Course
Autonomic Dysfunction in SCI
Course Highlights
- In this Autonomic Dysfunction in SCI course, we will learn about spinal cord injuries.
- You’ll also learn about autonomic dysreflexia and its pathophysiology.
- You’ll leave this course with a broader understanding of the signs and symptoms of autonomic dysreflexia.
About
Contact Hours Awarded: 3
Course By:
Joe Brandon
BSN, RN, CRRN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Autonomic dysreflexia is a potentially life-threatening complication that affects individuals with spinal cord injuries at or above the sixth thoracic level 6 (T6) (1, 2). Autonomic dysreflexia is characterized by an uncontrolled sympathetic nervous system response to various stimuli, leading to hypertension, tachycardia, and other systemic symptoms (3, 4).
As healthcare professionals, it is essential to understand the effects of autonomic dysreflexia on our patients with spinal cord injuries, as well as how to provide quick and proficient treatment to avoid more severe consequences.
This course will focus solely on the underlying causes, effects, and front-line treatments of autonomic dysreflexia and the education the healthcare provider can give their clients to proactively avoid and treat this disorder in both the clinical and nonclinical setting. Throughout the course, we will follow Mr. Jose Nieves, a 32-year-old male with a T4 spinal cord injury. The case study will demonstrate the disease process and explain the treatment of the client’s autonomic dysreflexia effectively.
Case Study
Jose Nieves is a 32-year-old male with a T4 spinal cord injury following a motor vehicle accident. He presents with symptoms that include a severe headache, profuse sweating, and a sudden increase in blood pressure.
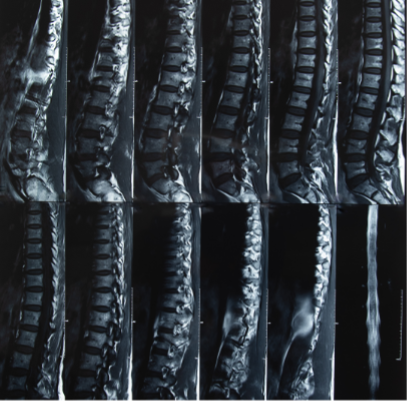
Spinal Cord Injury
The spinal cord is a delicate, tube-like structure that contains millions of neurons responsible for transmitting signals between the brain and all bodily systems (3). A spinal cord injury results when the spinal cord is damaged due to compression, contusion, or laceration. This disrupts the standard transmission of signals, creating a cascade of adverse signaling effects.
The injury can be classified into two main categories: complete and incomplete. A complete spinal cord injury results in total separation of the spinal cord and results in loss of motor and sensory function at and below the level of injury. An incomplete spinal cord injury is damage due either to compression or partial separation and results in damage but also may preserve some degree of motor and sensory function.
Individuals who sustain these injuries are subject to a plethora of other ailments because of their primary spinal cord injury, one of the most common and severe being autonomic dysreflexia.
Definition
Autonomic dysreflexia is a potentially life-threatening complication that affects individuals with spinal cord injuries at or above the sixth thoracic level T6 (1, 2). Autonomic dysreflexia is characterized by the nervous system’s uncontrolled sympathetic response to various stimuli, leading to hypertension, tachycardia, and other systemic symptoms (3, 4).
The definition of autonomic dysreflexia has evolved to include added nonexclusive parameters. Autonomic dysreflexia is now recognized as a complex condition that requires an immediate and practical approach to managing the potentially fatal pitfalls associated with its side effects.
Autonomic dysreflexia requires prompt recognition as well as fast interventional treatment as it can lead to severe complications if left untreated that include things such as stroke, heart failure, and even death in the most severe cases. Healthcare professionals should be aware of the signs and symptoms of autonomic dysreflexia, take an aggressive approach to managing the condition in the clinical setting, and ensure that the client is correctly educated to have the best chance of a positive outcome when returning to their prospective daily lives.


Self-Quiz
Ask Yourself...
- Who is affected by autonomic dysreflexia?
- What are the dangers of some of the more severe cases of autonomic dysreflexia?
- Are healthcare providers given the knowledge and tools to identify autonomic dysreflexia?
Assessment
An assessment based on knowing what to look for is crucial in identifying autonomic dysreflexia in spinal cord injury patients. Healthcare professionals should be vigilant for signs of autonomic dysreflexia, which could include hypertension, tachycardia, headache, sweating, and flushing (5, 6). The Ashworth Scale and the Spinal Cord Injury Autonomic Dysreflexia Scale (SCI-ADS) are valuable tools for assessing autonomic dysreflexia severity (7, 8).
