Course
Texas Renewal Bundle
Course Highlights
- In this Texas Renewal Bundle course you will learn about Texas nursing jurisprudence and ethics.
- You’ll also learn the basics of sexual assault as a public health problem and its impact on the state of Texas.
- You’ll leave this course with a broader understanding of how to define, exemplify, and recognize various types of human trafficking, its victims, and its offenders.
About
Contact Hours Awarded: 20
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Texas Nursing Jurisprudence and Ethics
Texas Nursing Jurisprudence and Ethics
Introduction - Texas Nursing Jurisprudence and Ethics
The purpose of this course is to review nursing ethics and jurisprudence specifically as these relate to Texas state nursing practice and law (1). Each state nursing board works to promote the safety and welfare of clients in their state by ensuring nurses are competent to practice nursing safely.
As outlined by the Texas Board of Nursing continuing education requirements, Nursing Jurisprudence and Nursing Ethics Board Rule 216.3, all nurses, including APRNs, must complete the required two contact hours of CNE relating to nursing jurisprudence and ethics before the end of every third two-year licensing period. This requirement applies to licensing periods that began on or after January 1, 2014. All new nurses must also pass the Nursing Jurisprudence Exam (NJE) (2,3).
Requirements also outline that education includes information related to the Texas Nursing Practice Act, the Board's rules, including Standards of Nursing Practice, the Board's position statements, principles of nursing ethics, and professional boundaries. Nurses are named in negligence and malpractice lawsuits that may claim unethical behavior/conduct, practice outside the scope of licensure, or lack of nursing supervision. Nurses must understand their state nurse practice act, scope of practice of nurse licensure, standards of practice, ethics, and professional boundaries to avoid litigation (2).

Self Quiz
Ask yourself...
- What is the number of contact hours required by the Board of Nursing in Texas Nursing Jurisprudence and Ethics before the end of every third two-year licensing period?
- What are the categories of required course information that must be contained?
- What training have you had regarding Texas jurisprudence and ethics?
- How do you feel that ethics have changed throughout your years of practice?
- Where can you find Texas' nurse practice act?
The Texas Nursing Practice Act – Overview
Registered Nurse Scope of Practice
The Texas Nursing Practice Act (NPA) defines the legal scope of practice for professional registered nurses (RNs) (4). "Professional nursing" means performing an act that requires substantial specialized judgment and skill, the proper performance of which is based on knowledge and application of the principles of biological, physical, and social science as acquired by a completed course in an approved school of professional nursing. The term does not include acts of medical diagnosis or the prescription of therapeutic or corrective measures. Professional nursing involves: (4)
- the observation, assessment, intervention, evaluation, rehabilitation, care, and Counsel, or health teachings of a person who is ill, injured, infirm, or experiencing a change in normal health processes.
- The maintenance of health or prevention of illness.
- A physician, podiatrist, or dentist orders medication administration or treatment.
- The supervision or teaching of nursing.
- The administration, supervision, and evaluation of nursing practices, policies, and procedures.
- The requesting, receiving, signing for, and distributing prescription drug samples to patients at practices where an advanced practice registered nurse is authorized to sign prescription drug orders as provided by Subchapter B, Chapter 157.
- The performance of an act delegated by a physician under Section 157.0512, 157.054, 157.058, or 157.059.
- The development of the nursing care plan.
The RN accepts responsibility for practicing within the legal scope of practice, is prepared to work in all healthcare settings, and may engage in independent nursing practice without supervision by another healthcare provider. The RN, focusing on patient safety, must function within the legal scope of practice and by the federal, state, and local laws, rules and regulations, and policies, procedures, and guidelines of the employing health care institution or practice setting. The RN provides safe, compassionate, and comprehensive nursing care to patients and their families with complex healthcare needs (5).
Self Quiz
Ask yourself...
- What does the term "Professional nursing" mean?
- What is professional nursing performance based on in Texas nursing jurisprudence and ethics?
- Does professional nursing include medical diagnosis or the prescription of therapeutic or corrective measures?
- Does professional nursing involve the supervision or teaching of nursing or the development of the nursing care plan?
- Can an RN engage in independent nursing practice without the supervision by another health care provider?
Texas Nursing Jurisprudence and Ethics - Board Rules
Texas Board of Nursing, Chapter 217, Rule §217.11, Standards of Nursing Practice (6)
The Texas Board of Nursing regulates nursing practice within the State of Texas for Vocational Nurses, Registered Nurses, and Registered Nurses with advanced practice authorization. The standards of practice establish a minimum acceptable level of nursing practice in any setting for each level of nursing licensure or advanced practice authorization. Failure to meet these standards may result in action against the nurse's license even if no actual patient injury resulted (6).
- Standards Applicable to All Nurses. All vocational nurses, registered nurses, and registered nurses with advanced practice authorization shall:
- Know and conform to the Texas Nursing Practice Act, the Board's rules and regulations, and all federal, state, or local laws, rules, or regulations affecting the nurse's current area of nursing practice.
- Implement measures to promote a safe environment for clients and others.
- Know the rationale for and the effects of medications and treatments and shall correctly administer the same.
- Accurately and completely report and document:
- The client's status, including signs and symptoms, is as follows:
- Nursing care rendered.
- Physician, dentist, or podiatrist orders.
- Administration of medications and treatments.
- client response(s).
- contacts with other healthcare team members concerning significant events regarding the client's status.
- Respect the client's right to privacy by protecting confidential information unless required or allowed by law to disclose the information.
- Promote and participate in education and counseling to a client(s) and, where applicable, the family/significant other(s) based on health needs.
- Obtain instruction and supervision as necessary when implementing nursing procedures or practices.
- Make a reasonable effort to obtain orientation/training for competency when encountering new equipment and technology or unfamiliar care situations.
- Notify the appropriate supervisor when leaving a nursing assignment.
- Know, recognize, and maintain professional boundaries of the nurse-client relationship.
- Comply with mandatory reporting requirements of Texas Occupations Code Chapter 301 (Nursing Practice Act), Subchapter I, which includes reporting a nurse:
- Who violates the Nursing Practice Act or a board rule and contributed to the death or severe injury of a patient.
- Whose conduct causes a person to suspect that the nurse's practice is impaired by chemical dependency or drug or alcohol abuse?
- Whose actions constitute abuse, exploitation, fraud, or a violation of professional boundaries.
- Whose actions indicate that the nurse lacks knowledge, skill, judgment, or conscientiousness to such an extent that the nurse's continued practice of nursing could reasonably be expected to pose a risk of harm to a patient or another person, regardless of whether the conduct consists of a single incident or a pattern of behavior.
- Except for minor incidents (Texas Occupations Code §§301.401(2), 301.419, 22 TAC §217.16), peer review (Texas Occupations Code §§301.403, 303.007, 22 TAC §217.19), or peer assistance if no practice violation (Texas Occupations Code §301.410) as stated in the Nursing Practice Act and Board rules (22 TAC Chapter 217).
- Provide, without discrimination, nursing services regardless of the age, disability, economic status, gender, national origin, race, religion, health problems, or sexual orientation of the client served.
- Institute appropriate nursing interventions that might be required to stabilize a client's condition and prevent complications.
- Clarify any order or treatment regimen the nurse has reason to believe is inaccurate, non-efficacious, or contraindicated by consulting with the appropriate licensed practitioner and notifying the ordering practitioner when the nurse decides not to administer the medication or treatment.
- Implement measures to prevent exposure to infectious pathogens and communicable conditions.
- Collaborate with the client, members of the health care team, and, when appropriate, the client's significant other(s) in the interest of the client's health care.
- Consult with, utilize, and make referrals to appropriate community agencies and health care resources to provide continuity of care.
- Be responsible for one's continuing competence in nursing practice and individual professional growth.
- Make assignments to others that consider client safety and are commensurate with the educational preparation, experience, knowledge, and physical and emotional ability of the person to whom the assignments are made.
- Accept only those nursing assignments that consider client safety and are commensurate with the nurse's educational preparation, experience, knowledge, and physical and emotional ability.
- Supervise nursing care provided by others for whom the nurse is professionally responsible.
- Ensure the verification of current Texas licensure or other Compact State licensure privileges and credentials of personnel for whom the nurse is administratively responsible when acting in the role of nurse administrator.
- Standards Specific to Vocational Nurses. The licensed vocational nurse practice is a directed scope of nursing practice under the supervision of a registered nurse, advanced practice registered nurse, physician's assistant, physician, podiatrist, or dentist. Supervision is the process of directing, guiding, and influencing the outcome of an individual's performance of an activity. The licensed vocational nurse shall assist in the determination of predictable healthcare needs of clients within healthcare settings and:
- Shall utilize a systematic approach to provide individualized, goal-directed nursing care by:
- Collecting data and performing focused nursing assessments.
- Participating in the planning of nursing care needs for clients.
- Participating in developing and modifying the comprehensive nursing care plan for assigned clients.
- Implementing appropriate aspects of care within the LVN's scope of practice.
- Assisting in the evaluation of the client's responses to nursing interventions and the identification of client needs.
- Shall utilize a systematic approach to provide individualized, goal-directed nursing care by:
-
- Shall assign specific tasks, activities, and functions to unlicensed personnel commensurate with the educational preparation, experience, knowledge, and physical and emotional ability of the person to whom the assignments are made and shall maintain appropriate supervision of unlicensed personnel.
- May perform other acts that require education and training as prescribed by board rules and policies, commensurate with the licensed vocational nurse's experience, continuing education, and demonstrated licensed vocational nurse competencies.
- Standards Specific to Registered Nurses. The registered nurse shall assist in the determination of healthcare needs of clients and shall:
- Utilize a systematic approach to provide individualized, goal-directed nursing care by:
- Performing comprehensive nursing assessments regarding the health status of the client.
- Making nursing diagnoses serves as the basis for the care strategy.
- Developing a plan of care based on the assessment and nursing diagnosis.
- Implementing nursing care.
- Evaluating the client's responses to nursing interventions.
-
- Delegate tasks to unlicensed personnel in compliance with Chapter 224 of this title, relating to clients with acute conditions or in acute environments, and Chapter 225, relating to independent living environments for clients with stable and predictable situations.
- Standards Specific to Registered Nurses with Advanced Practice Authorization. Standards for a specific role and specialty of advanced practice nurses supersede standards for registered nurses where conflict between the standards, if any, exists. In addition to paragraphs (1) and (3) of this subsection, a registered nurse who holds authorization to practice as an advanced practice nurse (APN) shall:
- Practice in an advanced nursing practice role and specialty by the authorization granted under Board Rule Chapter 221 of this title (relating to practicing in an APN role; 22 TAC Chapter 221) and standards set out in that chapter.
- Prescribe medications in accordance with the prescriptive authority granted under Board Rule Chapter 222 of this title (relating to APNs prescribing; 22 TAC Chapter 222) and standards set out in that chapter and compliance with state and federal laws and regulations relating to the prescription of dangerous drugs and controlled substances. (4)

Self Quiz
Ask yourself...
- Why is it important for Texas Nursing Jurisprudence and Ethics that a nurse know the rationale for and the effects of medications and treatments before administering these to a client?
- Are there negative consequences if a nurse is not trained to perform a task or procedure? If so, what are 1-2 consequences of lack or training or errors?
- How do nurses utilize a systematic approach to providing individualized, goal-directed, nursing care?
- What challenges of appropriate delegation have you encountered and how have you over come them?
- What techniques have helped you to be successful in delegation?
The Board's Position Statements
15.28 The Registered Nurse Scope of Practice (See also the LVN Scope of Practice) (7)
The Board of Nursing recommends that all nurses utilize the Scope of Practice Decision-Making Model (DMM) when deciding if an employer's assignment is safe and legally within the nurse's scope of practice (8).
The Texas Board of Nursing (BON or Board) is authorized by the Texas Legislature to regulate the nursing profession to ensure that every licensee is competent to practice safely. The Texas Nursing Practice Act (NPA) defines the legal scope of practice for professional registered nurses (RN) (4, 9).
The RN takes responsibility and accepts accountability for practicing within the legal scope of practice, is prepared to work in all healthcare settings, and may engage in independent nursing practice without supervision by another healthcare provider. With a focus on patient safety, the RN must function within the legal scope of practice and in accordance with federal, state, and local laws, rules, and regulations. In addition, the RN must comply with policies, procedures, and guidelines of the employing health care institution or practice setting. The RN provides safe, compassionate, and comprehensive nursing care to patients and their families with complex healthcare needs (9).
This position statement aims to provide direction and recommendations for nurses and their employers regarding the safe and legal scope of practice for RNs and to promote an understanding of the differences in the RN programs of study and between the RN and LVN levels of licensure. The LVN scope of practice is interpreted in Position Statement (9).
Every nursing education program in Texas must ensure that their graduates exhibit competencies outlined in the Board's Differentiated Essential Competencies of Graduates of Texas Nursing Programs Evidenced by Knowledge, Clinical Judgements, and Behaviors. These competencies are included in the program of study so that every graduate has the knowledge, clinical judgment, and behaviors necessary for RN entry into safe, competent, and compassionate nursing care. The DECs serve as a guideline for employers to assist RNs in transitioning from the educational environment into nursing practice. As RNs enter the workplace, the DECs are the foundation for developing the RN scope of practice (9).
Completion of ongoing, informal continuing nursing education offerings and on-the-job training in an RN's area of practice serves to develop, maintain, and expand competency. Because the RN scope of practice is based upon the educational preparation in the RN program of study, there are limits to expanding the scope. The Board believes that successfully transitioning from one level of nursing practice to another requires the nurse to complete a formal education program. (10)
The RN Scope of Practice
The professional RN advocates for the patient and the patient's family and promotes safety by practicing within the NPA and the BON Rules and Regulations. The RN provides nursing services that require substantial specialized judgment and skill. The planning and delivery of professional nursing care are based on knowledge and application of biological, physical, and social science principles as acquired by a completed course of study in an approved school of professional nursing. Unless licensed as an advanced practice registered nurse, the RN's scope of practice does not include acts of medical diagnosis or the prescription of therapeutic or corrective measures. RNs utilize the nursing process to establish the plan of care in which nursing services are delivered to patients. The level and impact of the nursing process differ between the RN and LVN, as well as the levels of RN education (9).
Assessment
The comprehensive assessment is the first step and lays the foundation for the nursing process. The thorough evaluation is the initial and ongoing, extensive data collection, analysis, and interpretation. Nursing judgment is based on the assessment findings. The RN uses clinical reasoning and knowledge, evidence-based outcomes, and research as the basis for decision-making and comprehensive care (9).
Based upon the comprehensive assessment, the RN determines the physical and mental health status, needs, and preferences of culturally, ethnically, and socially diverse patients and their families using evidence-based health data and knowledge synthesis. Surveillance is an essential step in the comprehensive assessment process. The RN must anticipate and recognize changes in patient conditions and determine when reassessments are needed (9).
Patient Diagnosis/Problem Identification/Planning
The second step in the nursing process is nursing diagnosis and problem identification. The role of the RN is to synthesize comprehensive assessment data to identify problems, formulate goals/outcomes, and develop plans of care for patients, families, populations, and communities using information from evidence-based practice and published research in collaboration with these groups and the interdisciplinary health care team (9).
The third step in the nursing process is planning. The RN synthesizes the data collected during the comprehensive assessment to identify problems, make nursing diagnoses, and formulate goals, teaching plans, and outcomes. A nursing plan of care for patients is developed by the RN, who is responsible for coordinating nursing care for patients. Teaching plans address health promotion, maintenance, restoration, and risk factors prevention. The RN utilizes evidence-based practice, published research, and information from patients and the interdisciplinary healthcare team during the planning process (9).
Implementation
Implementing the plan of care is the fourth step in the nursing process. The RN may begin, deliver, assign, or delegate specific interventions within the care plan for patients within legal, ethical, and regulatory parameters and consider health restoration, disease prevention, wellness, and promotion of healthy lifestyles (9).
The RN's duty to patient safety when making assignments to other nurses or delegating tasks to unlicensed staff is to consider the education, training, skill, competence, and physical and emotional abilities of those to whom the assignments or delegation is made. The RN is responsible for reasonable and prudent decisions regarding assignments and delegation. The RN's scope of practice may include the supervision of LVNs or other RNs. Supervision of LVN staff is defined as the process of directing, guiding, and influencing the outcome of an individual's performance and activity. The RN may have to directly observe and evaluate the nursing care provided depending on the LVN's skills and competence, patient conditions, and level of urgency in emergent situations (9).
The RN may determine when to delegate tasks to unlicensed personnel and maintain accountability for how they perform the tasks. The RN is responsible for supervising the unlicensed personnel when tasks are delegated. The proximity of supervision depends upon patient conditions and the skill level of the unlicensed personnel. In addition, teaching and counseling are interwoven throughout the implementation phase of the nursing process. (10,11)
Evaluation and Reassessment
A critical and final step in the nursing process is evaluation. The RN evaluates and reports patient outcomes and responses to therapeutic interventions compared to benchmarks from evidence-based practice and research findings and plans any follow-up care and referrals to appropriate resources that may be needed. The evaluation phase is one of the times when the RN reassesses patient conditions and determines if interventions were effective and if any modifications to the care plan are necessary (9).
Essential Skills Used in the Nursing Process
Communication
Communication is an essential and fundamental component used during the nursing process. The RN must communicate verbally, in writing, or electronically with healthcare team members, patients, and their families in all aspects of the nursing care provided to patients. The patient record or nursing care plan must appropriately document these communications. Because RNs plan, coordinate, initiate, and implement a multidisciplinary team's approach to patient care, collaboration is crucial to communication. When patient conditions or situations exceed the RN's level of competency, the RN must be prepared to seek out other RNs with greater competency or other health care providers with differing knowledge and skillsets and actively cooperate to ensure patient safety (9).
Clinical Reasoning
Clinical reasoning is another integral component of the nursing process. RNs use critical thinking skills to problem-solve and make decisions in response to patients, their families, and the healthcare environment. RNs are accountable and responsible for the quality of nursing care provided and must exercise prudent and professional nursing judgment to ensure the standards of nursing practice are always met (9).
Employment Setting
When an employer hires an RN to perform a job, the RN must ensure that it is safe and legal. Caution must be exercised to stay within the legal parameters of nursing practice when an employer may not understand the limits of the RN's scope of practice and makes an assignment that is not safe. Before engaging in an activity or assignment, the RN must determine whether he or she has the education, training, skill, competency, and physical and emotional ability to carry out the activity or assignment safely. The RN must always provide patients with safe, compassionate, and comprehensive nursing care (9).
Summary of RN Scope of Practice
The RN, with a focus on patient safety, must function within the legal scope of practice and by the federal, state, and local laws, rules and regulations, and policies, procedures, and guidelines of the employing health care institution or practice setting. The RN functions under his or her license and assumes accountability and responsibility for the quality of care provided to patients and their families according to the standards of nursing practice. The RN demonstrates responsibility for continued competence in nursing practice and develops insight through reflection, self-analysis, self-care, and lifelong learning (9).
The table below offers a brief synopsis of how the scope of practice for nurses differs based on educational preparation and level of licensure. These are minimum competencies but also set limits on what the LVN or RN can do at his or her given level of licensure, regardless of experience (9).
Synopsis of Differences in Scope of Practice for Licensed Vocational, Associate, Diploma and Baccalaureate Degree Nurses (10)
Synopsis of Differences in Scope of Practice for Licensed Vocational, Associate, Diploma and Baccalaureate Degree Nurses (4)
| Nursing Practice |
LVN Scope of Practice Directed/Supervised Role |
ADN or Diploma RN Scope of Practice Independent Role |
BSN RN Scope of Practice Independent Role |
| Education |
|
|
|
| Setting |
|
|
|
| Assessment |
|
|
|
| Nursing Diagnosis/ Problem Identification/ Planning |
|
|
|
| Implementation |
|
|
|
|
Evaluation
|
|
|
|
Nursing board Position Statements are not laws, but they provide direction for nurses on issues of concern to the Board relevant to public protection. These Position Statements are reviewed annually for relevance and accuracy to current practice, the Nurse Practice Act, and Board of Nursing rules. Examples of Position Statements include the following: (9)
- Nurses Carrying out Orders from Physician Assistants
- Role of the Licensed Vocational Nurse in the Pronouncement of Death
- LVNs Engaging in IV Therapy, Venipuncture, or PICC Lines
- Educational Mobility
- Nurses with Responsibility for Initiating Physician Standing Orders
- Board Rules Associated with Alleged Patient "Abandonment"
- The Role of LVNs & RNs in the Management and Administration of Medications via Epidural or Intrathecal Catheter Routes
- The Role of the Nurse in Moderate Sedation
- Performance of Laser Therapy by RNs or LVNs
- Continuing Education: Limitations for Expanding Scope of Practice
- Delegated Medical Acts
- Use of American Psychiatric Association Diagnoses by LVN, RNs, or APRNs
- Role of LVNs & RNs As School Nurses
- Duty of a Nurse in any Practice Setting
- Board's Jurisdiction Over a Nurse's Practice in Any Role and Use of the Nursing Title
- Development of Nursing Education Programs
- Texas Board of Nursing/Board of Pharmacy Joint Position Statement on Medication Errors
- Nurses Carrying Out Orders from Advanced Practice Registered Nurses (APRN)
- Nurses Carrying Out Orders from Pharmacists for Drug Therapy Management
- Registered Nurses in the Management of an Unwitnessed Arrest in a Resident in a Long-Term Care Facility (9)

Self Quiz
Ask yourself...
-
What are advantages for nurses to consistently use the nursing process during care and documentation of care of clients?
-
How could communication breakdown among employee nurse team members impact a client's care?
-
Are nursing board Position Statements laws?
-
Name one example of a nursing board Position Statement.
-
What do RNs use to problem-solve and make decisions regarding care of clients, when it comes to Texas Nursing Jurisprudence and Ethics?
Principles of Texas Nursing Jurisprudence and Ethics
Professional Boundaries
15.29 Professional Boundaries including use of social media by nurses (11)
The purpose of this Position Statement is to guide nurses regarding expectations related to professional boundaries, including social media, and to provide nurses with guidance to prevent boundary violations (5).
In keeping with its mission to protect public health, safety, and welfare, the Texas Board of Nursing (BON or Board) holds nurses accountable for knowing, recognizing, and maintaining professional boundaries of the nurse-patient/client relationship. The term professional boundaries is defined as the appropriate limits that the nurse should establish in the nurse/client relationship due to the nurse's power and the patient's vulnerability. Professional boundaries refer to the provision of nursing services within the limits of the nurse/client relationship, which promote the client's dignity, independence, and best interests and refrain from inappropriate involvement in the client's relationships and the obtainment of the nurse's gain at the client's expense (5).
The National Council of State Boards of Nursing (NCSBN) defines professional boundaries as the spaces between the nurse's power and the patient's vulnerability. The nurse's power comes from the nurse's professional position and access to sensitive personal information. The difference in personal information the nurse knows about the patient versus the personal information the patient knows about the nurse creates an imbalance in the nurse-patient relationship. Nurses should respect the power imbalance and ensure a patient-centered relationship (5).
Common to the definition of professional boundaries from the Texas Board of Nursing and the NCSBN is that a nurse abstains from personal gain at the client's expense and refrains from inappropriate involvement with the patient or the patient's family (5).
Duty of a Nurse in Maintenance of Professional Boundaries
There is a power differential between the nurse and the patient. The patient depends on the nurse's knowledge and relies on the nurse to advocate for the patient and ensure actions are taken in the patient's best interest. The nurse must protect the patient, establishing and maintaining professional boundaries in the nurse-patient/client relationship. Under or over-involvement can harm the patient and may interfere with the nurse-patient relationship. Visualizing the two ends of the spectrum may assist the nurse in knowing, recognizing, and maintaining the professional boundaries of nurse-patient relationships (5).
Patients each have their own unique needs and abilities. The boundary line for any one patient may change over time and may not be the same as the boundary line for another patient. It is up to the nurse to assess and recognize the patient's needs, adjusting the nursing care accordingly. Every nurse is responsible for knowing, identifying, and maintaining the professional boundaries of the nurse-client relationship (5).
Boundary Violations
A violation of professional boundaries is one element of the definition of "conduct subject to reporting [Tex. Occ.Ide Sec. 301.401(1)(C)]. A professional boundary violation is also considered unprofessional conduct [22 TAC §217.12 (6)(D)]. Some of the specific categories of professional boundary violations include but are not limited to, physical, sexual, emotional, or financial boundary violations (5).
Use of Social Media and the Protection of Health Information
Social media and other electronic communication are expanding exponentially as the number of social media outlets, platforms, and applications available continues to increase. Nurses play a significant role in identifying, interpreting, and transmitting knowledge and information within healthcare. As technological advances expand connectivity and communication, rapid knowledge exchange and dissemination can pose risks to patients and nurses. While the Board recognizes that using social media can be a valuable tool in healthcare, there are potentially severe consequences if misused. A nurse's use of social media may cause the nurse to unintentionally blur the lines between the nurse's professional and personal life (5).
Online postings may harm patients if protected health information is disclosed. In addition, social media postings may reflect negatively on individual nurses, the nursing profession, the public's trust in the nursing profession, or the employer and may jeopardize careers. In an NCSBN survey, many responding boards reported receiving complaints about nurses misusing social media sites. The survey results indicated that boards fired by employers have disciplined nurses and are criminally charged for the inappropriate or unprofessional use of social media (5).
To ensure the mission to protect and promote the welfare of the people of Texas, the Texas Board of Nursing supports the guidelines and principles of social media use by the NCSBN and the American Nurses Association. By the NCSBN guidelines and Board rules, it is the Board's position that (5):
Nurses have an ethical and legal obligation to maintain patient privacy and confidentiality. When using social media, nurses do not identify patients by name or post or publish information that may lead to patient identification. Limiting access to postings through privacy settings is not sufficient to ensure privacy. Nurses must promptly report any identified breach of confidentiality or privacy (5).
Nurses maintain professional boundaries in the use of electronic media. The nurse must establish, communicate, and enforce professional boundaries with patients online. Nurses do not refer to patients disparagingly, even if the patient is not identified, or transmit information that may be reasonably anticipated to violate patient rights to confidentiality or privacy or otherwise degrade or embarrass the patient (5).
Nurses must provide nursing services without discrimination and not make threatening, harassing, profane, obscene, sexually explicit, racially derogatory, homophobic, or other offensive comments (5).
Nurses must be aware of and comply with all laws and rules, including employer policies regarding using electronic devices, including employer-owned computers, cameras, and personal devices. In addition, nurses must ensure appropriate and therapeutic use of all patient-related electronic media, including patient-related images, photos, or videos, by applicable laws, rules, and institutional policies and procedures (5).
The use of social media can be of tremendous benefit to nurses and patients alike, for example, the dissemination of public safety announcements. However, nurses must know the potential consequences of disclosing patient-related information via social media. Nurses must always maintain professional standards, boundaries, and compliance with local, state, and federal laws. All nurses must protect their patients' privacy and confidentiality, which extends to all environments, including social media (5).
The following are ways to avoid problems when using social media:
- Never post any healthcare-related images, client information, or even general client information
- Only use your organization's name or a client or family member's name to post content about or speak for your employer if your organization authorizes you to follow their specific policy and procedures.
- Never post comments about a client, even if the client is not named.
- Never post photos or videos of your healthcare organization or clients
- Never post any comments about your employer or other team members
- Never use obscenity, profanity, racial slurs, sexually inappropriate comments, homophobic comments, threats, harassing/abusive language, or any other offensive comments. Never post any image that contains the above content.
Prevention of Boundary Violations
The ability of a client to rely on employees as concerned and caring individuals who remain objective in their guidance is one of the tents of a safe, therapeutic relationship. The relationship may no longer be objectively therapeutic when staff interacts with patients personally. Accepting gifts, financial transactions, and romantic entanglement could lead to various negative consequences for an organization, employee, or client. Many organizations enforce a non-fraternization policy between employees and current or former clients. While there are exceptions, the expectation is that employees are not to establish a personal relationship with a current or former client. Organizations do recognize that there are times when peers, friends, family, or neighbors of employees seek treatment. In these circumstances, the relationship must remain the nature it was before admission if in the client's best interest, and the treatment plan should address the relationship to best meet the client's therapeutic needs. Employees should also notify a supervisor when an individual with whom he or she has a relationship is admitted for treatment (5).
Texas Nurses are required to comply with mandatory reporting requirements of Texas Occupations Code Chapter 301 NPA Subchapter I, which include reporting a nurse (11):
- Who violates the NPA or a board rule and contributed to the death or severe injury of a patient.
- Whose conduct causes a person to suspect that the nurse's practice is impaired by chemical dependency or drug or alcohol abuse?
- Whose actions constitute abuse, exploitation, fraud, or a violation of professional boundaries.
- Whose actions indicate that the nurse lacks knowledge, skill, judgment, or conscientiousness to such an extent that the nurse's continued practice of nursing could reasonably be expected to pose a risk of harm to a patient or another person, regardless of whether the conduct consists of a single incident or a pattern of behavior.
The exception is for minor incidents, peer review, or peer assistance if there is no practice violation as stated in the Nursing Practice Act and Board rules (6, 11).
Organizations also take many precautions to ensure appropriate employee-client relationships, including (13):
- Criminal background checks of employees
- Employee, student, and volunteer education regarding therapeutic boundaries and issues and consequences of any violations
- Mandatory, supportive, and confidential reporting of any violation
Employee supervision also includes the identification of early signals that an employee may be crossing therapeutic boundaries and the institution of appropriate interventions. Employees educate clients regarding the importance of maintaining a therapeutic relationship and proper boundaries. Organizations work to ensure adequate supervision of staff and appropriate supervision of clients, such as increased observation or same-gender staff working with a client when appropriate (13).
There must be mandatory reporting by any employee who becomes aware of a boundary violation. The employee should report this immediately to their supervisor, who will evaluate the nature and severity of the claim and initiate an investigation of the situation. In conjunction with Human Resources and Risk Management, the immediate supervisor will determine whether an accused employee should be put on immediate leave pending investigation results and whether mandatory reporting of the allegations to outside agencies is required. Legal Counsel may also be consulted when necessary. An employer may not suspend or terminate employment or otherwise discipline, retaliate, or discriminate against a person who reports, in good faith, or advises a nurse of the nurse's rights and obligations (5, 9, 11, 12).

Self Quiz
Ask yourself...
- Why is it important to Texas Nursing Jurisprudence and Ethics for a nurse to maintain professional and appropriate boundaries with a client?
- Name two examples of how social media may cause a nurse to blur the lines between his/her personal and professional life?
- Is reporting of boundary violations mandatory? If so, name two examples of when a nurse should report.
- How do organizations take precautions to ensure appropriate employee-client relationships?
- List two examples of nurses whom a nurse in Texas would report for violations of the Nurse Practice Act.
Unprofessional Conduct - Rule §217.12
The following unprofessional conduct rules are intended to protect clients and the public from incompetent, unethical, or illegal conduct of licensees. The purpose of these rules is to identify behaviors in the practice of nursing that are likely to deceive, defraud, or injure clients or the public. Actual injury to a client need not be established. These behaviors include but are not limited to: (all from 5)
1.Unsafe practice – actions or conduct including, but not limited to:
- Carelessly failing, repeatedly failing, or exhibiting an inability to perform vocational, registered, or advanced practice nursing in conformity with the standards of a minimum acceptable level of nursing practice set out in §217.11 of this chapter.
- Failing to conform to generally accepted nursing standards in applicable practice settings.
- Improper management of client records.
- Delegating or assigning nursing functions or a prescribed health function when the delegation or assignment could reasonably be expected to result in unsafe or ineffective client care.
- Accepting the assignment of nursing functions or a prescribed health function when the acceptance of the assignment could be reasonably expected to result in unsafe or ineffective client care.
- Failing to supervise the performance of tasks by any individual working pursuant to the nurse's delegation or assignment.
- Failure of a clinical nursing instructor to adequately supervise or to assure adequate supervision of student experiences.
2. Failure of a chief administrative nurse to follow standards and guidelines required by federal or state law or regulation or by facility policy in providing oversight of the nursing organization and nursing services for which the nurse is administratively responsible.
3. Failure to practice within a modified scope of practice or with the required accommodations, as specified by the Board in granting an encumbered license or any stipulated agreement with the Board.
4. Conduct that may endanger a client's life, health, or safety.
5. Inability to Practice Safely – a demonstration of actual or potential inability to practice nursing with reasonable skill and safety to clients by reason of illness, use of alcohol, drugs, chemicals, or any other mood-altering substances, or as a result of any mental or physical condition.
6. Misconduct – actions or conduct that include, but are not limited to:
- Falsifying reports, client documentation, agency records, or other documents.
- Failing to cooperate with a lawful investigation conducted by the Board.
- Causing or permitting physical, emotional, or verbal abuse or injury or neglect to the client or the public, or failing to report same to the employer, appropriate legal authority and/or licensing Board.
- Violating professional boundaries of the nurse/client relationship including but not limited to physical, sexual, emotional, or financial exploitation of the client or the client's significant other(s).
- Engaging in sexual conduct with a client, touching a client in a sexual manner, requesting, or offering sexual favors, or language or behavior suggestive of the same.
- Threatening or violent behavior in the workplace.
- Misappropriating, in connection with the practice of nursing, anything of value or benefit, including but not limited to, any property, real or personal of the client, employer, or any other person or entity, or failing to take precautions to prevent such misappropriation.
- Providing information, which was false, deceptive, or misleading in connection with the practice of nursing.
- Failing to answer specific questions or providing false or misleading answers in a licensure or employment matter that could reasonably affect the decision to license, employ, certify, or otherwise utilize a nurse.
- Offering, giving, soliciting, or receiving, or agreeing to receive, directly or indirectly, any fee or other consideration to or from a third party for the referral of a client in connection with the performance of professional services.
7. Failure to pay child support payments as required by the Texas Family Code §232.001, et seq.
8. Drug diversion – diversion or attempts to divert drugs or controlled substances.
9. Dismissal from a board-approved peer assistance program for noncompliance and referral by that program to the Board.
10. Other drug-related actions or conduct that include, but are not limited to:
- Use of any controlled substance or any drug, prescribed or unprescribed, or device or alcoholic beverages while on duty or on call and to the extent that such use may impair the nurse's ability to safely conduct to the public the practice authorized by the nurse's license.
- Falsification of or making incorrect, inconsistent, or unintelligible entries in any agency, client, or other record pertaining to drugs or controlled substances.
- Failing to follow the policy and procedure in place for the wastage of medications at the facility where the nurse was employed or working at the time of the incident(s).
- A positive drug screen for which there is no lawful prescription.
- Obtaining or attempting to obtain or deliver medication(s) through means of misrepresentation, fraud, forgery, deception and/or subterfuge.
11. Unlawful practice – actions or conduct that include, but are not limited to:
- Knowingly aiding, assisting, advising, or allowing an unlicensed person to engage in the unlawful practice of vocational, registered, or advanced practice nursing.
- Violating an order of the Board, or carelessly or repetitively violating a state or federal law relating to the practice of vocational, registered, or advanced practice nursing, or violating a state or federal narcotics or controlled substance law.
- Aiding, assisting, advising, or allowing a nurse under Board Order to violate the conditions set forth in the Order.
- Failing to report violations of the Nursing Practice Act and/or the Board's rules and regulations.
12. Leaving a nursing assignment, including a supervisory assignment, without notifying the appropriate personnel.
There is a Texas State Board of Nursing Disciplinary Matrix that nurses can review to see the process followed when a review of a nurse's conduct is necessary. The Board will consider public safety, the seriousness of the violation, and any aggravating or mitigating factors. Other factors considered include the presence of multiple violations, prior violations, and costs which could result in a more severe disciplinary action. (13)

Self Quiz
Ask yourself...
- Name two examples of unsafe nursing practice that will result in a nursing board review.
- Is violating boundaries of the employee-client relationship considered misconduct?
- Is failing to report violations of the Nursing Practice Act misconduct?
- Is failing to report violations of the Nursing Board's rules and regulations misconduct?
- Name two examples of unsafe nursing practice that will result in a nursing board review.
- Is violating boundaries of the employee-client relationship considered misconduct?
- Is failing to report violations of the Texas Nursing Jurisprudence and Ethics misconduct?
- Is failing to report violations of the Nursing Board's rules and regulations misconduct?
- What qualifies as an unlawful practice?
- What policies does your facility have regarding drug screening and reporting?
Provisions of the Code of Ethics for Nurses
Provision 1
The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person. (1)
Provision 2
The nurse's primary commitment is to the patient, whether an individual, family, group, community, or population. (1)
Provision 3
The nurse promotes, advocates for, and protects the rights, health, and safety of the patient. (1)
Provision 4
The nurse has authority, accountability, and responsibility for nursing practice, makes decisions, and takes action consistent with the obligation to provide optimal patient care. (1)
Provision 5
The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth. (1)
Provision 6
The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care. (1)
Provision 7
The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy. (1)
Provision 8
The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities. (1)
Provision 9
The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy. (1)

Self Quiz
Ask yourself...
- Who is a Texas nursing jurisprudence and ethics-oriented nurse primarily committed to?
- Name two examples of how a nurse advocates for a client.
- Name three ways a nurse committed to Texas nursing jurisprudence and ethics protects a client's rights.
- Which of the abovementioned provisions have you found to be the most challenging to meet?
- What resources are available in your area to help navigate difficult ethical situations?
Case Study
Rachel is a 13-year-old adolescent female client admitted to an inpatient behavioral health unit for bipolar disorder, alcohol and marijuana abuse, and borderline personality disorder. The client has a history of sexual promiscuity, lying, and has alleged abuse and rape by history. Rachel approaches the Charge RN at bedtime, saying that an employee and she "have been having sex" many times over the course of two weeks and that she realizes now that "she should have told someone". The alleged employee is currently on duty.
As Charge RN, using what you learned about Texas Nursing Jurisprudence and Ethics, how would you respond, and what are your next steps?
Conclusion - Texas Nursing Jurisprudence and Ethics
When a nurse is named in a negligence or malpractice lawsuit, it can create stress for the client, the employee, and the employer. A nurse maintaining professional, ethical, and jurisprudent conduct will help to ensure standards of practice are consistently followed. Maintaining appropriate boundaries with clients at all times helps maintain a therapeutic employee-client relationship.
It is important that nurses understand their state nurse practice act, the scope of practice of nurse licensure, standards of practice, ethics, and professional boundaries in order to maintain professionalism, meet performance standards, and avoid a breach of duty, injury, and litigation.
Resources
Educational Requirements:
Texas Board of Nursing (2010), Differentiated Essential Competencies (DECs) of graduates of Texas Nursing Programs. (12)
Texas Occupations Code, Chapter 301 (12)
Nursing Practice Act (NPA) Section 301.002, Definitions (12)
Rule 217.11 - Standards of Nursing Practice (12)
Scope of Practice Position Statements: (12)
- Position Statement 15.28 The Registered Nurse Scope of Practice Web version for viewing
- Position Statement 15.14 - Duty of a Nurse Web version for viewing
- Position Statement 15.14 - Duty of a Nurse - HHSC/DADS/BON poster
For the complete list of position statements, click here. (12)
Texas Nursing Forensics
Texas Nursing Forensics
Introduction
In the United States, sexual assault was historically considered a judicial problem; however, it is now considered a major public health concern because of the health and psychological effects on individuals. The problem most notably emerged in the public eye in the 1960s with the women's liberation movement. In recent times the #METOO movement has increased awareness of the problem, and many organizations have surfaced to assist the assaulted. This course will focus on the problem in rural areas in the state of Texas and how nurses working in these facilities can best assist patients who have been sexually assaulted.

