Course
Puerto Rico LPN Bundle
Course Highlights
- In this Puerto Rico RN Bundle course, we will learn about the importance of bioethics in nursing practice.
- You’ll also learn how to understand sepsis and the core elements of sepsis treatment and recognition.
- You’ll leave this course with a broader understanding of current research trends in ethics and science.
About
Contact Hours Awarded: 21
Course By:
Various authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Bioethics in Nursing
Introduction
Nursing practice is deeply rooted in ethical principles that guide decision-making and client care. Bioethics is a crucial aspect of healthcare that provides a framework for analyzing ethical dilemmas and promoting individualized client-centered care respectfully and compassionately. Nursing ethics involves applying bioethical principles in practice, such as maintaining client confidentiality and respecting autonomy. Nurses face ethical dilemmas regularly. One of the most common is providing care that conflicts with personal beliefs (6).

Self Quiz
Ask yourself...
- How do you think bioethics influences nursing practice
- What are some examples of ethical dilemmas nurses may face?
- Can you describe a situation where a nurse's personal beliefs conflicted with their professional obligations?
- How would you navigate such a scenario?
Definition and Purpose
Bioethics is the study of ethical and moral principles guiding healthcare decisions and practices (10). Its purpose is to ensure that healthcare providers make informed decisions that respect clients' values, beliefs, and rights (5).
Bioethics provides a framework for analyzing ethical issues in healthcare while considering the interests of the clients, their families, and the healthcare providers involved in their care (5). By understanding the definition and purpose of bioethics, nurses can develop a strong foundation for addressing ethical challenges in practice, such as informed consent, client confidentiality, and when it may infringe upon others’ health and proper resource allocation (5,6,10).


Self Quiz
Ask yourself...
- How does the definition of bioethics impact its application in nursing practice?
- What are some potential consequences of ignoring ethical principles?
- Can you think of a situation where a nurse's understanding of bioethics helped them navigate an ethical dilemma?
- What was the outcome?
Principles of Bioethics
The principles of bioethics include autonomy, beneficence, non-maleficence, and justice (5,6,7,9). Autonomy respects clients' decision-making capacity, beneficence promotes a client's well-being, non-maleficence avoids any harm to the client, and justice ensures fairness and equity for all involved in the client’s care (5,6,9).
These principles serve as the guiding force in nursing practice; influencing the decisions related to client care, research, and policy development (1). Autonomy empowers clients to make informed choices about their care (5,6,9). This may include decisions that the client’s family and even healthcare providers may disagree with personally. Beneficence compels nurses to act in the best interests of their clients and advocate for the client’s desires (5,6,9). Non-maleficence reminds nurses to avoid causing harm; this includes not just physical but emotional and mental harm as well (5,6,9).

Self Quiz
Ask yourself...
- How do the principles of bioethics guide nursing practice?
- What are some examples of how these principles are applied in different healthcare settings?
- Can you describe a situation where a nurse had to balance the principles of autonomy and beneficence in their practice?
- How did they navigate this ethical dilemma?
Types of Ethics and Professions
Different professions have specific ethical guidelines, such as the American Nurses Association (ANA) Code of Ethics for nurses (1). Understanding the ethical framework of various professions is essential to the interdisciplinary healthcare approach.
Interdisciplinary collaboration requires an understanding of diverse ethical perspectives and principles, an approach that coincides with an equally diverse client population. Nurses should be aware of the ethical guidelines that govern their practice and be able to apply them in diverse healthcare settings. They must also be aware of their own beliefs and guidelines and how these may affect their decision-making, adversely affecting client care (5,6).

Self Quiz
Ask yourself...
- How do different professional ethical guidelines impact interdisciplinary collaboration?
- What are some potential consequences of ignoring these guidelines?
- Can you describe a situation where a nurse had to navigate an ethical dilemma with an interdisciplinary team?
Ethics in Nursing
Nursing ethics involves applying principles in practice that benefit the client, healthcare providers, and loved ones of the client. Examples include things such as maintaining client confidentiality and respecting autonomy, helping the client make the right decision for themselves, and advocating for those decisions to others (1,5). One of the most difficult decisions nurses face involves those that conflict with their personal belief system (6).
Nurses must be equipped with the knowledge and skills to navigate these ethical challenges and provide care that respects clients' values and beliefs while also nurturing their thoughts and feelings (6). By exploring bioethics in nursing, we can promote a culture of ethical practice that is compassionate and client-centered.
Henrietta Lacks Story
Henrietta Lacks was a Black tobacco farmer who had her cancer cells taken without her knowledge or consent which led to numerous scientific breakthroughs, including the development of the polio vaccine (7,8). Her story raises important questions about medical ethics, racism, and the intersection of science and human compassion.
In 1951, Henrietta Lacks was diagnosed with cervical cancer and began treatment at Johns Hopkins Hospital in Baltimore. During her treatment, a sample collection of her cancer cells was taken by her doctor, Dr. George Gey without her knowledge and or consent (7,8). Dr. Gey discovered that Henrietta's cells were extraordinary in nature and could be of great value for cancer research and future developments as they could survive and thrive in a laboratory setting thus making them ideal for scientific research.
Henrietta's cells, known as HeLa cells, were soon being used in laboratories worldwide, leading to numerous scientific breakthroughs, including the polio vaccine development, in vitro fertilization, and gene mapping (7,8). However, Henrietta's family was never informed or financially compensated for the use of her cells, and her story remained largely unknown until the publication of Rebecca Skloot's book "The Immortal Life of Henrietta Lacks" in 2010 (2).
Henrietta's story highlights the unethical practices that were common in the medical field at the time, particularly in relation to clients that lacked resources, particularly those belonging to minority groups (2). Her cells were taken without her consent, and she was never compensated or acknowledged for her contribution to science. This raised some very important questions about medical ethics, informed consent, and the exploitation of vulnerable populations.
Still, Henrietta's story is a powerful reminder of the intersection of science and the need for personal autonomy. Her cells have been used to advance scientific knowledge, but they also represent a person, a family, and a community. The use of her cells without her consent or compensation is a violation of her humanity and a reminder of the need for ethical considerations in scientific research.

Self Quiz
Ask yourself...
- How do nursing ethics impact patient care?
- What are some potential consequences of ignoring ethical principles in practice?
- Can you describe a situation where a nurse's understanding of ethics helped them provide high-quality care
- What were the benefits for the patient?
Tuskegee Syphilis Experiments
The Tuskegee Syphilis Study was a highly controversial and unethical medical experiment conducted on African American men in Macon County, Alabama between 1932 and 1972 (4,11). The study, led by the Department of U.S. Public Health Services, involved withholding treatment from hundreds of African American men infected with syphilis despite the availability of effective therapies, to study the natural progression of the disease (4,11).
The men, who were mostly illiterate and poor, were not informed that they had syphilis, their partners were not informed of the disease, nor were they given treatment for the disease (4,11). Instead, they were given placebos and misleading information about their condition. The study continued for 40 years, during which time many of the men died from syphilis-related complications, and many others suffered serious health problems which included the spreading of syphilis to unsuspecting sexual partners.
The Tuskegee Syphilis Study is widely regarded as one of the most unethical medical experiments in history. The study was conducted without the men's knowledge or consent, and it violated basic human rights and principles of medical ethics. By way of public outcry and shock, the awareness of these experiments led to major changes in the way human subjects are protected in medical research and a desire for closer oversight by governing groups.
In 1974, a class-action lawsuit was filed on behalf of the men who were involved in the study, resulting in a multimillion-dollar settlement (11). The study also led to the establishment of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, which developed guidelines for the ethical conduct of research involving human subjects (11).
The Tuskegee Syphilis Study has had a lasting impact on the field of medicine and beyond. It highlighted the importance of informed consent and the need for ethical oversight in the field of medical research. It has also led to the increased scrutiny of medical experiments and a greater emphasis on protecting human subjects, their privacy, and most importantly honest care and explanations of medical conditions and treatments.
Today, the Tuskegee Syphilis Study is remembered as a cautionary tale about the dangers of unethical medical research. It serves as a reminder of the importance of prioritizing the well-being and safety of people and the need for ongoing vigilance in ensuring that medical research is conducted ethically and responsibly, and ensuring there are the proper checks and balances in place to provide the oversight needed.
The study also highlighted the need for diversity in medical research and the importance of including diverse populations in clinical trials (11). It led to increased efforts to address health disparities and to ensure that medical research is conducted in a way that is fair and equitable to all.
In addition, the Tuskegee Syphilis Study led to changes in the way that medical research is regulated and overseen (11). It led to the establishment of institutional review boards (IRBs) and independent ethics committees (IECs) which are responsible for reviewing and approving research protocols and ensuring they meet the ethical standards set in place (11).
Transparency and accountability in medical research have also been placed at the forefront of research since these events took place. Highlighting the importance of disclosing potential conflicts of interest and ensuring research is conducted in a way that is transparent and open to scrutiny; there inevitably was major change and growth that came from this huge medical injustice.
The Tuskegee Syphilis Study was a highly unethical and controversial medical experiment that had a profound impact on the field of medicine and beyond. It highlighted the importance of informed consent, ethical oversight, and diversity in medical research, and led to major changes in the way medical research is conducted and regulated. In these ways, it acted as a catalyst of growth and change in the way the U.S. views and treats research participants. It serves as a reminder of the need for ongoing vigilance in ensuring medical research is conducted ethically and responsibly.
The Tuskegee Syphilis Studies and Henrietta Lacks' cases highlight the importance of informed consent in research.
Other examples include: (5,9)
- Abortion and reproductive rights
- Euthanasia and end-of-life care
- Gene editing and genetic research
- Healthcare access and disparities


Self Quiz
Ask yourself...
- How do bioethical issues like informed consent impact healthcare outcomes
- What are some potential consequences of ignoring these issues?
- Can you describe a situation where a bioethical issue like euthanasia sparked a debate?
- How did healthcare professionals navigate this ethical dilemma?
Research in Ethics
Research ethics involves applying bioethical principles in research (3). Obtaining informed consent and ensuring participant confidentiality are two ways in which the provider can best provide ethical care to those that entrust the healthcare system with their voluntary well-being.
Researchers must be aware of ethical principles that guide research and ensure their studies are conducted ethically and responsibly which puts the client first (3).
Ethical Decision-Making
Ethical decision-making involves critical thinking, moral principles, and professional standards. Nurses can use ethical frameworks, such as the MORAL model and Nursing Process model, to guide decision-making (5). Ethical decision-making is a crucial aspect of nursing practice as it enables nurses to navigate complex healthcare issues and promote clients' well-being.

Self Quiz
Ask yourself...
- How do ethical principles guide research?
- What are some potential consequences of ignoring these principles?
- Can you describe a situation where a researcher had to navigate an ethical dilemma in their study?
Conclusion
Bioethics plays a vital role in nursing practice, ensuring that clients receive respectful and compassionate care. Understanding bioethical principles and applications is essential for nurses to provide high-quality care. By applying ethical principles and frameworks, nurses can navigate complex healthcare issues and promote clients' well-being.

Self Quiz
Ask yourself...
- How does the ethical framework guide decision-making in nursing practice and what are some potential consequences of ignoring these frameworks?
- How do personal values and beliefs impact nursing practice what are the implications for patient care?
- How does the principle of autonomy impact informed consent in healthcare?
- What are some potential consequences of prioritizing beneficence over non-maleficence in healthcare, and how can nurses balance these principles?
- How does the concept of justice impact healthcare resource allocation and what are the implications for nurses and patients?
- How do nurses balance the need for patient confidentiality with the need for transparency?
- What are some potential consequences of ignoring the principle of non-maleficence in healthcare, and how can nurses prioritize patient safety?
- How does the principle of autonomy impact patient decision-making?
- How do nurses balance the need for patient education with the need for autonomy?
- Are there any potential consequences for prioritizing patient satisfaction over patient well-being?
- How does the concept of vulnerability impact healthcare ethics?
- How do nurses balance the need for patient advocacy with the need for patient autonomy?
- What are some potential consequences of ignoring the principle of justice in healthcare?
- How does the principle of beneficence impact healthcare resource allocation?
- How do nurses balance the need for patient education with the need for patient confidentiality?
- What are some potential consequences of prioritizing patient well-being over patient autonomy?
- Could the Henrietta Lacks case and the Tuskegee Syphilis cases have an affect the way minorities view medical treatment in the U.S?
Infection Control and Barriers
Introduction
Healthcare professionals are responsible for adhering to scientifically accepted principles and practices of infection control in all healthcare settings. Healthcare professionals also oversee and monitor those medical and ancillary personnel for whom the professional is responsible, including nurses. The following sections explore the sources and definitions of standards of professional conduct as they apply to infection prevention and control (1,2).
Element I – Infection Control and Prevention Overview
As the largest healthcare workforce in the nation, nurses can positively affect infection rates at the bedside and within healthcare centers. Various agencies, workplaces, institutions, and legislation influence infection control and prevention recommendations, guidelines, and policies. As science and evidence-based research evolves, so does the role of infection control and prevention. It is important to remember that nurses set the stage for infection control and prevention efforts from the patient's point of view, as there was a time when nurses would care for patients without wearing gloves or washing hands. Hand washing, wearing gloves, and using masks are much more commonplace than ever in healthcare (1,2,3).
Implications of Professional Conduct Standards
As healthcare professionals who participate in and supervise patient care, nurses are responsible for knowing the guidelines set by their local, state, and federal legislation and nursing boards.
The responsibility also applies to delegated activities to other healthcare personnel. The nurse must ensure that the five delegation rights are considered when assigning a task to unlicensed assistive personnel (UAP) and that appropriate infection control policies and protocols are followed appropriately. Refer to facility policies and procedures to avoid potentially adverse outcomes (3,4).
Failure to follow the accepted infection prevention and control standards may have serious health consequences for patients and healthcare workers. Hospital-acquired infections (HAI) have increased overall in the past decade in all infections, including central line-associated bloodstream infections (CLABSI), catheter-associated urinary tract infections (CAUTI), ventilator-associated infections, and methicillin-resistant Staphylococcus aureus (MRSA) (5,6). The chain of command should first be utilized when nurses observe incompetent care or unprofessional conduct regarding infection control standards.
Considering the type of misconduct, the infection control violation should be addressed according to facility policy. Charge nurses and managers would be wise to first address the issue with the nurse involved to gather information and address any education deficits. In cases where apparent misconduct is evident, management and workplace facilities should address infection control and prevention efforts. Severe misconduct may result in the loss or revocation of a nursing license. Also, in cases where the neglect to follow appropriate conduct has harmed a patient or coworker, there is potential for professional liability through a malpractice suit brought against the nurse (5,6,7,8,9).
Methods of Compliance
Nurses are responsible for knowing the licensure guidelines, renewal of continuing education, and targeted education in their state(s) of practice. Education on infection control best practices, compliance with local and state requirements, and following facility practices and policies will provide the best protection for self, patients, and staff in preventing and controlling infection during patient care.


Self Quiz
Ask yourself...
- What are the consequences of a one-size-fits-all method for infection prevention?
- What are some infection control and prevention concerns you witness in your current workplace?
- How have infection control and prevention efforts changed throughout your nursing career?
- What is the policy in your workplace for reporting an infection control issue?
- How has infection control evolved in your workplace since the COVID-19 pandemic?
- How could natural disasters, such as hurricanes or tornadoes, influence the spread or development of infectious diseases?
Element II – Modes of Transmission
Modes and mechanisms of transmission of pathogenic organisms in the healthcare setting and strategies for prevention control.
Definitions:
Pathogen or infectious agent: A biological, physical, or chemical agent capable of causing disease. Biological agents may be bacteria, viruses, fungi, protozoa, helminths, or prions.
Portal of entry: How an infectious agent enters the susceptible host.
Portal of exit: The path by which an infectious agent leaves the reservoir.
Reservoir: A place in which an infectious agent can survive but may or may not multiply or cause disease. Healthcare workers may be a reservoir for several nosocomial organisms spread in healthcare settings, allowing an infection to be spread outside of healthcare settings into the general public.
Standard precautions: A group of infection prevention and control measures that combine the significant features of Universal Precautions and Body Substance Isolation and are based on the principle that all blood, body fluids, secretions, excretions except sweat, non-intact skin, and mucous membranes may contain transmissible infectious agents.
Susceptible host: A person or animal not possessing sufficient resistance to a particular infectious agent to prevent contracting infection or disease when exposed.
Transmission: Any mechanism by which a source or reservoir spreads a pathogen to a person.
Standard vehicle: Contaminated material, product, or substance that serves as a means of transmission of an infectious agent from a reservoir to one or more susceptible hosts through a suitable portal of entry (11,12,13).
Component of the Infectious Disease Process
The infectious disease process follows a particular sequence of events commonly described as the chain of infection. Nurses must have a solid understanding of this process to identify points in the chain where the spread of infection may be prevented or halted.
The sequence involves six factors: pathogen, reservoir, portal of exit, portal of entry, mode of transmission, and a susceptible host. The chain's cyclical and consistent nature provides many opportunities to use scientific, evidence-based measures to combat infection spread (11-19).
Pathogens within healthcare are widespread and plentiful, putting patients and healthcare workers at particular risk for contamination. The manifestation of symptoms and mode of transmission varies depending upon the characteristics of the specific infectious agent.
Healthcare workers are at a considerably higher risk for bloodborne pathogens, such as human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV). Influenza, methicillin-resistant Staphylococcus aureus (MRSA), COVID-19, and Tuberculosis (TB) also pose a higher risk and can lead to chronic health damage. Due to the immunocompromised systems of several patients, pathogens cause a considerable risk. They can result in HAIs, such as CLABSIs, CAUTIs, surgical site infections (SSI), and ventilator-associated pneumonia (VAP).
Pathogens require a reservoir, typically a human or animal host; however, they may also be from the environment, such as standing water or a surface. The pathogen is spread from the reservoir via a mechanism such as body fluid, blood, and secretions. Common sites for contact within patient care include the respiratory, genitourinary, and gastrointestinal tracts, as well as skin/mucous membranes, transplacental, or blood. From here, the mechanism must come into contact with another portal of entry. Transmission may occur through respiratory, genitourinary, and gastrointestinal tracts, skin and/or mucous membranes, and parenteral pathways. Some sites may have compromised during patient care due to percutaneous injury, invasive procedures or devices, or surgical incisions.
To acquire a pathogen, a mode of transmission must be provided. Transmission can be from contact, transmission via a standard vehicle, or vector-borne (11-19).
Contact with a pathogen may be categorized as direct, indirect, droplet, or airborne. Contact transmission is through direct or indirect contact with a patient or objects in contact with the patient. Pathogens related to this include Clostridium difficile and multidrug-resistant organisms such as MRSA. Droplet transmission occurs when a pathogen can infect via droplets through the air by talking, sneezing, coughing, or breathing. The pathogen can travel three to six feet from the patient. Airborne transmission occurs when pathogens are 5 micrometers or smaller in size and can be suspended in the air for long periods.
These pathogens include TB, measles, chickenpox, COVID-19 disseminated herpes zoster, and anthrax. Transmission may also occur through a standard vehicle that affects multiple hosts and can come from food, intravenous fluid, medication, biofilms, or shared equipment (fomites), often leading to widespread outbreaks. Vector-borne pathogens are derived from living vectors such as mosquitoes, fleas, or ticks. The last factor in the chain of infection is a susceptible host with a mode of entry. This is why patients are at a much higher risk for developing secondary infections within the healthcare system, even if they had no infection before admission (11-19).

Factors Influencing the Outcome of Exposures
The human body provides several natural defenses against acquiring infection from a pathogen. The most prominent defense is the integumentary system, and the focus should be on maintaining skin integrity to prevent a mode of entry. This is especially true for patients who are immobile or unable to move without assistance, such as those who are post-operative, those with physical disabilities, or those who have extensive nerve damage—respiratory cilia function to move microbes and debris from the airway. Gastric acid is at a pH that prevents the growth of many pathogens. Bodily secretions provide defense through flushing out and preventing back-flow of potential infectious agent colonization. The normal flora within the gastrointestinal system also provides a layer of defense that must be protected from the action of antibiotics. Probiotics are commonly administered to patients on antibiotics to prevent a secondary infection due to disrupted normal flora. Host immunity is the secondary defense that utilizes the host’s immune system to target invasive pathogens. There are four types of host immunity(11-19):
- The inflammatory response is pathogen detection by cells in a compromised area that then elicit an immune response that increases blood flow. This inflammatory provides delivery of phagocytes or white blood cells to the infected site response. Phagocytes are designed to expunge bacteria.
- Cell-mediated immunity uses B-cells and T-cells, specialized phagocytes, which are cytotoxic cells that target pathogens.
- Humoral immunity is derived from serum antibodies produced by plasma cells.
- Immune memory is the immune system's ability to recognize previously encountered antigens of pathogens and effectively initiate a targeted response.
Pathogen or Infection Agent factors
For each type of infectious agent, specific factors determine the risk to the host. Infectivity refers to the number of exposed individuals that become infected. Pathogenicity is the number of infected individuals that develop clinical symptoms, and virulence is the mortality rate of those infected. The probability of an infectious agent causing symptoms depends upon the size of the inoculum (amount of exposure) and the route and duration of exposure. The environment is another factor that warrants attention in limiting the probability of exposure in the healthcare setting. Fomites are materials, surfaces, or objects capable of harboring or transmitting pathogens. Common fomites can be bedside tables, scrubs, gowns, bedding, faucets, and other items in contact with patients and healthcare providers. Equipment may factor into the spread of infection; incredibly portable medical equipment can contact numerous patients daily. This can include vital signs monitoring machines, IV pumps, wheelchairs, and computers on wheels, among countless other care items frequently used. Care must be taken to ensure cleaning in between each patient’s use. For patients in isolation precautions, dedicated equipment for that patient should remain in the room for the duration of their stay (11-17).
Methods to Prevent the Spread of Pathogenic Organisms
Standard Precautions
Standard precautions are the minimal caution and procedure applied to typical patient care. The basis of standard precautions is proper hand hygiene performed by healthcare providers, patients, and visitors. Standard precautions provide guidelines for respiratory hygiene and cough etiquette. As a result of the COVID-19 pandemic and emerging respiratory pathogen resurgence, such as TB and measles, many healthcare facilities are implementing masking for patients and staff, regardless of confirmed case or not, as part of their standard precautions. Hand hygiene must be performed after contact with respiratory secretions or potentially contaminated items. As mentioned, healthcare workers are at a higher risk for bloodborne infections due to the handling of sharps. Needle stick and sharps injuries are reported by healthcare workers in hospitals and outpatient care settings in upwards of 100,00 cases each year. Specific spinal procedures that access the epidural or subdural space provide a means of transmission for infections such as bacterial meningitis (7,8,15-22).
For Patients Infected with Organisms Other Than Bloodborne Pathogens
Special considerations must be given to patient populations infected with organisms other than bloodborne pathogens. A thorough health history should be obtained during the triage of a patient entering a facility. This would include exposure to infectious agents, travel to certain countries, and previous infections resistant to antibiotics (i.e., MRSA, VRE, TB, or carbapenem-resistant Enterobacteriaceae). Patients identified with a risk or history of any of these pathogens may be placed on the appropriate precautions in an isolation room. Infection prevention and the attending physician should be consulted immediately for further orders and treatment (20-22).
Control of Routes of Transmission
Controlling the routes of transmission is a key factor in preventing infection spread. Hand hygiene has been established as the primary prevention method (18).
Care must be taken to follow guidelines for proper hand washing, including:
- Use antibacterial soap and water when hands are visibly soiled or when a Clostridium difficile infection is known or suspected.
- Hands should be gathered. Scrubbing should last at least 20 seconds on all surfaces, between fingers, and under nails.
- Thoroughly rinse the soap from your hands with running water, pat dry with a paper towel, and use a paper towel to turn off the faucet.
- Hand sanitizer, at least 60% alcohol-based, between soap and water may be used.
- A dime-sized amount of hand sanitizer should be rubbed over the surface of hands and fingers and then allowed to air dry.
Barriers to proper hand hygiene include knowledge gaps and the availability of appropriate supplies. Training programs to educate healthcare providers on proper hand washing should be accompanied by ongoing assessment and feedback to ensure compliance.
Incorporating hand hygiene into each nurse's professional development plan is also recommended. Healthcare facilities should diligently ensure that hand washing stations are located in convenient areas and that hand cleaning products are frequently monitored and refilled. Signage and educational materials may be posted in high-traffic areas and at hand washing stations to encourage use by healthcare providers, patients, and visitors. Nurses and healthcare personnel must be aware of the potential of hand hygiene materials as being a potential source of contamination or cross-contamination. Hand hygiene dispensers are touched frequently with contaminated hands and must be often cleaned. It is recommended that the manufacturer's recommendations for cleaning be followed. Hand hygiene systems that allow products to be refilled pose a risk of contaminating the contents. If refilling is a requirement, this should be accomplished using an aseptic technique as much as possible. Facilities should avoid purchasing this product type and move to pre-filled dispensing units, if possible (1-4,18).
Use of Appropriate Barriers
Appropriate barriers are essential in keeping patients and healthcare providers safe from transmitting or contracting pathogens. The type of personal protective equipment (PPE) chosen depends on variables such as patient care, standard, and transmission-based precautions. The minimal amount of PPE recommended are as follows (18,20,21,22,23,24):
- Contact precautions include gloves and gowns. A mask and eye protection are required if bodily secretions may be contacted.
- Droplet precautions require a surgical mask.
- Airborne precautions require wearing gloves, a gown, and an approved N95 respirator mask that has been fit-tested for the individual wearing it. Unfavorable pressure rooms that can filter 6 to 12 air exchanges per hour are also recommended.
Be mindful that these are the minimal recommendations based solely on the identified transmission status of the patient. Selection of PPE should be made using critical thinking to identify potential risks depending on the type of patient care being performed, procedure, behavioral considerations, and other factors that may deviate from the standard. Confirming their infection control and prevention guidelines with your workplace is also essential. The following are current evidence-based recommendations for donning and doffing PPE(18,20,21,22,23,24):
How to Put On (Don) PPE Gear:
More than one donning method may be acceptable. Training and practicing using your healthcare facility’s procedure is critical, as facilities can vary in PPE supply and protocols. Below is one example of donning (18,20,21,22,23,24).
- Identify and gather the proper PPE to wear. Ensure the choice of gown size is correct (based on training).
- Perform hand hygiene using hand sanitizer.
- Put on an isolation gown and tie all of the ties on it. Other healthcare personnel may need assistance.
- Put on NIOSH-approved N95 filtering face-piece respirator or higher (use a facemask if a respirator is unavailable). If the respirator has a nosepiece, it should be fitted to the nose with both hands, not bent or tented. Do not pinch the nosepiece with one hand. The respirator/facemask should be extended under the chin. Both your mouth and nose should be protected. Please do not wear a respirator/facemask under your chin or store it in a scrubs pocket between patients.
- Respirator: Respirator straps should be placed on the crown of the head (top strap) and base of the neck (bottom strap). Perform a user seal check each time you put on the respirator.
- Face mask: Mask ties should be secured on the crown of the head (top tie) and base of the neck (bottom tie). If the mask has loops, hook them appropriately around your ears.
- Put on a face shield or goggles. When wearing an N95 respirator or half-face-piece elastomeric respirator, select the proper eye protection to ensure that the respirator does not interfere with the correct positioning of the eye protection and that the eye protection does not affect the fit or seal of the respirator. Face shields provide full face coverage. Goggles also offer excellent protection for the eyes, but fogging is common.
- Put on gloves. Gloves should cover the cuff (wrist) of the gown.
- Healthcare personnel may now enter the patient’s room.
How to Take Off (Doff) PPE Gear:
More than one doffing method may be acceptable. Training and practicing using your healthcare facility’s procedure is critical. Below is one example of doffing (18,20,21,22,23,24).
- Remove gloves one at a time. Ensure glove removal does not cause additional contamination of hands. Gloves can be removed using multiple techniques, such as the glove-in-glove or bird-beak.
- Remove the gown. Untie all ties (or unsnap all buttons). Some gown ties can be broken rather than untied. Do so gently, avoiding forceful movement. Reach up to the shoulders and carefully pull the gown away from the body. Rolling the gown down is an acceptable approach. Dispose of it in the designated trash receptacle.
- Healthcare personnel may now exit the patient’s room.
- Perform hand hygiene.
- Remove face shields or goggles. Carefully remove them by grabbing the strap and pulling upwards and away from the head. Do not touch the front of your face shield or goggles.
- Remove and discard the respirator (or face mask if used instead of respirator). Do not touch the front of the respirator or face mask.
- Respirator: Remove the bottom strap by touching only it and carefully bringing it over the head. Grasp the top strap, carry it carefully over the head, and then pull the respirator away from the face without touching the front of the respirator.
- Face mask: Carefully untie (or unhook from the ears) and pull away from the face without touching the front.
- If your workplace practices reuse, perform hand hygiene after removing the respirator/face mask and before putting it on again.

Appropriate Isolation/Cohorting of Patients with Communicable Diseases
Co-hosting patients is a common practice within facilities, especially with limited rooms and an increasing number of patients with multidrug-resistant organisms (MDROs). To combat these issues, placing patients with the same type of pathogen in one room when single rooms are unavailable is an option. The minimal standard for all patients is standard precautions (1,2,18,20,21,22,23,24).
Contact: If available, patients with a known or suspected pathogen transmitted via contact should be placed in a private room. Co-horting can be achieved if the co-horted patients share the same type of pathogen.
Droplet: Unless a single patient room is not available, patients in droplet precautions should only be co-horted if neither have an excessive cough or sputum production. The cohorts should be tested to ensure they are infected with the same type of pathogen. Immunocompromised patients are at an increased risk and should not be co-horted. Patients must be separated at least three feet apart, and a privacy curtain should remain between their respective areas. Care providers must don and doff new PPE while caring for each patient. Patients should be given masks to be worn when possible.
Airborne: An airborne infection isolation room (AIIR) with negative air pressure that exchanges air at least six to 12 changes per hour is required. The door must remain closed except for entry and exit. Co-horting of patients is not recommended except in the case of an outbreak or a large number of exposed patients. In these instances, evidence-based guidelines recommend the following:
- Consult infection control professionals before patient placement to determine the safety of alternative rooms that do not meet engineering requirements for AIIR.
- Place together (cohort) patients who are presumed to have the same infection (based on clinical presentation and diagnosis when known) in areas of the facility that are away from other patients, especially patients who are at an increased risk for infection (e.g., immunocompromised patients).
- Use temporary portable solutions (e.g., an exhaust fan) to create a hostile pressure environment in the converted area of the facility. Discharge air directly to the outside, away from people and air intakes, or direct all the air through high-efficiency particulate arresting (HEPA) filters before introducing it to other air spaces.
Host Support and Protection
Vaccinations to prevent disease are highly recommended by numerous health organizations such as the Centers for Disease Control and Prevention (CDC), the World Healthcare Organization (WHO), and several public health departments (1,25-28). As healthcare providers, nurses are positioned to review the patient's history for gaps in appropriate vaccination coverage and educate the patient. Additionally, healthcare providers are ethically responsible for maintaining current vaccinations and can prevent transmitting known communicable diseases by receiving an influenza vaccination each year.
Further evidence suggests that additional boosters for tetanus and pertussis, COVID-19, and measles might benefit several nurses and patients. Pre- and/or post-prophylaxis may be recommended during specific exposures or for patients at an increased risk for infection. This is commonly used for emergent or planned procedures and surgeries that access areas at higher risk for becoming a portal of entry, such as the respiratory, gastrointestinal, and genitourinary tracts. Antibiotics may be ordered when it is known that the sterile field has been broken during a procedure or there has been a concern of contamination of a wound or incision site (1,25-28).
In cases of exposure to an infectious pathogen, the decision to treat includes factors such as the type of exposure, source of the patient's symptoms, time frame since exposure, the health status of the individual exposed, and the risks and benefits of the treatment. Pre-prophylaxis may be considered in the prevention of HIV for high-risk individuals. Typically, after exposure, the host’s blood is drawn to determine pathogen risk regardless of if there is a known pathogen. Based on results, post-exposure prophylactics are given within a short time frame from the exposure. The individual who is exposed will have baseline testing for HIV, HBV, and HCV antibodies. Follow-up testing occurs six weeks, three months, and six months after initial exposure. Maintaining skin and immune system integrity is of the utmost importance to prevent the transmission of infectious pathogens (1,25-28).
Nursing interventions to promote skin and immune system integrity are (6):
- Perform a thorough skin assessment every shift and with changes in condition.
- Accurately document any wounds or incisions
- Use gentle cleansers on the skin and pat dry.
- Use moisturizers and barrier creams on dry or tender skin.
- Prevent pressure ulcer development by turning and repositioning the patient every 2 hours if the patient cannot move independently.
- Maintain aseptic technique during wound care, dressing changes, IV manipulation or blood draws, and catheter care.
- Use neutropenic guidelines when providing care to immunocompromised patients.
- Encourage adequate nutritional and hydration intake.
Environmental Control Measures
The cleaning, disinfection, and sterilization of patient care equipment should be performed per the manufacturer's and facility protocol's recommendations. Cleaning should be performed between each patient encounter. For equipment used in an isolation room, a terminal clean must be performed before being used in other patient care. Environmental cleaning personnel must be educated on the appropriate cleaning for all precautionary patient environments. The Material Safety Data Sheets (MSDS) for all chemicals are to be available to all healthcare personnel for reference as to the proper use and storage. These should be referred to ensure the correct cleaning product is effective in terminally cleaning isolation rooms based on pathogens (17,18,22,25).
Ventilation should be thoroughly managed and maintained by the environmental operations team. Unfavorable pressure rooms should be consistently monitored, and alarms should be investigated to ensure proper air exchange. Concerns from nursing regarding ventilation issues should be directed to the environmental team for follow-up. Regulated medical waste (RMW) within the healthcare system that must follow guidelines for disposal includes (17,18,22,25):
- Human pathological waste
- Human blood and blood products
- Needles and syringes (sharps)
- Microbiological materials (cultures and stocks)
- Other infection waste
Bodily fluid, such as urine, vomit, and feces, may be safely disposed of in any utility sink, drain, toilet, or hopper that drains into a septic tank or sanitary sewer system. Healthcare personnel must don appropriate PPE during disposal. Linen and laundry management in shared health facilities shall (17,18,22,25):
- Provide a sufficient quantity of clean linen to meet the requirements of patients.
- Separately bag or enclose used linens from infectious patients in readily identified containers distinguishable from other laundry.
- Transport and store clean linen in a manner to prevent contamination.
Environment controls include medical devices and systems to isolate or remove the bloodborne pathogens hazard from the workplace. These include sharps disposal containers, self-sheathing needles, and safer medical devices, such as sharps with engineered sharps injury protections and needleless systems. Per facility specifications, continuous training and education should be provided to healthcare personnel on the various methods and modes of environmental control measures that are put in place to prevent and contain pathogen spread (1,2,3).

Self Quiz
Ask yourself...
- How must an organization balance single-use versus reusable, portable medical equipment when considering infectious disease spread?
- What is your workplace's protocol for donning PPE?
- What is your workplace's protocol for doffing PPE?
- What common infections have been reported in your workplace?
- How often do you engage with leadership or management on HAI reduction measures?
- Have you ever cared for a patient with an HAI? How did they react or respond to knowing that they contracted an HAI? What education did you provide to this patient?
- Have you ever "brought home" a work infection? If so, what happened? Did your workplace provide any compensation or assistance?
- What is your workplace's protocol on needlestick and sharps exposure?
- How often do you and other nurses discuss PPE, infection control, and prevention in the workplace?
ELEMENT III – Infection Control in the Workplace
Engineering and work practice controls should be used to reduce the opportunity for patient and healthcare worker exposure to potentially infectious material in all healthcare settings (4-9).
Definitions (4-9)
Healthcare-associated infections (HAIs): Infections associated with healthcare delivery in any setting, such as hospitals, long-term care facilities, ambulatory settings, home care, etc.
Engineering Controls: Controls, such as sharps disposal containers, self-sheathing needles, and safer medical devices, such as sharps with engineered sharps injury protections and needleless systems, can isolate or remove the bloodborne pathogens hazard from the workplace.
Injection safety (or safe injection practices): A set of measures to perform injections optimally safely for patients, healthcare personnel, and others. A safe injection does not harm the recipient, expose the provider to any avoidable risks, and does not result in dangerous waste for the community. Injection safety includes practices intended to prevent transmission of bloodborne pathogens between one patient and another or between a healthcare worker and a patient and to prevent harm such as needlestick injuries. Single-use vials contain only one dose of medication and should only be used once for one patient, using a new sterile needle and a new sterile syringe.
Multidose medication vial: a bottle of liquid medication that contains more than one dose of drugs and is often used by patients with diabetes or for vaccinations.
Work Practice Controls: Controls that reduce the likelihood of exposure to bloodborne pathogens by altering how a task is performed, such as prohibiting the recapping of needles by a two-handed technique).
High-risk Practices and Procedures
Percutaneous exposures are a work hazard within the healthcare industry. Millions of healthcare workers are at risk, with nurses ranking number one. Studies have shown that needlestick injuries occur most frequently within a patient or operating room. Exposures can occur through not following safe practices. The following practices in handling contaminated needles and other sharp objects, including blades, can increase the risk of percutaneous exposure and should be avoided (1,2,3,4,7,17,18,19,22,24,26):
- Manipulating contaminated needles and other sharp objects by hand, such as removing scalpel blades from holders, removing needles from syringes
- Delaying or improperly disposing of sharps, such as leaving contaminated needles or sharp objects on counters/workspaces or disposing in non-puncture-resistant receptacles
- Recapping contaminated needles and other sharp objects using a two-handed technique
- Performing procedures where there is poor visualization, such as:
- Blind suturing
- Non-dominant hand opposing or next to a sharp
- Performing procedures where bone spicules or metal fragments are produced.
Mucous membrane/non-intact skin exposures occur with direct blood or body fluids contact with the eyes, nose, mouth, or other mucous membranes via:
- Contact with contaminated hands.
- Contact with open skin lesions/dermatitis.
- Splashes or sprays of blood or body fluids during irrigation, suctioning, or close contact
Parenteral exposure is subcutaneous (SC), intramuscular (IM), or IV contact with blood or other body fluid. Injection with infectious material may occur during:
- Administration of parenteral medication
- Sharing of blood monitoring devices, such as glucometers, hemoglobinometers, lancets, or lancet platforms/pens
- Infusion of contaminated blood products or fluids
- Human bites, abrasions, or cuts
Unsafe injection practices have resulted in more than 50 outbreaks of infectious disease transmission since 2001. As well, since that time, over 150,000 patients were potentially exposed to HIV, HBV, and HCV solely due to unsafe practices (1,2,3,4,7,17,18,19,22,24,26). These deviations from best practice have resulted in one or more of the following consequences:
- Transmission of bloodborne viruses
- Notification of thousands of patients of possible exposure to bloodborne pathogens and recommendation that they be tested for bloodborne pathogens
- Referral of providers to licensing boards for disciplinary action
- Malpractice suits filed by patients
Pathogens, including HCV, HBV, and HIV, can be present in sufficient quantities to produce infection in the absence of visible blood (26).
- Bacteria and other microbes can be present without clouding or other visible evidence of contamination.
- The absence of visible blood or signs of contamination in a used syringe, IV tubings, multi- or single-dose medication vial, or blood glucose monitoring device does NOT mean the item is free from potentially infectious agents, as many things cannot be seen, with the naked eye.
- All used injection supplies and materials are potentially contaminated and should be discarded.
Proper infection control techniques require that healthcare providers follow best practices to prevent injury and pathogen transfer. Aseptic techniques should always be used to prepare and administer an injection (14,15,17,26). The following are best practice guidelines:
- Medications should be drawn up in a designated “clean” medication area that is not adjacent to areas where potentially contaminated items are placed.
- Use a new sterile syringe and needle to draw up medications while preventing contact between the injection materials and the non-sterile environment.
- Ensure proper hand hygiene before handling medications.
- If a medication vial has been opened, the rubber septum should be disinfected with alcohol before piercing it.
- Never leave a needle or other device inserted into a medication vial septum or IV bag/bottle for multiple uses. This directly routes microorganisms to enter the vial and contaminate the fluid.
- Medication vials should be discarded upon expiration or when concerns arise regarding the medication's sterility.
Never administer medications from the same syringe to more than one patient, even if the needle is changed. Never use the same syringe or needle to administer IV medications to more than one patient, even if the drug is administered into the IV tubing, regardless of the distance from the IV insertion site (14,15,17,26).
- All infusion components are interconnected, from the infusion to the patient's catheter.
- All components are directly or indirectly exposed to the patient's blood and cannot be used for another patient. These components should also be discarded in the appropriate receptacle.
- Syringes and needles intersecting through any IV system port also become contaminated. They cannot be used for another patient or to re-enter a non-patient-specific multidose medication vial.
- Separation from the patient’s IV by distance, gravity, and/or positive infusion pressure does not ensure that small amounts of blood are not present in these items.
- Never enter a vial with a syringe or needle used for a patient if the same medication vial might be used for another patient.
Dedicate medication vials to a single patient, per your workplace's protocols (14,15,17,26), whenever possible.
- Medications packaged as single-use must never be used for more than one patient.
- Never combine leftover contents for later use
- Medications packaged as multiuse should be assigned to a single patient whenever possible.
- Never use bags or bottles of intravenous solution as a standard supply source for more than one patient.
- Never use peripheral capillary blood monitoring devices packaged for single-patient use on multiple patients.
- Restrict the use of peripheral capillary blood sampling devices to individual patients.
- Never reuse lancets. Use single-use lancets that permanently retract upon puncture whenever possible.

