Course
Basic Ventilator Management
Course Highlights
- In this Basic Ventilator Management course, we will learn about the mechanism of action of invasive and noninvasive ventilation.
- You'll also learn the basic modes of mechanical ventilation.
- You'll leave this course with a broader understanding of essential nursing care for the invasive and non-invasive ventilated patient.
About
Contact Hours Awarded: 2
Course By:
Abbie Schmitt
RN, MSN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Ventilator management can be an intimidating subject, especially if the user is not savvy with technology. Fortunately, modern ventilator manufacturers have put significant effort into making ventilators “user-friendly”. This course will further support those who manage ventilators. We will discuss basic respiratory function, the types and mechanism of action of ventilators, and indications for use. It is also important to gain understanding of the settings, modes, alarms, and essential nursing care.
Ventilator Fundamentals
Mechanism of Action
Knowledge of basic respiratory function is essential for understanding mechanical ventilation (MV). The respiratory system is comprised of the airway, lung, and chest wall. Respiratory mechanics represents the lung function in terms of pressure, gas flow, and volume (1).
Pressure refers to the physical movement of the lungs and chest wall muscles. During spontaneous and unassisted inspiration, our lungs expand due to the transpulmonary pressure caused by negative pleural pressure that is created by the inspiratory muscles (2). Essentially, the lung spontaneously pulls inwards while the chest wall pushes outwards.
Gas exchange refers to the process of transferring atmospheric oxygen (O2) from the alveolar gas into the bloodstream and carbon dioxide (CO2) from the bloodstream transferred to the alveolar gas phase; CO2 is then eliminated into the atmosphere by ventilation (1). Gas exchange occurs within areas of the lung lined by alveoli, which are tiny air sacs encased in capillary beds (1).
Volume simply refers to the amount of airflow, which is affected by factors such as lung elasticity, space to expand, presence of fluid, and surface tension.
The mechanism of action of mechanical (artificial) ventilation had evolved over time. The first type of mechanical ventilators provided negative pressure ventilation, which applied external negative pressure to mimic chest muscle pressure (1). Although it was helpful and prolonged life to many patients, this method was not effective for gas exchange abnormalities.
Controlled positive pressure ventilation was first applied in 1952 and pushes air into the central airways, causing air to flow into distal airways and alveoli (1). Positive pressure does not work in the same way as spontaneous respiration, which is negative pressure. This forced airflow provides the encounter for gas exchange to occur. This airflow also provides pressure that prevents the alveoli from collapsing.
Types
As we discussed, modern mechanical ventilators apply positive pressure that pushes air into the lungs. The types of positive pressure ventilators include invasive and noninvasive.
Invasive Mechanical Ventilation. Invasiveness refers to the intrusion of medical instruments into the body. In invasive ventilation, a tube from the ventilator is connected to the airway. When a tube enters the mouth and into airway, it is called intubation. A tracheostomy is utilized when the tube must enter the airway through the trachea (2).
Noninvasive Mechanical Ventilation. A noninvasive ventilation type is less intrusive into the body cavities. A facemask with straps is typically used.

Figure 1. Algorithm for Types of Ventilation. Photo credit: (1)
Understanding Ventilation Terminology
Ventilation describes the bulk movement into and out of our lungs (3). Ventilation can be categorized into tidal volume (VT), respiratory rate (f), and minute ventilation (VE). Tidal volume is the volume of gas exhaled following a normal inspiration; respiratory rate is the number of breaths taken over one minute; minute ventilation is the tidal volume times the respiratory rate (3). These will be important terms as we review mechanical ventilator settings and modes.
Ventilator capacity refers to the amount of air that a ventilator pump can push into the lungs. The ventilatory capacity is significant because this amount must be sufficiently maintaining tissue oxygenation and carbon dioxide (CO2) removal (3). When you hear the term respiratory drive, think about the neurological system driving the respiratory vehicle. Essentially, breathing is generated by neuron activity located in the brainstem, which produces a neural signal directed to respiratory muscles to create inspiratory effort and tidal breathing (4). There are receptors that monitor carbon dioxide levels in the body and when a high level of carbon dioxide is detected a signal is sent to stimulate the drive to breathe to blow off the excess carbon dioxide (5). Essentially, the level of carbon dioxide dictates the drive to breath and the respiratory rate.

Self Quiz
Ask yourself...
- Have you ever cared for a patient on a mechanical ventilator?
- Can you explain how the physiology of the lungs (airway, alveoli) impacts gas exchange?
