Course
Puerto Rico APRN Bundle Part 1
Course Highlights
- In this course, we will learn about the importance of bioethics in nursing practice.
- You’ll also learn the basic infection control practices and how to apply them.
- You’ll leave this course with a broader understanding of commonly prescribed opioids for pain management and understand their side effects and indications of use.
About
Contact Hours Awarded: 20
Pharmacology contact hours included: 5
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
Bioethics in Nursing
Introduction
Nursing practice is deeply rooted in ethical principles that guide decision-making and client care. Bioethics is a crucial aspect of healthcare that provides a framework for analyzing ethical dilemmas and promoting individualized client-centered care respectfully and compassionately. Nursing ethics involves applying bioethical principles in practice, such as maintaining client confidentiality and respecting autonomy. Nurses face ethical dilemmas regularly. One of the most common is providing care that conflicts with personal beliefs (6).

Self Quiz
Ask yourself...
- How do you think bioethics influences nursing practice
- What are some examples of ethical dilemmas nurses may face?
- Can you describe a situation where a nurse's personal beliefs conflicted with their professional obligations?
- How would you navigate such a scenario?
Definition and Purpose
Bioethics is the study of ethical and moral principles guiding healthcare decisions and practices (10). Its purpose is to ensure that healthcare providers make informed decisions that respect clients' values, beliefs, and rights (5).
Bioethics provides a framework for analyzing ethical issues in healthcare while considering the interests of the clients, their families, and the healthcare providers involved in their care (5). By understanding the definition and purpose of bioethics, nurses can develop a strong foundation for addressing ethical challenges in practice, such as informed consent, client confidentiality, and when it may infringe upon others’ health and proper resource allocation (5,6,10).


Self Quiz
Ask yourself...
- How does the definition of bioethics impact its application in nursing practice?
- What are some potential consequences of ignoring ethical principles?
- Can you think of a situation where a nurse's understanding of bioethics helped them navigate an ethical dilemma?
- What was the outcome?
Principles of Bioethics
The principles of bioethics include autonomy, beneficence, non-maleficence, and justice (5,6,7,9). Autonomy respects clients' decision-making capacity, beneficence promotes a client's well-being, non-maleficence avoids any harm to the client, and justice ensures fairness and equity for all involved in the client’s care (5,6,9).
These principles serve as the guiding force in nursing practice; influencing the decisions related to client care, research, and policy development (1). Autonomy empowers clients to make informed choices about their care (5,6,9). This may include decisions that the client’s family and even healthcare providers may disagree with personally. Beneficence compels nurses to act in the best interests of their clients and advocate for the client’s desires (5,6,9). Non-maleficence reminds nurses to avoid causing harm; this includes not just physical but emotional and mental harm as well (5,6,9).

Self Quiz
Ask yourself...
- How do the principles of bioethics guide nursing practice?
- What are some examples of how these principles are applied in different healthcare settings?
- Can you describe a situation where a nurse had to balance the principles of autonomy and beneficence in their practice?
- How did they navigate this ethical dilemma?
Types of Ethics and Professions
Different professions have specific ethical guidelines, such as the American Nurses Association (ANA) Code of Ethics for nurses (1). Understanding the ethical framework of various professions is essential to the interdisciplinary healthcare approach.
Interdisciplinary collaboration requires an understanding of diverse ethical perspectives and principles, an approach that coincides with an equally diverse client population. Nurses should be aware of the ethical guidelines that govern their practice and be able to apply them in diverse healthcare settings. They must also be aware of their own beliefs and guidelines and how these may affect their decision-making, adversely affecting client care (5,6).

Self Quiz
Ask yourself...
- How do different professional ethical guidelines impact interdisciplinary collaboration?
- What are some potential consequences of ignoring these guidelines?
- Can you describe a situation where a nurse had to navigate an ethical dilemma with an interdisciplinary team?
Ethics in Nursing
Nursing ethics involves applying principles in practice that benefit the client, healthcare providers, and loved ones of the client. Examples include things such as maintaining client confidentiality and respecting autonomy, helping the client make the right decision for themselves, and advocating for those decisions to others (1,5). One of the most difficult decisions nurses face involves those that conflict with their personal belief system (6).
Nurses must be equipped with the knowledge and skills to navigate these ethical challenges and provide care that respects clients' values and beliefs while also nurturing their thoughts and feelings (6). By exploring bioethics in nursing, we can promote a culture of ethical practice that is compassionate and client-centered.
Henrietta Lacks Story
Henrietta Lacks was a Black tobacco farmer who had her cancer cells taken without her knowledge or consent which led to numerous scientific breakthroughs, including the development of the polio vaccine (7,8). Her story raises important questions about medical ethics, racism, and the intersection of science and human compassion.
In 1951, Henrietta Lacks was diagnosed with cervical cancer and began treatment at Johns Hopkins Hospital in Baltimore. During her treatment, a sample collection of her cancer cells was taken by her doctor, Dr. George Gey without her knowledge and or consent (7,8). Dr. Gey discovered that Henrietta's cells were extraordinary in nature and could be of great value for cancer research and future developments as they could survive and thrive in a laboratory setting thus making them ideal for scientific research.
Henrietta's cells, known as HeLa cells, were soon being used in laboratories worldwide, leading to numerous scientific breakthroughs, including the polio vaccine development, in vitro fertilization, and gene mapping (7,8). However, Henrietta's family was never informed or financially compensated for the use of her cells, and her story remained largely unknown until the publication of Rebecca Skloot's book "The Immortal Life of Henrietta Lacks" in 2010 (2).
Henrietta's story highlights the unethical practices that were common in the medical field at the time, particularly in relation to clients that lacked resources, particularly those belonging to minority groups (2). Her cells were taken without her consent, and she was never compensated or acknowledged for her contribution to science. This raised some very important questions about medical ethics, informed consent, and the exploitation of vulnerable populations.
Still, Henrietta's story is a powerful reminder of the intersection of science and the need for personal autonomy. Her cells have been used to advance scientific knowledge, but they also represent a person, a family, and a community. The use of her cells without her consent or compensation is a violation of her humanity and a reminder of the need for ethical considerations in scientific research.

Self Quiz
Ask yourself...
- How do nursing ethics impact patient care?
- What are some potential consequences of ignoring ethical principles in practice?
- Can you describe a situation where a nurse's understanding of ethics helped them provide high-quality care
- What were the benefits for the patient?
Tuskegee Syphilis Experiments
The Tuskegee Syphilis Study was a highly controversial and unethical medical experiment conducted on African American men in Macon County, Alabama between 1932 and 1972 (4,11). The study, led by the Department of U.S. Public Health Services, involved withholding treatment from hundreds of African American men infected with syphilis despite the availability of effective therapies, to study the natural progression of the disease (4,11).
The men, who were mostly illiterate and poor, were not informed that they had syphilis, their partners were not informed of the disease, nor were they given treatment for the disease (4,11). Instead, they were given placebos and misleading information about their condition. The study continued for 40 years, during which time many of the men died from syphilis-related complications, and many others suffered serious health problems which included the spreading of syphilis to unsuspecting sexual partners.
The Tuskegee Syphilis Study is widely regarded as one of the most unethical medical experiments in history. The study was conducted without the men's knowledge or consent, and it violated basic human rights and principles of medical ethics. By way of public outcry and shock, the awareness of these experiments led to major changes in the way human subjects are protected in medical research and a desire for closer oversight by governing groups.
In 1974, a class-action lawsuit was filed on behalf of the men who were involved in the study, resulting in a multimillion-dollar settlement (11). The study also led to the establishment of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, which developed guidelines for the ethical conduct of research involving human subjects (11).
The Tuskegee Syphilis Study has had a lasting impact on the field of medicine and beyond. It highlighted the importance of informed consent and the need for ethical oversight in the field of medical research. It has also led to the increased scrutiny of medical experiments and a greater emphasis on protecting human subjects, their privacy, and most importantly honest care and explanations of medical conditions and treatments.
Today, the Tuskegee Syphilis Study is remembered as a cautionary tale about the dangers of unethical medical research. It serves as a reminder of the importance of prioritizing the well-being and safety of people and the need for ongoing vigilance in ensuring that medical research is conducted ethically and responsibly, and ensuring there are the proper checks and balances in place to provide the oversight needed.
The study also highlighted the need for diversity in medical research and the importance of including diverse populations in clinical trials (11). It led to increased efforts to address health disparities and to ensure that medical research is conducted in a way that is fair and equitable to all.
In addition, the Tuskegee Syphilis Study led to changes in the way that medical research is regulated and overseen (11). It led to the establishment of institutional review boards (IRBs) and independent ethics committees (IECs) which are responsible for reviewing and approving research protocols and ensuring they meet the ethical standards set in place (11).
Transparency and accountability in medical research have also been placed at the forefront of research since these events took place. Highlighting the importance of disclosing potential conflicts of interest and ensuring research is conducted in a way that is transparent and open to scrutiny; there inevitably was major change and growth that came from this huge medical injustice.
The Tuskegee Syphilis Study was a highly unethical and controversial medical experiment that had a profound impact on the field of medicine and beyond. It highlighted the importance of informed consent, ethical oversight, and diversity in medical research, and led to major changes in the way medical research is conducted and regulated. In these ways, it acted as a catalyst of growth and change in the way the U.S. views and treats research participants. It serves as a reminder of the need for ongoing vigilance in ensuring medical research is conducted ethically and responsibly.
The Tuskegee Syphilis Studies and Henrietta Lacks' cases highlight the importance of informed consent in research.
Other examples include: (5,9)
- Abortion and reproductive rights
- Euthanasia and end-of-life care
- Gene editing and genetic research
- Healthcare access and disparities


Self Quiz
Ask yourself...
- How do bioethical issues like informed consent impact healthcare outcomes
- What are some potential consequences of ignoring these issues?
- Can you describe a situation where a bioethical issue like euthanasia sparked a debate?
- How did healthcare professionals navigate this ethical dilemma?
Research in Ethics
Research ethics involves applying bioethical principles in research (3). Obtaining informed consent and ensuring participant confidentiality are two ways in which the provider can best provide ethical care to those that entrust the healthcare system with their voluntary well-being.
Researchers must be aware of ethical principles that guide research and ensure their studies are conducted ethically and responsibly which puts the client first (3).
Ethical Decision-Making
Ethical decision-making involves critical thinking, moral principles, and professional standards. Nurses can use ethical frameworks, such as the MORAL model and Nursing Process model, to guide decision-making (5). Ethical decision-making is a crucial aspect of nursing practice as it enables nurses to navigate complex healthcare issues and promote clients' well-being.

Self Quiz
Ask yourself...
- How do ethical principles guide research?
- What are some potential consequences of ignoring these principles?
- Can you describe a situation where a researcher had to navigate an ethical dilemma in their study?
Conclusion
Bioethics plays a vital role in nursing practice, ensuring that clients receive respectful and compassionate care. Understanding bioethical principles and applications is essential for nurses to provide high-quality care. By applying ethical principles and frameworks, nurses can navigate complex healthcare issues and promote clients' well-being.

Self Quiz
Ask yourself...
- How does the ethical framework guide decision-making in nursing practice and what are some potential consequences of ignoring these frameworks?
- How do personal values and beliefs impact nursing practice what are the implications for patient care?
- How does the principle of autonomy impact informed consent in healthcare?
- What are some potential consequences of prioritizing beneficence over non-maleficence in healthcare, and how can nurses balance these principles?
- How does the concept of justice impact healthcare resource allocation and what are the implications for nurses and patients?
- How do nurses balance the need for patient confidentiality with the need for transparency?
- What are some potential consequences of ignoring the principle of non-maleficence in healthcare, and how can nurses prioritize patient safety?
- How does the principle of autonomy impact patient decision-making?
- How do nurses balance the need for patient education with the need for autonomy?
- Are there any potential consequences for prioritizing patient satisfaction over patient well-being?
- How does the concept of vulnerability impact healthcare ethics?
- How do nurses balance the need for patient advocacy with the need for patient autonomy?
- What are some potential consequences of ignoring the principle of justice in healthcare?
- How does the principle of beneficence impact healthcare resource allocation?
- How do nurses balance the need for patient education with the need for patient confidentiality?
- What are some potential consequences of prioritizing patient well-being over patient autonomy?
- Could the Henrietta Lacks case and the Tuskegee Syphilis cases have an affect the way minorities view medical treatment in the U.S?
Infection Control and Barrier Precautions
Introduction
Healthcare professionals are responsible for adhering to scientifically accepted principles and practices of infection control in all healthcare settings. Healthcare professionals also oversee and monitor those medical and ancillary personnel for whom the professional is responsible, including nurses. The following sections explore the sources and definitions of standards of professional conduct as they apply to infection prevention and control (1,2).
Element I – Infection Control and Prevention Overview
As the largest healthcare workforce in the nation, nurses can positively affect infection rates at the bedside and within healthcare centers. Various agencies, workplaces, institutions, and legislation influence infection control and prevention recommendations, guidelines, and policies. As science and evidence-based research evolves, so does the role of infection control and prevention. It is important to remember that nurses set the stage for infection control and prevention efforts from the patient's point of view, as there was a time when nurses would care for patients without wearing gloves or washing hands. Hand washing, wearing gloves, and using masks are much more commonplace than ever in healthcare (1,2,3).
Implications of Professional Conduct Standards
As healthcare professionals who participate in and supervise patient care, nurses are responsible for knowing the guidelines set by their local, state, and federal legislation and nursing boards.
The responsibility also applies to delegated activities to other healthcare personnel. The nurse must ensure that the five delegation rights are considered when assigning a task to unlicensed assistive personnel (UAP) and that appropriate infection control policies and protocols are followed appropriately. Refer to facility policies and procedures to avoid potentially adverse outcomes (3,4).
Failure to follow the accepted infection prevention and control standards may have serious health consequences for patients and healthcare workers. Hospital-acquired infections (HAI) have increased overall in the past decade in all infections, including central line-associated bloodstream infections (CLABSI), catheter-associated urinary tract infections (CAUTI), ventilator-associated infections, and methicillin-resistant Staphylococcus aureus (MRSA) (5,6). The chain of command should first be utilized when nurses observe incompetent care or unprofessional conduct regarding infection control standards.
Considering the type of misconduct, the infection control violation should be addressed according to facility policy. Charge nurses and managers would be wise to first address the issue with the nurse involved to gather information and address any education deficits. In cases where apparent misconduct is evident, management and workplace facilities should address infection control and prevention efforts. Severe misconduct may result in the loss or revocation of a nursing license. Also, in cases where the neglect to follow appropriate conduct has harmed a patient or coworker, there is potential for professional liability through a malpractice suit brought against the nurse (5,6,7,8,9).
Methods of Compliance
Nurses are responsible for knowing the licensure guidelines, renewal of continuing education, and targeted education in their state(s) of practice. Education on infection control best practices, compliance with local and state requirements, and following facility practices and policies will provide the best protection for self, patients, and staff in preventing and controlling infection during patient care.


Self Quiz
Ask yourself...
- What are the consequences of a one-size-fits-all method for infection prevention?
- What are some infection control and prevention concerns you witness in your current workplace?
- How have infection control and prevention efforts changed throughout your nursing career?
- What is the policy in your workplace for reporting an infection control issue?
- How has infection control evolved in your workplace since the COVID-19 pandemic?
- How could natural disasters, such as hurricanes or tornadoes, influence the spread or development of infectious diseases?
Element II – Modes of Transmission
Modes and mechanisms of transmission of pathogenic organisms in the healthcare setting and strategies for prevention control.
Definitions:
Pathogen or infectious agent: A biological, physical, or chemical agent capable of causing disease. Biological agents may be bacteria, viruses, fungi, protozoa, helminths, or prions.
Portal of entry: How an infectious agent enters the susceptible host.
Portal of exit: The path by which an infectious agent leaves the reservoir.
Reservoir: A place in which an infectious agent can survive but may or may not multiply or cause disease. Healthcare workers may be a reservoir for several nosocomial organisms spread in healthcare settings, allowing an infection to be spread outside of healthcare settings into the general public.
Standard precautions: A group of infection prevention and control measures that combine the significant features of Universal Precautions and Body Substance Isolation and are based on the principle that all blood, body fluids, secretions, excretions except sweat, non-intact skin, and mucous membranes may contain transmissible infectious agents.
Susceptible host: A person or animal not possessing sufficient resistance to a particular infectious agent to prevent contracting infection or disease when exposed.
Transmission: Any mechanism by which a source or reservoir spreads a pathogen to a person.
Standard vehicle: Contaminated material, product, or substance that serves as a means of transmission of an infectious agent from a reservoir to one or more susceptible hosts through a suitable portal of entry (11,12,13).
Component of the Infectious Disease Process
The infectious disease process follows a particular sequence of events commonly described as the chain of infection. Nurses must have a solid understanding of this process to identify points in the chain where the spread of infection may be prevented or halted.
The sequence involves six factors: pathogen, reservoir, portal of exit, portal of entry, mode of transmission, and a susceptible host. The chain's cyclical and consistent nature provides many opportunities to use scientific, evidence-based measures to combat infection spread (11-19).
Pathogens within healthcare are widespread and plentiful, putting patients and healthcare workers at particular risk for contamination. The manifestation of symptoms and mode of transmission varies depending upon the characteristics of the specific infectious agent.
Healthcare workers are at a considerably higher risk for bloodborne pathogens, such as human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV). Influenza, methicillin-resistant Staphylococcus aureus (MRSA), COVID-19, and Tuberculosis (TB) also pose a higher risk and can lead to chronic health damage. Due to the immunocompromised systems of several patients, pathogens cause a considerable risk. They can result in HAIs, such as CLABSIs, CAUTIs, surgical site infections (SSI), and ventilator-associated pneumonia (VAP).
Pathogens require a reservoir, typically a human or animal host; however, they may also be from the environment, such as standing water or a surface. The pathogen is spread from the reservoir via a mechanism such as body fluid, blood, and secretions. Common sites for contact within patient care include the respiratory, genitourinary, and gastrointestinal tracts, as well as skin/mucous membranes, transplacental, or blood. From here, the mechanism must come into contact with another portal of entry. Transmission may occur through respiratory, genitourinary, and gastrointestinal tracts, skin and/or mucous membranes, and parenteral pathways. Some sites may have compromised during patient care due to percutaneous injury, invasive procedures or devices, or surgical incisions.
To acquire a pathogen, a mode of transmission must be provided. Transmission can be from contact, transmission via a standard vehicle, or vector-borne (11-19).
Contact with a pathogen may be categorized as direct, indirect, droplet, or airborne. Contact transmission is through direct or indirect contact with a patient or objects in contact with the patient. Pathogens related to this include Clostridium difficile and multidrug-resistant organisms such as MRSA. Droplet transmission occurs when a pathogen can infect via droplets through the air by talking, sneezing, coughing, or breathing. The pathogen can travel three to six feet from the patient. Airborne transmission occurs when pathogens are 5 micrometers or smaller in size and can be suspended in the air for long periods.
These pathogens include TB, measles, chickenpox, COVID-19 disseminated herpes zoster, and anthrax. Transmission may also occur through a standard vehicle that affects multiple hosts and can come from food, intravenous fluid, medication, biofilms, or shared equipment (fomites), often leading to widespread outbreaks. Vector-borne pathogens are derived from living vectors such as mosquitoes, fleas, or ticks. The last factor in the chain of infection is a susceptible host with a mode of entry. This is why patients are at a much higher risk for developing secondary infections within the healthcare system, even if they had no infection before admission (11-19).

Factors Influencing the Outcome of Exposures
The human body provides several natural defenses against acquiring infection from a pathogen. The most prominent defense is the integumentary system, and the focus should be on maintaining skin integrity to prevent a mode of entry. This is especially true for patients who are immobile or unable to move without assistance, such as those who are post-operative, those with physical disabilities, or those who have extensive nerve damage—respiratory cilia function to move microbes and debris from the airway. Gastric acid is at a pH that prevents the growth of many pathogens. Bodily secretions provide defense through flushing out and preventing back-flow of potential infectious agent colonization. The normal flora within the gastrointestinal system also provides a layer of defense that must be protected from the action of antibiotics. Probiotics are commonly administered to patients on antibiotics to prevent a secondary infection due to disrupted normal flora. Host immunity is the secondary defense that utilizes the host’s immune system to target invasive pathogens. There are four types of host immunity(11-19):
- The inflammatory response is pathogen detection by cells in a compromised area that then elicit an immune response that increases blood flow. This inflammatory provides delivery of phagocytes or white blood cells to the infected site response. Phagocytes are designed to expunge bacteria.
- Cell-mediated immunity uses B-cells and T-cells, specialized phagocytes, which are cytotoxic cells that target pathogens.
- Humoral immunity is derived from serum antibodies produced by plasma cells.
- Immune memory is the immune system's ability to recognize previously encountered antigens of pathogens and effectively initiate a targeted response.
Pathogen or Infection Agent factors
For each type of infectious agent, specific factors determine the risk to the host. Infectivity refers to the number of exposed individuals that become infected. Pathogenicity is the number of infected individuals that develop clinical symptoms, and virulence is the mortality rate of those infected. The probability of an infectious agent causing symptoms depends upon the size of the inoculum (amount of exposure) and the route and duration of exposure. The environment is another factor that warrants attention in limiting the probability of exposure in the healthcare setting. Fomites are materials, surfaces, or objects capable of harboring or transmitting pathogens. Common fomites can be bedside tables, scrubs, gowns, bedding, faucets, and other items in contact with patients and healthcare providers. Equipment may factor into the spread of infection; incredibly portable medical equipment can contact numerous patients daily. This can include vital signs monitoring machines, IV pumps, wheelchairs, and computers on wheels, among countless other care items frequently used. Care must be taken to ensure cleaning in between each patient’s use. For patients in isolation precautions, dedicated equipment for that patient should remain in the room for the duration of their stay (11-17).
Methods to Prevent the Spread of Pathogenic Organisms
Standard Precautions
Standard precautions are the minimal caution and procedure applied to typical patient care. The basis of standard precautions is proper hand hygiene performed by healthcare providers, patients, and visitors. Standard precautions provide guidelines for respiratory hygiene and cough etiquette. As a result of the COVID-19 pandemic and emerging respiratory pathogen resurgence, such as TB and measles, many healthcare facilities are implementing masking for patients and staff, regardless of confirmed case or not, as part of their standard precautions. Hand hygiene must be performed after contact with respiratory secretions or potentially contaminated items. As mentioned, healthcare workers are at a higher risk for bloodborne infections due to the handling of sharps. Needle stick and sharps injuries are reported by healthcare workers in hospitals and outpatient care settings in upwards of 100,00 cases each year. Specific spinal procedures that access the epidural or subdural space provide a means of transmission for infections such as bacterial meningitis (7,8,15-22).
For Patients Infected with Organisms Other Than Bloodborne Pathogens
Special considerations must be given to patient populations infected with organisms other than bloodborne pathogens. A thorough health history should be obtained during the triage of a patient entering a facility. This would include exposure to infectious agents, travel to certain countries, and previous infections resistant to antibiotics (i.e., MRSA, VRE, TB, or carbapenem-resistant Enterobacteriaceae). Patients identified with a risk or history of any of these pathogens may be placed on the appropriate precautions in an isolation room. Infection prevention and the attending physician should be consulted immediately for further orders and treatment (20-22).
Control of Routes of Transmission
Controlling the routes of transmission is a key factor in preventing infection spread. Hand hygiene has been established as the primary prevention method (18).
Care must be taken to follow guidelines for proper hand washing, including:
- Use antibacterial soap and water when hands are visibly soiled or when a Clostridium difficile infection is known or suspected.
- Hands should be gathered. Scrubbing should last at least 20 seconds on all surfaces, between fingers, and under nails.
- Thoroughly rinse the soap from your hands with running water, pat dry with a paper towel, and use a paper towel to turn off the faucet.
- Hand sanitizer, at least 60% alcohol-based, between soap and water may be used.
- A dime-sized amount of hand sanitizer should be rubbed over the surface of hands and fingers and then allowed to air dry.
Barriers to proper hand hygiene include knowledge gaps and the availability of appropriate supplies. Training programs to educate healthcare providers on proper hand washing should be accompanied by ongoing assessment and feedback to ensure compliance.
Incorporating hand hygiene into each nurse's professional development plan is also recommended. Healthcare facilities should diligently ensure that hand washing stations are located in convenient areas and that hand cleaning products are frequently monitored and refilled. Signage and educational materials may be posted in high-traffic areas and at hand washing stations to encourage use by healthcare providers, patients, and visitors. Nurses and healthcare personnel must be aware of the potential of hand hygiene materials as being a potential source of contamination or cross-contamination. Hand hygiene dispensers are touched frequently with contaminated hands and must be often cleaned. It is recommended that the manufacturer's recommendations for cleaning be followed. Hand hygiene systems that allow products to be refilled pose a risk of contaminating the contents. If refilling is a requirement, this should be accomplished using an aseptic technique as much as possible. Facilities should avoid purchasing this product type and move to pre-filled dispensing units, if possible (1-4,18).
Use of Appropriate Barriers
Appropriate barriers are essential in keeping patients and healthcare providers safe from transmitting or contracting pathogens. The type of personal protective equipment (PPE) chosen depends on variables such as patient care, standard, and transmission-based precautions. The minimal amount of PPE recommended are as follows (18,20,21,22,23,24):
- Contact precautions include gloves and gowns. A mask and eye protection are required if bodily secretions may be contacted.
- Droplet precautions require a surgical mask.
- Airborne precautions require wearing gloves, a gown, and an approved N95 respirator mask that has been fit-tested for the individual wearing it. Unfavorable pressure rooms that can filter 6 to 12 air exchanges per hour are also recommended.
Be mindful that these are the minimal recommendations based solely on the identified transmission status of the patient. Selection of PPE should be made using critical thinking to identify potential risks depending on the type of patient care being performed, procedure, behavioral considerations, and other factors that may deviate from the standard. Confirming their infection control and prevention guidelines with your workplace is also essential. The following are current evidence-based recommendations for donning and doffing PPE(18,20,21,22,23,24):
How to Put On (Don) PPE Gear:
More than one donning method may be acceptable. Training and practicing using your healthcare facility’s procedure is critical, as facilities can vary in PPE supply and protocols. Below is one example of donning (18,20,21,22,23,24).
- Identify and gather the proper PPE to wear. Ensure the choice of gown size is correct (based on training).
- Perform hand hygiene using hand sanitizer.
- Put on an isolation gown and tie all of the ties on it. Other healthcare personnel may need assistance.
- Put on NIOSH-approved N95 filtering face-piece respirator or higher (use a facemask if a respirator is unavailable). If the respirator has a nosepiece, it should be fitted to the nose with both hands, not bent or tented. Do not pinch the nosepiece with one hand. The respirator/facemask should be extended under the chin. Both your mouth and nose should be protected. Please do not wear a respirator/facemask under your chin or store it in a scrubs pocket between patients.
- Respirator: Respirator straps should be placed on the crown of the head (top strap) and base of the neck (bottom strap). Perform a user seal check each time you put on the respirator.
- Face mask: Mask ties should be secured on the crown of the head (top tie) and base of the neck (bottom tie). If the mask has loops, hook them appropriately around your ears.
- Put on a face shield or goggles. When wearing an N95 respirator or half-face-piece elastomeric respirator, select the proper eye protection to ensure that the respirator does not interfere with the correct positioning of the eye protection and that the eye protection does not affect the fit or seal of the respirator. Face shields provide full face coverage. Goggles also offer excellent protection for the eyes, but fogging is common.
- Put on gloves. Gloves should cover the cuff (wrist) of the gown.
- Healthcare personnel may now enter the patient’s room.
How to Take Off (Doff) PPE Gear:
More than one doffing method may be acceptable. Training and practicing using your healthcare facility’s procedure is critical. Below is one example of doffing (18,20,21,22,23,24).
- Remove gloves one at a time. Ensure glove removal does not cause additional contamination of hands. Gloves can be removed using multiple techniques, such as the glove-in-glove or bird-beak.
- Remove the gown. Untie all ties (or unsnap all buttons). Some gown ties can be broken rather than untied. Do so gently, avoiding forceful movement. Reach up to the shoulders and carefully pull the gown away from the body. Rolling the gown down is an acceptable approach. Dispose of it in the designated trash receptacle.
- Healthcare personnel may now exit the patient’s room.
- Perform hand hygiene.
- Remove face shields or goggles. Carefully remove them by grabbing the strap and pulling upwards and away from the head. Do not touch the front of your face shield or goggles.
- Remove and discard the respirator (or face mask if used instead of respirator). Do not touch the front of the respirator or face mask.
- Respirator: Remove the bottom strap by touching only it and carefully bringing it over the head. Grasp the top strap, carry it carefully over the head, and then pull the respirator away from the face without touching the front of the respirator.
- Face mask: Carefully untie (or unhook from the ears) and pull away from the face without touching the front.
- If your workplace practices reuse, perform hand hygiene after removing the respirator/face mask and before putting it on again.

Appropriate Isolation/Cohorting of Patients with Communicable Diseases
Co-hosting patients is a common practice within facilities, especially with limited rooms and an increasing number of patients with multidrug-resistant organisms (MDROs). To combat these issues, placing patients with the same type of pathogen in one room when single rooms are unavailable is an option. The minimal standard for all patients is standard precautions (1,2,18,20,21,22,23,24).
Contact: If available, patients with a known or suspected pathogen transmitted via contact should be placed in a private room. Co-horting can be achieved if the co-horted patients share the same type of pathogen.
Droplet: Unless a single patient room is not available, patients in droplet precautions should only be co-horted if neither have an excessive cough or sputum production. The cohorts should be tested to ensure they are infected with the same type of pathogen. Immunocompromised patients are at an increased risk and should not be co-horted. Patients must be separated at least three feet apart, and a privacy curtain should remain between their respective areas. Care providers must don and doff new PPE while caring for each patient. Patients should be given masks to be worn when possible.
Airborne: An airborne infection isolation room (AIIR) with negative air pressure that exchanges air at least six to 12 changes per hour is required. The door must remain closed except for entry and exit. Co-horting of patients is not recommended except in the case of an outbreak or a large number of exposed patients. In these instances, evidence-based guidelines recommend the following:
- Consult infection control professionals before patient placement to determine the safety of alternative rooms that do not meet engineering requirements for AIIR.
- Place together (cohort) patients who are presumed to have the same infection (based on clinical presentation and diagnosis when known) in areas of the facility that are away from other patients, especially patients who are at an increased risk for infection (e.g., immunocompromised patients).
- Use temporary portable solutions (e.g., an exhaust fan) to create a hostile pressure environment in the converted area of the facility. Discharge air directly to the outside, away from people and air intakes, or direct all the air through high-efficiency particulate arresting (HEPA) filters before introducing it to other air spaces.
Host Support and Protection
Vaccinations to prevent disease are highly recommended by numerous health organizations such as the Centers for Disease Control and Prevention (CDC), the World Healthcare Organization (WHO), and several public health departments (1,25-28). As healthcare providers, nurses are positioned to review the patient's history for gaps in appropriate vaccination coverage and educate the patient. Additionally, healthcare providers are ethically responsible for maintaining current vaccinations and can prevent transmitting known communicable diseases by receiving an influenza vaccination each year.
Further evidence suggests that additional boosters for tetanus and pertussis, COVID-19, and measles might benefit several nurses and patients. Pre- and/or post-prophylaxis may be recommended during specific exposures or for patients at an increased risk for infection. This is commonly used for emergent or planned procedures and surgeries that access areas at higher risk for becoming a portal of entry, such as the respiratory, gastrointestinal, and genitourinary tracts. Antibiotics may be ordered when it is known that the sterile field has been broken during a procedure or there has been a concern of contamination of a wound or incision site (1,25-28).
In cases of exposure to an infectious pathogen, the decision to treat includes factors such as the type of exposure, source of the patient's symptoms, time frame since exposure, the health status of the individual exposed, and the risks and benefits of the treatment. Pre-prophylaxis may be considered in the prevention of HIV for high-risk individuals. Typically, after exposure, the host’s blood is drawn to determine pathogen risk regardless of if there is a known pathogen. Based on results, post-exposure prophylactics are given within a short time frame from the exposure. The individual who is exposed will have baseline testing for HIV, HBV, and HCV antibodies. Follow-up testing occurs six weeks, three months, and six months after initial exposure. Maintaining skin and immune system integrity is of the utmost importance to prevent the transmission of infectious pathogens (1,25-28).
Nursing interventions to promote skin and immune system integrity are (6):
- Perform a thorough skin assessment every shift and with changes in condition.
- Accurately document any wounds or incisions
- Use gentle cleansers on the skin and pat dry.
- Use moisturizers and barrier creams on dry or tender skin.
- Prevent pressure ulcer development by turning and repositioning the patient every 2 hours if the patient cannot move independently.
- Maintain aseptic technique during wound care, dressing changes, IV manipulation or blood draws, and catheter care.
- Use neutropenic guidelines when providing care to immunocompromised patients.
- Encourage adequate nutritional and hydration intake.
Environmental Control Measures
The cleaning, disinfection, and sterilization of patient care equipment should be performed per the manufacturer's and facility protocol's recommendations. Cleaning should be performed between each patient encounter. For equipment used in an isolation room, a terminal clean must be performed before being used in other patient care. Environmental cleaning personnel must be educated on the appropriate cleaning for all precautionary patient environments. The Material Safety Data Sheets (MSDS) for all chemicals are to be available to all healthcare personnel for reference as to the proper use and storage. These should be referred to ensure the correct cleaning product is effective in terminally cleaning isolation rooms based on pathogens (17,18,22,25).
Ventilation should be thoroughly managed and maintained by the environmental operations team. Unfavorable pressure rooms should be consistently monitored, and alarms should be investigated to ensure proper air exchange. Concerns from nursing regarding ventilation issues should be directed to the environmental team for follow-up. Regulated medical waste (RMW) within the healthcare system that must follow guidelines for disposal includes (17,18,22,25):
- Human pathological waste
- Human blood and blood products
- Needles and syringes (sharps)
- Microbiological materials (cultures and stocks)
- Other infection waste
Bodily fluid, such as urine, vomit, and feces, may be safely disposed of in any utility sink, drain, toilet, or hopper that drains into a septic tank or sanitary sewer system. Healthcare personnel must don appropriate PPE during disposal. Linen and laundry management in shared health facilities shall (17,18,22,25):
- Provide a sufficient quantity of clean linen to meet the requirements of patients.
- Separately bag or enclose used linens from infectious patients in readily identified containers distinguishable from other laundry.
- Transport and store clean linen in a manner to prevent contamination.
Environment controls include medical devices and systems to isolate or remove the bloodborne pathogens hazard from the workplace. These include sharps disposal containers, self-sheathing needles, and safer medical devices, such as sharps with engineered sharps injury protections and needleless systems. Per facility specifications, continuous training and education should be provided to healthcare personnel on the various methods and modes of environmental control measures that are put in place to prevent and contain pathogen spread (1,2,3).

