Course
Michigan Renewal Bundle – Part 3
Course Highlights
- In this Michigan Renewal Bundle – Part 3 course, we will learn about potential cases of hypertension and screen individuals at risk, fostering interventions and mitigating adverse outcomes through prompt diagnosis.
- You’ll also learn how to identify the pathophysiology of the upper and lower gastrointestinal tract and list examples of underlying conditions that cause gastrointestinal bleeding.
- You’ll leave this course with a broader understanding of the six stages of pressure injuries based on National Pressure Injury Advisory Panel guidelines.
About
Contact Hours Awarded: 7
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Hypertension Updates
Introduction
This course aims to provide nurses and healthcare professionals with an up-to-date understanding of hypertension (HTN). The course covers epidemiological evidence, etiology, diagnostic tools, medication management, other interventions, and future research on HTN.
Hypertension, or high blood pressure, is a chronic condition and a significant risk factor for heart disease, stroke, kidney failure, and other serious health problems. The American College of Cardiology defines hypertension as systolic blood pressure greater than 130 mmHg or diastolic blood pressure greater than 80 mmHg [1].
Statistical Evidence/Epidemiology
According to the Centers for Disease Control and Prevention (CDC), hypertension afflicts 108 million Americans and contributes to almost 500,000 deaths per year in the United States [2]. The prevalence of hypertension varies by race and ethnicity, with non-Hispanic Black adults having the highest majority (57.1%), followed by Hispanic adults (43.7%) and non-Hispanic White adults (43.6%).
Hypertension is also more common among older adults, with (74.5%) of adults aged 60 and over having high blood pressure [3]. Despite the high prevalence of hypertension, less than a quarter of all adults with hypertension in the United States have their blood pressure under control [2].
This leaves millions at risk for serious health problems from uncontrolled hypertension, such as heart disease, stroke, kidney failure, and eye problems. In 2021, high blood pressure was a primary or contributing cause of death for more than 691,095 Americans [4].
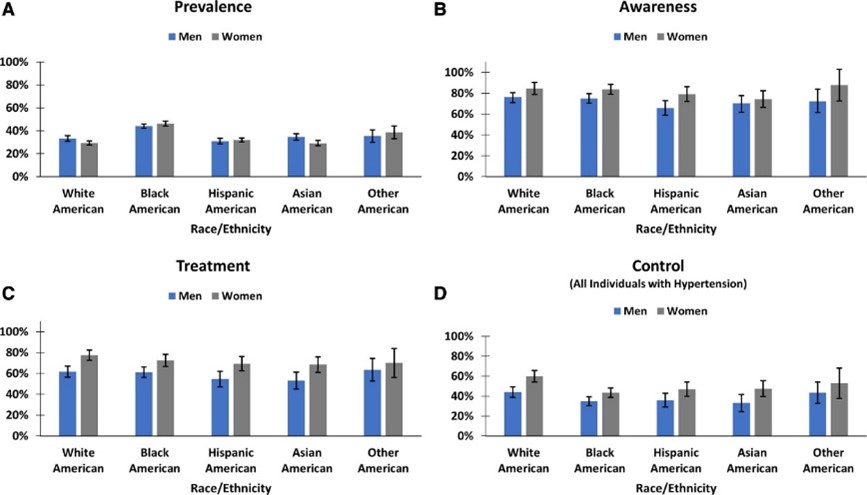
[31]

Self Quiz
Ask yourself...
- How do the current epidemiological statistics about hypertension affect healthcare planning and resource allocation?
- Given that hypertension is a significant public health problem and a major risk factor for serious health problems, what are the essential things that nurses and healthcare professionals should know about hypertension to manage their patients?
- Why do you think there exists such a pronounced disparity in the prevalence of hypertension among different racial and ethnic groups, and what societal and medical strategies might be employed to address this?
Etiology/Pathophysiology of Hypertension
Hypertension (high blood pressure) is a multifactorial disease characterized by persistent elevated blood pressure in the systemic arteries. Understanding hypertension's etiology, pathophysiology, and sequela is crucial for effective management and treatment.
There are two main types of hypertension: primary hypertension and secondary hypertension. Primary or essential hypertension (idiopathic hypertension), which accounts for about 80-95% of all cases, has no identifiable cause and results from complex interactions between genetic, environmental, and other unknown factors [5].
The cause of secondary hypertension (15-30% of cases) is often an underlying medical condition, such as kidney disease, adrenal gland tumors, diabetes, or thyroid disease [6]. Family history plays a role, although science has identified no genetic factor as the "hypertension gene" [7].
A key mechanism in hypertension is the imbalance between the forces that constrict and dilate blood vessels. This imbalance can be caused by several factors, including increased activity of the sympathetic nervous system, which leads to vasoconstriction, increased production of vasoconstrictor hormones, such as angiotensin II and aldosterone, a decreased output of vasodilator hormones, such as nitric oxide, and structural changes in the blood vessels, such as thickening of the vessel walls [8].
The most understood mechanism of hypertension involves increased peripheral vascular resistance due to constriction of small arterioles. The Renin-Angiotensin-Aldosterone System (RAAS) is a hormonal system that regulates blood pressure. Dysfunction of the RAAS can lead to fluid retention and vasoconstriction [9]. Endothelial dysfunction involves the inner lining of the blood vessels (endothelium) and the release of nitric oxide, which promotes blood vessel relaxation. The dysfunction of nitric oxide is a primary contributor to hypertension [10].
Secondary hypertension often involves:
- The kidneys and volume overload.
- Leading to elevated blood pressure.
- Often affecting younger patients and those with resistant or refractory hypertension.
The typical secondary causes of hypertension include:
- Primary aldosteronism (PA).
- Renovascular disease.
- Chronic kidney disease (CKD).
- Obstructive sleep apnea (OSA).
- Drug-induced or alcohol-induced hypertension [11].
Overactivation within the sympathetic nervous system can result in increased heart rate (tachycardia) and vasoconstriction, both of which can cause a temporary elevation in blood pressure. Within the metabolic process, insulin resistance has been associated with endothelial dysfunction and hypertension [12].

Self Quiz
Ask yourself...
- What underlying mechanisms or factors might contribute to the development of primary hypertension when classified as having no identifiable cause, and how might this classification influence our approach to treatment and management?
- What common myths and misconceptions about hypertension have you encountered in your practice?
- How do mechanisms like vascular resistance, RAAS dysfunction, and endothelial dysfunction interact or possibly counteract each other in the pathophysiology of hypertension, and what are the implications of this interplay for targeted therapeutic interventions?
- If hypertension is a complex disease with multiple causes, how can we develop effective treatments and prevention strategies?
Diagnostic and Screening Tools
The primary current diagnostic and screening tools around hypertension include blood pressure measurement. Blood pressure consists of systolic blood pressure (SBP) and diastolic blood pressure (DBP).
SBP is the pressure when the heart is beating, and DBP is the pressure when the heart is resting. A diagnosis of hypertension can be established when the Systolic Blood Pressure (SBP) is 130 mmHg or above or when the Diastolic Blood Pressure (DBP) is at least 80 mmHg [1].
The American Heart Association (AHA) recommends that all adults have their blood pressure checked at least once a year. People with risk factors for hypertension, such as obesity, diabetes, and kidney disease, should have their blood pressure checked more often [13].
Secondary tools for evaluating hypertension include ambulatory blood pressure monitoring (ABPM). ABPM is a more accurate way to measure blood pressure, measuring blood pressure over 24 hours. ABPM is an integral part of hypertensive care [14].
Urine tests can check for protein in the urine, a sign of kidney damage. Kidney damage is a risk factor for hypertension. Blood tests can be used to check for other medical conditions that can cause hypertension, such as diabetes and kidney disease, cholesterol levels, and other risk factors for heart disease.
Hormonal Tests can measure hormones produced by the adrenal and thyroid glands, which can help diagnose secondary hypertension. Regardless of the diagnostic or screening tools, early diagnosis and management of hypertension save lives [15].

Self Quiz
Ask yourself...
- What are the advantages and disadvantages of using blood pressure measurement as the primary diagnostic and screening tool for hypertension?
- What are some of the challenges of implementing ABPM as a routine screening tool for hypertension?
- How can we improve the early diagnosis and management of hypertension in all populations?
Imaging and Other Diagnostic Tests
Ultrasound of the Kidneys: To rule out kidney abnormalities.
Echocardiogram: To assess heart function and structure. Useful if hypertension has been longstanding.
Eye Exam: A fundoscopic examination can reveal changes in the retinal blood vessels, indicative of chronic hypertension.
Telemedicine: Remote monitoring can be helpful for ongoing assessment and titration of treatment.
Healthcare Apps: Smartphone apps can log and track blood pressure readings over time.

Self Quiz
Ask yourself...
- Considering the variety of diagnostic and screening tools available for hypertension—from traditional blood pressure measurements to digital devices like telemedicine and healthcare apps—how can healthcare providers ensure that they employ the most practical combination of methods for accurate diagnosis and long-term management of the condition?
- How does an early diagnosis contribute to better management and prognosis in hypertension patients?
Medication Management
The management of hypertension has evolved over the years, with numerous classes of medications available for treatment. The type of medication best suited for your patients will depend on their needs and health history.
Treatment strategies often begin with monotherapy, a single drug, usually a diuretic, beta-blocker, ACE inhibitor, or Angiotensin II receptor blocker (ARBs) [16]. Combination therapy for patients with stage 2 hypertension or those not reaching the target BP with monotherapy, which may include two or more drug classes, is also used.[16].
Step therapy involves starting with one drug and adding others to achieve the desired effect. A tailored approach is considered if comorbid conditions are present, such as diabetes or heart failure, which may influence drug choice.
Several standard classes of antihypertensive medications are used to treat hypertension, including first-line thiazides such as hydrochlorothiazide, which help rid excess salt and water and lower blood pressure [17]. Angiotensin-converting enzyme (ACE) inhibitors such as lisinopril and ramipril block the production of angiotensin II, a hormone that narrows blood vessels.
Angiotensin II Receptor Blockers (ARBs) such as losartan and valsartan which inhibit the action of angiotensin II, leading to vasodilation [17]. Beta-blockers such as atenolol or metoprolol slow the heart rate and reduce the force of the heart's contractions, which can lower blood pressure [17].
Calcium channel blockers such as amlodipine and diltiazem relax the muscles of the blood vessels by inhibiting the movement of calcium into vascular smooth muscle cells, thus lowering blood pressure [17]. Alpha-blockers such as doxazosin work by blocking alpha-adrenergic receptors, leading to vasodilation. Vasodilators such as hydralazine and minoxidil relax the muscles in blood vessel walls [17].
Central action agents such as clonidine, methyldopa, and moxonidine work on the central nervous system to lower blood pressure [17]. Moxonidine is a new-generation antihypertensive drug that works by activating imidazoline-I1 receptors in the brain, and it may be used when other antihypertensive drugs, such as thiazides, beta-blockers, ACE inhibitors, and calcium channel blockers, are not appropriate or have failed [18].
Thiazide-like diuretics such as chlorthalidone and indapamide have found increased use for their more prolonged duration of action and better cardiovascular outcomes when compared to traditional thiazides [19]. New evidence-based medications are coming into play, such as angiotensin receptor-neprilysin inhibitors (ARNIs), and a clinical trial is underway to test the effectiveness of a new drug called finerenone in preventing heart failure and kidney disease in people with hypertension and diabetes [20] [21].
Due to their safety profiles, there are special considerations with hypertensive management, including methyldopa and labetalol for pregnancy [22].
For older people, care is taken to avoid overtreatment, considering the risks of low blood pressure. For patients with chronic kidney disease (CKD), ACE inhibitors and ARBs are often favored due to their renal protective effects.
Generics are preferred when appropriate to reduce patient costs [23]. Digital adherence tools, including smartphone apps and telemedicine platforms, monitor patient compliance and adjust treatment as necessary.
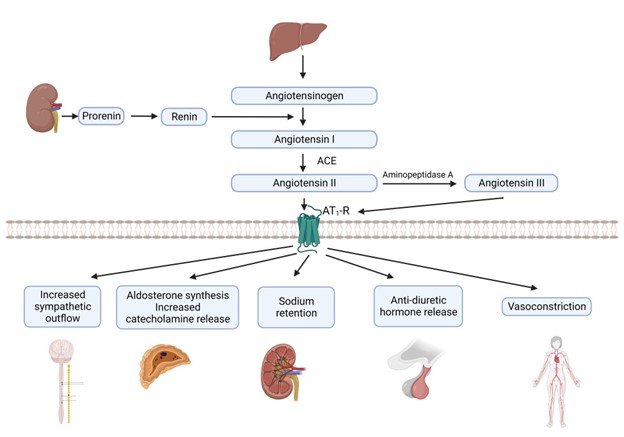
[32]

Self Quiz
Ask yourself...
- What challenges do healthcare providers face in medication compliance among hypertensive patients?
- Given the myriad antihypertensive drug classes and treatment strategies available, coupled with considerations for special populations such as pregnant women, older adults, and those with chronic kidney disease, how can healthcare providers effectively customize treatment plans while maintaining a consistent standard of care across different patient profiles?
Other Interventions
Beyond medication, lifestyle changes, including dietary interventions like the DASH diet and exercise, have proven effective in managing hypertension [24]. The DASH diet focuses on a high intake of fruits, vegetables, and low-fat dairy foods and is low in saturated and total fat.
A reduction in dietary sodium has been shown to lower blood pressure, with a general recommendation to consume less than 2,300 mg per day, with an ideal limit of 1,500 mg for most adults [24]. Regular aerobic exercise such as walking, jogging, or swimming can lower blood pressure.
Weight loss of even 5-10% can significantly impact reducing blood pressure [25]. Alcohol moderation and smoking cessation can also lead to blood pressure reduction.
Behavioral therapies, including stress management techniques such as deep breathing, meditation, and relaxation exercises, can help reduce short-term spikes in blood pressure. There is some evidence that suggests that Cognitive CBT can be effective in managing hypertension [26].
Biofeedback can help manage stress triggers and measure physiological functions like heart rate and blood pressure [26]. Although evidence is mixed, some studies suggest acupuncture can help lower blood pressure.
Renal denervation is an invasive procedure using radiofrequency energy to destroy kidney nerves contributing to hypertension. Central sleep apnea therapy can treat central sleep apnea and lower blood pressure.
Weight loss surgery can be an effective way to lower blood pressure in people who are obese or overweight. Several stress management techniques, such as yoga, meditation, and deep breathing, can be helpful.
Self-monitoring and regular medical check-ups can ensure that the treatment plan is effective and can be adjusted as needed. Remote consultations can offer more frequent touchpoints for adjustments in treatment plans.
Various mobile applications can help patients track blood pressure readings, medication schedules, and lifestyle changes. Community-based interventions to educate the public about hypertension risks, prevention, and management can be effective.
On a policy level, changes and initiatives that reduce sodium in processed foods can have a broader societal impact [27].

Self Quiz
Ask yourself...
- How do non-pharmacological interventions compare with medication management in terms of effectiveness and patient compliance?
- What roles do genetics and lifestyle factors play in the development of hypertension?
- How might the interactions among genetic factors, diet, obesity, lifestyle choices, and psychological elements contribute to the complex etiology of primary hypertension, and what does this complexity imply for diagnosing and treating secondary hypertension?
Upcoming Research
Using "Omics" genomic, proteomic, and metabolomic data to tailor antihypertensive therapies to individuals' researchers are working to identify the genes that contribute to hypertension and specific genetic markers that can help predict an individual's risk for developing hypertension and their potential response to treatments [28].
This information could be used to create new genetic tests to identify people who are at risk of developing the condition. Personalized medicine seeks to create customized approaches to managing hypertension, which would involve tailoring treatment to the individual's needs and risk factors.
Non-invasive treatments, such as devices worn on the body to deliver medication or stimulate the nerves, may also be effective. Researchers are developing a new type of blood pressure monitor that can be worn on the wrist and measure blood pressure throughout the day.
A study is underway to investigate the use of artificial intelligence to develop personalized treatment plans for people with hypertension. With predictive analytics, AI models are trained to predict hypertension risk and disease progression using large-scale electronic health records [29].
In the area of new therapeutic targets, researchers are looking into novel ways to improve endothelial function and vascular health. Studies into how the gut microbiome may influence blood pressure regulation offer potential for new treatment modalities [30]. Research on how diet interacts with genes within the gut microbiome may affect blood pressure.

