Course
Texas Tick-Borne Diseases
Course Highlights
- In this Texas Tick-Borne Diseases course, we will learn about the various types of ticks found in Texas.
- You’ll also learn tick-borne illnesses prevalent in Texas, including but not limited to Lyme disease, Rocky Mountain spotted fever, and ehrlichiosis.
- You’ll leave this course with a broader understanding of the symptoms, diagnosis methods, and treatment protocols for each tick-borne illness.
About
Pharmacolgy Contact Hours Awarded: 2
Course By:
Abbie Schmitt
MSN-Ed, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Ticks are more than just a bothersome pest; they are carriers of debilitating diseases. Tickborne diseases are unfortunately increasing in incidence. Clinicians should expect tickborne disease in patients presenting with flu-like symptoms during the spring and summer months. This is especially true in regions with rich biodiversity like Texas.
We will review the most common types of ticks and the diseases they carry. These diseases, while potentially severe, are treatable, especially when caught early. The course will review symptoms, stages, and the epidemiology of tick-borne diseases.
It is meaningful to explore the diagnostic tests and treatment protocols for tick-borne illnesses, including the use of antibiotics and supportive care measures. Prompt diagnosis and treatment can prevent complications and death.
We will closely examine the pharmacokinetics of each medication used to treat the diseases, including the uses, mechanism of action, side effects, and contraindications. Counseling patients on preventative measures for protective clothing and tick repellents during outdoor activities can help minimize the risk of infection.
Introduction to Ticks
Ticks found in Texas encompass a variety of species, each with their unique characteristics and disease implications. Ticks are most active in the warmer months of spring and summer. The most common ticks in Texas are the Lone Star tick, American dog tick, Black-legged tick, and the Brown dog tick. These species vary in appearance, habitat preferences, and the diseases they can transmit.
Lone Star Tick
Lone Start Tick (Amblyomma Americanum): A distinct white dot or "lone star" on the female's back helps this tick to be identified easily. It is found throughout Texas, especially in wooded, bushy areas. Lone star ticks are known for transmitting diseases such as Ehrlichiosis and Southern Tick-Associated Rash Illness (STARI). In addition to their competence for pathogen transmission, Amblyomma Americanum (A. Americanum) has recently been associated with delayed red meat allergy (7).
American Dog Tick
American Dog Tick (Dermacentor variabilis): This tick prefers grassy areas with little to no tree cover. It primarily targets dogs but will bite humans and can transmit Rocky Mountain spotted fever and Tularemia.
Black-legged Tick
Black-legged Tick (Ixodes scapularis): This tick is also called the deer tick. It is prevalent in the eastern and northern parts of Texas. This tick is known for transmitting Lyme disease, Anaplasmosis, and Babesiosis to humans. The black-legged tick prefers wooded and brushy habitats.
Brown Dog Tick
Brown Dog Tick (Rhipicephalus sanguineus): Unlike other ticks, the brown dog tick is more adapted to dryer environments and can live and reproduce indoors.
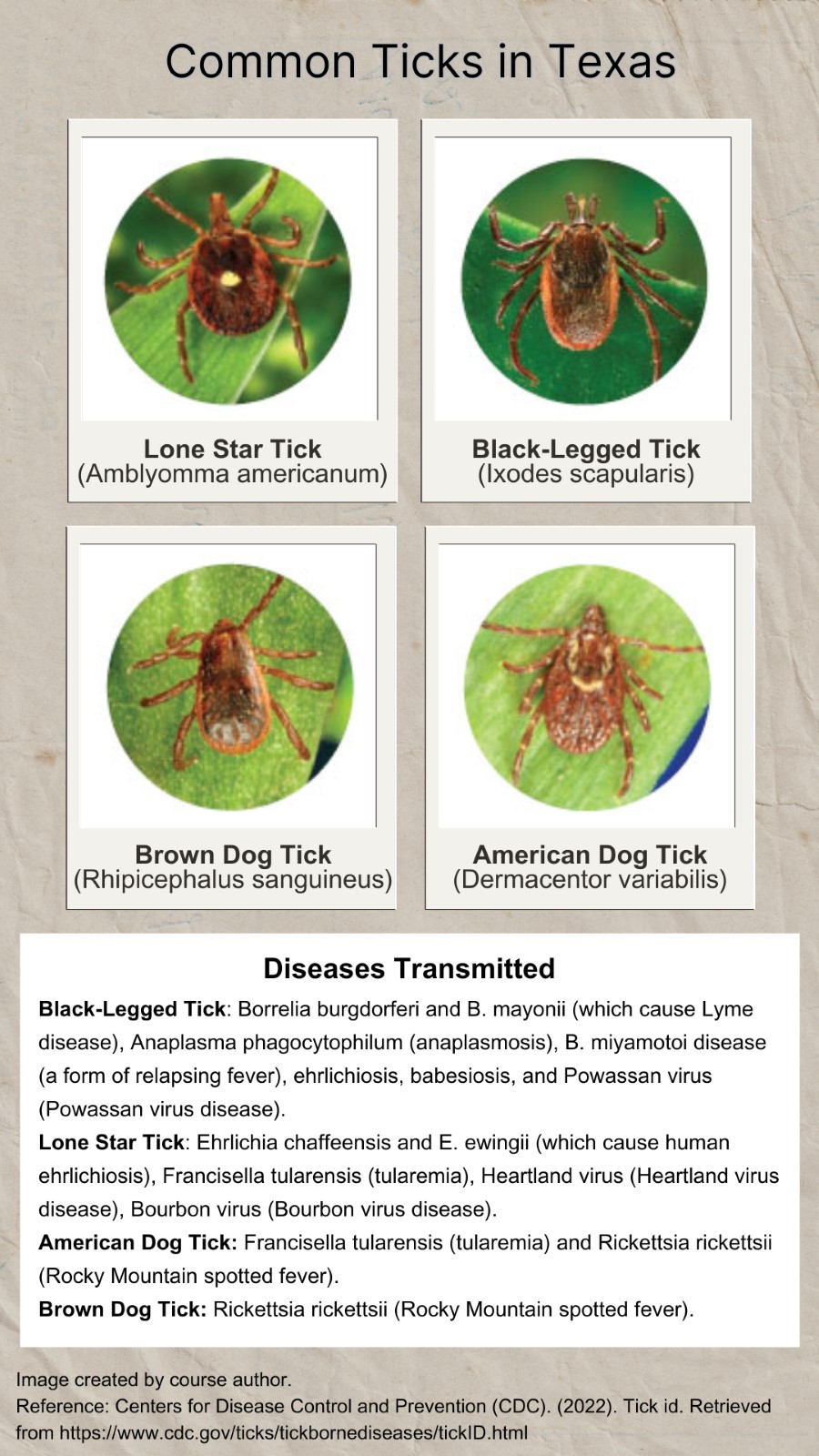
Image 1. Common Ticks in Texas (3)

Self Quiz
Ask yourself...
- Can you name the most common ticks found in Texas?