Self Quiz
Ask yourself...
- How must an organization balance single-use versus reusable, portable medical equipment when considering infectious disease spread?
- What is your workplace's protocol for donning PPE?
- What is your workplace's protocol for doffing PPE?
- What common infections have been reported in your workplace?
- How often do you engage with leadership or management on HAI reduction measures?
- Have you ever cared for a patient with an HAI? How did they react or respond to knowing that they contracted an HAI? What education did you provide to this patient?
- Have you ever "brought home" a work infection? If so, what happened? Did your workplace provide any compensation or assistance?
- What is your workplace's protocol on needlestick and sharps exposure?
- How often do you and other nurses discuss PPE, infection control, and prevention in the workplace?
ELEMENT III – Infection Control in the Workplace
Engineering and work practice controls should be used to reduce the opportunity for patient and healthcare worker exposure to potentially infectious material in all healthcare settings (4-9).
Definitions (4-9)
Healthcare-associated infections (HAIs): Infections associated with healthcare delivery in any setting, such as hospitals, long-term care facilities, ambulatory settings, home care, etc.
Engineering Controls: Controls, such as sharps disposal containers, self-sheathing needles, and safer medical devices, such as sharps with engineered sharps injury protections and needleless systems, can isolate or remove the bloodborne pathogens hazard from the workplace.
Injection safety (or safe injection practices): A set of measures to perform injections optimally safely for patients, healthcare personnel, and others. A safe injection does not harm the recipient, expose the provider to any avoidable risks, and does not result in dangerous waste for the community. Injection safety includes practices intended to prevent transmission of bloodborne pathogens between one patient and another or between a healthcare worker and a patient and to prevent harm such as needlestick injuries. Single-use vials contain only one dose of medication and should only be used once for one patient, using a new sterile needle and a new sterile syringe.
Multidose medication vial: a bottle of liquid medication that contains more than one dose of drugs and is often used by patients with diabetes or for vaccinations.
Work Practice Controls: Controls that reduce the likelihood of exposure to bloodborne pathogens by altering how a task is performed, such as prohibiting the recapping of needles by a two-handed technique).
High-risk Practices and Procedures
Percutaneous exposures are a work hazard within the healthcare industry. Millions of healthcare workers are at risk, with nurses ranking number one. Studies have shown that needlestick injuries occur most frequently within a patient or operating room. Exposures can occur through not following safe practices. The following practices in handling contaminated needles and other sharp objects, including blades, can increase the risk of percutaneous exposure and should be avoided (1,2,3,4,7,17,18,19,22,24,26):
- Manipulating contaminated needles and other sharp objects by hand, such as removing scalpel blades from holders, removing needles from syringes
- Delaying or improperly disposing of sharps, such as leaving contaminated needles or sharp objects on counters/workspaces or disposing in non-puncture-resistant receptacles
- Recapping contaminated needles and other sharp objects using a two-handed technique
- Performing procedures where there is poor visualization, such as:
- Blind suturing
- Non-dominant hand opposing or next to a sharp
- Performing procedures where bone spicules or metal fragments are produced.
Mucous membrane/non-intact skin exposures occur with direct blood or body fluids contact with the eyes, nose, mouth, or other mucous membranes via:
- Contact with contaminated hands.
- Contact with open skin lesions/dermatitis.
- Splashes or sprays of blood or body fluids during irrigation, suctioning, or close contact
Parenteral exposure is subcutaneous (SC), intramuscular (IM), or IV contact with blood or other body fluid. Injection with infectious material may occur during:
- Administration of parenteral medication
- Sharing of blood monitoring devices, such as glucometers, hemoglobinometers, lancets, or lancet platforms/pens
- Infusion of contaminated blood products or fluids
- Human bites, abrasions, or cuts
Unsafe injection practices have resulted in more than 50 outbreaks of infectious disease transmission since 2001. As well, since that time, over 150,000 patients were potentially exposed to HIV, HBV, and HCV solely due to unsafe practices (1,2,3,4,7,17,18,19,22,24,26). These deviations from best practice have resulted in one or more of the following consequences:
- Transmission of bloodborne viruses
- Notification of thousands of patients of possible exposure to bloodborne pathogens and recommendation that they be tested for bloodborne pathogens
- Referral of providers to licensing boards for disciplinary action
- Malpractice suits filed by patients
Pathogens, including HCV, HBV, and HIV, can be present in sufficient quantities to produce infection in the absence of visible blood (26).
- Bacteria and other microbes can be present without clouding or other visible evidence of contamination.
- The absence of visible blood or signs of contamination in a used syringe, IV tubings, multi- or single-dose medication vial, or blood glucose monitoring device does NOT mean the item is free from potentially infectious agents, as many things cannot be seen, with the naked eye.
- All used injection supplies and materials are potentially contaminated and should be discarded.
Proper infection control techniques require that healthcare providers follow best practices to prevent injury and pathogen transfer. Aseptic techniques should always be used to prepare and administer an injection (14,15,17,26). The following are best practice guidelines:
- Medications should be drawn up in a designated “clean” medication area that is not adjacent to areas where potentially contaminated items are placed.
- Use a new sterile syringe and needle to draw up medications while preventing contact between the injection materials and the non-sterile environment.
- Ensure proper hand hygiene before handling medications.
- If a medication vial has been opened, the rubber septum should be disinfected with alcohol before piercing it.
- Never leave a needle or other device inserted into a medication vial septum or IV bag/bottle for multiple uses. This directly routes microorganisms to enter the vial and contaminate the fluid.
- Medication vials should be discarded upon expiration or when concerns arise regarding the medication's sterility.
Never administer medications from the same syringe to more than one patient, even if the needle is changed. Never use the same syringe or needle to administer IV medications to more than one patient, even if the drug is administered into the IV tubing, regardless of the distance from the IV insertion site (14,15,17,26).
- All infusion components are interconnected, from the infusion to the patient's catheter.
- All components are directly or indirectly exposed to the patient's blood and cannot be used for another patient. These components should also be discarded in the appropriate receptacle.
- Syringes and needles intersecting through any IV system port also become contaminated. They cannot be used for another patient or to re-enter a non-patient-specific multidose medication vial.
- Separation from the patient’s IV by distance, gravity, and/or positive infusion pressure does not ensure that small amounts of blood are not present in these items.
- Never enter a vial with a syringe or needle used for a patient if the same medication vial might be used for another patient.
Dedicate medication vials to a single patient, per your workplace's protocols (14,15,17,26), whenever possible.
- Medications packaged as single-use must never be used for more than one patient.
- Never combine leftover contents for later use
- Medications packaged as multiuse should be assigned to a single patient whenever possible.
- Never use bags or bottles of intravenous solution as a standard supply source for more than one patient.
- Never use peripheral capillary blood monitoring devices packaged for single-patient use on multiple patients.
- Restrict the use of peripheral capillary blood sampling devices to individual patients.
- Never reuse lancets. Use single-use lancets that permanently retract upon puncture whenever possible.

Evaluation/Surveillance of Exposure Incidents
A plan to evaluate and follow up on exposure incidents should be implemented at every facility. At a minimum, this plan should include the following elements (1,2,3,6,11,13,14,15):
- Identification of who is at risk for exposure
- Identification of what devices cause exposure
- Identification of areas/settings where exposures occur
- Circumstances by which exposures occur
- Post-exposure management
- Education for all healthcare employees who use sharps. This would include the fact that ALL sharp devices can cause injury and disease transmission if not used and disposed of properly. Specific focus should be on the devices that are more likely to cause injury, such as:
- Devices with higher disease transmission risk (hollow bore) and
- Devices with higher injury rates (“butterfly”-type IV catheters, devices with recoil action)
- Blood glucose monitoring devices (lancet platforms/pens).
Engineer Controls
Engineer controls are implemented to provide healthcare workers with the safest equipment to complete their jobs. Safer devices should be identified and integrated into safety protocols whenever possible. When selecting engineer controls to be aimed at preventing sharps injuries, the following should be considered (1,2,3,6,11,13,14,15):
- Evaluate and choose safer devices
- Passive vs. active safety features
- Mechanisms that provide continuous protection immediately
- Integrated safety equipment vs. accessory devices:
- Properly educate and train all staff on safer devices.
- Consider eliminating traditional or non-safety alternatives whenever possible.
- Explore engineering controls available for specific areas/settings.
- Use puncture-resistant containers for the disposal and transport of needles and other sharp objects:
- Refer to published guidelines for sharps disposal container selection, evaluation, and use (e.g., placement).
- Use splatter shields on medical equipment associated with risk-prone procedures (e.g., locking centrifuge lids).
Work Practice Controls (1,2,3,6,11,13,14,15,17,18)
- General practices:
- Hand hygiene includes the appropriate circumstances in which alcohol-based hand sanitizers, soap, and water hand washing should be used.
- Proper procedures for cleaning blood and body fluid spills
- Initial removal of bulk material followed by disinfection with an appropriate disinfectant.
- Proper handling/disposal of blood and body fluids, including contaminated patient care items.
- Proper selection, donning, doffing, and disposal of PPE as trained
- Adequate protection for work surfaces in direct proximity to patient procedure treatment area with appropriate barriers to prevent instruments from becoming contaminated with bloodborne pathogens
- Preventing percutaneous exposures:
- Avoid unnecessary use of needles and other sharp objects
- Use care in the handling and disposing of needles and other sharp objects:
- Avoid recapping unless medically necessary
- When recapping, use only a one-hand technique or safety device
- Pass sharp instruments using designated “safe zones."
- Disassemble sharp equipment by use of forceps or other devices
- Discard used sharps into a puncture-resistant sharps container immediately after use
Modify Procedures to Avoid Injury (1,2,3,6,11,13,14,15,17,18):
- Use forceps, suture holders, or other instruments for suturing
- Avoid holding tissue with fingers when suturing or cutting
- Avoid leaving exposed sharps of any kind on patient procedure/treatment work surfaces
- Appropriately use safety devices whenever available:
- Always activate safety features
- Never circumvent safety features

Self Quiz
Ask yourself...
- What best practices should always be employed when delivering injections and intravenous medications?
- Have you or a coworker experienced a needlestick injury at work? How was that situation managed?
- What sort of infection surveillance does your workplace use, such as documentation notes, managerial updates, and so on?
- How has what you learned in nursing school changed the infection prevention and control measures you practice in your nursing career?
- Are nurses in your workplace involved in infection surveillance? If so, what is the nurse's role in infection surveillance?
- What role does leadership take in infection surveillance and HAI reduction?
- What is your workplace's policy on multiuse vials?
- How often do you wash your hands during a typical nursing shift? Do you tend to wash your hands more or use hand sanitizer more?
ELEMENT IV – Defining PPE
Selection and use of barriers and/or personal protective equipment for preventing patient and healthcare worker contact with potentially infectious material (19-26).
Definitions
Personal protective equipment (PPE) is specialized clothing or equipment an employee wears to protect against a hazard. PPE is typically for one-time use but can be reused depending on the supply, protocol, and infection prevention measures in place.
Barriers: Equipment such as gloves, gowns, aprons, masks, or protective eyewear can reduce the risk of exposure of the healthcare worker's skin or mucous membranes to potentially infective materials (19-26).
Types of PPE/Barriers and Criteria for Selection
Per OSHA guidelines, employers must provide employees with appropriate PPE that protects them from potential infectious pathogen exposure. PPE includes gloves, coveralls, masks, face shields, and eye protection. All PPE is intended to provide a barrier between the healthcare worker and potential contamination, whether from a patient, object, or surface (19-26).
Gloves are intended to provide coverage and protection for hands. There are several types of gloves, and the kind of patient care or activity should guide choice (19-26).
- Sterile – to be utilized when performing sterile procedures and aseptic technique
- Non-sterile – medical grade, non-sterile gloves may be used for general patient care and clean procedures, such as nasogastric tube insertion
- Utility – not medical grade and should not be used in patient care
The choice of glove material is often dictated by cost and facility preference. When given a choice, considerations should be made regarding the material being handled (19-26).
- Natural rubber latex – rarely used in facilities due to allergen risk
- Vinyl – made from PVC, lower in cost, protects in non-hazardous and low-infection environments
- Nitrile – more durable, able to withstand chemical and bio-medical exposure
An appropriately sized glove fits securely to the fingertips and palm without tightness or extra room. A glove should be replaced immediately if it develops a tear or is heavily soiled.
A cover garb is a protective layer worn over scrubs or clothes to protect garments and skin. Examples include laboratory coats, gowns, and aprons. As with gloves, consideration should be given to size, sterility, the type of patient care involved, and the material characteristics of the gown.
- Fluid impervious – does not allow passage of fluids
- Fluid resistant – resists penetration of fluids, but fluid may seep with pressure
- Permeable – does not offer protection against fluids
Masks protect the wearer’s mouth and nose, with respirators providing an extra layer of protection to the respiratory tract against airborne infection pathogens. Goggles are designed to protect the eyes from splashes and droplet exposure, while face shields offer additional protection to the entire face. It is important to note that face shields are not designed to replace masks (19-26,28). The choice of PPE is based on the factors reasonably anticipated to occur during the patient care encounter. Potential contact with blood or other infectious material can occur via splashes, respiratory droplets, and/or airborne pathogens.
The type of PPE chosen will be based on standard or transmission-based precaution recommendations. Follow your facility policy and procedures for guidance on the appropriate choice. The nurse must also anticipate whether fluid will be encountered, such as emptying a drain or foley collection device. In situations where a large amount of fluid is likely to be experienced, it would be wise to choose a higher level of protection, such as an impermeable gown, if available, and to wear eye protection to ward off splashes (19-26). Choosing Barriers/PPE Based on Intended Need
Barriers and PPE are designed to keep patients and healthcare providers safe. In certain circumstances, specific PPE is selected based on patient care or circumstances (19-26).
Patient Safety
During invasive procedures, such as inserting a central line or during surgery, staff directly involved in performing the procedure or surgery must maintain sterility. Appropriate sterile PPE will be selected based on the type of procedure, and the patient will be draped in a sterile fashion according to recommended guidelines. Patients in droplet precautions pose a significant risk to healthcare workers and visitors. The patient and anyone inside the patient's room should wear a mask for the most effective prevention of transmission (19-26).
Employee Safety
Employees must evaluate the types of exposure that are likely to occur during patient care. Selection of PPE and appropriate barriers should consider the following (19-26,28):
Barriers to contamination prevention (16,19-26,28):
- Standard precautions are to be used with any potential exposure to blood, mucous membranes, compromised skin, contaminated equipment or surfaces, and body fluids. Barriers may include gloves, gowns, and eye and face protection.
- Employees must be judicious in identifying any precautions placed on a patient (e.g., contact, droplet, airborne) and following recommended PPE guidelines to protect themselves and other patients.
- PPE should be donned prior to entering a patient room and doffed upon exit. All gloves must be changed between uses, and hands must be washed or sanitized upon removal of gloves.
- Additionally, social distancing of 6 feet should occur within the work environment whenever possible. When not possible, adherence to mask guidelines is sufficient.
Masks for preventing exposure to communicable diseases (16,19-26,28):
With the onset of COVID-19 across the globe, masks are an essential tool in preventing the transmission of respiratory pathogens. At a minimum, a medical mask must be donned during all patient care, and surgical masks must be utilized during procedures or surgery.
N95 masks are reserved for patient care with known or suspected COVID-19 or other airborne pathogens if airborne precautions are ordered or during procedures that may aerosolize, such as during intubations or specific endoscopy procedures.
Standard N95 respirators are recommended for all other care involving confirmed or suspected Covid-19 patients.
Guidance on Proper Utilization of PPE/Barriers (16,19-26,27,28)
Proper fit is required for PPE to be adequate, as everyone has different body sizes and facial structures that can influence PPE effectiveness. The gowns and gloves chosen should fit well, allow movement, and not be too baggy or too tight. For particulate respirators, all workers required to wear tight-fitting respirators (e.g., N95 respirators, elastomeric) must have a medical evaluation to determine the worker's ability to wear a respirator. If medically cleared, a respirator fit test must be performed using the exact model available in the workplace. Before donning PPE, it should be inspected for anomalies, tears, or vulnerable spots. A compromised PPE should be disposed of, and a new garment should be selected. Nurses must consider the selection of PPE to ensure that it is the correct type for the job and anticipate any circumstances where splashes or fabric saturation is likely to occur. The PPE provided by the employer may be single-use or reusable. Always verify with the manufacturer’s guidelines and facility policy on correctly using and processing worn garments. The facility must ensure that reusable gowns are laundered according to local, state, and federal guidelines.
Healthcare facilities have a legal duty to protect their workers. Employers and healthcare workers must understand the cost versus benefit ratio balance in PPE selection and use. While it is important to be good stewards of resources, always erring on the side of caution and choosing PPE based on anticipated exposure risk is the most effective way to protect healthcare workers and patients.

Self Quiz
Ask yourself...
- How would you handle working at an organization that does not provide sufficient PPE to protect frontline staff?
- What is an example of an acceptable refusal by a healthcare provider to don PPE?
- What do you think causes healthcare providers to forgo established safety measures?
- What other industries are healthcare analogous to when considering the safety of people?
- What are your workplace's policies on PPE?
- Have you ever had to educate a patient on PPE? How was that conversation? What talking points would you address when talking about PPE with a geriatric patient compared to a pediatric patient?
- How involved are nurses in your workplace in PPE use, cost, and distribution?
- If a patient developed an allergic reaction to PPE, how would you handle that situation?
- How can caregivers play a role in a patient's health history?
ELEMENT V – Maintaining a Safe Environment (1,2,3,29)
Create and maintain a safe environment for patient care in all healthcare settings by applying infection control principles and practices for cleaning, disinfection, and sterilization.
Definitions
Contamination: The presence of microorganisms on an item or surface.
Cleaning: The process of removing all foreign material (dirt, body fluids, lubricants) from objects by using water and detergents or soaps and washing or scrubbing the object
Critical device: An item that enters sterile tissue or the vascular system (e.g., IV catheters, needles). These must be sterile before contact with tissue.
Decontamination: The use of physical or chemical means to remove, inactivate, or destroy bloodborne pathogens on a surface or item to the point where they can no longer transmit infectious particles.
Disinfection: The use of a chemical procedure that eliminates virtually all recognized pathogenic microorganisms but not necessarily all microbial forms (bacterial endospores) on inanimate objects.
High-level disinfection: This type of disinfection kills all organisms except high levels of bacterial spores and is affected by a chemical germicide cleared for marketing as a sterilant by the U.S. Food and Drug Administration (FDA).
Intermediate level disinfection: Disinfection that kills mycobacteria, most viruses, and bacteria with a chemical germicide registered as a “tuberculocide” by the U.S. Environmental Protection Agency (EPA).
Low-level disinfection: Disinfection that kills some viruses and bacteria with a chemical germicide registered as a hospital disinfectant by the EPA.
Noncritical device: An item that contacts intact skin but not mucous membranes (e.g., blood pressure cuffs, oximeters). It requires low-level disinfection.
Semi-critical device: An item that comes in contact with mucous membranes or non-intact skin and minimally requires high-level disinfection (e.g., oral thermometers, vaginal specula).
Sterilization: Using a physical or chemical procedure to destroy all microbial life, including highly resistant bacterial endospores.
Universal Principles (1,2,3,29)
Instruments, medical devices, and equipment should be managed and reprocessed according to the recommended and appropriate methods regardless of a patient's diagnosis, except for suspected prion disease cases. Because of the infective nature and steam-resistant properties of prion diseases, special procedures are required for handling brain, spinal, or nerve tissue from patients with known or suspected prion disease, such as Bovine spongiform encephalopathy [BSE].
Consultation with infection control experts before performing procedures on such patients is warranted. Industry guidelines, equipment, and chemical manufacturer recommendations should be used to develop and update reprocessing policies and procedures. Written instructions must be made available for each instrument, medical device, and equipment reprocessed (1,2,3,29).
Potential for Contamination (1,2,3,29)
The type of instrument, medical device, equipment, or environmental surface cause variables more likely to be a source of contamination. The presence of hinges, crevices, or multiple interconnecting pieces may cause external contamination. If able, these devices should be disassembled. Endoscopes provide a particular challenge for internal and external contamination because of their lumens and the crevices and joints present. The disinfectant must reach all surfaces and ensure no air pockets or bubbles impede penetration. As well, these devices may be made of material that is not heat resistant, which prevents the ability to sterilize.
In these instances, chemicals must be utilized to provide disinfection. Once rendered sterile, there are multiple opportunities for potential contamination because of the frequency of hand contact with the device or surface. Packaging may be overhandled and breached. If the item may come into contact with potential contaminants via poor storage, improper opening, or environmental factors, follow facility protocol for sterilization and disinfection. The efficacy of sterilization and disinfection depends on the number and type of microorganisms present. Various pathogens carry an innate resistance, making successful decontamination more challenging. Bacteria, viruses, fungi, protozoa, and prions cause most infections. Because of the nature of their outer membranes, spores, and gram-negative bacteria have a natural barrier that prevents the absorption of disinfectants.
Bacterial spores are incredibly resistant to chemical germicides. The number of microorganisms present on a medical instrument, device, or surface affects the time that must be factored into disinfection and sterilization efficacy (1,2,3,29). Generally, used medical devices are contaminated with a relatively low bioburden of organisms. Inconsistencies or incorrect methods of reprocessing can easily lead to the potential for cross-contamination.
Steps of Reprocessing (1,2,3,29)
Reprocessing medical instruments and equipment is completed sequentially depending on the instrument and chosen process.
Pre-cleaning removes soil, debris, and lubricants from internal and external surfaces through mopping, wiping, or soaking. After use, it must be done as soon as possible to lower the number of microorganisms on the object.
Cleaning may be accomplished manually or mechanically. Manual cleaning relies upon friction and fluidics (fluids under pressure) to remove debris and soil from the instrument's inner and outer surfaces. Several machines are used in mechanical cleaning, including ultrasonic cleaners, washer-disinfectors, washer-sterilizers, and washer-decontaminators.
Disinfection involves using disinfectants, either alone or in combination, to reduce the microbial count to near insignificant. Common disinfectants used in the healthcare setting include chlorine and chlorine compounds, hydrogen peroxide, alcohols, iodophors, and quaternary ammonium compounds. The EPA and FDA formulate and approve these products for specific uses.
Most medical and surgical devices in healthcare facilities are sterilized. This requires sufficient exposure time to heat, chemicals, or gases to ensure that all microorganisms are destroyed.
Choice/Level of reprocessing sequence (1,2,3,29)
The choice or Level of reprocessing is based on the intended use:
- Critical instruments and medical devices require sterilization.
- Semi-critical instruments and medical devices minimally require high-level disinfection.
- Noncritical instruments and medical devices minimally require cleaning and low-level disinfection.
Manufacturer and workplace recommendations must always be consulted to ensure that appropriate methods, actions, and solutions are used. There is a wide variety of compatibility among equipment components, materials, and chemicals. Rigorous training is required to appropriately understand the various equipment heat and pressure tolerance and the time and temperature requirements for reprocessing. Failure to follow the manufacturer or workplace recommendations may lead to equipment damage, elevated instrument microbial counts after reprocessing, increased infection risk, and possibly patient death (1,2,3,29).
Effectiveness of reprocessing instruments, medical devices, and equipment (1,2,3,29)
Pre-cleaning and cleaning before disinfection is one of the most effective ways to reduce the microbial count. This is only effective when completed before disinfection. Disinfection relies upon the action of products to eliminate microbial count. Depending on the medical instrument or device design, the product may only be required to cover the surface.
However, immersion products and dwell times are necessary because of the lumens of scopes, crevices, or hinges on specific instruments. The presence of organic matter, such as blood, serum, exudate, lubricant, or fecal material, can drastically reduce the efficacy of a disinfectant. This may occur because the presence of organic material acts as a barrier. It may also arise from a chemical reaction between the organic material and the disinfectant being utilized.
Biofilms pose a particular challenge and offer protection from the action of disinfectants. Biofilms are composed of microbes that build adhesive layers onto objects' inner and outer surfaces, including instruments and medical devices, rendering certain disinfectants ineffective. Chlorine and Monochloramines remain effective against inactivating biofilm bacteria.
After disinfection, staff and management must adopt a system of record keeping and tracking of instrument usage and reprocessing. Reprocessing equipment must be maintained and regularly cleaned on a schedule, according to the manufacturer’s guidelines. There are several methods of sterilization, such as steam sterilization (autoclaves), flash sterilization, and, more recently, low-temperature sterilization techniques created for medical devices that are heat sensitive.
Selection depends upon the type of instrument, material, ability to withstand heat or humidity, and targeted microbes. There are several methods of ensuring that sterilized instruments are processed and tracked appropriately. Indicators or monitors are test systems that verify that the sterilization methods were sufficient to eradicate the regulated number of microbes during the process. These safeguards include (1,2,3,29):
- Biologic monitors
- Process monitors (tape, indicator strips, etc.)
- Physical monitors (pressure, temperature gauges)
- Record keeping and recall/ tracking system for each sterilization processing batch/item
The best practice of handling and storing reprocessed medical equipment and instruments uses a system of event-related shelf life rather than time-related. The rationale for this lies in the theory that the sterile items remain sterile as long as the packaging is not compromised. Factors considered event-related include internal or external contamination such as damage to the packaging, humidity, insects, vermin, open shelving, temperature fluctuations, flooding, location, and the composition of packaging material. Standards for handling must also focus on protecting workers from health issues (1,2,3,29).
Recognizing Potential Sources of Cross-Contamination in The Healthcare Environment (1,2,3,29)
- Surfaces or equipment that require cleaning between patient procedures/treatments.
- Practices that contribute to hand contamination and the potential for cross-contamination
- Consequences of reuse of single-use/disposable instruments, medical devices, or equipment
Factors That Have Contributed to Contamination in Reported Disease Transmission Cases (1,2,3,29)
In reprocessing or handling equipment, breaks in infection control practices can compromise the integrity of instruments, medical devices, or equipment. Specific factors include:
- Failure to reprocess or dispose of items between patients.
- Inadequate cleaning
- Inadequate disinfection or sterilization
- Contamination of disinfectant or rinse solutions
- Improper packaging, storage, and handling
- Inadequate/inaccurate record keeping of reprocessing requirements.
Expectations Regarding Differing Levels of Disinfection and Sterilization Methods (1,2,3,29)
Professionals who practice in settings where handling, cleaning, and reprocessing equipment, instruments, or medical devices is performed elsewhere (e.g., in a dedicated Sterile Processing Department) are responsible for ensuring understanding of the core concepts and principles (1,2,3,29):
- Standard and Universal Precautions (e.g., wearing of personal protective equipment)
- Cleaning, disinfection, and sterilization
- Appropriate application of safe practices for handling instruments, medical devices, and equipment in the area of professional practice
- Designation and physical separation of patient care areas from cleaning and reprocessing areas
- Verify with those responsible for reprocessing what steps are necessary before submission of pre-cleaning and soaking.
Professionals who have primary or supervisory responsibilities for equipment, instruments, or medical device reprocessing (e.g., Sterile Processing Department staff or clinics and physician practices where medical equipment is reprocessed on-site) are responsible for understanding core concepts and principles (1,2,3,29):
- Standard and Universal Precaution
- Cleaning, disinfection, and sterilization
- Appropriate application of safe practices for handling instruments, medical devices, and equipment in the area of professional practice
- Designation and physical separation of patient care areas from cleaning and reprocessing areas
Facilities must be fastidious in developing appropriate reprocessing practices that follow regulatory guidelines. When selecting relevant methods, consideration must be given to the antimicrobial efficacy, time constraints, and requirements of these methods, as well as compatibility. Compatibility among equipment/materials includes corrosiveness, penetrability, leaching, disintegration, heat tolerance, and moisture sensitivity. The products' toxicity can pose occupational and environmental hazards to staff and patients. Facilities must adopt procedures and policies to reduce exposure to harmful substances, monitor for toxic exposures, and train staff using reprocessing cleaning and chemicals (1,2,3,29).
Other considerations in developing a safety plan for appropriate reprocessing practices include (1,2,3,29):
- Potential for patient/health care worker toxicity/allergy
- Residual effects include antibacterial residual and patient toxicity/allergy.
- Ease of use
- Stability of products, including concentration, potency, efficacy of use, and effects of organic material
- Odor
- Cost
- Monitoring requirements and regulations
- Specific labeling requirements for reprocessing single-use devices


Self Quiz
Ask yourself...
- You are concerned that the sterilized equipment your coworker just opened onto a sterile field was compromised. The coworker assures you it is okay. How would you handle this situation?
- When would it be appropriate for a facility to deviate from the manufacturer’s recommendations in processing medical and surgical equipment?
- Why do you think there is variation in the Level of reprocessing of medical instruments?
- How would you verify that a shelf-stable system does not compromise sterile instruments?
- What sort of training does your workplace offer for contamination protocol and awareness?
- How often are nurses contaminating and disinfecting patient care spaces in your workplace?
- How have trends in a cleaner work environment evolved in your nursing career?
ELEMENT VI – Health Assessment (1,2,3,7,8,11,12)
Prevention and control of infectious and communicable diseases in healthcare workers is essential (1,2,3,7,8,11,12).
Definitions
Infectious Disease: A clinically manifest disease of humans or animals resulting from an infection.
Communicable Disease: An illness due to a specific infectious agent or its toxic products that arises through transmission of that agent from an infected person, animal, or inanimate source to a susceptible host.
Occupational Health Strategies: As applied to infection control, a set of activities intended to assess, prevent, and control infections and communicable diseases in healthcare workers.
Pre-Placement and Periodic Health Assessments
Occupational health strategies are aimed at ensuring employees are healthy and keeping them healthy. Employees should undergo an initial health screening that reviews immunization records upon hiring. Examples include (1,2,3,7,8,11,12):
- Immunity to vaccine-preventable diseases, such as measles, mumps, rubella, varicella, HBV, influenza, and other recommended or mandated requirements.
- Personalized health counseling.
- Thorough history and physical.
Tuberculosis (TB) screening should be completed before a new employee provides patient care and upon possible exposure for an existing employee. A thorough assessment should include an evaluation of the following symptoms (1,2,3,7,8,11,12):
- Fever
- Cough
- Chest pain, or pain with breathing or coughing
- Night sweats
- Chills
A Mantoux tuberculin skin test (TST) must also be completed. The test is performed by injecting a small amount of tuberculin into the epidermis of the forearm. The test is then evaluated for a reaction in 48 to 72 hours. If there is no reaction, the test result is negative. If reactive, a scale is used to interpret the measurement of induration and to direct further testing or treatment. Nursing staff must be healthy to provide optimal care when working in healthcare. This is especially true in caring for vulnerable patients with weakened immune symptoms.
The following symptoms require immediate evaluation by a licensed medical professional:
- Fever
- Cough
- Rash
- Vesicular lesions
- Draining wounds
- Vomiting
- Diarrhea
Upon evaluation, restrictions on patient care activities may be imposed, and work clearance must be completed prior to return (1,2,3,7,8,11,12).
Management Strategies for Potentially Communicable Conditions (1,2,3,7,8,11,12)
Management and the infection prevention department should collaborate and strategize to ensure that employees who have had an exposure or possible exposure are protected and supported in seeking treatment without fear of retaliation or job loss. Managerial support should prioritize (1,2,3,7,8,11,12):
- Appropriate evaluation and treatment
- Limiting contact with susceptible patients and staff
- Placement in a non-clinical setting
- Depending on the severity of symptoms or potential transmission, a furlough may be necessary until no symptoms are present.
Prevention and Control Strategies for Bloodborne Pathogen Transmission (1,2,3,7,8,11,12,22)
Robust training and educational programs are essential for preventing healthcare worker exposure and transmission. Prevention strategies should include education, training, and availability of the following (1,2,3,7,8,11,12,22):
- Information on potential agents, such as HBV, HCV, and HIV
- HBV vaccination (including safety, efficacy, components, and recommendations for use)
- Hand hygiene
- Appropriate PPE and barrier precautions
- Sharps safety
- Standard and universal Precautions
- Education on the availability of confidential and anonymous testing for bloodborne pathogens
Post-Exposure Evaluation and Management (1,2,3,7,8,11,12,22)
Each facility must plan for post-exposure evaluation and management if any employee or patient experiences a potential or actual bloodborne exposure. The plan should incorporate the following (1,2,3,7,8,11,12,22):
- Prompt evaluation by a licensed medical professional.
- Risk assessment in occupational exposures.
- Recommendations for approaching source patient and healthcare worker evaluations.
- Recommendations for post-exposure prophylaxis emphasizing the most current public health guidelines.
- Post-exposure management of patients or other healthcare workers when the exposure source is a healthcare worker obligates the patient to be informed of the type of exposure, whether it is the healthcare worker’s blood or other potentially infectious material.
Airborne or droplet pathogens require several special considerations. The above guidelines should be applied appropriately. Reporting of suspected or confirmed communicable diseases is mandated under various laws. The primary responsibility for reporting rests with the physician; laboratories, school nurses, daycare center directors, nursing homes/hospitals, and state institutions or other locations providing health services are also required to report(1,2,3,7,8,11,12,22).
All patients and healthcare workers who have been potentially exposed to any pathogens should be educated and counseled about (1,2,3,7,8,11,12,22):
- Risk of exposure or illness
- Testing
- Options for and risks and benefits of post-exposure prophylaxis or treatment
- Need for specialty care
- Follow-up testing and treatment
- Work restrictions, if indicated
- Risk of transmitting infections to others and methods to prevent transmission
- Signs and symptoms of illness to report after exposure, including side effects such as prophylaxis
Evaluation of Healthcare Workers Infected with Bloodborne Pathogens (1,2,3,7,8,11,12,22)
The following rules and recommendations are based on scientific evidence-based practice about policies to prevent infected healthcare personnel-related bloodborne pathogen transmission (HIV, HBV, HCV)(1,2,3,7,8,11,12,22) :
- Strict adherence to standard precautions
- Voluntary testing without fear of disclosure or discrimination
- Mandatory screening for bloodborne pathogens is not recommended. Such a program would cost millions of dollars and not produce any appreciable gain in public safety. Negative antibody tests for HIV, HBV, and HCV do not rule out the presence of infection since it can take some time for measurable antibodies to appear.
- Employer notification of a bloodborne pathogen is not a requirement for employment.
Criteria must be followed when evaluating infected healthcare workers for the risk of transmission to adhere to laws protecting workers from discrimination and disability laws. The following outlines a general assessment to determine the risks posed (1,2,3,7,8,11,12,22):
- Nature and scope of professional practice
- Techniques used in the performance of procedures may pose a transmission risk to patients
- Assessed compliance with infection control standards.
- Presence of weeping dermatitis, draining, or open skin wounds
- Ability to carry out duties with cognitive status examination.
Expert Panels for Evaluating Healthcare Workers Infected with Bloodborne Pathogens (1,2,3,7,8,11,12,22)
Upon request, a bloodborne pathogen-infected healthcare worker may seek advice from the local health department regarding potential risk during patient care of bloodborne disease transmission. A state advisory panel would convene with, at minimum, representation by a state or local public officer, an epidemiologist, and an infectious disease expert (1,2,3,7,8,11,12,22).

Self Quiz
Ask yourself...
- What are your thoughts on a proposal to test all healthcare workers for bloodborne illness before licensing?
- Should nurses caring for vulnerable patients require health screenings before patient care?
- A colleague confides in you that they are concerned they may have been exposed to HCV but are wary of being tested. What options are available to support the colleague and protect patients?
- Who should be responsible for providing post-exposure prophylaxis to potentially infectious material when the employee is not following regulated guidelines for care delivery?
- What is your workplace's policy on post-exposure management?
- How can technology be used to track and inform patients and nurses of post-exposure management?
- What common infectious diseases have you seen or encountered in your workplace recently?
ELEMENT VII – Sepsis Awareness (1,30)
Sepsis is a life-threatening condition caused by a host’s extreme response to infection. Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection. Septic shock is a subset of sepsis that manifests with circulatory and cellular/metabolic dysfunction; septic shock is associated with a higher mortality risk (1,30).
Over one million Americans are diagnosed with sepsis each year, and sepsis is a life-threatening medical emergency that requires early recognition and intervention. Sepsis occurs when the body overcompensates in response to an infection, resulting in multiple organ dysfunction and damage. Most sepsis cases are community-acquired. Early recognition and treatment are the most effective ways to combat sepsis.
Bacterial infections commonly trigger sepsis, although other microbial infections (e.g., fungal or viral) can also trigger sepsis. The triggering infection most commonly originates from the lungs, urinary tract, skin, and/or gastrointestinal tract. Specific populations are at an increased risk of developing sepsis, including (1,30):
- Babies (under 1 year) and individuals 65 and older.
- People with chronic conditions such as diabetes, lung disease, kidney disease, or cancer
- People with impaired immune systems.
Early Recognition of Sepsis (1,30)
- Manifestations of sepsis vary based on the type of infection and host factors.
- Some people may have subtle sepsis presentations.
- Signs and symptoms that may be associated with sepsis in persons with confirmed or suspected infection can include:
- Altered mental state
- Shortness of breath
- Fever
- Clammy or sweaty skin
- Extreme pain or discomfort
- High heart rate
Signs and symptoms in children and older adults may not present the same. In children and the elderly, sepsis symptoms may present as above or any of the following: decreased temperature; pallor or bluish tone to the skin; non-blanching rash; high respiratory rate; lethargy; and seizure.
Sepsis can progress to more severe forms, including septic shock. When septic shock occurs, the body's inflammatory response causes extensive vasodilation, which results in a sudden drop in blood pressure that can quickly lead to organ failure and damage. If a person presents with suspected or confirmed infection, healthcare professionals should assess for signs and risk factors for sepsis following facility sepsis protocols (1,30).
Principles of Sepsis Treatment (1,30)
Sepsis treatment starts with prompt recognition and diagnosis. The diagnosis of sepsis starts with assessing a patient with a known or suspected infection. For adults, sepsis is defined as having two or more symptoms of systemic inflammatory response syndrome, which includes (1,30) :
- Temperature (>38 o C or <36 o C)
- Elevated heart rate > 90 bpm
- WBC (<4×109/L or >12×109/L)
- Respiratory rate (>20 breaths/min, PACO2<32 mm Hg
Severe sepsis has traditionally been defined as having sepsis plus organ failure, while septic shock involves sepsis along with refractory hypotension after fluid resuscitation or requiring vasopressors to maintain hemodynamics.
In addition to blood cultures, types and screens may be ordered for urine, wound exudate, or respiratory secretions, depending on where the suspected infection originates. Blood tests may also include a complete blood count and a basic metabolic panel to assess for kidney or liver damage. Other diagnostic imaging may include diagnostic imaging and ultrasounds. Fluid resuscitation and vasopressors, if needed, will continue until the patient is hemodynamically stable. Healthcare providers should be notified when blood cultures result to ensure the ordered antibiotic is effective against the identified organism (1,30).
Patient Education and Prevention (1,30)
Patient education should strive to provide memorable and straightforward ways to stay free of infection. Adequate hand hygiene is the number one method of preventing disease.
Patients at higher risk should be notified of their risk factors, including (1,30):
- Adults 65 or older
- People with chronic medical conditions, such as diabetes, lung disease, cancer, and kidney disease
- People with weakened immune systems
- Sepsis survivors
- Children younger than one
Patients should be encouraged to give relevant history and information to clinicians, including if they have had a recent infection or sepsis or are immunocompromised (1,30).


