Course
Understanding the Different Types of Strokes
Course Highlights
- In this course we will learn about the non-ischemic causes of a stroke, and why it is important for nurses to recognize early symptoms for all types of strokes.
- You’ll also learn the causes of subarachnoid, intracerebral, and intracranial hemorrhages.
- You’ll leave this course with a better understanding of how to calculate cerebral perfusion pressure.
About
Contact Hours Awarded: 1.5
Course By:
Joanne Kuplicki
MA, RN, ccrn, Nc-bc
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Nurses are at the forefront of recognition and treatment of all types of strokes. It is imperative that we as nurses are aware that there are multiple causes and types of strokes, each of which has a varied treatment. The health care team must be mindful of newly recognized treatments for strokes related to the anatomical disorder causing it. Ischemic stroke is still the leading cause of a stroke, but we will expand our knowledge of other reasons for it during this course. The entire multidisciplinary team can make a difference in patient outcomes with swift assessment and treatment of the several types of strokes.
Epidemiology
Worldwide, stroke is the second leading cause of death, affecting 101 million people, with one new person diagnosed with a stroke every three seconds (1). Approximately one in every four people on the planet will suffer from a stroke in their lifetime; that number has grown by 50% in less than two decades (1). With all types of strokes considered, men and women are affected about equally throughout the world, though the incidence is higher in American women than their male counterparts (1,4). In the U.S., stroke is the fifth leading cause of death and the leading cause of disability (3).
Even during the recent COVID-19 worldwide pandemic, the World Health Organisation (WHO) still considered strokes a public health emergency (2). \The American Stroke Association (ASA, website: https://www.stroke.org/) and World Stroke Organization (WSO, website: https://www.world-stroke.org/) provide public and professional education links and materials for all. World Stroke Day occurs on October 29 yearly to increase public awareness of all types of strokes and prevention.

Self-Quiz
Ask Yourself...
- Are you aware of your organization’s stroke awareness activities?
- If your organization does not have any current activities for stroke awareness, particularly in October, what resources can you share with management to help introduce the topic?
- What would you describe as causes and risk factors for stroke?
- How do you screen patients for stroke in your practice and out in the community?
- What teaching do you have for your patients regarding ways they can reduce their risk of stroke?
Stroke Causes
Strokes occur when the blood vessels that carry oxygen and nutrients to the brain are either blocked by clots or bursts (ruptures), causing reduced blood flow and oxygen (3). As much as 80% of strokes are preventable, increasing the need for patient/family education and the aggressive treatment of risk factors (3).
The main risk factors for strokes are as follows (4,10):
- High blood pressure
- High cholesterol
- Heart disease, especially coronary artery disease, and atrial fibrillation
- Diabetes
- Obesity
- Sickle cell disease
Furthermore, the following factors increase the risk of having a stroke (4):
- Diets high in trans/saturated fats and cholesterol
- Lack of regular physical activity
- Drinking too much alcohol
- Using tobacco products
- Genetic factors
- Age (one in seven strokes occur in those ages 15-49; after age 55, the chance of having a stroke doubles every ten years)
- Sex (women are more likely to die from strokes than men; pregnancy and birth control pills increase the risk of stroke)
- Race (non-Hispanic Black or Pacific Islander)
- Suffering a fall or other trauma while also on anticoagulant therapy
Nurses are often given rigorous training in recognizing and treating several types of strokes. However, we often make assumptions that a clot leading to an ischemic stroke is the main culprit since it is the cause of approximately 87% of strokes in the United States (5).
Ischemia, or inadequate blood supply, occurs from a blockage or clot, and transient ischemic attack (TIA) occurs when a temporary blockage or clot causes shorter and often fleeting symptoms. Some refer to TIA as a “mini-stroke.” TIAs should be taken seriously because they can increase the risk of a stroke (3). A cryptogenic stroke is one in which the cause cannot be determined and accounts for one in three ischemic stroke cases (6). Some possible underlying causes of these cryptogenic strokes might include atrial fibrillation, heart structure problems (i.e., patent foramen ovale), extensive artery atherosclerosis, or thrombophilia (6).

Self-Quiz
Ask Yourself...
- Have you had a patient or client in your practice who described symptoms of stroke, though you may have thought nothing of them? For example, “I slept on my arm,” or “I get weak when I overdo activities since I am older,” or “My speech was slow for a moment, but quickly became normal again.”