- Do you notice defining features among each tick mentioned above?
- Can you discuss the diseases that each tick transmits?
- What seasons are ticks most active?
- What training have you had regarding ticks at your facility?
- Do you feel that you have seen an increase or decrease in tick-related bites?
- What is a lone star tick?
- What is an American dog tick?
- What is a black legged tick?
- Define a brown dog tick.
Tick-Borne Diseases in Texas
Ticks are vectors for a wide array of bacterial, protozoan, and viral pathogens causing such diseases as Lyme borreliosis, spotted fever rickettsioses, anaplasmosis, tularemia, ehrlichiosis, babesiosis, and the recently emerging viruses: Heartland (HRTV), Powassan (POWV) and Bourbon (BRBV).
These vectors are found in many geographic areas of Texas and unfortunately have a steady increase in presence. Cases of tick-borne diseases have more than doubled in the last decade in the United States and territories, and account for 77% of all vector-borne disease reports (7).
Lyme Disease
Lyme disease (LD) is caused by the bacterium Borrelia burgdorferi and rarely, Borrelia mayonii. It is transmitted to humans through the bite of infected black-legged ticks. Lyme disease is the most frequently diagnosed tick-borne illness in the United States, however, it oddly has a low incidence in the state of Texas.
The incubation period is 3–30 days (5). Research shows the probability of host infection gradually increases as tick attachment continues, reaching 70% after 72 hours of attachment and a greater than 90% probability of infection after a complete tick blood meal (13).
Clinically, B. mayonii-infected patients show higher loads of spirochetes in the blood, and some have had focal or diffuse rash, or developed neurological symptoms.
There is significant research that explores and combats this bacterium’s ability to avoid immune detection and response. Similar to other blood-borne pathogens, LD spirochetes have developed multiple strategies to overcome innate immunity, thereby avoiding clearance by the immune system of the host by ways such as changing their surface composition (13). This action makes it difficult for the immune system to create antibodies against it.
Early clinical signs and symptoms (3 to 30 days after a tick bite) include (5):
- Erythema migrans (EM)— This is a worrisome “target” or “bull’s-eye” rash. It is a red annular or homogeneous rash at the site of a tick bite. The rash typically expands slowly over several days and may feel warm to the touch (5). EM occurs in 70–80% of infected individuals (5) [See image 2].
- Headache
- Fever
- Chills
- Malaise or fatigue, myalgia, arthralgia § Lymphadenopathy
Lyme disease that is not treated will progress to disseminated disease for about 60% of patients with varied manifestations (5) Rheumatologic signs and symptoms are particularly delayed and can cause severe damage to the joints, heart, and nervous system (5).
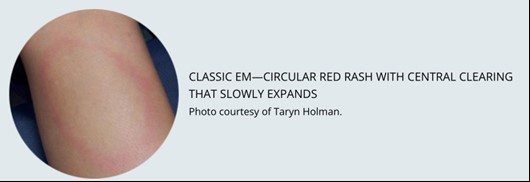
Image 2. Class Erythemia migrans rash (5)
Anaplasmosis and Ehrlichiosis
Anaplasmosis, known as human granulocytic anaplasmosis (HGA), is a disease caused by the bacterium Anaplasma phagocytophilum (A. Phagocytophilum). These bacteria are spread to people by tick bites primarily from the black-legged tick (Ixodes scapularis) and the western black-legged tick (Ixodes pacificus). The first case of human anaplasmosis was described in 1990 when a patient in Wisconsin developed a severe febrile illness following a tick bite and died two weeks later (6).
