Course
Performing a Full Neurological Assessment
Course Highlights
- In this course we will learn about the components of a comprehensive neurological assessment, and why it is important for nurses to understand it in its entirety.
- You’ll also learn the basics of how to assess mental status, motor and sensory functions, and cranial nerves.
- You’ll leave this course with a broader understanding of how to complete a full neurological assessment.
About
Contact Hours Awarded: 1.5
Course By:
Cheryl Carlin
MSN, RN, CNE
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Assessment is a key component of nursing care. It establishes a baseline of the patient’s condition, informs the nurse of changes to the patient’s health status, and allows the nurse to evaluate if interventions have been effective. When working with patients who have suffered injury or impairment to the neurological system, a complex neurological assessment is often needed to guide care.
The purpose of this course is to guide nurses who are performing neurological assessments. We will identify the components of a neurological exam, discuss how the exam should be performed, and explore both normal and abnormal findings that may be seen.
What are the Components of the Nervous System?
The neurological system is complex and affects all other systems of the body. The nervous system is divided into the central nervous system and the peripheral nervous system. The central nervous system (CNS) consists of the brain and spinal cord. The brain is made up of the cerebrum (which includes the cerebral cortex), brain stem, and cerebellum. The peripheral nervous system (PNS) consists of the nerves, which are classified as cranial, spinal, peripheral, and association nerves, also known as interneurons, which link the sensory neurons and motor neurons within the CNS (8).
With both sensory and motor neurons, the peripheral nervous system is further divided into the autonomic nervous system and the somatic nervous system (9). The peripheral nervous system relays information about the environment back to the brain for interpretation and action. Responses can be automatic (or autonomic), or they can be conscientiously planned by the person.
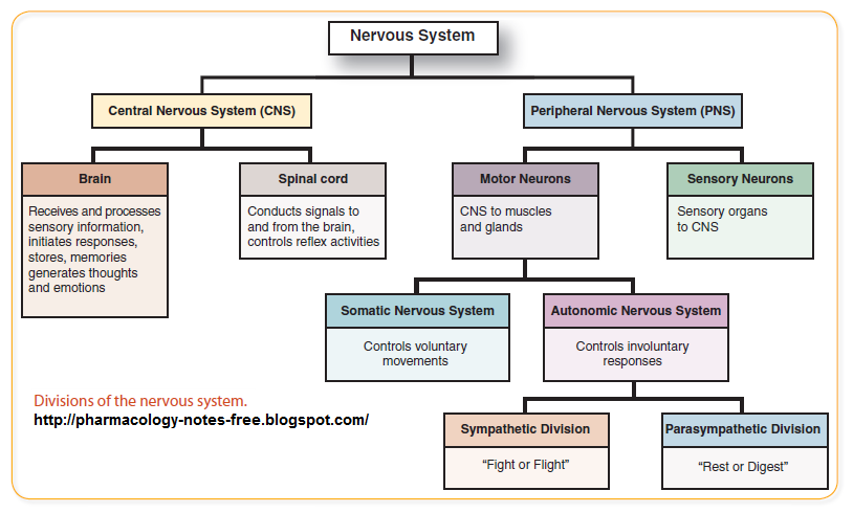
(13)
The Components of a Comprehensive Neurological Assessment
Assessing the nervous system should be a standard component of a basic physical assessment for every patient. As with any assessment, it is important to gather information from the patient before conducting the initial assessment. This will help to establish the patient’s baseline and help to identify other factors which might impact assessment findings. The nurse should question the patient about past medical history, current medications, environmental risk factors, and current functional level, making a note of any information relevant to the neurological system.
For an unconscious patient, the comprehensive neurological assessment is still done but without the verbal input of the patient. For patients who present with a stroke or head injury, a comprehensive neurological exam should be completed initially and regularly to assess for acute changes. An extensive neurological exam done for patients with a stroke includes a comprehensive neurological assessment and more and is known as the National Institute of Health Stroke Scale (NIH Stroke Scale) (12).
The comprehensive neurological assessment should evaluate the following:
- Mental status
- Motor function
- Sensory function
- Cerebellar function
- Cranial nerves
- Reflexes
Mental Status
Mental status is often one of the first aspects assessed during a comprehensive neurological assessment and provides information on cerebral functioning.
Key components of a mental status exam include general appearance, verbal response, behavior, cognition, and mood, also known as affect.
