Course
Colorado Substance Use Prevention
Course Highlights
- In this Colorado Substance Use Prevention course, we will learn about Colorado State and Federal Laws governing correct prescription and monitoring of controlled substances.
- You’ll also learn evidence-based approaches to assess and manage acute and chronic pain across diverse patient populations.
- You’ll leave this course with a broader understanding of multimodal pain management strategies including pharmaceutical treatments.
About
Pharmacology Contact Hours Awarded: 2
Course By:
Sarah Schulze
MSN, APRN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Pain can vary according to the source and intensity, as well as an individual’s age, gender, culture, and interpretation by the individual. Unfortunately, everyone will eventually experience pain. The nurse’s role is crucial in providing comprehensive patient care by evaluating and treating pain effectively.
Colorado allows a board certified and licensed advanced practice nurse to prescribe and monitor medications both in a provisional and full practice capacity, depending on the clinicians amount of experience. The state requires mandatory completion of a course on safe narcotic prescription and identification of potential substance use disorder, which is discussed in this course.
Colorado Laws Regarding Safe Controlled Substance Prescriptions
Colorado state and federal laws govern the prescribing and monitoring of controlled substances including all narcotics. The Controlled Substances Act (CSA), administered by the Drug Enforcement Administration (DEA), regulates all aspects of controlled substance manufacturing, distribution, dispensing, prescribing and distribution. The DEA regulations offer healthcare providers specific guidelines regarding prescribing practices, record keeping practices, and monitoring (38).
At the federal level, any prescriber of narcotics or scheduled drugs must apply for and be approved to be a prescriber, which includes physicians, nurse practitioners, and physician assistants. Nurse practitioners in the state of Colorado are first granted provisional prescriptive authority, allowing them to prescribe and monitor necessary medications, including controlled substances, to clients within their scope of practice while engaged in a synchronous mentorship with either a physician or full practice APRN. The supervising role in the mentorship must be filled by a Colorado-licensed physician or APRN who is qualified to treat the same or similar patient population and the mentorship must be completed within a three-year time period.
Once the nurse practitioner has completed and has documented approval of 750 hours of successful mentorship during this provisional period, they may be granted full practice authority and continue prescribing necessary medications to the population within their scope without any mentorship or supervision (50).
Colorado also has a Prescription Drug Monitoring Program (PDMP) to track the prescribing and dispensing of controlled substances to clients. Registration with the PDMP is required for clinicians with prescriptive authority and healthcare providers must check this database prior to dispensing controlled substances to clients (50).
Additionally, continuing education in the form of two contact hours of education related to the prescribing and monitoring of controlled substances is required every two years when APRNs renew their Colorado state licensure (50).
Healthcare providers in Colorado must remain up to date with both federal and state regulations to ensure safe prescribing practices, compliance, and ensure patient and colleague communication regarding controlled substances such as narcotics (50). Regular review is key.

Self Quiz
Ask yourself...
- For patients with both chronic pain and substance use disorder, how can you collaborate with the interdisciplinary medical team to provide comprehensive care?
- How can you help a patient with SUD with re-occurring and chronic pain?
- How can the integration of complementary and alternative therapies enhance the effectiveness of pain management for patients with substance use disorders?
Incidence And Prevalence of Substance Use Disorders
By conducting a careful pain assessment, nurses can gain an understanding of a patient’s subjective pain perceptions as well as its severity, causes, and symptoms. Nurses may implement both non-pharmacologic and pharmaceutical interventions to manage pain appropriately.
The role of the nurse practitioner is to formally diagnose and order treatment, so a thorough understanding of pain management and identification of addiction risk factors is crucial. For DEA-registered practitioners, care should be given when choosing which pharmacological interventions to utilize, to minimize risks for substance abuse disorders and achieve maximum pain relief.
Uncontrolled pain or the development of substance use disorders can disrupt functional living and complicate comorbidities. Collaboration among members of the health care team and patients themselves is also key, including setting realistic goals for managing pain effectively and actively participating in their plan of care.
Pain, including abdominal, head, throat, and back pain, continues to be the top four most common patient complaints seen in primary care (1). In efforts to address and treat pain, both pharmacological approaches are given by nurse practitioners.
Unfortunately, a result of prescribed pain medications is the possibility of substance use disorders, which is a continued important issue in the United States. The opioid epidemic continues to be a serious public health concern. Assessing, diagnosing, treating pain, and identifying risk factors for substance use disorder are important topics for every nurse practitioner.
The most common substance use disorders in the United States are (2):
- Alcohol use disorder (29.5 million)
- Cannabis use disorder (16.3 million)
- Methamphetamine use disorder (1.6 million)
- Opioid Use disorder (5.0 million)
- Tobacco use disorder (16 million)