Evaluation/Surveillance of Exposure Incidents
A plan to evaluate and follow up on exposure incidents should be implemented at every facility. At a minimum, this plan should include the following elements (1,2,3,6,11,13,14,15):
- Identification of who is at risk for exposure
- Identification of what devices cause exposure
- Identification of areas/settings where exposures occur
- Circumstances by which exposures occur
- Post-exposure management
- Education for all healthcare employees who use sharps. This would include the fact that ALL sharp devices can cause injury and disease transmission if not used and disposed of properly. Specific focus should be on the devices that are more likely to cause injury, such as:
- Devices with higher disease transmission risk (hollow bore) and
- Devices with higher injury rates (“butterfly”-type IV catheters, devices with recoil action)
- Blood glucose monitoring devices (lancet platforms/pens).
Engineer Controls
Engineer controls are implemented to provide healthcare workers with the safest equipment to complete their jobs. Safer devices should be identified and integrated into safety protocols whenever possible. When selecting engineer controls to be aimed at preventing sharps injuries, the following should be considered (1,2,3,6,11,13,14,15):
- Evaluate and choose safer devices
- Passive vs. active safety features
- Mechanisms that provide continuous protection immediately
- Integrated safety equipment vs. accessory devices:
- Properly educate and train all staff on safer devices.
- Consider eliminating traditional or non-safety alternatives whenever possible.
- Explore engineering controls available for specific areas/settings.
- Use puncture-resistant containers for the disposal and transport of needles and other sharp objects:
- Refer to published guidelines for sharps disposal container selection, evaluation, and use (e.g., placement).
- Use splatter shields on medical equipment associated with risk-prone procedures (e.g., locking centrifuge lids).
Work Practice Controls (1,2,3,6,11,13,14,15,17,18)
- General practices:
- Hand hygiene includes the appropriate circumstances in which alcohol-based hand sanitizers, soap, and water hand washing should be used.
- Proper procedures for cleaning blood and body fluid spills
- Initial removal of bulk material followed by disinfection with an appropriate disinfectant.
- Proper handling/disposal of blood and body fluids, including contaminated patient care items.
- Proper selection, donning, doffing, and disposal of PPE as trained
- Adequate protection for work surfaces in direct proximity to patient procedure treatment area with appropriate barriers to prevent instruments from becoming contaminated with bloodborne pathogens
- Preventing percutaneous exposures:
- Avoid unnecessary use of needles and other sharp objects
- Use care in the handling and disposing of needles and other sharp objects:
- Avoid recapping unless medically necessary
- When recapping, use only a one-hand technique or safety device
- Pass sharp instruments using designated “safe zones."
- Disassemble sharp equipment by use of forceps or other devices
- Discard used sharps into a puncture-resistant sharps container immediately after use
Modify Procedures to Avoid Injury (1,2,3,6,11,13,14,15,17,18):
- Use forceps, suture holders, or other instruments for suturing
- Avoid holding tissue with fingers when suturing or cutting
- Avoid leaving exposed sharps of any kind on patient procedure/treatment work surfaces
- Appropriately use safety devices whenever available:
- Always activate safety features
- Never circumvent safety features

Self Quiz
Ask yourself...
- What best practices should always be employed when delivering injections and intravenous medications?
- Have you or a coworker experienced a needlestick injury at work? How was that situation managed?
- What sort of infection surveillance does your workplace use, such as documentation notes, managerial updates, and so on?
- How has what you learned in nursing school changed the infection prevention and control measures you practice in your nursing career?
- Are nurses in your workplace involved in infection surveillance? If so, what is the nurse's role in infection surveillance?
- What role does leadership take in infection surveillance and HAI reduction?
- What is your workplace's policy on multiuse vials?
- How often do you wash your hands during a typical nursing shift? Do you tend to wash your hands more or use hand sanitizer more?
ELEMENT IV – Defining PPE
Selection and use of barriers and/or personal protective equipment for preventing patient and healthcare worker contact with potentially infectious material (19-26).
Definitions
Personal protective equipment (PPE) is specialized clothing or equipment an employee wears to protect against a hazard. PPE is typically for one-time use but can be reused depending on the supply, protocol, and infection prevention measures in place.
Barriers: Equipment such as gloves, gowns, aprons, masks, or protective eyewear can reduce the risk of exposure of the healthcare worker's skin or mucous membranes to potentially infective materials (19-26).
Types of PPE/Barriers and Criteria for Selection
Per OSHA guidelines, employers must provide employees with appropriate PPE that protects them from potential infectious pathogen exposure. PPE includes gloves, coveralls, masks, face shields, and eye protection. All PPE is intended to provide a barrier between the healthcare worker and potential contamination, whether from a patient, object, or surface (19-26).
Gloves are intended to provide coverage and protection for hands. There are several types of gloves, and the kind of patient care or activity should guide choice (19-26).
- Sterile – to be utilized when performing sterile procedures and aseptic technique
- Non-sterile – medical grade, non-sterile gloves may be used for general patient care and clean procedures, such as nasogastric tube insertion
- Utility – not medical grade and should not be used in patient care
The choice of glove material is often dictated by cost and facility preference. When given a choice, considerations should be made regarding the material being handled (19-26).
- Natural rubber latex – rarely used in facilities due to allergen risk
- Vinyl – made from PVC, lower in cost, protects in non-hazardous and low-infection environments
- Nitrile – more durable, able to withstand chemical and bio-medical exposure
An appropriately sized glove fits securely to the fingertips and palm without tightness or extra room. A glove should be replaced immediately if it develops a tear or is heavily soiled.
A cover garb is a protective layer worn over scrubs or clothes to protect garments and skin. Examples include laboratory coats, gowns, and aprons. As with gloves, consideration should be given to size, sterility, the type of patient care involved, and the material characteristics of the gown.
- Fluid impervious – does not allow passage of fluids
- Fluid resistant – resists penetration of fluids, but fluid may seep with pressure
- Permeable – does not offer protection against fluids
Masks protect the wearer’s mouth and nose, with respirators providing an extra layer of protection to the respiratory tract against airborne infection pathogens. Goggles are designed to protect the eyes from splashes and droplet exposure, while face shields offer additional protection to the entire face. It is important to note that face shields are not designed to replace masks (19-26,28). The choice of PPE is based on the factors reasonably anticipated to occur during the patient care encounter. Potential contact with blood or other infectious material can occur via splashes, respiratory droplets, and/or airborne pathogens.
The type of PPE chosen will be based on standard or transmission-based precaution recommendations. Follow your facility policy and procedures for guidance on the appropriate choice. The nurse must also anticipate whether fluid will be encountered, such as emptying a drain or foley collection device. In situations where a large amount of fluid is likely to be experienced, it would be wise to choose a higher level of protection, such as an impermeable gown, if available, and to wear eye protection to ward off splashes (19-26). Choosing Barriers/PPE Based on Intended Need
Barriers and PPE are designed to keep patients and healthcare providers safe. In certain circumstances, specific PPE is selected based on patient care or circumstances (19-26).
Patient Safety
During invasive procedures, such as inserting a central line or during surgery, staff directly involved in performing the procedure or surgery must maintain sterility. Appropriate sterile PPE will be selected based on the type of procedure, and the patient will be draped in a sterile fashion according to recommended guidelines. Patients in droplet precautions pose a significant risk to healthcare workers and visitors. The patient and anyone inside the patient's room should wear a mask for the most effective prevention of transmission (19-26).
Employee Safety
Employees must evaluate the types of exposure that are likely to occur during patient care. Selection of PPE and appropriate barriers should consider the following (19-26,28):
Barriers to contamination prevention (16,19-26,28):
- Standard precautions are to be used with any potential exposure to blood, mucous membranes, compromised skin, contaminated equipment or surfaces, and body fluids. Barriers may include gloves, gowns, and eye and face protection.
- Employees must be judicious in identifying any precautions placed on a patient (e.g., contact, droplet, airborne) and following recommended PPE guidelines to protect themselves and other patients.
- PPE should be donned prior to entering a patient room and doffed upon exit. All gloves must be changed between uses, and hands must be washed or sanitized upon removal of gloves.
- Additionally, social distancing of 6 feet should occur within the work environment whenever possible. When not possible, adherence to mask guidelines is sufficient.
Masks for preventing exposure to communicable diseases (16,19-26,28):
With the onset of COVID-19 across the globe, masks are an essential tool in preventing the transmission of respiratory pathogens. At a minimum, a medical mask must be donned during all patient care, and surgical masks must be utilized during procedures or surgery.
N95 masks are reserved for patient care with known or suspected COVID-19 or other airborne pathogens if airborne precautions are ordered or during procedures that may aerosolize, such as during intubations or specific endoscopy procedures.
Standard N95 respirators are recommended for all other care involving confirmed or suspected Covid-19 patients.
Guidance on Proper Utilization of PPE/Barriers (16,19-26,27,28)
Proper fit is required for PPE to be adequate, as everyone has different body sizes and facial structures that can influence PPE effectiveness. The gowns and gloves chosen should fit well, allow movement, and not be too baggy or too tight. For particulate respirators, all workers required to wear tight-fitting respirators (e.g., N95 respirators, elastomeric) must have a medical evaluation to determine the worker's ability to wear a respirator. If medically cleared, a respirator fit test must be performed using the exact model available in the workplace. Before donning PPE, it should be inspected for anomalies, tears, or vulnerable spots. A compromised PPE should be disposed of, and a new garment should be selected. Nurses must consider the selection of PPE to ensure that it is the correct type for the job and anticipate any circumstances where splashes or fabric saturation is likely to occur. The PPE provided by the employer may be single-use or reusable. Always verify with the manufacturer’s guidelines and facility policy on correctly using and processing worn garments. The facility must ensure that reusable gowns are laundered according to local, state, and federal guidelines.
Healthcare facilities have a legal duty to protect their workers. Employers and healthcare workers must understand the cost versus benefit ratio balance in PPE selection and use. While it is important to be good stewards of resources, always erring on the side of caution and choosing PPE based on anticipated exposure risk is the most effective way to protect healthcare workers and patients.

Self Quiz
Ask yourself...
- How would you handle working at an organization that does not provide sufficient PPE to protect frontline staff?
- What is an example of an acceptable refusal by a healthcare provider to don PPE?
- What do you think causes healthcare providers to forgo established safety measures?
- What other industries are healthcare analogous to when considering the safety of people?
- What are your workplace's policies on PPE?
- Have you ever had to educate a patient on PPE? How was that conversation? What talking points would you address when talking about PPE with a geriatric patient compared to a pediatric patient?
- How involved are nurses in your workplace in PPE use, cost, and distribution?
- If a patient developed an allergic reaction to PPE, how would you handle that situation?
- How can caregivers play a role in a patient's health history?
ELEMENT V – Maintaining a Safe Environment (1,2,3,29)
Create and maintain a safe environment for patient care in all healthcare settings by applying infection control principles and practices for cleaning, disinfection, and sterilization.
Definitions
Contamination: The presence of microorganisms on an item or surface.
Cleaning: The process of removing all foreign material (dirt, body fluids, lubricants) from objects by using water and detergents or soaps and washing or scrubbing the object
Critical device: An item that enters sterile tissue or the vascular system (e.g., IV catheters, needles). These must be sterile before contact with tissue.
Decontamination: The use of physical or chemical means to remove, inactivate, or destroy bloodborne pathogens on a surface or item to the point where they can no longer transmit infectious particles.
Disinfection: The use of a chemical procedure that eliminates virtually all recognized pathogenic microorganisms but not necessarily all microbial forms (bacterial endospores) on inanimate objects.
High-level disinfection: This type of disinfection kills all organisms except high levels of bacterial spores and is affected by a chemical germicide cleared for marketing as a sterilant by the U.S. Food and Drug Administration (FDA).
Intermediate level disinfection: Disinfection that kills mycobacteria, most viruses, and bacteria with a chemical germicide registered as a “tuberculocide” by the U.S. Environmental Protection Agency (EPA).
Low-level disinfection: Disinfection that kills some viruses and bacteria with a chemical germicide registered as a hospital disinfectant by the EPA.
Noncritical device: An item that contacts intact skin but not mucous membranes (e.g., blood pressure cuffs, oximeters). It requires low-level disinfection.
Semi-critical device: An item that comes in contact with mucous membranes or non-intact skin and minimally requires high-level disinfection (e.g., oral thermometers, vaginal specula).
Sterilization: Using a physical or chemical procedure to destroy all microbial life, including highly resistant bacterial endospores.
Universal Principles (1,2,3,29)
Instruments, medical devices, and equipment should be managed and reprocessed according to the recommended and appropriate methods regardless of a patient's diagnosis, except for suspected prion disease cases. Because of the infective nature and steam-resistant properties of prion diseases, special procedures are required for handling brain, spinal, or nerve tissue from patients with known or suspected prion disease, such as Bovine spongiform encephalopathy [BSE].
Consultation with infection control experts before performing procedures on such patients is warranted. Industry guidelines, equipment, and chemical manufacturer recommendations should be used to develop and update reprocessing policies and procedures. Written instructions must be made available for each instrument, medical device, and equipment reprocessed (1,2,3,29).
Potential for Contamination (1,2,3,29)
The type of instrument, medical device, equipment, or environmental surface cause variables more likely to be a source of contamination. The presence of hinges, crevices, or multiple interconnecting pieces may cause external contamination. If able, these devices should be disassembled. Endoscopes provide a particular challenge for internal and external contamination because of their lumens and the crevices and joints present. The disinfectant must reach all surfaces and ensure no air pockets or bubbles impede penetration. As well, these devices may be made of material that is not heat resistant, which prevents the ability to sterilize.
In these instances, chemicals must be utilized to provide disinfection. Once rendered sterile, there are multiple opportunities for potential contamination because of the frequency of hand contact with the device or surface. Packaging may be overhandled and breached. If the item may come into contact with potential contaminants via poor storage, improper opening, or environmental factors, follow facility protocol for sterilization and disinfection. The efficacy of sterilization and disinfection depends on the number and type of microorganisms present. Various pathogens carry an innate resistance, making successful decontamination more challenging. Bacteria, viruses, fungi, protozoa, and prions cause most infections. Because of the nature of their outer membranes, spores, and gram-negative bacteria have a natural barrier that prevents the absorption of disinfectants.
Bacterial spores are incredibly resistant to chemical germicides. The number of microorganisms present on a medical instrument, device, or surface affects the time that must be factored into disinfection and sterilization efficacy (1,2,3,29). Generally, used medical devices are contaminated with a relatively low bioburden of organisms. Inconsistencies or incorrect methods of reprocessing can easily lead to the potential for cross-contamination.
Steps of Reprocessing (1,2,3,29)
Reprocessing medical instruments and equipment is completed sequentially depending on the instrument and chosen process.
Pre-cleaning removes soil, debris, and lubricants from internal and external surfaces through mopping, wiping, or soaking. After use, it must be done as soon as possible to lower the number of microorganisms on the object.
Cleaning may be accomplished manually or mechanically. Manual cleaning relies upon friction and fluidics (fluids under pressure) to remove debris and soil from the instrument's inner and outer surfaces. Several machines are used in mechanical cleaning, including ultrasonic cleaners, washer-disinfectors, washer-sterilizers, and washer-decontaminators.
Disinfection involves using disinfectants, either alone or in combination, to reduce the microbial count to near insignificant. Common disinfectants used in the healthcare setting include chlorine and chlorine compounds, hydrogen peroxide, alcohols, iodophors, and quaternary ammonium compounds. The EPA and FDA formulate and approve these products for specific uses.
Most medical and surgical devices in healthcare facilities are sterilized. This requires sufficient exposure time to heat, chemicals, or gases to ensure that all microorganisms are destroyed.
Choice/Level of reprocessing sequence (1,2,3,29)
The choice or Level of reprocessing is based on the intended use:
- Critical instruments and medical devices require sterilization.
- Semi-critical instruments and medical devices minimally require high-level disinfection.
- Noncritical instruments and medical devices minimally require cleaning and low-level disinfection.
Manufacturer and workplace recommendations must always be consulted to ensure that appropriate methods, actions, and solutions are used. There is a wide variety of compatibility among equipment components, materials, and chemicals. Rigorous training is required to appropriately understand the various equipment heat and pressure tolerance and the time and temperature requirements for reprocessing. Failure to follow the manufacturer or workplace recommendations may lead to equipment damage, elevated instrument microbial counts after reprocessing, increased infection risk, and possibly patient death (1,2,3,29).
Effectiveness of reprocessing instruments, medical devices, and equipment (1,2,3,29)
Pre-cleaning and cleaning before disinfection is one of the most effective ways to reduce the microbial count. This is only effective when completed before disinfection. Disinfection relies upon the action of products to eliminate microbial count. Depending on the medical instrument or device design, the product may only be required to cover the surface.
However, immersion products and dwell times are necessary because of the lumens of scopes, crevices, or hinges on specific instruments. The presence of organic matter, such as blood, serum, exudate, lubricant, or fecal material, can drastically reduce the efficacy of a disinfectant. This may occur because the presence of organic material acts as a barrier. It may also arise from a chemical reaction between the organic material and the disinfectant being utilized.
Biofilms pose a particular challenge and offer protection from the action of disinfectants. Biofilms are composed of microbes that build adhesive layers onto objects' inner and outer surfaces, including instruments and medical devices, rendering certain disinfectants ineffective. Chlorine and Monochloramines remain effective against inactivating biofilm bacteria.
After disinfection, staff and management must adopt a system of record keeping and tracking of instrument usage and reprocessing. Reprocessing equipment must be maintained and regularly cleaned on a schedule, according to the manufacturer’s guidelines. There are several methods of sterilization, such as steam sterilization (autoclaves), flash sterilization, and, more recently, low-temperature sterilization techniques created for medical devices that are heat sensitive.
Selection depends upon the type of instrument, material, ability to withstand heat or humidity, and targeted microbes. There are several methods of ensuring that sterilized instruments are processed and tracked appropriately. Indicators or monitors are test systems that verify that the sterilization methods were sufficient to eradicate the regulated number of microbes during the process. These safeguards include (1,2,3,29):
- Biologic monitors
- Process monitors (tape, indicator strips, etc.)
- Physical monitors (pressure, temperature gauges)
- Record keeping and recall/ tracking system for each sterilization processing batch/item
The best practice of handling and storing reprocessed medical equipment and instruments uses a system of event-related shelf life rather than time-related. The rationale for this lies in the theory that the sterile items remain sterile as long as the packaging is not compromised. Factors considered event-related include internal or external contamination such as damage to the packaging, humidity, insects, vermin, open shelving, temperature fluctuations, flooding, location, and the composition of packaging material. Standards for handling must also focus on protecting workers from health issues (1,2,3,29).
Recognizing Potential Sources of Cross-Contamination in The Healthcare Environment (1,2,3,29)
- Surfaces or equipment that require cleaning between patient procedures/treatments.
- Practices that contribute to hand contamination and the potential for cross-contamination
- Consequences of reuse of single-use/disposable instruments, medical devices, or equipment
Factors That Have Contributed to Contamination in Reported Disease Transmission Cases (1,2,3,29)
In reprocessing or handling equipment, breaks in infection control practices can compromise the integrity of instruments, medical devices, or equipment. Specific factors include:
- Failure to reprocess or dispose of items between patients.
- Inadequate cleaning
- Inadequate disinfection or sterilization
- Contamination of disinfectant or rinse solutions
- Improper packaging, storage, and handling
- Inadequate/inaccurate record keeping of reprocessing requirements.
Expectations Regarding Differing Levels of Disinfection and Sterilization Methods (1,2,3,29)
Professionals who practice in settings where handling, cleaning, and reprocessing equipment, instruments, or medical devices is performed elsewhere (e.g., in a dedicated Sterile Processing Department) are responsible for ensuring understanding of the core concepts and principles (1,2,3,29):
- Standard and Universal Precautions (e.g., wearing of personal protective equipment)
- Cleaning, disinfection, and sterilization
- Appropriate application of safe practices for handling instruments, medical devices, and equipment in the area of professional practice
- Designation and physical separation of patient care areas from cleaning and reprocessing areas
- Verify with those responsible for reprocessing what steps are necessary before submission of pre-cleaning and soaking.
Professionals who have primary or supervisory responsibilities for equipment, instruments, or medical device reprocessing (e.g., Sterile Processing Department staff or clinics and physician practices where medical equipment is reprocessed on-site) are responsible for understanding core concepts and principles (1,2,3,29):
- Standard and Universal Precaution
- Cleaning, disinfection, and sterilization
- Appropriate application of safe practices for handling instruments, medical devices, and equipment in the area of professional practice
- Designation and physical separation of patient care areas from cleaning and reprocessing areas
Facilities must be fastidious in developing appropriate reprocessing practices that follow regulatory guidelines. When selecting relevant methods, consideration must be given to the antimicrobial efficacy, time constraints, and requirements of these methods, as well as compatibility. Compatibility among equipment/materials includes corrosiveness, penetrability, leaching, disintegration, heat tolerance, and moisture sensitivity. The products' toxicity can pose occupational and environmental hazards to staff and patients. Facilities must adopt procedures and policies to reduce exposure to harmful substances, monitor for toxic exposures, and train staff using reprocessing cleaning and chemicals (1,2,3,29).
Other considerations in developing a safety plan for appropriate reprocessing practices include (1,2,3,29):
- Potential for patient/health care worker toxicity/allergy
- Residual effects include antibacterial residual and patient toxicity/allergy.
- Ease of use
- Stability of products, including concentration, potency, efficacy of use, and effects of organic material
- Odor
- Cost
- Monitoring requirements and regulations
- Specific labeling requirements for reprocessing single-use devices


Self Quiz
Ask yourself...
- You are concerned that the sterilized equipment your coworker just opened onto a sterile field was compromised. The coworker assures you it is okay. How would you handle this situation?
- When would it be appropriate for a facility to deviate from the manufacturer’s recommendations in processing medical and surgical equipment?
- Why do you think there is variation in the Level of reprocessing of medical instruments?
- How would you verify that a shelf-stable system does not compromise sterile instruments?
- What sort of training does your workplace offer for contamination protocol and awareness?
- How often are nurses contaminating and disinfecting patient care spaces in your workplace?
- How have trends in a cleaner work environment evolved in your nursing career?
ELEMENT VI – Health Assessment (1,2,3,7,8,11,12)
Prevention and control of infectious and communicable diseases in healthcare workers is essential (1,2,3,7,8,11,12).
Definitions
Infectious Disease: A clinically manifest disease of humans or animals resulting from an infection.
Communicable Disease: An illness due to a specific infectious agent or its toxic products that arises through transmission of that agent from an infected person, animal, or inanimate source to a susceptible host.
Occupational Health Strategies: As applied to infection control, a set of activities intended to assess, prevent, and control infections and communicable diseases in healthcare workers.
Pre-Placement and Periodic Health Assessments
Occupational health strategies are aimed at ensuring employees are healthy and keeping them healthy. Employees should undergo an initial health screening that reviews immunization records upon hiring. Examples include (1,2,3,7,8,11,12):
- Immunity to vaccine-preventable diseases, such as measles, mumps, rubella, varicella, HBV, influenza, and other recommended or mandated requirements.
- Personalized health counseling.
- Thorough history and physical.
Tuberculosis (TB) screening should be completed before a new employee provides patient care and upon possible exposure for an existing employee. A thorough assessment should include an evaluation of the following symptoms (1,2,3,7,8,11,12):
- Fever
- Cough
- Chest pain, or pain with breathing or coughing
- Night sweats
- Chills
A Mantoux tuberculin skin test (TST) must also be completed. The test is performed by injecting a small amount of tuberculin into the epidermis of the forearm. The test is then evaluated for a reaction in 48 to 72 hours. If there is no reaction, the test result is negative. If reactive, a scale is used to interpret the measurement of induration and to direct further testing or treatment. Nursing staff must be healthy to provide optimal care when working in healthcare. This is especially true in caring for vulnerable patients with weakened immune symptoms.
The following symptoms require immediate evaluation by a licensed medical professional:
- Fever
- Cough
- Rash
- Vesicular lesions
- Draining wounds
- Vomiting
- Diarrhea
Upon evaluation, restrictions on patient care activities may be imposed, and work clearance must be completed prior to return (1,2,3,7,8,11,12).
Management Strategies for Potentially Communicable Conditions (1,2,3,7,8,11,12)
Management and the infection prevention department should collaborate and strategize to ensure that employees who have had an exposure or possible exposure are protected and supported in seeking treatment without fear of retaliation or job loss. Managerial support should prioritize (1,2,3,7,8,11,12):
- Appropriate evaluation and treatment
- Limiting contact with susceptible patients and staff
- Placement in a non-clinical setting
- Depending on the severity of symptoms or potential transmission, a furlough may be necessary until no symptoms are present.
Prevention and Control Strategies for Bloodborne Pathogen Transmission (1,2,3,7,8,11,12,22)
Robust training and educational programs are essential for preventing healthcare worker exposure and transmission. Prevention strategies should include education, training, and availability of the following (1,2,3,7,8,11,12,22):
- Information on potential agents, such as HBV, HCV, and HIV
- HBV vaccination (including safety, efficacy, components, and recommendations for use)
- Hand hygiene
- Appropriate PPE and barrier precautions
- Sharps safety
- Standard and universal Precautions
- Education on the availability of confidential and anonymous testing for bloodborne pathogens
Post-Exposure Evaluation and Management (1,2,3,7,8,11,12,22)
Each facility must plan for post-exposure evaluation and management if any employee or patient experiences a potential or actual bloodborne exposure. The plan should incorporate the following (1,2,3,7,8,11,12,22):
- Prompt evaluation by a licensed medical professional.
- Risk assessment in occupational exposures.
- Recommendations for approaching source patient and healthcare worker evaluations.
- Recommendations for post-exposure prophylaxis emphasizing the most current public health guidelines.
- Post-exposure management of patients or other healthcare workers when the exposure source is a healthcare worker obligates the patient to be informed of the type of exposure, whether it is the healthcare worker’s blood or other potentially infectious material.
Airborne or droplet pathogens require several special considerations. The above guidelines should be applied appropriately. Reporting of suspected or confirmed communicable diseases is mandated under various laws. The primary responsibility for reporting rests with the physician; laboratories, school nurses, daycare center directors, nursing homes/hospitals, and state institutions or other locations providing health services are also required to report(1,2,3,7,8,11,12,22).
All patients and healthcare workers who have been potentially exposed to any pathogens should be educated and counseled about (1,2,3,7,8,11,12,22):
- Risk of exposure or illness
- Testing
- Options for and risks and benefits of post-exposure prophylaxis or treatment
- Need for specialty care
- Follow-up testing and treatment
- Work restrictions, if indicated
- Risk of transmitting infections to others and methods to prevent transmission
- Signs and symptoms of illness to report after exposure, including side effects such as prophylaxis
Evaluation of Healthcare Workers Infected with Bloodborne Pathogens (1,2,3,7,8,11,12,22)
The following rules and recommendations are based on scientific evidence-based practice about policies to prevent infected healthcare personnel-related bloodborne pathogen transmission (HIV, HBV, HCV)(1,2,3,7,8,11,12,22) :
- Strict adherence to standard precautions
- Voluntary testing without fear of disclosure or discrimination
- Mandatory screening for bloodborne pathogens is not recommended. Such a program would cost millions of dollars and not produce any appreciable gain in public safety. Negative antibody tests for HIV, HBV, and HCV do not rule out the presence of infection since it can take some time for measurable antibodies to appear.
- Employer notification of a bloodborne pathogen is not a requirement for employment.
Criteria must be followed when evaluating infected healthcare workers for the risk of transmission to adhere to laws protecting workers from discrimination and disability laws. The following outlines a general assessment to determine the risks posed (1,2,3,7,8,11,12,22):
- Nature and scope of professional practice
- Techniques used in the performance of procedures may pose a transmission risk to patients
- Assessed compliance with infection control standards.
- Presence of weeping dermatitis, draining, or open skin wounds
- Ability to carry out duties with cognitive status examination.
Expert Panels for Evaluating Healthcare Workers Infected with Bloodborne Pathogens (1,2,3,7,8,11,12,22)
Upon request, a bloodborne pathogen-infected healthcare worker may seek advice from the local health department regarding potential risk during patient care of bloodborne disease transmission. A state advisory panel would convene with, at minimum, representation by a state or local public officer, an epidemiologist, and an infectious disease expert (1,2,3,7,8,11,12,22).

Self Quiz
Ask yourself...
- What are your thoughts on a proposal to test all healthcare workers for bloodborne illness before licensing?
- Should nurses caring for vulnerable patients require health screenings before patient care?
- A colleague confides in you that they are concerned they may have been exposed to HCV but are wary of being tested. What options are available to support the colleague and protect patients?
- Who should be responsible for providing post-exposure prophylaxis to potentially infectious material when the employee is not following regulated guidelines for care delivery?
- What is your workplace's policy on post-exposure management?
- How can technology be used to track and inform patients and nurses of post-exposure management?
- What common infectious diseases have you seen or encountered in your workplace recently?
ELEMENT VII – Sepsis Awareness (1,30)
Sepsis is a life-threatening condition caused by a host’s extreme response to infection. Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection. Septic shock is a subset of sepsis that manifests with circulatory and cellular/metabolic dysfunction; septic shock is associated with a higher mortality risk (1,30).
Over one million Americans are diagnosed with sepsis each year, and sepsis is a life-threatening medical emergency that requires early recognition and intervention. Sepsis occurs when the body overcompensates in response to an infection, resulting in multiple organ dysfunction and damage. Most sepsis cases are community-acquired. Early recognition and treatment are the most effective ways to combat sepsis.
Bacterial infections commonly trigger sepsis, although other microbial infections (e.g., fungal or viral) can also trigger sepsis. The triggering infection most commonly originates from the lungs, urinary tract, skin, and/or gastrointestinal tract. Specific populations are at an increased risk of developing sepsis, including (1,30):
- Babies (under 1 year) and individuals 65 and older.
- People with chronic conditions such as diabetes, lung disease, kidney disease, or cancer
- People with impaired immune systems.
Early Recognition of Sepsis (1,30)
- Manifestations of sepsis vary based on the type of infection and host factors.
- Some people may have subtle sepsis presentations.
- Signs and symptoms that may be associated with sepsis in persons with confirmed or suspected infection can include:
- Altered mental state
- Shortness of breath
- Fever
- Clammy or sweaty skin
- Extreme pain or discomfort
- High heart rate
Signs and symptoms in children and older adults may not present the same. In children and the elderly, sepsis symptoms may present as above or any of the following: decreased temperature; pallor or bluish tone to the skin; non-blanching rash; high respiratory rate; lethargy; and seizure.
Sepsis can progress to more severe forms, including septic shock. When septic shock occurs, the body's inflammatory response causes extensive vasodilation, which results in a sudden drop in blood pressure that can quickly lead to organ failure and damage. If a person presents with suspected or confirmed infection, healthcare professionals should assess for signs and risk factors for sepsis following facility sepsis protocols (1,30).
Principles of Sepsis Treatment (1,30)
Sepsis treatment starts with prompt recognition and diagnosis. The diagnosis of sepsis starts with assessing a patient with a known or suspected infection. For adults, sepsis is defined as having two or more symptoms of systemic inflammatory response syndrome, which includes (1,30) :
- Temperature (>38 o C or <36 o C)
- Elevated heart rate > 90 bpm
- WBC (<4×109/L or >12×109/L)
- Respiratory rate (>20 breaths/min, PACO2<32 mm Hg
Severe sepsis has traditionally been defined as having sepsis plus organ failure, while septic shock involves sepsis along with refractory hypotension after fluid resuscitation or requiring vasopressors to maintain hemodynamics.
In addition to blood cultures, types and screens may be ordered for urine, wound exudate, or respiratory secretions, depending on where the suspected infection originates. Blood tests may also include a complete blood count and a basic metabolic panel to assess for kidney or liver damage. Other diagnostic imaging may include diagnostic imaging and ultrasounds. Fluid resuscitation and vasopressors, if needed, will continue until the patient is hemodynamically stable. Healthcare providers should be notified when blood cultures result to ensure the ordered antibiotic is effective against the identified organism (1,30).
Patient Education and Prevention (1,30)
Patient education should strive to provide memorable and straightforward ways to stay free of infection. Adequate hand hygiene is the number one method of preventing disease.
Patients at higher risk should be notified of their risk factors, including (1,30):
- Adults 65 or older
- People with chronic medical conditions, such as diabetes, lung disease, cancer, and kidney disease
- People with weakened immune systems
- Sepsis survivors
- Children younger than one
Patients should be encouraged to give relevant history and information to clinicians, including if they have had a recent infection or sepsis or are immunocompromised (1,30).


Self Quiz
Ask yourself...
- A facility has implemented a sepsis screening program; chart reviews indicate inconsistent order sets. What is the best action for the facility to take to improve compliance?
- What are ways that nursing can promote sepsis screening upon admission?
- A unit-based council is preparing education for the public regarding sepsis recognition and prevention. What methods would be most effective in reaching the most vulnerable populations?
- How are sepsis and septic shock interrelated? How does treatment differ for each sequela?
- How would you explain sepsis to a pregnant patient compared to a geriatric patient?
- What is your workplace's policy on sepsis management?
- How does management in your workplace get involved in sepsis management cases?
- How has care for a patient with sepsis evolved in your nursing career?
- What sort of training does your workplace mandate on sepsis education and prevention?
- How can artificial intelligence (AI) and other technology help patients at risk or experiencing sepsis?
- What are some possible complications of sepsis if left untreated?
- What are some infection prevention techniques to educate patients regarding sepsis and bacterial infections?
- How would you assess if a client is progressing on their treatment plan?
- What sort of protocols does your facility have for remote patient monitoring?
- How can nurses educate patients on maintaining their scheduled medication regime?
Hypertension Updates
Introduction
This course aims to provide nurses and healthcare professionals with an up-to-date understanding of hypertension (HTN). The course covers epidemiological evidence, etiology, diagnostic tools, medication management, other interventions, and future research on HTN.
Hypertension, or high blood pressure, is a chronic condition and a significant risk factor for heart disease, stroke, kidney failure, and other serious health problems. The American College of Cardiology defines hypertension as systolic blood pressure greater than 130 mmHg or diastolic blood pressure greater than 80 mmHg [1].
Statistical Evidence/Epidemiology
According to the Centers for Disease Control and Prevention (CDC), hypertension afflicts 108 million Americans and contributes to almost 500,000 deaths per year in the United States [2]. The prevalence of hypertension varies by race and ethnicity, with non-Hispanic Black adults having the highest majority (57.1%), followed by Hispanic adults (43.7%) and non-Hispanic White adults (43.6%).
Hypertension is also more common among older adults, with (74.5%) of adults aged 60 and over having high blood pressure [3]. Despite the high prevalence of hypertension, less than a quarter of all adults with hypertension in the United States have their blood pressure under control [2].
This leaves millions at risk for serious health problems from uncontrolled hypertension, such as heart disease, stroke, kidney failure, and eye problems. In 2021, high blood pressure was a primary or contributing cause of death for more than 691,095 Americans [4].
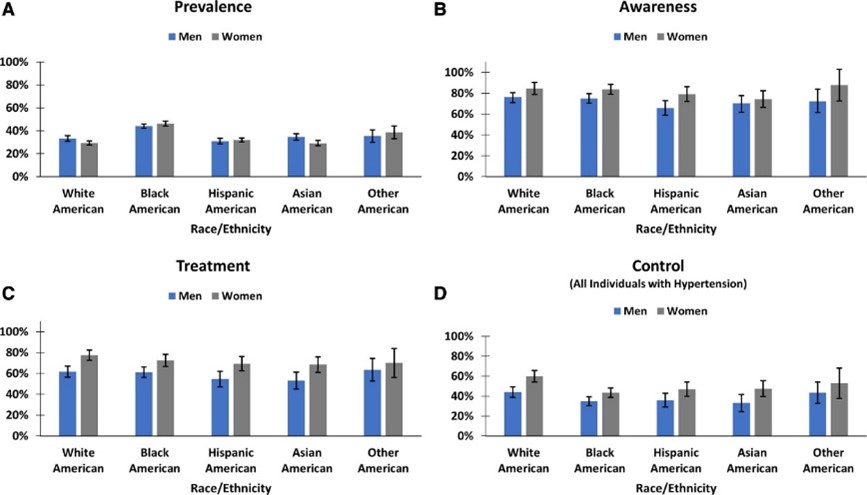
[31]

Self Quiz
Ask yourself...
- How do the current epidemiological statistics about hypertension affect healthcare planning and resource allocation?
- Given that hypertension is a significant public health problem and a major risk factor for serious health problems, what are the essential things that nurses and healthcare professionals should know about hypertension to manage their patients?
- Why do you think there exists such a pronounced disparity in the prevalence of hypertension among different racial and ethnic groups, and what societal and medical strategies might be employed to address this?
Etiology/Pathophysiology of Hypertension
Hypertension (high blood pressure) is a multifactorial disease characterized by persistent elevated blood pressure in the systemic arteries. Understanding hypertension's etiology, pathophysiology, and sequela is crucial for effective management and treatment.
There are two main types of hypertension: primary hypertension and secondary hypertension. Primary or essential hypertension (idiopathic hypertension), which accounts for about 80-95% of all cases, has no identifiable cause and results from complex interactions between genetic, environmental, and other unknown factors [5].
The cause of secondary hypertension (15-30% of cases) is often an underlying medical condition, such as kidney disease, adrenal gland tumors, diabetes, or thyroid disease [6]. Family history plays a role, although science has identified no genetic factor as the "hypertension gene" [7].
A key mechanism in hypertension is the imbalance between the forces that constrict and dilate blood vessels. This imbalance can be caused by several factors, including increased activity of the sympathetic nervous system, which leads to vasoconstriction, increased production of vasoconstrictor hormones, such as angiotensin II and aldosterone, a decreased output of vasodilator hormones, such as nitric oxide, and structural changes in the blood vessels, such as thickening of the vessel walls [8].
The most understood mechanism of hypertension involves increased peripheral vascular resistance due to constriction of small arterioles. The Renin-Angiotensin-Aldosterone System (RAAS) is a hormonal system that regulates blood pressure. Dysfunction of the RAAS can lead to fluid retention and vasoconstriction [9]. Endothelial dysfunction involves the inner lining of the blood vessels (endothelium) and the release of nitric oxide, which promotes blood vessel relaxation. The dysfunction of nitric oxide is a primary contributor to hypertension [10].
Secondary hypertension often involves:
- The kidneys and volume overload.
- Leading to elevated blood pressure.
- Often affecting younger patients and those with resistant or refractory hypertension.
The typical secondary causes of hypertension include:
- Primary aldosteronism (PA).
- Renovascular disease.
- Chronic kidney disease (CKD).
- Obstructive sleep apnea (OSA).
- Drug-induced or alcohol-induced hypertension [11].
Overactivation within the sympathetic nervous system can result in increased heart rate (tachycardia) and vasoconstriction, both of which can cause a temporary elevation in blood pressure. Within the metabolic process, insulin resistance has been associated with endothelial dysfunction and hypertension [12].

Self Quiz
Ask yourself...
- What underlying mechanisms or factors might contribute to the development of primary hypertension when classified as having no identifiable cause, and how might this classification influence our approach to treatment and management?
- What common myths and misconceptions about hypertension have you encountered in your practice?
- How do mechanisms like vascular resistance, RAAS dysfunction, and endothelial dysfunction interact or possibly counteract each other in the pathophysiology of hypertension, and what are the implications of this interplay for targeted therapeutic interventions?
- If hypertension is a complex disease with multiple causes, how can we develop effective treatments and prevention strategies?
Diagnostic and Screening Tools
The primary current diagnostic and screening tools around hypertension include blood pressure measurement. Blood pressure consists of systolic blood pressure (SBP) and diastolic blood pressure (DBP).
SBP is the pressure when the heart is beating, and DBP is the pressure when the heart is resting. A diagnosis of hypertension can be established when the Systolic Blood Pressure (SBP) is 130 mmHg or above or when the Diastolic Blood Pressure (DBP) is at least 80 mmHg [1].
The American Heart Association (AHA) recommends that all adults have their blood pressure checked at least once a year. People with risk factors for hypertension, such as obesity, diabetes, and kidney disease, should have their blood pressure checked more often [13].
Secondary tools for evaluating hypertension include ambulatory blood pressure monitoring (ABPM). ABPM is a more accurate way to measure blood pressure, measuring blood pressure over 24 hours. ABPM is an integral part of hypertensive care [14].
Urine tests can check for protein in the urine, a sign of kidney damage. Kidney damage is a risk factor for hypertension. Blood tests can be used to check for other medical conditions that can cause hypertension, such as diabetes and kidney disease, cholesterol levels, and other risk factors for heart disease.
Hormonal Tests can measure hormones produced by the adrenal and thyroid glands, which can help diagnose secondary hypertension. Regardless of the diagnostic or screening tools, early diagnosis and management of hypertension save lives [15].

Self Quiz
Ask yourself...
- What are the advantages and disadvantages of using blood pressure measurement as the primary diagnostic and screening tool for hypertension?
- What are some of the challenges of implementing ABPM as a routine screening tool for hypertension?
- How can we improve the early diagnosis and management of hypertension in all populations?
Imaging and Other Diagnostic Tests
Ultrasound of the Kidneys: To rule out kidney abnormalities.
Echocardiogram: To assess heart function and structure. Useful if hypertension has been longstanding.
Eye Exam: A fundoscopic examination can reveal changes in the retinal blood vessels, indicative of chronic hypertension.
Telemedicine: Remote monitoring can be helpful for ongoing assessment and titration of treatment.
Healthcare Apps: Smartphone apps can log and track blood pressure readings over time.

Self Quiz
Ask yourself...
- Considering the variety of diagnostic and screening tools available for hypertension—from traditional blood pressure measurements to digital devices like telemedicine and healthcare apps—how can healthcare providers ensure that they employ the most practical combination of methods for accurate diagnosis and long-term management of the condition?
- How does an early diagnosis contribute to better management and prognosis in hypertension patients?
Medication Management
The management of hypertension has evolved over the years, with numerous classes of medications available for treatment. The type of medication best suited for your patients will depend on their needs and health history.
Treatment strategies often begin with monotherapy, a single drug, usually a diuretic, beta-blocker, ACE inhibitor, or Angiotensin II receptor blocker (ARBs) [16]. Combination therapy for patients with stage 2 hypertension or those not reaching the target BP with monotherapy, which may include two or more drug classes, is also used.[16].
Step therapy involves starting with one drug and adding others to achieve the desired effect. A tailored approach is considered if comorbid conditions are present, such as diabetes or heart failure, which may influence drug choice.
Several standard classes of antihypertensive medications are used to treat hypertension, including first-line thiazides such as hydrochlorothiazide, which help rid excess salt and water and lower blood pressure [17]. Angiotensin-converting enzyme (ACE) inhibitors such as lisinopril and ramipril block the production of angiotensin II, a hormone that narrows blood vessels.
Angiotensin II Receptor Blockers (ARBs) such as losartan and valsartan which inhibit the action of angiotensin II, leading to vasodilation [17]. Beta-blockers such as atenolol or metoprolol slow the heart rate and reduce the force of the heart's contractions, which can lower blood pressure [17].
Calcium channel blockers such as amlodipine and diltiazem relax the muscles of the blood vessels by inhibiting the movement of calcium into vascular smooth muscle cells, thus lowering blood pressure [17]. Alpha-blockers such as doxazosin work by blocking alpha-adrenergic receptors, leading to vasodilation. Vasodilators such as hydralazine and minoxidil relax the muscles in blood vessel walls [17].
Central action agents such as clonidine, methyldopa, and moxonidine work on the central nervous system to lower blood pressure [17]. Moxonidine is a new-generation antihypertensive drug that works by activating imidazoline-I1 receptors in the brain, and it may be used when other antihypertensive drugs, such as thiazides, beta-blockers, ACE inhibitors, and calcium channel blockers, are not appropriate or have failed [18].
Thiazide-like diuretics such as chlorthalidone and indapamide have found increased use for their more prolonged duration of action and better cardiovascular outcomes when compared to traditional thiazides [19]. New evidence-based medications are coming into play, such as angiotensin receptor-neprilysin inhibitors (ARNIs), and a clinical trial is underway to test the effectiveness of a new drug called finerenone in preventing heart failure and kidney disease in people with hypertension and diabetes [20] [21].
Due to their safety profiles, there are special considerations with hypertensive management, including methyldopa and labetalol for pregnancy [22].
For older people, care is taken to avoid overtreatment, considering the risks of low blood pressure. For patients with chronic kidney disease (CKD), ACE inhibitors and ARBs are often favored due to their renal protective effects.
Generics are preferred when appropriate to reduce patient costs [23]. Digital adherence tools, including smartphone apps and telemedicine platforms, monitor patient compliance and adjust treatment as necessary.
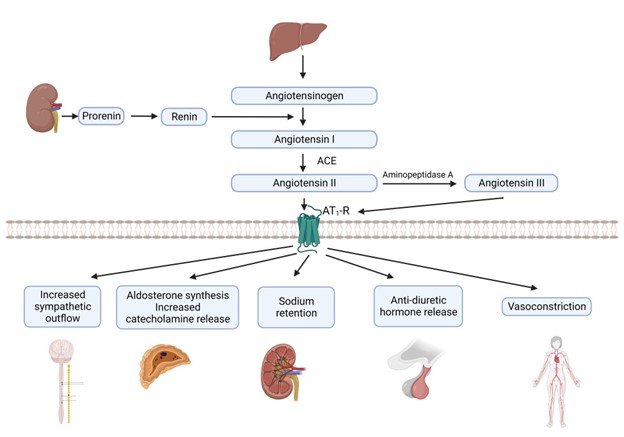
[32]

Self Quiz
Ask yourself...
- What challenges do healthcare providers face in medication compliance among hypertensive patients?
- Given the myriad antihypertensive drug classes and treatment strategies available, coupled with considerations for special populations such as pregnant women, older adults, and those with chronic kidney disease, how can healthcare providers effectively customize treatment plans while maintaining a consistent standard of care across different patient profiles?
Other Interventions
Beyond medication, lifestyle changes, including dietary interventions like the DASH diet and exercise, have proven effective in managing hypertension [24]. The DASH diet focuses on a high intake of fruits, vegetables, and low-fat dairy foods and is low in saturated and total fat.
A reduction in dietary sodium has been shown to lower blood pressure, with a general recommendation to consume less than 2,300 mg per day, with an ideal limit of 1,500 mg for most adults [24]. Regular aerobic exercise such as walking, jogging, or swimming can lower blood pressure.
Weight loss of even 5-10% can significantly impact reducing blood pressure [25]. Alcohol moderation and smoking cessation can also lead to blood pressure reduction.
Behavioral therapies, including stress management techniques such as deep breathing, meditation, and relaxation exercises, can help reduce short-term spikes in blood pressure. There is some evidence that suggests that Cognitive CBT can be effective in managing hypertension [26].
Biofeedback can help manage stress triggers and measure physiological functions like heart rate and blood pressure [26]. Although evidence is mixed, some studies suggest acupuncture can help lower blood pressure.
Renal denervation is an invasive procedure using radiofrequency energy to destroy kidney nerves contributing to hypertension. Central sleep apnea therapy can treat central sleep apnea and lower blood pressure.
Weight loss surgery can be an effective way to lower blood pressure in people who are obese or overweight. Several stress management techniques, such as yoga, meditation, and deep breathing, can be helpful.
Self-monitoring and regular medical check-ups can ensure that the treatment plan is effective and can be adjusted as needed. Remote consultations can offer more frequent touchpoints for adjustments in treatment plans.
Various mobile applications can help patients track blood pressure readings, medication schedules, and lifestyle changes. Community-based interventions to educate the public about hypertension risks, prevention, and management can be effective.
On a policy level, changes and initiatives that reduce sodium in processed foods can have a broader societal impact [27].

Self Quiz
Ask yourself...
- How do non-pharmacological interventions compare with medication management in terms of effectiveness and patient compliance?
- What roles do genetics and lifestyle factors play in the development of hypertension?
- How might the interactions among genetic factors, diet, obesity, lifestyle choices, and psychological elements contribute to the complex etiology of primary hypertension, and what does this complexity imply for diagnosing and treating secondary hypertension?
Upcoming Research
Using "Omics" genomic, proteomic, and metabolomic data to tailor antihypertensive therapies to individuals' researchers are working to identify the genes that contribute to hypertension and specific genetic markers that can help predict an individual's risk for developing hypertension and their potential response to treatments [28].
This information could be used to create new genetic tests to identify people who are at risk of developing the condition. Personalized medicine seeks to create customized approaches to managing hypertension, which would involve tailoring treatment to the individual's needs and risk factors.
Non-invasive treatments, such as devices worn on the body to deliver medication or stimulate the nerves, may also be effective. Researchers are developing a new type of blood pressure monitor that can be worn on the wrist and measure blood pressure throughout the day.
A study is underway to investigate the use of artificial intelligence to develop personalized treatment plans for people with hypertension. With predictive analytics, AI models are trained to predict hypertension risk and disease progression using large-scale electronic health records [29].
In the area of new therapeutic targets, researchers are looking into novel ways to improve endothelial function and vascular health. Studies into how the gut microbiome may influence blood pressure regulation offer potential for new treatment modalities [30]. Research on how diet interacts with genes within the gut microbiome may affect blood pressure.

