Course
New Mexico Non-Cancer Pain Management
Course Highlights
- In this New Mexico Non-Cancer Pain Management course, we will learn about commonly prescribed opioids for pain management and understand their side effects, indications of use, and safe prescribing practices.
- You’ll also learn common opioids used to treat addiction disorders.
- You’ll leave this course with a broader understanding of specific controlled substances regulations for New Mexico APRNs.
About
Pharmacology Contact Hours Awarded: 5
Course By:
Sadia A
MPH, MSN, WHNP-BC
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Pain is complex and subjective. The experience of pain can significantly impact an individual’s quality of life. According to the National Institute of Health (NIH) (40), pain is the most common complaint in a primary care office, with 20% of all patients reporting pain. Chronic pain is the leading cause of disability, and effective pain management is crucial to health and well-being, particularly when it improves functional ability.
Effective pain treatment starts with a comprehensive, empathic assessment and a desire to listen and understand. Nurse Practitioners are well-positioned to fill a vital role in providing comprehensive and empathic patient care, including pain management (23).
While the incidence of chronic pain has remained a significant problem, how clinicians manage pain has significantly changed in the last decade, primarily due to the opioid epidemic. This course aims to discuss pain and the assessment of pain, federal guidelines for prescribing, the opioid epidemic, addiction and diversion, and recommendations for managing pain.
Definition of Pain
Understanding the definition of pain, differentiating between various types of pain, and recognizing the descriptors patients use to communicate their pain experiences are essential for Nurse practitioners involved in pain management. By understanding the medical definition of pain and how individuals may communicate it, nurse practitioners can differentiate varying types of pain to target assessment.
According to the International Association for the Study of Pain (27), pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or terms of described such in damage.”
The IASP, in July 2020, expanded its definition of pain to include context further. Their expansion is summarized below:
- Pain is a personal experience influenced by biological, psychological, and social factors.
- Pain cannot be inferred solely from activity in sensory neurons.
- Individuals learn the concept of pain through their life experiences.
- A person’s report of an experience in pain should be respected.
- Pain usually serves an adaptive role but may adversely affect function and social and psychological well-being.
- The inability to communicate does not negate the possibility of the experience of pain.
(27)

Self-Quiz
Ask Yourself...
- How can changes to the definition of pain affect your practice?
- Discuss how you manage appointment times, knowing that 20% of your scheduled patients may seek pain treatment.
- How does the approach to pain management change in the presence of a person with a disability?
Types of Pain:
Pain originates from different mechanisms, causes, and areas of the body. As a nurse practitioner, understanding the type of pain a patient is experiencing is essential for several reasons (23):
- Determining an accurate diagnosis. This kind of pain can provide valuable clues to the underlying cause or condition.
- Creating a treatment plan. Different types of pain respond better to specific treatments or interventions.
- Developing patient education. A nurse practitioner can provide targeted education to patients about their condition, why they may experience the pain as they do, its causes, and treatment options. Improving the patient’s knowledge and control over their condition improves outcomes.
Acute Pain
Acute pain is typically short-lived and is a protective response to an injury or illness. Patients are usually able to identify the cause. This type of pain resolves as the underlying condition improves or heals (12).
Chronic Pain
Chronic pain is diagnosed when it continues beyond the expected healing time. Pain is defined as chronic when it persists for longer than three months. It may result from an underlying disease or injury or develop without a clear cause.
Chronic pain often significantly impacts a person’s physical and emotional well-being, requiring long-term management strategies. The prolonged experience of chronic pain usually indicates a central nervous system component of pain that may require additional treatment. Patients with centralized pain often experience allodynia or hyperalgesia (12).
Allodynia is pain evoked by a stimulus that usually does not cause pain, such as a light touch. Hyperalgesia is the effect of a heightened pain response to a stimulus that usually evokes pain (12).
Nociceptive Pain
Nociceptive pain arises from activating peripheral nociceptors, specialized nerve endings that respond to noxious stimuli. This type of pain is typically associated with tissue damage or inflammation and is further classified into somatic and visceral pain subtypes.
Somatic pain is the most common type and occurs in muscles, skin, or bones; patients may describe it as sharp, aching, stiffness, or throbbing.
Visceral pain occurs in the internal organs, such as indigestion or bowel spasms. It is more vague than somatic pain; patients may describe it as deep, gnawing, twisting, or dull (12).
Neuropathic Pain
Neuropathic pain is a lesion or disease of the somatosensory nervous system. Examples include trigeminal neuralgia, painful polyneuropathy, postherpetic neuralgia, and central poststroke pain (10).
Neuropathic pain may be ongoing, intermittent, or spontaneous pain. Patients often describe neuropathic pain as burning, prickling, or squeezing quality. Neuropathic pain is a common chronic pain.
Patients commonly describe allodynia and hyperalgesia as part of their chronic pain experience (10).
Affective Pain
Affective descriptors reflect the emotional aspects of pain and include terms like distressing, unbearable, depressing, or frightening. These descriptors provide insights into the emotional impact of pain on an individual’s well-being (12).

Self-Quiz
Ask Yourself...
- How can nurse practitioners effectively elicit patient descriptors to accurately assess the type of pain the patient is experiencing?
- Expand on how pain descriptors can guide interventions even if the cause is not yet determined.
- What strategies ensure patients feel comfortable describing their pain, particularly regarding subjective elements such as quality and location?
Case Study
Mary Adams is a licensed practical nurse who has just relocated to town. Mary will be the utilization review nurse at a local long-term care facility. Mary was diagnosed with Postherpetic Neuralgia last year, and she is happy that her new job will have her mostly doing desk work and not providing direct patient care as she had been before the relocation. Mary was having difficulty at work at her previous employer due to pain. She called into work several times, and before leaving, Mary’s supervisor had counseled her because of her absences.
Mary wants to establish primary care immediately because she needs ongoing pain treatment. She is hopeful that, with her new job and pain under control, she will be able to continue a successful career in nursing.
When Mary called the primary care office, she specifically requested a nurse practitioner as her primary care provider because she believes that nurse practitioners tend to spend more time with their patients.

Assessment
The assessment effectively determines the type of treatment needed, the options for treatment, and whether the patient may be at risk for opioid dependence. Since we know that chronic pain can lead to disability and pain has a high potential to negatively affect the patient’s ability to work or otherwise, be productive, perform self-care, and potentially impact family or caregivers, it is imperative to approach the assessment with curiosity and empathy.
This approach will ensure a thorough review of pain and research on pain management options. Compassion and support alone can improve patient outcomes related to pain management (23).
Record Review
Regardless of familiarity with the patient, reviewing the patient’s treatment records is essential, as the ability to recall details is unreliable. Reviewing the records can help identify subtle changes in pain description and site, the patient’s story around pain, failed modalities, side effects, and the need for education, all impacting further treatment (23).
Research beforehand the patient’s current prescription and whether or not the patient has achieved the maximum dosage of the medication. Analysis of the patient’s past prescription could reveal a documented failed therapy even though the patient did not receive the maximum dose (23).
A review of documented allergens may indicate an allergy to pain medication. Discuss with the patient the specific response to the drug to determine if it is a true allergy, such as hives or anaphylaxis, or if the response may have been a side effect, such as nausea and vomiting.
Research whether the patient tried any non-medication modalities for pain, such as physical therapy (PT), occupational therapy (OT), or Cognitive Behavioral Therapy (CBT). Note any non-medication modalities documented as failed therapies.
The presence of any failed therapies should prompt further discussion with the patient, family, or caregiver about the experience. The incompletion of therapy should not be considered failed therapy. Explore further if the patient abandoned appointments.
Case Study:
You review the schedule for the week, and there are three new patient appointments. One is Mary Adams. The interdisciplinary team requested and received Mary’s treatment records from her previous primary care provider.
You make 15 minutes available to review Mary’s records and the questionnaire Mary filled out for her upcoming appointment. You see that Mary has been diagnosed with Postherpetic Neuralgia and note her current treatment regimen, which she stated was ineffective.
You write down questions you will want to ask Mary. You do not see evidence of non-medication modalities or allergies to pain medication.

Self-Quiz
Ask Yourself...
- What potential risks or complications can arise from neglecting to conduct a thorough chart review before initiating a pain management assessment?
- In your experience, what evidence supports reviewing known patient records?
- What is an alternative to reviewing past treatment if records are not available?
Pain Assessment
To physically assess pain, several acronyms help explore all the aspects of the patient’s experience. Acronyms commonly used to assess pain are SOCRATES, OLDCARTS, and COLDERAS. These pain assessment acronyms are also helpful in determining treatment since they include a character and duration of pain assessment (23).
| O-Onset | S-Site | C-Character |
| L-Location | O-Onset | O-Onset |
| D-Duration | C-Character | L-Location |
| C-Character | R-Radiate | D-Duration |
| A-Alleviating | A-Associated symptoms | E-Exacerbating symptoms |
| R-Radiating, relieving | T-Time/Duration | R-Relieving, radiating |
| T-Temporal patterns (frequency) | E-Exacerbating | A-Associated symptoms |
| S-Symptoms | S-Severity | S-Severity of illness |
Inquire where the patient is feeling pain. The patient may have multiple areas and types of pain. Each type and location must be explored and assessed. Unless the pain is from a localized injury, a body diagram map, as seen below, is helpful to document, inform, and communicate locations and types of pain.
In cases of Fibromyalgia, rheumatoid arthritis, or other centralized or widespread pain, it is vital to inquire about radiating pain. The patient with chronic pain could be experiencing acute pain or a new pain site, such as osteoarthritis, that may need further evaluation and treatment (23).