Self Quiz
Ask yourself...
- A facility has implemented a sepsis screening program; chart reviews indicate inconsistent order sets. What is the best action for the facility to take to improve compliance?
- What are ways that nursing can promote sepsis screening upon admission?
- A unit-based council is preparing education for the public regarding sepsis recognition and prevention. What methods would be most effective in reaching the most vulnerable populations?
- How are sepsis and septic shock interrelated? How does treatment differ for each sequela?
- How would you explain sepsis to a pregnant patient compared to a geriatric patient?
- What is your workplace's policy on sepsis management?
- How does management in your workplace get involved in sepsis management cases?
- How has care for a patient with sepsis evolved in your nursing career?
- What sort of training does your workplace mandate on sepsis education and prevention?
- How can artificial intelligence (AI) and other technology help patients at risk or experiencing sepsis?
- What are some possible complications of sepsis if left untreated?
- What are some infection prevention techniques to educate patients regarding sepsis and bacterial infections?
- How would you assess if a client is progressing on their treatment plan?
- What sort of protocols does your facility have for remote patient monitoring?
- How can nurses educate patients on maintaining their scheduled medication regime?
Alzheimers Nursing Care
Introduction
Alzheimer’s disease is a destructive, progressive, and irreversible brain disorder that slowly destroys memory and thinking. Alzheimer’s is the most common cause of dementia in older adults (1). For most people who have Alzheimer’s disease, symptoms first appear in their mid 60’s (1).
Studies suggest more than 5.5 million Americans, most 65 or older, may have dementia caused by Alzheimer’s (1). It is currently listed as the sixth leading cause of death in the United States. It is essential to understand the signs and symptoms of Alzheimer’s dementia and how to manage the care of a patient, family member, or friend suffering from the disease.
Dementia is the loss of cognitive functioning, such as thinking, remembering, reasoning, and behavioral abilities, such as a decreased ability to perform activities of daily living (1). The severity of dementia ranges from mild to severe. Dmentia’s mildest stage often begins with forgetfulness, while its most severe stage consists of complete dependence on others for general activities of daily living (1).
History of Alzheimer’s
Alzheimer’s disease is named after Dr. Alois Alzheimer. In the early 1900s, Dr. Alzheimer noticed changes in the brain tissue of a patient who had died of an unknown mental illness. The patient’s symptoms included memory loss, language problems, and unpredictable behavior.
After her death, her brain was examined and was noted to have abnormal clumps known as amyloid plaques and tangled bundled fibers, known as neurofibrillary or tau tangles (1). These plaques and tangles within the brain are considered some of the main features of Alzheimer’s disease. Another feature includes connections of neurons in the brain. Neurons are a type of nerve cell responsible for sending messages between different parts of the brain and from the brain to other parts of the body (1).
Scientists are continuing to study the complex brain changes involved with the disease of Alzheimer’s. The changes in the brain could begin ten years or more before cognitive problems start to surface.
During this stage of the disease, people affected seem to be symptom-free; however, toxin changes occur within the brain (1). Initial damage in the brain occurs within the hippocampus and entorhinal cortex, which are the parts of the brain that are necessary for memory formation. As the disease progresses, additional aspects of the brain become affected, and overall brain tissue shrinks significantly (1).

Signs and Symptoms & Diagnosis of Alzheimer’s Disease
Memory problems are typically among the first signs of cognitive impairment related to Alzheimer’s disease. Some people with memory problems have Mild Cognitive Impairment (MCI) (2). In this condition, people have more memory problems than usual for their age; however, their symptoms do not interfere with their daily lives.
Older people with MCI are at increased risk of developing Alzheimer’s disease. The first symptoms of Alzheimer’s may vary from person to person. Many people display a decline in non-memory-related aspects of cognition, such as word-finding, visual issues, impaired judgment, or reasoning (2).
Healthcare providers use several methods and tools to determine the diagnosis of Alzheimer’s Dementia. Diagnosis and evaluation involve memory, problem-solving, attention, counting, and language tests. Healthcare providers may perform brain scans, including CVT. MRI or PET is used to rule out other causes of symptoms.
Various tests may be repeated to give doctors information about how memory and cognitive functions change over time. They can help diagnose different causes of memory problems, such as stroke, tumors, Parkinson’s disease, and vascular dementia. Alzheimer’s disease can be diagnosed only after death by linking clinical measures with an examination of brain tissue in an autopsy (3).

Self-Quiz
Ask Yourself...
- Have you experienced a patient in your practice with dementia or Alzheimer’s disease? What did their symptoms look like?
- What standard diagnostic tools do healthcare providers use to diagnose this disease?
- What is the definitive diagnosis of Alzheimer’s disease?
Stages of Disease
Mild Alzheimer’s
People experience significant memory loss and other cognitive problems as the disease progresses. Most people are diagnosed in this stage (1).
- Wandering/getting lost
- Trouble handling money or paying bills
- Repeating questions
- Taking longer to complete basic daily tasks
- Personality/behavioral changes (1)
Moderate Alzheimer’s
In this stage, damage occurs in the area of the brain that controls language, reasoning, sensory processing, and conscious thought (1).
- Memory and confusion worsen.
- Problems recognizing family and friends
- Unable to learn new things
- Trouble with multi-step tasks such as getting dressed
- Trouble coping with situations
- Hallucinations/delusions/paranoia (1)
Severe Alzheimer’s
- Plaques and tangles spread throughout the brain, and brain tissue shrinks significantly.
- Cannot communicate
- Entirely dependent on others for care
- Bedridden – most often as the body shuts down

Self-Quiz
Ask Yourself...
- What are some of the signs and symptoms that differentiate each stage of Alzheimer’s disease?
- A person is in what stage of Alzheimer’s disease when they struggle to recognize family members and friends?
Prevention
Many aging patients worry about developing Alzheimer’s disease and dementia. Especially if they have had a family member who suffered from the disease, patients may worry about genetic risk. Although there have been many ongoing studies on the prevention of the disease, nothing has been proven to prevent or delay dementia caused by Alzheimer’s disease (2).
More research suggests that women are more likely to develop dementia and Alzheimer’s compared to men. Further research is needed to determine the role between genetics, sex, and Alzheimer’s risk (4).
A review led by experts from the National Academies of Sciences, Engineering, and Medicine found encouraging yet inconclusive evidence for three types of interventions related to ways to prevent or delay Alzheimer’s Dementia or age-related cognitive decline (2):
- Increased physical activity
- Blood pressure control
- Cognitive training

Treatment of the Disease
Alzheimer’s disease is complex and is continuously being studied. Current treatment approaches focus on helping people maintain their mental function, manage behavioral symptoms, and lower the severity of symptoms. The FDA has approved several prescription drugs to treat those diagnosed with Alzheimer’s (3).
Treating symptoms of Alzheimer’s can provide patients with comfort, dignity, and independence for a more significant amount of time while simultaneously assisting their caregivers. The approved medications are most beneficial in the early or middle stages of the disease (3).
Cholinesterase inhibitors are prescribed for mild to moderate Alzheimer’s disease; they may help to reduce symptoms. Medications include Rzadyne®, Exelon®, and Aricept® (3). Scientists do not fully understand how cholinesterase inhibitors work to treat the disease; however, research indicates that they prevent acetylcholine breakdown. Acetylcholine is a brain chemical believed to help memory and thinking (3).
For those suffering from moderate to severe Alzheimer’s disease, a medication known as Namenda®, which is an N-methyl D-aspartate (NMDA) antagonist, can be prescribed. This drug helps to decrease symptoms, allowing some people to maintain certain essential daily functions slightly longer than they would without medication (3).
For example, this medication could help a person in the later stage of the disease maintain their ability to use the bathroom independently for several more months, benefiting the patient and the caregiver (3). This drug works by regulating glutamate, an essential chemical in the brain. When it is produced in large amounts, glutamate may lead to brain cell death. Because NMDA antagonists work differently from cholinesterase inhibitors, these rugs can be prescribed in combination (3).

Self-Quiz
Ask Yourself...
- Is there a cure for this disease?
- What are some of the treatment forms that have been used for the management of Alzheimer’s disease?
- Can medications be used in conjunction with one another to treat the disease?
Medications to be Used with Caution in those Diagnosed with Alzheimer’s
Some medications, such as sleep aids, anxiety medications, anticonvulsants, and antipsychotics, should only be taken by a patient diagnosed with Alzheimer’s after the prescriber has explained the risks and side effects of the medications (3).
Sleep aids: They help people get to sleep and stay asleep. People with Alzheimer’s should not take these drugs regularly because they could make the person more confused and at a higher risk for falls.
Anti-anxiety: These treat agitation and can cause sleepiness, dizziness, falls, and confusion (3).
Anticonvulsants: These are used to treat severe aggression and have possible side effects of mood changes, confusion, drowsiness, and loss of balance.
Antipsychotics: they are used to treat paranoia, hallucinations, agitation, and aggression. Side effects can include the risk of death in older people with dementia. They would only be given when the provider agrees the symptoms are severe enough to justify the risk (3).
Caregiving
Coping with Agitation and Aggression
People with Alzheimer’s disease may become agitated or aggressive as the disease progresses. Agitation causes restlessness and causes someone to be unable to settle down. It may also cause pacing, sleeplessness, or aggression (5). As a caregiver, it is essential to remember that agitation and aggression are usually happening for reasons such as pain, depression, stress, lack of sleep, constipation, soiled underwear, a sudden change in routine, loneliness, and the interaction of medications (5). Look for the signs of aggression and agitation. It is helpful to prevent problems before they happen.
Ways to cope with agitation and aggression (5):
- Reassure the person. Speak calmly. Listen to concerns and frustrations.
- Allow the person to keep as much control as possible.
- Build in quiet times along with activities.
- Keep a routine.
- Try gently touching, soothing music, reading, or walks.
- Reduce noise and clutter.
- Distract with snacks, objects, or activities.
Common Medical Problems
In addition to the symptoms of Alzheimer’s disease, a person with Alzheimer’s may have other medical conditions over time. These additional health conditions can cause confusion and behavior changes. The person may be unable to communicate with you about their circumstances. As a caregiver, it is essential to watch for various signs of illness and know when to seek medical attention for the person being cared for (6).
Fever
Fever could indicate potential infection, dehydration, heatstroke, or constipation (6).
Flu and Pneumonia
These are easily transmissible. Patients 65 years or older should get the flu and Pneumonia shot each year. Flu and Pneumonia may cause fever, chills, aches, vomiting, coughing, or trouble breathing (6).
Falls
As the disease progresses, the person may have trouble with balance and ambulation. They may also have changes in depth perception. To reduce the chance of falls, clean up clutter, remove throw rugs, use armchairs, and use good lighting inside (6).
Dehydration
It is important to remember to ensure the person gets enough fluid. Signs of dehydration include dry mouth, dizziness, hallucinations, and rapid heart rate (6).
Wandering
Many people with Alzheimer’s disease wander away from their homes or caregivers. As the caregiver, it is essential to know how to limit wandering and prevent the person from becoming lost (7).
Steps to follow before a person wanders (7)
- Ensure the person carries an ID or wears a medical bracelet.
- Consider enrolling the person in the Medic Alert® + Alzheimer’s Association Safe Return Program®.
- Alert neighbors and local police that the person tends to wander and ask them to alert you immediately if they are seen alone.
- Place labels on garments to aid in identification.
Tips to Prevent Wandering (7)
- Keep doors locked. Consider a key or deadbolt.
- Use loosely fitting doorknob covers or safety devices.
- Place STOP, DO NOT ENTER< or CLOSED signs on doors.
- Divert the attention of the person away from using the door.
- Install a door chime that will alert when the door is opened.
- Keep shoes, keys, suitcases, coats, and hats out of sight.
- Make sure not to leave a person who has a history of wandering unattended.

Self-Quiz
Ask Yourself...
- What are the basic implementations you can make as a caregiver to make handling confusion and aggression easier in a patient with Alzheimer’s?
- What are some of the types of medical problems that people with Alzheimer’s may face, and how can they be monitored for prevention?
Conclusion
Alzheimer’s is a sad, debilitating, progressive disease that robs patients of their lives and dignity. As research continues on the causes, treatment, and prevention of the disease, healthcare workers and caregivers need to know the signs and symptoms of a patient with Alzheimer’s disease and potential coping mechanisms and management strategies of the disease. More information on the disease is available through several various resources, including:
Family Caregiver Alliance
800-445-8106
NIA Alzheimer’s and Related Dementias Education and Referral Center
800-438-4380
Nursing Care in Lewy Body Dementia
Introduction
Lewy body dementia is one of the more common causes of dementia. Currently it is the second most common dementia disorder following Alzheimer’s disease [2]. This condition is shown to affect more than 1.4 million people in the United States [1] [2]. Of dementia cases in older adults, Lewy body dementia is said to make up 5% of people with dementia [2]. Lewy body dementia is a disorder that progresses over time [1]. The progression of the disease differs between individuals and the severity of the symptoms [1].
On average an individual lives between five to eight years after diagnosis [1]. Currently there is not a cure for this disease [1]. This course will examine the causes of this disease, signs and symptoms patients might experience, diagnostic tests, types of management, and educational resources for family members. This course is designed to inform nurses about this common disease and to use this information in their daily practice to care for their patients.

Self-Quiz
Ask Yourself...
- What do you think is the most common form of dementia in the United States?
- How common is Lewy body dementia in other parts of the world?
- Is there currently a cure for Lewy body dementia?
- Why do you think Alzheimer’s disease is more common than Lewy body dementia?
Definition
Lewy body is an umbrella term that includes two separate diagnoses: Dementia with Lewy bodies and Parkinson’s disease dementia [5]. As these diseases progress, they develop together and are seen as one entity, not two separate conditions [4]. Lewy body dementia is a condition that involves neurocognitive disorders that include hallucinations, memory loss, behavior changes, and parkinsonism features [2]. This disease can also affect intellectual abilities and cause individuals to act out dreams during REM (rapid eye movement) sleep [2]. REM sleep behavior disorder sometimes may be experienced before any other symptoms are exhibited [2].
Lewy body dementia is known for a buildup of deposits of alpha- synuclein proteins called Lewy bodies [1]. Diagnosing this condition can be difficult because many neurological disorders have similar symptoms. Lewy body dementia and Parkinson disease dementia are very similar. For a diagnosis of Lewy body dementia, there must be a cognitive impairment with motor symptoms occuring in less than 12 months [3]. Parkinson’s disease dementia affects an individual’s movements; cognitive symptoms appear later (greater than one year) [5].
Lewy body dementia is known to affect older adults generally between the ages of 50 and 85 [2]. This disease is said to be underdiagnosed due to a large number of diagnoses occuring post-death during autopsies [4]. Several medications used to treat neurocognitive and behavioral symptoms in other conditions can worsen the symptoms of Lewy body dementia [4]. Therefore, an accurate diagnosis can impact an individual’s quality of life.

Self-Quiz
Ask Yourself...
- What are the two forms of Lewy body dementia?
- What are the differences between dementia with Lewy bodies and Parkinson’s disease dementia?
- Why is it difficult to diagnose Lewy body dementia?
Epidemiology
Lewy body dementia affects a significant number of individuals in the United States. This condition is found more often in men than women [4]. Age is thought to be the greatest risk factor for an individual developing this disease [4]. An individual who has a family history of Lewy body dementia and Parkinson’s disease is at a higher risk for developing this condition [3].
Lewy Body dementia is more widespread in European, Asian, and African ethnic groups [3]. In individuals with Parkinson’s disease, the incidence of Parkinson’s disease dementia is said to be around 25-30% [4]. The incidence of individuals with Parkinson disease developing this type of dementia after having Parkinson’s for more than 20 years increases to around 83% [4].


Self-Quiz
Ask Yourself...
- What is the greatest risk factor for developing Lewy body dementia?
- Are there certain ethnic groups that have a higher rate of Lewy body dementia?
- Which gender is Lewy body dementia prominent in?
Pathophysiology
There is a buildup of alpha- synuclein proteins that causes neurons to die in Lewy body dementia [2] [5]. As mentioned above in this course, this buildup of proteins is called Lewy bodies. The death of neurons that produce dopamine result in problems with movement, cognitive impairment, a decline in cognition, and sleep disturbances [4]. In Lewy body dementia there is a deficiency of acetylcholine [3]. There is also a decrease in acetylcholine with Alzheimer’s disease, but the deficiency is greater with Lewy body dementia [3]. The decrease in neurons that produce acetylcholine causes memory loss and learning impairment [4].
The mutation of synuclein alpha and synuclein beta genes can cause dementia with Lewy bodies [2]. Mutations in apolipoprotein E and GBA genes are potential risk factors for developing the disease [2]. There have been cases where a buildup of alpha-synuclein was found during an autopsy, but the individual did not show any clinical signs of Lewy Body dementia when alive [4]. The function of these proteins in this condition is still undetermined [5].

Self-Quiz
Ask Yourself...
- What are considered Lewy bodies?
- What other disease besides Lewy body dementia has a decrease in acetylcholine?
- What symptoms are a result of destruction of neurons that produce dopamine?
Etiology
The exact cause of Lewy body dementia is still unknown. While research is ongoing and new developments are occuring, the specific cause has not been determined. The accumulation of Lewy bodies cause cell death which causes symptoms, however, the reason for the buildup of Lewy bodies is still under research [5]. As mentioned earlier, there are specific gene mutations that have been shown to increase the likelihood of producing altered alpha- synuclein proteins, in turn causing them to clump together (forming the Lewy bodies) [2].
The mutation of the GBA gene interferes with the function of lysosomes, which can affect the breakdown of the alpha- synuclein proteins, causing the proteins to accumulate [2]. The e4 allele type of the APOE gene has been shown to increase the risk of developing Lewy body dementia [2]. These clumps of Lewy bodies form inside and outside of neurons in different areas of the brain, where they can alter the function of the cell and can cause the cell to die [2].
The neurons that develop the neurotransmitter dopamine are especially impacted by these clumps of Lewy bodies, which was addressed earlier in this course [2]. Further research is required to find out why these Lewy bodies develop in certain individuals. Currently, age, genetics, and environmental factors are some of the greatest risk factors [3].

Self-Quiz
Ask Yourself...
- What is the cause of Lewy body dementia?
- Why is age a risk factor for developing this disease?
- What does the buildup of Lewy bodies do to cells?
Clinical Signs and Symptoms
Lewy body dementia is a progressive disorder – the signs and symptoms worsen over time. The symptoms that are more common are sleep changes, impaired behavior, movement, and cognition [5]. Research shows that the location of Lewy body accumulation impacts the clinical signs and symptoms the individual experiences [3]. If Lewy bodies develop in the brainstem and cerebral cortex first, the condition is called dementia with Lewy bodies, and the onset of the dementia is early [3]. If Lewy bodies accumulate in the brain stem and then develop into the cerebral cortex as time passes, the onset of dementia appears later, and this condition is called Parkinson’s disease dementia [3].
Rapid Eye Movement Sleep Behavior Disorder
Rapid eye movement (REM) sleep behavior disorder is sometimes the first clinical sign of dementia with Lewy bodies [2]. Individuals with this disorder move and talk while dreaming in their sleep [2]. The movements can be violent and cause the individual to fall out of bed [5]. Individuals may kick, punch, and scream in REM sleep (the second half of their sleep) [4]. REM sleep behavior disorder is seen in 76% of patients with dementia with Lewy bodies [4].
This disorder can cause fractures and contusions in some individuals resulting from falling out of bed [4]. This can not only affect the individual, but also the sleep partner of the patient [4]. In some cases, separate sleeping arrangements are needed for the safety of the individual and their sleeping partner. A questionnaire by the patient and sleep partner is part of the diagnosis of REM sleep behavior disorder [14]. If the individual does sleep next to someone, this questionnaire can be helpful as most of the time the patient cannot recall the events while asleep [14]. Video polysomnography is required for a complete diagnosis of this disorder [14]. These events while asleep must be repeated to meet the diagnostic criteria [14].
Other Sleep Disorders
Other disorders of sleep include sleepiness in the daytime, restless leg syndrome, confusion when awakened, and obstructive sleep apnea [4].
Visual Hallucinations
Visual hallucinations are present in about 80% of individuals with Lewy body dementia [1]. Visual hallucinations are a core clinical symptom of dementia with Lewy bodies [4]. They are more common in women than in men [4]. Individuals are aware of these hallucinations and can tell others what they experienced [4]. Visual hallucinations are vivid to individuals and have been said to range from people walking around the house to seeing people that have died sitting next to them [6]. During the beginning stages of the disease, the hallucinations do not seem to affect the patient as much as when the disease progresses [6]. Patients are said to be afraid of these hallucinations in the later stages of the disease [6]. Nonvisual hallucinations are less common, however can occur in some patients [1]. These hallucinations include smelling or hearing something that is not in their surroundings [1].
Fluctuation in Cognition
Fluctuation in cognition is also a clinical sign that is associated with dementia with Lewy bodies [4]. This symptom includes changes in attention, concentration, and alertness [5]. These changes are random and can differ day-to-day [1]. Symptoms can include delirium, and mimic symptoms that are caused by metabolic diseases, which can further the difficulty with identifying the correct diagnosis [4]. To diagnose dementia with Lewy bodies, one of the episodes must be confirmed [4]. These fluctuations can be present in other forms of dementia in their later stages but when present in earlier stages, they point to dementia with Lewy bodies [4].
Memory loss that impacts activities of daily living can be found in later stages of Lewy body dementia [1]. Memory loss early on is more often a characteristic sign of Alzheimer’s dementia [1]. Confusion about the individual’s whereabouts, and inability to multitask can also occur in dementia with Lewy bodies [4].
Problems with Movement
Problems with movement are signs of Lewy body dementia. Bradykinesia (slow movements) and rigidity occur in about 85% of individuals with dementia with Lewy bodies [4]. Tremor at rest is less common in individuals with this condition [4]. Loss of coordination and difficultly swallowing can occur [1]. Problems with movement greatly increase the risk of falls for these individuals [4]. This can place strain on the individual’s caregivers [4].
Autonomic Dysfunction
Autonomic dysfunction can be present in dementia with Lewy bodies and Parkinson’s disease dementia. This symptom is seen in about 90% of patients with Lewy body dementia [4]. The symptoms that result from autonomic dysfunction can be constipation, urinary incontinence, orthostatic hypotension, erectile dysfunction, and dizziness [1] [4]. Orthostatic hypotension appears as early as five years prior to the diagnosis of Lewy body dementia [4]. Syncope and falls are usually the result of orthostatic hypotension [4]. Constipation can also occur earlier in the disease process [4].


Self-Quiz
Ask Yourself...
- What is REM sleep behavior disorder?
- Are visual hallucinations common in Lewy body dementia?
- What does cognitive fluctuation mean?
- What are symptoms of autonomic dysfunction seen in dementia with Lewy bodies?
Diagnostic Tests and Evaluations
Throughout this course, it has been mentioned that Lewy body dementia is significantly underdiagnosed. Individuals are usually diagnosed as the disease progresses due to the symptoms that overlap with other forms of dementia and other neurological and psychiatric disorders [3]. An autopsy of the brain after death is one of the only ways to have a conclusive diagnosis of Lewy body dementia [16]. There are certain diagnostic criteria and diagnostic tests that are used to diagnose an individual with Lewy body dementia.
Diagnosis by Symptoms
Lewy body dementia is probable when an individual experiences dementia and two main features of the disease. Lewy body dementia is a potential diagnosis if the individual experiences progressive dementia and one main feature of the disease [3]. As discussed in the clinical signs and symptoms section of this course, key features of Lewy body dementia are cognitive fluctuations, dementia that progresses, problems with movement (signs of parkinsonism), REM sleep behavior disorder, and visual hallucinations [3] [16].
Timing of symptoms is relevant for distinguishing between the two forms of Lewy body dementia [3]. Currently healthcare providers use the time span of one year to distinguish the two forms [3]. If dementia occurs within one year of the appearance of movement problems, then a diagnosis of dementia with Lewy bodies is used [3]. If an individual is diagnosed with Parkinson’s disease and starts experiencing symptoms of dementia more than one year after their Parkinson’s diagnosis, then Parkinson’s disease dementia is used [3]. Some indicative biomarkers in addition to clinical symptoms are used in diagnosis [4]. Some of these biomarkers can be found in cerebral spinal fluid (CSF) and are still under research [4].
Cognitive Tests
Cognitive testing can be used to show the cognitive impairment of patients with Lewy body dementia [3]. The Mini-Mental State Examination can be used as an initial screening test [4]. This exam tests cognitive function by focusing on concentration, orientation, and memory [15]. This test can be limited since symptoms of these patients can fluctuate day to day [3]. Another cognitive function test is the Montreal Cognitive Assessment (MoCA) [15]. Providers do not usually diagnose based on a single test; instead, they use the results to look for other signs and symptoms of Lewy body dementia [4].
Imaging Tests
There are certain imaging tests that can help with diagnosis and distinguishing between other dementia disorders. A single-photon emission computerized tomography (SPECT) scan can help support a diagnosis [16]. This is a nuclear scan that can sense radioactivity [16]. If the SPECT scan shows a reduced dopamine transporter uptake in the basal ganglia, this can be a sign of Lewy body dementia [16]. This will separate the diagnosis between Lewy body dementia and Alzheimer’s disease [4]. Performing this scan alone will not lead to a possible diagnosis of Lewy body dementia; however, in combination with other diagnostic tests, the scan can lead to a more certain diagnosis [4]. Results from these scans can appear normal initially, and the scan may need to be repeated [4].
An iodine- MIBG myocardial scintigraphy can be performed to support Lewy body dementia [16]. This would show decreased communication of cardiac nerves [16]. The results may be skewed by heart disease or certain drugs [4]. A CT or MRI may be used but these imaging tests can present mixed results [4]. With Alzheimer’s disease, significant atrophy is seen in the medial temporal lobes [4]. There is normally minimal atrophy in Lewy body dementia [4].
As mentioned earlier in the course, video polysomnography is needed for the diagnosis of REM sleep behavior disorder [14]. This sleep study without the loss of muscle tone can also point towards a diagnosis of Lewy body dementia as REM sleep behavior disorder has now moved to a key feature of this disease [14].

Self-Quiz
Ask Yourself...
- What types of imaging tests can be used in the diagnosis of Lewy body dementia?
- Why are cognitive tests used in diagnosis of this disease?
- What criteria are needed for a probable diagnosis of Lewy body dementia?
- Can the cost of diagnostic imaging lead to a reduction in diagnosing Lewy body dementia?
Case Studies
Case Study #1
A 74-year-old male presents to his primary care provider after his wife reports abnormal behavior over the past several months. His wife reports the patient kicks and screams during sleep. The patient reports seeing little people walking around the living room during the day. The wife states the patient some days will fall asleep throughout the day while completing activities. The patient states difficulty walking and muscle stiffness.
The wife states last week the patient was supposed to go to the local grocery store to buy milk. After two hours passed, the wife called her husband as she was worried about him. He states he got lost finding the grocery store and did not know where he was. The wife said she had to drive to find her husband and bring him home. The patient also reports dizziness when standing. After the nurse obtained an orthostatic blood pressure, the patient was positive for orthostatic hypotension.
- Which form of dementia is the patient most likely experiencing?
- What type of symptoms is the patient experiencing that would point to that diagnosis?
- What diagnostic tests or evaluations should the patient undergo?
- What types of supportive treatment should the healthcare provider include in the treatment plan for this patient?
Case Study #2
A 70-year-old female presents to the emergency department via EMS after falling at home. The patient’s daughter called 911 after finding her on the floor when going to visit her. Upon arrival at the emergency department the patient is oriented to self. The patient does not know where she is or what happened to precipitate the fall. The patient has a past medical history of hypertension, diabetes type II, and Parkinson’s disease.
The patient was diagnosed with Parkinson’s disease two years prior. The daughter states the patient has been forgetful lately and not acting like herself. The daughter reports that her mom’s behavior is different from day-to-day. An MRI and the National Institutes of Health Stroke Scale (NIHSS) are used to rule out a cerebrovascular accident. A complete blood count (CBC), a complete metabolic count (CMP), and urinalysis are obtained. The patient suffered a contusion to her right cheek and a right radius fracture. The patient states that she sees figures dancing in the room and smells popcorn. The patient appears to be frightened by the hallucinations. The patient’s daughter states for the last six months the patient has had difficulty swallowing and a reduced appetite.
- Which form of dementia is the patient most likely experiencing?
- What would the MRI of the patient most likely show?
- What clinical signs of dementia is the patient exhibiting?
Management
Currently there is not a cure for Lewy body dementia, only supportive treatment. The management of this disease involves a multifaceted approach, including therapies, pharmacological treatments, and family support.
Therapies
Specific therapies can help with symptom management and help improve the individual’s quality of life. Occupational therapy can help improve a patient’s ability to complete activities of daily living. Speech therapy can help with swallowing coordination and improve the clarity and volume of speech [5]. Physical therapy can aid patients with problems with movement [5]. Mental health counseling can help individuals and their families with managing behaviors and their emotions [5].
Medications
Pharmacotherapy can help with supportive treatment but can also worsen symptoms if certain medications are taken. Below are some examples of medications that are used by patients with Lewy body dementia.
- Cholinesterase Inhibitors are used to help cholinergic activity to improve cognitive function [6].
- Rivastigmine was one of the first of these drugs to be tested [6]. Patients were noted to have improved on their cognitive exams [6]. It is also shown to reduce hallucinations and lessen anxiety [6]. This class of drugs has been said to improve the quality of life for some patients [4].
- Donepezil and Galantamine are also used to reduce dementia symptoms of hallucinations [6]. These drugs were initially targeted for patients with Alzheimer dementia, however, they are effective for individuals with Lewy body dementia as well [3]. A study was done stating even if there is not a sign of cognitive improvement, this should not be the criteria to stop the medication as this medication has been proven to protect the individual from further impairment of cognition [4].
- Atypical Antipsychotics are prescribed to patients that are not seeing a reduction of symptoms while on cholinesterase inhibitors [3]. These types of drugs are seen as controversial due to the many adverse effects that have been seen in patients [4]. Drugs such as haloperidol and olanzapine should be avoided in patients with Lewy body dementia as they can cause neuroleptic malignant syndrome (a life-threatening condition) [5]. Quetiapine, clozapine, pimavanserin, and aripiprazole are atypical antipsychotic drugs that can be used to improve agitation and help prevent cognitive fluctuations [5].
- Carbidopa-Levodopa can be used in patients to manage problems with movement [3]. This medication can cause side effects and can result in hallucinations, delusions, and increase confusion [3]. Providers should begin with low doses of this medication [3].
- Clonazepam is a benzodiazepine that can lessen the REM sleep behavior disorder that patients with dementia with Lewy bodies can experience [5]. Between 33-65% of patients with REM sleep behavior disorder can experience an injury while sleeping [5]. This medication has been proven to decrease injuries that occur during sleep [5]. Clonazepam can adversely affect individuals with gait disorders or sleep apnea [5].
- Melatonin is a hormone that can be used for patients that are affected by REM sleep behavior disorder (5). Studies have shown that the use of melatonin lessened the frequency and the severity of symptoms associated with REM sleep behavior disorder [5]. Melatonin can have side effects such as headaches in the morning, sleepiness during the day, and hallucinations [5].
- Memantine is used to treat dementia symptoms [5]. This medication is an NMDA receptor antagonist that stops effects of glutamate in the brain [5]. Memantine has been shown to improve symptoms of patients early in the disease [5].


Self-Quiz
Ask Yourself...
- What type of therapies are used in management of Lewy body dementia?
- What class of drugs are used to help improve cognitive function?
- What are some medications that should be avoided in patients with Lewy body dementia?
- Why is melatonin used in patients with Lewy body dementia?
Nursing Care
As mentioned before, there is not a cure for Lewy body dementia. Caring for patients with Lewy body dementia includes supportive treatment. Nurses can play a significant role in caring for these patients and providing the family with support. Home health nurses can help with frequent assessment of the patient and their environment [3]. Environmental changes may be needed to protect the patient from falls and other accidents. Home health nurses can assess the type of assistance the patient would benefit from.
Nurses can aid the family by providing education to assist in how to care for the patient. Family members and caregivers must be aware of the changes in behavior, fluctuations in cognition, and hallucinations that the individual might experience [3]. Nurses must also provide education to the caregiver of the patient on the side effects of certain medications, as they can affect an individual with this disease [7].

Self-Quiz
Ask Yourself...
- Are there any modifications that nurses must apply to care for patients with Lewy body dementia?
- Whose role is it to educate patients and their family members?
Family Support
Lewy body dementia is growing in recognition; however, many people might not be aware of this condition and the disease process. Family members need support from health care professionals to better care for their loved ones. Support can come in the form of education and preparing the family for the symptoms the individual may experience. The cognitive function of patients with this disease can be very limited [3]. Family members must be educated on monitoring the individual closely to promote safety [3]. These individuals are at a high risk for falling and developing aspiration pneumonia (due to swallowing difficulties) [3]. Family members should be educated in preparing for an emergency.
Individuals with Lewy body dementia may need care and the family needs to know how to inform health care providers of their specific needs. It is important to educate family members that their roles in their past relationship with the patient will likely change due to the disease process. To prevent caregiver burnout, family members must be aware of their limitations and know when they need help [7]. Modifying the patient’s home may be needed for patient safety [3]. Each patient may have specific needs and family members should know what modifications may be necessary [3].

Self-Quiz
Ask Yourself...
- What type of support do you feel is important to give family members of loved ones with this disease?
- What should nurses include in education for fall risk safety for family members while the individual is at home?
- Can nurses help to prevent caregiver burnout?
Prognosis
The prognosis of Lewy body dementia can be viewed as poor. As mentioned briefly earlier in this course, this disease is progressive and after diagnosis, the life expectancy is five to eight years [3]. The range of expectancy has also been attributed to delay in diagnosis, which can further delay supportive treatment to improve quality of life for the individual [3]. Patients can die from complications from the disease. Complications can include cardiac complications, falls, adverse effects from medications, pneumonia, and suicide [3].
Compared to Alzheimer’s dementia, the risk of hospitalization or death due to respiratory infections is higher in patients with Lewy body dementia [8]. The median age at death is said to be similar between patients with Alzheimer’s dementia and Lewy body dementia [8]. The life expectancy from diagnosis to death is shorter in patients with Lewy body dementia [8]. The patient’s environment has been shown to play a role in the increased risk of mortality [8]. Patients in nursing homes have been shown to have a higher risk of mortality [8]. Caregivers can decrease the risk of complications by educating themselves on this disease and keeping their loved ones safe.

Self-Quiz
Ask Yourself...
- What are some complications of Lewy body dementia?
- How can the patient’s environment increase the risk of mortality with this disease?
- Why do you think there is delay in diagnosis with Lewy body dementia?
Resources for Family Support
Lewy body dementia is a diagnosis that can affect all aspects of an individual’s life and their family members lives. As nurses we must provide support for family members so they can better care for their loved ones and improve their quality of life. As recognition of this condition grows, family support resources are increasing. The Lewy Body Dementia Association is a nonprofit organization that raises awareness and provides support for families with individuals that suffer from Lewy body dementia [10]. Support groups can be found on their website to help families across the country in their local area [10].
The Lewy Body Dementia Association was started by caregivers of individuals with this condition. They also focus on education and research into the disease. This association is a resource for family members [10].
Another resource for family members is The Lewy Body Dementia Resource Center. This is a nonprofit charitable organization that gives assistance and support to those who care for someone with Lewy body dementia [9]. This organization was founded by caregivers of individuals with Lewy body dementia. They have a support phone line that is available seven days a week to answer questions [9]. They also promote research and early diagnosis of this disease [9].

Self-Quiz
Ask Yourself...
- How can support of family members improve the quality of life of a patient with Lewy body dementia?
- What are some examples of resources for caregivers of individuals with Lewy body dementia?
- Can providing resources to the community help with early diagnosis of this disease?
Research Programs
Lewy body dementia is the second most common form of dementia in the United States [4]. This illness is thought to be underdiagnosed and commonly mistaken for other neurological disorders [3]. Research on Lewy body dementia can decrease the time it takes to diagnose a patient, and can help with management of the condition.
The National Institute of Neurological Disorders and Stroke provides support for a variety of research endeavors for Lewy body dementia [11]. In 2021 The National Institute of Health spent $93 million dollars on Lewy Body dementia research [11]. One program is the Biomarkers for Lew body dementias program. This program aims to increase clinical data collection from patients with this condition, find biomarkers to expand further research, and allow access to the science community to help with further studies [11]. Another program is the Parkinson’s Disease Biomarkers Program. This program’s purpose is to collectively research with healthcare professionals, patients and family members, and technology professionals to increase biomarker research [11].
Biomarker research has been increasing in Lewy body dementia. A biomarker is a feature that can specifically indicate a certain disease [12]. For quite some time there were not any identified biomarkers for Lewy body dementia. There are certain biomarkers that aid in distinguishing Alzheimer’s disease from Lewy Body dementia [13]. These biomarkers can be assessed through imaging or in cerebral spinal fluid [13]. Currently these biomarkers are only helpful if another disease is doubtful [13].
New biomarkers are needed to separate Alzheimer’s dementia from Lewy Body dementia and other neurological disorders [13]. Biomarkers that can help with early diagnosis would be beneficial for early treatment [13].