- General appearance is assessed by observing the patient. This assessment should include the level of consciousness, body posture, speech patterns, and patient’s movement. Previous assessments should be compared if possible. If previous assessments are not available, family members may offer insight as to the normal posture or speech patterns of the patient.
- The Glasgow Coma Scale is often used to assess the level of consciousness (LOC). It is typically used in patients with head injuries, stroke, or coma, but also has value in other situations to quickly determine the LOC. The scale looks at pupil size, verbal response, and motor response to determine a score. The score ranges from 3 to 15, and the higher the score the better. Patients with a score of less than 8 are usually in a comatose state. In patients who do not respond to verbal or touch stimuli, painful stimuli should be used to elicit a response. Common techniques include nail bed pressure, supraorbital pressure, trapezius grip, and a sternal rub (1).
- Cognition is assessed by determining orientation and memory. The nurse should determine the patient’s orientation to time, place, person, and situation by asking the patient to identify the current date, location, full name, and situation, or what brought them to the medical facility. Memory can be tested in a variety of ways.
Most commonly, it might be asking the patient common knowledge questions or giving the patient three words or phrases and then asking them to repeat these several minutes later. It is important to note that questions asked to determine cognition should not be above the patient’s intellectual ability.
A mini-mental state exam (MMSE) is an additional cognitive screening tool used to assess cognitive impairment, such as dementia (10).
- Mood and affect are assessed by observing the patient and asking questions regarding their mood. Mood and affect should be appropriate to the situation and should match. For example, a patient who states they are angry or sad but is smiling is abnormal.
|
Level of Consciousness Terminology |
|
| Fully Conscious |
Alert, oriented, is able to pay attention and respond. |
| Lethargic | Able to wake up but remains sleepy. Response to questions or commands is slow. |
| Obtunded | Difficult to arouse and keep awake. Can be awoken repeatedly to provide one- or two-word answers. |
| Stuporous | Requires repeated and often vigorous stimuli to awaken. |
| Coma | Does not respond to any type of stimuli. |

Self-Quiz
Ask Yourself...
The nurse is caring for a patient who is in recovery following orthopedic surgery. Upon approaching the patient’s bedside, the nurse observes the patient is lying in bed, and their eyes are closed.
- What type of stimuli would the nurse use to determine if the patient is arousable?
- The patient arouses but seems slow to respond to questions. During the assessment, the patient falls asleep. How would the nurse document the patient’s condition?
- Based upon what is known about the patient, is this a normal finding?
Components of the Nervous System (cont.)
Motor Function
Assessment of motor function evaluates strength, tone, coordination, and symmetry of muscles. Testing of motor function is more easily completed if the patient can follow instructions or commands. When testing motor function during a neurological assessment, it should be done bilaterally and simultaneously to compare each side. Muscle strength is graded on a scale from 0 to 5+, where 0 is no muscle contraction, 1+ is barely detectable, 2+ is active movement with assistance, 3+ is active movement without assistance, 4+ is active movement against some resistance, and 5+ is active movement with full resistance (5).
- Upper extremities: Begin the assessment by observing the upper extremities and shoulders for muscle atrophy, hypertrophy, asymmetrical development, fasciculations (twitching), myotonia (slow relaxation), tremors, or other involuntary movements (6).
Assess strength by having the patient move their arms independently and against resistance. Have the patient flex their arms, bending at the elbows, apply resistance to the lower arms, and ask the patient to straighten their arms. The nurse should ask the patient to grasp two of the nurse’s fingers and gently squeeze to assess for grip strength. Assess for pronator drift by asking the patient to close their eyes and to put arms out straight with palms up for 10 seconds (5). Downward drift is indicative of muscle weakness (5).
- Lower extremities: Begin by assessing the legs for muscle atrophy, hypertrophy, asymmetrical development, fasciculations (twitching), myotonia (slowed relaxation), tremors, or other involuntary movements (6).
Have the patient move their legs independently and against resistance. Have the patient attempt to lift the leg while applying resistance on the thigh or lower leg. Have the patient hold the leg straight and attempt to lift it against gravity.
Test foot strength by placing a hand on the patient’s foot and applying resistance as they flex and extend the foot.
- Posturing: Normal patient posture is relaxed, however, in patients with neurological injury, decorticate or decerebrate posturing may be present. Decorticate posturing occurs with damage to the corticospinal pathway (4).
In decorticate posturing, the patient’s arms are folded in, hands are turned inwards, and both legs and feet are extended.
