Course
Kentucky SANE Guidelines for Adult/Adolescent Populations
Course Highlights
- In this SANE Guidelines for Adult/Adolescent Populations course, you will learn to describe the key components of sexual assault care.
- You’ll also learn to explain the process of collecting and handling evidence.
- You’ll leave this course with the ability to describe documentation needs related to sexual assault.
About
Contact Hours Awarded: 2.5
Course By:
Keith Wemple
RN, BSN, CCRN-CMC, SRNA
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
This course is a review for the important Sexual Assault Nurse Examiner (SANE) certification. We will be discussing the defining characteristics of forensic nursing and sexual assault.
We will discuss the multi-disciplinary approach to caring for these patients. Specifics of forensic health assessment, specimen collection, and forensic photography will be described. The all-important documentation requirements will be reviewed. Sexually transmitted diseases and pregnancy implications will also be discussed.
Overview of Forensic Nursing
Forensic nursing is an important field that cares for victims at an incredibly vulnerable time. This leads to a high level of responsibility for Sexual Assault Nurse Examiners (SANE) and many requirements to help protect victims. We will navigate these requirements in as straightforward a way as possible.
Forensic nursing is a multi-disciplinary approach involving not just different medical providers, but also law enforcement and community health. Forensic nurses must understand each professional’s role in caring for sexual assault victims.
In general, it is best to have one trusted person (that would be you SANE nurses) perform most care, especially care that would jeopardize privacy or comfort. Care of these patients requires knowledge and skills very different from standard nursing. You have already proven you have this knowledge and skills; we will simply hone them a little bit.

Self-Quiz
Ask Yourself...
- What techniques have you found useful when caring for sexual assault victims?
- How do you establish trust with your patients?
Sexual Violence Against Adults/Adolescents
In this course, we will be discussing sexual assault and the care of adults and adolescents. The International Association of Forensic Nurses (IAFN) defines adolescence as age 13-18 and adults as 18 and older (14). Sexual assault is non-consensual sexual contact that is often accompanied by physical assault. Sexual assault may be perpetrated by a stranger, or someone known to the victim, including an intimate partner. Forms of physical assault include physical blows, grabbing or restraints, involuntary ingestion of drugs, biting, and strangulation (8).
Prevalence and Statistics
Sexual assault is a serious issue, affecting 18% of women (8) and 3% of men (10) in the United States (4). Internationally, the numbers range from 15-71% for females and 5-10% for males (14). Sexual violence is conducted by an intimate partner 5 times more often than by a stranger (14). Young people (age 18-34) are at the highest risk. Males in this age group attending college are 5x more likely to be victims of sexual assault (10). Native Americans, people with disabilities, transgender individuals, and people identifying as gay, lesbian, or bisexual are more likely to suffer sexual assault (8, 10, 14). Specific to intimate partner violence, the risk is increased with young age, lower socioeconomic status, mental health disorders, substance misuse, history of abuse, and poor community support system (14). Sadly, many victims either present late or later withdraw their allegation of sexual assault because of the shame associated with it. Be aware of these risk factors when assessing patients with injuries concerning sexual assault.
Long-Term Effects
Sexual assault is a crime with long-lasting effects on victims, both mentally and physically. Sexually transmitted diseases (STDs), such as Human Immunodeficiency Virus (HIV) and Herpes Simplex Virus (HSV) are not curable and will last the duration of the victim’s life. Other STDs can have serious health impacts if not recognized and treated appropriately. If pregnancy occurs, this presents long-term psychological and financial problems for the victim on top of the physical consequences.
Mental health is another major concern following sexual assault. 30% of sexually assaulted women had PTSD 9 months after the rape (11) and 33% contemplated suicide (12). These are serious mental health concerns that require treatment. Sexual assault victims are more likely to use drugs after their assault (12). Additionally, 38% of victims even experienced problems at work or school following the assault (13). This highlights how sexual assault affects every aspect of a victim’s life.

