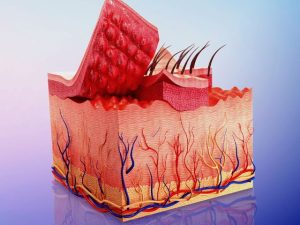
Areas of Focus in an Integumentary Assessment
The following areas are important to focus on when completing an integumentary exam:
Ask Questions
Nurses must ask the patient or family member questions regarding any history of skin problems, allergic reactions, and family history of skin disorders.
Symptoms or Complaints
Questions should be asked about the onset, duration, and frequency of symptoms. It is important to ask specific questions about the skin, hair, and nails.
Pain
Ask specific questions about any pain relating to the skin, hair, and nails. It is important to ask about the type of pain, duration, any triggers, pain level on a scale of 0-10, and any treatments that have been used.
Inspect Color of the Skin
Is the color the same all over? Or different? Are there areas of hyperpigmentation or hypopigmentation? Look carefully at the skin tones and be mindful that these can range from pink to darkish brown. Observe for any lesions, rashes, moles, and freckles.
Are there any skin discolorations such as pallor – the loss of the pinkish tones of the skin due to decreased blood flow to the surface of the skin; erythema – a reddish color to the skin due to a rush of blood to the surface of the skin typically due to inflammation; cyanosis – a bluish tone to the skin due to a decrease in oxygenation to the tissues which usually indicates hypoxemia; jaundice – a yellow tint to the skin, sclera of the eye, or mucous membranes due to increased levels of bilirubin in the blood.
Inspect and Palpate the Skin
Assess for temperature, moisture, thickness, texture, and turgor.
Assess for Edema
Edema is due to the accumulation of fluid in the intercellular spaces. It is important to assess for pitting edema and grade the edema on a scale based on mild, moderate, deep, and very deep pitting edema.
Inspect and Palpate the Nails
Assess the nail beds, length of nails, appearance, and nail edges.
Inspect and Palpate the Hair
Analyze color, texture, and distribution of the hair.