What is an Ostomy?
An ostomy is a surgical procedure in which an opening, called a stoma, is created in the abdomen “to reroute the usual path of urine or stool as it exits the body,” according to the American Nurse Journal. Most ostomy patients wear a pouch that covers the opening in order to collect waste.
Several health conditions could result in the need for an ostomy, such as: cancer; bowel disease, including Crohn’s and diverticulitis; obstructions; birth defects; incontinence; and spinal cord injury.
There are three common types of ostomies:
- Colostomy- colostomies are typically in the lower left quadrant or right lower quadrant. Colostomies can be ascending (upward,) transverse (across), descending (downward), or sigmoid (curved).
- Ileostomy- Ileostomies are usually located in the right, lower quadrant.
- Urostomy- located in the right, lower quadrant.
Each patient’s situation is unique — some “grow up with an ostomy while others require surgery as adults” — and requires an individualized care plan, according to the American Nurse Journal.
Healthy Stoma vs. Unhealthy Stoma
A healthy stoma, according to the American Nurse Journal, is “red moist and shows signs of output.”
An unhealthy stoma may be dry, bleed or discharge from inside the stoma, and an unusual color change such as pale, blue, or even black.
Most common stoma complications
- Skin problems and irritation: Sore skin can be “extremely uncomfortable,” according to the Bladder and Bowel Community, and compromise pouch’s attachment to the skin. This can result in leaks and further skin damage. Several reasons exist for peristomal skin irritations, including: Fecal contact with the skin, Poor fitting stoma appliance; Skin irritation and allergies from products or the pouch; stoma bleeding
- Retraction or prolapse of the stoma: A stoma normally extends slightly above the skin level. The length of the extension depends on whether the patient has a colostomy or ileostomy. A retraction occurs when the stoma “lays flat to the skin or below skin surface level,” according to the Bowel and Bladder Community. It can affect how the stoma pouch fits and cause leaks. To resolve this, use a stoma pouch with a wafer to push the stoma forward and consider an ostomy belt for support or barrier rings to keep the output off the skin. In serious cases, a surgeon might suggest resetting the stoma. In a prolapse, the stoma “extends to an abnormal length” and is more susceptible to abrasions or infection. Prolapses are more common in loop colostomies (when a loop of colon is removed through a cut in the abdomen). A prolapse could occur because of a weak abdominal wall, rapid weight gain, pregnancy, surgical technique or a sudden pressure in the abdomen spurred by excessive coughing. Monitor prolapsed stomas for changes in size and color. A prolapsed stoma could also become extra obstructed making it impossible for feces to pass through. Nurses should seek advice from the provider if the patient’s stoma becomes obstructed or looks more pale than usual. As the nurse you may also need to change the patient’s stoma pouch to accommodate the size of the extended stoma. This is another instance where the patient’s surgeon may decide to re-sit the stoma should it become problematic.
- Peristomal hernias: A parastomal hernia occurs when loops of intestine bulge through “weakened abdominal muscles behind the stoma.” A bulge or lump formed behind the stoma is typically indicative of a hernia and can grow over time. A hernia can cause alternating diarrhea and constipation, cause the stoma to retract, or affect adherence of the bag. Peristomal hernia symptoms include:
- A dull ache or dragging sensation.
- Skin becoming thinner and tearing more easily when the stoma pouch is removed.
- Water can struggle to navigate collapsed loops of the patient’s bowel.
- In extreme cases, the loops of bowel may become obstructed, causing pain and vomiting. Nurses should get emergency medical attention if this occurs.
Roughly 70% of ostomies develop a hernia, but stoma belts and specialist support underwear can help reduce the risk. Nurses, in addition to monitoring the patient‘s weight, can also suggest the following: Don’t lift anything heavy in the first three months post-surgery; hold your abdominal muscles when coughing or sneezing; and wear light support from the start and while exercising.
Blockages and bowel obstructions with a stoma
Partial or complete bowel obstruction could occur with a stoma, due to foods that are difficult to digest or adhesions and scar tissues within the bowel that prevent waste from passing. Bowel obstruction symptoms include: Acute abdominal pain; no output or extremely watery output; nausea or vomiting; swollen and hard abdomen.
How can you assist in relieving the patient’s blockage?
- Increase the patient’s fluid intake.
- Have the patient take a warm bath.
- Ask the patient to draw their knees to their chest and rock from side to side.