Anaplasma organisms are small, gram-negative, and intracellular. A. phagocytophilum targets neutrophils, alters their function in the host, and forms morulae within vacuoles. The majority of damage it causes is thought to be related to host inflammatory processes. Since Ixodes ticks are also carriers for Lyme disease, babesiosis, and tick-borne encephalitis, coinfection with multiple diseases can and does occur in humans.
Ehrlichiosis, known as Human Monocytic Ehrlichiosis (HME), is similar to anaplasmosis in molecular structure but is less commonly found than anaplasmosis.
The median age of patients with anaplasmosis and ehrlichiosis is around 50 years old (6).
Doxycycline is the drug of choice for adults and children of all ages with anaplasmosis (5).
Clinical signs and symptoms of anaplasmosis and ehrlichiosis are non-specific and typically include:
- Fever
- Headache
- Muscle aches
- Fatigue
Spotted Fever Group Rickettsioses
Spotted fever group rickettsioses (spotted fevers) are a group of diseases caused by similarly structured bacteria. Rocky Mountain Spotted Fever is within this group of diseases and is considered the most serious and most commonly reported spotted fever group rickettsiosis in the United States (5). These bacteria are spread to people through the bite of infected mites and ticks. The ticks responsible are typically the American dog ticks (Dermacentor variabilis), Rocky Mountain wood tick (Dermacentor andersoni), and the brown dog ticks (Rhipicephalus sanguineus) (5).
Spotted fevers have a wide range of signs and symptoms, including (5):
- Eschar - dark scab at the site of the tick bite
- Fever
- Headache
- Rash
Doxycycline is the treatment of choice for all spotted fever infections (5).
Tick-borne Relapsing Fever
Tick-borne relapsing fever (TBRF) is an infection caused by certain species of Borrelia bacteria. Relapsing fever Borrelia infections are categorized into three main groups based on the vector that transmits the bacteria: soft ticks, hard ticks, and body lice. These diseases differ in their epidemiology and severity.
TBRF is uniquely caused by soft ticks, instead of hard ticks (like the other diseases). Soft ticks are generally found in animal burrows, dens, caves, or human dwellings such as huts, cabins, or sheds. The disease is often linked to someone recently sleeping in a rustic cabin in the mountains. Soft ticks have a wrinkled body appearance and do not latch as long as hard ticks (5).
The main symptoms of TBRF are:
- High fever (e.g., 103° F)
- Headache
- Muscle and joint aches.
The fever comes in a unique pattern of lasting roughly 2-7 days, followed by 4-14 days without fever, followed by another 3 days of fever. Without antibiotic treatment, this process can repeat several times.
Babesiosis
Babesiosis is an emerging tick-borne disease caused by parasites of the genus Babesia (9). This disease has increasing incidence worldwide and a risk of human-to-human transmission through blood transfusion.
The majority of those infected by babesiosis remain asymptomatic or present with mild flu-like symptoms (9). However, in susceptible populations, such as the elderly or immunocompromised individuals, symptoms can include severe anemia, acute respiratory distress, organ failure, and death (9).
Tularemia
Tularemia is caused by infection with the bacteria Francisella tularensis. Transmission routes include tick bite, deer fly bite, inhalation, ingestion, and skin contact with infected animals (4). Signs and symptoms of tularemia can vary widely depending on the route of exposure and subtype of F. tularensis. Tularemia can become serious or fatal without adequate treatment.
Possible signs and symptoms include (4):
- Fever, chills
- Headache
- Malaise, fatigue
- Anorexia
- Myalgia
- Chest discomfort
- Non-productive cough
- Sore throat
- Vomiting, diarrhea
- Abdominal pain
- Localized or regional lymphadenopathy
- Cutaneous ulcer at the site of bite/infection
- Photophobia
- Vision impairment/loss
- Conjunctivitis
General laboratory findings:
- Hyponatremia
- Leukocytosis
- Thrombocytopenia
- Elevated hepatic transaminases
- Elevated creatine kinase
- Elevated erythrocyte sedimentation rate
- Myoglobinuria
- Sterile pyuria
Viral Pathogens: Heartland (HRTV), Powassan (POWV) and Bourbon (BRBV)
Arboviral disease is a broad term used to describe infections caused by a group of viruses spread by the bite of infected arthropods (insects) such as mosquitoes and ticks (15). These include Heartland (HRTV), Powassan (POWV) and Bourbon (BRBV). Other diseases spread by the bite of an infected tick are bacterial infections and babesiosis (a parasitic infection), which are not arboviruses. It is important to note that if a highly suspected infected individual (positive for symptoms and tick bite) does not have improvement of symptoms following an antibiotic regimen, a viral pathogen from a tick may be the culprit.

Self Quiz
Ask yourself...
- How does the length of time an infected tick is attached correlate with the probability of acquiring Lyme disease?
- What is the most common sign of Lyme disease?
- Which ticks transmit anaplasmosis and ehrlichiosis?
- Can you describe the presentation of patients infected with Rickettsioses or tularemia?
- What bacteria are known to cause Lyme disease?
- What is erythema migrans?
- What are three signs of Anaplasmosis and Ehrlichiosis?
- What are the symptoms of tick-borne relapsing fever?