Self-Quiz
Ask Yourself...
- Why is researching biomarkers important for early diagnosis of Lewy body dementia?
- Is there more research conducted on Alzheimer dementia than on Lewy body dementia?
- What are some organizations that promote research for this disease?
Conclusion
Lewy Body dementia affects 1.4 million Americans [2]. The disease is underdiagnosed and often diagnosed incorrectly. Incorrect diagnoses can lead to worsening of symptoms and the administration of drugs that can lead to adverse effects.
Educating healthcare providers and the community about Lewy body dementia can improve quality of life for individuals with the disease. As nurses, we must be informed about this disease to better educate our patients and their caregivers, and to know how to advocate for our patients.
Sexual Harassment Prevention
Introduction
Sexual harassment is a serious issue within the healthcare workplace. One systematic review research study found that sexual harassment rates against female nurses was as high as approximately 43% (5). According to an article published in the American Journal of Critical Care in 2021, recent studies estimate around 60% of female nurses and 30% of male nurses have reported sexual harassment (3).
For both student and registered nurses, patients were the most likely perpetrators. However, this varies, and some research suggests that physicians and patient relatives were also at an increased likelihood of being perpetrators of sexual harassment toward registered nurses (8). It is important to remember that sexual harassment is not limited to female registered nurses; male nurses are also at risk of experiencing sexual harassment in the workplace.
The impacts of sexual harassment affect nurses in many negative ways. There are obvious psychological consequences, but there is also evidence to suggest that work performance and productivity can also be negatively affected (12). Many states have recognized the significant impact of this issue and have taken measures to empower nurses to prevent and/or address sexual harassment.
What Is Sexual Harassment?
Sexual harassment is commonly thought to be unwelcome contact. However, sexual harassment takes many forms. It can be defined as unwelcome sexual behaviors or actions which may be verbal, physical, mental, or visual (13).
Listed below are some common examples of potential sexual harassment:
- Actual or attempted rape or sexual assault
- Pressure for sexual favors
- Deliberate touching, leaning over, or cornering
- Sexual looks or gestures
- Letters, telephone calls, personal e-mails, texts, or other materials of a sexual nature
- Pressure for dates
- Sexual teasing, jokes, remarks, or questions
- Referring to an adult as “girl,” “hunk,” “doll.” “babe,” “honey,” or other similar terms
- Whistling at someone
- Turning work discussions to sexual topics
- Asking about sexual fantasies, preferences, or history
- Sexual comments, innuendos, or sexual stories
- Sexual comments about a person’s clothing, anatomy, or looks
- Kissing sounds, howling, and smacking lips
- Telling lies or spreading rumors about a person’s sex life
- Neck and/or shoulder massage
- Touching an employee’s clothing, hair, or body (4, 13)
The U.S. Equal Employment Opportunity Commission defines sexual harassment as “unwelcome sexual advances, requests for sexual favors, and other verbal or physical harassment of a sexual nature.” Sexual harassment can also include offensive remarks about an individual’s gender or sexual orientation. No matter the type or amount of harassment, it can disrupt the workplace and potentially create a hostile work environment (10,11) As you can see, the definition of sexual harassment is broad and can encompass many situations.

Self Quiz
Ask yourself...
- Many nurses do not know that the definition of sexual harassment is broad. Knowing this, are there any situations you would consider sexual harassment, where you previously would not have?
Why Are Nurses Vulnerable to Sexual Harassment?
Nurses are vulnerable to sexual harassment by the very nature of their position. The role of nursing surpasses many societal norms regarding physical contact and involves intimate care of patients both physically and emotionally. This role is often exploited by perpetrators – they may take advantage of a nurse’s position and caring demeanor as a means to harass them (8).
Staff-on-staff harassment is also commonly reported by nurses (8). Nurses are potentially predisposed to this type of harassment due to their subservient position to many staff members (physicians, administration) and the subsequent power imbalance that results.

Self Quiz
Ask yourself...
- What workplace environmental factors can lead to nurses experiencing sexual harassment?
Key Points for Sexual Harassment
Sexual misconduct vs. sexual harassment – Sexual misconduct is a type of sexual harassment. Sexual behavior can turn into sexual harassment when the recipient receives the behavior in an unwelcome manner. The term “unwelcome” refers to unsolicited or uninvited behavior and undesirable or offensive behavior (11).
Females and males can both be victims – Any unwelcome sexual behavior may be considered sexual harassment, regardless of the gender of the perpetrator and recipient. Male-on-male, female-on-female, female-on-male, and male-on-female types of harassment may occur (11).
Sexual harassment can affect witnesses – Anyone who is affected by the sexually offensive conduct may be a victim. This may include a person witnessing or overhearing sexually-harassing behavior (1).
It can occur outside the working environment – The “working environment” is not limited to the physical location of work. A “working environment” may be extended to any location where work occurs, such as remote locations, off-site locations, and temporary working locations (1, 11).
It doesn’t only occur in person – Sexual harassment can occur on and off the clock. It can occur physically and virtually. Unwelcome sexual conduct through email, phone calls, texts, social media postings, and other mediums may constitute sexual harassment (6).
Two Types of Sexual Harassment
- Quid pro quo – Quid pro quo means “a favor for a favor.” In this sense, it refers to an authority figure (manager or supervisor) requesting a sexual favor in exchange for preferential treatment. This could be in the form of a promotion, raise, preferred assignment, or any other job benefit which they may affect (7).
- Hostile work environment – Another method by which an individual may coerce sexual favors is through the threat or actuality of a hostile work environment. This refers to creating or threatening to create an intimidating, hostile, or offensive work environment in order to influence sexual favors or behavior (7).

Self Quiz
Ask yourself...
- What would be an example of quid pro quo?
- How is this type of harassment different than hostile work environment?
What Should Nurses Do If They Experience Sexual Harassment?
If you feel you have been the victim of unwelcome sexual behavior (sexual harassment) there are avenues available to you for support and to report the behavior.
- While it may not be an easy thing to do (or even possible), try to make it known that the sexual behavior is unwelcome and unwanted. It is your right to inform the person of your stance and to demand the behavior cease. Though this can be difficult and uncomfortable, it is often the most effective method (2). If you decide to confront the perpetrator, try to remain calm and de-escalate the situation as much as possible.
- You should be explicit in explaining the behaviors that are unwelcome so that the perpetrator can fully understand his/her actions. If you are uncomfortable confronting the perpetrator, consider confiding in a close friend, coworker, or supervisor who can accompany you or advise you on the next steps.
- Another way is to interrupt the harasser to distract them from the situation (2)
- Next, make sure to document the scenario. Write down all of the details that you can recall; including any witnesses. This can be helpful in the future.
- Reporting the issue through the appropriate channels is the next step. Oftentimes, this involves speaking with your supervisor and someone in human resources. While discussing the situation, do not make excuses for the perpetrator or try to “shrug it off.”
How or whether you report sexual harassment is a personal choice, and you are not limited. However, you should strongly consider reporting the incident because it could escalate further in the future. The perpetrator may also be sexually harassing others. Every workplace should be free from sexual harassment and many states have laws protecting nurses against workplace sexual harassment, including harassment received from patients and family members. There are several options for reporting sexual harassment, and there are several nuances with jurisdiction and handling of complaints. However, you should not be discouraged from reporting through the appropriate avenues.
1. Within your organization.
You may contact your supervisor or human resources representative to report an incident. This is often a more comfortable route for nurses as they may be familiar with these individuals. Your organization should have policies and procedures for handling sexual harassment reports which may include escalation to law enforcement as necessary. This is often the fastest method for reporting. Remember that reporting to your supervisor, ethics officer, or human resources official does not preclude you from reporting to other agencies as appropriate. If you wish to remain anonymous, check with your organization to see if they have a policy that gives you that option.
2. Law enforcement.
Criminal incidents of sexual harassment may be reported to law enforcement as appropriate. Oftentimes your human resource officer can assist in determining if this is necessary or required by state law. If you ever feel that your physical safety is threatened, do not hesitate to contact law enforcement.
3. Office of Executive Inspector General (state government employees).
State employees may file a report directly with the OEG. To initiate a report, it is best to contact your ethics officer for guidance.
4. U.S. Equal Employment Opportunity Commission (EOCC).
Sexual harassment is a violation of section 703 VII. The EOCC is charged with administering this statute and provides another option of relief for those who have experienced sexual harassment. The statute for reporting an offense to the EOCC is 180 days from the date of the incident. Of note, the EOCC may hold employers responsible for taking all steps to create an environment free of sexual harassment and can offer an additional avenue for support. This law may be extended up to 300 days depending in the state laws surrounding sexual harassment (10).

Self Quiz
Ask yourself...
- How would you handle sexual harassment differently knowing your rights and reporting avenues?
- Are there any previous situation you would have handled differently?
Whistleblower Protections
Retaliation for reporting sexual harassment is illegal under both federal and state statutes. The U.S. Equal Employment Opportunity Commission prohibits retaliation aimed at employees who assert their rights to be free of harassment (9).
Concluding Points
- Sexual harassment can take place in many venues and formats. It is broadly defined as any unwanted or unwelcome sexual behavior or advances.
- Sexual harassment is experienced frequently by nursing professionals due to the nature of their positions.
- You have a right per federal and state laws to be free of sexual harassment in the workplace.
- If you experience sexual harassment, you should tell the harasser to stop and report the incident in one of the various methods listed above. Do not forget to document provide a thorough report of the incident.
- You have a right to report sexual harassment without retaliation per federal laws.
Connecticut Domestic and Sexual Violence
Introduction
Each year, more than 10 million men and women in the United States experience physical abuse from an intimate partner. One in three women and one in four men have experienced some form of physical violence from an intimate partner in their lifetime and one in 10 women has been raped by an intimate partner (18). Such experiences have a lasting impact on physical and mental wellbeing, employment and economic status, effects on children who may witness such abuse, and, in severe cases, may even result in death.
Healthcare professionals are on the front lines of screening and prevention for domestic and sexual abuse and may be able to recognize early signs of abusive relationships, improve client connections to resources, and reduce the overall incidence of acute and long-term injury from abuse. This course aims to educate healthcare professionals on risk factors, signs of abuse, characteristics of abusers, and the role of healthcare in interrupting the abuse cycle.
Defining Domestic Abuse
The Department of Justice defines domestic violence, or intimate partner violence, as “a pattern of abusive behavior in any relationship that is used by one partner to gain or maintain power and control over another intimate partner.” Violence involving intimate partners accounts for 15% of all crime (18). There are various categories of abuse.
- Physical
Physically harming a partner by any manner, including hitting, slapping, shoving, etc. Can also involve denying medical care to someone in need as well as forcing drugs or alcohol use upon someone so as to alter their cognition.
- Sexual
Attempted or successful coercion to participate in sexual contact without consent. Includes rape (including within marriage), sexually demeaning, harming genitals, or forcing sexual acts after physical violence.
- Emotional
Patterns of chronic criticism, name-calling, or demeaning behaviors that damage a person’s self-worth.
- Economic
Use of coercion, fraud, or manipulation to restrict a person’s access to money, assets, or financial information. Or unethically acquiring and/or using someone’s economic resources through exploitation or improper conducting of power of attorney, guardianship, or conservatorship roles.
- Psychological
Threats or intimidation, forced isolation, destruction of property.
- Technological
Use of technology, such as online platforms, computers, mobile phones, cameras, apps, etc. to threaten, harm, control, harass, stalk, impersonate, or monitor another person (22).
Each of these categories has its own nuances and examples, but all consist of acts or threats that influence the weaker or subordinate partner. For the purpose of this course, we will mostly cover physical and sexual abuse, but all forms of abuse are valid and many times overlap with each other. Abusers use tactics such as (22):
- Intimidation
- Manipulation
- Humiliation
- Isolation
- Fear
- Coercion
- Blame
- Injuries/pain
Further information about the epidemiology of domestic violence will be covered below, but it is important to note that anyone can become a victim of domestic violence, including people of all races, ages, sexual orientations, and gender identities. People of all socioeconomic and education levels can be affected, and all types of relationships can be involved; including couples who are opposite-sex, same-sex, married, dating, co-parenting, or living together.
Affected individuals include not only the abused, but also family members (particularly children), coworkers, friends, and other members of the abused person’s community. Frequently witnessing domestic violence as a child increases the risk of becoming a victim of domestic abuse or an abuser in adulthood by demonstrating this as a “normal” way of life (22).


Self Quiz
Ask yourself...
- Which types of abuse do you think may be the most obvious or easy to identify?
- Which types are more subtle or difficult to identify?
- Before reviewing the epidemiology information in the following section, are there particular groups of people or characteristics that you think would be most susceptible to each type of abuse?
- What preconceived notions do you think might contribute to those opinions?
Epidemiology of Abuse
As discussed above, anyone can be a victim of domestic violence, however there are particular populations who are at an increased risk and more likely to be victimized. Awareness of these demographics is useful for healthcare professionals when trying to detect situations where abuse may be more likely. An overview of domestic violence prevalence for at-risk populations is discussed below.
Gender
Women are much more likely to be affected by domestic violence than men.
- 1 in 3 women has experienced some form of physical violence form an intimate partner, though the severity varies widely.
- 1 in 4 women has experienced severe intimate partner violence either of a physical or sexual nature, compared to 1 in 9 men.
- 1 in 7 women have experienced a physical injury from an intimate partner, as opposed to 1 in 25 men.
- 1 in 7 women has been stalked by a partner to a point where they feared harm; conversely 1 in 18 men have had this experience.
- 1 in 10 women have been raped by an intimate partner.
- 72% of all murder-suicides involve intimate partners and 94% of the victims of murder-suicides are women (18).
- Women are at risk for contraception coercion, where a partner pressures them to become pregnant or tampers with contraception to cause pregnancy (1).
Pregnant Women
Pregnant women are particularly vulnerable, and their risk of abuse is higher during this time, further complicating the health risks of abuse.
- 1 in 6 abused women is first abused during pregnancy
- Over 320,000 women experience domestic violence during pregnancy annually (14)
Ethnicity/Race
Minority race groups are more at risk for experiencing domestic violence. Department of Justice (DOJ) survey data indicates that 51.3% and 17.7% of white women report having experienced physical and sexual violence respectively, while non-white women report experiencing these at 54% and 19.8% respectively (26).
Among minorities, American Indian and Alaskan Natives are among the most at risk. This group experiences high poverty rates, particularly on reservations, increased drug and alcohol use, and minimal resources for Natives seeking culturally specific shelter or safety from abuse, all of which increases the risk and prevalence of domestic violence, particularly among Native women (26)
- Over 84% of Native women experience some form of violence during their life
- American Indians are 3 times more likely to be a victim of sexual violence than all other ethnic groups
- 55.5% of Native women experience domestic violence in their lifetime
- 66.6% experience psychological abuse from a partner
- Over half have experienced sexual assault (26)
For the Black community, factors like racist societal and legal structures have created gaps in economic opportunities, education, access to healthcare, and access to safety/resources that puts Black men and women at higher risk of domestic violence than their white peers. Due to stereotypes and inconsistent cultural competence among law enforcement, jurors, and judges, Black victims of abuse are more likely to be arrested and less likely to be believed by the legal system than white victims (13).
- 45.1% of Black women and 40.1% of Black men experience domestic violence of a physical or sexual nature in their lifetimes
- 53.8% of Black women and 56.1% of Black men have been victims of psychological abuse in their lifetime
- 8.8% of Black women have been raped by a partner in their lifetime
- Homicide involving domestic partners was highest among Black women in 2017, at 2.5 per 100,000 (16)
Age
Opposing ends of the age spectrum are both at increased risk of victimization, with teens and young adults as well as elderly people being at higher risk than the rest of the population.
Teens are at an increased risk due to their inexperience with dating and relationships and susceptibility to peer pressure. They may also feel hesitant to tell an adult about abuse for fear of consequences or punishment. They may not recognize behaviors as abusive right away and may perceive controlling or jealous behaviors as signs of love. Teens who have witnessed repeated domestic violence among parents or other family members may also believe that this is how normal relationships function.
According to 2023 data, one in 12 high school students report physical violence and one in 12 report sexual violence in a dating relationship (5).
- 1.5 million high school students are abused in a dating relationship annually (only 33% ever tell anyone about it)
- 26% of teens are victims of cyber dating abuse; female teens were twice as likely to experience this as male teens
- 57% of teens report knowing someone who has been physically, sexually, or verbally abused in a relationship (19)
Older adults are also at an increased risk, often due to impaired physical or cognitive abilities that require them to rely on a caretaker. They may be isolated, with limited social support or without the ability to tell someone what is happening to them.
- It is estimated more than 10% of older adults who live in communities experience physical, psychological, sexual, or financial abuse from a caretaker
- Only about 1 in 14 of these incidents are reported
- A spouse or intimate partner is the perpetrator in 57% of physical abuse, 87% of psychological abuse, and 40% of sexual abuse cases
- 39% of firearm homicides involving older adults were committed by a domestic partner (21)

Self Quiz
Ask yourself...
- Why do you think pregnancy puts women at an increased risk of being a victim of domestic violence?
- Think of an elderly client you have cared for before. How easy do you think it would be for a caregiver to take advantage of them?
- Are there other clients of the same age who might be more or less susceptible to this risk?
- What factors do you think affect the level of risk for elderly clients?
LGBTQ Community
Though it is well-known that members of the Lesbian, Gay, Bisexual, Transgender, Queer (LGBTQ) community are at increased risk of violence or harm. In the general population, awareness of domestic violence rates for the LGBTQ community is just beginning to rise, as most existing data is based on heterosexual relationships. Emerging data is revealing that people in the LGBTQ community experience domestic violence at equal or greater rates than their straight and cis-gender peers (20).
*Note: A basic understanding of sex, gender, and sexual orientation is necessary when caring for members of the LGTBQ community so as to offer comprehensive and competent care. These common terms and their definitions are included below for anyone needing clarification.
Quick Terminology Lesson
Sex: A label, typically of male or female, assigned at birth, based on the genitals or chromosomes of a person. Sometimes the label is “intersex” when genitals or chromosomes do not fit into the typical categories of male and female. This is static throughout life, though surgery or medications can attempt to alter physical characteristics related to sex.
Gender: Gender is more nuanced than sex and is related to socially constructed expectations about appearance, behavior, characteristics based on gender. Gender identity is how a person feels about themselves internally and how this matches (or does not match) the sex they were assigned at birth. Gender identity is not related to who a person finds physically or sexually attractive. Gender identity is on a spectrum and does not have to be purely feminine or masculine and can also be fluid and change throughout a person's life.
- Cis-gender: When a person identifies with the sex they were assigned at birth and feels innately feminine or masculine.
- Transgender: When a person identifies with the opposite sex they were assigned at birth. This can lead to gender dysphoria or feeling distressed and uncomfortable when conforming with expected gender appearances, roles, or behaviors.
- Nonbinary: When a person does not feel innately or overwhelming feminine or masculine. A nonbinary person can identify with some aspects of both male and female genders or reject both entirely.
Sexual orientation: A person’s identity in relation to who they are attracted to romantically, physically, and/or sexually. This can be fluid and change over time, so do not assume a client has always or will always identify with the same sexual orientation throughout their life.
Types of sexual orientation include:
- -Heterosexual/Straight: Being attracted to the opposite sex or gender as oneself
- -Homosexual/Gay/Lesbian: Being attracted to the same sex or gender as oneself.
- -Bisexual: Being attracted to both the same and opposite sex or gender as oneself
- -Pansexual: Being attracted to any person across the gender spectrum, including non-binary people
(11)
There are elements of domestic violence that are specific to the LGBTQ community. One example is “outing” or threatening to disclose a person’s sexual orientation or gender identity without their consent. Threatening to out someone can be used as leverage or a power dynamic in psychological abuse, and actually outing someone can lead to an increased risk of rejection and physical or sexual harm depending on who the information is revealed to.
Additionally, members of the LGBTQ community may be afraid to seek help in abusive situations or may even experience discrimination when they do seek help, putting them at greater risk of significant harm. Poorly trained staff, implicit biases of staff, and even gender-specific resources such as women’s shelters can be difficult to navigate for LGBTQ victims (20). Statistics about domestic violence in LBGTQ relationships include the following:
- 61.1% of bisexual women and 43.8% of lesbian women report experiencing rape, physical violence, or stalking by a domestic partner at some point in their life; compared to 35% of heterosexual women
- 37.3% of bisexual men and 26% of gay men report experiencing rape, physical violence, or stalking by a domestic partner at some point in their life; compared to 29% of heterosexual men
- 26% reported experiences of near-lethal violence in male-male relationships
- Fewer than 5% of all LGBTQ domestic violence victims seek orders of protection
- Transgender people are more likely to experience domestic violence in a public setting compared to cis-gender individuals
- Transgender individuals experience unique forms of psychological/emotional abuse such as being called “it” or being ridiculed for physical appearance
- Bisexual individuals are more likely to experience sexual violence than other sexual orientations
- Black LGBTQ individuals are more likely to experience physical violence from a partner than other races
- White LGBTQ individuals are more likely to experience sexual violence from a partner than other races (20)
Disabled Populations
Nearly a quarter of all U.S. adults have some type of physical, cognitive, or emotional disability. People with disabilities are particularly vulnerable to domestic violence.
- Nearly 70% of people who have a disability experience domestic abuse
- People who have a disability are three times as likely to be sexually assaulted than their non-disabled peers (23)
People with disabilities relying at least partially on others to function in their daily life are particularly vulnerable to being intimidated, isolated, or controlled by someone they trust (power imbalance). Some 75% to 80% of domestic abuse of people with a physical disability and 95% of abuse of those with a cognitive disability goes unreported. The types of abuse are often unique to the disability as well, including:
- Invalidation or minimization of disability
- Shaming or ridiculing for disability
- Refusal to help with daily tasks such as bathing, dressing, or eating
- Over or under medicating
- Sexual acts without consent
- Denying access to healthcare services/appointments or medications
- Limiting access to mobility devices such as walkers, wheelchairs, or prosthetics
- Withholding finances
- Threatening abandonment (23)
Certain populations with disabilities are more at risk than others.
- Women who have a disability:
-
- 80% of women who have a disability report sexual assault
- 40% higher rates of domestic abuse
- Violence experienced by women with disabilities may be more frequent or of greater severity
- More likely to experience reproductive coercion, stalking, or psychological abuse
- People in the LGBTQ community who have a disability:
-
- LGBTQ facilities may not be accessible for those with disabilities
- Disability services may not be competent with issues of the LGBTQ community
- Black, Indigenous, People of Color (BIPOC) with disabilities:
-
- Increased risk for police brutality
- Half of Black people with disabilities have been arrested at least once by age 28
- Half of people killed by law enforcement have disabilities (23)
Geographic Location
A person’s location also plays a role in the risk of domestic violence, with rural locations and homelessness increasing the risk.
Twenty percent of U.S. residents live in a rural location (17). Unique characteristics of rural living increase the prevalence and severity of domestic violence in the following three ways.
Geographic Isolation
- 80% of rural counties do not have a domestic violence program
- >25% of rural communities are more than 40 miles from the nearest domestic violence program
- Rural communities lack robust public transportation, and many people are without a car
- Decreased likelihood that a neighbor or community member will see or hear abuse occurring
- Significantly increased time needed for first responders to arrive after an emergency call
- Scarcity of housing options, especially of lower cost, make it difficult to leave (17)
Social/Cultural Barriers
- Rural regions are often more conservative with traditional gender roles (physical or sexual violence against women may be viewed as “normal”)
- Physical and sexual violence or assault may be viewed as private matters not to be discussed outside of the home
- Friends or family may encourage victims to stay in abusive relationships to avoid divorce or for children
- Women may be shamed or not believed for reporting abuse
- Small-town gossip or lack of anonymity may keep victims from pressing charges or seeking assistive services
- Women may be less likely to have a job or financial independence from their partners (17)
Poor or Impartial Criminal Justice Response
- Domestic violence may be seen as commonplace and low priority among law enforcement
- Law enforcement, prosecutors, or judges may have relationships with perpetrators or their families that impede their ability to be impartial
- Law enforcement may hold a patriarchal sense of loyalty to other men and put that above the safety of women in the community (“Good ol’ boys club” attitude) (17)
Due to geographic isolation and lack of resources, as well as potential lack of income or financial independence, many victims in rural locations wind up homeless if they leave an abusive relationship. This comes with its own significant struggles and risks and is often not sustainable, leading the victims back to live with their perpetrators rather than continue being homeless, essentially creating a vicious cycle between homelessness and abuse.
- A 2003 survey revealed 46% of homeless women reported being a victim of physical or sexual abuse in the last year.
- In 2005, 50% of U.S. cities cited domestic violence as a leading cause of homelessness.
- Some landlords have a zero-tolerance policy for domestic violence and will either evict or refuse to rent in the first place to victims of domestic violence. This was as high as 28% in a survey in New York City (27)

Self Quiz
Ask yourself...
- Think of the type of geographic area you work in. What types of resources are available and how long would it take to get there?
- Is public transportation available to take clients there?
- If you had a client who was physically assaulted, how likely would neighbors be to hear or see the incident?
- How long would it take emergency services to get there if your client called 911?
- Now think about how those factors might differ in a location very different from your own
Socioeconomic Status and Education Level
Though people of any socioeconomic status are susceptible to domestic abuse, those with a low socioeconomic status or education level are at an increased risk. This is in part due to the increased isolation and lack of available resources to people in poverty or with low education. Particularly, women who do not work outside of the home or do not have any professional skills with which to get a job are at risk of being more easily isolated or kept from utilizing resources. Those with lower education levels are also more likely to view physical or sexual violence within a relationship as “normal” and tolerate the abuse without attempting to leave.
Women with household incomes below $75,000 annually are seven times more likely to experience physical or sexual violence than women whose household incomes are above $75,000 (27).
There is also a circular relationship between low socioeconomic status and domestic violence, as victims of abuse are both more likely to be poor and also more likely to experience economic loss or financial insecurity due to the abuse. Access to money or work can also be restricted by the abuse as part of the attempt to maintain power and control.
- Between 21-60% of abuse victims lose their jobs from abuse-related reasons (missing work, distracted or poor job performance, etc.)
- Domestic abuse victims lose a combined eight million days of paid work annually due to injuries or home conflict (18).
Immigrants, in particular, may be affected by this as they may be of lower education (or at least unable to fluently speak the language of the new country), often poor or without any assets, and may be unable to work or earn money. They may rely on an abusive partner for money, a place to live, and even communication, keeping them isolated in a relationship that feeds on control/power (25).


Self Quiz
Ask yourself...
- Are there any of the above statistics or risk factors that surprised you?
- Do you think any of the above information might change your awareness of potential abuse situations?
- Think of a time when you cared for someone at an increased risk of abuse. Do you think you were aware of the risk or were you on the lookout for signs of abuse?
- If you have cared for known victims of abuse, what risk factors did they have?
Health Implications of Abuse
There are many health implications for people in abusive relationships. Acute or short-term injuries are typically physical in nature and include things like (9):
- Cuts
- Bruises
- Broken bones
- Concussions
- Burns
Additionally, only 34% of people who sustained a physical injury from domestic violence sought medical care for those injuries, meaning many may have poorly healed injuries or long-term sequelae from lack of proper treatment (18).
There are also long-term consequences or chronic health conditions that result from domestic violence, including:
- HIV or other sexually transmitted infections (STIs) from sexual abuse
- Bladder and kidney infections
- Circulatory/cardiovascular conditions
- Asthma
- Unintended pregnancy, including teenage pregnancy
- Chronic pain
- Arthritis or joint disorders
- Gastrointestinal disorders or nutritional deficiencies
- Neurological disorders including migraines and neuropathy
- Sexual dysfunction (9)
Mental health effects are also significant with victims experiencing increased rates of:
- Anxiety
- Depression
- Post-traumatic stress disorder (PTSD)
- Suicidal thoughts and attempts
- Addiction to drugs or alcohol (9)
Certain populations, such as individuals in the LGBTQ community, are already at an increased risk for mental health issues and suicidal ideations. Therefore, abused members of this population are at a further increased risk.
Additionally, victims of abuse may experience social or economic consequences that in turn worsen their overall health through poorer living conditions, nutrition, and access to healthcare. Economic consequences include (9):
- Interrupted or lost educational opportunities
- Lost professional opportunities
- Damage or destruction to property or items of value
- Medical or legal debt
Health implications may be dependent on age or situation as well. Among the unique risks are pregnant, very young, and very old victims.
Abuse during pregnancy can result in intrauterine hemorrhage, preterm labor, or miscarriage. Chronic stress during pregnancy, lack of prenatal care, or trauma to the fetus can lead to long-term health effects of the infant once born (14). Some women may also be victims of contraceptive or reproductive coercion, where an abuser pressures them to become pregnant or tampers with their contraception to cause pregnancy. Unwanted pregnancy puts these women into a more vulnerable position to be victims of abuse and the above complications (1).
Surveys of youth show that 50% of teens and young adults who have experienced dating violence or rape have also attempted suicide compared to 12.5% of youths without a history of abuse (19). Domestic violence also increases the risk of pregnancy and STIs which can have a more extreme and lasting impact on teens, affecting reproductive or sexual health for the rest of their lives.
For older adults, the risks are increased as well, with elderly victims of abuse having a shorter lifespan than their peers who are not abused. Mental health effects such as depression, anxiety, fear, isolation, loss of self-esteem, and feelings of shame, powerlessness, and hopelessness may be exacerbated because people in this age group are already struggling with a lack of independence or isolation from a social network. Overall, this can reduce quality of life and dignity in an already difficult period of decline (21).
Exposure to domestic violence, even when not directly victimized, also has a lasting impact on health. Children are particularly vulnerable to witnessing or being exposed to abuse:
- 1 in 15 children are a witness to domestic violence during childhood (of those, nearly 60% experience maltreatment themselves).
- Homes with both child maltreatment and intimate partner violence often have more severe levels of abuse.
- 1 in 5 child homicides between ages 2-14 are related to domestic violence cases (15).
Children who are exposed to domestic violence may experience acute symptoms such as:
- Anxiety
- Aggression
- Sleep disruption
- Nightmares
- Bedwetting
- Concentration deficits or poor school performance
Over time, children who are exposed to domestic violence are:
- 3 times as likely to engage in violent behavior as their peers
- More likely to be either perpetrators or victims in their own future relationships
- At greater risk of health conditions like obesity, cancer, cardiovascular disease, substance abuse, depression, and unintentional pregnancy (15)


Self Quiz
Ask yourself...
- Have you ever cared for an acute victim of physical or sexual violence?
- What types of injuries did they have and how might those injuries have healed differently if the client had not sought care?
- To your knowledge, have you cared for any clients with long-term sequelae of abuse?
- How do you think coping with a chronic illness sustained from violence might be different from coping with a chronic illness not sustained from violence?
Perpetrators of Abuse
It is important for healthcare professionals to not only recognize risk factors for victims of abuse, but also risks for becoming a perpetrator of abuse. Truly mitigating risks and reducing the prevalence of domestic abuse requires recognizing and offering services to victims, but also identifying potential abusers and providing interventions to stop abuse at the source.
Risk Factors
The conditions that lead to perpetrators becoming abusers are nuanced and multifaceted, involving individual experiences, past relationships, attitudes of the person’s community, and societal implications (4).
Individual
Individual risk factors are based on lived experiences, existing mental health conditions, and individual stressors. Individual risk factors include:
- Poor self esteem
- Low education level
- Young age
- Problem behaviors in youth
- Drug or alcohol abuse
- Depression or anxiety
- Poor coping or problem-solving skills
- Poor impulse control
- Personality disorders
- Isolation or few friends, small support network
- Economic stress such as unemployment or low income
- Hostile/misogynistic attitudes towards women and strict gender role of male dominance
- Being physically or emotionally abused as a child
Relationship
Relationship risk factors are based on the characteristics of the people involved in the relationship and their attitudes and behaviors within the relationship. Relationship risk factors include:
- Relationships with frequent jealousy, possessiveness, tension, or divorces and separation
- One partner with clear dominance or control the majority of the time
- Families undergoing economic stress or low income
- Network of peers in aggressive or violent relationships
- Parents with low education levels
- Witnessing violence between parents during childhood
Community
Community risk factors are based on the attitudes and social norms of people in the neighborhoods, workplace, or schools a person is involved in. Community risk factors include:
- High poverty and low education rates
- High unemployment rates
- High crime/violence rates
- High drug use
- Low sense of community among neighbors
Societal
Societal risk factors are based on the attitudes and political policies where a person lives on a broader scale, including city and state level. Societal risk factors include (4):
- Emphasis on traditional gender roles (women at home/unemployed/submissive, men work and make family decisions)
- Cultural norms of aggression
- Weak education, health, and social policies or support
Protective Factors
There are some factors that are protective against becoming a perpetrator of abuse, even for people who may have grown up around domestic abuse. Protective factors include (4):
- A strong social support network
- Exposure to strong, positive relationships
- An involved and neighborly community
- Available services and resources within a person’s community
- Access to stable and safe housing
- Access to medical and mental health care
The Cycle of Abuse
In addition to recognizing who may become or be an abuser, it is important to understand and recognize the pattern or cycle of abuse and how perpetrators maintain control in the relationship. While each abuse scenario is unique, the overall patterns are the same and exist in a cycle which may progress quickly or over longer stretches of time. The four main stages are tension, incident, reconciliation, and calm (10).
Tension Phase
During the tension phase, there is a slow increase in the frequency and intensity of irritability, short temper, emotional outbursts, and impatience. There may be external factors such as life stressors, financial strain, work struggles, etc. that make the abuser feel out of control, adding to this rising tension. Victims may report “walking on eggshells” during this time, as they feel the tension build (10).
Incident Phase
Once the tension builds to a breaking point, one or more abusive incidents will occur. Abuse perpetrators do not have an “anger problem” as they are able to control their emotions in places like work, school, or in public. The anger and aggression displayed by a perpetrator is an intentional use of power to regain or maintain control over the weaker partner in the relationship. Incidents can look like (10):
- Intimidation
- Threats
- Physical violence
- Sexual violence
- Verbal violence (insults, name calling)
- Shaming/humiliation
- Blaming
- Social isolation
- Manipulation
- Financial abuse
- Emotional abandonment
Abusers can use many methods of violence and a variety of tactics within each of those methods. The ultimate goal of all behaviors is to maintain control over the victim and remain in a position of power. Figure 1 below provides examples of specific behaviors within each type of violence.
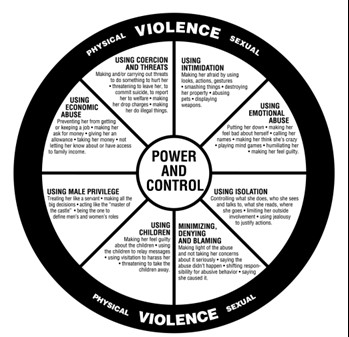
Figure 1. Domestic Abuse Intervention Programs (3)
Reconciliation Phase
Once the incident is over, the perpetrator feels a relief of tension, though the victim likely is at peak anxiety. The abuser may seem to show remorse in the form of apologies, affection, or promises to never become violent again. Victims are often willing to give abusers another chance during this stage because they seem to show genuine remorse or intent to reform (10).
Calm Phase
Next the relationship moves into a calm phase where the perpetrator’s remorse dissipates, and they may begin to dismiss the incident by shifting blame or saying things like “it wasn’t really that bad.” For the victim, this can be confusing or feel like a letdown when the abuser’s previous intent to make changes fades. This eventually shifts back into rising tension and the cycle repeats itself (10).

