed of two kidneys, a pair of ureters, a bladder, and a urethra. The kidneys are located at the back of the abdominal wall and at the beginning of the urinary system. The size of each kidney is dependent on age, sex, and height, but the average length is approximately 10–12 cm, and the right kidney may be slightly smaller than the left kidney (3). The kidneys are made up of nephrons, which are microscopic structures composed of a renal corpuscle and a renal tubule.
The average human kidney is composed of approximately one million individual functioning nephrons, each containing a single glomerulus or filtering unit (3). The function of filtration is accomplished by three major components of nephron activity: (1) glomerular filtration, (2) tubular reabsorption, and (3) tubular secretion. These components respond to factors including renal blood flow, neuroendocrine effects, and the fluid and nutrient supply to the body.
Vascular Structure of the Kidneys
The kidneys are perfused with 1.2 liters of blood per minute, which represents about 25% of the cardiac output (3). From the abdominal aorta, the main renal artery carries blood into the kidney and then branches to segmental arteries, then to interlobar arteries, then branches to arcuate arteries, followed by branching to interlobular arteries, and finally onto afferent arterioles (3). Vascular resistance in the kidney is low when compared to other vascular beds within the body.
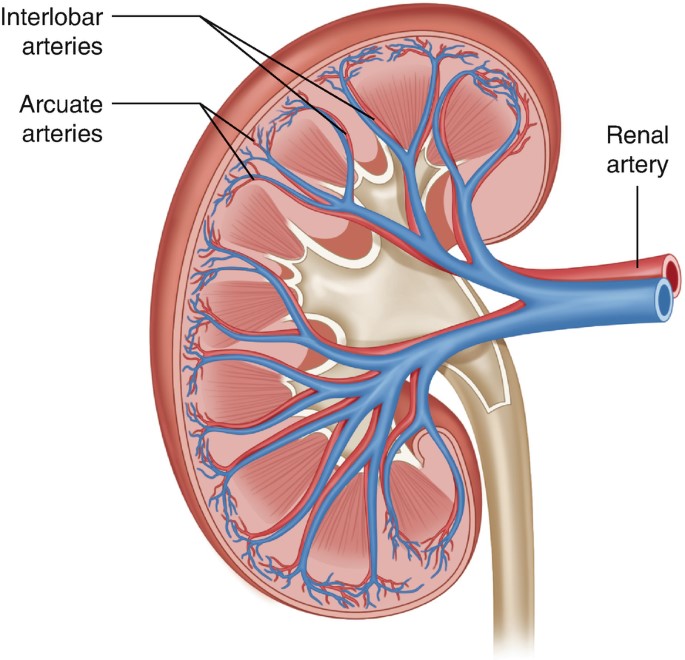
Figure 2. Vascular Structure of the Kidneys (3)

Self Quiz
Ask yourself...
- Can you explain the major functions of the kidneys?
- How would you describe the vascular structure of the kidneys?
- Are you familiar with focused physical assessment techniques for assessing peripheral edema?
- Have you ever cared for a patient with impaired renal function?
Pathophysiology of Lupus Nephritis

Have you ever played dominos? If aligned properly, the domino effect will rapidly cause a consecutive reaction. The immune response can be compared to this domino effect. One cellular action will cause the response and activation of many other cells. A perceived foreign body activates certain immune responses. In most cases, this maintains life. In some cases, it is harmful to vital tissue.
An autoimmune response to the renal system involves the T- and B-cell interactions stimulating interstitial plasma cell generation in the kidney; interstitial tissue leads to restricted autoantibody-producing plasma cells (6). This cascade of inflammatory response is facilitated by the production of interferon-α (IFN-α), which augments autoreactive B-cell activation and its reciprocal interaction in T-cell activation. This prolonged local injury and inflammation attracts neutrophils that try to help alleviate this inflammation, but the sustained local injury leads to neutrophil apoptosis (cell death), which further causes local injury. This injury further augments the inflammatory response by enhancing the intrarenal autoimmunity and inflammation, leading to kidney tissue injury (6).
Lupus nephritis is considered a type-3 hypersensitivity reaction. A hypersensitivity reaction is an inappropriate or overreactive immune response to an antigen. Symptoms typically appear when an individual has had a previous exposure to the antigen. Hypersensitivity reactions can be classified into four types (9).
- Type I - IgE mediated immediate reaction
- Type II - Antibody-mediated cytotoxic reaction (IgG or IgM antibodies)
- Type III - Immune complex-mediated reaction
- Type IV - Cell-mediated, delayed hypersensitivity reaction
In type III hypersensitivity reactions, antigen-antibody aggregates called "immune complexes” are formed. When someone has lupus, a number of DNA are damaged and have cell death, which exposes parts of the nucleus in the cell, and parts of the nucleus are recognized by the immune system as “nuclear antigens.” Remember, the immune system attacks antigens. The antigen-antibody complexes are transported by the blood and are deposited in various tissues, such as the kidneys.
When the complexes are deposited, it initiates the recruitment of inflammatory cells (monocytes and neutrophils) that release lysosomal enzymes and free radicals at the site of immune complexes, causing damage to that tissue (9). Examples of tissues that it may deposit in include skin, joints, blood vessels, or glomeruli. In the case of LN, the site of damage is the glomeruli of the kidneys, and it can have a disastrous impact.

Self Quiz
Ask yourself...
- Can you describe the differences between the types of hypersensitivity reactions?
- How would you describe the composition of the antigen-antibody complexes?
- Can you name types of inflammatory cells?
- Can you think of reasons the glomeruli of the kidneys may be a deposit site for free radicals and antigen-antibody complexes?
Clinical Presentation
The clinical manifestations of LN can be unpredictable and very different among patients. Patients may present with no symptoms at all, while other patients may have significant proteinuria progressing to acute renal failure. Understanding the disease and its progress is vital for nurses to provide optimal care and education to the patient. Remember, these patients may have signs and symptoms from their lupus already, so isolating renal impairment is essential.
Signs and Symptoms
Signs and symptoms of systemic lupus erythematosus depend on the body systems that are affected by the disease. Systemic symptoms include fatigue, malaise, weight loss, anorexia, and fever. The patient may report musculoskeletal symptoms, including joint and muscle pain, joint swelling and tenderness, hand deformities, and skin lesions such as the characteristic “butterfly rash” or maculopapular rash (small, colored area with raised red pimples). Other symptoms stem from the central nervous system (visual problems, memory loss, mild confusion, headache, depression).
It is important for the nurse to establish a history of symptoms related to the hematological system (venous or arterial clotting, bleeding tendencies), cardiopulmonary system (chest pain, shortness of breath, lung congestion), or gastrointestinal system (vomiting, difficulty swallowing, diarrhea, and bloody stools). To differential LN, it is important to focus on specific function impairment and manifestations arising from the kidneys (1).
Nephritic symptoms related to hypertension and poor kidney function:
- Peripheral edema
- Headache and dizziness
- Nausea and vomiting
Nephrotic symptoms related to proteinuria:
- Peripheral or periorbital edema
- Coagulopathy
Patients may report the following:
- Foamy urine
- Blood in the urine
- Dark urine
- Changes in the frequency of urination
- Weight gain and swelling, including the legs and hands
Classifications of Lupus Nephritis
There are six classifications of lupus nephritis:
- Class I: Minimal mesangial
- Prevalence 10-25% of people with lupus (SLE)
- 5% of lupus nephritis cases
- Clinical findings: Kidney biopsy shows build-up of antigen-antibody complex deposits; urinalysis is normal
- Class II: Mesangial proliferative
- Prevalence: 20% of lupus nephritis cases
- Clinical findings: Mesangial hypercellularity of any degree with mesangial immune deposits
- Class III: Focal LN
- Prevalence: 25% of lupus nephritis cases
- Clinical Findings: Active lesions exist in less than half of the glomeruli; hematuria and proteinuria
- Class IV: Diffuse proliferative
- Prevalence: 40% of lupus nephritis cases
- Very severe subtype
- Clinical findings: More than 50% of the glomeruli are affected with active lesions
- Immune complex deposits exist under the endothelial when viewed with an electron microscope
- Hematuria and proteinuria
- Hypertension, elevated serum creatinine, and raises anti-dsDNA (an antibody tested to diagnose lupus)
- Kidney failure is common
- Class V: Membranous
- Prevalence: 10% of lupus nephritis cases
- Clinical findings:
- Hematuria and proteinuria
- Significant systemic edema
- The glomerular capillary wall is thicker in segments
- High risk for renal vein thromboses, pulmonary embolism, or other thrombotic complications; active lesions are present
- Class VI: Advanced sclerotic LN
- Global sclerosis – typically more than 90% of the glomeruli are damaged and have active lesions
- Clinical findings: Progressively worsening kidney function

Self Quiz
Ask yourself...
- What are some differences in clinical manifestations between renal impairment and renal failure?
- Can you name the different classes of LN?
- How are clinical findings of Class I and Class IV different?
- Can you describe the glomerular function impairment in Class IV LN?
Diagnosis
LN is often the presenting manifestation resulting in the diagnosis of SLE (1). SLE is diagnosed clinically and serologically with the presence of certain autoantibodies. Evaluating kidney function in patients diagnosed with SLE is important as timely detection and management of renal impairment has been shown to greatly improve renal outcomes. The clinical presentation and laboratory findings for LN may differ, ranging from normal urinalysis and normal renal function test results to severe proteinuria, nephrotic syndrome, or acute nephritic syndrome, which can result in acute kidney failure (1). Monitoring for the development of lupus nephritis is done by a urinalysis, creatinine, urine albumin-to-creatine ratio, glomerular filtration rate (GFR), and a kidney biopsy.
Laboratory tests for SLE disease activity include the following:
- Antibodies to double-stranded DNA (dsDNA)
- Complement (C3, C4, and CH50)
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein (CRP)
Laboratory tests to evaluate kidney function in SLE patients:
- Urinalysis
- Check for protein, red blood cells (RBCs), and cellular casts
- Serum creatinine assessment
- Blood urea nitrogen (BUN) testing
- Spot urine test for creatinine and protein concentration
- 24-hour urine test for creatinine clearance and protein excretion
Urinalysis
A high level of protein or red blood cells in the urine signifies kidney damage. The Systemic Lupus International Collaborating Clinics (SLICC) define renal involvement in lupus as a 24-hour urinary protein excretion of 0.5 g daily or the presence of red blood cell casts in urinary sediment (1). Urinary protein excretion in a 12-hour or 24-hour urine collection provides the best estimate of proteinuria. The most common abnormalities in urinary sediment in patients with LN are leukocyturia, hematuria, and granular casts (1).
Blood Tests
Creatinine is a waste product from the normal breakdown of muscles in your body. Kidneys remove creatinine from the blood. An elevated creatinine reveals damage to the kidneys because it is not functioning as it should. Glomerular filtration rate (GFR) also is an important test to determine how well the kidneys are functioning.
Kidney Biopsy
The next step in diagnosing LN would be a kidney biopsy. Kidney biopsy is currently the gold standard for confirming a diagnosis of LN and characterizing the LN subtype on the basis of histological patterns (1). A kidney biopsy is usually performed as a percutaneous needle biopsy with minimization of risk factors for bleeding complications. The piece of tissue removed is examined under a microscope by a pathologist.
A kidney biopsy can (1):
- Confirm a diagnosis of lupus nephritis
- Help in determining how far the disease has progressed
- Guide treatment

Self Quiz
Ask yourself...
- Can you describe what the glomerular filtration rate (GFR) is important for?
- Can you name components of a urinalysis?
- Have you cared for a patient with hematuria?
- Can you think of reasons a patient may be apprehensive about having a kidney biopsy?
Treatment
Treatment of LN is highly individualized. There is not a specific FDA-approved drug specifically given for the treatment of LN. Treatment cannot be a “one-size fits all” approach, but a plan to target renal impairment and avoid causing further damage. The goal of immunosuppressive therapy is the resolution of inflammatory and immunologic activity. Unfortunately, aggressive treatments can result in additional harm to patients. As the therapy of LN consists of potentially toxic drugs, it may be harmful to begin treatment without a definitive diagnosis (4).
Treatment of LN usually involves immunosuppressive therapy and glucocorticoids. The goals of LN treatment are to achieve rapid remission of active disease, prevent renal flares, prevent progression of chronic kidney disease (CKD), minimize treatment-associated toxicity, and preserve fertility (1). Immunosuppressive therapy is used to treat active focal (class III) or diffuse (class IV) LN or lupus membranous nephropathy (class V); but not usually used to treat minimal mesangial (class I), mesangial proliferative (class II), or advanced sclerosing (class VI) LN.
The treatment of focal or diffuse LN has two main components: initial therapy with anti-inflammatory and immunosuppressive agents to slow kidney injury, followed by long-term subsequent immunosuppressive therapy to control the chronic autoimmune processes of SLE and encourage the repair of damaged nephrons (1).
Treatment Goals
- Reduce inflammation in the kidneys
- Decrease immune system activity by blocking immune cells from attacking the kidneys directly and making antibodies that attack the kidneys
- Treatment of systems (hypertension, fluid retention)
- Support kidney function
Medications
Medications for the treatment of LN include (2):
- Corticosteroid
- Prednisone
- Immunosuppressant
- Cyclophosphamide
- Mycophenolate mofetil
- Hydroxychloroquine (Quinoline drug used to treat or prevent malaria; used for autoimmune response)
Blood pressure control:
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs)
- Diuretics
- Beta blockers
- Calcium channel blockers
| Risk Target and Goals | Interventions |
| Lupus nephritis-related mortality | Chloroquine or hydroxychloroquine |
| Control of blood pressure and hyperlipidemia | |
| SLE and LN activity to avoid ESRD | Immunosuppression no less and no more than necessary |
| Hyperfiltration and proteinuria to avoid end-stage renal disease (ESRD) | Renin-angiotensin-aldosterone system inhibition |
| Avoid drug toxicity | Infections: Reduce or eliminate corticosteroids, PJP prophylaxis, vaccination, personal infection control |
| Malignancy: Avoid cumulative cyclophosphamide of over 30 grams | |
| Fractures: Reduce or eliminate corticosteroids, vitamin D supplementation, bone density monitoring | |
| Symptoms | Improvement or stabilization of the serum |
| Improvement of the urinary sediment | |
| Nephrotic syndrome: loop of Henle diuretics |
Treatment Guidelines
Key points of American College of Rheumatology guidelines for managing lupus nephritis (1):
- Patients with clinical evidence of active and previously untreated lupus nephritis should have a kidney biopsy to classify the disease according to the International Society of Nephrology/Renal Pathology Society (ISN/RPS) criteria.
- Patients with lupus nephritis should receive background therapy with hydroxychloroquine, unless contraindicated.
- Glucocorticoids plus either cyclophosphamide intravenously or mycophenolate mofetil orally should be administered to patients with class III or IV LN.
- Patients with class I/II nephritis do not require immunosuppressive therapy.
- Angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers should be administered if proteinuria reaches or exceeds 0.5 g/day (1).
- Blood pressure should be monitored and maintained at or below 130/80 mm Hg.
- Patients with class V lupus nephritis are generally treated with prednisone for one to three months, followed by tapering for one to two years if a response occurs.
For those who progress to kidney failure, treatment options include dialysis and kidney transplant.