Self-Quiz
Ask Yourself...
- What mental health resources do you have available where you work?
- Do you know how to access these resources?
The Sexual Assault Response Team
It may be helpful to institute a Sexual Assault Response Team (SART) to coordinate a response among the different professionals involved. Members of a typical SART include advocates, law enforcement, prosecutors, and of course health care providers.
Advocates are victim support resources, such as the National Sexual Assault Hotline, which provides emotional support, language assistance services, and referrals. Their level of involvement depends on the advocacy group, and whether they have an in-person component or not.
Law enforcement ensures victim safety, collects evidence, interviews the suspect, and prepares the criminal case against the assailant. Law enforcement will likely be involved in most sexual assault cases, especially if the victim is seeking criminal charges against their aggressor.
Healthcare providers include you and the other providers you collaborate with to assess and treat health concerns. Common examples are emergency medical technicians (EMTs) from initial contact and physicians, nurse practitioners, or physician assistants for prescribing treatment.
Prosecutors determine if there is sufficient evidence to charge the suspect with a crime and if so, prosecute the case against them. Prosecutors will typically deal more directly with the victim, but you should be aware of their role in educating the patient.
Whether your workplace uses a formal SART or not, you will interact with most, if not all, of these different professions in your care of a sexual assault victim. It is important to understand and respect the role of each member of the care team. This of course includes your role as the Sexual Assault Nurse Examiner (SANE). As we will discuss, many aspects of caring for sexual assault survivors fall on you. Make use of these other professions but don’t forget how valuable you are!


Self-Quiz
Ask Yourself...
- Does your workplace utilize a Sexual Assault Response Team (SART)?
- Do you think a SART is or would be beneficial at your workplace?
- Have you encountered issues when working with these other professions?
- What are some strategies you use to effectively collaborate with other professionals?
Key Aspects of Sexual Assault Care
It is important to always keep forensic nursing victim-centered. Sexual assault victims presenting for care should be treated as a priority when triaging patients. Ensuring privacy and comfort is crucial to providing care for victims. It is best not to leave sexual assault victims in the common waiting area but to move them to a more private location whenever possible. When assessing the patient be extra vigilant in maintaining privacy by closing doors or curtains and draping the patient when appropriate.
Victims will – rightly so – fear for their safety. It is important to ensure their safety and the safety of staff if the assailant pursues the victim. Collaborate with your facility’s resources and law enforcement to ensure security. Be sure to record the names of any visitors the victim wants to see in case someone comes looking for them at the hospital. Formulate a plan for if the assailant or a stranger comes looking for the patient. Ensure confidentiality so that the patient cannot be easily identified from outside the room in case the aggressor gains access to the care area.
It is vital to get informed consent from the victim before performing any procedure, including specimen collection, forensic photography, sexually transmitted infection (STI) testing, and pregnancy testing. Informed consent should be given both verbally and written in a language the patient understands. Victim support advocates can help arrange translation if needed.

Self-Quiz
Ask Yourself...
- What is your facility’s protocol for handling an invader?
- Have you ever had an experience such as this one? How was it handled?
- What interpreting services are available where you work?
- Do you know how to use these services?
Always maintain confidentiality and assure the victim that assessments are kept confidential. Sexual assault survivors have had their privacy violated in a serious way. To properly care for the patient and build trust it is important to respect their right to confidentiality. Remember, consent and confidentiality are legal requirements. Educating the patient on this may help ease their concerns.
When it comes to involving law enforcement, this should generally be guided by patient preference. In some jurisdictions, there are requirements to report sexual violence, even without patient consent. These usually involve the abuse of vulnerable adults/adolescents by caregivers or authorities. Outside of these exceptions, criminal reporting should be done only with patient consent.
The Rape, Abuse, and Incest National Network (RAINN) is a good resource for finding laws related to sexual assault in each state (15). If criminal reporting is being pursued, contact local law enforcement early in the process. If reporting the assault because it is mandated, be sure to inform the patient of this and what they can expect from law enforcement.

