Course
Recognizing the Signs of Impaired Tissue Perfusion in Trauma Patients
Course Highlights
- In this course we will learn about the causes, signs, and symptoms of impaired tissue perfusion and why it is important for nurses to recognize them quickly.
- You’ll also learn the basics of brain and renal perfusion.
- You’ll leave this course with a broader understanding of perfusion assessment skills and what findings indicate notifying a patient’s provider.
About
Contact Hours Awarded: 1.5

Course By:
Tiffany Jakubowski
MS, APRN, AGCNS-BC, CMSRN, ONC
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Caring for a patient with traumatic injuries means recognizing and discerning different signs and symptoms at once, which is why these patients are often kept in the Intensive Care Unit (ICU) or other higher levels of care. A patient may initially be considered stable enough for a medical, surgical, or telemetry floor but then needs to be transferred to a higher level of care due to a worsening condition.
One sign of a deteriorating condition is impaired tissue perfusion. Impaired tissue perfusion can have a wide range of negative effects, including organ dysfunction, loss of limb, and even death (4). All nurses must be aware of the signs of impaired tissue perfusion so they can act quickly to support their patients as required.

Self-Quiz
Ask Yourself...
- How do you currently assess tissue perfusion in your patients?
- What specific signs or symptoms are you assessing for?
Causes of Impaired Tissue Perfusion
Any condition that limits blood flow can cause reduced perfusion to vital organs and distal extremities. This reduced blood flow can result in tissue death, leading to organ damage, loss of limb, or even patient death. The complicated injuries and complex mechanisms of compensation and coagulation in a trauma patient mean that the nurse needs to be aware of the various causes of impaired tissue perfusion.
Impaired tissue perfusion may be caused by hypovolemia. Hypovolemia can be caused by poor intake, or in the case of trauma by internal or external bleeding. Hypovolemia presents as hypotension – especially orthostatic hypotension – and a high hematocrit (4). Signs of internal bleeding include unexplained hypotension, decreased hemoglobin, pain, and firmness at the site of bleeding (6). Internal bleeding inside an enclosed space, such as a limb, can result in compartment syndrome. Compartment syndrome is when pressure inside a closed compartment increases to the point that nerves and blood vessels are compressed, resulting in ischemia and nerve injury (5).
Conditions that lead to decreased cardiac output such as cardiac shock, cardiac arrest, and myocardial infarction (MI), also cause decreased perfusion. The decreased cardiac output from these conditions inhibits the delivery of oxygen-rich blood to tissues, despite an adequate blood volume. Impaired blood flow because of a physical blockage, either internal (such as a thrombus) or external (too tight of a cast) can cause impaired tissue perfusion. Medications used in critical care, vasopressors or “pressers,” can decrease distal perfusion to the point of tissue death, a known risk.

Self-Quiz
Ask Yourself...
- What is one internal and one external cause of impaired tissue perfusion?
- Which organs are at risk for impaired tissue perfusion?
- What conditions do you regularly see that could cause impaired tissue perfusion?
Brain Perfusion
Impaired brain perfusion may be caused by intracranial swelling, intracranial hemorrhage, physical blockage (thrombus or embolus), hypovolemia, or low cardiac output.
The brain normally consumes about 20% of a person’s cardiac output, making it very susceptible to impaired perfusion (1). A patient’s level of consciousness is a strong indicator of brain perfusion (1). Assessing and documenting the patient’s level of consciousness, and any changes is essential in a trauma patient. Commonly used and validated tools for assessing cognition and level of consciousness include the Glasgow Coma Scale (GCS), Mini-Mental Status Examination (MMSE), and the Montreal Cognitive Assessment (MoCA) (1).
Before obvious changes, such as changes in the level of consciousness, subtle changes may be observed by asking the patient orientation questions. Ask the patient concrete questions and be consistent (1). Use the documentation tool provided by your facility to note alertness, responsiveness, and orientation.
Orientation questions may include the current season, month, president, etc. Be careful not to ask questions that are too difficult, which may frustrate patients. For example, questions about the day of the week or the specific date may be frustrating and are often confusing, even for those of us without brain trauma!
Note that there are things that can affect the level of consciousness (LOC), such as pain medication, sedation, and fatigue. Traumatic brain injuries may result in fluctuations in LOC depending on fatigue. It is essential to document changes in LOC and report trends to the provider and the next shift. Significant changes in orientation or decreases in LOC should be reported to the provider immediately, as it may indicate impaired brain tissue perfusion.


