Course
2022 Florida Renewal Bundle
Course Highlights
- In this course we will cover all of the topics necessary for a Florida RN License Renewal.
- You will learn about the Florida Board of Nursing’s requirements, laws, and regulations, as well as helpful practice tips.
- You’ll leave this course with a broader understanding of topics ranging from domestic violence, human trafficking, vaping, and so much more.
About
Contact Hours Awarded: 27
Course By:
Multiple Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Florida Domestic Violence
Introduction
Domestic violence is defined as violent or aggressive behavior occurring within the home and usually involves the abuse of a spouse or partner. In the United States alone, it is estimated that more than 10 million adults have been subjected to domestic violence during the course of a year. This statistic translates to an incident of domestic violence occurring every 3 seconds. The National Coalition Against Domestic Violence [1] reports some daunting statistics:
- 1 in 3 women and 1 in 4 men have experienced some form of physical violence by an intimate partner.
- 1 in 4 women and 1 in 7 men have been victims of severe physical violence (such as beating, burning, strangling) by an intimate partner in their lifetime.
- On average, more than 20,000 phone calls placed to domestic violence hotlines nationwide.
- The presence of a gun in a domestic violence situation increases the risk of homicide by 500%; 19% of domestic violence involves a weapon; Most intimate partner homicides are committed with firearms.
- 1 in 15 children are exposed to intimate partner violence each year, and 90% of these children are eyewitnesses to this violence.
- From 2016 through 2018, the number of intimate partner violence victimizations in the United States increased 42%.
Due to the increasing prevalence of domestic violence in society, there is a high probability that all healthcare professionals will evaluate and treat a victim (and quite possibly a perpetrator as well) of domestic violence at some time during their healthcare career. The importance of ongoing education and global awareness cannot be understated.
In 2020, the COVID-19 pandemics’ stay at home/shelter in place orders resulted in spikes in calls to domestic violence hotlines. From layoffs and loss of income to decreased availability of shelters and backlogged courtrooms, fewer resources were made available to victims of domestic violence. These measures resulted in increases in both the incidence and severity of domestic violence. Sadly, the effects of this pandemic, especially on this issue, continue years later [2].
Forms of Domestic Violence
Domestic violence may encompass physical abuse, sexual abuse, emotional and verbal abuse, and spiritual and economic abuse. Defined as a pattern of behavior used to gain power or control over an intimate partner, a domestic violence abuser may use tactics that frighten, intimidate, hurt, blame, or injure a person. These behaviors often escalate over time and intensity and have resulted, at times, in life-threatening injuries or death of a victim [3].
Intimate partner violence (IPV) is abuse or aggression that occurs in a romantic relationship. The term “intimate partner” refers to both current and former spouses and dating partners, including heterosexual and same-sex couples. The Centers for Disease Control and Prevention [4] further delineates IPV into four separate groups: physical violence, sexual violence, stalking, and psychological aggression.
- Physical violence may include hitting, kicking, and punching someone.
- Sexual violence may include using force to get a partner to partake in a sexual act.
- Stalking may include unwanted and threatening phone calls or text messages.
- Psychological aggression may include insults, threats, name-calling, or belittling a partner.
Teen Dating Violence (TDV) [5] is defined as dating violence affecting millions of teenagers annually. In addition to the threats from physical and sexual violence and other forms of aggression, TDV is often done electronically through repeated texting and placing sexual pictures of a person online without permission.
The CDC statistics on teen dating violence report:
- Nearly 1 in 11 female and about 1 in 15 male high school students report having experienced physical dating violence in the last year.
- About 1 in 9 female and 1 in 36 male high school students report having experienced sexual dating violence in the last year
- 26% of women and 15% of men who were victims of contact sexual violence, physical violence, and/or stalking by an intimate partner in their lifetime first experienced these or other forms of violence by that partner before age 18.
Domestic violence transects every community and affects all people, regardless of age, socio-economic status, race, religion, gender, or nationality [6]. Whether the violence results in physical or psychological injury, the effects can last a lifetime and affect multiple generations.
Healthcare professionals are in a pivotal position to impact the lives of those affected by domestic violence positively. Oftentimes, they may be the first person to encounter a victim of domestic violence. Their ability to effectively evaluate the situation and provide time-sensitive, patient-centered care (including but not limited to treatment interventions, appropriate referrals, and follow-up care) can enhance immediate victim safety and reduce further injury, and improve the home front circumstances, moving forward.
Healthcare professionals must be able to identify and assess all patients for suspected abuse, and be able to offer treatment, counseling, education, and referrals, as appropriate. These referrals may extend out to shelter options, advocacy groups, child protection services and legal assistance [7].
Profiles of Victims/Abusers
Anyone can become a victim of domestic violence. Victims of domestic violence come from all walks of life, all age groups, all socio-economic groups, all religions, and all nationalities [8]. Violence can occur in any relationship when one person feels they are entitled to control another person through whatever means of abuse possible. This abuse is cyclical and usually increases in frequency and intensity. Victims of such violence report feelings of isolation, helplessness, guilt, anxiety, and embarrassment. They may become suicidal, start abusing drugs and alcohol, and feel that they have no one to turn to for help.
Although there isn’t a specific set of factors that result in “being a victim,” there are many thoughts as to what might affect a person’s active willingness to remain in a violent relationship. The following lists serve only as general guidance to inform the healthcare professional of possible underlying causes. Again, anyone can become a victim of domestic violence.
Victims of Domestic Abuse
There is no single “characteristic” or risk factor that automatically causes a person to become a victim of domestic violence. Instead, it may be a series of events that cause a person to become more vulnerable and enter and remain within an abusive relationship [9].
Domestic violence victims may have experienced violence during childhood, experienced total financial dependence on another person, or lacked basic social support (family and friends). These factors affect both the physical and psychological make-up of a person. Without intervention, these victims can develop personal esteem and confidence issues, further social isolation, economic dependency, and general feelings of insecurity. These effects may negatively affect the decision to stay in an abusive relationship.
Researchers [10] have found the following factors may place a person at a higher risk of becoming a victim of domestic violence, including (but not limited to):
- Poor self-image/ low self-esteem
- Financial dependence on the abuser
- Feeling powerless to stop the violence or leave the relationship
- Personal belief that jealousy is an expression of love
Common characteristics of victims of domestic violence include, but are not limited to:
- A history of abuse
- A history of alcohol or substance abuse (for themselves or their partners)
- Financial and family stressors- low income, limited family/friends contact, poverty status
- A member of an ethnic minority/ immigrant group; Limited English vocabulary
- Holds traditional beliefs that they should be submissive in a relationship
Reasons a victim may choose to stay in the relationship:
- A desire to end the abuse but not necessarily the relationship; they do love their abuser.
- Feelings of isolation and helplessness
- Fear of judgment if they reveal the abuse by seeking help.
- Feelings that they may not be able to support themselves if they leave their abuser; Fears for the safety of children involved in the relationship.
- Fear of backlash from community or family and friends/lack of knowledge of services available
- Strong religious/cultural belief system that reinforces staying in a relationship at all costs.
Abusers/Perpetrators of Domestic Violence
As with the domestic violence victim, there is no one set of traits to identify a domestic violence abuser/ perpetrator correctly. There are, however, some signs that may raise the red flag of suspicion when observed in a suspected domestic violence case.
The National Coalition on Domestic Abuse [11] has created a list of “red flag” indicators, including, but not limited to, the following:
- Extreme jealousy and possessiveness
- Verbally abusive
- Extremely controlling behavior
- Blaming the victim for anything bad that happens
- Control over all the finances in the relationship
- Demeaning the victim publicly or privately
- Humiliating or embarrassing the victim in front of other people
- Control over what the victim wears
- Abuse of other family members, including children (and even pets)
The following is a general list of indicators that help “may” identify a possible abuser [12].
- History of abuse within one’s family
- History of personal physical or sexual abuse
- A lack of appropriate coping skills
- Low self-esteem
- Codependent behavior
- Untreated mental illness
- Drug or alcohol abuse
- Socio-economic pressures related to the lower income status
- Prior criminal history

Self-Quiz
Ask Yourself...
- Describe interventions/ resources currently available at your facility to assist a victim of domestic violence. What resources are currently available for domestic abuse perpetrators?
Initial Interaction and Screening Tools
Screening rates are as low as 1.5% to 13% among emergency and primary care physicians. The Academy of Medicine recommendation suggested that all women should be screened for sexual violence. Research found that healthcare providers working in emergency department only screened 20–25% of their encounters. As a result, this decreased opportunities for intervention, increased safety, and prevention of future violence [13].
Domestic violence (including Intimate partner violence) is an unfortunate cycle that may not be broken with a single emergency department visit; however, identifying and providing resources is necessary to make a difference, increase confidence and safety, and improve the overall health outcome for patients.
Compassionate, nonjudgmental screening by healthcare professionals affords the best opportunity for domestic violence victims to disclose their abuse. By recognizing signs of abuse and inquiring further, the nurse validates that the victim is worthy of care and confirms that the violence is a legitimate concern [14].
The screening for domestic abuse should be done in a private environment. Language interpreters, not family and friends, should be utilized if needed. Universal screening should be used; therefore, preventing any victim from being “singled out” and ensuring all potential victims are screened appropriately. All healthcare professionals should remain nonjudgmental and compassionate during the screening process [15].
During the interview process, assure the victim that all patients are screened for domestic violence. Be sure to include that DV affects many families and services are available to everyone who may be concerned about violence in their home.
An overview of domestic violence screenings follows. Links have been provided to an online copy of each screening tool.
Hurt, Insult, Threaten and Scream (HITS)
5 question screening tool assessing physical and verbal interactions with the partner; scores rank 1 (never) -5 (frequently); a score of 10 is considered positive.
- Physically hurt you?
- Insult or talk down to you?
- Threaten you with harm?
- Scream or curse at you?
- Force you to do sexual acts that you are not comfortable with?
http://www.ctcadv.org/files/4615/6657/9227/HPO_HITS_Screening_Tool_8.19.pdf
Woman Abuse Screening Tool (WAST)
8 question screening tool assessing physical, emotional, and sexual intimate partner violence.
http://womanabuse.webcanvas.ca/documents/wast.pdf
Partner Violence Screen (PVS)
3 question screening tool for interpersonal violence:
- Have you been hit, kicked, punched, or otherwise hurt by someone within the past year? If so, by whom?
- Do you feel safe in your current relationship?
- Is there a partner from a previous relationship who is making you feel unsafe now?
http://www.nnepqin.org/wp-content/uploads/2018/08/Screening-Tools-Partner-Violence-Screen-PVS.pdf
Abuse Assessment Screen (AAS)
A multiple section assessment tool for sexual and physical violence, including body maps for documentation of injuries.
https://idph.iowa.gov/Portals/1/Files/FamilyHealth/abuse_assessment_tool.pdf
The Crisis Prevention Institute (CPI) [16] encourages you to always be aware of physical signs and injuries that could be related to domestic violence, including but not limited to the following:
- Bruising in the chest and abdomen
- Multiple injuries
- Minor lacerations
- Ruptured eardrums
- Delay in seeking medical attention
- Patterns of repeated injury
- Injuries inconsistent with the presenting complaints
Oftentimes, a domestic violence victim may seek medical attention for issues unrelated to a physical injury, such as:
- A stress-related illness
- Anxiety, panic attacks, stress, and/or depression
- Chronic headaches, asthma, vague aches, and pains
- Abdominal pain, chronic pelvic pain
- Vaginal discharge and other gynecological problems
- Joint pain, muscle pain
- Suicide attempts, psychiatric illness
Other observations that may indicate a suspected domestic violence situation include:
- Appear nervous, ashamed, or evasive.
- Seem uncomfortable or anxious when around their partner.
- Be accompanied by their partner, who controls the conversation.
- Be reluctant to follow advice.
As you continue to assess the patient, encourage them to talk and then listen carefully. Only upon listening will you have a better understanding of the patient’s current state and provide the necessary resources and referrals for them to find safety. Above all else, maintain open lines of communication in a safe, accepting environment and assure the victim that they do not deserve the abuse.

Self-Quiz
Ask Yourself...
- What screening tools are currently available at your facility to assess for possible domestic abuse? Do you feel that they are effective?
- Domestic abuse victims may seek medical attention for issues unrelated to abuse (chronic headache, vague aches, and pain, anxiety, or depression). What further assessments can be done to assess for domestic violence?
Importance of Trauma-Informed Care
While nurses play a critical role in recognizing suspected domestic abuse victims, they often do not feel confident in their role or the screening process itself. This may be due to a lack of communication skills, ongoing training on domestic violence or simple confusion over what victim assistance programs and resources are available [17].
Facility-wide education on domestic violence should be ongoing. Policies and procedures should be on file, and collateral relationships should be in place with the local community and national resources. Finally, nurses should be trained in the delivery of trauma-informed care to ensure the highest quality of interaction with victims of domestic violence, much less all victims of trauma.
Trauma-informed care has been defined as the patient-centered approach that encourages healthcare professionals to provide care that does not retraumatize the patient and the staff [18]. Trauma-informed care ensures that policies and practices in the healthcare setting are not only safe but non-threatening to the physical and mental well-being of those involved. Perceived threats can cause a “flight or fright” mentality that impacts both the ability to administer care and receive immediate care and follow-up recommendations.
The experience of seeking medical care, whether in an emergency department setting or a clinic, can in and of itself being another source of trauma. Trauma-informed care aims at reducing the impact of trauma on both the patient and provider by focusing on various checkpoints overseeing all interactions: safety, trustworthiness, empowerment, and respect.
The following examples are practical tips that encourage trauma-focused care, ensuring the delivery of care in the least threatening manner to a suspected human trafficking victim (as well as each patient you may intersect with).
- Always introduce yourself and your role within the patient’s care with every interaction.
- Use open body language (direct eye contact, avoid standing “over “the patient as it may be perceived as threatening).
- Explain procedures and timelines for results (“wait times”) to give patients a sense of control. Keep them informed of any changes/delays in their care.
- Always ask before you touch a patient. This is a sign of respect and gives the patients a sense of control over their bodies.
- Protect patient privacy. Ask them who they would like present during their care; limit visitors if requested; close room doors (with their permission).
During the interview and intervention process, it is also equally important that some things NOT be said to a suspected victim of domestic violence, such as negating, challenging, or doubting the victim. Examples include:
- Why haven’t you called the police before now?
- Some level of fighting occurs in all relationships.
- Maybe you’re both going through a phase; it will probably stop on its own.
- You wouldn’t stay in this situation if you really care about yourself/ your kids.
- What did you do to make them get so angry?
- Why didn’t you leave the first time you were hurt?
By applying trauma-informed care to all your patients, you lower the risk of perceiving any (nursing and medical) interventions being perceived as a threat. This ensures a higher level of trust and respect, and safety for all patients (and staff) across the care spectrum.

Self-Quiz
Ask Yourself...
- Describe the possible consequences of doubting a victim of domestic violence.
- What can you do as a healthcare professional to ensure all patients are screened for domestic violence?
Legal Issues: Florida Mandatory Reporting Laws
The United States Department of Justice [19], defines domestic violence to include felony or misdemeanor crimes of violence committed by:
- a current of former spouse or intimate partner of the victim,
- by a person with whom the victim shares a child in common,
- by a person cohabitating with or has cohabitated with the victim as a spouse or intimate partner,
- by a person similarly situated to a spouse of the victim under the domestic or family violence laws of the jurisdiction receiving grant monies,
- by any other person against an adult or youth protected from that person’s acts under the jurisdiction’s domestic or family violence laws.
The Florida Department of Children and Families defines domestic violence as patterns of actions or behaviors that adults or adolescents use against their partners or former partners to establish power and control. It can potentially include physical abuse, sexual abuse, emotional abuse, and economic abuse. It may also include threats, isolation, pet abuse, using children, and a variety of other behaviors used to maintain fear, intimidation, and power over one’s partner (19).”
Under Florida law [21], Domestic Battery is classified as a first-degree misdemeanor, with penalties including up to one year in jail or twelve months’ probation and a $1,000 fine. In addition, the accused may face additional penalties of a mandated Batterer Intervention Program.
RAINN (Rape, Abuse, and Incest National Network) [22] is the nation’s largest anti-sexual violence organization. Under the “Laws of your state” section, they outline the mandatory reporting laws for Florida.
Mandatory Reporting Requirements on Children
Children are defined as any unmarried person under the age of 18 years who has not been emancipated by court order.
Who is required to report (from a healthcare professional standpoint):
- Physicians
- Osteopaths
- Medical examiners
- Chiropractors
- Nurses
- Hospital personnel
When is a report required:
- When any person knows or has cause to suspect that a child is abused, abandoned, or neglected by a parent, legal custodian, caregiver, or another person responsible for the child’s welfare, or that a child is in need of supervision and care and has no one to provide supervisional care.
- When any person knows or has cause to suspect that a child is abused by an adult other than a parent, legal custodian, or another person responsible for the child’s welfare.
- When any person knows or has cause to suspect that the child is a victim of childhood sexual abuse or the victim of a known or suspected juvenile sexual offender.
Reports can be made to the Department of Children and Family Services’ abuse hotline at (1-800-962-2873)

Self-Quiz
Ask Yourself...
- What policies and protocols are in place at your facility regarding mandatory reporting?
- Who can initiate a report?
- What departments are notified, at your facility, if a report is made?
Elements of a Safety Plan (Escape Plan)
Abusers may go to extremes to prevent a victim from leaving. This may result in the decision to escape an abusive relationship, one of the most dangerous times for the victim of domestic violence. The creation of a safety plan can assist in enhancing the safety of a victim during all phases of a relationship and during the planning phase of actually leaving the abuser.
Knowledge of the various elements of a safety plan will enable the healthcare professional to initiate dialogue with a victim and guide them in the development of a personalized plan of safety moving forward. Discussion of safety plans/escape plans can be very difficult during the limited interactions of an emergency room or clinic visit; therefore, familiarity with the key elements of a plan will help navigate the victim to the most appropriate resources for their situation.
The following overviews of a safety plan are from Safe Horizon [23] and the National Domestic Violence Hotline [24]. The Safe Horizon is victim assistance nonprofit for victims of violence and abuse in New York City since 1978. The following outline provides a detailed overview of the many aspects to consider when formulating a safety plan. Review the entire plan outlined on their website. Consider creating a template handout for your facility to distribute to domestic violence victims.
A safety plan is an outline that includes ways to remain safe while in a relationship, planning to leave, or after you leave (23). A personalized safety plan assists in coping with emotions, telling friends and family about the abuse, and the steps to be taken in the event of necessary legal action. An effective safety plan should have specific details tailored to your unique situation.
Considerations in creating your safety plan:
- Do you have a trusted confidant – a friend, family member, or neighbor?
- Where are some areas in your neighborhood that you could go to in an emergency?
- Are there phone numbers you need to memorize in the event of an emergency?
- Do you have children that need to be part of your safety plan? Where would your children go if they witnessed violence?
- Do you need a safety plan for work school?
- Where can you safely store your safety plan? Computer? Phone?
Before Leaving
The decision to leave an abusive relationship requires courage and pre-planning. Consider these measures before leaving to reduce the risk of violence (23):
- Record evidence of physical abuse
- Plan with children and identify a safe place where they can go during moments of crisis. Reassure them that their job is to stay safe, not to protect you.
- Call ahead to see what the shelter’s policies are. They can provide information on how they can help and secure a space when it is time to leave.
- Try to set money aside or ask trusted friends or family members to hold money for you.
When Leaving
The following list of items serves as a guide for what to take (23):
Identification
- Driver’s license or state I.D. card, social security card
- Birth certificate and children’s birth certificates
- Money and/or credit cards
- Checking and/or savings account books
Legal papers
- A protective order, if applicable
- Health and life insurance papers
- Legal documents, including divorce and custody papers
- Marriage license
Emergency numbers
- Local domestic violence program or shelter
- Trusted friends and family members
- The Hotline
Other items to keep in mind:
- Medications and refills (if possible)
- Emergency items, like food, bottles of water, and a first aid kit
- Multiple changes of clothes
- Emergency money
- Address book
- Safe cell phone, if possible
After Leaving
The safety plan should always include ways to ensure your continued safety after leaving an abusive relationship. Here are some precautions to consider (23):
- Change locks and phone numbers if possible.
- If possible, change work hours and the typical route.
- Alert school authorities of the situation.
- If a protection order is present, keep a certified copy present at all times, and inform friends, neighbors, and employers that you have a protection order in effect.
- Consider renting a post office box or using a trusted friend’s address for mail (remember that addresses are used for restraining orders and police reports)
- Use different stores and frequent different social spots.
- Alert neighbors and work colleagues about how and when to seek help.
Tell people who take care of children (if you are comfortable doing so) or transport them to/from school and activities.
Again, these suggestions provide an extensive overview of an escape plan. They are meant to assist a victim in the required methodical preplanning of a safety plan that reduces the threat of violence. Not all sections will apply to every victim, but healthcare professionals should be comfortable in discussing any aspects of a safety plan specific to the individual victim.
The Effects of COVID-19 on Domestic Violence
As discussed at the beginning of this educational offering, the COVID-19 pandemic has negatively affected domestic violence incidence. Stay at home /shelter in place orders, job losses, and mounting financial concerns, and lack of available shelters in many areas became the norm. Domestic violence victims have met with further hurdles to their safety and well-being, as they found themselves sheltering in place with their abuser, along with fewer resources available to them in their time of crisis.
Domestic violence hotlines prepared for an increase in calls; many organizations found the opposite was occurring. Calls to hotlines dropped, in some places greater than 50 percent. Victims were not able to safely connect with necessary services [25].
Due to the restrictions of movement (curfews, travel bans, 14-day quarantine advisories), not only is it more difficult to escape, but injury from abuse may go unnoticed by family and friends as face-to-face interactions have been sidelined. In addition to job losses and financial insecurities, this isolation may force a victim to become even more dependent on their abuser [26].
In March 2020, U.S. police departments reported an increase in domestic violence calls as high as 27% after stay-at-home orders were implemented. The number of Google searches for family violence-related help during the outbreak has been substantial. This increase in domestic violence has not only affected the United States. In the United Kingdom, calls to the Domestic Violence Helpline increased by 25% in the first week after implementing lockdown measures. Furthermore, In China, domestic violence has reportedly increased three times in Hubei Province during the lockdown [27]. The importance of ongoing domestic education and awareness cannot be overstated.
In review, healthcare settings are often treating victims of domestic violence. Trauma-informed care that is patient-focused affords both the staff and patient (victim) the best outcome in terms of successfully navigating the challenges of domestic violence and mandatory reporting laws.
Facility-wide protocols should be in place regarding all aspects of patient care for suspected victims of domestic violence: national hotline numbers, community resources, scene safety protocols, and house-wide education. Staff should be regularly in-serviced on interviewing techniques, suspected DV victim indicators, and ongoing community collateral relationships. Improved recognition of these victims and knowledge on how to proceed with specific treatment protocols will lead to a higher level of positive outcomes for domestic violence victims and other forms of abuse.
Time is of the essence when dealing with victims of DV. There may be a small window of opportunity to help these victims when they present to your facility. There may be numerous needs identified quickly (transportation, housing, interpretation services, crisis intervention, case management, safety planning, transitional shelter, and protective orders, to name a few). Staff must feel confident in their abilities to identify possible victims, guide them through the process of seeking help, and advocate for their safety and well-being. Knowledge of their facility protocols and community, state, and national resources will afford them the opportunity to deliver optimal care.