Self Quiz
Ask yourself...
- Aside from the hospital, what other setting might you encounter victims of sexual assault?
- In your opinion, what factors contribute to limited care for victims of sexual assault in rural areas?
- What types of psychological problems do you suspect victims of sexual assault may struggle with?
- When was the last time you received training in nursing forensics?
- How has the assessment and management of victims of assault changed since you have been in practice?
- Have you seen an increased incidence of sexual assault occur since you have been in practice? How has your facility managed the change?
- How has technology impacted the reporting and documenting of assault?
- What policies and procedures does your facility have regarding victims of assault?
- What resources does your community offer to help victims of assault?
- What policies does your facility have regarding the management of forensics in victims of assault?
Statistical Evidence
National Statistics
According to the Rape Abuse and Incest National Network (RAINN) (1), every 68 seconds someone is sexually assaulted in the United States, and every nine minutes, that victim is a child (1). Only 25 out of every 1,000 perpetrators will end up in prison (1).in less than every 80 seconds, a person is sexually assaulted. In 2015 the Texas Statewide Sexual Assault Prevalence Study found that 33.2% of adult Texans or 413,000 individuals reported having been sexually assaulted at some point during their lives (2).
Each year in the United States (1):
- 80,600 inmates are sexually assaulted or raped
- 60,000 children were victims of “substantiated or indicated” sexual abuse
- 433,648 people 12 and older were sexually assaulted or raped
- 18,900 military personnel experienced unwanted sexual contact
- 1 out of every 6 women have been the victim of attempted or completed rape in her lifetime (14.8% completed, 2.8% attempted)
- 1 in 3 men have experienced an attempted or completed rape in their lifetime
- More women and children are sexually assaulted than men, and that girls under 18 years of age are at the highest risk. According to RAINN (1), men and boys, especially college-aged, are also at risk with transgender students at the highest risk of this group.
Most common locations where sexual assault occurs in the U.S. (1):
- 55% at or near the victim’s home
- 15% in an open public space
- 12% at or near a relative’s home
- 10% in an enclosed but public area (i.e. parking garage or lot)
- 8% on school property
Activities the victims were doing when they were assaulted (1):
- 48% were sleeping or performing another activity at home
- 29% were traveling to and from work or school, or traveling to shop or run errands
- 12% were working
- 7% were attending school
- 5% were doing an unknown or other activity
Sexual Assault on Children (1):
- 1 in 9 girls and 1 in 20 boys under the age of 18 experience sexual abuse or assault
- 2 out of 3 victims of sexual assault or rape (under the age of 18) are age 12 – 17
- Victims of sexual assault or rape under the age of 18 are about 4 times more likely to develop symptoms of drug abuse and PTSD as adults, and about 3 times more likely to experience a major depressive episode as adults

Self Quiz
Ask yourself...
- What statistic surprised you the most? Why?
- Do you feel that these statistics represent what you see in your area? Why do you think that is the case?
- What factors do you think contribute the highest number of sexual assault cases occurring in the home?
- What are some strategies to help victims feel safe reporting their sexual assault?
- What strategies can communities use to protect children from sexual assault?
- In your opinion, what factors impact the reduced reporting from men after being sexually assaulted?
- What education can you provide to victims regarding the incidence of sexual assault?
- What policies does your facility have regarding children who are suspected victims of assault?
- What role does a community and or public health nurse play in the education and prevention of sexual assault?
- How has the education and management of sexual assault prevention changed since you have been in practice?
Texas Statistics
The latest statistics on sexual assault in the state of Texas were from 2018 and is as follows (2):
- Total number of reported sexual assault incidents was 19,816, a 9.4% increase from the prior year
- Of victim-to-offender relationships, 11% were romantic, 14% parental/child, 19% other family, and 55% other.
- Victims were 88% were female and 12% male
- Victims who were aged 10 – 14 were the group with highest number of cases
- Of all victims, 82% were white, 17% black, and 1% American Indian/Alaskan Native, Asian, or Native Hawaiian/Pacific Islander
Location of sexual assault incidents in Texas in 2018 (2):
- 16,015 in residents/homes
- 2,041 in unknown or other areas
- 657 in a hotel/motel
- 718 in school/college
- 710 in a highway/road/alley
- 506 in a parking lot/garage
- 268 in fields/woods
- 185 in commercial/office buildings
- 176 in drug stores, doctor’s offices, or hospitals

Self Quiz
Ask yourself...
- Do you think the care should be different for a patient sexually assaulted by a family member versus a romantic partner?
- The age of sexual assault is younger in Texas (10 to 14) than the country (12 to 17). What strategies can Texas employ for prevention?
- What is the benefit of knowing statistical evidence about sexual assault?
- What might need to be considered when caring for a male patient who had been sexually assaulted versus a female patient?
- What are your thoughts on the incidence of sexual assault in Texas in comparison to that of the U.S.?
- Have you seen an increase in sexual assault in your area? What do you feel has contributed to that?
- Do you feel that the Texas statistics listed above are accurate? Or do you think that they are higher or lower? Why?
- Which population group have you encountered most frequently in practice?
- How does your education and communication change in different genders, ages, and ethic groups who are victims of sexual assault?
- What prevention techniques have you seen to help prevent the incidence of sexual assault?
The Basics: Sexual Assault
What is Sexual Assault?
Sexual assault, also termed sexual violence, is described as “any type of unwanted sexual contact, including words and actions of a sexual nature against a person’s will and without their consent; a person may use force, threats, manipulation, or coercion to commit sexual violence” (3). Sexual assault is often defined separate from rape. Rape consists of penetration, whether vaginally, anally, or orally. Sexual assault is any type of unwanted sexual content and is not limited to rape. Sexual abuse, as described by the American Psychological Association (APA) "is unwanted sexual activity, with perpetrators using force, making threats or taking advantage of victims not able to give consent" (3). Assault can be the product of domestic abuse, gang violence, date rape, and incest. Assault can be inflicted on any age or gender and often occurs by someone who is related to or knows the victim.
What is SANE?
In many parts of the United States, Sexual Assault Nurse Examiners (SANE), nurses who are expertly trained in performing forensic examinations and collection of evidence, are utilized (5). SANEs are nurses who specialize in forensic nursing. In forensic nursing, the health and legal system intersect (10). SANE programs began as early as the 1970s. At that time, nurses noticed that victims of sexual assault were not provided high quality care like other patients were in the emergency department. Nurses also noticed that the victims were very concerned about STDs and pregnancy and needed special treatment. Over the next 20 years, the forensic specialty grew, and the First SANE programs were started in Tennesse, Minnesota, and Texas. Today, Texas registered nurses working in the emergency departments must learn the SANE process to perform the forensics exams and evidence collection by completing a 2-hour educational program.

Self Quiz
Ask yourself...
- Why do you think sexual assault has changed from a judicial problem to a health problem?
- How can nurses contribute to a decrease in the costs associated with sexual assault?
- What organizations in Texas can you connect with to learn more about sexual assault and how you can impact the problem?
- Where can you find more information on SANE programs?
- What additional training can you complete to help better prepare you to manage sexual assault victims?
- What is the definition of sexual assault?
- How many nurses are available in your facility who are SANE nurses?
- What resources does your facility and community offer to help pay for the cost of becoming a SANE nurse?
- What additional resources are you aware of to assist with the management of sexual assault victims?
- What barriers to identifying sexual assault have you encountered? How have you overcome them?
Nursing's Role
Sexual assault is an extremely traumatic experience. Those affected can have a wide range of issues, emotionally, spiritually, physically, and psychologically. Nurses working in the emergency department are often first responders. Compassion, empathy, and privacy are a hallmark of excellent practice when caring for patients who have been sexually assaulted.
Many patients will experience shock and disbelief. "Why me? Will I be okay?" or "It's no big deal, I'm fine" (6). There may be "fear of responses from friends, family, the public, and criminal justice providers" (7). Victims of rape may also have concerns about pregnancy, STIs, and HIV/AIDS. These patients may feel their world has turned upside down. They may be scorned, told it was deserved, and fear their names could be made public (7).
In order to provide excellent care, all gender identities must be taken into consideration, as well as age and sexual orientation. No bias or judgment should be displayed to the patient. Customs, beliefs, religious, and spiritual needs should also be considered during the visit
Team Collaboration
Working with all personnel in the emergency department is essential. From paramedics, law enforcement officers, family, or anyone accompanying the patient to physicians, social workers, and forensic medical examiners, each professional has a specific skill set and role in the patient's care. Teamwork among these groups of individuals will provide the best possible outcomes for the patient. Team members involved in a victim’s care may include (8):
- “Community-based advocates
- Law enforcement officers
- SANEs, physicians or nurses trained in sexual assault medical forensic evidence collection
- Law enforcement victim service advocates
- District Attorney’s Office personnel, legal victim advocates and attorneys”
Interview
The interviewing nurse should actively listen, believe what the patient discloses, validate the patient’s feelings, maintain confidentiality, and honor the patient’s decisions on what to do about the assault. When caring for patients who have sexually assaulted, treating the whole person rather than the "problem" alone is vital. Repeating information back to the patient can help to elicit more precise information. Repeating information can also help to validate what the patient is saying, creating an atmosphere of trust. Consider that patients may not want to talk about the assault, as reliving it could bring out unwanted emotions.
If the patient arrives alone, the nurse should inquire if the patient wants a companion or an advocate to be present. An advocate could be a family member, friend, member of the clergy, or social worker. The patient can choose if they want someone present. Care must be taken to ensure the patient feels comfortable, as the presence of someone emotionally involved (or even the assaulter themselves) may deter the patient from being open and honest. An interpreter should also be arranged if needed, with the patient's consent.
If the patient has not alerted the local police, the nurse should inquire if they wish to report the assault and if so, the police should then be called. If available, a sexual assault response team (SART) should be immediately contacted. It is of the utmost importance to remember that the patient always makes the primary decision of what to do surrounding the case. Also, the patient must give consent first before any decisions are made. Admitting the patient to a private room in a quiet area of the emergency department lessens interruptions from outside sources.

Self Quiz
Ask yourself...
- Does your facility have a Sexual Assault Response Team (SART)?
- Have you ever taken care of a patient who had been sexually assaulted?
- What are some strategies you can employ if your emergency department does not have a private room to interview a victim of sexual assault?
- What is the protocol at your facility if a parent brings their child into the emergency department with sexual assault injuries?
- What techniques during the interview process of a sexual assault victim have you found to be unsuccessful?
- What techniques during the interview process of a sexual assault victim have you found to be successful?
- What types of collaboration have you seen in the facilities where you have worked?
- What role does law enforcement play in managing victims of sexual assault?
- What education do you provide to patients regarding STIs after sexual assault?
- How do you ensure the privacy of victims after admitting them to the hospital?
Assessment
After obtaining consent to perform the assessment, the patient should be advised of every step before each part of the exam. The patient should be informed they have total control of what is happening. It is important for the nurse to help the patient understand they always have the right to refuse any and all steps in the examination.
When performing the initial assessment and gathering information, documentation must include a very detailed and complete history, including any physical trauma to the patient’s body. The history should include any bruises, lacerations, or other visual injuries and how and when they occurred. The nurse should perform the interview slowly, giving the patient time to process and answer each question. The patient may or may not want to identify the person who assaulted them and should not be coerced into doing so.
A complete medical, surgical, and gynecologic history, in the case of a female patient, and any new symptoms occurring after the assault should be asked. Drug allergies, medications, and any alcohol or illegal drugs used at the time of the event are also documented. A compassionate and empathic tone should always be used to allow the patient to feel safe. The patient should not feel any judgment from any emergency department personnel. Patients should be given the opportunity and encouraged to grieve and react during this time. They should feel comfortable enough to ask and answer questions throughout the interview.
According to Texas law, nurses must obtain written consent from the patient. During the complete physical exam, the nurse will be charged with ensuring physical evidence of the assault from clothing or body fluids is not disturbed. Also, during this time, suicidality and emotional support should be assessed. Providing expert treatment for patients who have been sexually assaulted is of utmost importance. When available, a SANE nurse will perform the forensic examination. This examination is vital to collect and preserve physical evidence from the patient while also assessing life and limb injuries. If a SANE nurse is unavailable, as may be the case in Texas's rural areas, a "medical forensic examiner" will perform the examination.


Self Quiz
Ask yourself...
- How would you handle a situation in which a patient who has recently been sexually assaulted does not want to participate in the physical assessment?
- Are you familiar with medical forensic examiners?
- How often does your facility audit documentation?
- How might a nurse address their own biases when caring for a victim of sexual assault?
- What barriers to assessment have you encountered? How have you overcome them?
- Do you have to receive written consent from a patient before a physical exam?
- What policies does your facility have regarding the psychosocial assessment of patients of sexual assault?
- How do you ensure that your patient stays informed of their care while respecting their emotions?
- How can a complete medical, surgical, and gynecological history improve patient care and outcomes?
- What is a medical forensic examiner?
Documentation
When documenting the case, the nurse should use open-ended questions to elicit the patient's best and clearest responses. Documentation must be complete and exact, including every stage of the assault with times, dates, and descriptions, with consideration for the patient's emotional state and ability to recall. Using motivational interviewing can be helpful as well. Documenting in the patient’s own words is best practice. Nurses should try their best to document all of the following about the case (8):
- “All those present during the patient’s history and examination
- Time, date, and location of assault(s)
- Contact and/or penetrative acts by suspect(s)
- Was the suspect injured in any way, if known?
- Use of lubricant, including saliva
- Patient’s actions between the sexual assault and arrival at the facility (brushing teeth, using mouthwash, smoking, vaping, changing clothes, vomiting, swimming, showering, or bathing)
- Was a condom used?
- Did ejaculation occur? Where?
- Any weapon use or physical force, or threat of weapon use or physical force?
- Description of condition of clothing (and was clothing torn or stained prior to assault?)”
In the case of a minor, a parent will give consent, and if no parent is available or is the assaulter, the child will be turned over to the appropriate child and family services in the state. If the assaulted patient has dementia or is an elder with cognitive issues and is therefore unable to consent, adult protective services should be contacted (8). There are also rules governing military sexual offenses. Remember when documenting these cases, whether using handwritten or electronic medical records, any and all information is subject to HIPAA.

Self Quiz
Ask yourself...
- What skills do you have that could best be used when caring for patients who have sexually assaulted?
- How would you, as the initial contact, approach an individual who has been sexually assaulted?
- What skills would you need to learn or improve when caring for a patient who has been sexually assaulted?
- Currently, do you feel capable of caring for a patient who has been sexually assaulted without judgment and with compassion?
- What documentation policies do you have at your facility regarding sexual assault victims?
Texas Forensic Law
The Texas government code 420.031 (9) describes the protocol that must be taken to develop and protect evidence collection in a sexual assault case. Since a major part of Texas is rural, the code was enacted to protect and care for patients and the collected evidence in areas where a SANE nurse is not available. In these cases, a medical forensic examiner may perform the exam and evidence collection.
A medical forensic examiner is described as any practitioner Medical Doctor, Registered Nurse, Nurse Practitioner, or Physician's Assistant who has undergone a minimum of 2 hours of training in forensic evidence collection. The law outlines requirements in the collection and preservation of evidence. In 2019, the code was amended to require written informed consent from the patient or guardian for release of the evidence and must be gained prior to the history and physical. Obtaining consent also carries important psychological implications after a sexual assault since the patient's right to consent was violated by the assaulter. Sexual assault examination teams should always be involved as early as possible.
Texas Forensic Law: Statute of Limitations
The statute of limitations for sexual assault cases can be defined as a deadline in which a person can report a sexual assault. The statute of limitations vary per state and the length of time for reporting can depend on whether the case is criminal or civil. Criminal cases are committed against the state and prosecuted by the state; civil cases occur between individuals/groups and are prosecuted by a civil court (i.e. family court or personal injury cases) (12). In Texas, the statute of limitations varies by age and whether the case is criminal or civil. The following are general statute of limitations regarding sexual assault in Texas (13)(14). The legal age of sexual consent in Texas is 17.
For adults, the statute of limitation is 10 years from the victim’s 18th birthday. As of 2019, victims of sexual assault can file a personal injury claim for injuries arising from childhood sexual abuse up to 30 years from the incident.
There is no statute of limitations if:
- During the investigation of the offense, biological matter (evidence) is collected, and the matter has not yet been subjected to forensic DNA testing
- Forensic DNA testing results show that the matter does not match the victim or any other person whose identity is readily ascertained
- Probable cause exists to believe that the defendant has committed the same or a similar sex offense against five more victims
- Continuous sexual abuse of young child or disabled individual occurs
- Indecency with a child occurs

Self Quiz
Ask yourself...
- How would you handle a situation in which an adult patient wants to file a claim for a sexual assault that occurred 35 years ago?
- If your 16-year-old patient does not want to file a police report on her boyfriend who sexually assaulted her, how would you respond?
- In which situation would you involve social services?
- How often do you make reports to child or adult protective services?
- How do you become a medical forensic examiner?
- What is a statute of limitations in Texas?
- When is there no statute of limitations?
- What is the difference between criminal and civil cases?
Texas Forensic Law: Evidence
Sexual assault evidence can be found in several areas, including the crime scene, the patient's body, skin, hair, nails and clothing, and other items belonging to the patient (11). There is a specific kit used to collect this evidence. As described by RAINN, the kit is best known as a RAPE or Sexual Assault Evidence Kit (SAEK) and is inclusive of the items listed below (11):
- Bags and paper sheets to put on the floor and collect clothing or other evidence that may fall off the patient while undressing,
- A comb to collect evidence from hair
- Forms for documentation
- Envelopes and containers for the evidence
- Instructions on use of the kit
- Sampling materials and swabs
Types of evidence collected are usually skin samples, scrapings from fingernails, and oral, genital, and anal swabbing internal and external. Directions on how to collect this evidence are included in the kit. The forensic examiner can also use special types of photography to document internal injurie. (11). Personal cameras should never be used. Remember, it is the law that the patient consents to each part of the exam.
As described by RAINN, prior to the forensic exam, it is best if the patient has not changed clothes, combed their hair, brushed their teeth, tried to clean the area, showered, or bathed, or used a restroom. If needing to use the restroom, a urine sample should be collected, educating the patient not to cleanse the perianal area. If they have already showered or bathed and have not arrived at the emergency room yet, emergency personnel need to educate the patient to keep the clothes they were wearing and any other belongings they had with them at the time of the assault in a paper bag in order to preserve the evidence (11). If the patient comes to the emergency department up to 7 days after being sexually assaulted, the exam can still be performed. After the 7 days, it is at the forensic examiner's discretion whether the exam should be performed. Collecting and protecting forensic evidence is a legal, moral, and professional responsibility (12).
Any medical witness who testifies in court is held in the highest regard and as experts in sexual assault cases (5). Courts will closely scrutinize the chain of custody, and if broken, it can cause a conflict in the case and question of validity. Cases may be heard in criminal, civil, juvenile, military courts, or grand juries. If a forensics examiner is called to be a "fact" witness, no opinions on the case will be heard. Only the procedures that were performed on the patient will be admitted, and if the testifier is not the professional who performed the examination, they may be questioned regarding SANE protocols.
If called upon to be an expert witness, the SANE nurse not only has knowledge of protocols but can educate and give opinions to the court. In either case, the necessity for excellent knowledge of SANE protocols is important. Nurses must be comfortable testifying in court as it is a rigorous and stress-provoking experience. Working with your organization's lawyers and prosecutors, as well as reviewing the case extensively, will prepare the nurse to testify in a case (5).

Self Quiz
Ask yourself...
- Have you ever used a sexual assault evidence kit (SAEK)?
- If your emergency department does not have a SAEK, how would you obtain one?
- How well do you feel you could testify in court?
- Where in your facility can you find support if you had to testify?
- What policies does your facility have regarding forensic evidence?
- What training has your facility provided regarding forensic evidence collection?
- What is a medication witness?
- What policies does your facility have in place regarding photographing and placing images in the patient's chart?
- How does your facility store and protect forensic evidence that has been collected?
- What is the time period in which the medical forensic examiner should perform an exam?
Texas Law: Chain of Custody
In order to protect the patient and evidence for the courts, a chain of custody of the evidence must be followed precisely. Failure to comply does not mean the evidence is not admissible in the courts; however, the more complete the evidence, the better chance of conviction of the assaulter. Texas A&M's nursing program offers a chain of evidence handbook outlining each step in the collection of evidence. The information below highlights the collection process from that handbook (8).
Collection of Evidence and Packing
- “Collect evidence so that it will be admissible as evidence in legal proceedings later. Therefore, chain of custody must be maintained and documented throughout the entire patient assessment and evidence collection processes.
- Chain of custody documents the dates and times of everyone who handles every piece of evidence, from the time it is collected through to legal proceedings."
- Evidence should be labeled with patient’s name, date of birth, unique identifier number, examiner’s initials, date, and time.
- If adult patient chooses non-reporting method, the external SAEK is labeled only with the unique identifier number (often the medical record number or the Track-Kit barcode). The Track-Kit identifier can be utilized.
- Consider also labeling additional evidence not included in the kit (i.e., clothing collected when patient is reporting to law enforcement) with Track-Kit labels without the barcode.
- Evidence inside the SAEK is labeled according to standard facility procedure. Follow facility protocols on non-reporting evidence collection.
- Consider providing a card with the unique identifier for the patient if the Track-Kit identifier is not utilized.”
Chain of Custody Documentation
Documentation must include:
- Receipt of evidence
- Storage of the evidence
- Transfer of the evidence
- Date and time of each transfer
- The printed name and signature of each person in possession of or transferring the evidence
- Signatures of all persons transferring or receiving the evidence


Self Quiz
Ask yourself...
- Does your facility evidence collection protocol vary from what is listed above? In what ways?
- At your facility, what is the protocol if the evidence is mishandled or mislabeled?
- Aside from nurses, who else might handle the evidence kit?
- Can you think of any other that should be documented that are not listed above?
- What is the chain of custody?
Conclusion
Sexual assault has become a major health problem in the United States. The state of Texas has implemented a code of laws to identify, protect, and collect evidence from patients who have experienced this crisis. The utilization of SANE nurses is common in major metropolitan area hospitals, but many rural areas in that state are not equipped with the program. To properly care for these patients and collect and protect evidence appropriately, Texas has mandated education for emergency department nurses not served by SANE personnel.
It is imperative that emergency department nurses become educated on the use of SAEK kits for evidence collection and chain of custody protocols. The utilization of the SANE method allows for standardized care that is safe, and protective of the patient and their rights.
Quality Improvement for Nurses
Introduction
Welcome to the world of Quality Improvement (QI) in healthcare, a dedicated field committed to continually enhancing patient care and outcomes. Quality Improvement involves a systematic approach to identify, analyze, and address areas for improvement within healthcare processes, ultimately resulting in improved patient safety, satisfaction, and overall healthcare excellence (13). In this course, we will embark on a journey to explore the fundamental principles and practical applications of QI, explicitly tailored for nurses who aspire to make a positive impact in their healthcare settings.
As a nurse, you know the significance of providing high-quality patient care. However, you may wonder how you can actively contribute to improving the systems and processes in your workplace.
Imagine this scenario: You observe a recurring issue with medication administration, where doses are occasionally missed due to workflow inefficiencies. Through this course, you will acquire the knowledge and skills to apply QI methodologies like Plan-Do-Study-Act (PDSA) cycles to investigate such issues, implement changes, and monitor the impact of your interventions. By understanding QI principles and tools, you will be better equipped to collaborate with your colleagues, drive meaningful improvements, and ensure that your patients receive the best care possible.
Introduction
Welcome to the world of Quality Improvement (QI) in healthcare, a dedicated field committed to continually enhancing patient care and outcomes. Quality Improvement involves a systematic approach to identify, analyze, and address areas for improvement within healthcare processes, ultimately resulting in improved patient safety, satisfaction, and overall healthcare excellence (13). In this course, we will embark on a journey to explore the fundamental principles and practical applications of QI, explicitly tailored for nurses who aspire to make a positive impact in their healthcare settings.
As a nurse, you know the significance of providing high-quality patient care. However, you may wonder how you can actively contribute to improving the systems and processes in your workplace.
Imagine this scenario: You observe a recurring issue with medication administration, where doses are occasionally missed due to workflow inefficiencies. Through this course, you will acquire the knowledge and skills to apply QI methodologies like Plan-Do-Study-Act (PDSA) cycles to investigate such issues, implement changes, and monitor the impact of your interventions. By understanding QI principles and tools, you will be better equipped to collaborate with your colleagues, drive meaningful improvements, and ensure that your patients receive the best care possible.

Self Quiz
Ask yourself...
- How can nurses leverage their unique position at the bedside to identify opportunities for quality improvement in healthcare settings?
- Can you provide an example from your own experience or knowledge where a quality improvement project led to tangible improvements in patient care?
- What potential challenges could a nurse encounter when attempting to implement quality improvement projects?
What is Quality Improvement?
Quality Improvement (QI) in healthcare represents an ongoing, systematic effort to elevate the quality of patient care and healthcare services that involves identifying areas needing improvement, implementing changes, and evaluating the effects of those changes to ensure better patient outcomes (12).
Let’s envision a scenario where a hospital's surgical department grapples with a higher-than-average rate of post-operative infections. Through a QI initiative, the healthcare team can meticulously scrutinize the surgical processes, pinpoint potential sources of infection, and introduce evidence-based practices such as enhanced sterilization techniques or more rigorous antibiotic prophylaxis protocols. Over time, they can gauge the effectiveness of these changes by monitoring infection rates for a reduction.
Commonly used QI methodologies in healthcare include the DMAIC (Define, Measure, Analyze, Improve, Control) process and the Plan-Do-Study-Act (PDSA) cycle. These approaches provide structured frameworks for healthcare professionals to tackle issues systematically and iteratively. For example, imagine a bustling primary care clinic with extended patient wait times.
Here, the PDSA cycle can come into play using the systematic iterative steps below:
- The team defines the problem (lengthy wait times)
- The team proceeds to test a change (for example, adjusting appointment scheduling)
- The team then scrutinizes the results and acts accordingly to refine the process.


Self Quiz
Ask yourself...
- How does the concept of Quality Improvement (QI) align with the goal to provide the best possible care for patients?
- Can you think of a specific healthcare scenario where QI methodologies like DMAIC or PDSA could significantly improve patient care?
- What are the advantages of using structured frameworks like DMAIC and PDSA in QI initiatives?
- How do DMAIC or PDSA contribute to the success of improvement projects?
History and Background of Quality Improvement
The history and background of Quality Improvement (QI) in healthcare have a rich and evolving timeline, dating back to the early 20th Century, with significant developments occurring over the years. One pivotal moment in this journey was the introduction of statistical quality control by Dr. Walter A. Shewhart in the 1920s (24). Dr. Shewhart's pioneering work laid the foundation for using statistical methods to monitor and enhance processes, a concept that would become integral to QI initiatives (24).
In the mid-20th Century, the contributions of Dr. W. Edwards Deming further propelled QI principles forward (7). Dr. Deming emphasized the significance of continuous improvement, active employee engagement, and process variability reduction. His ideas found fertile ground in post-World War II Japan, playing a crucial role in the nation's economic recovery and the emergence of renowned companies like Toyota, famous for its Toyota Production System (TPS), incorporating QI concepts (7).
Until today, QI has become indispensable to healthcare systems worldwide (16). To illustrate, envision a scenario where a hospital grapples with a high readmission rate among heart failure patients. By scrutinizing historical data and implementing evidence-based protocols for post-discharge care, hospitals can effectively lower readmissions, enhance patient outcomes, and potentially evade financial penalties under value-based reimbursement models (16).

Self Quiz
Ask yourself...
- How did the work of Dr. Walter A. Shewhart in the early 20th Century contribute to the foundation of QI, and how do statistical methods continue to play a role in healthcare improvement today?
- What fundamental principles were introduced by Dr. W. Edwards Deming, and how did they influence QI practices in healthcare and other industries?
- Can you provide an example of how QI methodologies, inspired by Deming's principles, have been successfully applied in modern healthcare settings to address specific challenges or improve patient care?
- How has continuous improvement evolved, and why is it considered a cornerstone of QI in healthcare?
Models
At the heart of ongoing transformations in healthcare lies various Quality Improvement (QI) models. These models provide structured frameworks for identifying and addressing areas of improvement within healthcare systems (14). These models offer healthcare professionals a systematic approach to instigate meaningful process changes, ultimately resulting in elevated care quality. See some models below.
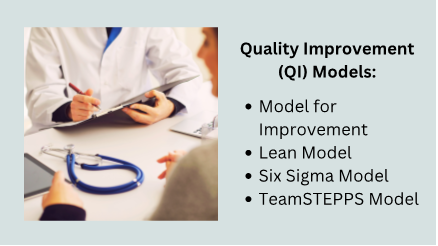
Model for Improvement
The Model for Improvement is a widely recognized and highly effective framework for Quality Improvement (QI) in healthcare. This is because it empowers healthcare professionals to systematically test and fine-tune their ideas for process improvement, ensuring that changes are grounded in evidence and proven effective (17).
The Model for Improvement offers a structured and systematic approach to identifying, testing, and implementing changes to enhance healthcare processes and ultimately elevate patient outcomes.
Developed by Associates in Process Improvement (API), this model revolves around the iterative "Plan-Do-Study-Act" (PDSA) cycle, which forms the foundational structure of QI initiatives (17). The Plan-Do-Study-Act (PDSA) cycle is a systematic approach that guides healthcare teams through quality improvement, and it comprises the four key phases below, each contributing to developing and implementing meaningful changes in healthcare practices (12).
- Plan: In this initial phase, healthcare teams define the specific problem they aim to address, set clear and measurable goals, and craft a comprehensive plan for implementing the proposed change. For instance, if a hospital seeks to reduce patient wait times in the emergency department, the plan may involve adjustments to triage protocols or streamlining documentation processes.
- Do: Once the plan is established, the proposed change is implemented, typically on a small scale or within a controlled or pilot environment. This enables healthcare professionals to assess the feasibility and potential impact of the change without making widespread adjustments.
- Study: The study phase involves rigorous data collection and analysis to evaluate the effects of the change. In our example, the hospital would measure the impact of the new triage protocols on wait times, closely examining whether they have decreased as expected.
- Act: Based on the findings from the study phase, the healthcare team makes informed decisions about the change. They may adopt the change if it has successfully reduced wait times, adapt it further for enhanced effectiveness, or, if necessary, abandon it.
The PDSA cycle's iterative nature means adjustments can be made, and the cycle repeats until the desired improvement is achieved (12).
Lean Model
The Lean model, initially conceived in the manufacturing sector, has found considerable success and applicability in healthcare as a potent tool for process enhancement and waste reduction (22). At its core, Lean thinking revolves around the principles of efficiency and value optimization because it focuses on refining processes to eliminate wasteful elements while simultaneously delivering care of the highest quality (22).
Healthcare organizations have adopted Lean methodologies to tackle many challenges, from reducing patient wait times to improving inventory management and elevating overall patient satisfaction (22). For instance, when a hospital is challenged with prolonged wait times in its outpatient clinic, it can apply Lean principles to systematically analyze the patient flow, pinpoint bottlenecks, and streamline processes.
This might involve reconfiguring furniture to enhance flow, adjusting appointment scheduling, or implementing standardized work procedures. The ultimate objective is to cultivate a patient-centric, efficient environment that ensures timely access to care while meticulously conserving time and resources.
Another integral aspect of Lean thinking is the unwavering commitment to continuous improvement and the pursuit of perfection through the systematic identification and eradication of various forms of waste (19). The forms of waste are often categorized into seven types: overproduction, waiting, unnecessary transportation, overprocessing, excess inventory, motion, and defects (19). By keenly identifying and addressing these forms of waste, healthcare organizations not only enhance the utilization of resources but also curtail costs and elevate the overall quality of care delivery.
Six Sigma model
The Six Sigma model is a robust and widely adopted healthcare method for improving processes and reducing mistakes (9). It was first used in manufacturing but is now used in healthcare to make processes more consistent and improved by finding and fixing mistakes and inefficiencies (9).
An example is when a hospital is concerned about the accuracy of medication dosing for pediatric patients, a Six Sigma team might include: indicating the problem, gathering data on mistakes regarding dosing, and finding out why the mistakes happened. The strategy may encompass the implementation of standardized dosing protocols, refining staff training programs, and closely monitoring the medication administration process to ensure that mistakes are eliminated.
Six Sigma uses a framework called DMAIC (Define, Measure, Analyze, Improve, Control) to make improvements. This framework utilizes data-driven tools to discern problems, quantify their origins, develop practical solutions, and institute control mechanisms to sustain improvements (11). Through this systematic journey, healthcare organizations position themselves to deliver care of elevated quality, curtail costs, and bolster patient safety.
TeamSTEPPS model
TeamSTEPPS, which stands for Team Strategies and Tools to Enhance Performance and Patient Safety, is a teamwork and communication model designed explicitly for healthcare settings (4). Developed by the U.S. Department of Defense and the Agency for Healthcare Research and Quality (AHRQ), TeamSTEPPS focuses on improving patient safety by enhancing team collaboration, communication, and decision-making among healthcare professionals (4).
One key element of TeamSTEPPS is using structured communication techniques to prevent errors and misunderstandings. For instance, during patient handoffs from one healthcare provider to another, TeamSTEPPS emphasizes using a structured tool like SBAR (Situation, Background, Assessment, Recommendation) to convey critical information succinctly and accurately. This ensures that essential patient details are noticed, reducing the risk of adverse events (18).
In a surgical team scenario, TeamSTEPPS principles can be applied to improve teamwork and communication among surgeons, nurses, and anesthesiologists. The model encourages briefings before procedures to set clear objectives, huddles during surgery to address emerging issues, and debriefings afterward to reflect on the process and identify areas for improvement. By fostering a culture of open communication and mutual respect, TeamSTEPPS contributes to safer, more efficient healthcare delivery (4).