Self Quiz
Ask yourself...
- How might advancements in technology and research change the landscape of hypertension management in the next decade?
- How can we balance the potential benefits of personalized medicine for hypertension with the challenges of ensuring that everyone has access to these new treatments?
Awareness and Patient Education
What your patients should know:
- Early diagnosis and treatment of hypertension are essential for preventing complications.
- There are several different types of medications available to treat hypertension.
- Lifestyle changes, such as eating a healthy diet, exercising regularly, and maintaining a healthy weight, can also help to lower blood pressure.
Nurses and healthcare professionals should be aware of the following:
- Nurses and healthcare professionals play a vital role in educating patients about hypertension and helping them manage their condition.
- The latest epidemiological statistics on hypertension, including its prevalence, risk factors, and impact on public health.
- The etiology and pathophysiology of hypertension, including the different types of hypertension and their underlying causes.
- The diagnostic tools used to diagnose hypertension include blood pressure measurement, ambulatory blood pressure monitoring, urine tests, blood tests, and imaging tests.
- The different types of medications available to treat hypertension, as well as their side effects and interactions.
Nurses and healthcare professionals can help patients to manage their hypertension by:
- Educating patients about hypertension and its risks.
- Helping patients develop a treatment plan that includes lifestyle changes and medications.
- Monitoring their blood pressure and adjusting their treatment plan as needed.
- Providing support and encouragement.
By working together, nurses and healthcare professionals can help patients manage their hypertension and reduce their risk of complications.

Self Quiz
Ask yourself...
- What are your key takeaways from this course, and how do you plan to implement these learnings in your clinical practice?
Conclusion
Hypertension is a significant public health problem in the United States and worldwide [1]. It is a chronic condition that can lead to serious health problems like heart disease, stroke, kidney failure, and eye problems. However, despite its complexity, hypertension is manageable with lifestyle changes, medications, and the potential information from future genomic discoveries [25] [17].
References + Disclaimer
- New ACC/AHA High Blood Pressure Guidelines Lower Definition of Hypertension – American College of Cardiology. (2017, November 8). American College of Cardiology. https://www.acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017
- 2. Facts about hypertension | CDgov. (2023, July 6). Centers for Disease Control and Prevention. https://www.cdc.gov/bloodpressure/facts.htm
- 3. Ostchega, Y., Fryar, C. D., Nwankwo, T., & Nguyen, D. T. (2020). Hypertension Prevalence Among Adults Aged 18 and Over: United States, 2017-2018. NCHS data brief, (364), 1–8.
- 4. Multiple cause of death data on CDC WONDER. (2023, September 8). Retrieved September 18, 2023, from https://wonder.cdc.gov/mcd.html.
- Carretero, O. A., & Oparil, S. (2000). Essential Hypertension. Circulation, 101(3), 329–335. https://doi.org/10.1161/01.cir.101.3.329
- 6. Koch, C. (2020, February 4). Overview of Endocrine Hypertension. Endotext – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK278980/
- 7. Manosroi, W., & Williams, G. H. (2018). Genetics of Human Primary Hypertension: Focus on Hormonal Mechanisms. Endocrine Reviews, 40(3), 825–856. https://doi.org/10.1210/er.2018-00071
- Ayada, C. (2015, June 1). The relationship of stress and blood pressure effectors. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4938117/
- Terry, K. W., Kam, K. K., Yan, B. P., & Lam, Y. (2010). Renin-angiotensin-aldosterone system blockade for cardiovascular diseases: current status. British Journal of Pharmacology, 160(6), 1273–1292. https://doi.org/10.1111/j.1476-5381.2010.00750.x
- Bryan, N. S. (2022). Nitric oxide deficiency is a primary driver of hypertension. Biochemical Pharmacology, 206, 115325. https://doi.org/10.1016/j.bcp.2022.115325
- Sarathy, H., Salman, L. A., Lee, C., & Cohen, J. B. (2022). Evaluation and Management of Secondary Hypertension. Medical Clinics of North America, 106(2), 269–283. https://doi.org/10.1016/j.mcna.2021.11.004
- Muniyappa, R., Iantorno, M., & Quon, M. J. (2008). An Integrated View of Insulin Resistance and Endothelial Dysfunction. Endocrinology and Metabolism Clinics of North America, 37(3), 685–711. https://doi.org/10.1016/j.ecl.2008.06.001
- Heart-Health Screenings. (2022, August 23). www.heart.org. https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/heart-health-screenings
- Pena-Hernandez, C., Nugent, K., & Tuncel, M. (2019). Twenty-Four-Hour Ambulatory Blood Pressure Monitoring. Journal of Primary Care & Community Health, 11, 215013272094051. https://doi.org/10.1177/2150132720940519
- Gulec, S. (2013). Early diagnosis saves lives: focus on patients with hypertension. Kidney International Supplements, 3(4), 332–334. https://doi.org/10.1038/kisup.2013.69
- UpToDate. (2023, June 22). UpToDate. Retrieved September 18, 2023, from https://www.uptodate.com/contents/choice-of-drug-therapy-in-primary-essential-hypertension/print
- Types of Blood Pressure Medications. (2023, June 6). www.heart.org. https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications
- Moxonidine: a new antiadrenergic antihypertensive agent. (1999, August 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/10489098/
- Liang, W., Ma, H., Cao, L., Yan, W., & Yang, J. (2017). Comparison of thiazide-like diuretics versus thiazide-type diuretics: a meta-analysis. Journal of Cellular and Molecular Medicine, 21(11), 2634–2642. https://doi.org/10.1111/jcmm.13205
- Greenberg, B. (2019). Angiotensin Receptor-Neprilysin Inhibition (ARNI) in Heart Failure. International Journal of Heart Failure, 2(2), 73. https://doi.org/10.36628/ijhf.2020.0002
- Filippatos, G., Anker, S. D., Agarwal, R., Ruilope, L., Rossing, P., Bakris, G. L., Tasto, C., Joseph, A., Kolkhof, P., Lage, A., & Pitt, B. (2022). Finerenone Reduces Risk of Incident Heart Failure in Patients With Chronic Kidney Disease and Type 2 Diabetes: Analyses From the FIGARO-DKD Trial. Circulation, 145(6), 437–447. https://doi.org/10.1161/circulationaha.121.057983
- Brown, C., & Garovic, V. D. (2014). Drug Treatment of Hypertension in Pregnancy. Drugs, 74(3), 283–296. https://doi.org/10.1007/s40265-014-0187-7
- Zhang, Y., He, D., Zhang, W., Xing, Y., Guo, Y., Wang, F., Jia, J., Yan, T., Liu, Y., & Lin, S. (2020). ACE Inhibitor Benefit to Kidney and Cardiovascular Outcomes for Patients with Non-Dialysis Chronic Kidney Disease Stages 3–5: A Network Meta-Analysis of Randomised Clinical Trials. Drugs, 80(8), 797–811. https://doi.org/10.1007/s40265-020-01290-3
- McGuire, H. L., Svetkey, L. P., Harsha, D. W., Elmer, P. J., Appel, L. J., & Ard, J. D. (2004). Comprehensive Lifestyle Modification and Blood Pressure Control: A Review of the PREMIER Trial. Journal of Clinical Hypertension, 6(7), 383–390. https://doi.org/10.1111/j.1524-6175.2004.03147.x
- Vasheghani-Farahani, A., Mansournia, M. A., Asheri, H., Fotouhi, A., Yunesian, M., Jamali, M., & Ziaee, V. (2010). The Effects of a 10-Week Water Aerobic Exercise on the Resting Blood Pressure in Patients with Essential Hypertension. Asian Journal of Sports Medicine, 1(3). https://doi.org/10.5812/asjsm.34854
- Li, Y., Buys, N., Li, Z., Li, L., Song, Q., & Sun, J. (2021). The efficacy of cognitive behavioral therapy-based interventions on patients with hypertension: A systematic review and meta-analysis. Preventive Medicine Reports, 23, 101477. https://doi.org/10.1016/j.pmedr.2021.101477
- Jachimowicz, K., & Winiarska-Mieczan, A. (2023). Initiatives to Reduce the Content of Sodium in Food Products and Meals and Improve the Population’s Health. Nutrients, 15(10), 2393. https://doi.org/10.3390/nu15102393
- Currie, G., & Delles, C. (2017). The Future of “Omics” in Hypertension. Canadian Journal of Cardiology, 33(5), 601–610. https://doi.org/10.1016/j.cjca.2016.11.023
- Chaikijurajai, T., Laffin, L. J., & Tang, W. W. (2020). Artificial Intelligence and Hypertension: Recent Advances and Future Outlook. American Journal of Hypertension, 33(11), 967–974. https://doi.org/10.1093/ajh/hpaa102
- Palmu, J., Lahti, L., & Niiranen, T. J. (2021). Targeting Gut Microbiota to Treat Hypertension: A Systematic Review. International Journal of Environmental Research and Public Health, 18(3), 1248. https://doi.org/10.3390/ijerph18031248
- Aggarwal, R. (2021, December 1). Racial/Ethnic Disparities in Hypertension Prevalence, Awareness, Treatment, and Control in the United States, 2013 to 2018. Hypertension. https://www.ahajournals.org/doi/full/10.1161/HYPERTENSIONAHA.121.17570
- Fountain, J. H. (2023, March 12). Physiology, Renin Angiotensin System. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470410/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
GI Bleed: An Introduction
Introduction
Gastrointestinal bleeding (GI Bleed) is an acute and potentially life-threatening condition. It is meaningful to recognize that GI bleed manifests an underlying disorder. Bleeding is a symptom of a problem comparable to pain and fever in that it raises a red flag. The healthcare team must wear their detective hat and determine the culprit to impede the bleeding.
Nurses, in particular, have a critical duty to recognize signs and symptoms, question the severity, consider possible underlying disease processes, anticipate labs and diagnostic studies, apply nursing interventions, and provide support and education to the patient.
Epidemiology
The incidence of Gastrointestinal Bleeding (GIB) is broad and comprises cases of Upper gastrointestinal bleeding (UGIB) and lower gastrointestinal bleeding (LGIB). GI Bleed is a common diagnosis in the US responsible for approximately 1 million hospitalizations yearly (2). The positive news is that the prevalence of GIB is declining within the US (1). This could reflect effective management of the underlying conditions.
Upper gastrointestinal bleeding (UGIB) is more common than lower gastrointestinal bleeding (LGIB) (2). Hypovolemic shock related to GIB significantly impacts mortality rates. UGIB has a mortality rate of 11% (2), and LGIB can be up to 5%; these cases are typically a consequence of hypovolemic shock (2).
Certain risk factors and predispositions impact the prevalence. Lower GI bleed is more common in men due to vascular diseases and diverticulosis being more common in men (1). Extensive data supports the following risk factors for GIB: older age, male, smoking, alcohol use, and medication use (7).
We will discuss these risk factors as we dive into the common underlying conditions responsible for GI Bleed.

Self Quiz
Ask yourself...
- Have you ever cared for a patient with GIB?
- Can you think of reasons GIB is declining in the US?
- Do you have experience with patients with hypovolemic shock?
Etiology/ Pathophysiology
Gastrointestinal (GI) bleeding includes any bleeding within the gastrointestinal tract, from the mouth to the rectum. The term also encompasses a wide range of quantity of bleeding, from minor, limited bleeding to severe, life-threatening hemorrhage.
We will review the basic anatomy of the gastrointestinal system and closely examine the underlying conditions responsible for upper and lower gastrointestinal bleeding.
Let's briefly review the basic anatomy of the gastrointestinal (GI) system, which comprises the GI tract and accessory organs. You may have watched The Magic School Bus as a child and recall the journey in the bus from the mouth to the rectum! Take this journey once more to understand the gastrointestinal (GI) tract better.
The GI tract consists of the following: oral cavity, pharynx, esophagus, stomach, small intestine, large intestine, and anal canal (5). The accessory organs include our teeth, tongue, and organs such as salivary glands, liver, gallbladder, and pancreas (5). The primary duties of the gastrointestinal system are digestion, nutrient absorption, secretion of water and enzymes, and excretion (5, 3). Consider these essential functions and their impact on each other.
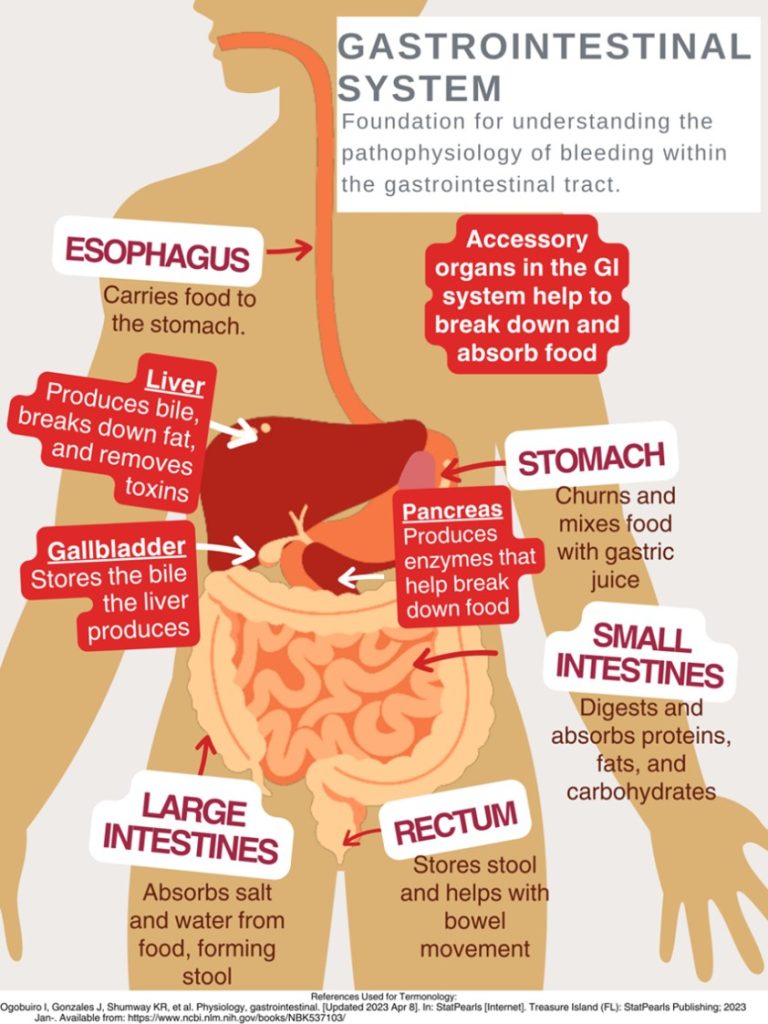
This design was created on Canva.com on August 31, 2023. It is copyrighted by Abbie Schmitt, RN, MSN and may not be reproduced without permission from Nursing CE Central.
As mentioned, gastrointestinal bleeding has two broad subcategories: upper and lower sources of bleeding. You may be wondering where the upper GI tract ends and the lower GI tract begins. The answer is the ligament of Treitz. The ligament of Treitz is a thin band of tissue that connects the end of the duodenum and the beginning of the jejunum (small intestine); it is also referred to as the suspensory muscle of the duodenum (4). This membrane separates the upper and lower GI tract. Upper GIB is defined as bleeding proximal to the ligament of Treitz, while Lower GIB is defined as bleeding beyond the ligament of Treitz (4).
Upper GI Bleeding (UGIB) Etiology
Underlying conditions that may be responsible for the UGIB include:
- Peptic ulcer disease
- Esophagitis
- Foreign body ingestion
- Post-surgical bleeding
- Upper GI tumors
- Gastritis and Duodenitis
- Varices
- Portal hypertensive gastropathy (PHG)
- Angiodysplasia
- Dieulafoy lesion
- Gastric antral valvular ectasia
- Mallory-Weiss tears
- Cameron lesions (bleeding ulcers occurring at the site of a hiatal hernia
- Aortoenteric fistulas
- Hemobilia (bleeding from the biliary tract)
- Hemosuccus pancreaticus (bleeding from the pancreatic duct)
(1, 4, 5, 8. 9)
Pathophysiology of Variceal Bleeding. Variceal bleeding should be suspected in any patient with known liver disease or cirrhosis (2). Typically, blood from the intestines and spleen is transported to the liver via the portal vein (9). The blood flow may be impaired in severe liver scarring (cirrhosis). Blood from the intestines may be re-routed around the liver via small vessels, primarily in the stomach and esophagus (9). Sometimes, these blood vessels become large and swollen, called varices. Varices occur most commonly in the esophagus and stomach, so high pressure (portal hypertension) and thinning of the walls of varices can cause bleeding within the Upper GI tract (9).
Liver Disease + Varices + Portal Hypertension = Recipe for UGIB Disaster
Lower GI Bleeding (LGIB) Etiology
- Diverticulosis
- Post-surgical bleeding
- Angiodysplasia
- Infectious colitis
- Ischemic colitis
- Inflammatory bowel disease
- Colon cancer
- Hemorrhoids
- Anal fissures
- Rectal varices
- Dieulafoy lesion
- Radiation-induced damage
(1, 4, 5, 9)
Unfortunately, a source is identified in only approximately 60% of cases of GIB (8). Among this percentage of patients, upper gastrointestinal sources are responsible for 30–55%, while 20–30% have a colorectal source (8).

