Course
Wound Debridement Basics
Course Highlights
- In this Wound Debridement Basics course, we will learn about and understand the different types of wound debridement and when each is appropriate.
- You’ll also learn basic wound debridement techniques safely and efficiently
- You’ll leave this course with a broader understanding of the risks and complications linked to wound debridement and how to mitigate them.
About
Contact Hours Awarded: 1
Course By:
Edith Fomuso RN MSN CCM DPM
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Welcome to the Wound Debridement Basics Course! In this course, we will learn how to assess wounds, understand when wound debridement is necessary, and discover the best techniques to promote the best outcomes.
By the end of the course, you will feel confident about identifying the right debridement method and handling any challenges that come your way.
What Is Wound Debridement?
Wound debridement is the process of removing contaminated, infected, or dead tissue from a wound to create an environment that promotes healing (1). Without proper debridement, necrotic tissue on the wound can breed bacteria, leading to infection or even sepsis. In addition to that, non-viable tissue delays the formation of healthy granulation tissue, which is helpful for wound healing. For example, if dead tissue is present in a diabetic foot ulcer, it would be necessary to remove it to promote the healing process.
Let’s review the four phases of wound healing (11, 15):
- Hemostasis: Immediately after a wound occurs, the body initiates clotting to prevent excessive blood loss.
- Inflammation: In this phase, immune cells enter the wound to destroy bacteria and remove debris.
- Proliferation: In this phase, healthy tissue begins to form as the body produces collagen to rebuild the wound and new blood vessels to provide nutrients.
- Maturation: Finally, the wound contracts and strengthens as new tissue continues to grow. The length of this phase depends on the severity of the wound.
Now that we’ve gone through the stages of wound healing, let’s see the goals that wound debridement helps to achieve (8, 16):
- Prevent Infection: Removing necrotic tissue eliminates the environment where bacteria can grow.
- Promote Healing: Debridement promotes wound healing by exposing healthy tissue to encourage the growth of new cells.
- Reduce Inflammation: Debridement helps decrease inflammation in the wound area and promotes natural healing.
- Improve Aesthetic Outcomes: In some cases, debridement can improve the appearance of a wound as it heals.
When is Debridement Necessary?
Debridement is not required for every wound. However, according to (21) and (23), it becomes necessary in the following situations:
- Presence of Necrotic Tissue: The appearance of black eschar (hard, dry dead tissue) or slough (soft, yellow dead tissue) indicates the need for debridement.
- Stalled Wound Healing: If a wound is not healing as expected or shows no signs of improvement after several weeks, debridement can be used to promote healing.
- Infection: If there are signs of infection, such as pus, foul odor, or increased redness around the wound, removing infected tissue can help control the infection.
- Chronic Wounds: In chronic wounds, such as diabetic ulcers or venous leg ulcers, debridement helps remove layers of bacteria and cells that prevent healing.

Self-Quiz
Ask Yourself...
- What is the main purpose of wound debridement?
- How might the presence of dead tissue impact the healing of a wound?
- What could happen if a wound is not properly debrided?
- In what situations might debridement be unnecessary or even harmful?
Types of Wound Debridement
There are several types of wound debridement, and each method has its advantages and challenges. The choice of the debridement method depends on factors such as the type and severity of the wound, the patient’s condition, and the goals of wound management (9) and (10). According to (13) and (19), when healthcare providers understand the appropriate use of each method, they can provide effective care, promote faster healing and reduce the risk of complications. Let’s discuss the types of wound debridement according to according to (1).
Autolytic Debridement
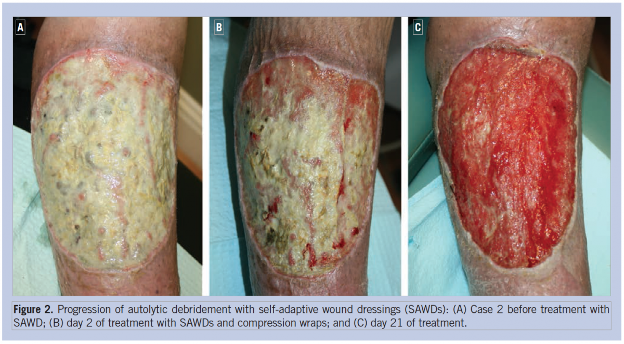
Autolytic debridement is a gentle way to help wounds heal by using the body’s own enzymes and moisture to break down dead tissue (9). The process is done by keeping the wound moist, using occlusive or semi-occlusive dressings, such as hydrocolloids or hydrogels. This method is usually preferred because it targets only the damaged tissue while leaving healthy tissue alone. For instance, if someone has a shallow pressure ulcer on their heel, covering it with a hydrocolloid dressing can help to keep the wound moist, allowing the body’s natural enzymes to gradually soften and remove the dead tissue. Even though this is a slower approach, it is safe and much less painful than other methods of debridement (9).