Self-Quiz
Ask Yourself...
- What measures does your facility have to ensure the safety and privacy of sexual assault victims?
- Are these measures effective? Why or why not?
- What are the circumstances where reporting is required where you work?
- Where can you obtain this information?
Health History, Observation, and Assessment
Sexual assault victims have had their privacy and autonomy violated by the assault, so as caregivers we must promote privacy and autonomy as much as possible. Provide privacy during all parts of the exam. It is important to accommodate patients’ requests to have a support person present to promote feelings of security and comfort. Also, accommodate patient requests for caregivers of a specific gender when feasible. Carefully explain and obtain consent for each part of the exam. We do not want victims to feel further violated by the exam, which at times can feel very invasive. Allow the patients as much autonomy and control as possible in the examination process to minimize this. If transfer to another facility is necessary to care for the patient, do so while minimizing time delays and loss of evidence.
Physical Assessment
Remember, health and safety always come first. Assessment should be thorough and methodical. This helps uncover all injuries and potential sources of evidence. Assess for any major trauma and treat any findings before completing history. Any airway compromise, bleeding, and severe pain should be treated urgently. Control bleeding and replace volume loss with IV fluid or blood products as appropriate. Treatment of these physical conditions is no different than for any other patient, other than the emphasis on privacy and obtaining consent.
Strangulation as part of sexual assault can have dire consequences. For strangulation victims assess if the victim lost consciousness, if they were shaken, if they hit their head, if they are having difficulty breathing, and if they are experiencing any neurologic or vision changes (13). These assess for the most serious concerns of airway trauma, traumatic brain injury, cervical spine injury, and stroke. Imaging of the head, neck, and/or brain may be necessary.13

Self-Quiz
Ask Yourself...
- What is your treatment plan if the patient has a compromised airway?
Equipment
There is specific equipment that can help in the proper assessment of a sexual assault victim. A copy of the most current exam protocol for your jurisdiction should be available. A sexual assault evidence collection kit should be available (more to come on this later). A device or method for drying evidence should be available to properly prepare evidence. A camera and related supplies should be on hand for forensic photography. An anoscope or colposcope may be used in cases of anal or genital penetration or trauma for a more thorough assessment and careful evidence collection (8). Finally, standard exam and testing supplies should be readily available.

Self-Quiz
Ask Yourself...
- Does your workplace have an anoscope or colposcope for use in sexual assault cases?
- What equipment is used to dry and process evidence where you work?
Medical Forensic Health History
When it is feasible, the investigative and medical forensic history should be done together. This requires coordination between you and the investigative team. This is part of why it is important to contact law enforcement early in the process. The forensic health history should contain 9 specific elements (8).
- Date and time of the sexual assault: timing can influence evidence collection, testing, and treatment of the patient. Many aspects of evidence collection and testing are time-sensitive, so accurate timing of the assault is important.
- Pertinent medical history, especially those that may affect the assessment or treatment of injuries: this should be limited to history that affects care of the assault injuries. Examples include previous injuries, bleeding disorders or health conditions affecting the area of the assault.
- Any recent consensual sexual activity: this can aid the criminal investigation by eliminating any DNA of consensual partners from evidence.
- What the patient did after the assault: including things such as showering or bathing, urinating, or defecating, brushing teeth, eating, or drinking, changing clothes or similar activities that may affect what evidence is left on the patient.
- Assault-related history: location of injured body parts and any associated pain, bleeding, or trauma.
- Any known information about the suspect: including a physical description, name, or any other identifiable characteristics.
- Nature of the physical assault: such as the location, if the assault included strangling, blows, biting, or restraints, and whether the suspect was injured.
- Any alcohol or drug use: this may affect the memory of the event. If a drug was used a toxicology sample within 120 hours (5 days) is recommended.
- Description of the sexual assault: this should be accurate but brief. Include if the anus, genitals, or mouth were penetrated, any objects used, and whether contraception or lubricants were used.

Self-Quiz
Ask Yourself...
- Does your facility have a form or protocol to ensure all required elements are captured on the medical forensic health history?
- Do you think the current protocol is effective? What would you change or improve?
Toxicology
Routine toxicology is not recommended, however, if alcohol or drugs were a factor in the sexual assault, toxicology should be performed (8). This requires explaining and obtaining consent from the patient. A blood sample should be used if the drug was ingested within 24 hours, or a urine sample may be used if the drug was ingested within 96 hours (4 days) (8). Toxicology can be useful both for treating the patient appropriately and prosecuting the assailant.
Voluntary drug use should not discredit a patient’s claim of sexual assault. Law enforcement should be careful pressing charges of illegal drug use, as it may make the victim less likely to follow through with the investigation of the assault (8). Some jurisdictions even protect sexual assault victims from such charges. If voluntary drug use is reported, the patient should be referred to addiction counseling.