Self Quiz
Ask yourself...
- How can healthcare organizations determine which QI model suits their specific challenges or improvement goals?
- How do QI models emphasize data collection and analysis, and why is this critical in healthcare?
- Can you imagine a real-world scenario where the Lean Six Sigma framework can successfully improve healthcare processes and outcomes?
- What are some emerging trends or innovations in QI models and methodologies, and how might they shape the future of healthcare quality improvement?
IOM Six Domains of Patient Care
The Institute of Medicine (IOM), now known as the National Academy of Medicine, introduced the Six Domains of Quality in Healthcare as a framework to assess and improve the quality of patient care (14). These domains, introduced in 2001, encompass various aspects of care delivery and patient experience, helping healthcare organizations and providers identify areas for improvement (14). The domains serve as pillars for assessing the different dimensions of care delivery, ensuring that healthcare organizations and providers address the holistic needs of patients (14).
Definitions
The Six Domains of Patient Care are essential for providing high-quality healthcare. See definitions of each of the IOM's six domains of patient care below.
- Safe: Safety is the foundational domain, emphasizing the importance of reducing the risk of patient harm. This includes preventing medical errors, preventing infections, and ensuring the safe administration of medications. Healthcare organizations implement safety protocols and engage in continuous monitoring to minimize risks (14).
- Effective: Effective care ensures that patients receive evidence-based treatments and interventions that result in the desired outcomes. It involves using the best available scientific knowledge to make informed decisions about patient care avoiding unnecessary or ineffective treatments (14).
- Patient-Centered: Patient-centered care focuses on individualizing healthcare to meet each patient's unique needs and preferences. It involves respecting patients' values and preferences, engaging them in shared decision-making, and delivering care with empathy and compassion (14).
- Timely: Timely care emphasizes reducing delays in healthcare delivery. It includes providing care promptly and avoiding unnecessary waiting times for appointments, tests, and treatments. Timely care is especially critical in emergencies (14).
- Efficient: Efficiency in healthcare means maximizing resource utilization and minimizing waste while providing high-quality care. This domain emphasizes streamlining processes, reducing unnecessary costs, and optimizing healthcare resources (14).
- Equitable: Equitable care underscores the importance of providing healthcare that is fair and just, regardless of a patient's background, socioeconomic status, or other factors. It aims to eliminate healthcare access and outcomes disparities among different patient populations (14).
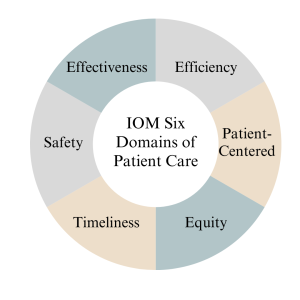
Measures
Measures in the context of the Institute of Medicine (IOM) six domains of patient care refer to the metrics and indicators used to assess and evaluate the quality of care provided in each domain. According to (14), the measures below are essential for monitoring and improving healthcare services. See details below.
- The "Safe" domain measures focus on tracking and reducing adverse events and medical errors. Key indicators include rates of medication errors, hospital-acquired infections, falls, and complications from procedures. Safety measures also assess the implementation of safety protocols, such as hand hygiene compliance and patient identification bracelets.
- Measures in the "Effective" domain assess how evidence-based practices and treatments are utilized. These measures include adherence to clinical guidelines, appropriate use of medications, and the success rates of medical interventions. Additionally, outcomes such as patient recovery, remission, or improvement are indicators of the effectiveness of care.
- The "Patient-Centered" domain focuses on assessing the patient’s experience and satisfaction with care. Patient surveys and feedback are standard measures, evaluating aspects like communication with healthcare providers, involvement in decision-making, and overall satisfaction with the care received. Healthcare organizations also measure shared decision-making and respect for patient preferences.
- Measures related to the "Timely" domain evaluate the efficiency of healthcare delivery. Key metrics include waiting times for appointments, diagnostic tests, and procedures. Additionally, measures track the timely delivery of urgent care and the avoidance of unnecessary delays in treatment.
- Efficiency measures aim to quantify resource utilization and the reduction of waste in healthcare. Metrics may include the cost of care per patient, length of hospital stays, and resource allocation efficiency. Improvement in resource utilization and cost-effectiveness are vital indicators of efficiency.
- Measures within the "Equitable" domain assess disparities in healthcare access and outcomes among different patient populations. Healthcare utilization and outcomes data are stratified by demographics, socioeconomic status, race, and ethnicity to identify and address inequities. Key indicators include access to preventive care, healthcare utilization rates, and health outcomes across various demographic groups.

Self Quiz
Ask yourself...
- How can healthcare providers ensure their care aligns with patients' values, preferences, and cultural backgrounds?
- What challenges might patients face in accessing healthcare services, and how can healthcare organizations improve access for all patients?
- What are the potential consequences of poor care coordination among healthcare providers, and how can interdisciplinary teams work together to enhance coordination?
- Why must healthcare organizations continually assess and improve the quality of care they provide, and what mechanisms can be implemented to support ongoing improvement efforts?
Nursing Quality Indicators
According to (5), nursing quality indicators are essential metrics used to evaluate and improve the quality of nursing care in healthcare settings. These indicators provide valuable insights into nursing practice and patient outcomes, helping healthcare organizations and nursing staff deliver safe, effective, patient-centered care. Let's delve into some key nursing quality indicators and their significance below.
Patient Falls
Patient falls are a critical quality indicator in nursing care since they can result in severe injuries and complications for patients (5). As a result, healthcare organizations measure and monitor the rate of patient falls to identify trends and implement preventive measures.
For example, when a hospital notices an increase in the rate of falls among elderly patients in a particular unit, they may introduce interventions such as nonslip flooring, improved lighting, and patient education as fall prevention strategies to reduce the incidence of falls.

Medication Administration Errors
Ensuring accurate medication administration is crucial in nursing practice because medication errors can lead to adverse events, including patient harm or death (5). Nursing quality indicators related to medication administration errors include the rate of medication errors and adherence to medication reconciliation processes (5). For instance, nurses are encouraged to verify patient allergies and cross-check medication orders to prevent errors. If there is an increase in medication errors in a healthcare facility, it may prompt a review of medication administration protocols and additional staff training.

Pressure Ulcers (Bedsores)
Pressure ulcers are a quality indicator of patient skin integrity since they develop when patients remain immobile for extended periods (5). As a result, healthcare organizations measure the incidence and prevalence of pressure ulcers as an indicator of the quality of nursing care (5).
Patient Satisfaction
Patient satisfaction is a patient-centered nursing quality indicator since it reflects the overall patient experience and perception of care (5). Surveys and feedback mechanisms are used to measure patient satisfaction. For example, a scenario might involve patients receiving post-discharge surveys that assess various aspects of their hospital experience, including nurse responsiveness, communication, and pain management. Healthcare organizations can use this feedback to identify areas for improvement and enhance patient-centered care.
In summary, nursing quality indicators encompass a range of metrics that evaluate nursing care quality, patient safety, and patient experiences. By monitoring and responding to these indicators, healthcare organizations and nursing staff can continuously improve their quality of care, leading to better outcomes and increased patient satisfaction (5).

Self Quiz
Ask yourself...
- Why is data collection critical in nursing quality improvement efforts?
- What types of data should nurses prioritize collecting to assess patient safety?
- How can nurses ensure the accuracy and reliability of the data they collect for quality improvement purposes?
- What challenges might nurse face when collecting patient-related data, and how can these challenges be overcome?
Data Collection
Quality improvement data collection is a critical component of healthcare quality initiatives, providing the necessary information to assess the current state of care, identify areas for improvement, and monitor progress over time (2). Accurate and meaningful data collection enables healthcare organizations to make informed decisions, implement evidence-based interventions, and ultimately enhance patient outcomes. Let's explore the methods of data collection below.
- Clinical Outcome Collection: Clinical outcome data collection is essential for assessing the effectiveness of healthcare interventions (2). For example, consider a scenario where a hospital is implementing a quality improvement project to reduce surgical site infections (SSIs) following orthopedic surgeries. Data collection would involve tracking the number of SSIs occurring over a specific period and collecting information on patient characteristics, surgical techniques, and post-operative care protocols. By analyzing this data, the healthcare team can identify trends, risk factors, and areas for improvement, ultimately leading to targeted interventions to reduce SSIs.
- Patient Satisfaction Survey Data Collection: Patient satisfaction surveys are valuable tools for collecting data on patient experience (2). A primary care clinic that aims to improve patient satisfaction may administer surveys to patients after each visit, asking about aspects of care such as communication with healthcare providers, wait times, and overall experience. The collected data can reveal areas of strength and areas requiring improvement. For instance, if survey results consistently indicate longer-than-desired wait times, the clinic can adjust scheduling practices or implement strategies to reduce wait times and enhance patient satisfaction.
- Process Measures Data Collection: Process measure data collection focuses on evaluating the efficiency and effectiveness of healthcare processes (2). For instance, in a medication reconciliation scenario, a healthcare organization might collect data on the accuracy and completeness of medication lists during care transitions. By tracking the frequency of medication reconciliation discrepancies, they can identify process inefficiencies and implement standardized protocols for reconciliation, leading to safer care transitions and reduced medication errors.
- Adverse Event Reporting Data Collection: Adverse event reporting is a crucial mechanism for collecting data on incidents that result in patient harm or near misses (2). For example, consider a scenario where a nurse administers the wrong medication dose to a patient but catches the error before any harm occurs. Reporting this near-miss event allows the healthcare organization to investigate the root causes, implement preventive measures, and share lessons learned with the care team to prevent similar incidents in the future.
Types of Data
Data types play a crucial role in understanding the current state of care, identifying areas for improvement, and implementing evidence-based interventions (2). Let’s explore the different types of data used in quality improvement below.
- Quantitative Data: Quantitative data involves numerical measurements and is particularly useful for assessing the frequency and extent of specific events or outcomes (2). For instance, in a hospital's quality improvement project focused on reducing hospital-acquired infections, the team collects quantitative data on the number of infections over time, allowing them to track trends and measure the impact of interventions, such as hand hygiene protocols or disinfection practices.
- Qualitative Data: Qualitative data provides insights into the "why" and "how" behind healthcare processes and patient experiences (2). This data type is collected through interviews, focus groups, and open-ended surveys. For example, in a primary care setting aiming to improve patient satisfaction, qualitative data may be collected through patient interviews to gather in-depth information about their perceptions of care. Qualitative data can uncover nuances and provide valuable context to complement quantitative findings (2).
- Patient-Reported Data: Patient-reported data includes information directly provided by patients about their health, symptoms, experiences, and preferences. Patient-reported outcome measures (PROMs) and patient-reported experience measures (PREMs) are standard data collection tools. In a scenario involving chronic disease management, patients with diabetes may be asked to complete a PROM assessing their quality of life and symptom management. This data helps healthcare providers tailor care plans to individual patient needs and preferences (2).
- Process Data: Process data track the steps and activities involved in healthcare delivery to help assess the efficiency and effectiveness of care processes. For example, in a surgical quality improvement initiative, process data may include the time from patient admission to surgery, surgical team checklist completion, and adherence to anesthesia protocols. By collecting and analyzing process data, healthcare organizations can identify bottlenecks and areas for improvement in care delivery processes.
In summary, quality improvement data collection relies on various data types, including quantitative, qualitative, patient-reported, and processed data. Each data type contributes to a comprehensive understanding of healthcare quality and supports evidence-based decision-making to enhance patient care and outcomes.

Identification Stage
The identification stage for quality improvement data collection is a critical initial phase where healthcare organizations and teams define what data to collect, why it is relevant, and how it aligns with their quality improvement goals (23). This stage is essential for ensuring meaningful data collection efforts will lead to actionable insights. Let's explore the identification stage in more detail.
- Defining Objectives and Goals: During this stage, healthcare organizations must clearly define the objectives and goals of their quality improvement initiative (23). For instance, a hospital aiming to reduce readmission rates for heart failure patients may set a specific goal of reducing readmissions by 20% within the following year.
- Selecting Relevant Metrics: Identifying the right metrics and data points is crucial, and organizations should choose metrics that directly relate to their quality improvement goals (23). Continuing with the example of reducing heart failure readmissions, relevant metrics might include the number of heart failure patients readmitted within 30 days, the reasons for readmission, and patient characteristics. By selecting these metrics, the organization ensures that data collection efforts are aligned with their specific improvement goal.
- Determining Data Sources: Healthcare organizations must identify where the necessary data will be sourced (23). This may involve looking at electronic health records, claims data, patient surveys, or other sources. For instance, to collect data on heart failure readmissions, the hospital may extract relevant information from electronic health records, including admission and discharge dates, diagnosis codes, and patient demographics.
- Creating Data Collection Protocols: Establishing clear data collection protocols is essential for consistency and reliability (23). Healthcare teams should define how data will be collected, who will be responsible for data collection, and the frequency of data collection. For example, in a hospital project aiming to improve hand hygiene compliance, data collection protocols might specify that trained observers will monitor hand hygiene practices at random intervals and record their findings on standardized forms.
By carefully navigating the identification stage, healthcare organizations ensure that their quality improvement data collection efforts are purposeful and aligned with their goals. This sets the stage for collecting meaningful data to drive evidence-based decisions and interventions to enhance healthcare quality.
Gathering Stage
The gathering stage of quality improvement data collection is crucial for healthcare organizations to collect the identified data based on their quality improvement objectives and goals (23). This stage involves systematically collecting data from various sources and often requires careful planning and coordination to ensure data accuracy and completeness. Let's delve into the gathering stage in detail below.
- Data Collection Methods: To gather data, healthcare organizations must determine the most suitable methods for collecting the identified data, which may involve a combination of electronic health records, patient surveys, direct observations, and administrative databases (23). For example, in a quality improvement project aimed at reducing hospital readmissions, data may be collected by reviewing electronic health records to track patient outcomes, conducting patient surveys to gather feedback on discharge instructions, and analyzing administrative data to identify trends in readmission rates.
- Ensuring Data Accuracy and Consistency: Data accuracy is critical in the gathering stage, and organizations must implement procedures to collect data consistently and without errors (23). For instance, if a healthcare facility is collecting data on medication administration, nurses may use standardized protocols to accurately record medication administration times and doses. Regular training and quality checks may also be implemented to maintain data accuracy.
- Timely Data Collection: Timeliness is another important aspect of the gathering stage, and data should be collected promptly to ensure it is current and relevant for analysis and decision-making (23). In a scenario involving tracking patient outcomes, healthcare teams may set specific intervals for data collection, such as collecting post-surgical complication data daily or weekly, depending on the project's requirements.
- Data Security and Privacy: Protecting patient data is a paramount concern in healthcare. As a result, healthcare organizations must adhere to strict privacy and security protocols during the gathering stage to ensure that patient information is handled confidentially and complies with applicable laws and regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) (23). For example, when collecting patient-reported data, organizations may anonymize responses to protect patient identities and comply with privacy regulations.
By effectively managing the gathering stage, healthcare organizations can ensure that they collect accurate, timely, and secure data that will serve as the foundation for subsequent analysis and quality improvement efforts.
Analysis stage
The analysis stage for quality improvement data collection is a critical phase where collected data is processed, examined, and transformed into actionable insights. This stage involves various analytical techniques and tools to identify patterns, trends, and areas for improvement (2). Let's explore the analysis stage in detail below.
- Descriptive Analysis: Descriptive analysis is the initial step in data analysis, focusing on summarizing and presenting data meaningfully (2). For example, in a quality improvement project aimed at reducing patient wait times in an emergency department, an analysis may involve calculating and displaying key statistics, such as average wait times, 95th percentile wait times, and the distribution of wait times (2). These descriptive statistics provide an overview of the current situation and help identify areas that need attention.
- Root Cause Analysis (RCA): Root cause analysis is a critical aspect of the analysis stage, as it helps pinpoint the underlying causes of issues or problems (2). In our scenario, if the analysis reveals prolonged wait times in the emergency department, RCA may involve a thorough investigation into the factors contributing to the delays. Potential root causes include staffing shortages, inefficient triage processes, or bottlenecks in diagnostic testing. Identifying these root causes is essential for developing effective interventions.
- Statistical Analysis: Statistical analysis plays a vital role in quality improvement by examining the relationships between variables and testing hypotheses (2). In reducing hospital readmissions, statistical analysis may be used to identify factors associated with readmission risk. For example, healthcare teams can use logistic regression to analyze patient data to determine which variables, such as comorbidities or medication adherence, are statistically significant predictors of readmission risk. This information can guide the development of targeted interventions for at-risk patients.
- Benchmarking: Benchmarking involves comparing an organization's performance data with industry standards or best practices to identify performance gaps (2). When a hospital is looking to improve patient satisfaction, benchmarking may involve comparing its patient satisfaction scores to those of similar hospitals or national averages. Identifying areas where the hospital falls behind benchmarks can inform strategies for improvement, such as implementing best practices from higher-performing institutions.
The analysis stage is critical for transforming raw data into actionable insights and understanding healthcare quality factors (2). Through descriptive analysis, root cause analysis, statistical techniques, and benchmarking, healthcare organizations can gain valuable insights that drive evidence-based decisions and interventions to improve care quality (6).
Benchmarking
The benchmarking stage in quality improvement data collection is a crucial phase where healthcare organizations compare their performance against established benchmarks or best practices (1). This gives healthcare organizations a clear understanding of their position relative to recognized standards and allows them to effectively identify areas for improvement, prioritize, and focus their improvement efforts (5). Let's delve into the benchmarking stage in detail below.
- Defining Benchmarks: In the benchmarking stage, healthcare organizations must define the benchmarks or standards against which they will measure their performance. These benchmarks can be internal (comparing current performance to historical data) or external (comparing to industry standards, best practices, or similar organizations) (1). For example, a primary care clinic seeking to improve appointment scheduling efficiency may choose to benchmark its appointment wait times against industry benchmarks for acceptable wait times.
- Collecting Comparative Data: Gathering data that allows for a meaningful comparison is critical in benchmarking, so healthcare organizations must collect data from relevant sources to measure their performance against the chosen benchmarks (1). Continuing with the appointment scheduling example, the clinic may collect data on the time it takes to schedule an appointment, the number of scheduling errors, and patient feedback. This data is then compared to industry benchmarks or best practices.
- Identifying Performance Gaps: The benchmarking process reveals gaps or disparities between an organization's performance and the benchmarks to highlight improvement areas (1). For instance, if the clinic discovers that its appointment wait times are significantly longer than industry benchmarks, this identifies a performance gap that needs to be addressed to enhance patient access and satisfaction.
- Developing Improvement Strategies: Healthcare organizations can develop targeted improvement strategies once performance gaps are identified. These strategies are based on evidence from the benchmarking process and aim to align performance with or exceed established benchmarks (1). In our scenario, the clinic may implement strategies such as optimizing appointment scheduling processes, enhancing staff training, or using technology to improve scheduling efficiency.


Self Quiz
Ask yourself...
- Why is data collection a crucial step in the quality improvement process?
- What types of data are typically collected during the data collection stage of quality improvement?
- How do you determine which data points are relevant to your quality improvement project?
- What methods and tools can be used to collect data accurately and efficiently?
Change Models in Healthcare
Change models are essential frameworks used in healthcare, including nursing, to guide and manage the effective implementation of quality improvement initiatives (15). These models offer structured approaches to initiate, plan, execute, and sustain changes in healthcare practice (15). Let’s discuss some prominent change models used in nursing quality improvement below.
- Kotter's 8-Step Change Model: Developed by Dr. John Kotter, this model emphasizes the importance of creating a sense of urgency, building a guiding coalition, and sustaining the change (15). For instance, in a nursing scenario focused on reducing hospital-acquired infections, the 8-step model would involve creating urgency by highlighting the impact of infections on patient safety, assembling a coalition of nurses and infection control specialists, and sustaining change by monitoring infection rates over time and continually reinforcing hygiene protocols.
- Lewin's Change Management Model: Lewin's model consists of three stages: unfreezing, changing, and refreezing (15). Let's consider implementing a new electronic health record (EHR) system in nursing. Nurses first "unfreeze" by acknowledging the need for a new system and undergoing training. Then, they "change" by adopting the EHR and adjusting workflows. Finally, they "refreeze" by becoming proficient and maintaining the new system's use as a standard practice.
- PDSA Cycle (Plan-Do-Study-Act): This model emphasizes iterative cycles of planning, implementing, observing, and adjusting (15). For instance, if a nursing unit aims to improve patient handoffs, they might "plan" by identifying handoff best practices, "do" by implementing changes, "study" by assessing the impact on patient outcomes, and "act" by making further refinements based on their findings. This continuous cycle allows for gradual, data-driven improvements.
- ADKAR Model: The ADKAR model focuses on individual change management, and this could apply to a scenario where nurses are adopting new pain management protocols (15). Nurses would first need awareness of the change (A), followed by desire (D) to participate, knowledge (K) of how to implement the new protocols, ability (A) to do so, and reinforcement (R) to sustain the change over time.
In summary, change models provide structured approaches to drive quality improvement initiatives in nursing, and by applying these models, nurses and healthcare organizations can systematically plan, implement, and evaluate changes to enhance patient care, safety, and outcomes (15).

Self Quiz
Ask yourself...
- Why are change models essential in nursing quality improvement initiatives?
- What is the primary purpose of creating a sense of urgency in change models like Kotter's 8-Step model?
- How does Lewin's Change Management Model address the need to "unfreeze" existing practices in nursing before implementing change?
- Why is individual change management crucial in nursing practice, as the ADKAR model emphasizes?
Implementing Change
Implementing changes for quality improvement in nursing is a multifaceted process that requires careful planning, effective communication, and the engagement of healthcare professionals at all levels. According to (15), successful implementation ensures that desired changes are integrated into daily nursing practice, improving patient outcomes. Let’s explore key strategies and considerations for implementing changes in nursing quality improvement below.
- Engage Interdisciplinary Teams: According to (15), collaborative engagement is crucial when implementing changes in nursing practice, and healthcare organizations should assemble interdisciplinary teams that include nurses, physicians, administrators, and other stakeholders. For example, in a scenario involving the adoption of a new pain management protocol, nurses can collaborate with physicians to ensure the consistent application of evidence-based pain management practices. This team approach facilitates a shared understanding of the change and fosters buy-in from all parties.
- Effective Communication: Clear and consistent communication is essential during the implementation phase, so nurses should communicate the rationale behind the change, its expected benefits, and the specific steps involved (15). For example, suppose a hospital is transitioning to a new electronic health record system. In that case, nurses can attend training sessions to understand its features and communicate effectively with patients about how it will enhance their care. This ensures that all stakeholders are informed and can adapt to the change seamlessly.
- Training and Education: Providing adequate training and education is critical to equip nursing staff with the knowledge and skills to implement the change effectively (15). In the case of introducing a new wound care protocol, nurses would require training on the updated practices, wound assessment techniques, and the use of new wound care products. In addition to initial training, ongoing education would ensure that nursing staff stay current with best practices to provide quality care confidently.
- Continuous Monitoring and Feedback: According to (15), implementing change is an ongoing process that requires constant monitoring and feedback since feedback mechanisms allow for adjustments and refinements to the change process. As a result, nursing quality improvement initiatives benefit from the regular collection and analysis of data to assess the impact of the change. For example, suppose a hospital introduces a sepsis screening tool. In that case, nurses can track the number of patients screened, identify missed cases, and evaluate whether early interventions have reduced sepsis-related mortality rates. By engaging interdisciplinary teams, fostering effective communication, providing training and education, and implementing continuous monitoring and feedback mechanisms, nurses can successfully implement changes that improve the quality of patient care and enhance overall healthcare outcomes (8).

Self Quiz
Ask yourself...
- Why is it crucial for nursing teams to engage in interdisciplinary collaboration when implementing changes for quality improvement?
- How can effective communication strategies help nursing staff understand the purpose and benefits of a proposed change in healthcare practice?
- What role does ongoing training and education play in ensuring that nursing staff are well-prepared to implement and sustain changes in their practice?
- What methods can be employed to gather feedback from nursing staff while implementing a new practice or protocol?
Evaluating Change
Evaluating change for quality improvement in nursing is a critical phase that involves assessing the impact and effectiveness of implemented changes on patient care outcomes, safety, and the overall quality of healthcare services. According to (15), rigorous evaluation ensures that improvements are sustained, and necessary adjustments are made. Let’s explore key strategies and considerations for evaluating changes in nursing quality improvement below.
- Establishing Clear Evaluation Metrics: To evaluate change effectively, it is essential to define clear and measurable evaluation metrics, and according to (15), these metrics should align with the specific objectives of the change initiative. For example, suppose a nursing unit has introduced a new hand hygiene protocol to reduce hospital-acquired infections. In that case, evaluation metrics may include the number of infections before and after the change, adherence to hand hygiene guidelines, and patient satisfaction scores related to cleanliness and infection prevention.
- Data Collection and Analysis: Data collection is a fundamental component of the evaluation process, and nursing teams should collect relevant data using standardized methods and tools (15). In our scenario, data on infection rates can be collected regularly, and statistical analysis can be performed to determine whether the change has had a statistically significant impact. Nurses can then use run charts or control charts to visualize trends in infection rates over time, allowing for early detection of any potential issues.
- Patient and Staff Feedback: Patient and nursing staff feedback is invaluable in evaluating change since patients' perspectives on the quality of care and their experiences following the change can provide insights into the initiative's effectiveness (15). Additionally, nursing staff can provide feedback on the practicality and feasibility of the new practices. For instance, nursing staff may suggest further improvements in infection control procedures.
- Sustainability and Continuous Improvement: Evaluating change is not solely about assessing immediate outcomes but also ensuring sustainability and continuous improvement. According to (15), nursing teams should determine whether the positive effects of the change are maintained over time and whether there is room for further refinement. For example, when a nursing unit has reduced infection rates, regular audits and monitoring should continue to ensure sustained compliance with hygiene protocols.

Self Quiz
Ask yourself...
- Why must nursing teams establish clear and measurable evaluation metrics when assessing the impact of change in healthcare practice?
- How can nurses effectively collect and analyze data to evaluate the success of a change in their nursing practice?
- What role does patient feedback play in evaluating the impact of a change on the quality of nursing care, and how can this feedback be gathered and utilized?
- How can nursing staff engage in ongoing self-assessment to determine their practice changes' effectiveness and identify improvement areas?
- What specific infection prevention measures should nurses prioritize in their daily practice to reduce hospital-acquired infections, and why are these measures effective?
- What are the primary goals of a quality improvement project to reduce hospital-acquired infections, and how can nursing staff contribute to achieving these goals?
- Why is continuous monitoring and evaluation crucial in quality improvement projects, and how can nursing staff use data to drive ongoing improvements in patient care quality?

Self Quiz
Ask yourself...
- What specific infection prevention measures should nurses prioritize in their daily practice to reduce hospital-acquired infections, and why are these measures effective?
- What are the primary goals of a quality improvement project to reduce hospital-acquired infections, and how can nursing staff contribute to achieving these goals?
- Why is continuous monitoring and evaluation crucial in quality improvement projects, and how can nursing staff use data to drive ongoing improvements in patient care quality?
- Enhancing Medication Safety: Medication errors can have severe consequences for patients (6). A quality improvement project may target medication safety by introducing barcode scanning systems for medication administration, implementing double-check procedures for high-risk medications, and providing ongoing training to nursing staff. The project's effectiveness can be assessed by monitoring the number of medication errors reported and verifying that the new safety measures reduce the occurrence of such errors. For example, a nursing team could reduce the incidence of wrong-patient medication administration by implementing barcode scanning during medication administration.

Self Quiz
Ask yourself...
- How can nurses ensure that barcode scanning systems and double-check procedures are effectively integrated into their daily workflow in medication safety improvement projects?
- What potential challenges and barriers can nurse units encounter when implementing medication safety improvements, and how can these challenges be addressed?
- Improving Nurse-to-Patient Ratios: Adequate nurse staffing levels are crucial for patient safety and quality of care (6). A quality improvement project may involve adjusting nurse-to-patient ratios based on patient acuity levels, introducing workload management tools, and conducting regular staffing needs assessments. In this case, the project's success can be measured by tracking patient outcomes, nurse workload, and patient satisfaction scores. For example, a nursing unit could reduce nurse burnout and improve patient care by optimizing staffing ratios during peak hours.

Self Quiz
Ask yourself...
- Why is it important to regularly assess and adjust nurse-to-patient ratios in a healthcare setting, and what strategies can nurse leaders employ to optimize staffing levels?
- In a quality improvement project focused on nurse-to-patient ratios, what key factors should nurse leaders consider when determining staffing needs during different shifts and patient acuity levels?
- Enhancing Discharge Planning and Care Transitions: Effective care transitions from the hospital to home or other healthcare settings are essential to preventing readmissions and ensuring continuity of care (6). A quality improvement project may focus on improving the discharge planning process, including patient education, medication reconciliation, and post-discharge follow-up. Success can be assessed by monitoring readmission rates and patient-reported experiences. For example, a nursing team could work on reducing hospital readmissions by ensuring that patients receive thorough discharge instructions and have access to follow-up care.

Self Quiz
Ask yourself...
- What steps can nurse teams take to enhance the discharge planning process and ensure seamless care transitions for patients moving from the hospital to home care?
- What strategies can nurse teams employ to ensure that patient education during discharge planning is effective and leads to better patient outcomes and satisfaction?
The above examples illustrate the diverse range of quality improvement projects in nursing, each addressing specific challenges to enhance patient safety and care quality.