(42)
Inquire with the patient how long their pain has been present and any associated or known causative factors. Pain experienced longer than three months defines chronic versus acute pain. Chronic pain means that the pain is centralized or a function of the Central Nervous system, which should guide treatment decisions.
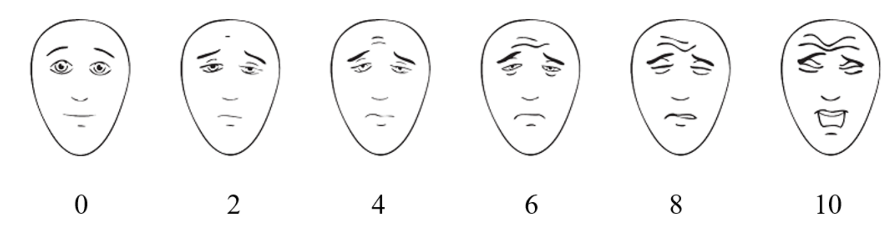
To help guide treatment, ask the patient to describe their pain. The description helps identify what type of pain the patient is experiencing: Allodynia and hyperalgesia indicate centralized pain; sharp, shooting pain could indicate neuropathic pain. Have the patient rate their pain. There are various tools, as shown below, for pain rating depending on the patient’s ability to communicate. Not using the pain rating number alone is imperative.
Ask the patient to compare the severity of pain to a previous experience. For example, a 1/10 may be experienced as a bumped knee or bruise, whereas a 10/10 is experienced on the level of a kidney stone or childbirth (23).
Besides the 0-10 rating scale and depending on the patient’s needs, several pain rating scales are appropriate. They are listed below.
The 0-5 and Faces scales may be used for all adult patients and are especially effective for patients experiencing confusion.
(25)
The Defense and Veterans Pain Rating Scale (DVPRS) is a five-item tool that assesses the impact of pain on sleep, mood, stress, and activity levels (20).
For patients unable to self-report pain, such as those intubated in the ICU or late-stage neurological diseases, the FLACC scale is practical.
The FLACC scale was initially created to assess pain in infants. Note: The patient need not cry to be rated 10/10.
| Behavior | 0 | 1 | 2 |
| Face | No particular expression or smile | Occasional grimace or frown, withdrawn, disinterested | Frequent or constant quivering chin, clenched jaw |
| Legs | Normal position or relaxed | Uneasy, restless, tense | Kicking or legs drawn |
| Activity | Lying quietly, in a normal position, or relaxed | Squirming, shifting back and forth, tense | Arched, rigid, or jerking |
| Cry | No cry wake or asleep | Moans or whimpers: occasional complaints | Crying steadily, screams, sobs, frequent complaints |
| Consolability | Content, relaxed | Distractable, reassured by touching, hugging, or being talked to | Difficult to console or comfort |
(21).
Assess contributors to pain such as insomnia, stress, exercise, diet, and any comorbid conditions. Limited access to care, socioeconomic status, and local culture also contribute to the patient’s experience of pain (23). Most patients have limited opportunity to discuss these issues, and though challenging to bring up, it is compassionate and supportive care. A referral to social work or another agency may be helpful if you cannot explore it fully.
Assess for substance abuse disorders, especially among male, younger, less educated, or unemployed adults. Substance abuse disorders increase the likelihood of misuse disorder and include alcohol, tobacco, cannabis, cocaine, and heroin (29).
Inquire as to what changes in function the pain has caused. One question to ask is, “Were it not for pain, what would you be doing?”
As seen below, a Pain, Enjoyment, and General Activity (PEG) three-question scale, which focuses on function and quality of life, may help determine the severity of pain and the effect of treatment over time.
| What number best describes your pain on average in the past week? 0-10 |
| What number best describes how, in the past week, pain has interfered with your enjoyment of life? 0-10 |
| What number determines how, in the past week, pain has interfered with your general activity? 0-10 |
(21)
Assess family history, mental health disorders, chronic pain, or substance abuse disorders. Each familial aspect puts patients at higher risk for developing chronic pain (23).
Evaluate for mental health disorders the patient may be experiencing, particularly anxiety and depression.
The Patient Health Questionnaire (PHQ4) is a four-question tool for assessing depression and anxiety:
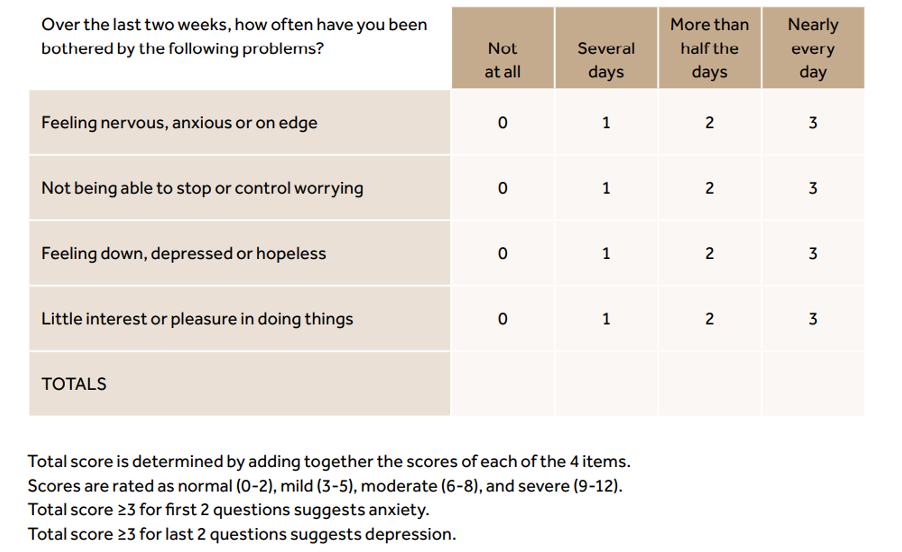
(34)
In some cases, functional MRI or imaging studies effectively determine the cause of pain and the treatment. If further assessment is needed to diagnose and treat pain, consult Neurology, Orthopedics, Palliative care, and pain specialists (23).

Self-Quiz
Ask Yourself...
- How do you assess and evaluate a patient’s pain level?
- What are the different types of pain and their management strategies?
- How do you determine the appropriate dosage of pain medications for a patient?
- How do you assess the effectiveness of pain medications in your patients?
Case Study:
You used OLDCARTS to evaluate Mary’s pain and completed a body diagram. Mary is experiencing allodynia in her back and shoulders, described as burning and tingling. It is exacerbated when she lifts, such as moving patients at the long-term care facility and, more recently, boxes from her move to the new house. Mary has also been experiencing anxiety due to fear of losing her job, the move, and her new role. She has moved closer to her family to help care for her children since she often experiences fatigue. Mary has experienced a tumultuous divorce in the last five years and feels she is still undergoing some trauma.
You saw in the chart that Mary had tried Gabapentin 300 mg BID for her pain and inquired what happened. Mary explained that her pain improved from 8/10 to 7/10 and had no side effects. Her previous care provider discontinued the medication and documented it as a failed therapy. You reviewed the minimum and maximum dosages of Gabapentin and know Mary can take up to 1800mg/day.
During the assessment, Mary also described stiffness and aching in her left knee. She gets a sharp pain when she walks more than 500 steps, and her knee is throbbing by the end of the day. Mary rated the pain a 10/10, but when she compared 10/10 to childbirth, Mary said her pain was closer to 6/10. Her moderate knee pain has reduced Mary’s ability to exercise. She used to like to take walks. Mary stated she has had knee pain for six months and has been taking Ibuprofen 3 – 4 times daily.
Since Mary’s pain is moderate, you evaluate your options of drugs for moderate to severe pain.

Self-Quiz
Ask Yourself...
- How do you adjust medication dosages for elderly patients with pain or addiction?
- How do you address the unique challenges in pain management for pediatric patients?
- What is the role of non-pharmacological interventions in pain management?
- How do you incorporate non-pharmacological interventions into your treatment plans?
Opioid Classifications and Drug Schedules
A comprehensive understanding of drug schedules and opioid classifications is essential for nurse practitioners to ensure patient safety, prevent drug misuse, and adhere to legal and regulatory requirements. Nurse practitioners with a comprehensive understanding of drug schedules and opioid classifications can effectively communicate with colleagues, ensuring accurate medication reconciliation and facilitating interdisciplinary care.
Nurse practitioners’ knowledge in facilitating discussions with pharmacists regarding opioid dosing, potential interactions, and patient education is essential (49).
Drug scheduling became mandated under the Controlled Substance Act. The Drug Enforcement Agency (DEA) Schedule of Controlled Drugs and the criteria and common drugs are listed below.
| Schedule | Criteria | Examples |
| I | No medical use; high addiction potential | Heroin, marijuana, PCP |
| II | Medical use; high addiction potential | Morphine, oxycodone, Methadone, Fentanyl, amphetamines |
| III | Medical use; high addiction potential | Hydrocodone, codeine, anabolic steroids |
| IV | Medical use, low abuse potential | Benzodiazepines, meprobamate, butorphanol, pentazocine, propoxyphene |
| V | Medical use; low abuse potential | Buprex, Phenergan with codeine |
(Pain Physician, 2008)
Listed below are drugs classified by their schedule and mechanism of action. “Agonist” indicates a drug that binds to the opioid receptor, causing pain relief and also euphoria. An agonist-antagonist indicates the drug binds to some opioid receptors but blocks others. Mixed antagonist-agonist drugs control pain but have a lower potential for abuse and dependence than agonists (7).
|
|
Schedule I |
Schedule II |
Schedule III |
Schedule IV |
Schedule V |
|
Opioid agonists |
BenzomorphineDihydromor-phone, Ketobemidine, Levomoramide, Morphine-methylsulfate, Nicocodeine, Nicomorphine, Racemoramide |
Codeine, Fentanyl, Sublimaze, Hydrocodone, Hydromorphone, Dilaudid, Meperidine, Demerol, Methadone, Morphine, Oxycodone, Endocet, Oxycontin, Percocet, Oxymorphone, Numorphan |
Buprenorphine Buprenex, Subutex, Codeine compounds, Tylenol #3, Hydrocodone compounds, Lortab, Lorcet, Tussionex, Vicodin |
Propoxyphene, Darvon, Darvocet |
Opium, Donnagel, Kapectolin |
|
Mixed Agonist -Antagonist |
|
|
BuprenorphineNaloxone, Suboxone |
Pentazocine, Naloxone, Talwin-Nx |
|
|
Stimulants |
N-methylampheta-mine 3, 4-methylenedioxy amphetamine, MDMA, Ecstacy |
Amphetamine, Adderal, Cocaine, Dextroamphetamine, Dexedrine, Methamphetamine, Desoxyn, Methylphenidate, Concerta, Metadate, Ritalin, Phenmetrazine, Fastin, Preludin |
Benapheta-mine, Didrex, Pemolin, Cylert, Phendimetra-zine, Plegine |
Diethylpropion, Tenuate, Fenfluramine, Phentermine Fastin |
1-dioxy-ephedrine-Vicks Inhaler |
|
Hallucinogen-gens, other |
Lysergic Acid Diamine LSD, marijuana, Mescaline, Peyote, Phencyclidine PCP, Psilocybin, Tetrahydro-cannabinol |
|
Dronabinol, Marinol |
|
|
|
Sedative Hypnotics |
Methylqualine, Quaalude, Gamma-hydroxy butyrate, GHB
|
Amobarbitol, Amytal, Glutethamide, Doriden, Pentobarbital, Nembutal, Secobarbital, Seconal |
Butibarbital. Butisol, Butilbital, Florecet, Florinal, Methylprylon, Noludar |
Alprazolam, Xanax, Chlordiazepoxide, Librium, Chloral betaine, Chloral hydrate, Noctec, Chlorazepam, Clonazepam, Klonopin, Clorazopate, Tranxene, Diazepam, Valium, Estazolam, Prosom, Ethchlorvynol, Placidyl, Ethinamate, Flurazepam, Dalmane, Halazepam, Paxipam, Lorazepam, Ativan, Mazindol, Sanorex, Mephobarbital, Mebaral, Meprobamate, Equanil, Methohexital, Brevital Sodium, Methyl-phenobarbital, Midazolam, Versed, Oxazepam, Serax, Paraldehyde, Paral, Phenobarbital, Luminal, Prazepam, Centrax, Temazepam, Restoril, Triazolam, Halcion, Sonata, Zolpidem, Ambien |
Diphenoxylate preparations, Lomotil |
(41)