- Can you describe the difference in pressure between spontaneous breathing and mechanical ventilation?
- The nervous system is a vital part of the breathing process. Have you ever performed a neurological and respiratory assessment with abnormal findings?
Indications for Use
Mechanical ventilation is indicated when spontaneous breathing is insufficient (tachypnea, hypercapnia) or absent (apnea). Respiratory failure is the inability of the heart and lungs to adequately supply the tissue with oxygen and remove carbon dioxide (3).
Indications for Invasive Mechanical Ventilation
Compromised or Diseased Airway: (4)
- Trauma to airway
- Oropharyngeal infection.
- Proximal airway obstruction
- Angioedema
- Anaphylaxis
- Distal airway obstruction
- Asthmatic bronchospasm
- Acute exacerbation of chronic obstructive pulmonary disease (COPD).
Hypoventilation: (4, 5)
- Impaired central drive
- Pharmacology or illegal drug overdose
- General anesthesia for surgery
- Traumatic brain injury
- Respiratory muscle weakness
- Muscular dystrophy and myositis
- Peripheral nervous system defects
- Guillain-Barré syndrome
- Myasthenic crisis
- Restrictive ventilatory defects
- Trauma or impact to chest wall
- Pneumothorax
- Pleural effusion
Inability to exchange oxygen or delivery to the peripheral tissues (hypoxemic respiratory failure): (4)
- Alveolar unable to fill.
- Pneumonia
- Acute respiratory distress syndrome (ARDS)
- Pulmonary edema
- Pulmonary vascular insufficiency
- Massive pulmonary embolism
- Air emboli
Failure to meet increased ventilatory demand: (4)
- Severe sepsis
- Shock
- Severe metabolic acidosis
Indications for Noninvasive Pressure Ventilation
Noninvasive pressure ventilation attempts to deliver oxygen to the lungs without endotracheal intubation (1).
Before intubation
- Acute exacerbation of COPD
- Hydrostatic pulmonary edema
- Asthma
- Bronchoscopy
- Chest Trauma
Used instead of invasive mechanical ventilation (intubation)
- Acute respiratory failure (ARF) [According to the latest ATS/ERJ (American Thoracic Society and European Respiratory Society) guidelines from 2020] (4)
- BPAP for acute or acute-on-chronic respiratory acidosis secondary to COPD exacerbation where pH < or = 7.35 (8)
- BPAP or continuous positive airway pressure (CPAP) for cardiogenic pulmonary edema (8)
- Obesity hypoventilation syndrome (1)
- Obstructive sleep apnea (4)
- Restrictive thoracic disorders (4)
**ATS/ERJ guidelines carry a conditional recommendation for the following in the setting of ARF:
- Early NIV (non-invasive ventilation) for immunocompromised patients with ARF
- Palliative care for terminal conditions
- Chest trauma patients with ARF
Following Intubation
- Post-operative ARF
- Preventative measure in high-risk patients following extubating.

Self Quiz
Ask yourself...
- Can you think of certain populations or diseases that are at a high risk for needing mechanical ventilation?
- Have you experienced caring for a patient following general anesthesia?
Ventilator Settings
Knowledge of the settings on mechanical ventilators is critical for care. Each parameter should be initially determined and adjusted based on the patient’s condition and unique needs. This is within the scope of practice of qualified physicians and respiratory therapists only. The nurse should know the settings and include them in the nursing handoff report.
There are several types of ventilator settings to be familiar with, including the following:
- Tidal Volume
- FiO2
- Respiratory Rate (Frequency)
- PEEP
- Mode
- Alarms
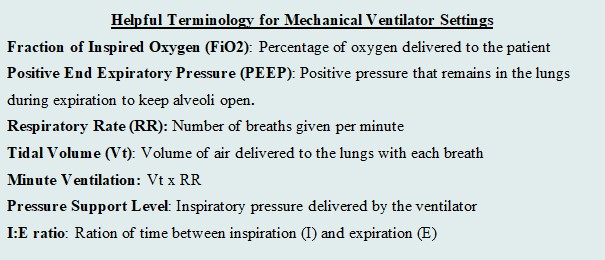
Figure 3. Helpful Terminology for Mechanical Ventilator Settings. (Designed by course author)
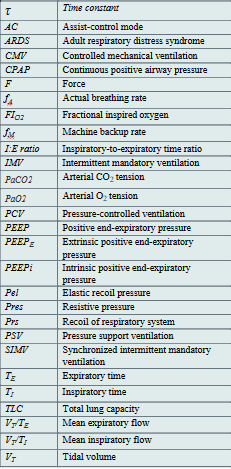
Table 1. List of Abbreviations for Ventilation. (1, 2, 5) (Designed by course author)

Self Quiz
Ask yourself...
