TBI Treatment and Management in Nursing Care
Contact Hours: 1.5
Author(s):
Carlana Coogle DNP, RN, CEN
Course Highlights
- In this course, we will learn about TBI treatment and why it is important for trauma nurses to assess their patients’ symptoms accurately.
- You’ll also learn the basics of subdural hematomas (SDH).
- You’ll leave this course with a broader understanding of effectively practicing TBI treatments.
Introduction
Assessments are the foundation to ensure no injury or abnormality is overlooked. Trauma centers across the country utilize a systematic method to ensure this is done. The following case study will review the elements used in the Trauma Nurse Core Course (TNCC) to ensure no injuries are overlooked for this patient.
The Centers for Disease Control and Prevention (CDC) report that more than 32,000 people are killed in MVCs and 2 million are injured each year from an MVC (4). Identification and thorough assessments can lead to successful TBI treatment plans, and it is of the utmost importance for trauma nurses to remain up to date on the current best practices. TBIs are commonly seen in patients after an MVC. The following case study will walk you through the assessment, physician orders, diagnostics, TBI treatment, and outcome for an MVC patient.

Case Study and Trauma Nurse Assessment for Potential TBI Treatment
A 46-year-old man presents to the emergency department (ED) after an MVC. He was a restrained passenger, with airbag deployment, and no reported loss of consciousness. The accident occurred when another car failed to stop at a traffic light and hit the victim‘s car on the passenger side. EMS reports heavy damage and difficult extraction. The victim is complaining of a headache, nausea, and right shoulder pain. Below is your complete trauma nurse assessment:
| Assessment | Findings | |
| A | Airway & Alertness (cervical spine stabilization, if required) |
|
| B | Breathing status, rapid assessment |
|
| C | Circulation status, rapid assessment |
|
| D | Disability = Neuro Status, Glasgow Coma Scale (GCS) |
|
| E | Expose the patient, and rewarm |
|
| F | Full set of vital signs & family presence
|
|
| G | Get adjuncts: labs, ECG monitor, Naso-Orogastric tube, oxygen, pain assessment & treatment
|
|
| H | History & head–to-toe exam
|
|
| I | Inspect posterior
|
|
CDC TBI Fast Facts
All of the following are from a 2014 CDC report:
- About 2.87 million TBI-related emergency department (ED) visits, hospitalizations, and deaths occurred in the United States, including over 837,000 of these health events among children.
- TBI contributed to the deaths of 56,800 people, including 2,529 deaths among children.
- TBI was diagnosed in approximately 288,000 hospitalizations, including over 23,000 among children, consisting of either TBI alone or TBI with another injury.
- An average of 155 people in the United States die each day from injuries that include a TBI (4).
Ask yourself...
- Which of these abnormal assessment findings are a priority?
- What assessments will you be monitoring and reassessing on at least an hourly basis?
- What additional diagnostic testing do you think this patient needs?
- What are you most concerned about with this patient?
- What other interventions are you going to implement for this patient?
- What medications do you anticipate giving to this patient?
- What other hospital resources would you want to utilize for this patient?
- What information is the priority to ask the patient’s wife when she arrives?
- What is this patient most at risk for?
- Which of the fast facts was the biggest surprise to you?
- How familiar are you with TBI assessment and TBI treatment?
Case Study (cont.)
Time elapsed since arrival: 3 hours
- Labs: CBC, CMP
- Chest x-ray, C-Spine, R Shoulder
- CT-head
- Wound care per protocol
- Tdap 0.5ml IM NOW
- EKG
- Zofran 4mg IVP NOW
Nursing Assessment:
- Patient is alert to name
- Stated he was at another local ED,
- Stated the wrong year
- Vital signs:
- Temp 97.7
- Heart rate 108
- Resp 16
- BP 148/82
- SPO2 95%
- Complaining of pain in the right shoulder (6/10)
- Headache (9/10)
- C/o nausea and feeling dizzy.
- GCS=14
- Also noted was that L hand grasp had declined from 5/5 to 3/5, and R/L lower extremities were 4/5.
The following labs/radiology results are back:
- CBC- results WNL expect for WBC 14,000/mL and platelets 135,000/mL
- CMP- WNL
- PT/PTT- WNL
- CT Head Report- An abnormal hyperdense area of blood was noted along the R cerebral convexity, crescent-shaped from the fronto-temporal to the parietal area. These are positive findings for a subdural hematoma.
- C-Spine- All cervical spine bodies and intervertebral spaces are in correct alignment, with no noted cervical spine abnormalities.
- R shoulder- inferior subluxation of R humeral head
Ask yourself...
- Which assessment findings will you immediately notify the provider of?
- What are some ways to decrease stimulation for this patient? Hint: A flip of a switch can help!
- The ED nurse always assesses and plans where this patient will most likely go. What should you do to prepare him?
- Why does this patient need a Tdap vaccine?
- Why do we want to avoid having the patient throw up?
- What additional assessments do you want for this patient?
- How would you define the patient’s status? Improving? Declining? Why?