Self-Quiz
Ask Yourself...
- What are the potential risks and benefits of using opioids for pain management?
- How can nurse practitioners effectively monitor patients on long-term opioid therapy?
- What are the potential risks and benefits of using long-acting opioids for chronic pain?
- How do you monitor patients on long-acting opioids for safety and efficacy?
Commonly Prescribed Opioids, Indications for Use, and Typical Side Effects
Opioid medications are widely used for managing moderate to severe pain. Referencing NIDA (2023), this section aims to give healthcare professionals an overview of the indications and typical side effects of commonly prescribed Schedule II opioid medications, including hydrocodone, oxycodone, morphine, Fentanyl, and hydromorphone.
Opioids are derived and manufactured in several ways. Naturally occurring opioids come directly from the opium poppy plant. Synthetic opioids are manufactured by chemically synthesizing compounds that mimic the effects of a natural opioid. Semi-synthetic is a mix of naturally occurring and man-made (35).
Understanding the variations in how an opioid is derived and manufactured is crucial in deciding the type of opioid prescribed, as potency and analgesic effects differ. Synthetic opioids are often more potent than naturally occurring opioids. Synthetic opioids have a longer half-life and slower elimination, affecting the duration of action and timing for dose adjustments. They are also associated with a higher risk of abuse and addiction (38).
Hydrocodone
Mechanism of Action and Metabolism
Hydrocodone is a Schedule II medication. It is an opioid agonist and works as an analgesic by activating mu and kappa opioid receptors located in the central nervous system and the enteric plexus of the bowel. Agonist stimulation of the opioid receptors inhibits nociceptive neurotransmitters’ release and reduces neuronal excitability (17).
Hydrocodone has the following effects:
- Produces analgesia.
- Suppresses the cough reflex at the medulla.
- Causes respiratory depression at higher doses.
Hydrocodone is indicated for treating severe pain after nonopioid therapy has failed. It is also indicated as an antitussive for nonproductive cough in adults over 18.
Available Forms
Hydrocodone immediate release (IR) reaches maximum serum concentrations in one hour with a half-life of 4 hours. Extended-release (ER) Hydrocodone reaches peak concentration at 14-16 hours and a half-life of 7 to 9 hours.
Hydrocodone is metabolized to an inactive metabolite in the liver by cytochrome P450 enzymes CYP2D6 and CYP3A4. Hydrocodone is converted to hydromorphone and is excreted renally. Plasma concentrations of hydromorphone are correlated with analgesic effects rather than hydrocodone.
Hydrocodone is formulated for oral administration into tablets, capsules, and oral solutions. Capsules and tablets should never be crushed, chewed, or dissolved. These actions convert the extended-release dose into immediate release, resulting in uncontrolled and rapid release of opioids and possible overdose.
Dosing and Monitoring
Hydrocodone IR is combined with acetaminophen or ibuprofen. The dosage range is 2.5mg to 10mg every 4 to 6 hours. If formulated with acetaminophen, the dosage is limited to 4gm/day.
Hydrocodone ER is available as tablets and capsules. Depending on the product, the dose of hydrocodone ER formulations in opioid-naïve patients is 10 to 20 mg every 12 to 24 hours.
Nurse practitioners should ensure patients discontinue all other opioids when starting the extended-release formula.
Side Effects and Contraindications
Because mu and kappa opioid receptors are in the central nervous system and enteric plexus of the bowel, the most common side effects of hydrocodone are constipation and nausea (>10%).
Other adverse effects of hydrocodone include:
- Respiratory: severe respiratory depression, shortness of breath
- Cardiovascular: hypotension, bradycardia, peripheral edema
- Neurologic: Headache, chills, anxiety, sedation, insomnia, dizziness, drowsiness, fatigue
- Dermatologic: Pruritus, diaphoresis, rash
- Gastrointestinal: Vomiting, dyspepsia, gastroenteritis, abdominal pain
- Genitourinary: Urinary tract infection, urinary retention
- Otic: Tinnitus, sensorineural hearing loss
- Endocrine: Secondary adrenal insufficiency
(17)
Hydrocodone, being an agonist, must not be taken with other central nervous system depressants as sedation and respiratory depression can result. In formulations combined with acetaminophen, hydrocodone can increase the international normalized ratio (INR) and cause bleeding. Medications that induce or inhibit cytochrome enzymes can lead to wide variations in absorption.
The most common drug interactions are listed below:
- Alcohol
- Benzodiazepines
- Barbiturates
- Other Opioids
- Rifampin
- Phenytoin
- Carbamazepine
- Cimetidine
- Fluoxetine
- Ritonavir
- Erythromycin
- Diltiazem
- Ketoconazole
- Verapamil
- Grapefruit.
- Phenytoin
- St. John’s Wort
- Glucocorticoids
Considerations
Use with caution in the following:
- Patients with Hepatic Impairment: Initiate 50% of the usual dose
- Patients with Renal Impairment: Initiate 50% of the usual dose
- Pregnancy: While not contraindicated, the FDA issued a black-boxed warning since opioids cross the placenta, and prolonged use during pregnancy may cause neonatal opioid withdrawal syndrome (NOWS).
- Breastfeeding: Infants are susceptible to low dosages of opioids. Non-opioid analgesics are preferred.
Pharmacogenomic: Genetic variants in hydrocodone metabolism include ultra-rapid, extensive, and poor metabolizer phenotypes. After administration of hydrocodone, hydromorphone levels in rapid metabolizers are significantly higher than in poor metabolizers.
Oxycodone
Mechanism of Action and Metabolism
Oxycodone has been in use since 1917 and is derived from Thebaine. It is a semi-synthetic opioid analgesic that works by binding to mu-opioid receptors in the central nervous system. It primarily acts as an agonist, producing analgesic effects by inhibiting the transmission of pain signals (4).
Oxycodone is primarily metabolized in the liver by CYP3A4/5. It is metabolized in the liver to noroxycodone and oxymorphone. The metabolite oxymorphone also has an analgesic effect and does not inhibit CYP3A4/5. Because of this metabolite, oxycodone is more potent than morphine, with fewer side effects and less drug interactions. Approximately 72% of oxycodone is excreted in urine (4).
Available Forms
Oxycodone can be administered orally, rectally, intravenously, and as an epidural. For this sake, we will focus on immediate-release and extended-release oral formulations.
- Immediate-release (IR) tablets
- IR capsules
- IR oral solutions
- Extended-release (ER) tablets
Dosing and Monitoring
The dosing of oxycodone should be individualized based on the patient’s pain severity, previous opioid exposure, and response. Initial dosages for opioid naïve patients range from 5-15 mg for immediate-release formulations, while extended-release formulations are usually initiated at 10-20 mg.
Dosage adjustments may be necessary based on the patient’s response, but caution should be exercised. IR and ER formulations reach a steady state at 24 hours and titrating before 24 hours may lead to overdose.
Regular monitoring is essential to assess the patient’s response to treatment, including pain relief, side effects, and signs of opioid misuse or addiction. Monitoring should include periodic reassessment of pain intensity, functional status, and adverse effects (4).
Side Effects and Contraindications
Common side effects of oxycodone include:
- Constipation
- Nausea
- Sedation
- Dizziness
- Respiratory depression
- Respiratory arrest
- Hypotension
- Fatal overdose
Oxycodone is contraindicated in patients with known hypersensitivity to opioids, severe respiratory depression, paralytic ileus, or acute or severe bronchial asthma. It should be used cautiously in patients with a history of substance abuse, respiratory conditions, liver, or kidney impairment, and those taking other medications that may interact with opioids, such as alcohol (4).
It is also contraindicated with the following medications and classes:
- Antifungal agents
- Antibiotics
- Rifampin
- Carbamazepine
- Fluoxetine
- Paroxetine
Considerations
- Nurse practitioners should consider the variations in the mechanism of action for the following:
- Metabolism differs between males and females: females have been shown to have less concentration of oxymorphone and more CYP3A4/5 metabolites.
- Infants have reduced clearance of oxycodone, increasing side effects.
- Pediatrics have 20-40% increased clearance over adults.
- Reduced clearance with age increases the half-life of oxycodone.
- Pregnant women have a greater clearance and reduced half-life.
- Impairment of the liver reduces clearance.
- Cancer patients with cachexia have increased exposure to oxycodone and its metabolite.
- Maternal and neonate concentrations are similar, indicating placenta crossing (4)
Morphine
Mechanism of Action and Metabolism
Morphine is a naturally occurring opioid alkaloid extracted from the opium poppy. It was isolated in 1805 and is the opioid against which all others are compared. Morphine binds to mu-opioid receptors in the brain and spinal cord, inhibiting the transmission of pain signals and producing analgesia. It is a first-line choice of opioid for moderate to severe acute, postoperative, and cancer-related pain (8).
Morphine undergoes first-pass metabolism in the liver and gut. It is well absorbed and distributed throughout the body. Its main metabolites are morphine-3-glucuronide and morphine-6-glucuronide. Its mean plasma elimination half-life after intravenous administration is about 2 hours. Approximately 90% of morphine is excreted in the urine within 24 hours (8).
Available Forms
Morphine is available in various forms, including.
- Immediate-release tablets
- Extended-release tablets
- Oral IR solutions
- Injectable solutions
- Transdermal patches
Dosing and Monitoring
Morphine is hydrophilic and, as such, has a slow onset time. The advantage of this is that it is unlikely to cause acute respiratory depression even when injected. However, because of the slow onset time, there is more likelihood of morphine overdose due to the ability to “stack” doses in patients experiencing severe pain (8).
The dosing of morphine depends on the patient’s pain severity, previous opioid exposure, and other factors. It is usually initiated at a low dose and titrated upwards as needed. Monitoring pain relief, adverse effects, and signs of opioid toxicity is crucial. Reevaluate benefits and harms with patients within 1 to 4 weeks of starting opioid therapy or of dose escalation. General recommendations for initiating morphine (8).
Prescribe IR opioids instead of ER opioids.
Prescribe the lowest effective dosage, below 50 Morphine Milligram Equivalents (MME) /day.
Side Effects and Contraindications
Because morphine binds to opioid receptors in the brain and spinal cord, is metabolized in the liver and gut, and has a slow onset, the following side effects are common:
- Constipation
- Nausea
- Vomiting
- Sedation
- Dizziness
- Respiratory depression
- Pruritis
- Sweating
- Dysphoria/Euphoria
- Dry mouth
- Anorexia
- Spasms of urinary and biliary tract
Contraindications of morphine are:
- Known hypersensitivity or allergy to morphine.
- Bronchial asthma or upper airway obstruction
- Respiratory depression in the absence of resuscitative equipment
- Paralytic ileus
- Risk of choking in patients with dysphagia, including infants, children, and the elderly (8)
- Concurrent use with other sedating medications: Amitriptyline, diazepam, haloperidol, chlorpromazine
Morphine interacts with the following medications:
- Ciprofloxacin
- Metoclopramide
- Ritonavir
Considerations for Nurse Practitioners
Assess for medical conditions that may pose serious and life-threatening risks with opioid use, such as the following:
- Sleep-disordered breathing, such as sleep apnea.
- Pregnancy
- Renal or hepatic insufficiency
- Age >= 65
- Certain mental health conditions
- Substance use disorder
- Previous nonfatal overdose
Fentanyl
Mechanism of Action and Metabolism
Fentanyl is a synthetic opioid more potent than morphine and was approved in 1968. Fentanyl is an agonist that works by binding to the mu-opioid receptors in the central nervous system. This binding inhibits the transmission of pain signals, resulting in analgesia. Fentanyl is often used for severe pain management, particularly in the perioperative and palliative care settings, or for severe pain in patients with Hepatic failure (8).
It is a mu-selective opioid agonist. However, it can activate other opioid receptors in the body, such as the delta and kappa receptors, producing analgesia. It also activates the Dopamine center of the brain, stimulating relaxation and exhilaration, which is responsible for its high potential for addiction (8).
Indications for fentanyl are as follows:
- Preoperative analgesia
- Anesthesia adjunct
- Regional anesthesia adjunct
- General anesthesia
- Postoperative pain control
- Moderate to severe acute pain (off-label)
Available Forms
Fentanyl is available in various forms, including:
- Transdermal patches
- Injectable solutions
- Lozenges
- Nasal sprays
- Oral tablets
(8)
Dosing and Monitoring
Fentanyl is metabolized via the CYP3A4 enzyme in the liver. It has a half-life of 3 to 7 hours, and 75% of Fentanyl is excreted in the urine and 9% in feces.
The dosing of fentanyl depends on the route of administration and the patient’s needs. For example, transdermal patches are typically applied every 72 hours, while injectable solutions are titrated to achieve the desired analgesic effect. Monitoring should include assessing pain levels, respiratory rate, blood pressure, and sedation scores (8).
Fentanyl is most commonly dosed as follows:
- Post-operative pain control
-
- 50 to 100 mcg IV/IM every 1 to 2 hours as needed; alternately 0.5 to 1.5 mcg/kg/hour IV as needed. Consider lower dosing in patients 65 and older.
- PCA (patient-controlled analgesia)
-
- 10 to 20 mcg IV every 6 to 20 minutes as needed; start at the lowest effective dose for the shortest effective duration – refer to institutional protocols (8).
- Moderate to severe acute pain (off-label)
-
- 1 to 2 mcg/kg/dose intranasally each hour as needed; the maximum dose is 100 mcg.
- Use the lowest effective dose for the shortest effective duration
(8)
Side Effects and Contraindications
Common side effects of fentanyl include:
- Respiratory depression
- Sedation
- Constipation
- Nausea
- Vomiting
- Euphoria
- Confusion
- Respiratory depression/arrest
- Visual disturbances
- Dyskinesia
- Hallucinations
- Delirium
- Narcotic ileus
- Muscle rigidity
- Addiction
- Loss of consciousness
- Hypotension
- Coma
- Death
(8)
The use of fentanyl is contraindicated in patients in the following situations:
- After operative interventions in the biliary tract, these may slow hepatic elimination of the drug.
- Respiratory depression or obstructive airway diseases (i.e., asthma, COPD, obstructive sleep apnea, obesity hyperventilation, also known as Pickwickian syndrome)
- Liver failure
- Known intolerance to fentanyl or other morphine-like drugs, including codeine or any components in the formulation.
- Known hypersensitivity (i.e., anaphylaxis) or any common drug delivery excipients (i.e., sodium chloride, sodium hydroxide)
(8)
Considerations for Nurse Practitioners
Nurse practitioners prescribe fentanyl should thoroughly assess the patient’s pain, medical history, and potential risk factors for opioid misuse. They should also educate patients about the proper use, storage, and disposal of fentanyl. It should be used cautiously in patients with respiratory disorders, liver or kidney impairment, or a history of substance abuse. Fentanyl is contraindicated in patients with known hypersensitivity to opioids and those without exposure to opioids.
Alcohol and other drugs, legal or illegal, can exacerbate fentanyl’s side effects, creating multi-layered clinical scenarios that can be complex to manage. These substances, taken together, generate undesirable conditions that complicate the patient’s prognosis (8).
Hydromorphone
Mechanism of Action and Metabolism
Hydromorphone is a semi-synthetic opioid derived from morphine. It binds to the mu-opioid receptors in the central nervous system. It primarily exerts its analgesic effects by inhibiting the release of neurotransmitters involved in pain transmission, thereby reducing pain perception. Hydromorphone also exerts its effects centrally at the medulla level, leading to respiratory depression and cough suppression (1).
Hydromorphone is indicated for:
- Moderate to severe acute pain
- Severe chronic pain
- Refractory cough suppression (off-label)
(1)
Available Forms
Hydromorphone is available in various forms, depending on the patient’s needs and severity of pain.
- Immediate-release tablet
- Extended-release tablets
- Oral liquid
- Injectable solution
- Rectal suppositories
Dosing and Monitoring
The immediate-release oral formulations of hydromorphone have an onset of action within 15 to 30 minutes. Peak levels are typically between 30 and 60 minutes with a half-life of 2 to 3 hours. Hydromorphone is primarily excreted through the urine.
The dosing of hydromorphone should be individualized based on the patient’s pain intensity, initiated at the lowest effective dose, and adjusted gradually as needed. Close monitoring of pain relief, adverse effects, and signs of opioid toxicity is essential. Patients should be assessed regularly to ensure they receive adequate pain control without experiencing excessive sedation or respiratory depression.
The following are standard dosages that should only be administered when other opioid and non-opioid options fail:
- Immediate-release oral solutions dosage: 1 mg/1 mL
- Oral tablets are available in 2 mg, 4 mg, and 8 mg.
- Extended-release oral tablets are available in dosages of 8 mg, 12 mg, 16 mg, and 32 mg.
- Injection solutions are available in concentrations of 1 mg/mL, 2 mg/mL, 4 mg/mL, and 10 mg/mL.
- Intravenous solutions are available in strengths of 2 mg/1 mL, 2500 mg/250 mL, ten mg/1 mL, and 500 mg/50 mL.
- Suppositories are formulated at a strength of 3 mg (1).
Side Effects and Contraindications
Hydromorphone has potential adverse effects on several organ systems, including the integumentary, gastrointestinal, neurologic, cardiovascular, endocrine, and respiratory.
Common side effects of hydromorphone include:
- Constipation
- Nausea
- Vomiting
- Dizziness
- Sedation
- Respiratory depression
- Pruritus
- Headache
- Somnolence
- Severe adverse effects of hydromorphone include:
- Hypotension
- Syncope
- Adrenal insufficiency
- Coma
- Raised intracranial pressure.
- Seizure
- Suicidal thoughts
- Apnea
- Respiratory depression or arrest
- Drug dependence or withdrawal
- Neonatal drug withdrawal syndrome
- Hydromorphone is contraindicated in patients with:
- Known allergies to the drug, sulfites, or other components of the formulation.
- Known hypersensitivity to opioids.
- Severe respiratory depression
- Paralytic ileus
- Acute or severe bronchial asthma
(1)
Caution should be exercised in patients with:
- Respiratory insufficiency
- Head injuries
- Increased intracranial pressure
- Liver or kidney impairment
Considerations for Nurse Practitioners
As nurse practitioners, it is crucial to assess the patient’s pain intensity and overall health status before initiating Hydromorphone. Start with the lowest effective dose and titrate carefully for optimal pain control. Regular monitoring for adverse effects, signs of opioid toxicity, and therapeutic response is essential.
Educate patients about the potential side effects, proper dosing, and the importance of not exceeding prescribed doses. Additionally, nurse practitioners should be familiar with local regulations and guidelines regarding opioid prescribing and follow appropriate documentation and monitoring practices.
Additional Considerations
In terminal cancer patients, clinicians should not restrain opioid therapy even if signs of respiratory depression become apparent.
Hydromorphone requires careful administration in cases of concurrent psychiatric illness.
Specific Patient Considerations
- Hepatic impairment and Renal Impairment: Initiate hydromorphone treatment at one-fourth to one-half of the standard starting dosage, depending on the degree of impairment.
- Pregnancy considerations: Hydromorphone can traverse the placental barrier and induce NOWS.
- Breastfeeding considerations: Nonopioid analgesic agents are preferable for breastfeeding women.
- Older patients: Hydromorphone is categorized as a potentially inappropriate medication for older adults

