Workplace Violence Against Nurses
Contact Hours: 1
Author(s):
Phillip Meredith MSN, RN
Course Highlights
- In this Workplace Violence Against Nurses course, we will learn about types of workplace violence.
- You’ll also learn the impact of violence on nurses.
- You’ll leave this course with a broader understanding of strategies to combat workplace violence against nurses.
Introduction
The role of the registered nurse, while fundamentally dedicated to the care and well-being of patients, has long been fraught with challenges that extend beyond the complexities of medical care. One such pressing concern is workplace violence, an issue that nurses confront with alarming frequency. Recent statistics show that healthcare workers, particularly nurses, are at a higher risk of workplace violence compared to other professions.
Given nurses’ vital role in patient care and the broader healthcare system, it is imperative to understand the scope, sources, and solutions to this pressing issue. This continuing education course is dedicated to arming nurses with the knowledge, tools, and strategies to recognize, respond to, and prevent incidents of workplace violence, thereby ensuring their safety and the uninterrupted provision of quality care.
Definitions
The Occupational and Safety Health Administration (OSHA) (3) defines workplace violence (WPV for the purpose of this course) as any act or threat of physical violence, harassment, intimidation, or other threatening, disruptive behavior that occurs at the work site. This can also include verbal, written, or acts of sabotage against an individual while they are at work.
Workplace violence crosses all demographic barriers and is indiscriminate in who it can and does affect. Seeing workplace violence influences morale, attendance, and the overall well-being of employees and their co-workers.
Types of Violence
Currently, there are four categories of workplace violence according to the American Nurses Association (5).
- Criminal Intent – typically involves theft from the business or employees.
- Example: Carol is working on documentation and notices a person lingering in the hallway. Carol doesn’t really think anything of it, assuming they are family members of one of the patients. Several minutes later, the person exits quickly from the supply room and down the stairs. Carol calls security to inform them, but they can’t locate the individual. After looking through the supply room, they found several missing wound dressing supplies.
- Customer/client/patient – the individual becomes violent with employees while receiving services.
- Example: David was updating a family on their father’s critical condition. David could tell the family was upset, but the patient’s son seemed more frustrated than the others. During David’s explanation, the son grabbed David’s clipboard and yelled, “You’re not doing anything! You’re just letting him die!” The son then threw the clipboard at David’s head. David blocked the clipboard with his arm, receiving a relatively deep cut. Security became involved, and David had to go to the ER for treatment.
- Worker on worker – an employee bullies, attacks, or threatens another employee.
- Example: Emily was rounding when Dr. G. came onto the floor. This doctor was well known for being difficult to work with, and he always required the nurses to stand behind him in the room while he talked with his patients. Emily had one of Dr. G.’s patients today, and was in the room; he asked her if the patient had ambulated. Emily told him they had not, but they planned to before and after lunch. The doctor made an audible sigh and, while shaking his head at the patient, said, “See…this is what I deal with every day. These nurses can’t get anything right. They’re all useless.”
- Personal relationship: This involves a person who has an interpersonal relationship with the nurse but no association with the nurse’s employer or the business.
- Example: Rebecca was walking to her car after work. Halfway to her car, she noticed an individual leaning against the trunk of her vehicle. Rebecca recognized this person as someone her friend was currently dating. This person approached Rebecca aggressively, yelling about gossiping and trying to break their relationship. Rebecca started back toward the building, hoping security was nearby, and was pursued by the female. Eventually, Rebecca made it to the building and got inside. Luckily, the door only opened with an employee badge, and Rebecca was safe. She went ahead to security.
Currently, the customer/client type of workplace violence is the most prominent, especially in healthcare and toward nurses. The American Nurses Association (ANA) reports that OSHA does not require employers to implement workplace violence prevention programs. Still, it supplies voluntary guidelines and may cite employers for not delivering a workplace without recognized serious hazards.
Some states have legislated that employers develop a program. In contrast, most states have advanced laws that amend existing statutes for assaults on first responders by adding health care providers/nurses and/or increasing the penalty associated with such behavior. (3)
It is worth noting that, since there are, in most cases, no actual requirements for employers to provide safe work environments for nurses, preventing and dealing with WPV proves problematic. It falls on nurses to understand what constitutes WPV, how to manage it, how to cope with it, how to report it, and how to ensure action is taken and a resolution is reached when WPV occurs.