Wrinkled sheets can cause pressure points and skin irritation, which can trigger autonomic dysreflexia in individuals with spinal cord injuries (1). The client’s bed sheets, clothing, and shoes should be checked for wrinkles or creases. It is also wise to check the client’s bladder for fullness, as an inability to empty a full bladder is often the cause.
A thorough assessment should also include reviewing the patient’s medical history, any medications the client may have taken, and any previous autonomic dysreflexia episodes the patient may have experienced.
Regular assessment of these clients is essential as it enables healthcare professionals to monitor for signs of autonomic dysreflexia and promptly intervene and manage triggers, possibly preventing episodes, which can help reduce the risk of severe consequences, including hypertension, headaches, and even death (3). A comprehensive assessment of autonomic dysreflexia should include a thorough physical examination, which most notably contains accurate blood pressure and the patient’s current heart rate, as an elevation of either could indicate autonomic dysreflexia.
A client’s list of current medications and the addition or discontinuation of any medications will also help find the root of the problem.
A medical history that includes autonomic dysreflexia may point the clinician in the right direction. Each patient’s unique circumstances can help healthcare clinicians better identify potential triggers and develop an effective treatment plan to help manage any future incidences the patient may have.


Self-Quiz
Ask Yourself...
- Why is assessment of this population so critical?
- What main warning signs should the clinician assess for?
- Is there a good starting place for these assessments?
Case Study
Upon assessment, it is determined that Mr. Nieves is experiencing autonomic dysreflexia. The healthcare team promptly recognizes the signs and symptoms of autonomic dysreflexia, including hypertension and tachycardia, and initiates appropriate interventions.
Epidemiology
Studies suggest that autonomic dysreflexia affects approximately 50-70% of individuals with spinal cord injuries at or above a level T6 (9, 10). The incidence of autonomic dysreflexia increases with the level of injury as well as the completeness of the spinal cord injury itself, adding to the complications one with a spinal cord injury is already faced (11). The epidemiology of autonomic dysreflexia is complex and can be influenced by various uncontrollable risk factors that often include the client’s age, gender, and any comorbidities the patient previously suffered from.
The epidemiology of autonomic dysreflexia is an essential area of study. It can help healthcare professionals understand the risk factors and prevalence of the condition, thereby enabling the sufferer to enjoy a better quality of life. The information gathered can help develop targeted interventions and improve patient outcomes.

Self-Quiz
Ask Yourself...
- What are some of the primary factors that increase the risk of developing autonomic dysreflexia in individuals with spinal cord injuries?
- What level and severity of spinal cord injury patients run the most significant risks?
Pathophysiology
Autonomic dysreflexia occurs when the sympathetic nervous system is disrupted, leading to an uncontrolled response to stimuli (12). The exact mechanisms are multifaceted and involve the interplay between the sympathetic and parasympathetic nervous systems (13). During Autonomic Dysreflexia, the relay between neurons is disrupted, leading to an uncontrolled sympathetic response. In healthy individuals, neurons communicate through a complex process involving electrical and chemical signals. However, in individuals with spinal cord injuries, the injury can damage the neural pathways, disrupting the standard transmission of signals (3). Further research is still needed to fully understand the pathophysiology of autonomic dysreflexia as well as the development of effective management strategies to treat the disorder.
The pathophysiology of autonomic dysreflexia is a complex and multifaceted process involving the interplay between various physiological systems and the external factors triggering their responses. Further research is needed to understand the underlying mechanisms and develop targeted interventions fully.

Self-Quiz
Ask Yourself...
- What are the neurological mechanisms involved in causing autonomic dysreflexia?
- How do the neurological pathways of this patient population differ from those that have not endured a spinal cord injury?
Clinical Signs and Symptoms
Common clinical signs and symptoms of autonomic dysreflexia include hypertension, tachycardia, headache, sweating, flushing, and cardiac arrhythmias (14). Yet another first warning sign is ecchymosis, often around the face, shoulder, chest, and neck. In severe cases of autonomic dysreflexia may lead to seizures, coma, and even death may occur as a result (15). Recognizing the early signs and symptoms of the disease process is essential in preventing complications.
Early recognition of autonomic dysreflexia is critical, as it can help prevent serious complications. Clinicians should always be aware of these signs and symptoms, take a proactive approach to managing the condition and teaching, and teach the client the skills he or she needs to manage these symptoms in a nonclinical setting.

Self-Quiz
Ask Yourself...
- What are some early warning signs the client is experiencing autonomic dysreflexia?
- What are the signs and symptoms of severe autonomic dysreflexia, and how do these issues put the client’s cardiovascular system at risk?
Case Study
Mr. Nieves’ healthcare team immediately addresses his autonomic dysreflexia, first checking his shoes and clothing to alleviate ant triggering stimulus. His bladder is also assessed for extension, and an ultrasound is performed to check for any urine that may be retained. Additionally, they administer antihypertensive medication to reduce his blood pressure and prevent further complications rapidly.
Etiology
Various stimuli can trigger autonomic dysreflexia in spinal cord injury patients, including urinary tract infections, inability to void, bowel distension, and pressure sores (16). Other potential triggers include medication side effects and recent surgical procedures (17). Identifying and managing these triggers is crucial in preventing episodes of autonomic dysreflexia.
Identifying and managing triggers is an important aspect of managing and caring for these patients. Healthcare clinicians should work closely with patients and ask questions to identify potential triggers and develop strategies to prevent future episodes of autonomic dysreflexia.

Self-Quiz
Ask Yourself...
- What questioning methods can the healthcare provider use to identify the clients’ triggers?
- Are there risk factors that all spinal cord injury patients have in common that the clinician should universally assess for?
Treatment
Prompt recognition and management of autonomic dysreflexia is a critical part of the prevention of complications. The clinician should check for irritating stimuli, starting with the most noninvasive option. This would include things such as wrinkled sheets, tight shoes, or something poking the patient’s skin. Other treatment options may consist of pharmacological interventions, such as vasodilators and antihypertensives, as well as nonpharmacological approaches, such as elevation of the head of the bed (18, 19).
A study published in the Journal of Neurotrauma found that early administration of vasodilators reduced the severity of autonomic episodes (23). Individualized treatment plans should be developed for each patient in preparation for autonomic dysreflexia, considering their individualized needs and circumstances.
To produce the best clinical outcomes, treatment of autonomic dysreflexia must be approached from a position of preparation. Healthcare professionals should work with patients to develop a comprehensive treatment plan that addresses their unique needs and circumstances.


Self-Quiz
Ask Yourself...
- How can a thorough assessment lead to better patient outcomes by way of early recognition?
- What pharmacological measures can be taken early on to help reduce the effects of negative cardiovascular responses caused by autonomic dysreflexia?
Safety Considerations
Healthcare professionals must be aware of the potential risks associated with autonomic dysreflexia. The more severe risks include cardiac complications and respiratory failure (20). Appropriate assessment and fast clinical interventions are essential to ensuring patient safety. The American Association of Spinal Cord Injury Nurses recommends closely monitoring patients with autonomic dysreflexia, including continuous blood pressure and heart rate assessments (24). More clients at risk of experiencing autonomic dysreflexia should be educated on self-management strategies and when to seek medical attention.
Patient education is an important aspect of the management of autonomic dysreflexia. To ensure their safety and well-being, patients should be educated on self-management strategies, including how to do assessments in the nonclinical setting, how to re-leave their bladder, when and how to ask a trusted family member for assistance, and when to seek medical attention.


Self-Quiz
Ask Yourself...
- What role does the client’s level of injury play in determining their risks of autonomic dysreflexia?
- How does education impact the patient’s ability to be more self-sufficient and improve one’s quality of life?
Case Study
After successful management of the acute episode, Mr. Nieves is closely monitored for any lingering effects and provided with education regarding autonomic dysreflexia. A follow-up appointment is scheduled to assess his condition and answer any questions. This appointment will also be used as an opportunity to reinforce and assess the client’s knowledge of the disorder and reinforce any teaching that may have been missed.
Conclusion
Autonomic dysreflexia is a critical concern for individuals with spinal cord injuries, particularly those at or above the T6 level. Healthcare professionals play a crucial part in understanding, identifying, and managing this potentially life-threatening condition. Clinicians are also the first point of contact for education regarding the disorder.
The course objectives, including defining autonomic dysreflexia, recognizing its signs and symptoms, understanding its effects, and implementing evidence-based management strategies, are essential for providing effective care to these patients, thus ensuring that they have an improved quality of life.
By conducting a thorough assessment, healthcare providers can promptly identify autonomic dysreflexia at its onset and initiate appropriate interventions, potentially preventing severe complications, including death. Additionally, educating patients on recognizing and managing autonomic dysreflexia in nonclinical settings is vital for their well-being.
Healthcare professionals must stay updated on evidence-based guidelines and best practices to ensure optimal management of autonomic dysreflexia in spinal cord injury patients. By understanding the pathophysiology, recognizing the signs and symptoms, and implementing appropriate interventions, healthcare professionals can play a pivotal role in mitigating the risks associated with autonomic dysreflexia and promoting the well-being of individuals with spinal cord injuries.

Self-Quiz
Ask Yourself...
Final Reflection Questions
- What are the potential consequences of untreated autonomic dysreflexia, and how can healthcare professionals mitigate these risks?
- How does the level and completeness of spinal cord injury impact the incidence and severity of autonomic dysreflexia?
- What roles do sympathetic and parasympathetic nervous systems play in the pathophysiology of autonomic dysreflexia?
- How can healthcare professionals differentiate between autonomic dysreflexia and other conditions with similar symptoms, such as hypertension or anxiety attacks?
- What are the benefits and limitations of using vasodilators and antihypertensives in managing autonomic dysreflexia?
- How can patients with spinal cord injuries be empowered to manage their autonomic dysreflexia episodes, and what education and support are necessary to facilitate self-management?
- What are the implications of autonomic dysreflexia for patients’ quality of life, and how can healthcare professionals address these concerns?
- How does autonomic dysreflexia affect patients’ mental health and emotional well-being, and what interventions can be implemented to address these issues?
- What are the potential interactions between autonomic dysreflexia and other comorbidities, such as diabetes or cardiovascular disease?
- How can healthcare professionals optimize the management of autonomic dysreflexia in patients with complex medical histories or multiple comorbidities?
- What are the ethical considerations surrounding the management of autonomic dysreflexia, particularly regarding patient autonomy and decision-making capacity?
- How can healthcare professionals balance the need for prompt intervention in autonomic dysreflexia with the risk of over-treatment or medication side effects?
- What are the implications of autonomic dysreflexia for patients’ social and family relationships, and how can healthcare professionals address these concerns?
- How can healthcare professionals facilitate communication and collaboration among patients, family members, and healthcare teams to optimize autonomic dysreflexia management?
- What are the potential applications of emerging technologies, such as wearable devices or mobile apps, in monitoring and managing autonomic dysreflexia?
- How can healthcare professionals ensure cultural sensitivity and individualized care for patients with autonomic dysreflexia from diverse backgrounds?
- What are the implications of autonomic dysreflexia for patients’ sexual health and fertility, and how can healthcare professionals address these concerns?
- How can healthcare professionals optimize the management of autonomic dysreflexia in patients with spinal cord injuries at different levels and completeness?
- What are the potential interactions between autonomic dysreflexia and other spinal cord injury-related complications, such as pressure ulcers or respiratory failure?
- How can healthcare professionals facilitate patient education and empowerment to prevent autonomic dysreflexia episodes and optimize management?
- What are the implications of autonomic dysreflexia for patients’ vocational and recreational activities, and how can healthcare professionals address these concerns?
- How can healthcare professionals optimize the management of autonomic dysreflexia in patients with comorbid mental health conditions, such as anxiety or depression?
- What are the potential benefits and limitations of alternative and complementary therapies, such as acupuncture or massage, in managing autonomic dysreflexia?
- How can healthcare professionals ensure continuity of care and coordination of services for patients with autonomic dysreflexia across different healthcare settings?
- What are the potential consequences of untreated autonomic dysreflexia, and how can healthcare professionals mitigate these risks? Consider the impact on cardiovascular health, respiratory function, and patient quality of life.
- How does the level and completeness of spinal cord injury impact the incidence and severity of autonomic dysreflexia? Discuss the differences in presentation and management between patients with incomplete and complete injuries.
- What roles do sympathetic and parasympathetic nervous systems play in the pathophysiology of autonomic dysreflexia? Explain the neural pathways involved and how they contribute to the development of autonomic dysreflexia.
- How can healthcare professionals differentiate between autonomic dysreflexia and other conditions with similar symptoms, such as hypertension or anxiety attacks? What diagnostic tools and assessments are most helpful in making an accurate diagnosis?
- What are the benefits and limitations of using vasodilators and antihypertensives in managing autonomic dysreflexia? Consider the potential interactions with other medications and the impact on patient outcomes.
- How can patients with spinal cord injuries be empowered to manage their autonomic dysreflexia episodes, and what education and support are necessary to facilitate self-management? Discuss the importance of patient-centered care and shared decision-making.
- What are the implications of autonomic dysreflexia for patients’ quality of life, and how can healthcare professionals address these concerns? Consider the impact on daily activities, relationships, and mental health.
- How does autonomic dysreflexia affect patients’ mental health and emotional well-being, and what interventions can be implemented to address these issues?
- Discuss the role of counseling, stress management, and social support.
- What are the potential interactions between autonomic dysreflexia and other comorbidities, such as diabetes or cardiovascular disease?
- How can healthcare professionals optimize management and minimize complications?
- How can healthcare professionals optimize the management of autonomic dysreflexia in patients with complex medical histories or multiple comorbidities?
- Consider the importance of interdisciplinary collaboration and individualized care plans.
- What are the ethical considerations surrounding the management of autonomic dysreflexia, particularly regarding patient autonomy and decision-making capacity?
- Discuss the importance of informed consent and patient-centered care.
- How can healthcare professionals balance the need for prompt intervention in autonomic dysreflexia with the risk of over-treatment or medication side effects?
- Consider the importance of careful monitoring and titration of medications.
- What are the implications of autonomic dysreflexia for patients’ social and family relationships, and how can healthcare professionals address these concerns?
- Discuss the importance of family support and counseling.
- How can healthcare professionals facilitate communication and collaboration among patients, family members, and healthcare teams to optimize autonomic dysreflexia management?
- Consider the importance of clear communication and shared goal setting with the client. What do they hope to gain by a better understanding of autonomic dysreflexia?
- What are the potential applications of emerging technologies, such as wearable devices or mobile apps, in monitoring and managing autonomic dysreflexia?
- Discuss the potential benefits and limitations of these technologies.
- How can healthcare professionals ensure cultural sensitivity and individualized care for patients with autonomic dysreflexia from diverse backgrounds? Consider the importance of cultural competence and patient-centered care.
- What are the implications of autonomic dysreflexia for patients’ sexual health and fertility, and how can healthcare professionals address these concerns?
- Discuss the importance of open communication and specialized care.
- How can healthcare professionals optimize the management of autonomic dysreflexia in patients with spinal cord injuries at different levels and completeness? Consider the importance of individualized care plans and specialized expertise.
- What are the potential interactions between autonomic dysreflexia and other spinal cord injury-related complications, such as pressure ulcers or respiratory failure? How can healthcare professionals minimize these risks?
- How can healthcare professionals facilitate patient education and empowerment to prevent autonomic dysreflexia episodes and optimize management? Consider the importance of patient-centered care and shared decision-making.
- What are the implications of autonomic dysreflexia for patients’ vocational and recreational activities, and how can healthcare professionals address these concerns? Discuss the importance of occupational therapy and rehabilitation.
- How can healthcare professionals optimize the management of autonomic dysreflexia in patients with comorbid mental health conditions, such as anxiety or depression? Consider the importance of interdisciplinary collaboration and individualized care plans.
- What are the potential applications of alternative and complementary therapies, such as acupuncture or massage, in managing autonomic dysreflexia? Discuss the possible benefits and limitations of these therapies.
- How can healthcare professionals ensure continuity of care and coordination of services for patients with autonomic dysreflexia across different healthcare settings?
- Consider the importance of quality of life for the client. What does an incidence of autonomic dysreflexia look like in the home setting, and what types of tools may enable the patient to best treat this condition in public?
Appendix
A. Glossary of Terms
- Autonomic dysreflexia: a potentially life-threatening complication of spinal cord injury characterized by an uncontrolled sympathetic response to various stimuli.
- Spinal cord injury: a traumatic injury to the spinal cord resulting in partial or complete loss of motor and sensory function.
- Sympathetic nervous system: a branch of the autonomic nervous system responsible for the “fight or flight” response.
- Parasympathetic nervous system: a branch of the autonomic nervous system responsible for promoting relaxation and reducing stress.
- Vasodilators: medications that dilate blood vessels and reduce blood pressure.
- Antihypertensives: medications that reduce blood pressure.
- Hypertension: elevated blood pressure.
- Tachycardia: rapid heart rate.
- Headache: pain in the head or neck region.
- Sweating: excessive perspiration.
- Flushing: redness of the skin.
- Cardiac arrhythmias: abnormal heart rhythms.
B. Resources
American Association of Spinal Cord Injury Nurses (AASCIN)
National Spinal Cord Injury Association (NSCIA)
Spinal Cord Injury Research Network (SCIRN)
Journal of Neurotrauma
Spinal Cord
Journal of Neurosurgery
C. Suggested Readings
Krassioukov et al. (2020). Autonomic dysreflexia in spinal cord injury: A review of the literature. Journal of Neurotrauma, 37(1), 1-12.
Elliott et al. (2019). Autonomic dysreflexia in spinal cord injury: A systematic review. Spinal Cord, 57(1), 1-14.
Karlsson et al. (2018). Autonomic dysreflexia in spinal cord injury: A review of the pathophysiology. Journal of Neurophysiology, 120(1), 1-9.
D. FAQ
Q: What is autonomic dysreflexia?
A: Autonomic dysreflexia is a potentially life-threatening complication of spinal cord injury characterized by an uncontrolled sympathetic response to various stimuli.
Q: What are some of the signs and symptoms of autonomic dysreflexia?
A: Common signs and symptoms of autonomic dysreflexia may include hypertension, tachycardia, headache, sweating, flushing, and cardiac arrhythmias.
Q: How is autonomic dysreflexia diagnosed?
A: Autonomic dysreflexia is diagnosed through clinical evaluation, medical history, and laboratory tests.
Q: What are the treatment options for autonomic dysreflexia?
A: Treatment options for autonomic dysreflexia include first nonpharmacological interventions such as bladder and skin checks, as well as assessing the patient’s footwear, ensuring that the size is proper, the elevation of the head of the bed, and removal of triggering stimuli and a second line defense that is noninvasive. Pharmacological interventions, such as vasodilators and antihypertensives, may be used and should be on hand with any patient at risk for autonomic dysreflexia.
Q: How can autonomic be prevented?
A: Autonomic dysreflexia can be prevented by identifying and managing triggers, such as urinary tract infections, bowel distension, and pressure ulcers, and ensuring the client’s bladder empties thoroughly.
Q: What is the prognosis for patients with autonomic dysreflexia?
A: The prognosis for patients with autonomic dysreflexia is generally good, given a proactive approach is taken, and it is appropriately managed, but complications can arise if left untreated.
References + Disclaimer
- Allen, K. J., & Leslie, S. W. (2023, May 30). Autonomic dysreflexia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482434/
- Alwashmi A. H. (2022). Spinal cord injury and autonomic dysreflexia: A case report on an overlooked complication of spinal cord injury. Cureus, 14(10), e30259. https://doi.org/10.7759/cureus.30259
- American Spinal Injury Association & International Spinal Cord Society. (2019, April). International Standards for Neurological Classification of Spinal Cord Injuries. https://www.asia-spinalinjury.org/wp-content/uploads/2019/10/ASIA-ISCOS-Worksheet_10.2019_PRINT-Page-1-2.pdf
- Cleveland Clinic. (2022, October 27). Autonomic dysreflexia (AD). https://my.clevelandclinic.org/health/diseases/24378-autonomic-dysreflexia-ad
- Harb, A., & Kishner, S. (2023, May 1). Modified Ashworth Scale. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK554572/
- Kaydok, E. (2023). Nurses and physiotherapists’ knowledge levels on autonomic dysreflexia in a rehabilitation hospital. The Journal Of Spinal Cord Medicine, 46(4), 569–573. https://doi.org/10.1080/10790268.2021.1983313
- Khan, Y. S., & Lui, F. (2023, July 24). Neuroanatomy, spinal cord. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559056/
- Mercado, J., Ruiz, A., & Parsh, B. (2022). Autonomic dysreflexia: Recognition and intervention. Nursing2025, 52(10), 10-10. https://www.nursingcenter.com/journalarticle?Article_ID=6457644#P30
- National Institute of Neurological Disorders and Stroke. (2025, January). Spinal cord injury. https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury
- Paralyzed Veterans of America. (2001, July). Acute management of autonomic dysreflexia: Individuals with spinal cord injury presenting to health-care facilities, 2nd Edition. Consortium for Spinal Cord Medicine Clinical Practice Guidelines. https://pva.org/wp-content/uploads/2021/09/cpg_autonomic-dysreflexia.pdf
- Solinsky R. (2023). Autonomic dysreflexia: Current pharmacologic management. PM & R: The Journal of Injury, Function, and Rehabilitation, 15(12), 1519–1523. https://doi.org/10.1002/pmrj.13051
- Trueblood, C. T., Singh, A., Cusimano, M. A., & Hou, S. (2024). Autonomic dysreflexia in spinal cord injury: Mechanisms and prospective therapeutic targets. The Neuroscientist: A Review Journal Bringing Neurobiology, Neurology and Psychiatry, 30(5), 597–611. https://doi.org/10.1177/10738584231217455
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