- What is babesiosis?
- What viral infections are linked to ticks?
Removal of Ticks
Imagine you are evaluating a patient who has not removed a tick attached to their skin. It is imperative that you quickly, yet appropriately, remove it manually (unless your facility has another method). There are other commercially available tick-removal devices, but there are currently no substantial studies that have evaluated their usefulness.
The Centers for Disease Control and Prevention (CDC) provides the following steps as a guide on how to manually remove a tick:
- Apply gloves and clean the area well.
- Use blunt forceps (tweezers). Do not use sharp forceps.
- Grasp the tick as close to the skin’s surface as possible, and pull upward with steady, even pressure.
- Do not squeeze or puncture the tick’s body.
- Do not twist or jerk the tick (this can cause the mouth-parts to break off and remain in the skin)
- If you notice the mouth-parts remain on the skin after removal, grasp and pull with tweezers.
- After removing the tick, thoroughly clean the bite with an antiseptic solution.

Self Quiz
Ask yourself...
- When removing a tick, why is it important to get as close to the skin’s surface as possible?
- Why do you think it’s recommended to avoid squeezing or puncturing the tick’s body?
- What types of forceps should you use when removing a tick?
- What should you clean the skin with after the removal of a tick?
- Have you ever had to remove a tick? What was your experience like?
Medications Used to Treat Tick-Borne Diseases
The treatment of tick-borne diseases often involves antibiotics, with the choice of medication depending on the specific disease diagnosed. It would be helpful to consult an infectious disease specialist about individual patient treatment plans as the specific duration of treatment can vary based on each disease, the severity of symptoms, and individual patient traits.
Here's a brief overview of treatments for some of the most common tick-borne diseases:
Lyme Disease
The first-line treatment for Lyme disease is typically oral antibiotics, with doxycycline, amoxicillin, and cefuroxime axetil being the most commonly prescribed. In cases of more severe Lyme disease, intravenous antibiotics, such as ceftriaxone, may be used. Depending on a person’s age, medical history, underlying health conditions, pregnancy status, or allergies, these regimens may need to be adjusted. The table below outlines treatment regimens for the erythema migrans rash, which is the most common manifestation of early Lyme disease.

Table 1. Treatment Regimen for Erythema Migrans Rash (5)
Rocky Mountain Spotted Fever (RMSF)
Doxycycline is the treatment of choice for RMSF for both adults and children. Early treatment is critical to prevent severe disease complications.
Ehrlichiosis and Anaplasmosis
Doxycycline is also the preferred treatment for both ehrlichiosis and anaplasmosis, regardless of the patient's age.
Southern Tick-Associated Rash Illness (STARI)
Although the cause of STARI is not well understood, doxycycline may be used to treat the rash and possible infection, similar to the treatment for Lyme disease.
Babesiosis
This disease is typically treated with a combination of atovaquone and azithromycin. In more severe cases, clindamycin and quinine may be used instead.
Tularemia
Treatment can include several different antibiotics, such as gentamicin, streptomycin, doxycycline, or ciprofloxacin (4). The table below outlines treatment regimens for Tularemia.
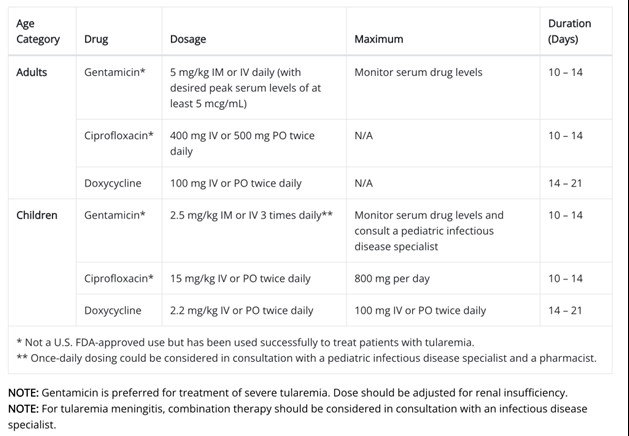
Table 2. Treatment Regimen for Tularemia (4)

Self Quiz
Ask yourself...
- Can you name the various factors to consider when prescribing treatment for a tick-borne disease?
- Why is it important to get a thorough medical history before prescribing antibiotics?
- Do you have experience with intravenous antibiotic administration?
- What are some patient education topics on these diseases and why treatment is necessary?
- What education should you provide to patients being started on doxycycline?
- What education should you provide to patients being started on amoxicillin?
- What education should you provide to patients being started on cefuroxime?
- What is the medication of choice to treat Rocky Mountain spotted fever?
- What is the treatment regimen for tularemia?
- What is the treatment regimen for babesiosis?
Antibiotics that Inhibit Protein Synthesis
When treatment is initiated for patients with tick-borne diseases, the prescriber needs to understand the pharmacokinetics of antibiotics that inhibit protein synthesis and biochemistry. Examples of these antibiotics include tetracyclines, chloramphenicol, macrolides, lincosamides, streptogramins, oxazolidinones, mupirocins, and peptide deformylase inhibitors (1). Knowledge of the mechanisms of action of antibiotics in interfering with the life cycle of these bacteria is critical in evaluating patient outcomes.