(1)
Tramadol
Mechanism of Action and Metabolism
Tramadol is a Schedule IV opioid medication with a higher potential for dependency and misuse than non-opioid medications. It binds to opioid receptors in the central nervous system, inhibiting the reuptake of norepinephrine and serotonin. It also has weak mu-opioid receptor agonist activity.
The liver metabolizes tramadol mediated by the cytochrome P450 pathways (particularly CYP2D6) and is mainly excreted through the kidneys.
Tramadol is used for moderate to severe pain.
Available Forms of Tramadol include:
- Immediate-release-typically used for acute pain management.
- Extended-release-used for chronic pain.
Dosing and Monitoring
Tramadol has an oral bioavailability of 68% after a single dose and 90–100% after multiple doses and reaches peak concentrations within 2 hours. Approximately 75% of an oral dose is absorbed, and the half-life of tramadol is 9 hours (18).
Tramadol dosing should be individualized based on the patient’s pain severity and response.
- The initial dose for adults is usually 50-100 mg orally every 4-6 hours for pain relief.
- The maximum daily dose is 400 mg for immediate-release formulations and 300 mg for extended-release formulations (18).
It is essential to monitor the patient’s pain intensity, response to treatment, and any adverse effects. Regular reassessment and adjustment of the dosage may be necessary.
Side Effects and Contraindications
Tramadol is responsible for severe intoxications leading to consciousness disorder (30%), seizures (15%), agitation (10%), and respiratory depression (5%). The reactions to Tramadol suggest that the decision to prescribe should be carefully considered.
Common side effects of tramadol include:
- Nausea
- Vomiting
- Dizziness
- Constipation
- Sedation
- Headache
- CNS depression
- Seizure
- Agitation
- Tachycardia
- Hypertension
- Reduced appetite
- Pruritus and rash
- Gastric irritation
Serious side effects include:
- Respiratory depression
- Serotonin syndrome
- Seizures
Contraindications
Tramadol is contraindicated in patients with:
- History of hypersensitivity to opioids
- Acute intoxication with alcohol
- Opioids, or other psychoactive substances
- Patients who have recently received monoamine oxidase inhibitors (MAOIs)
Additionally, the following can be observed in tramadol intoxication:
- Miosis
- Respiratory depression
- Decreased level of consciousness
- Hypertension
- Tremor
- Irritability
- Increased deep tendon reflexes
Poisoning leads to:
- Multiple organ failure
- Coma
- Cardiopulmonary arrest
- Death
Considerations for Nurse Practitioners
Tramadol has been increasingly misused with intentional overdoses or intoxications. Suicide attempts were the most common cause of intoxication (52–80%), followed by abuse (18–31%), and unintentional intoxication (1–11%).
Chronic tramadol or opioid abuse was reported in 20% of tramadol poisoning cases. Fatal tramadol intoxications are uncommon except when ingested concurrent with depressants, most commonly benzodiazepines and alcohol (18).
Tramadol poisoning can affect multiple organ systems:
- Gastrointestinal
- Central nervous system: seizure, CNS depression, low-grade coma, anxiety, and over time anoxic brain damage
- Cardiovascular system: palpitation, mild hypertension to life-threatening complications such as cardiopulmonary arrest
- Respiratory system
- Renal system: renal failure with higher doses of tramadol intoxication
- Musculoskeletal system: rhabdomyolysis
- Endocrine system: hypoglycemia, serotonin syndrome
(18)

Self-Quiz
Ask Yourself...
- How do you address patients’ misconceptions about pain medications?
- What are the mechanisms of action for commonly prescribed pain medications?
- How do these mechanisms of action contribute to pain relief?
- What are the potential side effects and risks associated with commonly prescribed pain medications?
Cannabis
Mechanism of Action and Metabolism
Cannabis is classified as a Schedule I status. It contains various cannabinoids, with delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) being the most studied. THC primarily acts on cannabinoid receptors in the brain, producing psychoactive effects, while CBD has more diverse effects on the nervous system.
These cannabinoids interact with the endocannabinoid system, modulating neurotransmitter release and influencing various physiological processes (32).
Similar to opioids, cannabinoids are synthesized and released in the body by synapses that act on the cannabinoid receptors present in presynaptic endings (32).
They perform the following actions related to analgesia:
- Decrease the release of neurotransmitters.
- Activate descending inhibitory pain pathways.
- Reduce postsynaptic sensitivity and alleviate neural inflammation.
- Modulate CB1 receptors within central nociception processing areas and the spinal cord, resulting in analgesic effects.
- Attenuate inflammation by activating CB2 receptors (32).
- Emerging research shows cannabis is indicated for:
- Migraines
- Chronic pain
- Back pain
- Arthritic pain
- Pain associated with cancer and surgery.
- Neuropathic pain
- Diabetic neuropathic pain when administered early in the disease progression.
- Sickle cell disease
- Cancer
- Inflammatory bowel disease
(32)
Available Forms
Cannabis refers to products sourced from the Cannabis sativa plant. There are differences between cannabis, cannabinoids, and cannabidiol (CBD). Cannabinoids are extracted from the cannabis plants. Cannabinoid-based treatments, such as dronabinol and CBD, are typically approved medical interventions for specific indications.
THC (9-tetrahydrocannabinol) is the psychoactive component of the cannabis plant. CBD is a non-psychoactive component (32).
Cannabis can be consumed in different forms, each with a different onset and duration.
Patients may have individual preferences, including:
- Smoking/vaporizing dried flowers.
- Consuming edibles
- Tinctures or oils
- Applying topicals
(32)
Dosing and Monitoring
Inhaling marijuana via the lungs by smoking or vaping causes maximum plasma concentration within minutes. Psychiatric effects begin within seconds to a few minutes after inhalation and peak after 15 to 30 minutes. The effect diminishes throughout 2 to 3 hours (32).
Oral ingestion of marijuana causes psychiatric effects that typically occur between 30 and 90 minutes and reach maximum effect after 2 to 3 hours. Ingested marijuana effects last about 4 to 12 hours (32).
Dosing cannabis is challenging due to variations in potency and individual responses. Start with low doses and titrate slowly to achieve the desired effect while minimizing side effects. Regular monitoring is crucial, including assessing symptom relief, adverse effects, and potential drug interactions. Encourage patients to keep a diary to track their cannabis use and its effects (32).
Side Effects and Contraindications
Cannabis can exacerbate mental health conditions such as anxiety and psychosis. Common side effects of cannabis include (32):
- Dizziness
- Dry mouth
- Increased heart rate
- Impaired memory
- Psychoactive effects
Contraindications include:
- Pregnancy
- Breastfeeding
- Heart disease
- Respiratory conditions
- History of substance abuse
- Mental health disorders
Considerations for Nurse Practitioners
Cannabis is currently not approved by the United States Food and Drug Administration (FDA) and is considered an illicit drug by the US Drug Enforcement Agency (DEA). However, several US states have legalized its use in certain medical conditions.
Multiple studies have indicated that patients undergoing pain treatment can effectively substitute their opioid medication with cannabis, potentially contributing to mitigating the opioid epidemic. Cannabinoids also reduce neuropathic pain associated with different conditions and prevent diabetic neuropathic pain when administered early in the disease progression.[59][60]
In addition, cannabinoids also reduce inflammatory pain and thus can be used in conditions such as arthritis, sickle cell disease, cancer, and inflammatory bowel disease.[61][62]
Nurse Practitioners prescribing opioids, tramadol, or Cannabis should thoroughly understand their potential risks, benefits, and appropriate use. They should assess the patient’s pain intensity, medical history, and concurrent medications before prescribing these medications for pain. Close monitoring is crucial to evaluate the patient’s response to treatment, adjust the dosage as needed, and identify any adverse effects.
Nurse practitioners should educate patients about the proper use of opioids, tramadol, or cannabis, potential side effects, and the importance of adherence to the prescribed regimen. Nurse Practitioners should also be aware of local regulations and guidelines regarding opioid prescribing and follow them accordingly.