Self-Quiz
Ask Yourself...
- Can you give examples of what your facility is doing to address the issue of domestic violence?
- How has COVID-19 affected your facility in terms of the availability of community resources for victims of domestic violence?
- What improvements can be made at your facility regarding domestic violence education and awareness?
Case Study on Domestic Abuse
Mary, 26 years old, presents to the emergency department with complaints of abdominal pain, vague body aches, and a headache. During the triage screening, Mary has minimal eye contact with the nurse and appears inadequately dressed for the cold weather, arriving in only jeans, a t-shirt, gym shoes, and a light sweater. While the nurse helps Mary change into a hospital gown in a private examination room, she notices various bruises on Mary’s lower back, arms, and legs, all varying size and color. Mary states she slipped and fell recently at home. You observe that Mary is now avoiding all eye contact, staring down at the ground. She keeps looking at the door, and wall clock, mumbling, “he can’t know I’m here.”
What are your initial thoughts about Mary’s physical appearance?
What can you do to make Mary feel more relaxed, comfortable, and safe during her emergency room visit?
Mary lives with her boyfriend, Bill. He works part-time; she is currently unemployed. She admits to the occasional use of alcohol and recreational use of marijuana “to help me relax; my anxiety is very bad lately.” She mentions that her anxiety has increased because “Bill’s hours at work have been cut due to COVID-19 and were strapped for money. He is under a lot of pressure”.
On further examination and laboratory testing, including a pelvic examination, it is confirmed that Mary is approximately six weeks pregnant and has a suspected STI. Mary bursts into tears and says, “he is going to kill me. We can’t afford a baby; what am I going to do?!”
What are your concerns about this scenario? How will you address these concerns with your patient, Mary?
Why might healthcare professionals, in general, feel uncomfortable talking with Mary?
What are the top priorities of Mary’s care at this time?
What information would you document in the patient record during this visit?
Mary begins to feel comfortable speaking to you about her situation. She reluctantly tells you that Bill pushed her down the back stairs yesterday after an argument but quickly apologized afterward. On another occasion, Bill “beat me up” when he ran out of beer before payday. She states he has been really angry lately over his hours being cut at work and is looking for another job. “A baby now”, Mary confides, “would be a terrible thing for Bill, but I want it. It’s my first, and I want it. Please help me”. Mary gives consent for you to contact your department social worker for additional guidance but does not want law enforcement notified.
What other key staff members need to be part of the care team for Mary?
What local and national resources can you refer Mary to at this time?
How would your plan of care change if Mary did not give consent for the social worker to be notified?
Mary wants to “go back home” tonight so as not to upset Bill when he returns later this evening. “It will be better this way.” She promises to leave him tomorrow and follow-up with the community referrals you gave her. Knowing that these plans may change, you advise Mary to create a safe escape plan “just in case.”
What items should be part of a safe escape plan?
How safe is it for Mary to return home?
What are your legal obligations to Mary regarding Florida’s mandatory reporting laws?
As you are getting ready to leave at the end of your shift hours later, you see Mary arrive by ambulance. She is visibly injured with a broken nose and bloody lip. EMS staff state the neighbors called 911 when they heard Mary screaming in her apartment next door. No one else was in the apartment when they entered, and Mary will not tell them who injured her. You escort them to a private examination room. Mary sees you and yells, “he’s coming after me. Help me. He is going to kill me.”
What are your top priorities for Mary and the staff at this time?
What other hospital departments need to be notified?
Mary’s boyfriend shows up, intoxicated, at the triage window, demanding to see Mary. He threatens to kick in the door to the main examination room if he cannot see Mary immediately. He is pacing back and forth in the triage area and refuses to sit down.
What additional security measures need to be in place upon the boyfriend’s arrival?
Mary’s boyfriend is removed from the premises by local law enforcement. Mary is given the national hotline number and is contacting the local shelter at this time. Upon discharge, she is escorted by security personnel to the exit and leaves the facility with a shelter representative.
Domestic Violence Resources
Florida Specific Domestic Violence Resources
1. Community Legal Services of Mid- Florida
https://www.clsmf.org/violence-protection/
A full service civil legal aid law firm that promotes equal access to justice, providing professional legal aid on domestic violence to help low-income people protect their health, and their families.
2. Coast to Coast Legal Aid of South Florida
https://www.coasttocoastlegalaid.org/
The Family Law Unit primarily focuses on representing victims of domestic violence in family law matters, such as obtaining an injunction (restraining order), dissolution of marriage cases (divorce), and custody litigation.
3. Domestic Shelters.org
https://www.domesticshelters.org/help/fl.florida
Overview of 58 Florida based organizations offering domestic violence services in 47 different cities.
Florida Department of Children and Families
1. Florida Family Policy Council
https://www.flfamily.org/get-help/domestic-violence
Resources to assist victims (and family members) to find help, safe shelter, legal aid, transitional services, and counseling.
2. Child Protective Services
https://www.myflfamilies.com/service-programs/abuse-hotline/
1-800-962-2873 / TTY: 1-800-955-8771
3. The Florida Abuse Hotline accepts reports 24 hours a day and 7 days a week of known or suspected child abuse, neglect, or abandonment and reports of known or suspected abuse, neglect, or exploitation of a vulnerable adult.
https://reportabuse.dcf.state.fl.us/
5. Domestic Violence Hotline 1-800-500-1119
These services include emergency shelter, counseling, safety planning, case management, child assessments, information, and much more.
These shelters may be viewed on the MyFlFamilies.com website. Healthcare professionals should be familiar with shelters available in their surrounding area.
6. Harbor House of Central Florida
https://www.harborhousefl.com/get-help/safety/ (407) 886-2856
Offering housing placements service, legal aid, safety planning, support groups, and crisis intervention.
7. The 15th Judicial Circuit of Florida Batterers Intervention Program (BIP)
https://www.15thcircuit.com/program-page/bip
The Florida BIP is a 6-month intensive program to address root causes of domestic violence; it is at least 26 weeks of group counseling sessions. A list of statewide providers is available on this site.
8. The Salvation Army
https://salvationarmyflorida.org/domestic-violence-program/
Offering emergency and transitional housing, as well as counseling and rehabilitation services.
National Domestic Violence Resources
1. Amend, Inc.
AMEND is a nonprofit organization working to end domestic violence by providing counseling to men who have been abusive, advocacy and support to their partners and children, and education to the community. Based in Colorado.
2. Emerge
https://www.emergedv.com/ 617-547-9879
Emerge is a Massachusetts Certified Batterer Intervention Program & Training Site, offering abuser education groups and batterer intervention. Based in Massachusetts.
3. National Domestic Violence Hotline
1-800-799-SAFE (7233)
4. Domestic Violence Prevention, Inc
https://www.dvptxk.org/ 903-793-HELP (4357)
501C3 nonprofit offering education, counseling, and support services to domestic violence clients in multiple counties in Texas and Arkansas.
5. National Center on Domestic Violence, Trauma and Mental Health
http://www.nationalcenterdvtraumamh.org/resources/national-domestic-violence-organizations/
Offering direct website links to multiple national organizations working with domestic violence cases
6. National Network to End Domestic Violence
Offers a range of programs and initiatives to address the complex causes and far-reaching consequences of domestic violence.
7. New York Model for Batterer Programs
https://www.nymbp.org/ 845-842-9125
Court-ordered program for batterer education, which includes a court-imposed consequence if the offender does not attend. Based in New York.
8. Women’s Law
Providing state-specific legal information and resources for survivors of domestic violence.
References
- National Statistics. (n.d.). National Coalition Against Domestic Violence. Retrieved February 7, 2021, from https://ncadv.org
- Sharma, A., & Borha, S. (2020, July 28). Covid-19 and Domestic Violence: An Indirect Path to Social and Economic Crisis. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386835/
- What is domestic abuse? (n.d.). Https://Www.Un.Org/En/Coronavirus/What-Is-Domestic-Abuse. Retrieved February 8, 2021, from https://www.un.org/en/coronavirus/what-is-domestic-abuse
- Centers for Disease Control and Prevention. (2020, October 9). Intimate Partner Violence. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/violenceprevention/intimatepartnerviolence
- Centers for Disease Control and Prevention. (2020a, March 9). Preventing Teen Dating Violence. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/injury/features/dating-violence
- National Coalition Against Domestic Violence (2020). Domestic violence. Retrieved from https://assets.speakcdn.com/assets/2497/domestic_violence-2020080709350855.pdf?1596811079991
- Yousefnia, N., Nekuei, N., & Farajzadegan, Z. (2018, July 10). Injury and Violence. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6101232/
- National Coalition Against Domestic Violence. (n.d.). Dynamics of Abuse. National Coalition Against Domestic Violence (NCADV). Retrieved February 9, 2021, from https://ncadv.org/dynamics-of-abuse
- Pereira, M., Azeredo, A., Moreira, D., Brandão, I., & Almeida, F. (2020, May). Personality characteristics of victims of intimate partner violence: A systematic review. Science Direct. https://www.sciencedirect.com/science/article/abs/pii/S1359178919302642
- Axelrod, J. (2016, May 17). Who Are the Victims of Domestic Violence? PsychCentral. https://psychcentral.com/lib/who-are-the-victims-of-domestic-violence#1
- National Coalition Against Domestic Violence. (n.d.-b). Signs of Abuse. Retrieved February 9, 2021, from https://ncadv.org/signs-of-abuse
- Domestic Shelters (2014, July 1). Profile of an Abuser. Domestic Shelters. https://www.domesticshelters.org/articles/identifying-abuse/profile-of-an-abuser
- Emergency Nurses Association. (2018). Intimate Partner Violence. Emergency Nurses Association (ENA). https://www.ena.org/docs/default-source/resource-library/practice-resources/position-statements/joint-statements/intimatepartnerviolence.pdf?sfvrsn=4cdd3d4d_8
- Bettencourt, E. (2019, October 4). Domestic Violence and How Nurses Can Help Victims. Diversity Nursing. http://blog.diversitynursing.com/blog/domestic-violence-and-how-nurses-can-help-victims
- Stanford Medicine. (2020). How to Ask. https://domesticabuse.stanford.edu/screening/how.html
- Power, C. (n.d.). Domestic Violence: What Can Nurses Do? Crisis Prevention Institute (CPI). Retrieved February 11, 2021, from https://www.crisisprevention.com/Blog/Domestic-Violence-What-Can-Nurses-Do
- Alshammari, K., McGarry, J., & Higginbottom, G. (2018, July 5). Nurse education and understanding related to domestic violence and abuse against women: An integrative review of the literature. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6056448/
- Fleishman, J., Kamsky, H., & Sundborg, S. (2019, May). Trauma-Informed Nursing Practice. The Online Journals of Issues in Nursing (OJIN). https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-24-2019/No2-May-2019/Trauma-Informed-Nursing-Practice.html
- The United States Department of Justice. (n.d.). Domestic Violence. U.S. Department of Justice. Retrieved February 9, 2021, from https://www.justice.gov/ovw/domestic-violence
- Houseman, B., & Semien, G. (2020, October 17). Florida Domestic Violence. National Center for Biotechnology Information (NCBI). https://www.ncbi.nlm.nih.gov/books/NBK493194/
- Domestic Battery under Florida Law. (2019). Hussein and Webber, PL. http://www.husseinandwebber.com/crimes/violent-crimes/domestic-violence-battery/
- Rape, Abuse, and Incest National Network (RAINN). (n.d.). The laws in your state: Florida. Retrieved February 14, 2021, from https://apps.rainn.org/policy/?&_ga=2.161880060.1354221772.1613679799-1191886798.1613418373#report-generator
- Safe Horizon. (n.d.). Safety Plan for Domestic Violence Survivors. Retrieved February 9, 2021, from https://www.safehorizon.org/our-services/safety-plan/?gclid=Cj0KCQiApY6BBhCsARIsAOI_GjYsM6rkXLswOpzipsjGADI_JOewgRMdKX39WcUjaB14uFcYieLmM5saAmFREALw_wcB
- National Domestic Violence Hotline. (n.d.). Create a safety plan. Retrieved February 12, 2021, from https://www.thehotline.org/create-a-safety-plan/
- Evans, M. L., Lindauer, M., & Farrell, M. E. (2020). A Pandemic within a Pandemic — Intimate Partner Violence during Covid-19. New England Journal of Medicine, 383(24), 2302–2304. https://doi.org/10.1056/nejmp2024046
- Wallace, A. (2020, November 4). 11 Things to Know About Domestic Violence During COVID-19 and Beyond. Healthline. https://www.healthline.com/health/things-to-know-about-domestic-violence
- Xue, J., Chen, J., Chen, C., Hu, R., & Zhu, T. (2020). The Hidden Pandemic of Family Violence During COVID-19: Unsupervised Learning of Tweets. Journal of Medical Internet Research, 22(11), e24361. https://doi.org/10.2196/24361
Florida HIV/AIDS
Introduction
An estimated 1.2 million Americans are living with HIV. As many as 1 in 7 of them do not even know they are infected. The others utilize the healthcare system in a variety of ways, from testing and treatment regimens to hospitalizations for symptoms and opportunistic infections. Healthcare professionals in nearly every setting have the potential to encounter patients with HIV as the disease can affect patients of any age or stage of life (4). Proper understanding of HIV is important in order to provide high-quality and holistic care to these patients. For nurses practicing in the state of Florida, it is also important to understand the laws, statutes, and regulations regarding testing, treatment, reporting, and confidentiality related to HIV and AIDS within the state.
Today, approximately 1.2 million people in the United States are living with HIV, though 1 in 7 people don’t know it. Rates of infection are not equal across demographic groups, and certain factors may increase a person’s risk (7). Patient information to consider when determining someone’s risk includes:
Age
As of 2018, the age group with the highest incidence of new HIV diagnoses is 25-34 years or approximately 36% of new infections. Ages 13-24 are next, though the numbers in this age range are coming down in recent years. From there, the risk seems to decrease as people age, with the 55 years and older group accounting for only around 10% of new diagnoses each year (7).
Race/Ethnicity
Currently, the highest rate of new infections is in African Americans, at approximately 45%. This is incredibly high when you consider that African Americans only make up 13% of the general population. This is followed by Hispanic/Latinos at 22% of new infections and people of multiple races at 19% (6).
Gender
Men are disproportionately affected by HIV, accounting for five times the amount of new infections as females each year. This data refers to the sex of someone at birth. When looking at the transgender population, there is a nearly equal rate of new infections among those who have transitioned male-to-female and female-to-male. Together, transgender people account for 2% of new cases in 2018 (6).
Sexual Orientation
Gay and bisexual men remain the population most at risk of HIV, accounting for around 69% of all new infections in 2018 and 86% of all males diagnosed. Similar racial and ethnic disparities affecting all people with HIV still existed among gay and bisexual men (6).
Location
Different areas of the country are affected at different rates for a variety of factors, including population density, racial distribution, and access to healthcare. The southern states are unmistakably more affected than other regions, with anywhere from 13-45 people per 100,000 having a diagnosis of HIV. California, Nevada, New York, and DC all having similar rates of infection as the southern states and are among the highest in the country. The Midwest and Pacific Northwest are next most affected, with 9-13 people per 100,000. The Northeast and Northwest have the lowest rates nationally at just up to 5 people per 100,000 (6).
Transmission
Perhaps the most elusive part of this virus for many years was how it spreads. We now know that HIV is spread only through certain bodily fluids. An accurate understanding of HIV transmission is important for healthcare professionals to provide proper education to their patients, reduce misconceptions and stigmas, and prevent transmission and protect themselves and other patients (8).
Bodily fluids that can transmit the virus include:
- Blood
- Semen and pre-seminal fluid
- Rectal fluid
- Vaginal fluid
- Breastmilk
- Fluids that may contain blood such as amniotic fluid, pleural fluid, pericardial fluid, and cerebrospinal fluid
If one of these fluids comes in contact with a mucous membrane such as the mouth, vagina, rectum, etc., or damaged tissue such as open wounds, or is directly injected into the bloodstream, then transmission of HIV is possible (8).
Scenarios where transmission is possible include:
- Vaginal or anal sex with someone who has HIV (condoms and appropriate treatment with antivirals reduce this risk)
- Sharing needles or syringes with someone who has HIV
- Mother-to-child transmission during pregnancy, delivery, or breastfeeding (appropriate treatment during pregnancy, c-section delivery, and alternative feeding methods reduce this risk)
- Receiving a transfusion of infected blood or blood products (this is very rare now because of screening processes for blood donations)
- Oral sex with someone who has HIV (though this is very rare)
- A healthcare worker receiving a needle stick with a dirty sharp (risk of transmission is very low in this scenario)
HIV cannot be transmitted via:
- Saliva
- Sputum
- Feces
- Urine
- Vomit
- Sweat
- Mucous
- Kissing
- Sharing food or drink
Reducing Transmission & Infection Control
Patient education about risk and protection against HIV, testing, and what to do if exposed should be standard practice for healthcare professionals in nearly all healthcare settings. Primary care should include risk screenings and patient education routinely to ideally help prevent infections from even occurring or catch those that have occurred early on in the disease process (8).
Strategies include:
- Identifying those most at risk, incredibly gay or bisexual men, minority patients, and those using drugs by injection
- Ensure patients are aware of and have access to protective measures such as condoms and clean needle exchange programs
- Provide routine screening blood work for anyone with risk factors or desiring testing
- Providing access to PrEP medications where indicated (discussed further below)
- Staying up to date on current CDC recommendations and HIV developments
- Maintaining a nonjudgmental demeanor when discussing HIV with patients to welcome open discussion (8)
For patients with a repeated or frequent high risk of HIV exposure, such as those with an HIV+ partner or those routinely using IV drugs, pre-exposure prophylaxis (PrEP) may be a good choice to reduce the risk of them contracting the virus. When used correctly, PrEP is 99% effective at preventing infection from high-risk sexual activity and 74% effective at preventing infection from injectable drug use. Depending on the type of exposure risk (anal sex, vaginal sex, needle sharing, etc.), PrEP needs to be taken anywhere from 7-21 days before it reaches its maximum effectiveness. Most insurances, including Medicaid programs, cover PrEP at least in part. There are also federal and state assistance programs available to make PrEP available to as many people who need it as possible. Some side effects are commonly reported, primarily GI symptoms, headaches, and fatigue (8).
For those who have a confirmed diagnosis of HIV/AIDS, the focus should be promoting interventions that will prevent further transmission. One of the biggest determinants for transmission is the infected person’s viral load. Individuals being treated for HIV can have their viral load measured to ensure viral replication is being controlled as intended. A viral load lower than 20-40 copies per milliliter of blood is considered undetectable, meaning the virus is not transmissible to others. Even for those not receiving treatment, there are methods to reduce transmission (8).
Methods of infection control for healthcare professionals include:
- Universal precautions when handling any bodily fluids
- Eyewear when at risk for fluid splashing
- Careful and proper handling of sharps
- Facilities having a standard plan in place for potential exposures
If exposure or needlestick do occur for healthcare professionals, the patient would ideally submit to testing for HIV to determine if the staff member is even at any risk. If the HIV status of the patient is unknown or confirmed to be positive, four weeks of post-exposure prophylaxis (PEP) may be advised within 72 hours of exposure (8).
Treatment
When HIV is appropriately treated, advancement from HIV to AIDS can be significantly reduced, and quality and longevity of life maximized. In 2018, the CDC estimated around 65% of all US citizens living with HIV were virally suppressed, and 85% of those receiving regular HIV-related care were considered virally suppressed. However, an estimated13% of all HIV cases do not know they are infected. Appropriate medical care and keeping viral loads undetectable is one of the single most effective methods of preventing transmission (4, 5).
For those receiving treatment, a multifaceted and individualized approach can reduce a person’s viral load, reduce the risk of transmission, reduce the likelihood of developing AIDS, and preserve the immune system. Regardless of how early someone receives treatment, there is no cure for HIV, and an infected person will be infected for life. All individuals diagnosed with HIV (even asymptomatic people, infants, and children) should receive antiretroviral therapy or ART as quickly as possible after a diagnosis of HIV is made.
The classes and available meds for ART include (1):
- Nucleoside reverse transcriptase inhibitors (NRTIs): these inhibit the transcription of viral RNA to DNA
- Abacavir (Ziagen)
- Emtricitabine (Emtriva)
- Lamivudine (Epivir)
- Tenofovir disoproxil fumerate (Viread)
- Zidovudine (Retrovir)
- Non-nucleoside reverse transcriptase inhibitors (NNRTIs): these inhibit the transcription of viral RNA to DNA
- Doravirine (Pifeltro)
- Efavirenz (Sustiva)
- Etravirine (Intelence)
- Nevirapine (Viramune, Viramune XR)
- Rilpivirine (Edurant)
- Protease inhibitors: inhibit the final step of viral budding
- Atazanavir (Reyataz)
- Darunavir (Prezista)
- Fosamprenavir (Lexiva)
- Ritonavir (Norvir)
- Saquinavir (Invirase)
- Tipranavir (Apitvus)
- Fusion inhibitors: prevent the virus from fusing with CD4-T cells
- Enfuvirtide (Fuzeon)
- Integrase strand transfer inhibitors (INSTIs): these stop HIV from inserting its DNA into cells
- Dolutegravir (Tivicay)
- Raltegravir (Isentress, Isentress HD)
- Chemokine receptor antagonists (CCR5 antagonists): prevent the virus from binding to CD4-T cells
- Maraviroc (Selzentry)
- Entry inhibitors: prevent the virus from binding to and entering cells
- Ibalizumab-uiyk (Trogarzo) (1)
Florida Law on HIV/AIDS
The Omnibus AIDS Act is based on the premise that illness can be best controlled through public knowledge. If the public is aware of potential illness, and ways to avoid contracting and transmitting illness, that is the best method of prevention and further spread (2). The state of Florida became one of the first states with high rates of HIV infection within their population to enact legislation surrounding the AIDS epidemic. Transmission of HIV, as aforementioned, occurs through direct contact with virus-containing body fluids. Activities by which transmission involves such as sexual activity, needle stick, blood transfusion, or mother to baby, the government cannot regulate. Therefore, the governmental response to a disease epidemic must rely primarily upon the education of the public and its cooperation with their educational efforts and recommendations (2).
Protocols and Procedures for Testing
Healthcare providers performing HIV tests must have advanced procedures in place regarding patient consent, testing samples, and informing patients of their results (2). The informed consent requirement based on the Omnibus act allows the patient to control when and where an HIV test can occur (2).
Health care providers must: (2)
- Disclose that they, as the healthcare provider, are required by law to report the patient’s name to the local county health department if the HIV test results as positive.
- Alert the patient that they may secure an HIV test at a testing site that performs anonymous testing, which the provider is required to make available.
- Explain that the information identifying the patient and the results of the test are confidential and protected.
The rule that parental consent is required before medical diagnosis or treatment of a minor does not apply when sexually transmitted diseases are involved (2). Florida expressly forbids telling parents information relating to the minor’s consultation, examination, or treatment for an STD such as an HIV infection, either directly or indirectly (2). The state of Florida does not require providers to have the patient sign a written document authorizing the test. The health care provider is only responsible for entering a note within the patient’s medical record that the test was explained, and verbal consent was obtained (2).
Exceptions to informed consent requirements by HCP’s (2).
Pregnancy
In 2005, the Florida statute was amended to establish the system of “opt out” testing. In this system, pregnant women are advised that the HCP will conduct an HIV test. However, they have a right of refusal. If an objection is present, it is required in writing to be placed within the patient’s medical record. The rule 64D-2.004, FAC, also requires repeating testing procedures at 28-32 weeks gestation for all STD’s including HIV (2).
Emergencies
A provider can test without consent in a medical emergency only if the provider documents it within the medical record that the results are medically necessary to provide appropriate treatment to the patient if they are unable to consent. This is based on §381.004(3)(h)3, FS.
Therapeutic Privilege
Therapeutic Privilege bypasses informed consent requirements when the provider’s medical record documents that obtaining informed consent would be detrimental to the health of a patient suffering from an acute illness and that the test results are necessary for medical diagnostic purposes to provide appropriate treatment to the patient. This is based on §381.004(3)(h)4, FS.
Sexually Transmissible Diseases
The state law of Florida permit HIV testing for HIV on specific subjects such as convicted prostitutes (§796.08, F.S.), inmates prior to release (§945.355, FS), and cadavers over which a medical examiner has asserted authority(§381.004(3)(h)1.c) without the consent of the subject.
Criminal Acts
Victims of criminal offenses involving transmission of body fluids may require the person convicted or charged of the offenses to be tested for HIV by requests of a court order (§960.003, FS (2).
Organ and Tissue Donations
Provisions permit testing without informed consent with certain blood and tissue donations (§§381.004 (3), 5 and 9, FS.
Research
Established epidemiologic research methods that ensure test subject anonymity is expected from informed consent (§381.004(3)(h)8, FS)
Abandoned Infants
When a physician determines that it is medically indicated that a hospitalized infant have HIV test, but the infant’s parents or legal guardian cannot be located after reasonable attempts, the test may be performed without consent, with the reason being documented in the medical record and the test result being provided to the parent or guardian once they are located (§381.004(3)(h)13, FS).
Significant Exposure
The blood source of significant exposure to medical personnel or to others who render emergency medical assistance may be tested without informed consent (§381.004(3)(h)10-12, FS).
Repeat HIV Testing
Renewed consents agree not required for repeat HIV testing to monitor the clinical progress of a previously diagnosed HIV-positive patient (§§381.004(2)(h)14 and 15, FS.)
Judicial Authority
A court may order an HIV test to be performed without the individual’s consent (§381.004(3)(h)7, FS).
Confidentiality
If an HIV test was performed on an identifiable individual, and any “HIV test result” (negative or positive) is specially protected (§381.004(2)(e), FS). The state of Florida defines the definition of an HIV test and an HIV test result explicitly. An HIV test, as defined by the Florida Statutes, is “a test ordered after July 6, 1988, to determine the presence of the antibody or antigen to human immunodeficiency virus or the presence of human immunodeficiency virus infection (2).” An HIV test result as defined by the Florida statutes is “A laboratory report of a human immunodeficiency virus test result entered into a medical record on or after July 6, 1988, or any report or notation in a medical record of a laboratory report of a human immunodeficiency virus test (2).”
The results are excluded as an acceptable “HIV test result” if a patient reports of their HIV- test status from Department of Health anonymous testing sites, from home access HIV test kids, or from any other sources that do not constitute “HIV test results” unless separately confirmed by the provider through a laboratory report or as a medical record (2)
Any patient disclosures of an HIV test or positive infection to any persons other than health care providers caring for the patient under the provisions of the Omnibus Act also do not fall within the statute’s special confidentiality protections.
Voluntary Partner Notification
The person ordering the HIV test is required to advise their patients with HIV-positive test results of the importance of notifying partners who may have been exposed (2). Practitioners are also advised to tell the patient of the availability of voluntary partner notification services provided by the Department of Health. When notifying partners, county health department staff are required NOT to reveal the original client’s identity. Partner notification makes persons aware of their potential exposure to HIV, providing them with referrals to testing, treatment options, and other services (§381.004(3)(c), FS). Notification services also benefit the community by leading to earlier HIV identification and treatment of previously undiagnosed cases of HIV.
HIV Infection Reporting
Florida was one of the first states with a high incidence of AIDS to authorize regulatory procedures requiring physicians and labs to report HIV-positive test results to local health authorities (§384.25, FS). Per Florida law, practitioners and clinical labs that fail to report HIV0positive test results are subject to a $500 fine along with disciplinary action by their individual licensing boards (§384.25, FS) (2,3).
The Ryan White CARE Act, which was enacted in 1990 and reauthorized in 2009 as the Ryan White HIV/AIDS Treatment Extension Act, provides funding to urban areas, states, and localities to improve the availability of care for low income, uninsured and under-insured AIDS and HIV-infected patients and their families (2).
Florida’s HIV infection reporting requirement increases the funding for persons with the illness and enables the HOH to link them to medical support and services in the early stages of infection.
Under the rules by the DOH of Florida (2,3):
- Practitioners must report to their local county health department within two weeks of the HIV-positive diagnosis of all persons, EXCEPT infants born to HIV-positive women, which must be reported the next business day (Rule 64D-3.029, FAC and Rule 64D-3.030(5), FAC.)
- Clinical laboratories must report to the local health department HIV test results from blood specimens within three days of diagnosis (Rule 64D-3.029, FAC).
References
- Arts, E. J., & Hazuda, D. J. (2012). HIV-1 antiretroviral drug therapy. Cold Spring Harbor perspectives in medicine, 2(4), a007161. https://doi.org/10.1101/cshperspect.a007161
- Hartog, J., & Robinson, G. (2013, August). Florida’s Omnibus Act: A brief legal guide for healthcare professionals. Retrieved February 25, 2021, from http://www.floridahealth.gov/diseases-and-conditions/aids/administration/_documents/Omnibus-booklet-update-2013.pdf
- Hartog, J., & Robinson, G. (2013, August). Florida’s Omnibus Act: A brief legal guide for healthcare professionals. Retrieved February 25, 2021, from http://www.floridahealth.gov/diseases-and-conditions/aids/administration/_documents/Omnibus-booklet-update-2013.pdf
- Centers for Disease Control. (2016). Today’s HIV/AIDS epidemic. Retrieved from: https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508.pdf
- Centers for Disease Control. (2020). Evidence of HIV treatment and viral suppression in preventing the sexual transmission of HIV. Retrieved from: https://www.cdc.gov/hiv/pdf/risk/art/cdc-hiv-art-viral-suppression.pdf
- Centers for Disease Control. (2020). HIV. Retrieved from: https://www.cdc.gov/hiv/basics/whatishiv.html
- HIV.gov. (2020). US statistics. Retrieved from: https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics
- Nursing Times. (2020). HIV: epidemiology, pathophysiology, and transmission. Retrieved from: https://www.nursingtimes.net/clinical-archive/immunology/hiv-1-epidemiology-pathophysiology-and-transmission-15-06-2020/
Florida Laws and Regulations
Introduction
The state of Florida has several statutes that govern the practice of nurses. These statues consist of Chapters 456 and 464 located in Title XXXII Regulation of Professions and Occupations. The Florida Administrative Code is where Division 64B9 is located.
Chapter 464, often referred to as the Nurse Practice Act, is separated into two parts. Part I discusses the advanced practiced registered nurse, registered nurse, and licensed practical nurse. The purpose of this statue is to ensure that every nurse practicing in the state of Florida is held to and meets the same minimum standards for safe practice. Because of this, nurses who do not meet the minimum standards or display a harm to society are not allowed to practice nursing in the state of Florida. The Board of Nursing is the governing body for the Nurse Practice Act and deal with matters such as provide licensure, create rules, and manage disciplinary actions. Part II focuses on the certified nursing assistant.
Chapter 456 is a statute that is directed at all health care providers and professions. This statute lists the provisions that Chapter 464 is built on.
Division 64B9 is part of the Florida Administrative Code that provides specific rules that pertain to nurses and how the profession is regulated in terms of eligibility to take the examination of selected practice; set standards for nursing education curriculum and institutions; continuing education requirements; license renewal; rules for impairment of the nurse in the workplace and more.
This course is designed to meet the requirements of Division 64B9-5 as it pertains to two continuing educational hours about Florida’s laws and regulations of the nursing practice.
Definitions
Advanced or specialized nursing practice — completion of post-basic specialized, training, experience, and education that are appropriately performed by an advanced practice registered nurse. The advanced-level nurse can “perform acts of medical diagnosis and treatment, prescription, and operation” under the authorization of a protocol with supervision of a physician (2).
Advanced practice registered nurse (APRN) — any individual that is licensed in this state to practice professional nursing as defined above and holds a license in an advanced nursing practice, including (2):
Certified Nurse Midwives (CNM or nurse midwife)
- Able to perform superficial or minor surgical procedures as defined by a protocol and approved by the employing medical facility or with a backup physician in the case of a home birth/
- Start and perform approved anesthetic procedures.
- Order appropriate medications based on patient and condition.
- Mange care of the normal obstetrics patient and the newborn patient.
Certified Nurse Practitioners (CNP)
- Able to manage certain medical problems guided by facility or supervising provider protocols.
- Manage and monitor patients who have stable, chronic illnesses.
- Start, monitor, and adjust therapies for select, uncomplicated illnesses.
- Order occupational and physical therapy based on patient need.
Certified Registered Nurse Anesthetists (CRNA)
- Able to order preanesthetic medications as stated and approved by facility protocols and staff.
- Determine and consult with supervising anesthesiologist about the proper anesthesia for patients based on labs, history, and physical, and patient condition.
- Assist with managing the patient in the post-anesthesia care unit.
Clinical Nurse Specialists (CNS)
- A nurse who is prepared in a CNS-focused program that meets the requirements of a typical APRN program. Additionally, they are trained in the area of expertise as it pertains to the advanced practice of nurses.
Board — the Board of Nursing (2).
Licensed practical nurse (LPN) — any person licensed in this state or holding an active multistate license under s. 464.0095 to practice practical nursing as defined below (2).
Practice of practical nursing — the performance of select actions including the management of certain treatments and medications, while taking care of the ill, injured, or infirm; prevention of illness, promotion of wellness, and health maintenance in others under the direction of a registered nurse, or a licensed provider: physician, osteopathic physician, podiatric physician, or dentist; and the teaching of general health principles and wellness to the public and to students other than nursing students. A practical nurse is responsible and accountable for making decisions that are based upon their educational preparation and experience in the profession (2).
Practice of professional nursing — the performance of actions requiring substantial specialized knowledge, judgment, and nursing skill based on applied principles of physical, psychological, social, and biological sciences which shall include, but are not limited to (2):
- The nursing process consisting of assessment, nursing diagnosis, planning, intervention, and evaluation, of care; teaching and counseling of the ill, injured, or infirm in matters of health; prevention of illness, promotion of wellness, and maintenance of health of others.
- The administration of medications and treatments as prescribed or authorized by a duly licensed practitioner as they are authorized to do so by the laws of this state to prescribe such medications and treatments.
- The management and education of other individuals in the theory and performance of any of the acts described above such as nursing students.
A professional nurse is responsible and accountable for making decisions that are based upon the individual’s educational preparation and experience (2).
Registered nurse (RN) — means any person licensed in this state or holding an active multistate license under s. 464.0095 to practice professional nursing as defined above (2).
Registered nurse first assistant (RNFA) — means a registered nurse who assists in surgery while in the hospital setting under a physician. They help maintain cost-effective and quality surgery for patients in the state of Florida. They must be certified in perioperative nursing via core curriculum approved by the Association of Operating Room Nurses, Inc. (2).

Self-Quiz
Ask Yourself...
- What license do you currently hold?
- Have you held another license in the past?
- What types of other licensed providers do you work with?
Board of Nursing: Members and Headquarters Location
13 members sit on the Board of Nursing in Florida with their headquarters located in Tallahassee. These members are approved by the Governor of the state and consist of a diverse group of individuals. Seven of these members are RNs who have been practicing for a minimum of four years. One of these seven must be an APRN, a nurse educator from an approved program, and a nurse executive. Three of the total membership should be LPNs with a minimum of four years of practice, just as the RNs. The remaining three members are individuals who have no connection to the nursing profession and are not affiliated or contracted with a health care agency, facility, or insurance company. One member must be 60 years or older. All members of the Board must be residents of the state of Florida. Terms last for a total of 4 years, and at the end of each term the Governor can, but does not have to, appoint a successor to the position (2).
The members of the Board have a few duties. Their primary job is to ensure that nurses practicing in the state of Florida are doing so safely. In order to do this, the Board members can create and implement rules or provisions to the Nurse Practice Act. Approve educational programs for institutions wishing to teach nursing. They can take disciplinary action against a nurse for violation of the Nurse Practice Act or other Florida laws. Citations, fines, or disciplinary guidelines can be issued by the Board as well (2).
Licensure by Examination and Endorsement
Initial licensure requires an individual take an examination for their desired profession: NCLEX-RN, NCLEX-LPN, and either the American Nurses Credentialing Center (ANCC) or American Association of Nurse Practitioners (AANP) version for those wishing to become an APRN. In order for the Board of Nursing to approve an individual to sit for their desired examination, a list of requirements must be met in full (4):
- Must correctly complete an application for the desired examination and submit a fee set by the Board.
- Submit to a background check conducted by the Department of Law Enforcement.
- Must be in good physical and mental health and is a recipient of a high school diploma or equivalent.
- Has completed the following requirements:
- Graduate from an approved program on or after July 1, 2009, OR
- Graduate from a prelicensure nursing education program that has been determined to be equivalent to an approved program by the Board before July 1, 2009
- Must have the ability to communicate effectively in the English language as determined by the Department of Health through another examination.
It is important to note that there is a section dedicated to the scenario of it an individual fails the examination or does not take it within six months of graduating.
Any individual that does not pass their examination of choice after three attempts must take a Board-approved remediation course before they are allowed to sit for the examination again. From there, they are able to take the test three more times before remediation is required again. Reexamination must be done within six months of taking the approved remediation course (2).
If an individual does not take their examination within six months of their graduation, the individual must take an exam preparation course approved by the Board. It is to be advised that the individual must pay for the course without the use of federal or state financial aid (2).
Courses successfully completed in a professional nursing education program that are at least equivalent to a practical nursing education program may be used to satisfy the education requirements for licensure as a licensed practical nurse (2).
If a nurse holds licensure in another state or US territory decides to obtain Florida licensure can do so through endorsement. The state of Florida requires those who apply to submit a nonrefundable fee, completed application, and fingerprints for a criminal background check. The Florida Board of Nursing will not issue a license to an individual that is under investigation at the time of applying (2).
Military Spouses
Applying for a license through endorsement is a route that can be used for nurses who are following military spouses on official military orders. Nurses must have actively practiced nursing two of the three years prior to applying for a license. Military spouses also have the option of obtaining a 12-month temporary Florida license if they meet the requirements: holds a valid nursing license in another state, has a negative criminal background check, has not failed their licensure exam, and has not had any disciplinary action taken against them in another state (1).
Licensure by Compact
Over 30 states in the US have created legislation to allow nurses to work under one multistate license. This means that a nurse who is originally licensed in Florida could work in any other state that participates in the Nurse Licensure Compact without obtaining licensure for each state they wish to work in as long as they have a multistate license. This has proven to be especially useful over the years due to the growing nursing shortage and global pandemic.
Many states like Florida are offering to provide multistate licenses to nurses during their initial examination. If a nurse does not obtain a multistate license initially, they are able to do so later. They must pay a fee and submit fingerprints for a background check. Nurses must also meet any other requirements set by the state of Florida.
It is important to note that in the state of Florida, the nurse who holds the compact license must claim residency in the state. If the nurse were to claim residency in another state, they would no longer have a multistate license.

Self-Quiz
Ask Yourself...
- Do you feel as though Florida’s Board of Nursing has a diverse nursing population?
- Who do you feel should appoint members to the Board?
- What information were you required to provide to the Board of Nursing when you applied to take your exam?
- Have you obtained licensure through endorsement, either it be in Florida or another state?
- Do you think more states should participate in the nursing licensure compact?
Delegation to the Unlicensed Assistive Personnel (UAP) or Unlicensed Personnel (UP)
Delegation is defined by the Nurse Practice Act as the transfer of a task or activity during a specific situation by a qualified nurse, through licensure and experience in the task, to a competent individual. Different facilities may have many ways of determining the competence of the individuals, but ultimately the decision rests with the RN or LPN. The licensed provider must determine the difficulty of the task, the potential for predictable or unpredictable harm or rapid change in patient condition, and level of communication required with the patient. They must also consider resources available and skills the UAP at their facility can do (4).
When delegating, it is important to assess the UAP’s skill set through validation or verification. The nurse should provide clear communication when it comes to the task delegated and explain the desired outcomes. They should also explain what undesired outcomes could occur, what should be done if an undesired outcome does happen when the task should be completed, and if supervision is required. The nurse should follow up to ensure that the task was done correctly and within the set time frame. The nurse should be aware that the delegated task and any outcomes of the task are the nurse’s responsibility, and they are ultimately held accountable for it. So, if it is an important task, it may be better to do it yourself (4).
There are a few skills that cannot be delegated to the UAP:
- A skill that is not within the delegating nurse’s scope of practice
- Activities that require the use of the nursing process or require specific education, nursing judgement, training, or skills.
- Initial assessments and progress evaluation as it relates to the patient’s plan of care.
- Skills that an UAP has not displayed competence.
IV Administration by LPNs
As mentioned above, LPNs and RNs have a few differences in their scopes of practice. LPNs are able to administer and perform some parts of IV medication therapy as opposed to the RN. The definition of IV therapy administration is defined as the infusion or injection of a medication via the intravenous system. This method involves several aspects including: evaluating, observing, monitoring, discontinuing, titrating, management, planning, documenting, and intervening as needed during the administration. RNs do not always have to be onsite when delegating IV administration to an LPN but is important to know policies and when an RN must be present (4).
LPNs cannot do any of the following (4):
- Initiate blood or blood products or plasma extenders.
- Mix IV solutions.
- Administer or initiate cancer treatments such as chemotherapy or investigational medications.
- IV pushes with the exceptions of heparin or saline flushes.
Note that LPNs may care for patients receiving these types of therapies, such as a patient who is actively receiving a blood transfusion, but they cannot do the above aspects.
LPNs are able to (4):
- Calculate and adjust flow rates.
- Observe and report any signs of adverse effects of IV medications.
- Assess IV insertion sites and change dressings as educated and needed.
- Remove IV catheters or needles from peripheral veins.
- Hang IV hydrating fluids.
In order for an LPN to administer IV medications through a central line they must do so under the direction of a RN and have four hours of IV therapy education on central lines. This four-hour requirement can be applied to the 30 total hours LPNs must do on IV therapy (4).
LPN Supervision in Nursing Homes
According to Florida law LPNs can supervise other LPNs, certified nursing assistant (CNAs) or UAPs in the nursing home setting. In order to be considered for a supervisory position, the LPN must have completed 30 hours of Board approved, post-basic education courses under the supervision of a RN. The LPN must also have at least six months of full-time clinical experience either in a hospital or nursing home setting. If the LPN takes a course outside of the Board’s approval courses, the provider of said course must test the LPN and provide attestation of the LPN’s competency (4).
The supervisory LPN’s role is to provide other LPNs, CNAs, and UPAs with guidance and inspection of their completed task as their pertain to their appropriate scope of practice. The LPN can only delegate tasks within their scope of practice and be assured that the one they are delegating to demonstrates competency (4).
Certified Nursing Assistant (CNA)
The certified nursing assistant is similar to the UAP but in order to be certified they must have competed a background check conducted by the Board of Nursing, prove they are able to read and write, and pass the nursing assistant examination. Once the criteria listed has been met, CNAs can provide general care and assist with activities of daily living under the direction of a RN or LPN. They can also participate in postmortem care and perform CPR.