Self Quiz
Ask yourself...
- What is your role in helping combat the opioid epidemic and growing prevalence of substance use disorder in the U.S.?
- What are causative factors for the most common pain conditions?
- What is your role in identifying and treating the most common substance use disorders in your practice?
Types of Pain
Pain can be an ordinary response to illness or injury and doesn’t typically require medical intervention. Pain may be divided into various categories depending on its onset and duration, including acute, chronic, or breakthrough (3).
Acute pain is experienced from within minutes of an injury up to several months afterwards. Chronic pain is experienced beyond six months and usually due to a continuous medical issue or condition. Breakthrough pain occurs when pain that was controlled with medication begins to be felt beyond the pharmacological properties of the pain medication. Pain is divided further into neuropathic, nociceptive, and radicular (35).
|
Type of Pain |
Definition |
|
Acute |
Short-term from minutes to less than 6 months |
|
Chronic |
Continues beyond 6 months |
|
Neuropathic |
Damage to nerves felt as sharp, stabbing, burning. |
|
Nociceptive |
Damage to body tissues felt as sharp, achy, or burning. |
|
Radicular |
Damage from a compressed or inflamed spinal nerve, felt as constant and steady pain. |
|
Phantom Pain (a type of neuropathic pain) |
Sensation of pain from a limb/digit that has been amputated. Nerve endings have memory. |
Table 1. Types of Pain

