Course
The Role of a Nurse in the Correctional Setting
Course Highlights
- In this course we will learn about the role of a nurse in the correctional setting and the unique patient population.
- You’ll also learn about the health disparities of incarcerated populations.
- You’ll leave this course with a broader understanding of the evolution of correctional healthcare.
About
Contact Hours Awarded: 2
Course By:
Sheila Burns
MSc, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Nurses are often unaware of the opportunities and realities of working in the correctional setting, as few nursing schools can find placements for students during their training. This course is intended for nurses who are interested in correctional nursing to understand what their role may be and the importance of it. This course will also be beneficial for current correctional nurses to review different ideas and perspectives that may help to improve their provision of care.
Introduction
Correctional Nursing is a specialty in the nursing world that gets little attention and is usually poorly funded. However, it is a specialty that is key to our community’s health and public health by upholding the U.S. Supreme Court’s 1976 ruling via Estelle v. Gamble, which established inmates as people with a constitutional right to healthcare access (1).
Over 95% of incarcerated people are released back into the community at some point; however, 75% of those are expected to be reincarcerated (1). Of the 2.3 million incarcerated citizens in the United States, approximately 80 to 90 percent are afflicted with acute and chronic health problems. These include infectious disease, long-term illness, and mental health and substance abuse conditions (2).
Nurses often need to be made aware of the importance of the opportunities and realities of working in this setting, as only some nursing schools can find placements for students to be exposed to during their training. This article is intended to allow nurses interested in correctional nursing to determine their role and allow current correctional nurses to review different ideas and perspectives that can enable them to improve their care provision.
Evolution of Correctional Health Care
Nursing, as a profession, is ever-evolving and changing. Nurses are constantly pioneering and working within a research-driven environment. The profession is supported by a multidisciplinary team of medical and nursing personnel who can collaborate effectively and are all focused on the same goal. Unfortunately, correctional institutions are silos that make equitable access to healthcare challenging (3).
Correctional nursing is a minor specialty involving a smaller team environment with limited access to resources such as training, research, staffing, etc. Correctional nurses face a different financial outlook than privately or publicly funded specialties and institutions. Correctional healthcare is reliant upon national or local funding determined by the government. This minor sector accounts for approximately 0.5% of the registered nurse population; thus, extra-curricular services, such as research, are not prioritized in this environment (3).
Literature and data may also be gained from international perspectives on the nursing profession in correctional settings. The World Health Organization (WHO) has been active in prison health care since the Ottawa Charter for Health Promotion in 1986 (1). This charter provided the impetus for the Health Promoting Prison (HPP) movement in which 25 European and former Eastern Bloc countries participated (to varying degrees).
Within this movement, progress was made with documents/reports related to mental health promotion topics, prison health as a part of public health, HIV in Prisons, Drugs, and Society, and promoting young people’s health. For the past 40 years, the WHO has promoted an organizational commitment to correctional health care, including policy and lawmakers at the government level, right down to the facilities’ security and health team.
***Note: Jails and Prisons are interchangeable when discussing correctional settings abroad. Some countries house all prisoners in the same building and call it a “jail” or “prison” – this does not distinguish their legal standing).
Unfortunately, there is no similar information regarding the U.S. using this method to progress correctional care (1). Studies on health disparities of inmates within the U.S. population have found an increase in infectious diseases, cancer, asthma, hypertension, and blood-borne pathogens, such as hepatitis C and HIV (6,7).
The U.S. Constitution set the standard that there is no right to healthcare. Several landmark court cases have challenged that this indifference may be considered a paradox toward standards of decency. The courts have overall maintained that negligent medical treatment must be grossly incompetent, deviate highly from standards, and that a severe medical threat must be defined by symptoms of degeneration, extreme pain, and the threat of impending death (5, 6).