Self Quiz
Ask yourself...
- Why is continuous monitoring and evaluation crucial in quality improvement projects, and how can nursing staff use data to drive ongoing improvements in patient care quality?
- What are the primary goals and objectives of QI models, and how do they contribute to the overall quality of healthcare?
Conclusion
In conclusion, this course provides essential knowledge and skills valuable for nurses aiming to deliver high-quality, safe, patient-centered care. Quality improvement in nursing is not merely a theoretical concept but a practical approach that can be applied to various aspects of healthcare, and one critical aspect to remember is the importance of interdisciplinary collaboration. As frontline caregivers, nurses must collaborate with physicians, administrators, pharmacists, and other healthcare professionals to drive improvements in healthcare delivery.
As nurses continue to play a pivotal role in healthcare delivery, the knowledge and skills gained from this course will empower them to lead and actively participate in quality improvement initiatives. By applying quality improvement principles, nurses can contribute to better patient experiences, patient outcomes, and overall healthcare quality.
Final Reflection Questions
- What have you learned from this course?
- Why is interdisciplinary collaboration essential for nurses to effectively implement quality improvement initiatives in healthcare settings, and how can nurses foster collaboration among healthcare professionals?
- How does the concept of continuous learning and adaptation align with the dynamic nature of healthcare, and what strategies can nurses employ to stay current with evolving best practices and guidelines?
- In what ways does Quality Improvement benefit both healthcare providers and patients?
- What are the potential challenges in implementing QI initiatives in a healthcare organization?
- In what ways has QI in healthcare become intertwined with the broader goals of healthcare reform, such as improving patient outcomes and reducing healthcare costs?
- What role does leadership play in the effective implementation of QI models?
- How can leaders promote a culture of continuous improvement within healthcare organizations?
- How do QI models facilitate interdisciplinary collaboration among healthcare professionals to drive improvements in patient care?
- What challenges might healthcare organizations face when attempting to adopt and sustain QI models, and how can these challenges be overcome?
- How does the "testing and learning" concept in the PDSA cycle align with the principles of evidence-based practice in healthcare?
- In what ways do QI models promote patient-centered care and patient safety, and can you provide examples of tangible improvements in these areas achieved through QI initiatives?
- How can the Six Sigma model contribute to the reliability and consistency of healthcare processes?
- Safe: What steps can healthcare organizations take to minimize the risk of medical errors and adverse events?
- Practical: How do healthcare providers ensure that evidence-based treatments and interventions lead to positive patient outcomes?
- Patient-centered: Why is it important to involve patients in their care decisions, and how can healthcare professionals effectively engage patients in the decision-making process?
- Timely: What are some key factors contributing to delays in healthcare delivery, and how can these delays be reduced to improve timeliness?
- Efficient: How can healthcare processes and workflows be streamlined to enhance efficiency and reduce waste?
- Equitable: What are some barriers to achieving healthcare equity, and how can healthcare organizations address these disparities?
- How can nurses actively involve patients in data collection to enhance patient-centered care?
- What tools or technologies are available to streamline data collection processes in nursing practice?
- How can nurses effectively collaborate with interdisciplinary teams to gather comprehensive data for quality improvement initiatives?
- What strategies can nurses employ to maintain patient privacy and confidentiality while collecting sensitive healthcare data?
- What methods can nurse use to analyze and interpret the data they collect to identify areas for improvement?
- Why must nurses regularly review and assess the data they collect to drive continuous quality improvement in healthcare settings?
- Regarding patient falls, what strategies can healthcare organizations implement to reduce the incidence of patient falls, and how can nursing staff actively contribute to fall prevention efforts?
- How can nurses ensure the accurate and safe administration of medications, and what measures can be taken to minimize medication errors?
- What are the key nursing practices and interventions that can prevent the development of pressure ulcers in hospitalized patients, and how can nursing staff collaborate to achieve this goal?
- Why is patient satisfaction an important nursing quality indicator, and what actions can nurses take to enhance the overall patient experience?
- What impact do nurse-to-patient staffing ratios have on the quality of nursing care, and how can healthcare organizations ensure safe nurse staffing levels?
- How can nurses enhance patient education to promote better understanding and self-management of their health conditions?
- How can you ensure that the data collected is reliable and valid?
- What role does standardization play in data collection for quality improvement?
- How can you establish baseline data for comparison in your quality improvement project?
- What challenges or obstacles might you encounter when collecting data for quality improvement?
- How frequently should data be collected to monitor progress in a quality improvement project?
- How can you involve frontline staff in the data collection to ensure accuracy?
- What measures can be taken to protect patient privacy and confidentiality during data collection?
- How can you analyze the data collected to identify trends or patterns?
- What actions should be taken if the data collected indicates a problem or deviation from the desired outcome?
- What strategies can ensure that data collection remains an ongoing and sustainable practice in healthcare quality improvement efforts?
- What are the potential challenges or resistance nurses might encounter when implementing changes using these models?
- How can a guiding coalition or interdisciplinary team be effectively assembled to support nursing quality improvement efforts?
- What strategies can nurses employ to sustain changes and prevent reverting to previous practices once implemented?
- How can nursing leaders ensure that staff have the necessary knowledge and skills to embrace the changes outlined in these models?
- How can nurses use these change models to promote a culture of continuous improvement in healthcare settings?
- How can nurses ensure their implementation changes align with evidence-based best practices and clinical guidelines?
- What potential challenges or barriers might nurse teams encounter when trying to implement changes for quality improvement?
- What strategies can address resistance to change among nursing staff and promote their active participation in the implementation process?
- How can nursing leaders effectively communicate the expected outcomes and benefits of the change to gain support and commitment from their teams?
- What are the advantages of using data and performance metrics to monitor the progress and impact of change implementation in nursing practice?
- How can nursing staff ensure that changes are sustained and become integral to their daily practice rather than temporary modifications?
- Why is it crucial to consider the sustainability of change when evaluating its long-term impact on nursing quality improvement?
- What challenges or obstacles might nurse teams encounter when collecting and analyzing data for change evaluation, and how can these challenges be addressed?
- How can nursing leaders encourage a culture of continuous improvement among their teams as part of the change evaluation process?
- What strategies can be employed to ensure that the feedback and insights gathered during the evaluation phase are actively used to refine and optimize nursing practices?
- What are the potential consequences of not conducting thorough and systematic evaluations of changes in nursing practice for quality improvement?
- How can nursing staff and healthcare organizations ensure that the lessons learned from change evaluations are applied to future improvement initiatives to enhance patient care outcomes?
Workplace Violence Against Nurses
Introduction
The role of the registered nurse, while fundamentally dedicated to the care and wellbeing of patients, has long been fraught with challenges that extend beyond the complexities of medical care. One such pressing concern is workplace violence, an issue that nurses confront with alarming frequency. Recent statistics show that healthcare workers, particularly nurses, are at a higher risk for workplace violence compared to other professions.
Given the vital role nurses play in patient care and the broader healthcare system, it is imperative to understand the scope, sources, and solutions to this pressing issue. This continuing education course is dedicated to arming nurses with the knowledge, tools, and strategies to recognize, respond to, and prevent incidents of workplace violence, thereby ensuring their safety and the uninterrupted provision of quality care.
Introduction
The role of the registered nurse, while fundamentally dedicated to the care and wellbeing of patients, has long been fraught with challenges that extend beyond the complexities of medical care. One such pressing concern is workplace violence, an issue that nurses confront with alarming frequency. Recent statistics show that healthcare workers, particularly nurses, are at a higher risk for workplace violence compared to other professions.
Given the vital role nurses play in patient care and the broader healthcare system, it is imperative to understand the scope, sources, and solutions to this pressing issue. This continuing education course is dedicated to arming nurses with the knowledge, tools, and strategies to recognize, respond to, and prevent incidents of workplace violence, thereby ensuring their safety and the uninterrupted provision of quality care.
Workplace Violence
Definitions
The Occupational and Safety Health Administration (OSHA) (3) defines workplace violence (WPV for the purpose of this course) as any act or threat of physical violence, harassment, intimidation, or other threatening, disruptive behavior that occurs at the work site. This can also include verbal, written, or acts of sabotage against an individual while they are at work.
Workplace violence crosses all demographic barriers and is indiscriminate in who it can and does affect. Even seeing workplace violence influences morale, attendance, and the overall well-being of employees and their co-workers.
Types of Violence
Currently, there are four categories of workplace violence according to the American Nurses Association (5).
1: Criminal Intent - normally involves theft from the business or employees.
Example: Carol is working on documentation and notices a person lingering in the hallway. Carol doesn’t really think anything of it, assuming they are family members of one of the patients. Several minutes later, the person exits quickly from the supply room and down the stairs. Carol calls security to let them know, but they can’t locate the individual. After looking through the supply room, they find that several containers of wound dressing supplies are missing.
2: Customer/client/patient - the individual becomes violent with employees while receiving services.
Example: David was updating a family on their father’s critical condition. David could tell the family was upset, but the patient’s son seemed more frustrated than the others. During David’s explanation, the son grabbed David’s clipboard and yelled, “You’re not doing anything! You’re just letting him die!” The son then threw the clipboard at David’s head. David blocked the clipboard with his arm, receiving a rather deep cut as a result. Security became involved, and David had to go to the ER for treatment.
3: Worker on worker - an employee bullies, attacks, or threatens another employee.
Example: Emily was rounding when Dr. G. came onto the floor. This doctor was well known for being difficult to work with, and he always required the nurses to stand behind him in the room while he talked with his patients. Emily had one of Dr. G.’s patients today and was in the room, he asked her if the patient had ambulated. Emily told him they had not, but they planned to before and after lunch. The doctor made an audible sigh and while shaking his head at the patient said, “See…this is what I deal with every day. These nurses can’t get anything right. They’re all useless.”
4: Personal relationship - involves a person who has an interpersonal relationship with the nurse, but no association with the nurse’s employer or the business.
Example: Rebecca was walking to her car after work. Halfway to her car, she noticed an individual leaning against the trunk of her vehicle. Rebecca recognized this person as the someone her friend was currently dating. This person approached Rebecca aggressively and began yelling about gossiping and trying to break their relationship. Rebecca started back toward the building, hoping security was nearby, and was pursued by the female. Eventually, Rebecca made it to the building and got inside. Luckily, the door only opened with an employee badge, and Rebecca was safe. She went ahead to security.
Currently, the customer/client type of workplace violence is the most prominent, especially in healthcare and toward nurses. The American Nurses Association (ANA) reports that OSHA does not require employers to implement workplace violence prevention programs, but it supplies voluntary guidelines and may cite employers for not supplying a workplace free from recognized serious hazards.
Some states have legislated that employers develop a program while most states have advanced laws that amend existing statute for assaults of first responders by adding health care providers / nurses and/or increasing the penalty associated with such behavior. (3)
It is worth noting that since there are, in most cases, no actual requirements for employers to provide safe work environments for nurses, preventing and dealing with WPV proves problematic. It falls on nurses to understand what constitutes WPV, how to manage it, how to cope with it, how to report it, and how to ensure action is taken and a resolution is reached when WPV occurs.

Self Quiz
Ask yourself...
- In the scenarios above, should the employees report these incidents to administration at once?
- How would you describe the earlier scenarios on workplace violence?
- Why is it important to ask how you would find and describe workplace violence?
- Can you provide any examples of workplace violence you have experienced or seen?
Epidemiology
Workplace violence can take many forms, and the possible varieties and scenarios are endless. Regardless of how it manifests, the effects of workplace violence are clear and widespread. It can affect productivity of employees, morale, attendance, turnover rates, quality of work, patient outcomes, and much more.
Workplace violence can affect and involve workers, clients, customers, and visitors. WPV ranges from threats and verbal abuse to physical assaults and even homicide. In 2010, the Bureau of Labor Statistics (BLS) data reported healthcare and social aid workers were the victims of approximately 11,370 assaults by persons; a greater than 13% increase over the number of such assaults reported in 2009 (10). Almost 19% of these assaults occurred in nursing and residential care facilities alone. Unfortunately, many more incidents probably go unreported (5).

Impact on Nurses Well-Being
Workplace violence can take a heavy toll on nurses. These tolls can be emotional, mental, and physical as well as short-term or long-term. The seriousness of these injuries can vary widely ranging from minor upset to permanent injury and in worst cases, even death. (13)
This harm doesn’t stop with the nurse. The effects of workplace violence may also include effects spanning the unit the nurse works on or even the entire facility. Low morale, reduced productivity, lack of trust in employers, and fear of going to work can be results of violent events occurring to even a single co-worker.
Workplace violence can also have a financial effect on nurses and their employers related to lost time at work from injury or callouts, costs of care for treatment related to the incident (physical and/or psychological), or even legal fees. (13)
Given that incidents of workplace violence are rapidly increasing, these impacts are expected to increase as well. It is easy to see how this harm is widespread and can potentially ripple outward into the nurse’s professional and personal life. The stress and harm do not stay at work, and can spread to the nurse’s family, social interactions, and more.

Self Quiz
Ask yourself...
- How far reaching do you think workplace violence is?
- Can you give some examples of how workplace violence has affected you or your co-workers?
- What are some examples of how workplace violence against someone else can affect you or the patients on your unit?
Barriers to Reporting
One way to combat workplace violence is knowledge of its existence, its nature, and its frequency. Unfortunately, there are many factors that either prevent or discourage nurses from coming forward with reports when they are the victims of WPV.
A study presented in a Chinese nursing journal surveyed 325 nurses. Of these nurses, 266 were spread across 165 hospitals, and these hospitals were in 72 cities.
A total of 172 nurses (64.7%) experienced violent incidents during the past year. Of these incidents, 45.5% were reported; and the reporting rate of physical assaults (69.0%) was higher than those of verbal abuse (36.9%), threatening behavior (51.7%), and sexual harassment (60.0%). Formal reporting accounted for 25.4% (15.4% in written form and 10.0% through a computer-assisted reporting system.
Almost half of the nurses (49.6%) said that the hospital had no reporting system, or they were uncertain about the reporting system. For reasons of not reporting, 51.9% of the nurses were unaware of how and what types of violence to report, and 50.6% of the nurses believed that the hospital paid greater attention to patients rather than staff. (7)
Interestingly, almost fifty percent of the nurses surveyed had limited knowledge, if any, of a reporting system available to them, while fifty percent felt the hospital favored the patients over their own employees. Combined with an actual or perceived lack of supervisory support, this encourages an environment where nurses feel powerless to protect themselves or to take proper action when threatened or harmed.
The Minnesota Nurses Association, in August of 2022, published a press release with the results of a nursing survey on the topic of workplace violence. In this survey, ninety-seven percent of the nurses surveyed observed WPV or harassment over the previous two years.
The top reasons cited by nurses who did not report workplace violence were lack of time due to overwork and under-staffing, cited by fifty-eight percent of respondents, and lack of action by hospital management, cited by fifty-three percent of nurses in the survey. (4)
It would appear from these studies that many nurses feel it is futile to report incidents of workplace violence they encounter, and even if they realized an incident was reportable, they may not be aware of a way to report it or have time to do it. This perceived powerlessness and sense of futility in the face of abuse and violence will only continue to worsen unless action is taken to remove barriers to reporting and for nurses to have access to aid and support for supervisory staff.

Self Quiz
Ask yourself...
- Can you think of any examples of when you or a co-worker tried to report an incident of workplace violence and were unable to?
- If so, what was the barrier that prevented you from reporting?
- Can you name three alternative ways to report workplace violence at your organization?
Culture of Safety
A commonly used phrase is “Culture of Safety”, but is there a standardized definition of what it is or could be? Many resources point to the safety of patients about medical errors, patient rights, and protecting the patient’s information, but few address the issue facing caregivers and especially nurses. However, there is no agreed-upon or standard definition of what exactly a “culture of safety” is or what it should look like.
The American Nurses Association approaches the concept by saying, “Establishing a culture of safety in health care is essential to the security and well-being of your patients, staff, and organization. Effective nurse leaders embrace safety protocols that ensure their organization delivers a secure, protective environment that prioritizes patients and caregivers.” (12)
Currently, there is only a single federal legislation in place about the issue.
The only federal regulation currently in place is the General Duty Clause of the Occupational Safety and Health Act of 1970. This clause requires employers to supply a work environment free from recognized hazards that are causing or likely to cause death or serious physical harm. However, the general duty clause offers no specific recommendations about management of workplace violence.
The Occupational Safety and Health Administration (OSHA) issued guidelines for workplace violence prevention for health care and social service workers. First issued in 1996 and later updated, the guidelines are only advisory. (1)
It is paramount that nurses and other direct care providers accept the responsibility of creating policies and procedures within their organizations to define and enforce a work environment where violence is not tolerated and dealt with accordingly.
There is currently a small body of research and work of the effects workplace violence has on nurses as human beings. Most of the evidence focuses on how workplace violence increases the risk nurses present to patients in the form of medical errors, staffing issues due to missed work, poor documentation, etc.
The main body of evidence discussing how workplace violence affects nurses is noted in research around nurse burnout. A 2020 study published by the National Health Institute (10) states, “Workplace aggression is a source of extreme socio-emotional stress, which may lead to the experience of psychological strain.
A large body of research shows that exposure to workplace aggression and violence may severely impair healthcare workers’ mental health, including symptoms of post-traumatic stress disorder, depression, and burnout.”
This study also shows an important association with workplace aggression and violence targeting nurses and drastically increased levels of emotional exhaustion, depersonalization, and deep feelings of poor personal accomplishment. Over time, these feelings lead to complete burnout, and even worse, possibly psychological and/or physical conditions in the nurse affected.
Even with this preliminary information and research, we still have a long way to go to show the full and far-reaching effects of workplace violence on nurses. Again, by being proactive and acting now, we as nurses can foster this research and bring to light the issues so they can be addressed.

Self Quiz
Ask yourself...
- How does your organization define a “culture of safety”?
- Do you agree with the definition?
- How would you define a “culture of safety” from your own perspective given your experiences and challenges?
ANA Zero Tolerance Policy
In 2019 the American Nurses Association (ANA) (2) release a brief titled “Reporting Incidents of Workplace Violence”. In it, they discussed several issues surrounding workplace violence, barriers to its reporting, and made recommendations to healthcare organizations on strategies relating to the issues of workplace violence.
They also set forth a “Zero Tolerance Policy on Workplace Violence”, which provided some definitions and several recommendations on how to deal with WPV.
The introduction to the “Culture of Safety” part of this brief is as follows:
By prioritizing, developing, and sustaining an organizational culture focused on safety, we can drive the future of healthcare to a place where patients and those who care for them are free from harm. It is not only one of many priorities but is the overriding ethical imperatives for all leaders. (9)
The ANA also suggested a three-level prevention strategy, each with a part for the employer and the employee. Essentially, the role of the employer is gathering data, providing a “safe” work environment, non-punitive reporting, and development of programs to provide a safe work environment for nurses. The employee’s role is to take part in the implementation and evaluation of said programs.
Unfortunately, these are only suggestions and employers do not have to implement any programs or services to protect employees against workplace violence. Also, healthcare employers do not have to report any incidents to JCAHO who consider events of workplace violence to be “sentinel events”.
In the end, it falls on the nurses and employees directly affected by WPV to assume the charge against workplace violence, hold employers accountable, communicate with local and state legislators, and effect change to protect themselves.

Self Quiz
Ask yourself...
- Considering the recommendations and guidelines set forth by these entities, do you think they are adequate or effective? Why nor why not?
- How has this information changed your perception of the overall reporting process on workplace violence against nurses?
- What generalizations can you make from this information on the reporting process from an employer perspective?
Strategies to Prevent Workplace Violence
To end nurse abuse for good, Boston-Leary says it takes every nurse speaking up and reporting abuse within an organizational culture that has an established process for allowing nurses to report abuse without fear of recrimination and then follows up with a resolution. (8)
There are some suggested actions to help prevent and combat workplace violence in your practice setting. These actions include:
Know the definition of abuse.
The National Institute for Occupational Safety and Health (NIOSH) defines workplace violence as “the act or threat of violence, ranging from verbal abuse to physical assaults directed toward persons at work or on duty.”
Agreeing on this definition is an important first step to achieving widespread acknowledgement of the distinct types of nurse abuse, particularly non-physical abuse, Boston-Leary explains. (8)
Report Abuse
Ask about how your workplace manages abuse reporting, whether it is in your current workplace or when you are applying for a position, Boston-Leary suggests. “Ask about how reporting abuse happens during any shift because there should be a reporting mechanism in place for everyone, even if it’s on a weekend or evening shift with no manager easily accessible to report to.”
If (when) you do experience abuse, it’s essential that you speak up immediately and note any witnesses who could corroborate your description of the incident, she says.
Even after you experience abuse and even if you didn’t report it, it’s important to share your past abuse with others to empower them to report abuse they experience. (8)
Change Your Culture
Join or meet a committee to build or strengthen zero-tolerance abuse policies. Based on ANA’s Zero Tolerance Policy on Workplace Violence, Boston-Leary suggests these crucial elements of a zero-tolerance abuse program:
Stop violence before it starts through education to find risks and reduce vulnerabilities for workplace violence.
Create an effective response to violence immediately after it occurs, including emergency care.
Establish long-term responses that reduce the long-term negative effects of workplace abuse. (8)
Communicate with your Legislator!
Congress was considering legislation to #End Nurse Abuse by passing The Workplace Violence Prevention for Health Care and Social Service Workers Act (H.R 1195). If approved, this law would have required health care and social service industry employers to develop and implement a comprehensive workplace violence prevention plan that protects nurses and other healthcare professionals from on-the-job abuse.
Boston-Leary believes legislators are very attuned to the trusted voice of nurses to share about what is happening in health care today (8).

Self Quiz
Ask yourself...
- What is your organization’s primary method of reporting abuse or violence against employees?
- Do you know who your local and state legislators are and how to contact them?
- Are you aware of any committees or groups within your organization that actively address the issue of workplace violence?
Nurse-led Strategies
You can join these committees or work with your employer to create them. Collaborating with your supervisory staff and HR, you can create workflows, policies, reporting methods, and provide education on prevention of workplace violence and make a difference in your overall work environment.
Regarding Your Legislators
As mentioned before, 2021 Congress was considering federal legislation to end nurse abuse by passing The Workplace Violence Prevention for Health Care and Social Service Workers Act (H.R. 1195). The bill was passed by the House on April 16, 2021, but was never passed by the Senate.
You can find your local and state legislator contact information very easily on the internet. A simple search for “how to find state legislator contact information” is a wonderful place to start. As a voting citizen, you have every right to contact them, and demand laws be created to protect you while you work.
Below are some links to help you find elected officials:
- https://www.usa.gov/elected-officials
- https://www.usa.gov/state-governor
- https://www.senate.gov/senators/senators-contact.htm
- https://www.house.gov/representatives/find-your-representative
Advocate for your own safety the same way you would for your patients!
As nurses we aren’t afraid of stepping up to bat for our patients when they need something, but we are notorious for taking a hit and letting it slide, sometimes even to our own detriment.
We owe it to ourselves to offer that same level of advocacy to ourselves and our co-workers.
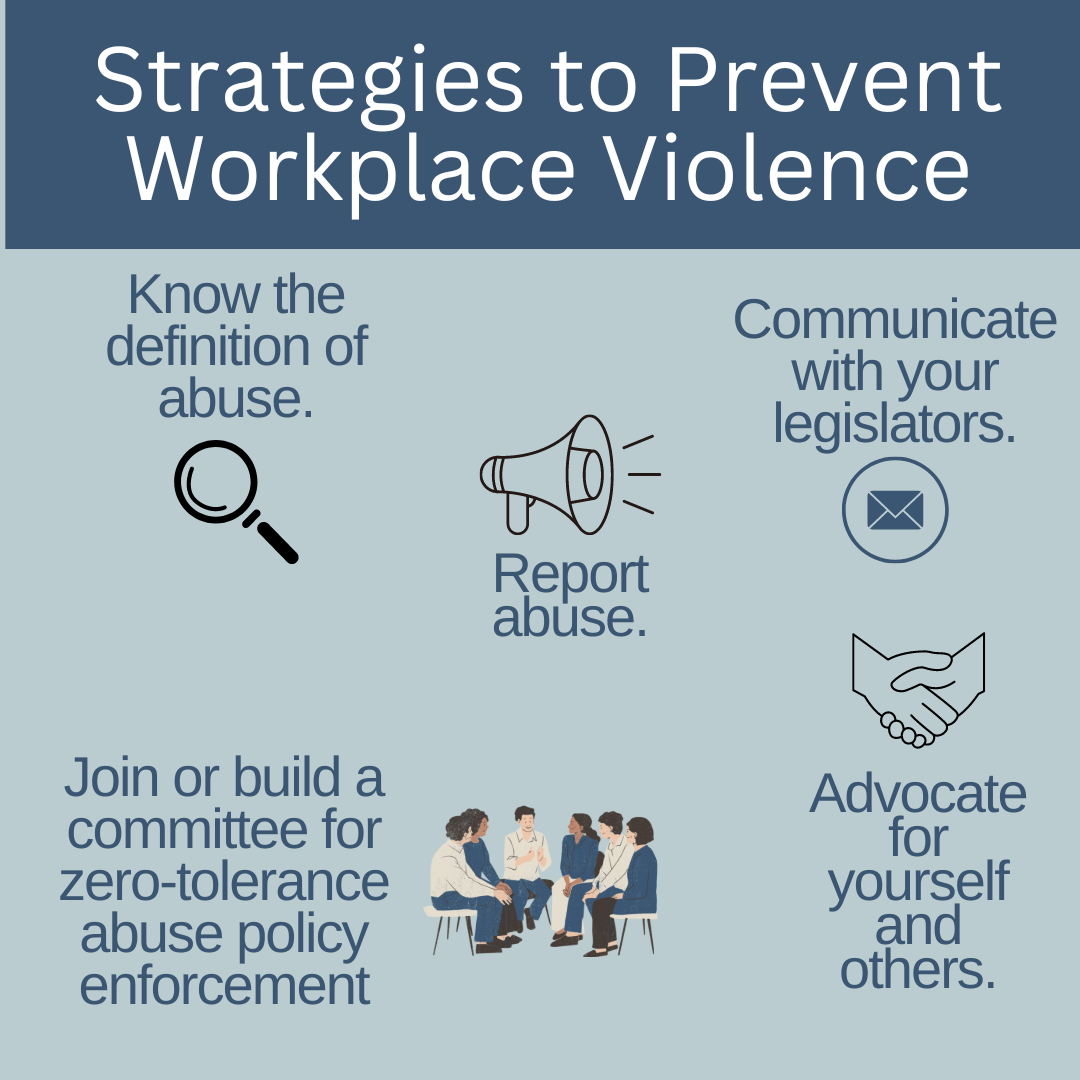

Self Quiz
Ask yourself...
- How can you become an advocate for yourself or your co-workers when it comes to workplace violence?
- Who is the contact in your organization for instances of workplace violence?
Resources
The Joint Commission supplies resources available to report and learn about how to report workplace violence. The links included are for federal, state, professional, and other resources. The direct link to this page is:
The Joint Commission: Workplace Violence Prevention Resources
Local law enforcement
As a private citizen, you are protected by laws about assault, battery, and other attacks on your person. You are within your rights to call the police on events of workplace violence, especially if your life or health are threatened, or you are physically attacked. It is likely your employer will not support you in this situation due to legal implications. It is best to ask your HR department and supervisory staff how these situations should be managed if they occur.
Legal Counsel
Consult with a lawyer about your legal rights in situations on workplace violence and how to best manage them. Be sure to bring scenarios, information on how your employer suggests dealing with these situations, and examples of violence you have seen or have experienced.
Educate and Train Yourself
Learn as much as you can about recognizing and managing workplace violence. Your employer may supply these courses, and if they don’t, it may be prudent to request them. Also, you can seek outside education and training on these topics including self-defense classes and crisis management courses.
Practice Self-Awareness
We all have inherent beliefs, perspectives, and feelings that can prevent us from acting in certain situations. Knowing yourself and understanding possible nuances within yourself that could be a detriment to you appropriately handling a situation of workplace violence could mean the difference between prevention and becoming a victim.

Self Quiz
Ask yourself...
- What training opportunities does your organization provide on management and follow-up for workplace violence?
- What information would you ask local law enforcement or a legal counsel for on workplace violence?
- What might someone who believes abuse against nurses is “just part of the job” do when they find themselves a victim of workplace violence?
- What can you do to help individuals that may simply allow workplace violence to affect their well-being?
Conclusion
Being an agent of change can be intimidating, terrifying, and even force us to deal with feelings and beliefs we didn’t even realize were in our way. Incidents of WPV have been rising sharply over the past several years, and there is no sign of slowing. It’s up to us as front-line workers, nurses, and co-workers to take responsibility for our own safety and work environment.
Through cooperation and consistency, we can create and bring solutions to the workplace and hopefully one day, aid in the creation of laws that make our jobs safer for us to supply the care and support our patients need. We owe it to ourselves to take the necessary steps to show our employers it’s time to address this issue. “Be the change you wish to see in the world.” ~Mahatma Gandhi –
Telemetry Basics - Rhythm Recognition
Introduction
To truly understand telemetry, nurses must have knowledge about the anatomy of the heart and how electricity passes through it, how the electrocardiograph (EKG) works to receive and record the electrical activity, and how this information is transmitted via telemetry to the appropriate receiving device.
Defined as the transmission of instrumental readings by various methods such as radio waves or wires, telemetry gathers and transmits EKG readings to a central or remote monitor for interpretation and storage (71). The ability to read EKG rhythms from a variety of monitors consists of more than looking at a rhythm strip and identifying the rhythm. It consists of knowing the anatomy of the heart, how electricity travels through it and translates into the EKG we know, and what changes can happen based on injury, electrolytes, or other causes.
Introduction
To truly understand telemetry, nurses must have knowledge about the anatomy of the heart and how electricity passes through it, how the electrocardiograph (EKG) works to receive and record the electrical activity, and how this information is transmitted via telemetry to the appropriate receiving device.
Defined as the transmission of instrumental readings by various methods such as radio waves or wires, telemetry gathers and transmits EKG readings to a central or remote monitor for interpretation and storage (71). The ability to read EKG rhythms from a variety of monitors consists of more than looking at a rhythm strip and identifying the rhythm. It consists of knowing the anatomy of the heart, how electricity travels through it and translates into the EKG we know, and what changes can happen based on injury, electrolytes, or other causes.
Heart Anatomy 101
As we know, the heart consists of four chambers, two atria—right atria (RA) and left atria (LA)—and two ventricles—right ventricle (RV) and left ventricle (LV)—working in a cycle to ensure adequate blood flow occurs. The heart receives blood from the inferior and superior vena cava (IVC and SVC) and enters the RA, moves to the RV, passes through the pulmonary artery (PA) and lungs, returns to the LA, enters the LV, and exits the heart through the aorta.
Heart cells, known as myocytes, are negatively charged, or “polarized” at rest. When these muscle cells contract, they become “depolarized” or positively charged. But how do the myocytes know when to contract? Less than 1% of the cells in the heart have a special role and name. These are known as the pacemaker cells and their role is to ensure that the heart beats. This is done through the action potential that is spontaneously created by the pacemaker cells. Some of these pacemaker cells have different speeds in depolarization, meaning that the fastest pacemaker cells are the ones controlling the speed. This will make more sense later when discussing specific cardiac rhythms (69).
Starting in the right atria, the sinoatrial node (SA node) is the primary group of pacemaker cells that determines the heart rhythm. The SA node, as well as the other pacemaker cells within the heart, progress through a rapid depolarization and repolarization process (2).
Pacemaker cells do not have a true resting potential, this means they are always in an “unstable” state to create spontaneous action potential. The action potential is the brief reversal of polarity in the cell; polarity consists of potassium (K+) in the cell with a negative charge, while sodium (Na+) and calcium (Ca++) are outside of the cell with a positive charge (2).
Starting at the beginning of the cardiac cycle the pacemaker cells always have a membrane potential or voltage—the voltage of the cellular membrane as a result of permeability and concentrations of ions inside and outside the cell—of -60 microvolts (mV). From -60mV to -50mV the channels within the cells open, leading to a slow influx of Na+ inside the cell and a slow depolarization of the cell. Once the membrane voltage has reached the minimum threshold of -50mV the Ca++ channels open, causing Ca++ to move into the cell. This is known as the rising depolarization phase. The membrane voltage reaches the peak and the next thing that happens is the falling repolarization phase. This is where the K+ channels open to return the cell to a repolarized state (2).
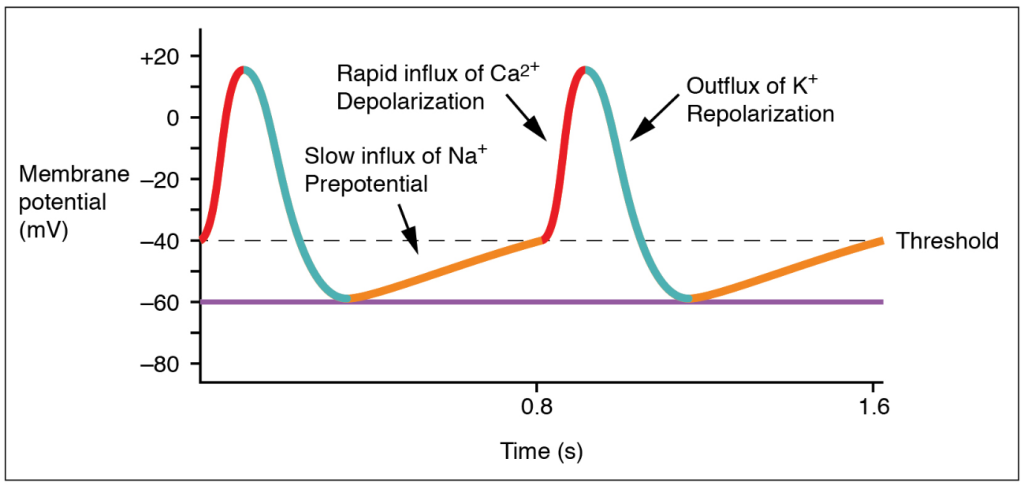
(20)
Once these steps have occurred, the energy is transferred to surrounding cells, and the cardiac cycle continues. However, the action potential in the other myocytes is slightly different. Myocytes have a resting potential, which is different from the pacemaker cells. The resting potential is around -90mV and these cells only start the depolarization process when stimulated by an external force. During the end of the pacemaker cell’s action potential phase, additional Ca++ is passed into the neighboring myocytes through gap junctions. The introduction of Ca++ into the cell causes a sharp rise in the membrane voltage that approaches the threshold which is -70mVs. Once that threshold has been reached, the NA+ fast channels open and a rapid depolarization occurs since Na+ is brought into the cell. The Ca++ slow channels open at -40mVs, further causing depolarization with Ca++ entering the cell (2).
At the peak of cellular depolarization, the Na+ channels close, leading to a slight repolarization through some K+ entering the cell. This is minor as the Ca++ channel is still open and continues to move K+ out of the cell. A plateau is created because of this and allows for the cell to go through two important phases. The first phase starts when the membrane voltage increases from the resting potential and continues until the plateau phase ends. This is known as the absolute refractory period and is where the myocytes relax before they can respond to additional stimuli. It prevents summation and tetanus which could lead to the heart not beating. The second phase is where additional Ca++ is pulled out of the sarcoplasmic reticulum (SR) to further push K+ out of the cell (2).
The phase ends when the Ca++ channel closes, extra Ca++ is sent back to the SR, and K+ is allowed back into the cell. The sodium/potassium pump allows Na+ to exit the cell, returning the cell to its resting potential. This rapid process occurs in every myocyte for the life of the cell. Pacemaker cells are the only cells that can generate a heartbeat. Impulses from the nervous system can increase or decrease the heart rate, but they are influencing the pacemaker cell to generate more beats, not creating them (2).
It is important to note that there are several sets of pacemaker cells within the heart. The SA node starts the process, but there are a few others spaced out along the electricity’s path to ensure that the atria and ventricles of the heart have time to fill and properly contract. The second set of pacemaker cells is the atrioventricular node (AV node) where a slight delay of 0.01-0.05 meters per second (m/s) happens to make sure that the ventricles fill up adequately. The bundle of His takes the electric impulse to the left and right bundle branches and from there, the Purkinje Fibers are triggered. These fibers have a speed of 2-4 m/s to provide enough force to eject the blood from the ventricles (69).
Correlating all of this back to telemetry, scientific development within the medical profession has allowed us to visualize this electrical activity and translate it into an effective method of diagnosing cardiac conditions such as abnormal heart rates or cell death.

Self Quiz
Ask yourself...
- Reflecting on what you know and what you have learned so far, what information would you consider important to know when it comes to reading EKGs or telemetry strips?
- What information, if any, was surprising to you in regard to the action potential of the pacemaker cells?
- Why do you think the pacemaker cells start with a voltage or an action potential?
Types of Telemetry
EKG
There are many ways to view cardiac rhythms now, however, the oldest method is the EKG. During the late 1700s, the Italian physician Luigi Galvani was experimenting with electricity and animal tissue. His experiments spanned at least three decades and inspired other physicians during and after his time. Using legs removed from the bodies of frogs, Galvani theorized that “animal electric fluid” enabled the muscles within the legs to move when touched by metals; according to him, this was “natural” fluid and not created as static electricity or friction is. He went on to theorize that the brain is an essential part of creating the “electric fluid” with nerves as the conductors (6).
Jumping forward to 1842, Doctor Carlo Matteucci made a significant contribution to EKGs. During his time researching electrical detection in animals, he discovered the electrical currents within the heart that accompany each heartbeat. Thirty-five years after Matteucci, Augustus Waller was able to use a capillary electrometer and electrodes to perform the first human EKG. These electrodes were placed on the chest and back of the participant and were vital in demonstrating there was electrical activity that preceded the contraction of the ventricles. William Bayliss and Edward Starling improved upon Waller’s research by using improved capillary electrometers to demonstrate triphasic cardiac electrical activity (1).
The Dutch physician most noted for creating the EKG known today was Doctor Willem Einthoven. He was inspired by Waller and those before him to improve the capillary electrometer, successfully identifying five deflections that were initially named ABCDE. Having to factor for inertia, Einthoven implemented mathematic correlation, resulting in the traditional EKG rhythm strips we use today with the letters PQRST depicted in the image below. Einthoven is also responsible for coining the word electrocardiogram or electrokardiogram in Dutch. This is where providers get the “k” in EKG from (1).
While Waller’s EKG utilized ten electrodes, Einthoven was able to condense that number to three, eliminating the right leg and the mouth electrodes. These three leads created Einthoven’s triangle; an important concept still used today and that will be discussed later. All of Einthoven's work resulted in him being awarded the Nobel Prize in Physiology and Medicine in 1924 (1).