- Are you familiar with the settings of mechanical ventilator?
- Have you ever cared for a patient that needed to “wean” from something, such as medication, addiction, etc.?
- Consider the feeling of wearing a breathing mask. How can the nurse provide physiological and psychological support?
As we discuss the settings, it is important to recognize short and long-term goals of mechanical ventilation. Short-term goals prioritize airway, breathing, circulation (ABCs) and maintaining respiratory gas exchange. Long-term goals should focus on weening and encouraging the patient to have a safe return of spontaneous breathing if possible. Independence should be a goal in certain circumstances.
The settings will reflect the minimal amount of assistance to maintain perfusion. Evidence supports the concept that hyperoxemia increases the risk of mortality in critically ill patients (2). An excess of oxygen is dangerous, as it can reduce respirations and heart rate. Tidal volume refers to the volume of air that is inhaled and exhaled from the lungs during spontaneous breathings, so the tidal volume setting determines the amount of the air delivered to the lungs by the machine (2).
Fi02
Fi02 stands for fraction of inspired oxygen. The range is 21% - 100% (Will). The Fi02 should be set to the lowest level to maintain a pulse oximetry (SP02) of 90% to 96% (2). A patient may initially require an FiO2 of 100% when mechanical ventilation is initiated, but the goal is to gradually wean the FiO2 percentage down to the lowest possible level that still provides adequate oxygenation for the patient. Research supports that a patient who receives mechanical ventilation with an Fi02 greater than 60% for an extended period of time is at greater risk of oxygen toxicity (1).
Positive End Expiratory Pressure (PEEP)
The PEEP settings refer to the positive pressure (greater than the atmospheric pressure) that will remain in the airways at the end of the respiratory exhalation (1). PEEP serves to distend the distal alveoli and prevent collapse. Imagine a balloon that you would like to keep inflated but air continuously seeps out. PEEP would determine the appropriate pressure to keep the balloon inflated. There are two types of PEEP: extrinsic and intrinsic (or auto-PEEP). Pressure that is applied during an inspiration is known as pressure support.
Extrinsic PEEP (PEEPe), or applied PEEP, is a setting on the ventilator and typically selected upon initiation of mechanical ventilator. Extrinsic PEEP ranges to small/ moderate (4 to 5 cmH2O) to high (>5 cmH2O). The level of PEEP is usually set at 5 cmH2O and titrated based on the underlying condition and oxygenation or perfusion needs (2). There is research and evidence-based guidelines to guide healthcare providers in properly setting and adjusting the PEEP on the mechanical ventilator. For example, in ARDS, there is a specific level of PEEP titrates according to regulatory evidence and guidelines.
Intrinsic PEEP, or auto-PEEP, refers to an incomplete expiration prior to the initiation of the next breath, which causes trapping and accumulation of air (2). If auto-PEEP is found, steps should be taken to stop or reduce the pressure build-up.
Respiratory Rate (RR)
Respiratory rate (RR) is the setting that simply determines how many breaths are delivered by the ventilator per minute. The RR is typically set at 12 to 16 breaths/minute (2). Certain circumstances warrant a higher RR (up to 35 breaths/minute). Higher RR is sometimes selected to achieve adequate minute ventilation. Examples include patients with ARDS, which would protect lung integrity and avoid severe hypercapnia, and patients with acidosis (2). Respiratory acidosis usually occurs due to failure of ventilation and accumulation of carbon dioxide, so increased respiration rate be used to balance acidosis (5). Important nursing implications are to closely monitor ABGs and titrate as ordered.
Flow Rate
The inspiratory flow rate is a rate that controls how fast a tidal volume is given by the ventilator; the setting can be adjusted depending on the patient’s inspiratory needs. The normal inspiratory flow rate should be set at around 60 L/min (2). In circumstances such as obstructive diseases, the ventilator can deliver up to 120 L/min if a patient needs a prolonged expiratory time (2). If the flow rate is set too low, it could cause unsynchronized patient-ventilator flow and an increased work of breathing; if the flow rate is set too high, it could result in lower airway pressure (2).
Respiratory therapists are an incredible resource and should be notified, as well as the physician, if this is suspected. Ventilator alarms are an essential tool for assessing inappropriate settings, we will discuss alarms later in the course. Please review the image below for a visual aid.