Self Quiz
Ask yourself...
- Can you think of examples of treatments for blood pressure control other than medications?
- Can you think of treatments for LN and the risks of these treatments?
Complications
Complications of LN can be categorized into comorbidities from the actual condition and treatment-associated adverse outcomes. As mentioned, immunosuppressive therapy and glucocorticoids have harmful risks of their own. Comorbidities can include complications of the renal system and cardiovascular system. Treatment-associated complications can include infections, osteoporosis, cardiovascular disease, and reproductive impairment (1).
SLE and treatments, including glucocorticoids and calcineurin inhibitors, can cause hypertension, hyperlipidemia, and nephrotic syndrome (1). Many patients with LN have progressive CKD with associated comorbidities, such as anemia, osteoporosis, and other bone and mineral diseases. These factors contribute to vascular risks of progressive CKD and can lead to cardiovascular disease.
The prevalence of osteopenia and osteoporosis is high in patients with LN taking immunosuppressive therapy. In patients with severe nephrotic syndrome, a loss of plasma proteins, including clotting inhibitors, transferrin, immunoglobulins, and hormone-carrying proteins (such as vitamin D-binding protein), can lead to protein malnutrition, anemia, hormonal and vitamin deficiencies, hyperlipidemia, and increased risk for venous or arterial thrombosis (1). High-dose cyclophosphamide therapy correlates with premature gonadal failure in some cases, which is a complication of male and female reproductive organs (1).
Immunosuppressive agents increase the risk of infection, which can be further increased by disease activity, leukopenia, and CKD-related factors, such as nephrotic syndrome. Patients receiving immunosuppressive treatment can be at risk for poor outcomes with pneumocystis jirovecii pneumonia, herpes, hepatitis B, tuberculosis, influenza, and pneumococcal infection (1).
End-stage renal disease (ESRD) is a major complication of LN. Some 5–20% of patients with LN develop ESRD (1). By definition, all patients with LN have chronic kidney disease (CKD), but not all patients with CKD progress to ESRD. Essentially, ESRD occurs when the kidneys are no longer able to function to maintain life and either dialysis or a kidney transplant is needed.

Figure 4. Complications of Lupus Nephritis

Self Quiz
Ask yourself...
- Can you describe how renal impairment impacts the cardiovascular system?
- Can you name signs and symptoms of renal impairment?
- Have you cared for a patient experiencing adverse reactions to medications for immunosuppression?
- Are you familiar with risk factors for long-term corticosteroid use?
Screening and Prevention of Lupus Nephritis
Screening for LN onset and relapses is important for prompt treatment to improve outcomes. There are many new biomarkers under exploration for predicting and assessing LN (1). Patients with SLE should be screened periodically, even during periods of remission, every six to 12 months, or more frequently when clinically indicated (1). During regular check-ups, screening for LN onset or flares in patients with SLE should include evaluation of volume status, blood pressure measurement, urinalysis, and measurement of serum parameters. Elevation of serum creatinine level, the appearance of dysmorphic erythrocytes, cellular casts and new-onset proteinuria may indicate onset of LN (1). Nurses should encourage patients to regularly attend their appointments.
Patient Education
Patient education must be individualized to each unique patient. Lupus or LN may be a new diagnosis, or the patient may have been diagnosed previously. Teaching topics should include education on the disease process, the purpose of treatment regimens, and the importance of compliance.
Education on medication regimens is essential. Include the purpose, dosage, and possible side effects of all medications. Teach the patient when to seek medical attention. Provide tips such as wearing a medical alert bracelet or lanyard noting the condition and medications so appropriate action can be taken in an emergency. Provide resources on smoking cessation for patients who use tobacco. Teach the female patient the importance of planning pregnancies with medical supervision because pregnancy is likely to cause an exacerbation of the disease and the disease may cause negative pregnancy outcomes.
Discuss all precipitating factors that need to be minimized or avoided, including fatigue, vaccination, infections, stress, surgery, certain drugs, and exposure to ultraviolet light. Teach the patient to avoid strenuous exercise, but instead set goals of steady pace and balance. Describe pain management strategies and the importance of adequate nutrition. The patients may have concerns about skin care products and cosmetics. Teach the patient that these products should be hypoallergenic and approved by a provider prior to use. Encourage the patient to contact appropriate support groups available in the area.
Diet
Education on diet and nutrition for patients with LN can be very helpful in managing this condition. A diet regimen can be challenging because many people with this condition may also experience weight loss or gain, inflammation, osteoporosis, high blood pressure, and atherosclerosis. Recognizing specific nutritional concerns for each condition is important. A registered dietitian would be a meaningful resource for those with LN.
A kidney-healthy diet consists of low salt, low fat, and low cholesterol, with an emphasis on fruits and vegetables. Eating the right foods can help patients manage kidney impairment, maintain a healthy weight, and lower their blood pressure. Steroid medications can cause significant fluctuation in weight and energy.
The provider may advise restrictions on dietary protein intake. According to nephrology research, consuming more than 1.5 g of protein per kilogram per day can overwork the kidney filters, causing hyperfiltration (5). Many proteins are composed of amino acids that are converted to acids that are harmful to the kidney in large amounts; a diet high in animal proteins also contains sulfuric and phosphate acids that promote kidney damage (5). Potassium intake is also an important aspect of diet for those with LN. Potassium is secreted by the kidneys and may rise when kidney function declines; abnormal potassium levels can impact muscle function and increase the risk of hypertension, coronary artery disease, or stroke (5). A balanced diet with special considerations is a key teaching factor. It may be helpful to seek out resources from registered dieticians when needed.
Overview of Teaching Topics
Topics for education:
- Disease process
- Treatment plan
- Diagnostic studies and lab results
- Medications
- Purpose
- Dosage
- Side effects
- Contraindications
- Infection control
- Diet
- Tobacco cessation resources
- Reproductive complications
- Techniques to minimize ultraviolet exposure
Resources
The American College of Rheumatology (ACR) and Lupus Foundation of America (LFA) are excellent resources for patient with lupus that provide education and resources to improve overall well-being. The Lupus Foundation of America has a team of physicians, scientists, health educators, and individuals with lupus who work together to create resources, support groups, awareness initiatives, and programs. Patients can go to the “Ask our Health Educator” portal and get answers to questions they may have.
Conclusion
Nurses need to have a good understanding of lupus nephritis to provide patients with appropriate support and advice about how to maintain wellbeing and lead meaningful active lives. Knowledge on disease pathophysiology, manifestations, treatments, and complications is valuable for this serious condition. Patients often rely on nurses to support and empower them on this pathway.

Self Quiz
Ask yourself...
- How would you describe lupus to a non-medical person?
- Can you describe the difference between normal immune response and autoimmune response?
- Can you name clinical signs and symptoms specific to lupus?
- What is the most reliable diagnostic tool for LN?
- What are some ways the nurse can advocate for a patient having a kidney biopsy?
- How would you empower a patient with a new diagnosis of LN in knowledge of medications and their treatment regimen?
Alcohol Use Disorder: Long Term Effects and Complications
Introduction
Alcohol use disorder (AUD) is one of the most widespread psychiatric disorders and is estimated to affect approximately 29 million individuals aged 12 and older in the United States (9). According to the 2021 National Survey on Drug Use and Health, 28.6 million adults ages 18 and older have AUD and roughly 900,000 adolescents ages 12 to 17 have AUD (7).
Alcohol is the most prevalent misused substance in America with alcohol-related issues causing more than 85,000 deaths annually in the United States and three million deaths a year globally (9, 12). Globally, about 240 million people are affected by AUD, especially in Europe and America (9).
AUD is linked to motor vehicle accidents, dementia, depression, homicide, and suicide (9). The condition can also lead to social complications, such as legal problems, relationship issues, and economic stressors (due to the cost of alcohol, required medical care, missed time at work, and job loss). Individuals with AUD can end up isolating themselves from the individuals who are trying to help them most, including family members and friends.
Moderate alcohol use for most adults—no more than two drinks a day for men and one for women—is relatively harmless. An alcoholic drink includes 12 fluid ounces of regular beer, 10 fluid ounces of malt liquor, five fluid ounces of wine, or 1.5 fluid ounces of 80-proof distilled spirits (3, 4). Heavy alcohol drinking is defined as having four or more drinks per day or eight or more drinks per week for women and five or more drinks per day or 15 or more drinks per week for men (4).
Small amounts of alcohol, in particular red wine, can have beneficial cardiovascular effects, but heavy drinking can lead to serious health issues, such as cancer, cardiovascular disease, liver disease, osteoporosis, and infections (3, 4). Men are more likely than women to develop AUD, but women’s health suffers more than men’s, even at lower levels of consumption (3). Individuals with lower levels of education and of lower income experience AUD more than their counterparts (9).
Drinking can become problematic for those people who have psychological traits of impulsiveness, low self-esteem, and the constant need for attention and approval. Individuals who lack personal insight about drinking can develop AUD. For example, those who use alcohol to emotionally self-medicate (i.e., unwind from a stressful day) can develop alcohol-related issues (3).
Unfortunately, many individuals with AUD deny having a problem with alcohol and therefore do not seek treatment until faced with medical issues or legal complications. Regardless of how severe a patient’s drinking problem may seem, evidence-based treatment that includes medications, behavioral therapies, and support groups can help individuals achieve and maintain recovery.


Self Quiz
Ask yourself...
- How extensive is AUD in the United States and globally?
- How many fluid ounces constitute an alcoholic drink for beer, malt liquor, wine, and distilled spirits?
- To which health risks does heavy drinking contribute?
- Which psychological traits can increase the risk of AUD?
Pathophysiology
Alcohol ethanol or ethyl alcohol is a chemical substance found in alcoholic beverages, such as beer, hard cider, malt liquor, wines, and distilled spirits (liquor). Alcohol is the byproduct of yeast fermentation of sugars and starches. Alcohol is also found in some medicines, mouthwashes, and household products, including vanilla extract and other flavorings (4).
Alcohol use disorder is defined by the National Institute on Alcohol Abuse and Alcoholism as a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences (7). The term alcohol use disorder includes the terms alcohol abuse, alcohol dependence, alcohol addiction, and alcoholism. The condition affects brain function and is classified as mild, moderate, or severe (7).
Several evidence-based theories explain the development of AUD in individuals. These theories are (9):
- Positive-effect regulation: This occurs when people consume alcohol to seek positive rewards like pleasure or euphoria. Alcohol may be consumed to enhance social experiences and positive emotions.
- Negative-effect regulation: Individuals may drink alcohol in response to negative or distressing situations as a means to self-medicate and alleviate feelings of anxiety, depression, or low self-worth.
- Pharmacological vulnerability: This theory explains the differences in how individuals respond to the acute and chronic effects of alcohol. Some individuals are more prone to the rewarding effects of alcohol, or they have a reduced ability to metabolize alcohol, thus increasing their chances of developing AUD.
- Deviance proneness: Individuals with a history of deviant behavior or impaired socialization during childhood are more prone to AUD because these individuals use alcohol to self-medicate to alleviate symptoms of anxiety, depression, or low self-worth.
Cytosolic alcohol dehydrogenase (ADH) is the enzyme that metabolizes alcohol in the liver, and this metabolism process produces acetaldehyde as a byproduct. Acetate is then formed by the metabolism of acetaldehyde by the enzyme aldehyde dehydrogenase (ALDH).
Acetate then enters the body’s various metabolic pathways. Additionally, ADH is present in the gastrointestinal tract as well as the liver, which leads to the initial metabolism of alcohol during its ingestion. This is referred to as first-pass metabolism. The enzyme CYP2E1 of the cytochrome P450 system is upregulated in chronic alcohol users, which leads to an increased rate of alcohol metabolism (9).
Several factors affect the metabolism of alcohol (9):
- Women have a higher initial blood alcohol concentration following consumption because they have a slower first-pass metabolism due to lower levels of ADH; however, women eliminate alcohol consumption faster than males.
- Alcohol elimination declines with age, which is why older adults may experience a lower tolerance to alcohol than when younger, or why they may experience more severe hangover symptoms.
- In pregnancy, the fetal liver has an incomplete expression of enzymes CYP2E1 and ADH, leading to slower alcohol metabolism. This means that the fetus is exposed to the mother’s consumption of alcohol for a prolonged period, increasing the risk of fetal alcohol spectrum disorders.
- Native Americans have been found to metabolize alcohol faster due to the expression of beta-3 Class 1 ADH isoforms than individuals who express only the beta-1 Class 1 ADH isoform.
- When an individual fasts, alcohol metabolism is slowed due to decreased levels of ADH during a fasting state. Alternatively, food intake increases blood flow to the liver and allows fructose and other sugars to speed the metabolism of alcohol.
- The highest rates of alcohol elimination occur in the late evening versus during the daytime hours.
- Medications that have ADH inhibition or H2 receptor-blocking properties decrease the rate of alcohol elimination. This reduces first-pass metabolism in the stomach and increases blood alcohol levels.
- Heavy drinking increases the expression of the CYP2E1 enzyme, which increases alcohol elimination; however, this is eventually slowed in individuals with advanced liver disease.
Alcohol use can permeate every organ and tissue in the body, resulting in systemic dysfunction. The Complications and Long-Term Effects section explores how alcohol use impacts the body.
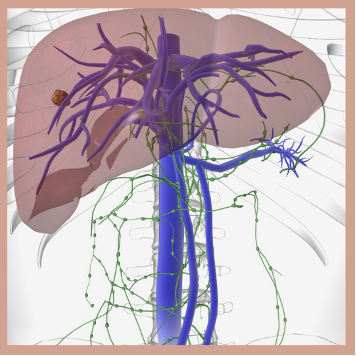

Self Quiz
Ask yourself...
- Which terms are included in AUD?
- What are the differences between positive-effect regulation and negative-effect regulation theories?
- How does the body’s metabolism process of alcohol work?
- How do pregnancy, fasting, and medications impact the metabolism of alcohol?
Risk Factors
Several factors are believed to contribute to the development of alcohol use disorder, including the home environment, peer interactions, genetic disposition, cognitive functioning, and other mental health disorders, such as schizophrenia, depression, and personality disorders (9).
Risk factors for AUD include (3, 7, 9):
- Genetics and family history. Hereditary factors can influence AUD by as much as 60%. Parents’ drinking habits are directly correlated to the child’s development of AUD. Certain genes have been found to increase an individual’s susceptibility to AUD, including:
- GABRG2 and GABRA2, COMT Val 158Met, DRD2 Taq1A, and KIAA0040.
- Drinking at an early age. Those individuals, especially females, who begin consuming alcohol before age 15 are three times more likely to have AUD. Research indicates that younger people who wait to start consuming alcohol until age 21 are less likely to have AUD.
- Mental health disorders. Psychiatric conditions, such as depression, post-traumatic stress disorder (PTSD), and attention deficit hyperactivity disorder (ADHD) are linked to an increased risk of AUD. Childhood trauma is also strongly correlated with AUD. The presence of both AUDs and psychiatric disorders leads to a worsened prognosis for both disorders.
- Social issues. Poverty and lack of education are significant risk factors for AUD.
Additionally, the risk for developing AUD can depend on how much, how often, and how quickly the individual consumes alcohol. Binge drinking and heavy drinking over time can lead to AUD (7).