- Name 2 additional interventions that you can do to help reduce the patient’s stimulus?
- What protocols and screen tools do you have in the facility to assess for increased intracranial pressure?
- What additional texts do you anticipate this patient needing?
Subdural Hematoma
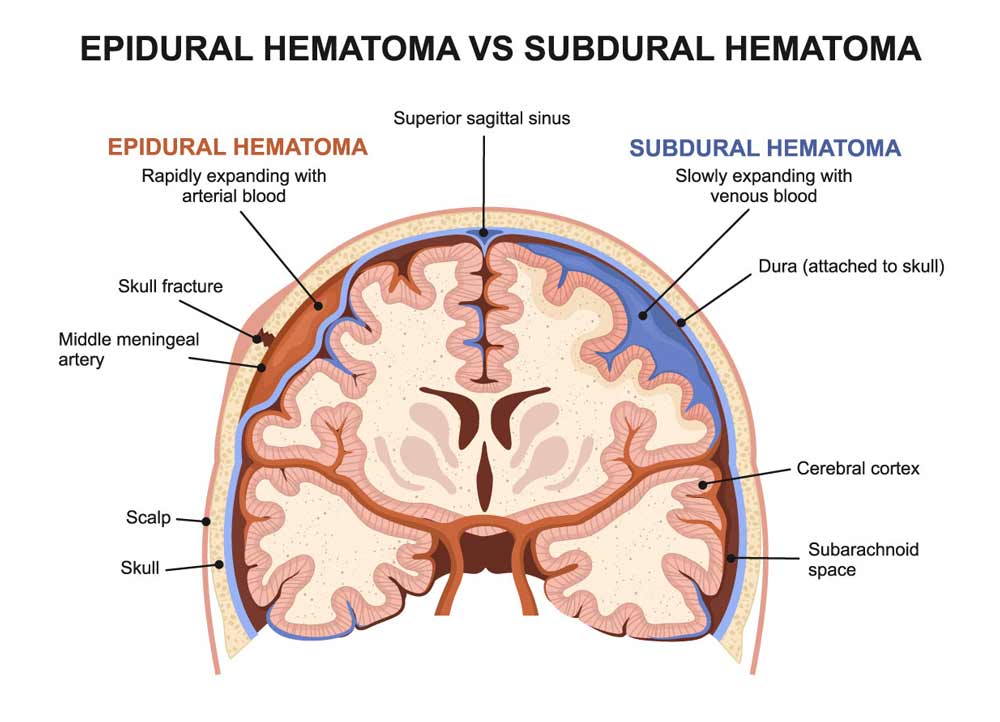
A subdural hematoma (SDH) forms when there is a venous hemorrhage into the space between the dura and the arachnoid membranes. The brain has three layers or coverings (called meninges) between the bony skull and the brain tissue. The layers from the skull to the brain are the dura mater, arachnoid mater, and pia mater. The purpose of the meninges is to cover and protect the brain.
The blood from an SDH is usually the result of damage to the cerebral veins as they empty into the dural venous sinuses (1). The bleeding from an SDH is under the skull and outside the brain, not in the brain itself. As the bleeding continues, it increases pressure on the brain, which usually causes symptoms. As the pressure in the skull rises to a high level, a subdural hematoma can lead to unconsciousness and death (1,2,3).
Causes
A subdural hematoma is usually caused by a head injury, such as a fall, MVC, or an assault. The sudden blow to the head tears blood vessels that run along the surface of the brain. This is referred to as an acute SDH and occurs in up to 25% of people who have experienced a head injury.
Types
- Acute: Most dangerous. The symptoms are usually severe and appear right after a head injury, often within minutes to hours. As blood develops, the pressure on the brain increases, and if not identified and treated quickly, a person can lose consciousness, become paralyzed, or death can occur.
- Subacute: The symptoms can appear from many hours to even weeks after the head injury
- Chronic: This is most common in older people; the bleeding is slow, and symptoms are often vague. It could be caused by even a minor head injury, which the person often does not remember (1,2).
Symptoms
Symptoms are mostly based on the rate of bleeding (1):
- Headache– that doesn‘t go away
- Confusion or drowsiness
- Change in behavior
- Dizziness, loss of balance
- Nausea and vomiting
- Lethargy or excessive drowsiness
- Weakness
- Apathy
If not identified and bleeding progresses, symptoms like seizures, paralysis, breathing issues, LOC, or coma can occur.
Other things that influence SDH are age, other medical conditions, and medications that influence clotting.
Differentiating SDH from Epidural Hematomas
An epidural hematoma is an abnormal collection of blood above the dura mater, so it is located between the skull and the dura mater. The middle meningeal artery is the main artery nourishing the skull and usually the causative agent in an epidural bleed; as with all arteries, it is a high-pressure system, not low like the subdural bleed and venous system.