Self Quiz
Ask yourself...
- What do you know of the history of the EKG and telemetry? Was there anything new you learned?
- What process of developing the EKG interested you the most? Why?
- Do you think there is more that can be done to improve EKG? If so, what do you think could be done?
Bedside Monitor
Emergency departments (ED), intensive care units (ICU), and other specialized areas that require continuous monitoring of a patient’s EKG and vital signs utilize various bedside monitors to ensure they are receiving accurate, real-time information on the patient. Cords are used to connect the patient to the monitor. The electrodes to display and document cardiac rhythm and heart rate are applied to patients in the standard 5 lead placement displayed in the below image. The vitals displayed on the monitor can also be displayed outside the room on a screen with multiple patients. Nurses, paramedics, or trained telemetry monitor technicians can watch many of these monitors at a time.
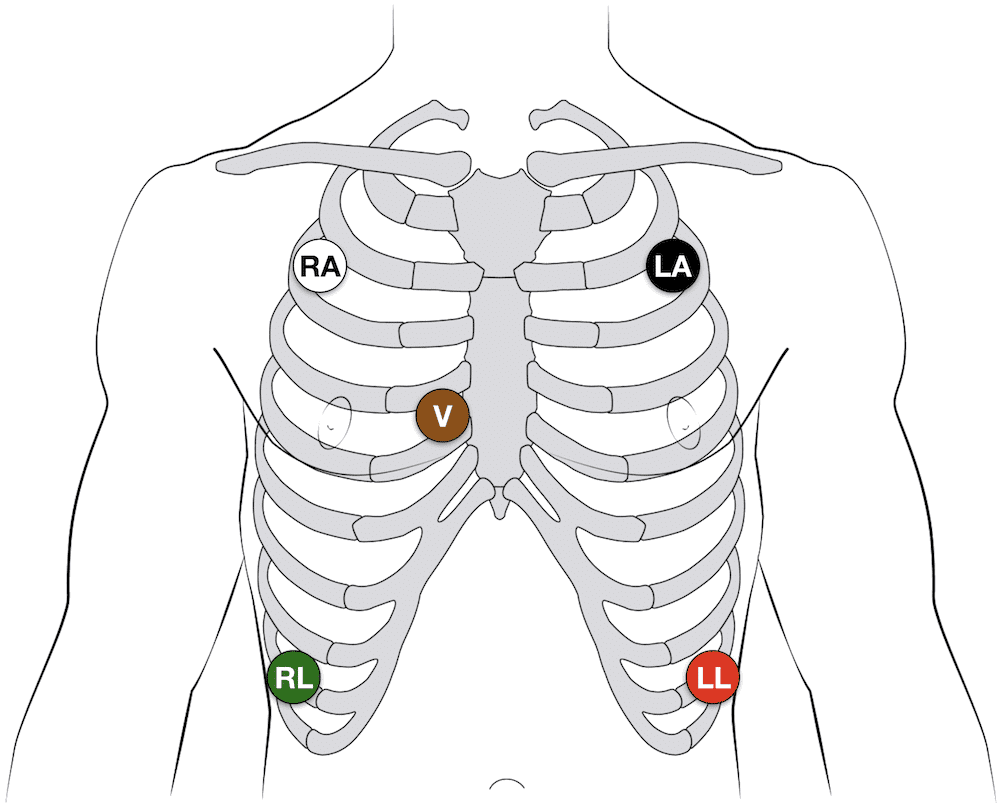
(14)
The placement of the five leads consists of the following:
- RA: 2nd intercostal space, anterior axillary on the right – some providers may put this lead higher on the chest or on the right arm
- LA: 2nd intercostal space, anterior axillary on the left – some providers may put this lead higher on the chest or on the left arm
- RL: 8th intercostal space, anterior axillary on the right – some providers may put this lead lower on the abdomen
- LL: 8th intercostal space, anterior axillary on the left – some providers may put this lead lower on the abdomen
- V: 4th intercostal space, right margin of the sternum
Note: Always follow the manufacturer’s instructions for specific lead placement.
Helpful Tip: Many healthcare providers quickly remember lead placement based on color is smoke (black) over fire (red) and snow (white) over grass (green). This leaves brown (chocolate) in the middle.
These bedside monitors can monitor pulse oximetry, respiratory rate, temperature, capnography, blood pressure, and arterial pressure. Some devices may have other unique monitoring features. These monitors may be portable or have a way to transfer the cords to a transport monitor. They come with alarms that can be adjusted based on the patient’s unique vital signs or hospital policy.
First responders have similar devices they use when transporting patients with the added benefit of having a defibrillator and a real-time feedback device built in (91).
Remote Monitoring
Remote cardiac monitoring is similar to bedside monitoring; however, the EKG rhythm, heart rate, and pulse oximetry are not displayed at the bedside. Instead, they are displayed in a different location, sometimes a monitor room, where a trained professional is watching many patients. When they recognize an abnormal rhythm, they will contact the appropriate staff to assess the patient. They may call for the leads to be removed, a change in rhythm, or a low battery.
The EKG leads are placed the same way as the bedside monitor leads are placed (always be sure to consult the manufacturer’s instructions). The information is transmitted wirelessly via wireless medical telemetry service (WMTS) from the “tele box,” but the leads must be wired to the box. WMTS does not use Wi-Fi and protects transmissions from Wi-Fi interference (48).
Mobile Cardiac Monitor and Event Monitor
A mobile cardiac or event monitor is a device attached to the skin that can perform continuous or event-specific monitoring. This device is attached to the patient’s chest near the heart and records when activated. This device is smaller than other portable cardiac monitoring devices like the Holter Monitor which will be discussed later. Information can be transmitted to the monitoring center to be reviewed by trained staff and/or artificial intelligence. Abnormalities like tachycardia, bradycardia, atrial fibrillation, or cardiac pauses are reported to a physician. The patient may or may not know about the rhythm abnormalities occurring as some patients are asymptomatic (18).
Event monitoring consists of the following methods (23):
- Patch monitor: depending on the manufacturer, the device is stuck to the chest and left on for a designated period of time.
- Loop memory monitor: the sensors always stay on the patient and the patient activates the devices to begin recording when symptoms occur in addition to a few minutes before the event starts and after it ends. There is an implanted option as well.
- Symptom event monitor: Patients place the monitor on them and activate it like a patch monitor, but only when symptoms start.
Insertable Monitor
Insertable or implantable cardiac monitors are just like mobile and event monitors, but they are surgically inserted into the patient. They perform the same actions, but there is an added benefit to these devices. If the patient has worn an external device in the past and has known cardiac arrhythmias, they may have an implanted cardioverter-defibrillator (ICD) inserted to detect and treat the abnormal rhythm. These devices are connected to the heart via wires (they may be placed in the right atria, the right ventricle, or both) and are operated by batteries that do need to be changed per manufacture direction. Patients and providers should be aware of magnets, or electrical signals from other devices that can interfere with the insertable device (61).
Healthcare providers can “interrogate” ICDs or pacemakers with a device created by the monitor’s manufacturer. When interrogated, the device’s information is transmitted to a monitor center who calls the provider to give them a verbal report of what the device has recorded; a paper copy is often faxed to the provider as well. Some newer interrogation devices may display the information of the device on the screen.
Holter Monitor
As mentioned with mobile cardiac monitors, the Holter monitor is another wearable device that can be used to monitor and diagnose cardiac arrhythmias outside of the hospital setting. This device consists of five electrodes and a monitor that the patient can wear or carry on them. It is similar to the remote telemetry devices used in the inpatient hospital setting as shown in the next image. Patients wear this device for a short time, and information is not transmitted to a monitor technician. Instead, information collected is sent to a monitoring center where it is interpreted and sent to the physician (58).
As covered in this section, there are many options for cardiac telemetry monitoring, and providers may encounter many types of them. It is important to know these devices and how they operate.

Self Quiz
Ask yourself...
- What types of telemetry/EKGs are you most familiar with? Which ones would you like to know more about?
- Are there any parts of the devices mentioned above that you have never heard of before?
- Out of all the devices which one do you like best? Which device do you not like?
- What devices do you think could be improved and how would you suggest improving them?
Lead Placement
Now that we have discussed the types of telemetry monitoring devices that are available, it is time to discuss how to properly place the EKG leads on a 12 lead, 15 lead, right-sided EKG, and where to place the V4R lead.
12 Lead EKG
For the 12 lead EKG, providers should start with the four limb leads (14):
- RA: On the upper or lower right arm
- LA: On the upper or lower left arm
- RL: on the upper or lower right leg
- LL: on the upper or lower left leg
From there, the six pericardial leads are placed strategically around the chest to create a partial circle around the heart (14):
- V1: 4th intercostal space, right margin of the sternum (this is lead V on the 5 lead EKG)
- V2: 4th intercostal space, left margin of the sternum
- V3: sits midway between leads V2 and V4 on the left
- V4: 5th intercostal space, mid-clavicular line on the left
- V5: 5th intercostal space, anterior axillary line on the left (aligned horizontally with V4, between V4 and V6) on the left
- V6: 5th intercostal space, mid-axillary line on the left (aligned horizontally with V4)
15 Lead EKG
The 15 lead EKG uses the same leads as the 12 lead EKG, but it adds V7, V8, and V9, known as the posterior leads, to encompass the posterior angles of the heart (14):
- V7: left posterior axillary line (aligned horizontally with V6, across from V5)
- V8: tip of the left scapula (aligned horizontally with V6, across from V4)
- V9: left of the spinal column (aligned horizontally with V6, across from V3)
Right Sided EKG
The right-sided EKG is important to rule out the diagnosis of a right-sided myocardial infarction (MI) or ischemia in or out while treating a patient. Lead placement is the same for the four limb leads, but the 6 precordial leads are flipped (14):
- V1: 4th intercostal space, left margin of the sternum
- V2: 4th intercostal space, right margin of the sternum (this is lead V on the 5 lead EKG)
- V3: sits midway between leads V2 and V4
- V4: 5th intercostal space, mid-clavicular line on the right
- V5: 5th intercostal space, anterior axillary line on the right (aligned horizontally with V4, between V4 and V6)
- V6: 5th intercostal space, mid-axillary line on the right (aligned horizontally with V4)
V4R Lead Placement
A full right-sided EKG is not always needed. Lead V4 on the right side of the heart is the most important lead when it comes to determining an MI on the right side of the heart (14):
- V1, V2, V3, V5, V6: same placement as the 12 and 15 lead EKGs.
- V4 is removed and placed on the right side of the chest
- V4R: 5th intercostal space, mid-clavicular line on the right (Where it is located on a complete right sided EKG)
- The “R” stands for right to ensure that those reading the EKG are aware that lead is on the right while the rest are located on the left side of the chest.
Limb Leads
Now that lead placement has been covered, we can now discuss how lead placement shows different parts of the heart.
Leads I, II, III, AVR, AVL, and AVF are considered limb leads when reading the EKG. It is important to note that the right leg lead is the grounding electrode and does not affect the EKG (83). Leads I, II, and III leads form a triangle over the chest known as Einthoven’s Triangle as reflected in the below image. Lead I always has negative polarity while lead III always has positive polarity. Lead II’s polarity depends on what side of the triangle is being discussed. If we are looking at lead I on the EKG, then lead II is positive, but if we are looking at lead III, then lead II is negative (82).
The importance of what leads are negative and positive comes from how electricity travels through the heart. It starts on the right side and moves to the left, so it would make sense for lead I to have negative polarity while leads II and III are positively charged (82). This is also why the height of a PQRST complex changes based on what lead is being looked at on an EKG as reflected below.
Augmented or unipolar leads AVR, AVL, and AVF have the heart as the negative electrode and the limb leads are the positive electrodes. AVR goes from the heart to the right arm lead, AVL goes from the heart to the left arm lead, and AVF goes from the heart to the left leg lead. Just as discussed with leads I, II, and III, the path of the electricity in the heart determines how the PQRST complex appears on the rhythm strip (82). Lead II is the preferred strip to read by providers due to the best view of the rhythm due to the way electricity travels through the heart and how lead II follows that path by starting at the right shoulder and going to the left leg.
The chest leads, V1 – V9, create a circle around the heart on a horizontal plane. These leads are unipolar as well, with the heart being the negative electrode. Multiple views of the heart are captured because of the many leads placed along the patient’s body. This can give providers valuable knowledge on what areas of the heart may be affected. The next image gives a visual depiction of how the leads display their view of the heart.
 (92)
(92)

Self Quiz
Ask yourself...
- What lead do you think is the most beneficial in reading EKGs? Why do you think that?
- What lead do you prefer to use when reading EKGs? What makes that your “go-to” lead?
- If you could make a policy on EKGs, would you include what type of EKG should be done on patients? Would all patients with chest pain get a 15 lead EKG instead of 12?
- Do you think that one type of EKG is better than the other? Or do they all have their specific uses and benefits?
Reading EKGs: EKG Components
To be able to interpret EKGs successfully, nurses must first have knowledge about the EKG components displayed on the EKG strips and how each part correlates to a part of a single heartbeat.
P wave
The P wave is the first deflection from the isoelectric line or baseline. Correlating this to the heart, this is where the atria depolarize or contract. The contraction of the right atria starts at the beginning of the P wave while the contraction of the left atria begins in the middle and end of it. Normal P waves are apparent between 120 and 200 milliseconds (msec) before the upward deflection of the QRS complex (44)
PR Interval
The next part of the PQRST complex is the PR interval. The interval symbolized the time between the depolarization of the atria and the depolarization of the ventricle. The normal speed is 120 to 200 msec (44).
PR Segment
Next is the PR segment. This is similar to the PR interval but starts at the end of the P wave and ends at the start of the Q wave. This line is important because if there is a deviation from the isoelectric line, it could indicate a cardiac rhythm abnormality like Wolff-Parkinson-White syndrome which will be discussed later. The EKG may have a “slurred” upstroke from the P to R points on the EKG, making the Q wave appear to be on the isoelectric line. This is because the ventricles were stimulated or excited early, leading to a shortened PR interval. The “slurred” area is known as a delta wave (13).
QRS Complex
The QRS complex is where the ventricles depolarize and contract. The first downward deflection of the beat is the Q wave that lasts for < 0.05 seconds. It is present in all leads save for V1 and V3 due to the angle of the vector. The R wave is the upward deflection of the complex. R waves do not have a set height, but severely elevated R waves can be an indicator of ventricular hypertrophy. The second downward deflection is the S wave. Overall, the QRS complex is 0.07 to 0.10 seconds long and variations to this time can be an indicator of abnormal heart rhythms (17).
ST Segment
The ST segment starts when the S wave ends by returning to the isoelectric line and ends when the T wave begins. This period represented the completion of ventricular depolarization (17). The ST segment lasts 0.08 seconds to 0.12 seconds (51).
T Wave
The final wave in the standard EKG components is the T wave. This wave symbolizes the ventricles repolarizing. Inverted T waves can be an indication of past or current infections. A peaked T wave—as opposed to the normal curved T wave—can be caused by hypocalcemia, hyperkalemia, and left ventricular hypertrophy (17). The T wave runs from 0.01 seconds to 0.25 seconds (51).
The image below depicts the components of an EKG with labels to assist with understanding how the waves appear.
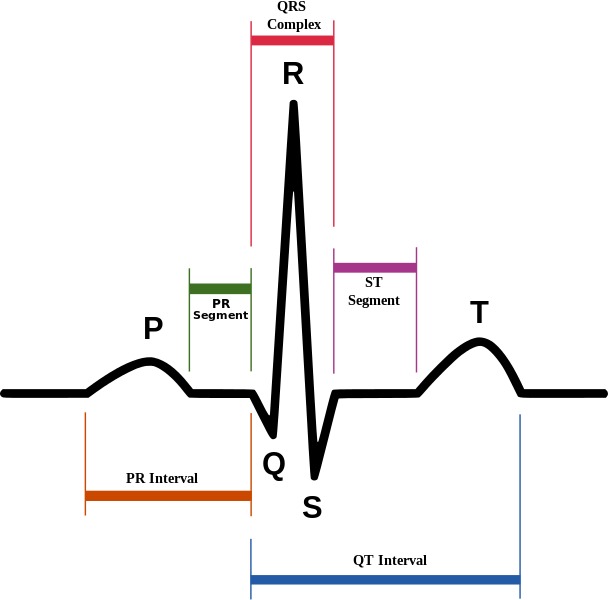
(4)
Reading EKGs: EKG Components
To be able to interpret EKGs successfully, nurses must first have knowledge about the EKG components displayed on the EKG strips and how each part correlates to a part of a single heartbeat.
P wave
The P wave is the first deflection from the isoelectric line or baseline. Correlating this to the heart, this is where the atria depolarize or contract. The contraction of the right atria starts at the beginning of the P wave while the contraction of the left atria begins in the middle and end of it. Normal P waves are apparent between 120 and 200 milliseconds (msec) before the upward deflection of the QRS complex (44)
PR Interval
The next part of the PQRST complex is the PR interval. The interval symbolized the time between the depolarization of the atria and the depolarization of the ventricle. The normal speed is 120 to 200 msec (44).
PR Segment
Next is the PR segment. This is similar to the PR interval but starts at the end of the P wave and ends at the start of the Q wave. This line is important because if there is a deviation from the isoelectric line, it could indicate a cardiac rhythm abnormality like Wolff-Parkinson-White syndrome which will be discussed later. The EKG may have a “slurred” upstroke from the P to R points on the EKG, making the Q wave appear to be on the isoelectric line. This is because the ventricles were stimulated or excited early, leading to a shortened PR interval. The “slurred” area is known as a delta wave (13).
QRS Complex
The QRS complex is where the ventricles depolarize and contract. The first downward deflection of the beat is the Q wave that lasts for < 0.05 seconds. It is present in all leads save for V1 and V3 due to the angle of the vector. The R wave is the upward deflection of the complex. R waves do not have a set height, but severely elevated R waves can be an indicator of ventricular hypertrophy. The second downward deflection is the S wave. Overall, the QRS complex is 0.07 to 0.10 seconds long and variations to this time can be an indicator of abnormal heart rhythms (17).
ST Segment
The ST segment starts when the S wave ends by returning to the isoelectric line and ends when the T wave begins. This period represented the completion of ventricular depolarization (17). The ST segment lasts 0.08 seconds to 0.12 seconds (51).
T Wave
The final wave in the standard EKG components is the T wave. This wave symbolizes the ventricles repolarizing. Inverted T waves can be an indication of past or current infections. A peaked T wave—as opposed to the normal curved T wave—can be caused by hypocalcemia, hyperkalemia, and left ventricular hypertrophy (17). The T wave runs from 0.01 seconds to 0.25 seconds (51).
The image below depicts the components of an EKG with labels to assist with understanding how the waves appear.
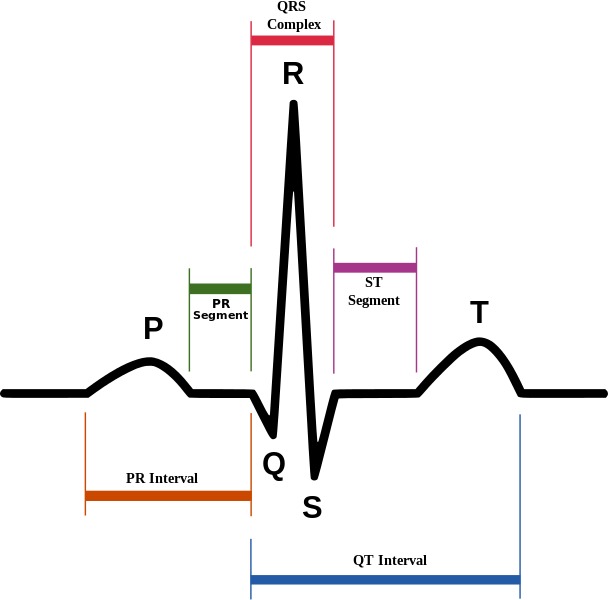
(4)
Reading EKGs: EKG Paper
The EKG paper has sets of squares, 25 little squares within one larger square. The smaller squares symbolize 0.04 seconds making the larger square 0.20 seconds. A single small square is 1mm while the large square is 5mm, this is because the larger square is five small squares tall.

(15)
Some EKG strips are presented in a six second format. To determine if the strip is a six-second, you must count the larger boxes. 30 larger boxes are required for the strip to be six seconds. Some may even have second markers that symbolize one second of time passed.
The 12 lead EKG can be more challenging to read and is often used to make an overall observation about the patient’s heart rate and rhythm. It can provide more information to providers than a single lead strip can.
As discussed previously, the leads are placed along the path of the heart, and providers can determine what part of the heart may be affected by knowing what leads are placed where.
| Lead | Location |
| II, III, AVF | Inferior |
| I, AVL, V5, V6 | Lateral |
| V2, V3, V4 | Anterior |
| V1, AVR | Right atrium, left ventricle |
(51)
Now that we have discussed leads, lead placement, the PQRST complex, and EKG paper, it is time to cover different cardiac rhythms that you may encounter.

Self Quiz
Ask yourself...
- What parts of the PQRST complex may not appear on the EKG strip?
- How do you remember what leads are associated with each part of the heart?
- What are some ways you can quickly determine heart rate using an EKG strip?
- Is there a part of the PQRST complex do you think is important to pay attention to? Why do you think that?
Rhythm Recognition
Normal Sinus (41):
- Rate: 60-100 beats per minute (bpm)
- Conduction:
- PR interval 120-200ms
- QRS width 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic (curves above and then dips below the isoelectric line) in V1
- Duration:
- Less than 0.12 seconds
- Rhythm Strip:
- The maximum height of the P wave is:
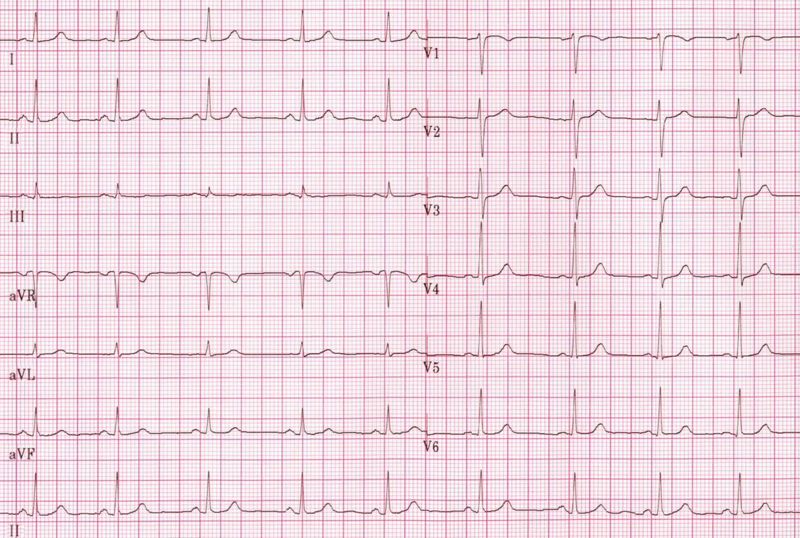
(29)
Sinus Bradycardia (87):
- Rate: less than 60bpm
- Conduction:
- PR interval 120-200ms
- QRS width 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- The maximum height of the P wave is:
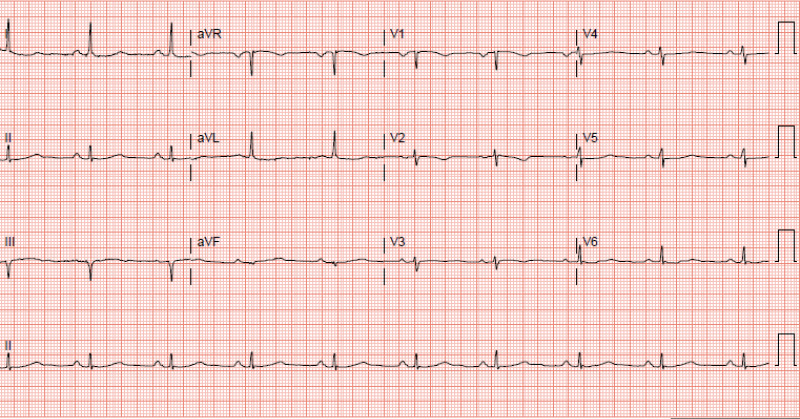
(87)
- Signs and Symptoms:
- None – depending on the patient
- Cyanosis
- Peripheral edema
- Shortness of breath
- Dizziness
- Fatigue
- Syncope or near syncope
- Lightheadedness
- Causes (not limited to):
- Normal physiology in an athlete
- Medications like beta-blockers
- Ischemia
- Heart diseases
- Sick sinus syndrome
- Hypothermia
- Hypothyroidism
- Neuro-mediated bradycardia as caused by a vasovagal reaction
- Pericarditis
- Hypoxia
- Electrolyte imbalances
- Treatment:
- None if asymptomatic, admission for observation may be indicated
- Medications:
- Atropine 0.5mg every 3 to 5 minutes for a maximum dose of 3mg
- Antidotes or reversal agents
- Transcutaneous cardiac pacing or pacemaker
- Return patient to a normothermic state if hypothermic
Sinus Tachycardia (55):
- Rate: greater than 100bpm but less than 150bpm
- Conduction:
- PR interval 120-200ms
- QRS width 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- The maximum height of the P wave is:
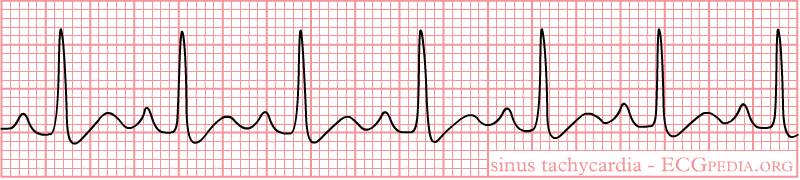
(42)
- Signs and Symptoms:
- Shortness of breath
- Chest pain
- Dizziness
- Syncope or near syncope
- Lightheadedness
- Palpitations
- Causes:
- Infection or sepsis
- Medications
- Withdrawal
- Electrolyte imbalances
- Blood loss or anemia
- Dehydration
- Hypoglycemia
- Pulmonary embolism
- Trauma
- Cardiac tamponade
- Myocarditis
- Pregnancy
- Treatment:
- Medications
- Antibiotics
- Antidotes or reversal agents
- Insulin
- Electrolyte replacement
- Fluids
- Heparin or other anticoagulant medications
- Blood replacement
- Surgery
- Medications

Self Quiz
Ask yourself...
- Looking at the signs and symptoms for sinus bradycardia what other signs and symptoms have you seen with patients who present with that heart rhythm?
- What other causes have you seen as the reason for sinus bradycardia?
- With sinus tachycardia, when would you be concerned with the causes of the rhythm?
- Are there any other treatments you could think of for either sinus bradycardia or tachycardia?
1st Degree AV Block (68):
- Rate: 60-100 beats per minute (bpm)
- Conduction:
- PR interval greater than 0.20 seconds
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- A QRS complex always follows the P wave
- The maximum height of the P wave is:
- Duration:
- Less than 0.12 seconds
- Rhythm Strip:
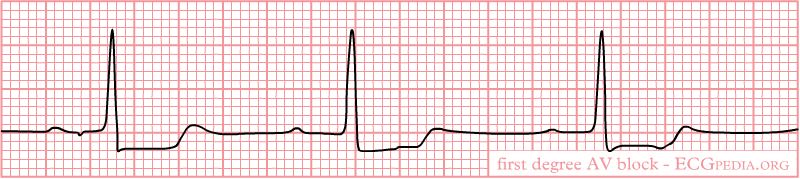
(32)
- Signs and Symptoms:
- None
- Fatigue
- Shortness of breath
- Syncope or near syncope
- Chest pain
- Lightheadedness
- Causes:
- Increased vagal tones in young patients
- Fibrotic changes in the elderly
- Cardiac disease
- Inflammation
- Medications
- Electrolyte abnormalities
- Treatment:
- None if asymptomatic
- Medications
- Antibiotics
- Antidotes or reversal agents
- Electrolyte replacement
2nd Degree Type I AV Block (Mobitz Type 1 or Wenckebach) (60):
- Rate: varies
- Conduction:
- PR interval increases with each beat, eventually “dropping off” and another P wave appears
- “Longer, longer, drop, that’s a Wenckebach.”
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- The maximum height of the P wave is:

(27)
- Signs and Symptoms:
- None
- Fatigue
- Shortness of breath
- Syncope or near syncope
- Chest pain
- Lightheadedness
- Causes:
- Increased vagal tones
- Cardiomyopathy
- Myocardial infarction
- Cardiac surgery
- Electrolyte abnormalities
- Medications
- Treatment:
- None if asymptomatic
- Medications
- Atropine if bradycardic
- Antidotes or reversal agents
- Electrolyte replacement
2nd Degree Type II AV Block (Mobitz II) (60):
- Rate: varies
- Conduction:
- PR interval varies
- QRS width 60-100ms when present
- QRS does not follow all P waves
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- The maximum height of the P wave is:
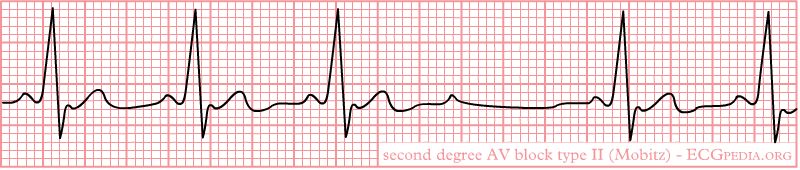
(40)
- Signs and Symptoms:
- Fatigue
- Shortness of breath
- Syncope or near syncope
- Chest pain
- Lightheadedness
- Cardiac arrest
- Causes:
- Structural heart disease
- Amyloidosis
- lymphoma
- Cardiac tumors
- Transcatheter placement of valves
- Myocardial infarction
- Genetics
- Treatment:
- None if asymptomatic
- Medications
- Atropine does not work on these patients
- Antidotes or reversal agents
- Transcutaneous cardiac pacing or pacemaker since this rhythm can progress to a complete heart block or cardiac arrest
3rd Degree AV Block (78):
- Rate: varies, but usually bradycardic
- Conduction:
- PR interval varies
- QRS width 60-100ms when present
- P wave and QRS complex do not communicate (called AV disassociation)
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- The maximum height of the P wave is:

(33)
- Signs and Symptoms:
- Fatigue
- Shortness of breath
- Syncope or near syncope
- Chest pain
- Lightheadedness
- Hemodynamic instability
- Cardiac murmurs
- Cardiac arrest
- Causes:
- Cardiac surgery
- Cardiac disease
- Medications
- Electrolyte imbalances
- Lyme disease
- Transcatheter aortic valve replacement
- Myocardial infarction
- Systemic lupus erythematosus
- Sarcoidosis
- Treatment:
- Medications
- Atropine usually does not work, but can be administered
- Epinephrine
- Dopamine
- Antidotes or reversal agents
- Electrolyte replacement
- Transcutaneous cardiac pacing or pacemaker
- Medications

Self Quiz
Ask yourself...
- 2nd degree Type I and Type II can be mixed up, what are your methods for remembering how each one appears on the EKG strip?
- What type of AV block would lead you to provide quick intervention and why?
- Have you encountered a patient with any of these rhythms? What was the cause? How was it resolved, if it was?
- Are there any causes for these rhythms that were not listed?
Premature Ventricular Contraction (PVC) (88):
- Rate: varies, underlying rhythm is usually normal sinus
- The impulse to beat comes from the ventricles, not from the SA node
- Conduction:
- PR interval varies, but in a regular PQRST complex PR interval is 120-200ms
- PR interval after a PVC is longer due to the PVC and the retrograde concealed conduction goes back into the AV node junction.
- PVC QRS width is at least 120ms but usually 160-200ms
- Regular QRS width is 60-100ms
- PR interval after a PVC is longer due to the PVC and the retrograde concealed conduction goes back into the AV node junction.
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave is:
- Positive or above the isoelectric line in II and AVF
- Biphasic in V1
- Rhythm Strip:
- Monomorphic: All PVCs are shaped the same
- The maximum height of the P wave is:
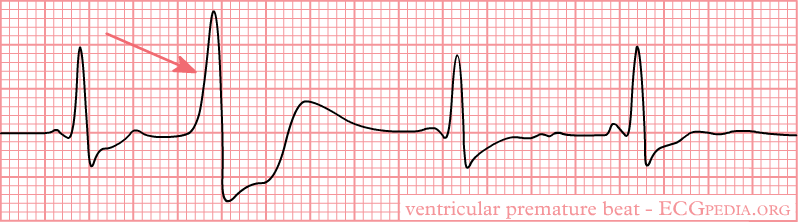
(38)
- Biomorphic: PVCs are shaped differently
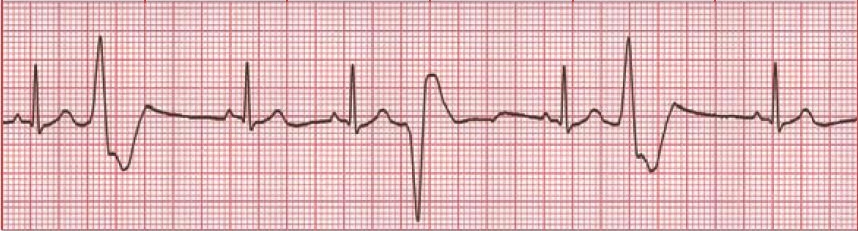
(64)
- Bigeminy: Every PVC is separated by one sinus beat.

(35)
- Trigeminy: Every PVC is separated by two sinus beats.

(9)
- Ventricular Couplet: Two PVC beats in a row.
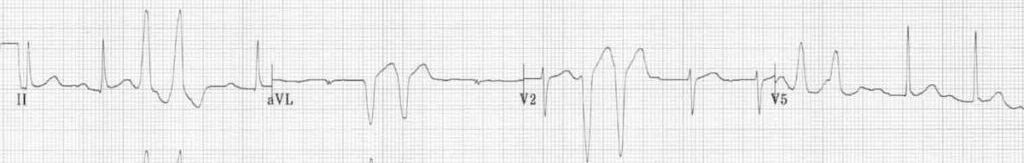
(9)
- Ventricular Triplet: Three PVC beats in a row.

