Tell Me About the Michigan Nurses Report
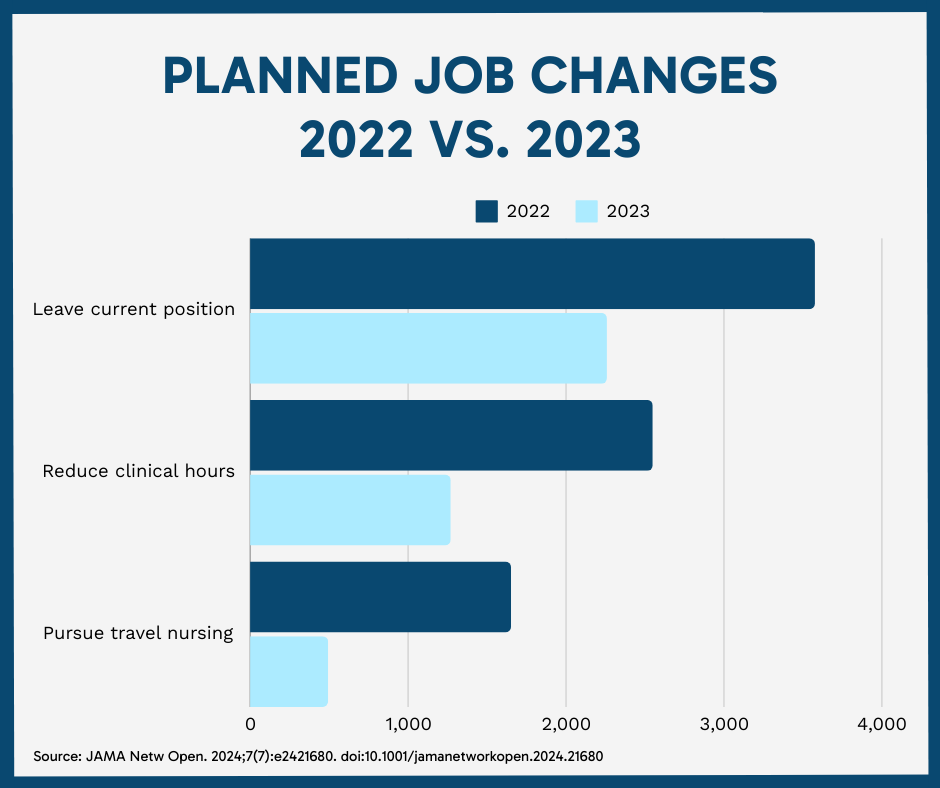
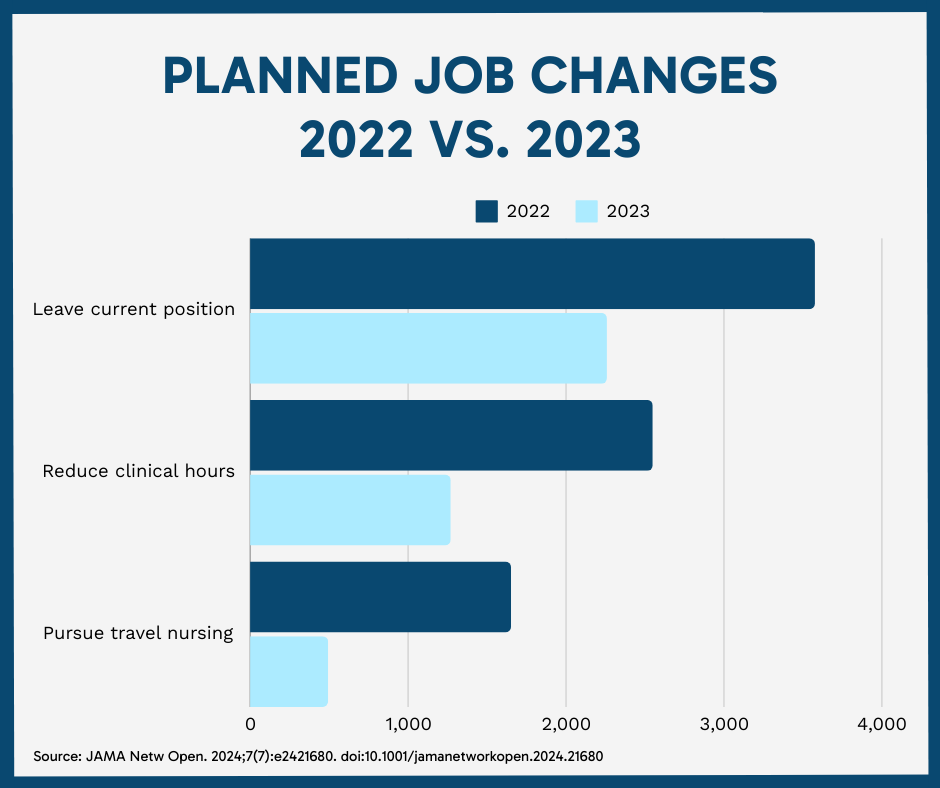
More than 7,000 Michigan registered nurses were surveyed between May 17 and June 1, 2023, and 9,150 nurses were surveyed between Feb. 22 and March 1, 2022. In comparing the data sets, the study authors found a roughly 7% drop (39.1% in 2022 vs. 32% in 2023) in nurses who planned to leave their job within one year.
“Fewer nurses in the 2023 survey reported plans to leave their current position, reduce their clinical hours, or pursue travel nursing,” the authors stated. “These findings suggest somewhat improved working conditions and possible easing of workforce pressures.”
However, new questions posed to the 2023 cohort dug further into motivations for leaving an employer, revealing that 13% intended to leave the profession as a whole (excluding retirements). With retirements included, the number of nurses exiting the industry came in at 36%.
Christopher Friese, the study’s principal investigator and a nursing professor, said the demographics of those who plan to leave the profession are concerning because, in theory, they have “years left in their nursing careers.”
“These nurses are leaving the profession Americans have trusted the most for two decades,” Friese stated in a University of Michigan news release. “This is the group we should be listening to very carefully. And they are leaving because health care leaders are not addressing their valid concerns about their workplaces and chronic understaffing.”
The one-third of respondents who planned to leave their role were asked if experiencing abuse or a “violent workplace event,” emotional exhaustion, or poor patient safety were contributing factors in their decision.
“There may be larger societal factors associated with the high rate of planned departures observed in the present study, including general economic conditions, family factors, and alternative job opportunities,” the authors stated.
A ‘Welcome Shift,’ Despite ‘Serious Problems’
Karen Lasater, Ph.D. and RN, called the survey findings a “welcome shift” following years of reports citing burnout, turnout and vacancies. But similar to the authors, she noted in her commentary response to the University of Michigan analysis that “serious problems” persist.
“Efforts to train and recruit more nurses are akin to fueling a car with a leaking gas tank,” she wrote.
Without action from hospital or organizational leadership, Lasater argued, legislators must take the lead in addressing workforce concerns.
“Policymakers should allocate funding and regulatory efforts to evidence-based strategies that address the retention crisis at the source,” Lasater wrote. “Policymakers need not solve for a low workforce supply issue … Instead, policies are needed to address the low retention caused by employers’ chronic understaffing, rigid scheduling options, and lack of responsiveness to clinicians’ recommendations to improve care, which drives nurses to burnout and depart for better working conditions.”
Lasater named California’s registered nurse staffing standards as proof that legislative policy can help improve both patient outcomes and nurse retention. Other states have followed suit with minimum, and the American Nurses Association (ANA) endorses such policies.