Self Quiz
Ask yourself...
- How might advancements in technology and research change the landscape of hypertension management in the next decade?
- How can we balance the potential benefits of personalized medicine for hypertension with the challenges of ensuring that everyone has access to these new treatments?
Awareness and Patient Education
What your patients should know:
- Early diagnosis and treatment of hypertension are essential for preventing complications.
- There are several different types of medications available to treat hypertension.
- Lifestyle changes, such as eating a healthy diet, exercising regularly, and maintaining a healthy weight, can also help to lower blood pressure.
Nurses and healthcare professionals should be aware of the following:
- Nurses and healthcare professionals play a vital role in educating patients about hypertension and helping them manage their condition.
- The latest epidemiological statistics on hypertension, including its prevalence, risk factors, and impact on public health.
- The etiology and pathophysiology of hypertension, including the different types of hypertension and their underlying causes.
- The diagnostic tools used to diagnose hypertension include blood pressure measurement, ambulatory blood pressure monitoring, urine tests, blood tests, and imaging tests.
- The different types of medications available to treat hypertension, as well as their side effects and interactions.
Nurses and healthcare professionals can help patients to manage their hypertension by:
- Educating patients about hypertension and its risks.
- Helping patients develop a treatment plan that includes lifestyle changes and medications.
- Monitoring their blood pressure and adjusting their treatment plan as needed.
- Providing support and encouragement.
By working together, nurses and healthcare professionals can help patients manage their hypertension and reduce their risk of complications.

Self Quiz
Ask yourself...
- What are your key takeaways from this course, and how do you plan to implement these learnings in your clinical practice?
Conclusion
Hypertension is a significant public health problem in the United States and worldwide [1]. It is a chronic condition that can lead to serious health problems like heart disease, stroke, kidney failure, and eye problems. However, despite its complexity, hypertension is manageable with lifestyle changes, medications, and the potential information from future genomic discoveries [25] [17].
GI Bleed: An Introduction
Introduction
Gastrointestinal bleeding (GI Bleed) is an acute and potentially life-threatening condition. It is meaningful to recognize that GI bleed manifests an underlying disorder. Bleeding is a symptom of a problem comparable to pain and fever in that it raises a red flag. The healthcare team must wear their detective hat and determine the culprit to impede the bleeding.
Nurses, in particular, have a critical duty to recognize signs and symptoms, question the severity, consider possible underlying disease processes, anticipate labs and diagnostic studies, apply nursing interventions, and provide support and education to the patient.
Epidemiology
The incidence of Gastrointestinal Bleeding (GIB) is broad and comprises cases of Upper gastrointestinal bleeding (UGIB) and lower gastrointestinal bleeding (LGIB). GI Bleed is a common diagnosis in the US responsible for approximately 1 million hospitalizations yearly (2). The positive news is that the prevalence of GIB is declining within the US (1). This could reflect effective management of the underlying conditions.
Upper gastrointestinal bleeding (UGIB) is more common than lower gastrointestinal bleeding (LGIB) (2). Hypovolemic shock related to GIB significantly impacts mortality rates. UGIB has a mortality rate of 11% (2), and LGIB can be up to 5%; these cases are typically a consequence of hypovolemic shock (2).
Certain risk factors and predispositions impact the prevalence. Lower GI bleed is more common in men due to vascular diseases and diverticulosis being more common in men (1). Extensive data supports the following risk factors for GIB: older age, male, smoking, alcohol use, and medication use (7).
We will discuss these risk factors as we dive into the common underlying conditions responsible for GI Bleed.

Self Quiz
Ask yourself...
- Have you ever cared for a patient with GIB?
- Can you think of reasons GIB is declining in the US?
- Do you have experience with patients with hypovolemic shock?
Etiology/ Pathophysiology
Gastrointestinal (GI) bleeding includes any bleeding within the gastrointestinal tract, from the mouth to the rectum. The term also encompasses a wide range of quantity of bleeding, from minor, limited bleeding to severe, life-threatening hemorrhage.
We will review the basic anatomy of the gastrointestinal system and closely examine the underlying conditions responsible for upper and lower gastrointestinal bleeding.
Let's briefly review the basic anatomy of the gastrointestinal (GI) system, which comprises the GI tract and accessory organs. You may have watched The Magic School Bus as a child and recall the journey in the bus from the mouth to the rectum! Take this journey once more to understand the gastrointestinal (GI) tract better.
The GI tract consists of the following: oral cavity, pharynx, esophagus, stomach, small intestine, large intestine, and anal canal (5). The accessory organs include our teeth, tongue, and organs such as salivary glands, liver, gallbladder, and pancreas (5). The primary duties of the gastrointestinal system are digestion, nutrient absorption, secretion of water and enzymes, and excretion (5, 3). Consider these essential functions and their impact on each other.
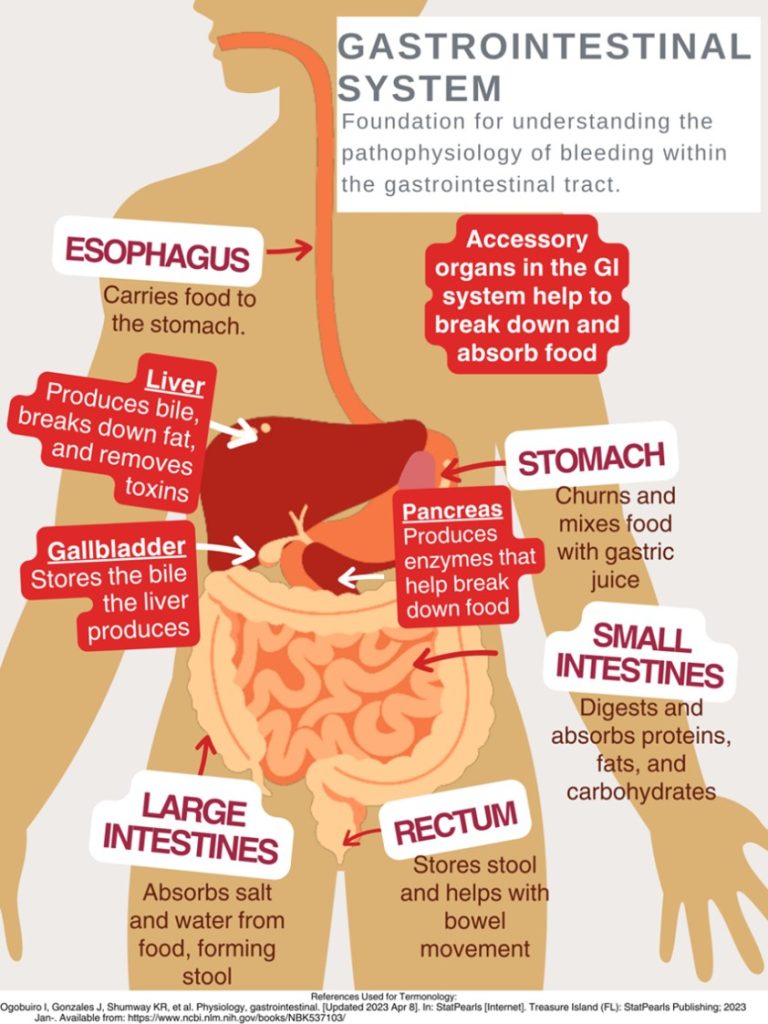
This design was created on Canva.com on August 31, 2023. It is copyrighted by Abbie Schmitt, RN, MSN and may not be reproduced without permission from Nursing CE Central.
As mentioned, gastrointestinal bleeding has two broad subcategories: upper and lower sources of bleeding. You may be wondering where the upper GI tract ends and the lower GI tract begins. The answer is the ligament of Treitz. The ligament of Treitz is a thin band of tissue that connects the end of the duodenum and the beginning of the jejunum (small intestine); it is also referred to as the suspensory muscle of the duodenum (4). This membrane separates the upper and lower GI tract. Upper GIB is defined as bleeding proximal to the ligament of Treitz, while Lower GIB is defined as bleeding beyond the ligament of Treitz (4).
Upper GI Bleeding (UGIB) Etiology
Underlying conditions that may be responsible for the UGIB include:
- Peptic ulcer disease
- Esophagitis
- Foreign body ingestion
- Post-surgical bleeding
- Upper GI tumors
- Gastritis and Duodenitis
- Varices
- Portal hypertensive gastropathy (PHG)
- Angiodysplasia
- Dieulafoy lesion
- Gastric antral valvular ectasia
- Mallory-Weiss tears
- Cameron lesions (bleeding ulcers occurring at the site of a hiatal hernia
- Aortoenteric fistulas
- Hemobilia (bleeding from the biliary tract)
- Hemosuccus pancreaticus (bleeding from the pancreatic duct)
(1, 4, 5, 8. 9)
Pathophysiology of Variceal Bleeding. Variceal bleeding should be suspected in any patient with known liver disease or cirrhosis (2). Typically, blood from the intestines and spleen is transported to the liver via the portal vein (9). The blood flow may be impaired in severe liver scarring (cirrhosis). Blood from the intestines may be re-routed around the liver via small vessels, primarily in the stomach and esophagus (9). Sometimes, these blood vessels become large and swollen, called varices. Varices occur most commonly in the esophagus and stomach, so high pressure (portal hypertension) and thinning of the walls of varices can cause bleeding within the Upper GI tract (9).
Liver Disease + Varices + Portal Hypertension = Recipe for UGIB Disaster
Lower GI Bleeding (LGIB) Etiology
- Diverticulosis
- Post-surgical bleeding
- Angiodysplasia
- Infectious colitis
- Ischemic colitis
- Inflammatory bowel disease
- Colon cancer
- Hemorrhoids
- Anal fissures
- Rectal varices
- Dieulafoy lesion
- Radiation-induced damage
(1, 4, 5, 9)
Unfortunately, a source is identified in only approximately 60% of cases of GIB (8). Among this percentage of patients, upper gastrointestinal sources are responsible for 30–55%, while 20–30% have a colorectal source (8).

Self Quiz
Ask yourself...
- How is the GI Tract subdivided?
- Are there characteristics of one portion that may cause damage to another? (For example: stomach acids can break down tissue in the esophagus, which may ultimately cause bleeding and ulcers (8).
- Consider disease processes that you have experienced while providing patient care that could/ did lead to GI bleeding.
Laboratory and Diagnostic Testing
Esophagogastroduodenoscopy (EGD) and colonoscopy identify the source of bleeding in 80–90% of patients (4). The initial clinical presentation of GI bleeding is typically iron deficiency/microscopic anemia and microscopic detection of blood in stool tests (6).
The following laboratory tests are advised to assist in finding the cause of GI bleeding (2):
- Complete blood count
- Hemoglobin/hematocrit
- International normalized ratio (INR), prothrombin time (PT), and activated partial thromboplastin time (PTT)
- Liver function tests
Low hemoglobin and hematocrit levels result from blood loss, and blood urea nitrogen (BUN) may be elevated due to the GI system's breakdown of proteins within the blood (9).
The following laboratory tests are advised to assist in finding the cause of GI bleeding:
- EGD (esophagogastroduodenoscopy)- Upper GI endoscopy
- Clinicians can visualize the upper GI tract using a camera probe that enters the oral cavity and travels to the duodenum (9)
- Colonoscopy- Lower GI endoscopy/ (9)
- Clinicians can visualize the lower GI tract.
- CT angiography
- Used to identify an actively bleeding vessel
Signs and Symptoms
Clinical signs and symptoms depend on the volume/ rate of blood loss and the location/ source of the bleeding. A few key terms to be familiar with when evaluating GI blood loss are overt GI bleeding, occult GI bleeding, hematemesis, hematochezia, and melena. Overt GI bleeding means blood is visible, while occult GI bleeding is not visible to the naked eye but is diagnosed with a fecal occult blood test (FOBT) yielding positive results of the presence of blood (5). Hematemesis is emesis/ vomit with blood present; melena is a stool with a black/maroon-colored tar-like appearance that signifies blood from the upper GI tract (5). Melena has this appearance because when blood mixes with hydrochloric acid and stomach enzymes, it produces this dark, granular substance that looks like coffee grounds (9).
Mild vs. Severe Bleeding
A patient with mild blood loss may present with weakness and diaphoresis (9). Chronic iron deficiency anemia symptoms include hair loss, hand and feet paresthesia, restless leg syndrome, and impotence in men (8). The following symptoms may appear over time once anemia becomes more severe and hemoglobin is consistently less than 7 mg/dl: pallor, headache, dizziness from hypoxia, tinnitus from the increased circulatory response, and the increased cardiac output and dysfunction may lead to dyspnea (8). Findings of a positive occult GI bleed may be the initial red flag.
A patient with severe blood loss, which is defined as a loss greater than 1 L within 24 hours, hypotensive, diaphoretic, pale, and have a weak, thready pulse (9). Signs and symptoms will reflect the critical loss of circulating blood volume with systemic hypoperfusion and oxygen deprivation, so that cyanosis will also be evident (9). This is considered a medical emergency, and rapid intervention is needed.
Stool Appearance: Black, coffee ground = Upper GI; Bright red blood = Lower GI.

Self Quiz
Ask yourself...
- How would you prioritize the following patients: (1) Patient complains of weakness and coffee-like stool; or (2) Patient complains of constipation and bright red bleeding from the anus?
- Have you ever witnessed a patient in hypovolemic shock? If yes, what symptoms were most pronounced? If not, consider the signs.
- What are ways that the nurse can describe abnormal stool?
History and Physical Assessment
History
A thorough and accurate history and physical assessment is a key part of identifying and managing GI bleed. Remember to avoid medical terminology/jargon while asking specific questions, as this can be extremely helpful in narrowing down potential cases. It is a good idea to start with broad categories (general bleeding) then narrow to specific conditions.
Assess for the following:
- Previous episodes of GI Bleed
- Medical history with contributing factors for potential bleeding sources (e.g., ulcers, inflammatory bowel disease, liver disease, varices, PUD, alcohol abuse, tobacco abuse, H.pylori, diverticulitis) (3)
- Contributory medications (non-steroidal anti-inflammatory drugs (NSAIDs, anticoagulants, antiplatelet agents, bismuth, iron) (3)
- Comorbid diseases that could affect management of GI Bleed (8)
Physical Assessment
- Head to toe and focused Gastrointestinal, Hepatobiliary, Cardiac and Pancreatic
- Assessments
Assess stool for presence of blood (visible) and anticipate orders/ collect specimen for occult blood testing. - Vital Signs
Signs of hemodynamic instability associated with loss of blood volume (3):
- Resting tachycardia
- Orthostatic hypotension
- Supine hypotension
- Abdominal pain (may indicate perforation or ischemia)
- A rectal exam is important for the evaluation of hemorrhoids, anal fissures, or anorectal mass (3)
Certain conditions place patients at higher risk for GI bleed. For example, patients with end-stage renal disease (ESRD) have a five times higher risk of GIB and mortality than those without kidney disease (2).

Self Quiz
Ask yourself...
- Are there specific questions to ask if GIB is suspected?
- What are phrases from the patient that would raise a red flag for GIB (For example: “I had a stomach bleed years ago”)
- Have you ever noted overuse of certain medications in patients?

Self Quiz
Ask yourself...
- Have you ever shadowed or worked in an endoscopy unit?
- Name some ways to explain the procedures to the patient?
Treatment and Interventions
Treatment and interventions for GIB bleed will depend on the severity of the bleeding. Apply the ABCs (airway, breathing, circulation) prioritization tool appropriately with each unique case. Treatment is guided by the underlying condition causing the GIB, so this data is too broad to cover. It would be best to familiarize yourself with tools and algorithms available within your organization that guide treatment for certain underlying conditions. Image 2 is an example of an algorithm used to treat UGIB (8). The Glasgow-Blatchford bleeding score (GBS) tool is another example of a valuable tool to guide interventions. Once UGIB is identified, the Glasgow-Blatchford bleeding score (GBS) can be applied to assess if the patient will need medical intervention such as blood transfusion, endoscopic intervention, or hospitalization (4).
Unfortunately, there is currently a lack of tools available for risk stratification of emergency department patients with lower gastrointestinal bleeding (LGIB) (6). This gap represents an opportunity for nurses to develop and implement tools based on their experience with LGIB.
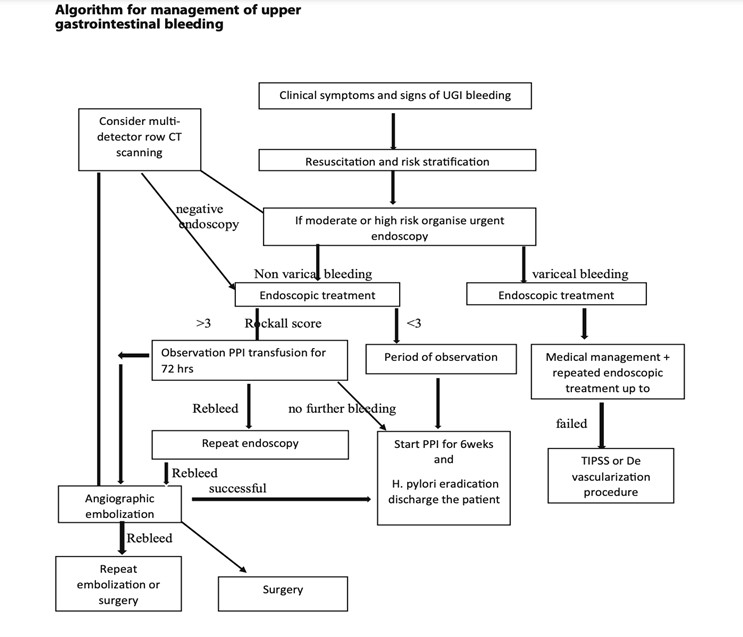
(8)

Self Quiz
Ask yourself...
- Are you familiar with GIB assessment tools?
- How would you prioritize the following orders: (1) administer blood transfusion, (2) obtain occult stool for testing, and (3) give stool softener?
The first step of nursing care is the assessment. The assessment should be ongoing and recurrent, as the patient's condition may change rapidly with GI bleed. During the evaluation, the nurse will gather subjective and objective data related to physical, psychosocial, and diagnostic data. Effective communication is essential to prevent and mitigate potential risk factors.
Subjective Data (Client verbalizes)
- Abdominal pain
- Nausea
- Loss of appetite
- Dizziness
- Weakness
Objective Data (Clinician notes during assessment)
- Hematemesis (vomiting blood)
- Melena (black, tarry stools)
- Hypotension
- Tachycardia
- Pallor
- Cool, clammy skin

Nursing Interventions
Ineffective Tissue Perfusion:
- Monitor vital signs frequently to assess blood pressure, heart rate, and oxygen saturation changes.
- Obtain IV access.
- Administer oxygen as ordered.
- Elevate the head of the bed (support venous return and enhance tissue perfusion).
- Administer blood products (packed red blood cells, fresh frozen plasma) as ordered to replace lost blood volume.
Acute Pain:
- Assess the patient's pain (quantifiable pain scale)
- Administer pain medications as ordered.
- Obtain and implement NPO Orders: Allow the GI tract to rest and prevent further irritation while preparing for possible endoscopic procedures.
- Apply heat/cold therapy for comfort.
Risk for Decreased Cardiac Output
- Assess the patient's heart rate and rhythm. (Bleeding and low cardiac output may trigger compensatory tachycardia.) (9)
- Assess and monitor the patient's complete blood count.
- Assess the patient's BUN level.
- Monitor the patient's urine output.
- Perform hemodynamic monitoring.
- Administer supplemental oxygenation as needed.
- Administer intravenous fluids as ordered.
- Prepare and initiate blood transfusions as ordered.
- Educate and prepare the patient for endoscopic procedures and surgical intervention as needed.
Risk for Deficient Fluid Volume:
- Monitor intake and output.
- Maintain hydration.
- Administer intravenous fluids as ordered.
- Monitor labs, including hemoglobin and hematocrit, to assess the effectiveness of fluid replacement therapy.
- Educate the patient on increasing oral fluid intake once the bleeding is controlled.
- Vital signs
- Assess the patient's level of consciousness and capillary refill time to evaluate tissue perfusion and response to fluid replacement.
- Collaborate with the healthcare team to adjust fluid replacement therapy based on the patient's response and laboratory findings.
Nursing Goals / Outcomes for GI Bleed:
- The patient's vital signs and lab values will stabilize within normal limits.
- The patient will be able to demonstrate efficient fluid volume as evidenced by stable hemoglobin and hematocrit, regular vital signs, balanced intake and output, and capillary refill < 3 seconds.
- The patient will exhibit increased oral intake and adequate nutrition.
- The patient will verbalize relief or control of pain.
- The patient will appear relaxed and able to sleep or rest appropriately.
- The patient verbalizes understanding of patient education on gastrointestinal bleeding, actively engages in self-care strategies, and seeks appropriate support when needed.

Self Quiz
Ask yourself...
- How can the nurse advocate for a patient with GIB?
- Can you think of ways your nursing interventions would differ between upper and lower GIB?
- Have you ever administered blood products?
- What are possible referrals following discharge that would be needed? (Example: gastroenterology, home health care)
Case Study
Mr. Blackstool presents to the emergency department with the following:
CHIEF COMPLAINT: "My stool looked like a ball of black tar this morning."
He also reports feeling "extra tired" and "lightheaded" for 3-5 days.
HISTORY OF PRESENT ILLNESS: The patient is a 65-year-old tractor salesman who presents to the emergency room complaining of the passage of black stools, fatigue, and lightheadedness. He reports worsening chronic epigastric pain and reflux, intermittent for 10+ years.
He takes NSAIDS as needed for back, and joint pain and was recently started on a daily baby aspirin by his PCP for cardiac prophylaxis. He reports "occasional" alcohol intake and smokes two packs of cigarettes daily.
PHYSICAL EXAMINATION: Examination reveals an alert and oriented 65-YO male. He appears anxious and irritated. Vital sips are as follows. Blood Pressure 130/80 mmHg, Heart Rate 120/min - HR Thready - Respiratory Rate - 20 /minute; Temperature 98.0 ENT/SKIN: Facial pallor and cool, moist skin are noted. No telangiectasia of the lips or oral cavity is noted. The parotid glands appear full.
CHEST: Lungs are clear to auscultation and percussion. The cardiac exam reveals a regular rhythm with an S4. No murmur is appreciated. Peripheral pulses are present but are rapid and weak.
ABDOMEN/RECTUM: The waist shows a rounded belly. Bowel sounds are hyperactive. Percussion of the liver is 13 cm (mal); the edge feels firm. Rectal examination revealed a black, tarry stool. No Dupuytren's contractions were noted.
LABORATORY TESTS: Hemoglobin 9gm/dL, Hematocrit 27%, WBC 13,000/mm. PT/PTT - normal. BUN 46mg/dL.
Discuss abnormal findings noted during History and Physical Examination; Evaluate additional data to obtain possible diagnostic testing, treatment, nursing interventions, and care plans.
Conclusion
After this course, I hope you feel more knowledgeable and empowered in caring for patients with Gastrointestinal bleeding (GIB). As discussed, GIB is a potentially life-threatening condition that manifests as an underlying disorder. Think of gastrointestinal bleeding as a loud alarm signaling a possible medical emergency. Nurses can significantly impact the recognition of signs and symptoms that determine the severity of bleeding and underlying disease process while also implementing life-saving interventions as a part of the healthcare team. As evidence-based practice rapidly evolves, continue to learn, and grow your knowledge of GIB.
Constipation Management and Treatment
Introduction
Constipation is more than just an uncomfortable topic—it’s a challenge that nurses encounter very frequently across diverse patient populations. From post-operative recovery to chronic conditions, managing constipation effectively can significantly impact a patient’s comfort, recovery, disease management, and overall quality of life. There is a deeper need for empathy, education, and evidence-based care. This course invites you to dive into the science of managing constipation with knowledge and compassion.
Understanding Constipation
Constipation is a condition characterized by infrequent, difficult, or incomplete bowel movements, often accompanied by hard or dry stools (3). It is one of the most common problems individuals face and occasionally results in emergent issues.
Constipation can be classified as a primary disorder or secondary to many potential causes.
Primary Constipation
Primary constipation is constipation that is not caused by an underlying medical condition, medication, or structural abnormality (8). Essentially, the problem arises from bowel functions rather than from a disease or physical obstruction. Primary constipation is also called idiopathic constipation (3). Causes of primary constipation include dietary, lifestyle, neuromuscular, and psychological factors.
Although primary constipation is not caused by an underlying medical condition, it can significantly affect quality of life. Understanding its types and causes is essential for effective management and improved patient outcomes.
Primary constipation can be considered as (1) functional constipation, in which stool appropriately passes through the colon at a normal rate, or (2) slow transit constipation, where stool passes through the colon at a prolonged, slow rate (3).
Anorectal dysfunction is the inefficient coordination of the pelvic musculature in the evacuation mechanism and is typically an acquired behavioral disorder.
Secondary Constipation
Secondary constipation is due to chronic diseases, certain medications, or anatomic abnormalities (3). The etiology will be further evaluated in an upcoming section.
Epidemiology
Constipation is a common symptom, impacting up to 10% to 20% of the general population (6). The exact prevalence is underestimated because studies show that most patients do not seek out medical care for constipation. The prevalence of chronic constipation is increasing due to changes in diet composition, accelerated pace of life, and the influence of complex social and psychological factors.
Epidemiological surveys have shown that the incidence of chronic constipation is between 14 and 30% worldwide, affecting individuals of all ages, races, socioeconomic status, and nationalities (10). However, certain populations are impacted at higher rates. The rates of constipation increase with age, affecting roughly one-third of individuals over 60 (6). Individuals residing in nursing homes are more commonly reported. Another risk factor is gender, as constipation affects women more than men (7). Recent studies have also noted a two-fold higher rate of constipation among African Americans and those with lower socioeconomic status (income <$20,000 per year) (6).
Social determinants of health (SDOH) are the non-medical factors that impact health outcomes, they encompass the environments in which people are born, grow, live, work, and age, as well as the systems and structures that shape these conditions (9). SDOH significantly impacts health, quality of life, and health disparities across different populations, and research shows a correlation with constipation. These include lifestyle, demographics, education, healthcare access, and adherence to medications (7).

Self Quiz
Ask yourself...
- How would you describe the difference between primary and secondary constipation?
- What populations are more impacted by constipation?
- How can lifestyle, demographics, and education impact overall health?
- Can you discuss the reasons that chronic constipation rates may be increasing?
Pathophysiology
The underlying pathophysiology of constipation varies among different individuals. There are basic mechanical pathophysiological functions, such as the changes in feces once it stays in the rectum for too long and changes in mucous membrane sensitivity and peristalsis if the urge is ignored.
The pathophysiology of constipation can be categorized based on the underlying causes and mechanisms. These categories help identify the specific factors contributing to constipation and guide appropriate interventions. The primary mechanisms are colonic sensorimotor dysfunction and microbiome alteration (10). Factors associated with these mechanisms include gastrointestinal motility and fluid transport, anorectal movement and sensory functions, and dietary and behavioral factors.
Constipation occurs when the fecal mass stays in the rectal cavity for an extended period that is either atypical for the patient or less than three times within a week (5). As the fecal material lingers in the rectum, additional water is absorbed, and the feces becomes smaller, firmer, drier, and more difficult (or painful) to pass.
Another pathophysiological process of constipation can be described by the common saying, “Use it or lose it!”. In this case, when the urge to defecate is ignored, it becomes less recognized. Laxation is the term used for the urge to have a bowel movement (8), so when the urge is ignored, the muscular and rectal mucous membranes become less sensitive to the presence of fecal matter in the rectum (8).
It is important to review gastrointestinal mobility.
Gastrointestinal Motility
Gastrointestinal (GI) motility is the coordinated contractions of the muscles in the gastrointestinal tract for the movement of food and waste products. This process is essential for digestion, absorption of nutrients, and the exit of stool.
Components of GI Motility:
- Peristalsis is the wave-like contractions that move food along the digestive tract.
- Segmental contractions are rhythmic contractions that mix food with digestive enzymes and promote absorption.
- Tonic contractions are sustained muscle contractions that maintain tone in certain areas, such as the sphincters.
Anorectal dyssynergy is a dysfunction of the coordination between the rectal and pelvic floor muscles during defecation. is a common cause of chronic constipation. Normally, defecation involves the relaxation of the anal sphincter and pelvic floor muscles, combined with an increase in intra-abdominal pressure. In anorectal dyssynergy, this process is disrupted, leading to difficulties in stool evacuation despite the presence of normal colonic transit.
Diagnosis is typically made using tests such as anorectal manometry or balloon expulsion tests, and treatment may involve biofeedback therapy, pelvic floor exercises, or other interventions aimed at strengthening the muscles for coordination during defecation.
One prospective study of patients with chronic constipation showed that there was an inability to coordinate the abdominal, rectal, and pelvic floor muscles during defecation. This inability includes impaired rectal contraction, paradoxical anal contraction, or inadequate anal relaxation.
(6)

Self Quiz
Ask yourself...
- What happens to fecal material when it is stored in the rectum for an extended period?
- Can you describe anorectal dyssynergy?
- What are possible reasons the urge to defecate may be ignored?
- Can you explain why gastrointestinal mobility (peristalsis, contraction, etc.) is essential to digestion, absorption of nutrients, and the exit of stool?
Etiology
Constipation can result from a variety of interconnected factors that influence bowel function. Nurses should recognize how the etiology of primary and secondary constipation is different.
Underlying Causes of Primary Constipation
Remember – primary constipation results from irregular bowel functions, not an underlying medical condition or medication. This type of constipation is commonly the cause of daily lifestyle factors. These lifestyle factors can be grouped as dietary and functional.
- Dietary factors
- Low fiber intake
- Lack of nutrient-dense foods
- Inadequate fluid intake
- Irregular eating patterns
- Functional factors
- Low or minimal physical activity
- Ignoring the urge to defecate
- Pain or discomfort with defecation
- Weak abdominal muscles
- Environmental changes or time constraints
- Lack of privacy leads to avoidance of a bowel movement for extended periods.
Underlying Causes of Secondary Constipation
- Endocrine/metabolic disorders
- Hyperparathyroidism
- Diabetes mellitus
- Uremia
- Hypercalcemia
- Hypothyroidism
- Myopathic conditions
- Amyloidosis
- Myotonic dystrophy
- Scleroderma
- Neurologic diseases
- Autonomic neuropathy
- Cerebrovascular disease
- Hirschsprung’s disease
- Multiple sclerosis
- Parkinson’s disease
- Spinal cord injury/tumor
- Psychological conditions
- Anxiety/depression
- Somatization
- Structural abnormalities
- Anal fissure/stricture or hemorrhoid
- Colonic stricture
- Inflammatory bowel disease
- Obstructive colonic mass
- Rectal prolapse or rectocele
- Others
- Irritable bowel syndrome
- Pregnancy
- Medications
- Antacids
- Anticholinergics
- Antidepressants
- Antihistamines
- Calcium channel blockers
- Clonidine
- Diuretics
- Iron
- Narcotics
- NSAIDS
- Opioids
- Psychotropics
- Sympathomimetics
(3)
Signs and Symptoms
The most common symptoms of constipation are abdominal distention and discomfort, indigestion, “rumbling” of the intestinal system, straining during bowel movements, sensation of incomplete emptying, and rectal pressure (8). The description of stool is a key factor in clinical symptomology. The stool will likely be dry, hard, fragmented, and difficult or painful to pass. There may be findings of fresh bleeding (bright red) around the rectum, or protrusions.
Patients may also report fatigue, decreased appetite, and headache (5). There may also be mood changes related to constipation, such as irritability or depression (4).
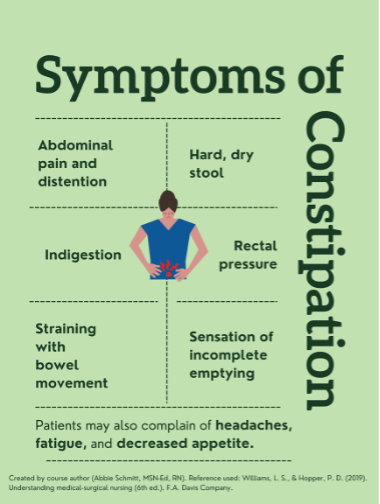
Pharmacological/Non-Pharmacological Treatment
Constipation management encompasses a harmonious blend of pharmacological and non-pharmacological strategies. Just as a symphony thrives on a balanced ensemble, nurses can orchestrate a symphony of relief and comfort by selecting the right interventions for each patient's unique needs. Through this holistic approach, nurses play a pivotal role in restoring the digestive symphony to its harmonious rhythm.
Pharmacological
As nurses step into the realm of constipation management, they encounter a diverse array of strategies that can harmonize the digestive symphony. Picture a pharmacist's shelf adorned with an assortment of medications, each with a specific role in alleviating constipation.
Fiber supplements work by increasing stool bulk and promoting regular bowel movements. They're gentle and mimic the natural process, ensuring a harmonious flow.
Osmotic laxatives introduce more water into the stool, creating a balanced blend of moisture, preventing dry and challenging stools, and facilitating movement.
Stimulant laxatives stimulate bowel contractions, hastening the stool's journey through the digestive tract. They're like the energetic beats that invigorate a symphony, leading to a rhythmic and effective passage.
Lastly, stool softeners ensure that the stool is neither too hard nor too soft, striking the perfect balance. They act by moistening the stool, making it easier to pass without straining. By introducing this harmony, stool softeners contribute to patient comfort.
Non-pharmacological
Beyond the realm of medications lies an equally vital avenue: non-pharmacological interventions. Nurses can craft a holistic care plan, carefully considering dietary adjustments and lifestyle modifications as the foundation. Examples of non-pharmacological interventions include the following:
A diet rich in fiber guides the stool's journey with ease. Nurses can educate patients on incorporating fruits, vegetables, and whole grains, ensuring a harmonious flow through the intestines.
Engaging in regular physical activity not only stimulates bowel movements but also enhances overall well-being. Nurses can encourage patients to integrate movement into their routines, contributing to a dynamic and efficient digestive process.
Relaxation techniques play a vital role in constipation management. Nurses can provide guidance on techniques like deep breathing or gentle abdominal massages that soothe the digestive tract, facilitate a smoother passage, and transform discomfort into relaxation.

Self Quiz
Ask yourself...
- What are the most common symptoms of constipation?
- Can you think of words patients may use to describe abdominal discomfort or indigestion?
- Are you familiar with ways of assessing rectal bleeding?
- What are mood changes that may correlate with constipation?
Assessment
A thorough history and physical examination are essential. Patients may feel uncomfortable or self-conscious when discussing bowel habits. It is important to establish a trusting and comfortable rapport before asking these questions. Providing privacy is meaningful.
Data Collection
- Onset, nature, duration of constipation.
- Past bowel movement patterns
- Current bowel patterns
- Occupation
- Lifestyle habits (nutrition, exercise, stress, coping, support)
- History of laxative or enema use
- Current medication regimen
(8)
Focused Assessment
- Inspect the abdomen for distention and symmetry
- Palpate the abdomen to assess for tenderness or distention.
- Rectal examination may identify anal fissures and hemorrhoids, which can contribute to painful bowel movements.
- Assessment of the anal sphincter tone can provide clues of neurological disorders which may impair sphincter function.
- A digital rectal exam may also reveal a rectal mass or retained stool.
(8)
Labs
- CBC
- BMP: calcium and creatinine levels
- TSH
Endoscopy
- Colonoscopy procedures should follow current guidelines.
- Patients with constipation and “red flag” symptoms of rectal bleeding, heme-positive stool, iron deficiency anemia, weight loss of >10 lbs., obstructive symptoms, or family history of colorectal cancer (3).
Radiography imaging is not especially helpful in underlying etiology, but it may detect stool retention. Barium radiographs may help detect Hirschsprung’s disease. Secondary tests such as anorectal manometry and colonic transit studies can be used to evaluate patients whose constipation is refractory (3).
Diagnosis Criteria
Chronic constipation is usually outlined by clinical symptoms known as the Rome criteria. The Rome IV diagnostic criteria define functional constipation as two or more of the following findings occurring in at least 25% of defecations
- Straining during the bowel movement
- Lumpy or hard stool
- A sensation of incomplete evacuation
- A sensation of anorectal obstruction/blockage
- The use of manual maneuvers to facilitate defecation.
- Loose stools are rare without the use of laxatives
- Having fewer than three spontaneous defecations per week.
The criteria also require these findings to be present for longer than 3 months, with an initial symptom onset of longer than 6 months.
(2,3)

Self Quiz
Ask yourself...
- Can you describe the Roma IV diagnostic criteria for constipation?
- Why are bowel patterns and history important to the assessment of constipation?
Treatment
Nonpharmacologic Treatments
- Bowel training – Encourage patients to attempt a bowel movement in the morning, shortly after awakening, when the bowels are more active, and 30 min after meals to encourage gastrocolic reflex.
- Increase dietary fiber intake
- The recommended intake is 20–35 g daily and an increase of 5 g daily until the recommended daily intake is reached. Increase fiber-rich foods: bran, fruits, vegetables, nuts, and prune juice.
- Psyllium and methylcellulose are the most effective forms of fiber replacement.
- Increase fluid intake – decreased intake may result in fecal impaction
- Regular exercise
- Biofeedback/ pelvic floor retraining – useful for anorectal dysfunction.
(3)
Pharmacologic Treatment
A clinical practice guideline jointly developed by the American Gastroenterological Association (AGA) and the American College of Gastroenterology (ACG) provides evidence-based recommendations for the pharmacological treatment of chronic idiopathic constipation (CIC) in adults (1).
The guidelines provide strong recommendations for the use of polyethylene glycol, sodium picosulfate, linaclotide, plecanatide, and prucalopride based on evidence for effectiveness. Conditional recommendations were given for the use of fiber, lactulose, senna, magnesium oxide, and lubiprostone, emphasizing the need for individualized treatment approaches. The guidelines highlight an individualized approach that considers patient preferences, lifestyle, costs, and medication availability (2).
Types of pharmacological treatments:
- Bulk laxatives – Citrucel and Metamucil absorb water from the intestinal lumen to increase stool mass and soften stool consistency.
- Recommended for patients with functional normal transit constipation.
- Side effects include bloating and increased gas production.
- Emollient laxatives—stool softeners: docusate lowers surface tension, thereby allowing water to more easily enter the bowel.
- Not as effective as bulk laxatives but useful in patients with painful defecation conditions such as hemorrhoids or anal fissures.
- Osmotic laxatives
- Milk of magnesia, magnesium citrate, MiraLAX, and lactulose hyperosmolar agents use osmotic activity to result in the secretion of water into the intestinal lumen.
Precautions:
- Monitor for electrolyte imbalances such as hypokalemia and hypermagnesemia.
- Use with caution in congestive heart failure and chronic renal insufficiency patients.
- Stimulant laxatives: Dulcolax, senna, tegaserod, castor oil, and bisacodyl increase intestinal motility and secretion of water into the bowel.
- Common side effects include abdominal discomfort and cramping as a result of increased peristalsis.
- Contraindicated for patients with suspected bowel obstruction.
(3)
Complications and Negative Impacts on Quality of Life
The most common complications associated with constipation are discomfort and irritation that can lead to:
- Hemorrhoids
- Rectal bleeding
- Anal fissures
Sometimes, the difficulty passing a bowel movement can cause more serious complications, such as:
- Rectal prolapse (the large intestine detaches inside the body and pushes out of the rectum)
- Fecal impaction (hard, dry stool is stuck in the body and unable to be expelled naturally)
Constipation significantly impacts quality of life (QOL), affecting both physical and emotional well-being. Patients with constipation may experience more negative QOL. Studies reported that chronic constipation also causes greater school and work absenteeism and loss of productivity (4).
Nursing Implications and Patient Education
Patient education is an important component of effective constipation management.
Assessment of Knowledge and Baseline Habits
- Assess the patient’s current understanding of constipation and its causes.
- Evaluate dietary habits, fluid intake, physical activity, and medication use that may contribute to constipation.
Provide education on the following:
- Causes and Risk Factors
- Risk factors include low fiber intake, inadequate hydration, lack of physical activity, and certain medications (e.g., opioids, and iron supplements).
- Discuss specific risk factors such as age, medical conditions (e.g., diabetes, hypothyroidism), or recent surgeries.
- Lifestyle Modifications
- Dietary Changes
- Hydration
- Physical Activity
- Healthy Bowel Habits
- Encourage patients to respond promptly to the urge to defecate to avoid hardening of stools and reduced sensitivity.
- Recommend a regular bowel routine, such as attempting bowel movements after meals to take advantage of the gastrocolic reflex.
- Discuss Medication Use
- Advise patients on the appropriate use of laxatives, stool softeners, and other medications for short-term relief.
- Discourage routine use of laxatives and enemas to avoid trauma to the intestinal mucosa, dehydration, and eventual failure of defecation stimulus. (Bulk-adding laxatives are not irritating and are usually permitted.)
- Address Psychological Factors
- Tailor Education to Special Populations
- Encourage Self-Monitoring Log
- Teach patients to track their bowel habits, dietary intake, and hydration levels to identify patterns and triggers.
- Provide Written Materials and Resources
- Offer brochures, handouts, or trusted websites for additional information.
In the inpatient settings, nursing interventions should include:
- Record intake and output accurately to ensure correct fluid replacement therapy.
- Note the color and consistency of stool and frequency of bowel movements to form the basis of an effective treatment plan.
- Promote ample fluid intake, if appropriate, to minimize constipation with increased intestinal fluid content.
- Encourage the patient to increase dietary intake of fiber to improve intestinal muscle tone and promote comfortable elimination.
- Encourage the patient to walk and exercise as much as possible to stimulate intestinal activity.
(Lip)

Self Quiz
Ask yourself...
- Why is it important to discourage patients from overusing laxatives and enemas?
- How can nurses encourage bowel training routines?
- Can you name the major lifestyle modifications that are important in constipation management?
- Are you familiar with fiber-rich foods?
Conclusion
Constipation is a common but complex condition that can significantly impact a person’s quality of life and overall health. Nurses play a meaningful role in identifying, preventing, and managing constipation through comprehensive assessment, evidence-based interventions, and patient education. Understanding the underlying causes and employing tailored strategies can empower patients to take control of their bowel health. This course has provided learners with the knowledge and tools to approach constipation with confidence, compassion, and clinical expertise. Remember that even small changes in habits can lead to meaningful improvements in well-being.

Self Quiz
Ask yourself...
- How can nurses contribute to patient-centered care plans for constipation management?
- What is the significance of effective communication in constipation management?
- Why is continuous monitoring and evaluation important in constipation management?
Conclusion
Constipation is a significant concern that impacts the comfort and well-being of hospitalized and long-term care patients. Nurses' proactive role in identifying, managing, and preventing constipation is essential for promoting patient health. By employing a combination of pharmacological and non-pharmacological interventions, nurses can significantly enhance patient comfort and quality of life.
Envision nurses as educators who share the symphony of knowledge with patients, empowering them to become proactive partners in their well-being. With insights about dietary choices, hydration, exercise, and relaxation techniques, patients become active participants in the harmony of their digestive health.
Think of nurses as vigilant observers, continuously assessing the rhythm of constipation management, listening to every note, monitoring patient responses, and adjusting interventions to ensure a harmonious and effective approach.
Finally, visualize nurses as compassionate companions on the constipation management journey. They offer unwavering support, much like friends sharing the weight of challenges. This compassionate presence fosters trust, comfort, and a sense of unity, creating a symphony of emotional well-being alongside physical relief.
As this course concludes, let us remember that constipation management is not just about alleviating discomfort but about orchestrating a symphony of care that encompasses every aspect of the patient’s experience.
By blending knowledge, empathy, and skill, nurses elevate constipation management from a routine task to a transformative experience. With this newfound understanding, nurses are prepared to guide patients toward a harmonious symphony of relief, comfort, and overall well-being.
Spinal Cord Injury: Bowel and Bladder Management
Introduction
Imagine one day you are able to walk and take care of your own needs. Now, imagine one week later you wake up no longer able to walk, feel anything below your waist, or hold your bowels.
This is a reality for many people who sustain spinal cord injuries. Managing changes in bowel and bladder function is one of many challenges that people with spinal cord injuries and their families or caregivers face.
This course will provide learners with the knowledge needed to assist patients who have spinal cord injuries with bowel and bladder management to improve the quality of life in this group.