(9)
- Signs and Symptoms:
- None
- Fatigue
- Shortness of breath
- Syncope or near syncope
- Chest pain
- Palpitations
- Lightheadedness
- Abnormal neck pulsation
- Hemodynamic instability with frequent PVCs
- Cardiac arrest
- Causes:
- Hypoxia
- Illicit drug use
- Amphetamines
- Alcohol
- Cocaine
- Electrolyte imbalances
- Myocarditis
- Mitral valve prolapse
- Hypercarbia
- Cardiomyopathies
- Myocardial infarction
- Medications
- Treatment:
- None if asymptomatic
- Medications
- Beta-blockers
- Calcium channel blockers
- Amiodarone is for those with preexisting coronary artery diseases, but used with caution and close observation and monitoring
- Antidotes or reversal agents
- Electrolyte replacement
- Cardiac ablation
- Defibrillation if cardiac arrest occurs
Premature Atrial Contractions (PAC) (54):
- Rate: varies, underlying rhythm is usually normal sinus
- Conduction:
- PR interval varies, but in a regular PQRST complex PR interval is 120-200ms
- PAC
- Regular QRS width is 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- The P wave:
- Can be inverted
- May be hidden in the T wave creating a hump or peaked T wave
- These rhythms can come in the same variations as PVCs:
- Bigeminy
- Trigeminy
- Couplet
- Triplet
- Rhythm Strip:
- The maximum height of the P wave is:
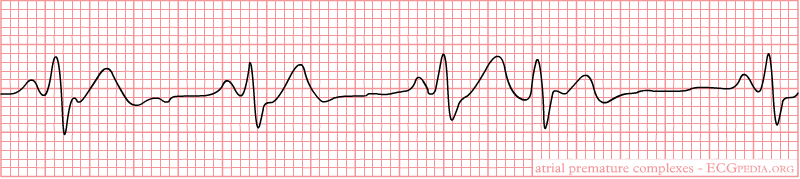
(37)
- Signs and Symptoms:
- None
- Palpitations
- Shortness of breath
- Anxiety
- Signs and symptoms of heart failure
- Early or additional heart sounds
- Pauses in rhythm
- Causes:
- Coronary artery disease
- Left ventricular hypertrophy
- Septal defects
- Congenital heart deformities
- Medications
- Beta-blockers
- Chemotherapeutic agents
- Congestive heart failure
- Diabetes mellitus
- Hypertension
- Chronic obstructive pulmonary disorder
- Anxiety
- Treatment:
- None if asymptomatic
- Avoiding triggers
- Medications
- Beta-adrenergic blockers
- Antiarrhythmic agents are used with caution and close observation and monitoring
- Antidotes or reversal agents
- Cardiac ablation

Self Quiz
Ask yourself...
- Between PACs and PVCs, which one would you be more concerned about? Why did you pick that rhythm?
- Have you encountered a patient with either of these rhythms? What treatments were ordered if any?
Ventricular Tachycardia (V Tach) (45):
- Rate: greater than 100bpm
- Conduction:
- PR interval none
- QRS width greater than 140ms
- P wave morphology:
- Not present
- Non-sustained V-Tach: three or more ventricular beats over a maximum of 30 seconds.
- Sustained V-Tach: a run of V Tach for more than 30 seconds or less is treated by cardioversion
- Monomorphic V-Tach: all ventricular beats look the same
- Polymorphic V-Tach: the ventricular beats look different.
- Biphasic V Teach: where the QRS complexes alternate with each beat.
- Digoxin intoxication
- Long QT syndrome
- Rhythm Strip:
- Monomorphic V-Tach
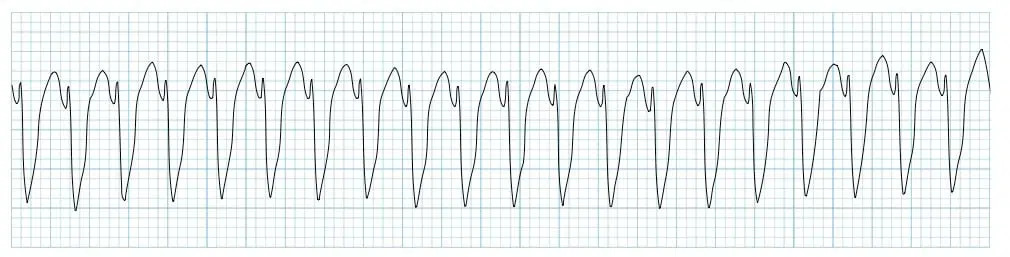
(11)
- Signs and Symptoms:
- Palpitations
- Shortness of breath
- Chest pain
- Syncope or near syncope
- Signs of heart failure
- Hemodynamic instability
- ICD shocks if the patient has one
- Cardiac arrest
- Also known as pulseless V-Tach
- Causes:
- Ischemic heart disease
- Acute coronary artery disease
- Myocardial scar-related reentry
- Congenital heart deformities
- Cardiomyopathy
- Illicit drugs
- Cocaine
- Digitalis toxicity
- Methamphetamine
- Medications
- Beta-blockers
- Chemotherapeutic agents
- Electrolyte imbalances
- Sepsis
- Metabolic acidosis
- Inherited cardiac channelopathies
- Treatment:
- Cardiopulmonary resuscitation (CPR) and defibrillation if no pulse present
- Cardioversion if hemodynamically unstable and has a pulse
- Treatment for myocardial infarction
- Medications
- Amiodarone, procainamide, sotalol
- Antidotes or reversal agents
- ICD
- Cardiac ablation

Self Quiz
Ask yourself...
- What would be the priorities when providing care to a patient with V-Tach with a pulse?
- If you were the only one in the room with the patient what would be your first action?
- Have you ever cardioverted a patient with this rhythm? What do you remember from the event?
- Do you think the patient should sign consent before cardioversion? Why or why not?
Torsades de Pointes (V Fib) (25):
- Rate: none
- Conduction:
- Polymorphic V-Tach with a prolonged QR interval
- P wave morphology:
- Not present
- Rhythm Strip:
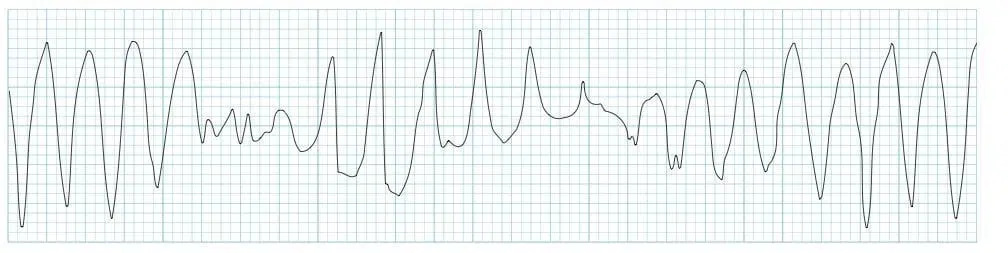
(12)
- Signs and Symptoms:
- None
- Syncope or near syncope
- Dizziness
- Lightheadedness
- Hypotension
- Rapid pulse
- Cardiac arrest
- No pulse
- Not breathing or only gasping for air
- Loss of consciousness
- Causes:
- Electrolyte imbalances
- Medications
- Zofran causes a long QT interval (19)
- Congenital prolonged QT:
- Jervell and Lange-Nielsen
- Romano-Ward syndrome
- Bradycardia
- Diuretic use
- Female gender
- Age
- Treatment:
- Electrolyte replacement
- CPR and defibrillation
- Medications
- Epinephrine
- Atropine
- Cardioversion
- Treatment of the underlying cause
Supraventricular Tachycardia (SVT) (72):
- Rate: Greater than 160bpm
- Conduction:
- PR interval not present
- QRS width less than 120 milliseconds = narrow complex, regular SVT
- QRS width greater than 120 milliseconds = wide complex, regular SVT
- P wave morphology:
- Not present
- Rhythm Strip:
- Narrow complex, regular SVT

(30)
- Wide complex, regular SVT

(79)
- Signs and Symptoms:
- None
- Hypotension
- Shortness of breath
- Lightheadedness
- Signs and symptoms of heart failure
- Shock
- Causes:
- Narrow complex, regular SVT - Orthodromic reentry phenomenon (56):
- Accessory pathway that connects the atria and ventricles without passing through the AV node
- A pulse goes through the AV node, down into the ventricles via the Bundle of His, up through the accessory pathway, and back into the AV node
- Wide complex, regular SVT - Atrioventricular reentry phenomenon (57):
- Signals from the SA node travel through the accessory pathway down the ventricles via the Bundle of His and up to the AV node, creating a backward cycle.
- This is slower than the orthodromic SVT because it is traveling against the regular path of conduction, leaving to a wide QRS complex
- Medications
- Caffeine
- Smoking
- Stress
- Alcohol
- Narrow complex, regular SVT - Orthodromic reentry phenomenon (56):
- Treatment:
- None if asymptomatic
- Vagal maneuvers
- Bearing down
- Blowing into a straw
- Medications
- Adenosine: 1st dose 6mg, 2nd dose 12mg
- Ensure rapid saline flush after pushing medication as it has an extremely short half-life
- Cardizem
- Antidotes or reversal agents
- Adenosine: 1st dose 6mg, 2nd dose 12mg
- Cardioversion
- Cardiac ablation

Self Quiz
Ask yourself...
- If you have encountered a patient in SVT, what vagal maneuvers have you seen used? Were they successful or not?
- If you have not encountered a patient with SVT, what vagal maneuvers could you think of that might be utilized?
- Would a patient’s age impact the vagal maneuvers used? Why or why not?
- Do you know the half-life of Adenosine? If not, will you look it up after this course?
Ventricular Fibrillation (V-Fib) (3):
- Rate: none
- Conduction:
- PR interval not present
- QRS width not present
- P wave morphology:
- Not present
- Rhythm Strip:
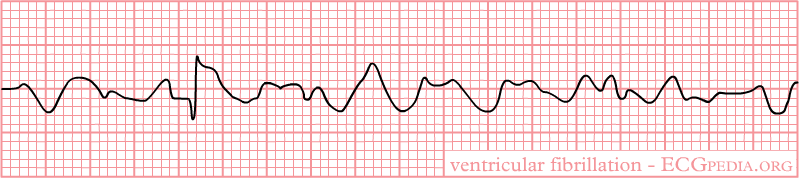
(39)
- Signs and Symptoms:
- Cardiac arrest
- No pulse
- Not breathing or only gasping for air
- Loss of consciousness
- Causes:
- Electrolyte imbalances
- Myocardial infarction
- Congenital heart defects
- Sudden blow to the chest right over the heart
- Medications
- Anemia
- Cardiomyopathy
- Electrocution
- Thoracic trauma
- Heart surgery
- Treatment:
- CPR and defibrillation
- Medications
- Epinephrine
- Atropine
- Electrolytes
- Surgery
- Coronary perfusion
- Treatment of the underlying cause
- Cardiac arrest
Asystole (59):
- Rate: none
- Conduction:
- PR interval not present
- QRS width not present
- P wave morphology:
- May or may not be present
- Rhythm Strip:

(21)
- Signs and Symptoms:
- Cardiac arrest
- No pulse
- Not breathing or only gasping for air
- Loss of consciousness
- Causes:
- Electrolyte imbalances
- Myocardial infarction
- Congenital heart defects
- Medications or illicit drugs
- Blood loss
- Cardiomyopathy
- Electrocution
- Trauma
- Treatment:
- CPR
- Since there is no electrical activity with this rhythm, defibrillation cannot be used
- Medications
- Epinephrine
- Atropine
- Electrolytes
- Surgery
- Coronary perfusion
- Treatment of the underlying cause
- CPR
- Cardiac arrest
Pulseless Electrical Activity (PEA) (22):
- Rate: varies
- There is no pulse with this rhythm despite the fact that it may appear as an organized rhythm
- Conduction:
- PR interval none
- QRS width greater than 110ms
- P wave morphology:
- Not present
- The P wave is:
- Not present
- Rhythm Strip:
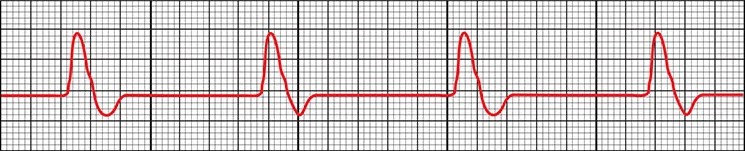
(22)
- Signs and Symptoms:
- Cardiac arrest
- No pulse
- Not breathing or only gasping for air
- Loss of consciousness
- Causes:
- Electrolyte imbalances
- Myocardial infarction
- Congenital heart defects
- Medications or illicit drugs
- Blood loss
- Cardiomyopathy
- Electrocution
- Trauma
- Hypothermia
- Pneumothorax or hemothorax
- Treatment:
- CPR
- Since there is no electrical activity with this rhythm, defibrillation cannot be used
- Medications
- Epinephrine
- Atropine
- Electrolytes
- Surgery
- Coronary perfusion
- Treatment of the underlying cause
- CPR
- Cardiac arrest

Self Quiz
Ask yourself...
- What are some misconceptions about V-Fib, asystole, and PEA?
- How do you educate other staff members and family members on these misconceptions?
- What treatments have you seen work on V Fib? What treatments did not work?
- Have you ever seen a patient’s rhythm change from asystole to another rhythm?
- What is the most prominent cause of cardiac arrest in your area?
Atrial Flutter (73):
- Rate: varies
- Depends on how many QRS complexes there are
- Atrial rate 250-350 bpm
- Ventricular rate 75-150bpm
- P waves can come in blocks
- 2 P waves per 1 QRS (2:1)
- 3 P waves per 1 QRS (3:1)
- 4 P waves per 1 QRS (4:1)
- Intervals of P waves per 1 QRS (2:1 then 3: 1 then 2:1 then 4:1)
- Conduction:
- PR interval varies
- QRS width 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- Sawtooth pattern
- Rhythm Strip:
- The maximum height of the P wave is:
- Depends on how many QRS complexes there are
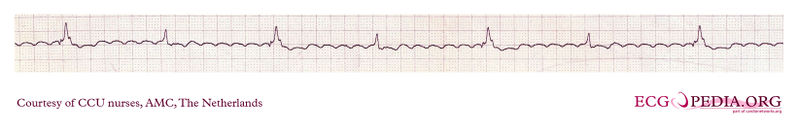
(31)
- Signs and Symptoms:
- None
- Palpitations
- Fatigue
- Syncope or near syncope
- Shortness of breath
- Regular or irregularly regular pulse
- Causes:
- COPD
- Heart failure
- Atrial size abnormalities
- Hypertension
- Diabetes mellitus
- Age
- Male gender
- Treatment:
- None if asymptomatic
- Medications
- Amiodarone
- Cardizem
- Metoprolol
- Anticoagulation to prevent stroke
- Catheter ablation
- Treatment of the underlying cause
Atrial Fibrillation (AFib) (89):
- Rate: varies
- Atrial rate 400-600 bpm
- Ventricular rate 75-175 bpm
- Anything over 100 is considered A Fib with rapid ventricular response (RVR)
- Conduction:
- PR interval varies
- QRS width 60-100ms
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- Rhythm Strip:
- A Fib
- The maximum height of the P wave is:
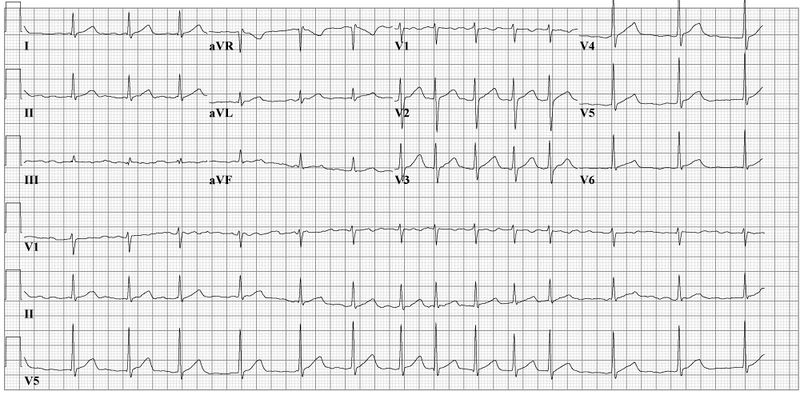
(28)
- A Fib RVR

(34)
- Signs and Symptoms:
- None
- Palpitations
- Fatigue
- Syncope or near syncope
- Shortness of breath
- Regular or irregular pulse
- Patients can go in and out of A Fib or it can be permanent,
- They can go in and out of RVR
- Causes:
- Heart disease
- Genetics
- Pulmonary embolism or other hemodynamic stressors
- Obstructive sleep apnea
- Heart failure
- Pericarditis
- Myocarditis
- Myocardial infarction
- Hypertension
- Diabetes mellitus
- Age
- Treatment:
- None if asymptomatic
- Medications
- Cardizem
- Metoprolol
- Amiodarone
- Anticoagulation to prevent stroke
- Catheter ablation
- Treatment of the underlying cause
Idioventricular Rhythms (47):
- Rate: varies
- Idioventricular rate 35-40bpm
- Accelerated rate 60-120bpm
- Conduction:
- PR interval not present
- QRS width greater than 120ms but can be greater than 160ms
- The normal conduction system does not transmit the signal to beat, the vertical signal is transmitted from cell to cell
- P wave morphology:
- Not present
- Rhythm Strip:
- Idioventricular rate

(36)
- Signs and Symptoms:
- None
- Palpitations
- Fatigue
- Lightheadedness
- Syncope or near syncope
- Cardiac arrest
- Causes:
- Electrolyte imbalances
- Reperfusion of cardiac cells after a myocardial infarction
- Medications
- Digoxin
- Beta-adrenoreceptor agonists
- Illicit drug use like cocaine
- Cardiomyopathies
- Congenital cardiac defects
- Athletes
- Treatment:
- None if asymptomatic
- Medications
- Atropine
- Amiodarone or lidocaine
- Reversal agents
- Rarely cardiac pacing
- Treatment of the underlying cause
Junctional Rhythms (52):
- Rate: varies
- Junctional bradycardia less than 40bpm
- Junctional escape rhythm 40-60bpm
- Accelerated junctional rhythm 60-100bpm
- Junctional tachycardia greater than 100bpm
- Conduction:
- PR interval not present
- QRS width 60-100ms
- P wave morphology:
- Not present
- Rhythm Strip:
- Accelerated Junctional Rhythm
- Rhythms look the same but have more beats depending on the type of rhythm
- Accelerated Junctional Rhythm

(52)
- Signs and Symptoms:
- None
- Shortness of breath
- Palpitations, intermittent or continuous
- Fatigue
- Lightheadedness
- Syncope or near syncope
- Causes:
- Electrolyte imbalances
- Can be caused by anorexia nervosa
- Thoracic trauma
- Myocarditis
- Reperfusion of cardiac cells after a myocardial infarction
- Medications
- Adenosine
- Clonidine
- Antiarrhythmics
- Lithium
- Digoxin
- Sleep apnea
- Hypoxia
- Coronary artery disease
- Congenital cardiac defects and repairs of these defects
- Electrolyte imbalances
- Treatment:
- None if asymptomatic
- Medications
- Atropine
- Reversal agents
- Transcutaneous pacing
- Permanent pacemaker
- Treatment of the underlying cause
Bundle Branch Blocks (BBB) (43, 53, 70):
- Rate: varies
- Conduction:
- Right BBB (RBBB):
- QRS interval greater than 120ms
- Septal depolarization that leads to a:
- Small R wave being present in V1
- Q wave in V6
- The left ventricle’s contraction leads to and:
-
- S wave in V1
- R wave in V6
-
- The right ventricle’s contraction leads to an:
- R wave in V1
- Deep S wave in V6
- Left BBB (LBBB):
- QRS interval greater than 120ms
- T wave inversion is due to abnormal repolarization
- From first principles:
- Septal depolarization that leads to a:
- Q wave in V1
- R wave in V6
- Right BBB (RBBB):
-
-
- The right ventricle’s contraction leads to an:
- R wave in V1
- S wave in V6
- The left ventricle’s contraction leads to and:
- S wave in V1
- R wave in V6
- The right ventricle’s contraction leads to an:
- P wave morphology:
- The maximum height of the P wave is:
- Lead II and III: 2.5 mm
- Rhythm Strip:
- RBBB
- The maximum height of the P wave is:
-
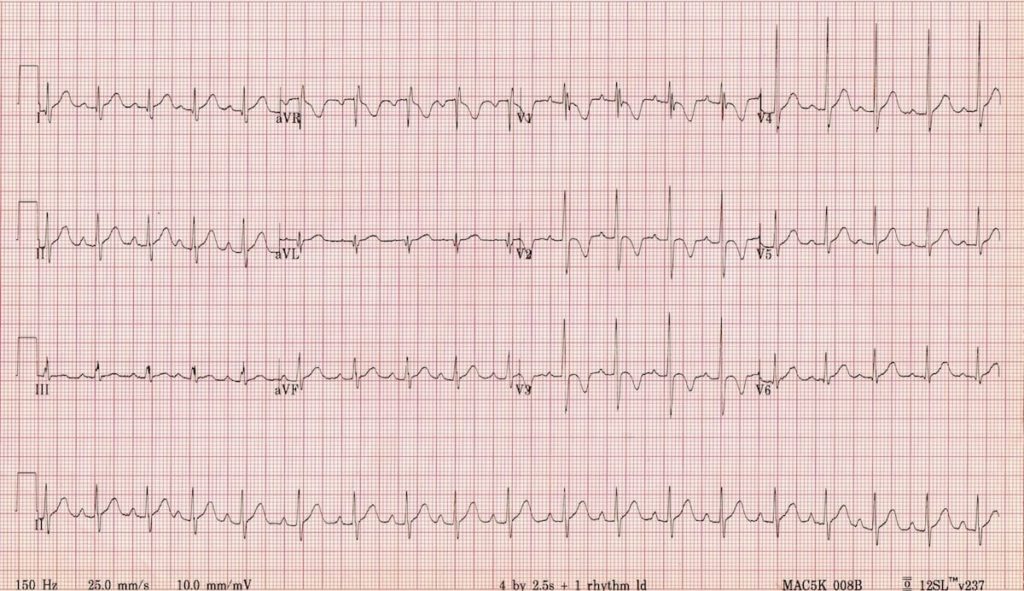
(71)
-
-
-
- LBBB
-
-
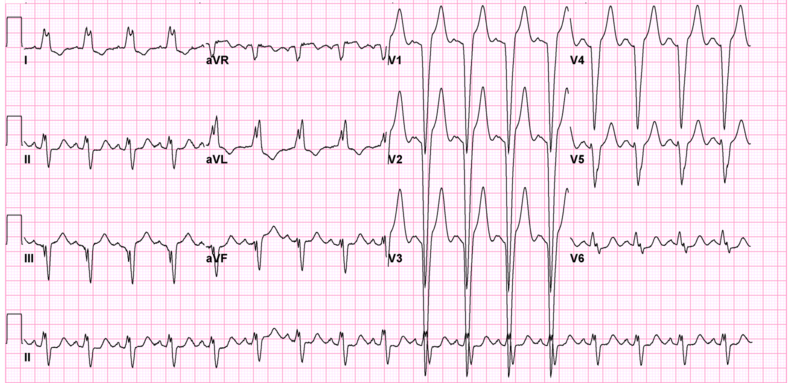
(71)
- Signs and Symptoms:
- None
- Lightheadedness
- Syncope or near syncope
- Causes:
- RBBB:
- Myocardial infarction
- Congenital cardiac defects
- Pulmonary embolism
- Myocarditis
- Pulmonary hypertension
- LBBB:
- Myocardial infarction
- Hypertension
- Cardiomyopathy
- Myocarditis
- Treatment:
- None if asymptomatic
- Treatment of the underlying cause
- RBBB:
Identifying Ischemia and Infarction
Known as coronary artery disease (CAD), acute myocardial ischemia is the decrease of blood flow to the heart by atherosclerosis or plaque. The atherosclerosis starts as a plaque streak within the large arteries and continues to build up. After the plaque has grown to a significant size, occlusion begins and blood flow to areas below the growing occlusion suffers a decrease in blood flow. This is what is known as ischemia (81).
When resting, patients may not experience any signs or symptoms. Upon exertion, however, patients may experience stable angina—chest pain, discomfort, pressure, etc.—as activity requires increased blood flow and the arteries constrict to pump blood through the body faster. This pain is relieved at rest and can be further treated by nitrates. The routine is what makes this stable angina (81).
Unstable angina begins once the artery has become occluded enough to create a significant obstruction of blood flow. Signs and symptoms can include chest pain or other discomfort that is challenging to relieve, even when at rest. Patients may be woken from sleep due to the pain and report that it takes longer for the pain to decrease or resolve completely. These signs and symptoms symbolize that the plaque within the artery is unstable and could potentially rupture (90).
Infarction is when the blood flow is completely obstructed and the cells below the obstruction begin to die off. This often occurs when the plaque within the artery ruptures, leading to the body’s natural clotting processing in an attempt to repair the rupture, and a complete occlusion of the artery occurs (46).
Now that we have discussed ischemia and infarction, it is time to discuss how a myocardial infarction (MI) appears on an EKG and how to identify it. You may also hear them referred to as STEMIs or ST-elevation myocardial infarction.
The progression of PQRST complex changes during an MI can start with hyperacute T waves. The T wave will increase with amplitude and become wider, while some ST elevation may be noted. This elevation begins to occur as injury to the heart muscle begins. From there, the ST elevation increases and creates the image often associated with an MI. Pathological Q wave may develop as the MI progresses. As discussed earlier, the Q wave is the first downward deflection of the QRS complex and is normally 1mm or less in depth. Pathological Q waves are measured by greater than 1mm wide or greater than 25% of the R wave’s amplitude (84).
T wave inversion occurs when the cells have become necrotized and begin to form fibrosis. Once all necrotized cells have become fibrotic, the Q waves will remain, but the T waves will become upright again (84).
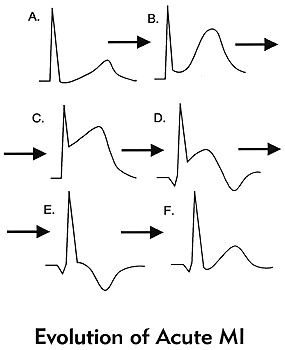
(84)
These changes should be present in at least 2 contiguous leads or leads that are side by side. To discuss this more, we will refer to the 12 lead EKG photo we used earlier. It is important to know that there will be leads with ST elevation and there will be leads with reciprocal ST depression based on the type of MI and how these leads are placed in relation to the area of the heart that is being affected.
| Type of MI | Leads with ST Elevation | Reciprocal ST Depression |
| Inferior | I, II, AVF | I, AVL |
| Lateral | V5, V6 | III, AVR |
| Anterior | I, AVL, V5, V6 | II, III, AVF |
| Posterior | V7, V8, V9 | V1, V2, V3 |
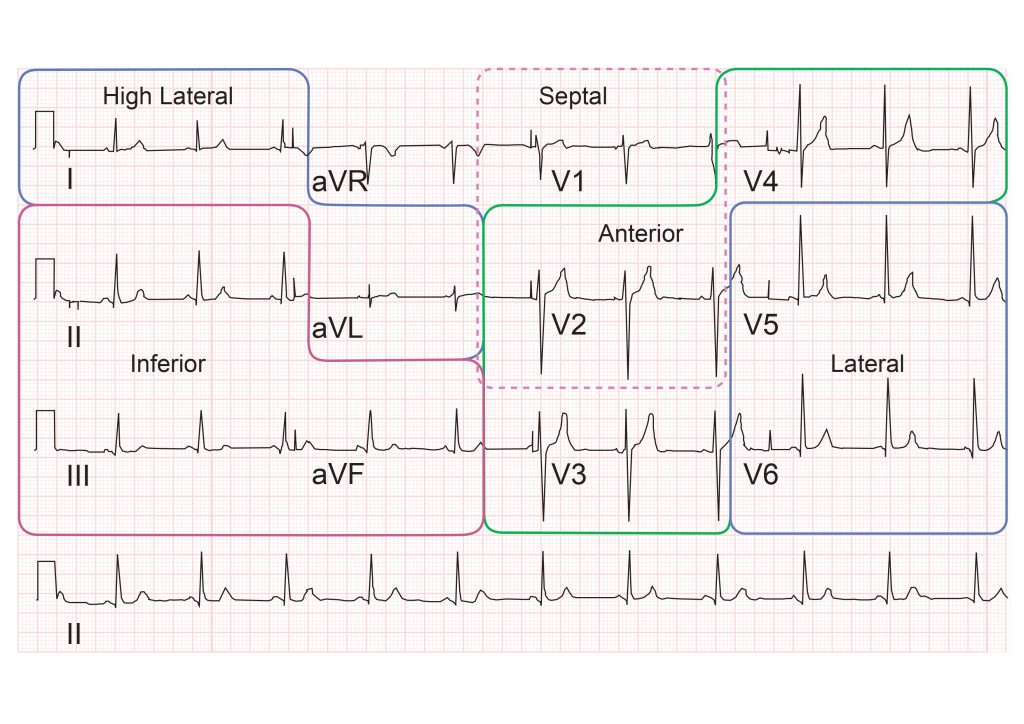
(82)
With posterior MIs the elevation must be at least 0.5mm, there will be tall, broad R waves of at least 30ms long, and the T wave will be upright. When looking at an EKG for a posterior MI, the ST depression is what will be observed in leads V1, V2, and V3. If a posterior MI is suspected, look at the EKG from the back of the paper by flipping it over and holding it to light. This will display the ST depression as ST elevation, prompting you to consider a posterior EKG. It is advised that a posterior EKG with leads V7, V8, and V9 be done. A quick method to do this is by removing leads V4, V5, and V6; placing them in the posterior lead positions; and relabeling them on the EKG. (77).
Right ventricular MIs can occur, and it is important to assess and treat them appropriately. To assess for a right-sided MI, first look at the standard EKG. If ST elevation is noted in leads II and III, but the ST elevation is greater in lead III than lead II, consider right ventricular involvement. As discussed previously, one method is to do a right-sided EKG, with lead placement along the right side of the chest. The second, quicker way to do this is to take lead V4 and place it on the right side of the chest and mark it as V4R on the EKG (77).
Another rhythm that can be an indicator of an MI is a bundle branch block. New or suspected new BBBs are to be treated as a MI by providers. But what if you have a copy of an old EKG and the BBB isn’t new, can the patient still be having an MI? The answer is yes. However, it can be challenging to determine what is a change from the MI and what is from the BBB. The Sgarbossa criteria is useful in making these determinations and can also be used for patients who have a pacemaker (77)
Sgarbossa criteria (77):
- Concordant ST elevation that is greater than 1mm
- Concordant ST depression that is greater than 1mm
- Excess discordant ST elevation that is greater than 5mm in leads with negative QRS complexes – these are complexes below the isoelectric line
For reference, concordance means that the ST segment and QRS complex go in the same direction, either both deflecting upwards or downwards. Discordance is what should be seen in a BBB or paced rhythm. This is where the ST segment and the QRS complex go in different directions. Smith et al. created a modification to the Sgarbossa criteria to include a greater than 1mm ST elevation to an S-wave amplitude ratio of greater than 0.25mm (7).
Another method that has been created, but not validated is the Barcelona criteria. This criterion has greater than 1mm ST deviation concordance or discordance with QRS polarity in any EKG lead. Discordant ST deviation is greater than 1mm in any lead where the R or S points of the QRS complex are less than 6mm (7).
There is an EKG rhythm that can indicate a future MI which is known as Wellens syndrome. This EKG has a deeply inverted or biphasic T wave in leads V2 and V3. The patient is often pain-free when the rhythm is present, ischemic chest pain can obscure the rhythm by creating a false normal appearance of the T waves in the affected leads. Their cardiac enzymes may not even be elevated. Any patient presenting with chest pain should have serial EKGs done for this reason, since they may be pain-free at a later time. These EKG changes symbolize the critical stenosis of the proximal left anterior descending artery (LAD). This is the artery that provides the left ventricle with blood (65).

Self Quiz
Ask yourself...
- Do you remember the first patient that you had that was experiencing an MI? What stood out about that patient in your mind?
- Patients have a variety of symptoms that can be experienced during an MI, what was the most interesting symptom a patient had during an MI?
- Have you ever encountered a patient with Wellens Syndrome? Do you know if they ended up having an MI later?
Cardiac Assessment:
A traditional cardiac assessment focuses on more than just the heart; it encompasses aspects of both the neurological and respiratory systems. However, we will begin our focus with the heart.
Pain may not be a word patients use to describe what they are feeling. As mentioned, they may vocalize discomfort, pressure, cramping, burning, or tightness. Women may have jaw or arm pain as opposed to the traditional chest pain that men may experience. Ask them to rate their pain on a scale of one to ten, looking for changes in the value. An EKG based on pain, discomfort, pressure, cramping, or tightness should be completed within the time frame set by hospital policy.
The PQRST pneumonic can assist providers in remembering the specific information they need to collect (90).
P: What provokes, precipitates, or palliates/alleviates the pain or discomfort the patient is feeling? Does it get worse or better when you do certain things, i.e., walk or rest?
Q: What is the quality of pain or discomfort you are feeling?
R: Does this pain or discomfort radiate anywhere else in your body? Jaw, arm, back?
S: Are there associated symptoms with the pain or discomfort? Shortness of breath, dizziness, heartburn?
T: What time elements are involved? When did it start? Did it stop and come back? Are you currently feeling it now? Was it gradual or did it occur suddenly? Did it wake you up?
Patients should be asked about palpitations or any experienced abnormal heart rhythms detected on monitoring devices. Many individuals have smartwatches that can detect heart rates and some rhythms. If the patient is wearing one, determine if the device has recorded anything.
Edema in the legs can be a sign of acute heart failure while pain in the calf can indicate a blood clot that could have traveled from another part of the body (85). In A Fib, the blood can clot in the ventricles due to poor circulation of blood. It will pool until it clots or is ejected from the heart. Once expelled, the clot will travel until it can no longer pass through the veins (63). Ensure a thorough assessment of the patient’s distal pulses is done as well to determine circulation. The further pulse locations can be an indicator of poor circulation (85).
Moving on to the respiratory system, we will reflect on the many arrhythmias that have shortness of breath as a sign or symptom. Providers should assess lung sounds to determine if there is any fluid buildup, a sign of acute heart failure. Determine if the shortness of breath is all the time, upon exertion, or at rest. Also, it is important to ask if the patient has been woken from sleep due to a shortness of breath. Sometimes arrhythmias occur at unexpected moments, even in the middle of the night (85).
Syncope was another common sign or symptom of cardiac arrhythmias due to decreased perfusion to the brain. Providers should determine if the patient currently feels lightheaded or dizzy, if they felt that way in the past, or if they have fainted. They should ask when this feeling happens—at rest, while moving, or both—and if they get any warning signs or auras beforehand. Always ensure you ask the patient to describe what happened so it can be added to the assessment (85).
A full medical history should be obtained, with a special focus on any past cardiac medical history the patient or their family has. Providers may consider asking the following questions:
- Have you been diagnosed with coronary artery disease, high blood pressure, peripheral vascular disease, valve problems, heart failure, high cholesterol, or other heart conditions?
- Have you had a heart attack or stroke in the past?
- Have you had any surgical procedures to help with your heart function? This may include things like ablation or stent placement.
Asking about medications can assist providers in determining any missed diagnoses with the patient while asking about social history can provide information about smoking, illicit drug use, alcohol consumption, and exercise habits (85).
Conclusion
Thanks to advancements within the medical profession, cardiac telemetry can be greatly beneficial to patients in and outside of the hospital setting. From devices you can carry, to devices implanted inside someone, patient outcomes have improved for identifying, treating, and managing cardiac arrhythmias that had once been deemed unmanageable. With proper knowledge of EKG rhythms, nurses can confidently provide the proper care for their patients by being an advocate for those they care for.