Ask yourself...
- In the scenarios above, should the employees report these incidents to administration at once?
- How would you describe the earlier scenarios on workplace violence?
- Why is it important to ask how you would find and describe workplace violence?
- Can you provide any examples of workplace violence you have experienced or seen?
Epidemiology
Workplace violence can take many forms, and the possible varieties and scenarios are endless. Regardless of how it manifests, the effects of workplace violence are clear and widespread. It can affect productivity of employees, morale, attendance, turnover rates, quality of work, patient outcomes, and much more.
Workplace violence can affect and involve workers, clients, customers, and visitors. WPV ranges from threats and verbal abuse to physical assaults and even homicide. In 2010, the Bureau of Labor Statistics (BLS) data reported healthcare and social aid workers were the victims of approximately 11,370 assaults by persons; a greater than 13% increase over the number of such assaults reported in 2009 (10). Almost 19% of these assaults occurred in nursing and residential care facilities alone. Unfortunately, many more incidents probably go unreported (5).

Impact on Nurse Well-Being
Workplace violence can take a heavy toll on nurses. These tolls can be emotional, mental, and physical as well as short-term or long-term. The seriousness of these injuries can vary widely ranging from minor upset to permanent injury and in worst cases, even death. (13)
This harm doesn’t stop with the nurse. The effects of workplace violence may also include effects spanning the unit the nurse works on or even the entire facility. Low morale, reduced productivity, lack of trust in employers, and fear of going to work can be results of violent events occurring to even a single co-worker.
Workplace violence can also have a financial effect on nurses and their employers related to lost time at work from injury or callouts, costs of care for treatment related to the incident (physical and/or psychological), or even legal fees. (13)
Given that incidents of workplace violence are rapidly increasing, these impacts are expected to increase as well. It is easy to see how this harm is widespread and can potentially ripple outward into the nurse’s professional and personal life. The stress and harm do not stay at work, and can spread to the nurse’s family, social interactions, and more.
Ask yourself...
- How far-reaching do you think workplace violence is?
- Can you give some examples of how workplace violence has affected you or your co-workers?
- What are some examples of how workplace violence against someone else can affect you or the patients on your unit?
Barriers to Reporting
One way to combat workplace violence is knowledge of its existence, its nature, and its frequency. Unfortunately, there are many factors that either prevent or discourage nurses from coming forward with reports when they are the victims of WPV.
A study presented in a Chinese nursing journal surveyed 325 nurses. Of these nurses, 266 were spread across 165 hospitals, and these hospitals were in 72 cities.
A total of 172 nurses (64.7%) experienced violent incidents during the past year. Of these incidents, 45.5% were reported; and the reporting rate of physical assaults (69.0%) was higher than those of verbal abuse (36.9%), threatening behavior (51.7%), and sexual harassment (60.0%). Formal reporting accounted for 25.4% (15.4% in written form and 10.0% through a computer-assisted reporting system.
Almost half of the nurses (49.6%) said that the hospital had no reporting system, or they were uncertain about the reporting system. For reasons of not reporting, 51.9% of the nurses were unaware of how and what types of violence to report, and 50.6% of the nurses believed that the hospital paid greater attention to patients rather than staff. (7)
Interestingly, almost fifty percent of the nurses surveyed had limited knowledge of a reporting system available to them. In comparison, fifty percent felt the hospital favored the patients over its employees. Combined with an actual or perceived lack of supervisory support, this encourages an environment where nurses feel powerless to protect themselves or to take proper action when threatened or harmed.
The Minnesota Nurses Association, in August of 2022, published a press release with the results of a nursing survey on the topic of workplace violence. In this survey, ninety-seven percent of the nurses surveyed observed WPV or harassment over the previous two years.
The top reasons cited by nurses who did not report workplace violence were lack of time due to overwork and understaffing, cited by fifty-eight percent of respondents, and lack of action by hospital management, cited by fifty-three percent of nurses in the survey. (4)
It would appear from these studies that many nurses feel it is futile to report incidents of workplace violence they encounter. Even if they realized an incident was reportable, they may not know how to report it or have time to do it. This perceived powerlessness and sense of futility in the face of abuse and violence will only continue to worsen unless action is taken to remove barriers to reporting and for nurses to have access to aid and support from supervisory staff.