Self-Quiz
Ask Yourself...
- Think of your facility.
- What types of UAPs do you have? CNAs, Patient Care Technicians (PCTs)?
- Are you aware of what you can and can’t delegate to them?
- Are there any LPNs where you work?
- What are they able to do, and what types of patients are the able to take care of?
Maintaining Medical Records
For RNs and APRNs in private practice the Florida Nurse Practice Act has two rules in place when it comes to maintaining medical records. The first applies to the death of the nurse. Whoever legally represents the RN or APRN must post a notification in the county newspaper stating where the medical records are being stored and who to contact if an individual would like to obtain the records. The records must be stored for at a minimum of two years after the death of the nurse (4).
At the 24-month mark, there must be several notices posted in the county newspaper, one notification for four consecutive weeks, that the medical records will be destroyed four weeks after the last day of the fourth week that the notice was published (4).
The second rule pertains to an RN or APRN that has terminated or relocated their practice. The rule states that the RN or APRN maintain and hold on to the medical records for a minimum of two years. They must let those that were patients know about the date of termination or relocation and where the medical records can be retrieved. The notice must be made public, such as in a newspaper, with a minimum appearance of four times over four weeks. A sign must be placed at the location of the business about the termination or relocation until the termination or relocation happens. This sign must tell patients about the opportunity to obtain their medical records (4).
Continuing Education (CE) Requirements
Florida law requires that for renewal of a nursing license, the nurse seeking renewal must complete a set amount of CE hours. Over the two-year period, 24 hours must be completed, one for each month. Two of those hours must be on the Florida Nurse Practice Act and the other laws that pertain to the nursing profession. Two hours are required on medication errors and how to prevent them. A one-hour HIV/AIDS is required for initial renewal but does not have to be repeated. There must be a two-hour course on domestic violence done every third renewal. As of August 2017, a two-hour course on recognizing impairment in the workplace is required with each renewal (4).
In the state of Florida, completed CE courses are either automatically reported to a tracking system created by the Department of Health’s Division of Medical Quality and Assurance (MQA) or by the individual manually. Those who attend CE courses will obtain a certificate of attendance. It is advised that the attendee maintain a copy of those certificates for four years or more. For Florida, the provider of the course has 90 days to report to the tracking system, so if the date to renew is less than 90 days, it is suggested that the course be manually reported (4).
If a nurse has two licenses, such as RN and LPN or APRN and RN, they may be able to comply with both license requirements through one set of CE requirements. For example, an RN who holds an LPN license can meet all the LPN license CE requirements by completing the RN requirements (4).
Nurses who serve as expert witnesses and provide expert opinions in a written format can obtain 2.5 hours for each case. The case must cite at least two current articles of reference and are being reviewed in regard to the Nurse Practice Act (4).
There are a few exemptions to the CE renewal requirements (1):
- If the nurse is on active duty for the US military within six months of the renewal date.
- This does not apply to short periods of active duty such as summer or weekend drills.
- This does not apply to those on duty in the US Public Health Service.
- If the nurse’s spouse is a member of the US military and the nurse was absent from the state of Florida because of military duty.
- The nurse must provide adequate proof of the absence and the military status of their spouse.

Self-Quiz
Ask Yourself...
- What types of classes do you take to complete your continuing education? Online, in-person, webinar?
- What Florida mandated classes do you have the hardest time obtaining?
- Do you hold licenses in two aspects of nursing, such as LPN and RN, or RN and APRN?
- If so, how do you complete your continuing education requirements for both?
Disciplinary Action
The Florida Board of Nursing, as outlined in the Nurse Practice Act, holds power to discipline nurses as they see fit regarding the violations of Florida rules and laws. The Board created a variety of ways a nurse can be disciplined, ranging from probable-cause panels to citations to disciplinary hearings. The severity of the violation reflects on which method the Board of Nursing may take (2).
There are three probable-cause panels in Florida: North Florida, Central Florida, and South Florida. The purpose of these panels is to determine if there was “probable cause” or reasonable ground for the reported case. They decide if a case needs action taken. The members of the panel review each case and compare it to others of similar nature, how the Board treated the cases in the past, and what the Board’s guidelines entail. The panel can recommend and consider rules regarding procedures, penalties, and disciplinary actions.
Citations can be given in lieu of other forms of discipline. The citation is issued within six months of a complaint being filed and contains the request for the recipient to fix the violation within a specified time frame. These violations are usually classified as “minor” in nature, such as false advertising, falsely using a nursing title, or failure to report the change of address or updates of information required by the Board. Other reasons a citation can be issued are a failure to report a misdemeanor within 30 days of a ruling or failing to utilize the law-required prescription drug monitoring system. Each of these citations can come with a fine, usually ranging from $100 to $250 in amount; however, if a nurse is found guilty of sharing passwords, codes, keys, or other forms of entry to a secure medication administration or information technology system a fine of $1,500 can be given. In addition, the nurse would have to take a two-hour CE course on legal nursing aspects within 60 days of the citation being issued.
The Board of Nursing has the power to take appropriate action against nurses that confirmed violation of the Nurse Practice Act (2):
- Probation, suspension, or revocation of a license
- Can be emergently done depending on the situation.
- Require CE course(s) to be done.
- Letter of concern
- Reprimand
- Give a fine
- Require a personal appearance in front of the Board of Nursing to monitor compliance.
- Restricting or limiting practice
- Referral to the Intervention Project for Nurses (IPN)
Any of these actions can be combined, depending on the severity of the violation. They can also accompany a fine determined by the Board (2).
The Board of Nursing has also created an extensive list of reasons why a nurse can be disciplined (2):
- Sexual misconduct
- Unprofessional conduct
- Participating in crime related to healthcare fraud.
- Making or filing a false report to appease state or federal law.
- Willfully hindering another individual in filing a report that is required by state or federal law.
- Testing positive on any drug screen when the individual has no medical/other reason for using the drug.
- Inability to practice nursing with satisfactory skill and provide safe patient care due to use of narcotics, drugs, alcohol, chemicals, or other substances that may impair an individual.
- Inability to practice nursing with satisfactory skill and provide safe patient care due to an illness, physical or mental condition.
- Failing to meet minimal standards of acceptable nursing practice.
- Accepting and performing professional responsibilities the nurse knows or has reason to know they are not skilled to perform.
- Delegating or contracting for the performance of professional responsibilities by a person who the nurse knows or has reason to know is not qualified by training, experience, and authorization required to perform.
- Failing to identify the type of license the nurse is practicing under through written (can include a nametag) or oral notice to a patient.
- Performing or attempting to perform healthcare services on the wrong-site or wrong procedure on the wrong patient. This includes unauthorized procedures.
- Performing or attempting to perform healthcare services that are medically unnecessary or otherwise not related to the patient’s diagnosis or medical condition(s).
- Being convicted or found guilty of or pleading nolo contendere to a crime in any jurisdiction that directly relates to the practice of nursing or ability to practice nursing.
- Being convicted of or found guilty of, or pleading nolo contendere to misdemeanors, related to failure to protect an adult from abuse, neglect, and exploitation; fraudulent practices; theft and robbery; or having committed an act of domestic violence or child abuse.
- Defaulting on a student loan that has been issued or guaranteed by the state or federal government.
As with everything in life, the Board of Nursing has created guidelines for imposing discipline. They have a set minimum and maximum amount when it comes to fines. They have time frames for probation or supervision, conditions regarding probation or the reinstatement of a license. What route they decide to take depends upon the specific case being presented to them. Sometimes the circumstances presented to the Board are enough to elicit decisions that are outside the general guidelines. Some of these circumstances are (2):
- Length of time a nurse has practiced.
- Presents a danger to the public.
- Any visible effort at rehabilitation.
- Treatment and disciplinary hearing costs.
- Actual physical or other forms of damage caused by the nurse.
- Financial hardships.
The Board has a timeframe in which a complaint must be filled. Most of the time, it is within a six-year window from the time the incident occurred. However, in certain circumstances—criminal actions, sexual misconduct, impairment of the nurse, or usage/diversion of controlled medications—the Board may go beyond the six-year timeframe. If action such as fraud, intentional misrepresentation, or concealment is utilized to hide the violation during the six-year period, the timeframe to file a complaint can be extended to 12 years from when the incident initially occurred (2).
If the Board of Nursing suspends a nurse’s license, or if the nurse agrees to have the licenses suspended to avoid further action against them, the nurse can file a petition to possibly have their license reinstated. Any final orders or terms issued during the initial suspension must be met in whole, and the nurse must be able to demonstrate the ability to perform nursing practice safely. Sometimes a time frame is placed for when a nurse can file a petition; sometimes, there is not. If this is the case, then a nurse can appeal as soon as they are able to do so after meeting the terms and conditions given to them by the Board (2).
The Board will determine what a nurse must do to demonstrate safe practice. This is based on the violation. For example, a nurse who is working while under the influence of medications or alcohol may be ordered to attend a treatment program with proof of sobriety, references, and completion of any court-mandated sanctions. Nurses are often required to present to the Board of Nursing in person and speak on their ability to safely practice nursing (2).
The three-strike policy is utilized when it comes to reinstating a license. If a nurse has been found guilty on three separate occasions of a complaint pertaining to drug/narcotic usage or the diversion of medications from patients to the nurse for personal use or to sell, the Board will not reinstate the license (2).
Relicensing a nurse who has had their license revoked is similar to what happens when a license is suspended. However, the nurse must reapply for the license and meet all conditions set by the Board. Nurses may have to sit for another examination or take Board approved continuing education if the nurse has been out of practice for an extended period of time. They may require a nurse to participate in Florida’s Intervention Project for Nurses (IPN) program or at least be evaluated for it (2).
Nurses are held accountable for reporting the actions of other nurses and any misconduct to the Board of Nursing. They must report sexual misconduct or healthcare fraud. If they know or have reason to believe that another nurse is not practicing safely or is practicing under the influence of alcohol or medications, they are required to report it.

Self-Quiz
Ask Yourself...
- Do you know anyone who has had action taken against them regarding the Nurse Practice Act?
- If so, do you know the outcome?
- What are some other violations that you think might violate the Nurse Practice Act?
- What do you think is the most severe violation?
- Do you think that the Board of Nursing’s list of potential actions that could be taken against a nurse’s license is fair?
- If you were on the Board, what types of disciplinary action would you recommend?
Florida’s Intervention Project for Nurses (IPN)
Created in 1983 under the authority of the Nurse Practice Act, IPN was designed to protect the public through monitoring nurses whose skills have been compromised due to improper use of medications or alcohol or the impairment of mental of physical health. IPN is not a treatment center. Instead, they provide nurses with access to Board-approved practitioners who specialize in addiction, mental health, and other medical conditions. They also conduct monitoring after a nurse has been discharged from treatment, interventional training, consultations, and advocacy for those who participate (3).
As mentioned above, nurses have an obligation to report themselves or nurses who are or they have reason to believe are unsafely practicing nursing while under the influence of alcohol or medications. If a nurse self-reports or is reported to the IPN only and they successfully complete treatment and five-year monitoring, the report is confidential. If the Board of Nursing becomes involved, either through a failure to report or failure to complete treatment, disciplinary action may be taken (3).
Initially, nurses are not able to practice during the initial evaluation and when the determination of treatment is being made. After that, it is up to the discretion of the IPN, and the providers involved in the treatment. Restrictions on a nurse’s practice are often implemented during the beginning phase of treatment (3).
In order to be determined “fit to practice,” the nurse must meet all requirements set by their providers and the IPN. They must sign an advocacy contract, submit to random drug tests, verbalize understanding any practice restrictions, and be involved in a weekly support group for nurses (3).

Self-Quiz
Ask Yourself...
- Do you think the IPN should be a treatment center as opposed to a resource center?
- Should the status of a nurse who has enrolled in this program, willingly or not, be confidential, even if they do not meet the requirements?
- Do you think a nurse should be allowed to practice nursing with set limitations while involved with IPN?
Summary
Despite the extensive outline of the Nurse Practice Act and other state rules provided in this course, it does not provide a complete narration of all Florida laws pertaining to nurses. In addition to this course, it is imperative for nurses to stay on top of new legislation being proposed and put into effect regarding their profession and continually review the content in the state laws. Nurses who travel to other states to practice their profession should be educated on each state’s rules regarding nursing practice as it can differ from state to state. A conscious effort should be made to follow the laws set in place to practice safely and legally in the state of Florida.
References
- The Florida Senate. “Chapter 456.” Chapter 456 – 2018 Florida Statutes – The Florida Senate, www.flsenate.gov/Laws/Statutes/2018/Chapter456.
- The Florida Senate. “Chapter 464.” Chapter 464 – 2018 Florida Statutes – The Florida Senate, www.flsenate.gov/Laws/Statutes/2018/Chapter464/All.
- Intervention Project for Nurses, 2016, www.ipnfl.org/.
- State of Florida. Department List – Florida Administrative Rules, Law, Code, Register – FAC, FAR, ERulemaking, https://www.flrules.org/gateway/Browse.asp
Florida Medical Errors Prevention
Introduction
For as long as there have been medical professionals, there have been medical errors. Medical errors can be small and seemingly insignificant to a catastrophic sentinel event.
The Joint Commission (TJC) is a healthcare accrediting agency that sets the standard for patient safety. Each year, TJC publishes a list of national patient safety goals. These goals are focused on the prevention of medical errors. In 2019, the World Health Organization (WHO) found that medical errors harmed up to 40% of patients within the global healthcare system. These medical errors not only cause harm to millions of people worldwide, but they also cost billions of dollars on an annual basis (9).
There are many different types of medical errors. They include, but are not limited to medication errors, healthcare-acquired infections, surgical errors, lab errors, falls, documentation issues, and omitted care. Healthcare workers must know the possible harm caused by medical errors and how they can be prevented.
Factors That Impact the Occurrence of Medical Errors
There are multiple factors that can increase the probability of a medical error occurring. Healthcare worker behaviors and attitudes, staffing, and communication are among those that have the most significant impact on medical errors.
In healthcare, a risky behavior is an action that may lead to a compromise in patient safety. Why would any healthcare worker engage in at-risk behaviors? Healthcare workers, especially nurses, are generally compassionate and are prioritize the patients’ welfare in their care. Risky behaviors produce a quick, positive reward without any perceived risk of patient harm. These risky behaviors can range from a simple short-cut like not checking two patient identifiers to a blatant disregard for hospital/facility policy. In all instances, the risk for patient harm is real and will eventually occur (7).
Understaffing in the hospital setting continues to be a factor contributing to medical errors. Poor nurse-to-patient ratios can lead to a variety of medical errors. Ordered patient care may go undone, leading to further medical errors adverse patient outcomes (8). Understaffing leads to fatigue and burnout. A nurse in this state of mind is prone to committing medical errors.
Miscommunication between healthcare professionals and patients and miscommunication between healthcare professionals also contribute to the occurrence of medical errors. As part of their national patient safety goals, TJC has had a communication component almost every year. They have recognized that effective communication is paramount in the prevention of medical errors. A lack of effective communication can be a leading cause of every type of medical error.
In an effort to decrease communication errors, TJC has taken measures to ensure that effective communication is promoted in a variety of different situations. TJC has instituted a list of unacceptable medical abbreviations. This list will decrease medication errors by removing confusion when medications are ordered (12). They also developed a handoff communication protocol for facilities to implement. The handoff communication occurs anytime that care is passed from one caregiver to another. It is used to ensure that all pertinent patient information is passed on to the next healthcare worker rendering care to the patient. By using effective handoff communication, all information should be passed on, and mistakes should be avoided (11).

Self-Quiz
Ask Yourself...
- Have you ever participated in at-risk behavior at my facility?
- Did that at-risk behavior contribute to the occurrence of a medical error?
- Is your unit staffed appropriately?
- Do healthcare professionals in your facility use an appropriate handoff communication tool?
- What is an example of a handoff communication tool?
Recognizing Error-Prone Situations
Studies have shown that most medical errors occur in the inpatient setting. The most common areas for medical errors are the operating room (OR), the emergency room (ER), the intensive care unit (ICU), and the medical/surgical floors (1).
What is it about the inpatient setting that makes it such an error-prone area? More specifically, why do medical errors occur in the ICU, OR, and ER? These are all high-stress areas where effective communication between all parties is vital. Breakdown in communication in these areas will lead to catastrophic medical errors. When the stress level rises, the probability of medical errors occurring also rises. These are also fast-paced areas where the condition can change in the blink of an eye. When we work in such a busy area, we can forget important details. Miscommunication in these environments is a recipe for medical errors.
As the most common type of medical errors is medication errors, we do need to talk about medication administration. Nurses are taught the five rights of medication administration in nursing school:
- Right drug.
- Right patient.
- Right dose.
- Right route.
- Right time.
When working in a busy inpatient setting, nurses may fail to perform the five rights in order to save time (5). Neglecting any one of the five rights of medication administration can cause a medical error.

Self-Quiz
Ask Yourself...
- Do you work in an error-prone environment?
- Which factors can make an environment error-prone?
- What can you do to decrease stress levels on the job?
Processes to Improve Patient Outcomes
In the technological age in which we live, it is more important than ever before that healthcare facilities consistently demonstrate good patient outcomes. The Centers for Medicare & Medicaid Services (CMS) places great importance on the patient experience and their perception of their healthcare experience quality. Every patient who experiences a hospital stay may be asked to complete a Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. The survey results are published quarterly on the CMS Hospital Compare website. There, patients can compare the hospital’s results and choose a hospital where they would like to have their care rendered (4). A medical error could very well cause a patient to give a facility a poor rating on the HCAHPS survey.
When medical errors have occurred, they will often result in a risk management response to investigate why the error has happened and how it can be prevented in the future – a root cause analysis (RCA). An RCA will often lead to department-driven performance improvement projects (PIP) to eradicate the problem and improve patient outcomes. A proactive facility trying to minimize medical errors will have multiple department and facility-wide PIP.
As previously stated, each year TJC publishes a list of patient safety goals. These goals will often guide a facility on specific patient outcomes that have required attention for improvement on a national level. They focus on the prevention of medical errors, and as such, they can steer PIP. Accreditation hinges on the ability of a facility to improve and consistently deliver positive patient outcomes. Below is the current list of TJC’s patient Safety Goals:
1. Identify patients correctly.
– Use at least two ways to identify patients. For example, use the patient’s name and date of birth. This is done to make sure that each patient gets the correct medicine and treatment.
2. Improve staff communication.
– Get important test results to the right staff person on time.
3. Use medicines safely.
– Before a procedure, label medicines that are not labeled. For example, medicines in syringes, cups, and basins. Do this in the area where medicines and supplies are set up.
– Take extra care with patients who take medicines to thin their blood.
– Record and pass along correct information about a patient’s medicines. Find out what medicines the patient is taking. Compare those medicines to new medicines given to the patient. Give the patient written information about the medicines they need to take. Tell the patient it is important to bring their up-to-date list of medicines every time they visit a doctor.
4. Use alarms safely.
– Make improvements to ensure that alarms on medical equipment are heard and responded to on time.
5. Prevent infection.
– Use the hand cleaning guidelines from the Centers for Disease Control and Prevention or the World Health Organization. Set goals for improving hand cleaning. Use the goals to improve hand cleaning.
6. Identify patient safety risks.
– Reduce the risk for suicide.
7. Prevent mistakes in surgery.
– Make sure that the correct surgery is done on the correct patient and at the correct place on the patient’s body.
– Mark the correct place on the patient’s body where the surgery is to be done.
– Pause before the surgery to make sure that a mistake is not being made.

Self-Quiz
Ask Yourself...
- How do you report a medical error in your facility?
- Who is the Risk Manager in your facility?
- Do you work in a culture of safety?
Safety Needs of Special Populations
There are certain groups of people that are especially vulnerable to experience a medical error.
Elderly
The elderly are especially susceptible to medical errors. Generally, as we get older, we tend to start taking more medications. Complex medication regimens offer a greater opportunity for medication errors. Many medications require close monitoring of vital signs and/or blood levels. Drug-related issues are a major driving force for both ER visits and nursing home admissions among the elderly (3). Declining cognition, poor vision, and increased forgetfulness associated with aging can also play a part in medication errors. Education with frequent reinforcement and the use of support people are crucial to help prevent medication errors.
The elderly are also at a higher risk for falls. Falls within a medical facility can lead to further medical complications, increased length of stay, and serious injury. Patients at risk for falls need to be identified and place on a fall prevention protocol.
Children
Children are on the other side of the spectrum and are also another group that are at higher risk for medical errors. Younger children may be unable to accurately voice exactly their problem is, or what symptoms they are experiencing. They must rely on both parents and other caregivers for the coordination of their care. Though a parent may know their child well, they may not be able to properly convey their child’s issues to the healthcare professional. It is also important to realize that children are not little adults. Care plans must be catered to their specific phase of life.
Limited Health Literacy
Another population that is vulnerable to medical errors are patients with limited health care literacy. These patients may have difficulty obtaining, retaining, and implementing health information to make proper decisions for their healthcare needs. Populations within this group may include the elderly, low-income populations, immigrants, and minorities. here is also a strong correlation between limited health literacy and the uninsured, undereducated, and unemployed populations. It is important that information be presented to this group at a level that they can understand. The use of interpreters can also be helpful if the patient does not have a good grasp of the English language (6).

Self-Quiz
Ask Yourself...
- What is the level of health literacy in the community where you live?
- What population to you work with daily?
- Do you present information to your patients in a way that they can understand?
Public Education
Now, more than ever before, the general public has greater access to information of all sorts. This includes access to health information, specifically, patient outcomes. The public can make informed decisions on where they would like to be cared for by comparing healthcare facilities.
The public is seeking information not only on which facility is the safest with the best outcomes but also on ways that they can actively prevent medical errors from happening to them. There are many resources that patients can find online to help them recognize scenarios that may place them at risk for the occurrence of medical errors. The Agency for Healthcare Research and Quality (AHRQ) has published a list of 20 tips patients can use to help prevent medical errors:
Medicines
1. Make sure that all your doctors know about every medicine you are taking. This includes prescription and over-the-counter medicines and dietary supplements, such as vitamins and herbs.
2. Bring all your medicines and supplements to your doctor visits. “Brown bagging” your medicines can help you and your doctor talk about them and find out if there are any problems. It can also help your doctor keep your records up to date and help you get better quality care.
3. Make sure your doctor knows about any allergies and adverse reactions you have had to medicines. This can help you to avoid getting a medicine that could harm you.
4. When your doctor writes a prescription for you, make sure you can read it. If you cannot read your doctor’s handwriting, your pharmacist might not be able to either.
5. Ask for information about your medicines in terms you can understand—both when your medicines are prescribed and when you get them:
– What is the medicine for?
– How am I supposed to take it, and for how long?
– What side effects are likely? What do I do if they occur?
– Is this medicine safe to take with other medicines or dietary supplements I am taking?
– What food, drink, or activities should I avoid while taking this medicine?
6. When you pick up your medicine from the pharmacy, ask: Is this the medicine that my doctor prescribed?
7. If you have any questions about the directions on your medicine labels, ask. Medicine labels can be hard to understand. For example, ask if “four times daily” means taking a dose every 6 hours around the clock or just during regular waking hours.
8. Ask your pharmacist for the best device to measure your liquid medicine. For example, many people use household teaspoons, which often do not hold a true teaspoon of liquid. Special devices, like marked syringes, help people measure the right dose.
9. Ask for written information about the side effects your medicine could cause. If you know what might happen, you will be better prepared if it does or if something unexpected happens.
Hospital Stays
10. If you are in a hospital, consider asking all health care workers who will touch you whether they have washed their hands. Handwashing can prevent the spread of infections in hospitals.
11. When you are being discharged from the hospital, ask your doctor to explain the treatment plan you will follow at home. This includes learning about your new medicines, making sure you know when to schedule follow-up appointments, and finding out when you can get back to your regular activities. It is important to know whether you should keep taking the medicines you were taking before your hospital stay. Getting clear instructions may help prevent an unexpected return trip to the hospital.
Surgery
11. If you are having surgery, make sure that you, your doctor, and your surgeon all agree on exactly what will be done. Having surgery at the wrong site (for example, operating on the left knee instead of the right) is rare. But even once is too often. The good news is that wrong-site surgery is 100 percent preventable. Surgeons are expected to sign their initials directly on the site to be operated on before the surgery.
12. If you have a choice, choose a hospital where many patients have had the procedure or surgery you need. Research shows that patients tend to have better results when they are treated in hospitals that have a great deal of experience with their condition.
Other Steps
13. Speak up if you have questions or concerns. You have a right to question anyone who is involved with your care.
14. Make sure that someone, such as your primary care doctor, coordinates your care. This is especially important if you have any health problems or are in the hospital.
15. Make sure that all your doctors have your important health information. Do not assume that everyone has all the information they need.
16. Ask a family member or friend to go to appointments with you. Even if you do not need help now, you might need it later.
17. Know that “more” is not always better. It is a good idea to find out why a test or treatment is needed and how it can help you. You could be better off without it.
18. If you have a test, do not assume that no news is good news. Ask how and when you will get the results.
19. Learn about your condition and treatments by asking your doctor and nurse and by using other reliable sources. For example, treatment options based on the latest scientific evidence are available from the Effective Health Care Web site.
20. Ask your doctor if your treatment is based on the latest evidence (2).

Self-Quiz
Ask Yourself...
- What is the level of health literacy in the community where you live?
- What population to you work with daily?
- Do you present information to your patients in a way that they can understand?
Case Studies
1. Mr. Smith
Mr. Smith is a 68-year-old male with diabetes type 2, hypertension, and chronic renal failure stage 4. He takes both long-acting and short-acting insulin for his diabetes and a beta-blocker for his high blood pressure. He is also taking a diuretic to help regulate his fluids. Mr. Smith was recently admitted to the hospital for a hypoglycemic event. Once in the hospital, Mr. Smith expressed to his nurse that he has been having difficulty reading his medication labels. He also confided that he feels dizzy when he stands up and has fallen back onto his bed on more than 1 occasion.
After two days, Mr. Smith was ready to be discharged. The diabetic educator brought him some pamphlets and educated him on proper blood glucose monitoring and insulin administration. His blood pressure medicines were also changed, and Mr. Smith was given a new prescription to be filled once he left the hospital. He was alone when discharge instructions were given, and his current medications were not removed from his medicine bag.
Two days later, Mr. Smith was readmitted to the hospital with hypoglycemia and hypotension (BP 87/52).
What are some factors that lead to the occurrence of medical errors with Mr. Smith?
What are the medical errors that occurred?
What could the nurse/educator have done differently to prevent further medical errors?
2. Bernice
Bernice is a staff nurse working in a busy ICU. Due to the COVID-19 pandemic, the unit has been short-staffed, with each nurse taking care of 3-4 patients. This is Bernice’s fifth day in a row, working fourteen plus hours. There have been multiple “code blue” situations in the ICU over the course of Bernice’s workweek, some involving her patients. She was only able to have a full lunch hour on her second day, and she has not been able to sleep much during the night.
One of her patients was having severe abdominal pain, 9/10 on the pain scale. Bernice went in to administer the ordered narcotic and injected the wrong patient.
What factors lead to Bernice’s medical error?
What could have been done to prevent the error?
Is this a situation that could happen in a unit where you work?
Conclusion
Medical errors are an ongoing problem in the healthcare setting. They affect patients in all phases of life and come with a large price tag of both money and medical resources. It is everyone’s responsibility to help prevent the occurrence of medical errors. Though we may not be able to totally eradicate them, we can all play a big part in their prevention by learning from previous mistakes and taking measures to ensure that they do not happen again.
References
- Ahmed, Z., Saada, M., Jones, A. M., & Al-Hamid, A. M. (2019, 05 22). Medical errors: Healthcare professional’s perspective at a tertiary hospital in Kuwait. PLoS ONE, 14(5), 1-14. doi: 10.1371/journal.pone.0217023
- AHRQ. (2020, 11 01). 20 Tips to Help Prevent Medical Errors: Patient Fact Sheet. Retrieved from AHRQ Agency for Healthcare Research and Quality: https://www.ahrq.gov/questions/resources/20-tips.html
- CDC. (2017, 10 11). Medication Safety Program. Retrieved from cdc.gov: cdc.gov/medicationsafety/adult_adversedrugevents.html
- CMS. (2020, 11 19). Hospital CAHPS (HCAHPS). Retrieved from CMS.gov: https:www.cms.gov/Research-Statistics-Data-and-Systems/Research/CAHPS/HCAHPS1
- Federico, F. (2021). Improvement Stories. Retrieved from ihi.org: https://www.ihi.org/resources/Pages/ImprovementStories/FiveRightsofMedicationAdministration.aspx
- MRMC. (2018). Community Health Needs Assessment 2018. Mission, TX. Retrieved from https://missionrmc.org/documents/Mission-Regional-Medical-Center-2018-CHNA.Final-Draft.pdf
- Reducing Medication Errors Associated with At-risk Behaviors by Healthcare Professionals. (2014, 8 30). Retrieved from NCCMERP: https://www.nccmerp.org/reducing-medication-errors-associated-risk-behaviors-healthcare-professionals
- Senek, M., Robertson, S., Ryan, T., King, r., Wood, E., & Tod, A. (2020, 7 10). The association between care left undone and temporary Nursing staff ratios in acute settings: a cross-sectional survey of registered nurses. BMC Health services Research, 20(1), 1-8. doi:10.1186/s12913-020-05493-y
- Sutcliffe, K. (2019, 11 25). How to Reduce Medical Errors. TIME Magazine, 194(22/23), 25-26.
- The 2020 Florida Statutes. (2020). Retrieved from www.leg.stste.fl.us/Statutes/index.cfm?App_mode=Display_Statute&Search_String=&URL=0300-399/0395/Sections/0395.0197.html
- TJC. (2017, 09 12). Inadequate handoff communication. Sentinel Event Alert (58), 1-5.
- TJC. (2020, 08 01). Official “Do Not Use” List. Retrieved from jointcommission.org: https://www.jointcommission.org/-/media/tjc/documents/fact-sheets/do-not-use-list-8-3-20.pdf?db=web&hash=2489CB1616A30CFFBDAAD1FB3F8021A5
- TJC. (2021). 2021 Hospital National Patient Safety Goals. Retrieved from www.jointcommission.org: https://www.jointcommission.org/-/media/tjc/documents/standards/national-patient-safety-goals/2021/simplified-2021-hap-npsg-goals-final-11420.pdf
- Trossman, S. (2016, May/June). ANA calls for a culture of safety in all health care settings. American Nurse, 48(3), 3.
Recognizing Impairment in the Workplace – Florida
Introduction
Substance use disorder, addiction, drug diversion, and other related impairment processes present a threat to the health and safety of those around them (4). Increasing in concern are overdoses and deaths that are on the rise due to substance abuse and addiction. Early identification of the signs and symptoms of a substance abuse disorder in the workplace contributes to reducing the risk and harm to patients and other healthcare team members. Co-workers play a crucial role in recognizing and reporting suspicious behaviors to their supervisors or appropriate personnel.
Impairment within the workplace of a healthcare environment is, unfortunately, more common than one may realize. Impairment results when a healthcare professional cannot provide competent and safe patient care because they may be impaired by alcohol, prescription, or non-prescription drugs, or other mind-altering substances (2). Impairment can also result from a psychological or neurological condition that may affect a person’s judgment. Because of impairment, the healthcare professional is unable to perform duties essential to their profession safely.
Acknowledging the Problem
Ideally, from a professional standpoint, healthcare personnel should acknowledge their condition and seek help voluntarily without requiring intervention; however, this is often not the case. Co-workers play a key role in helping the impaired person get treatment. Often, the abuser has denial with the condition, the social stigma, or fear of potential job loss. Colleagues are often reluctant to report their co-workers because they feel it is not their responsibility. They feel like the individual they are reporting may be punished excessively. They may believe that someone else has already addressed the issue or fear the loss of their colleague’s job or license. Despite these potential reasons, colleagues may have certain legal responsibilities in identifying and reporting. States may have specific reporting laws that could hold colleagues responsible for harm to patients if they fail to report.
Definitions
Substance Use Disorder – a disease of the brain characterized by the recurrent use of substances such as alcohol and drugs that cause clinical and functional impairment such as health problems, disability, and failure to meet responsibilities at work or school. The disease involves reward, withdrawal, memory, and motivation and can be classified as mild, moderate, or severe depending on the level of impairment (1).
Addiction – the most severe, chronic stage of substance use disorder. There is a substantial loss of self-control, indicated by compulsive substance use despite the desire to stop using (1).
Drug diversion – is the transfer of any substance from the purpose for which it was intended for any illicit use, such as personal use or sale (1).
Impairment – is the inability or impending inability to engage safely in professional and daily life activities as a result of physical, mental, or behavior disorders such as substance use, abuse, or addiction (1).

Self-Quiz
Ask Yourself...
- Have you experienced a co-worker with impairment in the workplace?
- Do you know of someone you currently work with or have worked with in the past that has had an issue with drug diversion or addiction related to their profession? Was there legal action taken?
- What is the difference between addiction and drug diversion?
- What are different ways that drug diversion can be used for?
- Can you as a healthcare worker be held responsible for failure to report impairment of a co-worker in the workplace?
Impairment Behaviors in the Workplace
Some behaviors are associated with emotional problems but are specific to alcohol or other drug abuse. Some signs common to alcohol and other drugs may also be signs of psychological or psychiatric conditions (2). Each situation is individualistic to the person. Health care professionals must be educated appropriately regarding the signs and symptoms of chemical dependence. The workplace is often the last place that addiction may manifest; disruptions in family, personal health, and social life can happen while the workplace remains unaffected.
Behaviors associated with Substance Abuse:
- Severe mood swings/personality changes
- Frequent or unexplained tardiness, work absence, illness, or physical complaint
- Elaborate excuses
- Underperformance
- Difficulty with authority
- Poorly explained errors, accident, or injury
- Confusion, memory loss, difficulty concentrating
- Visibly intoxicated
- Refuses drug testing
Signs Associated with Substance Abuse:
- Unreliability in keeping appointments and meetings
- Trouble with relationships (professional familial, marital)
- Physical indications such as track marks or bloodshot eyes
- Signs indicative of drug diversion
- Deterioration in personal appearance
- Significant weight loss or gain
- Discovered comatose or dead
Signs and Behaviors Associated to Drug Diversion Specific to Anesthesia Personnel (1):
- Consistently uses more drugs for cases than colleagues.
- Frequent volunteering to administer narcotics, relieve colleagues for casework
- Heavy wastage of drugs
- Frequent trips to the restroom or breaks
- Drugs and syringes in pockets
- Anesthesia record does not match up with drug dispensed and administered to patient
- Patient has unusually significant or uncontrolled pain after anesthesia.
- The patient has a higher pain score as compared to other anesthesia providers.
- Times of cases do not correlate when provider dispenses drug from automated dispenser
- Inappropriate drug choices and doses for patients are made by the provider
- Missing medications or prescription pads
Substances such as opioids (e.g., morphine and fentanyl), inhalational anesthetics and volatile agents (e.g., sevoflurane, nitrous oxide), and intravenous anesthetic agents (e.g., propofol) are readily available to many healthcare providers (1). Despite medication dispensing and audit controls in place, drugs can be diverted for misuse. This may happen through the procurement of medicines directly from the pharmacy, automated dispensing units, retrieval from sharps containers of medication remaining in syringes, directly from patient medications, or indirectly through dilution of a medication that appears that nothing is missing from the container (1).
Regardless of the substance being abused, impairment in the workplace can negatively impact patient and provider safety. Facilities should have policies and education addressing symptom awareness, prevention, and reporting to help minimize the risk of diversion and adverse outcomes. Studies have shown that substance use disorder is a disease of the brain (1). As a responsible healthcare provider, by arming yourself with knowledge and the signs and behaviors of impairment in the workplace, it will prevent further harm.
Healthcare providers are usually successful at disguising their issues or potential signs are ignored because they are respected or an intelligent member of the healthcare team. Significant changes in behavior in the workplace may various many causes. If signs of substance abuse and drug diversion are left unrecognized or reported, the user may be placed in danger and patient safety compromised. Impaired health professionals sometimes develop coping mechanisms that allow them to cover up their diminished capacity to provide safe and efficient patient care. Eventually, mistakes are made, including medication and procedural errors that become apparent to their co-workers (3).