Self Quiz
Ask yourself...
- Can you think of professionals in your workplace that are qualified to adjust the settings on a mechanical ventilator?
- What do you think the respiratory rate should be set to?
- What do you think the inspiratory flow rate should be set to?
- Do you think positive pressure is greater than or less than atmospheric pressure?
Ventilator Modes
Mechanical ventilation without patient effort is delivered by the ventilator with control of either volume or pressure. Volume and pressure-controlled ventilation modes differ from one another based on transpulmonary pressure generation (5). There are three basic ventilatory modes based on respiratory cycles to consider: Assist/Control ventilation (A/C), Pressure Support Ventilation (PSV) and Synchronized Intermittent Mandatory Ventilation (SIMV) with PS, which is a hybrid mode of the first two (1).
Interpreting Waveforms
Scalars and Loops. Modes are depicted and illustrated as waveforms. Ventilator waveforms are graphical descriptions of how the ventilator is delivering a breath to a patient. These include scalars, which are graphics that illustrate the entire breath from the beginning of inspiration to the end of expiration, and loops, which are graphics that represent either pressure or flow, and plotted against the volume during a breath (1). Most ventilators have three scalars displayed on the main screen: flow versus time, volume versus time, and pressure versus time (1). There are typically two loops: pressure-volume and flow-volume. It is vital that the bedside clinician can interpret these scalars and loops to understand if the patient’s ventilation demands are met.

Figure 4. Example of Volume vs Time Scaler. Photo Credit: (9)
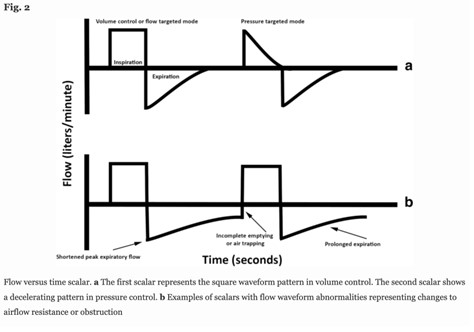
Figure 5. Example of Flow versus Time Scaler. Photo Credit: (9)
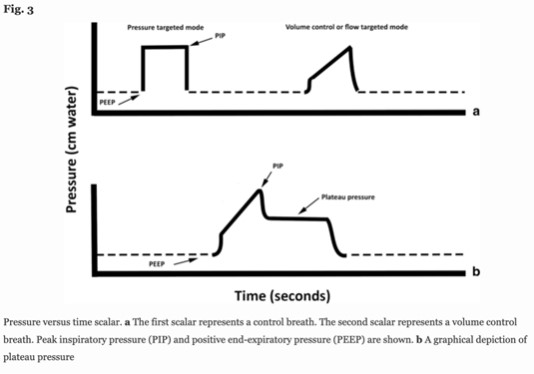
Figure 6. Example of Pressure versus Time Scaler. Photo Credit: (9)

Figure 7. Example of Pressure-Volume Loop. Photo Credit: (9)

Figure 8. Example of Flow-Volume Loop. Photo Credit: (9)
Volume and Pressure Controlled Modes
Monitoring respiratory mechanics in dynamic or stagnant conditions is extremely important to lung protection and adequate respiratory care. We will review the characteristics of volume and pressure-controlled modes.
Controlled mechanical ventilation (CMV) is when the ventilator controls one variable from the equation of motion, either flow (𝑉) or airway pressure (Paw) during the inspiratory phase. The flow or pressure must be a variable, because the others are constants: Rrs and Crs are intrinsic properties of the respiratory system, V(t) is the instantaneous volume above end-expiratory volume, PEEP is the end-expiratory pressure, and Pmus represents the pressure generated by inspiratory and expiratory muscles (1). Essentially, in this equation, the ventilator determines either the volume or the flow.
Paw(𝑡) = 𝑉(𝑡) / 𝐶𝑟𝑠 + 𝑅𝑟𝑠 × 𝑉 (𝑡) + PEEP – 𝑃𝑚𝑢𝑠 (𝑡)
This formula serves as a foundation for the common mechanical ventilator modes: Volume and Pressure Controlled.