Protein synthesis is an essential process in all cells, including bacterial cells. The ribosome performs protein synthesis by translating the genetic information encoded in messenger RNAs (mRNAs) into proteins. The bacterial ribosome is composed of three RNA chains (16S, 23S, and 5S) and more than 50 proteins assembled into two individual subunits. These include the small 30S and large 50S subunits, which join together to form the 70S ribosome. To proceed efficiently and translate the information, many protein factors need to interact sequentially with the ribosome.
Keep this process in mind as we discuss antibiotic drugs in effectively treating tick-borne diseases.
Doxycycline
Pharmacologic Category
Antibiotic, Tetracycline Derivative
Uses: Labeled Indications
- Acne
- Actinomycosis
- Acute intestinal amebiasis
- Clostridium: Treatment of infections caused by Clostridium spp. when penicillin is contraindicated.
- Ehrlichiosis and Anaplasmosis
- Gram-negative infections: Treatment of infections caused by Escherichia coli, Enterobacter aerogenes, Shigella spp., Acinetobacter spp., Klebsiella spp. (respiratory and urinary infections), and Bacteroides spp.; Neisseria meningitidis (when penicillin is contraindicated).
- Gram-positive infections: Treatment of infections caused by Streptococcus spp., when susceptible.
- Listeriosis
- Malaria prophylaxis
- Mycoplasma pneumoniae: Treatment of infections caused by Mycoplasma pneumoniae.
- Ophthalmic infections
- Periodontitis
- Relapsing fever: Treatment of relapsing fever caused by Borrelia recurrentis.
- Respiratory tract infections
- Rickettsial infections: Treatment of Rocky Mountain spotted fever, rickettsialpox, and tick fevers caused by Rickettsiae.
- Sexually transmitted infections
- Infections caused by Staphylococcus aureus (doxycycline is not the drug of choice in the treatment of any type of staphylococcal infection).
Mechanism of Action
All tetracyclines have the same mechanism of action to block the protein synthesis of bacteria.
Tetracyclines inhibit protein synthesis by binding to the 30S subunit of the ribosome (1). Essentially, the drug inhibits the binding of amino-acyl tRNA to the A-site of the ribosome. The 7S ribosomal protein is part of the binding site. Tigecycline also binds at the A-site of the 30S subunit of the ribosome and inhibits bacterial protein synthesis.
Tetracyclines can bind equally well to both prokaryotic (70S) and eukaryotic (80S) ribosomes. Eukaryotic cells are not affected by the antibiotic because they do not accumulate tetracycline in the cell. This makes tetracyclines selective against bacteria. Tetracyclines may also cause alterations in the cytoplasmic membrane (1).
Pharmacodynamics
Absorption: (Oral) Almost completely absorbed from the gastrointestinal tract (GI) tract; average peak plasma concentration may be reduced by high-fat meal or milk (16).
Distribution: Widely distributed into body tissues and fluids including synovial, pleural, prostatic, seminal fluids, and bronchial secretions. Saliva and cerebral spinal fluid (CSF) penetration is poor.
Protein binding: >90%
Bioavailability: Reduced at high pH; may be clinically significant in patients with gastrectomy, gastric bypass surgery, or who are otherwise deemed achlorhydric.
Metabolism and Excretion: Not hepatic; partially inactivated in the GI tract by chelate formation. 20-40% excreted unchanged in the urine; some inactivation in the intestines and enterohepatic circulation with excretion in bile and feces.
Half-life: 14-17 hours (longer time frame in severe renal impairment)

Figure 1. Pharmacodynamics of Doxycycline
Adverse Effects
1% to 10% has reported the following (16):
- Cardiovascular: Hypertension (3%)
- Central nervous system: Anxiety (2%), pain (2%)
- Endocrine & metabolic: Increased lactate dehydrogenase (2%), increased serum glucose (1%)
- Gastrointestinal: Diarrhea (5%), upper abdominal pain (2%), abdominal distention (1%), abdominal pain (1%), xerostomia (1%)
- Hepatic: Increased serum aspartate aminotransferase (2%)
- Infection: Fungal infection (2%), influenza (2%)
- Neuromuscular & skeletal: Back pain (1%)
- Respiratory: Nasopharyngitis (5%), sinusitis (3%), nasal congestion (2%)
Contraindications/Precautions
Hypersensitivity to doxycycline, other tetracyclines, or any component of the formulation. Contraindicated in infants and children younger than eight years of age, during the second or third trimester of pregnancy, and breastfeeding (16).
Patient Education
- Instruct the patient to finish the entire dose as directed, even if feeling better, and take missed doses as soon as possible unless it is almost time for the next dose.
- Advise patient to avoid taking antacids, calcium, magnesium-containing medications, sodium bicarbonate, and iron supplements within 1-3 hours of oral doxycycline.
- Caution patient to use sunscreen and protective clothing to prevent photosensitivity reactions.
- Advise patient to report signs of superinfection (black, furry overgrowth on the tongue, vaginal itching, discharge, watery or foul-smelling stools) or intracranial hypertension (headache, blurred vision, diplopia).

Self Quiz
Ask yourself...
- What are other uses for doxycycline?
- Can you describe the mechanism of action of these antibiotics that inhibit protein synthesis?
- Can you name adverse effects and patient education topics for doxycycline?