Self Quiz
Ask yourself...
- Have you seen changes in the patients admitted to your facilities that you could correlate to these indications?
- Do you agree with this list? Is there anything you feel should be added or removed? Why?
- Are there any time frames (how long a patient is on a telemetry monitor) that you think should be adjusted?
- Do you think sending patients home with wearable monitors could be used in the future to prevent admission in some of the patients who meet the criteria for admission with telemetry?
Conclusion
Thanks to advancements within the medical profession, cardiac telemetry can be greatly beneficial to patients in and outside of the hospital setting. From devices you can carry, to devices implanted inside someone, patient outcomes have improved for identifying, treating, and managing cardiac arrhythmias that had once been deemed unmanageable. With proper knowledge of EKG rhythms, nurses can confidently provide the proper care for their patients by being an advocate for those they care for.
Heart Failure Updates
Introduction
In 1997, Heart Failure (HF) was designated an epidemic due to the significant increase in hospitalizations. (2) This increase in hospitalizations appears to be due to accurate management of HF patients who re-hospitalize for stabilization and medication management rather than a new diagnosis or end-stage disease.
HF occurs when the heart is too weak to pump blood to the body and lungs. The blood then backs up into the heart, lungs, and lower extremities, causing less blood supply to the body. HF can also be so severe that it can cause death in patients. (1)
It is crucial for nurses to understand the pathophysiology of HF, risk factors, and what education and treatment a nurse can incorporate in the plan of care, which will slow the progression of disease and maintain quality of life.
Introduction
In 1997, Heart Failure (HF) was designated an epidemic due to the significant increase in hospitalizations. (2) This increase in hospitalizations appears to be due to accurate management of HF patients who re-hospitalize for stabilization and medication management rather than a new diagnosis or end-stage disease.
HF occurs when the heart is too weak to pump blood to the body and lungs. The blood then backs up into the heart, lungs, and lower extremities, causing less blood supply to the body. HF can also be so severe that it can cause death in patients. (1)
It is crucial for nurses to understand the pathophysiology of HF, risk factors, and what education and treatment a nurse can incorporate in the plan of care, which will slow the progression of disease and maintain quality of life.

Self Quiz
Ask yourself...
- How can you find the costs associated with HF patients at your place of work? What treatments are helping manage HF patients?
- How would you assess an HF patient on your initial encounter as a nurse?
Statistical Evidence/Epidemiology
Epidemiologists study a disease's incidence, mortality, and prevalence to predict health care costs, how many people have a disease, how it affects society, and when the numbers of a disease change.
According to the CDC, there are approximately 6.2 million patients with heart failure in the United States. The diagnosis was noted on 13.8% of death certificates in 2018. (2) $30.7 billion was spent on HF in 2012, including health care costs, days away from work, and medications that treat HF.
Although HF is higher in the elderly population, the more significant number of patients ages 35 and above who die with HF are concentrated in the southeast, southwest, Indiana, Wisconsin, and Illinois, with some counties in Utah, Oregon, Montana, South Dakota, and Nebraska.
Readmission rates declined when the Hospital Readmission Reduction Program (HRRP) began in 2012 to reduce costs and deliver care more safely.
Hospitals are penalized by the Centers for Medicare and Medicaid to lower readmission rates to less than 30 days for some diagnoses, and HF was among them. Hospitals began to look closer at the readmission rates, which helped them to focus on improved management. (2) . Using the information below, nurses can better assess the patient and add more information to their care plan.
The classifications of HF as defined by the New York Heart Association are:
- No symptoms with regular physical activity.
- Some mild symptoms with physical activity but not at rest
- Comfortable at rest but with moderate symptoms with some minor physical activity.
- Severe shortness of breath with rest. (2)
Providers typically use echocardiograms to measure heart failure using the ejection fraction (EF) percentage. Ejection fraction demonstrates the blood pumping rate from the left ventricle to the body.
An EF of below 30% indicates severe disease, while an EF at or above 50% indicates milder or no condition. Left ventricular failure with an EF of 50% or above is considered HF with preserved EF. An EF of 30% or below is considered HF with reduced EF. There is now a new category called HF with mid-range, which shows an EF of 40%-50%.
Approximately 15% of the HF population shows mid-range EF.
Incidence - is the number of new disease cases in certain patients. In HF, this number also helps scientists understand how the prevalence of the disease results from a lifestyle change. These studies aid in determining the burden of HF on society, which in turn helps to make changes in public policy and, eventually, how HF patients are treated. "For HF, incidence as a measure of new cases is particularly helpful to assess how the occurrences of HF might have changed over time as a result of changes in risk factors." (2)
Prevalence - measures the commonality of a disease, in this case HF, in the at-risk population at or over a given time. It also measures how often an HF patient will be encountered. (6)
Mortality - CHF is one of the top causes of death. Mortality rates are high, and the data shows that 50% of HF patients die at or within five years of diagnosis. (2) More recent studies show mortality rates in HF are increasing, which may be due in part to an aging population.

Self Quiz
Ask yourself...
- Where can you find more information on the epidemiology of HF?
- Where do epidemiologists get their information?
- Can you define the difference between incidence and prevalence?
Etiology and Pathophysiology
Heart failure is often caused by an injury to the heart's muscle, such as Myocardial Infarction (MI), valvular regurgitation, stenosis of the heart's valves, and arrhythmia. (4) It is essential that the provider determines the cause to treat these patients appropriately.
The most common cause of HF is cardiovascular disease. When fatty deposits or plaque buildup in the vessels supplying the heart, the arteries become narrowed and decrease blood flow to the heart muscle. This can cause ischemia (lack of oxygen) to the area of the heart's power involved, causing an MI. This, in turn, causes damage to the heart's muscle, reducing its ability to pump normally.
There are two main types of HF:
- Left ventricular HF or systolic (LHF)
- Right ventricular HF or diastolic (RHF)
LHF occurs when the damage to the left ventricle occurs, and RHF occurs when the damage is to the right ventricle.
The following Table taken from the National Institutes of Health shows comorbidities for Systolic and Diastolic HF:
Systolic (LHF)
- Coronary Heart disease
- Arterial Hypertension
- Valvular Heart Disease
- Arrhythmias
- Inflammatory disease
- Idiopathic cardiomyopathy
- Toxic Cardiomyopathy (alcohol)
Diastolic (RHF)
- Diabetes Mellitus
- Arterial Hypertension
- Valvular Heart Disease (pressure load)
- Hypertrophic Cardiomyopathy
- Restrictive Cardiomyopathy
- Constrictive Pericarditis
- Amyloidosis (storage disease)
HF causes volume overload in the ventricles of the heart. This is due to enlargement and stiffness of the ventricles, so they cannot pump enough blood to the lungs and the body. (1,4) The nurse can utilize this information to care for the patient and implement essential treatments.
Genetics also play a role in HF but are varied and complex. Studies have found more than 100 genes that may contribute to cardiomyopathy. Depending on where the failure occurs, more genetic testing is recommended in some instances: Left, Right, or Biventricular determines what signs and symptoms may be present in a patient.
In a patient with an MI or volume/pressure overload, the whole heart will change in structure and function. There will be hypertrophy of the Left ventricle and the dilatation of the chambers, which will cause further deterioration in cardiac function. (4)
Certain medications may also lead to HF in some patients. These are the diabetic medications Actos and Avandia. NSAIDS (non-steroidal inflammatory drugs) and certain medicines that treat hypertension, cancer, blood dyscrasias, mental health, lung urinary issues, and infections. (1)
Aging also contributes as the heart's ability to work decreases over time. Too much alcohol and smoking are also important considerations. Heart failure may also cause complications such as kidney damage and failure, more heart problems, and liver disease caused by the backup of fluid that the liver cannot handle.
The photo below shows the difference between a normal heart and an enlarged one (12).
Preventable and non-preventable risk factors for heart disease are:
- Poor diet
- Smoking
- Lack of exercise
- Alcoholism
- Obesity
- Genetics/Race-non preventable
It is also known that Hispanic women are at higher risk for diabetes, which can lead to heart disease if their diabetes is not managed well. Also, African American men are at higher risk for heart disease, possibly leading to HF.
Interestingly, some studies have shown that the incidence of hospitalizations has declined. This may be due to early diagnosis, better use of medications and newer devices, earlier and ongoing patient education of risk factors, and stellar outpatient and preventive care of those patients living with HF or at risk in the community (2).

Self Quiz
Ask yourself...
- Why do you think certain diseases and medications contribute to heart disease?
- How would you plan to educate your new patient on this disease?
- What are the mechanisms of HF that may cause other diseases?
Diagnostic and Screening Tools for Heart Failure (HF)
Essential diagnostic screening tools are heart rate, cholesterol testing, blood pressure, and weight. Blood pressure measurement is one of the most critical tests since it can have no symptoms.
If high, it significantly increases the risk of cardiac disease. Fortunately, diet exercise can control blood pressure to lose weight if needed, and medications.
According to the American Heart Association, the standard for blood pressure is 120/80 or below and should be measured starting at age 20. (5) Next is the fasting cholesterol profile. Again, starting at age 20, a fasting lipid profile should be done. (5) This will give the provider and patient a baseline to follow and assist nurses in developing and implementing care plans.
The following chart describes lab values for cholesterol. As you can see, the values in red are at the highest risk for cardiovascular disease, which could lead to HF.
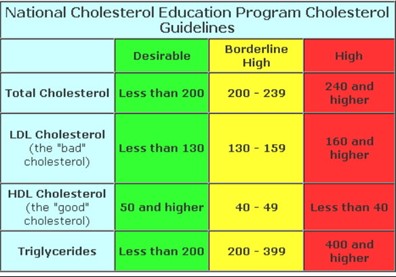
(13)
Body habitus is another crucial factor in predicting CAD. Body mass index (BMI), Waist measurements, and body structure can help predict how at risk a patient is for many diseases, including CAD, diabetes, atrial fibrillation, HF, and stroke. (7)
The typical Western diet is full of fats and sugars. In the US, many processed foods containing high salt, fat, and sugar are used.
These foods are unhealthy for the body and cause obesity and poor health. The Mediterranean diet, in turn, is full of fresh fruits and vegetables, lean meat, and a few processed foods. This is the most recommended diet for all populations.
High blood glucose is another indicator of poor health. Insulin resistance is the precursor to diabetes. A patient has insulin resistance when the body's muscles and tissues cannot respond to insulin, so glucose increases in the blood. (5)
Causes of insulin resistance are thought to be obesity with a large waist measurement. Blood glucose is usually tested with routine blood work. This gives the provider knowledge if a patient is at risk for diabetes and, therefore, heart disease. (5) Smoking and lack of physical activity can cause poor health, which may lead to cardiovascular disease.
Echocardiogram, Holter monitoring, stress tests, and nuclear stress tests are routinely used when a patient presents with symptoms of or has known cardiovascular disease. These tests provide a look at heart function and are used to determine disease progression or maintenance.

Self Quiz
Ask yourself...
- What are the waist measurements in males and females that are considered for a diagnosis of obesity?
- How would you care for a patient undergoing this testing using the nursing process?
- Why is diabetes a risk factor for HF?
Medication Management
Treating HF with medications can reduce disease progression, and relieve symptoms of dyspnea, fatigue, and edema. Several classes of drugs can be used to treat HF. Each one may be used to treat a different symptom.
The classes are as follows:
Angiotensin-Converting Enzyme (ACE) Inhibitors
These medications open blood vessels decreasing blood pressure and lowering the heart’s work to keep HF from worsening. (6)
Some common ACE inhibitors are:
- Captopril
- Enalapril
- Lisinopril
- Ramipril
Angiotensin-Receptor Blockers (Arbs)
- Losartan
- Valsartan
Angiotensin-Receptor Neprilysin Inhibitors (Arnis)
Entresto is a drug combination in the class of Angiotensin-receptor neprilysin inhibitors (ARNIs). ARNIs limit the enzyme neprilysin from breaking down natural substances in the body. By limiting this enzyme, the arteries can open to increase blood flow. This drug also limits the retention of sodium. (7)
Beta Blockers
Beta-blockers work to slow down the heart rate and increase blood flow by widening blood vessels. This also lowers blood pressure. (9)
Common Beta Blockers are:
- Atenolol
- Bisoprolol
- Carvedilol
- Labetalol
- Metoprolol succinate
- Metoprolol tartrate
- Nadolol
- Propranolol
Sodium-Glucose Cotransporter-2 (SGLT2) Inhibitors
Jardiance and Farxiga are Sodium-glucose cotransporter-2 (SGLT2) inhibitors that were designed to treat diabetes, but they have been found to be cardio-protective. (7)
Diuretics
Diuretics allow the body to release extra fluid and sodium through the kidneys. They cause increased urination so should be taken earlier in the day.
Most common diuretics are:
- Lasix
- Bumex
- Torsemide
- Diuril
- Hydrochlorothiazide (HCTZ)
- Metolazone
Other medications can be prescribed depending on the patient's needs, such as anticoagulants to keep the blood thin, statins to lower cholesterol, and Digoxin to control heart rate and increase pumping strength. Calcium channel blockers allow the heart muscle to relax, thereby reducing blood pressure and circulation within the heart. Potassium may be used with certain diuretics that cause potassium to leave the body.
It is needed to keep the heart's rhythm in control. Oxygen may also increase its amount in the blood, assisting with dyspnea and activity tolerance. (7) It is the nurse's responsibility to evaluate these medications and interventions for plan updates.

Self Quiz
Ask yourself...
- Which medications are the first line in controlling HF?
- Where can you find side effects of these medications?
- What would your care plan look like for a patient with HF?
Other Interventions
Several types of surgery can be utilized for the most severe cases of HF. Bypass surgery has been used for many years. This procedure bypasses blocked coronary arteries, allowing for better blood flow to the heart muscle.
Replacing damaged or stenosed heart valves will assist blood flow within the heart chambers. In some patients, biventricular pacing with a pacemaker allows both sides of the heart to work in sync. (10) An ICD, or implantable defibrillator, can shock the heart from a life-threatening rhythm back to normal.
The ventricular assist device or VAD can assist the ventricles to pump blood out to the body. (10) This device can be used either waiting for a transplant or permanently.
Heart Transplants can be used as the last intervention, with a success rate of 88% after one year and 75% after five. If a patient has sleep apnea, it can be linked to heart failure. In this case, an evaluation and treatment will be performed. (10)

Self Quiz
Ask yourself...
- Where can you learn more about assistive devices for HF?
- How many arteries can be bypassed in surgery at one time?
- How would you care for a person with a surgical device?
Current areas of research in HF are producing more effective drug therapy, genetic testing, non-surgical devices, transplants, and mechanical support. (8)
The research is now studying drugs that improve physical symptoms when added to the standard drug treatment and care. These drugs have shown improvement in reducing hospitalizations.
The newer diabetic medications Jardiance, Invokana, and Farxiga are being studied on HF patients without diabetes to learn if they will improve function and risk reduction of MI, stroke, or cardiovascular death. (8)
Non-invasive imaging such as MRI, ultrasound, nuclear testing, and radiology are being researched in the hope that advancing these technologies will "provide additional information about coronary arteries and heart tissue, coronary strain, the function and structure of the heart." (8)
Genetic testing is under investigation to help determine if there is an inherited disease, especially in specific cardiomyopathies. These cardiomyopathies present differently and may be treated with differing modalities.
One of the newest areas of HF management and treatment is remote monitoring. Nurses are at the forefront of home monitoring in many areas as they are the clinicians making home visits.
New types of VADs are emerging as treatments for advanced illnesses. They are being manufactured to be more durable and portable. (8)

Self Quiz
Ask yourself...
- Where can you find new research studies on HF?
- Where can you go to get educated on new devices?
- Who is conducting the new research?
Conclusion
As discussed in this course, Heart Failure affects over 6 million people in the US. Age, lifestyle, race, and genetics may predispose a patient to this disease.
HF burdens society and health care costs due to missed work, rehospitalizations, and poor outcomes. As a nurse, learning the mechanisms of HF is imperative. Understanding etiology, statistics, pharmaceuticals, and other interventions will assist nurses in administering the best care.
New research shows how emerging medications, improved implantable devices, and surgery can improve outcomes. However, patient education and prevention are vital to caring for HF patients.
Nurse Advocacy in Elder Abuse
Introduction
The term “advocate” refers to an individual that supports and promotes the interests of another person (1). As nurse advocates, we protect our patients against incompetency while safeguarding their wellbeing (2). As a nurse advocate in a suspected elder abuse situation, we are obligated, by law, to identify, report, and protect individuals experiencing elder abuse. As trusted members of the healthcare team, we are often the first interaction with a patient (and their family). Therefore, we are in a pivotal position to assess a situation for suspected abuse and neglect, while assuring patient safety, appropriate treatment, and improved outcomes.
Statistically, it is believed that approximately one in 10 Americans over the age of 60 years has experienced some type of elder abuse (3). As our aging population continues to grow, the likelihood of increased rates of elder abuse is a national concern. Nurse professionals often interact with the aging community and must be educated on the many aspects of caring for a person in a suspected abuse situation.

Self-Quiz
Ask Yourself...
- As a nurse, have you ever taken care of a suspected elder abuse case? What were some initial patient examination findings that raised the level of suspicion for abuse?
- With regard to caring for your suspected elder abuse victim, what were your observations as to the mental status of the alleged victim? Were they fearful and hesitant to discuss the situation, or did they welcome your inquiry?
Statistics
The aging population is facing many challenges related to finances, health and well-being, and safe secure housing options. In 2023, Senior List, a site dedicated to researching senior related products and services, reported some alarming statistics regarding the occurrence of elder abuse on a worldwide scale.
From financial fraud to nonfatal assaults and exploitation, it is estimated that “one in 10 older adults will experience some form of elder abuse, and many endure multiple types of abuse simultaneously” (4). The World Health Organization estimates that “320 million seniors will suffer from some form of elder abuse by the year 2050” (4).
According to a 2019 report by the Office of Inspector General, “1 in 5 emergency room visits among nursing home residents was attributed to abuse or neglect” (5). As the world population of elder persons continues to grow, the occurrence of elder abuse may also continue to grow, due to mental and physical decline, challenges with limited incomes, growing healthcare costs, and lack of appropriate age-related resources and support systems.

Self-Quiz
Ask Yourself...
- What types of financial challenges are elderly persons facing today? Have these challenges changed over the past few decades?
- What types of challenges are the elder population facing with respect to healthcare coverage?
Types of Elder Abuse
According to the World Health Organization, there are many types of elder abuse. In 2022, it was estimated that approximately one out of every six adults over the age of 60 had been subjected to some form of abuse in the prior calendar year (6). While rates are higher in institutions such as nursing homes and related long term care facilities, many forms of elder abuse occur in the home setting (6). The following list highlights various types of elder abuse. Any intentional act (or lack of appropriate action) that results in harm or distress to an older person is considered abuse.
Psychological Abuse
Psychological abuse is any action (or even the threat of action) that causes fear of violence or humiliation, a feeling of hopelessness, or isolation. This abuse may manifest itself as threats, verbal abuse, and intimidation tactics.
Physical Abuse
Physical abuse is any action that causes physical harm or injury to an elder person. This abuse may present itself as unexplained cuts, bruises, and broken bones.
Financial Abuse / Financial Exploitation
Financial abuse/exploitation is any action taken against an elder person’s money, belongings, or financial related documents. Financial exploitation can include unauthorized removal of money from bank accounts, fraudulent transfer of funds, unauthorized use of one’s savings and property, and internet scamming.
Sexual Abuse
Sexual abuse is any kind of sexual contact that occurs without the person’s consent. This abuse may present as unexplained sexually transmitted infections, torn or bloodied undergarments, difficulty walking, bruising on genitalia or inner thighs, and possible internal injuries.
Neglect
Neglect is a unique form of elder abuse, in that the abuse occurs from the lack of doing something (omitting care) versus the actual infliction of injury. Forms of neglect may include withholding medications and necessary medical treatment, withholding basic food and fluid requirements, and not seeking appropriate medical care for the elderly person when indicated. Victims of neglect may often present with dehydration, in under medicated (subtherapeutic) states, and often lacking basic hygiene care (dirty, soiled diapers or undergarments, disheveled appearance, malnourished).
Other Abuse Signs/Symptoms
Other signs and symptoms that may indicate elder abuse can include unintentional weight loss, a noted withdrawal from family and friends, unusual financial transactions, and a lack of basic medical needs such as routine medications and assistive devices (glasses, hearing aids, dentures). Further explanation is needed in these situations, as (the perception of) abuse and neglect may actually be the result of extenuating circumstances unrelated to actual abuse.


Self-Quiz
Ask Yourself...
- Psychological abuse may manifest itself as a feeling of hopelessness in an elder person. What other mental health issues may also heighten the risk of feelings of hopelessness?
- What do you think are some ways an alleged (elder abuse) perpetrator may psychologically abuse their victim?
- Have you ever taken care of a patient suffering from suspected neglect? What signs and symptoms did you observe?
- What are some reasons that a primary caregiver may appear to withhold an elder person’s routine medication?
- Unintentional weight loss in an elder person may indicate neglect. What other assessments should be done regarding such weight loss?
Risk Factors and Protective Factors
There are certain individual characteristics that put an elder person at risk for abuse. Persons with poor physical and mental health often do not have the ability to seek appropriate care within their community. Additionally, those who suffer from forms of cognitive impairment or physical disability may inadvertently place themselves in vulnerable situations.
Finally, those with low income and lack of a support system, especially those living alone, are at higher risk of becoming victims. Protective factors place an elder person at a lower risk for abuse. These include good health, financial stability, appropriate physical activity/physical ability, and a strong social support system. The important thing to remember is that elder abuse can occur across all cultures, races/ethnicities, and socioeconomic levels. There are no single identifiers that confirm or exclude an elder person from possible abuse.
Conversely, alleged perpetrators of elder abuse may suffer from issues that increase the risk of abuse to an elder person. Untreated medical and mental health issues such as mental illness, illegal substance abuse, and financial instability may all heighten the risk of abuse. Alleged abusers may be male or female, and in “almost 60% of elder abuse and neglect incidents,” the perpetrator is a family member” (7). “Two thirds of perpetrators are adult children or spouses,” who thus have had the opportunity to be well versed in knowing the victims physical and/or mental vulnerabilities (7).
Additionally, alleged perpetrators of elder abuse often have no other means of support, aside from the victim’s social security checks, personal savings, and housing (8). Many have a prior criminal record, suffer from mental illness or disabilities themselves, and frequently have a history of drug and alcohol abuse (8).

Self-Quiz
Ask Yourself...
- You suspect that an alleged elder abuse perpetrator is suffering from mental illness. What are your obligations to the suspected victim, in terms of their safety and well-being?
- How would you explain to the suspected victim that you must report your concerns to the local authorities? Consider your understanding of the term, “mandated reporter” as a licensed healthcare professional.
- How is the reporting of suspected abuse different (in your place of employment) for elder persons residing at home versus a long-term care facility?
- Why do you think that the majority of elder abuse perpetrators are immediate family members?
Prevention
The prevention of elder abuse is multifaceted. There is no single answer/action that prevents abuse in this vulnerable population. However, there are guidelines in place to maximize an elder person’s safety and well-being. The overall goal of elder abuse prevention is to lower the risk factors associated with heightening the occurrence of abuse. As nurses, we are in a pivotal position to advocate for the elder patient, as well as identify potential resources to benefit both patient and family (9).
The “accusation” of suspected abuse will most likely be ill-received. Caregivers, family members and others close to the elder person may feel threatened, defensive, and angry when a healthcare professional discusses their concerns over what appears to be suspected elder abuse.
The suspected victim may also feel humiliated, embarrassed, and fearful of law enforcement involvement. The suspected victim has most likely been abused by someone who has violated their trust and taken advantage of them. Therefore, it is possible that many victims of abuse are fearful of further retaliation, especially if the alleged perpetrator is an immediate family member.
When possible, the members of the healthcare team should interview caregivers and all suspected abusers separately from the alleged victim. Sometimes, subtle discrepancies between the suspected abuser and the victim interview may give unique insights worthy of further investigation.
Consider the following scenario. An elderly patient arrives via ambulance, from her private home, and appears malnourished, incontinent, and confused. As you document your findings, a team member voices concerns over suspected abuse. You are told the patient lives with an immediate family member. Initial calls are made to alert authorities of a possible elder abuse situation. The family member arrives, and states they are the patient’s primary caregiver.
- The primary caregiver is the 19-year-old granddaughter. What are your initial concerns over what appears to be neglect?
- The primary caregiver is the 78-year-old husband, appearing frail, walking with a cane, obviously undernourished. Do your concerns change?
- The primary caregiver is a 45-year-old son, unemployed, avoiding eye contact, appearing disheveled. Any additional concerns?
The nurse advocate must remain objective, nonjudgmental, and empathetic while investigating the situation. What initially appears as intentional abuse and neglect may also be due to the fact that many caregivers are also overwhelmed by the complexity of the situation, whether it be lack of knowledge, financial insecurity or mental/physical disabilities themselves.
The goal of nurse advocacy in these challenging situations is to fully assess not only the health and well-being of the elder, but that of the caregiver. All related documentation on a suspected abuse case must remain objective, reflecting only actual statements made by the patient and accompanying caregiver/ family member, as well as physical examination findings.
For guidance on medical record documentation when elder abuse is suspected, visit Documenting in the Medical Record by Stanford Medicine. ***Always check with your current worksite for site specific protocols/guidelines regarding approved documentation standards.
The current elder population is growing rapidly. By 2030, one in six people in the world will be aged 60 years or over. At this time the share of the population aged 60 years and over will increase from one billion in 2020 to 1.4 billion.
Common age-related health conditions occur often leading to complex medical issues at a time when finances, family/community support, safe housing options, and available resources may be in limited supply (10). Over time, the once healthy vibrant elder person can become frail, malnourished, depressed and isolated. This is the pivotal point in which many nurses first cross paths with the elder person.
A multidisciplinary team approach may be needed to address the various physical, mental and emotional needs of a vulnerable elder, dependent on the current health status, physical needs, and financial means. Team goals should include efforts to return the elder person to an environment best suited to support healthy eating, physical activity, a safe and affordable living environment, accessible transportation, and a supportive community.
Depending on the health status of the individual, the goal can vary the spectrum, from independent living to nursing home placement. Again, these efforts are best addressed by a multidisciplinary team approach.
In the acute phase, when elder abuse is suspected (or confirmed), the safety of the victim is the highest priority. As nurses, we are mandated to report all suspected abuse, including that of vulnerable adults. Your specific workplace should have written protocols regarding the reporting of suspected abuse, as well as guidelines of documentation of the suspected abuse.
Failure to do so may result in a variety of penalties, including but not limited to fines as well as criminal charges (ranging from misdemeanor to felony charges). It is imperative that you, as a licensed professional, become familiar with your state’s mandatory reporting laws (11).

Self-Quiz
Ask Yourself...
- Reflect on your current worksite. What community resources are available to assist with patient safe housing in suspected abuse cases?
- What members of your worksite multidisciplinary team can assist you with cases of suspected elder abuse?
- Do you feel comfortable in the role of nurse advocate? If not, what recommendations could you make to your organization to improve staff education in this area?
Reporting
As stated previously, a nurse’s workplace should have written protocols in place to report suspected elder abuse. The majority of states also have written guidelines in place for reporting suspected abuse. The United States Department of Health and Human Services also offers guidelines for all persons in the reporting of such abuse.
If the person is in immediate or life-threatening danger, the local authorities should be notified through 9-1-1. In the event that abuse is suspected, but there is no immediate threat to life or limb, the recommendation is to notify the local adult protective services (APS) or police department (12).


Self-Quiz
Ask Yourself...
- As a nurse professional, how can you advocate for the elder person / aging population outside of your worksite environment?
- As life expectancy rates continue to climb, what areas can healthcare professionals improve on with respect to elder patient care (assessment, documentation guidelines, treatment protocols)?
- Do you, as a nurse advocate, feel that there are any barriers to elder patient care that need to be addressed at your worksite? What outside agencies are available to assist you?
End of Life Considerations
According to the position statement on end of life care from the American Nurses’ Association, nurses “are often ideally positioned to contribute to conversations about end of life care and decisions, including maintaining a focus on patients’ preferences, and to establish mechanisms to respect the patient’s autonomy” (13). Similarly, a statement entitled “The Right to Self Determination” from the Code of Ethics for Nurses with Interpretive Statements also emphasizes the nurse’s role in end of life planning and care:
“The importance of carefully considered decisions regarding resuscitation status, withholding and with-drawing life-sustaining therapies, forgoing nutrition and hydration, palliative care, and advance directives is widely recognized. Nurses assist patients as necessary with these decisions. Nurses should promote advance care planning conversations and must be knowledgeable about the benefits and limits of various advance directive documents. The nurse should provide interventions to relieve pain and other symptoms in the dying process consistent with palliative care standards and may not act with the sole intent of ending a patient’s life” (13).
What these statements say is that nurses have ethical roles and responsibilities that are fundamental to nursing practice. Nurses should ensure that both patients and family members understand the options and treatments that have been presented to them, and should ensure that the patient’s autonomy is being respected throughout all aspects of their care. Nurses are first and foremost patient advocates, and this is especially crucial during the end of life stage. Nurse advocacy during this time can encompass anything from symptom and pain management, culturally sensitive care provision, and ethical decision making (14).
Talking to Patients and Families
Talking to a patient and their family about end of life care can be a huge challenge for nurses. In addition to managing patients’ and families’ emotions, nurses must manage their own emotions and approach the subject with professionalism as well as empathy.
Often, during the end of life planning phase, patients will go through the five stages of grief, as outlined in the book “On Death and Dying” by Elizabeth Kubler-Ross. The five stages of grief include (14):
Denial: Usually a temporary defense, patients may say that they’re fine, or that this is some mistake.
Anger: Once the patient is no longer in denial, anger is often the next stage. It may be difficult to care for the patient during this stage, as they may misplace their angry feelings on their caregivers.
Bargaining: At this stage, the patient seeks ways to postpone death – often in the form of promising to reform a lifestyle in exchange for more life.
Depression: This stage may involve the refusal of treatments or visitors, and the disconnection from people, love, and affection.
Acceptance: The final stage, which is not reached by all patients. In this stage, the patient has come to terms with their mortality and has accepted that death will happen.
It is important for the nurse to understand these five stages, as most patients will be experiencing one or more of the stages during the end of life process.
Here are some helpful techniques for nurses to use when talking to patients about hospice or end of life planning, according to the American Academy of Family Physicians (15):
Make sure you have time.
While this may seem impossible while on a shift when you have other patients, it’s imperative that a nurse allow enough time to have this difficult conversation. This is not a conversation that can be rushed – rushing through the conversation may make a nurse miss important details that the patient has shared.
Turn off your phone.
Minimizing distractions during these difficult conversations will ensure that the nurse can get ample information from this patient and family interaction.
Listen to the patient.
Above all, listen to what the patient is saying. Begin the conversation by asking what the patient and their doctor have already discussed. Be sure that the plan of care has been reviewed with the doctor prior to this conversation, then have the patient repeat their plan of care as they understand it. If there are major differences in the plan of care and what the patient says, this may warrant further conversation with the health care team to clarify and identify knowledge gaps.
Learn what the patient’s goals are.
Active listening is crucial during the conversation phase of end of life care planning. Once the nurse has determined that the patient understands the options that have been presented, it is vital to ask them what their goals are for palliative and comfort care. Understanding a patient’s goals can help identify what resources will be best suited for their individual needs.
Conversations surrounding end of life care should happen as soon as possible. Do not wait until the patient is no longer able to participate in the discussion. Encourage the presence of family members, but be sure to respect the patient’s wishes regarding who is involved in the planning process. Other members of the healthcare team that should be included in the planning process include social workers, patient navigators (if applicable in that setting), and any primary and specialist physicians involved in the patient’s care.