Self Quiz
Ask yourself...
- Which mental health disorders can contribute to AUD?
- Which types of drinking can lead to AUD over time?
- Which genes have been found to increase an individual’s susceptibility to AUD?
- Which social factors are significant risk factors for AUD?
Signs and Symptoms
Nurses need to perform a thorough assessment of those individuals suspected of having AUD. The Cut Down, Annoyed, Guilty, and Eye-opener (CAGE) questionnaire is the widely accepted gold-standard assessment tool and is comprised of these questions (2):
1. Have you ever felt that you need to cut down on your drinking?
2. Have people annoyed you by criticizing your drinking?
3. Have you ever felt bad or guilty about your drinking?
4. Have you ever had a drink first thing in the morning to steady your nerves or to get rid of a hangover (eye-opener)?
The scoring for the CAGE includes 0 for “no” answers and 1 for “yes” answers with a total score of two or greater being clinically significant for AUD. However, healthcare providers are encouraged to regard a total score of one or greater as the potential for substance abuse disorder that requires further patient exploration (2).
The Alcohol Use Disorders Identification Test (AUDIT) is a 10-item screening tool created by the World Health Organization (WHO) to assess alcohol-related conditions. There is a patient test that individuals may administer to themselves, and a test designed for healthcare providers to administer to patients. Both tests ask the same questions and use a similar scoring method. The provided answers are 0 for “never”, 1 for “monthly or less”, 2 for “2-4 times a month”, 3 for “2-3 times a week”, and 4 for “4 or more times a week”. A score of 8 or more indicates harmful alcohol use (8, 12).
The AUDIT questions are (8, 12):
- How often do you have a drink containing alcohol?
- How many drinks containing alcohol do you have on a typical day when you are drinking? (The answer options for this question are 0 for “1 or 2”, 1 for “3 or 4”, 2 for “5 or 6”, 3 for “7 to 9”, and 4 for “10 or more”.)
- How often do you have six or more drinks on one occasion?
- How often during the last year have you found that you were not able to stop drinking once you had started?
- How often during the last year have you failed to do what was normally expected to you because of drinking?
- How often during the last year have you needed a first drink in the morning to get yourself going after a heavy drinking session?
- How often during the last year have you had a feeling of guilt or remorse after drinking?
- How often during the last year have you been unable to remember what happened the night before because of your drinking?
- Have you or someone else been injured because of your drinking? (The answer options for this question are “no”, “yes, but not in the last year”, and “yes, during the last year”.)
- Has a relative, friend, doctor, or other healthcare worker been concerned about your drinking or suggested that you cut down? (The answer options for this question are “no”, “yes, but not in the last year”, and “yes, during the last year”.)
Nurses and other healthcare professionals can ask patients the additional questions below about their alcohol use to determine the risk and presence of AUD.
In the past year, have you (7):
- Ended up drinking more or longer than you intended?
- Tried to cut back on drinking, but have been unable to do so?
- Experienced symptoms of illness (hangover) related to your drinking?
- Craved a drink so much that it distracted you from your current activity?
- Found that your drinking has interfered with maintaining your responsibilities and obligations regarding home, family, work, or education?
- Continued to drink despite knowing that it caused problems with family and friends?
- Foregone pleasurable activities (hobbies, etc.) that you enjoy to drink?
- Increased your risk for injury (driving, swimming, using machinery, walking in a dangerous area, engaging in unsafe sexual behavior) due to drinking?
- Continued to drink despite the social, health, or economic problems it causes?
- Experienced feelings of anxiety, depression, or memory blackout due to your drinking?
- Needed to drink more alcohol than in the past to get the same effects?
- Experienced alcohol withdrawal symptoms, such as tremors, restlessness, irritability, nausea and vomiting, sweating, malaise, racing heartbeat, hallucinations, or seizures?
The patient’s positive response to two to three of these criteria indicates mild symptoms, four to five indicates moderate symptoms, and six or more indicates severe symptoms (7).
Patients with AUD often report frequent falls, blackout spells, motor instability and tremors, visual disturbances, hangover symptoms (headache, nausea and vomiting, dry mouth, photophobia), hypertension, heart palpitations, seizures, confusion, mood swings, and sleep disturbances. Social symptoms include school or job instability or loss, relationship separation or divorce, estrangement from family and friends, and homelessness (9). Nurses should also assess patients suspected of AUD for post-traumatic stress disorder, bipolar disorder, panic disorder, anxiety disorder, dysthymic disorder, major depressive disorder, and insomnia (9).
During the assessment of a patient with AUD, nurses may note ataxia, fine motor skill disturbances, mental status changes, mood changes, slurred speech, tachycardia, hypotension, nystagmus, asterixis, ruddy palms, jaundiced coloring, and ascites. Signs of liver disease include hepatomegaly, splenomegaly, cirrhosis, spider angiomata, and liver atrophy (9).

Self Quiz
Ask yourself...
- What are the four CAGE alcohol use screening questions?
- When using the AUDIT screening tool, which score indicates harmful alcohol use?
- Which social symptoms are individuals with AUD likely to experience?
- Which physical symptoms may the nurse observe in patients with AUD?

Prevention
The stage in life when a person is exposed to alcohol is an important predictor for alcohol misuse. Adolescence is a time when many people begin experimenting with drinking, and research indicates that drinking before the brain is fully formed (age 26) can negatively impact brain development and compromise cognitive function. The main goal of preventing AUD is to impede, or at least delay, the onset of drinking in the youth population (6).
Adolescents and young adults seek independence and favor transitioning to adult roles. Most of this population drives automobiles and spends more time with friends than family members, thus making them easily influenced by their peer group. This also means that this population is at high risk for alcohol-related injuries, with 5,000 18- to 24-year-olds dying each year due to alcohol-related incidents (6). This group engages in binge drinking, which can lead to blackouts, alcohol poisoning, sexual assault, sexually transmitted infections, and poor academic performance.
Other factors that influence drinking behaviors that should be considered in prevention interventions are genetics, health status, cultural background, educational background, socioeconomic status, community attitudes toward alcohol use, and exposure to social media. Preventative measures should also be geared toward pregnant women and older adults since these populations have special considerations, such as the risk for fetal alcohol spectrum disorders in pregnant women and the inability to effectively metabolize alcohol in older adults that can lead to injuries (6).
Regular screenings for alcohol misuse are a key prevention strategy, and research shows that most patients do not object to being screened for alcohol use and thus are open to receiving advice about alcohol use (6). Evidence also shows that alcohol-related incidents can be prevented by both individual and environmental interventions. For example, college students who are taught to monitor their drinking and how to effectively refuse alcohol when offered can prevent AUD. College communities that restrict happy hours, enforce the minimum drinking age, and prevent alcohol price promotions can decrease the risk of AUD (6).

Self Quiz
Ask yourself...
- Which factors are predictors of alcohol misuse?
- Which factors put adolescents and young adults at risk for alcohol-related injuries?
- How do most patients react to screenings and advice regarding alcohol use?
- Which measures can college students and college communities implement to prevent AUD?
Diagnostics and Treatment
The preliminary source used to diagnose alcohol use disorder is the Diagnostic and Statistical Manual of Mental Disorders (DSM).
According to the DSM, the criteria for alcohol use disorder include (11):
A maladaptive pattern of substance use leading to clinically significant impairment or distress, as manifested by two or more of the following, occurring at any time in the same 12-month period:
- Alcohol is often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control alcohol use.
- A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects.
- Craving, or a strong desire or urge to use alcohol.
- Recurrent alcohol use failing to fulfill major role obligations at work, school, or home.
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol.
- Important social, occupational, or recreational activities are given up or reduced because of alcohol use.
- Recurrent alcohol use in situations in which it is physically hazardous.
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol.
- Tolerance, as defined by either of the following:
- A need for markedly increased amounts of alcohol to achieve intoxication or desired effect.
- A markedly diminished effect with continued use of the same amount of alcohol.
- Withdrawal, as manifested by either of the following:
- The characteristic withdrawal syndrome of alcohol
- Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms.
Laboratory testing in patients with AUD can indicate blood disorders; vitamin, mineral, and electrolyte imbalances; cancers; cardiovascular disease; liver disease; and pancreatitis. Alcohol-related organ damage can be determined by biomarkers, such as aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transpeptidase (GGT), phosphatidylethanol (PEth), fatty acid ethyl ester (FAEE), total serum sialic acid (TSA), mean corpuscular volume (MCV), cholesteryl ester transfer protein (CETP), carbohydrate-deficient transferrin (CDT), N-Acetyl-β-Hexosaminidase (Beta-Hex), macrophage migration inhibitory factor (MIF), and D-dopachrome tautomerase (DDT). Biomarkers like alcohol and ethyl glucuronide levels can determine recent alcohol consumption. CDT and PEth levels can help monitor abstinence (1, 9).
Treatment approaches for AUD involve pharmacological and nonpharmacological interventions.
The Federal Drug Administration (FDA) has approved three pharmacological treatments for AUD (9, 10):
- Naltrexone (Vivitrol) is a mu-opioid antagonist that blocks the effects of opioids and is widely used in treating addiction to narcotics. In alcoholism, the medication blocks the effects of naturally occurring opioids, such as endorphins. Therefore, the drinker does not experience any psychological benefits or “high” from the alcohol. Naltrexone also reduces the craving for alcohol leading to improved abstention rates, reduced number of drinking days, and reduced risk of relapse. The potential side effects—nausea, headaches, and fatigue—also work as an alcohol deterrent.
- Acamprosate is a glutamate agonist that promotes a balance of inhibitory and excitatory neurotransmitters in the brain that are disrupted by alcohol abuse. The discontinued brand name is Campral, but the generic equivalent is still available. The medication can cause weight gain and severe depression.
- Disulfiram (Antabuse) is an alcohol antagonist drug that inhibits ALDH, resulting in the accumulation of acetaldehyde in the body. The purpose of disulfiram is to promote fear in the drinker because drinking alcohol in conjunction with taking the medication can result in serious adverse reactions, including flushing, headache, dyspnea, diaphoresis, dizziness, shock, and even death.
- Gabapentin (Neurontin) and topiramate (Topamax) are not yet FDA-approved for AUD, but they are currently being used to treat the disease. Gabapentin, an anticonvulsant used to treat neuropathic pain, corrects dysregulation caused by alcohol use and cessation; it also decreases alcohol cravings. Topiramate, also an anticonvulsant, decreases alcohol cravings.
The most effective non-pharmacological approach to AUD is psychological therapy, including (9):
- Motivational interviewing. This technique is most effective in those patients who are ambivalent about changing their behaviors and quitting alcohol. The approach is client-centered and helps patients recognize and address their issues. It helps them become motivated to make long-lasting, healthy changes.
- Motivational enhancement therapy (MET). MET is a manual-based intervention that includes motivational interviewing and focuses on strengthening the motivation of the patient to change their alcohol use behaviors.
- Cognitive behavioral therapy (CBT). CBT helps individuals explore the connections among their thoughts, emotions, and behaviors. This therapy can increase motivation to stop drinking, identify triggers that prompt alcohol use, and teach effective coping mechanisms to deal with alcohol cravings and alcohol-seeking behaviors. In one study, 58% of patients receiving cognitive-behavioral treatment fared better than those who did not receive this therapy (3).
Other programs that support patients with AUD are residential facilities (in-patient rehabilitation), community programs like Alcoholics Anonymous (AA) or other 12-step programs, and faith-based programs that align with the principles of certain religions.


Self Quiz
Ask yourself...
- How does the DSM define tolerance?
- Which biomarkers can indicate AUD?
- Which three medications has the FDA approved for AUD treatment?
- What are the differences among motivational interviewing, motivational enhancement therapy, and cognitive behavioral therapy?
Complications and Long-Term Effects
AUD impacts each body system and can cause complications that have long-term negative effects. For example, alcohol impairs the brain’s ability to regulate balance, memory, speech, and judgment, which can lead to injuries. With long-term, heavy drinking the neurons reduce in size, the brain’s mass shrinks, and the brain’s inner cavity grows larger.
Alcohol interferes with glutamate action, which inhibits the creation of new memories and leads to blackouts. Alcohol also influences the neurotransmitters dopamine and serotonin, which can cause mood dysregulation, impaired concentration, and decreased motivation. Even though alcohol can cause euphoria at first, it is a depressant that can lead to suicidal ideation, behaviors, and death.
Additionally, excessive alcohol consumption can weaken the immune system, which can lead to increased rates of infection, such as pneumonia (4).
Additional complications of AUD by the organ system are (4, 5, 7):
- Cardiac/Circulatory: Cardiomyopathy, arrythmias, stroke, hypertension, ischemic heart disease, heart failure
- Endocrine: Acute and chronic pancreatitis, pancreatic cancer, diabetes
- Gastrointestinal: Esophageal cancer, oral cavity cancer, larynx cancer, pharynx cancer, gut leakiness, gastritis, ulcers, microbial dysbiosis, colorectal cancer, inflammatory bowel disease (IBD)
- Hepatic: Steatosis, steatohepatitis, fibrosis, cirrhosis, alcohol-associated hepatitis, liver cancer
- Immune/Lymphatic: Infections, such as tuberculosis
- Integumentary: Melanoma
- Neurologic: Ischemic stroke, amyotrophic lateral sclerosis (ALS), Alzheimer’s disease, multiple sclerosis (MS)
- Reproductive: Breast cancer, sexually transmitted infections
- Respiratory: Acute respiratory distress syndrome, alcohol-associated lung disease, pneumonia
- Skeletal: Muscle myopathy, muscle wasting, impaired bone fracture repair, reduced bone density (osteopenia, osteoporosis)
- Urinary: Kidney disease, prostate cancer
Alcohol is a toxic substance that contains carcinogens, such as nitrosamines, asbestos fibers, phenols, and hydrocarbons, which are the cause of 3.5% of cancer deaths in the United States (4).
Some cancers associated with alcohol consumption are (4):
- Head and neck cancer. Drinkers are at increased risk for oral cavity, pharynx, and larynx cancers. The risk increases among those individuals who both drink and use tobacco.
- Esophageal cancer. Esophageal squamous cell carcinoma risk is high in moderate to heavy drinkers.
- Liver cancer. The risk for hepatocellular carcinoma and intrahepatic cholangiocarcinoma doubles in individuals who are heavy drinkers.
- Breast cancer. Light drinkers have a slightly increased risk of breast cancer, whereas moderate to heavy drinkers increase their risk substantially. Tobacco use in conjunction with alcohol use increases the risk of breast cancer.
There are multiple ways in which alcohol can increase the risk of cancer, such as (4):
- Metabolism of ethanol to acetaldehyde, which is a toxic carcinogen, acetaldehyde damages DNA and proteins.
- Oxidation can damage DNA, proteins, and lipids.
- Inability to digest and assimilate vital nutrients that can protect against cancers, such as vitamin A, vitamin B complex, vitamin C, vitamin D, vitamin E, and carotenoids.
- Increasing levels of estrogen can lead to breast cancer.
The prognosis for patients with AUD is very challenging with less than 20% to 30% achieving long-term abstinence and with most acquiring serious to permanent health conditions that are irreversible (9).