Enzymatic Debridement
According to (13), enzymatic debridement is a gentle, but effective way to clean out dead tissue from a wound using topical agents with specialized enzymes that digest the necrotic tissue while leaving the healthy tissue intact. This type of wound debridement is quicker than the natural, self-healing process of autolytic debridement, and less aggressive than sharp or surgical methods (13). For example, if a patient has a diabetic foot ulcer that is too painful for more invasive procedures, enzymatic debridement can be a great option.
Mechanical Debridement
Mechanical debridement uses physical methods like wet-to-dry dressings, high-pressure fluid irrigation, or scrubbing to remove dead tissue from a wound (9). For example, a patient with an infected wound from a traumatic injury might undergo mechanical debridement using high-pressure saline irrigation to cleanse debris and promote healing.
Sharp Debridement
According to (10) sharp debridement is a method where a healthcare provider uses tools such as scalpels or scissors to carefully remove dead or infected tissue from a wound. This method is often used when there’s an urgent need to get rid of dead tissue to prevent an infection from worsening (10). For example, if a patient has a severe pressure ulcer with signs of infection and necrosis, the provider might use a scalpel to carefully remove the dead tissue, and help the wound start healing properly
Biological (Maggot) Debridement
Biological debridement, or maggot therapy, might sound a bit strange, but it is a highly effective treatment. According to (19), it involves using sterile, lab-grown maggots from the greenbottle fly, to eat dead tissue, clean out wounds and prevent the risk of infection. For example, if a patient has a stubborn wound that just won’t heal, even after trying other treatments, biological debridement can be used by putting sterile maggots on the wound and covering it with special dressing. After a few days, the maggots are removed, leaving the wound bed clean and ready for healing (19).
Surgical Debridement
Surgical debridement is the most intense type of debridement and usually happens in an operating room under anesthesia. (1) describes that it is typically needed when there’s a lot of dead tissue that has to be removed quickly, like in cases of severe infections or deep, extensive wounds. For example, if someone has necrotizing fasciitis, a serious bacterial infection, they might need immediate surgical debridement to remove the infected tissue and potentially save the limb. In these situations, the surgeon removes all the dead tissue and may leave the wound open for additional treatments down the line (1).
 (24)
(24)

Self-Quiz
Ask Yourself...
- What do you think makes autolytic debridement a safer option than other debridement types?
- How might the patient’s healing process differ between enzymatic debridement and mechanical debridement?
- Why do you think sharp debridement is preferred in cases of severe infection?
- How might autolytic debridement support or hinder the body’s natural healing mechanisms? Can you think of a scenario where autolytic debridement might be inadequate?
Patient Assessment
Before performing a debridement procedure, the healthcare worker must assess the patient thoroughly. This means evaluating the wound, determining if debridement is needed, identifying any risks, and making sure the patient is comfortable throughout the procedure (22). Let’s discuss the assessment details below.
Wound Assessment: Size, Depth, and Tissue Type
According to (22), a good assessment begins with understanding the wound’s size, depth, and the types of tissue involved. It is important to accurately measure the wound using a ruler or a disposable measuring tool because that guides treatment decisions and helps to track healing over time.
(22) explains that the wound’s depth can be classified as either partial-thickness, affecting the epidermis and part of the dermis, or full-thickness, going through the dermis into deeper tissues. Knowing what type of tissue is present is also key. For example, you might see the following tissue types as listed in (22):
- Necrotic tissue: Black, dead tissue that needs to be removed.
- Slough: Yellow or white, moist tissue that can interfere with healing.