Self Quiz
Ask yourself...
- Think about the population you work with. Consider who might be at risk for being a victim of abuse but also think about what risk factors you’ve encountered for your clients becoming a perpetrator of abuse.
- What are the community or societal factors in your region that might increase the risk of becoming a perpetrator?
- Think about the abuse cycle and consider why victims may choose to stay in a violent relationship.
- At what point in the abuse cycle do you think healthcare professionals are most likely to encounter victims of abuse or pick up on abuse red flags?
Role of the Healthcare Professional in Abuse
Given all of this knowledge about who is at risk and what goes on in an abusive relationship, you may be wondering how healthcare professionals can help or what your role entails. The responsibility of the healthcare professional lies in a few main areas of identifying and handling abuse situations.
Risk Identification
One of the first steps in disrupting the abuse cycle is identifying those most at risk. Part of this is through knowledge of risk factors and vulnerable populations and signs of abuse, as already covered in this course. Another means of identification is through routine screening of certain populations. Unfortunately, there is a limited number of screening tools available, and tools are almost exclusively targeted at women of reproductive age. Available tools assess for domestic abuse within the last year; there is no recommended appropriate interval to administer screening and it is at the provider’s discretion, though at least annually is typical (24). Some examples of available screening tools include:
- HARK (Humiliation, Afraid, Rape, Kick): A four-question tool that assesses emotional and physical violence
- HITS (Hurt, Insult, Threaten, Scream): A four-item tool that assesses the frequency of domestic violence
- E-HITS (Extended version of HITS): Includes an additional question to assess the frequency of sexual violence
- PVS (Partner Violence Screen): A three-item tool that assesses physical abuse and safety
- WAST (Women Abuse Screening Tool): An eight-item tool that assesses physical and emotional abuse from domestic partner (24)
The above screening tools are well studied in women and have been shown to be effective. Currently, there is a lack of studied and effective domestic violence screening tools in the primary care setting, especially for teens, men, clients in the LGBTQ community, and the elderly. More work is needed in this area. Even for women, screening is not often conducted outside of the obstetrics/gynecology (OB/GYN) setting (24).
Simply asking “Do you feel safe at home?” or “Is there any history of violence in your home?” is also a basic way to cast a wide net among large volumes of patients and reduce the chance of domestic violence going unnoticed. Asking questions like these on admission in the emergency department (ED) or hospital, or during the intake process for office visits can easily be implemented as part of facility policy. Many offices or hospitals will also have signs up in bathrooms, changing areas, or exam rooms that encourage clients to disclose abuse in a confidential and safe way during their visit (24).
Screenings of any kind are most effective when the client is separated from their partner, even briefly. If the abuser is with them, they can be asked to step into the waiting room or, if it is necessary to be more subtle, clients can be asked to leave the room for something inconspicuous, like providing a urine sample, and then lead to a separate room for further, private discussion (24).
Appropriate Response
Timely referral to appropriate ongoing services has been shown to reduce physical and mental harm from violence and abuse. When domestic violence has been disclosed or a screening has come back positive, the attitudes and behaviors of the healthcare professional are important and can have a big impact on the client’s feelings about their care. Appropriate and sensitive behaviors include:
- Listening to clients actively and objectively
- Believing the client
- Validating the client’s feelings and fears
- Avoiding asking “why” questions or placing blame like “Why didn’t you call the police?” or “Why do you stay?”
- Respecting a client’s decision to stay or leave
Plan of Action
Interventions and next steps include (6):
Gathering Additional Information
- Getting a detailed history
- Assessing symptoms
- Taking photographs if necessary (bruise patterns, burns, cuts, etc.)
Assessing Safety
- Verbal/physical threats
- Weapons in the home
- Frequency of violence
- Children or others in the home
Develop a safety plan together with client
- Signs of rising tension
- Who to call or where to go
- Available resources in community
Provide referrals as desired by client
- Police (for order of protection or to press charges)
- Hotlines
- Shelters
- Counseling
Documentation and Reporting
Appropriate documentation of abuse, including detailed history, exam, and any pictures, as well as a safety plan and any resource connection should be included in the client’s chart. Laws about mandated reporting vary by state and healthcare professionals may need to report the documented abuse to authorities.
In Connecticut, there is no requirement to report domestic violence or abuse. Mandated reporting is reserved for abuse of children, disabled people, residents of long term care facilities, the elderly, and healthcare professionals who are impaired or negligent (8).
For situations which must be reported, the report must be made within 12 hours of when a clinician first suspects abuse or becomes aware of an abuse situation. Reports may be made through the Connecticut State Department of Public Health which has various resources and care lines depending on the type of suspected abuse being reported. Examples can be found in the table below (8).
|
Category of Abuse Victim |
Resource for Reporting |
|
Children |
Department of Children and Families (DCF) Child Abuse and Neglect Careline |
|
Disabled person |
Office of Protection and Advocacy for Persons with Disabilities |
|
Residents of long term care facilities |
Commissioner of Social Services |
|
Elderly |
Commissioner of Social Services |
|
Impaired clinicians |
Connecticut Department of Public Health |
If you are required to report an incident, it is best to notify the client prior to reporting so that they are aware and prepared and can utilize their safety plan if they feel this will anger the perpetrator (6).
Counseling/Therapy
When considering counseling, individual therapy is always recommended and beneficial, but it is important to note couples therapy may be contraindicated. If the goal is to maintain the relationship and address abuse cycles, couples therapy should be approached cautiously as this type of treatment may increase the abusive behaviors. Couples therapy may elicit a different viewpoint or information about the relationship that threatens the abuser's desire for control and may increase anger, minimization of abuse, or victim blaming as the abuser now has to work harder to maintain control. This can increase abusive behaviors outside of therapy sessions and put the victim at greater risk.
There is some evidence to suggest couples therapy can be helpful in breaking abuse cycles, but it should only be undergone with an experienced therapist with special knowledge of how to identify and address abuse in a manner that does not exacerbate the abuse (12 ).
Follow Up
Often domestic violence reoccurs and increases in frequency or intensity over time. Up to 75% of clients reporting domestic violence will continue to experience abuse. This can be frustrating for healthcare professionals, but it is important to remember that your role is to document the abuse, provide resources to clients, report when required, and not judge or verbalize opinions on what clients should do (2).
Appropriate follow up for healing wounds or injuries should be scheduled. Information about local domestic violence resources should be provided at each visit with clients. If a client does leave an abusive relationship, it is important to continue screening for violence as they may return to the relationship and are at an increased risk of entering new relationships that are also abusive (2).
Community Outreach
Healthcare professionals can have an impact on domestic violence in broader ways that direct client interactions as well. Advocacy on a community level can help increase awareness, shift harmful societal views on domestic violence, and create more robust community resources. Places where healthcare voices can help shift the narrative on domestic violence include (6):
- Parent Teacher Association (PTA) members
- Church members
- Community leadership positions
- Social clubs
- Political/voter groups
- Connecticut Coalition Against Domestic Violence (CCADV)
Nursing Education
RNs with a Connecticut license must apply for renewal every 6 years. They are not required to obtain CEUs specific to domestic or sexual violence for license renewal, though the topic is strongly recommended as these issues can impact clients across a variety of demographics and in many different healthcare settings. Required topics for license renewal include screening for PTSD, depression, and risk of suicide, and training for suicide prevention (7).
Connecticut APRNs must complete 50 hours of continuing education every 2 years and are required to complete at least 1 hour each on the topics of sexual assault and domestic violence. Having compassionate, knowledgeable, and competently prepared providers in delicate situations such as abuse, or violence can increase client safety and improve overall health outcomes (7).

Self Quiz
Ask yourself...
- What tools or processes does your current facility use to screen for abuse?
- How could your facility improve on those screening practices?
- If your facility does encounter someone who discloses abuse, what processes are in place for next steps of reporting and connecting with resources?
Case Studies
Kimari’s Case
Kimari is a Black, 22-year-old pregnant woman who presents to the OB clinic for a second trimester visit with complaints of abdominal pain. Kimari’s partner accompanies her to the visit today and the nurse notes that Kimari is unusually quiet and withdrawn compared to her previous visits. Her partner is answering most of the nurse’s questions for her. The nurse asks him to step into the waiting room so Kimari can change into a gown. Once he is gone, the nurse administers the HITS screening tool and opens a discussion with the client. Kimari reveals that her partner had been emotionally abusive in the past but never physically. However, since she has become pregnant, the abuse has worsened and has started to include forced sexual activity and physical violence. She admits her abdominal pain today is due to him shoving her down the stairs in the house the day before.
The nurse sits with Kimari and listens to her description of the events of the last few weeks. At this time, she wants to stay in the relationship as she does not have anywhere else to go and also has a two-year-old at home to think about. She is interested in individual counseling and develops a safety plan with the nurse which includes hotlines and local resources, as well as a plan to go to her sister’s house if tension seems to be rising again.
A physical exam reveals a healthy pregnancy with normally developing fetus and no complications from the fall down the stairs. The information from today’s visit is documented in her record and a follow-up appointment is scheduled for the following month.


Self Quiz
Ask yourself...
- What risk factors does this client have for being a victim of abuse?
- What potential complications can occur during pregnancy due to physical violence?
- What interventions did the nurse utilize appropriately when handling Kimari’s case?
- How do you feel about the outcome of this case? Do you have preconceived ideas about how this case should be handled that you would need to adjust in order to provide sensitive care like this nurse did?
Kevin’s Case
Kevin is a 28-year-old gay man presenting to the family practice clinic for an annual wellness visit. Kevin’s provider conducts a thorough physical assessment, orders labs, and administers screening tools for anxiety and depression. Kevin is found to be in good health but does score moderately high on his depression screening. The provider caring for him recommends individual counseling and offers an antidepressant which Kevin accepts. He is scheduled for a follow up in one month and the visit concludes.
Kevin returns home where he lives with an emotionally abusive husband. When Kevin reveals that he was given a prescription for an antidepressant, his husband ridicules him and calls him “crazy” and “weak.” They get into an argument and Kevin’s husband slaps him.
Later that evening, Kevin’s husband finds him unresponsive but still breathing in the bathroom with what appears to be an attempted overdose. He calls 911.


Self Quiz
Ask yourself...
- What risk factors does this client have for being a victim of abuse?
- What risk factors does this client have for suicidal thoughts or actions?
- How could this case have been handled differently?
- Without standard screening tools for domestic violence in LGBTQ relationships, how could Kevin’s provider have assessed for safety within his relationship?
Conclusion
Domestic violence, particularly physical and sexual abuse, is a problem with far-reaching consequences that affects people of all demographics. Identification of those most at risk, early intervention, and connection to resources, as well as prompt treatment of acute injuries and health implications are all important components in reducing the tragic impact of domestic violence. Healthcare professionals in all settings may encounter abuse situations and should be up to date on best practices for screening and management of these cases. Hopefully upon completion of this course, healthcare professionals will feel confident in their role in supporting victims.

Self Quiz
Ask yourself...
- Have you ever reported an abuse situation? If so, what was the process like? Did you find it effective or have concerns?
- What community involvement opportunities exist in your community that can have an impact on domestic violence resources?
HIV/AIDS
This course fulfills the continuing education requirement for the District of Columbia on HIV/AIDS.
Introduction and Objectives
An estimated 1.2 million Americans are living with HIV. As many as 1 in 7 of them do not even know they are infected. The others utilize the healthcare system in a variety of ways, from testing and treatment regimens to hospitalizations for symptoms and opportunistic infections. Healthcare professionals in nearly every setting have the potential to encounter patients with HIV as the disease can affect patients of any age or stage of life (4). Proper understanding of HIV is important in order to provide high–quality and holistic care to these patients.
Upon completion of this course, the learner will:
- Have an increased understanding of the history of HIV and how stigma around the disease developed and is being combated today.
- Demonstrate an understanding of how a person is infected with HIV and the various stages of the disease.
- Demonstrate understanding of transmission modalities and appropriate infection control measures.
- Have a basic knowledge of treatment approaches, common side effects, and barriers to proper treatment.
- Understand comorbidities and coinfections common with HIV.
- Understand ethical issues and confidentiality surrounding the care of HIV patients.
Epidemiology
In the early 1980s, a series of unusual and aggressive illnesses began popping up in clusters across the United States, affecting previously healthy men. Illnesses such as pneumocystis pneumonia, Kaposi‘s sarcoma, and severe wasting, all related to unexplained immunodeficiency, were suddenly rapidly increasing in prevalence, and the only common link seemed to be that it was occurring in gay men. By 1982, the term Acquired Immune Deficiency Syndrome (AIDS) was being used to describe a “moderately predictive…defect in cell–mediated immunity,“ but the details of disease trajectory and how men were contracting it were still foggy (2).
Over the next several years, cases continued to rise, and women and children began presenting with the disease, bringing scientists to the realization that it could be contracted through more ways than just homosexual sex. Amid the social panic, the retrovirus responsible was identified and named Human Immunodeficiency Virus, more reliable testing developed, and various other modes of transmission (like needle sharing, contaminated blood products, childbirth, and breastfeeding) were recognized. By 1989, less than a decade after the first cases were garnering attention, 142,000 cases were reported by 145 countries worldwide (2).
Over the next several decades, more and more information was discovered about HIV and AIDS, and scientists and legislators worked hard to understand and reduce transmission, increase quality and duration of life for those already infected, and fight the stigma and discrimination that had developed during the 1980s (2).
Today, approximately 1.2 million people in the United States are living with HIV, though 1 in 7 people don‘t know it. Rates of infection are not equal across demographic groups, and certain factors may increase a person‘s risk (10). Patient information to consider when determining someone‘s risk includes:
- Age: As of 2018, the age group with the highest incidence of new HIV diagnoses is 25-34 years or approximately 36% of new infections. Ages 13-24 are next, though the numbers in this age range are coming down in recent years. From there, the risk seems to decrease as people age, with the 55 years and older group accounting for only around 10% of new diagnoses each year (10).
- Race/Ethnicity: Currently, the highest rate of new infections is in African Americans, at approximately 45%. This is incredibly high when you consider that African Americans only make up 13% of the general population. This is followed by Hispanic/Latinos at 22% of new infections and people of multiple races at 19% (7).
- Gender: Men are disproportionately affected by HIV, accounting for five times the amount of new infections as females each year. This data refers to the sex of someone at birth. When looking at the transgender population, there is a nearly equal rate of new infections among those who have transitioned male-to-female and female-to-male. Together, transgender people account for 2% of new cases in 2018 (7).
- Sexual orientation: Gay and bisexual men remain the population most at risk of HIV, accounting for around 69% of all new infections in 2018 and 86% of all males diagnosed. Similar racial and ethnic disparities affecting all people with HIV still existed among gay and bisexual men (7).
- Location: Different areas of the country are affected at different rates for a variety of factors, including population density, racial distribution, and access to healthcare. The southern states are unmistakably more affected than other regions, with anywhere from 13-45 people per 100,000 having a diagnosis of HIV. California, Nevada, New York, and D.C. all having similar rates of infection as the southern states and are among the highest in the country. The Midwest and Pacific Northwest are next most affected, with 9-13 people per 100,000. The Northeast and Northwest have the lowest rates nationally at just up to 5 people per 100,000 (7).
While the effects of HIV and AIDS have resulted in a staggering 32 million deaths worldwide since the start of the epidemic, global and national numbers indicate that it peaked around 2005. Numbers of infections and deaths have been on a slow decline since then, mostly due to earlier and more accurate diagnosis, increased knowledge of how to prevent transmission, and effective and accessible treatments. An estimated 65% of Americans currently diagnosed with HIV are considered “virally suppressed,“ demonstrating that adherence to treatment guidelines means most infected people have virtually no risk of transmitting the virus to their partners and have a life expectancy nearly the same as non-infected people (6).
HIV/AIDS’s financial impact is also significant, with an estimated $380,000 spent throughout an individual‘s lifetime with the disease. In 2009, it was estimated that $16.6 billion was spent on HIV treatment in the U.S. alone. However, federal prevention programs do more than improve health outcomes and decrease the number of new infections; they also claim financial benefits and saved approximately $129 billion in the last two decades by averting new infections.
The Ryan White Program is notable and has been in place since 1990. It is a significant source of expanded coverage and funding for patients living with HIV who cannot afford health insurance or proper treatment. This safety net program is federally funded and named after a teenager who died from AIDS after receiving an HIV–contaminated blood transfusion. Ryan‘s story was also a turning point in the public perception of the disease, and the program helps fight the stigma surrounding HIV today (5).

Self-Quiz
Ask Yourself...
- Has the info about HIV/AIDs changed since you first learned it?
- Think about nurses who are from a different generation. How does their experience with this disease differ?
- How might your patients’ experiences or views of this illness be different from yours?
- Why is understanding the complicated history of this illness and its social stigma an important part of providing compassionate care?
- Is access to health insurance and quality healthcare more difficult for those with higher risk to obtain?
- What factors might make one area of the country more at risk than another?
Etiology and Pathogenesis
So just what is this virus that can cause so much devastation but took scientists years to understand? HIV is a type of retrovirus known as lentiviruses; these viruses have long incubation periods and lead to chronic and deadly infections in mammals. Studies indicate that the virus may have first infected humans hunting and eating the meat of infected chimpanzees in central Africa as early as the late 1800s. Once the virus jumped to humans, it spread slowly over many decades and across countries before picking up steam and attracting attention in the United States in the 1980s (7).
Once a host has been infected, the virus seeks out, attaches to, and enters CD4-T cells, immune cells largely responsible for attacking and clearing pathogens in the body. Once inside the cell, viral mRNA (or genetic code) directs the cell to become a factory of more HIV virions, which are then released through a process known as budding. Those virions travel through the body, enter other CD4-T cells, and produce more viruses in a slow but deadly cascade. As part of the body‘s defense against such pathogens, CD4-T cells are programmed for apoptosis (cell death) upon being taken over by a host. Others will experience cell death due to close proximity to infected cells. Still, others will be killed by other types of immune cells. While HIV ravages the body and continues to rise in viral load, the number of CD4-T cells will drop lower and lower until, eventually, the body‘s cell-mediated immunity is no longer viable. Without cell-mediated immunity, opportunistic infections and cancers can take over, and the infected person progresses from HIV infection to full–fledged AIDS (12).
Typically, the disease progresses in 3 stages.
- Stage 1 is acute HIV infection. The virus is reproducing rapidly, and affected individuals may experience flu–like symptoms, including fever, chills, headache, and fatigue. Not everyone experiences symptoms during Stage 1, but all are highly contagious during this period.
- Stage 2 is Chronic HIV infection; viral replication slows, and this stage can last for many years. A person in this stage is still contagious, but they may have no symptoms. Proper use of medication treatment may mean an infected person never moves past this stage.
- And finally, if the viral load continues to increase and the CD4-T cell count gets below 200 cells/mm, the illness transitions to Stage 3, AIDS. In this stage, even minor opportunistic pathogens can make a person very ill due to the lack of a properly functioning immune system. Symptoms and infections such as thrush, pneumonia, peripheral neuropathy, and Kaposi sarcoma are common. Stage 3 is very contagious and life expectancy is about 3 years if left untreated (7).

Self-Quiz
Ask Yourself...
- HIV is unique in that it primarily targets CD4-T cells inside the host. How does this directly contribute to symptoms and affect the trajectory of the disease?
- How does the body‘s natural defenses against such an invasion affect disease trajectory?
- Which stage do you think a person is most likely to be unknowingly transmitting the virus to others?
- Which stage do you think someone not undergoing routine testing is most likely to find out about their illness?
- What about someone who gets routine or yearly testing?
Transmissibility
Perhaps the most elusive part of this virus for many years was how it spreads. We now know that HIV is spread only through certain bodily fluids. An accurate understanding of HIV transmission is important for healthcare professionals to provide proper education to their patients, reduce misconceptions and stigmas, and prevent transmission and protect themselves and other patients (11).
Bodily fluids that can transmit the virus include:
- Blood
- Semen and pre-seminal fluid
- Rectal fluid
- Vaginal fluid
- Breastmilk
- Fluids that may contain blood such as amniotic fluid, pleural fluid, pericardial fluid, and cerebrospinal fluid
If one of these fluids comes in contact with a mucous membrane such as the mouth, vagina, rectum, etc., or damaged tissue such as open wounds, or is directly injected into the bloodstream, then transmission of HIV is possible (11).
Scenarios where transmission is possible include:
- Vaginal or anal sex with someone who has HIV (condoms and appropriate treatment with antivirals reduce this risk)
- Sharing needles or syringes with someone who has HIV
- Mother-to-child transmission during pregnancy, delivery, or breastfeeding (appropriate treatment during pregnancy, c-section delivery, and alternative feeding methods reduce this risk)
- Receiving a transfusion of infected blood or blood products (this is very rare now because of screening processes for blood donations)
- Oral sex with someone who has HIV (though this is very rare)
- A healthcare worker receiving a needle stick with a dirty sharp (risk of transmission is very low in this scenario)
HIV cannot be transmitted via:
- Saliva
- Sputum
- Feces
- Urine
- Vomit
- Sweat
- Mucous
- Kissing
- Sharing food or drink

Self-Quiz
Ask Yourself...
- What sort of PPE do you need to wear when helping an HIV+ patient use a bedpan?
- What about assisting with a procedure where blood splatter may occur?
- What factors about childbirth make this event particularly risky for transmission?
- What interventions might help reduce that risk?
- Think about the population you work with. What methods of transmission are they most at risk from?
- How might this differ among different populations or work settings?
Reducing Transmission
Patient education about risk and protection against HIV, testing, and what to do if exposed should be standard practice for healthcare professionals in nearly all healthcare settings. Primary care should include risk screenings and patient education routinely to ideally help prevent infections from even occurring or catch those that have occurred early on in the disease process (11).
Strategies include:
- Identifying those most at risk, incredibly gay or bisexual men, minority patients, and those using drugs by injection
- Ensure patients are aware of and have access to protective measures such as condoms and clean needle exchange programs
- Provide routine screening blood work for anyone with risk factors or desiring testing
- Providing access to PrEP medications where indicated (discussed further below)
- Staying up to date on current CDC recommendations and HIV developments
- Maintaining a nonjudgmental demeanor when discussing HIV with patients to welcome open discussion (11)
For patients with a repeated or frequent high risk of HIV exposure, such as those with an HIV+ partner or those routinely using IV drugs, pre-exposure prophylaxis (PrEP) may be a good choice to reduce the risk of them contracting the virus. When used correctly, PrEP is 99% effective at preventing infection from high–risk sexual activity and 74% effective at preventing infection from injectable drug use. Depending on the type of exposure risk (anal sex, vaginal sex, needle sharing, etc.), PrEP needs to be taken anywhere from 7-21 days before it reaches its maximum effectiveness. Most insurances, including Medicaid programs, cover PrEP at least in part. There are also federal and state assistance programs available to make PrEP available to as many people who need it as possible. Some side effects are commonly reported, primarily G.I. symptoms, headaches, and fatigue (11).
For those who have a confirmed diagnosis of HIV/AIDS, the focus should be promoting interventions that will prevent further transmission. One of the biggest determinants for transmission is the infected person’s viral load. Individuals being treated for HIV can have their viral load measured to ensure viral replication is being controlled as intended. A viral load lower than 20-40 copies per milliliter of blood is considered undetectable, meaning the virus is not transmissible to others. Even for those not receiving treatment, there are methods to reduce transmission (11).
Important considerations for transmission in patients who are HIV+ include:
- Referral for treatment and educating on the importance of treatment compliance in order to keep the viral load as low as possible
- Education on the importance (and possible legal consequences) of proper disclosure to any sexual or needle–sharing partners who may be at risk of exposure
- Encouraging and assisting with access to condom use and clean needle programs
- Providing information to HIV+ pregnant women about how interventions such as proper treatment during pregnancy, c-section delivery, and formula feeding can keep the risk of transmission as low as 1% (11)
Methods of infection control for healthcare professionals include:
- Universal precautions when handling any bodily fluids
- Eyewear when at risk for fluid splashing
- Careful and proper handling of sharps
- Facilities having a standard plan in place for potential exposures
If exposure or needlestick do occur for healthcare professionals, the patient would ideally submit to testing for HIV to determine if the staff member is even at any risk. If the HIV status of the patient is unknown or confirmed to be positive, four weeks of post–exposure prophylaxis (PEP) may be advised within 72 hours of exposure (11).
PEP is meant for emergency use only, such as for healthcare workers with a potential exposure or patients with an exposure that is not expected to become routine. PEP is not meant to replace the use of PrEP or other preventative measures. In order to be effective, PEP must be started within 72 hours of the potential exposure and must be taken for a 28–day course of treatment. When used correctly, it is highly effective and typically well–tolerated, with nausea being the most common side effect. For healthcare professionals taking it due to workplace exposure, your facility should cover the cost. For patients in the general population, insurance will usually cover it, or there are assistance programs available to make it affordable for everyone (11).

Self-Quiz
Ask Yourself...
- What screening questions or protocols are in place where you work to detect those most at risk of contracting HIV?
- In what ways, if any, could your facility improve its screening protocol to identify more at–risk patients?
- What information should be given to a pregnant woman with HIV who is asking about different infant feeding methods?
- Do you know what your facility‘s blood–borne pathogen protocol is?
- What steps are in place to help you if you get a dirty needle stick?
- Think about the population you work with. Are there any patients that might benefit from routine use of PrEP?
- What sorts of scenarios might indicate the need for the use of PEP?
Treatment Considerations
When HIV is appropriately treated, advancement from HIV to AIDS can be significantly reduced, and quality and longevity of life maximized. In 2018, the CDC estimated around 65% of all U.S. citizens living with HIV were virally suppressed, and 85% of those receiving regular HIV–related care were considered virally suppressed. However, an estimated13% of all HIV cases do not know they are infected. Appropriate medical care and keeping viral loads undetectable is one of the single most effective methods of preventing transmission (4, 6).
For those receiving treatment, a multifaceted and individualized approach can reduce a person‘s viral load, reduce the risk of transmission, reduce the likelihood of developing AIDS, and preserve the immune system. Regardless of how early someone receives treatment, there is no cure for HIV, and an infected person will be infected for life. All individuals diagnosed with HIV (even asymptomatic people, infants, and children) should receive antiretroviral therapy or ART as quickly as possible after a diagnosis of HIV is made. There are seven different classes of antiretroviral medications that disrupt various points in the viral replication process. Most treatment regimens use several of these medications combined with the most effective results; some combination pills are also available for administration ease. Medication regimens are chosen based on a patient‘s health status and history, tolerance or sensitivity to medication, and stage and severity of HIV infection. Patient condition and viral load should be monitored closely, and changes or inadequate response to treatment may indicate the need for a change in medication regimen at any time (1).
The classes and available medications for ART include (1):
Nucleoside reverse transcriptase inhibitors (NRTIs): these inhibit the transcription of viral RNA to DNA
- Abacavir (Ziagen)
- Emtricitabine (Emtriva)
- Lamivudine (Epivir)
- Tenofovir disoproxil fumerate (Viread)
- Zidovudine (Retrovir)
Non-nucleoside reverse transcriptase inhibitors (NNRTIs): these inhibit the transcription of viral RNA to DNA
- Doravirine (Pifeltro)
- Efavirenz (Sustiva)
- Etravirine (Intelence)
- Nevirapine (Viramune, Viramune XR)
- Rilpivirine (Edurant)
Protease inhibitors: inhibit the final step of viral budding
- Atazanavir (Reyataz)
- Darunavir (Prezista)
- Fosamprenavir (Lexiva)
- Ritonavir (Norvir)
- Saquinavir (Invirase)
- Tipranavir (Apitvus)
Fusion inhibitors: prevent the virus from fusing with CD4-T cells
- Enfuvirtide (Fuzeon)
Integrase strand transfer inhibitors (INSTIs): these stop HIV from inserting its DNA into cells
- Dolutegravir (Tivicay)
- Raltegravir (Isentress, Isentress HD)
Chemokine receptor antagonists (CCR5 antagonists): prevent the virus from binding to CD4-T cells
- Maraviroc (Selzentry)
Entry inhibitors: prevent the virus from binding to and entering cells
- Ibalizumab-uiyk (Trogarzo) (1)
These types of medication do not come without side effects or complications. Most side effects fit into a few major groups and may be bothersome but are not life–threatening or serious. More Serious or worrisome adverse effects may occur, and a patient‘s current health status, as well as medical history or existing conditions, should be carefully considered (3). The common categories of adverse medication reactions include:
- Gastrointestinal: Nausea, vomiting, diarrhea, decrease in appetite, reflux, constipation, damage to liver or pancreas
- CNS: Headache, dizziness, sleep disturbance, neuropathy, memory problems, hearing impairment or tinnitus
- Hematological: Anemia, hematuria, hyperbilirubinemia
- Psychological: Mood swings, anxiety, depression, confusion, nightmares/vivid dreams
- Dermatological: Rash, face discoloration, pruritus
- Musculoskeletal: Body aches, abnormal fat distribution
- GU: Menstrual cycle disruption
Due to the need to take medications for the rest of one‘s life and the long list of potentially bothersome side effects, medication adherence is a common issue in treating HIV appropriately (3).
There are several scenarios that increase the likelihood of poor compliance, including:
- Asymptomatic patients, since side effects of medications, maybe unpleasant and they are in a latent phase of disease without symptoms
- Young patients, including children or teenagers who may not understand the necessity of taking daily medications and face a lifetime of treatment
- Patients with substance abuse or mental health issues, as they may be in and out of cognitive and psychiatric crises
- Poor literacy or education level, as these patients may be easily confused by a complicated medication regimen or simply not understand the importance of lifelong therapy, especially if they are feeling well
- Social stigma, which may lead people to try and hide medications or not want their diagnosis to be discovered (3)

Self-Quiz
Ask Yourself...
- Why might it be important to take several medications that interrupt the viral replication process at different points?
- Think about the population you work with. What potential barriers to proper treatment are there?
- Think about the potential side effects of medications for HIV. How difficult do you think it would be to keep taking a medication like that, even if you understood why you needed it?
- Do you think it would be difficult to take daily medication if you had no symptoms and felt well?
Care Considerations for Comorbidities and Coinfections
Caring for patients with HIV or AIDS is a complicated task requiring compassion, patience, and understanding the many potential complications and ways that various body systems are affected. Many infections and comorbidities commonly present alongside HIV/AIDS, particularly as patients age, immune function declines, and effects of long-term medication use develop. The social stigma and psychological impact of such a devastating disease must also be considered to provide holistic care to these patients (9). Common coinfections/comorbidities include:
Tuberculosis
T.B. is a highly contagious airborne illness that affects the respiratory system. It is an opportunistic infection that frequently affects people with weakened immune systems, like those with AIDS. The bacteria can live in the body without causing symptoms in a latent phase for long periods. As the immune system in HIV weakens, a latent T.B. infection may become active, causing symptoms and deteriorating health. Most common symptoms include cough, hemoptysis, fever, fatigue, night sweats, or poor appetite, and weight loss. Seriously immunocompromised people may even experience disseminated T.B. where the infection affects more than the lungs and can even lead to septic shock and death. Annual PPD tests for T.B., or chest X-ray for anyone with a history of positive PPD, should be conducted on patients with HIV (9).
Hepatitis
About 1 in 10 people affected by HIV will also have viral hepatitis, as the diseases are spread in much the same way, particularly needle sharing and sexually and vertically (mother to fetus). Hepatitis infections progress quickly in immunocompromised patients and can greatly reduce liver function, which complicates the use of ART medications and can result in poor clearance from the body. All new HIV diagnoses should be screened for Hepatitis A, B, and C, and Hep A and B vaccines should be encouraged in unvaccinated patients (9).
STIs
Because HIV can be acquired via high–risk sexual activity, infection with other STIs is common. Sometimes, other STIs may even increase the risk of contracting HIV as they result in open sores or breaks in the skin where HIV can more easily enter. Bacterial STIs can typically be cured with antibiotics, but other viral STIs like Herpes and HPV do not have a cure. Routine screening for patients engaging in high–risk sexual activity or those already infected with HIV should be a typical part of care (9).
Cardiovascular Disease
Studies show that patients with HIV also increase inflammation of the arteries and plaque formations throughout the body due to a complicated effect on macrophages. Some of the ART medications also increase the risk of heart attack or stroke. Concurrent infection with hepatitis can increase cholesterol, which further deteriorates cardiovascular health and increases MI or stroke risk. Patients with HIV should be screened for family history and current heart health, and their plan of care should incorporate ways to reduce risks, including a focus on diet and activity level (9)l.
Osteoporosis
Bone density has been shown to decrease faster than normal in patients receiving ART medications, and it is recommended that patients over age 50 have annual bone density scans to estimate fracture risk. Treatment for osteoporosis should be added to the plan of care as needed (9).
Cancer
As science has become better equipped to detect and treat HIV and concomitant infection, cancer has remained a leading cause of death for HIV patients and is a considerable risk for those living with the disease. Most commonly, cancers of the head and neck, anus, lungs, liver, and lymph system occur. Smoking cessation, regular pap tests for women, HPV vaccines, and routine screenings like colonoscopies after a certain age should be heavily counseled in HIV patients to reduce their risk further. Earlier and consistent ART has been shown to reduce the risk of developing cancer (9).
Mental Health Issues
When considering the long–term and eventually fatal nature of this disease, along with the social stigma and complicated and expensive treatment regimens, it is no surprise that mental health disorders such as anxiety and depression are common for patients with HIV. Upwards of 22% of patients with HIV will suffer from depression, likely higher when you account for substance abuse disorders. In addition to assessing and treating body systems affected by the virus, it is important to screen patients for psychiatric disorders and be aware of the negative effects the diagnosis may be having on mental health. Medication treatment and therapy should be included in care where appropriate (9).

Self-Quiz
Ask Yourself...
- Think of the common health concerns in the population you work with, particularly when age and family history are factored in. How would a diagnosis of HIV affect those risks and health considerations?
- Consider what it would feel like to have a diagnosis of HIV and then be given a diagnosis of cancer or T.B. How do you think you would feel?
- How do you think your mental health would be affected?
- What other potential screenings or lifestyle changes would be a good idea for someone with HIV?
Ethical Concerns
Maintaining confidentiality under HIPAA laws is essential in the care of patients with any diagnosis, but the social stigma attached to HIV infection–in addition to the frequency and intensity of medical care needed and the responsibility to notify partners and prevent further spread–makes confidentiality particularly challenging with many ethical considerations to navigate.
The first issue with maintaining confidentiality occurs with testing itself. HIV is considered a reportable disease. Any positive results must be reported to a local health department and then on to the CDC for local and national statistics and to initiate follow–up with the positive person and provide education on the next steps. Patient names and identifying information are included with the positive result when reported to local and state health departments but is removed before it is reported to the CDC. There is an option for anonymous testing where patients are given a special identification number, and their names and identifying information are not included. These are often self–administered tests and are not available everywhere (8).
Testing for HIV requires informed consent, meaning healthcare professionals must discuss the risks, benefits, and potential consequences of testing for HIV and cannot test someone for HIV without their consent. Minors’ ability to get testing and treatment for HIV without a parent or guardian’s consent varies from state to state (8).
Once someone tests positive for HIV, the issue of disclosure presents itself. Patients need to inform their past and future sexual partners or anyone they share needles with of their HIV status. Health departments will help contact tracing and notifying past partners and help those potentially exposed with their testing and prophylactic treatment options. In some states, it is considered a criminal offense to withhold a positive infection status when a person may be exposing others. However, the responsibility to disclose falls on the patient, and healthcare professionals may not notify potential contacts without a patient‘s consent. Infected persons are not required to inform friends, family, employers, or others who are not at risk of contracting the disease (8).
Employers who provide health insurance for their employees may be given information about the costs and benefits of disclosing an HIV diagnosis indirectly. So while insurance companies cannot directly tell an employer about an HIV diagnosis, employees should be aware the information may come out indirectly. However, all workers with HIV are protected under the Americans with Disabilities Act. As long as they can complete their job duties, employers may not discriminate against them (8).
Finally, and of particular importance for healthcare professionals, is navigating the stigma or negative stereotypes that often accompany an HIV diagnosis. There are some societal misconceptions that HIV infections only occur as a result of immoral or taboo behavior or that those infected should be treated differently or avoided. People with HIV may have internalized these harmful stereotypes and feel a sense of shame around their diagnosis. It is important for healthcare professionals to understand that these stereotypes are untrue and harmful, but to provide non–judgemental and compassion that preserves dignity and views the patient as more than their diagnosis.

Self-Quiz
Ask Yourself...
- Why do you think there are laws in place requiring people to disclose their HIV status to potential sexual partners?
- Can you think of any other illnesses where your disclosure is as important as with this disease? Why or why not?
- Why is reporting data about new HIV infections to the CDC important?
- Think about your own internalized thoughts on HIV. Do you have any stereotypes or other negative views that might subconsciously affect your ability to provide non-judgmental care?
Conclusion
Professionals in any healthcare setting may encounter patients with HIV or AIDS. A basic understanding of this disease’s many considerations is fundamental to ensure that quality and compassionate care is being provided. Understanding the disease, treatments, and the unique struggles of these patients can significantly impact their healthcare experiences and promote quality of life.
Controlled Substances
Introduction
Pain is complex and subjective. The experience of pain can significantly impact an individual's quality of life. According to the National Institute of Health (NIH) (40), pain is the most common complaint in a primary care office, with 20% of all patients reporting pain. Chronic pain is the leading cause of disability, and effective pain management is crucial to health and well-being, particularly when it improves functional ability. Effective pain treatment starts with a comprehensive, empathic assessment and a desire to listen and understand. Nurse Practitioners are well-positioned to fill a vital role in providing comprehensive and empathic patient care, including pain management (23).
While the incidence of chronic pain has remained a significant problem, how clinicians manage pain has significantly changed in the last decade, primarily due to the opioid epidemic. This education aims to discuss pain and the assessment of pain, federal guidelines for prescribing, the opioid epidemic, addiction and diversion, and recommendations for managing pain.
Definition of Pain
Understanding the definition of pain, differentiating between various types of pain, and recognizing the descriptors patients use to communicate their pain experiences are essential for Nurse practitioners involved in pain management. By understanding the medical definition of pain and how individuals may communicate it, nurse practitioners can differentiate varying types of pain to target assessment.
According to the International Association for the Study of Pain (27), pain is "an unpleasant sensory and emotional experience associated with actual or potential tissue damage or terms of described such in damage." The IASP, in July 2020, expanded its definition of pain to include context further.
Their expansion is summarized below:
- Pain is a personal experience influenced by biological, psychological, and social factors.
- Pain cannot be inferred solely from activity in sensory neurons.
- Individuals learn the concept of pain through their life experiences.
- A person's report of an experience in pain should be respected.
- Pain usually serves an adaptive role but may adversely affect function and social and psychological well-being.
- The inability to communicate does not negate the possibility of the experience of pain.