The U.S. has the National Commission on Correctional Health Care (NCCHC), established in 1983. Their mission is “to improve health care quality in jails, prisons, and juvenile confinement facilities. NCCHC establishes standards for health services in correctional facilities, operates a voluntary accreditation program for institutions that meet those standards, produces resource publications, conducts educational conferences, and offers certification for correctional health professionals” (4). The NCCHC is the gold standard. Still, there is no government policy to ensure that all facilities abide by these standards– being accredited by NCCHC is optional.

Self-Quiz
Ask Yourself...
- In your facility, do you perform any research?
- What kind of research do you think would benefit correctional nursing?
- Have you been part of any improvements – small or large – in your facility?
Who are our Patients?
To identify a nurse’s role, we first need to identify our patients. It can sometimes become overwhelming with the comings and goings in a correctional setting. Unlike a hospital setting or a long-term care facility, correctional nurses often care for hundreds of patients at one time. Therefore, efficiently identifying the patients who require time and care is essential to nursing within this field.
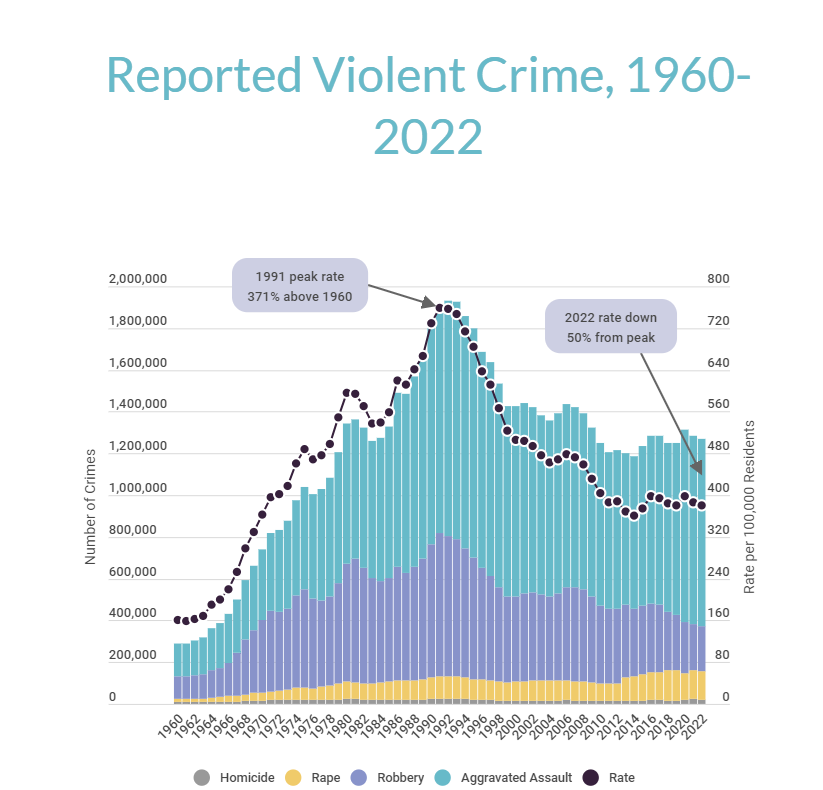
Our patient population is directly affected by what is happening in other spheres. It is essential to understand where we stand today with regard to the pressures of jail. Looking at crime and imprisonment rates in the graph below shows a dramatic increase in the 1990s despite a reduction in homicide rates, motor vehicle thefts, and burglary (5). So, what happened?
In the 1960s, when the major mental health institutions that housed the mentally ill closed, and the community resources were not prepared nor equipped to deal with this need. One study showed that this accounted for around 7% of the increase in jails and prisons from the 1980s to 2000 (5, 6).
There were also some politically based decisions made to deal with the drug issue in the 1980s. This led to an increase in drug crime penalties, including minimum sentencing and the “three-strikes” law, leading to people needing to serve 85% of their sentence (6). Lawmakers directly impact our patient population, from the massive increase in population shown in the graph to the more recent decrease in population due to the COVID-19 pandemic.