Self-Quiz
Ask Yourself...
- What are some of the signs and behaviors associated with substance abuse?
- What are some examples of substances that can be misused in the healthcare workspace?
- Are you familiar with the systems in place in your institution related to substance abuse, reporting, and addiction?
Consequences of Drug Diversion and Substance Abuse in the Workplace
Healthcare providers are responsible for their patients’ safety, including their duty to deliver safe and competent care without impairment. Impairment in the workplace can create a disorganized environment (1). The consequences associate with substance use and drug diversion in the workplace may cause the following consequences to the patient themselves, their colleagues, and the facility in which they are employed.
Patient
- Pain, anxiety, and side effects from improper dosing
- Allergic reaction to wrongly substituted drug
- Victim of medical errors
- Loss of trust in the healthcare system
- Communicable infection from a contaminated needle (1)
Impaired Professional
- Adverse health effects related to abuse
- Chronic health problems (heart disease, liver impairment)
- Familial and financial difficulties
- Loss of social status
- Felony prosecution, incarceration, and civil malpractice
- Actions against a professional license
- Accidents resulting from physical harm (1)
Colleagues
- Injury or infection from bloodborne pathogens from improperly stored equipment
- At risk for shared-patient care responsibilities with an impaired professional resulting in adverse patient outcomes
- The stress of increased workload from an impaired healthcare team member
- Disciplinary action for false witness of leftover medication, improper disposal, or failure to report (1)
Facility
- Costly investigation
- Civil liability for patient harm
- Damaged reputation due to public knowledge of mandatory reporting or drug diversion instances, especially those that led to patient harm
- Poor work quality
- Loss of revenue from diverted drugs or reimbursement from adverse events due to impaired provider (1)
The use of addictive substances over time may result in the deterioration of the healthcare professional’s overall health. For example, the use of stimulants may result in cardiovascular problems such as angina, hypertension, and Myocardial Infarction. Alcohol can lead to liver disease, such as cirrhosis. Depression, suicide, and anxiety are mental health disorders that are often coexisting problems with substance abuse. The healthcare workers’ impairment can also lead to traumatic injuries such as falls, fractures, and head injuries (1).

Self-Quiz
Ask Yourself...
- What are some of the adverse health effects that substance abuse can have on a user?
- What are potential detrimental effects that substance abuse of a healthcare professional can have on a patient? Have you experienced any of these in your workplace?
Florida Rules and Regulations
Many states have rules and regulations regarding the use of alcohol and controlled substances that include disciplinary action. Drug diversion is a significant offense that is taken very seriously. Almost every state requires the reporting of a health practitioner who is suspected of impairment in the workplace. The penalties associated with this vary state by state.
The state of Florida they have an efficient reporting system. Nurses report to the Florida Department of Health or Intervention Project for Nurses (IPN). The IPN’s mission is to enhance public safety by assisting nurses and other nursing related personnel whose practice may have been impaired by substance abuse (4). Their call of the acknowledgment of impairment remains confidential. The Intervention Project for Nurses in Florida allows for an opportunity for intervention and the monitoring of nurses that are using alcohol or controlled substances (4).
The IPN after receiving a referral of impairment will:
- Initiate a consultation.
- Provide an intervention.
- The nurse will be required to stop practicing within 1-3 days-the entire process may take up to 12 months.
- Assist the person in obtaining the appropriate treatment needed.
- Evaluate the progress of the person and the adherence to their treatment plan.
- Continue to monitor the person for 2-5 years.
Reporting and Intervention
Once a nurse or other employee has determined that there is an issue with a coworker regarding impairment in the workplace, an intervention must occur to prevent further harm from happening to patients, themselves, or other co-workers. According to the Intervention Project for Nurses, the co-worker determines that there is sufficient evidence and documentation to support their concerns of the impairment of a health professional, an intervention should be planned (4). The planning and participation related to such intervention is usually the responsibility of the employee’s nursing manager.
Intervention process steps: (4)
- Prepare a plan.
- Review documentation.
- Request help from others.
- Ask the person to listen to what is said before allowing them to respond.
- Stick to their job performance.
- Have evaluator options ready.
- Expect denial.
- Report as necessary to the Board of Nursing.
Return to Practice
A recovering nurse’s return to practice requires planning and oversight by a nursing manager. Once a nurse has been determined that they are safe to return to practice, several things must fall into place. These things include developing a return to practice guidelines for that specific employee, such as returning to work agreement. Experts must also advocate for the employees to return to work, provide support, review expectations, monitor requirements, and answer questions (4).
Considerations on Relapse
Substance use is a chronic illness that comes unfortunately with periods of remission and exacerbation. The rate of relapse among nurses is lower than the general population (4). This is due to several factors, such as support programs and stringent state monitoring programs. Despite the fact, some nurses relapse. Knowledge of the management of relapse in the workplace is a crucial part of impairment in the workplace and plays a significant role in the safety of patients and other employees (4).

Self-Quiz
Ask Yourself...
- In the state of Florida, who do nurses report impairment to?
- What are some of the things the Intervention Project for Nurses will do once they have received a referral?
- Can a nurse return to practice after disciplinary action for substance abuse?
Conclusion
Substance abuse is a chronic and progressive disease. Being able to recognize impairment in the workplace is imperative for the safety of patients, the impaired person, and other co-workers. Impairment can come in many forms. Being knowledgeable of the signs and symptoms as well as reporting responsibilities and policies will not only improve safety but also improve the overall practice environment. Nurses can be exceptionally good at picking up subtle clues as to another’s impairment. Be aware, be knowledgeable, and be supportive.
References
- American Association of Nurse Anesthetists. (n.d.). Addressing Substance Use Disorder for Anesthesia Professionals. Retrieved February 01, 2021, from https://cms.aana.com/docs/default-source/practice-aana-com-web-documents-(all)/professional-practice-manual/addressing-substance-use-disorder-for-anesthesia-professionals.pdf?sfvrsn=ff0049b1_4
- Washington Health Professional Services. (2016, March). A Guide for Assisting Colleagues Who Demonstrate Impairment in the Workplace. Retrieved February 03, 2021, from https://www.doh.wa.gov/portals/1/Documents/Pubs/600006.pdf
- Toney-Butler TJ, Siela D. Recognizing Alcohol and Drug Impairment in the Workplace in Florida. [Updated 2020 Dec 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507774/
- Employer Information. (n.d.). Retrieved February 03, 2021, from https://www.ipnfl.org/employer-information/#sec1
Florida Human Trafficking
Prevalence and Definition
The Polaris Project estimates that collectively there are over 25 million victims of human trafficking worldwide. These are individuals that have been forced into sexual or labor servitude. Of those, several hundred thousand are estimated to be in the United States (1). It is very difficult to estimate accurately as so often this is a crime that is unseen and hidden from the public eye. Since 2007, there were 14,906 contacts made concerning human trafficking reported within Florida to the National Human Trafficking Hotline via telephone calls, texts, or online submissions. These numbers exemplify the number of potential victims that are not reaching out for help.
Often, when human trafficking is discussed, a common misconception is that it is simply the transporting of humans. Human trafficking covers a much broader scope than this. It is this a modern age form of slavery and involves the exploitation of individuals for monetary or sexual gain. As stated by the Department of Homeland Security, “Human trafficking involves the use of force, fraud, or coercion to obtain some type of labor or commercial sex act” (3).
As defined by U.S. law, there are three categories of human trafficking (all from 1):
- Children under the age of 18 induced into commercial sex
- Adults (age 18 or over) induced into commercial sex through force, fraud, or coercion
- Children and adults induced to perform labor or services through force, fraud, or coercion
The majority of trafficking in the United States involves sex crimes, followed by labor (4). These crimes may be occurring simultaneously to the same victim. Types of trafficking can include forced prostitution, pornography, strip dancing, criminal enterprise and bonded labor in domestic servitude or migrant work. Outside of street prostitution, sex trafficking is most likely to be occurring in venues such as strip clubs, massage parlors, or other fictitious business fronts for prostitution. A major difference with sex trafficking of minors is that, unlike adults, force, coercion, or fraud does not need to be present for prosecution (6). As there are a number of different avenues for and types of human trafficking, recognition can be challenging.
Risk Factors
The profile of the human trafficking victim is not easy to define. Victims of human trafficking come from varied backgrounds that may or may not be what is expected or stereotypical. Victims may come from any race, socioeconomic status, color, religion, age, gender, sexual orientation or gender identity, and on. The main commonality is that there is a layer of deception whereby the human trafficker is targeting a vulnerability in the victim. As stated by the Department of Justice, trafficking victims are deceived with “… false promises of love, a good job, or a stable life and are lured into situations where they are made to work in deplorable conditions with little or no pay” (5). There are some trends noted that do make certain populations more at risk, but keep in mind that this does not encompass all potential victims and vigilance should be taken to avoid assumptions.
The risk factors for human trafficking are just as varied and dependent upon the type of trafficking and method by which the abuser is able to hold the victim indentured or captive. This figurative prison may be physically, emotionally, or monetarily induced. The Center for Disease Control and Prevention (CDC) lists the following characteristics and factors:
- Many victims are women and girls, though men and boys are also impacted.
- Victims include all races, ethnicities, sexual orientations, gender identifies, citizens, non-citizens, and income levels.
- Victims are trapped and controlled through assault, threat, false promises, perceived sense of protection, isolation, shaming, and debt.
Several higher risk populations have been identified through the data gathered from the Polaris Project. It was found that children who were or had been within the foster care system or runaway homeless youth were more likely to encounter sexual victimization. Other factors include substance abuse, recent relocation or migration, unstable housing situations, and underlying mental health disorders (7).
As a population that is often overlooked, shamed, or lacks resources, members of the lesbian, gay, bisexual, transgender, queer, or questions (LGBTQ) community are more vulnerable to being subject to human trafficking. Up to 40% of homeless youth are part of the LGBTQ community and may not seek assistance for fear of being shunned (8).
Illegal and sponsored immigration remains at a higher risk of trafficking and exploitation. The NHRTC reports a significant number of calls that reference foreign nationals (2). Individuals wishing to become American citizens are lured with the promise of freedom in exchange for large fees that are made impossible to be worked off. While there are laws in place to prevent, this type of servant bondage is forced upon the victims who are in a new country and often lack resources or are unable to seek assistance due to cultural, language, and accessibility barriers. Further, cases have been reported where the employer or trafficker withhold visas or identification barriers in order promote compliance and essentially are holding the victim hostage (9).

Self-Quiz
Ask Yourself...
- What percentage of homeless youth are a part of the LGBTQ community?
- What are some of the risk factors for human trafficking?
- Can boys and/or men be victims of human trafficking?
- What are the different methods that perpetrators use to control victims?
Recruitment Techniques
A major tactic of the perpetrators of these crimes is to prey on vulnerable individuals with a lack of resources. Thus, a primary ploy used is a layer of deception whereby the human trafficker is targeting the needs or wants of the victim.
Traffickers are often individuals that the victim has come to trust. This may be a girlfriend or boyfriend, spouse, or other family member. Victims are also commonly sold to outside parties.
In cases of sexual trafficking, typically young women and men are groomed and given preferential treatment, gifts, and drugs until they become reliant upon the “John”. In other cases, individuals are tempted with the promise of a better life, or in the case of immigration, the sponsorship for a visa (9).

Self-Quiz
Ask Yourself...
- What ploys do perpetrators use to deceive and lead their victims into sex trafficking?
- In Florida, human trafficking victims are commonly immigrants. What is a common promise that perpetrators make to these victims?
Mandatory Reporting
Mandatory reporting of human trafficking by health care professionals is incorporated into the law in a growing number of locations in the United States. Health care professionals are already mandated reporters through previous existing laws that require reporting of child abuse, domestic violence, as well as knife and gunshot wounds (11)
The following states the criminal and civil liability of failing to follow the law as a mandatory reporter in some states:
In a civil action, the mandated reporter may be held liable for all damages that any person suffers due to the mandated reporters’ failure to file a report. In a criminal action, the mandated reporter may be found guilty of a misdemeanor punishable by imprisonment for up to 93 days and a fine of $500.
Reporting of suspected adult human trafficking is not as clear in regard to mandatory reporting. However, vulnerable adults suspected of being abused, exploited, or victimized fall under the same guidelines and are reported to CI in the same manner as above.

Self-Quiz
Ask Yourself...
- Who can be held liable if they fail to report any act of human trafficking?
Federal Law
Today, there are 39 states that have committed to the crusade of establishing a statute banning human trafficking.
A specific U.S. Federal law addressing trafficking crimes was first enacted with the Trafficking Victims Protection Act of 2000. The bill has since been revised several times; however, the fundamental of it is to provide guidance and authorization for their “three-pronged approach that includes prevention, protection, and prosecution” and covers both sex and labor trafficking (12).
Preventing Sex Trafficking and Strengthening Families Act of 2014 and The Justice for Victims of Trafficking Act of 2015 are both aimed at providing victims increased protection for exploitation and increased resources specifically aimed at prevention and support for child and youth sex trafficking crimes (12).
The Customs and Facilitations and Trade Enforcement Reauthorization Act of 2009 is aimed towards prohibiting the importation of goods made by the benefit of human trafficking (12).
Recognizing Signs of Human Trafficking
According to the Department of Health and Human Services, close 90% of human trafficking victims visit a health care facility at least once while in servitude and are not identified as such by health care providers (14). This is due to a lack of education, lack of consistent use of identification and screening tools, and time constraints within the current health care system. As a mandatory reporter and healthcare team member, it is imperative to use best practice in recognizing the signs and symptoms as well as the tools that are available.
Signs and symptoms
Human trafficking victims may present to a healthcare setting with primary or underlying signs that may be related to physical or mental abuse. These signs and symptoms may be related to the reason that they are seeking treatment or may be identified by the healthcare provider during a thorough assessment. The following physical and psychological sequelae may be noted during an assessment as potential evidence of victimization (all derived from 9, 15):
Physical
- Unexplained or implausible injuries
- Bruising
- Wounds and Cuts
- Missing or broken teeth
- Closed head injuries
- Blunt force trauma
Neurological
- Headaches
- Migraines
- Memory loss or difficulty concentrating
- Vertigo
- Insomnia
- Brain trauma
Gastrointestinal
- Diarrhea
- Constipation
Dietary
- Malnutrition
- Anorexia
- Severe weight loss
Cardiovascular and Respiratory
- Tachyarrhythmias
- Hypertension
- Respiratory distress
Reproductive System
- Sexually transmitted disease
- Vaginal and/or anal fissures
- Previous Abortions
Psychological
- Depression
- Suicidal Ideation
- Anxiety
- Self-harm including cutting or branding
- Drug and alcohol abuse
- PTSD symptoms
- Regression
- Anger
- Dissociative and depersonalization tendencies
Red flags and Indicators
There are several characteristics that should be kept in mind as red flags during the interview and assessment that may indicate potential trafficking. These include, but are not limited to (all derived from 9, 15, 16):
- Tattoos that indicate ownership, a number, or tracking system or are out of character/obscene
- Inappropriate clothing for climate
- Workplace violence or abuse
- Unsanitary living conditions
- Multiple families or people sharing a living space that is too small
- Shares living space with employer
- Is not in control of financial assets
- Refusal to speak alone with health professionals
- Accompanied by individual that refuses to allow patient to speak for themselves or be alone
- Prostitution under age 18
- Answers are scripted
- Answers are implausible or contraindicative
- Appears younger or older than stated age

Self-Quiz
Ask Yourself...
- What red flags really stand out to you?
- Have you seen any of these in your practice?
- What are some of the signs and symptoms that victims of human trafficking may present with?
- What are a few red flags or indicators that someone may be a victim of human trafficking?
Interview Tools and Techniques
Check with your facilities protocol for specific guidance on assessment and examination protocols for suspected abuse victims. There are also many scripted interviewing tools available online that assist with asking targeted questions. First and foremost, it is important to establish the patient’s safety and to gain trust.
Gaining trust can be difficult and conducting assessments and interviews should be completed in a non-threatening environment with an unbiased and non-judgmental tone. Creating a space that is quiet and will not be interrupted is important. This will ensure that the potential victim feels safe communicating and is not concerned that she or he will be overheard. Present your demeanor in a non-threatening manner, at eye level, and focus on being attentive with observant listening. Maintain respectful eye contact to convey interest and reflective listening. If taking notes during the interview is required, explain to the patient what will be documented and what it will be utilized for (17).
The National Human Trafficking Resource Center (NHTRC) offers a plethora of resources and scripted questions. The following are general questions on assessing if the individual is being forced into a situation and can be applied to any of the specific types of human trafficking (all from 17):
“Did someone control, supervise or monitor your work/your actions?”
“Was your communication ever restricted or monitored?”
“Were you able to access medical care?”
“Were you ever allowed to leave the place that you were living/working? Under what conditions?”
“Was your movement outside of your residence/workplace ever monitored or controlled?”
“What did you think would have happened if you left the situation? Was there ever a time when you wanted to leave, but felt that you couldn’t? What do you think would have happened if you left without telling anyone?”
“Did you feel that it was your only option to stay in the situation?”
“Did anyone ever force you to do something physically or sexually that you didn’t feel comfortable doing?”
“Were you ever physically abused (shoved, slapped, hit, kicked, scratched, punched, burned, etc.) by anyone?”
“Were you ever sexually abused (sexual assault/unwanted touching, rape, sexual exploitation, etc.) by anyone?”
“Did anyone ever introduce you to drugs, medications as a method of control?”
While screening tools provide a base for asking difficult questions, the NHTRC advises “Before screening, users should also be prepared to draw upon the expertise of local legal and medical staff and to refer identified trafficking victims to appropriate housing, health, and social services in their area . . . the tool is a complement to, not a substitute for, specialized training in human trafficking, good professional practice and victim-centered service” (17).
The NHTRC also provides a 24-hour national hotline that is able to guide health professionals through completing assessments and determining the next best steps to intervene or offer the victim assistance.

Self-Quiz
Ask Yourself...
- How would you approach and interview a patient victim of human trafficking?
- Are there any additional questions that you would ask them other than tools learned within this course?
Interventions and Collaboration
When presented with a suspected human trafficking victim, it is likely that the individual will not be alone. Maintaining safety and support for the patient may require separation from the suspected trafficker. While this may not be possible, an attempt should be made to bring the patient to a room or examination area unaccompanied.
Be conscious of any cultural preferences that may affect the patient. If there are language barriers preventing meaningful communication, enlist the assistance of a professional interpreter. This is especially vital in cases where the accompanying visitor or family is attempting to interpret for the patient and may be filtering the victim’s responses.
For patients that seek healthcare related to sexual abuse, a SANE assessment and rape kit should be obtained per facility protocol. With permission, patients should be tested for sexually transmitted infections including HIV, gonorrhea, UTIs, syphilis, and pubic lice, as well as a pregnancy test for females. Forced and coerced abortions are frequent among minor females in the sex industry (18).
Thorough documentation of the patient’s reported reason for visit, physical and neurological assessment including any trauma, bruising, wounds, affect, and pertinent statements should be noted in the patient’s electronic medical record.
Educate yourself on local resources and be able to provide assistance with finding access to healthcare, mental health, and rehabilitative resources that are available in the community. Victims may not want to take pamphlets with them that may be found, so providing locations or addresses of shelters or clinics with operating times may be a safer option.
Collaborate with the healthcare team, law enforcement, and social work for suspected child or vulnerable adult trafficking.
Mandatory reporting of suspected cases of child abuse or trafficking is not encumbered by HIPAA disclosure when reporting to authorities; however, when reporting suspected adult trafficking, disclosure and permission must be granted unless there is an imminent threat to the safety of the patient, or the patient has been identified as a vulnerable population. Thoroughly assess if the individual meets criteria as a vulnerable adult and proceed accordingly. If the adult does not meet criteria, permission must be gained to report.
If a competent adult does disclose that they are a trafficking victim, determine if the patient is in immediate, life-threatening danger. If so, follow facility protocol and encourage and support the patient in reporting to a law enforcement agency. If there is no immediate danger, supportive care and assistance should be provided. The patient should be informed of the options available for social services, reporting, and resources. The creation of a safety plan is highly recommended (15).
Prevention
Prevention of human trafficking requires public education, awareness, and knowing how to properly respond when faced with suspicions. The Blue Campaign is a strategy from the Department of Homeland Security to bring national awareness to the issue and provide specialized training to law enforcement and federal employees. Blue Campaign pamphlets and other materials are available at their website, www.dhs.gov/blue-campaign, for distribution.
The Center for Disease Control takes the stance that sex trafficking is preventable via community awareness and acknowledging exploitation when it does occur. They state “Strategies based on the best available evidence exist to prevent related forms of violence, and they may also reduce sex trafficking. States and communities can implement and evaluate efforts that:
- Encourage health behaviors in relationships.
- Foster safe homes and neighborhoods.
- Identify and address vulnerabilities during health care visits.
- Reduce demand for commercial sex.
- End business profits from trafficking-related transactions.” (6)
One of the largest barriers to prevention in the healthcare system is the inability to recognize signs and symptoms. As cited above, a significant number of human trafficking victims have filtered in and out of healthcare systems without being recognized. This misses the opportunity to connect, provide resources, and offer further assistance. The NHTRC provides many resources for training within healthcare facilities and standardized forms and interviewing questions that may be tailored to individual situations and facility needs.
Patient Education
UNICEF provides excellent resources for human trafficking prevention. Below is an excerpt from UNICEF, with “key messages” for children, which can help prevent trafficking.
- Educate yourself on the issue, and learn the signs of a trafficked victim.
- Don’t accept friend requests from people you don’t know on social media. Traffickers commonly use sites like Twitter, Facebook, and Instagram to lure their victims.
- Be aware of how traffickers recruit people and pay attention to your surroundings.
- Don’t reveal too much about yourself (i.e., your full name, address, school, or living situation) to people you don’t know, whether on your social media sites or in person, no matter how friendly the person may be.
- Never agree to meet someone you don’t know without first consulting a trusted adult (i.e., parent, teacher, guidance counselor).
- If you feel uncomfortable or are hesitant about a situation, confide in an adult who you can help you make the best choices.
- Making a decision to leave a situation or relationship where you feel unsafe or are being harmed or threatened can be hard and scary. If possible, talk to someone you trust, like a friend, family member, counselor, or youth worker.
- If you are in immediate danger or are being physically harmed, call 911 for help.
- If running away from home, try to find a safe place to go or call the runaway switchboard at 1-800-Runaway.
- If you suspect you or a friend are at risk trafficking, call the National Human Trafficking Hotline at 888-3737-888 or text “BeFree” (233733)