Self Quiz
Ask yourself...
- How does alcohol negatively impact the brain?
- How does alcohol affect the gastrointestinal and integumentary systems?
- Why does oxidation increase the risk of cancer?
- What is the prognosis of patients with AUD?
Patient Education
Nurses play a critical role in educating patients with AUD, and they should do so in a non-judgmental and non-confrontational manner.
Educational topics nurses should address with patients include (9, 10):
- Healthy diet. Most patients with AUD suffer from malnourishment, particularly regarding folate. Foods rich in folate include legumes, eggs, leafy greens, citrus fruits, nuts and seeds, and fortified grains. Patients should be taught the importance of maintaining a healthy diet that is rich in protein, complex carbohydrates, fresh fruits and vegetables, healthy fats, and vitamins and minerals.
- Reducing risky behaviors. Individuals with AUD should be taught that alcohol consumption lowers inhibitions, which can lead to risk-taking behaviors, such as driving, swimming, operating heavy machinery, and engaging in unprotected sexual practices.
- Importance of support groups. Patients with AUD are more likely to make progress and stay motivated if they are supported by family, friends, and community resources like Alcoholics Anonymous (AA). Family members should also be encouraged to attend support groups like Al-Anon.
- Maintaining a temptation-free environment. Patients should be encouraged to remove all alcohol from their homes and offices. When traveling, they can request that hotels remove alcohol from the guest room minibar.
- Importance of maintaining health screenings. AUD can lead to other serious health conditions, such as cardiovascular disease, osteoporosis, and various cancers. Patients should be taught the importance of receiving regular medical check-ups and health screenings to maintain optimal health.
Nurses should also ensure that patients can access educational and support resources in their native language, as well as be provided with information about resources available to low-income individuals, if applicable.

Self Quiz
Ask yourself...
- Which foods high in folate should the nurse recommend for patients with AUD?
- Why do individuals with AUD engage in risky behaviors?
- Which serious health conditions are patients with AUD at risk of acquiring?
- How can alcoholics maintain a temptation-free environment at home and when traveling?
Resources
There are many resources available to assist patients with AUD.
- Alcoholics Anonymous: AA is a global fellowship community that helps individuals resolve their issues with alcohol. https://www.aa.org/
- Al-Anon Family Groups: Like AA, Al-Anon is a fellowship community that helps friends and family members of alcoholics gain the support they need. https://al-anon.org/
- Alateen: Alateen is a component of Al-Anon, a fellowship group for adolescents who have been affected by someone else’s drinking. https://al-anon.org/newcomers/teen-corner-alateen/
- Centers for Disease Control and Prevention: The CDC provides resources, such as publications, online tools, and healthcare information related to individual states. https://www.cdc.gov/alcohol/resource-center/index.html
- FindTreatment.gov: This is a national website for locating treatment facilities for mental and substance use disorders. https://findtreatment.gov/locator
- National Association for Children of Addiction (NACoA): This organization provides programs, such as The Clergy Education and Training Project, Celebrating Families, and Children’s Program Kit to support the children of addicted parents. https://nacoa.org/
- Rethinking Drinking: The National Institute on Alcohol Abuse and Alcoholism (NIAAA) website provides evidence-based information for patients and healthcare providers, as well as listings for treatment centers. https://www.rethinkingdrinking.niaaa.nih.gov/

Self Quiz
Ask yourself...
- Which organization assists friends and family members of individuals with AUD?
- Which organization supports teenagers who are affected by someone else’s drinking?
- Which programs by NACoA support the children of addicted parents?
- Which websites provide listings for treatment centers?
Case Study
B.P. is a 32-year-old Caucasian man who presents to the emergency department after a motor vehicle accident during which B.P. lost control of his car and drove it into a roadside ditch. There were no other cars on the road at the time, making the accident a one-person collision. B.P. was brought to the hospital by his girlfriend and presented with superficial lacerations and bruising to his face from deployment of the driver’s side airbag and more serious lacerations to his left forearm that were injured by the breaking glass of the driver’s side window. He states that he thinks he may have hit his head on the automobile’s steering wheel before airbag deployment, but then says, “I’m not completely sure about that little detail.”
B.P.’s vital signs are blood pressure 158/84 mmHg, pulse 78 beats per minute, respirations 16 breaths per minute, and oxygen saturation 95%. His lung fields are clear to auscultation bilaterally, and his cardiovascular exam reveals a regular rate and rhythm without murmurs. Bowel sounds are confirmed in four quadrants via auscultation. Radial, pedal, and dorsal pedal pulses are normal bilaterally. Pupils are sluggish to react to penlight; the patient’s eyes have a glassy appearance. B.P. is oriented to place, but not day or time.
He can state his name and birthdate without hesitation, but he pauses before stating his complete address and incorrectly states his zip code. When speaking, B.P.’s words are slurred, but his hearing bilaterally is intact. During the musculoskeletal and neurological assessments, B.P. is unable to follow all the instructions the nurse provides and at one point he whines, “Can we stop now? This is super hard and I’m so sleepy. I need to go to bed now.” The patient’s left forearm is red and edematous with two lacerations that are both roughly 1.5 inches in length.
There are evident shards of glass present in both lacerations and bleeding has slowed significantly since the patient arrived at the hospital. B.P.’s face has several minor red contusions and a couple of superficial lacerations. The patient denies any reports of pain, headache, nausea, or dizziness, and says that he only feels fatigued.
B.P.’s health history includes chronic hay fever for which he takes over-the-counter antihistamines. He denies any further health issues. The nurse is unable to obtain a detailed social history or family history due to B.P.’s noncompliance.
After B.P.’s face and left arm are cleaned, and the left arm sutured and bandaged, he is taken for a chest x-ray, which is normal, and a computerized tomography (CT) scan of the head, which shows no intracranial hemorrhage, mass, or stroke. Blood test results reveal folate deficiency, and ALT, AST, MCV, GGT, and CETP levels consistent with heavy alcohol use. Intravenous folate and normal saline are administered during the next several hours, and the patient is consistently monitored for pain and alcohol withdrawal symptoms. As B.P. becomes sober, the nurse initiates the AUDIT questionnaire; B.P. scores a 32.
When the nurse explains B.P.’s AUDIT score to him, he states, “Yeah, I’m not surprised. I’ve been drinking since I was 13, and my girlfriend keeps telling me that my drinking is getting worse. I just like to have a few to chill after a hard day at work; my job is super stressful. Maybe she’s right. And after tonight, I should probably look into it. These hospital and car bills aren’t going to be cheap.”
B.P. is discharged with a referral to a psychiatrist for further AUD evaluation and potential treatment. He is also given a couple of brochures about alcohol abuse and in-patient rehabilitation programs. B.P. is encouraged to follow up with his primary care physician for continued care of his injured arm.

Self Quiz
Ask yourself...
- Which social factors about B.P.’s situation put him at risk for AUD?
- Which assessment findings indicate B.P. may have AUD?
- Is B.P.’s AUDIT score concerning? If so, why?
- Which factors indicate it was effective for the nurse to wait to administer the AUDIT to B.P.?
Conclusion
AUD puts individuals at risk for serious health complications, legal problems, and impaired interpersonal relationships. Many alcoholics do not receive appropriate medical care for AUD due to a lack of screening by healthcare providers. Therefore, nurses must use their assessment skills to evaluate patients for AUD and provide them with proper education about the disease, including its long-term effects and complications.
Healthcare screenings for cardiovascular disease and mental health disorders, as well as referrals to community support programs such as Alcoholics Anonymous, help patients take responsibility for their health and recovery.
Bioethics in Nursing
Introduction
Nursing practice is deeply rooted in ethical principles that guide decision-making and client care. Bioethics is a crucial aspect of healthcare that provides a framework for analyzing ethical dilemmas and promoting individualized client-centered care respectfully and compassionately. Nursing ethics involves applying bioethical principles in practice, such as maintaining client confidentiality and respecting autonomy. Nurses face ethical dilemmas regularly. One of the most common is providing care that conflicts with personal beliefs (6).

Self Quiz
Ask yourself...
- How do you think bioethics influences nursing practice
- What are some examples of ethical dilemmas nurses may face?
- Can you describe a situation where a nurse's personal beliefs conflicted with their professional obligations?
- How would you navigate such a scenario?
Definition and Purpose
Bioethics is the study of ethical and moral principles guiding healthcare decisions and practices (10). Its purpose is to ensure that healthcare providers make informed decisions that respect clients' values, beliefs, and rights (5).
Bioethics provides a framework for analyzing ethical issues in healthcare while considering the interests of the clients, their families, and the healthcare providers involved in their care (5). By understanding the definition and purpose of bioethics, nurses can develop a strong foundation for addressing ethical challenges in practice, such as informed consent, client confidentiality, and when it may infringe upon others’ health and proper resource allocation (5,6,10).


Self Quiz
Ask yourself...
- How does the definition of bioethics impact its application in nursing practice?
- What are some potential consequences of ignoring ethical principles?
- Can you think of a situation where a nurse's understanding of bioethics helped them navigate an ethical dilemma?
- What was the outcome?
Principles of Bioethics
The principles of bioethics include autonomy, beneficence, non-maleficence, and justice (5,6,7,9). Autonomy respects clients' decision-making capacity, beneficence promotes a client's well-being, non-maleficence avoids any harm to the client, and justice ensures fairness and equity for all involved in the client’s care (5,6,9).
These principles serve as the guiding force in nursing practice; influencing the decisions related to client care, research, and policy development (1). Autonomy empowers clients to make informed choices about their care (5,6,9). This may include decisions that the client’s family and even healthcare providers may disagree with personally. Beneficence compels nurses to act in the best interests of their clients and advocate for the client’s desires (5,6,9). Non-maleficence reminds nurses to avoid causing harm; this includes not just physical but emotional and mental harm as well (5,6,9).

Self Quiz
Ask yourself...
- How do the principles of bioethics guide nursing practice?
- What are some examples of how these principles are applied in different healthcare settings?
- Can you describe a situation where a nurse had to balance the principles of autonomy and beneficence in their practice?
- How did they navigate this ethical dilemma?
Types of Ethics and Professions
Different professions have specific ethical guidelines, such as the American Nurses Association (ANA) Code of Ethics for nurses (1). Understanding the ethical framework of various professions is essential to the interdisciplinary healthcare approach.
Interdisciplinary collaboration requires an understanding of diverse ethical perspectives and principles, an approach that coincides with an equally diverse client population. Nurses should be aware of the ethical guidelines that govern their practice and be able to apply them in diverse healthcare settings. They must also be aware of their own beliefs and guidelines and how these may affect their decision-making, adversely affecting client care (5,6).

Self Quiz
Ask yourself...
- How do different professional ethical guidelines impact interdisciplinary collaboration?
- What are some potential consequences of ignoring these guidelines?
- Can you describe a situation where a nurse had to navigate an ethical dilemma with an interdisciplinary team?
Ethics in Nursing
Nursing ethics involves applying principles in practice that benefit the client, healthcare providers, and loved ones of the client. Examples include things such as maintaining client confidentiality and respecting autonomy, helping the client make the right decision for themselves, and advocating for those decisions to others (1,5). One of the most difficult decisions nurses face involves those that conflict with their personal belief system (6).
Nurses must be equipped with the knowledge and skills to navigate these ethical challenges and provide care that respects clients' values and beliefs while also nurturing their thoughts and feelings (6). By exploring bioethics in nursing, we can promote a culture of ethical practice that is compassionate and client-centered.
Henrietta Lacks Story
Henrietta Lacks was a Black tobacco farmer who had her cancer cells taken without her knowledge or consent which led to numerous scientific breakthroughs, including the development of the polio vaccine (7,8). Her story raises important questions about medical ethics, racism, and the intersection of science and human compassion.
In 1951, Henrietta Lacks was diagnosed with cervical cancer and began treatment at Johns Hopkins Hospital in Baltimore. During her treatment, a sample collection of her cancer cells was taken by her doctor, Dr. George Gey without her knowledge and or consent (7,8). Dr. Gey discovered that Henrietta's cells were extraordinary in nature and could be of great value for cancer research and future developments as they could survive and thrive in a laboratory setting thus making them ideal for scientific research.
Henrietta's cells, known as HeLa cells, were soon being used in laboratories worldwide, leading to numerous scientific breakthroughs, including the polio vaccine development, in vitro fertilization, and gene mapping (7,8). However, Henrietta's family was never informed or financially compensated for the use of her cells, and her story remained largely unknown until the publication of Rebecca Skloot's book "The Immortal Life of Henrietta Lacks" in 2010 (2).
Henrietta's story highlights the unethical practices that were common in the medical field at the time, particularly in relation to clients that lacked resources, particularly those belonging to minority groups (2). Her cells were taken without her consent, and she was never compensated or acknowledged for her contribution to science. This raised some very important questions about medical ethics, informed consent, and the exploitation of vulnerable populations.
Still, Henrietta's story is a powerful reminder of the intersection of science and the need for personal autonomy. Her cells have been used to advance scientific knowledge, but they also represent a person, a family, and a community. The use of her cells without her consent or compensation is a violation of her humanity and a reminder of the need for ethical considerations in scientific research.