Self-Quiz
Ask Yourself...
- What resources for addiction treatment are available in your area?
Special Populations
When caring for a patient with a disability respect their wishes to have or not have a personal caregiver present. Provide culturally sensitive care when treating victims of another culture. Cultural norms can affect a victim’s view of sexual assault and the type of care they want to receive. When feasible, accommodate patient requests for caregivers of a specific gender. It is also important to be sure to communicate clearly in a language the patient understands.
Adolescent patients may present with a parent. Performing some assessments without the presence of the parent may be necessary to obtain information, especially if the parent was involved in the abuse; use your clinical judgment here. Be sure to familiarize yourself with laws around adolescents’ ability to consent in your state. Again, RAINN is a good resource for local laws.
When caring for a transgender individual, treat their physical condition based on the sex organs present and treat their total person in a way appropriate for their identity. Respect the patient’s preference regarding their own name and pronouns while treating them. If the patient has female sex organs that were involved in the sexual assault inform them of the risk of pregnancy for transgender males, even when taking hormone therapy.
Make use of victim support services. Victim support services can help with translation for patients not proficient in English. Support services can also help arrange shelter and legal representation for victims. Contact support services early in the process, as some services may accompany the patient through the examination process if the patient so wishes.

Self-Quiz
Ask Yourself...
- What different cultural groups are there in your community?
- Do you understand these groups’ beliefs on sexuality?
- What techniques have you/could you use to separate an adolescent from their parent?
- How comfortable are you with the appropriate care of transgender patients?
- Do you have any personal beliefs or biases that would impact the care you provide?
- What support services are available in your community?
- What types of services do they offer?
Mental Health Assessment
Mental health assessment is another important part of the exam. Individuals react to major stressors differently, so it is important to not make judgments on an individual’s mental state based on their behavior. Always ask patients about their mental state to get a proper assessment.
A suicide risk assessment using a validated tool, such as the Suicidal Behaviors Questionnaire-Revised (SBQ-R), can help with diagnosing major mental health concerns.7 The SBQ-R includes four questions that assess a person’s risk for suicide. It is important to be empathetic but ask direct questions when assessing suicidality. Direct questioning helps elicit honest answers about suicidal thoughts.

Self-Quiz
Ask Yourself...
- Does your facility have a standardized mental health assessment you could use?
- Is there another designated professional responsible for completing the mental health assessment where you work? Do you know how to contact them?
Specimen Collection
Specimen collection kits must contain a container, an instruction sheet or checklist, forms for consent and evidence collection, and collection materials. These collection materials include material for collecting clothing/foreign materials for evidence, vaginal/cervical swabs, penile swabs, perianal swabs, oral swabs, and body swabs.
Assess patients for the presence of evidence with initial assessment. Take measures to prevent loss of evidence and collect it early in the process whenever possible. When collecting samples, always wear proper personal protective equipment (PPE) to protect yourself and use non-powdered gloves to prevent contamination of the sample.8 Store dry evidence in paper containers, and dry wet evidence in a drying box if available. Minimize the amount of time between the collection of evidence and the storage of the collection kit to best preserve evidence. Specimens should only be transported away from the site by law enforcement.

Self-Quiz
Ask Yourself...
- What is included in the specimen collection kit you use? Does it meet all the IAFN requirements?
- Does your jurisdiction have a policy in place for the storage of evidence when victims are undecided about reporting?
DNA Analysis
Most modern systems utilize DNA analysis. When collecting evidence for DNA analysis it is important to also collect a sample of the patient’s DNA to distinguish between victim and aggressor. A DNA sample of any recent consensual sexual partners should also be collected to narrow down DNA evidence to the suspect. This is usually done with a blood sample or a simple buccal swab inside the person’s mouth.8 Patient DNA samples should be used for comparison purposes only, not given to law enforcement for any other purposes.
DNA samples are processed in a forensic laboratory by separating the DNA from the specimen and then using polymerase chain reaction (PCR) to replicate the DNA. Different DNA strands can then be identified and separated for interpretation.5
Clothing Evidence
Evidence can exist on clothing that may have been washed off the body. To properly collect evidence from clothing place a clean hospital sheet on the floor, and then collection paper on top of the sheet. Have the patient disrobe over the collection paper to catch any falling potential evidence. Be thoughtful in how much clothing to collect as evidence, and only collect clothing with the patient’s consent. If the patient needs replacement clothes, advocate groups may be able to provide clothes to the patient.
Swab Collection
Use swabs to collect blood or other body fluid samples from the patient’s body, hair, and anogenital area. If fluids are dried, first moisten them with a wet swab and then collect them as a wet sample (8). This can be done using 2 wet swabs, or a wet swab followed by a dry swab (5). Properly collected DNA samples can be used to identify suspects even from touch contact (5). Vaginal or cervical swabs are often wet-mounted to detect sperm (8). Label all samples properly and store them appropriately after drying. If the sample cannot be dried in the facility, store it according to jurisdictional policy. This probably sounds like a lot of policies to remember – that’s why having the policies included in the collection kit is so important!