Self-Quiz
Ask Yourself...
- How do you educate patients about the risks and benefits of pain medications?
- How do you manage patients who require high-dose opioids for pain management?
- Is medical cannabis legal in your State? If yes, are you familiar with the prescribing guidelines?
- Do you have any personal biases against the use of medical cannabis? Why or why not?
Case Study
Mary is agreeable to trying an increased dose of Gabapentin. Mary would also like to see a counselor to discuss her past and get help with her anxiety. You made an appointment for Mary to see a Licensed Clinical Social Worker in your clinic.
You read the side effects and warnings for Gabapentin, and it is unsafe to use Gabapentin and Tramadol together since they are both depressants. You order a non-steroidal drug for Mary’s somatic knee pain and make a consult for imaging studies on her left knee. You also make a referral to Orthopedics.
You educated Mary about the side effects of Gabapentin and scheduled a follow-up appointment. The day after Mary began her treatment with the increased Gabapentin, you called Mary to follow up on its effect. Mary still has pain, but she is not having any untoward side effects. Gabapentin may not work immediately so you will schedule a follow-up call in 3 days.

Self-Quiz
Ask Yourself...
- In this case study, Mary has insurance. How might your practice be different were Mary not injured?
- In your experience, what are the possible reasons for Mary’s knee pain not being a part of her previous treatment record?
- Consider how your assessment of Mary’s needs differs from the above-mentioned case study.
- Explain the rationale for decisions made by the nurse practitioner in the case study mentioned above and if your decisions would differ.
Opioid Use, the Opioid Epidemic, and Statistics
The use and misuse of opioids has become a pressing public health concern, leading to a global epidemic. The history of opioid use, the opioid epidemic, and associated statistics provide essential context for healthcare professionals in addressing this public health crisis. More importantly, it is estimated that 1 in 4 patients receiving prescription opioids in primary care settings will misuse them.
In addition, 50% of opioid prescriptions are written by primary care providers, including nurse practitioners (22). Understanding the factors contributing to the epidemic and the magnitude of its impact is crucial for effective prevention, intervention, and treatment strategies.
History of Opioid Use
Opioids have a long history of medicinal use, dating back to ancient civilizations. They have been a drug of choice for pain relief for thousands of years. The introduction of synthetic opioids in the 19th century, such as morphine and later heroin, revolutionized pain management.
However, their potential for addiction and misuse soon became apparent (16).
The Opioid Epidemic
The opioid epidemic refers to the surge in opioid misuse, addiction, and overdose deaths. The epidemic gained momentum in the late 1990s with increased prescribing of opioids for chronic pain (43).
No doubt, increased prescribing put opioids in the hands of consumers, but increased prescribing resulted from a multifactorial influence. One of the main influences was aggressive marketing by pharmaceutical companies, which has been well publicized. However, due to the long history of under prescribing pain medications for fear of misuse and addiction, the medical community was primed to expand its opioid prescribing practices (31).
A historical event that increased comfort with prescribing opioids, in the writer’s opinion, was the introduction of the Medicare Hospice Benefit in 1986. Medical directors must be contracted or employed by hospices, and these medical directors had or soon gained pain management expertise. To further promote hospice and effective pain management, the hospice medical directors, with newly acquired skills, provided education throughout medical communities about pain management and specifically to decrease the fear of using opioids.
Pharmacies and attending physicians grew accustomed to giving opioids for home use. Hospice care is for terminally ill patients, defined as a life expectancy of 6 months or less. Still, the reality is that hospice discharges 12 to 40% of patients for ineligibility and other reasons.
A more prominent factor in increasing opioid prescribing was the 1996 American Pain Society’s introduction of pain as “the 5th Vital sign.” Soon after, The Joint Commission promoted pain as “the 5th Vital Sign” and began compliance surveys in healthcare organizations requiring pain assessment details to be as prominent as blood pressure and heart rate. The Joint Commission cited a quote from 1968 by a nurse from the University of California Los Angeles, Margo McCaffrey, who defined pain as “…Whatever the experiencing person says it is, existing whenever s/he says it does.”
The Joint Commission accreditation programs pursued pain management as part of the accreditation process throughout its healthcare accreditation programs, including hospice accreditation by 1989 per TJC Timeline (48).
The National Institute of Health published an article about the Joint Commission’s role in the opioid epidemic, particularly regarding the definition of pain, “This definition emphasizes that pain is a subjective experience with no objective measures. It also stresses that the patient, not the clinician, is the authority on the pain and that their self-report is the most reliable indicator of pain.
This set the tone for clinicians: Patients are always to be trusted to report pain accurately” (45).

Statistics on the Opioid Epidemic
In the United States alone, over 500,000 people died from opioid overdoses between 1999 and 2017. The number of opioid-related overdose deaths continues to increase, with synthetic opioids, mainly illicitly manufactured Fentanyl, playing a significant role in recent years (46).
Fentanyl-laced drugs, such as marijuana, are increasingly sold knowing and unknowingly to introduce medications with a high addiction rate, thus creating new consumers. This practice can potentially increase deaths due to the imprecise nature of manufacturing (16).
Opioid-related hospitalizations have also risen substantially. In 2014, there were approximately 1.27 million hospitalizations related to opioids in the United States. These hospitalizations not only place a burden on healthcare systems but also reflect the severe consequences of opioid misuse (3).

Self-Quiz
Ask Yourself...
- Have you experienced changes to your practice because of the opioid epidemic? If so, what are the changes?
- What is your opinion on the validity of Margo McCaffrey’s definition of pain?
- What factors influence your willingness or unwillingness to prescribe opioids?
Federal Regulations on Opioid Prescribing
The history of substance use disorder prevention that promotes opioid recovery and treatment for patients and communities can be traced back to the early 20th century. However, the current approach to addressing opioid addiction and promoting healing has evolved significantly in recent times (36).
In the early 1900s, health professionals treated opioid addiction with punitive measures, including incarceration and moralistic approaches. The focus was on punishing individuals rather than providing effective treatment. This approach persisted for several decades until the mid-20th century when the medical community started recognizing addiction as a medical condition rather than a moral failing (36).
The Controlled Substances Act (CSA), introduced in 1970, was a response to increasing drug abuse and illicit drug trafficking in the United States. The CSA is a federal law regulating the manufacture, possession, distribution, and use of certain substances, including drugs and medications, that can potentially cause abuse and dependence. Its primary purpose is to combat drug abuse, reduce drug-related crimes, and protect public health and safety. The Drug Enforcement Agency (DEA) plays a crucial role in enforcing the CSA by monitoring and controlling controlled substance production, distribution, and use (31).
In the 1990s, the significant increase in opioid prescribing, leading to a surge in opioid addiction and overdose deaths, prompted a shift in focus toward prevention. Efforts were made to educate healthcare providers about the risks of overprescribing opioids and to implement prescription drug monitoring programs to track and prevent abuse (36).
The Comprehensive Addiction and Recovery Act (CARA) was signed into law in 2016 to expand access to treatment and recovery services for opioid addiction. This legislation allocated funding for prevention, treatment, recovery, and support services while promoting evidence-based practices and programs (36).
The Centers for Disease Control and Prevention (CDC) published guidelines in 2016 for prescribing opioids for chronic pain, which was updated in 2022. These guidelines emphasize the importance of non-opioid alternatives, using the lowest effective dose for the shortest duration, and assessing the benefits and risks of continued opioid therapy (13).
Furthermore, the Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT) was signed into law in 2018, providing additional resources to address the opioid crisis. This legislation expanded access to medication-assisted treatment (MAT), increased the availability of naloxone, a medication used to reverse opioid overdose, and enhanced support for recovery housing (36).
In recent years, there has been a growing recognition of the importance of a comprehensive approach to opioid addiction, including harm reduction strategies, increased access to naloxone, and the integration of mental health services. Communities and organizations have been working together to address the underlying issues contributing to addiction, such as poverty, trauma, and social determinants of health (50).
Overall, the history of substance use disorder prevention that promotes opioid recovery and treatment has evolved from a punitive approach to a more compassionate and evidence-based model. Efforts are now focused on prevention, early intervention, and expanding access to comprehensive treatment and support services for individuals and communities affected by opioid addiction (36).
The most current federal regulations on opioid prescribing for healthcare providers are the amendments to the CSA in 2018, which added new rules to limit the quantity and duration of opioid prescriptions for acute pain to seven days.
In 2022, the CDC updated recommendations to the Clinical Practice Guidelines for Prescribing Opioids for Pain.
The 2022 CDC guidelines are summarized below (13):
- Non-opioid therapies should be considered the first-line treatment for chronic pain.
- Establish clear treatment goals with patients, including realistic pain management and functional improvement expectations.
- Conduct a thorough risk assessment for potential harms before initiating opioid therapy.
- When opioids are used, start with the lowest effective dose and consider immediate-release opioids instead of extended-release or long-acting opioids.
- Prescribe the lowest effective dose for the shortest duration possible, typically three days or less and rarely exceeding seven days.
- Reassess benefits and risks within one day after prescribing opioids, including checking the prescription drug monitoring database.
- Avoid prescribing opioids and benzodiazepines concurrently whenever possible due to the increased risk of overdose and death.
- Offer naloxone to patients at increased risk of opioid overdose, including those with a history of overdose, substance use disorder, or concurrent benzodiazepine use.
- When opioids are no longer needed, taper the dose gradually to minimize withdrawal symptoms.
- Arrange an evidence-based treatment for patients with opioid use disorder, including medication-assisted treatment (Naltrexone, Buprenorphine, or Methadone).

Self-Quiz
Ask Yourself...
- What are the general guidelines for prescribing opioids for acute pain?
- How do these guidelines differ for chronic pain management?
- Discuss how federal regulations impact the practice of nurse practitioners in terms of opioid prescribing.
- Describe the potential benefits and challenges nurse practitioners face when adhering to federal regulations on opioid prescribing.
Safe Prescribing and Prescription Monitoring Program
Prescription Drug Monitoring Programs (PDMP) are state-run electronic databases that track the prescribing and dispensing of controlled substances. PDMPs are designed to improve patients care and safety by giving clinicians access to patients’ prescription histories, allowing them to make informed decisions when prescribing controlled substances. PDMPs help identify patients at risk of substance misuse or prescription drug overdose. They also enable clinicians to identify potential drug interactions and prevent opioid diversion (14).
PDMPs collect and store data from pharmacies and prescribers in a centralized database. Clinicians can access this database to review a patient’s prescription history, including the types of medications prescribed, the prescribers involved, and the dispensing pharmacies (14).
In many states, PDMP use is mandated by law, and nurse practitioners may be required to register and use the system. It is essential to understand state-specific laws and regulations regarding PDMP use.
PDMPs have some limitations, such as incomplete data or delays in reporting. The CDC emphasizes that clinicians should use PDMP data for their clinical assessment and other relevant information to make informed decisions about prescribing controlled substances. Still, PDMP cannot be used as the sole basis for denying or providing treatment (14).