Ask yourself...
- Can you think of any examples of when you or a co-worker tried to report an incident of workplace violence and were unable to?
- If so, what was the barrier that prevented you from reporting?
- Can you name three alternative ways to report workplace violence at your organization?
Culture of Safety
A commonly used phrase is “Culture of Safety”, but is there a standardized definition of what it is or could be? Many resources point to the safety of patients about medical errors, patient rights, and protecting the patient’s information, but few address the issue facing caregivers and especially nurses. However, there is no agreed-upon or standard definition of a “culture of safety” or what it should look like.
The American Nurses Association approaches the concept by saying, “Establishing a culture of safety in health care is essential to the security and well-being of your patients, staff, and organization. Effective nurse leaders embrace safety protocols, ensuring their organization delivers a secure, protective environment, prioritizing patients and caregivers.” (12)
Currently, only a single federal legislation is in place about the issue.
The only federal regulation currently in place is the General Duty Clause of the Occupational Safety and Health Act of 1970. This clause requires employers to supply a work environment free from recognized hazards that are causing or likely to cause death or serious physical harm. However, the general duty clause offers no specific recommendations about managing workplace violence.
The Occupational Safety and Health Administration (OSHA) issued guidelines for workplace violence prevention for health care and social service workers. First issued in 1996 and later updated, the guidelines are only advisory. (1)
It is paramount that nurses and other direct care providers accept the responsibility of creating policies and procedures within their organizations to define and enforce a work environment where violence is not tolerated and dealt with accordingly.
There is currently a small body of research and work on the effects workplace violence has on nurses as human beings. Most of the evidence focuses on how workplace violence increases the risk nurses pose to patients in the form of medical errors, staffing issues due to missed work, poor documentation, etc.
The main body of evidence discussing how workplace violence affects nurses is noted in research around nurse burnout. A 2020 study published by the National Health Institute (10) states, “Workplace aggression is a source of extreme socio-emotional stress, which may lead to the experience of psychological strain.
A large body of research shows that exposure to workplace aggression and violence may severely impair healthcare workers’ mental health, including symptoms of post-traumatic stress disorder, depression, and burnout.”
This study also shows an essential association with workplace aggression and violence targeting nurses and drastically increased levels of emotional exhaustion, depersonalization, and deep feelings of poor personal accomplishment. Over time, these feelings lead to complete burnout, and even worse, possibly psychological and/or physical conditions in the nurse affected.
Even with this preliminary information and research, we still have a long way to go to show the complete and far-reaching effects of workplace violence on nurses. Again, by being proactive and acting now, we as nurses can foster this research and bring the issues to light.
Ask yourself...
- How does your organization define a “culture of safety”?
- Do you agree with the definition?
- How would you define a “culture of safety” from your own perspective given your experiences and challenges?
ANA Zero Tolerance Policy
In 2019, the American Nurses Association (ANA) (2) released a brief titled “Reporting Incidents of Workplace Violence.” In it, they discussed several issues surrounding workplace violence, barriers to reporting it, and recommendations to healthcare organizations on strategies relating to workplace violence.
They also established a “Zero Tolerance Policy on Workplace Violence,” which provided some definitions and several recommendations on how to deal with WPV.
The introduction to the “Culture of Safety” part of this brief is as follows:
By prioritizing, developing, and sustaining an organizational culture focused on safety, we can drive the future of healthcare to a place where patients and those who care for them are free from harm. It is one of many priorities and the overriding ethical imperatives for all leaders. (9)
The ANA also suggested a three-level prevention strategy, each with a role for the employer and the employee. Essentially, the employer’s role is to gather data, provide a “safe” work environment, non-punitive reporting, and develop programs to provide a safe work environment for nurses. The employee’s role is to participate in implementing and evaluating said programs.
Unfortunately, these are only suggestions; employers do not have to implement programs or services to protect employees against workplace violence. Also, healthcare employers do not have to report incidents to JCAHO, who consider workplace violence as “sentinel events”.
Ultimately, it falls on the nurses and employees directly affected by WPV to assume the charge against workplace violence, hold employers accountable, communicate with local and state legislators, and effect change to protect themselves.
Ask yourself...