Self-Quiz
Ask Yourself...
- What is the process for collecting and processing DNA samples at your workplace?
- What is the technique for drying samples where you practice?
- How are wet specimens collected and stored?
Medical Forensic Photography
Forensic photography is often included in the assessment and treatment of sexual assault. Some locations include photography as a standard, while others include it only when indicated. In either case, always be sure to explain the photograph procedure and get consent before taking any photographs.
Photography Technique
Photographs should include injured areas only. Be sure that photographs are in focus and include all borders of the wound. It is recommended that photographs include 3 different orientations with 2 shots at each orientation.
One shot should include a forensic measurement device by the wound for clear documentation of size, and the other without the measurement device to prove no features are covered by the measurement tool.
First take 2 full-scale shots, which show the injured area in context to the entire body. Next, take 2 medium-scale shots that show the affected body part. Finally, take 2 close-up shots of the injury to give clear details.
These photographs should be taken only by you, the examiner. Patients feel very vulnerable during this process, so it is important that photographs are taken by someone they trust, and that privacy and dignity are maintained throughout the process.
Once taken, photographs must be clearly labeled and follow the chain of custody if being used as evidence for criminal prosecution. Photographs are considered part of the patient’s medical forensic record and are not automatically turned over to law enforcement. Law enforcement must subpoena photographs that are required for their investigation.
Photography Equipment
SANE nurses should be familiar with the equipment used for forensic photography. You should be able to adjust the shutter speed and lens aperture to control the exposure of the photographs. A quality macro lens with ring strobe flash produces the best forensic photographs (8). Include a color bar in photographs to account for any distortion of color. If you are unsure of how to use certain features of your equipment, refer to the manufacturer’s instructions and owner’s manual.