Self Quiz
Ask yourself...
- How is the GI Tract subdivided?
- Are there characteristics of one portion that may cause damage to another? (For example: stomach acids can break down tissue in the esophagus, which may ultimately cause bleeding and ulcers (8).
- Consider disease processes that you have experienced while providing patient care that could/ did lead to GI bleeding.
Laboratory and Diagnostic Testing
Esophagogastroduodenoscopy (EGD) and colonoscopy identify the source of bleeding in 80–90% of patients (4). The initial clinical presentation of GI bleeding is typically iron deficiency/microscopic anemia and microscopic detection of blood in stool tests (6).
The following laboratory tests are advised to assist in finding the cause of GI bleeding (2):
- Complete blood count
- Hemoglobin/hematocrit
- International normalized ratio (INR), prothrombin time (PT), and activated partial thromboplastin time (PTT)
- Liver function tests
Low hemoglobin and hematocrit levels result from blood loss, and blood urea nitrogen (BUN) may be elevated due to the GI system's breakdown of proteins within the blood (9).
The following laboratory tests are advised to assist in finding the cause of GI bleeding:
- EGD (esophagogastroduodenoscopy)- Upper GI endoscopy
- Clinicians can visualize the upper GI tract using a camera probe that enters the oral cavity and travels to the duodenum (9)
- Colonoscopy- Lower GI endoscopy/ (9)
- Clinicians can visualize the lower GI tract.
- CT angiography
- Used to identify an actively bleeding vessel
Signs and Symptoms
Clinical signs and symptoms depend on the volume/ rate of blood loss and the location/ source of the bleeding. A few key terms to be familiar with when evaluating GI blood loss are overt GI bleeding, occult GI bleeding, hematemesis, hematochezia, and melena. Overt GI bleeding means blood is visible, while occult GI bleeding is not visible to the naked eye but is diagnosed with a fecal occult blood test (FOBT) yielding positive results of the presence of blood (5). Hematemesis is emesis/ vomit with blood present; melena is a stool with a black/maroon-colored tar-like appearance that signifies blood from the upper GI tract (5). Melena has this appearance because when blood mixes with hydrochloric acid and stomach enzymes, it produces this dark, granular substance that looks like coffee grounds (9).
Mild vs. Severe Bleeding
A patient with mild blood loss may present with weakness and diaphoresis (9). Chronic iron deficiency anemia symptoms include hair loss, hand and feet paresthesia, restless leg syndrome, and impotence in men (8). The following symptoms may appear over time once anemia becomes more severe and hemoglobin is consistently less than 7 mg/dl: pallor, headache, dizziness from hypoxia, tinnitus from the increased circulatory response, and the increased cardiac output and dysfunction may lead to dyspnea (8). Findings of a positive occult GI bleed may be the initial red flag.
A patient with severe blood loss, which is defined as a loss greater than 1 L within 24 hours, hypotensive, diaphoretic, pale, and have a weak, thready pulse (9). Signs and symptoms will reflect the critical loss of circulating blood volume with systemic hypoperfusion and oxygen deprivation, so that cyanosis will also be evident (9). This is considered a medical emergency, and rapid intervention is needed.
Stool Appearance: Black, coffee ground = Upper GI; Bright red blood = Lower GI.

Self Quiz
Ask yourself...
- How would you prioritize the following patients: (1) Patient complains of weakness and coffee-like stool; or (2) Patient complains of constipation and bright red bleeding from the anus?
- Have you ever witnessed a patient in hypovolemic shock? If yes, what symptoms were most pronounced? If not, consider the signs.
- What are ways that the nurse can describe abnormal stool?
History and Physical Assessment
History
A thorough and accurate history and physical assessment is a key part of identifying and managing GI bleed. Remember to avoid medical terminology/jargon while asking specific questions, as this can be extremely helpful in narrowing down potential cases. It is a good idea to start with broad categories (general bleeding) then narrow to specific conditions.
Assess for the following:
- Previous episodes of GI Bleed
- Medical history with contributing factors for potential bleeding sources (e.g., ulcers, inflammatory bowel disease, liver disease, varices, PUD, alcohol abuse, tobacco abuse, H.pylori, diverticulitis) (3)
- Contributory medications (non-steroidal anti-inflammatory drugs (NSAIDs, anticoagulants, antiplatelet agents, bismuth, iron) (3)
- Comorbid diseases that could affect management of GI Bleed (8)
Physical Assessment
- Head to toe and focused Gastrointestinal, Hepatobiliary, Cardiac and Pancreatic
- Assessments
Assess stool for presence of blood (visible) and anticipate orders/ collect specimen for occult blood testing. - Vital Signs
Signs of hemodynamic instability associated with loss of blood volume (3):
- Resting tachycardia
- Orthostatic hypotension
- Supine hypotension
- Abdominal pain (may indicate perforation or ischemia)
- A rectal exam is important for the evaluation of hemorrhoids, anal fissures, or anorectal mass (3)
Certain conditions place patients at higher risk for GI bleed. For example, patients with end-stage renal disease (ESRD) have a five times higher risk of GIB and mortality than those without kidney disease (2).

Self Quiz
Ask yourself...
- Are there specific questions to ask if GIB is suspected?
- What are phrases from the patient that would raise a red flag for GIB (For example: “I had a stomach bleed years ago”)
- Have you ever noted overuse of certain medications in patients?

Self Quiz
Ask yourself...
- Have you ever shadowed or worked in an endoscopy unit?
- Name some ways to explain the procedures to the patient?
Treatment and Interventions
Treatment and interventions for GIB bleed will depend on the severity of the bleeding. Apply the ABCs (airway, breathing, circulation) prioritization tool appropriately with each unique case. Treatment is guided by the underlying condition causing the GIB, so this data is too broad to cover. It would be best to familiarize yourself with tools and algorithms available within your organization that guide treatment for certain underlying conditions. Image 2 is an example of an algorithm used to treat UGIB (8). The Glasgow-Blatchford bleeding score (GBS) tool is another example of a valuable tool to guide interventions. Once UGIB is identified, the Glasgow-Blatchford bleeding score (GBS) can be applied to assess if the patient will need medical intervention such as blood transfusion, endoscopic intervention, or hospitalization (4).
Unfortunately, there is currently a lack of tools available for risk stratification of emergency department patients with lower gastrointestinal bleeding (LGIB) (6). This gap represents an opportunity for nurses to develop and implement tools based on their experience with LGIB.
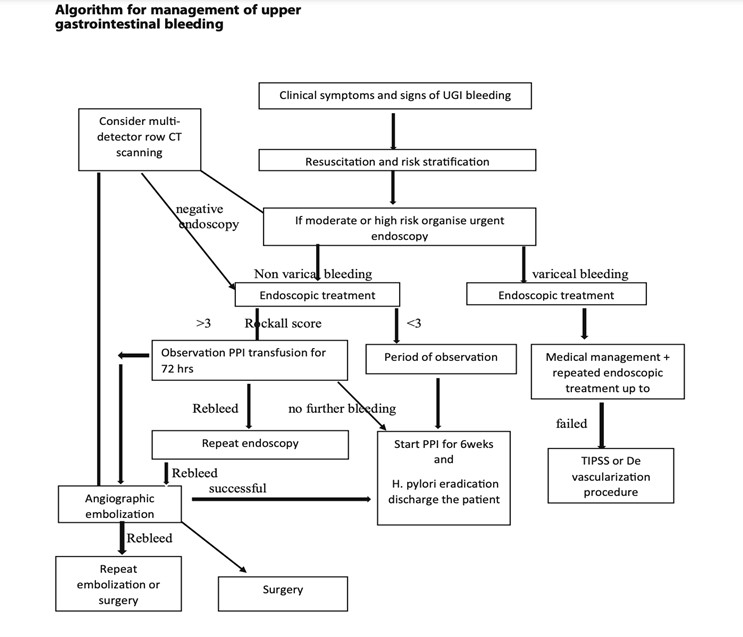
(8)

Self Quiz
Ask yourself...
- Are you familiar with GIB assessment tools?
- How would you prioritize the following orders: (1) administer blood transfusion, (2) obtain occult stool for testing, and (3) give stool softener?
The first step of nursing care is the assessment. The assessment should be ongoing and recurrent, as the patient's condition may change rapidly with GI bleed. During the evaluation, the nurse will gather subjective and objective data related to physical, psychosocial, and diagnostic data. Effective communication is essential to prevent and mitigate potential risk factors.
Subjective Data (Client verbalizes)
- Abdominal pain
- Nausea
- Loss of appetite
- Dizziness
- Weakness
Objective Data (Clinician notes during assessment)
- Hematemesis (vomiting blood)
- Melena (black, tarry stools)
- Hypotension
- Tachycardia
- Pallor
- Cool, clammy skin

Nursing Interventions
Ineffective Tissue Perfusion:
- Monitor vital signs frequently to assess blood pressure, heart rate, and oxygen saturation changes.
- Obtain IV access.
- Administer oxygen as ordered.
- Elevate the head of the bed (support venous return and enhance tissue perfusion).
- Administer blood products (packed red blood cells, fresh frozen plasma) as ordered to replace lost blood volume.
Acute Pain:
- Assess the patient's pain (quantifiable pain scale)
- Administer pain medications as ordered.
- Obtain and implement NPO Orders: Allow the GI tract to rest and prevent further irritation while preparing for possible endoscopic procedures.
- Apply heat/cold therapy for comfort.
Risk for Decreased Cardiac Output
- Assess the patient's heart rate and rhythm. (Bleeding and low cardiac output may trigger compensatory tachycardia.) (9)
- Assess and monitor the patient's complete blood count.
- Assess the patient's BUN level.
- Monitor the patient's urine output.
- Perform hemodynamic monitoring.
- Administer supplemental oxygenation as needed.
- Administer intravenous fluids as ordered.
- Prepare and initiate blood transfusions as ordered.
- Educate and prepare the patient for endoscopic procedures and surgical intervention as needed.
Risk for Deficient Fluid Volume:
- Monitor intake and output.
- Maintain hydration.
- Administer intravenous fluids as ordered.
- Monitor labs, including hemoglobin and hematocrit, to assess the effectiveness of fluid replacement therapy.
- Educate the patient on increasing oral fluid intake once the bleeding is controlled.
- Vital signs
- Assess the patient's level of consciousness and capillary refill time to evaluate tissue perfusion and response to fluid replacement.
- Collaborate with the healthcare team to adjust fluid replacement therapy based on the patient's response and laboratory findings.
Nursing Goals / Outcomes for GI Bleed:
- The patient's vital signs and lab values will stabilize within normal limits.
- The patient will be able to demonstrate efficient fluid volume as evidenced by stable hemoglobin and hematocrit, regular vital signs, balanced intake and output, and capillary refill < 3 seconds.
- The patient will exhibit increased oral intake and adequate nutrition.
- The patient will verbalize relief or control of pain.
- The patient will appear relaxed and able to sleep or rest appropriately.
- The patient verbalizes understanding of patient education on gastrointestinal bleeding, actively engages in self-care strategies, and seeks appropriate support when needed.

Self Quiz
Ask yourself...
- How can the nurse advocate for a patient with GIB?
- Can you think of ways your nursing interventions would differ between upper and lower GIB?
- Have you ever administered blood products?
- What are possible referrals following discharge that would be needed? (Example: gastroenterology, home health care)
Case Study
Mr. Blackstool presents to the emergency department with the following:
CHIEF COMPLAINT: "My stool looked like a ball of black tar this morning."
He also reports feeling "extra tired" and "lightheaded" for 3-5 days.
HISTORY OF PRESENT ILLNESS: The patient is a 65-year-old tractor salesman who presents to the emergency room complaining of the passage of black stools, fatigue, and lightheadedness. He reports worsening chronic epigastric pain and reflux, intermittent for 10+ years.
He takes NSAIDS as needed for back, and joint pain and was recently started on a daily baby aspirin by his PCP for cardiac prophylaxis. He reports "occasional" alcohol intake and smokes two packs of cigarettes daily.
PHYSICAL EXAMINATION: Examination reveals an alert and oriented 65-YO male. He appears anxious and irritated. Vital sips are as follows. Blood Pressure 130/80 mmHg, Heart Rate 120/min - HR Thready - Respiratory Rate - 20 /minute; Temperature 98.0 ENT/SKIN: Facial pallor and cool, moist skin are noted. No telangiectasia of the lips or oral cavity is noted. The parotid glands appear full.
CHEST: Lungs are clear to auscultation and percussion. The cardiac exam reveals a regular rhythm with an S4. No murmur is appreciated. Peripheral pulses are present but are rapid and weak.
ABDOMEN/RECTUM: The waist shows a rounded belly. Bowel sounds are hyperactive. Percussion of the liver is 13 cm (mal); the edge feels firm. Rectal examination revealed a black, tarry stool. No Dupuytren's contractions were noted.
LABORATORY TESTS: Hemoglobin 9gm/dL, Hematocrit 27%, WBC 13,000/mm. PT/PTT - normal. BUN 46mg/dL.
Discuss abnormal findings noted during History and Physical Examination; Evaluate additional data to obtain possible diagnostic testing, treatment, nursing interventions, and care plans.
Conclusion
After this course, I hope you feel more knowledgeable and empowered in caring for patients with Gastrointestinal bleeding (GIB). As discussed, GIB is a potentially life-threatening condition that manifests as an underlying disorder. Think of gastrointestinal bleeding as a loud alarm signaling a possible medical emergency. Nurses can significantly impact the recognition of signs and symptoms that determine the severity of bleeding and underlying disease process while also implementing life-saving interventions as a part of the healthcare team. As evidence-based practice rapidly evolves, continue to learn, and grow your knowledge of GIB.
Constipation Management and Treatment
Introduction
Constipation is more than just an uncomfortable topic—it’s a challenge that nurses encounter very frequently across diverse patient populations. From post-operative recovery to chronic conditions, managing constipation effectively can significantly impact a patient’s comfort, recovery, disease management, and overall quality of life. There is a deeper need for empathy, education, and evidence-based care. This course invites you to dive into the science of managing constipation with knowledge and compassion.
Understanding Constipation
Constipation is a condition characterized by infrequent, difficult, or incomplete bowel movements, often accompanied by hard or dry stools (3). It is one of the most common problems individuals face and occasionally results in emergent issues.
Constipation can be classified as a primary disorder or secondary to many potential causes.
Primary Constipation
Primary constipation is constipation that is not caused by an underlying medical condition, medication, or structural abnormality (8). Essentially, the problem arises from bowel functions rather than from a disease or physical obstruction. Primary constipation is also called idiopathic constipation (3). Causes of primary constipation include dietary, lifestyle, neuromuscular, and psychological factors.
Although primary constipation is not caused by an underlying medical condition, it can significantly affect quality of life. Understanding its types and causes is essential for effective management and improved patient outcomes.
Primary constipation can be considered as (1) functional constipation, in which stool appropriately passes through the colon at a normal rate, or (2) slow transit constipation, where stool passes through the colon at a prolonged, slow rate (3).
Anorectal dysfunction is the inefficient coordination of the pelvic musculature in the evacuation mechanism and is typically an acquired behavioral disorder.
Secondary Constipation
Secondary constipation is due to chronic diseases, certain medications, or anatomic abnormalities (3). The etiology will be further evaluated in an upcoming section.
Epidemiology
Constipation is a common symptom, impacting up to 10% to 20% of the general population (6). The exact prevalence is underestimated because studies show that most patients do not seek out medical care for constipation. The prevalence of chronic constipation is increasing due to changes in diet composition, accelerated pace of life, and the influence of complex social and psychological factors.
Epidemiological surveys have shown that the incidence of chronic constipation is between 14 and 30% worldwide, affecting individuals of all ages, races, socioeconomic status, and nationalities (10). However, certain populations are impacted at higher rates. The rates of constipation increase with age, affecting roughly one-third of individuals over 60 (6). Individuals residing in nursing homes are more commonly reported. Another risk factor is gender, as constipation affects women more than men (7). Recent studies have also noted a two-fold higher rate of constipation among African Americans and those with lower socioeconomic status (income <$20,000 per year) (6).
Social determinants of health (SDOH) are the non-medical factors that impact health outcomes, they encompass the environments in which people are born, grow, live, work, and age, as well as the systems and structures that shape these conditions (9). SDOH significantly impacts health, quality of life, and health disparities across different populations, and research shows a correlation with constipation. These include lifestyle, demographics, education, healthcare access, and adherence to medications (7).