Self Quiz
Ask yourself...
- What are some societal misconceptions or stereotypes about people with spinal cord injuries?
- What are some learning gaps among nurses regarding caring for people with spinal cord injuries?
- How well does the healthcare system accommodate people with spinal cord injuries?
Spinal Cord Injuries: The Basics
Spinal Cord Function
Before defining a spinal cord injury, it is important to understand the function of the spinal cord itself. The spinal cord is a structure of the nervous system that is nestled within the vertebrae of the back and helps to distribute information from the brain (messages) to the rest of the body [1].
These messages result in sensation and other neurological functions. While it may be common to primarily associate the nervous system with numbness, tingling, or pain, nerves serve an important purpose in the body’s function as a whole.
Spinal Cord Injury Definition
When the spinal cord is injured, messages from the brain may be limited or entirely blocked from reaching the rest of the body. Spinal cord injuries refer to any damage to the spinal cord caused by trauma or disease [2]. Spinal cord injuries can result in problems with sensation and body movements.
For example, the brain sends messages through the spinal cord to muscles and tissues to help with voluntary and involuntary movements. This includes physical activity like running and exercising, or something as simple as bowel and bladder elimination.
Spinal Cord Injury Causes
Spinal cord injuries occur when the spinal cord or its vertebrae, ligaments, or disks are damaged [3]. While trauma is the most common cause of spinal cord injuries in the U.S., medical conditions are the primary causes in low-income countries [4] [2].
Trauma
- Vehicle accidents: Accounts for 40% of all cases [2]
- Falls: Accounts for 32% of all cases [2]
- Violence: Includes gun violence and assaults; accounts for 13% of all cases [2] [5]
- Sport-related accidents: Accounts for 8% of all cases [2]
Medical Conditions
- Multiple Sclerosis (MS): Damage to the myelin (or insulating cover) of the nerve fibers [1]
- Amyotrophic Lateral Sclerosis (ALS): Lou Gehrig’s disease, damage to the nerve cells that control voluntary muscle movements [1]
- Post-Polio: Damage to the central nervous system caused by a virus [1]
- Spina Bifida: Congenital defect of the neural tube (structure in utero that eventually forms the central nervous system) [1]
- Transverse Myelitis (TM): Inflammation of the spinal cord caused by viruses and bacteria [1]
- Syringomyelia: Cysts within the spinal cord often caused by a congenital brain abnormality [1]
- Brown-Sequard Syndrome (BSS): Lesions in the spinal cord that causes weakness or paralysis on one side of the body and loss of sensation on the other [1]
- Cauda Equina Syndrome: Compression of the nerves in the lower spinal region [1]
Spinal Cord Injury Statistics
According to the World Health Organization, between 250,000 and 500,000 people worldwide are living with spinal cord injuries [4]. In the U.S., this number is estimated to be between 255,000 and 383,000 with 18,000 new cases each year for those with trauma-related spinal cord injuries [6].
Age/Gender
Globally, young adult males (age 20 to 29) and males over the age of 70 are most at risk. In the U.S., males are also at highest risk, and of this group, 43 is the average age [2].
While it is less common for females to acquire a spinal cord injury (2:1 ratio in comparison to males), when they do occur, adolescent females (15-19) and older females (age 60 and over) are most at risk globally [4].
Race/Ethnicity
In the U.S. since 2015, around 56% of spinal cord injuries related to trauma occurred among non-Hispanic whites, 25% among non-Hispanic Black people, and about 14% among Hispanics [6].
Mortality
People with spinal cord injuries are 2 to 5 times more likely to die prematurely than those without these injuries (WHO, 2013). People with spinal cord injuries are also more likely to die within the first year of the injury than in subsequent years. In the U.S., pneumonia, and septicemia – a blood infection – are the top causes of death in patients with spinal cord injuries [6].
Financial Impact
Spinal cord injuries cost the U.S. healthcare system billions each year [6]. Depending on the type, spinal cord injuries can cost from around $430,000 to $1,300,000 in the first year and between $52,000 and $228,000 each subsequent year [6].
These numbers do not account for the extra costs associated with loss of wages and productivity which can reach approximately $89,000 each year [6].

Self Quiz
Ask yourself...
- What is one function of the spinal cord?
- What is one way to prevent spinal cord injuries in any group?
- Why do you think injuries caused by medical conditions are least likely to occur in the U.S.?
- Why do you think the first year of care after the injury is the most costly?
Think about someone you know (or cared for) who had a spinal cord injury.
- Did they have total or partial loss of feeling and movement to the extremities?
- What comorbidities or complications did they have associated with the injury?
- In what ways did the injury affect their overall quality of life?
Spinal Cord Injuries: Types and Complications
Four Levels of the Spinal Cord
- Cervical (vertebrae C1 – C8): Neck; controls the back of the head down to the arms, hands, and diaphragm
- Thoracic (vertebrae T1 – T12): Upper mid-back; controls the chest muscles, many organs, some back muscles, and parts of the abdomen
- Lumbar (vertebrae L1 – L5): Lower back; controls parts of the lower abdomen, lower back, parts of the leg, buttocks, and some of the external genital organs
- Sacral (vertebrae S1 – S5): Lower back; controls the thighs down to the feet, anus, and most of the external genital organs
Types of Spinal Cord Injuries
Spinal cord injuries may be classified by level and degree of impairment. There are four types of spinal cord injuries [5].
Injury Level
- Tetraplegia or Quadriplegia: Injury at the cervical level; loss of feeling or movement to the head, neck, and down. People with this type of spinal cord injury have the most impairment.
- Paraplegia: Injury at the thoracic level or below; limited or complete loss of feeling or movement to the lower part of the body.
Impairment
- Incomplete spinal cord injury: Some sensation and mobility below the level of injury as the spinal cord can still transmit some messages from the brain.
- Complete spinal cord injury: Total loss of all sensation and mobility below the level of injury. Spinal cord injuries of this type have the greatest functional loss.

Spinal Cord Injury Complications
Complications from spinal cord injuries can be physical, mental, or social, and can impact overall quality of life. There are six common complications of spinal cord injuries [2].
Depression
Studies show that 32.9% of adults with disabilities experience frequent mental distress [7]. Mental distress may be related to functional limitations, chronic disease, and the increased need for healthcare services. Up to 37% of people with spinal cord injuries develop depression [2].
Pressure injuries
People with spinal cord injuries may have problems with circulation and skin sensation– both risk factors for pressure injuries. Some may be bedridden or wheelchair-bound which also places them at risk for pressure injuries. Up to 80% of people with spinal cord injuries will have a pressure injury during their lifetime and 30% will have more than one [2].
Spasticity
Around 65% - 78% of people with spinal cord injuries have spasticity [2]. Spasticity is uncontrolled muscle tightening or contraction. The damage from spinal cord injuries causes misfires in the nervous system leading to twitching, jerking, or stiffening of muscles.
Autonomic dysreflexia
In some people with spinal cord injuries, a full bladder or bowel distention can cause a potentially dangerous condition called autonomic dysreflexia. The full bladder or bowel triggers a sudden exaggerated reflex that causes an increase in blood pressure. This condition is also associated with a severe headache, low heart rate, cold skin, and sweating in the lower body [8].
Respiratory problems
If the diaphragm function is affected, as with cervical spinal cord injuries, there may be breathing difficulties. People with lumbar spinal cord injuries can even have respiratory problems as the abdominal muscles are used to breathe.
Sexual problems
Due to changes in muscle function and depending on the degree of damage, people with spinal cord injuries may have problems with arousal and climax due to altered sensations and changes in sexual reflexes.
Changes in bowel and bladder function
Many people with spinal cord injuries lose bowel control. Bowel problems can include constipation, impaction, and incontinence. They may also have problems with urination, for example, urinary retention.

Self Quiz
Ask yourself...
- Why might a person with a disability experience mental distress?
- In what type of spinal cord injury does a person lose all sensation and mobility below the waist?
- Why are people with spinal cord injuries at risk for pressure injuries?
- How can spinal cord injuries affect a person’s personal relationships?
Bowel and Bladder Dysfunction in Spinal Cord Injuries
This section will cover the normal function of the bowel and bladder, and the types of bowel and bladder dysfunction that occurs in patients with spinal cord injuries.


Self Quiz
Ask yourself...
Think about a time you assisted with bowel or bladder management in someone with a spinal cord injury.
- What types of activities were included in their bowel or bladder regimen?
- What challenges did you encounter during bowel or bladder care?
- What difficulties did they express to you about managing their bowel or bladder program?
- In what ways did you assist them in managing their own bowel or bladder program?
Normal Bowel and Bladder Function
In normal bowel and bladder function, when the rectum or bladder fills with stool/urine and presses on area nerves (stimulation), the message is sent to the spinal cord which sends it to the brain. The brain gives the person the “urge” feeling, allowing an option to control the elimination or not.
Whatever decision the person makes, the brain sends the message back to the spinal cord, which in turn sends a message to the elimination muscles (anal and bladder sphincters) to either relax or stay closed until the person is ready. In people with spinal cord injuries, the messages are limited or blocked, leading to problems with bowel and bladder control [9] [10].
Bowel Dysfunction with Spinal Cord Injuries
Reflex hypertonic neurogenic bowel occurs when a rectum full of stool presses against area nerves sending a message to the spinal cord, but it stops there. The message never makes it to the brain, so the person never gets the urge.
As a result, a reflex is set off, prompting the spinal cord to send a message to the anal muscle (sphincter) instead, causing it to relax and release the stool. This condition leads to bowel incontinence and usually occurs in spinal injuries at the cervical and thoracic levels [9] [10].
Flaccid hypotonic bowel occurs when area nerves are also stimulated by a full rectum, but the message does not even reach the spinal cord, so there is no reflex. The anal sphincter is always in a relaxed state.
As a result, the bowels simply empty when they are full, and this can occur at any time without the person having the ability to control it. This condition results in bowel incontinence and can lead to constipation as the patient does not have the urge and may not have the ability to push. This condition usually occurs in spinal injuries at the lumbar level [9] [10].
Bladder Dysfunction with Spinal Cord Injuries
Reflex neurogenic bladder occurs when the bladder automatically starts to contract after filling with a certain amount of urine. The person has no urge to go as the messages are either limited or blocked from reaching the brain, therefore leading to loss of bladder control. Similar to reflex hypertonic neurogenic bowel, the full bladder triggers are nerves that set off a reflex, prompting the spinal cord to send messages to the bladder releasing urine outside of the person’s control [9] [10].
Acontractile bladder occurs when the bladder loses muscle tone after a spinal cord injury, lessening its ability to contract, leading to bladder distention, and dribbling of urine. People with this condition need to use urinary catheters to help empty the bladder [9].


Self Quiz
Ask yourself...
- What is one role of the brain in bowel and bladder function?
- Which type of bowel dysfunction occurs in thoracic-level spinal cord injuries?
- In which type of bowel dysfunction might a suppository be most effective?
- In which type of bladder dysfunction does the bladder lose muscle tone?
The Nurse’s Role in Bowel and Bladder Management
This section will cover how nurses can assess, intervene, and teach when caring for patients with spinal cord injuries who have bowel and bladder dysfunction.

Self Quiz
Ask yourself...
Think about your experiences with patients with spinal cord injuries and their family or caregivers.
-
- How knowledgeable was the patient about their bowel or bladder care?
- In what ways were the family or caregiver involved in the plan of care?
- Did the family or caregiver have any learning gaps that needed to be addressed?
- What difficulties did the family or caregiver express to you about their role?
Nurse Assessments
When caring for patients with spinal cord injuries, nurses should obtain a detailed bowel and bladder history including diet, fluid intake, medications, and elimination patterns/habits [11]. Many of these patients may already manage their own bowel and bladder care at home.
If so, the nurse should obtain the patient’s current regimen and communicate the information to the physician. The physician may choose to continue the regimen or adjust as needed based on the patient’s current illness/condition.
Questions the nurse can ask the patient:
- What does your typical diet consist of?
- How much fluid do you drink on a daily basis?
- How often do you have a bowel movement or urinate?
- Do you schedule your bowel movements with assistance from medications?
- Are there certain body positions or things you do to help you pass stool more easily?
- How often do you use an intermittent urinary catheter for bladder relief?
- How much time do you spend on your bowel and bladder regimens?
- Do you care for all of your elimination needs or does someone help you?
- How does your bowel and bladder dysfunction affect your quality of life?
Some assessments may be observed. For example, nurses may notice that the patient has a surgically placed permanent suprapubic urinary catheter or colostomy (when the bowel is cut somewhere above the level of the rectum and diverted to the outside of the abdomen).
Nurse Interventions
Since many patients with spinal cord injuries have problems with bowel and bladder function, elimination must be scheduled. Nurses can help by implementing bowel and bladder programs and providing education and support to patients, families, or caregivers.
Regimens
Follow the patient’s home bowel and bladder regimen (as ordered). This may include maintaining intermittent catheterization every few hours or administering suppositories daily.
For patients who do not have a regimen already or wish to modify their current one, encourage them to pay attention to how often they urinate and pass stools, elimination problems, foods that alleviate or worsen the problem, and medications or other things that help. This can be done through a diary.
Dietary Considerations
Educate patients on the importance of a fiber-rich diet to avoid constipation. Patients should also be made aware that high-fat foods, spicy foods, and caffeine can alter gut dynamics and lead to bowel incontinence episodes [12].
Fluid Intake
Some patients may avoid drinking enough water to avoid bladder complications (e.g., frequent incontinent episodes) [12]. However, nurses should educate patients on the importance of adequate fluid intake to prevent constipation. Patients should be made aware that bladder and bowel elimination regimens go hand in hand.
Bladder Elimination
For bladder dysfunction, help patients perform intermittent urinary catheterization as needed or place a temporary urinary catheter (as ordered).
Bowel Elimination
For bowel dysfunction, administer ordered suppositories and laxatives to help the bowels move (use suppositories in conjunction with the level of sensation the patient has near the anus/rectum) [9]. Changes in body position may help as well.
While many of these interventions may not work in some patients with spinal cord injuries, bowel irrigation (water enemas) may be helpful [11]. Surgical placement of a colostomy may be indicated if all other measures have failed [11].
Emotional Support
Ensure privacy and sensitivity during all elimination care as patients may experience embarrassment or frustration.
Education for Families or Caregivers
Provide education to families or caregivers on the importance of helping patients stay consistent with their elimination regimen, follow diet and fluid intake recommendations, and comply with medication orders.
Referrals
Inform the physician if interventions are not effective or if the patient, family, or caregiver has a special need (e.g., counselor or dietician). Refer patients and families or caregivers to support groups as needed.
Support Groups and Resources
Christopher and Dana Reeve Foundation
Christopher Reeve – an actor who was left paralyzed after an equestrian accident – and his wife Dana’s legacy lives on through their foundation, an organization that advocates for people living with paralysis [13].
Miami Project to Cure Paralysis
In response to his son, who acquired a spinal cord injury during college football, NFL Hall of Famer Nick Buoniconti and world-renowned neurosurgeon Barth A. Green, M.D. started a research program aimed at finding a cure for paralysis and discovering new treatments for many other neurological injuries and disorders [14].
National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR)
The National Institute on Disability, Independent Living, and Rehabilitation Research, a part of the U.S. Department of Health and Human Services’ Administration for Community Living, helps people with disabilities integrate into society, employment, and independent living [15].
Paralyzed Veterans of America (PVA)
A group of World War II veterans who returned home with spinal cord injuries, started this organization to support those with spinal cord injuries and dysfunction. Today, the organization focuses on quality health care, research and education, benefits, and civil rights to affected veterans [16].
The United Spinal Association supports people with spinal cord injuries and those in wheelchairs. The organization advocates for disability rights like access to healthcare, mobility equipment, public transportation, and community support. Support groups can be found on their website [17).

Self Quiz
Ask yourself...
- What is one question a nurse can ask a patient to obtain a bowel and bladder history?
- How can nurses help patients with spinal cord injuries start or modify a bowel or bladder regimen?
- When might a colostomy be indicated for a patient with a spinal cord injury?
- What type of referral might be ordered for a patient with a spinal cord injury who has bowel or bladder dysfunction?
Conclusion
Spinal cord injuries can have devastating effects on patients and their families. Management of basic bodily functions like bowel and bladder elimination should be made as easy as possible for these patients.
When nurses learn how to effectively help patients with spinal cord injuries better manage their own bowel and bladder regimens, quality of life and health outcomes may be improved for this group.
Pressure Injury Prevention, Staging and Treatment
Introduction
When hearing the term HAPI, what comes to mind? The fact is, HAPI may not necessarily generate happy thoughts. Hospital-acquired pressure injuries (HAPIs) are a significant problem in the U.S. today. In fact, pressure injuries in general – whether acquired in a hospital or not – are a global problem.
Many articles have noted that staging and differentiating pressure injuries can be overwhelming for nurses [9]. The purpose of this course is to equip learners with the knowledge needed to reduce pressure injuries, resulting complications, financial risk, and associated death. The information in this course will serve as a valuable resource to nurses from all specialties and backgrounds.
What is a pressure injury?
The National Pressure Injury Advisory Panel (NPIAH) defines pressure injuries as “localized damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device” [17]. Pressure injuries can present as intact or opened skin and can be shallow or deep. Pressure injuries can be quite painful for patients and may require extensive treatment.
Prior to 2016, pressure injuries were termed “pressure ulcers.” However, since ulcer implies “open skin,” the NPIAH changed it to “pressure injury” as the skin is not always open with some of these injuries [22][25].
What causes a pressure injury to develop?
Pressure
Intense and/or prolonged pressure on the patient’s skin and/or tissue can cause compromised blood flow and decreased sensation [7]. This can occur when patients lay or sit on a bony prominence for an extended period of time [16].
Bony prominences are areas where you can easily feel a bone underneath the skin or tissue when palpating. These can include the heels, hips, elbows, and tailbone. Approximately two-thirds of all pressure injuries occur on the hip and buttocks area [7].
Friction and Shear
Friction and shear often happen when patients slide down in bed, for example, when the head of the bed is raised. Although “friction and shear” are often used together, there is actually a difference between the two.
While friction occurs when skin is dragged across a coarse surface (leading to surface-level injuries), shearing occurs when internal bodily structures and skin tissue move in opposite directions (leading to deep-level injuries) [10]. Shearing is often associated with a type of pressure injury called deep tissue injury (occurring in the deeper tissue layers rather than on the skin’s surface) [10].

[24]
What are risk factors for developing a pressure injury?
There are numerous risk factors for pressure injuries – some of which may not be directly related to the skin. These risk factors can be categorized as either intrinsic factors (occurring from within the body) or extrinsic (occurring from outside of the body) [2][13].
Intrinsic Risk Factors
- Poor skin perfusion (e.g., peripheral vascular disease or smoking)
- Sensation deficits (e.g., diabetic neuropathy or spinal cord injuries)
- Moist skin (e.g., urinary incontinence or excessive sweating)
- Inadequate nutrition (particularly poor protein intake)
- Poor skin elasticity (e.g., normal age-related skin changes)
- End of life/palliative (leads to organ failure including the skin)
- Limited mobility (i.e., bedridden, or wheelchair-bound)
Extrinsic Risk Factors
- Physical and chemical restraints (leads to limited mobility)
- Undergoing a procedure (laying down for extended periods of time)
- Length of hospital stay (for HAPIs)
- Medical devices (can lead to medical device-related pressure injuries)

Self Quiz
Ask yourself...
- What are the most common areas for pressure injuries to develop?
- What is the major difference between friction and shear?
- What is one reason why elderly adults are at an increased risk for developing a pressure injury?
Statistical Evidence
This section will cover pressure injury statistics both globally and nationally. This section will also cover the impact pressure injuries have on healthcare.
What is happening on a global scale?
In a global study, researchers found that the prevalence (all cases) and incidence (new cases) of pressure injuries in 2019 were 0.85 million and 3.17 million, respectively – numbers that have decreased over time [23][25]. Numbers were disproportionately high in high-income North America, Central Latin America, and Tropic Latin America [25]. Numbers were lowest in Central Asia and Southeast Asia. The report revealed that although numbers are high overall, they are much lower than what they were predicted to be, which may be attributed to better prevention and treatment initiatives.
What is happening nationally?
In the U.S., 2.5 million people develop pressure injuries each year [1]. This number does not account for the many people trying to manage pressure injuries on their own at home (i.e., when family acts as the caregiver).
HAPIs in particular are a growing problem. The most recent data on hospital-acquired conditions in the U.S. shows that from 2014 to 2017, HAPIs increased by 6% (647,000 cases in 2014 to 683,000 in 2017) [6]. Each year 60,000 patients in the U.S. die as a direct result of pressure injuries [1].
How do pressure injuries impact healthcare?
Pressure injuries can be quite costly to the healthcare system. These injuries can lead to persistent pain, prolonged infections, long-term disability, increased healthcare costs, and increased mortality [1].
In the U.S., pressure injuries cost between $9.1 - $11.6 billion per year [1]. These injuries are complex and can be difficult to treat [7]. Often requiring an interdisciplinary approach to care, the costs of one pressure injury admission can be substantial. Individual care for patients with pressure injuries ranges from $20,900 to $151,700 per injury [1]. Not to mention, more than 17,000 lawsuits are related to pressure injuries every year [1].
Due to the significant impact that these injuries have on healthcare, prevention and accurate diagnosis is imperative.

Self Quiz
Ask yourself...
- What are possible contributing factors to the increase in HAPIs in the U.S.?
- What are some factors that may contribute to the high costs of pressure injuries in healthcare settings?
Staging and Diagnosis
The section will cover the staging, varying types, and diagnosis of pressure injuries.
What is the difference between wound assessment and staging?
Pressure injury staging is more than a basic wound assessment. Wound assessment includes visualizing the wound, measuring the size of the wound, paying attention to odors coming from the wound, and lightly palpating the area on and/or around the wound for abnormalities. Pressure injury staging, however, involves determining the specific cause of injury, depth of skin or tissue damage, and progression of the disease.
What are the six stages of pressure injuries?
According to NPIAP guidelines, there are six types of pressure injuries – four of which are stageable [14].

[16]
Stage 1
In Stage 1 pressure injuries, there is intact skin with a localized area of non-blanchable erythema (pink or red in color), which may appear differently in darkly pigmented skin. Before visual changes are noted, there may be the presence of blanchable erythema or changes in sensation, temperature, or firmness. Stage 1 pressure injuries do not have a purple or maroon discoloration (this can indicate a deep tissue pressure injury).
Stage 2
In Stage 2 pressure injuries, there is partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist, and may represent an intact or opened serum-filled blister. Fat (adipose) and deeper tissues are not visible. Granulation tissue, slough (soft moist material, typically yellow or white), and eschar (hard necrotic tissue, typically black in color) are not present. Stage 2 injuries cannot be used to describe wounds associated with moisture-only, skin chaffing, medical adhesives, or trauma.
Stage 3
In Stage 3 pressure injuries, there is full-thickness loss of skin, in which fat is visible in the injury, and granulation tissue and rolled wound edges are often present. Slough and/or eschar may be noted. The depth of tissue damage is dependent on the area of the wound. Areas with a significant amount of fat can develop deep wounds.
Undermining (burrowing in one or more directions, may be wide) and tunneling (burrowing in one direction) may be present. Fascia, muscle, tendon, ligament, cartilage, and/or bone are not exposed. If slough or eschar covers the extent of tissue loss, this would be considered an unstageable pressure injury, not a Stage 3.
Stage 4
In Stage 4 pressure injuries, there is full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage, or bone in the wound. Slough and/or eschar may be visible. Rolled wound edges, undermining, and/or tunneling are often present. The area where the wound is present will determine the depth. As with stage 3 pressure injuries, if slough or eschar covers the extent of tissue loss, this would be considered an unstageable pressure injury.
Unstageable
In unstageable pressure injuries, there is full-thickness skin and tissue loss in which the extent of tissue damage within the wound cannot be confirmed because it is covered by slough or eschar. If the slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar (i.e., dry, adherent, intact without erythema or fluctuance) on an ischemic limb or the heel(s) should not be removed.
Deep Tissue Injury
In deep tissue pressure injuries (also termed: deep tissue injuries or DTIs), there is intact or non-intact skin with localized area or persistent non-blanchable deep red, maroon, purple discoloration, or epidermal separation revealing a dark wound bed or blood-filled blister.
Pain and temperature changes often precede skin color changes. Discoloration may appear differently in darker-pigmented skin. The injury may resolve without tissue loss or may worsen quickly and open up, revealing the actual extent of tissue injury. Deep tissue pressure injuries should not be used to describe vascular, traumatic, neuropathic, or dermatologic conditions.

Self Quiz
Ask yourself...
- How do basic wound assessments differ from pressure injury staging?
- What is the main difference between a Stage 1 pressure injury and deep tissue injury?
- What is one structure you might see in a Stage 4 pressure injury wound bed that you would not see in any other pressure injury?
What are other types of pressure injuries?
Mucosal Membrane Pressure Injury
Mucosal membrane pressure injuries are found on mucous membranes with a history of a medical device in use at the location of the injury. For example, a wound on the inside of a nostril from a nasogastric tube would be considered a mucosal membrane pressure injury. Due to the anatomy of the tissue, mucosal membrane pressure injuries cannot be staged [18].
Medical Device-Related Pressure Injury
Medical device-related pressure injuries, often associated with healthcare facilities, resulting from the use of devices designed and applied for diagnostic or therapeutic purposes [15]. The resulting pressure injury typically conforms to the pattern or shape of the device which makes identification easier. The injury should be staged using the staging system.
Hospital Acquired Pressure Injury (HAPI)
While the general hospital setting places patients at a 5% to 15% increased risk of developing a pressure injury (HAPI), patients in the intensive (or critical) care unit in particular have an even higher risk [17]. Critical care patients typically have serious illnesses and conditions that may cause temporary or permanent functional decline. There is also evidence that pressure injuries in this setting can actually be unavoidable.
The NPIAP defines “unavoidable” pressure injuries as those that still develop after several measures by the health provider have been taken. These measures include when the provider has (a) evaluated the patient’s condition and pressure injury risk factors, (b) defined and implemented interventions consistent with standards of practice and the patient’s needs and goals, and (c) monitored and evaluated the impact of interventions [20]. There are certain situations in which a critical care patient may have a higher risk of developing unavoidable pressure injuries.
In one study of 154 critical care patients, researchers found that 41% of HAPIs were unavoidable and those who had a pressure injury in the past were five times more likely to develop an unavoidable pressure injury during their stay [20]. The study also found that the chance of developing an unavoidable HAPI increased the longer patients stayed in the hospital – a 4% risk increase each day.

Self Quiz
Ask yourself...
- What type of pressure injury can be caused by nasogastric tube use?
- What is it about critical care patients that places them at a high risk for HAPIs?
- In what situation is a pressure injury considered unavoidable?
How are pressure injuries diagnosed?
Diagnosing a pressure injury is done by simply staging the injury. The health provider may stage the injury or rely on the nurse’s staging assessment before giving the final diagnosis and initiating treatment. There are tests that may be ordered to help identify the early stages of a developing injury.
For example, subepidermal moisture assessment (SEM) scanners may help to identify tissue changes early on in patients with darker skin tones [8]. Tests may also be ordered to determine the extent of the damage, disease, or infection caused by a pressure injury. A magnetic resonance imaging test (MRI) can be used to determine if the infection in a stage 4 pressure injury has spread to the bone.

Self Quiz
Ask yourself...
- What are some problems that can occur if a pressure injury is not staged correctly?
- What is one reason a provider would order an MRI of a pressure injury?
Prevention and Treatment
This section will cover various strategies that can be used to prevent and treat pressure injuries.
What are some ways to prevent pressure injuries?
Preventing pressure injuries takes more than just one nurse repositioning a patient every two hours. It involves a combination of strategies, protocols, and guidelines that facilities can implement across various departments, specialties, and care team members. The NIAPH recommends the following prevention strategies [19].
Risk assessment
Facilities should use a standardized risk assessment tool to help identify patients at risk for pressure injuries (i.e., the Braden or Norton Scale). Rather than using the tool as the only risk assessment strategy, risk factors should be identified by other means (for example, by gathering a detailed patient history).
Risk assessments should be performed on a regular basis and updated as needed based on changes in the patient’s condition. Care plans should include risk assessment findings to address needs.
Skin Care
Monitoring and protecting the patient’s skin is vital for pressure injury prevention. Stage 1 pressure injuries should be identified early to prevent the progress of disease. These include looking at pressure points, temperature, and the skin beneath medical devices.
The frequency of assessments may change depending on the department. Ideally, assessments should be performed upon admission and at least once daily. Skin should also be cleaned promptly after incontinence episodes.
Nutritional Care
Tools should be used that help to identify patients at risk for malnutrition. Patients at risk should be referred to a registered dietician or nutritionist. Patients at risk should be weighed daily and monitored for any barriers to adequate nutritional intake. These may include swallowing difficulties, clogged feeding tubes, or delays in intravenous nutrition infusions.
Positioning and mobilization
Immobility can be related to age, general poor health, sedation, and more. Using offloading pressure activities and keeping patients mobile overall can prevent pressure injuries. Patients at risk should be assisted in turning and repositioning on a schedule. Pressure-relieving devices may be used as well. Patients should not be positioned on an area of previous pressure injury.
Monitoring, training, and leadership
Current and new cases of pressure injuries should be documented appropriately and reported. All care team members should be educated on pressure injury prevention and the importance of up-to-date care plans and documentation.
All care team members should be provided with appropriate resources to carry out all strategies outlined. Leadership should be available to all care team members for support (this may include a specialized wound care nurse or wound care provider).


Self Quiz
Ask yourself...
- What is one reason why a patient at risk for pressure injuries would be weighed daily?
- What are two ways to prevent pressure injuries in a patient with limited mobility?
How are pressure injuries treated?
There is no one way to treat a pressure injury. Management of pressure injuries involves a specialized team of care providers and a combination of therapies that aim to target underlying factors and prevent complications [7]. Depending on the stage of the wound and skin risk factors, providers may order specific types of treatments.
Some pressure injury treatments may include the following [7].
- Wound debridement – a procedure in which necrotic tissue is removed from a wound bed to prevent the growth of pathogens in the wound, allowing for healing
- Antibiotic therapy (topical or systemic)
- Medicated ointments applied to the wound bed (e.g., hydrogels, hydrocolloids, or saline-moistened gauze to enable granulation tissue to grow and the wound to heal)
- Nutritional therapies (e.g., referrals to dieticians)
- Disease management (e.g., controlling blood sugar in diabetes)
- Pain medications
- Physical therapy (to keep the patient active)

Self Quiz
Ask yourself...
- In what way does debridement help to heal a pressure injury?
- What non-nursing care team member may be consulted for a patient with a pressure injury?
The Nurse’s Role
The section will cover the nurse’s role in preventing pressure injuries and the progression of disease.
What is the nurse’s role in pressure injury prevention?
Based on NPIAH guidelines, the Agency for Healthcare Research and Quality (AHRQ) – an agency that monitors pressure injury data for the U.S. – breaks down quality initiatives for preventing pressure injuries in a three-component care bundle [2].
A care bundle is a combination of best practices that when used together, can lead to better patient outcomes [2]. The care bundle includes skin assessments, risk assessments, and care planning. Nurses should follow the guidelines listed under each component.
Standardized pressure injury risk assessment
- Use risk assessment tools and processes to identify patients at risk
- Do not rely on tools only, use your own judgment as well (tools are meant to guide the assessment)
- Update risk scores at least once daily and if patient’s condition changes
- Document findings in the medical record
- Communicate findings to other staff involved for continuity of care (e.g., informing another nurse during patient handoff reporting)
Comprehensive skin assessment
- Identify any pressure injuries that may be present
- Determine whether there are other areas of skin breakdown or factors that may predispose the patient to develop a pressure injury (e.g., moist skin)
- Identify other skin issues
- Perform assessments at regular intervals
- Document findings in the medical record
- Communicate findings to other staff involved in care so that appropriate changes can be reported (e.g., informing the nursing assistant)
- Ask colleague to confirm findings for accuracy (i.e., two-nurse skin checks)
Care planning and implementation to address areas of risk
- Create care plans that include each skin risk factor (e.g., nutrition, mobility, and moisture)
- Update care plans as often as needed if there are any changes in the patient’s condition
- Evaluate whether care plan was effective by assessing patient response to interventions
- Individualize care plans for each patient based on risk assessment scores and other observed risks
- Identify patient learning needs and implement teaching as needed
- Document care plan in the medical record
- Communicate care plan to other staff involved for continuity of care (e.g., informing another nurse during patient handoff reporting)

Self Quiz
Ask yourself...
- Why should nurses avoid relying solely on standardized assessment tools?
- Why is documentation important when performing a skin assessment?
- What pressure injury information should nurses communicate during handoff report?
How can nurses prevent medical device-related pressure injuries?
The NPIAP outlined best practices to prevent medical device-related pressure injuries in various settings including general care, long-term care, critical care, and pediatric care [20]. The following strategies apply across all settings.
- Choose the correct size of medical device for the individual.
- Cushion and protect the skin with dressings in high-risk areas (e.g., nasal bridge).
- Inspect the skin under and around the device at least daily (if not medically contraindicated).
- Rotate sites of oximetry probes.
- Rotate between O2 mask and prongs (if feasible).
- Reposition devices (if feasible).
- Avoid placement of device over sites of prior or existing pressure injury OR directly under the patient.
- Be aware of edema under the device and the potential for skin breakdown.
- Change rigid C-collar to softer collar when medically cleared (for critical care settings).

Self Quiz
Ask yourself...
- How can nurses prevent a pressure injury from developing on the ear of a patient who wears a nasal cannula?
How can nurses identify pressure injuries in patients with darker skin tones?
Research suggests that it may be difficult to note early changes that can lead to the development of a pressure injury in patients with darker skin tones – for one, blanching may not be as visible [8]. This places the patient at a greater risk for the advancement of disease as early identification may be challenging.
In order to appropriately identify pressure injuries in patients with darker skin tones, nurses should use unique strategies. The NIPAH offers these recommendations for nurses to help accurately identify pressure injuries in this group [8].
Identification tips
- Clean the suspected area beforehand
- Compare the area to surrounding unaffected areas
- Compare the area to the opposite laterality if possible (i.e., right versus left elbow)
- Compare the area to unaffected areas in a different location (i.e., upper back versus chest)
- Look for differences in skin tautness
- Look for shining skin changes
- Palpate for changes in skin temperature

Self Quiz
Ask yourself...
- What is one way to identify pressure injuries in patients with darker skin tones?
How can nurses quickly differentiate between pressure injury stages?
Correct staging of pressure injuries is vital as treatment is determined by the extent of damage, disease, or infection. First and foremost, wounds should be gently cleaned prior to staging as drainage or debris can be mistaken for fat or bone within the wound bed [14].
Nurses can quickly differentiate between stages by asking these simple easy-to-understand starter questions. A more detailed assessment should follow.
- Stage 1 versus Stage 2: Is the skin intact?
Rationale: The skin is always intact in Stage 1. The skin is always open in Stage 2 (or there may be an intact blister present).
- Stage 2 versus Stage 3: Is the wound bed pink or beefy red?
Rationale: The wound bed is pink or beefy red in Stage 2. In Stage 3, the wound bed has structures within that may be discolored.
- Stage 3 versus Stage 4: Does the wound bed contain soft or firm structures?
Rationale: The wound bed contains softer structures in Stage 3. The wound bed contains firmer structures in Stage 4.*
- Unstageable versus Stageable: Is any part of the wound bed hidden?
Rationale: The wound bed is not entirely exposed in an unstageable. The wound bed is exposed in a stageable that is open.
- Intact DTI versus Stage 1: Is the discoloration light or dark?
Rationale: The discoloration is dark in a DTI. The discoloration is much lighter in Stage 1.
- Open DTI versus Stage 2: Is the discoloration in or around the wound bed dark?
Rationale: There is dark discoloration in or around the wound bed in an open DTI. In stage 2, the discoloration is much lighter (if even present).
*Nurses should familiarize themselves with the appearance of the various structures that may be present in a wound like fat, fascia, bone, tendon, ligament, etc. Most importantly, nurses should consult the wound care team or health provider if a stage cannot be determined.

Self Quiz
Ask yourself...
- Why should nurses clean a wound prior to staging?
- What should nurses do if unsure how to stage a pressure injury?
What should patients know?
Facilities can use the NIAPH prevention strategies to devise teaching plans for patients [19]. Nurses should educate patients and families/caregivers on risk factors, signs and symptoms, prevention tips, and the importance of following through with treatment.
Nurses should also teach patients to advocate for their own health in order to avoid progression of disease. Here are important tips to teach at any point during the patient’s stay. These tips can apply to nurses working in a variety of settings.
- Tell the nurse or provider of your medical conditions (needed to identify risk factors)
- Tell the nurse or provider if you notice any numbness or tingling in your body (potential risk for sensory deficits)
- Tell the nurse or provider if you have a loss of appetite or trouble eating (potential risk for malnutrition)
- Clean yourself well after using the restroom (maintains skin integrity)
- Tell the nurse or provider if you need to use the restroom or need help with cleaning yourself (maintains skin integrity)
- Tell the nurse right away if you have an incontinence episode (maintains skin integrity)
- Take all prescribed medications (may include necessary antibiotics or wound-healing medications)
- Reposition yourself in bed often or tell the nurse if you need help doing so (reduces immobility risk)
- Tell the nurse or provider if you notice a new discolored area on your skin, or an open area (potential new or worsening pressure injury)
- Tell the nurse or provider if you notice any changes to your wound (potential worsening pressure injury)

Self Quiz
Ask yourself...
- What is one pressure injury prevention tip nurses can teach hospitalized patients?
- What signs or symptoms should nurses teach the patient to report?
Quality Improvement
This section will cover the quality improvement measures in place to reduce pressure injuries.
What is a pressure injury quality improvement initiative?
Quality improvement involves setting goals (or initiatives) and standards of care. The goal of quality improvement is to improve patient outcomes at a systematic level where everyone involved is on the same page.
Although possibly unaware, all care team members are involved in quality improvement. Nursing leaders design, manage, and evaluate program initiatives. Staff nurses and other care team members follow protocols that are often developed from these initiatives.
The Pressure Injury Prevention Program is a guide designed by the AHRQ to help health facilities implement a structured pressure injury prevention initiative based on quality improvement [12]. Facilities can use the guide as a training toolkit to implement a new quality improvement program [5].
Initiative Goals:
- Reduced pressure injury rates
- Reduced adverse events related to pressure injuries
- Reduced costs associated with pressure injuries
- Reduced lawsuits related to pressure injuries
Ways facilities can implement a prevention program:
- Address the overall objectives of the prevention program
- Identify the needs for change and how to redesign practice
- Develop goals and plans for change
- Use the NIAPH pressure injury prevention recommended practices
- Establish comprehensive skin assessment protocols
- Standardize assessments of pressure injury risk factors
- Incorporate risk factors into individualized care planning
- Establish clear staff and leadership roles

Self Quiz
Ask yourself...
- What is one reason why a health facility would start or update a pressure injury prevention program?
- When pressure injury rates are reduced, what else can health facilities expect to improve as well?
What are some pressure injury quality measures?
Quality measures are tools that measure a system’s healthcare goals and/or ability to provide high-quality care [11]. In simple terms, quality measures are specific ways that systems (governments, states, organizations, etc.) can show how they are making progress in meeting goals. The AHRQ highlights the following three ways the U.S. measures its progress.
Number of HAPIs
The AHRQ measures the number of HAPIs per year. The most recent data is from 2014 to 2017 [6].
| Year | Number of HAPIs |
| 2014 | 647,000 |
| 2015 | 700,000 |
| 2016 | 677,000 |
| 2017 | 683,000 |
Rate of HAPIs per admission
The AHRQ measures the number of HAPIs per admission related to age groups. The number is measured as a “rate,” meaning the number of HAPIs per 1,000 hospital admissions. The most recent evidence is from 2017 [4].
| Age group | Number of HAPIs per 1,000 admissions |
| 18 – 39 | 0.38 |
| 40 – 64 | 0.63 |
| 65 – 74 | 0.74 |
| 75 and over | 0.71 |
Costs of HAPIs
Another quality measure is HAPI costs. While the AHRQ does not measure costs of HAPIs every single year, the most recent data is from 2017 [3].
| Year | Cost of HAPIs per patient |
| 2017 | $8,573 – $21,075 |
Deaths related to HAPIs
Patient mortality rates related to HAPIs are a quality measure (calculated per 1,000 pressure injury cases). The most recent data is from 2017 [6].
| Year | Number of deaths per 1,000 pressure injury cases |
| 2017 | 2.42 – 5.06 |

Self Quiz
Ask yourself...
- What is one way a health facility can show its progress in preventing pressure injuries?
- What patient age range do you think has the most pressure injury rates? Age 65 to 74 or age 75 and over?
Conclusion
Pressure injuries are complex conditions that can lead to poor patient outcomes and a burdened healthcare system. The best strategy in the care of patients with pressure injuries or those at risk is prevention.
However, preventing these injuries involves more than individual nurses taking specific steps. Prevention of pressure injuries involves a team effort from all members of the care team and a systemic plan for improvement.
Negative Pressure Wound Therapy (Wound Vac)
Introduction
Negative pressure wound therapy (NPWT), also known as a wound vac, can be a powerful tool in combatting acute and chronic wounds. It relies on generating a negative pressure on the surface of a difficult wound to promote wound healing.
The goal of this course is to develop an understanding of mechanism of action of NPWT, discuss appropriate nursing assessment of these wounds, evaluate adjunct treatment options and troubleshooting support tips.
We will review basic concepts of the integumentary system and the normal wound healing process to support the rationale of NPWT.
Definition
Negative pressure wound therapy (NPWT) is the application of sub-atmospheric pressure to help reduce inflammatory exudate and promote granulation tissue in an effort to enhance wound healing (4). The idea of applying negative pressure therapy is that once the pressure is lower around the wound, the gentle vacuum suction can lift fluid and debris away and give the wound a fighting chance to heal naturally.
NPWT has a long and interesting history. The idea of suctioning fluid from wounds as therapy is not a new concept. The process was first called “cupping” and was described in Ebers Papyrus around 500 BC; historians tell us that a form of wound suction was used around 1000 BC in China, 600 BC in Babylon and Assyria, and in 400 BC by Greeks who heated copper bowls over wounds to remove blood and fluids (5).
Modern medicine has built upon a very old concept. Thankfully, nurses have a slightly easier tool in NPWT devices than heating copper bowls.

Self Quiz
Ask yourself...
- Can you name the various methods of wound treatments that you have encountered?
- Do you recognize how negative pressure can create suction?
Indications for Use
Negative pressure wound therapy is widely used for the management of both acute and chronic wounds. This therapy is helpful for a broad range of wounds, from pressure ulcers to closed surgical incisions.
The system is now implemented routinely for open wounds, such as open fractures, fasciotomies, diabetic foot ulcers, and infected wounds. Delayed wound healing and difficult wounds are seen more commonly in elderly patients and those with comorbidities (1).
It’s important to review the basic anatomy of our integumentary system, types of wounds, and barriers to healing to understand the usefulness of NPWT.
Basic Anatomy of Integumentary System
Our integumentary system is considered the body’s largest organ. Our skin acts as a shield against heat, light, bacteria, infection, and injury. Other functions include body temperature regulation, storage of water and fat, sensory function, prevention of water loss, and a basic storage compartment for the organs (6).
The skin is made up of 3 layers. Each layer has unique functions:
- Epidermis
- Dermis
- Subcutaneous fat layer (hypodermis)
The epidermis is the thin outer layer of our skin, it contains squamous cells, basal cells, and melanocytes (gives skin its color). The dermis is the middle layer of skin, it contains blood vessels, hair follicles, sweat glands, nerves, lymph vessels, fibroblasts, and sebaceous glands (6). It is important to remember that the dermis contains nerves and nerve receptors.
The subcutaneous fat layer is the deepest layer of skin and is made up of a network of collagen and fat cells; this layer conserves the body's heat and protects the body from injury by acting as a shock absorber (6).