Self-Quiz
Ask Yourself...
- Have you noticed an increase or decrease in your patient population?
- Does this impact the type of work you can do?
Health Disparities of Incarcerated Populations
Today, 64% of patients being incarcerated in jails have mental health disorders (6), and 65% qualify as having substance abuse or addiction to drugs and alcohol (5,6). It is also widely reported that substance/alcohol abuse is interlinked with mental health issues.
40% of all incarcerated patients have a chronic medical condition (7). The prevalence inside facilities is higher in specific disease groups than in the general US population, as shown in the chart below (9).
| Disease | % US Population | % Incarcerated Population* |
| Diabetes | 6.5% | 9.8% |
| Hypertension | 25.6% | 29.4% |
| Asthma | 7.5% | 8.7% |
| HIV | 0.5% | 1.4% |
*This percentage of incarcerated population includes both federal and state facilities.
Demographics are also crucial factors to consider. 9.8% of incarcerated people are females (7). Females have different medical and nursing needs than men do, and healthcare must be flexible enough to manage this, especially with pregnancy and childbirth issues.
The racial disparities are also a reflection of community and governance issues outside the jail walls. 40% of the inmate population is African American, despite being only 13% of the U.S. population. Hispanics are also disproportionately detained – 20% of the inmate population but only make up 17% of the U.S. population (7). Health issues that are more prevalent in the African American population, for example, such as hypertension or sickle cell disease, reflect the need for a robust health system.

Self-Quiz
Ask Yourself...
- Think of your facility – what is the racial mix?
- Does this bring different challenges to how you can deliver care?
- Do you look after females?
- If so, what extra care plans are in place to ensure they are appropriately cared for?
Nurses’ Role
If you are reading this to discover what happens inside a correctional facility, this section might be for you! Correctional nursing is a constant challenge to your personal growth and being able to hone in on your clinical assessment skills.
The environment in which correctional nurses work could be more conducive to good health. It is quite the opposite. For a human being to be kept in a small space with limited access to socializing, a poor diet, minimal exercise, and no personal growth is nowhere near a healthy existence. Not only are the patients’ conditions poor, but the system we must work within is focused on security, and thus, delivering care is met with challenges.
This is when nurses can excel by being innovative and determined to deliver the care that our population needs. Thinking of your community is a great coping tool when faced with a complex case. This difficult patient will more than likely be released, and getting his or her health care to a gold standard will positively impact not only their life but your community’s health, too. This is the adage that Prison/Jail Health is part of Public Health that comes to the fore. Acknowledging biases before working in the correctional environment can prevent barriers to providing compassionate, patient-centered care. Identifying barriers to care, as well as being an advocate for improved healthcare conditions among noted deficiencies, will assist the nurse in remaining person rather than prison-focused (4).
A correctional nurse’s role varies from facility to facility; however, there are consistencies in job responsibilities in any correctional setting.
Intake and Screening
All patients should be screened on arrival to the facility to “ensure that emergent and urgent health needs are met” (8). Once the patient’s potential immediate needs are identified and managed – such as injuries, intoxication, psychosis, and the potential for being contagious, the nurse must spend some concentrated time with the patient for further investigation.
Obtaining a comprehensive medical and psychiatric history sets the care pathway for the patient on a solid trajectory. The receiving screening is often referred to as a pivotal point when we can get information on a patient’s needs. If we miss this opportunity, patients can miss out on vital intervention later in their incarceration. For example, the receiving screening is the first examined document during morbidity or mortality reviews. This allows the team to look for improvements in how questions are worded or if a question was not included, which may have prevented the negative outcome.
Being in the moment with the patient is essential to the assessment. Often, our patients are not happy to be where they are, belligerent, intoxicated, and sometimes aggressive. Being able to empathize with the patient is essential.
It is often particularly challenging to empathize with someone you know may have done something heinous. However, it is our job to determine their medical and psychiatric needs. The assessment still needs to be made, and care must be provided to ensure their pathway is the same as everyone else’s.