- Considering the recommendations and guidelines set forth by these entities, do you think they are adequate or effective? Why or why not?
- How has this information changed your perception of the overall reporting process on workplace violence against nurses?
- What generalizations can you make from this information on the reporting process from an employer perspective?
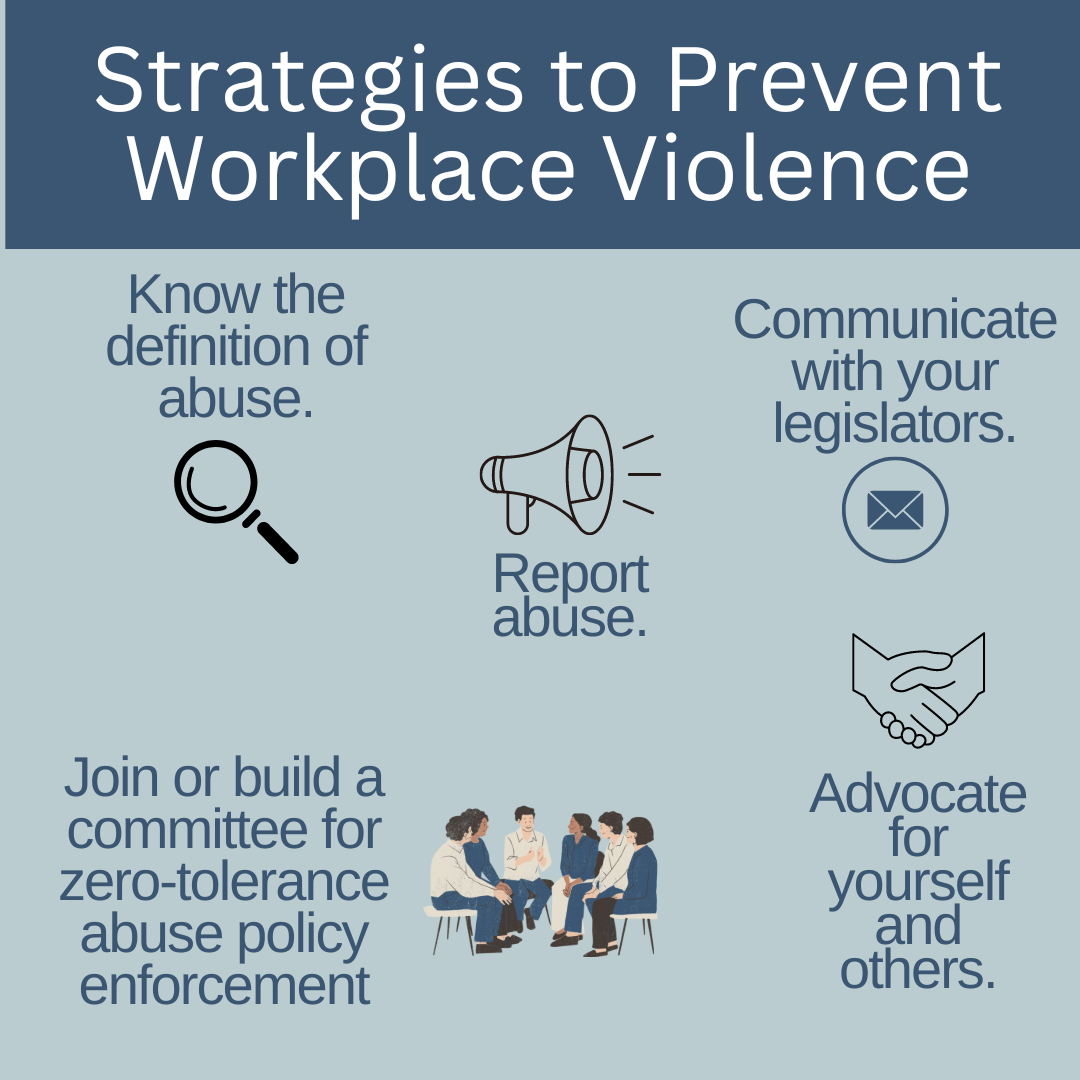
Strategies to Prevent Workplace Violence
To end nurse abuse for good, Boston-Leary says it takes every nurse speaking up and reporting abuse within an organizational culture that has an established process for allowing nurses to report abuse without fear of recrimination and then follows up with a resolution. (8)
There are some suggested actions to help prevent and combat workplace violence in your practice setting. These actions include:
- Know the definition of abuse.