Self Quiz
Ask yourself...
- How would you describe the difference between primary and secondary constipation?
- What populations are more impacted by constipation?
- How can lifestyle, demographics, and education impact overall health?
- Can you discuss the reasons that chronic constipation rates may be increasing?
Pathophysiology
The underlying pathophysiology of constipation varies among different individuals. There are basic mechanical pathophysiological functions, such as the changes in feces once it stays in the rectum for too long and changes in mucous membrane sensitivity and peristalsis if the urge is ignored.
The pathophysiology of constipation can be categorized based on the underlying causes and mechanisms. These categories help identify the specific factors contributing to constipation and guide appropriate interventions. The primary mechanisms are colonic sensorimotor dysfunction and microbiome alteration (10). Factors associated with these mechanisms include gastrointestinal motility and fluid transport, anorectal movement and sensory functions, and dietary and behavioral factors.
Constipation occurs when the fecal mass stays in the rectal cavity for an extended period that is either atypical for the patient or less than three times within a week (5). As the fecal material lingers in the rectum, additional water is absorbed, and the feces becomes smaller, firmer, drier, and more difficult (or painful) to pass.
Another pathophysiological process of constipation can be described by the common saying, “Use it or lose it!”. In this case, when the urge to defecate is ignored, it becomes less recognized. Laxation is the term used for the urge to have a bowel movement (8), so when the urge is ignored, the muscular and rectal mucous membranes become less sensitive to the presence of fecal matter in the rectum (8).
It is important to review gastrointestinal mobility.
Gastrointestinal Motility
Gastrointestinal (GI) motility is the coordinated contractions of the muscles in the gastrointestinal tract for the movement of food and waste products. This process is essential for digestion, absorption of nutrients, and the exit of stool.
Components of GI Motility:
- Peristalsis is the wave-like contractions that move food along the digestive tract.
- Segmental contractions are rhythmic contractions that mix food with digestive enzymes and promote absorption.
- Tonic contractions are sustained muscle contractions that maintain tone in certain areas, such as the sphincters.
Anorectal dyssynergy is a dysfunction of the coordination between the rectal and pelvic floor muscles during defecation. is a common cause of chronic constipation. Normally, defecation involves the relaxation of the anal sphincter and pelvic floor muscles, combined with an increase in intra-abdominal pressure. In anorectal dyssynergy, this process is disrupted, leading to difficulties in stool evacuation despite the presence of normal colonic transit.
Diagnosis is typically made using tests such as anorectal manometry or balloon expulsion tests, and treatment may involve biofeedback therapy, pelvic floor exercises, or other interventions aimed at strengthening the muscles for coordination during defecation.
One prospective study of patients with chronic constipation showed that there was an inability to coordinate the abdominal, rectal, and pelvic floor muscles during defecation. This inability includes impaired rectal contraction, paradoxical anal contraction, or inadequate anal relaxation.
(6)

Self Quiz
Ask yourself...
- What happens to fecal material when it is stored in the rectum for an extended period?
- Can you describe anorectal dyssynergy?
- What are possible reasons the urge to defecate may be ignored?
- Can you explain why gastrointestinal mobility (peristalsis, contraction, etc.) is essential to digestion, absorption of nutrients, and the exit of stool?
Etiology
Constipation can result from a variety of interconnected factors that influence bowel function. Nurses should recognize how the etiology of primary and secondary constipation is different.
Underlying Causes of Primary Constipation
Remember – primary constipation results from irregular bowel functions, not an underlying medical condition or medication. This type of constipation is commonly the cause of daily lifestyle factors. These lifestyle factors can be grouped as dietary and functional.
- Dietary factors
- Low fiber intake
- Lack of nutrient-dense foods
- Inadequate fluid intake
- Irregular eating patterns
- Functional factors
- Low or minimal physical activity
- Ignoring the urge to defecate
- Pain or discomfort with defecation
- Weak abdominal muscles
- Environmental changes or time constraints
- Lack of privacy leads to avoidance of a bowel movement for extended periods.
Underlying Causes of Secondary Constipation
- Endocrine/metabolic disorders
- Hyperparathyroidism
- Diabetes mellitus
- Uremia
- Hypercalcemia
- Hypothyroidism
- Myopathic conditions
- Amyloidosis
- Myotonic dystrophy
- Scleroderma
- Neurologic diseases
- Autonomic neuropathy
- Cerebrovascular disease
- Hirschsprung’s disease
- Multiple sclerosis
- Parkinson’s disease
- Spinal cord injury/tumor
- Psychological conditions
- Anxiety/depression
- Somatization
- Structural abnormalities
- Anal fissure/stricture or hemorrhoid
- Colonic stricture
- Inflammatory bowel disease
- Obstructive colonic mass
- Rectal prolapse or rectocele
- Others
- Irritable bowel syndrome
- Pregnancy
- Medications
- Antacids
- Anticholinergics
- Antidepressants
- Antihistamines
- Calcium channel blockers
- Clonidine
- Diuretics
- Iron
- Narcotics
- NSAIDS
- Opioids
- Psychotropics
- Sympathomimetics
(3)
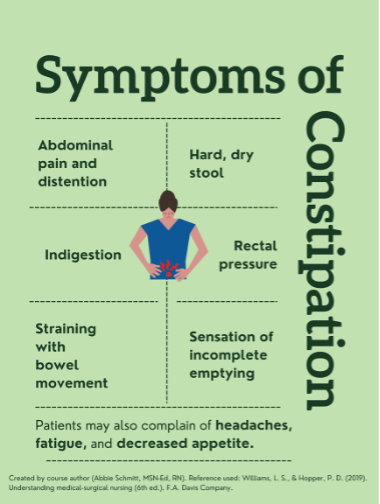
Signs and Symptoms
The most common symptoms of constipation are abdominal distention and discomfort, indigestion, “rumbling” of the intestinal system, straining during bowel movements, sensation of incomplete emptying, and rectal pressure (8). The description of stool is a key factor in clinical symptomology. The stool will likely be dry, hard, fragmented, and difficult or painful to pass. There may be findings of fresh bleeding (bright red) around the rectum, or protrusions.
Patients may also report fatigue, decreased appetite, and headache (5). There may also be mood changes related to constipation, such as irritability or depression (4).
Pharmacological/Non-Pharmacological Treatment
Constipation management encompasses a harmonious blend of pharmacological and non-pharmacological strategies. Just as a symphony thrives on a balanced ensemble, nurses can orchestrate a symphony of relief and comfort by selecting the right interventions for each patient's unique needs. Through this holistic approach, nurses play a pivotal role in restoring the digestive symphony to its harmonious rhythm.
Pharmacological
As nurses step into the realm of constipation management, they encounter a diverse array of strategies that can harmonize the digestive symphony. Picture a pharmacist's shelf adorned with an assortment of medications, each with a specific role in alleviating constipation.
Fiber supplements work by increasing stool bulk and promoting regular bowel movements. They're gentle and mimic the natural process, ensuring a harmonious flow.
Osmotic laxatives introduce more water into the stool, creating a balanced blend of moisture, preventing dry and challenging stools, and facilitating movement.
Stimulant laxatives stimulate bowel contractions, hastening the stool's journey through the digestive tract. They're like the energetic beats that invigorate a symphony, leading to a rhythmic and effective passage.
Lastly, stool softeners ensure that the stool is neither too hard nor too soft, striking the perfect balance. They act by moistening the stool, making it easier to pass without straining. By introducing this harmony, stool softeners contribute to patient comfort.
Non-pharmacological
Beyond the realm of medications lies an equally vital avenue: non-pharmacological interventions. Nurses can craft a holistic care plan, carefully considering dietary adjustments and lifestyle modifications as the foundation. Examples of non-pharmacological interventions include the following:
A diet rich in fiber guides the stool's journey with ease. Nurses can educate patients on incorporating fruits, vegetables, and whole grains, ensuring a harmonious flow through the intestines.
Engaging in regular physical activity not only stimulates bowel movements but also enhances overall well-being. Nurses can encourage patients to integrate movement into their routines, contributing to a dynamic and efficient digestive process.
Relaxation techniques play a vital role in constipation management. Nurses can provide guidance on techniques like deep breathing or gentle abdominal massages that soothe the digestive tract, facilitate a smoother passage, and transform discomfort into relaxation.

Self Quiz
Ask yourself...
- What are the most common symptoms of constipation?
- Can you think of words patients may use to describe abdominal discomfort or indigestion?
- Are you familiar with ways of assessing rectal bleeding?
- What are mood changes that may correlate with constipation?
Assessment
A thorough history and physical examination are essential. Patients may feel uncomfortable or self-conscious when discussing bowel habits. It is important to establish a trusting and comfortable rapport before asking these questions. Providing privacy is meaningful.
Data Collection
- Onset, nature, duration of constipation.
- Past bowel movement patterns
- Current bowel patterns
- Occupation
- Lifestyle habits (nutrition, exercise, stress, coping, support)
- History of laxative or enema use
- Current medication regimen
(8)
Focused Assessment
- Inspect the abdomen for distention and symmetry
- Palpate the abdomen to assess for tenderness or distention.
- Rectal examination may identify anal fissures and hemorrhoids, which can contribute to painful bowel movements.
- Assessment of the anal sphincter tone can provide clues of neurological disorders which may impair sphincter function.
- A digital rectal exam may also reveal a rectal mass or retained stool.
(8)
Labs
- CBC
- BMP: calcium and creatinine levels
- TSH
Endoscopy
- Colonoscopy procedures should follow current guidelines.
- Patients with constipation and “red flag” symptoms of rectal bleeding, heme-positive stool, iron deficiency anemia, weight loss of >10 lbs., obstructive symptoms, or family history of colorectal cancer (3).
Radiography imaging is not especially helpful in underlying etiology, but it may detect stool retention. Barium radiographs may help detect Hirschsprung’s disease. Secondary tests such as anorectal manometry and colonic transit studies can be used to evaluate patients whose constipation is refractory (3).
Diagnosis Criteria
Chronic constipation is usually outlined by clinical symptoms known as the Rome criteria. The Rome IV diagnostic criteria define functional constipation as two or more of the following findings occurring in at least 25% of defecations
- Straining during the bowel movement
- Lumpy or hard stool
- A sensation of incomplete evacuation
- A sensation of anorectal obstruction/blockage
- The use of manual maneuvers to facilitate defecation.
- Loose stools are rare without the use of laxatives
- Having fewer than three spontaneous defecations per week.
The criteria also require these findings to be present for longer than 3 months, with an initial symptom onset of longer than 6 months.
(2,3)

Self Quiz
Ask yourself...
- Can you describe the Roma IV diagnostic criteria for constipation?
- Why are bowel patterns and history important to the assessment of constipation?
Treatment
Nonpharmacologic Treatments
- Bowel training – Encourage patients to attempt a bowel movement in the morning, shortly after awakening, when the bowels are more active, and 30 min after meals to encourage gastrocolic reflex.
- Increase dietary fiber intake
- The recommended intake is 20–35 g daily and an increase of 5 g daily until the recommended daily intake is reached. Increase fiber-rich foods: bran, fruits, vegetables, nuts, and prune juice.
- Psyllium and methylcellulose are the most effective forms of fiber replacement.
- Increase fluid intake – decreased intake may result in fecal impaction
- Regular exercise
- Biofeedback/ pelvic floor retraining – useful for anorectal dysfunction.
(3)
Pharmacologic Treatment
A clinical practice guideline jointly developed by the American Gastroenterological Association (AGA) and the American College of Gastroenterology (ACG) provides evidence-based recommendations for the pharmacological treatment of chronic idiopathic constipation (CIC) in adults (1).
The guidelines provide strong recommendations for the use of polyethylene glycol, sodium picosulfate, linaclotide, plecanatide, and prucalopride based on evidence for effectiveness. Conditional recommendations were given for the use of fiber, lactulose, senna, magnesium oxide, and lubiprostone, emphasizing the need for individualized treatment approaches. The guidelines highlight an individualized approach that considers patient preferences, lifestyle, costs, and medication availability (2).
Types of pharmacological treatments:
- Bulk laxatives – Citrucel and Metamucil absorb water from the intestinal lumen to increase stool mass and soften stool consistency.
- Recommended for patients with functional normal transit constipation.
- Side effects include bloating and increased gas production.
- Emollient laxatives—stool softeners: docusate lowers surface tension, thereby allowing water to more easily enter the bowel.
- Not as effective as bulk laxatives but useful in patients with painful defecation conditions such as hemorrhoids or anal fissures.
- Osmotic laxatives
- Milk of magnesia, magnesium citrate, MiraLAX, and lactulose hyperosmolar agents use osmotic activity to result in the secretion of water into the intestinal lumen.
Precautions:
- Monitor for electrolyte imbalances such as hypokalemia and hypermagnesemia.
- Use with caution in congestive heart failure and chronic renal insufficiency patients.
- Stimulant laxatives: Dulcolax, senna, tegaserod, castor oil, and bisacodyl increase intestinal motility and secretion of water into the bowel.
- Common side effects include abdominal discomfort and cramping as a result of increased peristalsis.
- Contraindicated for patients with suspected bowel obstruction.
(3)
Complications and Negative Impacts on Quality of Life
The most common complications associated with constipation are discomfort and irritation that can lead to:
- Hemorrhoids
- Rectal bleeding
- Anal fissures
Sometimes, the difficulty passing a bowel movement can cause more serious complications, such as:
- Rectal prolapse (the large intestine detaches inside the body and pushes out of the rectum)
- Fecal impaction (hard, dry stool is stuck in the body and unable to be expelled naturally)
Constipation significantly impacts quality of life (QOL), affecting both physical and emotional well-being. Patients with constipation may experience more negative QOL. Studies reported that chronic constipation also causes greater school and work absenteeism and loss of productivity (4).
Nursing Implications and Patient Education
Patient education is an important component of effective constipation management.
Assessment of Knowledge and Baseline Habits
- Assess the patient’s current understanding of constipation and its causes.
- Evaluate dietary habits, fluid intake, physical activity, and medication use that may contribute to constipation.
Provide education on the following:
- Causes and Risk Factors
- Risk factors include low fiber intake, inadequate hydration, lack of physical activity, and certain medications (e.g., opioids, and iron supplements).
- Discuss specific risk factors such as age, medical conditions (e.g., diabetes, hypothyroidism), or recent surgeries.
- Lifestyle Modifications
- Dietary Changes
- Hydration
- Physical Activity
- Healthy Bowel Habits
- Encourage patients to respond promptly to the urge to defecate to avoid hardening of stools and reduced sensitivity.
- Recommend a regular bowel routine, such as attempting bowel movements after meals to take advantage of the gastrocolic reflex.
- Discuss Medication Use
- Advise patients on the appropriate use of laxatives, stool softeners, and other medications for short-term relief.
- Discourage routine use of laxatives and enemas to avoid trauma to the intestinal mucosa, dehydration, and eventual failure of defecation stimulus. (Bulk-adding laxatives are not irritating and are usually permitted.)
- Address Psychological Factors
- Tailor Education to Special Populations
- Encourage Self-Monitoring Log
- Teach patients to track their bowel habits, dietary intake, and hydration levels to identify patterns and triggers.
- Provide Written Materials and Resources
- Offer brochures, handouts, or trusted websites for additional information.
In the inpatient settings, nursing interventions should include:
- Record intake and output accurately to ensure correct fluid replacement therapy.
- Note the color and consistency of stool and frequency of bowel movements to form the basis of an effective treatment plan.
- Promote ample fluid intake, if appropriate, to minimize constipation with increased intestinal fluid content.
- Encourage the patient to increase dietary intake of fiber to improve intestinal muscle tone and promote comfortable elimination.
- Encourage the patient to walk and exercise as much as possible to stimulate intestinal activity.
(Lip)

Self Quiz
Ask yourself...
- Why is it important to discourage patients from overusing laxatives and enemas?
- How can nurses encourage bowel training routines?
- Can you name the major lifestyle modifications that are important in constipation management?
- Are you familiar with fiber-rich foods?
Conclusion
Constipation is a common but complex condition that can significantly impact a person’s quality of life and overall health. Nurses play a meaningful role in identifying, preventing, and managing constipation through comprehensive assessment, evidence-based interventions, and patient education. Understanding the underlying causes and employing tailored strategies can empower patients to take control of their bowel health. This course has provided learners with the knowledge and tools to approach constipation with confidence, compassion, and clinical expertise. Remember that even small changes in habits can lead to meaningful improvements in well-being.