Decerebrate posturing occurs with brainstem dysfunction (4). In decerebrate posturing, the patient’s body is rigid, arms are extended and turned out, both legs and feet are extended, and often spasms cause the body to arch.


Self-Quiz
Ask Yourself...
The nurse is assessing a patient and determines the patient has muscle strength of 2+ in the left upper extremity and 4+ in the right upper extremity.
- What further assessments of motor function should the nurse make?
Components of the Nervous System (cont.)
Sensory Function
During a neurological assessment, peripheral or spinal nerve impairment can be determined by identifying a patient’s sensory function. Assessment of the sensory system includes tactile, superficial pain, temperature, vibration, and proprioception or body awareness (3).
The patient needs to be alert and able to follow instructions to complete the assessment. The exam should occur with the patient’s eyes closed, and there should be pauses between stimulations to prevent it from being perceived as one long stimulation (5).
- Tactile: Using a cotton ball, touch the patient on the face and ask them to state where the sensation is felt (5). This can also be done using a finger and asking where the patient feels the touch (5).
- Superficial Pain: Use a sharp object, such as a clean safety pin or a broken cotton swab tip, lightly touch the skin, asking the patient where the sensation is felt (5).
- Temperature: This is only tested if tactile and painful stimulation cannot be felt (3, 5). Use a warm or cold object, apply it to the skin, and ask the patient which sensation is felt.
- Vibration: Strike a tuning fork on the palm and, holding only the base of the fork, place one finger under one of the patient’s distal phalangeal joints and place the tuning fork on the top of the joint (6). Have the patient indicate when they start and stop feeling the vibration. They should stop feeling it at the same time as the nurse stops feeling it through the bottom of the joint (6).
- Proprioception: Have the patient close their eyes and, starting at the most distal joint, move the toe or finger up and down a few degrees to determine if the patient can identify the movement (5, 6). If they cannot then move to the next proximal joint (5, 6).

Self-Quiz
Ask Yourself...
The nurse is accessing sensory function in a patient. The patient is unable to identify either touch or pain.
- What further action should be taken by the nurse?
Components of the Nervous System (cont.)
Cerebellar Function
The cerebellar function is evaluated by looking at both coordination and balance. Testing of cerebellar function can only be completed if the patient can follow commands. The nurse should test the upper extremities, lower extremities, and balance. The inability to do these activities smoothly or if the patient is unable to maintain their balance are abnormal findings, and the patient should be further evaluated for a problem in the cerebellum (4).
- Upper extremities: Have the patient perform rapid alternating movements and point-to-point testing (3). The patient should place the hand’s palm up and then palm down as quickly as possible (3). Then have the patient put their arms out to the side and touch the finger to the nose several times, with eyes open and then eyes closed (4).
- Lower Extremities: Have the patient sit or lie down, then run the heel of one foot down the shin of the other leg. The patient should be able to do this smoothly with both legs.
- Balance: In a mobile patient, this should be done by having the patient walk normally on heels, toes, and then heel-to-toe in a straight line while observing the patient’s gait. The inability to maintain balance, swaying, or a staggering gait is an abnormal finding (7).
A Romberg test is also commonly performed to test equilibrium. To complete this exam, the nurse should have the patient keep their eyes open and stand with their arms at their side and their feet together. Observe for swaying. Then ask the patient to close their eyes and again observe for swaying. If swaying only occurs when the eyes are closed, it is related to proprioception (7). However, if the patient is unable to balance regardless of if the eyes are opened or closed, this lack of balance is more indicative of a problem in the cerebellum (4).

Self-Quiz
Ask Yourself...
The nurse is caring for a patient with a spinal cord injury at the 2nd lumbar vertebrae.
- How might the nurse test this patient’s cerebellar function?
Comprehensive Neurological Assessment (cont.)