- what assessments would you want to do on the patient in these cases?
- What education would you give them at the moment?
- What interventions might you anticipate in the short- and long-term?
Let us discuss other reasons strokes occur. Even if they are not as common as ischemic strokes, they may undoubtedly be more devastating.
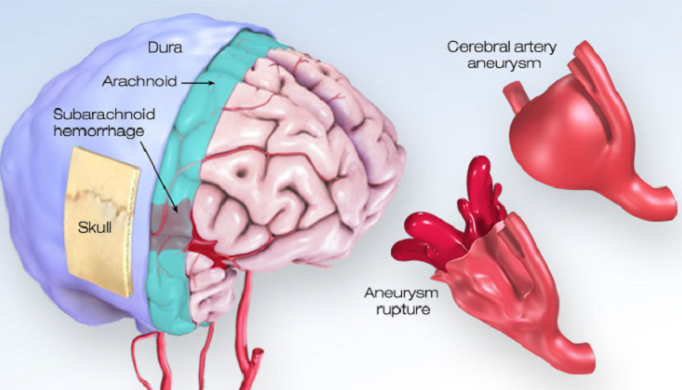
Hemorrhagic strokes account for approximately 13% of all strokes and occur when there is bleeding into the brain or the layers between the brain and the skull (3). Brain bleeds themselves are also called intracranial hemorrhages and are common after traumas like falls or motor vehicle accidents. To discuss the different types of hemorrhagic strokes, let us first refresh our knowledge about the three meninges, or membrane layers, between the skull and the brain. First, there is the dura mater (closest to the skull), then the arachnoid space (in the middle), and finally, the pia mater (closest to the brain) (7).
There are two main types of intracranial hemorrhages: inside the skull, outside the brain tissue, and inside the brain tissue itself. Further broken down, these stroke categories are as follows (7):
- Inside the skull, outside the brain tissue:
- epidural (between skull & dura mater, the outermost membrane layer)
- subdural (between dura mater and arachnoid membrane)
- subarachnoid (between the arachnoid membrane and pia mater)
- Inside brain tissue:
- intracerebral hemorrhage (in the lobes, brainstem, and cerebellum; anywhere within the brain tissue)
- intraventricular bleeding (in the ventricles, where cerebrospinal fluid is made)
Approximately 10% of hemorrhagic strokes are intracerebral, and 3% are subarachnoid; thus, these are the types that will be discussed below(3).

Self-Quiz
Ask Yourself...
- How would you explain the difference between an ischemic and hemorrhagic stroke to a patient and their family?
- How would you describe the subtypes of hemorrhagic strokes?
- Why do you think hemorrhagic strokes are so fatal?
- What might be risk factors for hemorrhagic strokes that are not present for ischemic strokes?
The Danger of Intracerebral Hemorrhages
Even though ischemic strokes are far more common than their hemorrhagic counterparts, it is this latter category that is particularly deadly and debilitating. For intracerebral hemorrhages (also called ICH, which occur within the brain tissue itself), mortality rates within 30 days are as high as 50% (8). Only about 27% of survivors are functionally independent after three months (8).
Subarachnoid Hemorrhage
A subarachnoid hemorrhage (SAH) results from bleeding within the brain’s subarachnoid space, which can also lead to inferior outcomes. Roughly 40% of patients diagnosed with a subarachnoid hemorrhage will have a fatal outcome within a month of onset (8). The team must recognize this occurrence early due to the high risk of morbidity and mortality.
Additionally, there are subcategories of SAHs. These are (10):
- Traumatic vs. non-traumatic
- Aneurysmal vs. non-aneurysmal
- Aneurysmal SAHs occur after a cerebral aneurysm ruptures, causing bleeding into the subarachnoid space.
- Non-aneurysmal SAHs occur most commonly with a blunt head injury, non-penetrating trauma, or sudden acceleration changes to the head, as in a car accident.

Self-Quiz
Ask Yourself...
- What type of physical activity would you consider ” a risk factor for patients who are already at risk for hemorrhagic strokes?
- Why do you think gyms/fitness classes have participants sign a waiver recommending a physical/practitioner clearance before participation?
- In which cases could you anticipate encouraging or discouraging certain types of exercise for patients based on their risks for different kinds of strokes?
Nurses can recognize any subtle neurological changes within a patient and report any decline in time for early intervention management. This type of bleeding in the subarachnoid space can be triggered by exertion, hypertension, and other stressful situations. Both situations increase the pressure within the blood vessels.