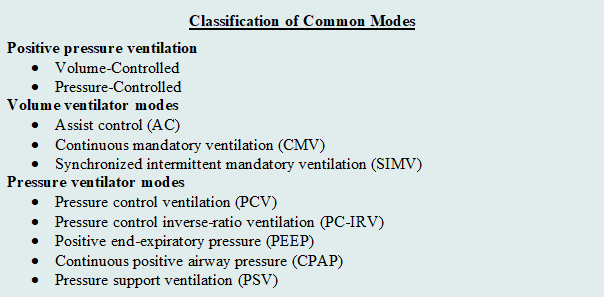
Figure 9. Classification of Common Modes. (Designed by Author)
Selection of mode differs from settings, as the mode of mechanical ventilation refers to the characteristics and phases of ventilation. The characteristics or phases mainly include trigger, cycle, and limit. (2)
Trigger: How does inspiration begin? The trigger is a type of signal that initiates the inspiratory phase by the ventilator.
- Patient-triggered: patient’s inspiratory effort triggers the ventilator to begin the inspiratory phase.
- Time-triggered: a time interval is set on the ventilator to begin the inspiratory phase.
Cycle: How does the inspiration end? The cycle is a type of signal that ends the inspiratory phase by the ventilator.
- Volume-cycled ventilation: the inspiratory phase ends when a set volume exits the ventilator.
- Pressure-cycled ventilation: the inspiratory phase ends according to a set driving pressure, airway resistance, lung compliance, and inspiratory effort of the patient.
- Time-cycled ventilation
Limit: When should inspiration be aborted? The limit is a set value (e.g., pressure) on the ventilator that should not be exceeded. If the preset limit is exceeded, the inspiration will be aborted. (2).
Volume Controlled (ACV/ VCV)
When you hear “volume”, think amount. The main characteristic of volume-controlled ventilation (VCV) is the delivery of fixed tidal volumes (1). The clinician sets the volume and how often it is delivered. Considering the respiratory rate is also set, minute ventilation is guaranteed. Essentially, this mode is driven by the amount of air entering the patient’s airway and how often. Inspiratory airway flows in predefined flow waveforms and the most common is square (1).
A max flow rate of the air being delivered is also set—think of it as the “speed” of the air being pushed into the lungs. The time it takes to deliver the inspiration will change because of the max flow rate that is set on the ventilator (1). If the flow rate is higher, the the inspiratory time of the breath to deliver the set volume will be shorter as a result.
It may be more likely nurses will be exposed to this type of mode in critical care settings. Volume-controlled ventilation (VCV) was the most used ventilatory mode in critical care when surveys were completed; however, both pressure-controlled and pressure-support modes have been reportedly utilized more frequently in recent years (1). VCV is primarily used when the patient is unable to breath on their own and essentially no spontaneous breathing occurs. VCV has also been the traditional controlled ventilation mode with anesthesia (3).
The concern of VCV is the constant flow may cause high peak pressures and increases the patient’s risk of barotraumas. Barotrauma is defined as physical tissue damage caused by a pressure difference between a closed space inside the body and the surrounding gas or fluid (7). Imagine trying to inflate a balloon in a glass bowl, if the pressure pushing air into the bowl continues and the glass bowl will not let it expand, the balloon itself will be damaged. Due to these risks, patients with lung disease and neonatal patients are not ideal candidates for this type of mode.
The nurse can gather information, such as the volume that is delivered per breath. If the volume is set at 4.5 liters, at a rate of 18, then the volume delivered with each breath will be 250mls per breath (4500mls / 18 = 250mls). The inspiratory time may fluctuate. The nurse must critically think and become aware of ventilation demands, considering factors including the set tidal volume, respiratory rate, and max flow rate. At end of shift nurse reporting, the nurse should communicate the following: mode, rate, tidal volume, fraction of inspired oxygen (Fi02), PEEP, and pressure support (PS).
Pressure Controlled (PCV)
In pressure-controlled ventilation, there is a set airway pressure for a given inspiratory time. Remember that the ventilator is programed with certain constants (specific setting and should not change) and variables (fluctuates based on constant settings). In the PCV mode, the peak airway pressure is constant (inspiratory pressure + PEEP) while the tidal volume is variable and can fluctuate depending on patient characteristics (compliance, airway/tubing resistance) and driving pressures (3). The clinician sets the inspiratory pressure level, PEEP, I:E ratio, respiratory rate, and FiO2.
Pressure-controlled mode provides the following advantages over volume-controlled breaths:
- Lower peak airway pressures to deliver the same volume amount.
- More efficient volume distribution within the lungs
- Better oxygenation
- Less risk of barotrauma
- Ability to ventilate every patient type.