Cranial Nerves
Cranial nerves (CN) are the only nerves branching from the brain instead of the spinal column. While abnormal findings in a CN assessment may indicate dysfunction within the brain, disorders affecting the nerve or injury to the nerve may also result in abnormal findings.
|
Cranial Nerve Assessment |
|
|
Cranial Nerve |
Assessment |
| I – Olfactory | Assess the patency of nares first. Have the patient close the eyes, close one nare, and have them inhale an easily recognizable scent. Repeat on the other nare. Inability to smell the scent is an abnormal finding (5). |
| II – Optic | Test visual acuity using a Snellen chart or other visual acuity charts. If the patient typically wears corrective lenses, identify what the patient’s normal acuity is with and without correction if possible. Changes to the patient baseline should be considered abnormal (5). |
| III – Oculomotor | III, IV, and VI work together and are therefore tested together. Assess pupil size, shape, and symmetry, test for accommodation and convergence, and test cardinal gaze by having the patient follow a penlight or finger among all four quadrants, across the midline and towards the nose (5). Abnormal findings would include unequal size, shape, and reaction, presence of nystagmus, or inability to follow objects (5). |
| IV – Trochlear | |
| VI – Abducens | |
| V – Trigeminal | Using a cotton ball and a sharp object, touch the scalp, cheeks, and chin, asking the patient to identify if it is soft or sharp. Dull or absent sensation is an abnormal finding (5). Check for the corneal reflex by lightly touching a fluffed piece of cotton to the sclera of the eye. If the reflex is present (normal) the patient should blink. |
| VII – Facial | Check for symmetrical facial movement by having the patient smile, raise eyebrows, show teeth, puff out cheeks, and purse lips (5). You can also test for the ability to taste by applying sour, sweet, bitter, and salty solutions to one side of the tongue than the other (5, 6). |
| VIII – Vestibulocochlear | Assess for the ability to hear during normal conversation (5). Assess if the patient has a history of hearing loss and uses a hearing aid or has an implant. For patients without hearing aids, test for hearing can also be done by whispering or rubbing fingers together near the ear. If the patient is unable to hear, a Rinne or Weber test may be performed. |
| IX – Glossopharyngeal | Assess for difficulty with swallowing (5). If the patient does not have any known restrictions, offer a small sip of water and observe for inability to swallow, coughing, choking, or repeated swallowing. Difficulty swallowing is often seen in patients who have suffered from a stroke. Further neurological evaluation and possibly evaluation by a speech therapist are needed if the patient has any difficulty with swallowing. |
| X – Vagus | Have the patient stick out their tongue and check if it is midline (5). Also, check for a midline uvula and the presence of a gag reflex (5) using a tongue depressor. |
| XI – Accessory | Place a hand on one side of the patient’s chin and ask the patient to press against the resistance, then repeat on the other side (5). Also, apply resistance to the shoulders and ask the patient to shrug (5). Weakness or unequal strength are abnormal findings (5). |
| XII – Hypoglossal | Have the patient stick out their tongue and assess for symmetry (5). |
Because CNs often work in conjunction with one another, additional assessments such as pupil response (CN II and III), corneal reflex (CN V and VII), and gag reflex (CN IX and X) are performed. While these assessments are done as a full CN assessment, they can also be done independently.
The nurse caring for these patients needs to be aware that abnormal findings in these assessments may be indicative of a single-nerve or multiple-nerve dysfunction. If abnormalities are found in any of the cranial nerves, after documenting the findings, the nurse should always include safety actions in the care plan as the patient may be at risk for falls or choking.
It is also important to note the role of the vagus nerve (CN X) in regulating heart rate, respiratory rate, and vasomotor activity. Conditions affecting the vagus nerve, such as traumatic brain injury, can result in alterations in respiration, pulse, and blood pressure. Because of this, vital signs should also be a component of a complete neurological assessment.


Self-Quiz
Ask Yourself...
After completing a CN assessment on a patient, the nurse identifies the abnormal findings in CN VII, IX, and X.
- How does this finding impact the plan of care?
Comprehensive Neurological Assessment (cont.)
Reflexes
Reflexes are involuntary movements as a result of a stimulus. Two types of reflexes can be assessed: deep tendon reflexes (DTR) and superficial reflexes. DTRs are rated on a scale of 0-4+, with 0 being absent, 1+ is weak or hypoactive, 2+ is normal, 3+ is brisk, and 4+ is exaggerated or hyperactive (2).
If a reflex is stimulated and clonus (uncontrollable shaking) occurs, it is also rated as a 4+ (2). Abnormal findings (absent, hypoactive, or hyperactive) may be indicative of a neurological disorder, and in some cases, may be the first sign of a degenerative neurological disorder (2).
DTRs are tested using a reflex hammer. The reflex occurs when the hammer strikes the tendon, which connects a muscle to a bone, causing the muscle to contract. DTRs should be tested bilaterally and include the following reflexes (11):
- Biceps: Flex the arm at the elbow and ensure the palm is down. Place a thumb or finger over the bicep tendon. Strike the thumb or finger with the reflex hammer. The bicep should contract, and there should be flexion at the elbow.