Self-Quiz
Ask Yourself...
- How can nurse practitioners navigate and stay updated with evolving federal regulations surrounding opioid prescribing to ensure safe and effective care?
- How do you ensure appropriate documentation when prescribing controlled substances?
Case Study
After five days on Gabapentin, Mary was doing well, and her neuropathic pain had decreased to 3/10. However, Mary suffered a fall after her knee “gave out” and injured her knee and back. She was in severe pain, and her family drove her to the ER. The ER doctors saw Mary, and orthopedics were consulted. Mary has surgery scheduled for a knee replacement a week from now.
Mary was prescribed Vicodin because she was in excruciating pain, but her prescription only allowed enough medication for two days. Mary has made an appointment with you to renew her prescription.
You evaluate Mary because you know that concomitant use of Gabapentin and opioids puts Mary at risk for respiratory depression and possible side effects, including accidental overdose.
Mary stated she has been more alert the past 24 hours and is afraid her functional status will continue to decline if she does not have more Vicodin because the pain in her back and knee makes it difficult to stand. You assess Mary. Mary stated she occasionally drinks alcohol but has not had a drink since she moved. She has no familial history of substance abuse or mental health disorders.
Mary’s mother stayed at her house to help her for the first 24 hours after Mary’s return from the ER, but Mary is providing her care now.
You check the PDMP database and see that Mary was prescribed eight pills she has taken over the last 48 hours.
Since the Vicodin has been effective without untoward side effects, and Mary’s function is improving, you decide to refill the prescription of Vicodin. You will taper the dose to three Vicodin daily for two days and two for one day. Mary will be near her appointment for a knee replacement as well.

Self-Quiz
Ask Yourself...
- What are the potential benefits and drawbacks of using PDMPs in your practice?
- How can PDMPs help you identify potential drug abuse or diversion cases among your patients? Can you provide examples from your own experience?
- In what ways do PDMPs impact your decision-making process when prescribing controlled substances?
- What are the key considerations when prescribing controlled substances?
- How do you ensure responsible prescribing practices for controlled substances?
Preventing Opioid Use Disorder
As previously discussed, opioid addiction is a growing concern worldwide, affecting individuals from all walks of life. According to the CDC, “anyone who takes prescription opioids can become addicted to them” (14).
As frontline healthcare professionals, nurse practitioners must recognize the signs of opioid addiction to provide timely intervention and support.
Indicators of Opioid Addiction
This section will outline the key indicators of opioid addiction.
Physical Symptoms
Physical symptoms are often the first noticeable signs of opioid addiction. These symptoms may include constricted pupils, drowsiness, slurred speech, impaired coordination, and increased sensitivity to pain. Additionally, individuals struggling with opioid addiction may exhibit frequent flu-like symptoms, such as a runny nose, sweating, itching, or gastrointestinal issues.
Behavioral Changes
Opioid addiction can significantly impact an individual’s behavior. These may include increased secrecy, frequent requests for early prescription refills, doctor shopping (seeking prescriptions from multiple healthcare providers), neglecting personal hygiene, and experiencing financial difficulties due to excessive spending on opioids (37).
Social Isolation
Opioid addiction often leads to social withdrawal and isolation. Individuals struggling with opioid addiction may distance themselves from family, friends, and social activities they once enjoyed. They may exhibit erratic mood swings, become defensive or hostile when confronted about their drug use, and display a general lack of interest in previously important activities (30).
Psychological Changes
The psychological impact of opioid addiction is significant. Individuals with opioid addiction may exhibit increased anxiety, depression, irritability, and restlessness. They may also experience cognitive impairments, memory lapses, and difficulties in decision-making. Healthcare professionals should be attentive to these changes, as they can indicate opioid addiction (51).
Tolerance and Withdrawal Symptoms
The development of tolerance and withdrawal symptoms are critical signs of opioid addiction. Individuals may require increased dosages of opioids to achieve the desired effect, indicating a growing tolerance. Furthermore, withdrawal symptoms such as muscle aches, nausea, vomiting, insomnia, and intense cravings for opioids may occur when the drug is discontinued or reduced abruptly (51).

Self-Quiz
Ask Yourself...
- Discuss how nurse practitioners can contribute to preventing opioid use disorder.
- Explain how nurse practitioners effectively communicate the risks and signs of opioid misuse without stigmatizing or alienating patients.
- What are the signs of opioid addiction or misuse in patients and how do you approach patients who may be at risk for opioid addiction?
- How do you ensure appropriate documentation when prescribing controlled substances?
Treatment for Opioid Overdose
The management of opioid overdose, withdrawal, and addiction requires a comprehensive approach that combines pharmacological interventions with psychosocial support. Naloxone remains a vital tool for reversing opioid overdose, while medications such as Methadone, buprenorphine, and naltrexone play crucial roles in withdrawal and addiction treatment (40).
Nurse practitioners must stay vigilant and informed about the evolving landscape of medications. This section aims to provide a comprehensive review of medications and treatment strategies for opioid overdose, withdrawal, and addiction and is excerpted from the NIH (40).
Naloxone
Mechanism of Action and Metabolism
Naloxone is an opioid receptor antagonist. It works by binding to opioid receptors and displacing any opioids present, thereby reversing the effects of opioid overdose. It has a higher affinity for opioid receptors than most opioids, effectively blocking their action.
Naloxone is indicated for emergency intervention of opioid overdose. It effectively reverses respiratory depression and other life-threatening effects. Studies suggest the potential benefits of combining naloxone with other medications, such as buprenorphine (see below), to improve outcomes. Initiatives promoting community-based naloxone distribution programs have shown promising results in reducing opioid-related deaths.
Available Forms
Naloxone is available in various formulations:
- Intranasal
- Intramuscular
- Intravenous
- Auto-injectors
The most used form is the intranasal spray, which is easy to administer and requires no specialized training. Intranasal naloxone formulations have gained popularity due to their ease of use and increased availability. A recent study showed that the non-FDA-approved compound spray was far less effective than either FDA compound (15).
Dosing and Monitoring
The recommended initial dose of naloxone for opioid overdose is 2mg intranasally or 0.4mg to 2mg intramuscularly or intravenously. If the patient does not respond within 2-3 minutes, additional doses may be administered every 2-3 minutes. Continuous monitoring of the patient’s respiratory status is essential, as repeat doses may be required due to the short half-life of naloxone.
Side Effects and Contraindications
Naloxone has been shown not to affect individuals without opioids in their system.
Common side effects of naloxone include:
- Withdrawal symptoms: increased heart rate, sweating, and agitation
- Nausea
- Vomiting
- Headache
Contraindications include known hypersensitivity to naloxone and situations where the use of naloxone may be unsafe or not feasible.
Considerations for Nurse Practitioners
Fentanyl and other opioids have a rapid onset, and the need to act quickly is paramount. As mentioned previously, the ease of use and higher plasma concentrations using the FDA-approved 4-mg FDA NxSpray device compared with the locally compounded nasal sprays should be considered when ordering Naloxone (15).
Fentanyl and other potent synthetic opioids may require multiple administrations of naloxone to achieve reversal of an overdose (15). As a nurse practitioner prescribing naloxone, it is crucial to assess the patient’s risk factors for opioid overdose, such as a history of substance use disorder or chronic pain management.
Education regarding the proper administration of naloxone should be provided to the patients and their caregivers. Additionally, it is essential to provide resources for follow-up care, including addiction treatment and ongoing support.

Self-Quiz
Ask Yourself...
- How do you support patients in their recovery from opioid use disorder?
- How do you address patients’ concerns and fears about addiction medications?
Methadone
Mechanism of Action and Metabolism
Methadone is a long-acting opioid agonist that effectively suppresses withdrawal symptoms and reduces cravings. It binds to the same opioid receptors in the brain as other opioids. It relieves withdrawal symptoms and reduces cravings by blocking the euphoric effects of opioids, thus helping individuals with opioid dependence to achieve stability (33).
Available Forms
Methadone is available in oral tablets and liquid formulations. The oral tablet is the most used form and is typically administered once daily (33).
Dosing and Monitoring
Methadone dosing is individualized based on the patient’s response and needs. Initially, the dose often started low and gradually increased until the patient reached a stable dose. Dosing may need to be adjusted based on the patient’s response, adherence, and any changes in their overall health. Regularly monitoring the patient’s vital signs, urine drug screens, and assessment of their withdrawal symptoms and cravings is essential.
Side Effects and Contraindications
Common side effects of methadone include:
- Constipation
- Dry mouth
- Drowsiness
- Sweating
- Weight gain
- Respiratory depression
Contraindications include:
- Known hypersensitivity to methadone
- Severe asthma
- Respiratory depression
- Certain heart conditions
(33)
Considerations for Nurse Practitioners
As a nurse practitioner prescribing methadone, conducting a comprehensive assessment of the patient’s medical history, current medications, and substance use history is crucial. Opioid treatment programs or specialized clinics are often involved in methadone treatment, so collaboration and coordination of care with these programs are essential.
Regularly monitoring the patient’s progress, adherence, and potential side effects or drug interactions is essential. Additionally, providing education on the risks and benefits of methadone and the importance of adherence to the prescribed regimen is crucial for successful treatment outcomes.
Buprenorphine
Mechanism of Action and Metabolism
Buprenorphine is a partial opioid agonist with a ceiling effect that minimizes the risk of overdose while reducing withdrawal symptoms. Buprenorphine is a partial opioid agonist that binds to the same receptors as other opioids, but produces a weaker response.
It has a high affinity for the mu-opioid receptors, which helps reduce cravings and withdrawal symptoms in individuals with opioid dependence.
Available Forms
Buprenorphine is available in different formulations, including sublingual tablets, buccal films, and extended-release injections. The sublingual tablets have different strengths, such as 2mg, 4mg, 8mg, and 12mg. Buprenorphine is taken as a daily tablet or weekly or monthly injection.
Dosing and Monitoring
The dosing of buprenorphine varies depending on the individual’s opioid dependence severity and treatment phase. Initially, a low dose (e.g., 2-4mg) is given, and it may gradually increase to a maintenance dose of 8-24 mg daily. Regular monitoring is essential to assess the patient’s response, adherence, and potential side effects.
Side Effects and Contraindications
Common side effects of buprenorphine include:
- Constipation
- Nausea
- Headache
- Insomnia
- Sweating
Serious side effects are rare but can include:
- Respiratory depression
- Allergic reactions
Buprenorphine is contraindicated in individuals with:
- Severe respiratory insufficiency
- Acute intoxication with opioids
- Known hypersensitivity
Considerations for Nurse Practitioners
Nurse practitioners can prescribe buprenorphine for opioid dependence treatment under the Drug Addiction Treatment Act (DATA). To become eligible, they must complete specific training requirements and obtain a waiver from the Substance Abuse and Mental Health Services Administration (SAMHSA).
Nurse practitioners should assess patients thoroughly, including their opioid use history, comorbidities, and medication compatibility, while ensuring appropriate counseling and referral for comprehensive treatment (40).
Clonidine + Lofexidine
Mechanism of Action and Metabolism
Both Clonidine and Lofexidine are alpha-2 adrenergic agonists. They work by stimulating alpha-2 receptors in the brain, which reduces sympathetic outflow and norepinephrine release. This results in decreased sympathetic activity, leading to various effects such as reduced blood pressure, decreased heart rate, and alleviated withdrawal symptoms (28).
Available Forms
Clonidine is available in oral tablets and patches. Lofexidine is available in oral tablets and is taken as needed (40).
Dosing and Monitoring
For opioid withdrawal, the Clonidine dose ranges from 0.1-0.3 mg every 4-6 hours. Lofexidine is usually initiated at 0.53 mg three times daily, and the dose can be increased to 2.88 mg daily. Monitoring blood pressure and heart rate is essential during treatment (40).
Side Effects and Contraindications
Common side effects of both medications include:
- Dry mouth
- Sedation
- Dizziness
- Constipation
- Orthostatic hypotension
(40)
Both medications are contraindicated in patients with:
- Hypotension
- Bradycardia
- Heart block
- History of hypersensitivity to the drugs
(40)
Considerations for Nurse Practitioners
An early study of lofexidine vs. clonidine for withdrawal symptoms showed that treatment with lofexidine resulted in lower withdrawal symptoms, fewer mood problems, less sedation, and hypotension. There were no significant differences in craving levels, morphine metabolites in urine, or dropout rates when both were compared.
Lofexidine can be a safe option for outpatient treatment as it does not lead to hypotension. However, nurse practitioners must closely monitor patients’ blood pressure and heart rate during treatment and educate them about possible side effects. If patients experience any concerning symptoms, they should inform their nurse practitioner immediately.
Gradual dose reduction of Clonidine is crucial to prevent rebound hypertension. Before prescribing either medication, nurse practitioners should assess for any contraindications or potential drug interactions (19).