As mentioned, PCV has a lower risk of barotrauma, so patients who already have lung disease and tissue damage are not appropriate for this type of mode. The tiny lungs of infants also have greater impact of tissue damage if barotrauma occurs. Nurses within the neonatal intensive care unit (NICU) may be more likely exposed to Pressure-controlled ventilation modes. PCV has become the standard approach to ventilation in the early days of neonatal care in small preterm infants, making it the prevailing mode of ventilation in the NICU in many parts of the world, including the US (3).

Self Quiz
Ask yourself...
- What are reasons for depicting the modes in waveforms?
- Can you name the three phases/characteristics of respiration that we discussed?
- What do you think the difference is between pressure and volume-controlled ventilation?
- Can you explain why pressure-controlled ventilation has a lower risk of barotrauma than volume-controlled ventilation?
Continuous Positive Airway Pressure (CPAP)
Continuous positive airway pressure (CPAP) is a type of positive airway pressure for patients that are breathing spontaneously. The goal of CPAP is to maintain a continuous pressure to constantly stent the airways open (7). If you recall, positive end-expiratory pressure (PEEP is the pressure within the alveoli at the end of expiration. CPAP is a method of maintaining PEEP and preserving the set pressure in the airway throughout the respiratory cycle. It is measured in centimeters of water pressure (cm H2O) (7). CPAP is aimed to prevent airway collapse in patients at risk. CPAP alone is often inadequate for supporting ventilation, but helpful for non-invasive ventilation. CPAP can support oxygenation via PEEP prior to intubation (6).
CPAP delivers air through the typical method of respiration; air is inhaled through the nose, travels through the nasopharynx, oropharynx, into the larynx, trachea, bronchi, bronchioles, and alveoli (7). This form of ventilation support can be used in inpatient and outpatient settings, long-term care facilities, and at home.
Common indications for CPAP include the following:
- Hypoxia: (7)
- Decrease the work of breathing
- Bronchiolitis or pneumonia
- Respiratory failure associated with congestive heart failure.
- Obstructive sleep apnea (OSA). Predisposition: Obesity, hypotonia, adenotonsillar hypertrophy, family history, use of alcohol or sedatives, etc. (8)
- Preterm infants
- Their lungs have not yet fully developed and respiratory distress syndrome can occur (2)
- Within NICU setting
- CPAP can be administered in several ways based on the type of mask used: (7)
- Nasal CPAP: Nasal prongs inserted directly into the nostrils or a small mask that fits over the nose.
- Nasopharyngeal (NP) CPAP: An airway tube placed through the nose that the tip travels to the nasopharynx.
- Face Mask CPAP: A full face mask is placed over the nose and mouth. The seal is critical.
High Frequency Ventilation (HFV)
High-frequency ventilation (HFV) delivers breaths at a rapid rate because conventional ventilation modes have failed (7). The respiratory rate set on the ventilator significantly exceeds the normal breathing rate and the tidal volume delivered is significantly less. An advantage is the reduced risk of barotrauma, thus reduced risk of lung tissue damage. However, the mode has many contraindications and HFV is not frequently used in adults, more commonly in neonates (7).

Self Quiz
Ask yourself...
- Do you have experience with patients who wear a CPAP for sleep apnea?
- Can you name other indications for CPAP?
- Do you think high-frequency ventilation would be a first or last choice for early choice of ventilator types?
Ventilator Alarms
Ventilator alarms can be a nurse’s best friend when coupled with in-depth understanding of types of alarms and troubleshooting techniques. These alarms are essential during mechanical ventilation because they notify the healthcare team of changes in a patient’s condition that may require intervention. Each alarm represents a different potential problem.
What is a Ventilator Alarm?
A ventilator alarm is a safety feature on the mechanical ventilator that applies a set of parameters to provide alerts whenever there is a problem related to the patient-ventilator interaction. The alarms can be visual, audible, or both, depending on the type of ventilator and settings. Ventilator manufacturers have taken various approaches to alarms. The majority of ventilators allow the user to program default alarm thresholds based on various patient populations (6). Many apply predefined settings, such as +/- 30% of the current minute ventilation. Typical ventilators provide the ability to set alarm thresholds for peak inspiratory pressure, tidal volume, frequency, and minute ventilation, while others do not provide limits (6).
There are many types of ventilator alarms, including:
- High Pressure
- Low Pressure
- Low Volume
- Apnea
- High or Low PEEP
High Pressure Alarm
A high-pressure alarm is triggered whenever the circuit pressure exceeds a preset pressure limit during the inspiratory phase of breathing. The preset limit for the high-pressure alarm is typically set around 10 cmH2O above the peak inspiratory pressure (PIP).