- The National Institute for Occupational Safety and Health (NIOSH) defines workplace violence as “the act or threat of violence, ranging from verbal abuse to physical assaults directed toward persons at work or on duty.”
- Agreeing on this definition is an essential first step to achieving widespread acknowledgement of the distinct types of nurse abuse, particularly non-physical abuse, Boston-Leary explains. (8)
- Report Abuse
- Ask about how your workplace manages abuse reporting, whether in your current workplace or when you are applying for a position, Boston-Leary suggests. “Ask about how reporting abuse happens during any shift because there should be a reporting mechanism in place for everyone, even on a weekend or evening shift with no manager easily accessible to report to.”
- If (when) you do experience abuse, you must speak up immediately and note any witnesses who could corroborate your description of the incident, she says.
- Even after you experience abuse and even if you didn’t report it, it’s essential to share your past abuse with others to empower them to report abuse they experience. (8)
- Change Your Culture
- Join or meet a committee to build or strengthen zero-tolerance abuse policies. Based on ANA’s Zero Tolerance Policy on Workplace Violence, Boston-Leary suggests these crucial elements of a zero-tolerance abuse program:
- Stop violence before it starts through education to find risks and reduce vulnerabilities for workplace violence.
- Create an effective response to violence immediately after it occurs, including emergency care.
- Establish long-term responses that reduce the long-term adverse effects of workplace abuse. (8)
- Communicate with your Legislator!
- Congress was considering legislation to #End Nurse Abuse by passing The Workplace Violence Prevention for Health Care and Social Service Workers Act (H.R. 1195). If approved, this law would have required health care and social service industry employers to develop and implement a comprehensive workplace violence prevention plan that protects nurses and other healthcare professionals from on-the-job abuse.
- Boston-Leary believes legislators are very attuned to the trusted voice of nurses to share about what is happening in health care today (8).
Ask yourself...
- What is your organization’s primary method of reporting abuse or violence against employees?
- Do you know who your local and state legislators are and how to contact them?
- Are you aware of any committees or groups within your organization that actively address the issue of workplace violence?
Nurse-led Strategies
You can join these committees or work with your employer to create them. Collaborating with your supervisory staff and HR, you can create workflows, policies, and reporting methods, provide education on preventing workplace violence, and make a difference in your overall work environment.
- Regarding Your Legislators
- As mentioned before, in 2021, Congress considered federal legislation to end nurse abuse by passing the Workplace Violence Prevention for Health Care and Social Service Workers Act (H.R. 1195). The bill was passed by the House on April 16, 2021, but it was never passed by the Senate.
- You can easily find your local and state legislators’ contact information on the internet. A simple search for “how to find state legislator contact information” is a wonderful place to start. As a voting citizen, you have every right to contact them and demand that laws be created to protect you while you work.
- Below are some links to help you find elected officials:
- Advocate for your safety the same way you would for your patients!
- As nurses, we aren’t afraid to step up to bat for our patients when they need something, but we are notorious for taking a hit and letting it slide, sometimes even to our own detriment.
- We owe it to ourselves to offer that same level of advocacy to ourselves and our co-workers.
Ask yourself...
- How can you become an advocate for yourself or your co-workers when it comes to workplace violence?
- Who is the contact in your organization for instances of workplace violence?
Resources
The Joint Commission supplies resources available to report and learn how to report workplace violence. The links included are for federal, state, professional, and other resources. The direct link to this page is:
The Joint Commission: Workplace Violence Prevention Resources
- Local law enforcement
- As a private citizen, you are protected by laws about assault, battery, and other attacks on your person. You are within your rights to call the police on events of workplace violence, especially if your life or health is threatened, or you are physically attacked. Your employer will likely not support you in this situation due to legal implications. It is best to ask your HR department and supervisory staff how these situations should be managed if they occur.
- Legal Counsel
- Consult with a lawyer about your legal rights in situations of workplace violence and how to best manage them. Be sure to bring scenarios, information on how your employer suggests dealing with these situations, and examples of violence you have seen or have experienced.