Self Quiz
Ask yourself...
- Analyze how changes to the definition of pain may affect your practice.
- Discuss how you manage appointment times, knowing that 20% of your scheduled patients may seek pain treatment.
- How does the approach to pain management change in the presence of a person with a disability?
Types of Pain
Pain originates from different mechanisms, causes, and areas of the body. As a nurse practitioner, understanding the type of pain a patient is experiencing is essential for several reasons (23).
- Determining an accurate diagnosis. This kind of pain can provide valuable clues to the underlying cause or condition.
- Creating a treatment plan. Different types of pain respond better to specific treatments or interventions.
- Developing patient education. A nurse practitioner can provide targeted education to patients about their condition, why they may experience the pain as they do, its causes, and treatment options. Improving the patient's knowledge and control over their condition improves outcomes.
Acute Pain
Acute pain is typically short-lived and is a protective response to an injury or illness. Patients are usually able to identify the cause. This type of pain resolves as the underlying condition improves or heals (12).
Chronic Pain
Chronic pain is diagnosed when it continues beyond the expected healing time. Pain is defined as chronic when it persists for longer than three months. It may result from an underlying disease or injury or develop without a clear cause. Chronic pain often significantly impacts a person's physical and emotional well-being, requiring long-term management strategies. The prolonged experience of chronic pain usually indicates a central nervous system component of pain that may require additional treatment. Patients with centralized pain often experience allodynia or hyperalgesia (12).
Allodynia is pain evoked by a stimulus that usually does not cause pain, such as a light touch. Hyperalgesia is the effect of a heightened pain response to a stimulus that usually evokes pain (12).
Nociceptive Pain
Nociceptive pain arises from activating peripheral nociceptors, specialized nerve endings that respond to noxious stimuli. This type of pain is typically associated with tissue damage or inflammation and is further classified into somatic and visceral pain subtypes.
Somatic pain is most common and occurs in muscles, skin, or bones; patients may describe it as sharp, aching, stiffness, or throbbing.
Visceral pain occurs in the internal organs, such as indigestion or bowel spasms. It is more vague than somatic pain; patients may describe it as deep, gnawing, twisting, or dull (12).
Neuropathic pain
Neuropathic pain is a lesion or disease of the somatosensory nervous system. Examples include trigeminal neuralgia, painful polyneuropathy, postherpetic neuralgia, and central poststroke pain (10).
Neuropathic pain may be ongoing, intermittent, or spontaneous pain. Patients often describe neuropathic pain as burning, prickling, or squeezing quality. Neuropathic pain is a common chronic pain. Patients commonly describe allodynia and hyperalgesia as part of their chronic pain experience (10).
Affective pain
Affective descriptors reflect the emotional aspects of pain and include terms like distressing, unbearable, depressing, or frightening. These descriptors provide insights into the emotional impact of pain on an individual's well-being (12).

Self Quiz
Ask yourself...
- How can nurse practitioners effectively elicit patient descriptors to accurately assess the type of pain the patient is experiencing?
- Expand on how pain descriptors can guide interventions even if the cause is not yet determined.
- What strategies ensure patients feel comfortable describing their pain, particularly regarding subjective elements such as quality and location?
Case Study
Mary Adams is a licensed practical nurse who has just relocated to town. Mary will be the utilization review nurse at a local long-term care facility. Mary was diagnosed with Postherpetic Neuralgia last year, and she is happy that her new job will have her mostly doing desk work and not providing direct patient care as she had been before the relocation. Mary was having difficulty at work at her previous employer due to pain. She called into work several times, and before leaving, Mary's supervisor had counseled her because of her absences.
Mary wants to establish primary care immediately because she needs ongoing pain treatment. She is hopeful that, with her new job and pain under control, she will be able to continue a successful career in nursing. When Mary called the primary care office, she specifically requested a nurse practitioner as her primary care provider because she believes that nurse practitioners tend to spend more time with their patients.
Assessment
The assessment effectively determines the type of treatment needed, the options for treatment, and whether the patient may be at risk for opioid dependence. Since we know that chronic pain can lead to disability and pain has a high potential to negatively affect the patient's ability to work or otherwise, be productive, perform self-care, and potentially impact family or caregivers, it is imperative to approach the assessment with curiosity and empathy. This approach will ensure a thorough review of pain and research on pain management options. Compassion and support alone can improve patient outcomes related to pain management (23).
Record Review
Regardless of familiarity with the patient, reviewing the patient's treatment records is essential, as the ability to recall details is unreliable. Reviewing the records can help identify subtle changes in pain description and site, the patient's story around pain, failed modalities, side effects, and the need for education, all impacting further treatment (23).
Research beforehand the patient's current prescription and whether or not the patient has achieved the maximum dosage of the medication. Analysis of the patient's past prescription could reveal a documented failed therapy even though the patient did not receive the maximum dose (23).
A review of documented allergens may indicate an allergy to pain medication. Discuss with the patient the specific response to the drug to determine if it is a true allergy, such as hives or anaphylaxis, or if the response may have been a side effect, such as nausea and vomiting.
Research whether the patient tried any non-medication modalities for pain, such as physical therapy (PT), occupational therapy (OT), or Cognitive Behavioral Therapy (CBT). Note any non-medication modalities documented as failed therapies. The presence of any failed therapies should prompt further discussion with the patient, family, or caregiver about the experience. The incompletion of therapy should not be considered failed therapy. Explore further if the patient abandoned appointments.
Case Study
You review the schedule for the week, and there are three new patient appointments. One is Mary Adams. The interdisciplinary team requested and received Mary's treatment records from her previous primary care provider. You make 15 minutes available to review Mary's records and the questionnaire Mary filled out for her upcoming appointment. You see that Mary has been diagnosed with Postherpetic Neuralgia and note her current treatment regimen, which she stated was ineffective. You write down questions you will want to ask Mary. You do not see evidence of non-medication modalities or allergies to pain medication.

Self Quiz
Ask yourself...
- What potential risks or complications can arise from neglecting to conduct a thorough chart review before initiating a pain management assessment?
- In your experience, what evidence supports reviewing known patient records?
- What is an alternative to reviewing past treatment if records are not available?
Pain Assessment
To physically assess pain, several acronyms help explore all the aspects of the patient's experience. Acronyms commonly used to assess pain are SOCRATES, OLDCARTS, and COLDERAS. These pain assessment acronyms are also helpful in determining treatment since they include a character and duration of pain assessment (23).
| O-Onset | S-Site | C-Character |
| L-Location | O-Onset | O-Onset |
| D-Duration | C-Character | L-Location |
| C-Character | R-Radiate | D-Duration |
| A-Alleviating | A-Associated symptoms | E-Exacerbating symptoms |
| R-Radiating, relieving | T-Time/Duration | R-Relieving, radiating |
| T-Temporal patterns (frequency) | E-Exacerbating | A-Associated symptoms |
| S-Symptoms | S-Severity | S-Severity of illness |
Inquire where the patient is feeling pain. The patient may have multiple areas and types of pain. Each type and location must be explored and assessed. Unless the pain is from a localized injury, a body diagram map, as seen below, is helpful to document, inform, and communicate locations and types of pain. In cases of Fibromyalgia, rheumatoid arthritis, or other centralized or widespread pain, it is vital to inquire about radiating pain. The patient with chronic pain could be experiencing acute pain or a new pain site, such as osteoarthritis, that may need further evaluation and treatment (23).
Inquire with the patient how long their pain has been present and any associated or known causative factors. Pain experienced longer than three months defines chronic versus acute pain. Chronic pain means that the pain is centralized or a function of the Central Nervous system, which should guide treatment decisions.
To help guide treatment, ask the patient to describe their pain. The description helps identify what type of pain the patient is experiencing: Allodynia and hyperalgesia indicate centralized pain; sharp, shooting pain could indicate neuropathic pain. Have the patient rate their pain. There are various tools, as shown below, for pain rating depending on the patient's ability to communicate. Not using the pain rating number alone is imperative. Ask the patient to compare the severity of pain to a previous experience. For example, a 1/10 may be experienced as a bumped knee or bruise, whereas a 10/10 is experienced on the level of a kidney stone or childbirth (23).
Besides the 0-10 rating scale and depending on the patient's needs, several pain rating scales are appropriate. They are listed below.
The 0-5 and Faces scales may be used for all adult patients and are especially effective for patients experiencing confusion.
The Defense and Veterans Pain Rating Scale (DVPRS) is a five-item tool that assesses the impact of pain on sleep, mood, stress, and activity levels (20).
For patients unable to self-report pain, such as those intubated in the ICU or late-stage neurological diseases, the FLACC scale is practical. The FLACC scale was initially created to assess pain in infants. Note: The patient need not cry to be rated 10/10.
| Behavior | 0 | 1 | 2 |
| Face | No particular expression or smile | Occasional grimace or frown, withdrawn, disinterested | Frequent or constant quivering chin, clenched jaw |
| Legs | Normal position or relaxed | Uneasy, restless, tense | Kicking or legs drawn |
| Activity | Lying quietly, in a normal position, or relaxed | Squirming, shifting back and forth, tense | Arched, rigid, or jerking |
| Cry | No cry wake or asleep | Moans or whimpers: occasional complaints | Crying steadily, screams, sobs, frequent complaints |
| Consolability | Content, relaxed | Distractable, reassured by touching, hugging, or being talked to | Difficult to console or comfort |
(21).
Assess contributors to pain such as insomnia, stress, exercise, diet, and any comorbid conditions. Limited access to care, socioeconomic status, and local culture also contribute to the patient's experience of pain (23). Most patients have limited opportunity to discuss these issues, and though challenging to bring up, it is compassionate and supportive care. A referral to social work or another agency may be helpful if you cannot explore it fully.
Assess for substance abuse disorders, especially among male, younger, less educated, or unemployed adults. Substance abuse disorders increase the likelihood of misuse disorder and include alcohol, tobacco, cannabis, cocaine, and heroin (29).
Inquire as to what changes in function the pain has caused. One question to ask is, "Were it not for pain, what would you be doing?" As seen below, a Pain, Enjoyment, and General Activity (PEG) three-question scale, which focuses on function and quality of life, may help determine the severity of pain and the effect of treatment over time.
| What number best describes your pain on average in the past week? 0-10 |
| What number best describes how, in the past week, pain has interfered with your enjoyment of life? 0-10 |
| What number determines how, in the past week, pain has interfered with your general activity? 0-10 |
(21).
Assess family history, mental health disorders, chronic pain, or substance abuse disorders. Each familial aspect puts patients at higher risk for developing chronic pain (23).
Evaluate for mental health disorders the patient may be experiencing, particularly anxiety and depression. The Patient Health Questionnaire (PHQ4) is a four-question tool for assessing depression and anxiety.
In some cases, functional MRI or imaging studies effectively determine the cause of pain and the treatment. If further assessment is needed to diagnose and treat pain, consult Neurology, Orthopedics, Palliative care, and pain specialists (23).
Case Study
You used OLDCARTS to evaluate Mary's pain and completed a body diagram. Mary is experiencing allodynia in her back and shoulders, described as burning and tingling. It is exacerbated when she lifts, such as moving patients at the long-term care facility and, more recently, boxes from her move to the new house. Mary has also been experiencing anxiety due to fear of losing her job, the move, and her new role. She has moved closer to her family to help care for her children since she often experiences fatigue. Mary has experienced a tumultuous divorce in the last five years and feels she is still undergoing some trauma.
You saw in the chart that Mary had tried Gabapentin 300 mg BID for her pain and inquired what happened. Mary explained that her pain improved from 8/10 to 7/10 and had no side effects. Her previous care provider discontinued the medication and documented it as a failed therapy. You reviewed the minimum and maximum dosages of Gabapentin and know Mary can take up to 1800mg/day.
During the assessment, Mary also described stiffness and aching in her left knee. She gets a sharp pain when she walks more than 500 steps, and her knee is throbbing by the end of the day. Mary rated the pain a 10/10, but when she compared 10/10 to childbirth, Mary said her pain was closer to 6/10. Her moderate knee pain has reduced Mary's ability to exercise. She used to like to take walks. Mary stated she has had knee pain for six months and has been taking Ibuprofen 3 – 4 times daily.
Since Mary's pain is moderate, you evaluate your options of drugs for moderate to severe pain.


Self Quiz
Ask yourself...
- How do you assess and evaluate a patient's pain level?
- What are the different types of pain and their management strategies?
- How do you determine the appropriate dosage of pain medications for a patient?
- How do you assess the effectiveness of pain medications in your patients?
- How do you adjust medication dosages for elderly patients with pain or addiction?
- How do you address the unique challenges in pain management for pediatric patients?
- What is the role of non-pharmacological interventions in pain management?
- How do you incorporate non-pharmacological interventions into your treatment plans?
Opioid Classifications and Drug Schedules
A comprehensive understanding of drug schedules and opioid classifications is essential for nurse practitioners to ensure patient safety, prevent drug misuse, and adhere to legal and regulatory requirements. Nurse practitioners with a comprehensive understanding of drug schedules and opioid classifications can effectively communicate with colleagues, ensuring accurate medication reconciliation and facilitating interdisciplinary care. Nurse practitioners’ knowledge in facilitating discussions with pharmacists regarding opioid dosing, potential interactions, and patient education is essential (49).
Drug scheduling became mandated under the Controlled Substance Act. The Drug Enforcement Agency (DEA) Schedule of Controlled Drugs and the criteria and common drugs are listed below.
|
Schedule |
Criteria | Examples |
|
I |
No medical use; high addiction potential |
Heroin, marijuana, PCP |
|
II |
Medical use; high addiction potential |
Morphine, oxycodone, Methadone, Fentanyl, amphetamines |
|
III |
Medical use; high addiction potential |
Hydrocodone, codeine, anabolic steroids |
|
IV |
Medical use, low abuse potential |
Benzodiazepines, meprobamate, butorphanol, pentazocine, propoxyphene |
| V | Medical use; low abuse potential |
Buprex, Phenergan with codeine |
(Pain Physician, 2008)
Listed below are drugs classified by their schedule and mechanism of action. "Agonist" indicates a drug that binds to the opioid receptor, causing pain relief and also euphoria. An agonist-antagonist indicates the drug binds to some opioid receptors but blocks others. Mixed antagonist-agonist drugs control pain but have a lower potential for abuse and dependence than agonists (7).
| Schedule I | Schedule II | Schedule III | Schedule IV | Schedule V | |
| Opioid agonists |
BenzomorphineDihydromor-phone, Ketobemidine, Levomoramide, Morphine-methylsulfate, Nicocodeine, Nicomorphine, Racemoramide |
Codeine, Fentanyl, Sublimaze, Hydrocodone, Hydromorphone, Dilaudid, Meperidine, Demerol, Methadone, Morphine, Oxycodone, Endocet, Oxycontin, Percocet, Oxymorphone, Numorphan |
Buprenorphine Buprenex, Subutex, Codeine compounds, Tylenol #3, Hydrocodone compounds, Lortab, Lorcet, Tussionex, Vicodin |
Propoxyphene, Darvon, Darvocet | Opium, Donnagel, Kapectolin |
| Mixed Agonist -Antagonist | BuprenorphineNaloxone, Suboxone |
Pentazocine, Naloxone, Talwin-Nx |
|||
| Stimulants | N-methylampheta-mine 3, 4-methylenedioxy amphetamine, MDMA, Ecstacy | Amphetamine, Adderal, Cocaine, Dextroamphetamine, Dexedrine, Methamphetamine, Desoxyn, Methylphenidate, Concerta, Metadate, Ritalin, Phenmetrazine, Fastin, Preludin | Benapheta-mine, Didrex, Pemolin, Cylert, Phendimetra-zine, Plegine | Diethylpropion, Tenuate, Fenfluramine, Phentermine Fastin | 1-dioxy-ephedrine-Vicks Inhaler |
| Hallucinogen-gens, other | Lysergic Acid Diamine LSD, marijuana, Mescaline, Peyote, Phencyclidine PCP, Psilocybin, Tetrahydro-cannabinol | Dronabinol, Marinol | |||
| Sedative Hypnotics |
Methylqualine, Quaalude, Gamma-hydroxy butyrate, GHB
|
Amobarbitol, Amytal, Glutethamide, Doriden, Pentobarbital, Nembutal, Secobarbital, Seconal |
Butibarbital. Butisol, Butilbital, Florecet, Florinal, Methylprylon, Noludar |
Alprazolam, Xanax, Chlordiazepoxide, Librium, Chloral betaine, Chloral hydrate, Noctec, Chlorazepam, Clonazepam, Klonopin, Clorazopate, Tranxene, Diazepam, Valium, Estazolam, Prosom, Ethchlorvynol, Placidyl, Ethinamate, Flurazepam, Dalmane, Halazepam, Paxipam, Lorazepam, Ativan, Mazindol, Sanorex, Mephobarbital, Mebaral, Meprobamate, Equanil, Methohexital, Brevital Sodium, Methyl-phenobarbital, Midazolam, Versed, Oxazepam, Serax, Paraldehyde, Paral, Phenobarbital, Luminal, Prazepam, Centrax, Temazepam, Restoril, Triazolam, Halcion, Sonata, Zolpidem, Ambien |
Diphenoxylate preparations, Lomotil |
(41).

Self Quiz
Ask yourself...
- What are the potential risks and benefits of using opioids for pain management?
- How can nurse practitioners effectively monitor patients on long-term opioid therapy?
- What are the potential risks and benefits of using long-acting opioids for chronic pain?
- How do you monitor patients on long-acting opioids for safety and efficacy?
Commonly Prescribed Opioids, Indications for Use, and Typical Side Effects
Opioid medications are widely used for managing moderate to severe pain. Referencing NIDA (2023), this section aims to give healthcare professionals an overview of the indications and typical side effects of commonly prescribed Schedule II opioid medications, including hydrocodone, oxycodone, morphine, Fentanyl, and hydromorphone.
Opioids are derived and manufactured in several ways. Naturally occurring opioids come directly from the opium poppy plant. Synthetic opioids are manufactured by chemically synthesizing compounds that mimic the effects of a natural opioid. Semi-synthetic is a mix of naturally occurring and man-made (35).
Understanding the variations in how an opioid is derived and manufactured is crucial in deciding the type of opioid prescribed, as potency and analgesic effects differ. Synthetic opioids are often more potent than naturally occurring opioids. Synthetic opioids have a longer half-life and slower elimination, affecting the duration of action and timing for dose adjustments. They are also associated with a higher risk of abuse and addiction (38).
Hydrocodone
Mechanism of Action and Metabolism
Hydrocodone is a Schedule II medication. It is an opioid agonist and works as an analgesic by activating mu and kappa opioid receptors located in the central nervous system and the enteric plexus of the bowel. Agonist stimulation of the opioid receptors inhibits nociceptive neurotransmitters' release and reduces neuronal excitability (17).
- Produces analgesia.
- Suppresses the cough reflex at the medulla.
- Causes respiratory depression at higher doses.
Hydrocodone is indicated for treating severe pain after nonopioid therapy has failed. It is also indicated as an antitussive for nonproductive cough in adults over 18.
Available Forms
Hydrocodone immediate release (IR) reaches maximum serum concentrations in one hour with a half-life of 4 hours. Extended-release (ER) Hydrocodone reaches peak concentration at 14-16 hours and a half-life of 7 to 9 hours. Hydrocodone is metabolized to an inactive metabolite in the liver by cytochrome P450 enzymes CYP2D6 and CYP3A4. Hydrocodone is converted to hydromorphone and is excreted renally. Plasma concentrations of hydromorphone are correlated with analgesic effects rather than hydrocodone.
Hydrocodone is formulated for oral administration into tablets, capsules, and oral solutions. Capsules and tablets should never be crushed, chewed, or dissolved. These actions convert the extended-release dose into immediate release, resulting in uncontrolled and rapid release of opioids and possible overdose.
Dosing and Monitoring
Hydrocodone IR is combined with acetaminophen or ibuprofen. The dosage range is 2.5mg to 10mg every 4 to 6 hours. If formulated with acetaminophen, the dosage is limited to 4gm/day.
Hydrocodone ER is available as tablets and capsules. Depending on the product, the dose of hydrocodone ER formulations in opioid-naïve patients is 10 to 20 mg every 12 to 24 hours.
Nurse practitioners should ensure patients discontinue all other opioids when starting the extended-release formula.
Side Effects and Contraindications
Because mu and kappa opioid receptors are in the central nervous system and enteric plexus of the bowel, the most common side effects of hydrocodone are constipation and nausea (>10%).
Other adverse effects of hydrocodone include:
- Respiratory: severe respiratory depression, shortness of breath
- Cardiovascular: hypotension, bradycardia, peripheral edema
- Neurologic: Headache, chills, anxiety, sedation, insomnia, dizziness, drowsiness, fatigue
- Dermatologic: Pruritus, diaphoresis, rash
- Gastrointestinal: Vomiting, dyspepsia, gastroenteritis, abdominal pain
- Genitourinary: Urinary tract infection, urinary retention
- Otic: Tinnitus, sensorineural hearing loss
- Endocrine: Secondary adrenal insufficiency (17)
Hydrocodone, being an agonist, must not be taken with other central nervous system depressants as sedation and respiratory depression can result. In formulations combined with acetaminophen, hydrocodone can increase the international normalized ratio (INR) and cause bleeding. Medications that induce or inhibit cytochrome enzymes can lead to wide variations in absorption.
The most common drug interactions are listed below:
- Alcohol
- Benzodiazepines
- Barbiturates
- other opioids
- rifampin
- phenytoin
- carbamazepine
- cimetidine,
- fluoxetine
- ritonavir
- erythromycin
- diltiazem
- ketoconazole
- verapamil
- Phenytoin
- John’s Wort
- Glucocorticoids
Considerations
Use with caution in the following:
- Patients with Hepatic Impairment: Initiate 50% of the usual dose
- Patients with Renal Impairment: Initiate 50% of the usual dose
- Pregnancy: While not contraindicated, the FDA issued a black-boxed warning since opioids cross the placenta, and prolonged use during pregnancy may cause neonatal opioid withdrawal syndrome (NOWS).
- Breastfeeding: Infants are susceptible to low dosages of opioids. Non-opioid analgesics are preferred.
Pharmacogenomic: Genetic variants in hydrocodone metabolism include ultra-rapid, extensive, and poor metabolizer phenotypes. After administration of hydrocodone, hydromorphone levels in rapid metabolizers are significantly higher than in poor metabolizers.
Oxycodone
Mechanism of Action and Metabolism
Oxycodone has been in use since 1917 and is derived from Thebaine. It is a semi-synthetic opioid analgesic that works by binding to mu-opioid receptors in the central nervous system. It primarily acts as an agonist, producing analgesic effects by inhibiting the transmission of pain signals (Altman, Clark, Huddart, & Klein, 2018).
Oxycodone is primarily metabolized in the liver by CYP3A4/5. It is metabolized in the liver to noroxycodone and oxymorphone. The metabolite oxymorphone also has an analgesic effect and does not inhibit CYP3A4/5. Because of this metabolite, oxycodone is more potent than morphine, with fewer side effects and less drug interactions. Approximately 72% of oxycodone is excreted in urine (Altman, Clark, Huddart, & Klein, 2018).
Available Forms
Oxycodone can be administered orally, rectally, intravenously, and as an epidural. For this sake, we will focus on immediate-release and extended-release oral formulations.
- Immediate-release (IR) tablets
- IR capsules
- IR oral solutions
- Extended-release (ER) tablets
Dosing and Monitoring
The dosing of oxycodone should be individualized based on the patient's pain severity, previous opioid exposure, and response. Initial dosages for opioid naïve patients range from 5-15 mg for immediate-release formulations, while extended-release formulations are usually initiated at 10-20 mg. Dosage adjustments may be necessary based on the patient's response, but caution should be exercised. IR and ER formulations reach a steady state at 24 hours and titrating before 24 hours may lead to overdose.
Regular monitoring is essential to assess the patient's response to treatment, including pain relief, side effects, and signs of opioid misuse or addiction. Monitoring should include periodic reassessment of pain intensity, functional status, and adverse effects (Altman, Clark, Huddart, & Klein, 2018).
Side Effects and Contraindications
Common side effects of oxycodone include:
- constipation
- nausea
- sedation
- dizziness
- respiratory depression
- respiratory arrest
- hypotension
- fatal overdose
Oxycodone is contraindicated in patients with known hypersensitivity to opioids, severe respiratory depression, paralytic ileus, or acute or severe bronchial asthma. It should be used cautiously in patients with a history of substance abuse, respiratory conditions, liver or kidney impairment, and those taking other medications that may interact with opioids, such as alcohol (4).
It is also contraindicated with the following medications and classes:
- Antifungal agents
- Antibiotics
- Rifampin
- Carbamazepine
- Fluoxetine
- Paroxetine
Considerations
- Nurse practitioners should consider the variations in the mechanism of action for the following:
- Metabolism differs between males and females: females have been shown to have less concentration of oxymorphone and more CYP3A4/5 metabolites.
- Infants have reduced clearance of oxycodone, increasing side effects.
- Pediatrics have 20-40% increased clearance over adults.
- Reduced clearance with age increases the half-life of oxycodone.
- Pregnant women have a greater clearance and reduced half-life.
- Impairment of the liver reduces clearance.
- Cancer patients with cachexia have increased exposure to oxycodone and its metabolite.
- Maternal and neonate concentrations are similar, indicating placenta crossing (4)
Morphine

Mechanism of Action and Metabolism
Morphine is a naturally occurring opioid alkaloid extracted from the opium poppy. It was isolated in 1805 and is the opioid against which all others are compared. Morphine binds to mu-opioid receptors in the brain and spinal cord, inhibiting the transmission of pain signals and producing analgesia. It is a first-line choice of opioid for moderate to severe acute, postoperative, and cancer-related pain (8).
Morphine undergoes first-pass metabolism in the liver and gut. It is well absorbed and distributed throughout the body. Its main metabolites are morphine-3-glucuronide and morphine-6-glucuronide. Its mean plasma elimination half-life after intravenous administration is about 2 hours. Approximately 90% of morphine is excreted in the urine within 24 hours (8).
Available Forms
Morphine is available in various forms, including.
- immediate-release tablets
- extended release tablets
- oral IR solutions
- injectable solutions
- transdermal patches
Dosing and Monitoring
Morphine is hydrophilic and, as such, has a slow onset time. The advantage of this is that it is unlikely to cause acute respiratory depression even when injected. However, because of the slow onset time, there is more likelihood of morphine overdose due to the ability to “stack” doses in patients experiencing severe pain (Bistas, Lopez-Ojeda, & Ramos-Matos, 2023).
The dosing of morphine depends on the patient's pain severity, previous opioid exposure, and other factors. It is usually initiated at a low dose and titrated upwards as needed. Monitoring pain relief, adverse effects, and signs of opioid toxicity is crucial. Reevaluate benefits and harms with patients within 1 to 4 weeks of starting opioid therapy or of dose escalation. General recommendations for initiating morphine (Bistas, Lopez-Ojeda, & Ramos-Matos, 2023).
Prescribe IR opioids instead of ER opioids.
Prescribe the lowest effective dosage, below 50 Morphine Milligram Equivalents (MME) /day.
Side Effects and Contraindications
Because morphine binds to opioid receptors in the brain and spinal cord, is metabolized in the liver and gut, and has a slow onset, the following side effects are common:
- Constipation
- Nausea
- Vomiting
- Sedation
- Dizziness
- Respiratory depression
- Pruritis
- Sweating
- Dysphoria/Euphoria
- Dry mouth
- Anorexia
- Spasms of urinary and biliary tract
Contraindications of morphine are:
- Known hypersensitivity or allergy to morphine.
- Bronchial asthma or upper airway obstruction
- Respiratory depression in the absence of resuscitative equipment
- Paralytic ileus
- Risk of choking in patients with dysphagia, including infants, children, and the elderly (8)
Concurrent use with other sedating medications: Amitriptyline, diazepam, haloperidol, chlorpromazine
Morphine interacts with the following medications:
- Ciprofloxacin
- Metoclopramide
- Ritonavir
Considerations for Nurse Practitioners
Assess for medical conditions that may pose serious and life-threatening risks with opioid use, such as the following:
- Sleep-disordered breathing, such as sleep apnea.
- Pregnancy
- Renal or hepatic insufficiency
- Age >= 65
- Certain mental health conditions
- Substance use disorder
- Previous nonfatal overdose
Fentanyl
Mechanism of Action and Metabolism
Fentanyl is a synthetic opioid more potent than morphine and was approved in 1968. Fentanyl is an agonist that works by binding to the mu-opioid receptors in the central nervous system. This binding inhibits the transmission of pain signals, resulting in analgesia. Fentanyl is often used for severe pain management, particularly in the perioperative and palliative care settings, or for severe pain in patients with Hepatic failure (8).
It is a mu-selective opioid agonist. However, it can activate other opioid receptors in the body, such as the delta and kappa receptors, producing analgesia. It also activates the Dopamine center of the brain, stimulating relaxation and exhilaration, which is responsible for its high potential for addiction (8).
Indications for fentanyl are as follows:
- Preoperative analgesia
- Anesthesia adjunct
- Regional anesthesia adjunct
- General anesthesia
- Postoperative pain control
- Moderate to severe acute pain (off-label)
Available Forms
- Fentanyl is available in various forms, including:
- transdermal patches
- injectable solutions
- lozenges
- nasal sprays
- oral tablets (8)
Dosing and Monitoring
Fentanyl is metabolized via the CYP3A4 enzyme in the liver. It has a half-life of 3 to 7 hours, and 75% of Fentanyl is excreted in the urine and 9% in feces.
The dosing of fentanyl depends on the route of administration and the patient's needs. For example, transdermal patches are typically applied every 72 hours, while injectable solutions are titrated to achieve the desired analgesic effect. Monitoring should include assessing pain levels, respiratory rate, blood pressure, and sedation scores (8).
Fentanyl is most dosed as follows:
- Post-operative pain control
- 50 to 100 mcg IV/IM every 1 to 2 hours as needed; alternately 0.5 to 1.5 mcg/kg/hour IV as needed. Consider lower dosing in patients 65 and older.
PCA (patient-controlled analgesia): 10 to 20 mcg IV every 6 to 20 minutes as needed; start at the lowest effective dose for the shortest effective duration - refer to institutional protocols (8).
Moderate to severe acute pain (off-label) 1 to 2 mcg/kg/dose intranasally each hour as needed; the maximum dose is 100 mcg. Use the lowest effective dose for the shortest effective duration (8).
Side Effects and Contraindications
Common side effects of fentanyl include:
- respiratory depression
- sedation
- constipation
- nausea
- vomiting
- euphoria
- confusion
- respiratory depression/arrest
- visual disturbances
- dyskinesia
- hallucinations
- delirium
- narcotic ileus
- muscle rigidity
- addiction
- loss of consciousness
- hypotension
- coma
- death (8).
The use of fentanyl is contraindicated in patients in the following situations:
- After operative interventions in the biliary tract, these may slow hepatic elimination of the drug.
- With respiratory depression or obstructive airway diseases (i.e., asthma, COPD, obstructive sleep apnea, obesity hyperventilation, also known as Pickwickian syndrome)
- With liver failure
- With known intolerance to fentanyl or other morphine-like drugs, including codeine or any components in the formulation.
- With known hypersensitivity (i.e., anaphylaxis) or any common drug delivery excipients (i.e., sodium chloride, sodium hydroxide) (8).
Considerations for Nurse Practitioners
Nurse practitioners prescribing fentanyl should thoroughly assess the patient's pain, medical history, and potential risk factors for opioid misuse. They should also educate patients about the proper use, storage, and disposal of fentanyl. It should be used cautiously in patients with respiratory disorders, liver or kidney impairment, or a history of substance abuse. Fentanyl is contraindicated in patients with known hypersensitivity to opioids and those without exposure to opioids.
Alcohol and other drugs, legal or illegal, can exacerbate fentanyl's side effects, creating multi-layered clinical scenarios that can be complex to manage. These substances, taken together, generate undesirable conditions that complicate the patient's prognosis (8).
Hydromorphone
Mechanism of Action and Metabolism
Hydromorphone is a semi-synthetic opioid derived from morphine. It binds to the mu-opioid receptors in the central nervous system. It primarily exerts its analgesic effects by inhibiting the release of neurotransmitters involved in pain transmission, thereby reducing pain perception. Hydromorphone also exerts its effects centrally at the medulla level, leading to respiratory depression and cough suppression (1).
Hydromorphone is indicated for:
- moderate to severe acute pain
- severe chronic pain
- refractory cough suppression (off-label) (1)
Available Forms
Hydromorphone is available in various forms, depending on the patient’s needs and severity of pain.
- immediate-release tablet
- extended release tablets
- oral liquid
- injectable solution
- rectal suppositories
Dosing and Monitoring
The immediate-release oral formulations of hydromorphone have an onset of action within 15 to 30 minutes. Peak levels are typically between 30 and 60 minutes with a half-life of 2 to 3 hours. Hydromorphone is primarily excreted through the urine.
The dosing of hydromorphone should be individualized based on the patient's pain intensity, initiated at the lowest effective dose, and adjusted gradually as needed. Close monitoring of pain relief, adverse effects, and signs of opioid toxicity is essential. Patients should be assessed regularly to ensure they receive adequate pain control without experiencing excessive sedation or respiratory depression.
The following are standard dosages that should only be administered when other opioid and non-opioid options fail.
- Immediate-release oral solutions dosage: 1 mg/1 mLoral tablets are available in 2 mg, 4 mg, and 8 mg.
- Extended-release oral tablets are available in dosages of 8 mg, 12 mg, 16 mg, and 32 mg.
- Injection solutions are available in concentrations of 1 mg/mL, 2 mg/mL, 4 mg/mL, and 10 mg/mL.
- Intravenous solutions are available in strengths of 2 mg/1 mL, 2500 mg/250 mL, ten mg/1 mL, and 500 mg/50 mL.
- Suppositories are formulated at a strength of 3 mg (1).
Side Effects and Contraindications
Hydromorphone has potential adverse effects on several organ systems, including the integumentary, gastrointestinal, neurologic, cardiovascular, endocrine, and respiratory.
Common side effects of hydromorphone include:
- Constipation
- Nausea
- Vomiting
- Dizziness
- Sedation
- respiratory depression
- pruritus
- headache
- Somnolence
- Severe adverse effects of hydromorphone include:
- Hypotension
- Syncope
- adrenal insufficiency
- coma
- raised intracranial pressure.
- seizure
- suicidal thoughts
- apnea
- respiratory depression or arrest
- drug dependence or withdrawal
- neonatal drug withdrawal syndrome
- Hydromorphone is contraindicated in patients with:
- known allergies to the drug, sulfites, or other components of the formulation.
- known hypersensitivity to opioids.
- severe respiratory depression
- paralytic ileus
- acute or severe bronchial asthma (1).
Caution should be exercised in patients with:
- respiratory insufficiency
- head injuries
- increased intracranial pressure.
- liver or kidney impairment.
Considerations for Nurse Practitioners
As nurse practitioners, it is crucial to assess the patient's pain intensity and overall health status before initiating Hydromorphone. Start with the lowest effective dose and titrate carefully for optimal pain control. Regular monitoring for adverse effects, signs of opioid toxicity, and therapeutic response is essential. Educate patients about the potential side effects, proper dosing, and the importance of not exceeding prescribed doses. Additionally, nurse practitioners should be familiar with local regulations and guidelines regarding opioid prescribing and follow appropriate documentation and monitoring practices.
Additional Considerations
In terminal cancer patients, clinicians should not restrain opioid therapy even if signs of respiratory depression become apparent.
Hydromorphone requires careful administration in cases of concurrent psychiatric illness.
Specific Patient Considerations:
- Hepatic impairment and Renal Impairment: Initiate hydromorphone treatment at one-fourth to one-half of the standard starting dosage, depending on the degree of impairment.
- Pregnancy considerations: Hydromorphone can traverse the placental barrier and induce NOWS.
- Breastfeeding considerations: Nonopioid analgesic agents are preferable for breastfeeding women.
- Older patients: hydromorphone is categorized as a potentially inappropriate medication for older adults (1).
Tramadol