Self-Quiz
Ask Yourself...
- Under what circumstances are you supposed to take photographs where you work?
- How is the confidentiality of photographs maintained at your workplace?
- How comfortable are you using the photographic equipment at your facility?
STD Testing and Prophylaxis
Sexually transmitted disease (STD) testing and prophylaxis is an important part of the sexual assault treatment process. If victims present within 72 hours of the assault, HIV and STD testing should be conducted. The CDC recommends baseline testing for HIV, Hepatitis B, Hepatitis C, syphilis, gonorrhea, and chlamydia (4). The most common STDs in sexual assault victims are trichomoniasis, gonorrhea, and chlamydia (8).
Symptoms (16)
Symptoms of chlamydia include painful urination, lower abdominal pain, vaginal or penile discharge, and pain or bleeding with intercourse.
Symptoms of gonorrhea include thick, cloudy, or bloody discharge, painful urination or bowel movements, painful testicles in males, and vaginal bleeding in females.
Symptoms of trichomoniasis include greenish or yellowish vaginal discharge, penile discharge, genital burning or itching, strong vaginal odor, and painful urination.
Early signs of HIV include fever, headache, sore throat, swollen lymph nodes, and rash.
Symptoms of herpes simplex virus include small red bumps or sores in the genital and anal area accompanied by pain or itching.
Symptoms of hepatitis include abdominal pain, nausea, vomiting, fever, dark urine, muscle pain, and jaundice.
Symptoms of syphilis include a reddish-brown rash with penny-sized sores, fever, enlarged lymph nodes, and aches.
Testing
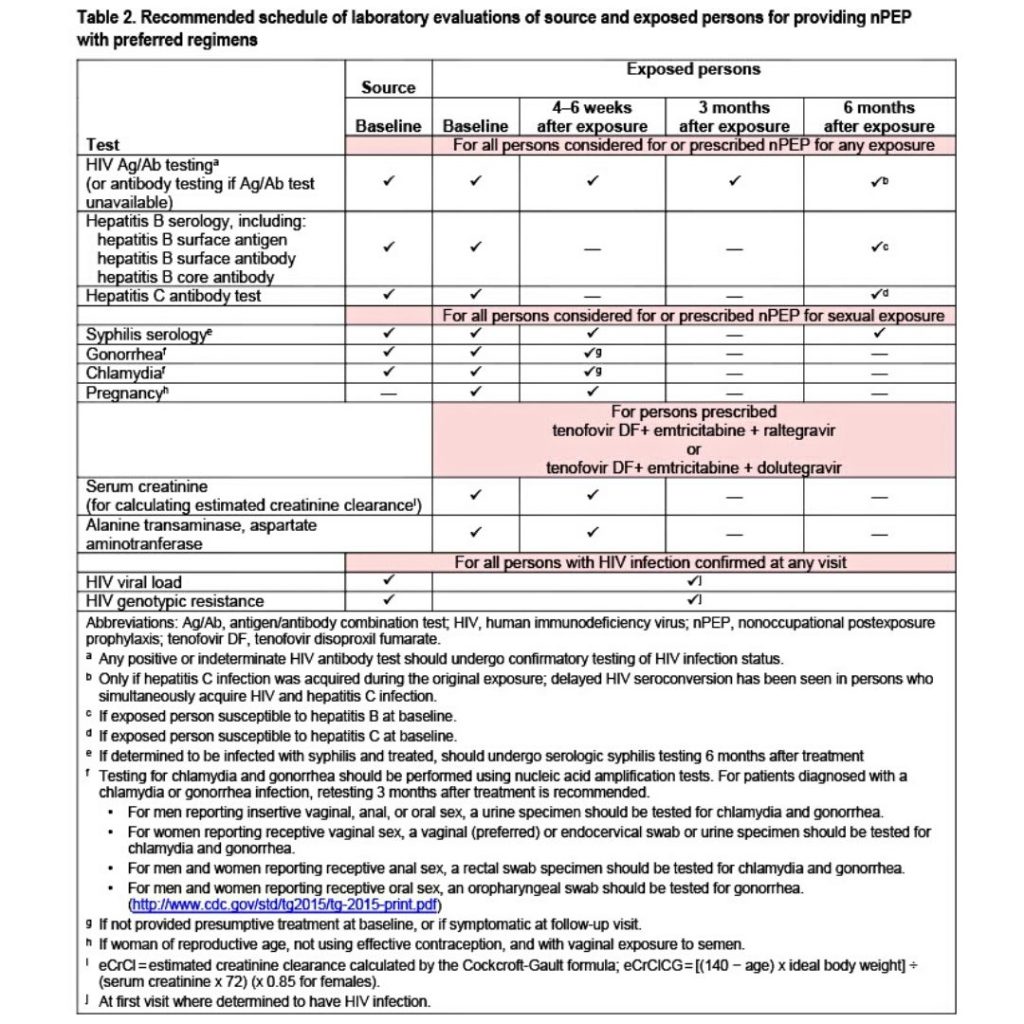
For HIV, testing should be repeated at 4-6 weeks and 3 months. Victims not vaccinated against hepatitis B should be vaccinated. The first dose should be given on exam, the second dose at 1-2 months, and the third dose at 4-6 months. Follow-up syphilis testing at 4-6 weeks is recommended. People with a high risk for developing hepatitis (because of immunosuppression or known exposure) should be retested at 6 months.
The following table from the Centers for Disease Control (CDC) summarizes testing requirements (4):
Treatment
Suspected or confirmed HIV-positive patients should be treated with a 28-day course of triple antiretroviral therapy. Preferred antiretroviral therapy is tenofovir disoproxil fumarate (TDF) 300mg daily, emtricitabine 200mg daily, and raltegravir 400mg BID or dolutegravir (DTG) 50mg daily (4).
Patients receiving triple antiretroviral therapy should have serum creatinine, alanine transaminase (ALT) and aspartate aminotransferase (AST) checked at baseline and end of therapy.
Prophylactic treatment is recommended against gonorrhea and chlamydia for all victims, with the addition of trichomonas for female victims. Treatment for gonorrhea is a single dose of ceftriaxone 250mg IM and a single dose of azithromycin 1g PO. Chlamydia treatment is 1g PO azithromycin (note this is the same as for gonorrhea – 2 diseases, 1 pill!) or doxycycline 100mg PO twice a day for 7 days. Trichomonas treatment is a single dose of metronidazole or tinidazole 2g PO.
To cover all diseases that would be: 1g azithromycin PO once, 2g metronidazole or tinidazole PO once, 250mg ceftriaxone IM once, and a 28-day course of triple antiretroviral therapy.
Common side effects of these medications to educate patients on are nausea, vomiting, diarrhea and fatigue (standard stuff). More serious side effects to be aware of are kidney stones, hepatitis, and hepatotoxicity. Except for a few antiretroviral drugs these are safe to give in pregnancy. (4)