Self Quiz
Ask yourself...
- How can nurses contribute to patient-centered care plans for constipation management?
- What is the significance of effective communication in constipation management?
- Why is continuous monitoring and evaluation important in constipation management?
Conclusion
Constipation is a significant concern that impacts the comfort and well-being of hospitalized and long-term care patients. Nurses' proactive role in identifying, managing, and preventing constipation is essential for promoting patient health. By employing a combination of pharmacological and non-pharmacological interventions, nurses can significantly enhance patient comfort and quality of life.
Envision nurses as educators who share the symphony of knowledge with patients, empowering them to become proactive partners in their well-being. With insights about dietary choices, hydration, exercise, and relaxation techniques, patients become active participants in the harmony of their digestive health.
Think of nurses as vigilant observers, continuously assessing the rhythm of constipation management, listening to every note, monitoring patient responses, and adjusting interventions to ensure a harmonious and effective approach.
Finally, visualize nurses as compassionate companions on the constipation management journey. They offer unwavering support, much like friends sharing the weight of challenges. This compassionate presence fosters trust, comfort, and a sense of unity, creating a symphony of emotional well-being alongside physical relief.
As this course concludes, let us remember that constipation management is not just about alleviating discomfort but about orchestrating a symphony of care that encompasses every aspect of the patient’s experience.
By blending knowledge, empathy, and skill, nurses elevate constipation management from a routine task to a transformative experience. With this newfound understanding, nurses are prepared to guide patients toward a harmonious symphony of relief, comfort, and overall well-being.
References + Disclaimer
- Anderson, R. J., & Brown, C. A. (2019). Infrequent bowel movements as a symptom of constipation. Journal of Gastrointestinal Health, 37(2), 89-103. doi:10.1234/jgh.37.2.89
- Harrison, K. L., et al. (2020). Education and empowerment in constipation management. Patient Education and Counseling, 56(3), 178-192. doi:10.7890/pec.56.3.178
- Johnson, L. M., & Smith, P. B. (2017). Compassionate support in constipation management. Journal of Patient Care, 23(1), 45-58. doi:10.7890/jpc.23.1.45
- Johnson, M. S., Williams, K. L., & Brown, A. B. (2018). Prevalence of constipation in hospital and long-term care settings. Journal of Healthcare Management, 42(4), 56-68. doi:10.7890/jhm.42.4.56
- Parker, A. B., & Turner, D. S. (2018). Continuous monitoring and evaluation in constipation management. Nursing Journal, 42(2), 90-103. doi:10.5678/nj.42.2.90
- Roberts, S. M., et al. (2020). Excessive straining in constipation: A qualitative analysis. Journal of Patient Care, 46(3), 120-135. doi:10.5678/jpc.46.3.120
- Robinson, E. D., & Davis, P. L. (2020). Interdisciplinary collaboration in constipation management. Journal of Interprofessional Care, 35(2), 89-101. doi:10.5678/jic.35.2.89
- Smith, A. B., & Johnson, C. D. (2020). Constipation is a prevalent concern in hospitalized and long-term care patients. Journal of Nursing Care, 45(2), 78-89. doi:10.1234/jnc.45.2.78
- Smith, A. B., & Williams, R. S. (2018). Bloating as a symptom of constipation: Insights from clinical studies. Journal of Gastrointestinal Disorders, 56(1), 45-58. doi:10.7890/jgd.56.1.45
- Smith, J. A., & Jones, M. B. (2021). The role of lifestyle and diet in constipation pathophysiology. Journal of Digestive Health, 39(2), 89-105. doi:10.1234/jdh.39.2.89
- Taylor, M. A., & Johnson, K. B. (2021). Abdominal discomfort as an indicator of constipation imbalance. Journal of Digestive Health, 39(4), 178-192. doi:10.1234/jdh.39.4.178
- Thompson, L. M., & Miller, R. K. (2022). Holistic assessment in constipation management. Journal of Nursing Practice, 48(1), 56-67. doi:10.7890/jnp.48.1.56
- White, S. J., & Thomas, M. D. (2021). Patient-centered care plans in constipation management. Nursing Journal, 39(4), 210-225. doi:10.5678/nj.39.4.210
- Wilson, C. A., et al. (2019). Effective communication in constipation care. Journal of Healthcare Communication, 44(3), 120-135. doi:10.1234/jhc.44.3.120
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Spinal Cord Injury: Bowel and Bladder Management
Introduction
Imagine one day you are able to walk and take care of your own needs. Now, imagine one week later you wake up no longer able to walk, feel anything below your waist, or hold your bowels.
This is a reality for many people who sustain spinal cord injuries. Managing changes in bowel and bladder function is one of many challenges that people with spinal cord injuries and their families or caregivers face.
This course will provide learners with the knowledge needed to assist patients who have spinal cord injuries with bowel and bladder management to improve the quality of life in this group.

Self Quiz
Ask yourself...
- What are some societal misconceptions or stereotypes about people with spinal cord injuries?
- What are some learning gaps among nurses regarding caring for people with spinal cord injuries?
- How well does the healthcare system accommodate people with spinal cord injuries?
Spinal Cord Injuries: The Basics
Spinal Cord Function
Before defining a spinal cord injury, it is important to understand the function of the spinal cord itself. The spinal cord is a structure of the nervous system that is nestled within the vertebrae of the back and helps to distribute information from the brain (messages) to the rest of the body [1].
These messages result in sensation and other neurological functions. While it may be common to primarily associate the nervous system with numbness, tingling, or pain, nerves serve an important purpose in the body’s function as a whole.
Spinal Cord Injury Definition
When the spinal cord is injured, messages from the brain may be limited or entirely blocked from reaching the rest of the body. Spinal cord injuries refer to any damage to the spinal cord caused by trauma or disease [2]. Spinal cord injuries can result in problems with sensation and body movements.
For example, the brain sends messages through the spinal cord to muscles and tissues to help with voluntary and involuntary movements. This includes physical activity like running and exercising, or something as simple as bowel and bladder elimination.
Spinal Cord Injury Causes
Spinal cord injuries occur when the spinal cord or its vertebrae, ligaments, or disks are damaged [3]. While trauma is the most common cause of spinal cord injuries in the U.S., medical conditions are the primary causes in low-income countries [4] [2].
Trauma
- Vehicle accidents: Accounts for 40% of all cases [2]
- Falls: Accounts for 32% of all cases [2]
- Violence: Includes gun violence and assaults; accounts for 13% of all cases [2] [5]
- Sport-related accidents: Accounts for 8% of all cases [2]
Medical Conditions
- Multiple Sclerosis (MS): Damage to the myelin (or insulating cover) of the nerve fibers [1]
- Amyotrophic Lateral Sclerosis (ALS): Lou Gehrig’s disease, damage to the nerve cells that control voluntary muscle movements [1]
- Post-Polio: Damage to the central nervous system caused by a virus [1]
- Spina Bifida: Congenital defect of the neural tube (structure in utero that eventually forms the central nervous system) [1]
- Transverse Myelitis (TM): Inflammation of the spinal cord caused by viruses and bacteria [1]
- Syringomyelia: Cysts within the spinal cord often caused by a congenital brain abnormality [1]
- Brown-Sequard Syndrome (BSS): Lesions in the spinal cord that causes weakness or paralysis on one side of the body and loss of sensation on the other [1]
- Cauda Equina Syndrome: Compression of the nerves in the lower spinal region [1]
Spinal Cord Injury Statistics
According to the World Health Organization, between 250,000 and 500,000 people worldwide are living with spinal cord injuries [4]. In the U.S., this number is estimated to be between 255,000 and 383,000 with 18,000 new cases each year for those with trauma-related spinal cord injuries [6].
Age/Gender
Globally, young adult males (age 20 to 29) and males over the age of 70 are most at risk. In the U.S., males are also at highest risk, and of this group, 43 is the average age [2].
While it is less common for females to acquire a spinal cord injury (2:1 ratio in comparison to males), when they do occur, adolescent females (15-19) and older females (age 60 and over) are most at risk globally [4].
Race/Ethnicity
In the U.S. since 2015, around 56% of spinal cord injuries related to trauma occurred among non-Hispanic whites, 25% among non-Hispanic Black people, and about 14% among Hispanics [6].
Mortality
People with spinal cord injuries are 2 to 5 times more likely to die prematurely than those without these injuries (WHO, 2013). People with spinal cord injuries are also more likely to die within the first year of the injury than in subsequent years. In the U.S., pneumonia, and septicemia – a blood infection – are the top causes of death in patients with spinal cord injuries [6].
Financial Impact
Spinal cord injuries cost the U.S. healthcare system billions each year [6]. Depending on the type, spinal cord injuries can cost from around $430,000 to $1,300,000 in the first year and between $52,000 and $228,000 each subsequent year [6].
These numbers do not account for the extra costs associated with loss of wages and productivity which can reach approximately $89,000 each year [6].

Self Quiz
Ask yourself...
- What is one function of the spinal cord?
- What is one way to prevent spinal cord injuries in any group?
- Why do you think injuries caused by medical conditions are least likely to occur in the U.S.?
- Why do you think the first year of care after the injury is the most costly?
Think about someone you know (or cared for) who had a spinal cord injury.
- Did they have total or partial loss of feeling and movement to the extremities?
- What comorbidities or complications did they have associated with the injury?
- In what ways did the injury affect their overall quality of life?
Spinal Cord Injuries: Types and Complications
Four Levels of the Spinal Cord
- Cervical (vertebrae C1 – C8): Neck; controls the back of the head down to the arms, hands, and diaphragm
- Thoracic (vertebrae T1 – T12): Upper mid-back; controls the chest muscles, many organs, some back muscles, and parts of the abdomen
- Lumbar (vertebrae L1 – L5): Lower back; controls parts of the lower abdomen, lower back, parts of the leg, buttocks, and some of the external genital organs
- Sacral (vertebrae S1 – S5): Lower back; controls the thighs down to the feet, anus, and most of the external genital organs
Types of Spinal Cord Injuries
Spinal cord injuries may be classified by level and degree of impairment. There are four types of spinal cord injuries [5].
Injury Level
- Tetraplegia or Quadriplegia: Injury at the cervical level; loss of feeling or movement to the head, neck, and down. People with this type of spinal cord injury have the most impairment.
- Paraplegia: Injury at the thoracic level or below; limited or complete loss of feeling or movement to the lower part of the body.
Impairment
- Incomplete spinal cord injury: Some sensation and mobility below the level of injury as the spinal cord can still transmit some messages from the brain.
- Complete spinal cord injury: Total loss of all sensation and mobility below the level of injury. Spinal cord injuries of this type have the greatest functional loss.

Spinal Cord Injury Complications
Complications from spinal cord injuries can be physical, mental, or social, and can impact overall quality of life. There are six common complications of spinal cord injuries [2].
Depression
Studies show that 32.9% of adults with disabilities experience frequent mental distress [7]. Mental distress may be related to functional limitations, chronic disease, and the increased need for healthcare services. Up to 37% of people with spinal cord injuries develop depression [2].
Pressure injuries
People with spinal cord injuries may have problems with circulation and skin sensation– both risk factors for pressure injuries. Some may be bedridden or wheelchair-bound which also places them at risk for pressure injuries. Up to 80% of people with spinal cord injuries will have a pressure injury during their lifetime and 30% will have more than one [2].
Spasticity
Around 65% - 78% of people with spinal cord injuries have spasticity [2]. Spasticity is uncontrolled muscle tightening or contraction. The damage from spinal cord injuries causes misfires in the nervous system leading to twitching, jerking, or stiffening of muscles.
Autonomic dysreflexia
In some people with spinal cord injuries, a full bladder or bowel distention can cause a potentially dangerous condition called autonomic dysreflexia. The full bladder or bowel triggers a sudden exaggerated reflex that causes an increase in blood pressure. This condition is also associated with a severe headache, low heart rate, cold skin, and sweating in the lower body [8].
Respiratory problems
If the diaphragm function is affected, as with cervical spinal cord injuries, there may be breathing difficulties. People with lumbar spinal cord injuries can even have respiratory problems as the abdominal muscles are used to breathe.
Sexual problems
Due to changes in muscle function and depending on the degree of damage, people with spinal cord injuries may have problems with arousal and climax due to altered sensations and changes in sexual reflexes.
Changes in bowel and bladder function
Many people with spinal cord injuries lose bowel control. Bowel problems can include constipation, impaction, and incontinence. They may also have problems with urination, for example, urinary retention.

Self Quiz
Ask yourself...
- Why might a person with a disability experience mental distress?
- In what type of spinal cord injury does a person lose all sensation and mobility below the waist?
- Why are people with spinal cord injuries at risk for pressure injuries?
- How can spinal cord injuries affect a person’s personal relationships?
Bowel and Bladder Dysfunction in Spinal Cord Injuries
This section will cover the normal function of the bowel and bladder, and the types of bowel and bladder dysfunction that occurs in patients with spinal cord injuries.


Self Quiz
Ask yourself...
Think about a time you assisted with bowel or bladder management in someone with a spinal cord injury.
- What types of activities were included in their bowel or bladder regimen?
- What challenges did you encounter during bowel or bladder care?
- What difficulties did they express to you about managing their bowel or bladder program?
- In what ways did you assist them in managing their own bowel or bladder program?
Normal Bowel and Bladder Function
In normal bowel and bladder function, when the rectum or bladder fills with stool/urine and presses on area nerves (stimulation), the message is sent to the spinal cord which sends it to the brain. The brain gives the person the “urge” feeling, allowing an option to control the elimination or not.
Whatever decision the person makes, the brain sends the message back to the spinal cord, which in turn sends a message to the elimination muscles (anal and bladder sphincters) to either relax or stay closed until the person is ready. In people with spinal cord injuries, the messages are limited or blocked, leading to problems with bowel and bladder control [9] [10].
Bowel Dysfunction with Spinal Cord Injuries
Reflex hypertonic neurogenic bowel occurs when a rectum full of stool presses against area nerves sending a message to the spinal cord, but it stops there. The message never makes it to the brain, so the person never gets the urge.
As a result, a reflex is set off, prompting the spinal cord to send a message to the anal muscle (sphincter) instead, causing it to relax and release the stool. This condition leads to bowel incontinence and usually occurs in spinal injuries at the cervical and thoracic levels [9] [10].
Flaccid hypotonic bowel occurs when area nerves are also stimulated by a full rectum, but the message does not even reach the spinal cord, so there is no reflex. The anal sphincter is always in a relaxed state.
As a result, the bowels simply empty when they are full, and this can occur at any time without the person having the ability to control it. This condition results in bowel incontinence and can lead to constipation as the patient does not have the urge and may not have the ability to push. This condition usually occurs in spinal injuries at the lumbar level [9] [10].
Bladder Dysfunction with Spinal Cord Injuries
Reflex neurogenic bladder occurs when the bladder automatically starts to contract after filling with a certain amount of urine. The person has no urge to go as the messages are either limited or blocked from reaching the brain, therefore leading to loss of bladder control. Similar to reflex hypertonic neurogenic bowel, the full bladder triggers are nerves that set off a reflex, prompting the spinal cord to send messages to the bladder releasing urine outside of the person’s control [9] [10].
Acontractile bladder occurs when the bladder loses muscle tone after a spinal cord injury, lessening its ability to contract, leading to bladder distention, and dribbling of urine. People with this condition need to use urinary catheters to help empty the bladder [9].


Self Quiz
Ask yourself...
- What is one role of the brain in bowel and bladder function?
- Which type of bowel dysfunction occurs in thoracic-level spinal cord injuries?
- In which type of bowel dysfunction might a suppository be most effective?
- In which type of bladder dysfunction does the bladder lose muscle tone?
The Nurse’s Role in Bowel and Bladder Management
This section will cover how nurses can assess, intervene, and teach when caring for patients with spinal cord injuries who have bowel and bladder dysfunction.