This design was created on Canva.com on September 28, 2023. It is copyrighted by Abbie Schmitt, RN, MSN and may not be reproduced without permission from Nursing CE Central.
Types of Wounds
Negative pressure wound therapy is primarily used to treat complex wounds that are non-healing or at risk of non-healing. It is also indicated for acute wounds when the wound cannot be closed due to the risk of infection, active infection, skin tension, or swelling (7).
Closure or skin grafting of acute wounds, such as open fractures or burns, are at high risk for infection due to microorganisms becoming trapped in the soft tissue leading to abscess development.
Examples of possible wounds to apply NPWT (1):
- Diabetic foot ulcers
- Bed sores
- Skin graft fixation
- Burns
- Crush injuries
- Sternal/abdominal wound dehiscence
- Fasciotomy wounds
- Animal bites
- Frostbite
Barriers to Healing
Age
- Increased risk of tearing and shearing due to thinning of epidermis and decrease in elastin
- Phases of healing are prolonged
- Increased risk of dehiscence as the dermis has slower contractility
- Skin more susceptible to bacterial growth and infections as pH becomes more neutral with age
Co-morbidities
- Cardiopulmonary Disease
- Oxygen-transport pathways are affected
- O2 necessary for wound healing
- Diabetes Mellitus
- High glycemic levels predispose patients to infection
- Microvasculature and neuropathic components of DM increase the risk for impaired healing
- Poor glycemic control can increase the risk of ulceration and delayed healing
- Immune-suppressing conditions (Cancer, HIV, immunosuppressive therapy, immunosuppression syndrome)
- Inflammatory phase (immunology) is impaired
- Increased risk for infection
Impaired Perfusion and Oxygenation
- Peripheral Vascular Impairment
- Proper perfusion is required for growth of new tissue and immunological responses of the tissue.
- Arterial insufficiency (blood flow to extremities) leads to necrosis or lack of response to edema.
Neurological Impairment
- Peripheral neuropathy
- Complication related to DM, alcoholism, chemotherapy
- Loss of neuronal signaling and transmission
- Loss of the sensory ability to recognize and react to sensations of touch, pressure, temperature, pain. Example: patient leaving foot on hot surface because there was no pain sensation, leading to burn wound.
- Spinal cord injury

Self Quiz
Ask yourself...
- Are you familiar with the layers and components that make up the integumentary system?
- Have you ever cared for a patient with a chronic wound?
- What are some ways the elderly population is at higher risk for prolonged wound healing?
Mechanism of Action
The mechanism of action is dependent on applying negative pressure, which is below atmospheric pressure, to the wound. This pressure allows the gentle vacuum suction to lift fluid and exudate away from the wound to enhance healing (3).
The vacuum is gentle because powerful suction would remove newly formed tissue as well. The mechanism of action is not only in removing fluid and debris from the tissue, but the pressure causes stimulation of the growth of granulation tissue at a macroscopic and microscopic level.
The porous foam shrinks in size with the application of negative pressure and exerts strain on the wound bed, which leads to macro- and micro-deformation of the wound (3). Microdeformation is simply a term used to describe microscopic tissue cell reactions. This reaction can be compared to a battery jump-start of a car; the stimulation causes the battery to engage.
NPWT systems consist of a sterile foam sponge, a semi-occlusive adhesive cover, a fluid collection system or canister, and a suction pump (1). The foam sponge is applied to the wound and covered. A fenestrated tube is embedded in the foam and the wound is sealed with adhesive tape to make it airtight, and the machine delivers continuous or intermittent suction, ranging from 50 to 125 mmHg (1).

This design was created on Canva.com on October 1, 2023. It is copyrighted by Abbie Schmitt, RN, MSN and may not be reproduced without permission from Nursing CE Central.
Proper application of the NPWT is important for the mechanism of action to be effective. Research supports that NPWT is effective at creating a stable wound environment, reduces inflammation and bacterial load, improves tissue perfusion, and stimulates granulation tissue and angiogenesis (1).
Imagine you want to plant a garden in a swampy location, you would first need to divert the water and algae from the land, cover it with a greenhouse with consistent heat and pressure, and cultivate the soil for optimal growth. Similarly, NPWT creates the most ideal conditions possible for tissue regeneration.

Self Quiz
Ask yourself...
- Can you name the components of NPWT?
- Have you ever applied a wound vac dressing?
- Are you familiar with the other semipermeable materials that serve as a filter?
Contraindications
NPWT would be contraindicated for the following:
- Wounds involving untreated osteomyelitis.
- Wounds that have exposed blood vessel
- Wounds with exposed nerves, anastomotic sites, or organs
- Wounds including open joint capsules
- Malignant wounds
- Wounds with necrotic tissue; it is recommended to excise first
The following wounds could benefit from NPWT, but caution should be given (5):
- Wounds with visible fistula
- Wounds with exposed bone or tendon
- The bone or tendon should be isolated from direct pressure
- Patient with clotting disorders or that are taking anticoagulants, due to an increased risk of bleeding.
- Compromised microvascular blood flow to the wound bed.

Self Quiz
Ask yourself...
- Can you think of reasons a malignant, cancerous wound should not have NPWT?
- Have you ever dressed a wound prior to or following debridement?
Assessment
A focused assessment should be done for patients with NPWT devices in place, both on the machine settings, the dressing, and the wound itself. Thorough documentation of the wound is essential to see the progression of wound healing.
Suction Device Settings:
- Continuous or intermittent
- Pressure Setting: Range of pressure settings from -40mmHg to -200mmHg, which can be tailored for different types of wounds (7). This is set by the medical provider.
Laboratory assessment is meaningful in wound care. Labs can be used to assess oxygenation or indicators of infection (6).
Dressing Assessment
The appearance of the NPWT and dressing should be clean, dry, intact, and sealed. The tubing should not be twisted or kinked, and the clear adhesive dressing should not be wrinkled or overlapping. Please see below an example of the appropriate appearance of a dressing.
Wound Assessment:
- Anatomic location
- Type of wound
- Degree of tissue damage
- Description of wound bed
- Wound size
- Wound edges and surrounding skin
- Signs of infection
- Pain
Anatomical Location
Anatomical terms and numbering should be used to make sure the location of each wound is documented. Patients often have more than one wound, so the treatment needs to be specified for each wound.
Wound Base
Assess the color of the wound base. Healthy granulation tissue appears pink and moist due to the new capillary formation. The appearance of slough (yellow) or eschar (black) in the wound base should be documented and communicated to the health care provider (1).
This tissue may need to be removed to optimize healing. If any discoloration or duskiness of the wound bed or wound edges are identified, the suction should initially be reduced or switched off (7).
Type and Amount of Exudate
Assess the color, thickness, and amount of exudate (drainage) The amount of drainage from wounds is categorized as scant, small/minimal, moderate, or large/copious.
Terms are used when describing exudate: sanguineous, serous, serosanguinous, and purulent (6).
- Sanguineous: fresh bleeding
- Serous: Clear, thin, watery plasma
- Serosanguinous: Serous drainage with small amounts of blood noted
- Purulent: Thick and opaque. The color can be tan, yellow, green, or brown. This is an abnormal finding and should be reported to a physician or wound care provider.
Wound Size
Wounds should be measured on admission, wound vac dressing changes, or as needed for abnormal events. Many healthcare facilities use disposable, clear plastic measurement tools to measure the area of a wound.
Consistent measurement is vital to the assessment of wound healing.
- Measure the greatest length, width, and depth of the wound in centimeters
- Examples of wound classification tools:
- NPUAP staging system for pressure injuries
- Payne-Martin classification system for skin tears
- CEAP (clinical, etiologic, anatomic, and pathophysiology) system for venous ulcers
Tunneling or Undermining
Tunneling is when a wound has moved underneath the skin, making a “tunnel.” The depth of tunneling can be measured by gently inserting a sterile, cotton-tipped applicator into the tunnel and noting the length from the wound base to the end of the tract (7). Undermining occurs when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound’s edge.
Healing Process
It is important to recognize the entire process of normal wound healing. There are four phases of wound healing: hemostasis, inflammatory, proliferative, and maturation (6).
Hemostasis begins immediately after injury, involving platelet aggregation and activation of clotting factor (6). A platelet “plug” is formed as fibrinogen converts to fibrin and binds to itself. Vasoconstriction occurs at this time, decreasing blood loss and allowing clot formation.
The inflammatory phase begins right after the injury and the injured blood vessels leak and cause localized swelling. The swelling, warmth, pain, and redness present during this stage of wound healing are related to the release of white blood cells, growth factors, nutrients, and enzymes to help control bleeding and prevent infection (6).
The proliferative phase of wound healing involves “rebuilding” with new tissue made up of collagen and extracellular matrix; granulation tissue is built stronger with proper oxygen and nutrients.
Key nursing knowledge: Dark granulation tissue can indicate infection, ischemia, or poor perfusion. The maturation phase of wound healing is when collagen is remodeled, aligns along tension lines, water is reabsorbed so the collagen fibers can lie closer together and cross-link, and the wound fully closes (1).
There are three types of wound healing: primary intention, secondary intention, and tertiary intention.
Primary intention means that the wound healing is supported by sutures, staples, glue, or otherwise closed so the wound heals beneath the closure (6).
Secondary intention must happen when the edges of a wound cannot be approximated, or “brought together,” so the wound heals with the production of granulation tissue from the bottom up (6).
Wounds that heal by secondary intention are at higher risk for infection, so contamination prevention is essential. Pressure ulcers are an example of wounds that heal by secondary intention.
Tertiary intention refers to a wound that needs to remain open, often due to severe infection. Wounds with secondary and tertiary intention have longer healing times (2).

Alternatives when NPWT fails
- Hyperbaric Oxygen Therapy (HBOT):
- HBOT is a treatment in which the wound is exposed to pure oxygen in a pressurized chamber to enhance wound healing (3).
- Bioengineered Tissue:
- Skin grafting or bioengineered tissue to promote tissue growth and healing.
- Skin grafts are considered as a treatment option if a wound is so large that it can’t close on its own. In this procedure, skin is taken from another part of your body – usually your thigh – and transplanted onto the wound (2).
- Some grafts are made from human cell products and synthetic materials. Studies have shown that these increase the chances of poorly healing venous leg ulcers closing faster. (2)
- Electrical Stimulation Therapy:
- Electrical stimulation therapy applies electrical currents to stimulate wound healing and tissue generation (4). It may be used to treat chronic wounds or pressure ulcers.

Self Quiz
Ask yourself...
- Have you ever cared for a patient with a wound that was unable to be stitched or sutured?
- Can you describe the importance of thorough, descriptive documentation of multiple wounds?
- Can you think of barriers to the normal wound healing process?
Adjunct Treatment Options
When selecting an adjunctive therapy for wound management, the patient's medical history, overall health, co-morbidities, ambulation status, psychosocial aspects, environmental factors, and the specific needs of the wound should all be considered. Each patient is unique, and an individualized care plan is the goal.
Treatment of the underlying contributing disorder will be essential. For example, a patient with uncontrolled diabetes that has led to poor circulation can benefit from glycemic control.
Take a look at the larger, holistic picture. It can be helpful for the healthcare team to create a concept map of problems that contribute to the wound.
Topical Agents and Dressings
Various creams, ointments, or dressings can promote wound healing and prevent infection. One example is silver-based products, which are commonly used in reducing bacterial burden and treating wound infection (4).
Nutrition Therapy for Wound Healing
Patients with wounds would benefit from nutrition consultation and ongoing support.
Nutrients from foods help the body build and repair tissue and fight infection. An increase in calories and protein is important, as well as blood sugar control for diabetics.
Vitamins C, D, B-6, B-12, folate, and others aid in repairing tissues (6). Minerals such as iron, magnesium, calcium, zinc, and others support the cardiovascular system making sure cells have enough oxygen, the nervous system, and immunological function (6).
Compression Therapy
Compression therapy uses pressure to reduce swelling and improve blood flow to the wound. There are common compression devices or stockings available. It is frequently used to treat venous leg ulcers (6).
Hyperbaric Oxygen Therapy (HBOT)
HBOT can also be used as an adjunct treatment in which the patient breathes pure oxygen in a pressurized chamber to increase the amount of oxygen in the blood, which enhances wound healing (3).

Self Quiz
Ask yourself...
- Have you ever provided patient education on how nutrition impacts the immune system and wound healing?
Troubleshooting Tips
You may encounter complications with the wound dressing or the wound vac equipment. The most common complications associated with NPWT are pain, bleeding, and infection (7).
The wound therapy relies on an adequate seal similar to a regular vacuum, so a loss of suction can result in ineffective treatment. If loss of seal occurs, the nurse should assess the seal around the wound dressing and note if the transparent adhesive sealant tape has either been misapplied or has come off due to poor contact with the underlying skin.
A loss of suction could also result from incorrect placement of the suction drain tube, loss of battery power, blockage of the suction drain tube, or if the suction device is full of output (7). Sometimes the location of the wound leads to difficulty in keeping the dressing seal in place; for example, the abdomen or near joints, so movement can misplace the dressing and break the seal. Patient education is key to maintaining proper suction.
Troubleshooting Tips:
- Confirm the machine is on and set to the appropriate negative pressure.
- Make sure the foam is collapsed and the NPWT device is maintaining the prescribed therapy and pressure.
- Assess the negative pressure seal and check for leaks.
- Check for kinks in the tubing and make sure all clamps are open.
- Avoid getting the machine wet.
- Assess the drainage chamber to make sure it is filling correctly and does not need changing.
- Address alarm issues:
- Canister may be full
- Leak in the system
- Low/dead Battery
- The device should not be turned off for more than two hours without ordered discontinuation.
- If the device is off, apply a moist dressing and notify the provider immediately.

Self Quiz
Ask yourself...
- Can you name reasons the NPWT device may sound an alarm?
- Can you think of barriers to proper suction? (ex: kinks in tubing, full canister, etc.)
Case Study
Mr. Smith is a 59-year-old male presented to his primary care provider and referred to general surgery; diagnosed with lymphedema and multiple, copiously draining ulcerations on the left lower extremity.
The patient presented with lymphedema and multiple ulcerations on the left lower extremity with copious amounts of drainage. This is an ongoing, worsening issue for over 8 months and has failed to respond to compression, foam dressings, or hydrocolloid dressing.
The hospitalist has ordered surgical consultation, who scheduled debridement of the wounds and application of a wound vac following the procedure; Negative pressure wound therapy (NPWT) orders in place.
CHIEF COMPLAINT: "The sores on my feet are draining more and I can no longer go to work because my boots do not fit on my foot.” He also reports a loss of appetite, chills, and loss of sensation to his left lower extremity.
HISTORY OF PRESENT ILLNESS: Patient is a 59-year-old truck driver who has previous medical history of DM Type II, hypertension requiring use of anti-hypertensive medication, and hyperlipidemia (non-compliant with medication regimen). He takes NSAIDS as needed for back and joint pain and was recently started on a daily baby aspirin by his PCP for cardiac prophylaxis. He denies alcohol intake. He reports smoking a pack of cigarettes per day.
PHYSICAL EXAMINATION: Examination reveals an alert and oriented 59-YO male. He appears anxious and irritated. Vital sips are as follows. Blood Pressure 155/90 mmHg, Heart Rate 120/min - HR Thready - Respiratory Rate - 20 /minute; Temperature 98.0
ENT/SKIN: Facial pallor and cool, moist skin are noted. No telangiectasia of the lips or oral cavity is noted. Wound: 3 cm x 2 cm x 1 cm wound to lateral LLE. Wound base is dark red with yellow-green drainage present. Removed 4 x 4 dressing has a 5 cm diameter ring of drainage present. The surrounding skin is red, warm, tender to palpation, and with a dusky appearance to the entire LLE.
CHEST: Lungs are clear to auscultation and percussion. The cardiac exam reveals a regular rhythm with an S4. No murmur is appreciated. Peripheral pulses are present but are rapid and weak. A positive Stemmer sign was noted and palpable pedal pulses with mild symptoms of venous insufficiency were noted.
ABDOMEN/RECTUM: The abdomen reveals a rounded abdomen. Bowel sounds are present.

Self Quiz
Ask yourself...
- Discuss abnormal findings noted during History & Physical Examination.
- Evaluate additional data to obtain possible diagnostic testing, treatment, nursing interventions, and care plans.
- Discuss how the patient’s comorbidities may be attributed to prolonged wound healing.
- What suction settings would the nurse expect to be ordered?
Conclusion
Hopefully, upon completion of this course, you feel empowered and curious about the use of negative pressure wound therapy (NPWT). Wound vacs can be a powerful tool in combatting acute and chronic wounds, it is a well-documented concept throughout history.
The nurse should be knowledgeable on the integumentary system makeup and types of wounds this therapy is indicated for. The mechanism of action of NPWT is critical knowledge when assessing the healing of a wound. Adjunct treatment options and troubleshooting support tips are also meaningful in the care of patients with NPWT.
Nutritional Interventions to Promote Wound Healing
Introduction
The medical field is an ever-evolving and constantly changing arena. Advances in technology and an increased understanding of how the body works have produced newer and better procedures and techniques in healing. These initiatives, as innovative as they may be, still depend on the body’s ability to heal itself as the foundation of the recovery process.
In turn, the body needs proper nutrition to support the healing process within itself. Nutrition is often overlooked by nurses even though it is arguably the most critical aspect of physical healing.
Factors That Impact Wound Healing
Wound healing is a complex process. There are a myriad of factors that impact the body’s ability to heal and recover from an injury. Comorbidities, genetic disorders, medications, and, in some cases, disease treatments (chemotherapy, radiation, steroids, etc.) can all have the potential to slow, change, or interfere with normal wound healing (2). For this course, we will discuss a few of the more common factors that nurses will undoubtedly come across during their practice.
Diabetes
It is estimated that this growing, global disease will impact forty million people by the year 2030. It has been proven that diabetes is responsible for more than one hundred changes in wound healing.
These alterations have been seen across all four phases of wound healing. Platelet activation, epithelialization, collagen deposition, and granulation tissue formation are among the alterations that take place with diabetes. Worsening renal function/failure and peripheral vascular disease as a result of diabetes also affect the wound-healing process (2).
Renal Failure
Though most patients who have chronic kidney disease or renal failure also have multiple comorbidities that cause the renal problem, renal failure does, independently, bring a risk of diminished wound healing. Tissue edema, delayed granulation, chronic inflammation, and decreased vessel formation are all ways that renal failure impacts wound healing.
Hemodialysis, a life-sustaining treatment of chronic renal failure, adds fuel to the fire when it comes to risks of diminished wound healing. Protein and water-soluble vitamins and nutrients are lost through the dialysis process. This includes zinc and iron and will lead to deficiencies in these needed nutrients. Further, patients on hemodialysis and patients who receive a kidney transplant as treatment for renal failure are both at higher risk for developing infections (2).

Smoking
Smoking causes multiple alterations within the body at the molecular level that affect normal wound healing. Vasoconstriction caused by smoking worsens wound ischemia. The highly documented negative impact that smoking has on wound healing has led physicians to decline some elective surgeries due to the risk of poor wound healing (2).
Infection
It is not fully understood how infection alters wound healing. It is believed to be a multifactorial process that has a range of properties that can be progressive in nature; infection-necrosis-sepsis-death. The bacteria create an environment where the collagen that repairs the injured tissue is destroyed (2).
Obesity
Obesity complicates virtually every disease process including normal wound healing. Wound healing complications due to obesity include increased rates of infection, hematomas, and dehiscence. Local hypoxia is also a complication that impacts wound healing (2).
Age
Aging also has an impact on wound healing. During the aging process, the skin loses elasticity, thickness, and water content. There is also a decrease in the skin’s blood vessels as it ages, reducing the capacity for oxygenation and nutrients. Wound closure becomes slower with aging; by age forty, the amount of time for an identical wound to heal doubles from age twenty. After the age of fifty, dermal collagen decreases by one percent per year (2).
Malnutrition
Malnutrition or undernutrition has a variety of effects on wound healing. Good nutrition is essential for proper wound healing and the overall recovery of the body after an injury.
Malnutrition can lead to the loss of immune function which will affect the body’s response to infection. With malnutrition, the skin becomes thin and frail thus more apt to develop wounds. Pressure wounds are also more likely as fat deposits over pressure points become depleted. The lack of energy during malnutrition leads to immobility, increasing the possibility of wounds. Collagen synthesis is also decreased (5).

Self Quiz
Ask yourself...
- Name three factors that can affect wound healing.
- How does age and aging impact wound healing?
- What are two ways that malnutrition impacts wound healing?
Phases of Wound Healing
Once again, wound healing is a complex process. From a simple pin prick to a stage-four decubitus ulcer, the wound healing process itself remains the same. The body will go through the four phases of wound healing to repair the damage.
Hemostasis
The first phase of wound healing is hemostasis. Whether by surgery or trauma, the body attempts to achieve hemostasis at the time of the injury. The intrinsic and extrinsic coagulation cascades are activated by the body.
Vasoconstriction takes place while platelet aggregation occurs to form a fibrin clot. This is all in an effort of the body to stop the bleeding to bring about hemostasis. As the platelets arrive at the site of injury, cytokines and growth factors are released by the platelets to initiate the inflammation process (3) (4) (5).
Inflammation
Inflammation is the second phase of wound healing. It starts once hemostasis has been re-established. During this phase, the previous vasoconstriction reverses and the vessels dilate.
This brings blood to the injury site along with neutrophils, macrophages, monocytes, and other inflammatory cells. Phagocytosis is initiated and the wound is cleansed by the removal of bacteria. The wound site will swell and there may be some restrictions in mobility to the affected area (3) (5).
Proliferation
Phase three is proliferation. In this phase, rebuilding of the wounded tissue begins. The number of fibroblasts increases and begins to build a collagen network and prepare the wound base for new granulation tissue.
At the same time, new blood vessels are created; a highway for oxygen and nutrients to be supplied to the site. By the end of this phase, the foundation will have been laid for full epithelialization (3) (5).
Remodeling
The final phase of wound healing is remodeling. Epithelialization is in full swing once granulation tissue has filled the wound. This process stimulates skin integrity restoration.
Scar tissue is formed as proteins such as collagen and elastin along with keratinocytes are produced. The wound closes and begins to strengthen and appear “normal”; it may take a couple of years for the site to return to its fully functional pre-injured status (3).

Self Quiz
Ask yourself...
- How many phases of wound healing are there?
- Name all the phases of wound healing in order.
- What happens during the proliferation phase of wound healing?
How Does Nutrition Impact Healing?
Nutrition is, perhaps, the most important underlying aspect of wound healing. The mechanism of wound healing and the role nutrition plays in that process is very complex.
Adding nutritional interventions to the wound healing care plan is generally low cost and will increase the probability of a full recovery. Nutrition is essential for all phases of the healing process. It is the foundation of wound healing.
The malnourished patient will have difficulty progressing through the wound healing phases. Proper nutrition will also help prevent wounds such as pressure ulcers from developing in the first place.
Understanding which nutrients are needed through the phases of wound healing will help to devise a nutritional plan of care. Energy is required in all the phases of wound healing and is only made possible through proper nutrition (3).

Self Quiz
Ask yourself...
- In what phase of wound healing is proper nutrition essential?
Common Deficiencies
Nutrients and proteins are the building blocks of life. They are needed for growth, maintenance, and healing of the body. Many types of nutrient deficiencies greatly impact the healing process. Here, we will discuss some of the more common nutrient deficiencies.
Iron
Iron plays a key role in the synthesis of hemoglobin. Hemoglobin delivers oxygen throughout the body; oxygen is required through all phases of wound healing. Iron deficiencies can lead to anemia and decreased tissue perfusion. An iron deficiency will also affect protein synthesis, macrophage function, and overall wound strength (3) (6).
Vitamin A
When it comes to wound healing, vitamin A quickens collagen synthesis and the overall inflammatory phase. A deficiency in vitamin A decreases collagen production, epithelization, and tissue granulation (9).
Vitamin B
There are eight vitamins included in the vitamin B complex. Each of the eight vitamins has its own daily recommended intake. Vitamin B promotes cell proliferation and promotes normal metabolism. In the presence of a wound, some dietitians promote doubling the daily recommended intake of the B vitamins (3).
Vitamin C
Vitamin C (ascorbic acid) assists with iron absorption. It is also essential in the process of collagen formation. Without vitamin C, the immune response cannot take place as needed. There are many sources of vitamin C readily available for everyday consumption (6).
Zinc
Zinc is used through all phases of the wound-healing process. It is used to initiate and modulate enzyme function throughout the wound healing phases. It affects immunity and assists in fibroblast proliferation and collagen production. It is also needed for granulation tissue formation (5) (6).
Amino Acids
Protein and amino acids are another set of nutrients that are highly essential in wound healing. The blood’s most abundant amino acid, glutamine, provides the body’s preferred energy source, glucose. Increased levels of glutamine have been shown to help with wound strength and increase the levels of mature collagen.
Generally, the body is able to produce enough glutamine for regular function. In times of stress on the body, such as a wound, glutamine is sought out in the diet. Arginine assists in modulating the collagen deposits, increases new vessel formation, and aids in wound contraction (3).

Self Quiz
Ask yourself...
- Name three common nutrient deficiencies that the nurse may encounter.
- What are two amino acids that play key roles in wound healing?
- An iron deficiency can lead to what issues?
- Which phases of wound healing require zinc to complete the phase?
Special Considerations
Tube Feedings
Patients who use tube feedings or enteral feedings are in a unique situation when it comes to wound healing and nutrition. Once a proper nutrition assessment has been performed, a tailor-made nutrition-rich diet can be formulated and administered directly into the gut.
Studies have shown that different formulas with supplemental nutrients have increased the ability of the body to heal faster than those without supplements. With tube feedings, patients don’t need to prefer the taste of one formula over another as it is delivered through the tube.
The amount of formula can also be adjusted as the patient’s needs change. Though some formulas may have side effects such as diarrhea, the overall benefits usually outweigh such side effects (8).

Self Quiz
Ask yourself...
-
What considerations are there for patients with tube feedings?
-
What is a pitfall when using tube feedings to deliver full nutrition?
Chronic and Terminal Illness
Autoimmune, inflammatory, and cancers are among the chronic and terminal diseases that are under special consideration when it comes to wound healing. These types of diseases can interrupt the immune/inflammatory response of the body thus prolonging the phases of wound healing.
When a wound develops on a patient who is immunocompromised, there is a higher incidence of wound infection which will delay wound healing. In many of these diseases, there may be circulatory issues that decrease the body’s ability to provide the affected area with nutrient-rich blood.
Chronic illnesses often decrease the patient’s energy levels. This can lead to immobility and increases the risk of wounds developing.
Further, for many of these types of issues, the treatment itself can have adverse effects on wound healing. Chemotherapy, radiation therapy, and immunosuppressants all decrease the body’s ability to heal and increase the rates of infection in wounds (2).

Self Quiz
Ask yourself...
- What are three types of chronic or terminal diseases?
- What issue is an immunocompromised patient at risk for?
- What are two treatments for chronic illness that can affect wound healing?
Supplements
Nutritional supplements have been shown to improve wound healing and recovery outcomes. It is important that the supplements are given under the supervision of a provider as too much of some nutrients can have a detrimental effect on wound healing.
A proper nutrition screening should be performed on all patients with wounds so that the nutrition plan can be tailored to the individual patient. These improvements to wound healing with nutritional supplementation differ based on the type of wound and the overall health of the patient.
The patient should be monitored and reassessed regularly by a dietitian. Again, there is no cookie-cutter supplement regimen.
Another factor to consider with supplements is the ease of following the supplement regimen. Hard to swallow pills or foul-tasting food/liquids may have a negative impact on the patient’s ability to adhere to the supplement regimen.
Allowing the patient to choose (with the input of the provider) the method of supplement delivery along with a choice of flavors will help increase compliance with the prescribed regimen (1).

Self Quiz
Ask yourself...
- What should be done prior to starting dietary supplements?
- Who should assess and reassess a patient’s dietary status?
- Why is the method of supplement delivery important?
Patient Education
Throughout the entire wound healing process, patient education is a must. Not only is it important so that the patient can make an informed decision about their care, but the patient should understand what is going on with their bodies.
Education fuels compliance. A comprehensive nutrition assessment will not only provide a baseline of the patient’s nutritional status but will also help identify gaps in the patient’s understanding.
This is where the education can be focused to best help the patient meet their wound healing goals. Education must include which foods contain which nutrients, the amount of these foods to eat, and which foods will interact with the absorption processes of the nutrients.
Discussing normal daily requirements and the requirements needed during wound healing is also needed (1).

Self Quiz
Ask yourself...
- Why is education important when discussing nutrition and wound healing?
Conclusion
Nutrition plays a key role in wound healing. There are many factors that affect the body’s ability to acquire and use the needed nutrients. One of the most important considerations that we as healthcare providers need to put into practice is determining a patient’s nutritional status.
A nutritional assessment should be done on patients with wounds so that a proper plan of care can be developed. Often, nutrition is an afterthought when in reality it is the foundation on which other treatments should be built upon.
Once this has been established, the patient’s plan of care can be implemented and must include nutritional education. Needed supplements to increase the patient’s ability to heal can be added or removed as necessary when the reassessments have been completed.
Ostomy Management
Introduction
Newton's law of gravity states: what goes up, must come down; similarly, the normal human gastrointestinal system has a law that what goes in, must come out. When disease inhibits the normal process, ostomy procedures are a life-saving intervention.
There are around one million people living with an ostomy or continent diversion in the US, and approximately 100,000 ostomy surgeries are performed annually in the US (1). We will build a stronger understanding of various types of ostomies, indication for the need, site selection, stoma care, complications, and patient education.
Types of Ostomies
An ostomy is a surgically created opening that reroutes stool or urine from the abdomen to the outside of the body through an opening called a stoma (9). The term stoma refers to the portion of the bowel that is sutured into the abdomen (9).
When you look at a stoma, you are looking at the lining (the mucosa) of the intestine. The color is similar to the mucosa inside your mouth and cheek. Throughout various healthcare environments, you may hear the terms ostomy or stoma interchangeably. The purpose of an ostomy is to bypass a diseased portion of the gastrointestinal tract that is not functioning properly or has been removed (2).
Ostomies are placed proximal to the diseased area, comparable to building a dam in a river to stop the flow of fluid and divert it somewhere else. An ostomy can be temporary or permanent.
There are three most common types of ostomies: ileostomy, colostomy, and urostomy (9). We will discuss these types, but it is important to recognize that gastrostomy, jejunostomy, duodenostomy, and cecostomy procedures are also done.
- Ileostomy: A stoma is attached at the end of the small intestine (ileum) to bypass the colon, rectum, and anus.
- Colostomy: A stoma is attached to a portion of the colon to bypass the rectum and anus.
- Urostomy: A stoma is attached to the ureters (the tubes that carry urine from the kidney to the bladder) to bypass the bladder.
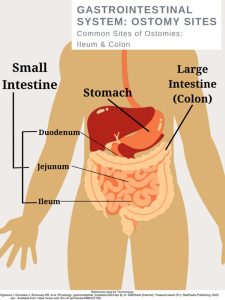
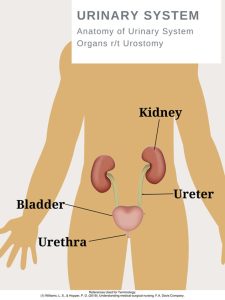
Ileostomy
The small intestine has three parts that are compact and folds over itself: the duodenum, jejunum, and the ileum. An ileostomy has a stoma attached and created from the ilium. The ileum is the final and longest segment of the small intestine (9).
The ileum terminates at the ileocecal valve, which controls the flow of digested material from the ileum into the large intestine and prevents the backup of bacteria into the small intestine (9). If a patient has this type of ostomy, the colon distal to the ostomy has a form of disease or disorder such as cancer. There are two main types of ileostomies, loop, and end ileostomy.
Loop ileostomy
In a loop ileostomy, a loop of the small bowel is lifted and held in place with a rod due to resection or repair to the distal bowel (Will). This ostomy is technically two stomas joined together (4). Loop ileostomies are typically temporary and will be closed or reversed through an operation in the future.
End ileostomy
In an end ileostomy, the ileum is surgically separated from the colon, the colon is removed or left to rest, and the end of the ileum is brought to the surface through the abdomen to form a stoma. Although end ileostomies are sometimes temporary and later rejoined, they are usually permanent (9).
Colostomy
A colostomy may be formed as an ascending, transverse, descending, or sigmoid colostomy (9). It is named according to the location of placement. An end colostomy is constructed from the ascending, transverse, descending, or sigmoid colon and has one opening for fecal elimination.
Loop Colostomy
The creation of a loop stoma takes a loop of the colon (usually the transverse colon) and pulls it to the outside of the abdominal wall (9). In this type of ostomy, the entire bowel is not dissected but left mostly intact.
End Colostomy
In end colostomies, the proximal end of the colon is dissected and pulled out of the abdominal cavity, which becomes the stoma (9). Additional procedures may involve repairing or removing portions of the distal colon or rectum.
Urostomy
Kidneys have an important job of filtering waste and excess fluid from your blood. This process creates urine, which then travels from the kidneys to the bladder through tubes called ureters (8). If the bladder is damaged or diseased, ostomies are a life-saving method of creating safe passage for the urine.
A urostomy is a surgical opening in the abdominal wall that redirects urine away from a bladder that’s diseased, has been injured, or isn't working properly (8). The bladder is either bypassed or removed (called a cystectomy) during surgery. Following the surgery, urine exits the body through a stoma.

Self Quiz
Ask yourself...
- Have you ever witnessed a GI or Urinary Surgery?
- Do you have experience with GI / Urinary procedures like a colonoscopy?
Indication for Ostomy Placement
Gastrointestinal Tract Ostomy
- Cancer
- Colorectal
- Rectal
- Trauma/ Injury
- Significant Disorders
- Crohn’s disease
- Ulcerative Colitis
- Diverticulitis
- Bowel perforation from a ruptured diverticulum or abscess
- Bowel obstruction
- Infection (9)
Urinary Tract Ostomy
- Bladder Cancer
- Neurogenic bladder disease (damage to the nerves that control the bladder)
- Birth defects
- Chronic inflammation of the bladder (9)

Self Quiz
Ask yourself...
- Have you cared for a patient with a new ostomy?
- Can you list reasons a patient is a candidate for an ostomy?
Site Selection
Wound, ostomy, and continence nurses (WOCN) play a vital role in site selection. Patients should have a pre-operative consultation prior to surgery. During this consultation, the nurse acts as an advocate and educator to prepare these patients for the physical and emotional path ahead of them. A significant amount of time should be spent with the patient before surgery to determine a stoma incision site (exit of ostomy).
It is important to make the presence of the ostomy (and collection bag) as comfortable as possible, striving to reduce the hindrance to ease movements and ability to wear their typical clothing (9). Studies show that preoperative education and stoma site marking has been directly responsible for improving quality of life and decreasing peristomal skin and pouching complications (4).
Site Assessment:
Locate positions for a site within the rectus muscle (4).
Observe the abdomen in various positions sitting, standing, or lying down.
Ask the patient about the types of clothing they wear most often. Examples: Level of pants (low, high), use of belts, dresses, etc. (9)
Determine a location that is visible to the patient, as they will need to see the site well for stoma care.
Avoid skin or fat folds (folds increase chances of leakage)
Avoid scars, bony prominences, and the umbilicus (4).

Self Quiz
Ask yourself...
- Locate places on yourself that would be appropriate for an ostomy site
- Can you think of reasons patients need to be able to see the site?
- Do you have a wound care nurse at your past or present workplace?
Post-operative Care
Post-operative care following ostomy placement is vital. The post-operative nurse assigned to this patient should read the surgery documentation to determine the type of procedure performed, intraoperative findings, type of stoma created, any advanced diseases, and unexpected events during surgery (2).
The nurse should be aware of the level of invasiveness; was this a laparoscopic, robotic, or open surgery? This type of surgery can have an impact on the post-op care plan and length of stay (2). Teaching can begin as soon as they are able to comprehend and focus on understanding new skills.
The stoma will gradually decrease in size over the weeks following the surgery. For a patient with a new ostomy, postoperative assessments should be done per facility protocol and the stoma should be inspected at least every 8 hours (9).
Note the type of closure (staples, sutures, liquid bonding agent), presence of abdominal drains, and presence of urinary catheter (C2). Assess for pain and address accordingly with repositioning, cold/heat therapy, and ordered pain medications. Assess for bowel sounds. Palpate the abdomen and note firmness and tenderness levels. Document strict Intake and Output for these patients.
Stoma Assessment:
Note the Appearance/ Color: The stoma should be pink to red in color, moist, and firmly attached to the surrounding skin (9). If the stoma appears bluish, it indicates inadequate blood supply; if the stoma appears black, necrosis has occurred. Immediate notification is needed from the provider, as the need to return to surgery will be assessed.
- Note the Presence of edema.
- Note the Surrounding skin
- Note any Ostomy Discharge
- Amount
- Color / Consistency
- Note any Bleeding
- Monitor for rupture or leakage.
Diet
Once bowel sounds and activity return, the patient’s diet may resume (2). Typically, patients are offered clear liquids to determine their ability to tolerate fluids. Nurses should encourage the patient to chew thoroughly, eat small frequent meals, and ambulate frequently to assist in gas movement and peristalsis (2).

Self Quiz
Ask yourself...
- Do you have experience with post-operative abdominal surgery?
- Explain possible respiratory or cardiovascular assessments that would be helpful for these patients
Stoma Care
Nursing Consideration / Reminders
Ostomy pouching system needs to be changed every 4 to 7 days, depending on the patient and type of pouch.
Patients should be encouraged to participate in stoma care. Instruct the patient to empty the pouch when it is one-third to one-half full as they become heavy and more prone to spilling or leaks.
Table 1. Ostomy Change Procedure SAMPLE (Always check with your agency policy)
| Steps | PURPOSE |
| 1. Perform hand hygiene. | This prevents the spread of germs and microorganisms. |
| 2. Gather supplies. |
Supplies:
|
| 3 Create privacy. Lift bed to comfortable height. |
Attention to psychosocial needs is imperative. Proper body mechanics is important for nurse. |
| 4. Place waterproof pad under pouch. | The pad prevents the spilling of effluent on patient and bed sheets. |
|
5. Remove ostomy bag. Apply non-sterile gloves. Support / hold the skin firmly with your other hand, apply adhesive remover if needed. Measure and empty contents. Place old pouching system in a garbage bag.
|
The pouch and flange can be removed separately or as one. Gentle removal helps prevent skin tears. Remove flange by gently pulling it toward the stoma. |
| 6. Clean stoma gently by wiping with warm water. Do not use soap. |
Aggressive cleaning can cause bleeding. If removing stoma adhesive paste from skin, use a dry cloth first. Soaps can irritate the stoma. Clean stoma and peristomal skin |
| 7. Assess stoma and peristomal skin. |
Stoma skin should be pink or red in color, raised above skin level, and moist (2). Skin surrounding the stoma should be intact and free from wounds, rashes, or skin breakdown. |
|
8. Measure the stoma diameter using the pre-cut measuring tool (or tracing template). Trace diameter of the measuring guide onto the flange and cut the outside of the pen marking. |
The opening should match the size of stoma. If there is skin exposed between the stoma and edge of the flange with an ileostomy, the drainage contains enzymes that will break down the skin (9). Cut out size to fit stoma, assess fit once cut. |
|
9. Prepare skin.
|
Paste can be applied directly to the skin or flange. |
|
10. Apply Flange
|
Press gently around the periphery of the stoma to create a seal |
|
11. Apply the ostomy bag Close the end of the bag with clip (follow the manufacturer’s instructions) |
Involve patient with this process, understanding instructions. |
| 12. Apply pressure to ostomy pouch to help with adhering to skin. | Heat/ warmth from hand can activate some flanges. |
| 13. Clean us supplies, perform hand hygiene. | Remove trash as quickly as possible to reduce odor. |
| 14. Document Procedure |
Example: Date/time: flange change complete. Stoma pink, moist, warm. Peristomal skin intact. Patient instructed in cutting flange to correct size, verbalized understanding of frequency of change. See ostomy flowsheet. (Abbie S., RN) |
| Data Source: Carmel, Colwell, J., & Goldberg, M. (2021). Wound, ostomy and continence nurse’s society core curriculum: ostomy management (Second Edition). Wolters Kluwer Health. | |

Self Quiz
Ask yourself...
- Are you familiar with your facility's ostomy care protocol (if appropriate)?
- How can the nurse implement safety measures with ostomy care?
- Do you feel comfortable with ostomy care documentation?
Complications
Ostomy Leakage
One of the most common and troublesome complications is leakage (4). Proper preoperative site selection (away from skin folds) is important. Patient education on proper techniques and supplies can aid in the prevention of leakage.
Educate patients on the risks of changing the ostomy too often. Frequent appliance changes lead to pain and frustration, as well as financial expenses on supplies (4). Leakage is more common in the early postoperative period but can also develop with weight changes later.
Interventions involve thickening the stool with antidiarrheals to form more solid excretion and pouching techniques to bolster the height of the stoma off of the peristomal skin (4). Helpful tips also include heating the appliance with a hair dryer before application, lying flat for several minutes following application, making sure the peristomal skin is dry before application, and the possible use of a fine dusting of stomal powder and skin sealant prior to application (4). Leakage is frustrating for patients, so support and encouragement is vital.
Mucocutaneous Separation
The stoma is sutured to the skin of the abdomen with absorbable sutures during surgery (4). Mucocutaneous separation is a complication that can occur if the sutures securing the stoma become too tight or if blood flow to the area is restricted (9). This complication requires appropriate treatment because the pouch leakage will occur from the open pocket.
The goal of treatment is to keep this open pocket covered properly until the wound heals on its own and closes. Appropriate covering of the opening can include an absorbent product such as an alginate, followed by a cover dressing such as a hydrocolloid, which is covered with the ostomy pouch (4).
Early High Ostomy Output
Early high ostomy output (HOO) is defined as ostomy output greater than fluid intake occurring within 3 weeks of stoma placement, which results in dehydration (4). This is more common with ileostomies (4). Strict Input and Output records are a vital nursing intervention. The most important treatment for this complication is hydration to prevent renal failure, which is typically done intravenously (4).
The site of a patient’s colostomy will impact the consistency and characteristics of the excretion. The natural digestive process of the colon involves the absorption of water, which causes waste from the descending colon to be more formed. Waste from an ileostomy or a colostomy placed in the anterior ascending colon will be a bit more loose or watery (2).
Peristomal Skin Issues
Irritant Contact Dermatitis (ICD) is the most common peristomal skin complication following ostomy placement (9). ICD is characterized by redness; loss of epidermal tissue; pain; and open, moist areas.
Newer and inexperienced patients and caregivers will increase the size of the pouching system opening to get a better seal and stop leakage (2) However, this only contributes to more skin breakdown and irritation. Patients may also develop a fungal rash, have allergic rashes to the ostomy appliance, or folliculitis (4).

Self Quiz
Ask yourself...
- Can you name measures to prevent leakage?
- Have you cared for a patient with Irritant Contact Dermatitis?
- Are you familiar with bulking agents for stool?
Patient Education
Patient education is a key aspect is caring for a patient with an ostomy, this process begins prior to surgery and remains constant throughout encounters. If you have not received specialized training on wound and ostomy care, you should reach out to the Wound, Ostomy and Continence Nurse (WON) within your healthcare setting to become involved if they are not already.
However, each nurse has a meaningful impact on discussing and managing expectations for life with an ostomy, including stoma care, complications, managing ostomy output, maintaining pouching appliances, and resources. Patients may feel inadequate and uneasy about caring for their stoma.
Nurses need to meet the unique learning needs of each patient and caregiver, providing education in verbal information, written pamphlets, online resources, videos, and demonstrations. The United Ostomy Associations of America, Inc. (UOAA), is a nonprofit organization that serves as an excellent resource for information, support, advocacy, and collaboration for those living with ostomies.
Nurses should be aware there is an “Ostomy and Continent Diversion Patient Bill of Rights” (PBOR) that outlines the best practices for providing high-quality ostomy care during all phases of the surgical experience (1). There are numerous national resources for patients, as well as community-based and online ostomy support groups.

Self Quiz
Ask yourself...
- Can you think of methods to assess patient knowledge on ostomy care?
- What are creative ways to involve an ostomy patient in care?
- Not all patients are savvy with online supply ordering, can you think of other ways to order supplies if they are not?
Promotion of Body Image and Self-Esteem
Ostomy surgery can have a major impact on how patients perceive themselves. A person’s body image is how they see themselves when they look in the mirror or how they picture themselves in their mind.
There are stigmas surrounding ostomies, such as being odorous, unhygienic, and unattractive due to the stoma, but the truth is that ostomies save lives and make life possible. Positivity should surround the conversation. Confirmations such as beauty, strength, celebration, and hope are meaningful.
Ways to become involved in celebrating ostomies:
- Become familiar with the United Ostomy Associations of America (UOAA) and their initiatives.
https://www.ostomy.org/ostomy-awareness-day/
National Ostomy Awareness Day on October 7, 2023
Worldwide Virtual Run for Resilience Ostomy 5k
- Social Media Sites
Celebrate Body Positivity for those with ostomies
Intimacy Encouragement
Conclusion
Ostomy care is an essential nursing skill. If you are caring for a patient with an ostomy, remember that this is a major life-altering event and condition. Reflect on ways to provide individualized care by understanding various types of ostomies, site selection, stoma care, complications, and patient education. Empower and encourage these ostomy patients’ confidence in themselves.
Diabetes Management Updates
Introduction
Diabetes Mellitus (DM), also known as diabetes, is a condition in which the body develops high levels of blood glucose due to the inability to produce insulin or for the cells to use insulin (1) effectively. If left untreated or mismanaged, it can lead to health complications such as heart disease, chronic kidney disease, blindness, nerve damage, oral and mental health problems (1)(15).
There are several classifications of DM, and the following will be discussed: T1DM, T2DM, gestational diabetes, and idiopathic diabetes.
Classifications of Diabetes
Type 1 Diabetes Mellitus (T1DM)
T1DM is formerly known as juvenile diabetes or insulin-dependent diabetes and usually occurs in children and young adults (1). Although, it can also occur at any age and accounts for 5 – 10% of cases. T1DM develops when one’s own immune system attacks and destroys the beta cells that produce insulin in the pancreas (6).
Type 2 Diabetes Mellitus (T2DM)
T2DM, formerly known as adult-onset diabetes or non-insulin-dependent diabetes, develops because of the body's inability to use insulin effectively. It is the most common type of diabetes and mainly occurs in adults aged 30 years and older (1). However, it is also becoming common in children and young adults due to obesity. It accounts for 90% of the population diagnosed with diabetes (6).
Gestational Diabetes
Gestational Diabetes occurs during pregnancy and in women who have never had a previous diagnosis of diabetes. It is a result of pregnancy hormones that are produced by the placenta or because of the insufficient use of insulin by the cells (1). Gestational diabetes can be temporary or in some cases can become chronic. It is also likely that children whose mothers have gestational diabetes can develop diabetes later in life (6).
Prediabetes
Prediabetes, also referred to as impaired glucose tolerance, is a stage when a person is at risk of developing diabetes. If well managed through proper diet management and exercise, this can help with the prevention or delay of type 2 diabetes (1).
Other Forms of Diabetes
Other forms of diabetes include monogenic diabetes syndrome, diabetes from the removal of the pancreas or damage to the pancreas from disease processes such as pancreatitis or cystic fibrosis, and drugs or chemical-induced diabetes from glucocorticoids used to treat HIV/Aids or organ transplant (1) (6).