Self-Quiz
Ask Yourself...
- Who might you call within the community as a resource as a nurse when you suspect a child or vulnerable adult human trafficking?
Resources
Children and adults can be victims of human trafficking. “If you see something, say something.”
- Contact the Florida Abuse Hotline 1-800-96-ABUSE (1-800-962-2873) to report known or suspected child abuse, neglect, or abandonment, and known or suspected abuse, neglect, or exploitation of a vulnerable adult.
- For help, contact the National Human Trafficking Hotline 1-888-373-7888.
- Text HELP to 233733 (BEFREE): To get help for victims and survivors of human trafficking or to connect with local services.
- Visit the National Human Trafficking Hotline online at: https://humantraffickinghotline.org.
References
- https://polarisproject.org
- https://humantraffickinghotline.org/state/michigan
- https://www.dhs.gov/blue-campaign/what-human-trafficking
- United Nations Office on Drugs and Crime. (2016). Global report on trafficking in persons, 2014. New York, NY: United Nations.
- https://www.justice.gov/humantrafficking/what-is-human-trafficking
- https://www.cdc.gov/violenceprevention/sexualviolence/trafficking.html
- https://polarisproject.org/2019-us-national-human-trafficking-hotline-statistics/
- https://polarisproject.org/wp-content/uploads/2019/09/LGBTQ-Sex-Trafficking.pdf
- Hachey, L., & Phillippi, J. (2017). Identification and management of human trafficking victims in the emergency department. Advanced Emergency Nursing Journal, 39(1), 31–51.doi: 10.1097/TME.0000000000000138
- RETRACTED:https://swmihumantrafficking.org/michigans-human-trafficking-law/
- Mandatory Reporting of Human Trafficking: Potential Benefits and Risks of Harm. AMA Journal of Ethics. Accessed d12/10/2020. https://journalofethics.ama-assn.org/article/mandatory-reporting-human-trafficking-potential-benefits-and-risks-harm/2017-01
- https://humantraffickinghotline.org/what-human-trafficking/federal-law
- RETRACTED: https://www.michigan.gov/mdhhs/0,5885,7-339-73971_7119_50648_44443-157836–,00.html
- Update: Identifying human trafficking patients alert. Patient Safety Monitor Journal. 2018;19(9):6. Accessed October 31, 2020. http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=131246408&site=eds-live
- Identifying Victims of Human Trafficking: What to Look for in a Healthcare Setting. Journal of Legal Nurse Consulting. 2020;31(3):30-33. Accessed October 31, 2020. http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=145452392&site=eds-live
- https://www.state.gov/identify-and-assist-a-trafficking-victim/
- National Human Trafficking Hotline. Comprehensive human trafficking assessment tool. Retrieved from https://humantraffickinghotline.org/sites/default/files/Comprehensive%20Trafficking%20Assessment.pdf
- https://www.acf.hhs.gov/sites/default/files/orr/fact_sheet_sex_trafficking.pdf
Opioid Abuse
What are Opiates?
Opiates are powerful substances which are commonly used to alleviate both acute and chronic pain. The history of opiate use / abuse goes back many thousands of years. The first recorded reference is from 3,400 B.C. when opium was cultivated in southwest Asia. There were even wars fought over the previous flow in the mid 1800s (1). The most famous historical event related to opium were the advent of “opium dens.” These were underground “dens” where opium was bought, sold, and used (1). Much like today, the addictive properties of opium overcame many individuals and caused great harm to the world and communities. Indeed, the opiate epidemic of the 2000’s is not the first in modern history, though it is much different and more severe than previous epidemics.
Today opiates are used for both acute and chronic pain. The ability to quickly, reliably, and (when used appropriately) safely reduce pain is what makes the drug class so valuable. Many common drugs are opiate derivatives or synthetics including morphine, codeine, oxycodone, heroin, hydromorphone, and fentanyl.
In the United States Opiates are considered controlled substances and most of them are classified as schedule II (with heroin classified as schedule I) (2). Opiates will always have a place in medicine and treatment of pain and are incredibly useful, however, the current opiate epidemic in America makes clear the potential consequences of opiate abuse.
Preventing Abuse, Misuse, and Harm
Every day 130 Americans die of opiate overdose (3). Additionally, there are 4.3 million Americans each month who engage in the non-medical (non-prescribed or illicit) use of opiates (5). However, it is key to remember that opiate-related deaths are not the only negative consequences. There are many overdoses which do not end in death, and on the other end of the spectrum many negative affects do not cause death. Addiction can cause loss of job, damage to relationships, psychologic distress, homelessness, and many more negative side-effects.
So how do healthcare professionals help reduce the impact of opiate addiction and misuse? The approach must be multi-modal, aimed at primary, secondary, and tertiary prevention.
- Primary prevention includes appropriate opiate prescribing, risk stratification with patients, and preventing opiate addiction.
- Secondary prevention is aimed at mitigating the effects of opiate addiction. This includes rehabilitation and cessation of opiates in addicted individuals, ideally in favor of non-opiate treatment options.
- Tertiary prevention is the reduction in harm from opiate addiction and overdose. This includes resuscitation of overdose patients and helping patients recover from the effects of opiate addiction.
Appropriate Prescribing
The Centers for Disease Control and Prevention (CDC) offers excellent guidance on how to appropriate prescribe opiates, though it will continue to require a great deal of knowledge and effort from individual prescribers and managers of chronic pain. For the purposes of this article, we will focus on the CDC recommendations. Below we will discuss the 12 key points of opiate management, per the CDC.
Opioids Are Not First-Line Therapy
“Nonpharmacologic therapy and nonopioid pharmacologic therapy are preferred for chronic pain. Clinicians should consider opioid therapy only if expected benefits for both pain and function are anticipated to outweigh risks to the patient. If opioids are used, they should be combined with nonpharmacologic therapy and nonopioid pharmacologic therapy, as appropriate.” (5)
Author’s Input: Many patients experience pain. Indeed, it is one of the most common complaints in primary care offices. When dealing with chronic pain, we should consider ALL non-opiate therapies for patients prior to prescribing opiates. This can include physical therapy, meditation, exercise / movement, treatment of underlying depression and/or psychiatric issues, meditation, modification of aggravating factors, and many more interventions. In some cases, none of these alone or combination will be enough to provide satisfactory relief, but we must utilize non-opiate and non-pharmacological solutions as much as possible to reduce opioid abuse, and dose (if opiates are necessary).
Establish Goals for Pain and Function
“Before starting opioid therapy for chronic pain, clinicians should establish treatment goals with all patients, including realistic goals for pain and function, and should consider how opioid therapy will be discontinued if benefits do not outweigh risks. Clinicians should continue opioid therapy only if there is clinically meaningful improvement in pain and function that outweighs risks to patient safety “(5).
Author’s Input: Many patients erroneously believe that cessation of pain is the goal of therapy. This is not based in fact nor is it reasonable, as many patients (even with opiate therapy) will not have complete remission of pain. The goal of the clinician should be to work with the patient to provide the minimal risk intervention that will provide acceptable pain control.
Discuss Risks and Benefits
“Before starting and periodically during opioid therapy, clinicians should discuss with patients known risks and realistic benefits of opioid therapy and patient and clinician responsibilities for managing therapy” (5).
Author’s Input: A prescription for an opiate should never be written to a patient without a through discussion of the risks and benefits. The clinician must first be convinced that the risk to benefit favors prescribing an opiate. Then, they must discuss their rationale with the patient. An individual assessment regarding the risks should be provided to each and every patient.
Prescribe Immediate-Release Opioids First
“When starting opioid therapy for chronic pain, clinicians should prescribe immediate-release opioids instead of extended-release/ long-acting (ER/LA) opioids” (5).
Author’s Input: Extended-release opioids have been associated with higher rates of overdose and higher potential for Opioid abuse. Immediate-release opioids should be utilized first, whenever possible.
Clinicians Should Prescribe the Lowest Effective Dosage
“Clinicians should use caution when prescribing opioids at any dosage, should carefully reassess evidence of individual benefits and risks when considering increasing dosage to ≥50 morphine milligram equivalents (MME)/day, and should avoid increasing dosage to ≥90 MME/day or carefully justify a decision to titrate dosage to ≥90 MME/day.”
Author’s Input: The clinician must keep in mind that the “minimum required dose” may change over time. As a patient implements more non-pharmacologic interventions the required dose may decrease. Conversely, there can be some degree of tachyphylaxis with opiates and the required dose may also increase. Dose titration requires careful clinician judgement.
Prescribe Short Durations for Acute Pain
“Long-term opioid use often begins with treatment of acute pain. When opioids are used for acute pain, clinicians should prescribe the lowest effective dose of immediate-release opioids and should prescribe no greater quantity than needed for the expected duration of pain severe enough to require opioids. Three days or less will often be sufficient; more than seven days will rarely be needed” (5).
Author’s Input: It is well established that chronic opioid therapy is not the most effective therapy for pain management. Clinicians should consider adjuncts for ongoing or chronic pain patients.
Evaluate Benefits and Harms Frequently
“Clinicians should evaluate benefits and harms with patients within 1 to 4 weeks of starting opioid therapy for chronic pain or of dose escalation. Clinicians should evaluate benefits and harms of continued therapy with patients every 3 months or more frequently. If benefits do not outweigh harms of continued opioid therapy, clinicians should optimize other therapies and work with patients to taper opioids to lower dosages or to taper and discontinue opioids” (5).
Author’s Input: It is important that clinicians consider changing circumstances. A patient’s health status or life circumstances may change such that opiate therapy benefits no longer outweigh the harm, or vice-versa.
Use Strategies to Mitigate Risk
“Before starting and periodically during continuation of opioid therapy, clinicians should evaluate risk factors for opioid-related harms. Clinicians should incorporate into the management plan strategies to mitigate risk, including considering offering naloxone when factors that increase risk for opioid overdose, such as history of overdose, history of substance use disorder, higher opioid dosages (≥50 MME/day)” (5).
Author’s Input: Naloxone therapy should be considered for all patients who are at high risk of Opioid overdose.
Review Prescription Drug Monitoring Program Data
“Clinicians should review the patient’s history of controlled substance prescriptions using state prescription drug monitoring program (PDMP) data to determine whether the patient is receiving opioid dosages or dangerous combinations that put him or her at high risk for overdose. Clinicians should review PDMP data when starting opioid therapy for chronic pain and periodically during opioid therapy for chronic pain, ranging from every prescription to every 3 months” (5).
Author’s Input: Each state has robust data regarding prescription medication; utilizing this data can help reduce opioid misappropriation and concurrent prescriptions (doctor shopping).
Use Urine Drug Testing
“When prescribing opioids for chronic pain, clinicians should use urine drug testing before starting opioid therapy and consider urine drug testing at least annually to assess for prescribed medications as well as other controlled prescription drugs and illicit drugs,” (5).
Author’s Input: The author recommends that clinicians take great care in this area. Indeed, drug testing can help identify those who are already abusing other substances, but it can also harm the trusting relationship developed between a patient and clinician. The patient should be re-assured that the testing is performed for their own good and out of concern for their own health, rather than punitively or because the clinician “mistrusts” them, as these may be the default thoughts of many patients.
Avoid Concurrent Opioid and Benzodiazepine Prescribing
“Clinicians should avoid prescribing opioid pain medication and benzodiazepines concurrently ‘whenever possible’ “(5).
Author’s Input: The highest risk of overdose of opioid abuse is commonly seen when opiates and benzodiazepine (or any combination of sedating medications) are prescribed concurrently, especially in conjunction with alcohol. For this reason, clinicians should strongly consider avoiding such risks and only prescribing this combination when absolutely necessary.
Offer Treatment for Opioid Abuse Disorder (OAD)
“Clinicians should offer or arrange evidence-based treatment (usually medication-assisted treatment with buprenorphine or methadone in combination with behavioral therapies) for patients with opioid abuse disorder” (5).
Author’s Input: In acute cares settings, clinicians often view OAD as a secondary illness and it is frequently left unaddressed. However, there are now effective treatments for OAD. Given the significant morbidity, mortality, and associated quality of life issues, patients with OAD should be offered treatment, even if it not the primary reason for treatment.
Risk Factors for Opiate Harm or Misuse
The risk to benefit has been discussed many times previously and is often referenced by the CDC. The benefits of opiate therapy are typically obvious (reduced pain, increased quality of life, etc.), but the risks are less often discussed. So how do nurses know who is at higher risk of the negative effects of opiates?
According to the CDC, actors are:
- Illegal drug use; prescription drug use for non-medical reasons.
- History of substance use disorder or overdose.
- Mental health conditions (e.g., depression, anxiety).
- Sleep-disordered , the major risk fbreathing. • Concurrent benzodiazepine use (6).
Mortality from opiates is highest in those who are middle-aged, have psychiatric conditions, and/or have previously abused substances (7). It is important that clinicians utilize this information when consider risk and benefits associated with opiate therapy.
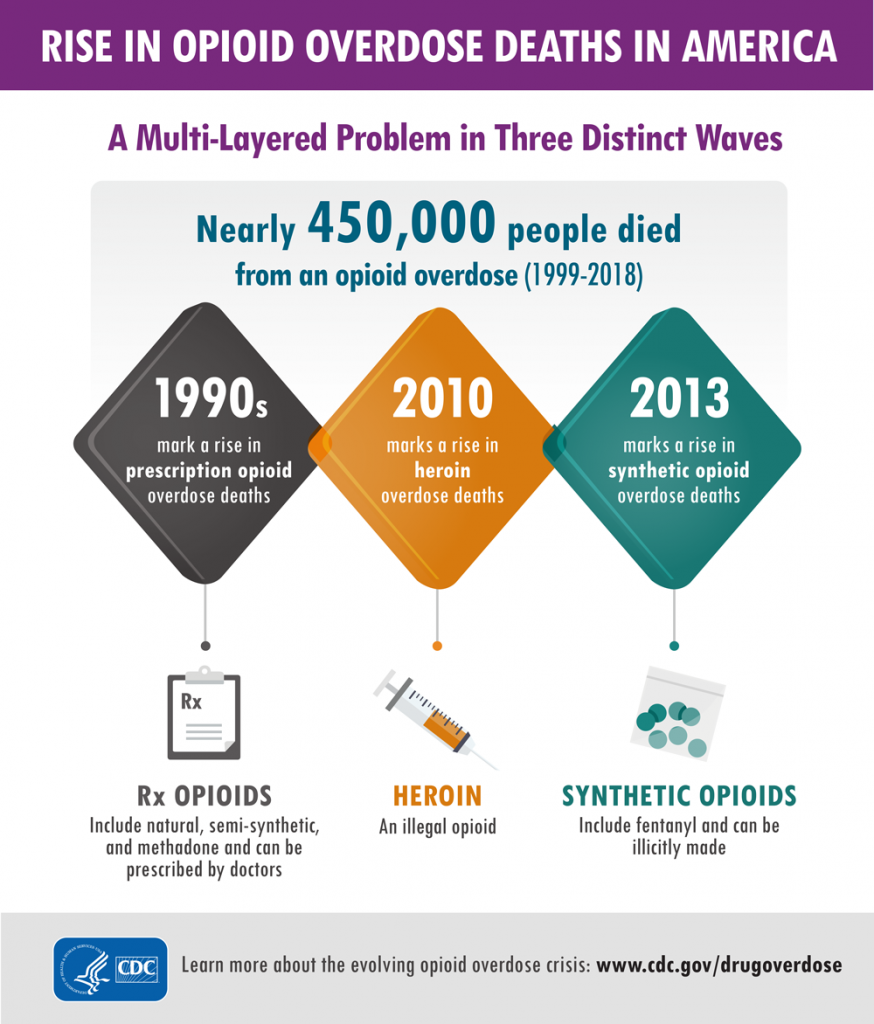
Signs of Abuse, Diversion, and Addiction
Clinicians should remain vigilant for signs of opiate use disorder, as it can occur in any patient (even those not prescribed opiates). Opiate use disorder is characterized in the DSM-5 as a desire to utilize opiates despite social and professional consequences (12). It includes dependence and addiction, with addiction being on the severe end of the spectrum (12). Opiate use disorder can be diagnosed when at least two of the following are observed in a 12-month period:
- Opioids are often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control opioid use.
- A great deal of time is spent in activities necessary to obtain the opioid, use the opioid, or recover from its effects.
- Craving, or a strong desire or urge to use opioids.
- Recurrent opioid use resulting in a failure to fulfill major role obligations at work, school, or home.
- Continued opioid use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of opioids.
- Important social, occupational, or recreational activities are given up or reduced because of opioid use.
- Recurrent opioid use in situations in which it is physically hazardous.
- Continued opioid use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance.
- Exhibits tolerance (discussed in the next section).
- Exhibits withdrawal (discussed in the next section) (centers for disease control, reference 13).
Urine drug screening can be useful in patients with suspected opiate abuse disorder as it may identify concurrently abused substances. If a patient is found to have opiate abuse disorder the “risk” side of the “risk-to-benefit” equation is now shifted, and the continued use should be carefully weighed against the potential for negative effects, including addiction. Addiction is defined as continued use despite adverse events or consequences (12).
For those prescribed opiates, clinicians should have candid conversations about the risks of continued use for those with OAD. The CDC offers some creative examples of how to discuss the condition with patients, which nurses may find helpful in their interactions (these are only examples, and the wording depends on the patient’s specific scenario and needs):
- “Trouble controlling the use of opioid medication makes it unsafe, and long-term risk over time is substantial.”
- “The medicine has become a problem in itself. You have developed a known complication of therapy that we should not ignore.”
- “Continuing the current medication is not a reasonable option due to the risks, but there are options for treating what we call opioid use disorder, also known as OUD.”
- “It seems as if you are running out of your medication more quickly than anticipated.”
- “Sometimes people become too comfortable with the medications and start to take them for reasons other than pain.”
- “You meet the criteria for opioid use disorder, also known as OUD. It’s helpful to put a name on it because it opens up a variety of approaches to help with your specific circumstance.” (All derived from source 13).
So, once we identify a patient with OAD, what do we do? At this point, as above, a candid conversation with the patient must occur. A treatment plan should be formulated, which would include a careful consideration for discontinuing for the opiate (if possible). This provides an excellent transition into our next section, opiate alternatives.
Opiate Alternatives
Opiate alternatives can be broadly classified as pharmacologic and non-pharmacologic. We will first discuss pharmacologic alternatives.
Pharmacologic:
- Acetaminophen: Commonly known as Tylenol ™ is over the counter and has a very favorable safety profile when used correctly. Acetaminophen is considered first-line therapy in any pain management regimen (9).
- NSAIDs (Nonsteroidal anti-inflammatory drugs): NSAIDs can be immensely powerful in pain management, as many pain conditions are related to inflammation. However, patient tolerance can be an issue with chronic NSAID exposure. Indeed, many clinicians shy away from NSAIDS due to the perceived risk profile (9).
- Tricyclic antidepressants: TCAs provide significant pain relief to many patients, as they have the unique ability to change the perceptions of pain (5). However, tricyclics have many side-effects of their own and thus have been phased out in lieu of newer antidepressants. This in the pain realm they should be considered for certain patients, particularly those with concurrent untreated depression.
- SSRI Antidepressants: SSRIs are typically tolerated better than tricyclics (9) but again are not recommend for first-line analgesia. They are typically reserved for those with concurrent psychiatric illness which may benefit from the overall effect of the drug, and on a case-by-case basis for selected patients.
- Muscle relaxants: Medications such as gabapentin can be extremely useful especially in pain originating from musculoskeletal causes. However, the mechanism of action is poorly understood (9) and side effects can be troublesome. In one study approximately 25% of patients taking muscle relaxants for chronic pain discontinued the agents due to adverse effects.
- Topicals: Many topical agents now exist, including NSAIDS (9). Topicals are typically considered analgesic-sparing rather than standalone treatment (9). The American College of Rheumatology has excellent and detailed guidance on how to utilize topicals, which deserves a course of its own.
- Corticosteroids: Corticosteroids have very potent anti-inflammatory effects (9) and have a proven role in pain management. Short-term therapy is typically favored over long-term therapy due to the potential issues of long-term systemic therapy (osteoporosis, immunosuppression, risk of serious or fatal infections, weight gain, muscle weakness, diabetes, Cushing’s syndrome, hypertension, glaucoma, and cataracts). Though some serious adverse events can occur with short-term therapy (psychosis, anxiety, avascular necrosis, etc.) (9). corticosteroids can be beneficial for patients with acute pain. Perhaps the best use of these agents is in targeted (injectable) delivery.
Non-Pharmacologic:
These therapies will be discussed less in-depth, as they typically require referrals for treatment. However, it is important that nurses are aware of the of the existence of these therapies and can make appropriate referrals and recommendations. Physical therapy consults are invaluable as they often utilize many of the tools below and are more knowledge about non-pharmacologic therapies in general.
- psychological interventions (including distraction, stress management, hypnosis, and other cognitive-behavioral interventions)
- acupuncture and acupressure
- transcutaneous electrical nerve stimulation
- physical therapies (including massage, heat/cold, physiotherapy, osteopathy, and chiropractic) (10)
Conclusion
Nurses should view the non-pharmacologic therapies as “tools” available to help patients dealing with acute and chronic pain. Though opiate therapy is a valuable tool as well, its potential negative effects are often under-considered, and the rate of opiate prescription currently is excessive (10).
When evaluating patients with pain, nurses should work with patients and providers to ensure that the patient is on an optimal pain regimen, which ideally should include both pharmacologic and non-pharmacologic therapies. Seeking referral and consultation from relevant professionals can also be powerful in pain management (physical therapists, chiropractors, psychiatrists, etc.).
References
- https://www.deamuseum.org/ccp/opium/history.html
- https://americanaddictioncenters.org/opiates/controlled-substances
- https://www.cdc.gov/injury/features/prescription-drug-overdose/index.html
- https://www.cdc.gov/drugoverdose/prescribing/guideline.html
- https://www.cdc.gov/drugoverdose/pdf/guidelines_at-a-glance-a.pdf
- https://www.cdc.gov/drugoverdose/pdf/pdo_checklist-a.pdf
- APA Webster, Lynn R. MD Risk Factors for Opioid-Use Disorder and Overdose, Anesthesia & Analgesia: November 2017 – Volume 125 – Issue 5 – p 1741-1748 doi: 10.1213/ANE.0000000000002496
- Andrea L. Nicol, Robert W. Hurley, Honorio T. Benzon Anesth Analg. Author manuscript; available in PMC 2018 Nov 1. Published in final edited form as: Anesth Analg. 2017 Nov; 125(5): 1682–1703. doi: 10.1213/ANE.0000000000002426
- Mart van Laar, Joseph V Pergolizzi, Jr, Hans-Ulrich Mellinghoff, Ignacio Morón Merchante, Srinivas Nalamachu, Joanne O’Brien, Serge Perrot, Robert B Raffa
- Open Rheumatol J. 2012; 6: 320–330. Published online 2012 Dec 13. doi: 10.2174/1874312901206010320
- Pak, S. C., Micalos, P. S., Maria, S. J., & Lord, B. (2015). Nonpharmacological interventions for pain management in paramedicine and the emergency setting: a review of the literature. Evidence-based complementary and alternative medicine: eCAM, 2015, 873039. https://doi.org/10.1155/2015/873039
- Safer D. J. (2019). Overprescribed Medications for US Adults: Four Major Examples. Journal of clinical medicine research, 11(9), 617–622. https://doi.org/10.14740/jocmr3906
- Dydyk AM, Jain NK, Gupta M. Opioid Use Disorder. [Updated 2020 Jun 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553166/
- https://www.cdc.gov/drugoverdose/training/oud/accessible/index.html
Vaping Induced Lung Injuries
Vaping Trends: The appeal and the rise in popularity
What started as a product designed for cigarette smokers wanting to wean off the habit while still allowing them to have the physical ritual of smoking, vaping has now become a cultural phenomenon. Minimal odor, sleek packaging, and few, if any, regulations about when and where people can vape created an appeal even to those who had never used nicotine before and the market quickly turned its attention to gaining new customers through the addition of flavors, additives like THC, and devices that look like flash drives.
The use of electronic cigarettes involves a battery-operated device and a cartridge of nicotine-containing liquid. The liquid is heated into an aerosol which is then inhaled (or vaped). The devices are most popular among adolescents, with 27.5% of high schoolers having used e-cigarettes in the last 30 days in a 2019 survey (1). Adults are using them too, with as many as 2.8% of US adults regularly vaping in 2019, many of whom had never even been cigarette smokers (1).
One of the main reasons vaping has become so popular so quickly is because of the common misconception that it is a low-risk alternative to cigarette smoking, with many companies claiming fewer toxins and not including complete ingredient lists. While e-cigarettes do contain fewer chemicals than traditional cigarettes, they are by no means a “healthy” alternative and contain their own slew of ingredients, including heavy metals such as nickel and lead, glycerin, carcinogens, and nicotine, which is a highly addictive substance (8). The nicotine level in the cartridges is also extremely high, with a typical “pod,” or cartridge, containing the same amount of nicotine as a package of cigarettes (6). This is enough to make even casual users quickly addicted. The FDA has cracked down on these loopholes in recent years, now requiring warning labels and attempting to regulate the production of flavors, but the popularity of vaping has already exploded and the effort to reverse the trend is an uphill battle.

Self-Quiz
Ask Yourself...
- What prior knowledge did you have about vaping and its posed dangers?
- What vaping induced lung injuries were you aware of?
- What are some misconceptions surrounding vaping, as well as vaping induced lung injuries, that have led to increased popularity?
Health Risks
EVALI (e-cigarette or vaping induced lung injury)
Not surprisingly, the increase in vaping has been followed by a rise in health issues for the users. Most notably among emerging illnesses (and in the media recently) is lung damage referred to as e-cigarette/vaping associated lung injury, or EVALI (2).
A recent Morbidity and Mortality Weekly Report classifies EVALI as a diagnosis of exclusion as there is currently no specific testing for the illness, but it is one that should be considered early in the presentation of symptoms to not delay treatment (3). Most patients affected presented with cough, chest pain, and dyspnea, with many others having fever, chills, weight loss, vomiting, or diarrhea. At least 30% of patients presented with an oxygen saturation of less than 95%. Tachypnea was not frequently noted, but tachycardia was common. Xray revealed abnormal lung findings in 82% of patients and CT of the lungs was abnormal in 96% (3). This emerging issue is placing significant burden on the healthcare system, as most of these patients require inpatient management with steroids and supplemental oxygen, at least for the first 24-48 hours.
When this diagnosis resulted in several deaths in mid to late 2019, it was met with panic in the media and general public as healthcare professionals scrambled to find what exactly about vaping was causing the decrease in lung function. Emerging evidence now strongly suggests that the injury to the respiratory tract is caused by Vitamin E acetate, an additive in many e-cigarette pods (3). Fluid collected from symptomatic patients’ lungs was found to contain Vitamin E acetate in most cases and buildup over time is believed to be responsible for this lung injury (3). It is too early to rule out damage from other additives (like the glycerin used for flavoring) and researchers note that while these components are safe for oral consumption and often found in food, the effects of inhalation have not been studied and frequent exposure to the lungs should not be considered safe (4).
For now, though, Vitamin E acetate is considered the main culprit and is most commonly found in cartridges containing THC, particularly those made informally by people at home rather than those purchased from a manufacturer (3).
While all vaping should be avoided, for those who do use e-cigarettes it is safest to avoid cartridges containing THC and home-made cartridges.
Other Health Concerns
In addition to the potentially lethal complications of EVALI, routine nicotine use of any kind can have serious health implications, and e-cigarettes are no different. Cardiovascular health is affected, with increased heart rate and blood pressure within minutes of nicotine use. Risk of heart attack, stroke, chronic cough, compromised immune system, and impaired oxygenation, all are increased. Nicotine’s effects on a young, developing brain are well documented as well, with attention problems, impulse control issues, and an increased addiction response all posing serious risks to teens who vape regularly (6). Substance use of any kind is closely tied to mental illnesses such as anxiety and depression as well as ongoing struggles with addiction and substance abuse throughout adulthood (6).
The risk of cancer is also not solely tied to traditional cigarettes, with many substances found in e-cigarettes believed to be carcinogenic. A 2018 study tested urine and saliva samples from vaping teens and found the levels of carcinogens present to be significant and concerning (7). In general, the belief that vaping is a low-risk alternative to cigarettes is grossly erroneous.

Self-Quiz
Ask Yourself...
- Based on the presented evidence, what is the cause of EVALI?
- What are the overall effects of nicotine on the body?
What Can Healthcare Providers Do?
Screen for Vaping Use
One of the best ways to prevent vaping related health issues is to ensure that patients do not start vaping in the first place. Pediatric providers or those working with children and teens 11 years and older are in a particularly advantageous position to start the conversations early and often. Ask questions about what they know about vaping, if they have any friends who vape, and if they themselves have tried vaping. Try to maintain a non-judgmental attitude and allow them to lead the conversation. Provide education to patients and their parents about the dangers and health risks of vaping. Talk about the strengths of the student (academics, sports, arts) and discuss how a nicotine addiction or disciplinary action for vaping at school could negatively impact these enjoyable activities. For any patients who are already vaping, create a plan for cessation (discussed below). Adult patients and established cigarette smokers should also be screened for vaping and health risks discussed (2).
Early Detection of Vaping Related Lung Injury
Screening for vaping is not only important at routine wellness visits, but also for acutely ill patients in the outpatient, inpatient, and emergency room settings. Any patient presenting with cough, chest pain, or other respiratory symptoms should be questioned about current or recent vaping habits, including the use of THC pods. Chest x-ray should be strongly considered in the workup for anyone with respiratory symptoms and a history of vaping, particularly those with a pulse oximetry <95%. Flu and pneumonia should be considered in the differential diagnosis, as vaping increases the risk of both illnesses. In patients hospitalized or treated outpatient for a suspected EVALI, close follow up for the first few weeks is recommended (2).
Cessation
For patients with or without acute lung injury related illness, vaping cessation should be counseled. For adults, many employers will offer smoking-cessation incentive programs which have been shown to be effective. Encourage your patients to ask their employer if this is offered and if they qualify. There are multiple nicotine products designed to help wean slowly from nicotine with the ultimate goal of cessation such as gum, patches, and lozenges. Either gain familiarity with prescribing these yourself or find a local provider who you can refer your patients to for these products (5). Psychotherapy or counseling can be beneficial for patients trying to break an addiction and there are typically addiction counselors available at mental health facilities. There is a Substance Abuse and Mental Health Services Treatment Locator tool that can be found at https://findtreatment.samhsa.gov/ or patients can call 1-800-662-HELP (4357) to find the nearest resources (1). Finally, if you have patients using vaping as a method of stopping cigarette smoking, you should counsel that this is not a long-term solution and has no current supportive evidence as an effective smoking cessation tool. The risks of vaping far outweigh any perceived benefits and vaping should not be counseled as a method of smoking cessation.

Self-Quiz
Ask Yourself...
- What tools can providers give vapers to help with cessation?
Case Study
Austin is a 19-year-old male presenting to the ED with 6 days of coughing, fever, lethargy, decreased appetite, and (in the last 2 days) increasing chest pain, particularly with deep inspiration.
He is a student at the local university with a history of ADHD for which he takes 20mg of Adderall XR daily. No other pertinent medical history and no other medications. He reports drinking socially on the weekends.
Vital signs are as follows: Temp: 100.9, HR: 147, BP: 134/85, RR: 20, SPO2: 87%. Physical exam reveals pallor, diaphoresis, diminished air exchange in all lung fields with crackles in the bases. Deep inspiration results in coughing fits with no improvement or clearance of crackles and rhonchi. He is most comfortable in the tripod position, but overall is restless. CBC with differential is normal, flu swab is negative. Chest x-ray reveals bilateral infiltrates.
The nurse notices a Juul device in the clear plastic bag of the patient’s belongings and when asked, he admits to vaping ¾-1 cartridge per day for 2 years. He also states he will use a THC cartridge 2-3 times per week with friends.
He is diagnosed with EVALI and admitted for treatment with corticosteroids and supplemental oxygen. He is discharged in stable condition after 2 days with scheduled follow up in 1 week. He is counseled on vaping cessation, particularly of THC cartridges, and makes a full recovery over the next 2 months.
Conclusion
Vaping is a fairly new trend and health risks are still emerging as the number of people using e-cigarettes grows. Staying abreast of trends in vaping and the growing information about symptoms, treatment, and causes of EVALI are important responsibilities of healthcare providers. Early detection of vaping related illnesses is key to best treatment outcomes and screening for vaping should become a routine part of all healthcare exams, both preventive and acute.
References
- Centers for Disease Control and Prevention. (2019). Electronic cigarettes. Retrieved from: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/index.htm
- Centers for Disease Control and Prevention. (2019). Smoking and tobacco use: for healthcare providers. Retrieved from: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease/healthcare-providers/index.html
- Chatham-Stephens, K, et al. (2019). Characteristics of hospitalized and non-hospitalized patients in a nationwide outbreak of e-cigarette, or vaping, product use-associated lung injury. Morbidity Mortality Weekly, 68(1076-1080). Retrieved from: https://www.cdc.gov/mmwr/volumes/68/wr/mm6846e1.htm?s_cid=mm6846e1_w
- Dinikar, C. & O’Connor, G. T. (2016). The health effects of electronic cigarettes. The New England Journal of Medicine, 375 (1372-1381). Retrieved from: https://www.nejm.org/doi/full/10.1056/NEJMra1502466
- Halpern, S. D., et al. (2018). A pragmatic trial of e-cigarettes, incentives, and drugs for smoking cessation. The New England Journal of Medicine, 378(2302-2310). Retrieved from: https://www.nejm.org/doi/full/10.1056/NEJMsa1715757
- Martinelli, K. (2018). Teen vaping: What you need to know. Child Mind Institute. Retrieved from: https://childmind.org/article/teen-vaping-what-you-need-to-know/
- Rubinstein, M. L., et al. (2018). Adolescent exposure to toxic volatile organic chemicals from e-cigarettes. Pediatrics, 141(4). Retrieved from: https://pediatrics.aappublications.org/content/141/4/e20173557
- U.S. Department of Health and Human Services. (2016). E-cigarette use among youth and young adults: a report of the Surgeon General. Retrieved from: https://e-cigarettes.surgeongeneral.gov/documents/2016_SGR_Full_Report_non-508.pdf
LGBTQ Cultural Competence
Introduction
Lesbian, gay, bisexual, transgender, and questioning (LGBTQ) individuals represent a rapidly growing segment of the U.S. population [1]. This rapid growth brings with it risk for stigmatization [1]. Implicit physician biases may result in LGBTQ patients receiving a lower standard of care or restricted access to services as compared to the general population [2]. Even when institutions and providers make commitments to equitable care explicit, implicit biases operating outside of conscious awareness may undermine that commitment. There is an urgent need to ensure that health care providers are prepared to identify and address their own implicit biases to ensure they do not contribute to the health care disparities experienced by LGBTQ and other vulnerable populations. Only by addressing their own implicit biases will health care providers be able to provide patient care in accordance with LGBTQ cultural competence.
LGBTQ individuals face significant disparities in physical and mental health outcomes [3]. Compared to their heterosexual counterparts, LGBTQ patients have higher rates of anal cancer [4], asthma, cardiovascular disease [5,6,7,8], obesity [6], substance abuse [8,9,10], cigarette smoking [11], and suicide [12]. Sexual minority women report fewer lifetime Pap tests [13,14,15], transgender youth have less access to health care [16], and LGBTQ individuals are more likely to delay or avoid necessary medical care [17] compared to heterosexual individuals. These disparities are due, in part, to lower health care utilization by LGBTQ individuals [3, 18,19,20]. Perceived discrimination from health care providers and denial of health care altogether are common experiences among LGBTQ patients and have been identified as contributing factors to health disparities [21,22,23,24]. Disparities in health care access and outcomes experienced by LGBTQ patients are compounded by vulnerabilities linked to racial identity [25,26,27] and geographic location [28].
Biases among health care professions students and providers toward LGBTQ patients are common [29, 30] despite commitments to patient care equality. These biases, also known as negative stereotypes, may be either explicit or implicit [31]. These biases contribute to a lack of LGBTQ cultural competence in patient care. A large study of heterosexual, first-year medical students demonstrated that about half of students reported having negative attitudes towards lesbian and gay people (i.e., explicit bias) and over 80% exhibited more negative evaluations of lesbian and gay people compared to heterosexual people that were outside of their conscious awareness (i.e., implicit bias) [29]. Research in social-cognitive psychology on intergroup processes defines explicit biases as attitudes and beliefs that are consciously accessible and controlled; they are typically assessed via self-report measures and are limited by an individual’s awareness of their attitudes, motivation to reveal these attitudes, and ability to accurately report these attitudes [32, 33]. In contrast, the term implicit bias refers to attitudes and beliefs that are unconscious (i.e., outside of conscious awareness) and automatic [34, 35]. Implicit bias can be assessed with the Implicit Association Test (IAT) [36], which measures the strength of association between concepts [37].
Health care provider biases are correlated with poorer access to services, quality of care, and health outcomes [31, 38,39,40]. Explicit biases held by health professionals towards racial/ethnic minorities, women, and older adults are known to affect clinical assessments, medical treatment, and quality of care [41]. Importantly, implicit bias measures are more strongly associated with real-world behaviors than explicit bias measures [42] and are linked to intergroup discrimination [43]. Health care provider’s implicit biases towards vulnerable patient groups may persist despite an absence of negative explicit attitudes [44], resulting in preconceived notions about patient adherence, poor doctor-patient communication, and micro-aggressions, all of which can interfere with optimal care. With less time and limited information processing capacity, provider’s decisions are increasingly governed by stereotypes and implicit biases [45]. Medical student and provider biases may contribute to health disparities in vulnerable populations by negatively impacting communication with patients and decisions about patient care [33, 35]. Taken together, these findings suggest that medical students and healthcare providers are likely to underestimate or to be unaware of their implicit biases towards LGBTQ patients, particularly when they are rushed or fatigued, which could impact their behavior and judgments in ways that contribute to health disparities experienced by LGBTQ populations. By learning about and addressing their implicit biases, health care providers can work towards demonstrating LGBTQ cultural competence and providing optimal care (Introduction section courtesy of Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P.- reference 45).

Self-Quiz
Ask Yourself...
- What are some cultural misconceptions regarding the LGBTQ community and providing medical care?
- How can you demonstrate LGBTQ cultural competence in everyday practice?
Terminology
Understanding the standard terminology utilized is pivotal to treating and interacting with LGBTQ patients. Below are listed some of the common terms and how they should be referenced.
Ally – A person not identifying as LGBTQ, but who promotes equality and support of LGBTQ peoples in a variety of ways.
Androgynous – Identifying as neither masculine nor feminine.
Bisexual – A person who is emotionally, romantically, or sexually attracted to more than one sex, gender, or gender identity.
Cisgender – A person who identifies with their gender which as assigned at birth. For example, a person assigned female gender at birth who identifies as female.
Gay – A person who is emotionally, romantically and/or sexually attracted to those of the same gender.
Gender-fluid – A person who identifies as a fluid or unfixed gender identity.
Lesbian – A woman who is emotionally, sexually, and/or romantically attracted to other women.
LGBTQ – Acronym for “lesbian, gay, bisexual, transgender, and queer.”
Non-binary – Adjective describing person(s) who do not identify exclusively as man nor woman.
Pansexual – A person who has the potential for romantic, emotional, and/or sexual attraction to people of any gender.
Queer – Often used interchangeably with “LGBTQ,” or to express fluid identities or orientations.
Sexual orientation – An inherent or enduring emotional, romantic, or sexual attraction to other people.
Transgender –Umbrella term for people whose gender identity and/or expression is different from cultural expectations based on the sex they were assigned at birth. It does not imply any specific sexual orientation and transgender persons may identify as straight, gay, lesbian, bisexual, etc.
*Definitions largely derived from (46).

Self-Quiz
Ask Yourself...
- What are some cultural misconceptions regarding the LGBTQ community and providing medical care?
- How can you demonstrate LGBTQ cultural competence in everyday practice?
Best Practices
Below we will list and discuss the best practices for ensuring a positive, equitable healthcare experience for LGBTQ persons, according to the Joint Commission (this is not a comprehensive list, just highlights).
Create a welcoming environment that is inclusive of LGBT patients and demonstrates LGBTQ cultural competence.
- Prominently display the hospital nondiscrimination policy and/or patient bill of rights.
- Waiting rooms and common areas should be inclusive of LGBTQ patients and families.
- Unisex or single-stall restrooms should be available.
- Ensure that visitation policies are fair and do not discriminate (even inadvertently) against LGBTQ patients and families.
- Foster an environment that supports and nurtures all patients and families.
Avoid assumptions about sexual orientation and gender identity.
- Refrain from making assumptions about a person’s sexual orientation and/or gender identity.
- Be cognizant of bias, stereotypes, and other communication barriers.
- Recognize that self-identification and behaviors do not always align.
Facilitate disclosure of sexual orientation and gender identity but be aware that disclosure is an individual process.
- Honor and respect patient’s decisions to provide or not provide sexual and/or gender information.
- All forms should contain inclusive, gender-neutral language that allows patients to self-identify.
- Use neutral and inclusive language when communicating with patients.
- Listen to and respect patients’ choice of language when they describe their own sexual orientation.
- Conduct confidential patient satisfaction surveys that include questions regarding sexual orientation and gender identity.
*Information largely derived from Joint Commission field guide, reference 47.
For more information on best-practices in the workforce, visit the Joint Commission website by clicking here.

Self-Quiz
Ask Yourself...
- Have you ever misused a pronoun, or overheard a co-worker misuse a pronoun in practice? How can you make sure this doesn’t happen again?
Establishing Relationships with LGBTQ Patients
When interacting with patients, one should not assume gender or sexuality. Addressing a patient who identifies as a female as a male can cause grave harm to the relationship. Instead, nurses should use open-ended questions. For example, rather than saying “Hi sir, what brings you to the hospital,” a nurse might say, “Welcome, what brings you to the hospital today (48)?”
If a nurse uses the incorrect pronoun, the best practice is to apologize and ask the patient what pronoun and name they prefer. For example, a nurse may say, “I apologize for assuming your gender. How would you like to be addressed? (48).
In conversation, the nurse should use the name and/or pronoun the patient prefers without drawing special attention to the subject (48). For example, if a male patient prefers to be identified as his partner’s wife, you should follow suit.
The core of relationship-building with LGBTQ patients is no different than any other patient, fundamentally. If nurses have a basic understanding of best practices and a healthy dose of respect and compassion for LGBTQ patients, a positive relationship is likely to develop.

Self-Quiz
Ask Yourself...
- Do you have any biases which may affect the care you provide to LGBTQ patients?
- Have you worked for someone who did NOT demonstrate LGBTQ cultural competence? In what ways could they improve their practice?
Health Disparities of LGBTQ Patients
LGBT Americans are at higher risk of substance use, sexually transmitted diseases, cancer, cardiovascular disease, obesity, bullying, isolation, anxiety, depression, and suicide when compared to the general population (49). LGBT youth are frequently bullied at schools (49). In fact, early victimization and subsequent emotional distress accounted for 50% of the disparities between LGBT youth (49). In other words, LGBT Americans are discriminated against and disadvantaged from a very young age.
When home life also reflects a lack of LGBTQ cultural competence, more problems arise. A major cause of LGBT distress is family rejection. Disclosure of gender identity or sexuality can cause very significant interpersonal conflicts among family and friends of LGBT persons (49). This explains some hesitancy and should help nurses understand the importance of respecting privacy, while giving options to patients about disclosing sexuality and gender.

Self-Quiz
Ask Yourself...
- Are there any circumstances in which your current hospital’s policies could discriminate against LGBTQ families?
- If so, how would you begin to work with leadership to change those policies, so they reflect LGBTQ cultural competence?
Providing an Inclusive and Accepting Care Environment
LGBTQ patients often experience difficulty in finding healthcare environments in which they feel accepted and understood (48). Past negative experiences, lack of knowledge among healthcare providers, and limited access to healthcare in general may become major barriers for LGBTQ persons when seeking care (48).
The core tenant of providing an inclusive environment is understanding the needs of LGBTQ patients and working diligently to create an environment which does not disadvantage or discourage them from seeking care.
Policies and procedures at institutions should be designed to reflect a non-discriminatory environment. For example, many hospital policies dictate that only legal family spouses or partners can visit in specific circumstances. Policies such as this are inherently discriminatory toward LGBTQ patients, as they may not have legal spousal status due to social, legal, or personal reasons.