Presentation of Subarachnoid Hemorrhage
Subarachnoid hemorrhage has a distinct presentation in patients as the worst headache of their life (also known as a “thunderclap headache;” 10); signs and symptoms are all related to an increase in intracranial pressure. Presentation of an SAH can also include nausea, vomiting, seizures, decreased/loss of consciousness, dizziness, nuchal rigidity, and diplopia (10). The hemorrhage creates edema in the brain that compresses nearby brain tissue, causing neurological changes. There is a higher incidence of intracerebral hemorrhage among populations with hypertension, including African Americans (10).
Intracerebral Hemorrhage:
Intracerebral hemorrhages (ICHs) are another subcategory of intracranial hemorrhages. The bleeding that occurs within the brain from an ICH is due to either traumatic or non-traumatic events; the non-traumatic type accounts for 10-15% of all strokes and is highly deadly and debilitating (10). In an ICH, a hematoma is formed in the brain’s parenchyma and may extend into the ventricles (10).
A patient’s prognosis can generally be predicted depending on the location and size of the hematoma in an ICH. As many as 50% of those with an ICH die within 30 days, most of those within the first 24 hours of presentation (10). Patients presenting with a Glasgow Coma Scale (GCS) of less than nine and a clot size of 60mL or more have a 90% mortality rate (10). For those who do survive, only 20% of them are autonomous six months after the hemorrhage (10).
Mini Case Study:
While giving birth to her first child, your 30-year-old African American patient experienced a lot of bleeding during the later stages of labor. Throughout her pregnancy, your patient had both gestational hypertension and gestational diabetes. Several hours after giving birth, she was still having postpartum hemorrhage (PPH). Shortly after the PPH, you note that she became obtunded, so she was emergently transferred to the surgical ICU. After imaging was acquired, the patient was diagnosed with a cerebral aneurysm. The labor and delivery (L&D) staff had a huddle about this patient since many of them had never seen a case like this before.

Self-Quiz
Ask Yourself...
- What assessment findings would the L&D nurses mark as red flags for indicators of a postpartum cerebral aneurysm (or subsequent hemorrhage)?
- What, if anything, could have helped reduce the patient’s risk factors before this event?
- What, if anything, can be done to improve the odds of the patient’s return to baseline after intervention?
- What teaching should be done to all expectant mothers regarding their increased risk of stroke?
Treating Strokes
There is an adage in the healthcare profession that “time is the brain,” since approximately 1.9 million neurons die each minute of an untreated large vessel stroke (11). Thus, the faster a stroke is recognized, the better the outcome for the patient. This concept is so crucial in the American hospital setting that the American Heart Association sets strict time guidelines to get suspected stroke patients the fastest care possible. Some of these guidelines include (11):
- Door-to-provider time: 10 minutes
- Door-to-neurology consult: 15 minutes
- Door-to-CT: 20 minutes
- Door-to-CT interpretation: 45 minutes
- Door-to-thrombolytics: 60 minutes
- Door-to-puncture time (if endovascular intervention): 90 minutes
- Door-to-recanalization: 120 minutes
- Door-to-ICU (or stroke unit) admission: 3 hours
Once a stroke is identified as ischemic or hemorrhagic, there is generally a set path of treatment that needs to be implemented in a highly timely manner.
For ischemic strokes, the IV thrombolytic alteplase (tPA) has been used for many years. However, tenecteplase (TNK) is becoming increasingly popular in treating cerebrovascular accidents (12). Thrombolytics are given within a specific time (usually 3-4 hours) of the patient’s last-known well (LKW), and other criteria must be met as well (11, 12). Another option for some patients, depending on a variety of factors, is an endovascular mechanical thrombectomy (MT), wherein the clot is surgically removed from the patient’s brain (11). An MT’s primary advantage over thrombolytics is that it can usually be done within 24 hours after the LKW, allowing a much greater treatment window (11).
For hemorrhagic strokes, the mainstay of treatments is first controlling the bleeding and associated effects. This usually includes rapid-sequence intubation (RSI), vigilant blood pressure management, a fast neurosurgery consult, and coagulopathy correction, possibly including the reversal of anticoagulation therapy the patient had been on (11). Surgical options include aneurysm clipping, blood transfusion, coil embolization, draining excess fluid in the brain, craniotomy, or measures to remove or shrink arteriovenous malformations (AVMs) (13).