Self-Quiz
Ask Yourself...
- How important do you think nurses are to the decision-making process for end of life care?
- Why is it important to include the patient and family in conversations about end-of-life care?
- What are some ways in which abuse can occur during the end of life stage?
- If you were a hospice nurse and suspected elder abuse, to whom should you report this?
Additional Resources
The Elder Abuse Guide for Law Enforcement (EAGLE)
Use this website to review state-specific elder justice laws.
https://eagle.usc.edu/state-specific-laws/
National Adult Protective Services Association
Use this website to find specific contact information for your state location
https://www.napsa-now.org/help-in-your-area
ElderCare Locator/ United States Administration on Aging
Use this website to connect with services for older adults and families.
https://eldercare.acl.gov/Public/Index.aspx
World Elder Abuse Awareness Day
June 15th has been declared World Elder Abuse Awareness Day (WEAAD). For more information, visit https://eldermistreatment.usc.edu/weaad-home/. The website offers multi-language downloads on elder abuse facts, as well as social media guides, awareness campaigns, elder justice groups, and associated tool kits.
Conclusion
As the elder population continues to grow, so does the risk of elder abuse. As nurse professionals, we must continue to advocate for the safety and well-being of our aging population. We must continue to stay informed and educated on identifying abuse throughout the age spectrum.
Lastly, we must be knowledgeable of our own available resources to best assist the elder population and their basic needs, including food and shelter, access to healthcare, and transportation, as well as community wide support services.
References + Disclaimer
- American Nurses Association. (2015). Code of ethics with interpretative statements. Silver Spring, MD: Author. Available from URL: http://www.nursingworld.org/MainMenuCategories/EthicsStandards/CodeofEthicsforNurses/Code-of1.
- Texas Administrative Code, RULE §216.3 Continuing Competency Requirements. Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=N&p_rloc=193277&p_tloc=&p_ploc=1&pg=85&p_tac=&ti=22&pt=11&ch=216&rl=3
- Texas Administrative Code, RULE §217.1 Nursing Jurisprudence Exam (NJE). Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=P&p_rloc=123209&p_tloc=&p_ploc=1&pg=111&p_tac=&ti=22&pt=11&ch=216&rl=3
- Texas Administrative Code, RULE 217.11 Standards of Nursing Practice. Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=N&p_rloc=113468&p_tloc=&p_ploc=1&pg=103&p_tac=&ti=22&pt=11&ch=216&rl=3
- Texas Administrative Code, RULE §217.12 Unprofessional Conduct. Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=N&p_rloc=133132&p_tloc=&p_ploc=1&pg=104&p_tac=&ti=22&pt=11&ch=216&rl=3
- Texas Board of Nursing, Nursing Board Position Statements. Available from URL: https://www.bon.texas.gov/practice_bon_position_statements_content.asp#15.28
- Texas Board of Nursing, Professional Boundaries Including the Use of Social Media by Nurses. Available from URL: https://www.bon.texas.gov/practice_bon_position_statements_content.asp#15.28
- Texas Board of Nursing, Rule §213.33(b)-Texas Board of Nursing Disciplinary Matrix. Available from URL: https://www.bon.texas.gov/pdfs/disciplinaryaction_pdfs/discp-matrix.pdf
- Texas Board of Nursing, Texas Board of Nursing Position Statement. Available from URL: https://www.bon.texas.gov/pdfs/practice_dept_pdfs/position_statements_pdfs/15.28mar20.pdf
- Texas Board of Nursing, Texas Board of Nursing – Practice – Registered Nurse Scope of Practice. Available from URL: https://www.bon.texas.gov/practice_scope_of_practice_rn.asp
- Texas Board of Nursing, The Registered Nurse Scope of Practice. Available from URL: https://www.bon.texas.gov/practice_bon_position_statements_content.asp#15.28
- Texas Board of Nursing Website, Available from URL: bon.texas.gov
- (2003) Institute on Domestic Violence and sexual assault. The University of Texas at Austin A Health survey of Texans: A focus on Sexual Assault Retrieved from: https://sites.utexas.edu/idvsa/?s=focus+on+sexual+assault
- (2015) The University of Texas. Stephen Hicks school of Social Work HEALTH AND WELL-BEING: Texas Statewide Sexual Assault Prevalence Study Final Report Retrieved from: https://sites.utexas.edu/idvsa/files/2019/03/TX-SA-Prevalence-Study-Final-Report.pdf
- (2015) National Alliance to End Sexual Violence. The Costs and Consequences of Sexual Violence and Cost-Effective Solutions. Retrieved from: https://endsexulavilolence.org/where_we_stand/costs-consequences-and-solutions
- (2021) Miller, Ted R; Cohen, Mark A; Wiersema, Brian; Victim Costs and Consequences: A New Look National Institutes of Justice Retrieved from: https://www.ojp.gov/pdffiles/victcost.pdf
- Office of Justice Programs. Office of Victims of Crime. SANE Program Development and Operation Guide. Retrieved from: https://www.ovcttac.gov/saneguide/introduction/what-is-a-sane
- Prescott Valley, Arizona official government site. Retrieved from: https://www.pvaz.net/DocumentCenter/View/8943/Common-Feelings-of-Survivors-of-Sexual-Assault
- RAINN articles: What is a SANE/SART? Retrieved from: https://www.rainn.org/articles/what-sanesart
- Texas A&M, College of Nursing, et al. Texas Attorney General Sexual Assault Prevention and Crisis Services Program. TEXAS EVIDENCE COLLECTION PROTOCOL Retrieved from: https://nursing.tamu.edu/documents/txecp-final-08212019.pdf
- Texas Legislature Online. Evidence Collection Protocol Kits. Retrieved from: https://statutes.capitol.texas.gov/Docs/GV/htm/GV.420.htm
- (2021) RAINN state database, Texas. Understanding Statute of Limitations of Sex Crimes Retrieved from: https://apps.rainn.org/policy/policy-crime-definitions.cfm?state=Texas&group=7
- RAINN. Stat Pearls. What is a Sexual Assault Forensic Exam? Retrieved from: https://rainn.org/articles/rape-kit 3/2/2021
- (2020) Slate, Melissa, RN, BA, MA, Forensic Evidence Collection for Nurses. Retrieved from: https://www.Rn.org/courses/coursematerial-173.pdf
- Victims of Trafficking and Violence Protection Act of 2000, Pub. L. No. 106-386 (2000). https://www.govinfo.gov/content/pkg/PLAW-106publ386/pdf/PLAW-106publ386.pdf
- 22 U.S. Code § 7102—Definitions. (n.d.). LII / Legal Information Institute. https://www.law.cornell.edu/uscode/text/22/7102
- Homeland Security. (2022). What Is Human Trafficking? https://www.dhs.gov/blue-campaign/what-human-trafficking
- United States Department of Defense (n.d.) Trafficking in Persons 101. https://ctip.defense.gov/Portals/12/Trafficking_in_Persons_101_Fact_Sheet_2020.pdf
- National Human Trafficking Hotline. (2023). Myths & Facts. https://humantraffickinghotline.org/en/human-trafficking/myths-facts
- United States Department of State (2022). Understanding Human Trafficking. https://www.state.gov/what-is-trafficking-in-persons/
- Department of Health and Human Services USA (2017). FACT SHEET: Human Trafficking. https://www.acf.hhs.gov/sites/default/files/documents/otip/fact_sheet_human_trafficking_fy18.pdf
- United States Department of Labor (2022). 2022 List of Goods Produced by Child Labor or Forced Labor. https://www.dol.gov/sites/dolgov/files/ILAB/child_labor_reports/tda2021/2022-TVPRA-List-of-Goods-v3.pdf
- Homeland Security. (2022). What is Forced Labor? https://www.dhs.gov/blue-campaign/forced-labor
- United States Department of State (n.d.). What Is Modern Slavery? https://www.state.gov/what-is-modern-slavery/#recruitment
- Polaris Project (2021). Human Trafficking 101. https://polarisproject.org/human-trafficking-101/
- Polaris Project (2023). Vulnerabilities and Recruitment. https://polarisproject.org/vulnerabilities-and-recruitment/
- Polaris Project (2023). Love and Trafficking. https://polarisproject.org/love-and-trafficking/
- National Human Trafficking Hotline (2023). Recognizing the Signs. https://humantraffickinghotline.org/en/human-trafficking/recognizing-signs
- National Human Trafficking Hotline (2023). Human Trafficking. https://humantraffickinghotline.org/en/human-trafficking
- Texas Attorney General (n.d.). Red Flags for Labor Trafficking. https://www.texasattorneygeneral.gov/human-trafficking-section/signs-trafficking/red-flags-labor-trafficking
- United Against Human Trafficking (2020). Prostitution and Human Trafficking: What’s the Difference? https://uaht.org/prostitution-and-human-trafficking/
- United States Department of State (2020). 2020 Trafficking in Persons Report. https://www.state.gov/wp-content/uploads/2020/06/2020-TIP-Report-Complete-062420-FINAL.pdf
- National Human Trafficking Resource Center (n.d.). Recognizing and Responding to Human Trafficking in a Healthcare Context. https://humantraffickinghotline.org/sites/default/files/Recognizing%20and%20Responding%20to%20Human%20Trafficking%20in%20a%20Healthcare%20Context_pdf.pdf
- Mukherji, P. (2015). Recognizing Human Trafficking Victims in the Emergency Department. Emergency Medicine Reports. https://www.reliasmedia.com/articles/134799-recognizing-human-trafficking-victims-in-the-emergency-department
- Hachey, L. M., & Phillippi, J. C. (2017). Identification and Management of Human Trafficking Victims in the Emergency Department. Advanced Emergency Nursing Journal, 39(1), 31–51. https://doi.org/10.1097/TME.0000000000000138
- Office for Victims of Crime Training and Technical Assistance Center (2012). Human Trafficking. https://www.ovcttac.gov/downloads/resourceLibrary/General/Color_HumanTraffickingResourcePaper12_final_508c_9132012.pdf
- Human Trafficking Institute (2019). On this day in history: The Trafficking Victims Protection Act passed in Congress. https://traffickinginstitute.org/on-this-day-in-history-the-trafficking-victims-protection-act-passed-in-congress/
- Office of the High Commissioner for Human Rights (2000). Protocol to Prevent, Suppress and Punish Trafficking in Persons Especially Women and Children, supplementing the United Nations Convention against Transnational Organized Crime. https://www.ohchr.org/en/instruments-mechanisms/instruments/protocol-prevent-suppress-and-punish-trafficking-persons
- Alliance to End Slavery and Trafficking (ATEST). (2017). Summary of the Trafficking Victims Protection Act (TVPA) and Reauthorizations FY 2017. https://endslaveryandtrafficking.org/summary-trafficking-victims-protection-act-tvpa-reauthorizations-fy-2017-2/
- Child Welfare Information Gateway (2023). Human Trafficking and Child Welfare: A Guide for Caseworkers. https://www.childwelfare.gov/pubPDFs/trafficking_caseworkers.pdf
- Polaris Project (2018). On-ramps, intersections, and exit routes: A roadmap for systems and industries to prevent and disrupt human trafficking. Health Care. https://polarisproject.org/wp-content/uploads/2018/08/A-Roadmap-for-Systems-and-Industries-to-Prevent-and-Disrupt-Human-Trafficking-Health-Care.pdf
- Office for Victims of Crime Training and Technical Assistance Center (n.d.) Human Trafficking Task Force e-Guide. https://www.ovcttac.gov/taskforceguide/eguide/3-operating-a-task-force/34-addressing-common-operational-challenges/interpreters/
- National Human Trafficking Training and Technical Assistance Center (n.d.). Barriers that prevent identification. https://nhttac.acf.hhs.gov/soar/eguide/observe/Barriers_to_Screening_and_Responding
- National Human Trafficking Training and Technical Assistance Center (n.d.). Language accessibility communication and language assistance. https://nhttac.acf.hhs.gov/soar/eguide/ask/Language%20Accessibility
- Substance Abuse and Mental Health Services Administration (2022). Trauma and violence. (2022) https://www.samhsa.gov/trauma-violence
- SAMHSA’s Trauma and Justice Strategic Initiative (2014). SAMHSA’s concept of trauma and guidance for a trauma-informed approach
- National Human Trafficking Training and Technical Assistance Center (2018). Adult human trafficking screening tool and guide. https://nhttac.acf.hhs.gov/sites/default/files/2018-07/adult_human_trafficking_screening_tool_and_guide.pdf
- National Human Trafficking Hotline (2008). Potential indicators of human trafficking https://humantraffickinghotline.org/en/resources/potential-indicators-human-trafficking
- National Human Trafficking Training and Technical Assistance Center (n.d.). Create and maintain safety. https://nhttac.acf.hhs.gov/soar/eguide/ask/Safety_is_Top_Priority
- Toney-Butler, T. J., Ladd, M., & Mittel, O. (2023). Human Trafficking. Stat Pearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK430910/
- Baldwin, S.B., Barrows, J., Stoklosa, H. (2017). Protocol Toolkit for Developing a Response to Victims of Human Trafficking. HEAL Trafficking & Hope for Justice. https://healtrafficking.org/wp-content/uploads/2022/08/HEAL-Trafficking-Protocol-Toolkit.pdf
- Texas Constitution and Statues (2015). Human Resources Code, Chapter 48: Investigations and protective services for elderly persons and persons with disabilities. https://statutes.capitol.texas.gov/Docs/HR/htm/HR.48.htm
- Texas Constitution and Statutes (2023). Family Code, Title 5: The parent-child relationship and the suit affecting the parent-child relationship. https://statutes.capitol.texas.gov/Docs/FA/htm/FA.261.htm
- Texas Health and Human Services Commission (2016). Welcome to the Texas Department of Family Abuse Hotline Website. https://www.txabusehotline.org/Login/Default.aspx
- Texas Human Trafficking Prevention Task Force (2014). Introduction to Human Trafficking: A Guide for Texas Education Professionals. https://www.texasattorneygeneral.gov/sites/default/files/files/divisions/criminal-justice/IntroHumanTrafficking2014.pdf
- National Human Trafficking Training and Technical Assistance Center (n.d.). Law Enforcement. https://nhttac.acf.hhs.gov/soar/eguide/resources_by_profession/Law_Enforcement
- Center for Substance Abuse Treatment (US) (2014). Trauma-Informed Care in Behavioral Health Services. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); Treatment Improvement Protocol (TIP) Series, No. 57.) Chapter 3, Understanding the Impact of Trauma. https://www.ncbi.nlm.nih.gov/sites/books/NBK207191/
- Treatment (US), C. for S. A. (2014). Understanding the Impact of Trauma. In Trauma-Informed Care in Behavioral Health Services. Substance Abuse and Mental Health Services Administration (US). https://www.ncbi.nlm.nih.gov/sites/books/NBK207191/
- Survivor Alliance (n.d.) Overview for Survivors. https://www.survivoralliance.org/survivors-overview
- Dovydaitis T. (2010). Human trafficking: the role of the health care provider. J Midwifery Women’s Health: 55(5):462-7. Doi: 10.1016/j.jmwh.2009.12.017. PMID: 20732668; PMCID: PMC3125713.
- Texas Health and Human Services (2023). Texas Human Trafficking Resource Center https://www.hhs.texas.gov/services/safety/texas-human-trafficking-resource-center
- US Department of Health & Human Services. (n.d.). Multidisciplinary Treatment and Referral Team. https://nhttac.acf.hhs.gov/soar/eguide/resources/Building_a_Referral_Network
- SimpliMBA (2023). SWOT Analysis. Retrieved from https://www.simplimba.com/swot-analysis-for-personal-development/
- Anusiewicz, C. V., Ivankova, N. V., Swiger, P. A., Gillespie, G. L., Li, P., & Patrician, P. A. (2020). How does workplace bullying influence nurses’ abilities to provide patient care? a nurse perspective. Journal of Clinical Nursing, 29(21-22), 4148–4160. https://doi.org/10.1111/jocn.15443
- Collins, B. (2022). Mobbing and workplace bullying among registered nurses in Mississippi. ABNFF Journal, 1(2), 20–28.
- Edmonson, C., & Zelonka, C. (2019). Our own worst enemies. Nursing Administration Quarterly, 43(3), 274–279. https://doi.org/10.1097/naq.0000000000000353
- Harassment definition & meaning. (n.d.). Dictionary.com. https://www.dictionary.com/browse/harassment
- Meires, J. (2018). Workplace incivility – the essentials: Here’s what you need to know about bullying in nursing. Urologic Nursing, 38(2), 95. https://doi.org/10.7257/1053-816x.2018.38.2.95
- Thompson, R. (Feb 2022). Getting Clear on Bullying Versus Incivility. Florida Nurse, 70(1), 19–19.
- Agency for Healthcare Research and Quality (AHRQ). (2021). Benchmarking for Quality Improvement. https://digital.ahrq.gov/health-it-tools-and-resources/evaluation-resources/workflow-assessment-health-it-toolkit/all-workflow-tools/benchmarking
- Agency for Healthcare Research and Quality (AHRQ). (2021). Data Collection and Management. https://www.ahrq.gov/talkingquality/measures/data-collection.html
- Agency for Healthcare Research and Quality (AHRQ). (2021). Nursing-sensitive indicators: AHRQ quality indicators. https://www.qualityindicators.ahrq.gov/Modules/nursing-sensitive_indicators.aspx
- Agency for Healthcare Research and Quality (AHRQ). (2019). TeamSTEPPS 2.0: Strategies and Tools to Enhance Performance and Patient Safety. https://www.ahrq.gov/teamstepps/index.html
- Agency for Healthcare Research and Quality (AHRQ). (2021). Types of Measures. https://www.ahrq.gov/talkingquality/measures/types.html
- Centers for Medicare & Medicaid Services (CMS). (2021). Quality Improvement and Evaluation System (QIES). https://www.cms.gov/medicare/health-safety-standards/quality-safety-oversight-general-information/iqies
- Deming, W. E. (1986). Out of the Crisis. MIT Press.
- Dowding, D., Randell, R., Gardner, P., Fitzpatrick, G., Dykes, P., & Favela, J. (2019). Dashboards for improving patient care: Review of the literature. International Journal of Medical Informatics, 124, 87-97. https://doi.org/10.1016/j.ijmedinf.2019.01.008
- Feldstein, A. C., Glasgow, R. E., Smith, D. H., & Aickin, M. (2019). Six-Sigma: A case study in a community health center. The Joint Commission Journal on Quality and Patient Safety, 45(2), 96-104. doi:10.1016/j.jcjq.2018.05.002
- George, M. L. (2020). Lean Six Sigma for Service: How to Use Lean Speed and Six Sigma Quality to Improve Services and Transactions (2nd ed.). McGraw-Hill Education.
- George, M. L., Rowlands, D., & Price, M. (2015). The Lean Six Sigma Pocket Tool book: A Quick Reference Guide to 100 Tools for Improving Quality and Speed. McGraw-Hill Education.
- Institute for Healthcare Improvement (IHI). (2020). Introduction to Quality Improvement. https://www.ihi.org/education/IHIOpenSchool/Courses/Pages/QualityImprovement.aspx
- Institute for Healthcare Improvement. (2019). What is Quality Improvement? https://www.ihi.org/education/IHIOpenSchool/Courses/Pages/QualityImprovement.aspx
- Institute of Medicine (IOM). (2001). Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press.
- Johnson, J. K., & Jolivet, R. R. (2018). Applying Kotter’s 8-Step Change Model in Nursing. Nurse Leader, 16(2), 117-119. https://doi.org/10.1016/j.mnl.2017.09.005
- Joynt Maddox, K. E., Orav, E. J., Zheng, J., Epstein, A. M. (2018). Evaluation of Medicare’s Bundled Payments Initiative for Medical Conditions. New England Journal of Medicine, 379(3), 260-269. doi:10.1056/NEJMsa1801569
- Langley, G. J., Moen, R. D., Nolan, K. M., Nolan, T. W., Norman, C. L., & Provost, L. P. (2009). The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. Jossey-Bass.
- Leonard, M., Graham, S., & Bonacum, D. (2004). The human factor: Effective teamwork and communication is critical in providing safe care. Quality and Safety in Health Care, 13(Suppl 1), i85-i90. doi:10.1136/qshc.2004.010033
- Mazzocato, P., Savage, C., Brommels, M., Aronsson, H., & Thor, J. (2010). Lean thinking in healthcare: A realist review of the literature. Quality & Safety in Health Care, 19(5), 376-382. doi:10.1136/qshc.2009.037986
- National Academies of Sciences, Engineering, and Medicine. (2018). Crossing the Global Quality Chasm: Improving Health Care Worldwide. National Academies Press.
- National Quality Forum (NQF). (2021). Safe Practices for Better Healthcare – 2021-2022. https://www.qualityforum.org/News_And_Resources/Press_Kits/Safe_Practices_for_Better_Healthcare.aspx
- Radnor, Z. J., & Holweg, M. (2012). Lean in healthcare: The unfilled promise? Social Science & Medicine, 74(3), 364-371. doi:10.1016/j.socscimed.2011.02.011
- Schweickert, P., Keller, M., & Reber, A. (2019). Using data to drive quality improvement in nursing: A guide. Journal of Nursing Management, 27(7), 1404-1408. https://doi.org/10.1111/jonm.12829
- Wheeler, D. J. (2003). Deming’s Profound Changes: When Will the Sleeping Giant Awaken? SPC Press.
- Womack, J. P., Jones, D. T., & Roos, D. (2019). The Machine That Changed the World: The Story of Lean Production–Toyota’s Secret Weapon in the Global Car Wars That Is Now Revolutionizing World Industry. Free Press.
- Arnetz, J. E. (2022, April). The Joint Commission’s new and revised Workplace violence prevention standards for hospitals: A major step forward toward improved quality and safety. Joint Commission journal on quality and patient safety. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8816837/
- American Nurses Association. (2019, January). Reporting incidents of Workplace Violence – Ana Enterprise. Reporting Incidents of Workplace Violence. https://www.nursingworld.org/~495349/globalassets/docs/ana/ethics/endabuse-issue-brief-final.pdf
- Occupational Safety and Health Administration. (n.d.). Healthcare – workplace violence. https://www.osha.gov/healthcare/workplace-violence/
- Minnesota Nurses Association. (2022, August 10). Hennepin Healthcare Nurses report rising violence against nurses and patients, cite under-staffing, unresponsive management as barriers in new survey. Minnesota Nurses Association. https://mnnurses.org/hennepin-healthcare-nurses-report-rising-violence-against-nurses-and-patients-cite-under-staffing-unresponsive-management-as-barriers-in-new-survey/
- ANA) Workplace violence. (2017). https://www.nursingworld.org/practice-policy/advocacy/state/workplace-violence2/
- Sahebi, A., Golitaleb, M., Moayedi, S., Torres, M., & Sheikhbardsiri, H. (2022, August 8). Prevalence of workplace violence against health care workers in hospital and pre-hospital settings: An umbrella review of meta-analyses. Frontiers in public health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9393420/#:~:text=The%20overall%20prevalence%20of%20WPV,%2C%20and%2010.5%25%20(95%25
- Song, C., Wang, G., & Wu, H. (2020, December 3). Frequency and barriers of reporting workplace violence in nurses: An online survey in China. International Journal of Nursing Sciences. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7859538/
- Staff, A. (2022, November 4). End Nurse Abuse: 4 Actions You Can Take Today. Aorn.org. https://www.aorn.org/article/2021-12-03-End-Nurse-Abuse
- Fountain, D., Zankowski, D., & Arriola, J. (n.d.). Reporting incidents of Workplace Violence – Ana Enterprise. Reporting incidents of Workplace Violence. https://www.nursingworld.org/~495349/globalassets/docs/ana/ethics/endabuse-issue-brief-final.pdf
- S. Bureau of Labor Statistics. (n.d.). Workplace violence in healthcare, 2018. U.S. Bureau of Labor Statistics. https://www.bls.gov/iif/factsheets/workplace-violence-healthcare-2018.htm
- Vincent-Höper, S., Stein, M., Nienhaus, A., & Schablon, A. (2020, May 1). Workplace aggression and burnout in nursing-the moderating role of follow-up counseling. International journal of environmental research and public health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7246829/
- Creating a culture of safety in nursing. ANA. (2023, September 12). https://www.nursingworld.org/resources/individual/nurse-managers/safety-in-nursing/
- AlGhatrif, M., & Lindsay, J. (2012). A brief review: History to understand fundamentals of electrocardiography. Journal of Community Hospital Internal Medicine Perspectives, 2(1), 14383. https://doi.org/10.3402/jchimp.v2i1.14383
- Alila Medical Media. (2017). Cardiac action potential, animation. [YouTube Video]. In YouTube. https://www.youtube.com/watch?v=v7Q9BrNfIpQ
- American Heart Association. (2016). Ventricular fibrillation. Www.heart.org. https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia/ventricular-fibrillation
- Atkielski, A. (2023). PQRST segment. In StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK551635/figure/article-20939.image.f1/?report=objectonly
- Benzoni, T., & Cascella, M. (2021). Procedural sedation. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551685/
- Bern Dibner. (2018). Luigi Galvani | Italian physician and physicist. In Encyclopædia Britannica. https://www.britannica.com/biography/Luigi-Galvani
- Birnbaum, Y., Ye, Y., Smith, S. W., & Jneid, H. (2021). Rapid diagnosis of STEMI equivalent in patients with left bundle‐branch block: Is it feasible? Journal of the American Heart Association, 10(18). https://doi.org/10.1161/jaha.121.023275
- Bracey, A. (2023). Posterior MI. In nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK553168/figure/article-698.image.f1/?report=objectonly
- Burns, E., & Buttner, R. (2021). PVCs. In com. https://litfl.com/premature-ventricular-complex-pvc-ecg-library/
- Burns, E., & Buttner, R. (2023a). Anterior MI. In com. https://litfl.com/anterior-myocardial-infarction-ecg-library/)
- Burns, E., & Buttner, R. (2023b). Monomorphic vtach. In com. https://litfl.com/ventricular-tachycardia-monomorphic-ecg-library/
- Burns, E., & Buttner, R. (2023c). Torsades de Pointes. In com. https://litfl.com/polymorphic-vt-and-torsades-de-pointes-tdp/
- Cadogan, M. (2018, August 1). Delta wave. Life in the Fast Lane. https://litfl.com/delta-wave-ecg-library/
- Cadogan, M. (2022). Lead positioning. In com. https://litfl.com/ecg-lead-positioning/
- Cardiac Science. (2021). ECG graph paper. In ca. https://cardiacsciencesmb.ca/ecg-graph-paper/
- Cardogan, M., & Buttner, R. (2021). Sgarbossa criteria. In com. https://litfl.com/sgarbossa-criteria-ecg-library
- Cascino, T., & Shea, M. (2022, September). Electrocardiography – cardiovascular disorders. MSD Manual Professional Edition. https://www.msdmanuals.com/professional/cardiovascular-disorders/cardiovascular-tests-and-procedures/electrocardiography
- Center for Advanced Cardiac and Vascular Interventions. (2023). Mobile cardiac telemetry (MCT). Center for Advanced Cardiac and Vascular Interventions. https://cacvi.org/services/diagnostic-procedures/mobile-cardiac-telemetry/
- Center for Drug Evaluation and Research. (2021, January 8). FDA drug safety communication: New information regarding QT prolongation with ondansetron (zofran). https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-new-information-regarding-qt-prolongation-ondansetron-zofran
- Chruścik, A., Kauter, K., Windus, L., & Whiteside, E. (2021). 6.2 cardiac muscle and electrical activity. In pressbooks.pub. University of Southern Queensland. https://usq.pressbooks.pub/anatomy/chapter/6-2-cardiac-muscle-and-electrical-activity/
- Cleveland Clinic. (2022a). Asystole. In clevelandclinic.org. https://my.clevelandclinic.org/health/symptoms/22920-asystole
- Cleveland Clinic. (2022b, June 3). Pulseless electrical activity (PEA): Causes and treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/23213-pulseless-electrical-activity
- Cleveland Clinic. (2022c, June 11). Cardiac event monitor: Types and uses. Cleveland Clinic. https://my.clevelandclinic.org/health/diagnostics/23272-cardiac-event-monitor
- Clip Art Library. (2023). EKG machine. In https://clipart-library.com/clipart/2049261.htm.
- Cohagan, B., & Dov Brandis. (2019, February 17). Torsade de Pointes. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459388/
- Costa, C. (2016). Figure 2.1: A) basic cardiac anatomy and blood circulation through the… In ResearchGate. ResearchGate. https://www.researchgate.net/figure/A-Basic-cardiac-anatomy-and-blood-circulation-through-the-hearts-cavities-and-valves_fig20_320411039
- de Jong, J. (2007a). 2nd AV block. In org. https://en.ecgpedia.org/index.php?title=File:Wenckebach2.png
- de Jong, J. (2007b). A fib. In org. https://en.ecgpedia.org/index.php?title=File:Afib_ecg.jpg
- de Jong, J. (2007c). Normal sinus rhythm. In org. https://en.ecgpedia.org/index.php?title=File:Nsr.jpg
- de Jong, J. (2008). SVT. In org. https://en.ecgpedia.org/index.php?title=File:Avrt_small.svg
- de Jong, J. (2009). A flutter. In org. https://en.ecgpedia.org/index.php?title=File:ECG000011.jpg
- de Jong, J. (2010a). 1st AV block. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_1stAVblock.png
- de Jong, J. (2010b). 3rd AV block. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_3rdAVblock.png
- de Jong, J. (2010c). A fib RVR. In org. https://en.ecgpedia.org/index.php?title=File:Afib_f_VR_ecg.jpg
- de Jong, J. (2010d). Bigeminy PVC. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_bigemini.png
- de Jong, J. (2010e). Idioventricular rhythm. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_idioventricular.png
- de Jong, J. (2010f). PAC. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_premature.png
- de Jong, J. (2010g). PVCs. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_ventricular_premature.png
- de Jong, J. (2010h). Ventricular fibrillation. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_ventricular_fibrillation.png
- de Jong, J. (2011a). Mobitz. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_Mobitz.png
- de Jong, J. (2011b, December 13). Normal tracing. En.ecgpedia.org. https://en.ecgpedia.org/index.php?title=Normal_Tracing
- de Jong, J. (2011c). Sinus tachycardia. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_tachycardia.png
- Dmitriy Scherbak, & Hicks, G. J. (2019, April 7). Left bundle branch block (LBBB). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482167/
- Douedi, S., & Douedi, H. (2020). P wave. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551635/
- Foth, C., Manesh Kumar Gangwani, & Alvey, H. (2020, January 13). Ventricular Tachycardia (VT, V Tach). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532954/
- Foth, C., & Mountfort, S. (2022). Acute myocardial infarction ST elevation (STEMI). National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532281/
- Gangwani, M. K., & Nagalli, S. (2020). Idioventricular rhythm. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK554520/
- GE HealthCare. (2023a). Apexpro ch telemetry system patient monitors. Www.gehealthcare.com. https://www.gehealthcare.com/products/patient-monitoring/patient-monitors/apexpro-ch-telemetry-system
- GE HealthCare. (2023b). Cardiac beside monitor. In com. https://www.gehealthcare.com/products/patient-monitoring/patient-monitors/carescape-monitor-b650
- Glenlarson . (2023). Inferior MI. In nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK470572/figure/article-23500.image.f1/?report=objectonly
- Gray, D. (2016). How to read an electrocardiogram (EKG/ECG) (K. Gaines , Ed.). Nurse.org. https://nurse.org/articles/how-to-read-an-ECG-or-EKG-electrocardiogram/
- Hafeez, Y., & Grossman, S. A. (2020). Junctional rhythm. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507715/
- Harkness, W. T., & Hicks, M. (2019, June 3). Right bundle branch block (RBBB). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507872/
- Heaton, J., & Yandrapalli, S. (2021). Premature atrial contractions. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559204/
- Henning, A., & Krawiec, C. (2022, August 8). Sinus tachycardia. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK553128/
- Ibrahim, H. (2022a, May 19). ECG tip 20. what about “orthodromic” SVT?youtube.com. https://www.youtube.com/watch?v=XcnU7mGKdis
- Ibrahim, H. (2022b, May 24). ECG tip 21. what about “antidromic” SVT?youtube.com. https://www.youtube.com/watch?v=qTaNeoGEKJc
- Johns Hopkins Medicine. (2019). Holter monitor. John Hopkins Medicine. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/holter-monitor
- Jordan, M. R., Lopez, R. A., & Morrisonponce, D. (2020). Asystole. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430866/
- Mangi, M. A., Jones, W. M., & Napier, L. (2019, November 6). Atrioventricular block second-degree. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482359/
- Mayo Clinic. (2017). Implantable cardioverter-defibrillators (ICDs). Mayoclinic.org. https://www.mayoclinic.org/tests-procedures/implantable-cardioverter-defibrillators/about/pac-20384692
- Mayo Clinic. (2019). Acute coronary syndrome – symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/acute-coronary-syndrome/symptoms-causes/syc-20352136
- Mayo Clinic. (2023, July 26). Atrial fibrillation – symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/atrial-fibrillation/symptoms-causes/syc-20350624
- McMurray, P. (2018). PVCs multiform. In com. https://bossrn.com/pvc
- Miner, B., Grigg, W. S., & Hart, E. H. (2020a). Wellens syndrome. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482490/
- Mountfort, S. (2023). Lateral MI. In nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK537228/figure/article-24110.image.f2/?report=objectonly
- National Heart, Lung, and Blood Institute. (2022). Atherosclerosis . In nih.gov. https://www.nhlbi.nih.gov/health/atherosclerosis
- Oldroyd, S. H., & Makaryus, A. N. (2020). First degree heart block. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448164/
- Osmosis by Elsevier. (2023). Cardiac electrophysiology notes: Diagrams & illustrations. Www.osmosis.org. https://www.osmosis.org/notes/Cardiac_Electrophysiology#page-1
- Oxford Medical Education. (n.d.). ECG (EKG) – bundle branch block. Oxford Medical Education. https://oxfordmedicaleducation.com/ecgs/bundle-branch-block/
- Parker, S. (n.d.). Telemetry – MeSH – NCBI. Www.ncbi.nlm.nih.gov. Retrieved September 8, 2023, from https://www.ncbi.nlm.nih.gov/mesh/?term=telemetry
- Patti, L., & Ashurst, J. V. (2019, June 4). Supraventricular tachycardia (SVT). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441972/
- Rodriguez Ziccardi, M., Goyal, A., & Maani, C. V. (2020). Atrial flutter. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK540985/
- RWJ Barnabas Health. (2023). Telemetry monitor technician. In org. https://www.rwjbh.org/community-medical-center/treatment-care/heart-and-vascular-care/programs-and-specialties/centralized-cardiac-telemetry-monitoring-program/
- Sandau, K. E., Funk, M., Auerbach, A., Barsness, G. W., Blum, K., Cvach, M., Lampert, R., May, J. L., McDaniel, G. M., Perez, M. V., Sendelbach, S., Sommargren, C. E., & Wang, P. J. (2017). Update to practice standards for electrocardiographic monitoring in hospital settings: A scientific statement from the American Heart Association. Circulation, 136(19). https://doi.org/10.1161/cir.0000000000000527
- Sattar, Y. (2023). Lead placement. In StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK549803/figure/article-20969.image.f1/?report=objectonly
- Sklavos, T. (2020, November 3). ECG interpretation: Myocardial ischaemia and infarction. LITFL. https://litfl.com/ecg-interpretation-myocardial-ischaemia-and-infarction/
- Slane, M., Knabben, V., & Chhabra, L. (2019). Third-Degree atrioventricular block. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK545199/
- Smith, S. (2014). Wide complex SVT. In hqmeded-ecg.blogspot.com. https://hqmeded-ecg.blogspot.com/2014/12/wide-complex-tachycardia-lewis-leads-do.html
- Vincent’s Hospital. (n.d.). Holter monitor. In svhhearthealth.com.au. https://www.svhhearthealth.com.au/Images/UserUploadedImages/976/10_HolterMonitor.jpg
- Thanassoulis, G., & Aziz, H. (2018). Atherosclerosis. Merck Manuals Professional Edition; Merck Manuals. https://www.merckmanuals.com/professional/cardiovascular-disorders/arteriosclerosis/atherosclerosis
- The Univeristy of Nottingham. (n.d.-a). Bipolar Leads. Www.nottingham.ac.uk. https://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/bipolar_leads.php
- The University of Nottingham. (n.d.-b). Limb leads. Www.nottingham.ac.uk. https://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/limb_leads.php
- University of Utah Health. (n.d.). ECG learning center – an introduction to clinical electrocardiography. Utah.edu. https://ecg.utah.edu/lesson/9
- Wisconsin Technical College System. (2021). 3 cardiovascular assessment. Wtcs.pressbooks.pub. https://wtcs.pressbooks.pub/nursingskills/chapter/9-3-cardiovascular-assessment/
- Wong, E. (2013). Action potential of cardiac muscles. In org. http://www.pathophys.org/physiology-of-cardiac-conduction-and-contractility/actionpotential/
- Yamama Hafeez, & Grossman, S. A. (2019, November 18). Sinus bradycardia. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK493201/
- Yasar Sattar, & Hashmi, M. F. (2019, December 3). Ventricular premature complexes. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK547713/
- Zeid Nesheiwat, Amandeep Goyal, & Mandar Jagtap. (2022). Atrial fibrillation . Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK526072/
- Zimmermann, P., & Hammond, B. (2023). Sheehy’s manual of emergency care. (8th ed.). Elsevier Health Sciences.
- ZOLL Medical Corporation. (2023). X series cardiac monitor/defibrillator for EMS – ZOLL medical. Www.zoll.com. https://www.zoll.com/products/defibrillators/x-series-for-ems
- Mayo Clinic Staff. Heart Failure at Mayo Clinic as retrieved from: https://www.ahajournals.org/doi/10.116/CIRCRESAHA.121.318172
- Roger, Veronique L., Epidemiology of Heart Failure. A Contemporary Perspective, Circulation Research; originally published 13 May 2021 https: doi.org/10.16/CIRCRESAHA.121.318172. Circulation Research, 2021 128:1421-1434
- Centers for Disease Control and Prevention. CDC.gov. Article: Heart Failure. retrieved https://www.cdc.gov/heartdisease/heart_failure.htm
- Schwinger, Robert H.G. Pathophysiology of heart failure. 2021 Feb;11 (1):263-276 doi: 10.21037-20-302. Retrieved from: https//: ncbinim,nih.gov/pmc/articles/PMC7944197/
- American Red Cross. Heart-Health Screenings. Retrieved from: https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/heart-health-screenings.
- Mayo Clinic Staff. Heart Failure. Retrieved from: https://www.mayoclinic.org/diseases-conditions/heart-failure/diagnosis-treatment/treatment/txc-20373144
- American Heart Association article. Medications Used to Treat Heart Failure. Retrieved from: https://www.heart.org/en/health-topics/heart-failure/treatment-options-for-heart-failure/medications-used-to-treat-heart-failure
- Editorial Team. Emerging Heart Failure Research. Retrieved from: https://heart-failure.net/research
- Mayo Clinic Staff. Beta Blockers. Retrieved from: https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/beta-blockers/art-20044522
- Johns Hopkins Medicine. Congestive Heart Failure: Prevention, Treatment and Research. Retrieved from: https://www.hopkinsmedicine.org/health/wellnss-and-prevention/heart-health. https://www.hopkinsmedicine.org/health/heart-and-vascular. Ventricular Assist Device (VAD) | Conditions & Treatments | UCSF Health. https://www.hopkinsmedicine.org/health/wellness-and-prevention/heart-conditions’
- University of Southern California Health. Ventricular Assist Device Retrieved from: https://www.ucsfhealth.org/treatments/ventricular-assist-device,
- Figure 1. Mayo Clinic mayoclinic.org/diseases-conditions/heart-failure/symptoms-causes/syc-2037314
- Figure 2. Healthy-Ojas Healthy Cholesterol Range. healthy-ojas.com/cholesterol/healthy-cholesterol-level.html
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