This alarm would be beneficial for patients with respiratory conditions that cause decreased lung compliance or increased airway resistance (2). Other causes of the alarm sounding include coughing, kinking of the airway, or thick and copious secretions. Correctly setting tidal volume alarms is imperative. In VCV, the action of the ventilator is directly controlling tidal volumes, so alarms can alert if this process has abnormalities.
Troubleshooting tips include: (8)
- Check for patient-ventilator asynchrony.
- Perform respiratory assessment.
- Provide endotracheal suctioning if needed.
- Check for a kink in tubing of the artificial airway.
- Relocate the endotracheal tube if it’s not in the correct position.
- Check for a malfunction of the inspiratory or expiratory valves.

Self Quiz
Ask yourself...
- Have you ever been able to recognize various alarms on medical equipment?
- Do you have experience with troubleshooting alarm notifications once you determine the alarm sounded due to an error?
Low Pressure Alarm
A low-pressure alarm is triggered when the peak inspiratory pressure (PIP) pressure in mechanical ventilation is below a preset level. This most commonly occurs whenever there is a leak or disconnection in the system (8). If the cause of the alarm is unknown, the patient should be manually ventilated until the source of the leak is identified.
Troubleshooting tips include:
- Check for a leak or disconnection in the circuit and exhalation valve.
- Check for a leak in the pilot balloon.
- Ensure that the endotracheal tube is properly located.
- Ensure that the endotracheal tube cuff is adequately inflated.
- Ask respiratory therapist or physician if the ventilator settings should be adjusted.
Low Volume Alarm
A low volume alarm is triggered whenever the expiratory volume decreases below a preset low volume threshold (6). This alarm is helpful because it assesses if the patient is receiving and exhaling a minimum tidal volume. If this alarm sounds, the respiratory therapist should be consulted.
Apnea Alarm
An apnea alarm is triggered whenever the total frequency decreases below a preset frequency limit. The alarm is critical to determine if the patient is receiving an adequate number of breaths. The apnea alarm most commonly sounds when there is a disconnection of the circuit from the endotracheal tube (6). If this occurs, the respiratory therapist must ensure that the patient is being ventilated by delivering manual breaths until the disconnection source is identified.
High or Low PEEP Alarm
A high or low PEEP alarm is triggered whenever the level of PEEP exceeds or falls below a preset PEEP limit. The high PEEP alarm most commonly sounds whenever auto-PEEP or air trapping is present (2). A potential cause of the low PEEP alarm is active inspiration by the patient (6). Active inspirator by the patient causes the PEEP level to drop below the preset alarm setting and the settings may be adjusted based on changes in the patient’s condition.
Alarm Fatigue
Although ventilator alarms have invaluable meaning, the alarms can sound frequently without a meaningful reason. Alarm fatigue is frustration felt by healthcare providers with unactionable or insignificant alarms (6). A recent study found that alarms can sound as many as 942 alarms per day (6). Nurses must become familiar with the sounds so they can prioritize their responsiveness. Research suggests that 80–99% of ventilator alarms in general are false or nonactionable (6). There have been policy changes and interventions regarding alarm fatigue and overwhelming alarms with no true significance.
The Joint Commission introduced “Use alarms safely” as a National Patient Safety Goal in 2014 (6). Phase 1 required hospitals to identify the most important alarm signals to manage and inquired, “what mechanical ventilation alarms are important?” and “who determines if an alarm is unnecessary?” (6). Policy changes like this are impactful to the individual nurse and patient, as it made practical changes that impact practice. Although nurses and clinicians appreciate meaningful alarms, it can take them away from issues with higher priority if it constantly alarms for unnecessary reasons.

Self Quiz
Ask yourself...
- Can you name the most common alarms on a mechanical ventilator?
- What do you think contributes to alarm fatigue (ex: high workload, patient frustration)?
- Can you name members of the healthcare team that can help with setting alarm parameters?
- Can you imagine how alarms can impact patient anxiety and sleep habits?
Nursing Care
Nursing care should prioritize maintenance of a patent airway, gas exchange, prevention of trauma, therapeutic communication, and assessment of cardiac and pulmonary complications.
Nursing Priorities
- Ensuring a patent airway and assessing for proper placement of the endotracheal tube
- Monitoring the patient’s respiratory status
- Assessing lung sounds
- Oxygen saturation levels, and
- End-tidal carbon dioxide (EtCO2) monitoring.
- Monitoring patient comfort and pain levels.