- Granulation tissue: Red, healthy tissue that indicates healing.
- Epithelial tissue: Pink, new skin that’s a sign of recovery.
Determining the Need for Debridement
Figuring out if a wound needs debridement is an important part of wound care. (15) describes major signs that include the presence of dead or non-viable tissue, signs of infection, and a wound that’s not healing despite proper care. For example, if a patient has a pressure ulcer that hasn’t improved after four weeks of treatment, the wound measures 4 cm by 4 cm and has black, necrotic tissue; debridement might be needed to remove the dead tissue and help the wound start healing by encouraging the growth of healthy tissue (15).
Identifying Contraindications
Knowing when not to perform debridement is just as important as knowing when it is necessary. According to (6), certain conditions can make the procedure more risky and potentially harmful. For example, if a patient has poor blood flow due to arterial insufficiency, removing tissue could make things worse by causing more damage or tissue death. In cases of infection, different treatments might be needed before debridement is considered. Also, if a patient is on blood thinners, the risk of bleeding during debridement is much higher, so extra caution is required.

Self-Quiz
Ask Yourself...
- What factors should we consider when assessing the size and depth of a wound? How might these factors influence our treatment approach?
- How can we differentiate between viable and non-viable tissue, and why is this distinction significant in the debridement process?
- What are the potential consequences of proceeding with debridement in patients with arterial insufficiency?
- How does the patient’s overall health status impact the decision to perform debridement? What specific health conditions might complicate this decision?
Techniques for Performing Debridement
Effective wound debridement requires various tools and materials to ensure safety. Commonly used tools include sterile scissors, forceps, scalpels, and curettes that are designed for tissue removal, in addition to dressings such as hydrogels, alginates, and foam dressings (17).
Sterile Technique and Infection Control Measures
Keeping things sterile is very necessary during wound debridement to prevent infections. According to (3), healthcare providers need to perform hand hygiene by washing hands with soap and water or using hand sanitizer before and after touching the patient. Using personal protective equipment (PPE) like gloves, masks, and gowns also promotes safety for everyone.
Dressing Choices Post-Debridement
Choosing the right dressing after debridement is essential for helping the wound heal and preventing infection. The dressing should keep the wound moist, soak up any excess fluid, and protect it from outside contaminating agents (14). For example, if there is a lot of drainage, a nurse might go with foam dressing because it can absorb the fluid while still maintaining moisture. On the other hand, if the wound is dry, a hydrogel dressing could be a better choice since it helps hydrate the tissue and encourage healing. In cases where there’s a high risk of infection, like with diabetic patients, an antimicrobial dressing might be the best option (14).
Care for the Patient Post-Debridement
Taking care of a wound after debridement is crucial for proper healing and avoiding complications. (7) recommends that clinicians should guide patients on what to watch for, like increased redness, swelling, or unusual discharge, and to encourage them to report these signs of infection right away.
Pain Management and Patient Comfort Considerations
Managing pain and keeping patients comfortable are crucial parts of wound debridement. (4) explains that it is common for patients to feel anxious or uneasy about their wounds and the procedure itself; so, having a good pain management plan is very important. This might include giving pain relief before the procedure, using numbing creams, or even sedation, depending on how severe the wound is and the patient’s needs. It is also important to explain what’s going to happen reassuringly, so patients know what to expect and feel more comfortable (4).


Self-Quiz
Ask Yourself...
- What criteria should healthcare professionals consider when choosing a debridement technique for a specific wound?
- How does the maintenance of a sterile technique impact patient outcomes in wound debridement?
Risks and Complications of Wound Debridement
Wound debridement involves certain risks and complications that healthcare providers must consider. Understanding these potential issues can help practitioners implement effective strategies to mitigate them and ensure best patient outcomes.
Infection
One of the biggest concerns with wound debridement is the risk of infection because when dead tissue is removed, it can expose deeper layers of the wound, making it easier for bacteria to get in (5). To prevent this complication, the healthcare provider must follow strict aseptic techniques in order to prevent increasing the bacterial load (5).
Bleeding
According to (12), Debridement can sometimes cause bleeding, especially when using sharp tools or working near major blood vessels; and the risk is higher for patients with bleeding disorders or those taking blood thinners.