Self-Quiz
Ask Yourself...
- What questions do you ask your patient to assess orientation?
- Think about two situations that would cause impaired perfusion of brain tissue.
- What cognitive changes have you noticed that prompted further investigation?
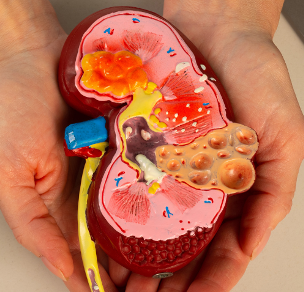
Renal Perfusion
The kidneys can be our best friends when we are assessing a patient for perfusion issues. Similar to the brain, the kidneys receive 20-25% of cardiac output making them one of the most sensitive organs to poor perfusion (7). Impaired renal perfusion may be caused by hypovolemia, low cardiac output, or physical blockage (swelling, thrombus, etc.).
The initial sign of impaired renal perfusion is low urinary output. Urinary output may be difficult to assess due to collection or documentation errors, so rising serum creatinine is another key indication of impaired renal function (2). It is easier to note accurate urinary output when the patient has an indwelling catheter, but it is also possible and important to measure output with patients using a bedpan, bedside commode, or bathroom toilet.
External catheter devices have gained popularity as an alternative to the indwelling catheter in an attempt to reduce the risk of urinary tract infections. Remember that once trauma patients are transferred to a lower level of care, they can still develop worsening conditions, and monitoring and documenting intake and output is essential for all nurses. Note that the acceptable minimum level of urine output can be considered either 30mL/hour as a general rule, or 0.5 to 1.5 mL/kg/hour for more accuracy (especially in pediatric patients) (3).
Because urinary output is essential to monitor and document, the nurse may need to advocate for an indwelling catheter for the patient with decreasing output, especially if the patient has become incontinent as their condition worsens. Keep in mind the risk for urinary tract infections and discuss the risk versus need with the provider.
In addition to low urine output, poor renal perfusion can cause an increase in blood urea nitrogen (BUN) or creatinine (7). These labs can help confirm suspected poor renal function. As a reminder, the normal range for BUN is 6-24mg/dL and normal creatinine is 0.6-1.3mg/dL (7). When the kidneys are not well perfused, they filter out less of these compounds and therefore the serum levels will rise.

Self-Quiz
Ask Yourself...
- A trauma patient was transferred to the medical floor after a week in the ICU. Their indwelling catheter remains in place as they experience bladder trauma. What is the minimum amount of urine output that you would want to observe in 12 hours?
- What does it mean if the patient does not have the minimum amount of urine output?
- What would you do?
Capillary Refill: Impaired Tissue Perfusion Assessment
Consider capillary refill time a standard part of the nursing assessment for any trauma patient, as well as post-surgical patients with limb injuries. Distal perfusion may be impaired because of hypovolemia, decreased cardiac output, blockage (thrombus or embolus), significant swelling (as seen in compartment syndrome), or medications (vasopressors). Any of these events may occur in the patient with traumatic injuries. Assess capillary refill by pinching the finger or toe at the nailbed for 5 seconds and then observing the time it takes for the blood flow and color to return to the tissue.
Normal capillary refill time in adults should be less than 3 seconds (4). It is essential to document and report capillary refill greater than 3 seconds as this may indicate decreasing peripheral perfusion and a worsening condition. Capillary refill time is both an early indicator of worsening condition and a reliable measure of improvement (4). Keep in mind that faster doesn’t always mean better with capillary refill times. Brisk cap refill may indicate acute compartment syndrome because the blood is not able to exit the tissues due to swelling and impaired circulation in the extremities (5).
Checking capillary refill time in more than one location can give you insight into total body perfusion versus perfusion to that specific area. This can help distinguish between hypovolemia – which affects the entire body – and a localized process, such as compartment syndrome or thrombus.

Self-Quiz
Ask Yourself...
- An emergency department (ED) patient with bilateral femur fractures, tension pneumothorax, and ruptured spleen has distal capillary refill times > 3 seconds. What is causing the delayed capillary refill time?
- The patient above was taken to the OR and is now in the ICU. He was given 2 units of blood and 4 liters of Lactated Ringers. Capillary refill time in his right great toe is less than 3 seconds. Capillary refill time in his left great toe is greater than 3 seconds. What are your concerns about the difference in cap refill time and what do you think is the cause?
- What is a potential treatment for this condition?
Distal Pulses: Impaired Tissue Perfusion Assessment
Limb trauma may result in decreased distal perfusion because of swelling or impaired circulation, but it may also be an indication of hypovolemia or decreased cardiac output. In an emergency, pulses closer to the heart, such as the carotid, are used to assess for a pulse. Remember this from basic life support training; we check the carotid for a pulse before starting CPR.
Assessing and documenting distal pulses and monitoring trends or changes are essential in assessing distal perfusion. Assess the radial and pedal artery pulses as a regular part of the physical assessment. Assess pulses distal to the site of injury for limb injury or vascular injury that affects that limb. It may be necessary to mark the area where the pulse is found to perform consistent assessments in that area, especially for pedal pulses. A Doppler may be necessary to confirm circulation to the area if the pulse is not palpable.
A patient may have a splint, cast, or another device in place to support the limb. If the pulse is not palpable because of a device in the way, be sure to assess and document the capillary refill frequently and note any signs/symptoms of compartment syndrome. For example, a patient with a splint from the right axilla to the mid-palm may need to have frequent assessments of the fingers since the splint blocks the radial pulse.
Placing a pulse oximeter on a digit of the affected limb is another way of assessing peripheral perfusion. Plethysmography (what we call the “pleth”) is directly related to blood flow to the digit being monitored (7). If there is a decrease in blood flow to the digit, there will also be a decrease in the pleth waveform.

