What Are Push Dose Vasopressors?
As an emergency room nurse, transporting a trauma patient with a labile blood pressure can be tenuous. If the patient develops significant hypotension, dysrhythmias, or cardiac arrest, what life-saving tools do you have in your toolbox? Managing the hypotensive patient is an essential skill in the emergency department (ED) as prolonged hypotension can lead to poor clinical outcomes in high-risk patients.
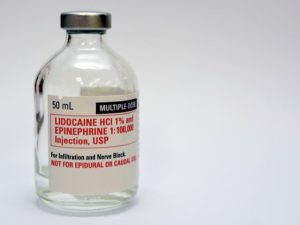
A rapid bolus of crystalloid fluids, either non-balanced 0.9% normal saline (NS) or balanced sodium lactate (LR), even when administered via pressure bag, requires time to produce a notable effect on hypotension. Depending on the policies and procedures of your institution, push-dose phenylephrine (PDP-PE) or epinephrine (PDP-E) can resolve transitory hypotension as a temporizing measure. Both drugs are safe to use in peripheral lines and are not complex to mix, but they can be prone to dosing errors.
The administration of push-dose vasopressors requires nursing diligence as they carry inherent risks, including miscalculations of dilution, dose calculations errors, push-dose administration errors, reliance on verbal orders and overriding medication safety checks during emergency use.
What is a push-dose pressor (PDP)? Push-dose vasopressors are small intravenous bolus doses (pushes) administered to hypotensive patients to increase cardiac output and brain perfusion. In the emergency room, the most common push-dose pressors are phenylephrine and epinephrine.
The indications for PDP are based on the urgent reversal of hypotension. Both phenylephrine and epinephrine are temporary measures to increase the perfusion of vital organs, and neither replaces proper resuscitation efforts.
Important indications on epinephrine. Epinephrine is the preferred drug over phenylephrine in patients with cardiogenic shock because phenylephrine may decrease cardiac output secondary to the potential for reflexive bradycardia.
Push-dose vasopressors in trauma patients is an accepted clinical practice. It is important that their reliance does not mask inadequate fluid resuscitation.