Self-Quiz
Ask Yourself...
- What symptoms are unique to each sexually transmitted disease?
- There are many antiretroviral drugs for HIV; does the antiretroviral therapy prescribed at your workplace match the CDC recommendations?
- Does your facility have patient education materials available for sexually transmitted diseases?
Pregnancy Risk Evaluation and Care
The overall risk of pregnancy from a sexual assault is similar to a consensual sexual encounter at 2-5%. (4). The risk is of course higher if no prophylactic was used. With patient consent, all patients with child-bearing capacity should be tested for pregnancy. This includes transgender males who have not had a hysterectomy, even if they are on hormone therapy.4
In the facility, a blood beta-HCG test can be used which is highly sensitive. Typical urine pregnancy tests can also be used and will detect pregnancy at 8-9 days post-conception (4).
If a pregnancy test is positive, then emergency contraception is contraindicated. For patients with a negative pregnancy test, emergency contraception should be offered to the patient.
Levonorgestrel is the recommended emergency contraceptive (8). Levonorgestrel is most effective if used within 120 hours (5 days) (8). Dosing consists of either two doses of 0.75mg PO 12 hours apart or a single dose of 1.5mg PO (8). Patients always have the option of deferring care and testing until they have follow-up with their provider. The patient should also be offered anti-nausea medications (8).


Self-Quiz
Ask Yourself...
- Does your facility provide emergency contraceptive care? If not, where can sexual assault victims receive this type of care in your area?
Documentation
Documentation of an evidence collection kit report is required. This report should contain only medical issues relating to the assault. Patient consent forms, forensic photography, and history of assault should also be included. A diagram depicting the location of injuries on the patient should also be included in the forensic medical record.
As discussed in the assessment section, required documentation on the medical forensic history includes date and time of the assault, pertinent medical history, recent consensual sexual activity, post-assault activities, assault-related history, suspect information, nature of the assault, alcohol or drug involvement, and description of the assault. The Department of Justice recommends a review process of documentation to ensure accurate, objective data is reported (8).
A medical forensic report should be kept separate from the patient’s primary medical record. This ensures privacy and confidentiality. Information in this report should be related to the assault only and be limited to objective information. Documentation is required each time a collection kit is transferred from one person to the next, including transferring to another healthcare facility or transferring over to law enforcement.

Self-Quiz
Ask Yourself...
- Does your facility have a documentation review process?
- Does your facility have a documentation review process?
- What is your workplace’s policy for developing a separate medical forensic report?
Discharge and Follow-Up
It is important to provide thorough patient education at discharge. Education should be both written and oral and include medical concerns, advocacy, and counseling services available and the investigative process.
Factors that affect patient compliance with recommended treatment include education level, employment status, and lack of health insurance – with lack of health insurance being the biggest factor (3). If the patient does not have health insurance, collaborating with social workers for resources may help improve compliance.
The Violence Against Women Act (VAWA) and STOP Violence Against Women Formula Grant Program will cover payment for the medical forensic exam, but not other forms of treatment provided during the visit (8).
Collaborate with community resources and law enforcement to give clear education on these areas and obtain patient resources. Any follow-up for STD testing or other health concerns should be arranged prior to discharge. Ensure that all medical and mental health needs of the patient are addressed prior to discharge.
It is also important to address patient safety concerns prior to discharge. Many cases of sexual assault involve someone the victims know. Collaborate with law enforcement and community resources to find a safe place for the patient to be discharged to.