- Educate and Train Yourself
- Learn as much as you can about recognizing and managing workplace violence. Your employer may supply these courses; if they don’t, it may be prudent to request them. Also, you can seek outside education and training on these topics, including self-defense classes and crisis management courses.
- Practice Self-Awareness
- We all have inherent beliefs, perspectives, and feelings that can prevent us from acting in certain situations. Knowing yourself and understanding possible nuances within yourself that could derail your ability to handle a situation of workplace violence appropriately could mean the difference between prevention and becoming a victim.
Ask yourself...
- What training opportunities does your organization provide on management and follow-up for workplace violence?
- What information would you ask local law enforcement or a legal counsel for on workplace violence?
- What might someone who believes abuse against nurses is “just part of the job” do when they find themselves a victim of workplace violence?
- What can you do to help individuals that may simply allow workplace violence to affect their well-being?
Conclusion
Being an agent of change can be intimidating and terrifying, and it can even force us to deal with feelings and beliefs we didn’t realize were in our way. WPV incidents have been rising sharply over the past several years, and there is no sign of slowing. As front-line workers, nurses, and co-workers, it’s up to us to take responsibility for our safety and work environment.
Through cooperation and consistency, we can create and bring solutions to the workplace and, hopefully, one day, aid in creating laws that make our jobs safer to supply the care and support our patients’ needs. We owe it to ourselves to take the necessary steps to show our employers it’s time to address this issue. “Be the change you wish to see in the world.” ~Mahatma Gandhi –
References + Disclaimer
- Arnetz, J. E. (2022, April). The Joint Commission’s new and revised Workplace violence prevention standards for hospitals: A major step forward toward improved quality and safety. Joint Commission journal on quality and patient safety. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8816837/
- American Nurses Association. (2019, January). Reporting incidents of Workplace Violence – Ana Enterprise. Reporting Incidents of Workplace Violence. https://www.nursingworld.org/~495349/globalassets/docs/ana/ethics/endabuse-issue-brief-final.pdf
- Occupational Safety and Health Administration. (n.d.). Healthcare – workplace violence. https://www.osha.gov/healthcare/workplace-violence/
- Minnesota Nurses Association. (2022, August 10). Hennepin Healthcare Nurses report rising violence against nurses and patients, cite under-staffing, unresponsive management as barriers in new survey. Minnesota Nurses Association. https://mnnurses.org/hennepin-healthcare-nurses-report-rising-violence-against-nurses-and-patients-cite-under-staffing-unresponsive-management-as-barriers-in-new-survey/
- ANA) Workplace violence. (2017). https://www.nursingworld.org/practice-policy/advocacy/state/workplace-violence2/
- Sahebi, A., Golitaleb, M., Moayedi, S., Torres, M., & Sheikhbardsiri, H. (2022, August 8). Prevalence of workplace violence against health care workers in hospital and pre-hospital settings: An umbrella review of meta-analyses. Frontiers in public health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9393420/#:~:text=The%20overall%20prevalence%20of%20WPV,%2C%20and%2010.5%25%20(95%25
- Song, C., Wang, G., & Wu, H. (2020, December 3). Frequency and barriers of reporting workplace violence in nurses: An online survey in China. International Journal of Nursing Sciences. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7859538/
- Staff, A. (2022, November 4). End Nurse Abuse: 4 Actions You Can Take Today. Aorn.org. https://www.aorn.org/article/2021-12-03-End-Nurse-Abuse
- Fountain, D., Zankowski, D., & Arriola, J. (n.d.). Reporting incidents of Workplace Violence – Ana Enterprise. Reporting incidents of Workplace Violence. https://www.nursingworld.org/~495349/globalassets/docs/ana/ethics/endabuse-issue-brief-final.pdf
- U.S. Bureau of Labor Statistics. (n.d.). Workplace violence in healthcare, 2018. U.S. Bureau of Labor Statistics. https://www.bls.gov/iif/factsheets/workplace-violence-healthcare-2018.htm
- Vincent-Höper, S., Stein, M., Nienhaus, A., & Schablon, A. (2020, May 1). Workplace aggression and burnout in nursing-the moderating role of follow-up counseling. International journal of environmental research and public health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7246829/
- Creating a culture of safety in nursing. ANA. (2023, September 12). https://www.nursingworld.org/resources/individual/nurse-managers/safety-in-nursing/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