Self Quiz
Ask yourself...
Think about your experiences with patients with spinal cord injuries and their family or caregivers.
-
- How knowledgeable was the patient about their bowel or bladder care?
- In what ways were the family or caregiver involved in the plan of care?
- Did the family or caregiver have any learning gaps that needed to be addressed?
- What difficulties did the family or caregiver express to you about their role?
Nurse Assessments
When caring for patients with spinal cord injuries, nurses should obtain a detailed bowel and bladder history including diet, fluid intake, medications, and elimination patterns/habits [11]. Many of these patients may already manage their own bowel and bladder care at home.
If so, the nurse should obtain the patient’s current regimen and communicate the information to the physician. The physician may choose to continue the regimen or adjust as needed based on the patient’s current illness/condition.
Questions the nurse can ask the patient:
- What does your typical diet consist of?
- How much fluid do you drink on a daily basis?
- How often do you have a bowel movement or urinate?
- Do you schedule your bowel movements with assistance from medications?
- Are there certain body positions or things you do to help you pass stool more easily?
- How often do you use an intermittent urinary catheter for bladder relief?
- How much time do you spend on your bowel and bladder regimens?
- Do you care for all of your elimination needs or does someone help you?
- How does your bowel and bladder dysfunction affect your quality of life?
Some assessments may be observed. For example, nurses may notice that the patient has a surgically placed permanent suprapubic urinary catheter or colostomy (when the bowel is cut somewhere above the level of the rectum and diverted to the outside of the abdomen).
Nurse Interventions
Since many patients with spinal cord injuries have problems with bowel and bladder function, elimination must be scheduled. Nurses can help by implementing bowel and bladder programs and providing education and support to patients, families, or caregivers.
Regimens
Follow the patient’s home bowel and bladder regimen (as ordered). This may include maintaining intermittent catheterization every few hours or administering suppositories daily.
For patients who do not have a regimen already or wish to modify their current one, encourage them to pay attention to how often they urinate and pass stools, elimination problems, foods that alleviate or worsen the problem, and medications or other things that help. This can be done through a diary.
Dietary Considerations
Educate patients on the importance of a fiber-rich diet to avoid constipation. Patients should also be made aware that high-fat foods, spicy foods, and caffeine can alter gut dynamics and lead to bowel incontinence episodes [12].
Fluid Intake
Some patients may avoid drinking enough water to avoid bladder complications (e.g., frequent incontinent episodes) [12]. However, nurses should educate patients on the importance of adequate fluid intake to prevent constipation. Patients should be made aware that bladder and bowel elimination regimens go hand in hand.
Bladder Elimination
For bladder dysfunction, help patients perform intermittent urinary catheterization as needed or place a temporary urinary catheter (as ordered).
Bowel Elimination
For bowel dysfunction, administer ordered suppositories and laxatives to help the bowels move (use suppositories in conjunction with the level of sensation the patient has near the anus/rectum) [9]. Changes in body position may help as well.
While many of these interventions may not work in some patients with spinal cord injuries, bowel irrigation (water enemas) may be helpful [11]. Surgical placement of a colostomy may be indicated if all other measures have failed [11].
Emotional Support
Ensure privacy and sensitivity during all elimination care as patients may experience embarrassment or frustration.
Education for Families or Caregivers
Provide education to families or caregivers on the importance of helping patients stay consistent with their elimination regimen, follow diet and fluid intake recommendations, and comply with medication orders.
Referrals
Inform the physician if interventions are not effective or if the patient, family, or caregiver has a special need (e.g., counselor or dietician). Refer patients and families or caregivers to support groups as needed.
Support Groups and Resources
Christopher and Dana Reeve Foundation
Christopher Reeve – an actor who was left paralyzed after an equestrian accident – and his wife Dana’s legacy lives on through their foundation, an organization that advocates for people living with paralysis [13].
Miami Project to Cure Paralysis
In response to his son, who acquired a spinal cord injury during college football, NFL Hall of Famer Nick Buoniconti and world-renowned neurosurgeon Barth A. Green, M.D. started a research program aimed at finding a cure for paralysis and discovering new treatments for many other neurological injuries and disorders [14].
National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR)
The National Institute on Disability, Independent Living, and Rehabilitation Research, a part of the U.S. Department of Health and Human Services’ Administration for Community Living, helps people with disabilities integrate into society, employment, and independent living [15].
Paralyzed Veterans of America (PVA)
A group of World War II veterans who returned home with spinal cord injuries, started this organization to support those with spinal cord injuries and dysfunction. Today, the organization focuses on quality health care, research and education, benefits, and civil rights to affected veterans [16].
The United Spinal Association supports people with spinal cord injuries and those in wheelchairs. The organization advocates for disability rights like access to healthcare, mobility equipment, public transportation, and community support. Support groups can be found on their website [17).

Self Quiz
Ask yourself...
- What is one question a nurse can ask a patient to obtain a bowel and bladder history?
- How can nurses help patients with spinal cord injuries start or modify a bowel or bladder regimen?
- When might a colostomy be indicated for a patient with a spinal cord injury?
- What type of referral might be ordered for a patient with a spinal cord injury who has bowel or bladder dysfunction?
Conclusion
Spinal cord injuries can have devastating effects on patients and their families. Management of basic bodily functions like bowel and bladder elimination should be made as easy as possible for these patients.
When nurses learn how to effectively help patients with spinal cord injuries better manage their own bowel and bladder regimens, quality of life and health outcomes may be improved for this group.
Pressure Injury Prevention, Staging and Treatment
Introduction
When hearing the term HAPI, what comes to mind? The fact is, HAPI may not necessarily generate happy thoughts. Hospital-acquired pressure injuries (HAPIs) are a significant problem in the U.S. today. In fact, pressure injuries in general – whether acquired in a hospital or not – are a global problem.
Many articles have noted that staging and differentiating pressure injuries can be overwhelming for nurses [9]. The purpose of this course is to equip learners with the knowledge needed to reduce pressure injuries, resulting complications, financial risk, and associated death. The information in this course will serve as a valuable resource to nurses from all specialties and backgrounds.
What is a pressure injury?
The National Pressure Injury Advisory Panel (NPIAH) defines pressure injuries as “localized damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device” [17]. Pressure injuries can present as intact or opened skin and can be shallow or deep. Pressure injuries can be quite painful for patients and may require extensive treatment.
Prior to 2016, pressure injuries were termed “pressure ulcers.” However, since ulcer implies “open skin,” the NPIAH changed it to “pressure injury” as the skin is not always open with some of these injuries [22][25].
What causes a pressure injury to develop?
Pressure
Intense and/or prolonged pressure on the patient’s skin and/or tissue can cause compromised blood flow and decreased sensation [7]. This can occur when patients lay or sit on a bony prominence for an extended period of time [16].
Bony prominences are areas where you can easily feel a bone underneath the skin or tissue when palpating. These can include the heels, hips, elbows, and tailbone. Approximately two-thirds of all pressure injuries occur on the hip and buttocks area [7].
Friction and Shear
Friction and shear often happen when patients slide down in bed, for example, when the head of the bed is raised. Although “friction and shear” are often used together, there is actually a difference between the two.
While friction occurs when skin is dragged across a coarse surface (leading to surface-level injuries), shearing occurs when internal bodily structures and skin tissue move in opposite directions (leading to deep-level injuries) [10]. Shearing is often associated with a type of pressure injury called deep tissue injury (occurring in the deeper tissue layers rather than on the skin’s surface) [10].

[24]
What are risk factors for developing a pressure injury?
There are numerous risk factors for pressure injuries – some of which may not be directly related to the skin. These risk factors can be categorized as either intrinsic factors (occurring from within the body) or extrinsic (occurring from outside of the body) [2][13].
Intrinsic Risk Factors
- Poor skin perfusion (e.g., peripheral vascular disease or smoking)
- Sensation deficits (e.g., diabetic neuropathy or spinal cord injuries)
- Moist skin (e.g., urinary incontinence or excessive sweating)
- Inadequate nutrition (particularly poor protein intake)
- Poor skin elasticity (e.g., normal age-related skin changes)
- End of life/palliative (leads to organ failure including the skin)
- Limited mobility (i.e., bedridden, or wheelchair-bound)
Extrinsic Risk Factors
- Physical and chemical restraints (leads to limited mobility)
- Undergoing a procedure (laying down for extended periods of time)
- Length of hospital stay (for HAPIs)
- Medical devices (can lead to medical device-related pressure injuries)

Self Quiz
Ask yourself...
- What are the most common areas for pressure injuries to develop?
- What is the major difference between friction and shear?
- What is one reason why elderly adults are at an increased risk for developing a pressure injury?
Statistical Evidence
This section will cover pressure injury statistics both globally and nationally. This section will also cover the impact pressure injuries have on healthcare.
What is happening on a global scale?
In a global study, researchers found that the prevalence (all cases) and incidence (new cases) of pressure injuries in 2019 were 0.85 million and 3.17 million, respectively – numbers that have decreased over time [23][25]. Numbers were disproportionately high in high-income North America, Central Latin America, and Tropic Latin America [25]. Numbers were lowest in Central Asia and Southeast Asia. The report revealed that although numbers are high overall, they are much lower than what they were predicted to be, which may be attributed to better prevention and treatment initiatives.
What is happening nationally?
In the U.S., 2.5 million people develop pressure injuries each year [1]. This number does not account for the many people trying to manage pressure injuries on their own at home (i.e., when family acts as the caregiver).
HAPIs in particular are a growing problem. The most recent data on hospital-acquired conditions in the U.S. shows that from 2014 to 2017, HAPIs increased by 6% (647,000 cases in 2014 to 683,000 in 2017) [6]. Each year 60,000 patients in the U.S. die as a direct result of pressure injuries [1].
How do pressure injuries impact healthcare?
Pressure injuries can be quite costly to the healthcare system. These injuries can lead to persistent pain, prolonged infections, long-term disability, increased healthcare costs, and increased mortality [1].
In the U.S., pressure injuries cost between $9.1 - $11.6 billion per year [1]. These injuries are complex and can be difficult to treat [7]. Often requiring an interdisciplinary approach to care, the costs of one pressure injury admission can be substantial. Individual care for patients with pressure injuries ranges from $20,900 to $151,700 per injury [1]. Not to mention, more than 17,000 lawsuits are related to pressure injuries every year [1].
Due to the significant impact that these injuries have on healthcare, prevention and accurate diagnosis is imperative.

Self Quiz
Ask yourself...
- What are possible contributing factors to the increase in HAPIs in the U.S.?
- What are some factors that may contribute to the high costs of pressure injuries in healthcare settings?
Staging and Diagnosis
The section will cover the staging, varying types, and diagnosis of pressure injuries.
What is the difference between wound assessment and staging?
Pressure injury staging is more than a basic wound assessment. Wound assessment includes visualizing the wound, measuring the size of the wound, paying attention to odors coming from the wound, and lightly palpating the area on and/or around the wound for abnormalities. Pressure injury staging, however, involves determining the specific cause of injury, depth of skin or tissue damage, and progression of the disease.
What are the six stages of pressure injuries?
According to NPIAP guidelines, there are six types of pressure injuries – four of which are stageable [14].

[16]
Stage 1
In Stage 1 pressure injuries, there is intact skin with a localized area of non-blanchable erythema (pink or red in color), which may appear differently in darkly pigmented skin. Before visual changes are noted, there may be the presence of blanchable erythema or changes in sensation, temperature, or firmness. Stage 1 pressure injuries do not have a purple or maroon discoloration (this can indicate a deep tissue pressure injury).
Stage 2
In Stage 2 pressure injuries, there is partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist, and may represent an intact or opened serum-filled blister. Fat (adipose) and deeper tissues are not visible. Granulation tissue, slough (soft moist material, typically yellow or white), and eschar (hard necrotic tissue, typically black in color) are not present. Stage 2 injuries cannot be used to describe wounds associated with moisture-only, skin chaffing, medical adhesives, or trauma.
Stage 3
In Stage 3 pressure injuries, there is full-thickness loss of skin, in which fat is visible in the injury, and granulation tissue and rolled wound edges are often present. Slough and/or eschar may be noted. The depth of tissue damage is dependent on the area of the wound. Areas with a significant amount of fat can develop deep wounds.
Undermining (burrowing in one or more directions, may be wide) and tunneling (burrowing in one direction) may be present. Fascia, muscle, tendon, ligament, cartilage, and/or bone are not exposed. If slough or eschar covers the extent of tissue loss, this would be considered an unstageable pressure injury, not a Stage 3.
Stage 4
In Stage 4 pressure injuries, there is full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage, or bone in the wound. Slough and/or eschar may be visible. Rolled wound edges, undermining, and/or tunneling are often present. The area where the wound is present will determine the depth. As with stage 3 pressure injuries, if slough or eschar covers the extent of tissue loss, this would be considered an unstageable pressure injury.
Unstageable
In unstageable pressure injuries, there is full-thickness skin and tissue loss in which the extent of tissue damage within the wound cannot be confirmed because it is covered by slough or eschar. If the slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar (i.e., dry, adherent, intact without erythema or fluctuance) on an ischemic limb or the heel(s) should not be removed.
Deep Tissue Injury
In deep tissue pressure injuries (also termed: deep tissue injuries or DTIs), there is intact or non-intact skin with localized area or persistent non-blanchable deep red, maroon, purple discoloration, or epidermal separation revealing a dark wound bed or blood-filled blister.
Pain and temperature changes often precede skin color changes. Discoloration may appear differently in darker-pigmented skin. The injury may resolve without tissue loss or may worsen quickly and open up, revealing the actual extent of tissue injury. Deep tissue pressure injuries should not be used to describe vascular, traumatic, neuropathic, or dermatologic conditions.

Self Quiz
Ask yourself...
- How do basic wound assessments differ from pressure injury staging?
- What is the main difference between a Stage 1 pressure injury and deep tissue injury?
- What is one structure you might see in a Stage 4 pressure injury wound bed that you would not see in any other pressure injury?
What are other types of pressure injuries?
Mucosal Membrane Pressure Injury
Mucosal membrane pressure injuries are found on mucous membranes with a history of a medical device in use at the location of the injury. For example, a wound on the inside of a nostril from a nasogastric tube would be considered a mucosal membrane pressure injury. Due to the anatomy of the tissue, mucosal membrane pressure injuries cannot be staged [18].
Medical Device-Related Pressure Injury
Medical device-related pressure injuries, often associated with healthcare facilities, resulting from the use of devices designed and applied for diagnostic or therapeutic purposes [15]. The resulting pressure injury typically conforms to the pattern or shape of the device which makes identification easier. The injury should be staged using the staging system.
Hospital Acquired Pressure Injury (HAPI)
While the general hospital setting places patients at a 5% to 15% increased risk of developing a pressure injury (HAPI), patients in the intensive (or critical) care unit in particular have an even higher risk [17]. Critical care patients typically have serious illnesses and conditions that may cause temporary or permanent functional decline. There is also evidence that pressure injuries in this setting can actually be unavoidable.
The NPIAP defines “unavoidable” pressure injuries as those that still develop after several measures by the health provider have been taken. These measures include when the provider has (a) evaluated the patient’s condition and pressure injury risk factors, (b) defined and implemented interventions consistent with standards of practice and the patient’s needs and goals, and (c) monitored and evaluated the impact of interventions [20]. There are certain situations in which a critical care patient may have a higher risk of developing unavoidable pressure injuries.
In one study of 154 critical care patients, researchers found that 41% of HAPIs were unavoidable and those who had a pressure injury in the past were five times more likely to develop an unavoidable pressure injury during their stay [20]. The study also found that the chance of developing an unavoidable HAPI increased the longer patients stayed in the hospital – a 4% risk increase each day.

Self Quiz
Ask yourself...
- What type of pressure injury can be caused by nasogastric tube use?
- What is it about critical care patients that places them at a high risk for HAPIs?
- In what situation is a pressure injury considered unavoidable?
How are pressure injuries diagnosed?
Diagnosing a pressure injury is done by simply staging the injury. The health provider may stage the injury or rely on the nurse’s staging assessment before giving the final diagnosis and initiating treatment. There are tests that may be ordered to help identify the early stages of a developing injury.
For example, subepidermal moisture assessment (SEM) scanners may help to identify tissue changes early on in patients with darker skin tones [8]. Tests may also be ordered to determine the extent of the damage, disease, or infection caused by a pressure injury. A magnetic resonance imaging test (MRI) can be used to determine if the infection in a stage 4 pressure injury has spread to the bone.