- How is doxycycline metabolized in the body?
- What is the onset of doxycycline?
- What education would you provide to patients being started on doxycycline?
- What is a contraindication to doxycycline?
- What age group should be avoided when administering doxycycline?
- What is the peak of doxycycline?
- What is the duration of doxycycline?
Aminoglycosides
Aminoglycosides include streptomycin, neomycin, kanamycin, amikacin, gentamicin, tobramycin, sisomicin, netilmicin, plazomicin, and others (2). Gentamicin and streptomycin are recommended in the treatment of tularemia, so we will closely examine this group.
ALERT: US Boxed Warning for Aminoglycosides
Toxicity (17):
As with other aminoglycosides, gentamicin is potentially nephrotoxic. The risk is greater with impaired renal function and prolonged therapy. Neurotoxicity, manifested by ototoxicity (both vestibular and auditory) can occur in patients treated with gentamicin.
Clinicians should closely monitor renal function and eighth cranial nerve function, especially in patients with reduced renal function at the onset of therapy. Assess urine for decreased specific gravity, increased excretion of protein, and the presence of cells or casts (17). Routinely check serum urea nitrogen (BUN), serum creatinine, or creatinine clearance (CrCl). Monitor serum concentrations of aminoglycosides to ensure adequate levels and to avoid potentially toxic levels.
Avoid concurrent use of other potentially neurotoxic and/or nephrotoxic drugs: cisplatin, cephaloridine, kanamycin, amikacin, neomycin, polymyxin B, colistin, paromomycin, streptomycin, tobramycin, vancomycin, and viomycin (2). Avoid the concurrent use of gentamicin with potent diuretics.
Pregnancy
Aminoglycosides can cause fetal harm when administered to a pregnant woman.
Gentamicin
Pharmacologic Category
Antibiotic, Aminoglycoside
Uses
Treatment of serious infections: Sepsis, meningitis, urinary tract infections, respiratory tract infections, peritonitis, bone infections, skin, and soft tissue infections, caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species, Escherichia coli, Klebsiella species, Enterobacter species, Serratia species, Citrobacter species (2).
Mechanism of Action
As with all aminoglycosides, gentamicin interferes with ribosomal peptide/protein synthesis (14). It binds to 16S rRNA (located on the smaller 30S component of the ribosome of the bacteria), stops its functionality, and halts ongoing protein synthesis (14). Aminoglycosides are not able to penetrate the hydrophobic bacterial cell membrane and are only active against aerobic bacteria because an electron transport system used during the cell’s respiratory cycle is needed to accomplish this (2).
Pharmacodynamics/Kinetics
Absorption: Intramuscular: Rapid and complete
Oral: Poorly absorbed
Distribution: Primarily into extracellular fluid (highly hydrophilic); high concentration in the renal cortex.
Protein binding: <30%
Half-life elimination:
- Adults: ~2 hours
- Neonates: <1 week: 3 to 11.5 hours; 1 week to 1 month: 3 to 6 hours
- Infants: 4 ± 1 hour
- Children: 2 ± 1 hour
Time to peak, serum:
- IM: 30 to 90 minutes
- IV: 30 minutes after a 30-minute infusion
Excretion: Urine
Clearance: Directly related to renal function
- Neonates: 0.045 ± 0.01 L/hour/kg
- Infants: 0.1 ± 0.05 L/hour/kg
- Children: 0.1 ± 0.03 L/hour/kg
- Adolescents: 0.09 ± 0.03 L/hour/kg
Adverse Effects
Some adverse effects include (17):
- Cardiovascular: Edema, hypertension, hypotension, phlebitis, thrombophlebitis
- Central nervous system: Abnormal gait, ataxia, brain disease, confusion, depression, dizziness, drowsiness
- Dermatologic: Alopecia, erythema, pruritus, skin rash, urticaria
- Endocrine & metabolic: Hypocalcemia, hypokalemia, hypomagnesemia, hyponatremia, weight loss
- Gastrointestinal: Anorexia, Clostridioides difficile-associated diarrhea, decreased appetite, enterocolitis, nausea, sialorrhea, stomatitis, vomiting
- Genitourinary: Casts in urine (hyaline, granular), oliguria, proteinuria
- Hematologic & oncologic: Agranulocytosis, anemia, thrombocytopenia
- Hepatic: Hepatomegaly, increased liver enzymes
- Hypersensitivity: Anaphylaxis, anaphylactoid reaction, hypersensitivity reaction
- Local: Injection site reaction, pain at injection site
- Neuromuscular & skeletal: Arthralgia, muscle cramps, muscle fatigue, weakness
- Ophthalmic: Visual disturbance
- Otic: Auditory impairment, tinnitus
- Renal: Decreased creatinine clearance, decreased urine specific gravity, increased blood urea nitrogen, increased serum creatinine, polyuria, renal failure (high trough serum concentrations), renal tubular necrosis
- Respiratory: Dyspnea, laryngeal edema, pulmonary fibrosis, respiratory depression
- Miscellaneous: Fever
Streptomycin
Pharmacologic Category
Antibiotic, Aminoglycoside
Uses
Primarily used for treating aerobic gram-negative bacterial infections, such as tularemia, brucellosis, tuberculosis (in combination with isoniazid, pyrazinamide, and rifampin), and certain cases of endocarditis when combined with beta-lactam antibiotics (14).