Self Quiz
Ask yourself...
- What are the four named types of diabetes?
- What are the differences between T1DM and T2DM?
- What is the most common type of diabetes?
Statistical Evidence/Epidemiology
Diabetes is now ranked as the 8th leading cause of death in the United States (6). There is no known cure for diabetes. It is one of the fastest-growing chronic diseases and the most diagnosed noncommunicable disease. It is also one of the leading causes of chronic kidney disease, adult blindness, and lower limb amputations (6).
In 2019, it was estimated that 37.3 million American adults have diabetes, which equals 11.3% of the population (4). Of those, 41% were men and 32% were women. 28.7 million were diagnosed with diabetes, and 8.5 million were undiagnosed.
There are 96 million American adults who are prediabetic, which means they are at risk of developing diabetes, but their blood glucose levels are not high enough to be diagnosed with diabetes (5).
Most of the population that is pre-diabetic is 65 years old or older. Type 2 diabetes accounts for 90% to 95% of cases (5). The risk of developing diabetes increases with age.
The prevalence of diabetes is much higher in both black and Hispanic/Latino adult men and women. Men are more likely to develop diabetes compared to women. Due to the rise in obesity in younger adults, there has been an increase in the number of new cases of diabetes in black teens (4).
The figure below represents trends in incidence of type 1 and type 2 diabetes in children and adolescents 2002–2018; results show the incidence of type 2 diabetes has significantly increased (4)
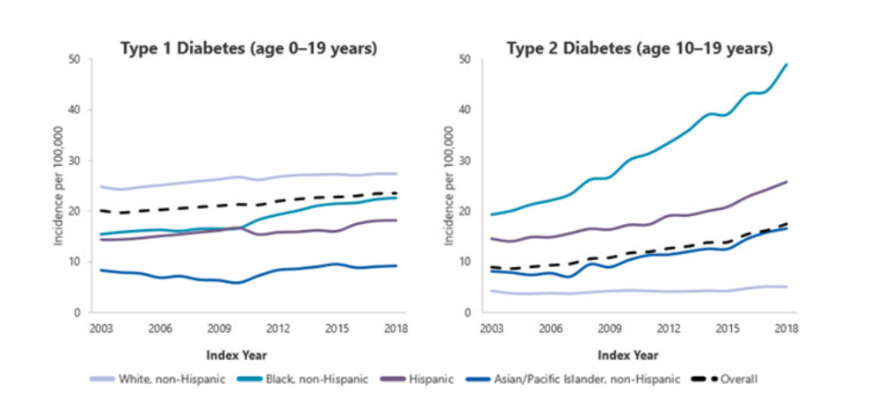

Self Quiz
Ask yourself...
- What is one of the major comorbidities caused by diabetes?
- What age group is at risk for developing type 2 diabetes?
- What is a risk factor that is contributing to the rise of diabetes in younger adults?
Etiology and Pathophysiology
In normal glucose metabolism, blood glucose is regulated by the two hormones insulin and glucagon (11). Insulin is secreted by the beta cells in the Islet of Langerhans in the pancreas and glucagon is secreted by the alpha cells in the pancreas.
When there is an increase in blood glucose, the function of insulin is to reduce blood glucose by stimulating its uptake in the cells. Glucose is stored as glycogen in the liver and muscles or as fat in the adipose tissues. When blood glucose levels start to fall, glucagon promotes the release of glycogen from the liver, which is used as a source of energy in the body (8) (13).
When there is a deficiency of insulin or a decreased response of insulin on the targeted cells in the body, it leads to hyperglycemia (high blood glucose). Meaning that the glucose that remains in the blood is not able to get to the cells. Diabetes develops mainly because of lifestyle and genetic factors (13).
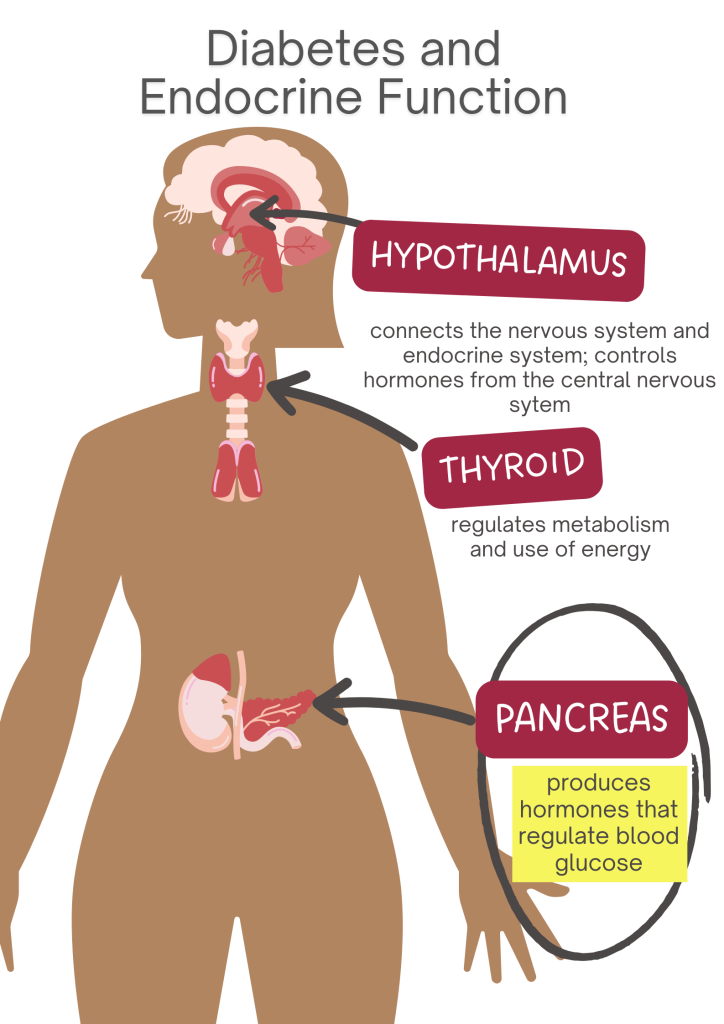
T1DM
The etiology is not well understood, though it is thought to be influenced by both environmental and genetic predispositions that are linked to specific HLA alleles. T1DM is considered an autoimmune disorder that is characterized by T-cell-mediated destruction of the pancreatic B-cells (13).
As a result, this leads to complete insulin deficiency and ultimately hyperglycemia, which requires exogenous insulin. The rate of destruction of the pancreatic B-cell-specific disorder is known to develop rapidly in infants and children or gradually in adults (8)(13).
T2DM
The etiology of T2DM is characterized by decreased sensitivity to insulin and decreased secretion of insulin. Insulin resistance occurs due to the disruption in the cellular pathways that result in a decreased response in the peripheral tissues, particularly the muscle, liver, and adipose tissue.
T2DM diabetes can progress slowly and asymptomatically over a period. Obesity and age can play a key role in the homeostatic regulation of systemic glucose because they influence the development of insulin resistance, which affects the sensitivity of tissues to insulin. Therefore, most patients with type 2 diabetes are overweight or obese 7) (8).

Self Quiz
Ask yourself...
- What are the two hormones that are responsible for maintaining blood glucose levels in the body?
- Can you describe the etiologies of both T1DM and T2DM?
- What are some of the factors that contribute to T2DM?
Diagnostic and Screening tools
There are a variety of tests that are used to diagnose and monitor diabetes. These vary based on the type of symptoms that a patient may have. Diagnosis of DM requires at least two abnormal test results, which should include fasting glucose and A1C. The tests should be one of two from the same sample or two abnormal test results drawn on different days (3).
The recommended diagnosis guidelines for diabetes must be based on the following criteria:
- Fasting Plasma Glucose (FPG) concentration with results greater than 126 mg/dL. This test involves measuring blood glucose at a single point. To have accurate results, the test should be conducted after one has had nothing to eat or drink for at least 8 hours (3).
- Glycated hemoglobin (Hb A1C) is indicative of the average levels of blood glucose in a period of two to three months. Results greater than 6.5% mean diagnosis of diabetes. This blood test does not require fasting. The A1C test is not suitable for pregnant women or those who have certain blood conditions (anemia) - NIDDK. This test should only be used for prediabetes screening (3).
- Oral Glucose Tolerance Test (OGTT): prior to conducting this test, an FPG level needs to be measured. One must ingest 75 grams of glucose liquid. Thereafter, their glucose level is measured 2 hours after they have taken the liquid. Test results greater than 200 mg/dL are indicative of diabetes. This test is commonly used in pregnant women (3).
- Random plasma glucose of 200 mg/dL. This test is suitable when one has symptoms of hyperglycemia, which are polydipsia, polyuria, and polyphagia (3).
Screening
Screening is generally recommended for adults aged 45 or older regardless of present risk factors. The updated recommendation guidelines for prediabetes screening include adults 35 years and older who are overweight or obese (3).
Screening for Prediabetes
Prediabetes is associated with the impairment of blood glucose levels between 100 – 125 mg/dL. The diagnosis of prediabetes should be confirmed with glucose testing when there is impaired glucose tolerance with plasma levels between 140 – 199 mg/dL 2 hours after one has ingested 75g of oral glucose. A1C levels of prediabetes are between 5.7% to 6.4% (3).
Screening for Pregnant women
It is recommended that all pregnant women between 24 – 28 weeks be screened for gestational diabetes to avoid missing those that are at risk. A positive 3-hour OGTT test of greater than 140 mg/dL meets the criteria for diagnosis (3).
Medication Management
Monitoring of blood glucose levels in patients is useful in determining the effectiveness of antidiabetic medication. To achieve better patient outcomes, it is important to recognize individual needs (11).
It is recommended that the approach to medication management should be based on each patient's hyperglycemic index and should include the following: the presence of comorbidities, risk of hypoglycemia, vascular disease, life expectancy, and disease duration (3).
When the management of diabetes cannot be achieved through diet and exercise alone, oral antidiabetic agents are the preferred treatment (14). Oral antidiabetics can help maintain and achieve glycemic goals for patients who are diagnosed with T2DM) (10)(14).
Diabetes Education and patient engagement is essential to managing diabetes (11). There are several classes of anti-diabetic medication. Below are some of the most utilized antidiabetic medications (9)(14).
Biguanides
Metformin is the only medication in this category.
- It is considered the 1st line of treatment in patients with T2DM unless contraindicated.
- Metformin helps to decrease hepatic glucose production.
- Decreases intestinal absorption of glucose by improving insulin sensitivity. Must be titrated initially to minimize adverse effects.
- Avoided in clients with chronic kidney disease.
- Side effects: Lactic acidosis, hypoglycemia.
GLP 1- Receptor Agonists (RAs)
Mimics glucagon-like peptide 1 (GLP -) hormone. Binds to GLP-1 receptors stimulate glucose-dependent insulin release and delay gastric emptying, which increases satiation.
- Known to have cardiovascular benefits.
- Can be taken orally or subcutaneously.
- Special considerations: Can cause weight loss, GI side effects such as nausea, vomiting and diarrhea, dehydration, increased satiation (fullness), acute pancreatitis, and reactions at the injection sites.
- Some labels may require renal dose adjustment.
- GLP - 1 RAs should be considered before starting clients on insulin to help reduce A1C then oral antihyperglycemic medications are not effective in treating diabetes.
Sulfonylureas 2nd generation
Stimulates insulin release in pancreatic beta cells.
- Risk for prolonged hypoglycemia. Therefore, it should be avoided with the concurrent use of insulin.
- Can cause weight gain.
- Can cause photosensitivity.
- Avoid use in clients with sulfa allergies and photosensitivity.
- Avoid use in clients with chronic kidney disease and liver disease.
Dipeptidyl Peptidase (DPP) - 4 inhibitors
Prevents DPP-4 enzymes from breaking down to GLP-1 hormone.
- Neutral weight.
- Monitor for acute pancreatitis, which can cause joint pain.
- May require renal dose adjustment with these brands: Saxagliptin (Onglyza), Sitagliptin (Januvia), and Alogliptin. Linagliptin does not require dose adjustment.
Sodium-Glucose transporter - 2 (SGLT-2) inhibitors
Reduce the reabsorption of glucose by up to 90%, therefore promoting the exclusion of glucose from the body.
- Known to have cardiovascular benefits for clients with cardiovascular disease.
- Use with caution in clients with increased risk of fractures.
- Avoided in clients with diabetic ketoacidosis and those prone to have frequent urinary tract infections.
- This medication should be avoided in clients with pure poor kidney function due to volume depletion and hypotension.
- There’s also a risk for Fournier gangrene.
Thiazolidinediones
Pioglitazone and rosiglitazone can help reduce insulin resistance which promotes improved sensitivity to insulin. As a result, it can help reduce the A1C levels.
- Can cause weight gain.
- Potential risk for heart failure when taking thiazolidines (brands: pioglitazone, rosiglitazone).
- Generally, it is not recommended for clients with renal impairment as medication has the potential to cause fluid retention.
- Risk for bone fractures, bladder cancer, and increased LDL cholesterol (rosiglitazone).
- Thiazolidines do not cause hypoglycemia and can be used in combination with other antidiabetic medications including insulin.

Self Quiz
Ask yourself...
- Which class of antidiabetic medications are known to put patients at risk for bone fractures?
- Can you name a condition that thiazolidines and sulfonylureas 2nd generation are generally not recommended for?
- What is a common side effect in both thiazolidines and sulfonylureas?
- What class of medication is suitable for clients with insulin resistance?
- Can you name two antidiabetic medications that can be used in combination with other antidiabetics because it has the benefit of not causing hypoglycemia?
Insulin therapy
Insulin therapy is commonly recommended for patients with T1DM. It can be used to help prevent the development and progression of diabetes (2). The ideal insulin regimen should be tailored based on individual needs and glycemic targets to better contend with physiological insulin replacement to maintain normoglycemia. Insulin therapy is also recommended for patients with hemoglobin A1c of greater than 9% - 10% and when symptoms of hyperglycemia are present (3).
Other Diabetes Interventions
The automation of glucose monitoring devices and insulin delivery systems is revolutionizing glucose management mainly because it promotes lifestyle flexibility and improved glucose management (2).
- Glucose Monitoring Devices- these devices are ideal for clients who are on insulin regimens and may become the standard for assessing glycemic controls in clients with DM (7).
- Continuous Glucose Monitoring (CGM)- devices that are inserted subcutaneously and measure interstitial blood glucose levels. CGMs are devices that are used to provide glucose readings, trends, and alerts to the user in real-time to inform diabetes treatment decisions. (2)(3)
- Importance- CGM is recommended for all patients with diabetes who receive treatment with intensive insulin therapy, defined as three or more insulin injections per day for all individuals with hypoglycemia (frequent, several, nocturnal) (3).
- Known to reduce hyperglycemia and A1C levels.
- Insulin Pump Therapy- also known as Continuous Subcutaneous Insulin Infusion (CSII) has had notable advances over the years. CSII is recommended for those with type 1 diabetes, although in recent studies, conventional CSII is also recommended for use in T2DM patients (2)(3). CSII is a small computer that is programmed to deliver fast-acting insulin continuously to the body using mechanical force via a cannula that is inserted under the skin (2).
- It is more precise and flexible in insulin dosing.
- Known to improve glycemic control.
- Cheaper than using Multi-Dose Insulin.
- Automated Insulin Delivery Systems (AIDS) - This is a diabetes management system that utilizes an insulin pump in conjunction with an integrated CGM and computer software algorithm (3).
- Advantages: precision and flexibility with insulin dosing.
- Recommended for T1DM: Achieve glycemic targets with less burden.

Self Quiz
Ask yourself...
- What is the main type of insulin used in CSII pumps?
- What type of diabetes category is more suitable for using CSII?
Upcoming Research
Islet cell transplant has been a biological solution to help treat patients with T1DM due to poor graft survival rates. Future research will focus on manipulating the beta cells in the pancreas to make them more viable. Other treatments that have been recently made available include incretins and Amylin which improve the absorption of insulin in the body (1).
- The development of other types of insulin that can be administered by inhalation.
- The development of immunosuppressant drugs that will help treat T1DM.

Self Quiz
Ask yourself...
- Can you name two recently developed medications to help with insulin absorption in the body?
Conclusion
Diabetes is a complex disease that requires a multi-disciplinary and patient-centered approach to help with effective management. Regular and early screening are necessary for those at risk for developing diabetes. Most importantly, ease and access to choices of managing diabetes are necessary.
Hospice and Palliative Care: What’s the Difference?
Introduction
Hospice and palliative care are unique health concepts often incorrectly used interchangeably. During my career as a hospice and palliative care nurse, I often heard the question, "What's the difference between Hospice and Palliative Care?"
I usually answered with a common phrase the Hospice and Palliative Care community uses to explain the difference, "All Hospice is palliative care, but not all Palliative Care is hospice." The statement is accurate but still confusing.
This course aims to shed light on these topics and emphasize the importance of enhancing end-of-life care, but let's start with Merriam-Webster's dictionary definitions.
- Hospice: "a program designed to provide palliative care and emotional support to the terminally ill in a home or homelike setting so that quality of life is maintained, and family members may be active participants in care” (4).
- Palliative: "relieving or soothing the symptoms of a disease or disorder without effecting a cure” (4).
The Merriam-Webster definitions help to clarify the differences further: Hospice is a program, and palliative care is a practice. They are two distinct approaches to providing comprehensive medical care and support for patients with serious illnesses, and they have essential differences worth exploring.
This course aims to delve into the different types of care, their philosophy, eligibility criteria, duration of services, and common myths and misconceptions surrounding hospice and palliative care. Additionally, it highlights nurses' crucial role as advocates and resources in these specialized fields.

Hospice Care
The modern hospice movement originated in the late 1960s in the United Kingdom, primarily through the work of Dame Cicely Saunders. Saunders, a nurse, and social worker, recognized the need for specialized care for patients with terminal illnesses. She founded St. Christopher's Hospice in London in 1967, which became the model for modern hospice care (12).
Saunders emphasized care that was less focused on disease treatment and more focused on an individual's physical, emotional, social, and spiritual needs. This approach prioritized providing comfort, pain management, and dignity for patients nearing the end of life (12).
The concept of hospice care gained international recognition and spread to other countries. By 1974, the first hospice program in the US was formed in Connecticut, and the hospice movement expanded rapidly (11).
Hospice care was primarily provided by volunteers who went into families' homes to care for their loved ones when no curative care was available. These same volunteers helped write the federal regulations adopted as the Medicare Hospice Benefit (MHB) in 1982 (5).
It is essential to discuss the MHB because the US government benefit made hospice a fundamental part of comprehensive medical care. It is the benefit through which most patients nearing the end of life receive care, and it has defined how we provide hospice care throughout the United States.
An integral part of hospice care is visits from a nurse, social worker, chaplain, and nurse aides. In addition, the patient and family have access to a hospice physician specializing in Hospice and Palliative Care (5). Hospice care focuses on providing compassionate, holistic, patient-centered care for individuals with terminal illnesses. The primary goal is to enhance the quality of life for patients and their families by addressing physical, emotional, social, and spiritual needs (5).
The MHB covers 100% of the financial cost for hospice services, including medications, supplies, and treatments required due to a terminal illness. The medicines commonly covered under the hospice benefit are for treating pain, nausea, anxiety, and other distressful symptoms, such as constipation (5).
Who can receive this care?
The MHB was designed for patients who are terminally ill with a six-month life expectancy, as determined by a physician (5). Life expectancy is one of the critical differences between Palliative Care and Hospice Care.
Healthcare providers, unlike statisticians or actuaries, are unskilled at predicting a six-month or less life expectancy. As part of the hospice federal regulations, local coverage determinations set by government intermediaries help healthcare providers determine who meets the criteria and, therefore, is eligible for hospice.
Key indicators predicting the end of life due to a specific disease process have been defined so that we can compare each patient to determine their eligibility for hospice care. Some key indicators are activity level, the times the patient has sought emergent care or has been hospitalized in the past six months, weight loss, and neurological status.
Patients generally receive hospice care when curative care is no longer an option. This is another crucial difference between Hospice and Palliative Care. There are exceptions, commonly for children, where curative and hospice care are provided. This is termed "concurrent" care.
How long do they receive services?
The key indicators that hospice physicians use to determine eligibility are based on averages of patients who have died with the specifically defined disease process. However, the average time to death is unreliable when judging how long an individual may live.
Therefore, hospice care is provided for as long as the patient's condition remains terminal, according to local coverage determinations, and they choose to continue receiving this specialized type of palliative care. In fact, the MHB has no end date, and the duration of services may vary depending on the progression of the illness and the patient's preferences.
For example, patients with chronic illnesses, such as heart failure, chronic obstructive pulmonary disease (COPD), and Alzheimer's, tend to have a less predictable trajectory of terminal illness due to periods of exacerbation and stability, which are common. Patients with chronic diseases tend to have a longer stay in hospice care. A waxing and waning pattern of decline is less typical with cancer-related disease, and these patients generally use fewer days of hospice care.

Self Quiz
Ask yourself...
- What is your understanding of the philosophy behind hospice care?
- How do you determine the appropriate duration of services for a hospice patient?
Palliative Care
The long-held theory regarding palliation, or soothing symptoms as defined by Merriam-Webster, is that if the treatment causes suffering with the result of a cure, the benefit of the treatment outweighs the burden. In other words, a person should be able to tolerate suffering for a positive end result. On the other hand, if no cure is available, suffering is inhumane.
Palliative Care emerged as an integral part of hospice care, focusing on providing comfort and support to patients with terminal illnesses (14). However, for people without terminal illnesses, some treatments and symptoms of curable diseases are so intolerable that patients may be unable or unwilling to continue curative treatment. Why should patients and families not receive physical, psychosocial, or spiritual support simply because they are not at the end of life?
The need for Palliative Care beyond hospice was identified in other healthcare settings, such as hospitals and home care. Over time, the philosophy and principles of Palliative Care gained recognition beyond the hospice setting. This led to the development of specialized palliative care services that aimed to provide comprehensive support to patients with serious illnesses, regardless of their prognosis (14).
In 1990, the World Health Organization (WHO) formally defined palliative care, emphasizing its holistic approach. The WHO defines palliative care as improving the quality of life of patients and their families facing life-threatening illnesses by preventing and relieving suffering through early identification and treatment of pain and other physical, psychosocial, and spiritual problems (13).
The American Academy of Hospice and Palliative Medicine (AAHPM) was established to promote and advance Palliative Care, and it has now become a recognized medical specialty. Palliative care education programs, certifications, and fellowships have been established to ensure the development of skilled professionals who provide palliative care (14).
Palliative Care is an essential part of healthcare, aiming to improve the quality of life for patients with serious illnesses and their families. It focuses on relieving symptoms, addressing psychosocial and spiritual needs, and enhancing communication and decision-making throughout the illness trajectory.
Philosophy
Palliative care aims to improve the quality of life for patients who suffer regardless of life expectancy, a key differentiator from hospice care. Palliative care focuses on symptom management, pain relief, and addressing patients' and their families' physical, emotional, and psychosocial needs.
Who can receive this care?
In the modern healthcare system, "palliative" is often used to define comfort care for patients with "serious illnesses." Palliative Care is available to individuals of any age and at any stage of a serious illness, including those undergoing curative treatments. It can be provided concurrently with curative treatments, such as chemotherapy and radiation, another differentiator from hospice care. Individuals with serious illnesses may receive palliative care during a hospitalization, at home, or office visits.
How long do they receive services?
Unlike Hospice Care, Palliative Care can be provided for an extended duration even if the patient's condition is not terminal. The duration of services varies based on the individual's needs.

Self Quiz
Ask yourself...
- How does Palliative Care differ from Hospice care in terms of philosophy and approach?
- Can you explain the eligibility criteria for receiving palliative care?
Common Myths and Misconceptions
| Myth |
Fact |
|
Hospice care hastens death. |
Studies show that patients with the same diagnosis and burden of illness live longer with hospice than without (2). |
|
Palliative care is only for people who are dying. |
Palliative care is available to people of any age and stage of serious illness. |
|
Hospice is a place. |
Hospice is a form of care provided to people wherever they reside. |
|
Palliative care is only available in hospitals. |
Palliative care is available in hospitals, at home, or in a doctor's office. This is dependent on the availability of practitioners in your area. |
|
Hospice is only for the last days of life. |
Hospice is for the terminally ill with a life expectancy of 6 months or less and continues as long as a person remains terminally ill (15). |
|
Palliative care is only for the elderly. |
Palliative care is for all individuals with a serious illness. |
|
Hospice is the same as Palliative Care. |
Hospice is palliative care for the terminally ill. Palliative care is for all patients receiving curative treatment no matter the stage of illness, depending on the Palliative Care team's defined practice. |
|
Hospice and Palliative Care mean you are giving up hope. |
Hospice and Palliative Care aim to manage symptoms and improve the quality of life. |
|
Hospice and Palliative Care are expensive and not covered by insurance. |
Hospice care is 100% covered by Medicare and most other insurance (15). Palliative care is covered as a medical practitioner's visit in most Palliative Care programs. |

Self Quiz
Ask yourself...
- What are common misconceptions you have encountered regarding hospice or palliative care?
- How did you resolve the misconceptions surrounding palliative and hospice care?
Handling Difficult Conversations
Conversations, especially regarding end-of-life, are difficult for the clinician, the patient, and the family. Sensitive conversations also take time, patience, and empathy. Often, more time than a general practitioner or clinician has available. In my experience, patients approaching the end of life are often referred to as Palliative Care practitioners because of the practitioner's experience with difficult conversations. I also believe this referral practice is part of the confusion in understanding the difference between Palliative and Hospice Care.
Palliative Care Practitioners are not the only ones with the time and the skill to broach difficult conversations. Nurses also play a critical role in facilitating difficult conversations about end-of-life decisions, goals of care, and advance care planning.
Nurses often spend more time with patients and families than other disciplines. The relationship and trust nurses build with patients and caregivers makes them especially adept at starting difficult conversations.
A nurse must take the following actions before, during, and after a difficult conversation (3).
- Build a strong relationship with the patient and their family through active listening, empathy, and creating a safe space for open communication.
- Assess the patient's and family's readiness and preferences to engage in discussions. Ask patients and families questions regarding the amount and detail of information they want and the personspeople that need to be involved in decision-making. This information helps to tailor the discussion.
- Use practical communication skills such as clear and concise language aimed at providing information in a way that is understandable and sensitive to the emotional needs of the patient and family.
- Begin the conversation by assessing the patient and family's understanding of the diagnosis and prognosis to address any misconceptions or gaps in knowledge and ensure everyone is on the same page.
- Engage in a collaborative discussion about the patient's goals and values. Exploring their priorities and preferences regarding treatment options, symptom management, and quality of life helps align the care plan with the patient's values and wishes.
- Acknowledge and validate emotions, offering support and empathy throughout the conversation. Referral to appropriate psychosocial or spiritual support services may be necessary.
- Document the discussion and decisions made in the patient's medical records. Follow-up conversations should be scheduled to address any further questions, concerns, or changes in the patient's condition or preferences (3).
Should you find yourself in a position to start a difficult conversation, the following practical framework may be of assistance (3):
- Set aside time and make a plan to minimize interruptions.
- Before the conversation, take a moment to center yourself and release stress.
- Acknowledge the family and offer support by inquiring about their immediate needs.
- Open the conversation by asking what the patient and family know about their condition.
- Repeating what they know, ask them how they want to experience the time they have left.
- Empathize and allow them time to discuss and consider what they want.
- Based on their desires, educate them about the options for care.
- Consult with the interdisciplinary team and make appropriate referrals.

Case Study
Emily is a registered nurse who works the day shift on a bustling med-surg floor. She has a reputation for excellent communication skills and the ability to handle difficult conversations with empathy and grace, but she admits she never feels comfortable doing so. When she must have a difficult conversation, she uses a structured format to guide her to maintain her composure and empathy. Emily needed to use this framework when the physician asked her to talk to the family of Mr. Johnson about hospice care.
Mr. Johnson was a 75-year-old man admitted with advanced pancreatic cancer. His condition was deteriorating rapidly, and it was clear that curative treatments were no longer effective. Mr. Johnson's wife, Judy, was consistently by his bedside, her worry and sadness evident in her eyes. Emily knew Mrs. Johnson needed a plan because the fear of not knowing can be far worse than the reality. Emily asked her co-workers to cover for her other patients for the next 20 minutes so she could have a conversation about hospice.
Emily approached the room; she stopped momentarily and took a deep, centering breath. She released the day's stress and gave herself space to focus on this task. Emily gathered her thoughts and reminded herself of the framework she would use. She knew this conversation would be challenging but discussing the next steps in Mr. Johnson's Care was necessary. She entered the room with a warm smile, acknowledging both Mr. and Mrs. Johnson.
Emily began by asking how Mr. Johnson was feeling, allowing him to express any concerns or symptoms he was experiencing. She listened attentively, validating his feelings, and reassuring him that his comfort was a top priority.
After addressing Mr. Johnson's immediate concerns, Emily asked, "Mr. Johnson, what has the doctor told you about your prognosis?" Mr. and Mrs. Johnson began to verbalize that they knew Mr. Johnson was not getting better and was worsening. Mr. Johnson offered that the doctor told them curative care was not an option and that his prognosis may be short. Emily noticed Mrs. Johnson's eyes welling up with tears as Mr. Johnson spoke. Sensing her emotional distress, Emily offered her a comforting hand.
Emily asked, "How do you see spending your remaining time?"
Mr. Johnson quickly stated, "I want to go home."
Mrs. Johnson had a worried look on her face. Emily turned to her, and Mrs. Johnson stated, "I don't know how I can care for him at home."
Emily reassured Mrs. Johnson that this was a fear expressed by many spouses experiencing similar circumstances. Then, Emily introduced the concept of hospice care, explaining that it could provide specialized support and comfort to Mr. Johnson in the comfort of his own home. She highlighted the benefits of hospice, such as nurse visits, pain management, emotional support, and assistance with daily activities by an aide.
Understanding the gravity of the situation, Mr. Johnson and his wife looked at each other, their love and concern evident. After a moment of silence, Mr. Johnson nodded, expressing his willingness to explore hospice care to enhance his quality of life during this challenging time.
Emily continued the conversation, outlining the next steps and assuring the couple that the hospice team would work closely with them to develop a customized care plan. She provided them with a referral to hospice and assured them that she would be available to answer any questions.
As the conversation came to a close, Emily thanked Mr. and Mrs. Johnson for their trust and assured them that their decision was an essential step towards ensuring Mr. Johnson's comfort and dignity. She could see more lightness in Mrs. Johnosn's eyes. She was standing taller and breathing easier.
Emily left the room, knowing that this difficult conversation had set the foundation for a new chapter of Care focused on providing the support and compassion that Mr. Johnson and his wife deserved.
Nurse Role as Advocate
Nurses are the center of the interdisciplinary team, often providing communication and updates from patients and families to other practitioners such as social workers and physicians. The focused time they spend with patients in guided conversations and daily assessments allows nurses to gain a more in-depth understanding of the patient, family dynamics, and care goals.
A particular time of vulnerability for patients and families is during a serious illness and at the end of life. Nurses are responsible for advocating for patients' rights, respecting their wishes, and facilitating open communication between healthcare providers, patients, and their families. They play a pivotal role in ensuring the patient's voice is heard, and their needs are met.
Here are some ways nurses advocate for patients:
- Patient-centered care: Nurses help guide decision-making processes and ensure care aligns with the patient's values and goals when they ensure patients' preferences, values, and goals are at the center of their care (18).
- Shared decision-making: Nurses facilitate shared decision-making between patients, families, and healthcare providers by acting as intermediaries, ensuring patients' voices are heard and respected during discussions about treatment options, advanced directives, and end-of-life care planning (19).
- Psychosocial and spiritual needs: Nurses advocate for patients by providing emotional support, facilitating discussions about fears and concerns, and connecting patients with appropriate resources (20).
- Pain and symptom management: Nurses advocate for optimal comfort by assessing and addressing patients' physical distress, collaborating with the healthcare team, and advocating for timely interventions (21).
- Patient autonomy: Nurses who involve patients in decision-making processes, including information about treatment options, risks, and benefits, support patients in making informed choices (24).
- Informed consent: Nurses ensure patients understand the nature of their treatment, potential risks, and alternatives serve to advocate for informed consent (23).
- Healthcare disparities: Nurses who identify and address healthcare disparities based on race, ethnicity, socioeconomic status, or geographic location work toward eliminating inequitable healthcare (8,10).
By advocating for patients during these critical times, nurses can help ensure that patients’ wishes are respected, their quality of life is optimized, and they receive compassionate and patient-centered care.

Self Quiz
Ask yourself...
- How is advocacy different with hospice and palliative care patients than patients with non-serious illness?
- During your career, in what ways have you advocated for patients with serious illness?
Providing Resources
To provide comprehensive care, nurses must be knowledgeable regarding hospice and palliative care and what each provides. Educating families and patients about their options is a great way to provide emotional support and help them navigate complex medical decisions.
As part of the MHB and many other insurers, hospice care is funded 100%. As a result, hospices are required to provide a specific set of resources (15). Medicare and private insurers frequently cover the cost of a Palliative Care practitioner on a per-visit basis. Thus, Palliative Care resources can vary widely per program. Knowing what resources are available through your local palliative care program is essential. Below is a chart of common hospice and palliative care resources and their benefits.
| Resource | Hospice | Palliative | Benefits |
| MD | Yes | Yes | Palliate symptoms through medical assessment and treatment. |
| NP | Maybe | Often | Palliate symptoms through medical assessment and treatment. |
| Registered nurse | Yes | Maybe | Care coordination, assessment, monitoring, symptom management, education, and communication with interdisciplinary teams. |
| Social Work | Yes | Maybe | Assist with community resources, counseling, advance directives, and other support. |
| Chaplain | Yes | Maybe | Assist with spiritual support, counseling, and connecting patients with their church affiliation and practices. |
| C.N.A. | Yes | Rare | Assist patients with physical care such as bathing and dressing. This is often a great support to caregivers. |
| Dietician | Yes | Rare | Assist and support patient’s dietary needs. |
| Pharmaceuticals | Yes | No | Alleviate common symptoms. |
| Medical Supplies | Yes | No | Wound care, other treatments, continence, and cleanliness needs. |
| DME | Yes | Maybe | Supports a patient’s ability to be independent. |
| PT, OT, ST | Yes | Able to make referrals | Support to maintain function, non-pharmacological pain management, assistance with communication, swallowing, wound care, and ADL support. |

Self Quiz
Ask yourself…
- How do you advocate for patient’s rights and ensure their wishes are respected in your healthcare setting?
- How do you support patients and their families during difficult conversations about end-of-life decisions?
- How do you provide emotional support to patients and families in need?
- What strategies do you employ to ensure effective communication between patients, families, and the interdisciplinary team?
- How do you manage your emotional well-being when working with families and patients nearing the end of life?
Becoming a Hospice or Palliative Care Nurse
Even though Hospice and Palliative Care are different, the skills and qualities of successful hospice and palliative nurses are similar. As previously discussed, Hospice and Palliative Care payment differs, with Palliative Care primarily funded by payment to medical practitioners. Because of the funding, it is rare for Palliative Care practices to employ nurses to the same degree as hospice. Many Palliative Care programs do not have nurses in their daily practice but may have them for patient follow-up or coordination of care.
For this education, we are focused on the requirements of becoming a hospice and palliative care nurse, understanding that positions for Hospice nursing are more prolific than strictly Palliative Care nurses.
Educational Requirements
While many nurses can specialize in a specific area of care, for example, geriatric, cardiac, critical care, surgical, or emergency care, hospice, and palliative care nurses care for patients with a wide range of illnesses, ages, and abilities.
Hospice and palliative care nurses need to understand the ordinary course of numerous conditions in multi-aged patients to anticipate, prepare, and quickly palliate symptoms of the specific disease. They must be skilled in the assessment of patients and able to detect subtle changes in conditions that affect the patient’s plan of care.
Certain requirements need to be met to become a hospice and palliative care nurse (17). Here are the general requirements:
- Licensure: Current, unrestricted license as a registered nurse (RN) or licensed practical/vocational nurse (LPN/LVN) in the state where they practice. The specific licensure requirements may vary by state.
- Certification: Hospice nurses are often required to have specialized certifications related to hospice and palliative care. The most common certification for hospice nurses is the Certified Hospice and Palliative Nurse (CHPN) credential, offered by the Hospice and Palliative Credentialing Center (HPCC). This certification demonstrates expertise in providing care to patients with life-limiting illnesses. This certification requires two years of hospice experience for eligibility to take the certification test (16).
- Education and Experience: There are no specific education requirements for hospice nurses required by regulatory bodies. However, most hospice agencies prefer nurses with a bachelor’s degree in nursing (BSN) or higher. As written above, hospice and palliative care patients range in age and illness. Therefore, many agencies also prefer nurses with two years of experience in a medical-surgical healthcare setting (17).
- Training: Hospice nurses must receive comprehensive training in hospice care and be knowledgeable about the philosophy, principles, and practices of hospice and palliative care. The hospice agency typically provides this training and covers pain management, symptom control, psychosocial support, communication, and end-of-life care (17).

Self Quiz
Ask yourself…
- What is your experience with the importance of certification as perceived by patients and families?
- What is your experience with the importance of certification as perceived by healthcare professionals?
Skills and Qualities
Hospice and palliative care nurses must thrive on working independently since more than 80% of hospice and palliative care is provided in patient's homes. While hospice and palliative care are under the management of the physician, the hospice nurse is the primary assessor and at the patient's bedside.
Hospice nurses must be organized, have firm boundaries, and be able to systematize their practice to see multiple patients in one day, with the requirements of driving, documenting, communicating with the interdisciplinary team, and providing care according to the individual patient care plan. In addition, they must provide support and education to the patients and their families.
Nurses in hospice and palliative care settings require excellent communication, empathy, and the ability to navigate complex ethical dilemmas and difficult conversations.

Self Quiz
Ask yourself...
- How do you stay current on the latest research and best practices regarding caring for patients with serious illnesses or at the end of life?
- Can you describe a situation where you had to manage complex pain or symptoms?
- What additional training or education have you pursued to better manage patients with serious illnesses or near the end of life?
Conclusion
In conclusion, Hospice and Palliative Care represent two distinct but interconnected approaches to providing comprehensive medical care for individuals with serious illnesses. While hospice care focuses on terminal patients and aims to enhance their quality of life, Palliative Care addresses the needs of individuals at any stage of a serious illness.
Nurses are crucial in advocating for patients, facilitating difficult conversations, and providing resources to support patients and their families. By understanding the philosophy, eligibility criteria, and duration of hospice and palliative care services, nurses can contribute to the holistic well-being of patients in these specialized fields.
As society continues to recognize the importance of providing comprehensive end-of-life care and support for patients with serious illnesses, it is crucial to foster awareness, education, and support for hospice and palliative care services. By doing so, we can collectively work towards enhancing the experiences of those facing life-limiting illnesses, offering comfort, compassion, and dignity throughout their journey.
Navigating Difficult End of Life Conversations
Introduction
Talking about death is generally difficult for the average person. It is even considered taboo in some cultures or situations. For some nurses, having end of life conversations is a routine part of the profession. A hospice nurse, for example, carries the responsibility of managing care for a dying patient, and ultimately informing the patient’s family that death is imminent.
A lack of training, experience, or confidence in this area could result in poor delivery, unrealistic expectations, and an overall negative dying experience. Most people do not have experience or even a baseline when it comes to death and dying. This makes end of life conversations much more important in the delivery of patient care.
Perspectives About Dying and Death (Philosophical, Psychological, and Spiritual)
Philosophical
The human experience of death and dying is not one sided. On the contrary, there are many things to be considered to understand it fully. This goes beyond a scientific approach. An understanding of philosophical reasoning related to death is imperative to provide a thorough explication of the human dying experience. Historically, death has been an intrinsic part of life throughout various civilizations.
Ancient Egyptians spent much time preparing for the next life. Life was perceived as a dream that passed quickly. Death was viewed as eternal. Egyptians believed that the dead would make their way over to The Kingdom of Orisis, where they would spend eternity.
Ancient Greek civilization also viewed death in a particular light. According to San Filippo, “Greeks perceived death as a release of the soul from the body. The soul, which was considered to be part of the mind, was believed to be immortal. It was considered that the soul lived before the body and would live again in another life” (1).
Lastly, it has been noted that when it comes to fearing death, people create philosophies and theologies due to an inability to visualize our own death and afterlife.
Psychological
The psychological aspect of death is just as important as the physical. The thought of death alone has the potential to evoke various memories and feelings. You will typically find that a person either accepts or fears death (positive outlook vs negative outlook). This can be a fear of suffering, pain, or of the unknown. These views are typically formed based on past experiences with death.
Often, a person may have no underlying baseline when it comes to dying or death. That first experience with death can potentially shape someone’s entire perspective. Fearing death could be attributed to a fear of the unknown, lack of relatable experience, a negative experience, or a lack of communication regarding death, due to a cultural taboo, for example.
On the other hand, things like faith, positive experiences, and imminent death may cause someone to be more accepting of death. Often, someone facing imminent death may be forced to think about it and come to terms with it. In a study of terminally ill patients facing death, “The participants were afraid of death and earnestly desired to live but felt that death was imminent. To escape their distress, they attempted to accept the situation by thinking that all lives are finite, and death had to be accepted” (2). This is an example of coming to terms with an impending death and accepting it.
Spiritual
Spiritual perspectives on death should be considered when discussing views on dying. History shows that humans have long held beliefs that life does end when the body dies. Many tend to believe that once a person dies, their soul is then freed, and can go on to another life or be reincarnated into someone or something else. Religious ideologies contain a vast amount of knowledge and wisdom regarding death. “Religion and spirituality help individuals make sense of what awaits them near the end of life and help the dying cope with their terminal condition” (7).
What happens after death may vary from one religion to the next. Many religions also have a heaven or heaven like final place where the deceased can rest and be with other who have also died. One of the oldest ideologies of human history is the belief that there can be life after death.

Self Quiz
Ask yourself...
- Historically, how has death been viewed in different civilizations?
- Why might a patient fear death and dying?
- What causes patients to be more accepting of death?

Impact on Nurses
Imagine working as a hospice nurse. Your sole purpose is to provide end-of-life care for terminally ill patients. This includes providing information on what to expect at the end of life. At any given time, you have patients that could be imminently dying.
You are a source of knowledge and comfort for a patient and their family during this time. In the end, you will likely be there when the patient takes their last breath. How can one prepare to handle this scenario time and time again? Should a nurse feel sadness for a patient that was expected to die, or should they emotionally separate themselves?
The latter may prove hard to do. The reality is that nurses are frequently exposed to death and dying in a variety of settings. A patient’s dying process can be planned or not and this distinction may mean different things for different people. Typically, nurses are taught skills to help prevent death.
This may be a hard thought process to overcome when the goal is not curative, but comfort focused. These patient interactions help to shape a nurse’s feelings on death and dying. “Nurses are frequently exposed to dying patients and death in the course of their work. This experience makes individuals conscious of their own mortality, often giving rise to anxiety and unease.
Nurses who have a strong anxiety about death may be less comfortable providing nursing care for patients at the end of their life” (3). This ‘death’ anxiety could lead to disastrous outcomes for both the nurse and the patient. Nurses should be aware of their own thoughts and attitudes towards death, and how these could affect their ability to provide patient care.
Caring for the dying involves both skill and emotional support from nurses. Younger nurses and nurses with less experience with death may have greater difficulty caring for dying patients. End of life education and an introspective look at oneself are imperative when it comes to providing quality care. “Nurses’ professional experience is positively correlated with their position, professional level (rank), EOL care experience, competence in EOL, and another knowledge.
Nurses who have a positive attitude seem more likely to have more competence in dealing with patients’ symptoms at EOL and better knowledge of EOL care (3). The more palliative knowledge nurses had, the more competence they felt. Moreover, competence dealing with patients’ symptoms in EOL care was correlated with older nurses” (8). Positive conversations about death and dying usually lead to a positive dying experience.
To reach this point, nurses and other healthcare professionals need to know how to have these conversations. In a society that is so focused on the living, receiving education on death can be difficult. When death is perceived as a part of life, only then will people feel more comfortable talking about it.