Self-Quiz
Ask Yourself...
- A trauma patient with a pelvic fracture should have which pulses assessed?
- A patient has a pressure band on their right radial artery following a cath lab procedure. How does the nurse assess the blood flow to the hand?
Conclusion
While trauma patients may not be your specialty, traumatic injuries can result from a fall, motor vehicle accident, or emergency procedure. If you are asked to float to a trauma unit you may find yourself caring for a trauma patient that is believed to be stable when in fact, they are not. Changes in the patient’s condition may be subtle but indicate a serious problem. Knowing the signs of impaired tissue perfusion can help you address circulatory emergencies faster and potentially save your patient’s life or limb! Many of these concepts related to perfusion can also be applied to situations outside of trauma. Make these assessments a part of your routine so you can be the nurse who notices something is wrong sooner rather than later.

Case Study
A 23-year-old male is brought in by EMS following a motor vehicle accident. He has an open femur fracture to the right leg, four broken ribs on the left, a head laceration over the left eye, and reports severe abdominal pain. The head CT is negative for acute trauma. The abdominal CT shows a liver laceration.
- Which interventions do you anticipate putting in place to assess for impaired perfusion?
- The patient is stabilized and transferred to the ICU overnight for monitoring and to prepare for surgical fixation of the femur the next day. The night shift nurse notes a slight decrease in the right posterior tibial and pedal pulses, as well as an increase in the cap refill time. Vitals are stable, and the left leg remains within normal limits. What do you suspect is happening, and what would you do?
- The patient is taken to the OR for an emergency fasciotomy to release the pressure in the compartment surrounding the femur fracture. After the procedure, he is returned to the ICU where he struggles to maintain his oxygen saturation, and a chest x-ray reveals that he has developed a hemothorax. He has a chest tube placed and 350mL of blood drains into the collection device. While the provider reviews the labs and plans the next interventions, the nurse notices there has been no output in the patient’s urinary catheter. What do you think is the cause of the lack of urine?
- The nurse reports the lack of urine output to the provider and that they suspect poor renal perfusion. What tests can confirm the nurse’s suspicion? What treatment(s) could the nurse suggest treating this condition?
- The patient is stabilized and several days later is transferred to the medical/surgical floor. The experienced nurse advises rotating the site for the oxygen saturation probe to the right second toe. What is the purpose of this action?
- When physical therapy attempts to mobilize the patient, he becomes dizzy, lightheaded, and feels like he is going to “pass out.” The nurse helps the physical therapist return the patient to bed. When lowering the head of the bed, they recognize that the patient experienced orthostatic hypotension. What perfusion issue is happening with orthostatic hypotension?
- The patient has continued to improve and is now adequately recovered for discharge. What education related to tissue perfusion should the nurse provide to the patient and their family? What is a simple test of perfusion the patient can perform at home?
References + Disclaimer
- Finney, G., Menagar, A., & Heilman, K. (2018). Assessment of Mental Status. Neurologic Clinics, 34(1), 1–16.
- Mercado MG, Smith DK, Guard EL. Acute Kidney Injury: Diagnosis and Management. Am Fam Physician. 2019 Dec 1;100(11):687-694. PMID: 31790176.
- Urine output. (n.d.). Retrieved February 27, 2021, from https://www.cdc.gov/dengue/training/cme/ccm/page57297.html
- Kattan E, Ibarra-Estrada M, Ospina-Tascón G, Hernández G. Perspectives on peripheral perfusion assessment. Curr Opin Crit Care. 2023 Jun 1;29(3):208-214. doi: 10.1097/MCC.0000000000001038. Epub 2023 Apr 7. PMID: 37078639.
- Guo J, Yin Y, Jin L, Zhang R, Hou Z, Zhang Y. Acute compartment syndrome: Cause, diagnosis, and new viewpoint. Medicine (Baltimore). 2019 Jul;98(27): e16260. doi: 10.1097/MD.0000000000016260. PMID: 31277147; PMCID: PMC6635163.https://www.npjournal.org/article/S1555-4155(15)01044-2/fulltext6)
- Di Carlo S, Cavallaro G, Palomeque K, Cardi M, Sica G, Rossi P, Sibio S. Prehospital Hemorrhage Assessment Criteria: A Concise Review. J Trauma Nurs. 2021 Sep-Oct 01;28(5):332-338. doi: 10.1097/JTN.0000000000000608. PMID: 34491952.
- Widmaier EP, Raff H, Strang KT, Vander AJ. Chapter 14: The Kidneys and Regulation of Water and Inorganic Ions. In: Vander’s Human Physiology: The Mechanisms of Body Function. McGraw Hill; 2023:362-444.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