As a result, healthcare professionals need to be trained to spot and handle excessive bleeding right away, whether by applying direct pressure or using special agents to stop the bleeding (12).
Delayed Healing
Wound debridement can sometimes slow down the healing process, especially if it is not done properly or if the wound doesn’t get proper care after the process (20). For example, if too much healthy tissue is removed during the procedure, it can leave a bigger wound that takes longer to heal. Research shows that keeping wounds at the right moisture level helps cells move and new tissue form, speeding up healing (20).
Pain and Discomfort
Pain is a natural part of the debridement process, and it can cause anxiety and discomfort for patients, which might not only affect their experience during the procedure but can also impact their willingness to follow through with care afterward (18). A study by (18) highlights how important it is to tailor pain management plans to each individual, as this approach can significantly improve patient satisfaction and help them stick to their treatment plans.
Emotional and Psychological Impact
Wound debridement isn’t just a physical process; it can take an emotional toll on patients, as seeing their wounds, feeling the pain, and fearing the procedure can lead to a lot of anxiety and distress (2). Because of this, it is very important to provide psychological support and to educate patients about the healing process, since when patients understand what’s happening, it can empower them, ease their stress, and help them engage more in their own care (2).

Self-Quiz
Ask Yourself...
- What is the purpose of wound debridement, and how might potential risks compromise the intended benefits?
- In what situations do the risks of wound debridement outweigh its benefits? Can you provide examples?
- How does the presence of comorbid conditions in patients influence the risks associated with wound debridement?
- What strategies can healthcare professionals implement to minimize the risk of infection during the debridement process?
- What are the risks associated with wound debridement, and how can they be minimized?
- Which types of debridement carry the most risk, and why?
- How might the skills of the healthcare provider influence the success of sharp debridement?
- What do you think are the most important factors to assess before choosing a specific type of debridement for a patient?
- How does the overall health of a patient impact the choice of debridement method?
- How can patient education and involvement in post-debridement care enhance the healing process?
- In what situations might biological debridement (maggot therapy) be more advantageous than surgical debridement?
- Why do you think maggot therapy is sometimes considered a last resort?
- How does the body’s natural healing process play a role in autolytic debridement, and what conditions are necessary for this to be effective?
- What challenges might arise if the wound environment is not properly maintained?
- How would you balance the immediate discomfort with the long-term benefits of debridement for the patient?
- Why is pain management an essential component of the wound debridement process? How can effective communication about pain expectations enhance patient comfort?
- What strategies can be employed to evaluate a patient’s readiness for debridement? How might we determine if a patient understands the procedure and its risks?
- In your experience, what are some common misconceptions patients can have about debridement? How can we address these misconceptions effectively?
- How can interdisciplinary collaboration enhance the patient assessment process for debridement? What roles can different healthcare professionals play in this assessment?
- How might a patient’s psychological factors, such as anxiety about pain or fear of the procedure, affect the overall outcomes of wound debridement?
- How can effective communication with patients about the risks and benefits of debridement enhance their compliance and comfort during treatment?
- How do different debridement techniques (e.g., mechanical vs. sharp) present unique risks, and how should practitioners choose the appropriate method?
- What role does patient education play in mitigating the emotional and psychological impacts associated with the risks of wound debridement?
- How can a multidisciplinary approach improve the management of complications arising from wound debridement?
Conclusion
To wrap things up, this course on wound debridement has highlighted how important effective wound management is for improving patient outcomes. We’ve discussed the different debridement techniques, like autolytic, enzymatic, mechanical, and sharp debridement; and discussed why thorough patient assessments, effective techniques, and risk management are very important. By putting this knowledge into action, healthcare providers can truly enhance the healing process and elevate the quality of care for their patients.
References + Disclaimer
- Atkin, L. (2020). The importance of wound debridement in the healing process. Journal of Wound Care, 29(3), 162-166.
- Cameron, M., Reid, M., & McCaffery, K. (2023). Psychological support in chronic wound care: A systematic review. Journal of Wound Care, 32(3), 145-156.
- Cacoub, P., Wechsler, B., & Cracowski, J. L. (2021). Infection control measures in wound management. Journal of Clinical Medicine, 10(12), 2654.