Self-Quiz
Ask Yourself...
- What community resources are available where you live to shelter sexual assault survivors?
- What is one piece of information you can take back to your practice as a SANE nurse?
Conclusion
In conclusion, we have discussed the key aspects and statistics of sexual assault. The impact this crime has on victims was described. More importantly, how we can assess and treat these patients was outlined. Techniques for maintaining patient dignity and privacy during the examination process were presented. The specifics of specimen collection and forensic photography were reviewed.
Hopefully, there are some take-home points from all this information you can carry with you in your care of this vulnerable population. Remember to collaborate with the other members of the sexual assault response team to provide the best care for the patient. Continue treating these patients with care and dignity and thank you for the work you do!
References + Disclaimer
- Mackler CD, Williams JR, Sharpe L. Gender-Affirming Sexual Assault Nurse Examiner Care: A Program Evaluation and Quality Improvement Project at a Community-Based Rape Crisis Center. J. forensic nurse. 2023;19(2):81-87. doi:10.1097/JFN.0000000000000422, 10.1097/JFN.0000000000000422
- Tao G, Li J, Johns M, Patel CG, Workowski K. Sexually Transmitted Infection/Human Immunodeficiency Virus, Pregnancy, and Mental Health-Related Services Provided During Visits with Sexual Assault and Abuse Diagnosis for US Medicaid Beneficiaries, 2019. Sex Transm Dis. 2023;50(7):425-431. doi:10.1097/OLQ.0000000000001806, 10.1097/OLQ.0000000000001806
- Scannell MJ, Rodgers RF, Molnar BE, Guthrie BJ. Factors Impacting HIV Postexposure Prophylaxis Among Sexually Assaulted Patients Presenting to Two Urban Emergency Departments. J. forensic nurse. 2022;18(4):204-213. doi:10.1097/JFN.0000000000000399, 10.1097/JFN.0000000000000399
- Dominguez, Kenneth L. et al. (2016). Updated guidelines for antiretroviral postexposure prophylaxis after sexual, injection drug use, or other nonoccupational exposure to HIV—United States, 2016.
- Valentine JL, Presler-Jur P, Mills H, Miles S. Evidence Collection and Analysis for Touch Deoxyribonucleic Acid in Groping and Sexual Assault Cases. J. forensic nurse. 2021;17(2):67-75. doi:10.1097/JFN.0000000000000324, 10.1097/JFN.0000000000000324
- Campbell R, Javorka M, Gregory K, Vollinger L, Ma W. The Right to Say No: Why Adult Sexual Assault Patients Decline Medical Forensic Exams and Sexual Assault Kit Evidence Collection. J. forensic nurse. 2021;17(1):3-13. doi:10.1097/JFN.0000000000000315, 10.1097/JFN.0000000000000315
- Cochran CB. An Evidence-Based Approach to Suicide Risk Assessment After Sexual Assault. J. forensic nurse. 2019;15(2):84-92. doi:10.1097/JFN.0000000000000241, 10.1097/JFN.0000000000000241
- US Department of Justice. A National Protocol for Sexual Assault Medical Forensic Examinations: Adults/Adolescents. Office on Violence Against Women. April 2013. https://www.safeta.org/wp-content/uploads/2021/12/SAFE_PROTOCOL_2012-508.pdf.
- US Department of Justice. A National Protocol for Sexual Assault Medical Forensic Examinations: Pediatric. Office on Violence Against Women. April 2016. https://www.safeta.org/wp-content/uploads/2021/12/national_pediatric_protocol_.pdf
- S. Riggs, T. Murdock, W. Walsh, A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress 455-475 (1992).
- DG Kilpatrick, CN Edumuds, AK Seymour. Rape in America: A Report to the Nation. Arlington, VA: National Victim Center and Medical University of South Carolina (1992).
- Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Socio-emotional Impact of Violent Crime (2014).
- International Association of Forensic Nurses. Non-Fatal Strangulation.; 2016. https://www.forensicnurses.org/wp-content/uploads/2022/01/strangulation_documentation_.pdf
- SANE Education Guidelines. forensicnurses.org. 2022. Accessed August 27, 2023. https://www.forensicnurses.org/wp-content/uploads/2022/03/SANE_EdGuidelines_2022_Updated_Resources_-2.pdf.
- Rape, Abuse, and Incest National Network. State law database. RAINN. Accessed September 8, 2023. https://apps.rainn.org/policy/?&_ga=2.211523605.165239645.1694194661-630795265.1692190289#report-generator.
- Mayo Clinic. Common STD symptoms. Mayo Clinic. May 5, 2022. Accessed September 8, 2023. https://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/in-depth/std-symptoms/art-20047081.
- https://www.safeta.org/page/protocoldocuments/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