Self-Quiz
Ask Yourself...
- Are there any circumstances in which your current hospital’s policies could discriminate against LGBTQ families?
- If so, how would you begin to work with leadership to change those policies, so they reflect LGBTQ cultural competence?
Exercises on LGBTQ Cultural Competence
To help solidify your learning, please complete the following exercises at your own pace. The answers/guidance for each are provided below.
Scenario 1
A patient enters your emergency department, and you assume the patient identifies as a female. You introduce yourself and say, “Ma’am, how can we help you? What brings you in today?”
The patient appears dismayed but answers the question. The nurse is confused and does not understand why the patient appears distressed. What is the best course of action?
Answer: The nurse should apologize to the patient and ask the patient how they would like to be addressed. Then, the nurse should update the patient’s records to reflect such, to reduce further confusion.
If the nurse does not address the issue, the patient may feel uncomfortable and develop a negative association with healthcare, which can lead to disparities in the future.
Scenario 2
A patient in your ICU has had a deterioration while his husband was in the room. After a family meeting, a member of the healthcare team makes a derogatory remark about the patient’s sexuality. What is the next best action for the nurse?
Answer: Pre-conceived phobias and stigmatizations can cause significant distress to LGBTQ patients, even if not stated directly to them. These types of remarks are abusive and should not be tolerated. The nurse should confront the co-worker (if safe) and consider reporting the comments to the Human Resources department.
Scenario 3
A LGBTQ patient is being admitted and prefers not to disclose their sexuality. However, the nurse is unable to proceed with the admission process without this information. What could be done to rectify this system-level issue?
Answer: The nurse should work with administration to ensure that all charting and paperwork allows individuals to self-report sexuality and/or gender if they want. However, healthcare systems should not force patients to “come out” unless it is absolutely medically necessary.

Self-Quiz
Ask Yourself...
- What information from this course can you take to your facility to encourage a positive change of LGBTQ patients, and create an environment for LGBTQ cultural competence?
Conclusion
LGBTQ cultural competence must be ingrained in our healthcare systems in order to foster excellent relationships between members of the LGBTQ community and medical staff. Hospitals and healthcare systems have a great deal of work to do in becoming LGBTQ-friendly. The efforts must continue until LGBTQ patients and families do not feel disadvantaged, anxious, or frustrated when interacting with healthcare systems. As the patient’s ultimate advocate, nurses are at the front-line and should advocate for patients both individually and from a policy perspective. Nurses should work with and spearhead efforts to ensure that healthcare policies reflect best-practice and do not discriminate against LGBTQ patients in any way.
References
- Waisel DB. Vulnerable populations in healthcare. Curr Opin Anesthesiol. 2013;26(2):186–92.
- Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: Trends over the past 10 years. NCHS Data Brief. 2012;2012(100):1–8.
- Institute of Medicine. Collecting sexual orientation and gender identity data in electronic health records: workshop summary. Washington DC: National Academy of Sciences; 2013.
- Quinn GP, Sanchez JA, Sutton SK, Vadaparampil ST, Nguyen GT, Green BL, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA-Cancer J Clin. 2015;65(5):384–400
- Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–60.
- Dilley JA, Simmons KW, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific northwest. Am J Public Health. 2010;100(3):460–7.
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health. 2013;103(10):1802–9.
- Bauermeister J, Eaton L, Stephenson R. A multilevel analysis of neighborhood socioeconomic disadvantage and transactional sex with casual partners among young men who have sex with men living in metro Detroit. Behav Med. 2016;42(3):197–204.
- Smalley KB, Warren JC, Barefoot KN. Differences in health risk behaviors across understudied LGBT subgroups. Health Psychol. 2016;35(2):103–14.
- Staats C, Capatosto K, Wright RA, Jackson VW. State of the science: Implicit bias review 2016. Columbus: Kirwan Institute.
- Cochran SD, Bandiera FC, Mays VM. Sexual orientation-related differences in tobacco use and secondhand smoke exposure among US adults aged 20 to 59 years: 2003-2010 National Health and nutrition examination surveys. Am J Public Health. 2013;103(10):1837–44.
- Remafedi G, French S, Story M, Resnick MD, Blum R. The relationship between suicide risk and sexual orientation: results of a population-based study. Am J Public Health. 1998;88(1):57–60.
- Charlton BM, Corliss HL, Missmer SA, Frazier AL, Rosario M, Kahn JA, et al. Reproductive health screening disparities and sexual orientation in a cohort study of U.S. adolescent and young adult females. J Adolesc Health. 2011;49(5):505–10.
- Matthews AK, Brandenburg DL, Johnson TP, Hughes TL. Correlates of underutilization of gynecological cancer screening among lesbian and heterosexual women. Prev Med. 2004;38(1):105–13.
- Tracy JK, Lydecker AD, Ireland L. Barriers to cervical Cancer screening among lesbians. J Women’s Health. 2010;19(2):229–37.
- Grossman AH, D’Augelli AR. Transgender youth: invisible and vulnerable. J Homosex. 2006;51(1):111–28.
- Krehely J. How to close the LGBT health disparities gap. Center for American Progress; 2009. p. 1–9.
- Buchmueller T, Carpenter CS. Disparities in health insurance coverage, access, and outcomes for individuals in same-sex versus different-sex relationships, 2000-2007. Am J Public Health. 2010;100(3):489–95.
- Heck JE, Sell RL, Gorin SS. Health care access among individuals involved in same-sex relationships. Am J Public Health. 2006;96(6):1111–8.
- Kamen C, Palesh O, Gerry AA, Andrykowski MA, Heckler C, Mohile S, et al. Disparities in health risk behavior and psychological distress among gay versus heterosexual male Cancer survivors. LGBT Health. 2014;1(2):86–U103.
- Legal L. When health care Isn’t caring: lambda Legal’s survey of discrimination against LGBT people and people with HIV. New York: Lamba Legal; 2010.
- Grant JM, Mottet LA, Tanis J. National Transgender Discrimination Survey Report on health and health care. Washington DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2010.
- Shires DA, Jaffee K. Factors associated with health care discrimination experiences among a National Sample of female-to-male transgender individuals. Health Soc Work. 2015;40(2):134–41.
- Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians’ experiences in the workplace. J Homosex. 2011;58(10):1355–71.
- Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54.
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
- Mereish EH, Bradford JB. Intersecting identities and substance use problems: sexual orientation, gender, race, and lifetime substance use problems. J Stud Alcohol Drugs. 2014;75(1):179–88.
- Torres CG, Renfrew M, Kenst K, Tan-McGrory A, Betancourt JR, Lopez L. Improving transgender health by building safe clinical environments that promote existing resilience: results from a qualitative analysis of providers. BMC Pediatr. 2015; 15:187.
- Burke SE, Dovidio JF, Przedworski JM, Hardeman RR, Perry SP, Phelan SM, et al. Do contact and empathy mitigate Bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. 2015;90(5):645–51.
- Sabin JA, Riskind RG, Nosek BA. Health care Providers’ implicit and explicit attitudes toward lesbian women and gay men. Am J Public Health. 2015;105(9):1831–41.
- Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–7.
- Wilson TD, Brekke N. Mental contamination and mental correction: unwanted influences on judgments and evaluation. Psychol Bull. 1994;116(1):117–42.
- Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit Bias in health care: a narrative review. Group Process Interg. 2016;19(4):528–42.
- Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102(1):4–27.
- Van Ryn M, Saha S. Exploring unconscious bias in disparities research and medical education. JAMA. 2011;306(9):995–6.
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74(6):1464–80.
- Nosek BA, Riskind RG. Policy implications of implicit social cognition. Soc Issue Policy Rev. 2012;6(1):113–47.
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
- Shavers VL, Fagan P, Jones D, Klein WMP, Boyington J, Moten C, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953–66.
- Chapman EN, Kaatz A, Carnes M. Physicians and implicit Bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–10.
- Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: Confronting racial and ethnic disparities in health care. Brian D. Smedley, Adrienne Y. Stith, and Alan R. Nelson, Editors; Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Board on Health Sciences Policy; Institute of Medicine. Washington, DC; 2003.
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41.
- Greenwald AG, Banaji MR, Nosek BA. Statistically small effects of the implicit association test can have societally large effects. J Pers Soc Psychol. 2015;108(4):553–61.
- Khan A, Plummer D, Hussain R, Minichiello V. Does physician bias affect the quality of care they deliver? Evidence in the care of sexually transmitted infections. Sex Transm Infect. 2008;84(2):150–1.
- Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P. (2019). Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC medical education, 19(1), 325. https://doi.org/10.1186/s12909-019-1727-3
- Human rights campaigns. Glossary of terms. Retrieved from https://www.hrc.org/resources/glossary-of-terms
- Advancing Effective Communication, Cultural Competence, and Patient– and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community, a field guide. Joint Commission. Retrieved from https://www.jointcommission.org/ /media/enterprise/tjc/imported-resource assets/documents/lgbtfieldguide_web_linked_verpdf.pdf?db=web hash=1EC363A65C710BCD1D4E14ED120CB2
- Delivering culturally sensitive care to LGBTQI Patients. The Journal for nurse practitioners. Volume 13, issue 5 p342-347.
Following a DNR: An Ethical Dilemma in Nursing
Introduction
End-of-life issues are often full of emotion and difficult to deal with for all involved. Do-not-resuscitate (DNR) orders can present many moral and ethical dilemmas in nursing. It takes the entire healthcare team, including the patient and their family, to ensure that all final wishes for the patient are followed. In order to understand this ethical dilemma in nursing, we must first define what ethical dilemmas are and what a DNR order is.
What is an Ethical Dilemma in Nursing?
Ethics are a system of moral principles or rules of conduct recognized by a particular group; however, the American Nurses Association (ANA) has developed its own code of ethics (1). The ANA Code of Ethics with Interpretive Statements includes nine provisions that direct a nurse’s moral and ethical practice, it reads:
Provision 1: The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
Provision 2: The nurse’s primary commitment is to the patient, whether an individual, family, group, community, or population.
Provision 3: The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
Provision 4: The nurse has authority, accountability, and responsibility for nursing practice; makes decisions; and takes action consistent with the obligation to provide optimal patient care.
Provision 5: The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
Provision 6: The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
Provision 7: The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
Provision 8: The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
Provision 9: The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy (2).
An ethical dilemma in nursing arises when decisions are made that go against the ANA Code of Ethics with Interpretive Statements.
It is important to note that the nurse’s main duty is to be an advocate for their patient, meaning that all actions should be in the patient’s best interest. Adhering to this principle will ensure a clear moral path where ethical dilemmas in nursing can be avoided.

Self-Quiz
Ask Yourself...
- What is an ethical dilemma in nursing?
- Thinking of your own practice, have you ever had to make choices that compromised your personal ethics or breached the ANA code of ethics?
- Can ethical issues be completely avoided?
DNR
A DNR is an order written by a physician that is usually given to those who are critically or terminally ill. The order states that in the event of cardiopulmonary arrest, should the patient’s heart stop or should they stop breathing, cardiopulmonary resuscitation (CPR) will not be administered. The decision for a DNR order is always discussed with the patient if they are conscious and have the capacity to make informed decisions. Should the patient be incapacitated, their power of attorney (POA), health care agent, or family member may be allowed to make the decision for a DNR. If a patient is known to be gravely ill, they may already have an existing DNR order, or an advanced directive/living will. Once this document is produced for the institution, the order will go into effect. If a DNR order has been put in place by the patient and physician, the family should not have the power to lift the order once the patient deteriorates and can no longer make decisions (3).
There was a time in the history of healthcare when there were different tiers of a DNR order. For example, there used to be a medication only/chemical code where medication could continue to be administered, but no compressions or artificial respirations could be performed by the healthcare team; in the end, this proved to be a wasted effort as the medication would be circulated and provide no effect. Many institutions have gotten away from the tires of DNR; what I mean by this is, either there is a DNR order in place for a patient, or there is not.

Self-Quiz
Ask Yourself...
-
Have you ever initiated a DNR order?
-
Have you ever been in a situation where a patient’s family or healthcare team did not agree with the DNR?
-
What is a DNR order?
Ethical Dilemma in Nursing: DNR
If a DNR order is put in place by the physician in conjunction with the patient, how could there possibly be any ethical dilemmas in nursing? There should be no problems associated with a DNR order; however, ethical dilemmas arise when the team (patient, physician, healthcare workers, and family) are not all on the same page regarding the DNR. One of the main problems is that different healthcare workers have different interpretations of what a DNR means. It must be understood that a DNR means “do not resuscitate,” and does not mean “do not treat.” To better explore the ethical dilemmas in nursing associated with a DNR order, we will look at scenarios that I have come across over my 25 years of nursing:
Scenario 1
A patient is sent from a telemetry unit to radiology for a CT scan. The patient has severe cardiomyopathy and requests a DNR upon admission. The order is noted on the patient’s chart. When they are sent to radiology for the scan, the floor nurse neglects to place the code status on the patient hand-off form. During the scan, the patient becomes unresponsive, and a code blue is called; CPR is initiated, and the patient is intubated.
During the resuscitation, it is discovered that the patient has a DNR order. The physician running the code continues with CPR, rationalizing that he could ‘not just stop’ the life-saving measures that they had already begun. The patient is revived and transferred to the ICU. Later, during the admission, the family withdraws life support, and the patient expires.
In this first scenario, we can see that a communication error led to the DNR order not being followed. Once discovered, the physician in charge refused to comply with the order. Ultimately, the patient passed after a few days on life support.
This ethical dilemma came to play once the code team realized that the patient had a DNR. The code could have been stopped at this point, and the lead physician could have spoken with the patient’s family to explain what had occurred. Many facilities do have policies in place where if a patient goes for a procedure/surgery, the DNR order may be on hold during the time that they are in the procedure; this does not generally include diagnostic scans.
Scenario 2
A G-tube is ordered for a terminally ill cancer patient. The patient is unable to eat and needs a G-tube for nutrition and medication administration. When the gastroenterologist comes in to do the consult, he discovers that the patient has a DNR order. He refuses to place the G-tube due to the DNR order and claims that the G-tube is a ‘life-saving’ measure. The patient is sent back up to their room without having the G-tube placed. After two days, a second consult is placed, and a different doctor approves and places the G-tube.
The ethical dilemma in this scenario is that the provider refuses to provide treatment based on a poor understanding of what a DNR really means. Again, DNR does not mean “do not treat.” There are many procedures that can and should be performed regardless of a patient’s code status. Though a G-tube can prolong someone’s life, it also serves as a means to keep them comfortable through both nutrition and the administration of needed medications, including analgesics. A G-tube insertion can ultimately assist the patient to die with dignity by allowing them to receive alimentation and medicines. It is not solely the provider’s responsibility to decide what measures are heroic and which are not. The entire multidisciplinary healthcare team should be involved in the care of the patient, especially when questions could arise as to if a certain procedure is ethical.
This scenario led to a peer review of the provider’s actions.
Scenario 3
A patient, along with his healthcare team and family, has decided to enact a DNR order. He has been gravely ill for a long time and wants “nature to take its course.” After the DNR order was placed, one of his daughters arrives from out of town; she does agree with the DNR order and wants it to be revoked. The patient refuses, and the DNR is left in place. The next day, the patient becomes unresponsive while the daughter is in the room. She insists that the nurse begin CPR and threatens legal action if the code blue is not started immediately. The nurse becomes intimidated by the daughter, as she does not fully understand the DNR order, and commences the code blue.
The patient is revived and is transferred to the ICU. He voices his anger to the healthcare team that his wishes were not followed; CPR was not to have been administered. Three days later, he becomes unresponsive and expires; however, this time CPR was not administered, and the DNR was followed.
Once again, the ethical issue occurred due to misunderstandings and a lack of knowledge from both the patient’s family and the healthcare team. The patient’s daughter sought to go against her father’s explicit wishes to cancel the DNR. When he would not, as soon as he became unresponsive, she demanded that the staff perform CPR. The nurse should have refused, as this daughter was not the legal decision-maker, and the patient’s expressed wishes were known prior to him falling unresponsive; instead, the nurse breached the DNR and performed life-saving measures.

Self-Quiz
Ask Yourself...
-
In your nursing practice, have you ever come across an ethical issue involving a DNR order?
-
In the three scenarios, what was the cause of the ethical issues?
-
Could these ethical issues have been avoided?
Conclusion
A DNR order is put in place when a patient does not want life-saving measures to be performed. The healthcare team and family are involved in the decision-making process, but the decision ultimately belongs to the patient. A patient with a DNR order still needs to be treated for their medical problems and, like any other patient, needs to be treated with dignity and respect. It is important that the healthcare team understands what the DNR encompasses and who can make decisions for the patient should they deteriorate. The nurse must always do what is best for the patient and follow the ANA Code of Ethics with Interpretive Statements.
References
-
Ethics. (2021). Retrieved from https://www.dictionary.com/browse/ethics
-
ANA. (2021). Retrieved from Ethics and Human Rights: https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/
-
Dugdale, D. C. (2020, January 12). Do-not-resuscitate order. Retrieved from MedlinePlus: https://medlineplus.gov/ency/patientinstructions/000473.htm
Effective Communication in Nursing
Introduction
Communication in nursing is key, and the ability to communicate effectively can be our lifeline. We depend on ourselves and others to be fluent and effective in the art of communication in order to perform our role as nurses successfully. When any link in our communication chain fails, we immediately see poor outcomes, wastage of resources, reductions in patient and staff satisfaction as well as a decline in the quality of patient care (1).
Types of Communication
In order to master effective communication in nursing, it is important to understand the various types of communication, their definitions, and the impact they can make.
Non-Verbal
This form of communication relies solely on the utilization of body language, including body and facial mannerisms, and completely lacks spoken words or sounds (2). We perform and identify non-verbal communication in nursing daily without giving it a second thought. We may see a newborn sucking on their hands, providing us a non-verbal cue that they are hungry. When assessing a patient holding their abdomen, we would look to initially target that area because they have communicated (non-verbally) that this is where they are experiencing discomfort. Smiling when the next shift nurse is walking in the door communicates to them that you are happy to see them, and that it’s about time for you to go home!
Since we perform non-verbal communication so often, it can become an incredibly powerful tool or an extremely negative one. This form of communication in nursing can be used positively to show our patients and co-workers that we have compassion, and we are engaged. Negative forms can make patients uncomfortable with sharing their medical history and result in a lower quality of patient care. Additionally, it can lead to dysfunctional teamwork among staff.
Verbal
Verbal communication occurs when we use words or sounds to discuss concepts with others (2). This form of communication in nursing has the conception to be a very easy notion, but it can create unfavorable consequences when used ineffectively. In order to produce clear verbal messages, we should always speak concisely and with confidence. As health care professionals, we have our own language, and understanding when to incorporate our medical jargon into conversations versus when to not is crucial in providing care. When communicating among co-workers, our medical knowledge can display professionalism and it is evident that they can follow along. However, when speaking with patients and their families, this may not always be the case and we must be able to effectively gauge our audience and ensure that they have a clear understanding of what we are teaching or explaining; this is an extremely valuable tool.
Written
This form of communication can be either a formal or informal transcription of words that are intended to serve as a direct communication form (2). Written communication in nursing is used daily and incorporates one of our most important duties, documentation. Throughout our nursing practice, we have learned the importance and necessity of our documentation; it can be useful for legal protection or provide critical data to other health care professionals. Written communication can also be accessed through the policies and procedures we employ to perform various tasks. Having sound, written communication, and interpretation skills is vital to the overall success of our nursing career.

Self-Quiz
Ask Yourself...
- What type of communication is being interpreted while watching a patient walk to the bathroom?
- Upon admission of a female patient for a fall, you are performing normal intake questions and a physical assessment. The patient is quiet and uses minimal verbal communication and looks down at the floor while you are in the room. What communication types are you interpreting?
Receiving Communication
The most common communication perception is usually directed to producing communication through non-verbal, verbal, or written forms. While the production of communication is important, the reception of it potentially holds even greater value. In nursing, ensuring our communication is received correctly affects every clinical, orientation, or job experience we have encountered thus far. Think about it…
- Taking notes in class or during a shift.
- When a preceptor or instructor educates you on a brand-new skill or piece of equipment.
- Teaching your patient, family, or student about a new diagnosis.
- Watching your patient breathe for rate, depth, and effort.
We must provide and receive communication in nursing through verbal, non-verbal, or written forms successfully. If communication fails, we will experience extremely negative effects throughout our entire nursing system.
Hearing & Listening
Hearing describes the process or act of perceiving sounds or spoken words (2). We hear sounds upon auscultation, varying frequencies of alarms, and patient concerns when they are voiced. Hearing all these sounds are heavily dependent on how they are used. To achieve successful implementation of these sounds, we must also listen to these sounds and words. To listen, we must hear and then interpret these sounds carefully (2). We interpret these sounds and words by asking additional questions, performing additional assessments, or paraphrasing the information presented.

Self-Quiz
Ask Yourself...
1. What is the best way to ensure a patient was actively listening while performing patient education?
2. Which type of scenario requires active listening skills?
a. Putting blood tubing into a pump.
b. Watching an EKG monitor.
c. Performing a pain assessment.
3. What techniques show others you are actively listening?
a. Reading a document while being talked to.
b. Making eye contact.
c. Making noises while someone is talking.
Communication Transmission Threads
Communication in nursing occurs multiple times a day between a wide range of communication threads. The type of communication through non-verbal, verbal, and written communication produced and received, must be effectively performed. Success and implementation are heavily dependent on the communication between the nurse and the communication thread.
Nurse-Nurse
Communication among nurses is continuous throughout a shift while working within a team environment. Whether it is us passing our documentation on to another nurse for review or vice versa, there is consistent communicative flow of all variants (non-verbal, verbal, and written) between the team in order to provide care for patients.
Nurse-Ancillary Staff
Your team members will vary depending on your nursing career setting, but some items will remain consistently important despite wherever you are. We must provide clear verbal communication when delegating or reporting critical information from the nurse to ancillary staff participating in patient, client, or resident care.
Charge Nurse-Team
When stepping into a charge nurse role, there will always be unexpected tasks, staff conflicts, or emergent situations. In this position, you will be taking all the communication skills you have acquired and putting them into practice at an all-time high. As the charge nurse, you will be viewed as a leader, meaning that you are a role model for your fellow team members. Now, in addition to producing and receiving communication effectively, you will now be identifying poor communication and assisting with its correction.
Nurse-Patient
The nurse-to-patient communication thread is one of the ultimate and most important exchanges in the nursing profession. Patients need us, so we must be able to keep consistent and effective communication flow with them because any assessment, report, and administration of medication is contingent upon it.
Nurse-Family
The thread between the nurse and the patient’s family can be the foundation for your nurse-to-patient communication and its effectiveness. The family could be the responsible party or guardian for your patient and could potentially serve as your sole historian for patient information if the patient is unable to communicate at the time of data collection. Ensuring that the family is aware of and understands discharge instructions can further help them to recognize any potential signs or symptoms that could result in calling a physician or visiting the emergency room in the future.

Self-Quiz
Ask Yourself...
- Which of the following is a beneficial way to ensure effective communication throughout multiple threads?
- One to one conversation.
- Reviewing a policy.
- Bedside report.
Barriers & Improvements to Communication
Barriers of communication in nursing happen frequently and are sometimes out of our control. These barriers include:
Language barriers
Utilizing available resources for language barriers through interpreter staff members or interpretation devices can ensure effective communication pathways between two individuals.
Cultural differences
Identification of cultural differences during admission and cultural awareness will allow for effective communication management throughout each culture you are presented with.
Patient acuity, staffing levels, time constraints
Patient acuity, staffing levels, and time constraints can be improved by utilizing staff huddles and working together with administration in order to overcome conflicts.
Emergent situations
Emergent situations that arise during your shift can be relieved through adequate knowledge of the policies and procedures and by performing debriefs after the situation resolves. Debriefings hold valuable insight into reflections of the emergent situations we face as nurses, especially on communication performance.
In each thread and form of communication in nursing, we must remember the following items to receive information. While producing communication, we must always be clear, concise, and accurate with the correct corresponding tone when expressed to others. When we are receiving the information, we must ensure we are understanding, investigating, and acting according to the communication presented to us. Utilizing various communication platforms, including emails, boards, and group messaging apps, can help to assist in ensuring education is received.
Benefits of Effective Communication in Nursing
When we achieve effective and therapeutic communication between both our team and patients, it will create opportunities for enhancements throughout our practice. Fostering a unity of teamwork with co-workers will increase satisfaction and reduce burnout rates. Reduced health care costs through reduced readmissions or emergency room visits will be established by successful patient education and understanding. Our quality of patient care will be heavily influenced by the nursing communication threads created through their care.
References
- Dictionary by Merriam-Webster: America’s most-trusted online dictionary. (n.d.). Retrieved February 22, 2021, from https://www.merriam-webster.com/
- Effects of poor communication in healthcare. (n.d.). Retrieved February 22, 2021, from https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare/?amp
Flu Treatment, Symptoms, and Red Flag
Introduction
Every year, emergency waiting rooms, outpatient clinics, and inpatient hospital beds fill up with patients seeking treatment for the miserable symptoms brought on by the influenza virus. This illness does not discriminate and afflicts all ages, from young babies to the elderly, and everyone in between. Symptoms can range in severity from several days of fever, chills, and cough in bed at home, to weeks of hospitalization, respiratory distress requiring mechanical ventilation, and even complications resulting in death.
Starting in October and often lasting well into spring, flu season tasks healthcare workers everywhere with promoting prevention, quickly and efficiently identifying those infected, and appropriately managing symptoms and any secondary complications that may arise. In the last two years, the overloading of the healthcare system with COVID-19 infections has meant hospitals and clinics are even more pressed to provide appropriate staffing, treatment, and medical resources to people affected by influenza.
An illness affecting the population on such a large scale requires healthcare professionals to stay up to date on disease trends, diagnosis and treatment protocols, and “red flags” of more serious cases in order to minimize the impact of flu season and keep complications and mortality as low as possible.
This course will review disease trends in recent years, common and more insidious symptoms to help identify flu infections, available testing methods and their accuracy, pharmacologic treatments and the importance of their timing, supportive treatments and symptom management, and the “red flags” of dangerous secondary infections and complications.
Upon completion of the course, the reader should be comfortable participating in prevention, identification, and management of the seasonal influenza virus.
Current Practice, Barriers and Need for Continued Education
Influenza is a serious global issue that has been affecting humanity since the beginning of recorded history. Despite medical advances in recent years, flu remains a major public health concern, with up to 20% of the US population being affected annually (13).
Between 140,000 and 710,000 people are hospitalized nationally each year, with around 52,000 deaths. Those most at risk are young children, those over age 65, and those with other chronic or underlying conditions such as asthma, diabetes, immunosuppression, etc.
Despite high rates of infection and risk of complications, the estimated annual vaccination rate amongst the general population remains at about half, 50.2% for adults (3) and 58.6% for children for the 2020-2021 flu season (4). There is an increased rate of vaccination amongst healthcare workers (78.6%), but as these are the people most likely to come in contact with and spread the virus, even that number could be improved upon (6).
Further complicating the situation, influenza virus has several strains and possesses the ability to change its DNA (referred to as “drift and shift”) as it replicates, making it difficult to produce a highly accurate vaccine (2). Because of this, vaccines cannot be created far in advance if the most current strain is to be targeted. Vaccine shortages can result if new vaccines are not created at a fast enough rate throughout flu season (6).
There are antiviral medications available for prevention and treatment of flu, however this requires proper identification of those infected or most at risk for infection, and the administration of these medications is typically time-sensitive (5). Health care professionals should be familiar with common symptoms of flu and be comfortable assessing patients, testing for and diagnosing flu.
All these considerations for flu illustrate the intense need for educated, proactive health care workers to promote vaccines, quickly identify those most at risk or with active infections, and treat effectively to keep the impact of flu minimized.
The National Institute of Health has ongoing projects to keep available resources robust (14), but this research is only as strong as the health care professionals who implement it and are on the front lines of patient care. Staying up to date on current practice is paramount for national and global management of this resilient pathogen.

Self-Quiz
Ask Yourself...
- Do you think that the current rate of vaccinations among healthcare providers (78.6%) could be improved?
- With up to 20% of the US population being affected annually, do you think enough resources are utilized in the prevention, recognition, and treatment of influenza?
- What could be done from a national, state, and local level to promote increased prevention, recognition, and treatment of influenza?
What is Influenza?
Viruses are small pathogens containing genetic material that infect host cells and replicate within that host. They can exist for short periods of time outside of a host as an infectious virion and are spread between hosts through a variety of ways. Influenza is a specific group of RNA viruses that replicate within the epithelial cells of the respiratory tract (15).
There are three main types of flu viruses (A, B, and C). Viruses B and C typically only exist in humans, but A has been found in other mammals such as pigs and horses (15). There are also subtypes of each virus, depending on specific structure of the virus; these are labeled as H1-16 and N1-9 for hemagglutinin and neuraminidase, however, further discussion of these is beyond the scope of this course (15).
As the virus replicates within host cells, there can be subtle changes to the RNA over time, eventually adding up to more noticeable changes and resulting in these different subtypes. These slow changes are referred to as antigenic “drift” and are part of why creating a highly accurate flu vaccine is so difficult (2).
Typically, viruses that have drifted some are still susceptible to the current vaccine or there is some acquired immunity within the population. However, there is sometimes a more dramatic structural change referred to as antigenic “shift” that results in a completely new viral subtype and a population with virtually no immunity to this new agent (15). This can result in serious infection of pandemic proportions, such as the 2009 H1N1 outbreak (15).
Influenza viruses are typically spread through droplet transmission, when an infected person spreads microscopic drops of bodily fluids, typically through sneezing or coughing, which then encounter another susceptible person (8). These droplets usually only travel across air distances of 6 feet or less, however they can be transferred further via indirect contact such as handshaking or by vectors (surfaces or objects where virions survive temporarily while waiting on contact with the next host) (8).
Once a host touches a contaminated vector and then touches their own mucous membranes (nose, mouth, eyes, etc.), they can become infected. Other bodily fluids such as loose stools, vomit, and sputum can contain viral RNA and contribute to disease spread (8).

Self-Quiz
Ask Yourself...
- The typical point of replication for influenza is upper respiratory tract, more specifically the nares.
- How does this correlate with influenza symptoms?
- As you can see, influenzas are spread via many modes. How will you use this information to better protect yourself and patients from influenza infection?
Prevention: Flu Vaccines
Once pathogenicity is understood, providers are better able to prevent spread of infection. The primary and most effective way to help prevent the spread of flu is through a high rate of vaccination in the general population. Current recommendations are for all individuals 6 months of age and older to receive a vaccine unless otherwise contraindicated (8).
It is especially important that those most at risk (children under age 2, adults older than 65, and those with comorbid conditions) and those working with high-risk individuals (healthcare and childcare workers) receive vaccines.
For the optimum protection, the goal for vaccine timing should be by the end of October, keeping in mind that full antibody production takes about two weeks after the vaccine is received. Though early vaccination is ideal, a flu vaccine can be administered at any point during flu season and patients requesting immunization later in the season should still be vaccinated (8).
The first-time children between 6 months and 8 years of age receive a flu vaccine, they will need 2 doses, 4 weeks apart (8). After receiving 2 doses, children only need 1 dose for all subsequent flu seasons (8).
There are some individuals who should not receive a flu vaccine, but this group is typically small. Among those who are absolutely contraindicated are infants under 6 months of age and anyone with a previous life-threatening reaction to a flu vaccine (6).
It was previously thought that anyone with an egg allergy should not receive the vaccine, since the viral components are grown in an egg medium, however most recent recommendations suggest that this does not cause a reaction for most people and should be reviewed on an individual basis with one’s own primary care provider (6).
Anyone with a history of Guillain-Barré Syndrome should also consult their provider and may be advised to omit the vaccine. Patients with a current cough or cold accompanied by fever may be advised to postpone the vaccine until their symptoms have resolved (6).
Each year, the Centers for Disease Control and Prevention (CDC) study two factors of the current flu vaccine, efficacy and effectiveness. Randomized controlled trials are used to study efficacy, or the intended result, of the vaccine in optimal conditions with healthy participants (6). Less formal observational studies are used to study effectiveness, or how well the vaccine is working in the “real world.”
As previously discussed, antigenic drift and shift mean that the annual vaccine is imperfect and does not always prevent illness as well as intended. For a general idea of the typical effectiveness, we can look at data from recent years: the vaccine was shown to be 38%, 29%, and 39% effective in 2017-2018, 2018-2019, and 2019-2020 flu seasons, respectively (12).
Regardless of the lower levels of effectiveness compared to other vaccines, such as MMR, vaccination against flu can still prevent substantial numbers of illness and death when considering the population of the United States.
There are a few side effects to be aware of and to include in patient education with administration of flu vaccines. The most reported side effect is local soreness around the injection site. This occurs in about 65% of patients vaccinated, does not typically interfere with activity, and resolves within a week (6).
More systemic symptoms such as fever, headache, and malaise are sometimes reported, but interestingly these symptoms are reported at similar rates in patients who received a placebo vaccine (6). Rarely, an allergic reaction can occur, ranging from urticaria to anaphylaxis.
Children under age 2 are at a slightly increased risk of febrile seizures, particularly if a flu vaccine is given in combination with Prevnar and DTaP vaccines, therefore timing of routine vaccines in conjunction with a seasonal flu vaccine should be discussed with parents of young children (6).
Though the actual correlation is unclear, there is also a suggested link between flu vaccines and the extremely rare condition of Guillain-Barre Syndrome (GBS). This often-life-threatening paralytic condition occurs in about 1-2 people per 100,000 each year, regardless of flu vaccine status.
Ongoing research indicates it is unlikely flu vaccines directly cause GBS and that other triggers such as recent viral illness are more likely to be the culprit, but the CDC estimates there may be a 2 per 1 million chance of experiencing this complication after receiving a flu vaccine (6).