Mechanism of Action
Interferes with bacterial protein synthesis by binding to 30S ribosomal subunit resulting in a defective bacterial cell membrane (2). These actions inhibit the bacteria from creating the needed ongoing protein synthesis.
Pharmacodynamics/Kinetics
Absorption:
- Oral: Poorly absorbed
- IM: Well-absorbed
Distribution: Distributes into most body tissues and fluids except the brain; small amounts enter the CSF only with inflamed meninges.
Protein binding: 34%
Half-life elimination:
- Newborns: 4 to 10 hours
- Adults: 2 to 4.7 hours (prolonged with renal impairment)
Time to peak: IM: Within 1 to 2 hours
Excretion: Urine (29% to 89% as unchanged drug); a small amount (1%) excreted in bile, saliva, sweat, and tears (18)
Adverse Reactions
Adverse reactions include (18):
- Cardiovascular: Hypotension
- Central nervous system: Drug fever, facial paresthesia, headache, neurotoxicity
- Dermatologic: Exfoliative dermatitis, skin rash, urticaria
- Gastrointestinal: Nausea, vomiting
- Genitourinary: Azotemia, nephrotoxicity
- Hematologic & oncologic: Eosinophilia, hemolytic anemia, leukopenia, pancytopenia, thrombocytopenia
- Hypersensitivity: Anaphylaxis, angioedema
- Neuromuscular & skeletal: Arthralgia, tremor, weakness
- Ophthalmic: Amblyopia
- Otic: Auditory ototoxicity, vestibular ototoxicity
- Respiratory: Dyspnea

Self Quiz
Ask yourself...
- What are other uses for aminoglycosides?
- Can you describe the mechanism of action of gentamicin and streptomycin?
- Can you name the adverse effects of these drugs?
- How is gentamycin excreted from the body?
- What is the primary use of streptomycin?
- What is the primary use of amoxicillin?
- What education would you provide to a patient being started on gentamicin?
- What education would you provide to a patient being started on streptomycin?
- How is streptomycin excreted from the body?
- Which method of administration has the best absorption for streptomycin?
Compound Use of Atovaquone and Azithromycin for Babesiosis
The current arsenal for the treatment of human babesiosis includes atovaquone, azithromycin, clindamycin, and quinine. The first-line compound typically used is atovaquone and azithromycin. Atovaquone is used to treat several human diseases, including Pneumocystis jirovecii pneumonia, toxoplasmosis, and malaria. In apicomplexan parasites such as the genus Babesia, atovaquone targets the cytochrome bc1 complex of the mitochondrial electron transport chain (9). Azithromycin is a relatively broad-spectrum antibiotic indicated for the treatment of numerous bacterial infections; it is a well-characterized protein synthesis inhibitor, which in apicomplexan parasites targets the translation machinery in the apicoplast (9).

Self Quiz
Ask yourself...
- Are single or compound antibiotics currently used in the treatment of babesiosis?
- Can you describe the possible adverse effects of using multiple antibiotics?
Tick Testing
The Department of State Health Services (DSHS) and the University of North Texas Health Science Center (UNTHSC) Tick-Borne Disease Research Laboratory have teamed up to test ticks for disease agents in the Borrelia, Ehrlichia, and Rickettsia genera using molecular methods (11).
Ticks should be submitted to the DSHS Zoonosis Control office for identification after which they will be forwarded to UNTHSC for testing (11). There is no charge for testing, however, this service is available only to Texas residents submitting ticks found at a location within Texas. Only ticks that were attached to a human should be submitted (11).
For free testing of ticks found in the environment or on pets, visit the Texas Tick Project. The program is designed for tick surveillance, not disease diagnosis. If infected with a tick-borne pathogen, individuals usually develop symptoms before the test results are available.

Self Quiz
Ask yourself...
- Should ticks from the family dog be sent in for testing in this program?
- Can you describe the purpose of the testing program?
- Are you familiar with the removal and examination of ticks?
- Should a Texas resident who removed a tick while vacationing in North Carolina send this tick into the program for testing?
Prevention and Control
It is meaningful to provide teaching on prevention tips if you notice a patient is at high risk for encountering a tick outdoors. This includes patients who enjoy hobbies outdoors (such as hiking) or whose job duties involve spending a significant amount of time outdoors.
Prevention teaching:
- Always inspect yourself, family members, and pets from head to toe for ticks after spending time outdoors.
- Keep grass trimmed and remove overgrowth.
- Remove bird feeders and other food sources that attract wildlife, such as deer, that can carry ticks.
- Discuss tick and flea prevention methods with your veterinarian if you have pets.
- Move picnic tables, swing sets, and outdoor lawn furniture away from trees and shrubs.
Upcoming Research
Significant research studies are being conducted on the treatment and prevention of tick-borne diseases, however, there is a need for prevention of the spread of tick bites. One interesting study is exploring the prevalence of common tick-borne pathogens in white-tailed deer and coyotes in south Texas (19). Identifying vehicles (various wildlife) that carry these tiny ticks over long distances can help researchers treat wildlife for ticks and ultimately slow the spread. Upcoming research relies on effective collaboration between medical professionals, wildlife and ecological professionals, researchers, and policymakers.