Mechanism of Action and Metabolism
Tramadol is a Schedule IV opioid medication with a higher potential for dependency and misuse than non-opioid medications. It binds to opioid receptors in the central nervous system, inhibiting the reuptake of norepinephrine and serotonin. It also has weak mu-opioid receptor agonist activity.
The liver metabolizes tramadol mediated by the cytochrome P450 pathways (particularly CYP2D6) and is mainly excreted through the kidneys.
Tramadol is used for moderate to severe pain.
Available Forms of Tramadol include:
- Immediate-release-typically used for acute pain management.
- Extended-release-used for chronic pain.
Dosing and Monitoring
Tramadol has an oral bioavailability of 68% after a single dose and 90–100% after multiple doses and reaches peak concentrations within 2 hours. Approximately 75% of an oral dose is absorbed, and the half-life of tramadol is 9 hours (18).
Tramadol dosing should be individualized based on the patient's pain severity and response.
The initial dose for adults is usually 50-100 mg orally every 4-6 hours for pain relief. The maximum daily dose is 400 mg for immediate-release formulations and 300 mg for extended-release formulations (18).
It is essential to monitor the patient's pain intensity, response to treatment, and any adverse effects. Regular reassessment and adjustment of the dosage may be necessary.
Side Effects and Contraindications
Tramadol is responsible for severe intoxications leading to consciousness disorder (30%), seizures (15%), agitation (10%), and respiratory depression (5%). The reactions to Tramadol suggest that the decision to prescribe should be carefully considered.
Common Side Effects of Tramadol Include:
- Nausea
- Vomiting
- Dizziness
- Constipation
- Sedation
- Headache
- CNS depression
- Seizure
- Agitation
- Tachycardia
- Hypertension
- reduced appetite
- pruritus and rash
- gastric irritation
Serious side effects include:
- respiratory depression
- serotonin syndrome
- seizures
Contraindications
Tramadol is contraindicated in patients with:
- history of hypersensitivity to opioids
- acute intoxication with alcohol
- opioids, or other psychoactive substances
- Patients who have recently received monoamine oxidase inhibitors (MAOIs)
Additionally, the following can be observed in tramadol intoxication:
- miosis
- respiratory depression
- decreased level of consciousness
- hypertension
- tremor
- irritability
- increased deep tendon reflexes
Poisoning leads to:
- multiple organ failure
- coma
- cardiopulmonary arrest
- death
Considerations for Nurse Practitioners
Tramadol has been increasingly misused with intentional overdoses or intoxications. Suicide attempts were the most common cause of intoxication (52–80%), followed by abuse (18–31%), and unintentional intoxication (1–11%). Chronic tramadol or opioid abuse was reported in 20% of tramadol poisoning cases. Fatal tramadol intoxications are uncommon except when ingested concurrent with depressants, most commonly benzodiazepines and alcohol (18).
Tramadol poisoning can affect multiple organ systems:
- gastrointestinal
- central nervous system: seizure, CNS depression, low-grade coma, anxiety, and over time anoxic brain damage
- Cardiovascular system: palpitation, mild hypertension to life-threatening complications such as cardiopulmonary arrest
- respiratory system
- renal system: renal failure with higher doses of tramadol intoxication
- musculoskeletal system: rhabdomyolysis
- endocrine system: hypoglycemia, serotonin syndrome (18)
Cannabis
Mechanism of Action and Metabolism
Cannabis is classified as a Schedule I status. It contains various cannabinoids, with delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) being the most studied. THC primarily acts on cannabinoid receptors in the brain, producing psychoactive effects, while CBD has more diverse effects on the nervous system. These cannabinoids interact with the endocannabinoid system, modulating neurotransmitter release and influencing various physiological processes (32).
Similar to opioids, cannabinoids are synthesized and released in the body by synapses that act on the cannabinoid receptors present in presynaptic endings (32). They perform the following actions related to analgesia:
- Decrease the release of neurotransmitters.
- Activate descending inhibitory pain pathways.
- Reduce postsynaptic sensitivity and alleviate neural inflammation.
- Modulate CB1 receptors within central nociception processing areas and the spinal cord, resulting in analgesic effects.
- Attenuate inflammation by activating CB2 receptors (32).
- Emerging research shows cannabis is indicated for:
- Migraines
- chronic pain
- back pain
- arthritic pain
- pain associated with cancer and surgery.
- neuropathic pain
- diabetic neuropathic pain when administered early in the disease progression.
- sickle cell disease
- cancer
- inflammatory bowel disease (32)
Available Forms
Cannabis refers to products sourced from the Cannabis sativa plant. There are differences between cannabis, cannabinoids, and cannabidiol (CBD). Cannabinoids are extracted from the cannabis plants. Cannabinoid-based treatments, such as dronabinol and CBD, are typically approved medical interventions for specific indications. THC (9-tetrahydrocannabinol) is the psychoactive component of the cannabis plant. CBD is a non-psychoactive component (32).
Cannabis can be consumed in different forms, each with a different onset and duration. Patients may have individual preferences, including:
- smoking/vaporizing dried flowers.
- consuming edibles
- tinctures or oils
- applying topicals (32)
Dosing and Monitoring
Inhaling marijuana via the lungs by smoking or vaping causes maximum plasma concentration within minutes. Psychiatric effects begin within seconds to a few minutes after inhalation and peak after 15 to 30 minutes. The effect diminishes throughout 2 to 3 hours (32).
Oral ingestion of marijuana causes psychiatric effects that typically occur between 30 and 90 minutes and reach maximum effect after 2 to 3 hours. Ingested marijuana effects last about 4 to 12 hours (32).
Dosing cannabis is challenging due to variations in potency and individual responses. Start with low doses and titrate slowly to achieve the desired effect while minimizing side effects. Regular monitoring is crucial, including assessing symptom relief, adverse effects, and potential drug interactions. Encourage patients to keep a diary to track their cannabis use and its effects (32).
Side Effects and Contraindications
Cannabis can exacerbate mental health conditions such as anxiety and psychosis. Common side effects of cannabis include (32):
- Dizziness
- dry mouth
- increased heart rate
- impaired memory
- psychoactive effects
Contraindications include:
- Pregnancy
- Breastfeeding
- heart disease
- respiratory conditions
- history of substance abuse
- mental health disorders

Self Quiz
Ask yourself...
- How do you address patients' misconceptions about pain medications?
- What are the mechanisms of action for commonly prescribed pain medications?
- How do these mechanisms of action contribute to pain relief?
- What are the potential side effects and risks associated with commonly prescribed pain medications?
- How do you educate patients about the risks and benefits of pain medications?
- How do you manage patients who require high-dose opioids for pain management?
- Is medical cannabis legal in your State? If yes, are you familiar with the prescribing guidelines?
- Do you have any personal biases against the use of medical cannabis? Why or why not?
Case Study
Mary is agreeable to trying an increased dose of Gabapentin. Mary would also like to see a counselor to discuss her past and get help with her anxiety. You made an appointment for Mary to see a Licensed Clinical Social Worker in your clinic.
You read the side effects and warnings for Gabapentin, and it is unsafe to use Gabapentin and Tramadol together since they are both depressants. You order a non-steroidal drug for Mary's somatic knee pain and make a consult for imaging studies on her left knee. You also make a referral to Orthopedics.
You educated Mary about the side effects of Gabapentin and scheduled a follow-up appointment. The day after Mary began her treatment with the increased Gabapentin, you called Mary to follow up on its effect. Mary still has pain, but she is not having any untoward side effects. Gabapentin may not work immediately so you will schedule a follow-up call in 3 days.


Self Quiz
Ask yourself...
- In this case study, Mary has insurance. How might your practice be different were Mary not insured?
- In your experience, what are the possible reasons for Mary's knee pain not being a part of her previous treatment record?
- Consider how your assessment of Mary's needs differs from the above-mentioned case study.
- Explain the rationale for decisions made by the nurse practitioner in the case study mentioned above and if your decisions would differ.
Opioid Use, the Opioid Epidemic, and Statistics
The use and misuse of opioids has become a pressing public health concern, leading to a global epidemic. The history of opioid use, the opioid epidemic, and associated statistics provide essential context for healthcare professionals in addressing this public health crisis. More importantly, it is estimated that 1 in 4 patients receiving prescription opioids in primary care settings will misuse them. In addition, 50% of opioid prescriptions are written by primary care providers, including nurse practitioners (22). Understanding the factors contributing to the epidemic and the magnitude of its impact is crucial for effective prevention, intervention, and treatment strategies.
History of Opioid Use
Opioids have a long history of medicinal use, dating back to ancient civilizations. They have been a drug of choice for pain relief for thousands of years. The introduction of synthetic opioids in the 19th century, such as morphine and later heroin, revolutionized pain management. However, their potential for addiction and misuse soon became apparent (16).
The Opioid Epidemic
The opioid epidemic refers to the surge in opioid misuse, addiction, and overdose deaths. The epidemic gained momentum in the late 1990s with increased prescribing of opioids for chronic pain (43).
No doubt, increased prescribing put opioids in the hands of consumers, but increased prescribing resulted from a multifactorial influence. One of the main influences was aggressive marketing by pharmaceutical companies, which has been well publicized. However, due to the long history of underprescribing pain medications for fear of misuse and addiction, the medical community was primed to expand its opioid prescribing practices (31).
A historical event that increased comfort with prescribing opioids, in the writer's opinion, was the introduction of the Medicare Hospice Benefit in 1986. Medical directors must be contracted or employed by hospices, and these medical directors had or soon gained pain management expertise. To further promote hospice and effective pain management, the hospice medical directors, with newly acquired skills, provided education throughout medical communities about pain management and specifically to decrease the fear of using opioids. Pharmacies and attending physicians grew accustomed to giving opioids for home use. Hospice care is for terminally ill patients, defined as a life expectancy of 6 months or less. Still, the reality is that hospice discharges 12 to 40% of patients for ineligibility and other reasons.
A more prominent factor in increasing opioid prescribing was the 1996 American Pain Society's introduction of pain as "the 5th Vital sign." Soon after, The Joint Commission promoted pain as "the 5th Vital Sign" and began compliance surveys in healthcare organizations requiring pain assessment details to be as prominent as blood pressure and heart rate. The Joint Commission cited a quote from 1968 by a nurse from the University of California Los Angeles, Margo McCaffrey, who defined pain as "…Whatever the experiencing person says it is, existing whenever s/he says it does." The Joint Commission accreditation programs pursued pain management as part of the accreditation process throughout its healthcare accreditation programs, including hospice accreditation by 1989 per TJC Timeline (48).
The National Institute of Health published an article about the Joint Commission's role in the opioid epidemic, particularly regarding the definition of pain, "This definition emphasizes that pain is a subjective experience with no objective measures. It also stresses that the patient, not the clinician, is the authority on the pain and that their self-report is the most reliable indicator of pain. This set the tone for clinicians: Patients are always to be trusted to report pain accurately” (45).
Statistics on the Opioid Epidemic
In the United States alone, over 500,000 people died from opioid overdoses between 1999 and 2017. The number of opioid-related overdose deaths continues to increase, with synthetic opioids, mainly illicitly manufactured Fentanyl, playing a significant role in recent years (46). Fentanyl-laced drugs, such as marijuana, are increasingly sold knowing and unknowingly to introduce medications with a high addiction rate, thus creating new consumers. This practice can potentially increase deaths due to the imprecise nature of manufacturing (16).
Opioid-related hospitalizations have also risen substantially. In 2014, there were approximately 1.27 million hospitalizations related to opioids in the United States. These hospitalizations not only place a burden on healthcare systems but also reflect the severe consequences of opioid misuse (3).


Self Quiz
Ask yourself...
- Have you experienced changes to your practice because of the opioid epidemic? If so, what are the changes?
- What is your opinion on the validity of Margo McCaffrey's definition of pain?
- What factors influence your willingness or unwillingness to prescribe opioids?
Federal Regulations on Opioid Prescribing
The history of substance use disorder prevention that promotes opioid recovery and treatment for patients and communities can be traced back to the early 20th century. However, the current approach to addressing opioid addiction and promoting healing has evolved significantly in recent times (36).
In the early 1900s, health professionals treated opioid addiction with punitive measures, including incarceration and moralistic approaches. The focus was on punishing individuals rather than providing effective treatment. This approach persisted for several decades until the mid-20th century when the medical community started recognizing addiction as a medical condition rather than a moral failing (36).
The Controlled Substances Act (CSA), introduced in 1970, was a response to increasing drug abuse and illicit drug trafficking in the United States. The CSA is a federal law regulating the manufacture, possession, distribution, and use of certain substances, including drugs and medications, that can potentially cause abuse and dependence. Its primary purpose is to combat drug abuse, reduce drug-related crimes, and protect public health and safety. The Drug Enforcement Agency (DEA) plays a crucial role in enforcing the CSA by monitoring and controlling controlled substance production, distribution, and use (31).
In the 1990s, the significant increase in opioid prescribing, leading to a surge in opioid addiction and overdose deaths, prompted a shift in focus toward prevention. Efforts were made to educate healthcare providers about the risks of overprescribing opioids and to implement prescription drug monitoring programs to track and prevent abuse (36).
The Comprehensive Addiction and Recovery Act (CARA) was signed into law in 2016 to expand access to treatment and recovery services for opioid addiction. This legislation allocated funding for prevention, treatment, recovery, and support services while promoting evidence-based practices and programs (36).
The Centers for Disease Control and Prevention (CDC) published guidelines in 2016 for prescribing opioids for chronic pain, which was updated in 2022. These guidelines emphasize the importance of non-opioid alternatives, using the lowest effective dose for the shortest duration, and assessing the benefits and risks of continued opioid therapy (13).
Furthermore, the Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT) was signed into law in 2018, providing additional resources to address the opioid crisis. This legislation expanded access to medication-assisted treatment (MAT), increased the availability of naloxone, a medication used to reverse opioid overdose, and enhanced support for recovery housing (36).
In recent years, there has been a growing recognition of the importance of a comprehensive approach to opioid addiction, including harm reduction strategies, increased access to naloxone, and the integration of mental health services. Communities and organizations have been working together to address the underlying issues contributing to addiction, such as poverty, trauma, and social determinants of health (50).
Overall, the history of substance use disorder prevention that promotes opioid recovery and treatment has evolved from a punitive approach to a more compassionate and evidence-based model. Efforts are now focused on prevention, early intervention, and expanding access to comprehensive treatment and support services for individuals and communities affected by opioid addiction (36).
The most current federal regulations on opioid prescribing for healthcare providers are the amendments to the CSA in 2018, which added new rules to limit the quantity and duration of opioid prescriptions for acute pain to seven days. In 2022, the CDC updated recommendations to the Clinical Practice Guidelines for Prescribing Opioids for Pain.
The 2022 CDC guidelines are summarized below (13):
- Non-opioid therapies should be considered the first-line treatment for chronic pain.
- Establish clear treatment goals with patients, including realistic pain management and functional improvement expectations.
- Conduct a thorough risk assessment for potential harms before initiating opioid therapy.
- When opioids are used, start with the lowest effective dose and consider immediate-release opioids instead of extended-release or long-acting opioids.
- Prescribe the lowest effective dose for the shortest duration possible, typically three days or less and rarely exceeding seven days.
- Reassess benefits and risks within one day after prescribing opioids, including checking the prescription drug monitoring database.
- Avoid prescribing opioids and benzodiazepines concurrently whenever possible due to the increased risk of overdose and death.
- Offer naloxone to patients at increased risk of opioid overdose, including those with a history of overdose, substance use disorder, or concurrent benzodiazepine use.
- When opioids are no longer needed, taper the dose gradually to minimize withdrawal symptoms.
- Arrange an evidence-based treatment for patients with opioid use disorder, including medication-assisted treatment (Naltrexone, Buprenorphine, or Methadone).

Self Quiz
Ask yourself...
- What are the guidelines general for prescribing opioids for acute pain?
- How do these guidelines differ for chronic pain management?
- Discuss how federal regulations impact the practice of nurse practitioners in terms of opioid prescribing.
- Describe the potential benefits and challenges nurse practitioners face when adhering to federal regulations on opioid prescribing.
- How can nurse practitioners navigate and stay updated with evolving federal regulations surrounding opioid prescribing to ensure safe and effective care?
- How do you ensure appropriate documentation when prescribing controlled substances?
Safe Prescribing and Prescription Monitoring Program
Prescription Drug Monitoring Programs (PDMP) are state-run electronic databases that track.
the prescribing and dispensing of controlled substances. PDMPs are designed to improve patients.
care and safety by giving clinicians access to patients' prescription histories, allowing them to make informed decisions when prescribing controlled substances. PDMPs help identify patients at risk of substance misuse or prescription drug overdose. They also enable clinicians to identify potential drug interactions and prevent opioid diversion (14).
PDMPs collect and store data from pharmacies and prescribers in a centralized database. Clinicians can access this database to review a patient's prescription history, including the types of medications prescribed, the prescribers involved, and the dispensing pharmacies (14).
In many states, PDMP use is mandated by law, and nurse practitioners may be required to register and use the system. It is essential to understand state-specific laws and regulations regarding PDMP use.
PDMPs have some limitations, such as incomplete data or delays in reporting. The CDC emphasizes that clinicians should use PDMP data for their clinical assessment and other relevant information to make informed decisions about prescribing controlled substances. Still, PDMP cannot be used as the sole basis for denying or providing treatment (14).
Case Study
After five days on Gabapentin, Mary was doing well, and her neuropathic pain had decreased to 3/10. However, Mary suffered a fall after her knee "gave out" and injured her knee and back. She was in severe pain, and her family drove her to the ER. The ER doctors saw Mary, and orthopedics were consulted. Mary has surgery scheduled for a knee replacement a week from now.
Mary was prescribed Vicodin because she was in excruciating pain, but her prescription only allowed enough medication for two days. Mary has made an appointment with you to renew her prescription.
You evaluate Mary because you know that concomitant use of Gabapentin and opioids puts Mary at risk for respiratory depression and possible side effects, including accidental overdose.
Mary stated she has been more alert the past 24 hours and is afraid her functional status will continue to decline if she does not have more Vicodin because the pain in her back and knee makes it difficult to stand. You assess Mary. Mary stated she occasionally drinks alcohol but has not had a drink since she moved. She has no familial history of substance abuse or mental health disorders.
Mary's mother stayed at her house to help her for the first 24 hours after Mary's return from the ER, but Mary is providing her care now.
You check the PDMP database and see that Mary was prescribed eight pills she has taken over the last 48 hours.
Since the Vicodin has been effective without untoward side effects, and Mary's function is improving, you decide to refill the prescription of Vicodin. You will taper the dose to three Vicodin daily for two days and two for one day. Mary will be near her appointment for a knee replacement as well.


Self Quiz
Ask yourself...
- What are the potential benefits and drawbacks of using PDMPs in your practice?
- How can PDMPs help you identify potential drug abuse or diversion cases among your patients? Can you provide examples from your own experience?
- In what ways do PDMPs impact your decision-making process when prescribing controlled substances?
- What are the key considerations when prescribing controlled substances?
- How do you ensure responsible prescribing practices for controlled substances?
Preventing Opioid Use Disorder
As previously discussed, opioid addiction is a growing concern worldwide, affecting individuals from all walks of life. According to the CDC, "Anyone who takes prescription opioids can become addicted to them" (14).
As frontline healthcare professionals, nurse practitioners must recognize the signs of opioid addiction to provide timely intervention and support. This section will outline the key indicators of opioid addiction.
Physical Symptoms
Physical symptoms are often the first noticeable signs of opioid addiction. These symptoms may include constricted pupils, drowsiness, slurred speech, impaired coordination, and increased sensitivity to pain. Additionally, individuals struggling with opioid addiction may exhibit frequent flu-like symptoms, such as a runny nose, sweating, itching, or gastrointestinal issues.
Behavioral Changes
Opioid addiction can significantly impact an individual's behavior. These may include increased secrecy, frequent requests for early prescription refills, doctor shopping (seeking prescriptions from multiple healthcare providers), neglecting personal hygiene, and experiencing financial difficulties due to excessive spending on opioids (37).

Social Isolation
Opioid addiction often leads to social withdrawal and isolation. Individuals struggling with opioid addiction may distance themselves from family, friends, and social activities they once enjoyed. They may exhibit erratic mood swings, become defensive or hostile when confronted about their drug use, and display a general lack of interest in previously important activities (30).
Psychological Changes
The psychological impact of opioid addiction is significant. Individuals with opioid addiction may exhibit increased anxiety, depression, irritability, and restlessness. They may also experience cognitive impairments, memory lapses, and difficulties in decision-making. Healthcare professionals should be attentive to these changes, as they can indicate opioid addiction (51).
Tolerance and Withdrawal Symptoms
The development of tolerance and withdrawal symptoms are critical signs of opioid addiction. Individuals may require increased dosages of opioids to achieve the desired effect, indicating a growing tolerance. Furthermore, withdrawal symptoms such as muscle aches, nausea, vomiting, insomnia, and intense cravings for opioids may occur when the drug is discontinued or reduced abruptly (51).

Self Quiz
Ask yourself...
- Discuss how nurse practitioners can contribute to preventing opioid use disorder.
- Explain how nurse practitioners effectively communicate the risks and signs of opioid misuse without stigmatizing or alienating patients.
- What are the signs of opioid addiction or misuse in patients?
- How do you approach patients who may be at risk for opioid addiction?
- How do you ensure appropriate documentation when prescribing controlled substances?
Opioid Overdose
The management of opioid overdose, withdrawal, and addiction requires a comprehensive approach that combines pharmacological interventions with psychosocial support. Naloxone remains a vital tool for reversing opioid overdose, while medications such as Methadone, buprenorphine, and naltrexone play crucial roles in withdrawal and addiction treatment (National Institute of Health, 2023). Nurse practitioners must stay vigilant and informed about the evolving landscape of medications. This section aims to provide a comprehensive review of medications and treatment strategies for opioid overdose, withdrawal, and addiction and is excerpted from the NIH (40).
Naloxone
Mechanism of Action and Metabolism
Naloxone is an opioid receptor antagonist. It works by binding to opioid receptors and displacing any opioids present, thereby reversing the effects of opioid overdose. It has a higher affinity for opioid receptors than most opioids, effectively blocking their action.
Naloxone is indicated for emergency intervention of opioid overdose. It effectively reverses respiratory depression and other life-threatening effects. Studies suggest the potential benefits of combining naloxone with other medications, such as buprenorphine (see below), to improve outcomes. Initiatives promoting community-based naloxone distribution programs have shown promising results in reducing opioid-related deaths.
Available Forms
Naloxone is available in various formulations:
- Intranasal
- Intramuscular
- Intravenous
- auto-injectors.
The most used form is the intranasal spray, which is easy to administer and requires no specialized training. Intranasal naloxone formulations have gained popularity due to their ease of use and increased availability. A recent study showed that the non-FDA-approved compound spray was far less effective than either FDA compound (15).
Dosing and Monitoring
The recommended initial dose of naloxone for opioid overdose is 2mg intranasally or 0.4mg to 2mg intramuscularly or intravenously. If the patient does not respond within 23- minutes, additional doses may be administered every 2-3 minutes. Continuous monitoring of the patient's respiratory status is essential, as repeat doses may be required due to the short half-life of naloxone.
Side Effects and Contraindications
Naloxone has been shown not to affect individuals without opioids in their system.
Common side effects of naloxone include
- Withdrawal symptoms: increased heart rate, sweating, and agitation
- nausea
- vomiting
- headache
Contraindications include known hypersensitivity to naloxone and situations where the use of naloxone may be unsafe or not feasible.
Considerations for Nurse Practitioners
Fentanyl and other opioids have a rapid onset, and the need to act quickly is paramount. As mentioned previously, the ease of use and higher plasma concentrations using the FDA-approved 4-mg FDANxSpray device compared with the locally compounded nasal sprays should be considered when ordering Naloxone (15).
Fentanyl and other potent synthetic opioids may require multiple administrations of naloxone to achieve reversal of an overdose (Chiang, Gyaw, & Krieter, 2019). As a nurse practitioner prescribing naloxone, it is crucial to assess the patient's risk factors for opioid overdose, such as a history of substance use disorder or chronic pain management. Education regarding the proper administration of naloxone should be provided to the patients and their caregivers. Additionally, it is essential to provide resources for follow-up care, including addiction treatment and ongoing support.
Methadone
Mechanism of Action and Metabolism
Methadone is a long-acting opioid agonist that effectively suppresses withdrawal symptoms and reduces cravings. It binds to the same opioid receptors in the brain as other opioids. It relieves withdrawal symptoms and reduces cravings by blocking the euphoric effects of opioids, thus helping individuals with opioid dependence to achieve stability (33).
Available Forms
Methadone is available in oral tablets and liquid formulations. The oral tablet is the most used form and is typically administered once daily (33).
Dosing and Monitoring
Methadone dosing is individualized based on the patient's response and needs. Initially, the dose often started low and gradually increased until the patient reached a stable dose. Dosing may need to be adjusted based on the patient's response, adherence, and any changes in their overall health. Regularly monitoring the patient's vital signs, urine drug screens, and assessment of their withdrawal symptoms and cravings is essential.
Side Effects and Contraindications
Common side effects of methadone include:
- Constipation
- dry mouth
- drowsiness
- sweating
- weight gain
- respiratory depression
Contraindications include:
- known hypersensitivity to methadone
- severe asthma
- respiratory depression
- certain heart conditions (33).
Considerations for Nurse Practitioners
As a nurse practitioner prescribing methadone, conducting a comprehensive assessment of the patient's medical history, current medications, and substance use history is crucial. Opioid treatment programs or specialized clinics are often involved in methadone treatment, so collaboration and coordination of care with these programs are essential. Regularly monitoring the patient's progress, adherence, and potential side effects or drug interactions is essential. Additionally, providing education on the risks and benefits of methadone and the importance of adherence to the prescribed regimen is crucial for successful treatment outcomes.
Buprenorphine
Mechanism of Action and Metabolism
Buprenorphine is a partial opioid agonist with a ceiling effect that minimizes the risk of overdose while reducing withdrawal symptoms. Buprenorphine is a partial opioid agonist that binds to the same receptors as other opioids but produces a weaker response. It has a high affinity for the mu-opioid receptors, which helps reduce cravings and withdrawal symptoms in individuals with opioid dependence.
Available Forms
Buprenorphine is available in different formulations, including sublingual tablets, buccal films, and extended-release injections. The sublingual tablets have different strengths, such as 2mg, 4mg, 8mg, and 12mg. Buprenorphine is taken as a daily tablet or weekly or monthly injection.
Dosing and Monitoring
The dosing of buprenorphine varies depending on the individual's opioid dependence severity and treatment phase. Initially, a low dose (e.g., 2-4mg) is given, and it may gradually increase to a maintenance dose of 8-24 mg daily. Regular monitoring is essential to assess the patient's response, adherence, and potential side effects.
Side Effects and Contraindications
Common side effects of buprenorphine include:
- Constipation
- Nausea
- Headache
- Insomnia
- Sweating
Serious side effects are rare but can include:
- Respiratory depression
- Allergic reactions
Buprenorphine is contraindicated in individuals with:
- Severe respiratory insufficiency
- Acute intoxication with opioids
- Known hypersensitivity
Considerations for Nurse Practitioners
Nurse practitioners can prescribe buprenorphine for opioid dependence treatment under the Drug Addiction Treatment Act (DATA). To become eligible, they must complete specific training requirements and obtain a waiver from the Substance Abuse and Mental Health Services Administration (SAMHSA). Nurse practitioners should assess patients thoroughly, including their opioid use history, comorbidities, and medication compatibility, while ensuring appropriate counseling and referral for comprehensive treatment (40).
Clonidine + Lofexidine
Mechanism of Action and Metabolism:
Both Clonidine and Lofexidine are alpha-2 adrenergic agonists. They work by stimulating alpha-2 receptors in the brain, which reduces sympathetic outflow and norepinephrine release. This results in decreased sympathetic activity, leading to various effects such as reduced blood pressure, decreased heart rate, and alleviated withdrawal symptoms (28).
Available Forms
Clonidine is available in oral tablets and patches. Lofexidine is available in oral tablets and is taken as needed (40).
Dosing and Monitoring
For opioid withdrawal, the Clonidine dose ranges from 0.1-0.3 mg every 4-6 hours. Lofexidine is usually initiated at 0.53 mg three times daily, and the dose can be increased to 2.88 mg daily. Monitoring blood pressure and heart rate is essential during treatment (40).
Side Effects and Contraindications:
Common side effects of both medications include:
- dry mouth
- sedation
- dizziness
- constipation
- orthostatic hypotension (40).
Both medications are contraindicated in patients with:
- Hypotension
- Bradycardia
- heart block
- history of hypersensitivity to the drugs (40).
Considerations for Nurse Practitioners:
An early study of lofexidine vs. clonidine for withdrawal symptoms showed that treatment with lofexidine resulted in lower withdrawal symptoms, fewer mood problems, less sedation, and hypotension. There were no significant differences in craving levels, morphine metabolites in urine, or dropout rates when both were compared.
Lofexidine can be a safe option for outpatient treatment as it does not lead to hypotension. However, nurse practitioners must closely monitor patients' blood pressure and heart rate during treatment and educate them about possible side effects. If patients experience any concerning symptoms, they should inform their nurse practitioner immediately.
Gradual dose reduction of Clonidine is crucial to prevent rebound hypertension. Before prescribing either medication, nurse practitioners should assess for any contraindications or potential drug interactions (19).
Emerging Therapies for Withdrawal
Extended-release naltrexone: Naltrexone is an opioid receptor antagonist that blocks the effects of opioids, reducing the risk of relapse. It is taken as a monthly injection.
Alpha-2 adrenergic agonists: Emerging evidence suggests the potential use of dexmedetomidine and guanfacine for managing opioid withdrawal symptoms.
Medication-Assisted Treatment (MAT):
Methadone was introduced in the 1960s and marked a significant turning point in opioid addiction treatment or MAT. Along with counseling and behavioral therapies, MAT became the cornerstone of opioid addiction recovery.
Examples of medications used:
- Methadone
- Buprenorphine:
- Naltrexone:
Adjunctive Pharmacotherapies:
Antidepressants: Selective serotonin reuptake inhibitors and tricyclic antidepressants may help manage co-occurring depression and anxiety.
Anticonvulsants:
Medications like Gabapentin and pregabalin show promise in reducing opioid cravings and improving treatment outcomes.


Self Quiz
Ask yourself...
- What are the mechanisms of action for commonly prescribed addiction medications?
- What are the potential risks and benefits of using benzodiazepines for pain management?
- How do you assess and manage patients with co-occurring pain and substance use disorders?
- What are the guidelines for prescribing addiction medications like buprenorphine or methadone?
- How do these medications work in the treatment of opioid use disorder?
- What are the potential side effects and risks associated with addiction medications?
- How do you support patients in their recovery from opioid use disorder?
- How do you address patients' concerns and fears about addiction medications?
- What are the federal guidelines around prescribing addiction medications for nurse practitioners?
- How do these guidelines influence your prescribing practices?
Other Substance Use Disorders
Patients in pain may struggle with Substance Use Disorders other than Opioid Use Disorder. Substance use disorders may often occur with mental health conditions such as anxiety, depression, and bipolar disorder. In addition, many individuals engage in polydrug use. Understanding the most common Substance Use Disorders aids in a comprehensive assessment of the patient and the development of appropriate treatment plans (28).
Alcohol Use Disorder (AUD):
The prevalence of AUD worldwide was estimated to be 9.8% in men and 5.5% in women in 2016 (28).
Cannabis Use Disorder (CUD):
the prevalence of CUD in the United States increased from 2.18% in 2001-2002 to 2.89% in 2012-2013. (28).
Cocaine Use Disorder:
According to the National Survey on Drug Use and Health (NSDUH), in 2019, approximately 1.9 million Americans aged 12 or older had cocaine use disorder in the past year (44).
Methamphetamine Use Disorder:
A study published in Drug and Alcohol Dependence reported that the prevalence of methamphetamine use disorder in the United States was estimated to be 0.2% in 2015-2016 (6).

Self Quiz
Ask yourself...
- What are the options available for managing opioid addiction and withdrawal?
- How can nurse practitioners support patients in their recovery from opioid addiction?
- What strategies can nurse practitioners employ to effectively engage and build trust with patients reluctant to disclose or seek help for substance abuse disorders?
- How can nurse practitioners collaborate with other healthcare professionals and community resources to provide comprehensive care and support for patients with substance abuse disorders?
- What techniques or tools can nurse practitioners employ to start these sensitive conversations with new patients?
- How do you assess and manage patients experiencing opioid withdrawal symptoms?
- What are the non-pharmacological interventions for managing opioid withdrawal?
- How do you educate patients about the risks and benefits of addiction medications?
- How do you monitor patients on addiction medications for adherence and progress?
- What are the drug potential interactions with commonly prescribed addiction medications?
Drug Diversion and Illegal opioids
Misuse of opioids is facilitated by diversion and is defined as "the transfer of drugs from lawful to unlawful use" (24). Most commonly, this occurs when family and friends share prescribed opioids with other family and friends. Opioids and other controlled drugs are also diverted from healthcare facilities. Statistics show that healthcare facility diversion has increased since 2015 (24)
Diversion affects patients, healthcare workers, healthcare facilities, and public health. Patients experience substandard care due to ineffective pain management and impaired healthcare workers. In addition, affected patients are at risk of infections from compromised syringes (24).
Healthcare employees who divert are at risk of overdose and death. If caught, they face criminal prosecution and malpractice suits. Healthcare facilities also bear the cost of diverted drugs via internal investigations, follow-up care for affected patients, regulatory fines for inadequate safeguards, and declining public trust (24).
Despite the enormous consequences of drug diversion, healthcare facilities have implemented few processes to detect and deter the diversion of controlled substances (24).

Self Quiz
Ask yourself...
- What protocols can nurse practitioners implement to prevent drug diversion within their healthcare setting?
Patient Teachings and Considerations
Opioids have significant side effects and carry a risk of addiction and overdose. Nurse practitioners can decrease the risks of misuse and addiction by educating patients on appropriate disposal, safe storage, and potential signs of addiction. Taking additional time to provide teaching nurse practitioners can promote patient safety, informed decision-making, and responsible opioid use.
Safe Storage and Disposal:
- Teach patients to store opioids securely, out of reach of children, pets, visitors, and non-caregiver family members, to prevent accidental ingestion or misuse (13). Only the caregiver, if applicable, or the patient should have access to pain medications.
- Instruct patients on proper disposal methods, such as using drug take-back programs or mixing opioids with undesirable substances (e.g., coffee grounds) before throwing them away (11) (13).
Medication Adherence:
- Emphasize the importance of taking opioids as prescribed, at the correct dose and frequency, to achieve optimal pain relief.
- Encourage patients to notify their healthcare provider if they experience inadequate pain control or side effects (35).
Potential Side Effects:
- Educate patients about common side effects of opioids, including constipation, nausea, sedation, and respiratory depression.
- Discuss strategies to manage side effects, such as maintaining adequate hydration, consuming a fiber-rich diet, and using over-the-counter laxatives as needed (11).
Risk of Dependence and Addiction:
- Explain the potential for opioid dependence and addiction, especially with long-term use or a history of substance abuse.
- Encourage patients to promptly report signs of opioid misuse, such as craving, loss of control, or continued use despite negative consequences (51).

Avoiding Alcohol and Other Central Nervous System Depressants:
- Instruct patients to avoid consuming alcohol or other medications that can enhance the sedative effects of opioids, increasing the risk of respiratory depression.
- Advise patients to contact the Nurse Practitioner before starting new medications, including over-the-counter drugs or herbal supplements (2).
Driving and Operating Machinery:
- Inform patients about the potential impairment caused by opioids, including reduced alertness, reaction time, and coordination.
- Advise patients to avoid driving or operating heavy machinery while taking opioids until they know how the medication affects them (14).