Self Quiz
Ask yourself...
- How do nursing ethics impact patient care?
- What are some potential consequences of ignoring ethical principles in practice?
- Can you describe a situation where a nurse's understanding of ethics helped them provide high-quality care
- What were the benefits for the patient?
Tuskegee Syphilis Experiments
The Tuskegee Syphilis Study was a highly controversial and unethical medical experiment conducted on African American men in Macon County, Alabama between 1932 and 1972 (4,11). The study, led by the Department of U.S. Public Health Services, involved withholding treatment from hundreds of African American men infected with syphilis despite the availability of effective therapies, to study the natural progression of the disease (4,11).
The men, who were mostly illiterate and poor, were not informed that they had syphilis, their partners were not informed of the disease, nor were they given treatment for the disease (4,11). Instead, they were given placebos and misleading information about their condition. The study continued for 40 years, during which time many of the men died from syphilis-related complications, and many others suffered serious health problems which included the spreading of syphilis to unsuspecting sexual partners.
The Tuskegee Syphilis Study is widely regarded as one of the most unethical medical experiments in history. The study was conducted without the men's knowledge or consent, and it violated basic human rights and principles of medical ethics. By way of public outcry and shock, the awareness of these experiments led to major changes in the way human subjects are protected in medical research and a desire for closer oversight by governing groups.
In 1974, a class-action lawsuit was filed on behalf of the men who were involved in the study, resulting in a multimillion-dollar settlement (11). The study also led to the establishment of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, which developed guidelines for the ethical conduct of research involving human subjects (11).
The Tuskegee Syphilis Study has had a lasting impact on the field of medicine and beyond. It highlighted the importance of informed consent and the need for ethical oversight in the field of medical research. It has also led to the increased scrutiny of medical experiments and a greater emphasis on protecting human subjects, their privacy, and most importantly honest care and explanations of medical conditions and treatments.
Today, the Tuskegee Syphilis Study is remembered as a cautionary tale about the dangers of unethical medical research. It serves as a reminder of the importance of prioritizing the well-being and safety of people and the need for ongoing vigilance in ensuring that medical research is conducted ethically and responsibly, and ensuring there are the proper checks and balances in place to provide the oversight needed.
The study also highlighted the need for diversity in medical research and the importance of including diverse populations in clinical trials (11). It led to increased efforts to address health disparities and to ensure that medical research is conducted in a way that is fair and equitable to all.
In addition, the Tuskegee Syphilis Study led to changes in the way that medical research is regulated and overseen (11). It led to the establishment of institutional review boards (IRBs) and independent ethics committees (IECs) which are responsible for reviewing and approving research protocols and ensuring they meet the ethical standards set in place (11).
Transparency and accountability in medical research have also been placed at the forefront of research since these events took place. Highlighting the importance of disclosing potential conflicts of interest and ensuring research is conducted in a way that is transparent and open to scrutiny; there inevitably was major change and growth that came from this huge medical injustice.
The Tuskegee Syphilis Study was a highly unethical and controversial medical experiment that had a profound impact on the field of medicine and beyond. It highlighted the importance of informed consent, ethical oversight, and diversity in medical research, and led to major changes in the way medical research is conducted and regulated. In these ways, it acted as a catalyst of growth and change in the way the U.S. views and treats research participants. It serves as a reminder of the need for ongoing vigilance in ensuring medical research is conducted ethically and responsibly.
The Tuskegee Syphilis Studies and Henrietta Lacks' cases highlight the importance of informed consent in research.
Other examples include: (5,9)
- Abortion and reproductive rights
- Euthanasia and end-of-life care
- Gene editing and genetic research
- Healthcare access and disparities


Self Quiz
Ask yourself...
- How do bioethical issues like informed consent impact healthcare outcomes
- What are some potential consequences of ignoring these issues?
- Can you describe a situation where a bioethical issue like euthanasia sparked a debate?
- How did healthcare professionals navigate this ethical dilemma?
Research in Ethics
Research ethics involves applying bioethical principles in research (3). Obtaining informed consent and ensuring participant confidentiality are two ways in which the provider can best provide ethical care to those that entrust the healthcare system with their voluntary well-being.
Researchers must be aware of ethical principles that guide research and ensure their studies are conducted ethically and responsibly which puts the client first (3).
Ethical Decision-Making
Ethical decision-making involves critical thinking, moral principles, and professional standards. Nurses can use ethical frameworks, such as the MORAL model and Nursing Process model, to guide decision-making (5). Ethical decision-making is a crucial aspect of nursing practice as it enables nurses to navigate complex healthcare issues and promote clients' well-being.

Self Quiz
Ask yourself...
- How do ethical principles guide research?
- What are some potential consequences of ignoring these principles?
- Can you describe a situation where a researcher had to navigate an ethical dilemma in their study?
Conclusion
Bioethics plays a vital role in nursing practice, ensuring that clients receive respectful and compassionate care. Understanding bioethical principles and applications is essential for nurses to provide high-quality care. By applying ethical principles and frameworks, nurses can navigate complex healthcare issues and promote clients' well-being.

Self Quiz
Ask yourself...
- How does the ethical framework guide decision-making in nursing practice and what are some potential consequences of ignoring these frameworks?
- How do personal values and beliefs impact nursing practice what are the implications for patient care?
- How does the principle of autonomy impact informed consent in healthcare?
- What are some potential consequences of prioritizing beneficence over non-maleficence in healthcare, and how can nurses balance these principles?
- How does the concept of justice impact healthcare resource allocation and what are the implications for nurses and patients?
- How do nurses balance the need for patient confidentiality with the need for transparency?
- What are some potential consequences of ignoring the principle of non-maleficence in healthcare, and how can nurses prioritize patient safety?
- How does the principle of autonomy impact patient decision-making?
- How do nurses balance the need for patient education with the need for autonomy?
- Are there any potential consequences for prioritizing patient satisfaction over patient well-being?
- How does the concept of vulnerability impact healthcare ethics?
- How do nurses balance the need for patient advocacy with the need for patient autonomy?
- What are some potential consequences of ignoring the principle of justice in healthcare?
- How does the principle of beneficence impact healthcare resource allocation?
- How do nurses balance the need for patient education with the need for patient confidentiality?
- What are some potential consequences of prioritizing patient well-being over patient autonomy?
- Could the Henrietta Lacks case and the Tuskegee Syphilis cases have an affect the way minorities view medical treatment in the U.S?
Medical Interpreter Use in Healthcare
Introduction
The presence of a medical interpreter can make a significant difference in the care of a patient with limited knowledge of the English language. Their presence is essential for numerous reasons. Along with addressing language barriers and improving communication, they assist in bridging cultural gaps. With the number of those in need of these services increasing, their presence is more important than ever.
Definition
The role of the medical interpreter is a very specialized one. It requires a very distinct set of skills, which includes the ability to speak fluently in several languages and to have an extensive understanding of medical terminology (1). They aim to help non-English speaking people communicate with their healthcare providers and other medical professionals.
The National Council on Interpreting in Health Care (NCIHC) defines a qualified interpreter. "An individual who has been assessed for professional skills demonstrates a high level of proficiency in at least two languages and has the appropriate training and experience to interpret with skill and accuracy while adhering to the National Code of Ethics and Standards of Practice published by the National Council on Interpreting in Health Care" (2).
The terms healthcare interpreter and medical interpreter may be used interchangeably, as they both handle communication in the medical setting (9).

Self Quiz
Ask yourself...
- Can you identify the skills a medical interpreter needs?
- Are you able to define the role of the medical interpreter?
Medical Interpreters
Medical interpreters play a vital role in bridging gaps in healthcare. They promote effective communication between healthcare providers and the individuals who speak different languages, in their care. Most importantly, they address and eliminate language barriers that could result in serious medical errors.
It is common knowledge that language barriers present significant challenges for healthcare providers and medical professionals. Miscommunication between them and their patients can reduce provider and patient satisfaction, decrease the quality of care, and impact patient safety (3).
Medical interpreters promote effective communication by giving the patient a voice. They ensure patients receive the care they are entitled to and assist in avoiding medical errors that could harm the patient. They are essential in advocating for patients experiencing communication barriers (4).
The Importance of Medical Interpreters
As the role of a medical interpreter is to facilitate communication, they are needed in a variety of different situations, which could include (5).
- When a patient needs to provide consent.
- When a healthcare provider is gathering medical history.
- During physical exams.
- When a patient is describing pain or other symptoms.
- When the patient has questions or concerns.
- For treatment discussions and decisions.
- To understand discharge instructions.
These situations can occur in different sites that provide care to patients with language barriers and involve various settings such as (6):
- Hospitals
- Clinics
- Private medical offices
- Rehabilitation centers
- Nursing homes
- Long-term care facilities
- Assisted living facilities
- Mental health facilities
- Forensic services
- Substance abuse clinics
- Domestic violence centers or programs

Differences between the Medical Interpreter and the Medical Translator
It is essential to differentiate between a medical interpreter and a medical translator. While some may use these terms interchangeably, there are significant differences. While a medical interpreter assists in communication between people, a medical translator focuses on written text and content (1).
The interpreter will use spoken words, while the translator will use written words. Therefore, the significant difference is in the way they communicate. Medical interpreters are needed to explain and clarify important events related to healthcare.
Some examples include (1):
- Medical procedures
- Surgical procedures
- Aftercare instructions
- Discharge planning
- Doctor’s explanations and recommendations
Medical translators play an important role in translating written content from one language to another in (1):
- Medical records
- Patient charts
- Patient history
- Family history
- Health issues

Self Quiz
Ask yourself...
- Can you list five situations in which a medical interpreter would be required?
- Explain the role the medical interpreter plays in healthcare.
- What are some settings where a medical interpreter would be employed?
- Identify the differences between a medical interpreter and a medical translator.
Qualifications and Training
The role of the medical interpreter is a very specialized one. They are a crucial healthcare team member, and their services are vital to those they are working with. Therefore, they must possess specific skills, qualifications, training, and credentials.
To start becoming a medical interpreter, the following prerequisites must be met (6):
- Must be 18 years of age.
- General education: Must have proof of a United States high school diploma/GED or equivalent from another country.
- Oral proficiency in the English language.
- Oral proficiency in the target language.
- Medical Interpreter education.
Medical Interpreter education includes training obtained at a college or university and must be at least three credit hours. It may also be obtained through a training course which consists of at least 40 hours (6).

Self Quiz
Ask yourself...
- Can you name the prerequisites needed to begin the process of becoming a medical interpreter?
Certification
The next step is to become a certified medical interpreter. If the above requirements have been met, then certification can be pursued. The benefits of becoming a certified medical interpreter include being on the national registry and the respect that accompanies certification.
In addition, certification identifies the recipient as a competent professional, who understands and follows the standards of practice (9). Certification is becoming important as more employers prefer certified medical interpreters (9).
Two organizations provide professional certification for medical interpreters.
- Certification Commission for Healthcare Interpreters (CCHI) (7).
- National Board of Certification for Medical Interpreters (NBCMI) (8).
Certification Commission for Healthcare Interpreters (CCHI)
The CCHI recognized that certification is fundamental to the medical interpreter's career. The mission of this organization is “to develop and administer a comprehensive national certification program for healthcare interpreters, bringing together representatives from interpreting associations, language companies, community-based organizations, educational institutions, hospitals, health and healthcare providers, and advocates for patients with limited English proficiency (10).
This organization offers three types of national certification (7):
- Core Certification Healthcare Interpreter™ (CoreCHI)
This certification is available to interpreters in all languages and tests the core professional knowledge, critical thinking, ethical decision-making, and cultural responsiveness skills needed to perform duties in healthcare settings (11).
- CoreCHI-Performance™ (CoreCHI-P™)
This is considered the second level of certification for interpreters in all languages. The requirements include meeting the CCHIs language proficiency criteria and passing two tests: The knowledge CoreCHI™ exam and the monolingual performance ETOE™ (English-to-English) exam (11).
- Certified Healthcare Interpreter™ (CHI™)
This language-specific performance certification for Spanish, Arabic, and Mandarin interpreters focuses on interpreting skills and abilities (11).
All three certifications are valid for four years from the issue date. The certification must be renewed at that time to ensure that the medical interpreter remains current and updated in their profession (7).
National Board of Certification for Medical Interpreters (NBCMI)
The NBCMI recognizes that medical interpreters are vital care team members in assisting people with limited English proficiency. They help medical interpreters advance their careers by providing the following.
Hub-CMI Credential
This credential applies to medical interpreters of any language and is a national standard to determine mastery of medical terminology and specialties, cultural competencies, and ethical judgment. This credential is a written exam demonstrating a baseline competency and knowledge level in the medical interpreter profession. This credential must be renewed every four years (14).
CMI Certification
This certification is an oral exam and is offered in six languages, including Cantonese, Korean, Mandarin, Russian, Spanish, and Vietnamese. The candidate must have successfully passed the Hub-CMI (8) to take this exam. CMI certification aims to ensure that candidates meet the standards of the medical interpreter’s profession safely and ethically. This certification must be renewed every five years (15).

Self Quiz
Ask yourself...
- Can you describe the benefits of becoming a certified medical interpreter?
- Identify the two organizations that provide professional certification for medical interpreters.
- How would you compare the different certifications offered?
Nationwide Impact
Statistics
It is estimated that over 25 million Americans have limited English proficiency (LEP), putting them at risk for poor health outcomes due to language barriers (20). Some certain groups and populations have a higher risk for LEP. Those who do not speak English in their homes, immigrants, and those with lower educational levels identify as higher risk (21).
LEP creates barriers to accessing healthcare, understanding health information, and preventative health care. Also, LEP has been linked to chronic health conditions.
LEP patients have (21):
- More extended hospital stays (when interpreters were not used at admission and/or discharge).
- Greater risk for surgical infections.
- Greater risk for falls.
- Greater risk for pressure injuries.
- Greater risk for surgical delays.
- Greater risk for readmission for chronic conditions.
The need for medical interpreters is evident. They are essential for communication between providers and patients with LEP.
Demand
Medical interpreters are in high demand in the healthcare system. The employment of interpreters is projected to grow by four percent from 2022 to 2032 (19). While there are approximately 52,000 interpreters and translators in the United States, it is estimated that there will be 7,200 job openings for interpreters and translators each year in the upcoming decade (19).