A patient’s security is also part of our assessment outcomes. Placing an 18-year-old male with educational difficulties in for his first arrest as ready for the general population is not protecting our patients. We must alert security staff to our findings and work with them to protect vulnerable patients.
Follow-up care is also a critical process that the intake nurse must activate. Chronic Care services, Mental Health Services, Dental Services, Chaplain Services, Medication Verification, Medical Records from an outside Provider, etc., are all follow-up care that the intake nurse can implement.

Self-Quiz
Ask Yourself...
- Do you feel empathetic to someone who has been arrested for a heinous crime?
- Does knowing what the patient has been accused of change the way you may treat them?
Case Study:
Cindy is a 23-year-old female. It is her first time in jail, and she presents extremely intoxicated. Cindy states she has had six shots of vodka and has verbally admitted to consuming cocaine. She also states that she takes benzodiazepines for anxiety. She admits to currently seeing a psychiatrist for her suicide attempt three months ago. During your assessment, you find she is pregnant, and she has no idea when her last period was.
Who does Cindy need to see?
How urgent do you think Cindy’s needs are?
What personal security concerns do you have for Cindy?
Our actions, or inactions, with Cindy can have a long-lasting effect on not just Cindy’s health but on her unborn baby.
What could happen to Cindy if we did nothing?
It is vital for the nurse to be able to recognize all the services that Cindy may needs. This may involve an urgent referral to OB/GYN or potentially ER, depending on the site’s relationship with the local specialties.
A referral to the Mental Health team would be appropriate for her history and to support her regarding her pregnancy. A medication verification form and medical records request form may also need to be sent to the Pharmacy/Doctor’s Office to support the Mental Health team in their care pathway.
If the Chaplain deals with diet preferences, it may be an option to help her with that process too.
Security will also need to be made aware of Cindy’s vulnerability and her pregnancy status to allow them to house her in a protected area.
Working in intake and completing receiving screenings can be an incredibly challenging job. There are often time pressures put upon the nurse to get patients processed quickly. Using communication skills to the highest level – from watching, actively listening, honing in on specific information, focusing your attention on clinical assessments, and being in the moment with your patient helps not only get the task completed but also gathers quality information for the patient to be on the correct care pathway.
Medication Administration
Medication administration is a large part of nurses’ role in the correctional setting, as in most settings.
The Pharmaceutical service setup can vary significantly from facility to facility. In some facilities, correctional officers administer medications, some have Medication Technicians, and some rely purely on the nursing staff.
Either way, patients have the right to receive their treatment promptly (8).
Along with the actual medication administration, nursing staff often fulfills medication orders. The nurse’s responsibility is to ensure that patients have their medications and that new orders from Providers are fulfilled.

Self-Quiz
Ask Yourself...
- Think of your facility – how many obstacles get in the way for you to administer medications on time?
Non-Emergent Health Care Requests – Sick Calls
Incarcerated individuals have no choice about who provides their care, but they do have the right to access care. In some facilities, patients can access an internal system to electronically complete a form to describe their health needs. In other facilities, the patient completes a paper form, which is picked up by the nurses and managed appropriately.
The challenge for the nursing team is time management. Sick calls can be highly time-consuming, and the ill call list can be extensive in large facilities. A face-to-face encounter must be conducted within 24 hours of receiving the sick call, and an evaluation must be completed in a clinical setting (8).
Clinic Care
A medical center is usually inside a facility – from a tiny clinic room to numerous clinical spaces and even short-term accommodations for medical observations.
The nurse’s role in the clinic is to manage the patient load, similar to an outpatient clinic in the community. Providers are often in the clinic rooms with patients referred from the sick call process for emergent/urgent issues and see patients with chronic care issues. The nurses work alongside these providers to take vital signs before the appointment and conduct other tests, such as EKGs, lab draws, urine samples, and so on, during or after the provider’s appointment.