Self Quiz
Ask yourself...
- What role do nurses play in death and dying?
- In what ways are nurses affected by death?
- How do previous experiences shape our views about death?
- What are some potential indicators of a nurse’s ability to provide quality care at EOL?
Communication Strategies
Many people are uncomfortable talking about death and dying and tend to shy away from such conversations. This may also be true for nurses. Talking about death should not be a formidable task. Nurses should be able to comfortably implement these conversations in their practice when needed. Effective communication is imperative throughout a patient’s trajectory.
Conversations about death and dying can impact patient care. “Research has shown that talking about and planning the EOL is important for how the final days in a patient’s life may play out and is associated with reduced costs as well as a higher quality of care in the final weeks of life” (4). In a society so focused on life, it may be difficult for nurses and other health professionals to obtain the skills needed to confidently speak with patients about death.
To effectively talk to patients about death, nurses should first be willing to initiate and discuss the topic. There are important strategies to remember when talking about the end of life. “Qualitative research on the end of life has revealed that medical personnel should consider the following strategies when conducting EOLD: open and honest conversation, setting treatment goals, and balancing hope with reality” (13).
Patients should also be encouraged to express their thoughts, fears, and to ask questions. It is also important to be honest and forward with patients. No “beating around the bush”. This means using words like “dying” and “death” while having these conversations.
One communication strategy, VALUE, “recommends to value and appreciate statements of family members, acknowledge their emotions, as well as to listen and ask questions to understand who the patient was as a person” (9). Nurses should keep the following in mind: a patient’s comfort level with death, goals of care, expectations, and cultural factors. Having this knowledge will help to guide the conversation.
Lastly, when a nurse feels confident and exhibits calmness while talking about death, a patient will more than likely feel the same way.

Self Quiz
Ask yourself...
- How do conversations about death impact patient care?
- What can nurses do to effectively communicate with their patients about death?
- What strategies should be utilized when talking about death?
Stages of Grief
Nurses are not immune from experiencing grief or loss. We mourn personally and we mourn alongside our patients and their families. “Grief and loss are something that all people will experience in their lifetime. The loss may be actual or perceived and is the absence of something that was valued. An actual loss is recognized and verified by others while others cannot verify a perceived loss.
Both are real to the individual who has experienced the loss. Grief is the internal part of the loss; it is the emotions related to the loss” (4). Grief allows a person to begin to deal with the pain associated with loss and to heal. There are five stages of grief which were identified in Dr. Elisabeth Kübler-Ross in her book Death and Dying.
- Denial: This stage Is not necessarily about denying that the loss happened. Instead, it is more about denying the feelings associated with the loss. Denial lets us face our feelings of grief. “As an individual is able to accept that this loss is their reality, they will be able to move into the healing process and denial will begin to diminish” (5).
- Anger: A grieving person may feel anger towards a variety of people associated with the loss. This is a normal and a necessary part of the healing process. “Under the anger is the individual’s pain. Anger provides structure, and that is better than preceding numbness. It can be a challenge for some to feel the anger; sometimes it is easier to try and suppress the anger. Feeling anger and addressing anger is part of the grieving process” (5).
- Bargaining: Grieving people may begin to say things to themselves like, “If this__, then this __”, or “I will do anything if you take the hurt away” (5). This stage may occur at any point in the grief process. Once this step is reached, the person can begin to move through the stages in different ways.
- Depression: This stage involves a realization that the situation is real. “Empty feelings come forward, and one’s grief moves in on a deeper level than before. This type of depression is not a sign of mental illness; although reaching out for help may be the right step. It is an appropriate response to a great loss. An individual may withdraw from their daily life activities, and they may feel a fog of intense sadness” (4). Depression after a major loss is normal and necessary in the healing process.
- Acceptance: Entering this final stage does not mean one is completely okay with what has happened. In fact, one may never be as they once were prior to the loss. “Acceptance, as a stage, is about accepting that this is their new reality, and it is permanent. Life cannot go on as it once did, but through acceptance, life can and will go on” (5). Individuals in this stage must realize that change is necessary to adjust to the new normal.
Not everyone experiences grief in the same way. Grief is a very personal experience that affects people in different ways. Nurses should be familiar with the stages of grief to be able to offer optimal patient care to grieving patients and their families. This includes recognizing signs of depression and possible suicidal ideation, providing empathy, compassion, education, and resources to those in need.

Self Quiz
Ask yourself...
- What are the stages of grief?
- Why should nurses be familiar with the stages of grief?
- What purpose does grief serve?
End of Life Process
Phases of Dying
Although everyone experiences death differently and on their own terms, there are two main pathways that most people take before dying. The dying process can be broken up into two phases: the transitioning phase, and the actively dying phase. The amount spent in each phase varies from person to person.
The transitioning phase usually begins 2-3 weeks prior to death. Major changes in function and the ability to do activities of daily life are observed during this time. Patients may even begin falling prior to entering this phase. Becoming bedbound is common as one will begin to spend most of their time sleeping.
This means decreased responsiveness, less interest in normal activities and hobbies, decreased interaction with family and friends, and an overall decline in one’s interest in external factors. It is possible to be roused during this phase, but this may only be possible in short intervals. It is not uncommon for transitioning patients to speak to or about loved ones that have already passed away. They may even report seeing deceased family in the room with them (11).
This should not be feared and is an important part of a person’s dying process. Incontinence may also begin during this time and briefs will be needed. Perhaps one of the most noticeable and difficult changes to witness, especially by friends and family, is changes in appetite. Patients will begin to show less interest in food and liquids. A greater difficulty swallowing will become apparent. “Refusal of food and fluid by a dying person is a common occurrence, particularly as the body slowly shuts down, and this may be the evidence signifying an actively dying process rather than starvation” (11).
Lastly, symptoms like restlessness, agitation, and pain may arise and detract from one’s comfort level. Although most patients will spend about two weeks transitioning, time can vary from days to weeks. The transitioning phase can also be skipped altogether, depending on the person.
Once the transitioning phase has concluded, the actively dying phase will begin. Actively dying immediately precedes death. This phase is usually short, lasting about 48 hours. Once actively dying, death is imminent, and a patient is expected to pass away at any moment. This phase is markedly different from the previous phase, and symptoms tend to become more apparent. “The following five changes constitute objective evidence of the end of life: diminished daily living performance, decreased food intake, changes in consciousness and increased sleep quantity, worsening of respiratory distress, and end-stage delirium” (12).
One key difference is one’s ability to response to tactile or verbal stimuli. The actively dying patient is obtunded and no longer responds to external forces. There could be slight reactions, but nothing meaningful. This is a comatose state.
There are many observable changes, including changes in vital signs. Blood pressure begins to drop, heart rate speeds up and eventually slow, respiratory rate picks up, and temperature may become elevated. Respiratory differences tend to be the most common observable changes. Cheyne-Stokes may occur, and the overall breathing pattern can be very irregular. Apnea is also common (11).
Many patients experience what is known as the “death rattle”. This very noticeable sound is due to an accumulation of secretions in the upper airway. This is a hallmark of the actively dying phase, but it is not experienced by everyone. “Death rattle is a strong predictor of imminent death, and nearly 80% of people die within 48 hours after its onset” (11).
Skin changes also occur. The body may become cool to touch, cyanosis may develop in the nail beds of fingers and toes, and mottling can occur usually beginning in the lower extremities and later spreading to other parts of the body. Skin may also become very pale. Urine output will decrease and become concentrated as evidenced by an amber color.

Self Quiz
Ask yourself...
- What are the dying phases?
- What changes are observed when someone is transitioning?
- What are some expected physical changes in the active dying phase?
- What education should a nurse provide to someone taking care of a patient that is actively dying?
Nursing Assessment and Care
Since there are so many drastic changes observed during the transitioning phase, proper education is crucial for caregivers. Nurses should reassure them that what the patient is experiencing is normal and to be expected. “At the end of life, most patients are in a state of lethargy, wherein their consciousness progressively declines, and sleep duration increases; therefore, it is necessary to provide appropriate explanations to patients and their families so that they can accept these symptoms as part of the natural end-of-life process” (12).
Family members usually try to wake the sleeping transitioning patient and have them attempt activities that could be done in the past. This is dangerous for the pt and can lead to injuries and more agitation. Becoming bedbound is a major change and puts the patient at risk for pressure injuries and increased pain. Fragile skin combined with new episodes of incontinence are topics that should be discussed, and proper supplies should be used.
Other potential barriers to a peaceful transitioning period are force feeding and aspiration. Nurses should provide education on what is acceptable and needed at this point. Patients will not die of hunger or lack of water. Allowing the patient to eat and drink small amounts is okay (12).
This amount will decrease as the body starts shutting down. Ice chips can be used while the patient is still alert. Utilizing mouth swabs with water is enough to hydrate the oral cavity and keep the patient comfortable until the end. During this time, symptoms can seemingly come out of the blue.
A once calm patient can become highly agitated in a short period of time. Medications should be added timely to ensure that the patient has a peaceful death. Information on medication and interventions to control uncomfortable end of life symptoms like pain, agitation, and restlessness should be provided to caregivers. Hospice patients, for example, have a comfort kit with various medications to use during this time.
Medications can be used as needed or scheduled to keep patients comfortable. (12). As the patient enters the actively dying phase and becomes less alert and aware, it is important that friends and family continue to talk to the patient and keep conversations positive around the patient. Hospice nurses, for example, are sure to tell caregivers that hearing is the last thing to go, so they should continue to speak to their loved one. Since vital signs start to become abnormal, reassurance is usually needed to keep family comfortable.
Not all vital signs need to be taken in the final stages. Taking blood pressure, for example, could cause discomfort. Death education related to respiratory changes is imperative. “Abnormal breathing patterns such as shallow breathing sound become increasingly common starting 1 week before death” (12).
Caregivers should be informed that breathing too fast or too slow at this point is not an emergency and there are things that can be done to promote comfort like applying oxygen, keeping the head of the bed upright, and keeping the room cool. Medications can also be given to decrease the death rattle. It should be noted that patients do not experience discomfort from the death rattle.
Lastly, not having a bowel movement or passing urine during the last few days of life is normal and interventions are not needed. Education and support are especially important during the final phases of life. With their peaceful words and deep knowledge base, nurses can be instrumental in facilitating a peaceful death.

Self Quiz
Ask yourself...
- Is it reasonable to obtain vital signs every two hours? Why or why not?
- If the family expresses concern about changes in bowel or urinary habits, what can you say to reassure them?

Resources and Support
Planning, coordinating, and executing quality end of life care can be challenging for health care workers. This period can also be one of the most challenging times for both patients and their loved ones. There are available resources for health care workers, patients, and their loved ones that provide information on end-of-life care.
Hospice care is an invaluable resource and source of support. This is available to terminally ill patients with a life expectancy of 6 months or less.” Hospice care is the term given to the care provided when a patient is given a prognosis of death within 6 months, and they do not pursue curative treatments They focus on improving the quality of life which can mean many things” (10).
Care can be provided in any setting that a patient calls home. The hospice team includes a medical director, registered nurse, chaplain, social worker, home health aide, and often a nurse practitioner. Symptoms and care can be managed at home with the help of covered medications, supplies, and medical equipment. Hospice allows patients to reach their goal of dying peacefully at home. A bereavement team also provides support during the process. (10?)
Palliative care, another form of comfort care, can also be utilized to maintain comfort at the end of life. Unlike hospice, patients receiving palliative care do not need to have a life expectancy of 6 months or less. “Research found that timely EOL care discussions allowed family members to make use of hospice and palliative care services sooner and maximize their time with the patient” (6).
Nurses should be educated in other end of life resource topics such as advanced directives, POLST (Physician Orders for Life Sustaining Treatment), and Durable Medical Power of Attorney. Looking ahead and having meaningful discussions regarding end-of-life planning can help prevent the stress of needing to address these things when death is imminent.

Self Quiz
Ask yourself...
- What care options are there for patients at the end of life?
- What is the difference between palliative and hospice care?
- What tools can the nurse use to help patients in end-of-life planning?
Conclusion
End of life conversations have a profound impact on not only patient care, but also on the dying process itself. Research shows that when implemented appropriately, these conversations improve patient relationships with healthcare workers, lead to better outcomes, and allow for a more positive dying experience. Nurses play a critical role in end-of-life processes in many different settings. With education, practice, experience, and confidence, nurses can incorporate conversations about death and dying to provide quality care.
Basic Ventilator Management
Introduction
Ventilator management can be an intimidating subject, especially if the user is not savvy with technology. Fortunately, modern ventilator manufacturers have put significant effort into making ventilators “user-friendly”. This course will further support those who manage ventilators. We will discuss basic respiratory function, the types and mechanism of action of ventilators, and indications for use. It is also important to gain understanding of the settings, modes, alarms, and essential nursing care.
Ventilator Fundamentals
Mechanism of Action
Knowledge of basic respiratory function is essential for understanding mechanical ventilation (MV). The respiratory system is comprised of the airway, lung, and chest wall. Respiratory mechanics represents the lung function in terms of pressure, gas flow, and volume (1).
Pressure refers to the physical movement of the lungs and chest wall muscles. During spontaneous and unassisted inspiration, our lungs expand due to the transpulmonary pressure caused by negative pleural pressure that is created by the inspiratory muscles (2). Essentially, the lung spontaneously pulls inwards while the chest wall pushes outwards.
Gas exchange refers to the process of transferring atmospheric oxygen (O2) from the alveolar gas into the bloodstream and carbon dioxide (CO2) from the bloodstream transferred to the alveolar gas phase; CO2 is then eliminated into the atmosphere by ventilation (1). Gas exchange occurs within areas of the lung lined by alveoli, which are tiny air sacs encased in capillary beds (1).
Volume simply refers to the amount of airflow, which is affected by factors such as lung elasticity, space to expand, presence of fluid, and surface tension.
The mechanism of action of mechanical (artificial) ventilation had evolved over time. The first type of mechanical ventilators provided negative pressure ventilation, which applied external negative pressure to mimic chest muscle pressure (1). Although it was helpful and prolonged life to many patients, this method was not effective for gas exchange abnormalities.
Controlled positive pressure ventilation was first applied in 1952 and pushes air into the central airways, causing air to flow into distal airways and alveoli (1). Positive pressure does not work in the same way as spontaneous respiration, which is negative pressure. This forced airflow provides the encounter for gas exchange to occur. This airflow also provides pressure that prevents the alveoli from collapsing.
Types
As we discussed, modern mechanical ventilators apply positive pressure that pushes air into the lungs. The types of positive pressure ventilators include invasive and noninvasive.
Invasive Mechanical Ventilation. Invasiveness refers to the intrusion of medical instruments into the body. In invasive ventilation, a tube from the ventilator is connected to the airway. When a tube enters the mouth and into airway, it is called intubation. A tracheostomy is utilized when the tube must enter the airway through the trachea (2).
Noninvasive Mechanical Ventilation. A noninvasive ventilation type is less intrusive into the body cavities. A facemask with straps is typically used.

Figure 1. Algorithm for Types of Ventilation. Photo credit: (1)
Understanding Ventilation Terminology
Ventilation describes the bulk movement into and out of our lungs (3). Ventilation can be categorized into tidal volume (VT), respiratory rate (f), and minute ventilation (VE). Tidal volume is the volume of gas exhaled following a normal inspiration; respiratory rate is the number of breaths taken over one minute; minute ventilation is the tidal volume times the respiratory rate (3). These will be important terms as we review mechanical ventilator settings and modes.
Ventilator capacity refers to the amount of air that a ventilator pump can push into the lungs. The ventilatory capacity is significant because this amount must be sufficiently maintaining tissue oxygenation and carbon dioxide (CO2) removal (3). When you hear the term respiratory drive, think about the neurological system driving the respiratory vehicle. Essentially, breathing is generated by neuron activity located in the brainstem, which produces a neural signal directed to respiratory muscles to create inspiratory effort and tidal breathing (4). There are receptors that monitor carbon dioxide levels in the body and when a high level of carbon dioxide is detected a signal is sent to stimulate the drive to breathe to blow off the excess carbon dioxide (5). Essentially, the level of carbon dioxide dictates the drive to breath and the respiratory rate.

Self Quiz
Ask yourself...
- Have you ever cared for a patient on a mechanical ventilator?
- Can you explain how the physiology of the lungs (airway, alveoli) impacts gas exchange?
- Can you describe the difference in pressure between spontaneous breathing and mechanical ventilation?
- The nervous system is a vital part of the breathing process. Have you ever performed a neurological and respiratory assessment with abnormal findings?
Indications for Use
Mechanical ventilation is indicated when spontaneous breathing is insufficient (tachypnea, hypercapnia) or absent (apnea). Respiratory failure is the inability of the heart and lungs to adequately supply the tissue with oxygen and remove carbon dioxide (3).
Indications for Invasive Mechanical Ventilation
Compromised or Diseased Airway: (4)
- Trauma to airway
- Oropharyngeal infection.
- Proximal airway obstruction
- Angioedema
- Anaphylaxis
- Distal airway obstruction
- Asthmatic bronchospasm
- Acute exacerbation of chronic obstructive pulmonary disease (COPD).
Hypoventilation: (4, 5)
- Impaired central drive
- Pharmacology or illegal drug overdose
- General anesthesia for surgery
- Traumatic brain injury
- Respiratory muscle weakness
- Muscular dystrophy and myositis
- Peripheral nervous system defects
- Guillain-Barré syndrome
- Myasthenic crisis
- Restrictive ventilatory defects
- Trauma or impact to chest wall
- Pneumothorax
- Pleural effusion
Inability to exchange oxygen or delivery to the peripheral tissues (hypoxemic respiratory failure): (4)
- Alveolar unable to fill.
- Pneumonia
- Acute respiratory distress syndrome (ARDS)
- Pulmonary edema
- Pulmonary vascular insufficiency
- Massive pulmonary embolism
- Air emboli
Failure to meet increased ventilatory demand: (4)
- Severe sepsis
- Shock
- Severe metabolic acidosis
Indications for Noninvasive Pressure Ventilation
Noninvasive pressure ventilation attempts to deliver oxygen to the lungs without endotracheal intubation (1).
Before intubation
- Acute exacerbation of COPD
- Hydrostatic pulmonary edema
- Asthma
- Bronchoscopy
- Chest Trauma
Used instead of invasive mechanical ventilation (intubation)
- Acute respiratory failure (ARF) [According to the latest ATS/ERJ (American Thoracic Society and European Respiratory Society) guidelines from 2020] (4)
- BPAP for acute or acute-on-chronic respiratory acidosis secondary to COPD exacerbation where pH < or = 7.35 (8)
- BPAP or continuous positive airway pressure (CPAP) for cardiogenic pulmonary edema (8)
- Obesity hypoventilation syndrome (1)
- Obstructive sleep apnea (4)
- Restrictive thoracic disorders (4)
**ATS/ERJ guidelines carry a conditional recommendation for the following in the setting of ARF:
- Early NIV (non-invasive ventilation) for immunocompromised patients with ARF
- Palliative care for terminal conditions
- Chest trauma patients with ARF
Following Intubation
- Post-operative ARF
- Preventative measure in high-risk patients following extubating.

Self Quiz
Ask yourself...
- Can you think of certain populations or diseases that are at a high risk for needing mechanical ventilation?
- Have you experienced caring for a patient following general anesthesia?
Ventilator Settings
Knowledge of the settings on mechanical ventilators is critical for care. Each parameter should be initially determined and adjusted based on the patient’s condition and unique needs. This is within the scope of practice of qualified physicians and respiratory therapists only. The nurse should know the settings and include them in the nursing handoff report.
There are several types of ventilator settings to be familiar with, including the following:
- Tidal Volume
- FiO2
- Respiratory Rate (Frequency)
- PEEP
- Mode
- Alarms
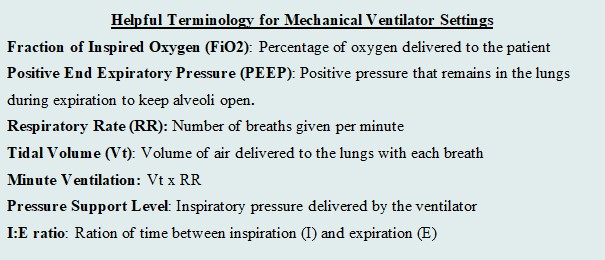
Figure 3. Helpful Terminology for Mechanical Ventilator Settings. (Designed by course author)
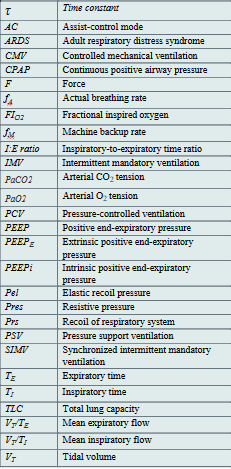
Table 1. List of Abbreviations for Ventilation. (1, 2, 5) (Designed by course author)

Self Quiz
Ask yourself...
- Are you familiar with the settings of mechanical ventilator?
- Have you ever cared for a patient that needed to “wean” from something, such as medication, addiction, etc.?
- Consider the feeling of wearing a breathing mask. How can the nurse provide physiological and psychological support?
As we discuss the settings, it is important to recognize short and long-term goals of mechanical ventilation. Short-term goals prioritize airway, breathing, circulation (ABCs) and maintaining respiratory gas exchange. Long-term goals should focus on weening and encouraging the patient to have a safe return of spontaneous breathing if possible. Independence should be a goal in certain circumstances.
The settings will reflect the minimal amount of assistance to maintain perfusion. Evidence supports the concept that hyperoxemia increases the risk of mortality in critically ill patients (2). An excess of oxygen is dangerous, as it can reduce respirations and heart rate. Tidal volume refers to the volume of air that is inhaled and exhaled from the lungs during spontaneous breathings, so the tidal volume setting determines the amount of the air delivered to the lungs by the machine (2).
Fi02
Fi02 stands for fraction of inspired oxygen. The range is 21% - 100% (Will). The Fi02 should be set to the lowest level to maintain a pulse oximetry (SP02) of 90% to 96% (2). A patient may initially require an FiO2 of 100% when mechanical ventilation is initiated, but the goal is to gradually wean the FiO2 percentage down to the lowest possible level that still provides adequate oxygenation for the patient. Research supports that a patient who receives mechanical ventilation with an Fi02 greater than 60% for an extended period of time is at greater risk of oxygen toxicity (1).
Positive End Expiratory Pressure (PEEP)
The PEEP settings refer to the positive pressure (greater than the atmospheric pressure) that will remain in the airways at the end of the respiratory exhalation (1). PEEP serves to distend the distal alveoli and prevent collapse. Imagine a balloon that you would like to keep inflated but air continuously seeps out. PEEP would determine the appropriate pressure to keep the balloon inflated. There are two types of PEEP: extrinsic and intrinsic (or auto-PEEP). Pressure that is applied during an inspiration is known as pressure support.
Extrinsic PEEP (PEEPe), or applied PEEP, is a setting on the ventilator and typically selected upon initiation of mechanical ventilator. Extrinsic PEEP ranges to small/ moderate (4 to 5 cmH2O) to high (>5 cmH2O). The level of PEEP is usually set at 5 cmH2O and titrated based on the underlying condition and oxygenation or perfusion needs (2). There is research and evidence-based guidelines to guide healthcare providers in properly setting and adjusting the PEEP on the mechanical ventilator. For example, in ARDS, there is a specific level of PEEP titrates according to regulatory evidence and guidelines.
Intrinsic PEEP, or auto-PEEP, refers to an incomplete expiration prior to the initiation of the next breath, which causes trapping and accumulation of air (2). If auto-PEEP is found, steps should be taken to stop or reduce the pressure build-up.
Respiratory Rate (RR)
Respiratory rate (RR) is the setting that simply determines how many breaths are delivered by the ventilator per minute. The RR is typically set at 12 to 16 breaths/minute (2). Certain circumstances warrant a higher RR (up to 35 breaths/minute). Higher RR is sometimes selected to achieve adequate minute ventilation. Examples include patients with ARDS, which would protect lung integrity and avoid severe hypercapnia, and patients with acidosis (2). Respiratory acidosis usually occurs due to failure of ventilation and accumulation of carbon dioxide, so increased respiration rate be used to balance acidosis (5). Important nursing implications are to closely monitor ABGs and titrate as ordered.
Flow Rate
The inspiratory flow rate is a rate that controls how fast a tidal volume is given by the ventilator; the setting can be adjusted depending on the patient’s inspiratory needs. The normal inspiratory flow rate should be set at around 60 L/min (2). In circumstances such as obstructive diseases, the ventilator can deliver up to 120 L/min if a patient needs a prolonged expiratory time (2). If the flow rate is set too low, it could cause unsynchronized patient-ventilator flow and an increased work of breathing; if the flow rate is set too high, it could result in lower airway pressure (2).
Respiratory therapists are an incredible resource and should be notified, as well as the physician, if this is suspected. Ventilator alarms are an essential tool for assessing inappropriate settings, we will discuss alarms later in the course. Please review the image below for a visual aid.

Self Quiz
Ask yourself...
- Can you think of professionals in your workplace that are qualified to adjust the settings on a mechanical ventilator?
- What do you think the respiratory rate should be set to?
- What do you think the inspiratory flow rate should be set to?
- Do you think positive pressure is greater than or less than atmospheric pressure?
Ventilator Modes
Mechanical ventilation without patient effort is delivered by the ventilator with control of either volume or pressure. Volume and pressure-controlled ventilation modes differ from one another based on transpulmonary pressure generation (5). There are three basic ventilatory modes based on respiratory cycles to consider: Assist/Control ventilation (A/C), Pressure Support Ventilation (PSV) and Synchronized Intermittent Mandatory Ventilation (SIMV) with PS, which is a hybrid mode of the first two (1).
Interpreting Waveforms
Scalars and Loops. Modes are depicted and illustrated as waveforms. Ventilator waveforms are graphical descriptions of how the ventilator is delivering a breath to a patient. These include scalars, which are graphics that illustrate the entire breath from the beginning of inspiration to the end of expiration, and loops, which are graphics that represent either pressure or flow, and plotted against the volume during a breath (1). Most ventilators have three scalars displayed on the main screen: flow versus time, volume versus time, and pressure versus time (1). There are typically two loops: pressure-volume and flow-volume. It is vital that the bedside clinician can interpret these scalars and loops to understand if the patient’s ventilation demands are met.

Figure 4. Example of Volume vs Time Scaler. Photo Credit: (9)
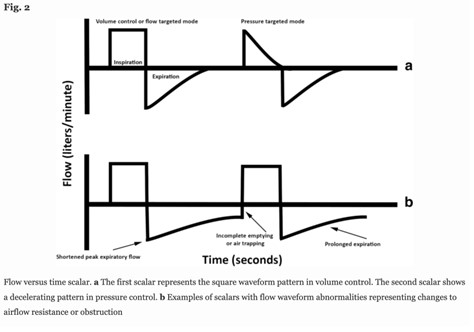
Figure 5. Example of Flow versus Time Scaler. Photo Credit: (9)
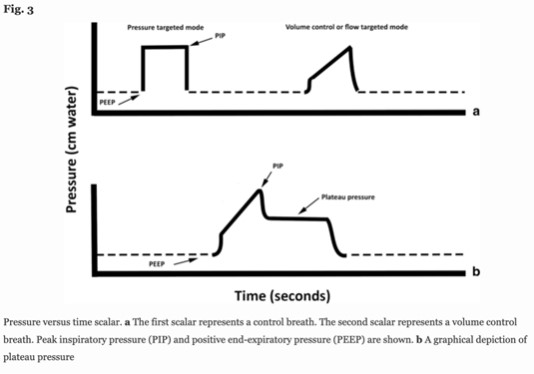
Figure 6. Example of Pressure versus Time Scaler. Photo Credit: (9)

Figure 7. Example of Pressure-Volume Loop. Photo Credit: (9)

Figure 8. Example of Flow-Volume Loop. Photo Credit: (9)
Volume and Pressure Controlled Modes
Monitoring respiratory mechanics in dynamic or stagnant conditions is extremely important to lung protection and adequate respiratory care. We will review the characteristics of volume and pressure-controlled modes.
Controlled mechanical ventilation (CMV) is when the ventilator controls one variable from the equation of motion, either flow (𝑉) or airway pressure (Paw) during the inspiratory phase. The flow or pressure must be a variable, because the others are constants: Rrs and Crs are intrinsic properties of the respiratory system, V(t) is the instantaneous volume above end-expiratory volume, PEEP is the end-expiratory pressure, and Pmus represents the pressure generated by inspiratory and expiratory muscles (1). Essentially, in this equation, the ventilator determines either the volume or the flow.
Paw(𝑡) = 𝑉(𝑡) / 𝐶𝑟𝑠 + 𝑅𝑟𝑠 × 𝑉 (𝑡) + PEEP – 𝑃𝑚𝑢𝑠 (𝑡)
This formula serves as a foundation for the common mechanical ventilator modes: Volume and Pressure Controlled.
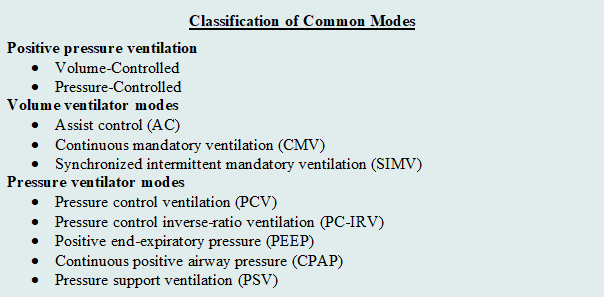
Figure 9. Classification of Common Modes. (Designed by Author)
Selection of mode differs from settings, as the mode of mechanical ventilation refers to the characteristics and phases of ventilation. The characteristics or phases mainly include trigger, cycle, and limit. (2)
Trigger: How does inspiration begin? The trigger is a type of signal that initiates the inspiratory phase by the ventilator.
- Patient-triggered: patient’s inspiratory effort triggers the ventilator to begin the inspiratory phase.
- Time-triggered: a time interval is set on the ventilator to begin the inspiratory phase.
Cycle: How does the inspiration end? The cycle is a type of signal that ends the inspiratory phase by the ventilator.
- Volume-cycled ventilation: the inspiratory phase ends when a set volume exits the ventilator.
- Pressure-cycled ventilation: the inspiratory phase ends according to a set driving pressure, airway resistance, lung compliance, and inspiratory effort of the patient.
- Time-cycled ventilation
Limit: When should inspiration be aborted? The limit is a set value (e.g., pressure) on the ventilator that should not be exceeded. If the preset limit is exceeded, the inspiration will be aborted. (2).
Volume Controlled (ACV/ VCV)
When you hear “volume”, think amount. The main characteristic of volume-controlled ventilation (VCV) is the delivery of fixed tidal volumes (1). The clinician sets the volume and how often it is delivered. Considering the respiratory rate is also set, minute ventilation is guaranteed. Essentially, this mode is driven by the amount of air entering the patient’s airway and how often. Inspiratory airway flows in predefined flow waveforms and the most common is square (1).
A max flow rate of the air being delivered is also set—think of it as the “speed” of the air being pushed into the lungs. The time it takes to deliver the inspiration will change because of the max flow rate that is set on the ventilator (1). If the flow rate is higher, the the inspiratory time of the breath to deliver the set volume will be shorter as a result.
It may be more likely nurses will be exposed to this type of mode in critical care settings. Volume-controlled ventilation (VCV) was the most used ventilatory mode in critical care when surveys were completed; however, both pressure-controlled and pressure-support modes have been reportedly utilized more frequently in recent years (1). VCV is primarily used when the patient is unable to breath on their own and essentially no spontaneous breathing occurs. VCV has also been the traditional controlled ventilation mode with anesthesia (3).
The concern of VCV is the constant flow may cause high peak pressures and increases the patient’s risk of barotraumas. Barotrauma is defined as physical tissue damage caused by a pressure difference between a closed space inside the body and the surrounding gas or fluid (7). Imagine trying to inflate a balloon in a glass bowl, if the pressure pushing air into the bowl continues and the glass bowl will not let it expand, the balloon itself will be damaged. Due to these risks, patients with lung disease and neonatal patients are not ideal candidates for this type of mode.
The nurse can gather information, such as the volume that is delivered per breath. If the volume is set at 4.5 liters, at a rate of 18, then the volume delivered with each breath will be 250mls per breath (4500mls / 18 = 250mls). The inspiratory time may fluctuate. The nurse must critically think and become aware of ventilation demands, considering factors including the set tidal volume, respiratory rate, and max flow rate. At end of shift nurse reporting, the nurse should communicate the following: mode, rate, tidal volume, fraction of inspired oxygen (Fi02), PEEP, and pressure support (PS).
Pressure Controlled (PCV)
In pressure-controlled ventilation, there is a set airway pressure for a given inspiratory time. Remember that the ventilator is programed with certain constants (specific setting and should not change) and variables (fluctuates based on constant settings). In the PCV mode, the peak airway pressure is constant (inspiratory pressure + PEEP) while the tidal volume is variable and can fluctuate depending on patient characteristics (compliance, airway/tubing resistance) and driving pressures (3). The clinician sets the inspiratory pressure level, PEEP, I:E ratio, respiratory rate, and FiO2.
Pressure-controlled mode provides the following advantages over volume-controlled breaths:
- Lower peak airway pressures to deliver the same volume amount.
- More efficient volume distribution within the lungs
- Better oxygenation
- Less risk of barotrauma
- Ability to ventilate every patient type.
As mentioned, PCV has a lower risk of barotrauma, so patients who already have lung disease and tissue damage are not appropriate for this type of mode. The tiny lungs of infants also have greater impact of tissue damage if barotrauma occurs. Nurses within the neonatal intensive care unit (NICU) may be more likely exposed to Pressure-controlled ventilation modes. PCV has become the standard approach to ventilation in the early days of neonatal care in small preterm infants, making it the prevailing mode of ventilation in the NICU in many parts of the world, including the US (3).

Self Quiz
Ask yourself...
- What are reasons for depicting the modes in waveforms?
- Can you name the three phases/characteristics of respiration that we discussed?
- What do you think the difference is between pressure and volume-controlled ventilation?
- Can you explain why pressure-controlled ventilation has a lower risk of barotrauma than volume-controlled ventilation?
Continuous Positive Airway Pressure (CPAP)
Continuous positive airway pressure (CPAP) is a type of positive airway pressure for patients that are breathing spontaneously. The goal of CPAP is to maintain a continuous pressure to constantly stent the airways open (7). If you recall, positive end-expiratory pressure (PEEP is the pressure within the alveoli at the end of expiration. CPAP is a method of maintaining PEEP and preserving the set pressure in the airway throughout the respiratory cycle. It is measured in centimeters of water pressure (cm H2O) (7). CPAP is aimed to prevent airway collapse in patients at risk. CPAP alone is often inadequate for supporting ventilation, but helpful for non-invasive ventilation. CPAP can support oxygenation via PEEP prior to intubation (6).
CPAP delivers air through the typical method of respiration; air is inhaled through the nose, travels through the nasopharynx, oropharynx, into the larynx, trachea, bronchi, bronchioles, and alveoli (7). This form of ventilation support can be used in inpatient and outpatient settings, long-term care facilities, and at home.
Common indications for CPAP include the following:
- Hypoxia: (7)
- Decrease the work of breathing
- Bronchiolitis or pneumonia
- Respiratory failure associated with congestive heart failure.
- Obstructive sleep apnea (OSA). Predisposition: Obesity, hypotonia, adenotonsillar hypertrophy, family history, use of alcohol or sedatives, etc. (8)
- Preterm infants
- Their lungs have not yet fully developed and respiratory distress syndrome can occur (2)
- Within NICU setting
- CPAP can be administered in several ways based on the type of mask used: (7)
- Nasal CPAP: Nasal prongs inserted directly into the nostrils or a small mask that fits over the nose.
- Nasopharyngeal (NP) CPAP: An airway tube placed through the nose that the tip travels to the nasopharynx.
- Face Mask CPAP: A full face mask is placed over the nose and mouth. The seal is critical.
High Frequency Ventilation (HFV)
High-frequency ventilation (HFV) delivers breaths at a rapid rate because conventional ventilation modes have failed (7). The respiratory rate set on the ventilator significantly exceeds the normal breathing rate and the tidal volume delivered is significantly less. An advantage is the reduced risk of barotrauma, thus reduced risk of lung tissue damage. However, the mode has many contraindications and HFV is not frequently used in adults, more commonly in neonates (7).

Self Quiz
Ask yourself...
- Do you have experience with patients who wear a CPAP for sleep apnea?
- Can you name other indications for CPAP?
- Do you think high-frequency ventilation would be a first or last choice for early choice of ventilator types?
Ventilator Alarms
Ventilator alarms can be a nurse’s best friend when coupled with in-depth understanding of types of alarms and troubleshooting techniques. These alarms are essential during mechanical ventilation because they notify the healthcare team of changes in a patient’s condition that may require intervention. Each alarm represents a different potential problem.
What is a Ventilator Alarm?
A ventilator alarm is a safety feature on the mechanical ventilator that applies a set of parameters to provide alerts whenever there is a problem related to the patient-ventilator interaction. The alarms can be visual, audible, or both, depending on the type of ventilator and settings. Ventilator manufacturers have taken various approaches to alarms. The majority of ventilators allow the user to program default alarm thresholds based on various patient populations (6). Many apply predefined settings, such as +/- 30% of the current minute ventilation. Typical ventilators provide the ability to set alarm thresholds for peak inspiratory pressure, tidal volume, frequency, and minute ventilation, while others do not provide limits (6).
There are many types of ventilator alarms, including:
- High Pressure
- Low Pressure
- Low Volume
- Apnea
- High or Low PEEP
High Pressure Alarm
A high-pressure alarm is triggered whenever the circuit pressure exceeds a preset pressure limit during the inspiratory phase of breathing. The preset limit for the high-pressure alarm is typically set around 10 cmH2O above the peak inspiratory pressure (PIP).
This alarm would be beneficial for patients with respiratory conditions that cause decreased lung compliance or increased airway resistance (2). Other causes of the alarm sounding include coughing, kinking of the airway, or thick and copious secretions. Correctly setting tidal volume alarms is imperative. In VCV, the action of the ventilator is directly controlling tidal volumes, so alarms can alert if this process has abnormalities.
Troubleshooting tips include: (8)
- Check for patient-ventilator asynchrony.
- Perform respiratory assessment.
- Provide endotracheal suctioning if needed.
- Check for a kink in tubing of the artificial airway.
- Relocate the endotracheal tube if it’s not in the correct position.
- Check for a malfunction of the inspiratory or expiratory valves.

Self Quiz
Ask yourself...
- Have you ever been able to recognize various alarms on medical equipment?
- Do you have experience with troubleshooting alarm notifications once you determine the alarm sounded due to an error?
Low Pressure Alarm
A low-pressure alarm is triggered when the peak inspiratory pressure (PIP) pressure in mechanical ventilation is below a preset level. This most commonly occurs whenever there is a leak or disconnection in the system (8). If the cause of the alarm is unknown, the patient should be manually ventilated until the source of the leak is identified.
Troubleshooting tips include:
- Check for a leak or disconnection in the circuit and exhalation valve.
- Check for a leak in the pilot balloon.
- Ensure that the endotracheal tube is properly located.
- Ensure that the endotracheal tube cuff is adequately inflated.
- Ask respiratory therapist or physician if the ventilator settings should be adjusted.
Low Volume Alarm
A low volume alarm is triggered whenever the expiratory volume decreases below a preset low volume threshold (6). This alarm is helpful because it assesses if the patient is receiving and exhaling a minimum tidal volume. If this alarm sounds, the respiratory therapist should be consulted.
Apnea Alarm
An apnea alarm is triggered whenever the total frequency decreases below a preset frequency limit. The alarm is critical to determine if the patient is receiving an adequate number of breaths. The apnea alarm most commonly sounds when there is a disconnection of the circuit from the endotracheal tube (6). If this occurs, the respiratory therapist must ensure that the patient is being ventilated by delivering manual breaths until the disconnection source is identified.
High or Low PEEP Alarm
A high or low PEEP alarm is triggered whenever the level of PEEP exceeds or falls below a preset PEEP limit. The high PEEP alarm most commonly sounds whenever auto-PEEP or air trapping is present (2). A potential cause of the low PEEP alarm is active inspiration by the patient (6). Active inspirator by the patient causes the PEEP level to drop below the preset alarm setting and the settings may be adjusted based on changes in the patient’s condition.
Alarm Fatigue
Although ventilator alarms have invaluable meaning, the alarms can sound frequently without a meaningful reason. Alarm fatigue is frustration felt by healthcare providers with unactionable or insignificant alarms (6). A recent study found that alarms can sound as many as 942 alarms per day (6). Nurses must become familiar with the sounds so they can prioritize their responsiveness. Research suggests that 80–99% of ventilator alarms in general are false or nonactionable (6). There have been policy changes and interventions regarding alarm fatigue and overwhelming alarms with no true significance.
The Joint Commission introduced “Use alarms safely” as a National Patient Safety Goal in 2014 (6). Phase 1 required hospitals to identify the most important alarm signals to manage and inquired, “what mechanical ventilation alarms are important?” and “who determines if an alarm is unnecessary?” (6). Policy changes like this are impactful to the individual nurse and patient, as it made practical changes that impact practice. Although nurses and clinicians appreciate meaningful alarms, it can take them away from issues with higher priority if it constantly alarms for unnecessary reasons.

Self Quiz
Ask yourself...
- Can you name the most common alarms on a mechanical ventilator?
- What do you think contributes to alarm fatigue (ex: high workload, patient frustration)?
- Can you name members of the healthcare team that can help with setting alarm parameters?
- Can you imagine how alarms can impact patient anxiety and sleep habits?
Nursing Care
Nursing care should prioritize maintenance of a patent airway, gas exchange, prevention of trauma, therapeutic communication, and assessment of cardiac and pulmonary complications.
Nursing Priorities
- Ensuring a patent airway and assessing for proper placement of the endotracheal tube
- Monitoring the patient’s respiratory status
- Assessing lung sounds
- Oxygen saturation levels, and
- End-tidal carbon dioxide (EtCO2) monitoring.
- Monitoring patient comfort and pain levels.
- Preventing complications associated with mechanical ventilation.
- Ventilator-associated pneumonia
- Ventilator-induced lung injury
- Collaborating with the healthcare team
- Optimize ventilator settings
- Weaning protocols
- Providing ongoing education for patient and family
Nursing Assessment
- Adventitious breath sounds
- Diminished lung sounds
- Increased or decreased respiratory rate.
- Dyspnea
- Decreased oxygen saturation (Sao2 <90%)
- Arterial pH less than 7.35
- Decreased tidal volume.
- Decreased Pao2 level (>50 to 60 mm Hg)
- Increased Paco2 level (50 to 60 mm Hg or higher)
- Restlessness
- Excessive secretions
- Ineffective cough
Nursing Interventions and Actions
- Assess the client’s respiratory rate, depth, and pattern, including the use of accessory muscles.
- Count the client’s respirations for one full minute and compare with ventilator set rate and desired respiratory rate.
- Observe changes in the level of consciousness.
- Early signs of hypoxia include disorientation, irritability, and restlessness; late signs include lethargy, stupor (8).
- Assess the client’s heart rate and blood pressure.
- Tachycardia may be a result of hypoxia (8).
- Auscultate the lung for normal or adventitious breath sounds.
- Bilateral basilar crackles may indicate pulmonary edema or volume overload, other signs of that includes jugular vein distention and lower limb edema (8). Wheezing and rhonchi are present in obstructive lung disease (8). Absent lung sounds may indicate massive pleural effusion or pneumothorax (8).
- Assess the skin color and examine the lips and nailbeds for cyanosis.
- Monitor oxygen saturation using pulse oximetry.
- Maintain the client’s airway.
- Use suctioning as needed.
- Monitor arterial blood gases (ABGs) as indicated.
- ABGs during respiratory failure may reveal increasing PaCo2 and decreasing PaO2 (8).
- Assess for correct endotracheal (ET) tube placement through observation for symmetrical chest rise, auscultation of bilateral breath sounds, and X-ray confirmation.
- Upon auscultation, if frequent crackles or rhonchi are heard and do not clear with coughing or suctioning, it may indicate developing atelectasis, acute bronchospasm, pneumonia, or pulmonary edema (6).
- Assess for the client’s comfort and pain level.
- Assess the ventilator settings and alarm system every hour.
- Patient positioning.
- Maintain the client in a High-Fowler’s position as tolerated and frequently check the position. This position encourages chest expansion and increases oxygenation.
- Promote optimal nutritional balance.
- Weigh the client regularly.
- Assess if patient can safely eat.
- Auscultate for bowel sounds. Document and report loose stool or absence of bowel movements. -Document abdominal girth measurements.
- Monitor gastric residual volumes following enteral feedings. Gastric residual volumes should be monitored to avoid gastric distention and avoid risk of regurgitation and aspiration.
- Offer food that the client desires and document when oral intake resumes.
- Consult nutritionist and be knowledgeable on nutrients that are vital. For example, protein is a vital nutrient to support wound healing and immune function and to maintain lean body mass (8)
- Assess the client’s and caregiver’s perception and understanding of mechanical ventilation.
- Assess the client’s readiness and ability to learn.
- Encourage the client or significant others to express feelings and ask questions about care.
- Provide ongoing education to patient and caregivers. Use material in multiple formats; for example, books, printed pamphlets, audiovisuals, demonstrations, and instruction sheets. Examples include, but not limited to:
- Explain the need for suctioning as needed.
- Explain that alarms, what they indicate, and that they may periodically sound off, which may be normal.
- Explain the weaning process.
- If long-term ventilation is anticipated, discuss, or plan for long-term ventilator care management and use appropriate referrals: long-term ventilator facilitates versus home care management.
- Community resources may include food and meal services, physical and occupational therapy transportation, and access to client support groups. Social workers should become involved if patient is going home with an invasive mechanical ventilator.