Self-Quiz
Ask Yourself...
- How would you react if a patient refused the influenza vaccine due to potential side effects?
- What education would you provide?
Standard Precautions
In addition to vaccines as the front line of disease prevention, there are multiple ways to help slow or prevent the spread of disease once flu season starts.
Hand hygiene and cough etiquette are amongst the most effective measures to prevent spread of illness (1). These steps are easy and can be followed by anyone, regardless of if they are ill or not.
Avoid touching your mouth and nose. When coughing or sneezing, use a tissue to cover your nose and mouth and then dispose of the tissue and wash your hands. Handwashing should be done with soap and water or alcohol based hand sanitizer (9). In addition to standard precautions during flu treatment, anyone with respiratory symptoms and/or fever is encouraged to wear a surgical mask, a recommendation that was in place prior to more widespread masking with COVID-19 pandemic.
Hospitals and clinics can help stop the spread of infection by separating well patients from those with respiratory symptoms (1). People who are ill should not attend work or school and should limit their contact with well people as much as possible while symptoms are present (9).
Infected individuals are considered contagious 1-2 days before showing symptoms and up to a week after illness begins; they should be fever free for 24 hours before returning to work/school (9).
Recognition and Treatment of Flu: Symptoms
Despite prevention efforts, hundreds of thousands of people nationwide will contract the influenza virus each season.
When prevention efforts fail, the next major step is early identification. It is important for all healthcare workers to be familiar with the symptoms of flu and be able to identify quickly and accurately those with a probable diagnosis of flu.
Typical influenza infections start suddenly with a combination of fever, headache, sore throat, fatigue, nasal congestion or runny nose, body aches, and chills.
Fever and acute symptoms can last more than 7 days, with fatigue and weakness lingering for weeks. While fever is typical of influenza infection, not all who are infected present with a fever (15).
Testing for Influenza
It should be noted that patients with suspected flu can be treated purely based on clinical presentation and regional flu trends at that time; rapid flu tests do not have the highest sensitivity and therefore should not be the determining factor in regard to the necessity of treatment. However, there are several methods of testing for flu that can help confirm a suspected diagnosis of flu.
There are two main types of testing for flu, molecular assays and antigen detection tests. Molecular assays work by identifying viral nucleic acids or RNA in a respiratory specimen (7). They are sensitive and specific, meaning they can detect the virus at extremely low levels and the risk of false positive is very low.
There are rapid molecular assays that can result in as little as 15 minutes, identifying flu A or B, and there are also Reverse Transcription-Polymerase Chain Reaction (RT-PCR) and nucleic acid amplification tests available which take closer to 45 minutes to an hour for results and can identify specific subtypes of flu for a more in-depth diagnosis (7). Antigen detection tests are typically used in outpatient settings due to their cost effectiveness and rapid results (10-15 minutes) These rapid tests are up to anywhere from 50-70% sensitive and have specificity >90% (7).
While more accessible to the clinic setting, antigen detection tests are less accurate and a negative result does not exclude a diagnosis of flu. In cases where flu is highly suspected and a rapid test result is negative, the result can be confirmed with a molecular assay or treatment can be started based on clinical presentation and a presumed false negative test result (7). Other illnesses such as COVID-19 may need to be ruled out or a simultaneous infection confirmed as well.
In fact, where high risk populations are concerned, such as asthma, heart disease, immune disorders, and other comorbid conditions, prompt treatment when flu is suspected may be recommended regardless of testing results (7).
Viral cultures are also available for the most in-depth results. While not practical for the clinical setting due to long result windows (3-10 days), viral cultures offer extremely detailed and useful information about the genetic details of current flu strains which is helpful when developing the next year’s vaccine (7).

Self-Quiz
Ask Yourself...
- Which patients are at highest risk of influenzas complications, including death?
- Is it justified to treat these individuals based on positive clinical symptoms even with a negative rapid test? Is it justified to treat them after 48 hours?
“Red Flags” – Potential Complications and What Not to Miss
Most flu cases make a full recovery after 1-2 weeks of illness, however there are some more serious complications that can develop, including life-threatening symptoms and even death (11). Flu can sometimes trigger systemic inflammation, leading to myocarditis, encephalitis, rhabdomyolysis, or multi-organ failure.
These conditions can be difficult to diagnose if suspicion is not high. Flu infections attack the usual defenses of the respiratory tract and predispose the body to secondary bacterial infections like pneumonia.
The body’s initial inflammatory response is beneficial to help the body fight off a flu infection but increasing inflammation or prolonged inflammation puts too much stress on the body and this extreme response can result in autoimmune disorders or sepsis (13). Those with asthma, heart disease, or other chronic conditions are at an increased risk of complications, as are young children and the elderly (11).
Post-influenza pneumonia is a well-described phenomenon, and the most common causative pathogen is Methicillin-resistant Staphylococcus Aureus (MRSA). This secondary infection should be considered in patients with respiratory symptoms and/or sepsis after a recent resolution of flu followed by returning or new/acute symptoms. It is important to consider MRSA as a causative agent when prescribing antibiotics to patients with post-influenza pneumonia (15).
“Red Flags” or warning signs that the body is working too hard to deal with the flu virus or is not compensating well include fast respiratory rate or difficulty breathing, cyanosis, tachycardia, hypotension, chest pain, dizziness, confusion, decreased urine output (>8 hours), severe muscle pain, or seizures. In children, fever >104 (or any fever in children <12 weeks of age) and retracting are concerning signs.
Any other signs/symptoms that are concerning or seem to be worsening warrant further workup and hospitalization to prevent further decline (11).

Self-Quiz
Ask Yourself...
- Have you ever seen a patient who displayed “red flags”?
- How would this change the patient’s management and what type of treatment / monitoring would they need?
Case Study 1
This case study involves a real patient’s experience with seasonal flu. Names, genders, ages, and some details have been changed to protect patient information.
Jennifer is a 35 year old female who presents to an urgent care clinic in mid February with 2 days of rhinorrhea, cough, sore throat, body aches, and tactile fever. She has not received a flu vaccine this season. Recent medical history significant for COVID-19 infection six weeks ago. Following triage, her vitals are recorded as: HR: 110, RR: 22, Temporal temp: 101.3, SPO2: 97%, BP: 110/76.
She is visibly uncomfortable but sitting up on the exam table and able to cooperate and carry on a conversation. She is breathing a little shallowly and has a frequent, coarse sounding cough, but is overall not in any respiratory distress. She is congested and has clear rhinorrhea, eyes are watery, she has some posterior pharynx erythema, no cervical lymphadenopathy, and some faint rhonchi to her lungs that she can clear when coughing.
Rapid strep, flu, and COVID-19 swabs are collected and the results are negative. She is given a prescription for 5 days of 75mg BID TamifluⓇ (oseltamivir) which she fills and begins taking that afternoon. A viral culture is collected from her via nasopharyngeal swab for confirmation of suspected influenza.
Within 3-4 more days, Jennifer is fever free and beginning to feel better despite some persistent fatigue. She works from home until her fever has resolved and cough is improving. She makes a full recovery without sequelae. Three days later her viral culture indicates she has type B influenza, despite her negative rapid influenza test. This is a typical case of influenza, and the Tamiflu may have hastened her recovery and prevented severe illness. It also illustrates that rapid influenza testing has a low sensitivity and per CDC guidelines treatment may be based on clinical signs and symptoms.
Case Study 2
This case study involves a real patient’s experience with seasonal flu. Names, genders, ages, and some details have been changed to protect patient information.
Braxton is a 9-year-old male who presents to his PCP’s office with sudden onset of high fever (tmax 103), headache, and cough that started that morning. It is December and he has not received a flu vaccine. His vitals are stable.
Exam reveals clear rhinorrhea, erythematous and enlarged tonsils, and frequent barky cough. Rapid strep and COVID-19 tests are negative, but a rapid flu test is positive for Influenza A. He is given a prescription for tamiflu (oseltamivir), however his parents have some reservations about the medication due to an article they read on social media and decide not to give him the medicine.
They manage his symptoms with analgesics, Gatorade, and rest. About 11 days later he follows up in the office with complaints of persistent fatigue and new complaints of dizziness and abdominal pain. Parents report a syncopal episode at home that morning, prompting today’s visit.
His cough is still present, but better than it was, and he has been afebrile for about 5 days now. He looks very pale and complains of some dizziness as he gets up onto the exam table, his behavior is sluggish. He has some abdominal bloating and tenderness with mild spleen enlargement. He has lost 4 lbs. since his previous visit. Vitals are somewhat concerning: HR: 145, RR: 27, Temporal temperature: 98.8, SPO2: 98%, BP: 90/54.
He seems poorly hydrated, and his overall appearance is concerning so you order some stat labs. Multiple abnormal lab values return, the most critical of which is a hemoglobin of 3.4. He is admitted to the local children’s hospital PICU and treated for hemolytic anemia secondary to viral infection as well as multisystem organ failure.
After multiple blood transfusions and aggressive steroid therapy, he is discharged home after over two weeks of hospitalization with no permanent organ damage.
This case illustrates one of the rare (but potential) complications of the viral influenza infection. It is possible that early antiviral treatment may have avoided this complication and/or minimized it.
Summary
While influenza is an annual problem and can often seem routine or overshadowed by COVID-19, it is still of utmost importance that healthcare professionals stay vigilant in their knowledge of flu treatment and treat each case on an individual basis.
As the front lines for promotion of flu prevention, early identification and treatment of flu, and maintaining alertness for potential complications, health care workers can have the biggest impact on the severity of the current flu season.
Staying up to date on current practice can help reduce overall numbers of infection, rate of complications, and mortality.
References
- Centers for Disease Control and Prevention. (2012). Respiratory hygiene/cough etiquette in healthcare settings. Retrieved from:
- https://www.cdc.gov/flu/professionals/infectioncontrol/resphygiene.htm
- Centers for Disease Control and Prevention. (2017). How the flu virus can change: “drift and shift”. Retrieved from: https://www.cdc.gov/flu/about/viruses/change.htm
- Centers for Disease Control and Prevention. (2021). Flu vaccination coverage, United States, 2020-21, influenza season. Retrieved from: https://www.cdc.gov/flu/fluvaxview/coverage-2021estimates.htm
- Centers for Disease Control and Prevention (2018). Estimates of flu vaccination coverage among children- US 2017-2018 flu season. Retrieved from: https://www.cdc.gov/flu/fluvaxview/coverage-1718estimates-children.htm
- Centers for Disease Control and Prevention. (2018a). Influenza antiviral medications: summary for clinicians. Retrieved from: https://www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm#
- Centers for Disease Control and Prevention. (2018b). Influenza vaccination: a summary for clinicians. Retrieved from: https://www.cdc.gov/flu/professionals/vaccination/vax-summary.htm
- Centers for Disease Control and Prevention. (2018c). Overview of influenza testing methods. Retrieved from: https://www.cdc.gov/flu/professionals/diagnosis/overview-testing-methods.htm
- Centers for Disease Control and Prevention. (2018d). Prevention strategies for seasonal influenza in healthcare settings. Retrieved from: https://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm
- Centers for Disease Control and Prevention. (2018e). Preventing the flu: good health habits can help stop germs. Retrieved from: https://www.cdc.gov/flu/protect/habits/index.htm
- Centers for Disease Control and Prevention. (2018f). Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization
- Centers for Disease Control and Prevention. (2021). Flu vaccination coverage, United States, 2020-21, influenza season. Retrieved from: https://www.cdc.gov/flu/fluvaxview/coverage-2021estimates.htm
Nursing Documentation 101
Introduction
“I just love charting,” said no nurse, ever. If you ask most people why they want a career in healthcare, their response is that they want to help people. They did not want to spend hours in front of a computer clicking boxes. This time-consuming task of documenting in the medical record, or charting, is dull, repetitive, and sometimes disconcerting. It takes time away from being able to provide care for the patient. Yet documentation in the medical record is truly a vital part of patient care.
Nursing documentation fills a significant portion of the medical record. Nurses need make sure what they are adding is accurate and complies with the guidelines set by their facility and the state board. This principle is the same, even though there are differences to be aware of now that the electronic medical record has become the standard.
The Who, What, When, Where, Why, and How
Who:
There are approximately 2.9 million working RNs in the United States, with about 1.6 million working in hospitals (1). Nurses on a med-surg unit typically spend about one-third of their total working hours documenting (2). Considering a nurse on a med-surg floor spends about 2.5 hours per shift charting, that roughly translates into 7 billion hours spent charting each year. And that is only for the nurses!
Every discipline of the healthcare team contributes to the patient’s medical record. These different clinicians may not have the opportunity to report off to one another, and they must refer to the medical record to gather the information they need in order to care for the patient. Even kitchen staff responsible for preparing meals for patients must be able to see the dietary order for the patient. The following are a few examples of the clinicians who contribute to or review the patient’s medical record:
- Medical Team: physicians, nurse practitioners, physician assistants, surgeons, specialists, residents
- Nurses and LPNs
- Medical Assistants, CNAs, patient care assistants or technicians
- Specialty technicians: radiology, anesthesia
- Therapists: physical, speech, occupational, respiratory
- Pharmacists
- Dieticians
- Case managers or social workers
- Coding and billing specialists
- Researchers
What:
The primary purpose of the medical record is to communicate data about the patient and care provided between different members of the healthcare team. The bulk of the medical record is a collection of assessment data obtained from the patient. Details concerning assessments and results from lab tests or radiology comprise a large portion of the data. Assessment data is usually collected on a flow sheet system. Progress notes are written by the medical team or therapists and help to guide the intended plan of care for the patient. This is considered narrative charting. The medical record also includes orders for prescribed medications and treatments from the medical team. The following are typical components found in a patient’s medical record.
- Patient demographics: name, age, gender, contact information, language, and insurance information
- Past medical history: surgeries, chronic conditions, family history, allergies, and home prescriptions
- History and Physical (H&P): this can contain information about admitting diagnosis or chief complaint and narrative of the story leading to admission
- Flowsheet of assessment data: vital signs, head-to-toe assessment, intake and output record
- Laboratory test results
- Diagnostic test results: from radiology or procedures
- Clinical notes: progress notes from the medical team, procedure notes, notes from consulting clinicians, education provided, and discharge planning
- Treatment orders
- Medication Administration Record (MAR)
When:
The medical record should document every interaction the patient had with a member of the healthcare team. An encounter is created upon admission and everything occurring during a particular admission becomes part of the medical record. Phone calls made to patients and/or families may also become a part of the medical record.
Where:
Medical records are stored in various ways depending on their format and the facility. Paper records from small outpatient offices may be kept onsite. Records are now largely kept electronically. This is referred to as the electronic medical record (EMR) or electronic health record (EHR) and consists of Protected Health Information (PHI). They will be stored on a secure server, typically only accessible by authorized personnel.
Why:
The medical record is essential to nursing documentation for several reasons. The primary reason for the medical record is that it allows members of the healthcare team the ability to review and analyze data in order to deliver appropriate care. It allows clinicians to keep track of all the care that has already been completed for the patient. It also provides the patient with a record of the treatment they received for as part of their lifetime medical history. The medical record is used for coding and creating a bill for the services the patient received. Medical records may also be used for reviewing processes and research purposes. Ultimately, it is also a legal document and may be used in a court of law as applicable.
How:
Medical records are in the final stages of evolution from a paper chart to an electronic medical record system (EMR). By 2017, 96% of acute care hospitals and over 80% of physician offices possessed certified health IT (3). This migration of medical records from paper to electronic format was made possible with advances in technology in the last 30 years. The EMR allows members of the healthcare team to access the medical record instantaneously and improves continuity of care. Utilization of the EMR ultimately reduces costs in healthcare (4) and increases efficiency.
While EMR does have some drawbacks, the benefits that it provides are substantial enough that the government has encouraged its adaptation. The Health Information Technology for Economic and Clinical Health (HITECH) Act was enacted in 2009. This program provided tens of billions of dollars in financial incentives for healthcare facilities to adopt an EMR system (5,6).
Privacy and Security
Since 1996, HIPAA, The Healthcare Information Portability and Accountability Act, has been the governing legislation that provides for the privacy protection of medical records. Compliance with HIPAA mandates that anyone who interacts with patients receives training that will ensure that they will maintain privacy for the patient. Part of the HIPAA legislation also allows the patient to request their medical records.
The patient also has the right to request to amend their medical record. Patient permission must be given prior to a third party’s access to their medical record (7). HIPAA legislation was introduced at the advent of EMR technology. A provision of HIPAA provided a framework to ensure privacy of electronic health records (8). However, breaches in security by hackers or cyberterrorists remains a potential threat.
Benefits of EMR:
- Immediate data accessibility and communication of patient status
- Clinicians can view records remotely, analyze the findings, and place orders immediately for faster patient treatment.
- Multiple clinicians can view the chart at one time.
- Records can be viewed easily from previous admissions and/or outpatients visits easily.
- Records can be instantly shared between facilities (in instances of shared systems).
- Reduction in errors
- Errors due to misinterpretation of handwriting in nursing documentation are eliminated.
- Allows for increased safety checks. The EMR can be set to flag missing components of information, tasks that were not yet completed or are overdue, recognize duplicates, and present warnings if documentation has not yet been validated or “signed.”
- Scanning medications is possible with EMR systems to reduce the risk of medication administration errors.
- Assists with appropriate billing by capturing charges of services provided to the patient.
- The EMR can provide reminders for necessity of certain preventative health screenings or vaccines.
- Automatic “signature” of data is completed simply by the user logging in with a unique ID and password. All entries are date and time stamped. If a correction is made, the original data can be accessed.
- Accessing patient EMR is tracked and can be audited to protect patient privacy from unnecessary viewing.
Downsides of EMR:
-
It is expensive to convert records system to an electronic system:
- The initial cost of the EMR software is very expensive
- More work hours must be paid for staff training and coverage of patients during initial implementation of the program
- Maintaining appropriate encryption and cybersecurity technology against viruses and hacking are also a costly component
Computer systems can be temporarily inaccessible, for example when updates and reboots are required. Paper charting is still necessary in the interim.
Template charting has limitations (9). Templates for nursing documentation may not exist for a specific problem and does not accurately reflect the patient’s condition. Atypical patients may have multiple problems or extensive interventions that must be documented in detail.
Templates may also encourage cloned or copied documentation. It creates unnecessary redundancy and at times inaccurate information in the EHR. Some EHR systems are designed to facilitate cloning with such popular features as:
- “Make me the author” to assume the content of another person’s entry
- “Demo recall” of “Duplicate Results” to copy forward vital signs or assessment data
- “Smart phrases” pulls in specific identical data elements
Automated insertion of previous or outdated information through EHR tools, when not modified to be patient-specific and pertinent to the visit, may raise significant quality of care and compliance concerns.

Self-Quiz
Ask Yourself...
- Think about your current charting system.
- How does your medical record system facilitate accurate charting?
- Do you believe that your system is efficient?
- What are some issues with your system that make it difficult to accurately and timely chart nursing care?
The Legal Requirements
If it wasn’t documented, it wasn’t done. Every healthcare practitioner has had this mantra ingrained in them from the very beginning of their career. Nurses are trained to document defensively, that is, if they are taught at all.
In a 2014 study, only 20% of new graduate nurses had received electronic medical record training as a part of their nursing school curriculum (6). It is not uncommon for clinicians to have the tendency to view the medical record as a defense tool against potential legal problems, rather than its more significant role as a communication tool for patient care.
Regardless, accurate and complete documentation is essential. Your career, and more importantly, patient care, depends on it.

Self-Quiz
Ask Yourself...
- Did you receive proper training on documentation in your nursing program?
- How can programs be improved to better prepare nurses?
When Documentation Becomes Your Defense
In the dreaded event of a legal problem, medical records will be scrutinized to every detail. It is usually the primary source of evidence for the case. A malpractice lawsuit requires four elements to be proven (10):
- That a medical professional assumed a duty to provide care for the patient.
- The clinician failed to provide appropriate care within their scope of practice for the patient.
- The failure in appropriate care caused an injury to the patient.
- The injury resulted in damage to the patient.
Potential legal problems that may arise include the following (11):
- Administrative liability – Professional licensure discipline and/or discharge (firing) from position.
- Civil Liability – Malpractice lawsuit, failure to provide necessary care.
- Criminal liability – Misdemeanor or felony charges for cases of gross negligence.
The Cost
Fortunately, medical malpractice claims have begun to drop since 2001. In 2004, the medical practitioners involved who were known as the defendants won the case 83% of the time. The legal fees can still amount to $18,000 if the case is dropped, to as much as $93,000 even when the case is won (12,13).
In 2018, there were 8,718 malpractice cases that resulted in payments to injured patients (14). Of those events, 310 reports of malpractice suits that resulted in payments related to nursing care.
However, 180 of those, about 60% of those had payments to the injured patient that were over $50,000 (14). However, there were nearly 15,000 adverse action reports filed against nurses, which was more than the number combined filed against physicians, NPs, and PAs combined.
The majority of medical malpractice cases primarily target the physician and the facility. However, anyone who made an entry into the patient’s medical record may be required to participate in legal proceedings.
Most common malpractice claims against nurses include failure to (15):
- Follow standards of care
- Follow safety protocols
- Perform procedures according to guidelines
- Use equipment properly
Use or operate equipment within the manufacture’s details
- Failure to correctly document
- Communication with the provider
- The care you completed
- Follow assess and monitor
- Report a change in status of the physician
- Assess a patient with change in status
- Communicate pertinent data
- Provide appropriate discharge education and information
- Communicate properly and completely between shifts

Self-Quiz
Ask Yourself...
- Think about the last difficult shift you had. Did you properly document?
- How would you prioritize documentation differently after reading this module?
What is Required for Nursing Documentation?
Necessary medical record nursing documentation can vary significantly depending on the care area. For example, the documentation a circulating nurse in the operating room completes will be very different from what is documented on an emergency room patient. While the basic principles of documentation stay constant, the nurse needs to be familiar with the documentation requirements for that area based on requirements of the state board of nursing, the facility, and the unit.
There are standard requirements for medical record documentation that are applicable in all patient care settings, and in both paper and EMR systems. These standards include the following (16):
- Accurate: Clinicians must be careful to proofread documentation to make sure it is free from errors. A small typo can have serious repercussions, as it is more likely to be misinterpreted by others.
- Relevant, concise, organized and complete: It is important to keep the information concise and relevant so that other care providers can quickly find the pertinent information that they need. Assessment data should be entered in a systematic way. Complete documentation ensures all of the unit policies for documentation are addressed.
- Free of bias: Clinicians should only include information that is pertinent to the care of the patient and remain free from personal bias. Direct quotations within the proper context should be utilized with proper context.
- Factual: Clinicians should not exaggerate or minimize findings. Charting is to be completed after completing a task, not before. Do not speculate data. Observations need to include exact times and measurements. Avoid approximations. Make sure to chart on the correct patient.
- Timely: What occurred during the shift should be documented during the shift. Documentation should be done as soon as possible after completing tasks. If something needs to be added in after the shift was completed, it should be denoted as a late entry with a reason as to why. Your facility likely has strict requirements regarding late entries.
- Legible/decipherable and clearly written: Paper documentation must be clearly legible. Writing must clearly convey meaning.
- Standardized: Clinicians must use appropriate medical terminology and approved acronyms and abbreviations.
- Labeled and Auditable: Paper documentation must be signed with credentials and must include date and time of the entry. When charting in the EMR, all entries and corrections are recorded and time stamped. Password sharing or having another clinician assist in documenting under incorrect username is fraudulent.

Self-Quiz
Ask Yourself...
- Do you currently incorporate all of the above principles in your documentation?
- If not, how can you change your practice to improve your documentation?
Examples of Effective and Ineffective Charting
The following will show some examples of these principles in action. These are based on the scenario of a patient admitted in the Emergency Department for chest pain.
| Example of effective documentation | Example of ineffective documentation | |
| Accuracy | Patient stated she took 800mg of Tylenol at 4pm, an hour after she began to feel chest pain. | Patient reports she took pain med for chest pain. |
| Relevant | Patient stated she has never experienced chest pain prior to this event and does not have a history of cardiac problems. | Patient was a competitive athlete 20 years ago and used to be in great shape. Patient thinks she is still pretty healthy. |
| Concise | Vital signs taken, telemetry monitor applied, lab samples collected, and PIV started per the chest pain protocol. | Patient was triaged and immediately brought to exam room. In accordance with the chest pain protocol, vital signs were taken first. Then the patient had a telemetry monitor applied. Next, the patient had blood samples drawn through the inserted PIV catheter. |
| Organized |
Patient reports no allergies. Prescriptions include hormone replacement therapy. Past medical history includes hysterectomy and foot surgery from a few years ago. Patient family history includes cardiovascular disease on her father’s side of the family. Patient denies smoking, illicit drug use, but does drink 3 times a week. Patient reports feeling fine until 1 hour after lunch when chest pain began. |
Patient was feeling fine until one hour after lunch, when she started to feel chest pain. Patient has no history of cardiac problems. However, there is family history of cardiovascular disease on the father’s side. Patient had a hysterectomy and foot surgery a few years ago. Patient denies smoking and illicit drug use. Patient does take hormone replacement therapy prescription. Patient does not have any allergies. Patient reports drinking alcohol x3/week. |
| Complete | Patient complaining of 8/10 chest pain, described as “stabbing.” Pain has been experiencing this pain for three hours. She has taken Tylenol, but nothing is able to alleviate the pain. | Patient is complaining of chest pain. |
| Free of Bias | Education provided per chest pain protocol. Patient was instructed to call 911 immediately if experiencing chest pain in the future. Patient verbalized understanding. | Patient was given needed education about chest pain since she clearly didn’t understand that chest pain cannot wait 3 hours and she need to call 911 right away because she can die of a heart attack. |
| Factual | Patient reports last meal was around 1300 which consisted of spicy foods. Her chest pain onset was 30 minutes after. She waited an additional three hours before seeking emergency care. | Patient presented to ER after lunch. |
| Legible/Decipherable | Patient was instructed to call for assistance with ambulation and how to utilize call light. | Patient cannot safely walk by she self. Call light assistance. Bathroom walk with me. |
| Standardized | Morphine Sulphate 2mg IV push, once PRN for 8/10 pain per chest pain protocol. | MSO4 2.0 mg, IV push, x1. |
| Timely | Documentation is completed in real-time, all documentation completed before transferring patient to telemetry. | Nurse documents three days later due to high volume of patients. |
Common Documentation Errors
- Falsification of a record. This can happen when charting an action isn’t completed in a timely manner, or from charting information before that action was completed.
- Fraudulent charting is the act of knowingly making a false record. Criminal charges of forgery can result if the misrepresentation is done for personal gain. An example of this would be a nurse documenting at administration of a controlled substance but instead was diverting the medication.
- Inappropriate use of cloning features. Information “copied and pasted” from a different patient’s record or that is completed by another provider. Data copied from previous shift assessments that isn’t updated to reflect current status is also a false record (9).
- Fail to document communication. Notification of the medical team of a change in patient status or critical lab values should always be included. Clarification or confirmation of orders should also be documented (17). Include notification of other providers who assisted with patient are. This includes failure to document transfer of care to another nurse.
- Failing to document a reason why something isn’t done. If a patient doesn’t receive a prescribed medication, the reason why the medication isn’t given needs to be described. If you communicate with the provider, this should also be included.

Self-Quiz
Ask Yourself...
- Have you ever failed to document or failed to document a critical portion of care?
- If you could alter your documentation, how would you better document in this situation?
Conclusion
Including all of the necessary information into each patient’s medical record can be a daunting task. The nurse must make sure that they have included all of the relevant and accurate information that is required by their facility guidelines. It must usually be done in a loud environment and is frequently interrupted by actually having to provide care to the patients.
It is not only a tedious chore, but it also tends to cause a lot of apprehension. There is usually a worry of “did I chart enough?” or “did I chart everything I needed to?” This is due to the defensive practices and attitudes healthcare workers have adapted to protect against malpractice lawsuits. In this way, charting is similar to paying taxes. No one likes it, but it still has to be done.
Perhaps a way to develop a healthy perspective toward charting is to change the focus to its original purpose: to communicate care about the patient. The purpose of charting is to relay to the other healthcare team members what is going on with the patient. With this objective in mind, the nurse will inevitably cover all the necessary details and it may also be a bit more satisfying to know that even though they are in front of the computer, they are performing and completing important information for the patient.
References
- 29-1141 Registered Nurses. (2018, March 30). Retrieved March 1, 2019, from https://www.bls.gov/oes/2017/may/oes291141.htm
- Hendrich, A., Chow, M. P., Skierczynski, B. A., & Lu, Z. (2008). A 36-hospital time and motion study: how do medical-surgical nurses spend their time? The Permanente journal, 12(3), 25-34.
- Health IT Quick Stats. (2019, February 6). Retrieved March 1, 2019, from https://dashboard.healthit.gov/quickstats/quickstats.php
- Medical Practice Efficiencies & Cost Savings. (2018, August 13). Retrieved March 1, 2019, from https://www.healthit.gov/topic/health-it-and-health-information-exchange-basics/medical-practice-efficiencies-cost-savings
- Meaningful Use. (2017, January 18). Retrieved March 1, 2019, from https://www.cdc.gov/ehrmeaningfuluse/introduction.html
- Miller, L., Stimely, M., Matheny, P., Pope, M., McAtee, R. & Miller, K. Novice Nurse Preparedness to Effectively Use Electronic Health Records in Acute Care Settings: Critical Informatics Knowledge and Skill Gaps. (2014). Online Journal of Nursing Informatics,18(2). Retrieved March 1, 2019, from https://www.himss.org/novice-nurse-preparedness-effectively-use-electronic-health-records-acute-care-settings-critical
- HHS Office of the Secretary,Health Information Privacy Division. (2016, February 25). Individuals’ Right under HIPAA to Access their Health Information. Retrieved March 1, 2019, from https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/access/index.html
- Office for Civil Rights (OCR). (2015, December 18). 2000-Why is the HIPAA Security Rule needed and what is the purpose of the security standards. Retrieved March 1, 2019, from https://www.hhs.gov/hipaa/for-professionals/faq/2000/why-is-hipaa-needed-and-what-is-the-purpose-of-security-standards/index.html
- AHIMA Work Group (2013). Integrity of the Healthcare Record: Best Practices for EHR Documentation (2013 update). Journal of AHIMA,84(8), 58-62. Retrieved March 1, 2019, from http://library.ahima.org/doc?oid=300257#.XHuU6YhKiUl
- What is Malpractice? (n.d.). Retrieved from https://www.abpla.org/what-is-malpractice#medical
- Cady, R. F., Esq. (2009). Criminal Prosecution for Nursing Errors. JONA’s Healthcare Law, Ethics, and Regulation,11(1), 10-16. Retrieved March 1, 2019, from https://www.nursingcenter.com/cearticle?an=00128488-200901000-00003&Journal_ID=260876&Issue_ID=848807
- Kann, B. R., Beck, D. E., Margolin, D. A., Vargas, D., & Whitlow, C. B. (Eds.). (2018). Improving Outcomes in Colon & Rectal Surgery. Retrieved March 1, 2019, from https://www.books.google.com/books?id=O61vDwAAQBAJ&dq=
- Improving Outcomes in Colon & Rectal Surgery edited by Brian R. Kann, David E. Beck, David A. Margolin, H. David Vargas, Charles B. Whitlow&source=gbs_navlinks_s
- Peters, P. G. (2008). Twenty Years of Evidence on the Outcomes of Malpractice Claims. Clinical Orthopaedics and Related Research, 467(2), 352-357. doi:10.1007/s11999-008-0631-7
- Singh, H. (2018). National Practitioner Data Bank Generated Data Analysis Tool. Retrieved March 1, 2019, from https://www.npdb.hrsa.gov/analysistool/
- Top 5 Malpractice Claims Made Against Nursing Professionals. (n.d.). Retrieved March 1, 2019, from https://www.proliability.com/portals/0/docs/nursemalpracticewhitepaper.pdf
- American Nurses Association. (2010). ANA’s Principles for Nursing Documentation. Retrieved February 28, 2019, from https://www.nursingworld.org/~4af4f2/globalassets/docs/ana/ethics/principles-of-nursing-documentation.pdf
- Lippincott Nursing Education. (2018, February 22). Lippincott Nursing Education Blog. Retrieved March 1, 2019, from http://nursingeducation.lww.com/blog.entry.html/2018/02/22/nursing_documentatio-S5hF.html
- Reising, D. L., & Allen, P. N. (February 2007). Protecting yourself from malpractice claims. American Nurse Today,2(2). Retrieved March 1, 2019, from https://www.americannursetoday.com/protecting-yourself-from-malpractice-claims/.
- Reising, D. L. (2012). Make your nursing care malpractice-proof. American Nurse Today,7(1). Retrieved March 1, 2019, from https://www.americannursetoday.com/make-your-nursing-care-malpractice-proof/
Drains: Everything Nurses Need to Know
Introduction
Picture this: you walk into your hospital unit, fresh off a good night’s sleep. You find your patient assignment and head over to get report. Then the outgoing nurse says something that makes your heart skip a beat. “This patient has an abscess drain. You need to flush it every X hour(s), record the output every X hour(s), call the doctor if __ happens…” Before long, your head is spinning, and then you realize you’ve been spelling ‘abscess’ incorrectly for who knows how long!
Drains can be intimidating, especially with little to no prior experience in drain management. They often come with a specific set of instructions that can be confusing. What’s worse, a patient may suffer a serious delay in recovery if something goes wrong. Nobody wants to be the one to make that call to the doctor about a malfunctioning drain. Fortunately, like anything else, managing drains becomes much easier with experience and a little education.
Types of Drains
A patient may require drain placement for several reasons. Often, they are placed at the end of a surgery or percutaneously to help eliminate any fluid that may accumulate within the wound. A common type of surgical drain is the Jackson-Pratt ®. Certain organs may require a drain to assist with the removal of their contents, such as foley catheters or nasogastric tubes. Drains may also be placed to help remove fluid or air from body cavities. A chest tube is a good example of this type of drain. Finally, if a patient develops an abscess, a drain is often required to help remove the infected fluid more quickly.
Drains serve a particularly important purpose (other than driving the patient and his/her nurses crazy). The accumulation of fluid in the wrong place can have a detrimental effect on the patient’s health and healing (1). Excess fluid in the surgical site can cause significant pain as well as injury to surrounding tissues and organs (1). It can also increase the chance of infection (1).
Medical drains can be divided into multiple categories.
Drains are often described as being active or passive. Passive drainage allows for gravity to help remove excess fluid, without the use of pressure (2). An example of passive drainage would be placing a foley catheter to gravity or using a penrose drain. A penrose drain is a flat, ribbon-like tube that creates a passage from a wound to the open air, which allows any excess fluid to simply flow outward (2). The area surrounding the opening is often lightly covered with gauze to collect fluid as it drains and must be changed when saturated (2).
The following image is an example of a penrose drain (3).
Active drains use actual pressure, typically negative pressure, to help remove excess fluid from the body.
An example of an active drainage system would be a Jackson-Pratt (JP) ® drain or hemovac ®. With both types of drains, the pressure is created by compressing the collection container, which creates a low-pressure vacuum that pulls the fluid out of the body (2). The following images are examples of hemovac (12) and JP ® drains (3).
Open vs. Closed
Drains can also be described as open or closed. An open system simply means that it is open to air. An example of an open system would be a penrose drain, as described above. A closed drain, on the other hand, is not open to the environment. Rather, the draining fluid is contained within the system, and the collection bulb or bag is simply emptied from time to time, as needed. A JP ® drain is an example of a closed drain.
Surgical vs. Percutaneous
While not a technical classification, it is interesting to note how the drain is placed. Surgical drains are usually positioned in the operating room or, more rarely, at the bedside by the physician. The JP ® is an example of a surgical drain.
Drains may also be placed percutaneously:
Percutaneous: (adjective) effected or performed through the skin (4)
Percutaneous drains are placed without surgical intervention. Rather, Interventional Radiologists use imaging, such as CT, ultrasound, or fluoroscopy to guide a needle into a fluid collection (5). This technique is less invasive (6). Before surgical or percutaneous insertion of a drain, the patients coagulation status and hemostasis risk must be evaluated (13).