- Triceps: Flex the elbow and turn the palm towards the body. Find the tricep muscle and strike the tendon just above the elbow. The elbow should extend, and the tricep should contract.
- Brachioradialis: The nurse should flex the arm at the elbow and rest the patient’s forearm on their arm. The brachioradialis tendon sits between 1-2 inches above the wrist on the thumb side. When the tendon is struck with the reflex hammer, the thumb will flex in, the elbow will flex, and the brachioradialis muscle will contract.
- Patellar: Sitting up, having the patient dangle their lower legs. Palpate for the patellar tendon just below the edge of the patella. When struck with a reflex hammer, the quadricep will flex, and the lower leg will extend.
- Achilles: With the patient sitting and legs dangling, palpate for the Achilles tendon on the back of the ankle. When the tendon is struck, the foot should plantarflex, and the large calf muscle (gastrocnemius) will flex.
Superficial reflexes are elicited by touching the skin or other surfaces, such as a mucous membrane or the cornea of the body. The corneal and gag reflex are technically superficial reflexes but are tested as part of the cranial nerve assessment.
While primitive reflexes are superficial reflexes, the only one typically assessed in adults is the plantar reflex. To elicit this reflex, a pointed object is stroked across the bottom of the foot. In adults, a normal finding is plantar flexion of the foot and toes. If the big toe extends and the toes splay, the patient has a positive Babinski sign. In patients over the age of 2, this often indicates some type of brain injury.

Self-Quiz
Ask Yourself...
The nurse is reviewing a reflex assessment of a patient and observes DTRs of 1+ in both triceps and 2+ in both biceps.
- How does the nurse interpret this assessment?
Conclusion
The neurological system interacts with and impacts other body systems and being able to identify potential problems early allows the nurse to intervene, potentially preventing lasting neurological damage. While comprehensive neurological assessments are commonly performed by nurses working in acute neurological units, they can be completed on any patient as an initial and follow-up assessment. A shortened version of the comprehensive neurological exam can be performed as part of a rapid assessment or general physical exam. Every nurse should be armed with the knowledge and skills to complete a comprehensive neurological assessment.
References + Disclaimer
- Cook, N. F., Braine, M. E., & Trout, R. (2019). Nurses’ understanding and experience of applying painful stimuli when assessing components of the Glasgow Coma Scale. Journal of Clinical Nursing, 28, 3827-3839. https://doi.org/10.1111/jocn.15011
- Gilreath-Osoff, A. & Caple, C. (2018). Neurological assessment: Assessing reflexes. CINAHL Nursing.
- Hinkle, J. L. & Cheever, K. H. (2018). Brunner & Suddarth’s textbook of medical-surgical nursing (14th ed.). Wolters Kluwer.
- Ignatavicius, D. D., Workman, M. L., & Rebar, C. R. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care (9th ed.). Elsevier.
- Jensen, S. (2019). Nursing health assessment: A best practice approach (3rd ed.). Wolters Kluwer.
- Newman, G. (2020). Neurological examination. https://www.merckmanuals.com/professional/neurologic-disorders/neurologic-examination/introduction-to-the-neurologic-examination
- Stanford Medicine. (2021). Introduction to cerebellar exam. https://stanfordmedicine25.stanford.edu/the25/cerebellar.html
- U.S. Department of Health and Human Services. National Institutes of Health. What are the parts of the nervous system? Retrieved from https://www.nichd.nih.gov/health/topics/neuro/conditioninfo/parts
- National Institute of Neurological Disorders and Stroke. (2018). Brain basics: Know your brain. Retrieved from https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Know-Your-Brain
- Su, Y., Dong, J., Sun, J. et al. Cognitive function assessed by Mini-mental state examination and risk of all-cause mortality: a community-based prospective cohort study. BMC Geriatr 21, 524 (2021). https://doi.org/10.1186/s12877-021-02471-9.
- Shahrokhi M, Asuncion RMD. Neurologic Exam. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557589/
- National Institute of Health Stroke Scale. 2024. Retrieved from https://www.ninds.nih.gov/health-information/public-education/know-stroke/health-professionals/nih-stroke-scale
- Socratic.org. (2017). What are the primary divisions and subdivisions of the nervous system? https://socratic.org/questions/what-are-the-primary-divisions-and-subdivisions-of-the-nervous-system
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