Self Quiz
Ask yourself...
- What strategies can nurse practitioners employ to effectively communicate the risks and benefits of opioid use while ensuring they clearly understand the potential side effects and the importance of adhering to the prescribed regimen?
- How can nurse practitioners promote patient engagement and shared decision-making regarding opioid pain management, considering the potential for dependence and addiction?
- How can nurse practitioners assess a patient's knowledge and understand the safe storage and disposal of opioids?
Case Study
You take some extra time with Mary to educate her on the taper dose of Vicodin, the potential for harm, and the risk of opioids, especially when used concomitantly with Gabapentin. You let Mary know it is unsafe to use alcohol, not only with Vicodin but also with Gabapentin. You let Mary know that Vicodin has a risk of dependency and misuse and, therefore, she will be monitored carefully. You also educate that Mary should store the Vicodin away from visibility by anyone but herself since she can self-administer her medication. You let Mary know that Vicodin can cause constipation and that she should increase her water intake and take a stool softener.
You ask Mary to call you if her pain is not adequately relieved or if her medications run out before the three days.
You let Mary know that if she does stop taking the Vicodin before she has completed all the medication, she should dispose of it by mixing the pills with liquid and coffee grounds to make them unpalatable to animals and others.
Mary complied with your education, completed her course of Vicodin, and was scheduled for surgery. Mary's social worker helped her communicate with her new employer and delayed her start date until after her recovery.
During her recovery, Mary received physical therapy and a short course of pain medication managed by her orthopedist.
Mary returned to the clinic for a follow-up visit after completing her therapy and before starting work. Mary's pain level in her knee is 3/10, and she already feels like she can walk further than pre-surgery. Gabapentin has continued to help Mary's neuropathic pain in her back, and she reports 2/10. Mary looks forward to beginning her new job and is optimistic about the future.
Conclusion
Pain management is the leading cause of primary care appointments and chronic pain is the leading cause of disability. Yet, prescribing opioids for primary care patients is also a factor in drug misuse and the opioid epidemic. Nurse practitioners are challenged to appropriately treat pain and effectively control diversion, addiction, and death from overdose.
It is imperative that nurse practitioners use evidence-based practices to assess, appropriately intervene, and educate about the benefits and potential harm caused by treatment with opioids. Nurse practitioners must stay up to date with the current federal regulations regarding PDMPs, clinical prescribing guidelines, and emerging treatments for pain and opioid abuse disorders.
References + Disclaimer
- American Nurses Association (ANA). (2015). Code of ethics with interpretative statements. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/
- Baptiste, D. L., Caviness-Ashe, N., Josiah, N., Commodore-Mensah, Y., Arscott, J., Wilson, P. R., & Starks, S. (2022). Henrietta Lacks and America’s dark history of research involving African Americans. Nursing Open, 9(5), 2236–2238. https://doi.org/10.1002/nop2.1257
- Barrow, J. M., Brannan, G. D., & Khandhar, P. B. (2022, September 18). Research ethics. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459281/
- Centers for Disease Control and Prevention. (2024, September 4). The untreated syphilis study at Tuskegee timeline. https://www.cdc.gov/tuskegee/about/timeline.html
- Christman, E., Christman, T., Demaster, V. Ernstmeyer, K., Kliminski, K., Olson, A., Pomietlo, M., Roesler, A., Stewart, J., Teeter, J., Tyznik, A. & Zwicky, J. (2022). Chapter 6: Ethical practice. In K. Ernstmeyer & E. Christman (Eds.), Nursing management and professional concepts [Internet]. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/nursingmpc/chapter/6-3-ethical-dilemmas/
- Haddad, L. M., & Geiger, R. A. (2023, August 14). Nursing ethical considerations. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/sites/books/NBK526054/0
- John Hopkins Medicine. (n. d.). The legacy of Henrietta Lacks. https://www.hopkinsmedicine.org/henrietta-lacks
- Office of Science Policy, National Institutes of Health. (2022, October). Significant research advances enabled by HeLa cells. https://osp.od.nih.gov/hela-cells/significant-research-advances-enabled-by-hela-cells/
- Olejarczyk, J. P., & Young, M. (2024, May). Patient rights and ethics. In: StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538279/
- Shea, B. (2023, October 18). Four principles of bioethics. In Ethical explorations: Moral dilemmas in a universe of possibilities. Minnesota Libraries Publishing Project; Rochester, MN. https://mlpp.pressbooks.pub/ethicalexplorations/chapter/chapter-12-bioethics12/
- Tobin, M. J. (2022). Fiftieth anniversary of uncovering the Tuskegee syphilis study: The story and timeless lessons. American Journal of Respiratory and Critical Care Medicine, 205(10), 1145–1158. https://doi.org/10.1164/rccm.202201-0136SO
ELEMENT I
- https://www.op.nysed.gov/title8/rules-board-regents/part-29
- https://regs.health.ny.gov/content/section-92-11-course-work-or-training
- https://www.cdc.gov/oralhealth/infectioncontrol/summary-infection-prevention-practices/standard-precautions.html
- https://www.nursingworld.org/practice-policy/work-environment/health-safety/infection-prevention/
- https://www.cdc.gov/infectioncontrol/guidelines/core-practices/index.html
- https://www.cdc.gov/hai/data/portal/progress-report.html
- https://www.ncsbn.org/filing-a-complaint.htm
ELEMENT II
- Douedi, S., & Douedi, H. (2020) Precautions, bloodborne, contact, and droplet. In StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK551555/
- https://www.cdc.gov/niosh/topics/healthcare/infectious.html
- Abbas AK, Lichtman AH, Pillai S. Properties and overview of immune responses. In: Abbas AK, Lichtman AH, Pillai S, eds. Cellular and Molecular Immunology. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 1.
- https://www.cdc.gov/training/publichealth101/e-learning/prevention-effectiveness/
- https://www.cdc.gov/infectioncontrol/basics/standard-precautions.html
- https://www.cdc.gov/injectionsafety/spinalinjection-meningitis.html
- Carrico, R., Garrett, H., Balcom, D, & Burton Glowicz, J. (2018). Infection prevention and control core practice: a roadmap for nursing practice. Nursing, 48(8), 28-29. doi: 10.1097.NURSE.0000544318.36012.b2
- Sands, M.,& Aunger, R. (2020). Determinants of hand hygiene compliance among nurses in US hospitals: a formative research study. PLoS ONE, 15(4), 2-29. doi: 10.1371/journal. pone.0230573
- Pyrek, K. (2017). Cleanliness of hands and surfaces play key role in cross-contamination prevention. Infection Control Today, 21(5).Retrieved from https://www.infectioncontroltoday.com/view/cleanliness-hands-and-surfaces-plays-key-role-cross-contamination-prevention
- Assadian, O., Kramer, A., Cristiansen, B., Exner, M., Martiny, H., Sorger, A., & Suchomel, M. (2012). Recommendations and requirements for soap and hand rub dispensers in healthcare facilities. GMS Krankenhhyg Interdisziplinar, 7(1), 4-5. doi: 10.3205/dgkh000187
- https://www.cdc.gov/infectioncontrol/projectfirstline/resources/ppe-covid-19.html
- Watson, N. (2007). Isolation and cohort care. The Journal of the Intensive Care Society, 8(3). Retreived from https://journals.sagepub.com/doi/pdf/10.1177/175114370700800308
- https://www.cdc.gov/infectioncontrol/guidelines/isolation/
- https://www.hhs.gov/vaccines/vaccines-national-strategic-plan/vision-and-goals/index.html
- https://www.cdc.gov/infectioncontrol/pdf/guidelines/environmental-guidelines-P.pdf
- https://www.dec.ny.gov/chemical/8789.html
- https://regs.health.ny.gov/content/section-83-117-linen-and-laundry
ELEMENT III
- https://www.osha.gov/etools/hospitals/hospital-wide-hazards/biological-hazards
- Kossover-Smith, R. Coutts, K., Hatfield, K., Cochran, R., Akselrod, H., Schaefer, . . . & Bruss, K. (2017). One needle, one syringe, only one time? A survey of physician and nurse knowledge, attitudes, and practices around injection safety. American Journal of Infection Control, 45(9), 1018-1023. doi: 10.1016/j.ajic.2017.04.292
- https://www.cdc.gov/sharpssafety/pdf/sharpsworkbook_2008.pdf
ELEMENT IV
- https://www.cdc.gov/infectioncontrol/pdf/strive/PPE103-508.pdf
- https://www.ventyv.com/blog/whats-the-difference-between-nitrile-latex-and-vinyl-gloves
- https://www.cdc.gov/niosh/npptl/topics/protectiveclothing/default.html
- https://www.cdc.gov/niosh/topics/respirators/
- https://www.cdc.gov/niosh/topics/bbp/
ELEMENT V
- https://www.cdc.gov/infectioncontrol/pdf/guidelines/disinfection-guidelines-H.pdf
- https://www.cdc.gov/infectioncontrol/guidelines/disinfection/efficacy.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3678066/
- https://www.cdc.gov/infectioncontrol/guidelines/disinfection/cleaning.html
- https://www.osha.gov/Publications/OSHA3512.pdf
ELEMENT VI
- https://www.cdc.gov/infectioncontrol/guidelines/healthcare-personnel/evaluation.html
- https://www.cdc.gov/tb/topic/testing/tbtesttypes.htm
- https://www.cdc.gov/infectioncontrol/pdf/guidelines/infection-control-HCP-H.pdf
- https://www.nyc.gov/assets/doh/downloads/pdf/hcp/reporting-guide.pdf
- https://www.cdc.gov/tb/topic/treatment/decideltbi.htm
- https://www.health.ny.gov/publications/1852/appenb.htm
- https://www.cdc.gov/infectioncontrol/guidelines/healthcare-personnel/exposures.html
ELEMENT VII
-
- https://www.health.ny.gov/diseases/conditions/sepsis/
- https://www.health.ny.gov/facilities/public_health_and_health_planning_council/meetings/2013-02-07/docs/13-01.pdf
- https://www.health.ny.gov/diseases/conditions/sepsis/docs/2019_sepsis_care_improvement_initiative.pdf
- https://www.sepsis.org/sepsis-basics/what-is-sepsis/
- https://www.nhsinform.scot/illnesses-and-conditions/blood-and-lymph/septic-shock
- Kim, H, & Park, S. (2019). Sepsis: Early recognition and optimized treatment. Tuberculosis and Respiratory Disease, 82(1), 6-14. doi: 10.4046/trd.2018.0041
- https://www.sccm.org/SurvivingSepsisCampaign/Guidelines/Adult-Patients
- https://www.mayoclinic.org/diseases-conditions/sepsis/diagnosis-treatment/drc-20351219
- https://www.cdc.gov/sepsis/pdfs/Consumer_fact-sheet_protect-yourself-and-your-family-P.pdf
- Alzheimer’s disease fact sheet. (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet
- Preventing Alzheimer’s disease: What do we know? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/preventing-alzheimers-disease-what-do-we-know
- How is Alzheimer’s disease treated? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/how-alzheimers-disease-treated
- Castro-Aldrete, L., Moser, M. V., Putignano, G., Ferretti, M. T., Diemch, A. S., and Chadha, A. S. (2023). Sex and gender considerations in Alzheimer’s disease: The Women’s Brain Project contribution. Frontiers in Aging Neuroscience, 15, 1-11. https://doi.org/10.3389/fnagi.2023.1105620
- Carrarini, C., Russo, M., Dono, F., Barbone, F., Rispoli, M. G., Ferri, L., Di Pietro, M., Digiovanni, A., Ajdinaj, P., Speranza, R., Granzotto, A., Frazzini, V., Thomas, A., Pilotto, A., Padovani, A., Onofrj, M., Sensi, S. L., & Bonanni, L. (2021). Agitation and Dementia: Prevention and Treatment Strategies in Acute and Chronic Conditions. Frontiers in neurology, 12, 644317. https://doi.org/10.3389/fneur.2021.644317
- Alzhimer’s Disease: Common Medical Problems. (n.d.). Retrieved January 9, 2024, 10, 2021, from https://www.nia.nih.gov/health/alzheimers-caregiving/alzheimers-disease-common-medical-problems #7 Wandering and Alzhimer’s Diease. (n.d.). Retrieved January 9, 2024, from https://www.nia.nih.gov/health/alzheimers-changes-behavior-and-communication/wandering-and-alzheimers-disease
- National Institute on Aging. (2021) What is Lewy Body Dementia? Causes, Symptoms, and Treatments. Retrieved on December 5, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/what-lewy-body-dementia-causes-symptoms-and-treatments
- Medline Plus [Internet] National Library of Medicine. (2021). Dementia with Lewy Bodies. Retrieved on December 5, 2023, from https://medlineplus.gov/genetics/condition/dementia-with-lewy-bodies/#causes
- Haider, A., Spurlin, B., and Sanchez-Manso, J. (2023). Lewy Body Dementia. In StatPearls. StatPearls [Internet]. Retrieved on December 7, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK482441/
- Prasad, S., Katta, M., Abhishek, S., Sridhar, R., Valisekka, S., Hameed, M., Kaur, J., and Walia, N. (2022). Disease-a-Month. Vol. 69, Issue 5, May 2023, 101441. Retrieved from https://www.sciencedirect.com/science/article/pii/S0011502922001250?via%3Dihub
- Medline Plus [Internet] National Library of Medicine. (2019). Lewy Body Dementia. Retrieved on December 7, 2023, from https://medlineplus.gov/lewybodydementia.html
- Hershey, L. and Coleman-Jackson, R. (2019). Pharmacological Management of Dementia with Lewy Bodies. Drugs Aging. 2019; 36(4) 309-319. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6435621/
- National Institute on Aging. (2018). Caring for a Person with Lewy Body Dementia. Retrieved on December 21, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/caring-person-lewy-body-dementia
- Capouch, S., Farlow, M., and Brosch, J. (2018). A Review of Dementia with Lewy Bodies’ Impact, Diagnostic Criteria and Treatment. Neurology and Therapy. 2018 Dec; 7(2): 249-263. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6283803/
- Lewy Body Dementia Resource Center. (2021) Our Mission & Vision. Retrieved on December 21, 2023, from https://lewybodyresourcecenter.org/about-us/mission/
- Lewy Body Dementia Association. (2023). About LBDA. Retrieved on December 20, 2023 from https://www.lbda.org/about-lbda/
- National Institute of Neurological Disorders and Stroke. (2023) Focus on Lewy BOdy Dementia (LBD). Retrieved on December 20, 2023, from https://www.ninds.nih.gov/current-research/focus-disorders/alzheimers-disease-and-related-dementias/focus-lewy-body-dementia-lbd-research
- National Institute of Neurological Disorders and Stroke. (2018). PDBP About. Retrieved on December 21, 2023, from https://pdbp.ninds.nih.gov/about
- Bousiges, O. and Blanc, F. (2022). Biomarkers of Dementia with Lewy Bodies: Differential Diagnostic with Alzheimer’s Disease. International Journal of Molecular Sciences. 2022 Jun; 23 (12): 6371. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9223587/
- Howell, M. and Schenk, C. Rapid Eye movement sleep behavior disorder. 2023) UpToDate. Retrieved on December 21, 2023 from https://www.uptodate.com/contents/rapid-eye-movement-sleep-behavior-disorder/print#:~:text=INTRODUCTION%20Rapid%20eye%20movement%20(REM,thrashing%2C%20punching%2C%20and%20kicking.
- Arevalo, I., Smailagic, N., Roque I Figuls, M., Ciapponi, A., Sanchez-Perez, E., Giannakou, A., Pedraza, O., Cosp, X., and Cullum, S. (2015). Mini-Mental State Examination (MMSE) FOR THE DETECTION OF Alzheimer’s disease and other dementia in people with milk cognitive impairment (MCI). Cochrane Library. 2015 Mar; 2015(30): CD010783. Retrieved from https://doi.org/10.1002/14651858.CD010783.pub2
- National Institute on Aging. (2021). Diagnosing Lewy Body Dementia: For Professionals. Retrieved on December 22, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/diagnosing-lewy-body-dementia-professionals
- Acquadro Maran D, Varetto A, Civilotti C. Sexual Harassment in the Workplace: Consequences and Perceived Self-Efficacy in Women and Men Witnesses and Non-Witnesses. Behav Sci (Basel). 2022 Sep 8;12(9):326. doi: 10.3390/bs12090326. PMID: 36135130; PMCID: PMC9495880.
- Cedeno, R., & Bohlen, J. (Updated 2023, June 25). Sexual Harassment and Prevention Training. In StatPearls. StatPearls Publishing, Inc. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK587339/
- Hope AA, Munro CL. Getting to Zero Sexual Harassment in the Workplace. Am J Crit Care. 2021 Jul 1;30(4):250-252. doi: 10.4037/ajcc2021198. PMID: 34195775.
- Illinois General Assembly. (2024). Illinois Compiled Statuses: State Officials and Employees Ethics Act. Retrieved from https://www.ilga.gov/legislation/ilcs/ilcs4.asp
- Kahsay WG, Negarandeh R, Dehghan Nayeri N, Hasanpour M. Sexual harassment against female nurses: a systematic review. BMC Nurs. 2020 Jun 29;19:58. doi: 10.1186/s12912-020-00450-w. Erratum in: BMC Nurs. 2020 Jul 13;19:64. PMID: 32612455; PMCID: PMC7324991.
- Salerno-Ferraro AC, Erentzen C, Schuller RA. Young Women’s Experiences With Technology-Facilitated Sexual Violence From Male Strangers. J Interpers Violence. 2022 Oct;37(19-20):NP17860-NP17885. doi: 10.1177/08862605211030018. Epub 2021 Jul 16. PMID: 34271829; PMCID: PMC9554274.
- Society for Human Resource Management. (2024, January 31). What are the different types of sexual harassment? Society for Human Resource Management. Retrieved from https://www.shrm.org/in/topics-tools/tools/hr-answers/different-types-sexual-harassment
- Strauss, S., (January 31, 2019) “Overview and Summary: Sexual Harassment in Healthcare” OJIN: The Online Journal of Issues in Nursing Vol. 24, No. 1, Overview and Summary.U.S. Department of Justice. (2022, September 12). Equal Employment Opportunity, Anti-Harassment, & Whistleblower Protection Policy. U.S. Department of Justice. Retrieved from https://www.justice.gov/media/1250821/dl?inline
- U.S. Equal Employment Opportunity Commission. (2024). Policy Guidance on Current Issues of Sexual Harassment. U.S. Equal Employment Opportunity Commission. Retrieved from https://www.eeoc.gov/laws/guidance/policy-guidance-current-issues-sexual-harassment
- U.S. Equal Employment Opportunity Commission. (2024). Sexual Harassment. U.S. Equal Employment Opportunity Commission. Retrieved from https://www.eeoc.gov/sexual-harassment
- Vara-Horna AA, Díaz-Rosillo A, Asencios-Gonzalez Z, Quipuzco-Chicata L. Direct and indirect effects of workplace sexual harassment on the productivity of victims and witnesses: The preventive role of equitable management. Heliyon. 2023 Oct 20;9(11):e21096. doi: 10.1016/j.heliyon.2023.e21096. PMID: 37920480; PMCID: PMC10618782.
- Zeng LN, Zong QQ, Zhang JW, Lu L, An FR, Ng CH, Ungvari GS, Yang FY, Cheung T, Chen L, Xiang YT. Prevalence of sexual harassment of nurses and nursing students in China: a meta-analysis of observational studies. Int J Biol Sci. 2019 Jan 29;15(4):749-756. doi: 10.7150/ijbs.28144. PMID: 30906207; PMCID: PMC6429024.
- American College of Obstetrics and Gynecology. (2022). Reproductive and sexual coercion. Retrieved from: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2013/02/reproductive-and-sexual-coercion#:~:text=Reproductive%20coercion%20is%20related%20to,pregnancy%20coercion%2C%20and%20pregnancy%20pressure.
- Burnett, L. B. (2018, July). Domestic violence follow up. Emergency Medicine. Retrieved from: https://emedicine.medscape.com/article/805546-overview?form=fpf
- Domestic Abuse Intervention Programs. (n.d.). Power and control wheel. NCADV. Retrieved from: https://www.theduluthmodel.org/wp-content/uploads/2017/03/PowerandControl.pdf
- Centers for Disease Control and Prevention. (2021, November). Risk and protective factors for perpetration. Retrieved from: https://www.cdc.gov/violenceprevention/intimatepartnerviolence/riskprotectivefactors.html
- Centers for Disease Control and Prevention. (2023, January). Fast fact: preventing teen dating violence. Retrieved from: https://www.cdc.gov/violenceprevention/intimatepartnerviolence/teendatingviolence/fastfact.html
- Connecticut Coalition Against Domestic Violence. (2024). https://www.ctcadv.org/
- Connecticut State Department of Public Health. (n.d.). Continuing education. DPH. https://portal.ct.gov/DPH/Practitioner-Licensing–Investigations/Registered-Nurse/Continuing-Education
- Connecticut State Department of Public Health. (n.d.). Mandatory reporters of abuse, neglect, exploitation, and impaired practitioners. DPH. https://portal.ct.gov/DPH/Practitioner-Licensing–Investigations/PLIS/Mandatory-Reporters-of-Abuse-Neglect-Exploitation-and-Impaired-Practitioners
- Connections for Abused Women and Their Children. (2023, February). The impact of domestic violence. Retrieved from: https://www.cawc.org/news/the-impact-of-domestic-violence/?gclid=Cj0KCQjwiIOmBhDjARIsAP6YhSWPF8eUFB4f_OF2oy4w6YdyGheawOkX8Heh_hvOCPT-Wg3vp9bICeIaAkH5EALw_wcB
- Gillette, H. (2022). The 4 stages of the cycle of abuse: from tension to calm and back. Retrieved from: https://psychcentral.com/health/cycle-of-abuse
- GLAAD. N.d. Glossary of terms: LGBTQ. Retrieved from: https://www.glaad.org/reference/terms
- Karakurt, G., Whiting, K., van Esch, C., Bolen, S. D., & Calabrese, J. R. (2016). Couples Therapy for Intimate Partner Violence: A Systematic Review and Meta-Analysis. Journal of marital and family therapy, 42(4), 567–583. https://doi.org/10.1111/jmft.12178
- Lantz, B., Wenger, M. R., & Craig, C. J. (2023). What If They Were White? The Differential Arrest Consequences of Victim Characteristics for Black and White Co-offenders. Social problems, 70(2), 297–320. https://doi.org/10.1093/socpro/spab043
- March of Dimes. (n.d.). Abuse during pregnancy. Retrieved from: https://www.marchofdimes.org/find-support/topics/pregnancy/abuse-during-pregnancy#:~:text=Unfortunately%2C%20some%20women%20experience%20abuse,is%20first%20abused%20during%20pregnancy.
- National Coalition Against Domestic Violence. (n.d.). Domestic violence and children. NCADV. Retrieved from: https://assets.speakcdn.com/assets/2497/dv_and_children.pdf
- National Coalition Against Domestic Violence (n.d.a,). Domestic violence and the black community. NCADV. Retrieved from: https://assets.speakcdn.com/assets/2497/dv_in_the_black_community.pdf
- National Coalition Against Domestic Violence (n.d.). Gender based violence in rural communities. NCADV. Retrieved from: https://assets.speakcdn.com/assets/2497/ncadv_fact_sheet_-_gbv_in_rural_communities.pdf
- National Coalition Against Domestic Violence. (n.d.b.). National statistics. NCADV. Retrieved from: https://ncadv.org/STATISTICS
- National Coalition Against Domestic Violence. (n.d.c.). Teen, campus, and dating violence. NCADV. Retrieved from:https://assets.speakcdn.com/assets/2497/dating_abuse_and_teen_violence_ncadv.pdf
- National Coalition Against Domestic Violence. (2018). Domestic violence and the LGBTQ community. NCADV. Retrieved from: https://ncadv.org/blog/posts/domestic-violence-and-the-lgbtq-community
- National Coalition Against Domestic Violence. (2022). Abuse in later life. NCADV. Retrieved from: https://assets.speakcdn.com/assets/2497/abuse_in_later_life.pdf
- Office of Violence Against Women (OVW). (2023, March). What is domestic violence? Department of Justice. Retrieved from: https://www.justice.gov/ovw/domestic-violence
- Sanctuary for Families. (2022, July). The link between disability and domestic violence. Retrieved from: https://sanctuaryforfamilies.org/disability-domestic-violence/
- Screening for Intimate Partner Violence, Elder Abuse, and Abuse of Vulnerable Adults: Recommendation Statement. (2019). American family physician, 99(10), .
- Taylor, V. (2022). When immigration becomes a tool in intimate partner violence. Retrieved from: https://bwjp.org/when-immigration-becomes-a-tool-in-intimate-partner-violence/?gclid=CjwKCAjwq4imBhBQEiwA9Nx1BjBxfxvBc9Mei36iutSPnSVwzwBynoEOQ5BDngmoCCcNu-pF7qY2xxoC2vkQAvD_BwE
- United States Department of Justice. (2000). Full Report of the Prevalence, Incidence, and Consequences of Violence Against Women. Retrieved from: https://www.ncjrs.gov/pdffiles1/nij/183781.pdf
- Women’s Rights Project. (n.d.). Domestic violence and homelessness. American Civil Liberties Union. Retrieved from: https://www.aclu.org/sites/default/files/pdfs/dvhomelessness032106.pdf
- Arts, E. J., & Hazuda, D. J. (2012). HIV-1 antiretroviral drug therapy. Cold Spring Harbor perspectives in medicine, 2(4), a007161. https://doi.org/10.1101/cshperspect.a007161.
- Avert. (2019). History of HIV and AIDS overview. Retrieved from: https://www.avert.org/professionals/history-hiv-aids/overview
- Bhatti, A. B., Usman, M., & Kandi, V. (2016). Current Scenario of HIV/AIDS, Treatment Options, and Major Challenges with Compliance to Antiretroviral Therapy. Cureus, 8(3), e515. https://doi.org/10.7759/cureus.515
- Centers for Disease Control. (2016). Today’s HIV/AIDS epidemic. Retrieved from: https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508.pdf
- Centers for Disease Control. (2019). HIV cost effectiveness. Retrieved from: https://www.cdc.gov/hiv/programresources/guidance/costeffectiveness/index.html.
- Centers for Disease Control. (2020). Evidence of HIV treatment and viral suppression in preventing the sexual transmission of HIV. Retrieved from: https://www.cdc.gov/hiv/pdf/risk/art/cdc-hiv-art-viral-suppression.pdf
- Centers for Disease Control. (2020). HIV. Retrieved from: https://www.cdc.gov/hiv/basics/whatishiv.html
- Centers for Disease Control. (2020). Sharing your test results. Retrieved from: https://www.cdc.gov/hiv/basics/hiv-testing/sharing-test-results.html/
- Currier, J. S., & Havlir, D. V. (2017). CROI 2017: Complications and Comorbidities of HIV Disease and Its Treatment. Topics in antiviral medicine, 25(2), 77–83.
- HIV.gov. (2020). U.S. statistics. Retrieved from: https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics
- Nursing Times. (2020). HIV: epidemiology, pathophysiology, and transmission. Retrieved from: https://www.nursingtimes.net/clinical-archive/immunology/hiv-1-epidemiology-pathophysiology-and-transmission-15-06-2020/
- Vaillant, A. J. and Guilick, P. G. (2020). HIV disease current practice. Statpearls. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK534860/.
- Abi-Aad, K., & Derain, A. (2023, August 17). Hydromorphone. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK470393/
- Adler, J., Ballantyne, J., Chou, R., Davies, P., Fanciullo, G., & Fine, P. (2009). Clinical Guidelines for the Use of Chronic Opioid Therapy in Chronic NonCancer Pain. The Journal of Pain, 113-130.
- Ahmad, F., Rossen, L., Sutton, P., & & Talih, M. (2018). Provisional drug overdose. National Vital Statistics Reports, pp. 1-12.
- Altman, R., Clark, M., Huddart, R., & Klein, T. (2018, October 28). Pharm GKB Summary: Oxycodone Pathway, Pharmacokinetics. Retrieved from Pharmacogenet Genomics: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6602093/#:~:text=Approximately%2072%25%20of%20an%20oxycodone,oxycodone%20is%20unconjugated%20%5B70%5D
- Atrux-Tallau, N., naimi, Z., & Jaudinot, E. (2022, November 4). Pharmocokinetics of Morphine Sulfate Orodispersible tablets and Bioequivalence with Immediate-Release Oral Morphine Sulfate Formulations in Healthy Adult SubjectsUnder fastin Conditions. Retrieved from Clinical Drig Investigation: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9705466/
- Baldwin, G., Compton, W. M., Han, B., Houry, D., Jones, C. M., & Vivolo-Kantor, A. (2021, September 24). Methamphetamine use in the United States: epidemiological update and implocations for prevention, treatment and harm reduction. Annual New York Academy of Science. New York: National Institute of Health.
- Berg, K. A., & Clarke, W. P. (2018). Making Sense of Pharmacology: Inverse Agonism and Functional Selectivtiy. International Journal of Neuropsychopharmacology, 962-977.
- Bistas, K., Lopez-Ojeda, W., & Ramos-Matos, C. (2023, May 29). Fentanyl. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK459275/
- Blyth, F., Briggs, A., Hoy, D. G., March, L. M., & Schneider, C. H. (2019). The Global Burden of Musculoskeletal Pain-Where to From Here? American Journal of Public Health, 35-40.
- Bramanti, P., Cavalli, E., Mammana, S., Mazzon, E., & Nicoletti, F. (2019). The neuropathic pain: An Overview of the current treatment and future therapeutic approaches. International Journal of Immunopathology and Pharmacology, 33.
- Brennan, F., Carr, D., Cousins, M., & Pain, D. (2013). Pain Management: A Fundamental Human Right. Anesthesia and Analgesia, 224-227.
- Carver, A. C., & Foley, K. (2003). Types of Pain. In D. Kufke, & R. W. Pollock, Cancer Medicine. Hamilton: Holland Frei Cancer Medicine.
- Centers for Disease Control and Prevention. (2022). CDCs Clinical Practice Guidelines for Prescribing Opioids. Retrieved from Opioids: https://www.cdc.gov/opioids/healthcare-professionals/prescribing/guideline/index.html?s_cid=DOP_Clinician_Search_Paid_001&gclid=CjwKCAjwrranBhAEEiwAzbhNtVKOCMzLLnwhfj7B2D_aBCZM_SryNcEyXl0GRigmorFhKve2ekCVrhoCNYQQAvD_BwE
- Centers for Disease Control and Prevention. (2023, August 8). Opioids. Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/opioids/basics/epidemic.html#print
- Chiang, N., Gyaw, S., & Krieter, P. A. (2019). Comparison of the Pharmacokinetic Properties of Naloxone Following the Use of FDA-Approved Intranasal and Intramuscular Devices Versus a Common Improvised Nasal Naloxone Device. Journal of Clinical Pharmacology, 1078-1084.
- Cicero, T., & Ellis, M. &. (2017). The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA, 673-681.
- Cofano, S., & Yellon, R. (2022, October 24). Stat Pearls: Hydrocodone. Retrieved from National Institutes of Health: https://www.ncbi.nlm.nih.gov/books/NBK537288/
- Dart, R., Hoyte, C., & Nakhee, S. (2021). A Review on Tramadol Toxicity: Mechanism of Action, Clinical Presentation, and Treatment. Forensic Toxicology, 293-310. Retrieved from Forensic Toxicology: https://link.springer.com/article/10.1007/s11419-020-00569-0
- Delsignor, R. e. (2001). Lofexidine versus clonidine in rapid opiate detoxification. Journal of Substance Abuse Treatment, 11-17.
- Department of Defense Veterans Association. (2023). Defense and Veterans Pain Rating Scale. Retrieved from VA.gov: https://www.va.gov/PAINMANAGEMENT/docs/DVPRS_2slides_and_references.pdf
- Department of Health and Aged Care. (2013, January 20). FLACC Pain Scale. Retrieved from health.gov: https://www1.health.gov.au/internet/publications/publishing.nsf/Content/triageqrg~triageqrg-pain~triageqrg-FLACC
- Donaldson, S. L. (2017). Provider-Based Interventions to Mitigate Risk for Opioid Pain Medication Abuse Among Adult Patients in a Primary Care Setting.
- Dydyk, A. M., & Grandhe, S. (2023, January 29). Pain Assessment. Retrieved from STAT PEARLS: https://www.ncbi.nlm.nih.gov/books/NBK556098/#:~:text=Pain%20is%20the%20most%20common,pain%20in%20the%20United%20States.
- Fan, M., Hamilton, M., Hyland, B., & Tscheng, D. (2019). Diversion of Controlled Drugs in Hospitals: A Scoping review of Contributors and Safeguards. Journal of Hospital Medicine.
- GeriatricPain.org. (2022, January). Fast Facts: Selected Pain Assessment Tools. Retrieved from Geriatricpain.org: Geriatricpain.org https://geriatricpain.org/selected-pain-assessment-tools-fc
- Haffajee, R., Jena, A., Weiner, S., & & Kesselheim, A. (2019). Mandatory use of prescription drug monitoring programs. Journal of the American Medical Association, 1667-1668.
- International Association for the Study of Pain . (2020, July 16). IASP Announces Revised Definition of Pain. Retrieved from International Association for the Study of Pain: https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
- JAMA. (2023). Substance Use and Addiction Medicine. Retrieved from JAMA Network: https://jamanetwork.com/collections/5921/substance-use-and-addiction-medicine
- John, W. S., Schwartz, R. P., Subramanian, G., & Wu, L.-T. (2018). Prevalence, Patterns and correlates of multiple substance use disorders among adults. Drug and Alcohol Dependency, 79-87.
- Jones, C., Einstein, E., & Compton, W. (2018). Changes in synthetic opioid involvement in drug overdose deaths in the United States. JAMA, 1819-1821.
- Kalava, A., King, K. C., & Preuss, C. V. (2023, April 29). Perscription of Controlled Substances: Benefits and Risks. Retrieved from STAT PEARLS: https://www.ncbi.nlm.nih.gov/books/NBK537318/
- Khalid, N., Patel, P., & Singh, A. (2023, January). Cannabis Versus Opioids for Pain. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK573080/
- Kreutzwiser, D., & Tawfic, Q. (2020). Mathadone for Pain Management. A Pharmacotherapeutic Review, 827-839.
- Kroenke, K., Spiter, R., Williams, J., & Lowe, B. (2011, Nov). An ultra-brief screening scale for anxiety and depression: the PHQ-4. From Principles of Neuropathic Pain Assessment and Management, 613-21. Psychosomatics 2009.
- Manchikanti, L., Kaye, A., Knezevic, N., McAnally, H., Slavin, K., Trescot, A., & Hirsch, J. (2018). Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians guidelines. Pain Physician, S3-S92.
- Marquez, C. B. (2020). Changing the outlook toward the problem of opioid addiction: From “War on Drug” to “Public Health Emergency”. Seton Hall: Law Student Scholarship.
- Marsch, L., Borodovsky, J., & Dallery, J. (2019). Advances in the psychosocial treatment of addiction: The role of technology in the delivery of evidence-based psychosocial treatment. The Psyciatric Clinics of North America, 585-596.
- McLellan, T., & Volkow, N. (2016). Opioid Abuse in Chronic Pain-Misconceptions and Mitigation Strategies. New England Journal of Medicine, 1253-1263.
- National Institute of Drug Abuse (NIDA). (2023, August 30). Prescription Opioid Drug Facts. Retrieved from National Institute on Drug Abuse: https://nida.nih.gov/publications/drugfacts/prescription-opioids
- National Institute of Health. (2023, August 25). Medications for Opioid Overdose, Withdrawal, & Addiction. Retrieved from National Institute of Drug Addiction: https://nida.nih.gov/research-topics/opioids/medications-opioid-overdose-withdrawal-addiction-infographic
- Pain Physician. (2008). Opioid Special Issue. Pain Physician, S133-S153.
- Ransford, e. a. (2019, February 08). The Ransford Pain Drawing . Retrieved from compassionandsupport.org: https://compassionandsupport.org/wp-content/uploads/sites/2/2019/08/PainScaleRansford.pdf
- Rudd, R. A., Zibbell, J., & Gladden, M. (2016). Increases in drug and opioid overdose deaths-Untied States. Morbidity and Mortlity Weekly Report, 1378-1382.
- SAMHSA. (2020). Key Substance Use and Mental Health Indicators in the United States: Ressults from the 2019 National Survey on Drug Use and Health. SAMHSA.
- Scalpel, S. (2016, November). The Joint Commission Deserves Some Blame for the Opioid Crisis. Retrieved from Missouri Medicine: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6139759/
- Scholl, L., Seth, P., Kariisa, M., Wilson, N., & Baldwin, G. (2019). Drug and opioid-involved overdose deaths-Unioted States, 2013-2017. Morbidity and Mortatlity Weekly Report 67, 1419-1427.
- Stauffer, L., & Gibson, S. (2017). The Nurse’s Role in Identifying and Educating Patients At Risk for Opioid Abuse. AAACN Viewpoint, 1.
- The Joint Commission. (2023, January). The Joint Commission History Timeline. Retrieved from JointCommission.org: https://www.jointcommission.org/-/media/tjc/documents/tjc-history-timeline-through-2022.pdf
- Toombs, K., Kral, L., Colleran, C., & & Varney, S. (2018). Nurse practitioner-pharmacist collaboration in pain management: Strategies for success. . Journal of the American Association of Nurse Practitioners, 141-148.
- U.S. Food and Drug Administration. (2023, May 23). FDA. Retrieved from Information about Medication Assisted Treatment (MAT): https://www.fda.gov/drugs/information-drug-class/information-about-medication-assisted-treatment-mat
- Volkow, N., Jones, E., Einstein, E., & Wargo, E. (2019). Prevention and Treatment of Opioid mIsuse and Addiction: A Review. JAMA Psychiatry, 208-216.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