The clinic can also have outside healthcare professionals seeing patients. Physical Therapists, X-ray technicians, Dental Services, and Telehealth sessions for various specialists, for example, are supported by the nursing team.
Initial Health Assessments are also a nurse’s responsibility within the correctional setting. All patients must complete this assessment before Day 14 of their stay in the facility (11). This assessment consists of reviewing the screening information, asking more detailed questions regarding identified issues, and physically examining the patient. Any immediate needs are referred to the appropriate level of care.
Emergency Response
Emergency calls happen regularly, and it is the role of the nurses to respond without delay. According to the National Commission on Correction Health Care, protocols must be developed to guide the response and treatment of emergencies. State regulatory acts and ensuring that medical treatment is delivered within the scope of the individual’s training and license are adhered to (8).
Emergency equipment, whether in carts or bags, should be available at a moment’s notice. This includes everything from Band-Aids to Glucose tablets to a defibrillator. The emergency bags should be checked every shift, with documentation of the daily check, and restocked after every use.
Educational aspects of this practice may require several days’ worth of training for nurses. The nursing role in these situations is similar to that of emergency medical personnel and may be unfamiliar to new hires. Specialized training or experience may be needed to function effectively in a jail or prison when a medical emergency arises (8).
As a result, the nursing team must have a strategy for answering emergency calls –who has what role, etc. to maximize the chances of a positive outcome for the patient. Using critical thinking skills, completing a primary and secondary assessment of the patient, and deciding on the best level of care are key factors.

Self-Quiz
Ask Yourself...
- Does your facility have an emergency response plan for individual emergencies?
- Who takes responsibility for the emergency equipment?
- Does your facility have a plan for a mass disaster?
- Think of a time when you have had to respond to an emergency with a positive or negative outcome. What skills did you feel comfortable using, and what skills did you feel you lacked?
Conclusion
Correctional health services continue to evolve, improve, and respond to the needs of their patients. The nurse has a pivotal role in identifying gaps in care provision and working locally to improve patient outcomes.
There are many challenges to being a correctional nurse, most coming from political and judicial structures and the fact that the environment in which we work is fundamentally unhealthy. Also, the patients we serve are often the most vulnerable in society and have complex medical and mental health issues.
The nurse’s role involves wearing many hats (not all roles are described above) – from handing out eyeglasses to responding to a mass disaster. Maintaining standards of care and using NCCHC (8) as a platform will enable nurses to focus on optimum patient care.
References + Disclaimer
- Nutbeam, D., Corbin, J. H., & Lin, V. (2021). The continuing evolution of health promotion. Health Promotion Internation, 36(1), i1-i3. https://www.doi.org/10.1093/heapro/daab150
- Wirmando, W., Astari, A., & Yuliatun, L. (2021). Caring for criminals. International Journal of Caring Sciences, 14(2), 1034-1044. Retrieved from https://www.internationaljournalofcaringsciences.org/docs/25_wirmando_original_14_2.pdf
- Solell, P., & Smith, K. (2019). ‘If we truly cared’: understanding barriers to person-centered nursing in correctional facilities. International Practice Development Journal, 9(2), 1-17. https://www.doi.org/10.19043/ipdj.92.007
- https://www.ncchc.org/about
- Council on Criminal Justice. (2024). Tracking the size of America’s criminal justice system. In The Footprint. Retrieved from https://counciloncj.foleon.com/the-footprint-trends-in-crime-arrests-and-the-total-correctional-population/the-footprint/
- The Sentencing Project. (2024). Mass incarceration trends. Retrieved from https://www.sentencingproject.org/app/uploads/2023/01/Mass-Incarceration-Trends.pdf
- U.S. Department of Health and Human Services. (2024). Incarceration. In Social Determinants of Health Literature Summaries. Retrieved from https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/incarceration
- National Commission on Correctional Health Care. (2018) Standards for health services in jails. NCCHC.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