Stoma leaks and odor
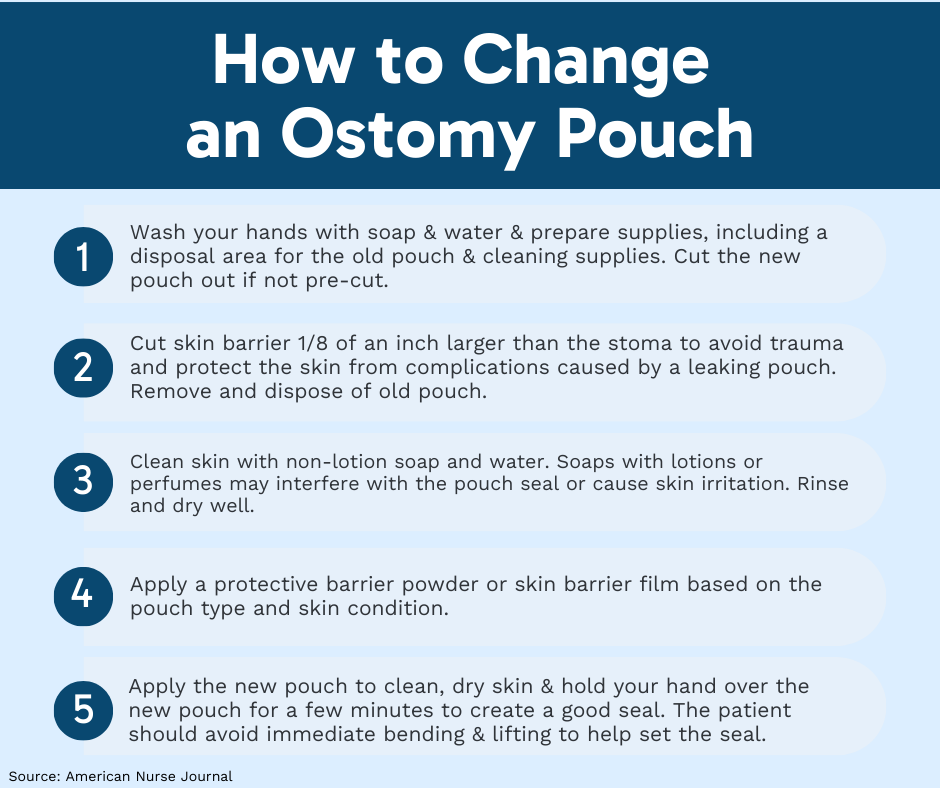
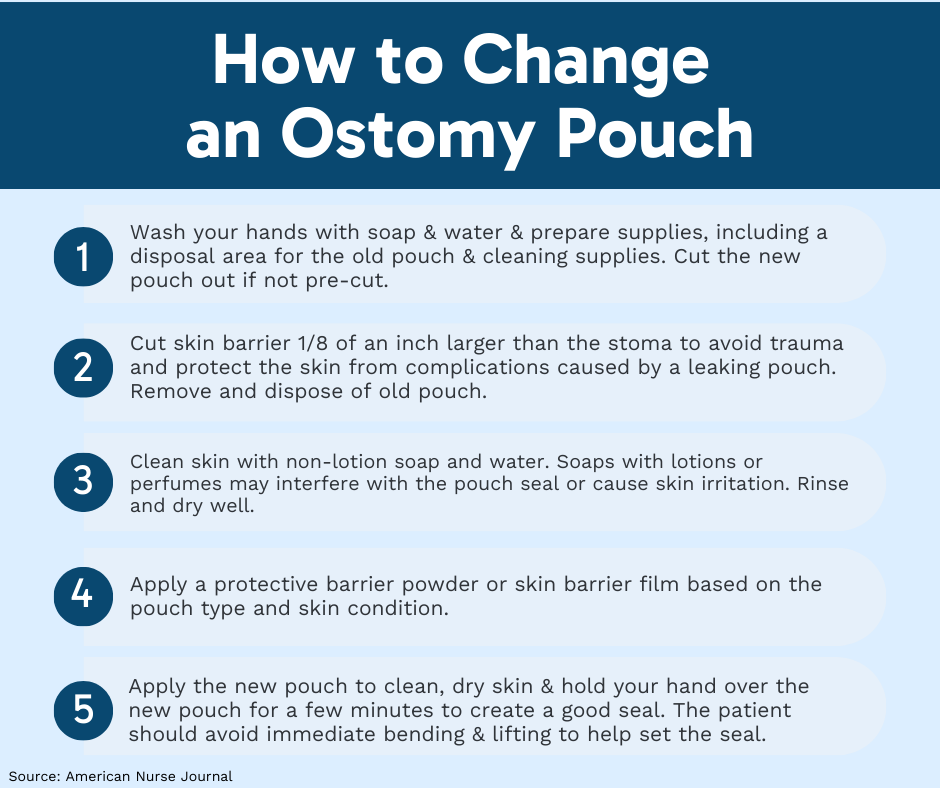
Itching or burning of the peristomal skin, odor, and the skin barrier edges lifting are indications that a pouch is about to leak, according to the American Nurse Journal. If a leak occurs, the entire pouch must be changed.
Common causes of leaks include:
Cutting the pouch too big or too small Skin folds or stoma within the skin fold Weight gain or loss, causing stoma size to change. Leaks can cause moisture-related skin damage, which should be treated with non-moisturizing soap and water, then rinsing and drying. Applying a “protective barrier powder” to the skin can help with healing, according to the American Nurse Journal. However, be sure to powders and barrier films approved for ostomy use. Avoid alcohol-based products because they could further damage the skin. Odor can be reduced by putting odor reducing drops in the ostomy pouch after changing.