Self Quiz
Ask yourself...
- What are some problems that can occur if a pressure injury is not staged correctly?
- What is one reason a provider would order an MRI of a pressure injury?
Prevention and Treatment
This section will cover various strategies that can be used to prevent and treat pressure injuries.
What are some ways to prevent pressure injuries?
Preventing pressure injuries takes more than just one nurse repositioning a patient every two hours. It involves a combination of strategies, protocols, and guidelines that facilities can implement across various departments, specialties, and care team members. The NIAPH recommends the following prevention strategies [19].
Risk assessment
Facilities should use a standardized risk assessment tool to help identify patients at risk for pressure injuries (i.e., the Braden or Norton Scale). Rather than using the tool as the only risk assessment strategy, risk factors should be identified by other means (for example, by gathering a detailed patient history).
Risk assessments should be performed on a regular basis and updated as needed based on changes in the patient’s condition. Care plans should include risk assessment findings to address needs.
Skin Care
Monitoring and protecting the patient’s skin is vital for pressure injury prevention. Stage 1 pressure injuries should be identified early to prevent the progress of disease. These include looking at pressure points, temperature, and the skin beneath medical devices.
The frequency of assessments may change depending on the department. Ideally, assessments should be performed upon admission and at least once daily. Skin should also be cleaned promptly after incontinence episodes.
Nutritional Care
Tools should be used that help to identify patients at risk for malnutrition. Patients at risk should be referred to a registered dietician or nutritionist. Patients at risk should be weighed daily and monitored for any barriers to adequate nutritional intake. These may include swallowing difficulties, clogged feeding tubes, or delays in intravenous nutrition infusions.
Positioning and mobilization
Immobility can be related to age, general poor health, sedation, and more. Using offloading pressure activities and keeping patients mobile overall can prevent pressure injuries. Patients at risk should be assisted in turning and repositioning on a schedule. Pressure-relieving devices may be used as well. Patients should not be positioned on an area of previous pressure injury.
Monitoring, training, and leadership
Current and new cases of pressure injuries should be documented appropriately and reported. All care team members should be educated on pressure injury prevention and the importance of up-to-date care plans and documentation.
All care team members should be provided with appropriate resources to carry out all strategies outlined. Leadership should be available to all care team members for support (this may include a specialized wound care nurse or wound care provider).


Self Quiz
Ask yourself...
- What is one reason why a patient at risk for pressure injuries would be weighed daily?
- What are two ways to prevent pressure injuries in a patient with limited mobility?
How are pressure injuries treated?
There is no one way to treat a pressure injury. Management of pressure injuries involves a specialized team of care providers and a combination of therapies that aim to target underlying factors and prevent complications [7]. Depending on the stage of the wound and skin risk factors, providers may order specific types of treatments.
Some pressure injury treatments may include the following [7].
- Wound debridement – a procedure in which necrotic tissue is removed from a wound bed to prevent the growth of pathogens in the wound, allowing for healing
- Antibiotic therapy (topical or systemic)
- Medicated ointments applied to the wound bed (e.g., hydrogels, hydrocolloids, or saline-moistened gauze to enable granulation tissue to grow and the wound to heal)
- Nutritional therapies (e.g., referrals to dieticians)
- Disease management (e.g., controlling blood sugar in diabetes)
- Pain medications
- Physical therapy (to keep the patient active)

Self Quiz
Ask yourself...
- In what way does debridement help to heal a pressure injury?
- What non-nursing care team member may be consulted for a patient with a pressure injury?
The Nurse’s Role
The section will cover the nurse’s role in preventing pressure injuries and the progression of disease.
What is the nurse’s role in pressure injury prevention?
Based on NPIAH guidelines, the Agency for Healthcare Research and Quality (AHRQ) – an agency that monitors pressure injury data for the U.S. – breaks down quality initiatives for preventing pressure injuries in a three-component care bundle [2].
A care bundle is a combination of best practices that when used together, can lead to better patient outcomes [2]. The care bundle includes skin assessments, risk assessments, and care planning. Nurses should follow the guidelines listed under each component.
Standardized pressure injury risk assessment
- Use risk assessment tools and processes to identify patients at risk
- Do not rely on tools only, use your own judgment as well (tools are meant to guide the assessment)
- Update risk scores at least once daily and if patient’s condition changes
- Document findings in the medical record
- Communicate findings to other staff involved for continuity of care (e.g., informing another nurse during patient handoff reporting)
Comprehensive skin assessment
- Identify any pressure injuries that may be present
- Determine whether there are other areas of skin breakdown or factors that may predispose the patient to develop a pressure injury (e.g., moist skin)
- Identify other skin issues
- Perform assessments at regular intervals
- Document findings in the medical record
- Communicate findings to other staff involved in care so that appropriate changes can be reported (e.g., informing the nursing assistant)
- Ask colleague to confirm findings for accuracy (i.e., two-nurse skin checks)
Care planning and implementation to address areas of risk
- Create care plans that include each skin risk factor (e.g., nutrition, mobility, and moisture)
- Update care plans as often as needed if there are any changes in the patient’s condition
- Evaluate whether care plan was effective by assessing patient response to interventions
- Individualize care plans for each patient based on risk assessment scores and other observed risks
- Identify patient learning needs and implement teaching as needed
- Document care plan in the medical record
- Communicate care plan to other staff involved for continuity of care (e.g., informing another nurse during patient handoff reporting)

Self Quiz
Ask yourself...
- Why should nurses avoid relying solely on standardized assessment tools?
- Why is documentation important when performing a skin assessment?
- What pressure injury information should nurses communicate during handoff report?
How can nurses prevent medical device-related pressure injuries?
The NPIAP outlined best practices to prevent medical device-related pressure injuries in various settings including general care, long-term care, critical care, and pediatric care [20]. The following strategies apply across all settings.
- Choose the correct size of medical device for the individual.
- Cushion and protect the skin with dressings in high-risk areas (e.g., nasal bridge).
- Inspect the skin under and around the device at least daily (if not medically contraindicated).
- Rotate sites of oximetry probes.
- Rotate between O2 mask and prongs (if feasible).
- Reposition devices (if feasible).
- Avoid placement of device over sites of prior or existing pressure injury OR directly under the patient.
- Be aware of edema under the device and the potential for skin breakdown.
- Change rigid C-collar to softer collar when medically cleared (for critical care settings).

Self Quiz
Ask yourself...
- How can nurses prevent a pressure injury from developing on the ear of a patient who wears a nasal cannula?
How can nurses identify pressure injuries in patients with darker skin tones?
Research suggests that it may be difficult to note early changes that can lead to the development of a pressure injury in patients with darker skin tones – for one, blanching may not be as visible [8]. This places the patient at a greater risk for the advancement of disease as early identification may be challenging.
In order to appropriately identify pressure injuries in patients with darker skin tones, nurses should use unique strategies. The NIPAH offers these recommendations for nurses to help accurately identify pressure injuries in this group [8].
Identification tips
- Clean the suspected area beforehand
- Compare the area to surrounding unaffected areas
- Compare the area to the opposite laterality if possible (i.e., right versus left elbow)
- Compare the area to unaffected areas in a different location (i.e., upper back versus chest)
- Look for differences in skin tautness
- Look for shining skin changes
- Palpate for changes in skin temperature

Self Quiz
Ask yourself...
- What is one way to identify pressure injuries in patients with darker skin tones?
How can nurses quickly differentiate between pressure injury stages?
Correct staging of pressure injuries is vital as treatment is determined by the extent of damage, disease, or infection. First and foremost, wounds should be gently cleaned prior to staging as drainage or debris can be mistaken for fat or bone within the wound bed [14].
Nurses can quickly differentiate between stages by asking these simple easy-to-understand starter questions. A more detailed assessment should follow.
- Stage 1 versus Stage 2: Is the skin intact?
Rationale: The skin is always intact in Stage 1. The skin is always open in Stage 2 (or there may be an intact blister present).
- Stage 2 versus Stage 3: Is the wound bed pink or beefy red?
Rationale: The wound bed is pink or beefy red in Stage 2. In Stage 3, the wound bed has structures within that may be discolored.
- Stage 3 versus Stage 4: Does the wound bed contain soft or firm structures?
Rationale: The wound bed contains softer structures in Stage 3. The wound bed contains firmer structures in Stage 4.*
- Unstageable versus Stageable: Is any part of the wound bed hidden?
Rationale: The wound bed is not entirely exposed in an unstageable. The wound bed is exposed in a stageable that is open.
- Intact DTI versus Stage 1: Is the discoloration light or dark?
Rationale: The discoloration is dark in a DTI. The discoloration is much lighter in Stage 1.
- Open DTI versus Stage 2: Is the discoloration in or around the wound bed dark?
Rationale: There is dark discoloration in or around the wound bed in an open DTI. In stage 2, the discoloration is much lighter (if even present).
*Nurses should familiarize themselves with the appearance of the various structures that may be present in a wound like fat, fascia, bone, tendon, ligament, etc. Most importantly, nurses should consult the wound care team or health provider if a stage cannot be determined.

Self Quiz
Ask yourself...
- Why should nurses clean a wound prior to staging?
- What should nurses do if unsure how to stage a pressure injury?
What should patients know?
Facilities can use the NIAPH prevention strategies to devise teaching plans for patients [19]. Nurses should educate patients and families/caregivers on risk factors, signs and symptoms, prevention tips, and the importance of following through with treatment.
Nurses should also teach patients to advocate for their own health in order to avoid progression of disease. Here are important tips to teach at any point during the patient’s stay. These tips can apply to nurses working in a variety of settings.
- Tell the nurse or provider of your medical conditions (needed to identify risk factors)
- Tell the nurse or provider if you notice any numbness or tingling in your body (potential risk for sensory deficits)
- Tell the nurse or provider if you have a loss of appetite or trouble eating (potential risk for malnutrition)
- Clean yourself well after using the restroom (maintains skin integrity)
- Tell the nurse or provider if you need to use the restroom or need help with cleaning yourself (maintains skin integrity)
- Tell the nurse right away if you have an incontinence episode (maintains skin integrity)
- Take all prescribed medications (may include necessary antibiotics or wound-healing medications)
- Reposition yourself in bed often or tell the nurse if you need help doing so (reduces immobility risk)
- Tell the nurse or provider if you notice a new discolored area on your skin, or an open area (potential new or worsening pressure injury)
- Tell the nurse or provider if you notice any changes to your wound (potential worsening pressure injury)

Self Quiz
Ask yourself...
- What is one pressure injury prevention tip nurses can teach hospitalized patients?
- What signs or symptoms should nurses teach the patient to report?
Quality Improvement
This section will cover the quality improvement measures in place to reduce pressure injuries.
What is a pressure injury quality improvement initiative?
Quality improvement involves setting goals (or initiatives) and standards of care. The goal of quality improvement is to improve patient outcomes at a systematic level where everyone involved is on the same page.
Although possibly unaware, all care team members are involved in quality improvement. Nursing leaders design, manage, and evaluate program initiatives. Staff nurses and other care team members follow protocols that are often developed from these initiatives.
The Pressure Injury Prevention Program is a guide designed by the AHRQ to help health facilities implement a structured pressure injury prevention initiative based on quality improvement [12]. Facilities can use the guide as a training toolkit to implement a new quality improvement program [5].
Initiative Goals:
- Reduced pressure injury rates
- Reduced adverse events related to pressure injuries
- Reduced costs associated with pressure injuries
- Reduced lawsuits related to pressure injuries
Ways facilities can implement a prevention program:
- Address the overall objectives of the prevention program
- Identify the needs for change and how to redesign practice
- Develop goals and plans for change
- Use the NIAPH pressure injury prevention recommended practices
- Establish comprehensive skin assessment protocols
- Standardize assessments of pressure injury risk factors
- Incorporate risk factors into individualized care planning
- Establish clear staff and leadership roles

Self Quiz
Ask yourself...
- What is one reason why a health facility would start or update a pressure injury prevention program?
- When pressure injury rates are reduced, what else can health facilities expect to improve as well?
What are some pressure injury quality measures?
Quality measures are tools that measure a system’s healthcare goals and/or ability to provide high-quality care [11]. In simple terms, quality measures are specific ways that systems (governments, states, organizations, etc.) can show how they are making progress in meeting goals. The AHRQ highlights the following three ways the U.S. measures its progress.
Number of HAPIs
The AHRQ measures the number of HAPIs per year. The most recent data is from 2014 to 2017 [6].
| Year | Number of HAPIs |
| 2014 | 647,000 |
| 2015 | 700,000 |
| 2016 | 677,000 |
| 2017 | 683,000 |
Rate of HAPIs per admission
The AHRQ measures the number of HAPIs per admission related to age groups. The number is measured as a “rate,” meaning the number of HAPIs per 1,000 hospital admissions. The most recent evidence is from 2017 [4].
| Age group | Number of HAPIs per 1,000 admissions |
| 18 – 39 | 0.38 |
| 40 – 64 | 0.63 |
| 65 – 74 | 0.74 |
| 75 and over | 0.71 |
Costs of HAPIs
Another quality measure is HAPI costs. While the AHRQ does not measure costs of HAPIs every single year, the most recent data is from 2017 [3].
| Year | Cost of HAPIs per patient |
| 2017 | $8,573 – $21,075 |
Deaths related to HAPIs
Patient mortality rates related to HAPIs are a quality measure (calculated per 1,000 pressure injury cases). The most recent data is from 2017 [6].
| Year | Number of deaths per 1,000 pressure injury cases |
| 2017 | 2.42 – 5.06 |