Self Quiz
Ask yourself...
- Can you explain why those with LEP are at higher risk for poor health outcomes?
- Are you able to identify why there is an increased need for Medical Interpreters?
Standards of Practice
Medical and healthcare interpreting is a distinct and specialized area of work. Standards of practice guide interpreters in their practice and improve the quality and consistency of interpreting (12).
In the past, interpreters lacked guidance for performance requirements, resulting in the quality of interpreting being inconsistent. This inconsistency led to incomplete and inaccurate communication during interpretation. The development of standards resulted from the need for clarity and consistency at a national level in defining the characteristics and competencies of a qualified healthcare interpreter (12).
Professional organizations such as the National Council on Interpreting in Health Care (NCIHC) and the International Medical Interpreters Association (IMIA) establish these standards. Adherence to these standards is vital for maintaining the integrity of medical interpretation services and promoting positive healthcare outcomes for patients with limited English proficiency.
The NCIHC Standards of Practice
The National Council on Interpreting in Health Care (NCIHC) developed the National Code of Standards for Interpreters in Health Care (16). These standards are used as a reference by interpreters, and those who work with and train the interpreters. They also serve as an important guide to the practice of all interpreters (12).
The standards of practice are used for (12).
- Training
- Hiring
- Performance Monitoring
- Discussion on Certification of Professional Competence
The NCIHC Standards of Practice are organized in nine areas consisting of the following (16).
- Accuracy
- Confidentiality
- Impartiality
- Respect
- Cultural Awareness
- Role Boundaries
- Professionalism
- Professional Development
- Advocacy
The International Medical Interpreters Association (IMIA)
The International Medical Interpreters Association (IMIA) has also developed standards that assist in maintaining the integrity of medical interpretation and promoting positive healthcare outcomes for those with limited English (17).
These standards are used for the following reasons (18).
- Guidance in the development of educational and training programs.
- Evaluation tool.
- Assist healthcare providers in working with interpreters.
- Foundation for certificate examination.
The IMIA Standards of Practice are organized in three major areas.
- Interpretation
- Cultural Interface
- Ethical Behavior

Self Quiz
Ask yourself...
- What are the organizations that developed Standards of Practice for medical interpreters?
- What are Standards of Practice used for?
- Consider how a medical interpreter can promote cultural understanding.
Code of Ethics
Ethical behavior is essential in all professions, and medical interpreters must follow professional codes. Ethics are principles and values which govern the conduct of members of a profession. The NCIHC, IMIA, and the CHIA provide a Code of Ethics for medical interpreters.
They are very similar and address the following areas (22):
- Accuracy
- Confidentiality
- Respect
- Professionalism
- Professional Development
- Role Boundaries
- Impartiality
- Cultural Awareness
- Advocacy
- Communication Flow
- Accepting Gifts

Self Quiz
Ask yourself...
- Define the purpose of the Code of Ethics for the medical interpreter.
- List the organizations that provide a Code of Ethics for medical interpreters.
Policies
As a result of the growing number of LEP patients, and the need to provide equal treatment to these individuals, language service policies addressing communication barriers and language gaps have been established. In addition, policies have been developed to mandate the practice of interpreter services (24). By offering access to medical interpreters, healthcare organizations achieve the goals of delivering culturally competent care and maintaining legal and regulatory compliance.
In the United States, it is a right for all individuals to have access to language services, and no one should be denied care or services because of a language barrier (28).
These rights originate from two laws (13):
- The Civil Rights Act of 1964
- Executive Order 13166
The Civil Rights Act of 1964
In 1964, Title VI of the Civil Rights Act was passed. This gave LEP individuals a legal right to language assistance services and prohibited discrimination (27).
Executive Order 13166
In 2000, the Executive Order (EO) 13166, Improving Access to Services for Persons with Limited English Proficiency, was issued (27). This order mandated laws requiring professional interpreters to be present in healthcare facilities receiving federal funding (28).
Both laws ensure that access to language services is a right and that no one can be denied services based on the language they speak (28).
What Nurses Need to Know
Effective communication is essential in healthcare. With over 25 million people having LEP, many nurses may encounter a patient with communication barriers. These language barriers can affect nursing practice and the care provided by nurses. There is abundant evidence indicating that language barriers impact patient outcomes. Nurses can make a difference by responding to the communication needs of patients with LEP by using a medical interpreter (26).
Nurses can improve health outcomes for LEP patients by effectively working with medical interpreters. To achieve this, nurses should know the standards, guidelines, and policies of working with a medical interpreter.
Some guidance for working effectively with medical interpreters includes these evidence-based interventions (25,26):
- Identify patients needing an interpreter in advance.
- Inform the interpreter of the specific language needed.
- Inform the interpreter how much time the interpretation will take.
- Introduce yourself to the interpreter and provide a report on the work needed.
- Provide a brief patient history.
- Greet the patient and introduce the interpreter.
- Explain to the patient the reason for the interpretation.
- Communicate directly to the patient.
- Have the interpreter sit next to or behind the patient.
- Speak in short sentences.
- If the interpreter appears confused, ask them if they need clarification or rephrasing.
- Do not interrupt the interpreter when they are translating.
- When the session is finished, ask the patient if they need anything else while the interpreter is present.
- After leaving the patient’s room, review the session with the interpreter, as they may have cultural insights helpful to care planning.
Nurses must advocate for their patients by bridging language barriers and providing optimal care. Utilizing medical interpreters and implementing evidence-based strategies can assist nurses in providing quality care by eliminating language barriers (26).
Resources
The U.S. Department of Health and Human Services provides an example of a policy and procedure for giving meaningful communication with persons with limited English proficiency (23).