The current evidence on babesiosis is not comprehensive and treatment consists of combinations of atovaquone and azithromycin or clindamycin and quinine (9). These drug compounds are associated with mild or severe adverse events and a rapid emergence of drug resistance, thus highlighting the need for new treatment therapies to combat Babesia parasites.

Self Quiz
Ask yourself...
- What are some ways to prevent tick attachment?
- Can you name examples of wildlife carriers or “vehicles” for ticks?
- What education can you provide to the community about preventing and controlling tick bites?
- How has the care of tick bites changed since you have been in practice?
- What role can community and public health nurses play in the education of tick bite prevention?
Conclusion
Ticks aren’t just annoying—they’re also a source of serious illnesses. As tickborne diseases become more common, healthcare professionals should be alert to the possibility of these diseases in patients who have flu-like symptoms in the spring and summer, especially in areas rich in wildlife, such as Texas.
This course provided information on prevalent ticks and the illnesses they transmit, as well as the symptoms, progression, and medications used to treat each pathogen. The pharmacokinetics, adverse effects, and uses are meaningful components of treating patients who are infected with a tick-borne disease.
References + Disclaimer
- Bhattacharjee, M. K. (2022). Chemistry of antibiotics and related drugs (2nd ed.). Springer. https://doi.org/10.1007/978-3-031-07582-7
- Beauduy C.E., & Winston L.G. Aminoglycosides & spectinomycin. Vanderah T.W.(Ed.), [publicationyear2] Katzung’s Basic & Clinical Pharmacology, 16th Edition. McGraw-Hill. https://accesspharmacy.mhmedical.com/content.aspx?bookid=3382§ionid=281754807
- Centers for Disease Control and Prevention (CDC). (2022). Tick id. Retrieved from https://www.cdc.gov/ticks/tickbornediseases/tickID.html
- Centers for Disease Control and Prevention (CDC). (2024). Tularemia: for clinicians. Retrieved from https://www.cdc.gov/tularemia/clinicians/index.html
- Centers for Disease Control and Prevention (CDC). (2022). Tickborne diseases of the United States: A reference manual for healthcare providers. Retrieved from https://www.cdc.gov/ticks/tickbornediseases/TickborneDiseases-P.pdf
- Columbia University Irving Medical Center. (2021). Anaplasmosis. Retrieved from https://www.columbia-lyme.org/anaplasmosis.
- Mendell, N. L., Reynolds, E. S., Blanton, L. S., Hermance, M. E., Londoño, A. F., Hart, C. E., Quade, B. R., Esterly, A. T., Hendrix, C. B., Teel, P. D., Bouyer, D. H., & Thangamani, S. (2019). Detection of Rickettsiae, Borreliae, and Ehrlichiae in Ticks Collected from Walker County, Texas, 2017-2018. Insects, 10(10), 315. https://doi.org/10.3390/insects10100315
- Pace EJ, O’Reilly M. Tickborne Diseases: Diagnosis and Management. Am Fam Physician. 2020 May 1;101(9):530-540. PMID: 32352736.
- Renard, I., & Ben Mamoun, C. (2021). Treatment of Human Babesiosis: Then and Now. Pathogens (Basel, Switzerland), 10(9), 1120. https://doi.org/10.3390/pathogens10091120
- Texas Department of State Health Services (DSHS). (2023). Tick-borne diseases. Retrieved from https://www.dshs.texas.gov/tick-borne-diseases.
- Texas Department of State Health Services (DSHS). (2023). Tick submission and testing. Retrieved from https://www.dshs.texas.gov/tick-borne-diseases/tick-submission-testing
- Vallerand, A. H., & Sanoski, C. A. (2023). Davis’s drug guide for nurses (Eighteenth edition.). F.A. Davis Company.
- Walter, L., Sürth, V., Röttgerding, F., Zipfel, P. F., Fritz-Wolf, K., & Kraiczy, P. (2019). Elucidating the Immune Evasion Mechanisms of Borrelia mayonii, the Causative Agent of Lyme Disease. Frontiers in immunology, 10, 2722. https://doi.org/10.3389/fimmu.2019.02722
- Waters M, Tadi P. Streptomycin. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555886/
- Wang Y, Griffiths A, Brackney DE, Verardi PH. Generation of Multiple Arbovirus-like Particles Using a Rapid Recombinant Vaccinia Virus Expression Platform. Pathogens. 2022; 11(12):1505. https://doi.org/10.3390/pathogens11121505
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Doxycycline. Access Pharmacy. Retrieved from https://accesspharmacy.mhmedical.com/drugs.aspx?gbosID=426591
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Gentamicin. Access Pharmacy.
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Streptomycin. Access Pharmacy. Retrieved from https://accesspharmacy.mhmedical.com/drugs.aspx?gbosID=425268#monoNumber=425268§ionID=243273707&tab=tab0
- Yu, S., Modarelli, J., Tomeček, J. M., French, J. T., Hilton, C., & Esteve-Gasent, M. D. (2020). Prevalence of common tick-borne pathogens in white-tailed deer and coyotes in south Texas. International journal for parasitology. Parasites and wildlife, 11, 129–135. https://doi.org/10.1016/j.ijppaw.2020.01.005
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