Self-Quiz
Ask Yourself...
- What are the mechanisms of action for commonly prescribed addiction medications?
- What are the potential risks and benefits of using benzodiazepines for pain management?
- How do you assess and manage patients with co-occurring pain and substance use disorders?
- What are the guidelines for prescribing addiction medications like buprenorphine or methadone?
Emerging Therapies for Withdrawal
- Extended-release naltrexone
- Naltrexone is an opioid receptor antagonist that blocks the effects of opioids, reducing the risk of relapse. It is taken as a monthly injection.
- Alpha-2 adrenergic agonists
- Emerging evidence suggests the potential use of dexmedetomidine and guanfacine for managing opioid withdrawal symptoms.
Medication-Assisted Treatment (MAT)
Methadone was introduced in the 1960s and marked a significant turning point in opioid addiction treatment or MAT. Along with counseling and behavioral therapies, MAT became the cornerstone of opioid addiction recovery.
Examples of medications used:
- Methadone
- Buprenorphine:
- Naltrexone
Adjunctive Pharmacotherapies
- Antidepressants
- Selective serotonin reuptake inhibitors and tricyclic antidepressants may help manage co-occurring depression and anxiety.
- Anticonvulsants:
- Medications like Gabapentin and pregabalin show promise in reducing opioid cravings and improving treatment outcomes.

Self-Quiz
Ask Yourself...
- How do these medications work in the treatment of opioid use disorder?
- What are the potential side effects and risks associated with addiction medications?
- What are the federal guidelines around prescribing addiction medications for nurse practitioners?
- How do these guidelines influence your prescribing practices?
Other Substance Use Disorders
Patients in pain may struggle with Substance Use Disorders other than Opioid Use Disorder. Substance use disorders may often occur with mental health conditions such as anxiety, depression, and bipolar disorder.
In addition, many individuals engage in polydrug use. Understanding the most common substance use disorders aid in a comprehensive assessment of the patient and the development of appropriate treatment plans (28).
Alcohol Use Disorder (AUD): The prevalence of AUD worldwide was estimated to be 9.8% in men and 5.5% in women in 2016 (28).
Cannabis Use Disorder (CUD): The prevalence of CUD in the United States increased from 2.18% in 2001-2002 to 2.89% in 2012-2013. (28).
Cocaine Use Disorder: According to the National Survey on Drug Use and Health (NSDUH), in 2019, approximately 1.9 million Americans aged 12 or older had cocaine use disorder in the past year (44).
Methamphetamine Use Disorder: A study published in Drug and Alcohol Dependence reported that the prevalence of methamphetamine use disorder in the United States was estimated to be 0.2% in 2015-2016 (6).

Self-Quiz
Ask Yourself...
- How do you educate patients about the risks and benefits of addiction medications?
- How do you monitor patients on addiction medications for adherence and progress?
- What are the drug potential interactions with commonly prescribed addiction medications?
Drug Diversion and Illegal opioids
Misuse of opioids is facilitated by diversion and is defined as “the transfer of drugs from lawful to unlawful use” (24). Most commonly, this occurs when family and friends share prescribed opioids with other family and friends. Opioids and other controlled drugs are also diverted from healthcare facilities. Statistics show that healthcare facility diversion has increased since 2015 (24)
Diversion affects patients, healthcare workers, healthcare facilities, and public health. Patients experience substandard care due to ineffective pain management and impaired healthcare workers. In addition, affected patients are at risk of infections from compromised syringes (24).
Healthcare employees who divert are at risk of overdose and death. If caught, they face criminal prosecution and malpractice suits. Healthcare facilities also bear the cost of diverted drugs via internal investigations, follow-up care for affected patients, regulatory fines for inadequate safeguards, and declining public trust (24).
Despite the enormous consequences of drug diversion, healthcare facilities have implemented few processes to detect and deter the diversion of controlled substances (24).

Self-Quiz
Ask Yourself...
- What protocols can nurse practitioners implement to prevent drug diversion within their healthcare setting?
- How can nurse practitioners collaborate with other healthcare professionals and community resources to provide comprehensive care and support for patients with substance abuse disorders?
- What techniques or tools can nurse practitioners employ to start these sensitive conversations with new patients?
Patient Teachings and Considerations
Opioids have significant side effects and carry a risk of addiction and overdose. Nurse practitioners can decrease the risks of misuse and addiction by educating patients on appropriate disposal, safe storage, and potential signs of addiction.
Taking additional time to provide teaching nurse practitioners can promote patient safety, informed decision-making, and responsible opioid use.
- Safe Storage and Disposal:
-
- Teach patients to store opioids securely, out of reach of children, pets, visitors, and non-caregiver family members, to prevent accidental ingestion or misuse (13). Only the caregiver, if applicable, or the patient should have access to pain medications.
- Instruct patients on proper disposal methods, such as using drug take-back programs or mixing opioids with undesirable substances (e.g., coffee grounds) before throwing them away (11) (13).
- Medication Adherence:
-
- Emphasize the importance of taking opioids as prescribed, at the correct dose and frequency, to achieve optimal pain relief.
- Encourage patients to notify their healthcare provider if they experience inadequate pain control or side effects (35).
- Potential Side Effects:
-
- Educate patients about common side effects of opioids, including constipation, nausea, sedation, and respiratory depression.
- Discuss strategies to manage side effects, such as maintaining adequate hydration, consuming a fiber-rich diet, and using over-the-counter laxatives as needed (11).
- Risk of Dependence and Addiction:
-
- Explain the potential for opioid dependence and addiction, especially with long-term use or a history of substance abuse.
- Encourage patients to promptly report signs of opioid misuse, such as craving, loss of control, or continued use despite negative consequences (51).
- Avoiding Alcohol and Other Central Nervous System Depressants:
-
- Instruct patients to avoid consuming alcohol or other medications that can enhance the sedative effects of opioids, increasing the risk of respiratory depression.
- Advise patients to contact the Nurse Practitioner before starting new medications, including over-the-counter drugs or herbal supplements (2).
- Driving and Operating Machinery:
-
- Inform patients about the potential impairment caused by opioids, including reduced alertness, reaction time, and coordination.
- Advise patients to avoid driving or operating heavy machinery while taking opioids until they know how the medication affects them (14).

Self-Quiz
Ask Yourself...
- What strategies can nurse practitioners employ to effectively communicate the risks and benefits of opioid use while ensuring they clearly understand the potential side effects and the importance of adhering to the prescribed regimen?
- How can nurse practitioners promote patient engagement and shared decision-making regarding opioid pain management, considering the potential for dependence and addiction?
- How can nurse practitioners assess a patient’s knowledge and understand the safe storage and disposal of opioids?
- What strategies can nurse practitioners employ to effectively engage and build trust with patients reluctant to disclose or seek help for substance abuse disorders?
Case Study
You take some extra time with Mary to educate her on the taper dose of Vicodin, the potential for harm, and the risk of opioids, especially when used concomitantly with Gabapentin. You let Mary know it is unsafe to use alcohol, not only with Vicodin but also with Gabapentin. You let Mary know that Vicodin has a risk of dependency and misuse and, therefore, she will be monitored carefully.
You also educate that Mary should store the Vicodin away from visibility by anyone but herself since she can self-administer her medication. You let Mary know that Vicodin can cause constipation and that she should increase her water intake and take a stool softener.
You ask Mary to call you if her pain is not adequately relieved or if her medications run out before the three days.
You let Mary know that if she does stop taking the Vicodin before she has completed all the medication, she should dispose of it by mixing the pills with liquid and coffee grounds to make them unpalatable to animals and others.
Mary complied with your education, completed her course of Vicodin, and was scheduled for surgery. Mary’s social worker helped her communicate with her new employer and delayed her start date until after her recovery.
During her recovery, Mary received physical therapy and a short course of pain medication managed by her orthopedist.
Mary returned to the clinic for a follow-up visit after completing her therapy and before starting work. Mary’s pain level in her knee is 3/10, and she already feels like she can walk further than pre-surgery. Gabapentin has continued to help Mary’s neuropathic pain in her back, and she reports 2/10. Mary looks forward to beginning her new job and is optimistic about the future.

New Mexico Controlled Substances for Advanced Practice Registered Nurses (APRNs)
APRNs in New Mexico can obtain prescriptive authority for controlled substances from the New Mexico Board of Nursing (NM BON) and controlled substance prescriptive authority from the New Mexico Board of Pharmacy if they meet the requirements laid out in Statute/Rule (depending on the type of APRN) (1, 2):
- Certified Nurse Practitioners (CNP): 61-3-23.2.C.- D. NMSA 1978; 16.12.2.13.N.(5) NMAC (2)
- Certified Registered Nurse Anesthetist (CRNA): CRNA 61-3-23.3.D.- E. NMSA 1978; 16.12.2.14.M.(5) NMAC (2)
- Certified Nurse Specialist (CNS): CNS 61-3-23.4.C.- D. NMSA 1978; 16.12.2.15.L.(5) NMAC (2)
In addition to the specific requirements in the statue/rule, APRNs must complete at least 400 hour of work experience in which prescribing dangerous drugs has occurred within the two years immediately preceding the date of application. This is verified via the Verification of APRN Education form completed by the APRN program; or successful competition of a prescriptive authority preceptorship consisting of 400 hours of precepted prescribing of dangerous drugs which must be completed within six months.
APRNs can submit the following to the NM BON: (1) An Affidavit Requesting Prescriptive Authority and (2) Preceptor must provide to the Board of Nursing, on letterhead, a letter including the name and license number of the prescription preceptor(s). Upon receipt, the NM BON will issue a letter of authorization for the preceptorship (1).
In addition, to obtain controlled substance prescriptive authority in New Mexico for APRNs who received non-controlled substance prescriptive authority from the NM BON, the APRN must apply for a controlled substance registration form the New Mexico Board of Pharmacy (3). APRNs must also apply for a Drug Enforcement Administration (DEA) license registration (4).
Further questions about this process can be directed to the NM BON.

Conclusion
Pain management is the leading cause of primary care appointments and chronic pain is the leading cause of disability. Yet, prescribing opioids for primary care patients is also a factor in drug misuse and the opioid epidemic. Nurse practitioners are challenged to appropriately treat pain and effectively control diversion, addiction, and death from overdose.
It is imperative that nurse practitioners use evidence-based practices to assess, appropriately intervene, and educate about the benefits and potential harm caused by treatment with opioids. Nurse practitioners must stay up to date with the current federal regulations regarding PDMPs, clinical prescribing guidelines as well as emerging treatments for pain and opioid abuse disorders.