- Preventing complications associated with mechanical ventilation.
- Ventilator-associated pneumonia
- Ventilator-induced lung injury
- Collaborating with the healthcare team
- Optimize ventilator settings
- Weaning protocols
- Providing ongoing education for patient and family
Nursing Assessment
- Adventitious breath sounds
- Diminished lung sounds
- Increased or decreased respiratory rate.
- Dyspnea
- Decreased oxygen saturation (Sao2 <90%)
- Arterial pH less than 7.35
- Decreased tidal volume.
- Decreased Pao2 level (>50 to 60 mm Hg)
- Increased Paco2 level (50 to 60 mm Hg or higher)
- Restlessness
- Excessive secretions
- Ineffective cough
Nursing Interventions and Actions
- Assess the client’s respiratory rate, depth, and pattern, including the use of accessory muscles.
- Count the client’s respirations for one full minute and compare with ventilator set rate and desired respiratory rate.
- Observe changes in the level of consciousness.
- Early signs of hypoxia include disorientation, irritability, and restlessness; late signs include lethargy, stupor (8).
- Assess the client’s heart rate and blood pressure.
- Tachycardia may be a result of hypoxia (8).
- Auscultate the lung for normal or adventitious breath sounds.
- Bilateral basilar crackles may indicate pulmonary edema or volume overload, other signs of that includes jugular vein distention and lower limb edema (8). Wheezing and rhonchi are present in obstructive lung disease (8). Absent lung sounds may indicate massive pleural effusion or pneumothorax (8).
- Assess the skin color and examine the lips and nailbeds for cyanosis.
- Monitor oxygen saturation using pulse oximetry.
- Maintain the client’s airway.
- Use suctioning as needed.
- Monitor arterial blood gases (ABGs) as indicated.
- ABGs during respiratory failure may reveal increasing PaCo2 and decreasing PaO2 (8).
- Assess for correct endotracheal (ET) tube placement through observation for symmetrical chest rise, auscultation of bilateral breath sounds, and X-ray confirmation.
- Upon auscultation, if frequent crackles or rhonchi are heard and do not clear with coughing or suctioning, it may indicate developing atelectasis, acute bronchospasm, pneumonia, or pulmonary edema (6).
- Assess for the client’s comfort and pain level.
- Assess the ventilator settings and alarm system every hour.
- Patient positioning.
- Maintain the client in a High-Fowler’s position as tolerated and frequently check the position. This position encourages chest expansion and increases oxygenation.
- Promote optimal nutritional balance.
- Weigh the client regularly.
- Assess if patient can safely eat.
- Auscultate for bowel sounds. Document and report loose stool or absence of bowel movements. -Document abdominal girth measurements.
- Monitor gastric residual volumes following enteral feedings. Gastric residual volumes should be monitored to avoid gastric distention and avoid risk of regurgitation and aspiration.
- Offer food that the client desires and document when oral intake resumes.
- Consult nutritionist and be knowledgeable on nutrients that are vital. For example, protein is a vital nutrient to support wound healing and immune function and to maintain lean body mass (8)
- Assess the client’s and caregiver’s perception and understanding of mechanical ventilation.
- Assess the client’s readiness and ability to learn.
- Encourage the client or significant others to express feelings and ask questions about care.
- Provide ongoing education to patient and caregivers. Use material in multiple formats; for example, books, printed pamphlets, audiovisuals, demonstrations, and instruction sheets. Examples include, but not limited to:
- Explain the need for suctioning as needed.
- Explain that alarms, what they indicate, and that they may periodically sound off, which may be normal.
- Explain the weaning process.
- If long-term ventilation is anticipated, discuss, or plan for long-term ventilator care management and use appropriate referrals: long-term ventilator facilitates versus home care management.
- Community resources may include food and meal services, physical and occupational therapy transportation, and access to client support groups. Social workers should become involved if patient is going home with an invasive mechanical ventilator.

Self Quiz
Ask yourself...
- Do you feel comfortable with airway suctioning?
- What do you think the most optimal patient position is for mechanical ventilation?
- Why would supine position not be appropriate for proper ventilation?
- Can you explain the interventions for maintaining nutrition in the mechanically ventilated patient?

Self Quiz
Ask yourself...
- What are some problems that may occur in the mechanically ventilated patient?
- What do you think the nurse should prioritize in the ventilated patient?
- Can you think of possible questions the patient or family may have regarding ventilator care?
- Can you name interventions to provide holistic care for patients on long-term mechanical ventilation?