Self Quiz
Ask yourself...
- Can you discuss how the nurse can improve health outcomes for the LEP patient?
- List ten evidence-based interventions used to work with medical interpreters effectively.
- How can nurses advocate for LEP patients?
- Explain the importance of the Civil Rights Act of 1964.
- Explain the importance of Executive Order 13166.
Conclusion
The role of the medical interpreter is an important one. As the need for professional and certified medical interpreters grows, healthcare organizations must realize this. Medical interpreters are very significant members of the healthcare team. They assist in eliminating one of the most challenging barriers faced by providers: language barriers.
It is common knowledge that language barriers cause miscommunication, resulting in poor outcomes for all. Medical interpreters improve many aspects of healthcare, by assisting in overcoming cultural and language barriers, encouraging effective communication, and improving overall patient safety and satisfaction. As the need for their services grows, so should recognition of the importance of their work.
References + Disclaimer
- Yu H, Flores DD, Bonett S, Bauermeister, JA. LGBTQ+ cultural competency training for health professionals: a systematic review. BMC Medical Education. 2023;23:558:1-83.
- Morris, M., Cooper, R.L., Ramesh, A. et al. Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC Med Educ 19, 325 (2019). https://doi.org/10.1186/s12909-019-1727-3
- Waisel DB. Vulnerable populations in healthcare. Curr Opin Anesthesiol. 2013;26(2):186–92.
- Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: Trends over the past 10 years. NCHS Data Brief. 2012;2012(100):1–8.
- Institute of Medicine. Collecting sexual orientation and gender identity data in electronic health records: workshop summary. Washington DC: National Academy of Sciences; 2013.
- Quinn GP, Sanchez JA, Sutton SK, Vadaparampil ST, Nguyen GT, Green BL, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA-Cancer J Clin. 2015;65(5):384–400
- Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–60.
- Dilley JA, Simmons KW, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific northwest. Am J Public Health. 2010;100(3):460–7.
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health. 2013;103(10):1802–9.
- Bauermeister J, Eaton L, Stephenson R. A multilevel analysis of neighborhood socioeconomic disadvantage and transactional sex with casual partners among Young men who have sex with men living in metro Detroit. Behav Med. 2016;42(3):197–204.
- Smalley KB, Warren JC, Barefoot KN. Differences in health risk behaviors across understudied LGBT subgroups. Health Psychol. 2016;35(2):103–14.
- Staats C, Capatosto K, Wright RA, Jackson VW. State of the science: Implicit bias review 2016. Columbus: Kirwan Institute.
- Cochran SD, Bandiera FC, Mays VM. Sexual orientation-related differences in tobacco use and secondhand smoke exposure among US adults aged 20 to 59 years: 2003-2010 National Health and nutrition examination surveys. Am J Public Health. 2013;103(10):1837–44.
- Ramchand, R., Schuler, M. S., Schoenbaum, M., Colpe, L., & Ayer, L. (2021). Suicidality among sexual minority adults: Gender, age, and race/ethnicity differences. American Journal of Preventive Medicine. https://doi.org/10.1016/j.amepre.2021.07.012
- Charlton BM, Corliss HL, Missmer SA, Frazier AL, Rosario M, Kahn JA, et al. Reproductive health screening disparities and sexual orientation in a cohort study of U.S. adolescent and Young adult females. J Adolesc Health. 2011;49(5):505–10.
- Agénor M, Krieger N, Austin SB, et al. Sexual Orientation Disparities in Papanicolaou Test Use Among US Women: The Role of Sexual and Reproductive Health Services. Am J Public Health. 2014;104(2):e68-72
- Tracy JK, Lydecker AD, Ireland L. Barriers to cervical Cancer screening among lesbians. J Women’s Health. 2010;19(2):229–37.
- Safer JD, Coleman E, Feldman J, Garofalo R, Hembree W, Radix A, Sevelius J. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016 Apr;23(2):168-71. doi: 10.1097/MED.0000000000000227. PMID: 26910276; PMCID: PMC4802845.
- Heck JE, Sell RL, Gorin SS. Health care access among individuals involved in same-sex relationships. Am J Public Health. 2006;96(6):1111–8.
- Kamen C, Palesh O, Gerry AA, Andrykowski MA, Heckler C, Mohile S, et al. Disparities in health risk behavior and psychological distress among gay versus heterosexual male Cancer survivors. LGBT Health. 2014;1(2):86–U103.
- Legal L. When health care Isn’t caring: lambda Legal’s survey of discrimination against LGBT people and people with HIV. New York: Lamba Legal; 2010.
- Grant JM, Mottet LA, Tanis J. National Transgender Discrimination Survey Report on health and health care. Washington DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2010.
- Shires DA, Jaffee K. Factors associated with health care discrimination experiences among a National Sample of female-to-male transgender individuals. Health Soc Work. 2015;40(2):134–41.
- Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians’ experiences in the workplace. J Homosex. 2011;58(10):1355–71.
- Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54.
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
- Mereish EH, Bradford JB. Intersecting identities and substance use problems: sexual orientation, gender, race, and lifetime substance use problems. J Stud Alcohol Drugs. 2014;75(1):179–88.
- Torres CG, Renfrew M, Kenst K, Tan-McGrory A, Betancourt JR, Lopez L. Improving transgender health by building safe clinical environments that promote existing resilience: results from a qualitative analysis of providers. BMC Pediatr. 2015;15:187.
- Burke SE, Dovidio JF, Przedworski JM, Hardeman RR, Perry SP, Phelan SM, et al. Do contact and empathy mitigate Bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. 2015;90(5):645–51.
- Sabin JA, Riskind RG, Nosek BA. Health care Providers’ implicit and explicit attitudes toward lesbian women and gay men. Am J Public Health. 2015;105(9):1831–41.
- Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–7.
- Wilson TD, Brekke N. Mental contamination and mental correction: unwanted influences on judgments and evaluation. Psychol Bull. 1994;116(1):117–42.
- Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit Bias in health care: a narrative review. Group Proccess Interg. 2016;19(4):528–42.
- Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102(1):4–27.
- Van Ryn M, Saha S. Exploring unconscious bias in disparities research and medical education. JAMA. 2011;306(9):995–6.
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41.
- Nosek BA, Riskind RG. Policy implications of implicit social cognition. Soc Issue Policy Rev. 2012;6(1):113–47.
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
- Shavers VL, Fagan P, Jones D, Klein WMP, Boyington J, Moten C, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953–66.
- Chapman EN, Kaatz A, Carnes M. Physicians and implicit Bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–10.
- Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: Confronting racial and ethnic disparities in health care. Brian D. Smedley, Adrienne Y. Stith, and Alan R. Nelson, Editors; Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Board on Health Sciences Policy; Institute of Medicine. Washington, DC; 2003.
- Greenwald AG, Banaji MR, Nosek BA. Statistically small effects of the implicit association test can have societally large effects. J Pers Soc Psychol. 2015;108(4):553–61.
- Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P. (2019). Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC medical education, 19(1), 325. https://doi.org/10.1186/s12909-019-1727-3
- Human rights campaigns. Glossary of terms. Retrieved from https://www.hrc.org/resources/glossary-of-terms
- Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community, a field guide. Joint Commission. Retrieved from https://www.jointcommission.org/ /media/enterprise/tjc/imported-resource assets/documents/lgbtfieldguide_web_linked_verpdf.pdf?db=web hash=1EC363A65C710BCD1D4E14ED120CB2
- Delivering culturally sensitive care to LGBTQI Patients. The Journal for nurse practitioners. Volume 13, issue 5 p342-347.
- Arts, E. J., & Hazuda, D. J. (2012). HIV-1 antiretroviral drug therapy. Cold Spring Harbor perspectives in medicine, 2(4), a007161. https://doi.org/10.1101/cshperspect.a007161.
- Avert. (2019). History of HIV and AIDS overview. Retrieved from: https://www.avert.org/professionals/history-hiv-aids/overview
- Bhatti, A. B., Usman, M., & Kandi, V. (2016). Current Scenario of HIV/AIDS, Treatment Options, and Major Challenges with Compliance to Antiretroviral Therapy. Cureus, 8(3), e515. https://doi.org/10.7759/cureus.515
- Centers for Disease Control. (2016). Today‘s HIV/AIDS epidemic. Retrieved from: https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508.pdf
- Centers for Disease Control. (2019). HIV cost effectiveness. Retrieved from: https://www.cdc.gov/hiv/programresources/guidance/costeffectiveness/index.html.
- Centers for Disease Control. (2020). Evidence of HIV treatment and viral suppression in preventing the sexual transmission of HIV. Retrieved from: https://www.cdc.gov/hiv/pdf/risk/art/cdc-hiv-art-viral-suppression.pdf
- Centers for Disease Control. (2020). HIV. Retrieved from: https://www.cdc.gov/hiv/basics/whatishiv.html
- Centers for Disease Control. (2020). Sharing your test results. Retrieved from: https://www.cdc.gov/hiv/basics/hiv-testing/sharing-test-results.html/
- Currier, J. S., & Havlir, D. V. (2017). CROI 2017: Complications and Comorbidities of HIV Disease and Its Treatment. Topics in antiviral medicine, 25(2), 77–83.
- HIV.gov. (2020). U.S. statistics. Retrieved from: https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics
- Nursing Times. (2020). HIV: epidemiology, pathophysiology, and transmission. Retrieved from: https://www.nursingtimes.net/clinical-archive/immunology/hiv-1-epidemiology-pathophysiology-and-transmission-15-06-2020/
- Vaillant, A. J. and Guilick, P. G. (2020). HIV disease current practice. Statpearls. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK534860/.
- Diab, A., Dastmalchi, L. N., Gulati, M., & Michos, E. D. (2023). A Heart-Healthy Diet for cardiovascular Disease Prevention: Where are we now? Vascular Health and Risk Management, Volume 19, 237–253. https://doi.org/10.2147/vhrm.s379874
- Cena, H., & Calder, P. C. (2020). Defining a Healthy Diet: Evidence for the role of contemporary dietary patterns in Health and disease. Nutrients, 12(2), 334. https://doi.org/10.3390/nu12020334
- Diab, A., Dastmalchi, L. N., Gulati, M., & Michos, E. D. (2023). A Heart-Healthy Diet for cardiovascular Disease Prevention: Where are we now? Vascular Health and Risk Management, Volume 19, 237–253. https://doi.org/10.2147/vhrm.s379874
- World Health Organization: WHO. (2019, June 11). Cardiovascular diseases. https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1
- Yusuf S., Hawken S., Ounpuu S., Dans T., Avezum A., Lanas F., McQueen M., Budaj A., Pais P., Varigos J., et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004; 364:937–952. doi: 10.1016/S0140-6736(04)17018-9.
- Akesson A., Weismayer C., Newby P.K., Wolk A. Combined effect of low-risk dietary and lifestyle behaviors in primary prevention of myocardial infarction in women. Arch. Intern. Med. 2007; 167:2122–2127. doi: 10.1001/archinte.167.19.2122
- Ford E.S., Bergmann M.M., Kröger J., Schienkiewitz A., Weikert C., Boeing H. Healthy living is the best revenge: Findings from the European Perspective Investigation into Cancer and Nutrition-Potsdam study. Arch. Intern. Med. 2009; 169:1355–1362. doi: 10.1001/archinternmed.2009.237.
- Chiuve S.E., McCullough M.L., Sacks F.M., Rimm E.B. Healthy lifestyle factors in the primary prevention of coronary heart disease among men: Benefits among users and nonusers of lipid-lowering and antihypertensive medications. Circulation. 2006; 114:160–167. doi: 10.1161/CIRCULATIONAHA.106.621417
- National Library of Medicine. (2022). Heart diseases. https://medlineplus.gov/heartdiseases.html
- Sharifi‐Rad, J., Rodrigues, C. F., Sharopov, F., Docea, A. O., Karaça, A. C., Sharifi‐Rad, M., Karıncaoglu, D. K., Gülseren, G., Şenol, E., Demircan, E., Taheri, Y., Suleria, H. a. R., Özçelik, B., Kasapoğlu, K. N., Gültekin-Özgüven, M., Daşkaya-Dikmen, C., Cho, W. C., Martins, N., & Calina, D. (2020). Diet, Lifestyle and Cardiovascular Diseases: Linking pathophysiology to cardioprotective effects of natural bioactive compounds. International Journal of Environmental Research and Public Health, 17(7), 2326. https://doi.org/10.3390/ijerph17072326
- Chacko, M., Sarma, P. S., Harikrishnan, S., Zachariah, G., & Jeemon, P. (2020). Family history of cardiovascular disease and risk of premature coronary heart disease: A matched case-control study. Welcome Open Research, 5, 70. https://doi.org/10.12688/wellcomeopenres.15829.2
- Holvoet P. Stress in obesity and associated metabolic and cardiovascular disorders. Scientifica. 2012; 2012:205027. doi: 10.6064/2012/205027
- Casas, R., Castro‐Barquero, S., Estruch, R., & Sacanella, E. (2018). Nutrition and cardiovascular health. International Journal of Molecular Sciences, 19(12), 3988. https://doi.org/10.3390/ijms19123988
- Coronary artery disease – Symptoms and causes – Mayo Clinic. (2022, May 25). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/symptoms-causes/syc-20350613
- NHS inform. (2023, November 9). Cardiovascular disease – Illnesses & conditions | NHS inform. NHS Inform. https://www.nhsinform.scot/illnesses-and-conditions/heart-and-blood-vessels/conditions/cardiovascular-disease/
- Data and Statistics on Congenital Heart Defects | CDC. (2023, September 19). Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/heartdefects/data.html
- Valvular heart Disease | Cdc.gov. (2019, December 9). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/valvular_disease.htm
- What is heart failure? | NHLBI, NIH. (2022, March 24). NHLBI, NIH. https://www.nhlbi.nih.gov/health/heart-failure
- Heart failure signs and symptoms. (2023, October 18). www.heart.org. https://www.heart.org/en/health-topics/heart-failure/warning-signs-of-heart-failure
- What is cardiomyopathy? | NHLBI, NIH. (2022, April 19). NHLBI, NIH. https://www.nhlbi.nih.gov/health/cardiomyopathy
- Cardiomyopathy | cdc.gov. (2023, February 21). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/cardiomyopathy.htm
- Khandaker, M. H., Espinosa, R. E., Nishimura, R. A., Sinak, L. J., Hayes, S. N., Melduni, R. M., & Oh, J. K. (2010). Pericardial Disease: Diagnosis and management. Mayo Clinic Proceedings, 85(6), 572–593. https://doi.org/10.4065/mcp.2010.0046
- What is an arrhythmia? | NHLBI, NIH. (2022, March 24). NHLBI, NIH. https://www.nhlbi.nih.gov/health/arrhythmias
- Atrial fibrillation | Cdc.gov. (2022, October 14). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
- Harris, C., Croce, B., & Cao, C. (2016). ACS Patient Page Type A aortic dissection. Annals of Cardiothoracic Surgery, 5(4), 256. https://doi.org/10.21037/acs.2016.05.04
- Milner, R., MD. (2022, January 25). What is aortic dissection: What you need to know about the causes, types and more. UChicago Medicine. https://www.uchicagomedicine.org/forefront/heart-and-vascular-articles/silent-killer-everything-you-need-to-know-about-aortic-dissection
- Yu, E., Rimm, E. B., Qi, L., Rexrode, K. M., Chen, A., Sun, Q., Willett, W. C., Hu, F. B., & Manson, J. E. (2016). Diet, lifestyle, biomarkers, genetic factors, and risk of cardiovascular disease in the nurses’ health studies. American Journal of Public Health, 106(9), 1616–1623. https://doi.org/10.2105/ajph.2016.303316
- Lichtenstein, A. H., Appel, L. J., Vadiveloo, M., Hu, F. B., Kris‐Etherton, P. M., Rebholz, C. M., Sacks, F. M., Thorndike, A. N., Van Horn, L., Wylie‐Rosett, J., & Biology, V. (2021). 2021 Dietary Guidance to Improve Cardiovascular Health: A scientific statement from the American Heart Association. Circulation, 144(23). https://doi.org/10.1161/cir.0000000000001031
- Schwingshackl L, Schwedhelm C, Hoffmann G, Boeing H. Potatoes, and risk of chronic disease: a systematic review and dose-response meta-analysis. Eur J Nutr. 2019; 58:2243–2251. doi: 10.1007/s00394-018-1774-2
- Preventing heart disease. (2023, February 2). The Nutrition Source. https://www.hsph.harvard.edu/nutritionsource/disease-prevention/cardiovascular-disease/preventing-cvd/
- Tosh SM, Bordenave N. Emerging science on benefits of whole grain oat and barley and their soluble dietary fibers for heart health, glycemic response, and gut microbiota. Nutr Rev. 2020; 78(suppl 1):13–20. doi: 10.1093/nutrit/nuz085
- Voskoboinik A, Kalman JM, De Silva A, Nicholls T, Costello B, Nanayakkara S, Prabhu S, Stub D, Azzopardi S, Vizi D, et al. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med. 2020; 382:20–28. doi: 10.1056/NEJMoa1817591
- Hardy DS, Garvin JT, Xu H. Carbohydrate quality, glycemic index, glycemic load and cardiometabolic risks in the US, Europe, and Asia: a dose-response meta-analysis. Nutr Metab Cardiovasc Dis. 2020; 30:853–871. doi: 10.1016/j.numecd.2019.12.050
- Sacks FM, Lichtenstein AH, Wu JHY, Appel LJ, Creager MA, Kris-Etherton PM, Miller M, Rimm EB, Rudel LL, Robinson JG, et al; American Heart Association. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. 2017; 136: e1–e23. doi: 10.1161/CIR.0000000000000510
- Chiavaroli, L., Viguiliouk, E., Nishi, S. K., Mejía, S. B., Rahelić, D., Kahleová, H., Salas‐Salvadó, J., Kendall, C. W., & Sievenpiper, J. L. (2019). DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients, 11(2), 338. https://doi.org/10.3390/nu11020338
- Satija, A., & Hu, F. B. (2018). Plant-based diets and cardiovascular health. Trends in Cardiovascular Medicine, 28(7), 437–441. https://doi.org/10.1016/j.tcm.2018.02.004
- Wang DD, Hu FB. Dietary fat and risk of cardiovascular disease: recent controversies and advances. Annu Rev Nutr. 2017; 37:423–446. doi: 10.1146/annurev-nutr-071816-064614
- Eckel RH, Borra S, Lichtenstein AH, Yin-Piazza SY; Trans Fat Conference Planning Group. Understanding the complexity of trans fatty acid reduction in the American diet: American Heart Association Trans Fat Conference 2006: report of the Trans Fat Conference Planning Group. Circulation. 2007; 115:2231–2246. doi: 10.1161/CIRCULATIONAHA.106.181947
- Heart-healthy diet: 8 steps to prevent heart disease. (2022, April 28). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/heart-disease/in-depth/heart-healthy-diet/art-20047702
- Bhattad, P. B., & Pacifico, L. (2022). Empowering patients: Promoting patient education and health literacy. Cureus. https://doi.org/10.7759/cureus.27336
- Pem, D. (2015, October 1). Fruit and Vegetable Intake: Benefits and Progress of Nutrition Education Interventions- Narrative Review article. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4644575/
- Marcus, C. (2014). Strategies for improving the quality of verbal patient and family education: a review of the literature and creation of the EDUCATE model. Health Psychology and Behavioral Medicine, 2(1), 482–495. https://doi.org/10.1080/21642850.2014.900450
- Woodgate, R. L., & Sigurdson, C. (2015). Building school-based cardiovascular health promotion capacity in youth: a mixed methods study. BMC Public Health, 15(1). https://doi.org/10.1186/s12889-015-1759-5