- Chambers, L., Kwan, J., & Tharakan, J. (2021). Pain Management in Wound Care: A Systematic Review. International Wound Journal, 18(4), 434-445.
- Cleveland Clinic. (2020). Wound debridement: Risks and benefits. Retrieved from Cleveland Clinic
- Davis, D., Moore, H., & Patel, M. (2022). Arterial Insufficiency and Its Implications for Wound Healing: A Review of Literature. Journal of Vascular Surgery, 75(1), 235-243.
- Dumont, N., Colle, M., & Wicky, A. (2023). Managing post-debridement care: A comprehensive guide. International Wound Journal, 20(4), 456-465.
- Fonder, M. A., Lazarus, G. S., Cowan, D. A., Aronson-Cook, B., Kohli, A. R., & Mamelak, A. J. (2021). Treating the chronic wound: A practical approach to the care of nonhealing wounds and wound care dressings. Journal of the American Academy of Dermatology, 74(4), 607-625.
- García-Morales, E., Lazaro-Martínez, J. L., Aragón-Sánchez, J., Cecilia-Matilla, A., García-Álvarez, Y., & Molines-Barroso, R. J. (2020). Clinical effectiveness of hydrocolloid dressings in the treatment of diabetic foot ulcers. Journal of Wound Care, 29(3), 165-171.
- Gould, L. J., Altman, I., & O’Connell, K. (2018). Wound care essentials: Practice principles. Lippincott Williams & Wilkins.
- Guo, S., & DiPietro, L. A. (2019). Factors affecting wound healing. Journal of Dental Research, 89(3), 219-229.
- Hawkins, D. B., Smith, E. H., & Jones, L. P. (2021). Hemorrhage control during wound debridement: Strategies and techniques. International Journal of Wound Care, 20(4), 229-234.
- Hoggarth, A., & Humphreys, N. (2019). Enzymatic debridement in wound care: An evidence-based review. Wound Care Advisor, 8(1), 34-40.
- Kang, K., Park, Y., & Han, J. (2022). Efficacy of dressing choices in wound care: A review. Wound Repair and Regeneration, 30(5), 612-623.
- Kim, P. J., Attinger, C. E., Oliver, N., Hoover, T., Wang, X., & Steinberg, J. S. (2021). The impact of debridement on wound healing in chronic wounds. Wound Repair and Regeneration, 29(1), 20-26.
- Kirsner, R. S. (2019). Debridement: Key to successful wound healing. Wounds, 31(9), 235-239.
- Liu, Y., Zhang, X., & Chen, J. (2020). The role of moisture in wound healing: A literature review. Advances in Wound Care, 9(10), 490-498.
- Majumdar, S., Gupta, A., & Choudhury, P. (2022). Managing pain in wound care: Best practices for clinicians. Wound Repair and Regeneration, 30(1), 24-31. https://doi.org/10.1111/wrr.13005
- Opletalová, K., Blaizot, X., Mourgeon, B., Chêne, Y., Creveuil, C., & Combemale, P. (2018). Maggot therapy for wound debridement in patients with chronic leg ulcers: A randomized controlled trial. British Journal of Dermatology, 178(2), 401-408.
- Perrin, B. M., Reynolds, S. L., & Smith, T. A. (2021). The importance of moisture balance in wound healing: A review. Advances in Wound Care, 10(5), 256-263.
- Sibbald, R. G., Goodman, L., Woo, K. Y., Krasner, D. L., & Smart, H. (2020). Special considerations in wound bed preparation 2020: An update. Advances in Skin & Wound Care, 33(4), 184-195.
- Steed, D. L., Attinger, C. E., & Mesenchymal, S. (2020). Wound Healing: A Review of the Fundamentals. Wound Repair and Regeneration, 28(5), 573-580.
- Wolcott, R. D., & Dowd, S. E. (2019). Biofilms and chronic wound inflammation. Journal of Wound Care, 18(12), 509-513.
- Image (Creative Commons License): Reyzelman, A.M. & Vartivarian, M. (2018). Evidence of intensive autolytic debridement with a self-adaptive wound dressing. Wounds. Retrieved from https://www.hmpgloballearningnetwork.com/site/wounds/article/evidence-intensive-autolytic-debridement-self-adaptive-wound-dressing. CC-BY-SA-4.0
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