Self-Quiz
Ask Yourself...
- What are the options available for managing opioid addiction and withdrawal?
- How can nurse practitioners support patients in their recovery from opioid addiction?
- How do you assess and manage patients experiencing opioid withdrawal symptoms?
- What are the non-pharmacological interventions for managing opioid withdrawal?
References + Disclaimer
- Abi-Aad, K., & Derain, A. (2023, August 17). Hydromorphone. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK470393/
- Adler, J., Ballantyne, J., Chou, R., Davies, P., Fanciullo, G., & Fine, P. (2009). Clinical Guidelines for the Use of Chronic Opioid Therapy in Chronic NonCancer Pain. The Journal of Pain, 113-130.
- Ahmad, F., Rossen, L., Sutton, P., & & Talih, M. (2018). Provisional drug overdose. National Vital Statistics Reports, pp. 1-12.
- Altman, R., Clark, M., Huddart, R., & Klein, T. (2018, October 28). Pharm GKB Summary: Oxycodone Pathway, Pharmacokinetics. Retrieved from Pharmacogenet Genomics: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6602093/#:~:text=Approximately%2072%25%20of%20an%20oxycodone,oxycodone%20is%20unconjugated%20%5B70%5D
- Atrux-Tallau, N., naimi, Z., & Jaudinot, E. (2022, November 4). Pharmocokinetics of Morphine Sulfate Orodispersible tablets and Bioequivalence with Immediate-Release Oral Morphine Sulfate Formulations in Healthy Adult SubjectsUnder fastin Conditions. Retrieved from Clinical Drig Investigation: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9705466/
- Baldwin, G., Compton, W. M., Han, B., Houry, D., Jones, C. M., & Vivolo-Kantor, A. (2021, September 24). Methamphetamine use in the United States: epidemiological update and implocations for prevention, treatment and harm reduction. Annual New York Academy of Science. New York: National Institute of Health.
- Berg, K. A., & Clarke, W. P. (2018). Making Sense of Pharmacology: Inverse Agonism and Functional Selectivtiy. International Journal of Neuropsychopharmacology, 962-977.
- Bistas, K., Lopez-Ojeda, W., & Ramos-Matos, C. (2023, May 29). Fentanyl. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK459275/
- Blyth, F., Briggs, A., Hoy, D. G., March, L. M., & Schneider, C. H. (2019). The Global Burden of Musculoskeletal Pain-Where to From Here? American Journal of Public Health, 35-40.
- Bramanti, P., Cavalli, E., Mammana, S., Mazzon, E., & Nicoletti, F. (2019). The neuropathic pain: An Overview of the current treatment and future therapeutic approaches. International Journal of Immunopathology and Pharmacology, 33.
- Brennan, F., Carr, D., Cousins, M., & Pain, D. (2013). Pain Management: A Fundamental Human Right. Anesthesia and Analgesia, 224-227.
- Carver, A. C., & Foley, K. (2003). Types of Pain. In D. Kufke, & R. W. Pollock, Cancer Medicine. Hamilton: Holland Frei Cancer Medicine.
- Centers for Disease Control and Prevention. (2022). CDCs Clinical Practice Guidelines for Prescribing Opioids. Retrieved from Opioids: https://www.cdc.gov/opioids/healthcare-professionals/prescribing/guideline/index.html?s_cid=DOP_Clinician_Search_Paid_001&gclid=CjwKCAjwrranBhAEEiwAzbhNtVKOCMzLLnwhfj7B2D_aBCZM_SryNcEyXl0GRigmorFhKve2ekCVrhoCNYQQAvD_BwE
- Centers for Disease Control and Prevention. (2023, August 8). Opioids. Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/opioids/basics/epidemic.html#print
- Chiang, N., Gyaw, S., & Krieter, P. A. (2019). Comparison of the Pharmacokinetic Properties of Naloxone Following the Use of FDA-Approved Intranasal and Intramuscular Devices Versus a Common Improvised Nasal Naloxone Device. Journal of Clinical Pharmacology, 1078-1084.
- Cicero, T., & Ellis, M. &. (2017). The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA, 673-681.
- Cofano, S., & Yellon, R. (2022, October 24). Stat Pearls: Hydrocodone. Retrieved from National Institutes of Health: https://www.ncbi.nlm.nih.gov/books/NBK537288/
- Dart, R., Hoyte, C., & Nakhee, S. (2021). A Review on Tramadol Toxicity: Mechanism of Action, Clinical Presentation, and Treatment. Forensic Toxicology, 293-310. Retrieved from Forensic Toxicology: https://link.springer.com/article/10.1007/s11419-020-00569-0
- Delsignor, R. e. (2001). Lofexidine versus clonidine in rapid opiate detoxification. Journal of Substance Abuse Treatment, 11-17.
- Department of Defense Veterans Association. (2023). Defense and Veterans Pain Rating Scale. Retrieved from VA.gov: https://www.va.gov/PAINMANAGEMENT/docs/DVPRS_2slides_and_references.pdf
- Department of Health and Aged Care. (2013, January 20). FLACC Pain Scale. Retrieved from health.gov: https://www1.health.gov.au/internet/publications/publishing.nsf/Content/triageqrg~triageqrg-pain~triageqrg-FLACC
- Donaldson, S. L. (2017). Provider-Based Interventions to Mitigate Risk for Opioid Pain Medication Abuse Among Adult Patients in a Primary Care Setting.
- Dydyk, A. M., & Grandhe, S. (2023, January 29). Pain Assessment. Retrieved from STAT PEARLS: https://www.ncbi.nlm.nih.gov/books/NBK556098/#:~:text=Pain%20is%20the%20most%20common,pain%20in%20the%20United%20States.
- Fan, M., Hamilton, M., Hyland, B., & Tscheng, D. (2019). Diversion of Controlled Drugs in Hospitals: A Scoping review of Contributors and Safeguards. Journal of Hospital Medicine.
- GeriatricPain.org. (2022, January). Fast Facts: Selected Pain Assessment Tools. Retrieved from Geriatricpain.org: Geriatricpain.org https://geriatricpain.org/selected-pain-assessment-tools-fc
- Haffajee, R., Jena, A., Weiner, S., & & Kesselheim, A. (2019). Mandatory use of prescription drug monitoring programs. Journal of the American Medical Association, 1667-1668.
- International Association for the Study of Pain . (2020, July 16). IASP Announces Revised Definition of Pain. Retrieved from International Association for the Study of Pain : https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
- JAMA. (2023). Substance Use and Addiction Medicine. Retrieved from JAMA Network: https://jamanetwork.com/collections/5921/substance-use-and-addiction-medicine
- John, W. S., Schwartz, R. P., Subramanian, G., & Wu, L.-T. (2018). Prevalence, Patterns and correlates of multiple substance use disorders among adults. Drug and Alcohol Dependency, 79-87.
- Jones, C., Einstein, E., & Compton, W. (2018). Changes in synthetic opioid involvement in drug overdose deaths in the United States. JAMA, 1819-1821.
- Kalava, A., King, K. C., & Preuss, C. V. (2023, April 29). Perscription of Controlled Substances: Benefits and Risks. Retrieved from STAT PEARLS: https://www.ncbi.nlm.nih.gov/books/NBK537318/
- Khalid, N., Patel, P., & Singh, A. (2023, January). Cannabis Versus Opioids for Pain. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK573080/
- Kreutzwiser, D., & Tawfic, Q. (2020). Mathadone for Pain Management. A Pharmacotherapeutic Review, 827-839.
- Kroenke, K., Spiter, R., Williams, J., & Lowe, B. (2011, Nov). An ultra-brief screening scale for anxiety and depression: the PHQ-4. From Principles of Neuropathic Pain Assessment and Management, 613-21. Psychosomatics 2009.
- Manchikanti, L., Kaye, A., Knezevic, N., McAnally, H., Slavin, K., Trescot, A., & Hirsch, J. (2018). Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians guidelines. Pain Physician, S3-S92.
- Marquez, C. B. (2020). Changing the outlook toward the problem of opioid addiction: From “War on Drug” to “Public Health Emergency”. Seton Hall: Law Student Scholarship.
- Marsch, L., Borodovsky, J., & Dallery, J. (2019). Advances in the psychosocial treatment of addiction: The role of technology in the delivery of evidence-based psychosocial treatment. The Psyciatric Clinics of North America, 585-596.
- McLellan, T., & Volkow, N. (2016). Opioid Abuse in Chronic Pain-Misconceptions and Mitigation Strategies. New England Journal of Medicine, 1253-1263.
- National Institute of Drug Abuse (NIDA). (2023, August 30). Prescription Opioid Drug Facts. Retrieved from National Institute on Drug Abuse: https://nida.nih.gov/publications/drugfacts/prescription-opioids
- National Institute of Health. (2023, August 25). Medications for Opioid Overdose, Withdrawal, & Addiction. Retrieved from National Institute of Drug Addiction: https://nida.nih.gov/research-topics/opioids/medications-opioid-overdose-withdrawal-addiction-infographic
- Pain Physician. (2008). Opioid Special Issue. Pain Physician, S133-S153.
- Ransford, e. a. (2019, February 08). The Ransford Pain Drawing . Retrieved from compassionandsupport.org: https://compassionandsupport.org/wp-content/uploads/sites/2/2019/08/PainScaleRansford.pdf
- Rudd, R. A., Zibbell, J., & Gladden, M. (2016). Increases in drug and opioid overdose deaths-Untied States. Morbidity and Mortlity Weekly Report, 1378-1382.
- SAMHSA. (2020). Key Substance Use and Mental Health Indicators in the United States: Ressults from the 2019 National Survey on Drug Use and Health. SAMHSA.
- Scalpel, S. (2016, November). The Joint Commission Deserves Some Blame for the Opioid Crisis. Retrieved from Missouri Medicine: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6139759/
- Scholl, L., Seth, P., Kariisa, M., Wilson, N., & Baldwin, G. (2019). Drug and opioid-involved overdose deaths-Unioted States, 2013-2017. Morbidity and Mortatlity Weekly Report 67, 1419-1427.
- Stauffer, L., & Gibson, S. (2017). The Nurse’s Role in Identifying and Educating Patients At Risk for Opioid Abuse. AAACN Viewpoint, 1.
- The Joint Commission. (2023, January). The Joint Commission History Timeline. Retrieved from JointCommission.org: https://www.jointcommission.org/-/media/tjc/documents/tjc-history-timeline-through-2022.pdf
- Toombs, K., Kral, L., Colleran, C., & & Varney, S. (2018). Nurse practitioner-pharmacist collaboration in pain management: Strategies for success. . Journal of the American Association of Nurse Practitioners, 141-148.
- U.S. Food and Drug Administration. (2023, May 23). FDA. Retrieved from Information about Medication Assisted Treatment (MAT): https://www.fda.gov/drugs/information-drug-class/information-about-medication-assisted-treatment-mat
- Volkow, N., Jones, E., Einstein, E., & Wargo, E. (2019). Prevention and Treatment of Opioid mIsuse and Addiction: A Review. JAMA Psychiatry, 208-216.
References for New Mexico Prescribing Regulation:
- New Mexico Board of Nursing. 2023. APRN Prescriptive Authority. Retrieved from https://www.bon.nm.gov/aprn-prescriptive-authority/
- New Mexico Legislature. TITLE 16 Occupational and Professional Licensing. Chapter 12 Nursing and Health Care Related Providers
- PART 2 NURSE LICENSURE. Retrieved from https://www.srca.nm.gov/parts/title16/16.012.0002.html
- New Mexico Regulation and Licensing Department. 2023. Pharmacy Applications and Forms. Retrieved from https://www.rld.nm.gov/boards-and-commissions/individual-boards-and-commissions/pharmacy/pharmacy-applications-and-forms/
- United States Department of Justice (DOJ). 2024. Registration Applications, Tools, and Resources. Retrieved from https://www.deadiversion.usdoj.gov/drugreg/registration.html
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