Self-Quiz
Ask Yourself...
- What are the advantages and of open vs closed drainage systems?
Infections 101: A Brief History of Drains
Before the advent of antibiotics, the development of an abscess or postoperative infection was often a death sentence (7). Thanks to advances in modern medicine, suffering patients now stand a chance. In certain situations, infections can be treated simply with a course of antibiotics. However, if there is any concern for the development of sepsis, further intervention is needed (6).
Until the 1970s, the most effective (and only) way to treat infection and abscess was surgical intervention (7). Surgeons would attempt to remove the infected material while striving for “directness, simplicity, and above all, avoidance of unnecessary contamination of uninvolved areas” (7). Unfortunately for these patients, this meant that a second surgery was required to heal them from complications of their first surgery. Even with the addition of antibiotics, these situations were associated with significant morbidity and mortality (6).
Luckily, rapid advances in technology allowed for the development of a less invasive solution. The advent of fluoroscopy, ultrasound, and especially CT provided physicians with a tool to see inside the body without having to cut someone open. The first studies involving the use of medical imaging for percutaneous drain placement were published in the late 1970s (7). Over the next several years, multiple studies reported success rates ranging from 60-80% using these new techniques (8).
Doctors are now able to drain up to 3 separate abscess/infection sites percutaneously (8). Recent studies report technical success of up to 90% with percutaneous drain placement, and it can offer immediate improvement in sepsis, with return to hemodynamic stability within 1-2 days (9). CT is considered the imaging modality of choice because of its ability to fully visualize the infection and surrounding structures as well as provide a pathway from the skin to the destination (9).

Self-Quiz
Ask Yourself...
- How has the increased use of medical drains altered the medical care and approach to managing abscesses?
Patient Considerations for Percutaneous Drain Placement
Not every infection or fluid collection requires percutaneous drain placement or even surgery. Thus, it is important for physicians to work together to determine the appropriate treatment for each patient individually. When a patient is found to have an abscess, multiple doctors may get involved, usually either a surgeon or interventional radiologist (sometimes both) and a clinical pharmacist if an infection is suspected or confirmed.
It is essential that providers choose patients carefully, as ineffective, or incomplete drainage of the infection can lead to significant morbidity and mortality (8). For example, percutaneous drainage is sometimes avoided in patients with chest infections, such as empyema, abscess, and pleural effusion because of the risk of pneumothorax (9). Additionally, pyogenic, and fungal abscesses in the lung parenchyma often resolve with more conservative management, namely through supportive care and antibiotics (9). Pancreatic abscesses remain at high risk of treatment failure with percutaneous drain placement; thus, surgery is usually still the intervention of choice (9).
Conversely, there are many types of abscesses that respond well to percutaneous drainage. Liver abscesses have an extremely low risk of complications with this type of drain placement, around 1-4% (9). It is also very effective in managing infections related to visceral perforation, which may result from Crohn’s disease, prior operations, diverticulitis, and appendicitis (9). Deep pelvic abscesses respond well to percutaneous drainage, although these can be more challenging and require careful planning because of the presence of nearby organs (9).
Percutaneous drainage is often considered for patients who are too ill for surgery, in the hopes that it may improve sepsis and promote increased strength/rest (8). It is also recommended for patients who have a good response to antibiotics and low risk of mortality.

Self-Quiz
Ask Yourself...
- Deciding who may benefit from a drain and who needs conservative therapy is difficult and nuanced.
- How would you consult with on this subject?
- Should medical therapy be initiated while awaiting intervention?
Image-Guided Drainage: How Does it Work?
When first contemplating percutaneous drainage, doctors must first decide which modality to use fluoroscopy, ultrasound, or CT. As mentioned previously, CT is most often used to guide drain placement because of its superior visualization.
The interventional radiologist will typically review any available imaging beforehand to plan the most appropriate route for drain placement. Care must be made to avoid major vessels and other important structures (6). To minimize the risk of complications, physicians are advised to use the safest, most direct route and attempt placement in the most dependent part of the fluid collection to encourage effective drainage (6).
Once the patient is properly positioned on the table, the physician will use the CT, ultrasound, or X-ray to guide the placement of a special needle, taking frequent pictures to monitor its progression from the skin through soft tissue and into the infection (6). Once the needle is in place, a wire is passed through the needle into the fluid collection and then the needle is removed, leaving only the wire in place.
Next, a drainage catheter is threaded across the wire to its final resting place. The tip of the catheter rests within the fluid collection. The drainage catheter contains holes to help fluid pass out of the body. Once the tube is in place, the wire is removed. A drainage bag is attached. Throughout the procedure, pictures are taken to ensure correct placement. Patients are often given moderate sedation to make them more comfortable, but not in every case.
Drain Management
Care for the patient with a drain can seem intimidating, but it doesn’t have to be. Often, the physician will write orders to guide nursing staff while caring for these patients. Drain management may also differ depending on what type of drain the patient has. If there are no orders it is reasonable to contact the physician who placed the drain for clarification.
Surgical Drains
Two of the more common types of surgical drains are the hemovac ® or JP ® drain. As mentioned previously, both drains are active, closed systems, meaning they use negative pressure to help remove excess fluid from a surgical wound, all of which is stored within the collection device.
When managing JP ® or hemovac ® drains, it is important to note the color of the drainage fluid. The fluid is typically bloody or purulent at first, but should gradually lighten to a light pink, clear, or yellow color (10). Indications for removal may vary, but in general, these drains remain in place until the daily output decreases to less than 30 ml (10).
Follow any written instructions provided by the ordering physician. Nurses will also be responsible for emptying the drain, observing the site, and documenting findings. The drain should be emptied no later than when it becomes half full, as it will lose suction and become ineffective (2). Observe the insertion site for drainage and signs of infection. Be sure to keep the skin clean. These drains may also be sutured in place. The drains should be further secured with medical adhesive or pinned to the patient’s gown with a safety pin to secure the drains before mobilizing and to avoid accidental removal.
Percutaneous Drains
Percutaneous drains usually look a little bit different. The interventional radiologist uses a special type of drainage tube that is also sometimes called a ‘pigtail.’ These tubes do not always have to be sutured in place, for they may contain a string that, when pulled, curls the distal end of the tube, making it a bit harder to pull out. They are then usually adhered to the skin with a dressing.
Again, it is important to note the color of the drain output. Keep in mind that percutaneous drains are often used for abscess or infection, meaning fluid will be purulent and/or bloody. Check for any specific written instructions for drain management. Monitor the drain site regularly for signs of infection or drainage. Empty the drainage bag as directed or as needed and document findings. These drains may also use a collection bag that applies suction through negative pressure.
Percutaneous abscess drains are more likely to require flushing because the purulent drainage can be thick and pose a risk for occluding the drain. They may be equipped with a three-way stopcock to allow for easy flushing.
(French pigtail catheter [Cook Inc., Bloomington, IN; C-PCS-830-LOCK]).

Self-Quiz
Ask Yourself...
- Image guidance has revolutionized drain placement.
- What are the advantages of surgical drains and what is their role currently?
Properties of a Well-Functioning Drain
Since humans lack x-ray vision, the inner workings of a drain can seem a little mysterious. What is going on in there? How can a nurse know if it is doing what it is supposed to do? Repeat imaging (CT, ultrasound, etc.) is the best way to visualize how infections and abscesses change over time. However, it is costly and unnecessary to expose patients to extra radiation as a matter of curiosity.
To get some idea of how a drain is functioning, one has to look at the drain itself. Even though drains may look different, they function in similar ways, thus these considerations can be applied to both surgical and percutaneous drains.
Output
The hallmark of a well-functioning drain is output. The purpose of a drain is to get fluid out of the body. Therefore, if the collection bag/bulb is capturing drainage fluid, this is a good indication that it is working correctly. Remember that the fluid is often bloody at first but should lighten over time. The drainage from an abscess may also be bloody at first before appearing purulent.
Skin Site Clean/Dry
The skin at the site of a drain should be kept clean and dry (2). Minimal amounts of fluid may leak around the tube, causing crusting on the skin or a small amount of visible drainage. This can be gently wiped away with clean gauze soaked with normal saline or warm, soapy water (10). Apply a fresh clean gauze at the site to protect the skin from breakdown (10). If a large amount of drainage is leaking from the skin and around the tube, this is not normal and should be addressed.
Stopcock in the Proper Position
Ensuring that the three-way stopcock (if present) is in the proper position is essential for proper function. The off switch should be pointing to the flush port at all times, unless the nurse is preparing to flush the drain. Turning the off switch to the flush port prevents fluid from draining outside of the system and creates an open pathway from the drain into the drain bag.
Active Suction
All active drains should be monitored closely to ensure that the bulb or accordion is adequately compressed (2). Constant negative pressure must be maintained in order for the drain to work. To compress a JP, use the “side-in method” where the nurse compresses the JP bulb at its largest diameter (in the middle) with fingers and thumb to compress the bulb (14). The drain should be emptied when it is approximately 25 percent full to maintain the pressure within the bulb (14).
These drains may require frequent assessment and emptying, especially at first. Examples of active drains include JP®, hemovac®, and most percutaneous drains.
Is this Normal? Drain Troubleshooting
Unfortunately, drains can develop complications. It is essential to know what to look for so that potential problems can be identified early. As mentioned previously, a delay in reporting or discovering a drain malfunction may cause delays in patient healing. Luckily, the problems are fairly easy to spot if you know what to look for.
Bleeding
Some bleeding is normal. The act of placing a drain may cause bleeding from nearby small vessels (9). This is usually self-limiting, which is why the nurse may note bleeding in the early hours after placement. The drainage should gradually lighten. Prolonged bleeding or the development of new bleeding warrants a prompt call to the physician.
Leaking
A leaky drain can be a messy business. If the source of the leak is not immediately known, the nurse should evaluate the drain. Assess the tubing for cracks or holes. Ensure all connections are tight. Sometimes the drainage bag/bulb may be punctured. If so, it is often easily replaced.
Leaking may also occur because the drain is occluded or kinked (2). Assess the tubing carefully for signs of obstruction. Flushing the drain can help dislodge occlusions. Again, never flush a drain without orders from the physician.
A drain may also leak at the skin. Minimal amounts of leakage can be expected because the drain creates a track for small amounts of fluid to escape. Moderate to severe leakage can cause skin breakdown and is not normal. It suggests that the drain is malfunctioning in some way, often due to an occlusion or displacement of the drain. Fluid travels the path of least resistance. If it can’t pass easily through the tube, it will find another way out. Notify the physician, who may order follow up imaging, like a CT scan. If a percutaneous drain is leaking, the patient may have to be sent down to interventional radiology for assessment and possible replacement.
No output
Drain output may cease for two reasons: there is no more fluid, or the fluid can’t get out. It is easy to assume the former. Yet, when faced with a drain without drainage, it is important to use critical thinking and common sense. Drainage usually tapers off, meaning it will drain a little less over time. An abrupt cessation of fluid could indicate a problem. Assess the drain for kinks or obstructions. If the drain is occluded, fluid may begin to leak around the tube at the skin. Carefully document drain output as dictated by the physician or facility protocol. Any time there is a concern, the physician should be notified.
Infection
Infection may occur with both surgical and percutaneous drains. It usually forms one of two ways: during initial drain placement or as a result of continued catheter presence (9). Infection may form during initial placement if the needle punctures a non-target area (such as the colon) or from prolonged dilation, which is why the procedure should be completed in a timely manner (9). Infections may also form at the skin if a drain is present for a long time (9).
The nurse should assess the drain site frequently. Signs of skin infection include redness, increased pain, swelling, fever, and purulent drainage (10). Additionally, sepsis is always a concern for the patient with an abscess (9). A patient with sepsis will sicken very quickly, with rapid increase in fever, chills, and rigors (9). Vital sign monitoring is essential. If the nurse suspects a new infection of any kind or deterioration, notify the physician immediately.
Displacement
Living with a drain takes some getting used to. It can be easy for patients to forget it’s there. Sometimes the tubing can become tangled up in the bed sheets or left behind when a patient stands up. Although drains come equipped with reinforcements, such as a suture or dressing to help keep the tubing in place, it is possible to pull the drain at least partially or sometimes completely out of the body.
If a drain is pulled out entirely, the nurse should cover the site with some gauze to catch any drainage. When drains are placed, they form a pathway from the abscess or infection to the skin. The tube’s job is to provide a conduit for the fluid to escape. If the tube is removed abruptly, that pathway still exists temporarily, so fluid will continue to leak out of the body in the absence of the tube. Do not attempt to put the tube back in, as it is no longer sterile. Notify the physician.
If the drain is only partially removed, reinforce the dressing as best as possible to maintain its current position and call the physician. Again, do not attempt to push the tubing back inside the patient. The physician may order imaging to assess the drain’s location (2). Removal and/or replacement may be necessary.

Self-Quiz
Ask Yourself...
- Managing drains can be intimidating at first.
- How would you troubleshoot the common issues listed here?
Drains – Frequently Asked Questions
What is an Accordion Drain?
An accordion drain is used to remove fluid from a wound, abdomen, or lung space. The drain is comprised of a bag and vale that does not allow air or fluid to return back into the open space, wound, or lungs. An accordion drain is considered a closed drainage system, meaning that the drain is formed by tubes draining into a bag.
What is the difference in a Penrose Drain and a Jackson Pratt Drain (JP Drain)?
Penrose Drain
A Penrose drain is a flat, ribbon-like tube usually made of latex, creating a passage from a wound. The drains are open to air, allowing excess fluid to flow outward. The surrounding area on the outside of the body is covered in gauze to collect the fluid, as it drains. The gauze must be drained frequently as it becomes saturated.
A Penrose Drain is considered a passive and open draining system – meaning that it allows for gravity to remove the fluid without the use of pressure.
Part of the Penrose drain is inside of the body cavity, with one or both ends coming out of the incision.
Although they are tubular, most of the drainage occurs outside of the tube, more so around it. It is used more as a “space-holder” to keep the tissue area open, allowing drainage to flow out.
Indications for a Penrose Drain
- Wounds
- Infected area or abscess
- Underneath of skin graft
- Septic joints
- Tendon sheaths
*NOT suitable for the abdominal or thoracic cavity
Jackson Pratt Drain (JP Drain)
A JP drain is considered an active and closed drainage system meaning that it uses negative pressure to remove excess fluid from the body. The pressure is created by compression the collection container (which looks like an egg), creating a low-pressure vacuum pulling fluid from the body. It is closed, meaning that it is not open to the external environment; instead, the fluid is contained within a collection bulb.
The drain is sutured in place at the skin at the insertion site to promote stability and prevent wound breakdown and pulling. The drain is left in place until the drainage is minimal. If pulled too early, the patient may be at risk of developing a seroma or hematoma.
Indications for a JP Drain
- Superficial wounds where there is pre-existing or anticipated fluid build-up.
- Surgery if large amounts of drainage is expected, such as:
- plastic surgery
- breast surgery
- orthopedic procedures
- chest surgery or drainage
- infected cysts
- neurosurgery
- biliary surgery
- pancreatic surgery
How do you flush a Jackson Pratt Drain (JP Drain)?
You should not flush a JP drain without a stopcock. There is no indication for doing so, it will only present additional bacteria into the drain.
IF you must, and there is a stop-cock present, make sure it is done under sterile conditions with sterile saline.
What is a Hemovac drain?
A Hemovac drain is used to remove fluids that build up within a body after a surgical procedure. It is a circular device connected to a tube. It may be anchored in place by sutures. The Hemovac is an active closed system that creates suction to removed fluid.
Summary
This course is designed to help readers become more familiar with drains. They come with all sorts of indications: to facilitate healing after surgery or infection, to assist with draining contents from affected organs, or remove fluids that have accumulated in body cavities.
Drains are classified based on their function: open or closed, passive or active. Familiarity with the different types of drains gives the nurse a basic understanding of how they work- which is important because they can look very different, depending on the manufacturer.
In the old days, surgery and antibiotics were the only way to treat intra-abdominal infections. Significant advances in technology have allowed interventional radiologists to specialize in using medical imaging (CT, ultrasound, X-ray, and MRI) to place drains without making an incision. However, patient selection is still very important, and physicians must know which patients are good candidates for percutaneous drain placement and which are better off heading to the OR.
This course is also designed to provide a basic understanding of drain management and troubleshooting. It is important for nursing staff to understand how a drain is supposed to behave when it is functioning normally so that potential problems are easier to spot. When in doubt, consult the physician. Always be aware of any written orders or policies that dictate drain management, as practices may vary from place to place.
As with anything else, the best way to become more comfortable with drains is to be around them!
References
- Makama, J. G., & Ameh, E. A. (2008). Surgical drains: What the residents need to know. Nigerian Journal of Medicine: Journal of the National Association of Resident Doctors of Nigeria, 17(3), 244-50. doi: 10.4314/njm.v17i3.37389
- Knowlton, M. C. (2015). Nurse’s guide to surgical drain removal. Nursing 2015, 45(9), 59-61. doi: 10.1097/01.NURSE.0000470418.02063.ca
- Lemone, P., & Burke, K. (2008). Medical-surgical nursing(4th ed.). Upper Saddle, New Jersey: Pearson.
- Percutaneous. (2019). In Merriam-Webster Dictionary Online. Retrieved from https://www.merriam-webster.com/dictionary/percutaneous#medicalDictionary
- Wallace, M. J., Chin, K. W., Fletcher, T. B., Bakal, C. W., Cardella, J. F., Grassi, C. J., … Kundu, S. (2010). Quality improvement guidelines for percutaneous drainage/aspiration of abscess and fluid collections. Journal of Vascular and Interventional Radiology, 21(4), 431-435. doi: https://doi.org/10.1016/j.jvir.2009.12.398
- Hearns, W. C. (2012). Abscess drainage. Seminars in Interventional Radiology, 29(4), 325-336. doi 10.1055/s-0032-1330068
- Rivera-Sanfeliz, G. (2008). Percutaneous abdominal abscess drainage: A historical perspective. American Journal of Roentgenology, 191(3), 642-643. doi: 10.2214/AJR.07.3903
- Cinat, M. E., & Wilson, S. E. (2002). Determinants for successful percutaneous image-guided drainage of intra-abdominal abscess. Arch Surg., 137(7), 845-849. doi:10.1001/archsurg.137.7.845
- Lorenz, J. & Thomas, J. L. (2006). Complications of percutaneous fluid collection. Seminars in Interventional Radiology, 23(2), 194-204. doi: 10.1055/s-2006-941450
- National Institutes of Health. (n.d.) Patient education: How to care for the Jackson-Pratt drain. Retrieved from https://www.cc.nih.gov/ccc/patient_education/pepubs/jp.pdf
- St. Jude Children’s Research Hospital. (2019). Caring for a pigtail drain. Retrieved from https://www.stjude.org/treatment/patient-resources/caregiver-resources/patient-family-education-sheets/home-care-guidelines/caring-for-a-pigtail-drain.html
- (Image) Doyle, G. R., & McCutcheon, J. A. (2015). Clinical Procedures for Safer Patient Care. Victoria, BC: BCcampus. Retrieved from https://opentextbc.ca/introductiontosociology2ndedition/.
- Patel IJ, Davidson JC, Nikolic B, Salazar GM, Schwartzberg MS, Walker TG, Saad WA; Standards of Practice Committee, with Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Endorsement. Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. J Vasc Interv Radiol. 2012 Jun;23(6):727-36. do: 10.1016/j.jvir.2012.02.012. Epub 2012 Apr 17. PMID: 22513394.
- Mamuyac, E. M., Pappa, A. K., Thorp, B. D., Ebert, C. S., Jr, Senior, B. A., Zanation, A. M., Lin, F. C., & Kimple, A. J. (2019). How Much Blood Could a JP Suck If a JP Could Suck Blood? The Laryngoscope, 129(8), 1806–1809. https://doi.org/10.1002/lary.27710
Alzheimer’s Nursing Care
Introduction
Alzheimer’s disease is a destructive, progressive, and irreversible brain disorder that slowly destroys memory and thinking. Alzheimer’s is the most common cause of dementia in older adults (1). For most people who have Alzheimer’s disease, symptoms first appear in their mid 60’s (1). Studies suggest more than 5.5 million Americans, most 65 or older, may have dementia caused by Alzheimer’s (1). It is currently listed as the sixth leading cause of death in the United States. It is important to understand the signs and symptoms of Alzheimer’s dementia and how to manage the care of a patient, family member, or friend suffering from the disease.
Dementia is the loss of cognitive functioning-thinking, remembering, and reasoning- and behavioral abilities to such extent that it interferes with activities of daily living (1). The severity of dementia ranges from mild to severe. In its mildest stage, it begins with forgetfulness, with its most severe stage consists of complete dependence on others for general activities of daily living (1).
Signs and Symptoms & Diagnosis of Alzheimer’s Disease
Memory problems are typically among the first signs of cognitive impairment related to Alzheimer’s disease. Some people with memory problems have a condition called Mild Cognitive Impairment (MCI) (4). In this condition, people have more memory problems than usual for their age; however, their symptoms do not interfere with their daily lives. Older people with MCI are at increased risk of developing Alzheimer’s disease. The first symptoms of Alzheimer’s may vary from person to person. Many people display a decline in non-memory related aspects of cognition such as word-finding, visual issues, impaired judgment, or reasoning (4).
Providers use several methods and tools to determine the diagnosis of Alzheimer’s Dementia. To diagnose, they may conduct tests of memory, problem-solving, attention, counting, and language. They may perform brain scans, including CVT. MRI or PET to rule out other causes for symptoms. Various tests may be repeated to give doctors information about how memory and cognitive functions change over time. They can help diagnose other causes of memory problems such as stroke, tumor, Parkinson’s disease, and vascular dementia. Alzheimer’s disease can be diagnosed only after death by linking clinical measures with an examination of brain tissue in an autopsy (4).
History of Alzheimer’s
Alzheimer’s disease is named after Dr. Alois Alzheimer. In the early 1900’s, Dr. Alzheimer noticed changes in the brain tissue of a patient who had died of an unknown mental illness. The patient’s symptoms included memory loss, language problems, and unpredictable behavior. After her death, her brain was examined, and was noted to have abnormal clumps known as amyloid plaques and tangled bundled fibers, known as neurofibrillary or tau tangles (1). These plaques and tangles within the brain are considered some of the main features of Alzheimer’s disease. Another feature includes connections of neurons in the brain. Neurons are responsible for the transmissions of messages between different parts of the brain and from the brain to other parts of the body (1).
Scientists are continuing to study the complex brain changes involved with the disease of Alzheimer’s. It seems that the changes in the brain could begin ten years or more before cognitive problems start to surface. During this stage of the disease, the people affected seem to be symptom-free; however, toxin changes occur within the brain (1). Initial damage in the brain occurs within the hippocampus and entorhinal cortex, which are the parts of the brain that are necessary in memory formation. As the disease progresses, additional aspects of the brain become affected, and overall brain tissue shrinks significantly (1).

Self-Quiz
Ask Yourself...
- Have you experienced a patient in your practice with dementia or Alzheimer’s disease? What did their symptoms look like?
- What are some common diagnostic tools that healthcare providers use in the diagnosis of this disease?
- What is the definitive diagnosis of Alzheimer’s disease?
Stages of Disease
Mild Alzheimer’s
As the disease progresses, people experience significant memory loss along with other cognitive problems. Most people are diagnosed in this stage (1).
- Wandering/getting lost
- Trouble handling money or paying bills
- Repeating questions
- Taking longer to complete basic daily tasks
- Personality/behavioral changes (1)
Moderate Alzheimer’s
In this stage, damage occurs in the area of the brain that controls language, reasoning, sensor processing, and conscious thought (1).
- Memory and confusion worsen
- Problems recognizing family and friends
- Unable to learn new things
- Trouble with multi-step tasks such as getting dressed
- Trouble coping with situations
- Hallucinations/delusions/paranoia (1)
Severe Alzheimer’s
- Plaques and tangles spread throughout the brain and brain tissue shrinks by a significant amount
- Cannot communicate
- Completely dependent on others for care
- Bedridden – most often as the body shuts down

Self-Quiz
Ask Yourself...
- What are some of the signs and symptoms that differentiate each stage of Alzheimer’s disease?
- A person is in what stage of Alzheimer’s disease when they struggle recognizing family members and friends?
Prevention
As a person ages, many worry about developing Alzheimer’s disease and dementia. Especially if they have had a family member who suffered from the disease, they may worry about genetic risk. Although there have been many studies on the prevention of the disease, and many are still ongoing, nothing has been proven to prevent or delay dementia caused by Alzheimer’s disease (2).
A review led by experts from the National Academies of Sciences, Engineering, and Medicine, found encouraging yet inconclusive evidence for three types of interventions related to ways to prevent or delay Alzheimer’s Dementia or age-related cognitive decline (2):
- Increased physical activity
- Blood pressure control
- Cognitive training
Treatment of the Disease
Alzheimer’s disease is complex and is continuously being studied. Current treatment approaches focus on helping people maintain their mental function, manage behavioral symptoms, and low the symptoms of the disease. The FDA has approved several prescription drugs to treat those diagnosed with Alzheimer’s (3). Treating symptoms of Alzheimer’s can provide patients diagnosed with comfort, dignity, and independence for a greater amount of time, simultaneously assisting their caregivers. The approved medications are most beneficial in the early or middle stages of the disease (3).
Cholinesterase inhibitors are prescribed for mild to moderate Alzheimer’s disease; they may help to reduce symptoms. Medications include Rzadyne®, Exelon ®, and Aricept ® (3). Scientists do not fully understand how cholinesterase inhibitors work to treat the disease; however, research indicates that they prevent acetylcholine breakdown. Acetylcholine is a brain chemical believed to help memory and thinking (3).
For those suffering from moderate to severe Alzheimer’s disease, a medication known as Namenda®, which is an N-methyl D-asparate (NMDA) antagonist, is prescribed. This drug helps to decrease symptoms, allowing some people to maintain certain essential daily functions slightly longer than they would without medication (3). For example, this medication could help a person in the later stage of the disease maintain their ability to use the bathroom independently for several more months, benefiting the patient and the caregiver (3). This drug works by regulating glutamate, which is an important chemical in the brain. When it is produced in large amounts, glutamate may lead to brain cell death. Because NMDA antagonists work differently from cholinesterase inhibitors, these rugs can be prescribed in combination (3).

Self-Quiz
Ask Yourself...
- Is there a cure for this disease?
- What are some of the treatment forms that have been used for the management of Alzheimer’s disease?
- Can medications be used in conjunction with one another for the treatment of the disease?
Medications to be Used with Caution in those Diagnosed with Alzheimer’s
Some medications such as sleep aids, anxiety medications, anticonvulsants, and antipsychotics should only be taken by a patient diagnosed with Alzheimer’s after the prescriber has explained the risk and side-effects of the medications (3).
Sleep aids: They are used to help people get to sleep and stay asleep. People with Alzheimer’s should not take these drugs regularly because they could make the person more confused and at a higher risk for falls.
Anti-anxiety: These are used to treat agitation and can cause sleepiness, dizziness, falls, and confusion (3).
Antipsychotics: they are used to treat paranoia, hallucinations, agitation, and aggression. Side effects can include the risk of death in older people with dementia. They would only be given when the provider agrees the symptoms are severe enough to justify the risk (3).
Caregiving
Coping with Agitation and Aggression
People with Alzheimer’s disease may become agitated or aggressive as the disease progresses. Agitation causes restlessness and causes someone to be unable to settle down. It may also cause pacing, sleeplessness, or aggression (5). As a caregiver, it is important to remember that agitation and aggression are usually happening for reasons such as pain, depression, stress, lack of sleep, constipation, soiled underwear, a sudden change in routine, loneliness, and the interaction of medications (5). Look for the signs of aggression and agitation. It is helpful to be able to prevent the problems before they happen.
Ways to cope with agitation and aggression (5):
- Reassure the person. Speak calmly. Listen to concerns and frustrations.
- Allow the person to keep as much control as possible.
- Build in quiet times along with activities.
- Keep a routine.
- Try gently touching, soothing music, reading, or walks.
- Reduce noise and clutter.
- Distract with snacks, objects, or activities.
Common Medical Problems
In addition to the symptoms of Alzheimer’s disease, a person with Alzheimer’s may have other medical problems over time. These problems can cause confusion and behavior changes. The person may be unable to communicate with you as to what is wrong. As a caregiver, it is important to watch for various signs of illness and know when to seek medical attention for the person being cared for.
Fever: Fever could be a sign of potential infection, dehydration, heatstroke, or constipation (4).
Flu and Pneumonia: These are easily transmissible. Patients 65 years or older should get the flu and Pneumonia shot each year. Flu and Pneumonia may cause fever, chills, aches, vomiting, coughing, or trouble breathing (4).
Falls: As the disease progresses, the person may have trouble with balance and ambulation. They may also have changes in depth perception. To reduce the chance of falls, clean up clutter, remove throw rugs use armchairs, and use good lighting inside (4).
Dehydration: It is important to remember to ensure the person gets enough fluid. Signs of dehydration include dry mouth, dizziness, hallucinations, and rapid heart rate (4).
Wandering
Many people with Alzheimer’s disease wander away from their homes or caregiver. As the caregiver, it is important to know how to limit wandering and prevent the person from becoming lost (5).
Steps to follow before a person wanders (5)
- Make sure the person carries a form of ID or wears a medical bracelet.
- Consider enrolling the person in the Medic Alert® + Alzheimer’s Association Safe Return Program®
- Alert neighbors and local police that the person tends to wander and ask them to alert you immediately if they are seen alone.
- Place labels on garments to aid in identification.
Tips to Prevent Wandering (5)
- Keep doors locked. Consider a key or deadbolt.
- Use loosely fitting doorknob covers or safety devices.
- Place STOP, DO NOT ENTER< or CLOSED signs on doors.
- Divert the attention of the person away from using the door.
- Install a door chime that will alert when the door is opened.
- Keep shoes, keys, suitcases, coats, and hats out of sight.
- Do not leave a person who has a history of wandering unattended.

Self-Quiz
Ask Yourself...
- What are basic implementations you can make as a caregiver to make handling confusion and aggression easier in a patient with Alzheimer’s?
- What are some of the types of medical problems that people with Alzheimer’s may face and how can they be monitored for prevention?
Conclusion
Alzheimer’s is a sad, debilitating, progressive disease that robs patients of their life and dignity. As research continues on the causes, treatment, and prevention of the disease, it is important for healthcare workers and caregivers to know the signs and symptoms of a patient with Alzheimer’s disease and potential coping mechanisms and management strategies of the disease. More information on the disease is available through several various resources, including:
Family Caregiver Alliance
800-445-8106
NIA Alzheimer’s and related Dementias Education and Referral Center
800-438-4380
References + Disclaimer
- Alzheimer’s disease fact sheet. (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet
- Preventing Alzheimer’s disease: What do we know? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/preventing-alzheimers-disease-what-do-we-know
- How is Alzheimer’s disease treated? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/how-alzheimers-disease-treated
- Behavior changes and communication in Alzheimer’s. (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/topics/behavior-changes-and-communication-alzheimers
- How is Alzheimer’s disease diagnosed? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/how-alzheimers-disease-diagnosed
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
Attention Florida Learners
In order to meet Florida Board of Nursing testing requirements for Continuing Education, you will be directed to a brief quiz upon clicking the complete button. Per state regulation, you must pass this quiz with a score of 80% or higher to receive your certificate.