Regardless of the cause, all stroke patients will need to be very carefully monitored for the first 24 hours after the incident, since this is when most complications occur (8). This includes ensuring the patient has a frequent and complete neurological assessment, that they are hemodynamically stable, and that there are no further signs of deterioration. If the patient survives, a good deal of follow-up care and education will be necessary, likely for the rest of their lives. Fortunately, as nurses, we can help improve their long-term outcomes by being vigilant in identifying and caring for strokes.

Self-Quiz
Ask Yourself...
- If you’re taking care of a potential stroke victim, why is it essential to identify the type of stroke as soon as possible?
- What interventions could you anticipate and prepare for if your patient has an ischemic stroke? What parameters should be measured for this type of treatment?
- What would you anticipate for a patient with a hemorrhagic stroke?
- What teaching should you provide to the family during the interventions?
- How can you improve your neurological assessment skills to identify stroke symptoms in a faster manner?
Conclusion
Since strokes affect such a large number of people worldwide, nurses must be able to identify and help treat these afflictions quickly. Knowing the different types of strokes will enable the nurse to anticipate the proper treatment modality for each efficiently. With these measures in place, we have the power to vastly improve both the quality and length of life for many of our patients and ourselves.
References + Disclaimer
- Feigin, V. L., Brainin, M., Norrving, B., Martins, S., Sacco, R. L., Hacke, W., Fisher, M., Pandian, J., & Lindsay, P. (2022). World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. International Journal of Stroke, 17(1), 18–29. https://doi.org/10.1177/17474930211065917
- Zedde, M., & Pascarella, R. (2023). Stroke Is an Emergency, Even During a Pandemic. Chest, 163(3), 471–472. https://doi.org/10.1016/j.chest.2022.11.017
- American Stroke Association. (2021) About Stroke. https://www.stroke.org/en/about-stroke
- Centers for Disease Control and Prevention. (2023). Know Your Risk for Stroke. https://www.cdc.gov/stroke/risk_factors.htm
- American Stroke Association (2024). Ischemic Stroke (Clots). https://www.stroke.org/en/about-stroke/types-of-stroke/ischemic-stroke-clots
- American Stroke Association. (2024). Cryptogenic Stroke or Stroke of Unknown Cause. https://www.stroke.org/en/about-stroke/types-of-stroke/cryptogenic-stroke
- Cleveland Clinic. (2023). Brain Bleed: When to Call for Help. https://my.clevelandclinic.org/health/diseases/14480-brain-bleed-hemorrhage-intracranial-hemorrhage
- Mahlamäki, K., Rautalin, I., & Korja, M. (2022). Case Fatality Rates of Subarachnoid Hemorrhage Are Decreasing with Substantial between-Country Variation: A Systematic Review of Population-Based Studies between 1980 and 2020. Neuroepidemiology, 56(6), 402–412. https://doi.org/10.1159/000526983
- Woo, D., Comeau, M. E., Venema, S. U., Anderson, C. D., Flaherty, M., Testai, F., Kittner, S., Frankel, M., James, M. L., Sung, G., Elkind, M., Worrall, B., Kidwell, C., Gonzales, N., Koch, S., Hall, C., Birnbaum, L., Mayson, D., Coull, B., … Langefeld, C. D. (2022). Risk Factors Associated with Mortality and Neurologic Disability After Intracerebral Hemorrhage in a Racially and Ethnically Diverse Cohort. JAMA Network Open, 5(3), e221103. https://doi.org/10.1001/jamanetworkopen.2022.1103
- Tenny, S., & Thorell, W. (2023). Intracranial Hemorrhage. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK470242/
- Gartley, C. E. (2023). Time is brain. American Nurse. https://www.myamericannurse.com/time-is-brain/
- Kobeissi, H., Ghozy, S., Turfe, B., Bilgin, C., Kadirvel, R., Kallmes, D. F., Brinjikji, W., & Rabinstein, A. A. (2023). Tenecteplase vs. alteplase for treatment of acute ischemic stroke: A systematic review and meta-analysis of randomized trials. Frontiers in Neurology, 14, 1102463. https://doi.org/10.3389/fneur.2023.1102463
- National Heart, Lung, and Blood Institute. (2023). Stroke—Treatment. https://www.nhlbi.nih.gov/health/stroke/treatment
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