- Trichopoulou, A., Martínez‐González, M. A., Tong, T. Y., Forouhi, N. G., Khandelwal, S., Prabhakaran, D., Mozaffarian, D., & De Lorgeril, M. (2014). Definitions and potential health benefits of the Mediterranean diet: views from experts around the world. BMC Medicine, 12(1). https://doi.org/10.1186/1741-7015-12-112
- Challa, H. J. (2023, January 23). DASH Diet to Stop Hypertension. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482514/
- Childs, C. E., Calder, P. C., & Miles, E. A. (2019). Diet and immune function. Nutrients, 11(8), 1933. https://doi.org/10.3390/nu11081933
- Centers for Disease Control and Prevention (CDC) (2023). Fast Facts: Preventing Adverse Childhood Experiences. https://www.cdc.gov/violenceprevention/aces/fastfact.html
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. https://doi.org/10.1016/S0749-3797(98)00017-8.
- Starecheski, L. (2015). Take the ACE quiz—And learn what it does and doesn’t mean. NPR. https://www.npr.org/sections/health-shots/2015/03/02/387007941/take-the-ace-quiz-and-learn-what-it-does-and-doesnt-mean
- Center on the Developing Child at Harvard University (n.d.). What are ACEs? And how do they relate to toxic stress? https://developingchild.harvard.edu/resources/aces-and-toxic-stress-frequently-asked-questions/
- CDC, (2022). About the CDC-Kaiser ACE study. https://www.cdc.gov/violenceprevention/aces/about.html
- CDC. (2021). Preventing adverse childhood experiences. https://www.cdc.gov/vitalsigns/aces/index.html
- CDC (2023). Risk and protective factors. https://www.cdc.gov/violenceprevention/aces/riskprotectivefactors.html
- Cleveland Clinic (2023). Adverse childhood experiences (ACEs) & childhood trauma. (2023). https://my.clevelandclinic.org/health/symptoms/24875-adverse-childhood-experiences-ace
- Merrick, M. T. (2019). Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention — 25 States, 2015–2017. Morbidity and Mortality Weekly Report, 68. https://doi.org/10.15585/mmwr.mm6844e1
- Child Trends. (2018). American Indians and Alaska Natives must be included in research on adverse childhood experiences. https://www.childtrends.org/blog/american-indians-alaska-natives-adverse-childhood-experiences
- Hughes, K., Bellis, M.A., Hardcastle, K.A., Sethi, D., Butchart, A., Mikton, C., Jones, L., Dunne, M.P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health; 2(8): e356-e366. doi: 10.1016/S2468-2667(17)30118-4.
- CDC (2023). Leading causes of death. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
- Merrick, M. T., Ports, K. A., Ford, D. C., Afifi, T. O., Gershoff, E. T., & Grogan-Kaylor, A. (2017). Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse & Neglect, 69, 10–19. https://doi.org/10.1016/j.chiabu.2017.03.016
- Center on the Developing Child at Harvard University (n.d.). Take the ACE quiz – And learn what it does and doesn’t mean. https://developingchild.harvard.edu/media-coverage/take-the-ace-quiz-and-learn-what-it-does-and-doesnt-mean/
- National Conference of State Legislatures (2022). Adverse Childhood Experiences. https://www.ncsl.org/health/adverse-childhood-experience
- National Center for Missing & Exploited Children (2023). CyberTipline http://www.missingkids.org/content/ncmec/en/gethelpnow/cybertipline.html
- Dowdell, E. B., & Speck, P. M. (2022). Ce: Trauma-informed care in nursing practice. AJN, American Journal of Nursing, 122(4), 30–38. https://doi.org/10.1097/01.naj.0000827328.25341.1f
- Eilers, H., aan het Rot, M., & Jeronimus, B. F. (2023). Childhood trauma and adult somatic symptoms. Psychosomatic Medicine, 85(5), 408–416. https://doi.org/10.1097/psy.0000000000001208
- Fleishman, J., Kamsky, H., & Sundborg, S. (2019). Trauma-informed nursing practice. OJIN: The Online Journal of Issues in Nursing, 24(2). https://doi.org/10.3912/ojin.vol24no02man03
- Purkey, E., Patel, R., & Phillips, S. P. (2018). Trauma informed care better care for everyone. Canadian Family Physician, 64(3), 170–172.
- Schulman, M., & Menschner, C. (2018, November 9). Laying the groundwork for trauma-informed care [PDF]. Trauma-Informed Care Implementation Resource Center. https://www.traumainformedcare.chcs.org/wp-content/uploads/2018/11/Brief-Laying-the-Groundwork-for-TIC.pdf
- Sweeney, A., & Taggart, D. (2018). (Mis)understanding trauma-informed approaches in mental health. Journal of Mental Health, 27(5), 383–387. https://doi.org/10.1080/09638237.2018.1520973
- National Institute on Aging. (2021) What is Lewy Body Dementia? Causes, Symptoms, and Treatments. Retrieved on December 5, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/what-lewy-body-dementia-causes-symptoms-and-treatments
- Medline Plus [Internet] National Library of Medicine. (2021). Dementia with Lewy Bodies. Retrieved on December 5, 2023, from https://medlineplus.gov/genetics/condition/dementia-with-lewy-bodies/#causes
- Haider, A., Spurlin, B., and Sanchez-Manso, J. (2023). Lewy Body Dementia. In StatPearls. StatPearls [Internet]. Retrieved on December 7, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK482441/
- Prasad, S., Katta, M., Abhishek, S., Sridhar, R., Valisekka, S., Hameed, M., Kaur, J., and Walia, N. (2022). Disease-a-Month. Vol. 69, Issue 5, May 2023, 101441. Retrieved from https://www.sciencedirect.com/science/article/pii/S0011502922001250?via%3Dihub
- Medline Plus [Internet] National Library of Medicine. (2019). Lewy Body Dementia. Retrieved on December 7, 2023, from https://medlineplus.gov/lewybodydementia.html
- Hershey, L. and Coleman-Jackson, R. (2019). Pharmacological Management of Dementia with Lewy Bodies. Drugs Aging. 2019; 36(4) 309-319. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6435621/
- National Institute on Aging. (2018). Caring for a Person with Lewy Body Dementia. Retrieved on December 21, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/caring-person-lewy-body-dementia
- Capouch, S., Farlow, M., and Brosch, J. (2018). A Review of Dementia with Lewy Bodies’ Impact, Diagnostic Criteria and Treatment. Neurology and Therapy. 2018 Dec; 7(2): 249-263. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6283803/
- Lewy Body Dementia Resource Center. (2021) Our Mission & Vision. Retrieved on December 21, 2023, from https://lewybodyresourcecenter.org/about-us/mission/
- Lewy Body Dementia Association. (2023). About LBDA. Retrieved on December 20, 2023 from https://www.lbda.org/about-lbda/
- National Institute of Neurological Disorders and Stroke. (2023) Focus on Lewy BOdy Dementia (LBD). Retrieved on December 20, 2023, from https://www.ninds.nih.gov/current-research/focus-disorders/alzheimers-disease-and-related-dementias/focus-lewy-body-dementia-lbd-research
- National Institute of Neurological Disorders and Stroke. (2018). PDBP About. Retrieved on December 21, 2023, from https://pdbp.ninds.nih.gov/about
- Bousiges, O. and Blanc, F. (2022). Biomarkers of Dementia with Lewy Bodies: Differential Diagnostic with Alzheimer’s Disease. International Journal of Molecular Sciences. 2022 Jun; 23 (12): 6371. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9223587/
- Howell, M. and Schenk, C. Rapid Eye movement sleep behavior disorder. 2023) UpToDate. Retrieved on December 21, 2023 from https://www.uptodate.com/contents/rapid-eye-movement-sleep-behavior-disorder/print#:~:text=INTRODUCTION%20Rapid%20eye%20movement%20(REM,thrashing%2C%20punching%2C%20and%20kicking.
- Arevalo, I., Smailagic, N., Roque I Figuls, M., Ciapponi, A., Sanchez-Perez, E., Giannakou, A., Pedraza, O., Cosp, X., and Cullum, S. (2015). Mini-Mental State Examination (MMSE) FOR THE DETECTION OF Alzheimer’s disease and other dementia in people with milk cognitive impairment (MCI). Cochrane Library. 2015 Mar; 2015(30): CD010783. Retrieved from https://doi.org/10.1002/14651858.CD010783.pub2
- National Institute on Aging. (2021). Diagnosing Lewy Body Dementia: For Professionals. Retrieved on December 22, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/diagnosing-lewy-body-dementia-professionals
- Anders, H., Ramesh, S., Ming-hui, Z., Ioannis, P., Salmon, J. E., & Mohan, C. (2020). Lupus nephritis (Primer). Nature Reviews: Disease Primers, 6(1). https://doi.org/10.1038/s41572-019-0141-9
- Arnaud, Laurent., & Vollenhoven, R. van. (2018). Advanced handbook of systemic lupus erythematosus. Adis. https://doi.org/10.1007/978-3-319-43035-5
- Hailemariam, F., Falkner, B. (2022). Renal Physiology for Primary Care Clinicians. In: McCauley, J., Hamrahian, S.M., Maarouf, O.H. (eds) Approaches to chronic kidney disease. Springer, Cham. https://doi.org/10.1007/978-3-030-83082-3_1
- Jaryal, A., & Vikrant, S. (2017). Current status of lupus nephritis. The Indian journal of medical research, 145(2), 167–178. https://doi.org/10.4103/ijmr.IJMR_163_16
- Kalantar-Zadeh, K., Mitch, W.E., Fadem, S.Z. (2022). Diet to preserve kidney function. In: Fadem, S.Z. (eds) Staying Healthy with Kidney Disease. Springer, Cham. https://doi.org/10.1007/978-3-030-93528-3_7 Maarouf, O.H. (2022). Lupus nephritis. In: McCauley, J., Hamrahian, S.M., Maarouf, O.H. (eds) Approaches to Chronic Kidney Disease . Springer, Cham. https://doi.org/10.1007/978-3-030-83082-3_10
- Parodis, I., & Sjöwall, C. (Eds.). (2023). Clinical Features and Long-Term Outcomes of Systemic Lupus Erythematosus. MDPI – Multidisciplinary Digital Publishing Institute.
- Pryor, K. P., Barbhaiya, M., Costenbader, K. H., & Feldman, C. H. (2021). Disparities in Lupus and Lupus Nephritis Care and Outcomes Among US Medicaid Beneficiaries. Rheumatic diseases clinics of North America, 47(1), 41–53. https://doi.org/10.1016/j.rdc.2020.09.004
- Usman N, Annamaraju P. (2023). Type III hypersensitivity reaction. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559122/
- Harris, J.C., Leggio, L., Farokhnia, M. (2021). Blood biomarkers of alcohol use: a scoping review. Current Addiction Reports, 8(4), 500-508. https://doi.org/10.1007/s40429-021-00402-7
- Johns Hopkins Medicine. (2023). CAGE substance abuse screening tool. Retrieved from: https://www.hopkinsmedicine.org/-/media/johns-hopkins-health-plans/documents/all_plans/cage-substance-screening-tool.pdf
- Nathan, P.E., Wallace, J., Zweben, J., Horvath, A. T. (2018). Understanding alcohol use disorders and their treatment. Retrieved from: https://www.apa.org/topics/substance-use-abuse-addiction/alcohol-disorders.
- National Cancer Institute. (2021). Alcohol and cancer risk. Retrieved from: https://www.cancer.gov/about-cancer/causes-prevention/risk/alcohol/alcohol-fact-sheet.
- National Institute on Alcohol Abuse and Alcoholism. (2023). Alcohol’s effects on the body. Retrieved from: https://www.niaaa.nih.gov/alcohols-effects-health/alcohols-effects-body.
- National Institute on Alcohol Abuse and Alcoholism. (2023). Goal 3: prevention. Retrieved from: https://www.niaaa.nih.gov/strategic-plan/prevention.
- National Institute on Alcohol Abuse and Alcoholism. (2023). Understanding alcohol use disorder. Retrieved from: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-alcohol-use-disorder.
- National Institute on Drug Abuse. (2023). AUDIT. Retrieved from: https://nida.nih.gov/sites/default/files/files/AUDIT.pdf.
- Nehring, S.M., Chen, R. J., Freeman A.M. (2023). Alcohol use disorder. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK436003/.
- Substance Abuse and Mental Health Services Administration, National Institute on Alcohol Abuse and Alcoholism. (2015). Medication for the treatment of alcohol use disorder: a brief guide. Retrieved from: https://store.samhsa.gov/sites/default/files/sma15-4907.pdf.
- Thompson, W., Lande, R. G., Kalapatapu, R.K. (2020). What are the DSM-5 criteria for alcohol use disorder? Retrieved from: https://www.medscape.com/answers/285913-41535/what-are-the-dsm-5-criteria-for-%20alcohol-use-disorder?form=fpf.
- World Health Organization. (2023). AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care. Retrieved from: https://www.who.int/publications/i/item/WHO-MSD-MSB-01.6a.
- American Nurses Association (ANA). (2015). Code of ethics with interpretative statements. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/
- Baptiste, D. L., Caviness-Ashe, N., Josiah, N., Commodore-Mensah, Y., Arscott, J., Wilson, P. R., & Starks, S. (2022). Henrietta Lacks and America’s dark history of research involving African Americans. Nursing Open, 9(5), 2236–2238. https://doi.org/10.1002/nop2.1257
- Barrow, J. M., Brannan, G. D., & Khandhar, P. B. (2022, September 18). Research ethics. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459281/
- Centers for Disease Control and Prevention. (2024, September 4). The untreated syphilis study at Tuskegee timeline. https://www.cdc.gov/tuskegee/about/timeline.html
- Christman, E., Christman, T., Demaster, V. Ernstmeyer, K., Kliminski, K., Olson, A., Pomietlo, M., Roesler, A., Stewart, J., Teeter, J., Tyznik, A. & Zwicky, J. (2022). Chapter 6: Ethical practice. In K. Ernstmeyer & E. Christman (Eds.), Nursing management and professional concepts [Internet]. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/nursingmpc/chapter/6-3-ethical-dilemmas/
- Haddad, L. M., & Geiger, R. A. (2023, August 14). Nursing ethical considerations. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/sites/books/NBK526054/0
- John Hopkins Medicine. (n. d.). The legacy of Henrietta Lacks. https://www.hopkinsmedicine.org/henrietta-lacks
- Office of Science Policy, National Institutes of Health. (2022, October). Significant research advances enabled by HeLa cells. https://osp.od.nih.gov/hela-cells/significant-research-advances-enabled-by-hela-cells/
- Olejarczyk, J. P., & Young, M. (2024, May). Patient rights and ethics. In: StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538279/
- Shea, B. (2023, October 18). Four principles of bioethics. In Ethical explorations: Moral dilemmas in a universe of possibilities. Minnesota Libraries Publishing Project; Rochester, MN. https://mlpp.pressbooks.pub/ethicalexplorations/chapter/chapter-12-bioethics12/
- Tobin, M. J. (2022). Fiftieth anniversary of uncovering the Tuskegee syphilis study: The story and timeless lessons. American Journal of Respiratory and Critical Care Medicine, 205(10), 1145–1158. https://doi.org/10.1164/rccm.202201-0136SO
- Bella. (2023, July 6). The top 10 list of Medical Interpreter Services in the USA – TLD. The Language Doctors. https://thelanguagedoctors.org/list-of-medical-interpreter-services-united-states/
- Niven, A. (n.d.). OD FAQs-translators and interpreters. OD FAQs-Translators and Interpreters. https://www.ncihc.org/faq-translators-and-interpreters#:~:text=A%20healthcare%20interpreter%20is%20one,clinics%2C%20and%20public%20health%20presentations
- Al Shamsi H, Almutairi AG, Al Mashrafi S, Al Kalbani T. Implications of Language Barriers for Healthcare: A Systematic Review. Oman Med J. 2020 Apr 30;35(2): e122. Doi: 10.5001/omj.2020.40. PMID: 32411417; PMCID: PMC7201401.
- Diving into the world of a medical interpreter. The World of a Medical Interpreter | Medical Interpreter Certification | Kent State MCLS. (n.d.). https://www.kent.edu/appling/matranslationonline/blog/world-of-a-medical-interpreter
- Sellers, J. (2023, December 27). How does medical interpreting work? Certified Languages International. https://certifiedlanguages.com/blog/how-does-medical-interpreting-work/
- Certified medical interpreter NBCMI candidate handbook. (n.d.). https://www.certifiedmedicalinterpreters.org/assets/docs/NBCMI_Handbook.pdf?v=20231011
- Certification Commission for healthcare interpreters: National, accredited, inclusive. CCHI. (n.d.). https://cchicertification.org/
- Martinez-Morales, C. (n.d.). Home. THE NATIONAL BOARD OF CERTIFICATION FOR MEDICAL INTERPRETERS. https://www.certifiedmedicalinterpreters.org/
- Antoine, R. (2023, May 18). How to become a Certified Medical Interpreter. InterpreterEd.com. https://interpretered.com/how-to-become-a-certified-medical-interpreter/#:~:text=A%20medical%20interpreter%20handles%20communication,between%20patients%20and%20medical%20staff.
- Fact sheet – cchicertification.org. (n.d.-b). https://cchicertification.org/uploads/CCHI_Factsheet.pdf
- Interpreter certification. CCHI. (n.d.-b). https://cchicertification.org/healthcare-administrators/certification-info/
- Of practice – NCIHC. (n.d.-c). https://www.ncihc.org/assets/z2021Images/NCIHC%20National%20Standards%20of%20Practice.pdf
- medical-interpretation-and-the-law-regulations-in-the-us-ebook.pdf. United Language Group. (n.d.). https://info.unitedlanguagegroup.com/hubfs/-%20ULG%20-%20Aug%202019/Services/Translation/medical-interpretation-and-the-law-regulations-in-the-us-ebook.pdf
- Wild, C. (n.d.). NBCMI programs – hub-CMI. THE NATIONAL BOARD OF CERTIFICATION FOR MEDICAL INTERPRETERS. https://www.certifiedmedicalinterpreters.org/hub-cmi
- Wild, C. (n.d.-a). NBCMI programs – CMI. THE NATIONAL BOARD OF CERTIFICATION FOR MEDICAL INTERPRETERS. https://www.certifiedmedicalinterpreters.org/nbcmi-program-cmi
- Niven, A. (n.d.-a). Ethics and standards of Practice. Ethics and Standards of Practice. https://www.ncihc.org/ethics-and-standards-of-practice
- Who we are. IMIA. (n.d.-b). https://www.imiaweb.org/about-us/who-we-are/
- International Medical Interpreters Association. IMIA. (n.d.-a). https://www.imiaweb.org/standards/standards.asp
- U.S. Bureau of Labor Statistics. (2023, September 6). Interpreters and translators: Occupational outlook handbook. U.S. Bureau of Labor Statistics.https://www.bls.gov/ooh/media-and-communication/interpreters-and-translators.htm
- Schulson, L. B., & Anderson, T. S. (2020, November 2). National estimates of professional interpreter use in the ambulatory setting – Journal of General InternalMedicine. SpringerLink. https://link.springer.com/article/10.1007/s11606-020-06336-6
- Language and literacy. Language and Literacy – Healthy People 2030. (n.d.). https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/language-and-literacy
- Wu, S. (2013, July 8). Code of ethics for medical interpreters. Their Words. Your Voice. https://shenyunwu.wordpress.com/2011/10/17/code-of-ethics-for-medical-interpreters/
- (OCR), O. for C. R. (2023, December 12). Example of a policy and procedure. HHS.gov. https://www.hhs.gov/civil-rights/for-providers/clearance-medicare-providers/example-policy-procedure-persons-limited-english-proficiency/index.html
- Kwan, M., Jeemi, Z., Norman, R., & Dantas, J. A. R. (2023). Professional Interpreter Services and the Impact on Hospital Care Outcomes: An Integrative Review of Literature. International journal of environmental research and public health, 20(6), 5165. https://doi.org/10.3390/ijerph20065165
- Sindhu, K. (n.d.). Working with medical interpreters. Wolters Kluwer. https://www.wolterskluwer.com/en/expert-insights/working-with-medical-interpreters
- Squires A. (2018). Strategies for overcoming language barriers in healthcare. Nursing management, 49(4), 20–27. https://doi.org/10.1097/01.NUMA.0000531166.24481.15
- Chen, A. H., Youdelman, M. K., & Brooks, J. (2007). The legal framework for language access in healthcare settings: Title VI and beyond. Journal of General Internal Medicine, 22 Suppl 2(Suppl 2), 362–367. https://doi.org/10.1007/s11606-007-0366-2
- Laws requiring interpreters in healthcare – certificate interpreter training programs® – official site. Certificate Interpreter Training Programs® – Official Site – Medical Interpreter Certificate & Legal Interpreter Certificate Training. (2017, July 9). https://interpretertrain.com/laws-requiring-interpreters-in-healthcare/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate