Course
Heart Failure Updates
Course Highlights
- In this Heart Failure Updates course, we will learn about Identify the many risk factors for HF.
- You’ll also learn the impact HF has on society and healthcare costs.
- You’ll leave this course with a broader understanding of newer medications and treatments.
About
Contact Hours Awarded: 1
Course By:
Elaine Enright
Author’s Credentials
RN, BS, AD
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
In 1997, Heart Failure (HF) was designated an epidemic due to the significant increase in hospitalizations. (2) This increase in hospitalizations appears to be due to accurate management of HF patients who re-hospitalize for stabilization and medication management rather than a new diagnosis or end-stage disease.
HF occurs when the heart is too weak to pump blood to the body and lungs. The blood then backs up into the heart, lungs, and lower extremities, causing less blood supply to the body. HF can also be so severe that it can cause death in patients. (1)
It is crucial for nurses to understand the pathophysiology of HF, risk factors, and what education and treatment a nurse can incorporate in the plan of care, which will slow the progression of disease and maintain quality of life.

Self Quiz
Ask yourself...
- How can you find the costs associated with HF patients at your place of work? What treatments are helping manage HF patients?
- How would you assess an HF patient on your initial encounter as a nurse?
Statistical Evidence/Epidemiology
Epidemiologists study a disease's incidence, mortality, and prevalence to predict health care costs, how many people have a disease, how it affects society, and when the numbers of a disease change.
According to the CDC, there are approximately 6.2 million patients with heart failure in the United States. The diagnosis was noted on 13.8% of death certificates in 2018. (2) $30.7 billion was spent on HF in 2012, including health care costs, days away from work, and medications that treat HF.
Although HF is higher in the elderly population, the more significant number of patients ages 35 and above who die with HF are concentrated in the southeast, southwest, Indiana, Wisconsin, and Illinois, with some counties in Utah, Oregon, Montana, South Dakota, and Nebraska.
Readmission rates declined when the Hospital Readmission Reduction Program (HRRP) began in 2012 to reduce costs and deliver care more safely.
Hospitals are penalized by the Centers for Medicare and Medicaid to lower readmission rates to less than 30 days for some diagnoses, and HF was among them. Hospitals began to look closer at the readmission rates, which helped them to focus on improved management. (2) . Using the information below, nurses can better assess the patient and add more information to their care plan.
The classifications of HF as defined by the New York Heart Association are:
- No symptoms with regular physical activity.
- Some mild symptoms with physical activity but not at rest
- Comfortable at rest but with moderate symptoms with some minor physical activity.
- Severe shortness of breath with rest. (2)
Providers typically use echocardiograms to measure heart failure using the ejection fraction (EF) percentage. Ejection fraction demonstrates the blood pumping rate from the left ventricle to the body.
An EF of below 30% indicates severe disease, while an EF at or above 50% indicates milder or no condition. Left ventricular failure with an EF of 50% or above is considered HF with preserved EF. An EF of 30% or below is considered HF with reduced EF. There is now a new category called HF with mid-range, which shows an EF of 40%-50%.
Approximately 15% of the HF population shows mid-range EF.
Incidence - is the number of new disease cases in certain patients. In HF, this number also helps scientists understand how the prevalence of the disease results from a lifestyle change. These studies aid in determining the burden of HF on society, which in turn helps to make changes in public policy and, eventually, how HF patients are treated. "For HF, incidence as a measure of new cases is particularly helpful to assess how the occurrences of HF might have changed over time as a result of changes in risk factors." (2)
Prevalence - measures the commonality of a disease, in this case HF, in the at-risk population at or over a given time. It also measures how often an HF patient will be encountered. (6)
Mortality - CHF is one of the top causes of death. Mortality rates are high, and the data shows that 50% of HF patients die at or within five years of diagnosis. (2) More recent studies show mortality rates in HF are increasing, which may be due in part to an aging population.

Self Quiz
Ask yourself...
- Where can you find more information on the epidemiology of HF?
- Where do epidemiologists get their information?
- Can you define the difference between incidence and prevalence?
Etiology and Pathophysiology
Heart failure is often caused by an injury to the heart's muscle, such as Myocardial Infarction (MI), valvular regurgitation, stenosis of the heart's valves, and arrhythmia. (4) It is essential that the provider determines the cause to treat these patients appropriately.
The most common cause of HF is cardiovascular disease. When fatty deposits or plaque buildup in the vessels supplying the heart, the arteries become narrowed and decrease blood flow to the heart muscle. This can cause ischemia (lack of oxygen) to the area of the heart's power involved, causing an MI. This, in turn, causes damage to the heart's muscle, reducing its ability to pump normally.
There are two main types of HF:
- Left ventricular HF or systolic (LHF)
- Right ventricular HF or diastolic (RHF)
LHF occurs when the damage to the left ventricle occurs, and RHF occurs when the damage is to the right ventricle.
The following Table taken from the National Institutes of Health shows comorbidities for Systolic and Diastolic HF:
Systolic (LHF)
- Coronary Heart disease
- Arterial Hypertension
- Valvular Heart Disease
- Arrhythmias
- Inflammatory disease
- Idiopathic cardiomyopathy
- Toxic Cardiomyopathy (alcohol)
Diastolic (RHF)
- Diabetes Mellitus
- Arterial Hypertension
- Valvular Heart Disease (pressure load)
- Hypertrophic Cardiomyopathy
- Restrictive Cardiomyopathy
- Constrictive Pericarditis
- Amyloidosis (storage disease)
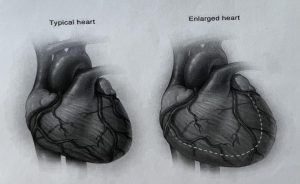
HF causes volume overload in the ventricles of the heart. This is due to enlargement and stiffness of the ventricles, so they cannot pump enough blood to the lungs and the body. (1,4) The nurse can utilize this information to care for the patient and implement essential treatments.
Genetics also play a role in HF but are varied and complex. Studies have found more than 100 genes that may contribute to cardiomyopathy. Depending on where the failure occurs, more genetic testing is recommended in some instances: Left, Right, or Biventricular determines what signs and symptoms may be present in a patient.
In a patient with an MI or volume/pressure overload, the whole heart will change in structure and function. There will be hypertrophy of the Left ventricle and the dilatation of the chambers, which will cause further deterioration in cardiac function. (4)
Certain medications may also lead to HF in some patients. These are the diabetic medications Actos and Avandia. NSAIDS (non-steroidal inflammatory drugs) and certain medicines that treat hypertension, cancer, blood dyscrasias, mental health, lung urinary issues, and infections. (1)
Aging also contributes as the heart's ability to work decreases over time. Too much alcohol and smoking are also important considerations. Heart failure may also cause complications such as kidney damage and failure, more heart problems, and liver disease caused by the backup of fluid that the liver cannot handle.
The photo below shows the difference between a normal heart and an enlarged one (12).
Preventable and non-preventable risk factors for heart disease are:
- Poor diet
- Smoking
- Lack of exercise
- Alcoholism
- Obesity
- Genetics/Race-non preventable
It is also known that Hispanic women are at higher risk for diabetes, which can lead to heart disease if their diabetes is not managed well. Also, African American men are at higher risk for heart disease, possibly leading to HF.
Interestingly, some studies have shown that the incidence of hospitalizations has declined. This may be due to early diagnosis, better use of medications and newer devices, earlier and ongoing patient education of risk factors, and stellar outpatient and preventive care of those patients living with HF or at risk in the community (2).

Self Quiz
Ask yourself...
- Why do you think certain diseases and medications contribute to heart disease?
- How would you plan to educate your new patient on this disease?
- What are the mechanisms of HF that may cause other diseases?
Diagnostic and Screening Tools for Heart Failure (HF)
Essential diagnostic screening tools are heart rate, cholesterol testing, blood pressure, and weight. Blood pressure measurement is one of the most critical tests since it can have no symptoms.
If high, it significantly increases the risk of cardiac disease. Fortunately, diet exercise can control blood pressure to lose weight if needed, and medications.
According to the American Heart Association, the standard for blood pressure is 120/80 or below and should be measured starting at age 20. (5) Next is the fasting cholesterol profile. Again, starting at age 20, a fasting lipid profile should be done. (5) This will give the provider and patient a baseline to follow and assist nurses in developing and implementing care plans.
The following chart describes lab values for cholesterol. As you can see, the values in red are at the highest risk for cardiovascular disease, which could lead to HF.
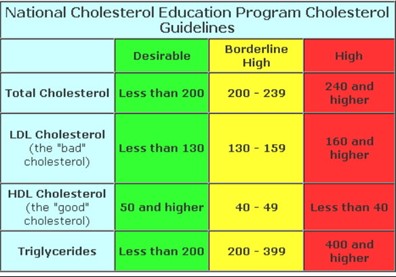
(13)
Body habitus is another crucial factor in predicting CAD. Body mass index (BMI), Waist measurements, and body structure can help predict how at risk a patient is for many diseases, including CAD, diabetes, atrial fibrillation, HF, and stroke. (7)
The typical Western diet is full of fats and sugars. In the US, many processed foods containing high salt, fat, and sugar are used.
These foods are unhealthy for the body and cause obesity and poor health. The Mediterranean diet, in turn, is full of fresh fruits and vegetables, lean meat, and a few processed foods. This is the most recommended diet for all populations.
High blood glucose is another indicator of poor health. Insulin resistance is the precursor to diabetes. A patient has insulin resistance when the body's muscles and tissues cannot respond to insulin, so glucose increases in the blood. (5)
Causes of insulin resistance are thought to be obesity with a large waist measurement. Blood glucose is usually tested with routine blood work. This gives the provider knowledge if a patient is at risk for diabetes and, therefore, heart disease. (5) Smoking and lack of physical activity can cause poor health, which may lead to cardiovascular disease.
Echocardiogram, Holter monitoring, stress tests, and nuclear stress tests are routinely used when a patient presents with symptoms of or has known cardiovascular disease. These tests provide a look at heart function and are used to determine disease progression or maintenance.

Self Quiz
Ask yourself...
- What are the waist measurements in males and females that are considered for a diagnosis of obesity?
- How would you care for a patient undergoing this testing using the nursing process?
- Why is diabetes a risk factor for HF?
Medication Management
Treating HF with medications can reduce disease progression, and relieve symptoms of dyspnea, fatigue, and edema. Several classes of drugs can be used to treat HF. Each one may be used to treat a different symptom.
The classes are as follows:
Angiotensin-Converting Enzyme (ACE) Inhibitors
These medications open blood vessels decreasing blood pressure and lowering the heart’s work to keep HF from worsening. (6)
Some common ACE inhibitors are:
- Captopril
- Enalapril
- Lisinopril
- Ramipril
Angiotensin-Receptor Blockers (Arbs)
- Losartan
- Valsartan
Angiotensin-Receptor Neprilysin Inhibitors (Arnis)
Entresto is a drug combination in the class of Angiotensin-receptor neprilysin inhibitors (ARNIs). ARNIs limit the enzyme neprilysin from breaking down natural substances in the body. By limiting this enzyme, the arteries can open to increase blood flow. This drug also limits the retention of sodium. (7)
Beta Blockers
Beta-blockers work to slow down the heart rate and increase blood flow by widening blood vessels. This also lowers blood pressure. (9)
Common Beta Blockers are:
- Atenolol
- Bisoprolol
- Carvedilol
- Labetalol
- Metoprolol succinate
- Metoprolol tartrate
- Nadolol
- Propranolol
Sodium-Glucose Cotransporter-2 (SGLT2) Inhibitors
Jardiance and Farxiga are Sodium-glucose cotransporter-2 (SGLT2) inhibitors that were designed to treat diabetes, but they have been found to be cardio-protective. (7)
Diuretics
Diuretics allow the body to release extra fluid and sodium through the kidneys. They cause increased urination so should be taken earlier in the day.
Most common diuretics are:
- Lasix
- Bumex
- Torsemide
- Diuril
- Hydrochlorothiazide (HCTZ)
- Metolazone
Other medications can be prescribed depending on the patient's needs, such as anticoagulants to keep the blood thin, statins to lower cholesterol, and Digoxin to control heart rate and increase pumping strength. Calcium channel blockers allow the heart muscle to relax, thereby reducing blood pressure and circulation within the heart. Potassium may be used with certain diuretics that cause potassium to leave the body.
It is needed to keep the heart's rhythm in control. Oxygen may also increase its amount in the blood, assisting with dyspnea and activity tolerance. (7) It is the nurse's responsibility to evaluate these medications and interventions for plan updates.

Self Quiz
Ask yourself...
- Which medications are the first line in controlling HF?
- Where can you find side effects of these medications?
- What would your care plan look like for a patient with HF?
Other Interventions
Several types of surgery can be utilized for the most severe cases of HF. Bypass surgery has been used for many years. This procedure bypasses blocked coronary arteries, allowing for better blood flow to the heart muscle.
Replacing damaged or stenosed heart valves will assist blood flow within the heart chambers. In some patients, biventricular pacing with a pacemaker allows both sides of the heart to work in sync. (10) An ICD, or implantable defibrillator, can shock the heart from a life-threatening rhythm back to normal.
The ventricular assist device or VAD can assist the ventricles to pump blood out to the body. (10) This device can be used either waiting for a transplant or permanently.
Heart Transplants can be used as the last intervention, with a success rate of 88% after one year and 75% after five. If a patient has sleep apnea, it can be linked to heart failure. In this case, an evaluation and treatment will be performed. (10)

Self Quiz
Ask yourself...
- Where can you learn more about assistive devices for HF?
- How many arteries can be bypassed in surgery at one time?
- How would you care for a person with a surgical device?
Current areas of research in HF are producing more effective drug therapy, genetic testing, non-surgical devices, transplants, and mechanical support. (8)
The research is now studying drugs that improve physical symptoms when added to the standard drug treatment and care. These drugs have shown improvement in reducing hospitalizations.
The newer diabetic medications Jardiance, Invokana, and Farxiga are being studied on HF patients without diabetes to learn if they will improve function and risk reduction of MI, stroke, or cardiovascular death. (8)
Non-invasive imaging such as MRI, ultrasound, nuclear testing, and radiology are being researched in the hope that advancing these technologies will "provide additional information about coronary arteries and heart tissue, coronary strain, the function and structure of the heart." (8)
Genetic testing is under investigation to help determine if there is an inherited disease, especially in specific cardiomyopathies. These cardiomyopathies present differently and may be treated with differing modalities.
One of the newest areas of HF management and treatment is remote monitoring. Nurses are at the forefront of home monitoring in many areas as they are the clinicians making home visits.
New types of VADs are emerging as treatments for advanced illnesses. They are being manufactured to be more durable and portable. (8)

Self Quiz
Ask yourself...
- Where can you find new research studies on HF?
- Where can you go to get educated on new devices?
- Who is conducting the new research?
Conclusion
As discussed in this course, Heart Failure affects over 6 million people in the US. Age, lifestyle, race, and genetics may predispose a patient to this disease.
HF burdens society and health care costs due to missed work, rehospitalizations, and poor outcomes. As a nurse, learning the mechanisms of HF is imperative. Understanding etiology, statistics, pharmaceuticals, and other interventions will assist nurses in administering the best care.
New research shows how emerging medications, improved implantable devices, and surgery can improve outcomes. However, patient education and prevention are vital to caring for HF patients.
References + Disclaimer
- Mayo Clinic Staff. Heart Failure at Mayo Clinic as retrieved from: https://www.ahajournals.org/doi/10.116/CIRCRESAHA.121.318172
- Roger, Veronique L., Epidemiology of Heart Failure. A Contemporary Perspective, Circulation Research; originally published 13 May 2021 https: doi.org/10.16/CIRCRESAHA.121.318172. Circulation Research, 2021 128:1421-1434
- Centers for Disease Control and Prevention. CDC.gov. Article: Heart Failure. retrieved https://www.cdc.gov/heartdisease/heart_failure.htm
- Schwinger, Robert H.G. Pathophysiology of heart failure. 2021 Feb;11 (1):263-276 doi: 10.21037-20-302. Retrieved from: https//: www.ncbinim,nih.gov/pmc/articles/PMC7944197/
- American Red Cross. Heart-Health Screenings. Retrieved from: https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/heart-health-screenings.
- Mayo Clinic Staff. Heart Failure. Retrieved from: https://www.mayoclinic.org/diseases-conditions/heart-failure/diagnosis-treatment/treatment/txc-20373144
- American Heart Association article. Medications Used to Treat Heart Failure. Retrieved from: https://www.heart.org/en/health-topics/heart-failure/treatment-options-for-heart-failure/medications-used-to-treat-heart-failure
- Editorial Team. Emerging Heart Failure Research. Retrieved from: https://heart-failure.net/research
- Mayo Clinic Staff. Beta Blockers. Retrieved from: https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/beta-blockers/art-20044522
- Johns Hopkins Medicine. Congestive Heart Failure: Prevention, Treatment and Research. Retrieved from: https://www.hopkinsmedicine.org/health/wellnss-and-prevention/heart-health. https://www.hopkinsmedicine.org/health/heart-and-vascular. Ventricular Assist Device (VAD) | Conditions & Treatments | UCSF Health. https://www.hopkinsmedicine.org/health/wellness-and-prevention/heart-conditions’
- University of Southern California Health. Ventricular Assist Device
- Retrieved from: https://www.ucsfhealth.org/treatments/ventricular-assist-device,
- Figure 1. Mayo Clinic www.mayoclinic.org/diseases-conditions/heart-failure/symptoms-causes/syc-2037314
- Figure 2. Healthy-Ojas Healthy Cholesterol Range. healthy-ojas.com/cholesterol/healthy-cholesterol-level.html
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