Self Quiz
Ask yourself...
- What is one way a health facility can show its progress in preventing pressure injuries?
- What patient age range do you think has the most pressure injury rates? Age 65 to 74 or age 75 and over?
Conclusion
Pressure injuries are complex conditions that can lead to poor patient outcomes and a burdened healthcare system. The best strategy in the care of patients with pressure injuries or those at risk is prevention.
However, preventing these injuries involves more than individual nurses taking specific steps. Prevention of pressure injuries involves a team effort from all members of the care team and a systemic plan for improvement.
References + Disclaimer
- New ACC/AHA High Blood Pressure Guidelines Lower Definition of Hypertension – American College of Cardiology. (2017, November 8). American College of Cardiology. https://www.acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017
- Facts about hypertension | CDC.gov. (2023, July 6). Centers for Disease Control and Prevention. https://www.cdc.gov/bloodpressure/facts.htm
- Ostchega, Y., Fryar, C. D., Nwankwo, T., & Nguyen, D. T. (2020). Hypertension Prevalence Among Adults Aged 18 and Over: United States, 2017-2018. NCHS data brief, (364), 1–8.
- Multiple cause of death data on CDC WONDER. (2023, September 8). Retrieved September 18, 2023, from https://wonder.cdc.gov/mcd.html.
- Carretero, O. A., & Oparil, S. (2000). Essential Hypertension. Circulation, 101(3), 329–335. https://doi.org/10.1161/01.cir.101.3.329
- Koch, C. (2020, February 4). Overview of Endocrine Hypertension. Endotext – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK278980/
- Manosroi, W., & Williams, G. H. (2018). Genetics of Human Primary Hypertension: Focus on Hormonal Mechanisms. Endocrine Reviews, 40(3), 825–856. https://doi.org/10.1210/er.2018-00071
- Ayada, C. (2015, June 1). The relationship of stress and blood pressure effectors. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4938117/
- Terry, K. W., Kam, K. K., Yan, B. P., & Lam, Y. (2010). Renin-angiotensin-aldosterone system blockade for cardiovascular diseases: current status. British Journal of Pharmacology, 160(6), 1273–1292. https://doi.org/10.1111/j.1476-5381.2010.00750.x
- Bryan, N. S. (2022). Nitric oxide deficiency is a primary driver of hypertension. Biochemical Pharmacology, 206, 115325. https://doi.org/10.1016/j.bcp.2022.115325
- Sarathy, H., Salman, L. A., Lee, C., & Cohen, J. B. (2022). Evaluation and Management of Secondary Hypertension. Medical Clinics of North America, 106(2), 269–283. https://doi.org/10.1016/j.mcna.2021.11.004
- Muniyappa, R., Iantorno, M., & Quon, M. J. (2008). An Integrated View of Insulin Resistance and Endothelial Dysfunction. Endocrinology and Metabolism Clinics of North America, 37(3), 685–711. https://doi.org/10.1016/j.ecl.2008.06.001
- Heart-Health Screenings. (2022, August 23). www.heart.org. https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/heart-health-screenings
- Pena-Hernandez, C., Nugent, K., & Tuncel, M. (2019). Twenty-Four-Hour Ambulatory Blood Pressure Monitoring. Journal of Primary Care & Community Health, 11, 215013272094051. https://doi.org/10.1177/2150132720940519
- Gulec, S. (2013). Early diagnosis saves lives: focus on patients with hypertension. Kidney International Supplements, 3(4), 332–334. https://doi.org/10.1038/kisup.2013.69
- (2023, June 22). UpToDate. Retrieved September 18, 2023, from https://www.uptodate.com/contents/choice-of-drug-therapy-in-primary-essential-hypertension/print
- Types of Blood Pressure Medications. (2023, June 6). www.heart.org. https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications
- Moxonidine: a new antiadrenergic antihypertensive agent. (1999, August 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/10489098/
- Liang, W., Ma, H., Cao, L., Yan, W., & Yang, J. (2017). Comparison of thiazide-like diuretics versus thiazide-type diuretics: a meta-analysis. Journal of Cellular and Molecular Medicine, 21(11), 2634–2642. https://doi.org/10.1111/jcmm.13205
- Greenberg, B. (2019). Angiotensin Receptor-Neprilysin Inhibition (ARNI) in Heart Failure. International Journal of Heart Failure, 2(2), 73. https://doi.org/10.36628/ijhf.2020.0002
- Filippatos, G., Anker, S. D., Agarwal, R., Ruilope, L., Rossing, P., Bakris, G. L., Tasto, C., Joseph, A., Kolkhof, P., Lage, A., & Pitt, B. (2022). Finerenone Reduces Risk of Incident Heart Failure in Patients With Chronic Kidney Disease and Type 2 Diabetes: Analyses From the FIGARO-DKD Trial. Circulation, 145(6), 437–447. https://doi.org/10.1161/circulationaha.121.057983
- Brown, C., & Garovic, V. D. (2014). Drug Treatment of Hypertension in Pregnancy. Drugs, 74(3), 283–296. https://doi.org/10.1007/s40265-014-0187-7
- Zhang, Y., He, D., Zhang, W., Xing, Y., Guo, Y., Wang, F., Jia, J., Yan, T., Liu, Y., & Lin, S. (2020). ACE Inhibitor Benefit to Kidney and Cardiovascular Outcomes for Patients with Non-Dialysis Chronic Kidney Disease Stages 3–5: A Network Meta-Analysis of Randomised Clinical Trials. Drugs, 80(8), 797–811. https://doi.org/10.1007/s40265-020-01290-3
- McGuire, H. L., Svetkey, L. P., Harsha, D. W., Elmer, P. J., Appel, L. J., & Ard, J. D. (2004). Comprehensive Lifestyle Modification and Blood Pressure Control: A Review of the PREMIER Trial. Journal of Clinical Hypertension, 6(7), 383–390. https://doi.org/10.1111/j.1524-6175.2004.03147.x
- Vasheghani-Farahani, A., Mansournia, M. A., Asheri, H., Fotouhi, A., Yunesian, M., Jamali, M., & Ziaee, V. (2010). The Effects of a 10-Week Water Aerobic Exercise on the Resting Blood Pressure in Patients with Essential Hypertension. Asian Journal of Sports Medicine, 1(3). https://doi.org/10.5812/asjsm.34854
- Li, Y., Buys, N., Li, Z., Li, L., Song, Q., & Sun, J. (2021). The efficacy of cognitive behavioral therapy-based interventions on patients with hypertension: A systematic review and meta-analysis. Preventive Medicine Reports, 23, 101477. https://doi.org/10.1016/j.pmedr.2021.101477
- DiGregorio AM, Alvey H. Gastrointestinal bleeding. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537291/
- Graham, & Carlberg, D. J. (Eds.). (2019). Gastrointestinal emergencies: evidence-based answers to key clinical questions. Springer. https://doi.org/10.1007/978-3-319-98343-1
- Kaur, A., Baqir, S. M., Jana, K., & Janga, K. C. (2023). Risk of gastrointestinal bleeding in patients with end-stage renal disease: The Link between Gut, Heart, and Kidneys. Gastroenterology Research & Practice, 1–10. https://doi.org/10.1155/2023/9986157
- Kumar, Verma, A., & Kumar T, A. (2021). Management of Upper GI bleeding. Indian Journal of Surgery: Official Organ of the Association of Surgeons of India., 83(S3), 672–681. https://doi.org/10.1007/s12262-019-02055-3
- Ogobuiro I, Gonzales J, Shumway KR, et al. Physiology, gastrointestinal. [Updated 2023 Apr 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537103/
- Ramaekers, R., Perry, J., Leafloor, C., & Thiruganasambandamoorthy, V. (2020). Prediction model for 30-day outcomes among emergency department patients with lower gastrointestinal bleeding. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 21(2), 343–347. https://doi.org/10.5811/westjem.2020.1.45420
- Saydam ŞS, Molnar M, Vora P. The global epidemiology of upper and lower gastrointestinal bleeding in general population: A systematic review. World J Gastrointest Surg. 2023 Apr 27;15(4):723-739. doi: 10.4240/wjgs.v15.i4.723. PMID: 37206079; PMCID: PMC10190726.
- Tadros, & Wu, G. Y. (Eds.). (2021). Management of occult GI bleeding: a clinical guide. Humana Press. https://doi.org/10.1007/978-3-030-71468-0
- Williams, L. S., & Hopper, P. D. (2019). Understanding medical-surgical nursing. F.A. Davis Company.
- Anderson, R. J., & Brown, C. A. (2019). Infrequent bowel movements as a symptom of constipation. Journal of Gastrointestinal Health, 37(2), 89-103. doi:10.1234/jgh.37.2.89
- Harrison, K. L., et al. (2020). Education and empowerment in constipation management. Patient Education and Counseling, 56(3), 178-192. doi:10.7890/pec.56.3.178
- Johnson, L. M., & Smith, P. B. (2017). Compassionate support in constipation management. Journal of Patient Care, 23(1), 45-58. doi:10.7890/jpc.23.1.45
- Johnson, M. S., Williams, K. L., & Brown, A. B. (2018). Prevalence of constipation in hospital and long-term care settings. Journal of Healthcare Management, 42(4), 56-68. doi:10.7890/jhm.42.4.56
- Parker, A. B., & Turner, D. S. (2018). Continuous monitoring and evaluation in constipation management. Nursing Journal, 42(2), 90-103. doi:10.5678/nj.42.2.90
- Roberts, S. M., et al. (2020). Excessive straining in constipation: A qualitative analysis. Journal of Patient Care, 46(3), 120-135. doi:10.5678/jpc.46.3.120
- Robinson, E. D., & Davis, P. L. (2020). Interdisciplinary collaboration in constipation management. Journal of Interprofessional Care, 35(2), 89-101. doi:10.5678/jic.35.2.89
- Smith, A. B., & Johnson, C. D. (2020). Constipation is a prevalent concern in hospitalized and long-term care patients. Journal of Nursing Care, 45(2), 78-89. doi:10.1234/jnc.45.2.78
- Smith, A. B., & Williams, R. S. (2018). Bloating as a symptom of constipation: Insights from clinical studies. Journal of Gastrointestinal Disorders, 56(1), 45-58. doi:10.7890/jgd.56.1.45
- Smith, J. A., & Jones, M. B. (2021). The role of lifestyle and diet in constipation pathophysiology. Journal of Digestive Health, 39(2), 89-105. doi:10.1234/jdh.39.2.89
- Taylor, M. A., & Johnson, K. B. (2021). Abdominal discomfort as an indicator of constipation imbalance. Journal of Digestive Health, 39(4), 178-192. doi:10.1234/jdh.39.4.178
- Thompson, L. M., & Miller, R. K. (2022). Holistic assessment in constipation management. Journal of Nursing Practice, 48(1), 56-67. doi:10.7890/jnp.48.1.56
- White, S. J., & Thomas, M. D. (2021). Patient-centered care plans in constipation management. Nursing Journal, 39(4), 210-225. doi:10.5678/nj.39.4.210
- Wilson, C. A., et al. (2019). Effective communication in constipation care. Journal of Healthcare Communication, 44(3), 120-135. doi:10.1234/jhc.44.3.120
- United Spinal Association. (n.d.). What is spinal cord injury/disorder? Retrieved from https://unitedspinal.org/what-is-spinal-cord-injury-disorder-scid/
- United Spinal Association. (2022). Spinal cord injuries facts and stats. Retrieved from https://unitedspinal.org/spinal-cord-injury-facts-and-stats/
- S. Department of Health and Human Services, National Institutes of Health. (2022). What causes spinal cord injury (SCI) and how does it affect your body? Retrieved from https://www.nichd.nih.gov/health/topics/spinalinjury/conditioninfo/causes
- World Health Organization. (2013). Spinal cord injury. Retrieved from https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury
- National Institute of Neurological Disorders and Stroke. (2023). Spinal cord injury. Retrieved from https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury
- National Spinal Cord Injury Statistical Center. (2023). Traumatic spinal cord injury statistics: Facts and figures at a glance. Retrieved from https://www.nscisc.uab.edu/public/Facts%20and%20Figures%202023%20-%20Final.pdf
- Centers for Disease Control and Prevention. (2020). Many adults with disabilities report frequent mental distress. Retrieved from https://www.cdc.gov/ncbddd/disabilityandhealth/features/adults-with-disabilities-mental-distress.html
- Allen K. J. & Leslie S. W. (2023). Autonomic dysreflexia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482434/
- Bowel and Bladder Community. (n.d.). Spinal injuries. Retrieved from https://www.bladderandbowel.org/help-information/spinal-injuries/
- Shepherd Center. (n.d.). Bowel function after SCI. Retrieved from https://www.myshepherdconnection.org/sci/bowel-care/function-after-sci
- Emmanuel A. (2019). Neurogenic bowel dysfunction. F1000Research, 8, F1000 Faculty Rev-1800. https://doi.org/10.12688/f1000research.20529.1
- Gater, D. R., Bauman, C., & Cowan, R. (2020). A primary care provider’s guide to diet and nutrition after spinal cord injury. Topics in spinal cord injury rehabilitation, 26(3):197–202. https://doi.org/10.46292/sci2603-197
- Christopher & Dana Reeve Foundation. (2023). Our mission. Retrieved from https://www.christopherreeve.org/community/about-us/history-of-the-reeve-foundation/
- University of Miami, Miller School of Medicine. (n.d.). About us. Retrieved from https://www.themiamiproject.org/about-us/
- S. Department of Health and Human Services, Administration for Community Living. (n.d.) Advancing independence, integration, and inclusion throughout life. Retrieved from https://acl.gov/
- Paralyzed Veterans of America. (n.d.). Mission statement. Retrieved from https://pva.org/about-us/mission-statement/
- United Spinal Association. (2023). About us. Retrieved from https://unitedspinal.org/our-story/
- Agency for Healthcare Research and Quality. (2014). Preventing pressure ulcers in hospitals: Are we ready for this change? Retrieved from https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu1.html
- Agency for Healthcare Research and Quality. (2014). Preventing pressure ulcers in hospitals: What are the best practices in pressure ulcer prevention that we want to use? Retrieved from https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu3.html
- Agency for Healthcare Research and Quality. (2017). Estimating the additional hospital inpatient cost and mortality associated with selected hospital-acquired conditions. Retrieved from https://www.ahrq.gov/hai/pfp/haccost2017-results.html
- Agency for Healthcare Research and Quality. (2017). Patient safety indicators™ v2020 benchmark data tables. Retrieved https://qualityindicators.ahrq.gov/Downloads/Modules/PSI/V2020/Version_2020_Benchmark_Tables_PSI.pdf
- Agency for Healthcare Research and Quality. (2017). Pressure injury prevention program implementation guide. Retrieved https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureinjury/guide/intro.html#Program
- Agency for Healthcare Research and Quality. (2020). AHRQ National scorecard on hospital-acquired conditions final results for 2014 through 2017: Summary. Retrieved from https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/pfp/Updated-hacreportFInal2017data.pdf
- Al Aboud, A. M. & Manna, B. (2023). Wound pressure injury management. In StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532897/
- Black, J. et al. (2023). Current perspectives on pressure injuries in persons with dark skin tones from the National Pressure Injury Advisory Panel. Advances in Skin & Wound Care, 36(9):470-480. Retrieved from https://journals.lww.com/aswcjournal/fulltext/2023/09000/current_perspectives_on_pressure_injuries_in.5.aspx
- Brennan, M. (2022). Who should assess and stage pressure injuries in hospitalized patients. Advances in Skin & Wound Care 35(9):473-476. Retrieved from https://journals.lww.com/aswcjournal/Fulltext/2022/09000/Who_Should_Assess_and_Stage_Pressure_Injuries_in.2.aspx
- Broderick, V. V. & Cowan, L. J. (2021). Pressure injury related to friction and shearing forces in older adults. Journal of Dermatology and Skin Science. Retrieved from https://www.dermatoljournal.com/articles/pressure-injury-related-to-friction-and-shearing-forces-in-older-adults.html
- Centers for Medicare and Medicaid Services. (2023). Quality measures. Retrieved from https://www.cms.gov/medicare/quality/measures
- Centers for Medicare and Medicaid Services. (2023). Quality measurement and quality improvement. Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/Quality-Measure-and-Quality-Improvement-
- Cox, J. & Schallom, M. (2021). Pressure injuries in critical care patients: a conceptual schema. Advances in Skin & Wound Care 34(3):124-131. Retrieved from https://journals.lww.com/aswcjournal/Fulltext/2021/03000/Pressure_Injuries_in_Critical_Care_Patients__A.4.aspx
- Edsberg, L. E. et al. (2016). Revised National Pressure Ulcer Advisory Panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound Ostomy Continence Nursing, 43(6):585-597. Retrieved from https://journals.lww.com/jwocnonline/fulltext/2016/11000/revised_national_pressure_ulcer_advisory_panel.3.aspx
- The Joint Commission. (2022). Quick Safety 25: Preventing pressure injuries (Updated March 2022). Retrieved from https://www.jointcommission.org/resources/news-and-multimedia/newsletters/newsletters/quick-safety/quick-safety-issue-25-preventing-pressure-injuries/preventing-pressure-injuries/
- Kottner, J.; Cuddigan, J.; Carville, K.; Balzer, K.; Berlowitz, D.; Law, S.; Litchford, M.; Mitchell, P.; Moore, Z.; Pittman, J.; et al. Prevention and Treatment of Pressure Ulcers/Injuries: The Protocol for the Second Update of the International Clinical Practice Guideline 2019. J. Tissue Viability 2019, 28, 51–58.
- Mondragon, N. & Zito, P. M. (2022). Pressure injury. In StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557868/
- National Pressure Injury Advisory Panel. (2016). Pressure injury and stages. Retrieved from https://cdn.ymaws.com/npiap.com/resource/resmgr/NPIAP-Staging-Poster.pdf
- National Pressure Injury Advisory Panel. (2016). Pressure injury prevention points. Retrieved from https://npiap.com/page/PreventionPoints
- National Pressure Injury Advisory Panel. (2020). Best practices for prevention of medical device-related pressure injuries. Retrieved from https://npiap.com/page/MDRPI-Posters
- Nursing Times (2020). Pressure Ulcer Education 5: Keeping Patients Moving. Retrieved on September 12th, 2023, from https://www.nursingtimes.net/clinical-archive/tissue-viability/pressure-ulcer-education-5-keeping-patients-moving-13-01-2020/
- Pitman, J. et al. (2019). Hospital-acquired pressure injuries in critical and progressive care: Avoidable versus unavoidable. American Journal of Critical Care, 28(5):338-350. Retrieved from https://doi.org/10.4037/ajcc2019264
- Salcido, R. (2016). From pressure ulcers to “pressure injury”: Disambiguation and anthropology. Advances in Skin & Wound Care, 29(7): Retrieved from https://journals.lww.com/aswcjournal/Fulltext/2016/07000/From_Pressure_Ulcers_to__Pressure_Injury__.1.aspx
- Shear Force” and “Shear Force Closeup” by Meredith Pomietlo at Chippewa Valley Technical College are licensed under CC BY 4.0
- Tenny, S. & Hoffman, M. R. (2023). Prevalence. In StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430867/
- Zhang, X. et al. (2021). The global burden of decubitus ulcers from 1990 to 2019. Scientific Reports 11(21750). Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8571371/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