Self Quiz
Ask yourself...
- Do you feel comfortable with airway suctioning?
- What do you think the most optimal patient position is for mechanical ventilation?
- Why would supine position not be appropriate for proper ventilation?
- Can you explain the interventions for maintaining nutrition in the mechanically ventilated patient?

Self Quiz
Ask yourself...
- What are some problems that may occur in the mechanically ventilated patient?
- What do you think the nurse should prioritize in the ventilated patient?
- Can you think of possible questions the patient or family may have regarding ventilator care?
- Can you name interventions to provide holistic care for patients on long-term mechanical ventilation?
Conclusion
BODY TEXT
References + Disclaimer
- American Nurses Association (ANA). (2015). Code of ethics with interpretative statements. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/
- Baptiste, D. L., Caviness-Ashe, N., Josiah, N., Commodore-Mensah, Y., Arscott, J., Wilson, P. R., & Starks, S. (2022). Henrietta Lacks and America’s dark history of research involving African Americans. Nursing Open, 9(5), 2236–2238. https://doi.org/10.1002/nop2.1257
- Barrow, J. M., Brannan, G. D., & Khandhar, P. B. (2022, September 18). Research ethics. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459281/
- Centers for Disease Control and Prevention. (2024, September 4). The untreated syphilis study at Tuskegee timeline. https://www.cdc.gov/tuskegee/about/timeline.html
- Christman, E., Christman, T., Demaster, V. Ernstmeyer, K., Kliminski, K., Olson, A., Pomietlo, M., Roesler, A., Stewart, J., Teeter, J., Tyznik, A. & Zwicky, J. (2022). Chapter 6: Ethical practice. In K. Ernstmeyer & E. Christman (Eds.), Nursing management and professional concepts [Internet]. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/nursingmpc/chapter/6-3-ethical-dilemmas/
- Haddad, L. M., & Geiger, R. A. (2023, August 14). Nursing ethical considerations. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/sites/books/NBK526054/0
- John Hopkins Medicine. (n. d.). The legacy of Henrietta Lacks. https://www.hopkinsmedicine.org/henrietta-lacks
- Office of Science Policy, National Institutes of Health. (2022, October). Significant research advances enabled by HeLa cells. https://osp.od.nih.gov/hela-cells/significant-research-advances-enabled-by-hela-cells/
- Olejarczyk, J. P., & Young, M. (2024, May). Patient rights and ethics. In: StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538279/
- Shea, B. (2023, October 18). Four principles of bioethics. In Ethical explorations: Moral dilemmas in a universe of possibilities. Minnesota Libraries Publishing Project; Rochester, MN. https://mlpp.pressbooks.pub/ethicalexplorations/chapter/chapter-12-bioethics12/
- Tobin, M. J. (2022). Fiftieth anniversary of uncovering the Tuskegee syphilis study: The story and timeless lessons. American Journal of Respiratory and Critical Care Medicine, 205(10), 1145–1158. https://doi.org/10.1164/rccm.202201-0136SO
ELEMENT I
- https://www.op.nysed.gov/title8/rules-board-regents/part-29
- https://regs.health.ny.gov/content/section-92-11-course-work-or-training
- https://www.cdc.gov/oralhealth/infectioncontrol/summary-infection-prevention-practices/standard-precautions.html
- https://www.nursingworld.org/practice-policy/work-environment/health-safety/infection-prevention/
- https://www.cdc.gov/infectioncontrol/guidelines/core-practices/index.html
- https://www.cdc.gov/hai/data/portal/progress-report.html
- https://www.ncsbn.org/filing-a-complaint.htm
ELEMENT II
- Douedi, S., & Douedi, H. (2020) Precautions, bloodborne, contact, and droplet. In StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK551555/
- https://www.cdc.gov/niosh/topics/healthcare/infectious.html
- Abbas AK, Lichtman AH, Pillai S. Properties and overview of immune responses. In: Abbas AK, Lichtman AH, Pillai S, eds. Cellular and Molecular Immunology. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 1.
- https://www.cdc.gov/training/publichealth101/e-learning/prevention-effectiveness/
- https://www.cdc.gov/infectioncontrol/basics/standard-precautions.html
- https://www.cdc.gov/injectionsafety/spinalinjection-meningitis.html
- Carrico, R., Garrett, H., Balcom, D, & Burton Glowicz, J. (2018). Infection prevention and control core practice: a roadmap for nursing practice. Nursing, 48(8), 28-29. doi: 10.1097.NURSE.0000544318.36012.b2
- Sands, M.,& Aunger, R. (2020). Determinants of hand hygiene compliance among nurses in US hospitals: a formative research study. PLoS ONE, 15(4), 2-29. doi: 10.1371/journal. pone.0230573
- Pyrek, K. (2017). Cleanliness of hands and surfaces play key role in cross-contamination prevention. Infection Control Today, 21(5).Retrieved from https://www.infectioncontroltoday.com/view/cleanliness-hands-and-surfaces-plays-key-role-cross-contamination-prevention
- Assadian, O., Kramer, A., Cristiansen, B., Exner, M., Martiny, H., Sorger, A., & Suchomel, M. (2012). Recommendations and requirements for soap and hand rub dispensers in healthcare facilities. GMS Krankenhhyg Interdisziplinar, 7(1), 4-5. doi: 10.3205/dgkh000187
- https://www.cdc.gov/infectioncontrol/projectfirstline/resources/ppe-covid-19.html
- Watson, N. (2007). Isolation and cohort care. The Journal of the Intensive Care Society, 8(3). Retreived from https://journals.sagepub.com/doi/pdf/10.1177/175114370700800308
- https://www.cdc.gov/infectioncontrol/guidelines/isolation/
- https://www.hhs.gov/vaccines/vaccines-national-strategic-plan/vision-and-goals/index.html
- https://www.cdc.gov/infectioncontrol/pdf/guidelines/environmental-guidelines-P.pdf
- https://www.dec.ny.gov/chemical/8789.html
- https://regs.health.ny.gov/content/section-83-117-linen-and-laundry
ELEMENT III
- https://www.osha.gov/etools/hospitals/hospital-wide-hazards/biological-hazards
- Kossover-Smith, R. Coutts, K., Hatfield, K., Cochran, R., Akselrod, H., Schaefer, . . . & Bruss, K. (2017). One needle, one syringe, only one time? A survey of physician and nurse knowledge, attitudes, and practices around injection safety. American Journal of Infection Control, 45(9), 1018-1023. doi: 10.1016/j.ajic.2017.04.292
- https://www.cdc.gov/sharpssafety/pdf/sharpsworkbook_2008.pdf
ELEMENT IV
- https://www.cdc.gov/infectioncontrol/pdf/strive/PPE103-508.pdf
- https://www.ventyv.com/blog/whats-the-difference-between-nitrile-latex-and-vinyl-gloves
- https://www.cdc.gov/niosh/npptl/topics/protectiveclothing/default.html
- https://www.cdc.gov/niosh/topics/respirators/
- https://www.cdc.gov/niosh/topics/bbp/
ELEMENT V
- https://www.cdc.gov/infectioncontrol/pdf/guidelines/disinfection-guidelines-H.pdf
- https://www.cdc.gov/infectioncontrol/guidelines/disinfection/efficacy.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3678066/
- https://www.cdc.gov/infectioncontrol/guidelines/disinfection/cleaning.html
- https://www.osha.gov/Publications/OSHA3512.pdf
ELEMENT VI
- https://www.cdc.gov/infectioncontrol/guidelines/healthcare-personnel/evaluation.html
- https://www.cdc.gov/tb/topic/testing/tbtesttypes.htm
- https://www.cdc.gov/infectioncontrol/pdf/guidelines/infection-control-HCP-H.pdf
- https://www.nyc.gov/assets/doh/downloads/pdf/hcp/reporting-guide.pdf
- https://www.cdc.gov/tb/topic/treatment/decideltbi.htm
- https://www.health.ny.gov/publications/1852/appenb.htm
- https://www.cdc.gov/infectioncontrol/guidelines/healthcare-personnel/exposures.html
ELEMENT VII
- https://www.health.ny.gov/diseases/conditions/sepsis/
- https://www.health.ny.gov/facilities/public_health_and_health_planning_council/meetings/2013-02-07/docs/13-01.pdf
- https://www.health.ny.gov/diseases/conditions/sepsis/docs/2019_sepsis_care_improvement_initiative.pdf
- https://www.nhsinform.scot/illnesses-and-conditions/blood-and-lymph/septic-shock
- Kim, H, & Park, S. (2019). Sepsis: Early recognition and optimized treatment. Tuberculosis and Respiratory Disease, 82(1), 6-14. doi: 10.4046/trd.2018.0041
- https://www.sccm.org/SurvivingSepsisCampaign/Guidelines/Adult-Patients
- https://www.mayoclinic.org/diseases-conditions/sepsis/diagnosis-treatment/drc-20351219
- https://www.cdc.gov/sepsis/pdfs/Consumer_fact-sheet_protect-yourself-and-your-family-P.pdf
- New ACC/AHA High Blood Pressure Guidelines Lower Definition of Hypertension – American College of Cardiology. (2017, November 8). American College of Cardiology. https://www.acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017
- Facts about hypertension | CDC.gov. (2023, July 6). Centers for Disease Control and Prevention. https://www.cdc.gov/bloodpressure/facts.htm
- Ostchega, Y., Fryar, C. D., Nwankwo, T., & Nguyen, D. T. (2020). Hypertension Prevalence Among Adults Aged 18 and Over: United States, 2017-2018. NCHS data brief, (364), 1–8.
- Multiple cause of death data on CDC WONDER. (2023, September 8). Retrieved September 18, 2023, from https://wonder.cdc.gov/mcd.html.
- Carretero, O. A., & Oparil, S. (2000). Essential Hypertension. Circulation, 101(3), 329–335. https://doi.org/10.1161/01.cir.101.3.329
- Koch, C. (2020, February 4). Overview of Endocrine Hypertension. Endotext – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK278980/
- Manosroi, W., & Williams, G. H. (2018). Genetics of Human Primary Hypertension: Focus on Hormonal Mechanisms. Endocrine Reviews, 40(3), 825–856. https://doi.org/10.1210/er.2018-00071
- Ayada, C. (2015, June 1). The relationship of stress and blood pressure effectors. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4938117/
- Terry, K. W., Kam, K. K., Yan, B. P., & Lam, Y. (2010). Renin-angiotensin-aldosterone system blockade for cardiovascular diseases: current status. British Journal of Pharmacology, 160(6), 1273–1292. https://doi.org/10.1111/j.1476-5381.2010.00750.x
- Bryan, N. S. (2022). Nitric oxide deficiency is a primary driver of hypertension. Biochemical Pharmacology, 206, 115325. https://doi.org/10.1016/j.bcp.2022.115325
- Sarathy, H., Salman, L. A., Lee, C., & Cohen, J. B. (2022). Evaluation and Management of Secondary Hypertension. Medical Clinics of North America, 106(2), 269–283. https://doi.org/10.1016/j.mcna.2021.11.004
- Muniyappa, R., Iantorno, M., & Quon, M. J. (2008). An Integrated View of Insulin Resistance and Endothelial Dysfunction. Endocrinology and Metabolism Clinics of North America, 37(3), 685–711. https://doi.org/10.1016/j.ecl.2008.06.001
- Heart-Health Screenings. (2022, August 23). www.heart.org. https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/heart-health-screenings
- Pena-Hernandez, C., Nugent, K., & Tuncel, M. (2019). Twenty-Four-Hour Ambulatory Blood Pressure Monitoring. Journal of Primary Care & Community Health, 11, 215013272094051. https://doi.org/10.1177/2150132720940519
- Gulec, S. (2013). Early diagnosis saves lives: focus on patients with hypertension. Kidney International Supplements, 3(4), 332–334. https://doi.org/10.1038/kisup.2013.69
- (2023, June 22). UpToDate. Retrieved September 18, 2023, from https://www.uptodate.com/contents/choice-of-drug-therapy-in-primary-essential-hypertension/print
- Types of Blood Pressure Medications. (2023, June 6). www.heart.org. https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications
- Moxonidine: a new antiadrenergic antihypertensive agent. (1999, August 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/10489098/
- Liang, W., Ma, H., Cao, L., Yan, W., & Yang, J. (2017). Comparison of thiazide-like diuretics versus thiazide-type diuretics: a meta-analysis. Journal of Cellular and Molecular Medicine, 21(11), 2634–2642. https://doi.org/10.1111/jcmm.13205
- Greenberg, B. (2019). Angiotensin Receptor-Neprilysin Inhibition (ARNI) in Heart Failure. International Journal of Heart Failure, 2(2), 73. https://doi.org/10.36628/ijhf.2020.0002
- Filippatos, G., Anker, S. D., Agarwal, R., Ruilope, L., Rossing, P., Bakris, G. L., Tasto, C., Joseph, A., Kolkhof, P., Lage, A., & Pitt, B. (2022). Finerenone Reduces Risk of Incident Heart Failure in Patients With Chronic Kidney Disease and Type 2 Diabetes: Analyses From the FIGARO-DKD Trial. Circulation, 145(6), 437–447. https://doi.org/10.1161/circulationaha.121.057983
- Brown, C., & Garovic, V. D. (2014). Drug Treatment of Hypertension in Pregnancy. Drugs, 74(3), 283–296. https://doi.org/10.1007/s40265-014-0187-7
- Zhang, Y., He, D., Zhang, W., Xing, Y., Guo, Y., Wang, F., Jia, J., Yan, T., Liu, Y., & Lin, S. (2020). ACE Inhibitor Benefit to Kidney and Cardiovascular Outcomes for Patients with Non-Dialysis Chronic Kidney Disease Stages 3–5: A Network Meta-Analysis of Randomised Clinical Trials. Drugs, 80(8), 797–811. https://doi.org/10.1007/s40265-020-01290-3
- McGuire, H. L., Svetkey, L. P., Harsha, D. W., Elmer, P. J., Appel, L. J., & Ard, J. D. (2004). Comprehensive Lifestyle Modification and Blood Pressure Control: A Review of the PREMIER Trial. Journal of Clinical Hypertension, 6(7), 383–390. https://doi.org/10.1111/j.1524-6175.2004.03147.x
- Vasheghani-Farahani, A., Mansournia, M. A., Asheri, H., Fotouhi, A., Yunesian, M., Jamali, M., & Ziaee, V. (2010). The Effects of a 10-Week Water Aerobic Exercise on the Resting Blood Pressure in Patients with Essential Hypertension. Asian Journal of Sports Medicine, 1(3). https://doi.org/10.5812/asjsm.34854
- Li, Y., Buys, N., Li, Z., Li, L., Song, Q., & Sun, J. (2021). The efficacy of cognitive behavioral therapy-based interventions on patients with hypertension: A systematic review and meta-analysis. Preventive Medicine Reports, 23, 101477. https://doi.org/10.1016/j.pmedr.2021.101477
- DiGregorio AM, Alvey H. Gastrointestinal bleeding. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537291/
- Graham, & Carlberg, D. J. (Eds.). (2019). Gastrointestinal emergencies: evidence-based answers to key clinical questions. Springer. https://doi.org/10.1007/978-3-319-98343-1
- Kaur, A., Baqir, S. M., Jana, K., & Janga, K. C. (2023). Risk of gastrointestinal bleeding in patients with end-stage renal disease: The Link between Gut, Heart, and Kidneys. Gastroenterology Research & Practice, 1–10. https://doi.org/10.1155/2023/9986157
- Kumar, Verma, A., & Kumar T, A. (2021). Management of Upper GI bleeding. Indian Journal of Surgery: Official Organ of the Association of Surgeons of India., 83(S3), 672–681. https://doi.org/10.1007/s12262-019-02055-3
- Ogobuiro I, Gonzales J, Shumway KR, et al. Physiology, gastrointestinal. [Updated 2023 Apr 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537103/
- Ramaekers, R., Perry, J., Leafloor, C., & Thiruganasambandamoorthy, V. (2020). Prediction model for 30-day outcomes among emergency department patients with lower gastrointestinal bleeding. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 21(2), 343–347. https://doi.org/10.5811/westjem.2020.1.45420
- Saydam ŞS, Molnar M, Vora P. The global epidemiology of upper and lower gastrointestinal bleeding in general population: A systematic review. World J Gastrointest Surg. 2023 Apr 27;15(4):723-739. doi: 10.4240/wjgs.v15.i4.723. PMID: 37206079; PMCID: PMC10190726.
- Tadros, & Wu, G. Y. (Eds.). (2021). Management of occult GI bleeding: a clinical guide. Humana Press. https://doi.org/10.1007/978-3-030-71468-0
- Williams, L. S., & Hopper, P. D. (2019). Understanding medical-surgical nursing. F.A. Davis Company.
- American Gastroenterological Association. (2023). ACG and AGA guideline on chronic constipation management is first to recommend supplements magnesium oxide and senna as evidence-based treatments. Retrieved December 24, 2024, from https://gastro.org/press-releases/acg-and-aga-guideline-on-chronic-constipation-management-is-first-to-recommend-supplements-magnesium-oxide-and-senna-as-evidence-based-treatments/
- Chang L, Chey WD, Imdad A, Almario CV, Bharucha AE, Diem S, Greer KB, Hanson B, Harris LA, Ko C, Murad MH, Patel A, Shah ED, Lembo AJ, Sultan S. American Gastroenterological Association-American College of Gastroenterology Clinical Practice Guideline: Pharmacological Management of Chronic Idiopathic Constipation. Gastroenterology. 2023 Jun;164(7):1086-1106. Doi: 10.1053/j.gastro.2023.03.214. PMID: 37211380; PMCID: PMC10542656.
- Huang, D. (2024). Constipation. In: Desai, B.K., Desai, A., Ganti, L., Elbadri, S. (eds) Primary Care for Emergency Physicians. Springer, Cham. https://doi.org/10.1007/978-3-031-64676-8_17
- Jiang Y, Tang Y, Lin L. Clinical Characteristics of Different Primary Constipation Subtypes in a Chinese Population. J Clin Gastroenterol. 2020 Aug;54(7):626-632. Doi: 10.1097/MCG.0000000000001269. PMID: 31592795; PMCID: PMC7368843.
- Lippincott Williams & Wilkins, editor, Cromar, K. C., & Moebius, C. (2023). Medical-surgical nursing made incredibly easy! (5th ed.). Wolters Kluwer.
- Rao, S. S. C., Parkman, H. P., & McCallum, R. W. (Eds.). (2024). Handbook of gastrointestinal motility and functional disorders (First edition.). CRC Press, Taylor & Francis Group. https://doi.org/10.1201/9781003524519
- Werth BL, Christopher SA. Potential risk factors for constipation in the community. World J Gastroenterol. 2021 Jun 7;27(21):2795-2817. Doi: 10.3748/wjg.v27.i21.2795. PMID: 34135555; PMCID: PMC8173388.
- Williams, L. S., & Hopper, P. D. (2019). Understanding medical-surgical nursing (6th ed.). F.A. Davis Company.
- World Health Organization (WHO). (2024). Social determinants of health. Retrieved, from https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1.
- Zhao Q, Chen YY, Xu DQ, Yue SJ, Fu RJ, Yang J, Xing LM, Tang YP. Action Mode of Gut Motility, Fluid and Electrolyte Transport in Chronic Constipation. Front Pharmacol. 2021 Jul 27;12:630249. Doi: 10.3389/fphar.2021.630249. PMID: 34385914; PMCID: PMC8353128.
- United Spinal Association. (n.d.). What is spinal cord injury/disorder? Retrieved from https://unitedspinal.org/what-is-spinal-cord-injury-disorder-scid/
- United Spinal Association. (2022). Spinal cord injuries facts and stats. Retrieved from https://unitedspinal.org/spinal-cord-injury-facts-and-stats/
- S. Department of Health and Human Services, National Institutes of Health. (2022). What causes spinal cord injury (SCI) and how does it affect your body? Retrieved from https://www.nichd.nih.gov/health/topics/spinalinjury/conditioninfo/causes
- World Health Organization. (2013). Spinal cord injury. Retrieved from https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury
- National Institute of Neurological Disorders and Stroke. (2023). Spinal cord injury. Retrieved from https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury
- National Spinal Cord Injury Statistical Center. (2023). Traumatic spinal cord injury statistics: Facts and figures at a glance. Retrieved from https://www.nscisc.uab.edu/public/Facts%20and%20Figures%202023%20-%20Final.pdf
- Centers for Disease Control and Prevention. (2020). Many adults with disabilities report frequent mental distress. Retrieved from https://www.cdc.gov/ncbddd/disabilityandhealth/features/adults-with-disabilities-mental-distress.html
- Allen K. J. & Leslie S. W. (2023). Autonomic dysreflexia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482434/
- Bowel and Bladder Community. (n.d.). Spinal injuries. Retrieved from https://www.bladderandbowel.org/help-information/spinal-injuries/
- Shepherd Center. (n.d.). Bowel function after SCI. Retrieved from https://www.myshepherdconnection.org/sci/bowel-care/function-after-sci
- Emmanuel A. (2019). Neurogenic bowel dysfunction. F1000Research, 8, F1000 Faculty Rev-1800. https://doi.org/10.12688/f1000research.20529.1
- Gater, D. R., Bauman, C., & Cowan, R. (2020). A primary care provider’s guide to diet and nutrition after spinal cord injury. Topics in spinal cord injury rehabilitation, 26(3):197–202. https://doi.org/10.46292/sci2603-197
- Christopher & Dana Reeve Foundation. (2023). Our mission. Retrieved from https://www.christopherreeve.org/community/about-us/history-of-the-reeve-foundation/
- University of Miami, Miller School of Medicine. (n.d.). About us. Retrieved from https://www.themiamiproject.org/about-us/
- S. Department of Health and Human Services, Administration for Community Living. (n.d.) Advancing independence, integration, and inclusion throughout life. Retrieved from https://acl.gov/
- Paralyzed Veterans of America. (n.d.). Mission statement. Retrieved from https://pva.org/about-us/mission-statement/
- United Spinal Association. (2023). About us. Retrieved from https://unitedspinal.org/our-story/
- Agency for Healthcare Research and Quality. (2014). Preventing pressure ulcers in hospitals: Are we ready for this change? Retrieved from https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu1.html
- Agency for Healthcare Research and Quality. (2014). Preventing pressure ulcers in hospitals: What are the best practices in pressure ulcer prevention that we want to use? Retrieved from https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu3.html
- Agency for Healthcare Research and Quality. (2017). Estimating the additional hospital inpatient cost and mortality associated with selected hospital-acquired conditions. Retrieved from https://www.ahrq.gov/hai/pfp/haccost2017-results.html
- Agency for Healthcare Research and Quality. (2017). Patient safety indicators™ v2020 benchmark data tables. Retrieved https://qualityindicators.ahrq.gov/Downloads/Modules/PSI/V2020/Version_2020_Benchmark_Tables_PSI.pdf
- Agency for Healthcare Research and Quality. (2017). Pressure injury prevention program implementation guide. Retrieved https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureinjury/guide/intro.html#Program
- Agency for Healthcare Research and Quality. (2020). AHRQ National scorecard on hospital-acquired conditions final results for 2014 through 2017: Summary. Retrieved from https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/pfp/Updated-hacreportFInal2017data.pdf
- Al Aboud, A. M. & Manna, B. (2023). Wound pressure injury management. In StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532897/
- Black, J. et al. (2023). Current perspectives on pressure injuries in persons with dark skin tones from the National Pressure Injury Advisory Panel. Advances in Skin & Wound Care, 36(9):470-480. Retrieved from https://journals.lww.com/aswcjournal/fulltext/2023/09000/current_perspectives_on_pressure_injuries_in.5.aspx
- Brennan, M. (2022). Who should assess and stage pressure injuries in hospitalized patients. Advances in Skin & Wound Care 35(9):473-476. Retrieved from https://journals.lww.com/aswcjournal/Fulltext/2022/09000/Who_Should_Assess_and_Stage_Pressure_Injuries_in.2.aspx
- Broderick, V. V. & Cowan, L. J. (2021). Pressure injury related to friction and shearing forces in older adults. Journal of Dermatology and Skin Science. Retrieved from https://www.dermatoljournal.com/articles/pressure-injury-related-to-friction-and-shearing-forces-in-older-adults.html
- Centers for Medicare and Medicaid Services. (2023). Quality measures. Retrieved from https://www.cms.gov/medicare/quality/measures
- Centers for Medicare and Medicaid Services. (2023). Quality measurement and quality improvement. Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/Quality-Measure-and-Quality-Improvement-
- Cox, J. & Schallom, M. (2021). Pressure injuries in critical care patients: a conceptual schema. Advances in Skin & Wound Care 34(3):124-131. Retrieved from https://journals.lww.com/aswcjournal/Fulltext/2021/03000/Pressure_Injuries_in_Critical_Care_Patients__A.4.aspx
- Edsberg, L. E. et al. (2016). Revised National Pressure Ulcer Advisory Panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound Ostomy Continence Nursing, 43(6):585-597. Retrieved from https://journals.lww.com/jwocnonline/fulltext/2016/11000/revised_national_pressure_ulcer_advisory_panel.3.aspx
- The Joint Commission. (2022). Quick Safety 25: Preventing pressure injuries (Updated March 2022). Retrieved from https://www.jointcommission.org/resources/news-and-multimedia/newsletters/newsletters/quick-safety/quick-safety-issue-25-preventing-pressure-injuries/preventing-pressure-injuries/
- Kottner, J.; Cuddigan, J.; Carville, K.; Balzer, K.; Berlowitz, D.; Law, S.; Litchford, M.; Mitchell, P.; Moore, Z.; Pittman, J.; et al. Prevention and Treatment of Pressure Ulcers/Injuries: The Protocol for the Second Update of the International Clinical Practice Guideline 2019. J. Tissue Viability 2019, 28, 51–58.
- Mondragon, N. & Zito, P. M. (2022). Pressure injury. In StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557868/
- National Pressure Injury Advisory Panel. (2016). Pressure injury and stages. Retrieved from https://cdn.ymaws.com/npiap.com/resource/resmgr/NPIAP-Staging-Poster.pdf
- National Pressure Injury Advisory Panel. (2016). Pressure injury prevention points. Retrieved from https://npiap.com/page/PreventionPoints
- National Pressure Injury Advisory Panel. (2020). Best practices for prevention of medical device-related pressure injuries. Retrieved from https://npiap.com/page/MDRPI-Posters
- Nursing Times (2020). Pressure Ulcer Education 5: Keeping Patients Moving. Retrieved on September 12th, 2023, from https://www.nursingtimes.net/clinical-archive/tissue-viability/pressure-ulcer-education-5-keeping-patients-moving-13-01-2020/
- Pitman, J. et al. (2019). Hospital-acquired pressure injuries in critical and progressive care: Avoidable versus unavoidable. American Journal of Critical Care, 28(5):338-350. Retrieved from https://doi.org/10.4037/ajcc2019264
- Salcido, R. (2016). From pressure ulcers to “pressure injury”: Disambiguation and anthropology. Advances in Skin & Wound Care, 29(7): Retrieved from https://journals.lww.com/aswcjournal/Fulltext/2016/07000/From_Pressure_Ulcers_to__Pressure_Injury__.1.aspx
- Shear Force” and “Shear Force Closeup” by Meredith Pomietlo at Chippewa Valley Technical College are licensed under CC BY 4.0
- Tenny, S. & Hoffman, M. R. (2023). Prevalence. In StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430867/
- Zhang, X. et al. (2021). The global burden of decubitus ulcers from 1990 to 2019. Scientific Reports 11(21750). Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8571371/
- Agarwal, P., Kukrele, R., & Sharma, D. (2019). Vacuum assisted closure (VAC)/ negative pressure wound therapy (NPWT) for difficult wounds: A review. Journal of clinical orthopaedics and trauma, 10(5), 845–848. https://doi.org/10.1016/j.jcot.2019.06.015
- Baranoski, & Ayello, E. A. (2020). Wound care essentials: practice principles (5th ed.). Wolters Kluwer.
- George, J. et al. (2017). Negative pressure wound therapy: principles and usage in orthopedic surgery. In: Shiffman, M., Low, M. (eds) Pressure Injury, Diabetes and Negative Pressure Wound Therapy. Recent Clinical Techniques, Results, and Research in Wounds, vol 3. Springer, Cham. https://doi.org/10.1007/15695_2017_53
- McNichol, Ratliff, C., & Yates, S. (2021). Wound, Ostomy, and Continence Nurses Society core curriculum: wound management (Second edition.). Wolters Kluwer Health.
- Shiffman, M.A. (2017). History of negative pressure wound therapy (NPWT). In: Shiffman, M., Low, M. (eds) Pressure Injury, Diabetes and Negative Pressure Wound Therapy. Recent Clinical Techniques, Results, and Research in Wounds, vol 3. Springer, Cham. https://doi.org/10.1007/15695_2017_50
- Williams, L. S., & Hopper, P. D. (2019). Understanding medical-surgical nursing. F.A. Davis Company.
- Zaver V, Kankanalu P. Negative pressure wound therapy. (2022). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK576388/
- Basiri, R., Spicer, M. T., Levenson, C. W., Ormsbee, M. J., Ledermann, T., & Arjmandi, B. H. (2020). Nutritional supplementation concurrent with nutrition education accelerates the wound healing process in patients with diabetic foot ulcers. Biomedicines, 8(8), 263. https://doi.org/10.3390/biomedicines8080263
- Beyene, R. T., Derryberry, S., & Barbul, A. (2020). The effect of comorbidities on wound healing. Surgical Clinics of North America, 100(4), 695–705. https://doi.org/10.1016/j.suc.2020.05.002
- Bishop, A., Witts, S., & Martin, T. (2018). The role of nutrition in successful wound healing. Journal of Community Nursing, 32(4), 44–50.
- Ellis, S., Lin, E. J., & Tartar, D. (2018). Immunology of wound healing. Current Dermatology Reports, 7(4), 350–358. https://doi.org/10.1007/s13671-018-0234-9
- Ghaly, P., Iliopoulos, J., & Ahmad, M. (2021). The role of nutrition in wound healing: An overview. British Journal of Nursing, 30(5), S38–S42. https://doi.org/10.12968/bjon.2021.30.5.s38
- Manley, S., & Mitchell, A. (2022). The impact of nutrition on pressure ulcer healing. British Journal of Nursing, 31(12), S26–S30. https://doi.org/10.12968/bjon.2022.31.12.s26
- Smith-Ryan, A. E., Hirsch, K. R., Saylor, H. E., Gould, L. M., & Blue, M. M. (2020). Nutritional considerations and strategies to facilitate injury recovery and rehabilitation. Journal of Athletic Training, 55(9), 918–930. https://doi.org/10.4085/1062-6050-550-19
- Talaska, K. (2020). A comparison of two protein supplements on the healing of stage iii and iv pressure injuries in enterally fed, ventilator dependent long – term care residents. Louisiana Tech Digital Commons. https://digitalcommons.latech.edu/theses/48
- Wei boon, Y., Azizan, N., Hasnol, E., Krishnan, K., Rajeswaran, S., Yin chow, J., Irwan, N., Indrajoth, P., Maran, munirah ismail, P., & Ismail, M. (2022). Potentials of immunonutrition in wound healing: A review. Jurnal Sains Kesihatan Malaysia, 20(2), 23–33. https://doi.org/10.17576/jskm-2022-2002-03
- Burgess-Stocks, Gleba, J., Lawrence, K., & Mueller, S. (2022). ostomy and continent diversion patient bill of rights. Journal of WOCN : Wound, Ostomy, and Continence Nursing., 49(3), 251–260. https://doi.org/10.1097/WON.0000000000000876
- Carmel, Colwell, J., & Goldberg, M. (2021). Wound, ostomy and continence nurse’s society core curriculum: ostomy management (Second edition.). Wolters Kluwer Health.
- Estrada, D. M. L., Benghi, L. M., & Kotze, P. G. (2021). Practical insights into stomas in inflammatory bowel disease: what every healthcare provider needs to know. Current Opinion in Gastroenterology, 37(4), 320–327. https://doi.org/10.1097/MOG.0000000000000737
- Hedrick, T. L., Sherman, A., Cohen-Mekelburg, S., & Gaidos, J. K. J. (2023). AGA Clinical Practice Update on Management of Ostomies: Commentary. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association, 21(10), 2473–2477. https://doi.org/10.1016/j.cgh.2023.04.035
- Hill, B. (2020). Stoma care: procedures, appliances and nursing considerations. British Journal of Nursing, 29(22), S14–S19. https://doi.org/10.12968/bjon.2020.29.22.s14
- Ogobuiro I, Gonzales J, Shumway KR, et al. Physiology, gastrointestinal. [Updated 2023 Apr 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537103/
- United Ostomy Associations of America, Inc. (2018). Know your ostomy pouching system & supplies. https://www.ostomy.org/know-your-ostomy-pouching-system-supplies/
- Urostomy and continent urinary diversion. (2006). U.S. Dept. of Health and Human Services, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
- Williams, L. S., & Hopper, P. D. (2019). Understanding medical-surgical nursing. F.A. Davis Company.
- American Association of Clinical Endocrinology (2021). What you need to know about diabetes. About Diabetes. https://www.aace.com/disease-and-conditions/diabetes/what-you-need-know-about-diabetes
- Berget, C., Messer, L. H., & Forlenza, G. P. (2019). A Clinical Overview of Insulin Pump Therapy for the Management of Diabetes: Past, Present, and Future of Intensive Therapy. Diabetes spectrum: a publication of the American Diabetes Association, 32(3), 194–204. https://doi.org/10.2337/ds18-0091
- Blonde, L., Umpierrez, G. E., Reddy, S. S., McGill, J. B., Berga, S. L., Bush, M., … & Weber, S. L. (2022). American Association of Clinical Endocrinology clinical practice guideline: developing a diabetes mellitus comprehensive care plan—2022 update. Endocrine Practice, 28(10), 923-1049.
- Center for Disease Control and Prevention. (2022). Estimates of diabetes and its burden in the United States. National diabetes statistics report. cdc.gov/diabetes/data/statistics-report/index.html
- Center for Disease Control and Prevention. (2022). Prevalence of both diagnosed and undiagnosed diabetes. https://www.cdc.gov/diabetes/data/statistics-report/diagnosed-undiagnosed-diabetes.html
- Center for Disease Control and Prevention. (2023). What is Diabetes? https://www.cdc.gov/diabetes/basics/diabetes.html
- ElSayed, N. A., Aleppo, G., Aroda, V. R., Bannuru, R. R., Brown, F. M., Bruemmer, D., … & Gabbay, R. A. (2023). 7. Diabetes technology: standards of care in diabetes—2023. Diabetes Care, 46(Supplement_1), S111-S127.
- Galicia-Garcia, U., Benito-Vicente, A., Jebari, S., Larrea-Sebal, A., Siddiqi, H., Uribe, K. B., Ostolaza, H., & Martín, C. (2020). Pathophysiology of Type 2 Diabetes Mellitus. International journal of molecular sciences, 21(17), 6275. https://doi.org/10.3390/ijms21176275
- Ganesan, K., Rana, M. B. M., & Sultan, S. (2018). Oral hypoglycemic medications.
- Feingold, K. R., Anawalt, B., Boyce, A., Chrousos, G., Dungan, K., Grossman, A, & Kopp, P. (2020). Oral and injectable (non-insulin) pharmacological agents for type 2 diabetes. South Dartmouth (MA).
- E. (2022). Pancreas hormones. https://www.endocrine.org/patient-engagement/endocrine-library/hormones-and-endocrine-function/pancreas-hormones
- Kreider, K. E. (2021). Patient-centered medication selection for type 2 diabetes: A collaborative, patient-centered approach that considers a variety of factors will be most effective. American Nurse Journal, 16(11), 33-37.
- Banday, M. Z., Sameer, A. S., & Nissar, S. (2020). Pathophysiology of diabetes: An overview. Avicenna journal of medicine, 10(4), 174–188. https://doi.org/10.4103/ajm.ajm_53_20
- Draznin, B., Aroda, V. R., Bakris, G., Benson, G., Brown, F. M., Freeman, R., & American Diabetes Association Professional Practice Committee. (2022). 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2022. Diabetes care, 45(Suppl 1), S125-S143.
- World Health Organization. (2023). https://www.who.int/news-room/fact-sheets/detail/diabetes
- Hospice and Palliative Nurse’s Association. (2023, September 14). Hospice and Palliative Credentialing Center. Retrieved from AdvancingExpertCare.org: https://www.advancingexpertcare.
- Connor, S., Fitch, K., Iwaski, K., & Pyenson, B. (2006). Comparing Hospice and Nonhospice Patient Survival Among Patients Who Die Within a Three-Year Window. Journal of Pain and Symptom Management, 238-46.
- Coyle, N., Ferrell, B., & Paice, J. (2023). Oxford Textbooks in Palliative Medicine. In Oxford Textbook of Palliative Nursing. New York: Oxford Academic.
- Encyclopedia Brittanica. (2023, September 14). Retrieved from Merriam-Webster.com: https://www.merriam-webster.com/
- National Hospice and Palliative Care Organization. (2023, September 14). Hospice Care Overview For Professionals. Retrieved from NHPCO.org: https://www.nhpco.org/hospice-care-overview/ References:
- Cho, J., & Trent, A. (2006). Validating a decisional conflict scale. Medical Decision Making, 26(4), 373-380.
- Mullaney, T., et al. (2019). Informed consent: The role of the nurse. Journal of Radiology Nursing, 38(2), 177-183.
- Betancourt, J. R., Green, A. R., & Carillo, J. E. (2002). Cultural competence in health care: Emerging frameworks and practical approaches. The Commonwealth Fund.
- Institute of Medicine. (2000). To err is human: Building a safer health system. National Academies Press.
- American Nurses Association. (2019). Nursing: Scope and standards of practice. American Nurses Association
- National Hospice and Palliative Care Organization. (n.d.). History of Hospice Care. Retrieved from https://www.nhpco.org/about/hospice-care/history-of-hospice-care/
- Hospice UK. (n.d.). The History of Hospice Care. Retrieved from https://www.hospiceuk.org/about-hospice-care/the-history-of-hospice-care
- Philosophy 1. World Health Organization. (202).0 Palliative Care. Retrieved from https://www.who.int/news-room/fact-sheets/detail/palliative-care
- American Academy of Hospice and Palliative Medicine. (n.d.). History of Hospice and Palliative Medicine. Retrieved from https://aahpm.org/about/history-of-hospice-and-palliative-medicine
- Centers for Medicare & Medicaid Services. (n.d.). Medicare Benefit Policy Manual: Chapter 9 – Coverage of Hospice Services Under Hospital Insurance. Retrieved from https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c09.pdf
- Hospice and Palliative Credentialing Center. (n.d.). CHPN – Certified Hospice and Palliative Nurse. Retrieved from https://www.nhpco.org/certification/chn-certified-hospice-nurse/
- National Hospice and Palliative Care Organization. (nice.d Nurse.). Hosp. Retrieved from https://www.nhpco.org/about/hospice-care/hospice-nurse/
- Patient-centered care(Reference: Institute of Medicine. (2014). Dying in America: Improving quality and honoring individual preferences near the end of life. National Academies Press).
- Shared decision making(Reference: Elwyn, G., et al. (2012). Shared decision making: A model for clinical practice. Journal of General Internal Medicine, 27(10), 1361-1367). 4.
- Psychosoc(Reference: Balboni, T. A., et al. (2010). Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Internal Medicine, 170(15), 1109-1117).
- Pain and symptom management (Reference: Ferrell, B. R., et al. (2017). Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. Journal of Clinical Oncology, 35(1), 96-112).
- Institute of Medicine. (2014). Dying in America: Improving quality and honoring individual preferences near the end of life. National Academies Press.
- Breen, C. M., Abernethy, A. P., & Abbott, K. H. (2011). Conflict associated with decisions to limit life-sustaining treatment in intensive care units. Journal of General Internal Medicine, 26(4), 389-394.
- Elwyn, G., et al. (2012). Shared decision making: A model for clinical practice. Journal of General Internal Medicine, 27(10), 1361-1367.
- Balboni, T. A., et al. (2010). Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Internal Medicine, 170(15), 1109-1117.
- Ferrell, B. R., et al. (2017). Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. Journal of Clinical Oncology, 35(1), 96-112.
- San Filippo, D. (2006). Philosophical, Psychological & Spiritual Perspectives on Death & Dying. Faculty Publications. 31. https://digitalcommons.nl.edu/faculty_publications/31
- Kyota, A. & Knda, K. (2019). How to come to terms with facing death: a qualitive study examining the experiences of patients with terminal cancer. https://doi.org/10.1186/s12904-019-0417-6
- Peters, L. et al. (2013). How death anxiety impacts nurses’ caring for patients at the end of life: a review of literature. The open nursing journal, 7, 14–21. https://doi.org/10.2174/1874434601307010014
- Bergenholtz, H. et al. (2020). Talking about death and dying in a hospital setting- a qualitative study of the wishes for end-of-life conversations from the perspective of patients and spouses. https://doi.org/10.1186/s12904-020-00675-1
- Oates J.R. & Maani-Fogelman P.A. (2022). Nursing Grief and Loss. https://www.ncbi.nlm.nih.gov/books/NBK518989/
- Bodi, S., Matus, C., & Hickey, D. (2022). Right place, right time: Facilitating end-of-life conversations. The Journal of family practice, 71(2), 74–79. https://doi.org/10.12788/jfp.0333
- Pentaris, P., & Tripathi, K. (2022). Palliative pProfessionals’ Views on the Importance of Religion, Belief, and Spiritual Identities Toward the End of Life. International journal of environmental research and public health, 19(10), 6031. https://doi.org/10.3390/ijerph19106031
- Lin, H. Y. et el. (2021). Nurses’ knowledge, attitude, and competence regarding palliative and end-of-life care: a path analysis. PeerJ, 9, e11864. https://doi.org/10.7717/peerj.11864
- Becker, C. et al. (2020). Communication challenges in end-of-life decisions. Swiss medical weekly, 150, w20351. https://doi.org/10.4414/smw.2020.20351
- Oates J.R. & Maani C. V. Death and Dying. [Updated 2022 Nov 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK536978/
- Ijaopo, E. O. et al. (2023). A Review of Clinical Signs and Symptoms of Imminent End-of-Life in Individuals With Advanced Illness. Gerontology & geriatric medicine, 9, 23337214231183243. https://doi.org/10.1177/23337214231183243
- Lee, E. K. et el. (2021). End-of-Life Assessments and Communication for Dying Patients and Their Families. Journal of hospice and palliative care, 24(3), 194–197. https://doi.org/10.14475/jhpc.2021.24.3.194
- Onishi H. (2021). Communication at the End of Life. Journal of hospice and palliative care, 24(3), 135–143. https://doi.org/10.14475/jhpc.2021.24.3.135
- Bellani, G. (2022). Mechanical ventilation from pathophysiology to clinical evidence. Springer. https://doi.org/10.1007/978-3-030-93401-9
- Hickey SM, Giwa AO. Mechanical Ventilation. [Updated 2023]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539742/
- Keszler M. (2019). Volume-targeted ventilation: One size does not fit all. Evidence-based recommendations for successful use. Arch. Dis. Child. Fetal Neonatal Ed.; 104: F108–12.
- Shelledy, & Peters, J. I. (2020). Mechanical ventilation (Proud, Ed.). Jones & Bartlett Learning.
- Spinelli, E., Mauri, T., Beitler, J.R. et al. (2020). Respiratory drive in the acute respiratory distress syndrome: pathophysiology, monitoring, and therapeutic interventions. Intensive Care Med 46, 606–618. Available from: https://doi.org/10.1007/s00134-020-05942-6
- Walsh, B. K., & Waugh, J. B. (2020). Alarm Strategies and Surveillance for Mechanical Ventilation. Respiratory Care, 65(6), 820–831. https://doi.org/10.4187/respcare.07546
- Wilcox, Aydin, A., & Marcolini, E. G. (2019). Mechanical ventilation in emergency medicine. Springer. https://doi.org/10.1007/978-3-319-98410-0
- Williams, L. S., & Hopper, P. D. (2019). Understanding medical-surgical nursing. F.A. Davis Company.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