Epidural hematomas are mainly caused by blunt trauma, especially to the temporal region, which is a thinner area. Patients with falls or skull fractures must always be assessed for TBI, and one should question any change in mental status as significant. Epidural bleeds to carry some common signs and symptoms, which include:
- Age, usually < 45
- A fall or blunt trauma has occurred with a brief loss of consciousness, followed by a period of the patient feeling normal, then getting drowsy 2-3 hours later (1,2).
- Nausea with vomiting and a headache (1,2).
- Head CT shows a convex or lens-shaped area where the bleed is located.
- TBI treatment is like the SDH; the size and symptoms are key drivers; the pressure must be relieved from the brain to ensure the patient does not have permanent damage.

Ask yourself...
- In your own words, describe a subdural hematoma.
- What is the difference between a subdural hematoma and an epidural hematoma?
- In this case scenario, what was the cause of this patient’s SDH?
- Based on the last assessment of this patient, can you identify any other symptoms of a possible SDH?
- When you care for your next trauma patient, which assessment findings will you monitor more closely?
- Have you cared for a patient with a subdural hematoma? Did their presentation resemble that of this patient? How were they different?
- What symptoms would indicate that the patient is declining and needs further interventions?
- What neurological assessments do you feel most indicate a patient’s condition?
- What education would you provide to the wife about her husband’s condition?
- What additional services would be beneficial to add to this patient’s treatment team?
Diagnosing and Treating SDH
A computed tomography (CT) scan or magnetic resonance imaging (MRI) is the two diagnostic interventions usually ordered to outline any potential TBI treatment (3).
Treatment of SDH depends on the patient’s severity and can range from watchful waiting to brain surgery.
If a patient has a small SDH with mild symptoms, the provider may recommend close observation and a repeated CT of the head to assess for changes.
More severe SDHs require surgery to reduce the pressure on the brain. In general, the surgeons will use one of these three techniques to treat SDHs (1):
- Burr hole trephination
- Craniotomy
- Craniectomy

Case Study (cont.)
Time elapsed since arrival: 4.5 hours
Nursing Assessment:
- Patient is alert to name and wife
- Unable to state the year or place
- Vital signs:
- emp: 97.7
- Heart rate: 118
- Resp: 14
- BP: 158/88
- SPO2 95%
- Complaining of R shoulder pain (5/10)
- Headache (10/10)
- Nausea continues.
- GCS=14
- No change in motor function from prior.
- Pt is acting very sleepy and is having a hard time focusing on questions.
Physician Update:
- A neurologist consult was obtained, and the patient is being prepped for the OR.
- Surgical Checklist completed.
Time elapsed since arrival: 24 hours
The patient is now in the Surgical ICU and is expected to go home tomorrow; the surgeon was able to evacuate the SDH using the Burr hole method.
- His mental status is now at baseline, and the patient only has a mild headache (2/10).
- Vital signs are all WNL.
- The laceration was cleansed, and derma bond was used to close.
- The R shoulder subluxation was positioned in the correct alignment, and a repeat X-ray was taken to ensure alignment. Then, a shoulder immobilizer was placed on the patient; it should heal within 4-6 weeks of limited movement.
Ask yourself...
- Have you ever provided care to a patient who had a burr hole, caniotomy, or cainectomy? What was your experience?
- Why is repeat diagnostic testing often needed with brain injuries?
- What additional teaching do you want to provide to the patient’s wife about their recovery?
- What follow-up would be needed for this patient after discharge?
- What documentation would you include for this patient?
- Upon discharge, should this patient have any long-term effects? Why or why not?
- Would you have done anything different with this patient? If so, what?
Conclusion
A systematic and detailed nursing assessment is critical in identifying any and all changes with patients; as you have learned many times, there are similarities with TBI. To provide your patients the best TBI treatment plans, asking the right questions and completing systematic neurological assessments is important. Proper TBI treatment can make all the difference in your patient’s recovery.
References + Disclaimer
- McBride, W. (2020). Subdural hematoma in adults: etiology, clinical features, and diagnosis. UpToDate. Retrieved 3/6/21, from https://www.uptodate.com/contents/subdural-hematoma-in-adults-etiology-clinical-features-and-diagnosis?search=subdural%20hematoma&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- Wang, S., Ma, Y., Zhao, X., Yang, C., Gu, J., Weng, W., Hui, J., Mao, Q., Gao, G., & Feng, J. (2019). Risk factors of hospital mortality in chronic subdural hematoma: A retrospective analysis of 1117 patients, a single institute experience. Journal of Clinical Neuroscience : Official Journal of the Neurosurgical Society of Australasia, 67, 46–51. https://doi.org/10.1016/j.jocn.2019.06.026
- Carroll, J. J., Lavine, S. D., & Meyers, P. M. (2017). Imaging of Subdural Hematomas. Neurosurgery Clinics of North America, 28(2), 179–203. https://doi.org/10.1016/j.nec.2016.11.001
- Centers for Disease Control and Prevention (2019). Surveillance Report of Traumatic Brain Injury-related Emergency Department Visits, Hospitalizations, and Deaths—United States, 2014. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. https://www.cdc.gov/vitalsigns/motor-vehicle-safety/index.html
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