Self Quiz
Ask yourself...
- What are resources you can offer your patient about options for pain management?
- What questions should you ask your patient to identify the type of pain they are experiencing?
- How can you identify the type and source of pain your patient is experiencing?
Pain Assessment
Pain is considered the fifth vital sign and provides significant information about a patient’s lived experience.
In 1995, it was proposed by a practicing physician James Campbell that pain should be considered the fifth vital sign, which was later supported by the American Pain Society as a standard practice guideline (6). In addition to blood pressure, heart rate, respiratory rate, temperature, and pulse oximetry, a pain assessment provides information necessary for holistic care.
A regular pain assessment allows nurses to manage patient discomfort more effectively by creating personalized plans of action to effectively address pain management needs. Prior to ordering or administering pain medications, nurses must perform an in-depth pain evaluation that includes gathering data from various sources, including the patient’s medical history, chief complaint, and a physical exam. A follow-up is important to evaluate any therapeutic results of prescribed medication.
Components of a Pain Assessment
A systematic pain assessment is key to correctly identifying all the components of pain (7).
- Assess risks for pain. For example, advanced age, cancer, anxiety, recent surgery/invasive procedures increase the likelihood of experiencing pain and discomfort.
- Assess pain using an approved pain scale to create a baseline for the current pain level (which will be discussed later). Remember pain is subjective and influenced by age, gender, and cultural factors.
- Identifying the pain source such as nociceptive, neuropathic, referred, somatic, visceral, or phantom pain.
- Assess the type of pain (acute or chronic) and contributory factors.
- Evaluate their past response to pharmacological interventions and analgesics, including any adverse reactions they experience.
- The assessment should include physical, behavioral, and emotional signs of pain including confusion, diaphoresis, moaning, decreased activity levels, irritability, guarding, clenched teeth, muscle tension, depression, insomnia, confusion, diaphoresis, moaning, and grimacing.
Pain Assessment Mnemonics
Nurses often use three mnemonics to remember standardized questions for conducting a comprehensive pain assessment:
- COLDSPA
- OLDCARTES
- PQRSTU
Each letter presents important questions to ask the patient about their pain.
Nurses may ask any number of questions to obtain information for each category. Examples of each of these mnemonics can help the practitioner remember to ask important questions relevant to pain.
| COLDSPA | Questions to ask: |
|
C: Character |
What does the pain feel like? Does it feel like burning, stabbing, aching, dull, throbbing, etc.? |
|
O: Onset |
When did the pain start? What were you doing when the pain started? |
|
L: Location |
Where do you feel the pain? Does it move around or radiate elsewhere? Can you point to where it hurts? |
|
D: Duration |
How long has the pain lasted? Is the pain constant or does it come and go? If the pain is intermittent, when does it occur? |
|
S: Severity |
How would you rate your pain on a scale of 0 to 10, with “0” being no pain and “10” being the worst pain you’ve ever experienced? How much does it bother you? |
|
P: Pattern |
What makes your pain feel better? What makes your pain worse? Does the pain increase with movement, certain positions, activity, or eating? |
|
A: Associated Factors |
What do you think is causing the pain? What other symptoms occur with the pain? How does the pain affect you? |
The “OLDCARTES” mnemonic consists of the letter of each category of questions to ask.
- O: Onset
- L: Location
- D: Duration
- C: Characteristics
- A: Aggravating factors
- R: Radiating
- T: Treatment
- E: Effect
- S: Severity
The “PQRSTU” mnemonic also helps the clinician to ask about components of pain.
- P: Provocative/Palliative
- Q: Quality/Quantity
- R: Region/Radiation
- S: Severity
- T: Timing/Treatment
- U: Understanding
Regardless of the pain assessment framework utilized, it is critical that open-ended questions allow patients to describe the pain in their own words. Closed-ended questions result in either yes/no responses or fail to capture an accurate account of the patient’s pain.
It is also vitally important for the nurse to follow-up on initial responses by asking clarifying questions so they can create and implement an individualized pain treatment plan to address all aspects of pain. In completing a pain assessment with patients, the nurse practitioner gains better trust with the patient, which can result in better patient adherence to prescribed treatment.
Pain is Subjective
Given that everyone responds differently, each person’s experience of pain will vary widely, even for stimuli with similar properties. For instance, some may feel considerable discomfort after receiving injections while others experience none, which means consequently we must treat pain according to whatever the individual claims it to be.
Due to this completely subjective nature of describing pain, the evaluation of the response to pain medication is also subjective. Clinicians must recognize the biological, psychological, and social factors that affect the perception of pain as shown in the following table.
| Biological Factors | Psychological Factors | Social Factors |
|
|
|
Table 2. The biological, psychological, and social influences on pain. (47)
Pain Scales
At the core of any pain assessment is determining the intensity. As pain cannot be objectively tested to pinpoint an individual’s sensations, providers use pain scales as tools for objectively understanding each patient’s discomfort and setting realistic pain goals. Nurses have access to numerous standardized pain scales.
A popular one is numerical, in which patients rate their discomfort between zero and 10, with zero being no pain and 10 being the worst pain ever experienced. While simple and user-friendly, numerical pain scales cannot be used by children or other populations who cannot accurately quantify pain, therefore alternative pain scales such as FACES scale, FLACC scale comfort behavioral scale or PAINAD scale may be used.
The FACES scale is a visual assessment tool for children and other people who cannot use numeric scales. When using it with children or others who cannot describe numbers accurately, explain to the patient that each face represents either no pain, some discomfort, or intense distress. For instance: Face 0 doesn’t hurt at all while Faces 2-6 hurts just slightly more, while Face 8 hurts even further before reaching 10, which represents extreme suffering. Ask the individual which of those depictions best represents their discomfort.

Figure 1. Wong Baker FACES Scale used to help score pain level.
The FLACC scale is used to assess pain in children aged two months to seven years and those unable to verbalize. It comprises five criteria such as face, legs, activity, cry, and consolability. Care providers assign each criteria a score between zero and two upon observation of their patient and then combine all five scores together into an overall pain score between zero (no pain) and 10 (10 severe) (8).
The Pain Assessment in Advanced Dementia (PAINAD) Scale is used to assess pain in patients with advanced dementia (9). This scale has five criteria including breathing independent of vocalization, negative vocalization, facial expression, body language, and consolability.
Like the FLACC scale, each of the five criteria are assigned a score of 0, 1, or 2. The provider observes the patient, assigns a score for each criterion, and adds the scores. The total pain score will be between 0 and 10, with 0 being no pain and 10 being severe pain. Like FLACC, the PAINAD scale is simple, valid, and reliable, but it may not always result in the most accurate pain assessment, as it requires the nurse to calculate the score based upon observed patient behaviors rather than the patient’s subjective pain rating.
Online Resources:

Self Quiz
Ask yourself...
- How does culture affect a patient’s expression of pain?
- What pain scales do you commonly use in assessing pain and are they appropriate for the age, gender, and verbal skills of the patient?
- What other questions should you ask about a patient’s tolerance of pain and how they have handled pain in the past?
Cultural Influence on Pain
Culture plays an intricate role in how individuals express physical and emotional discomfort. Some cultures, such as those found in East Asia, place strong value on self-discipline and control and may choose not to show any emotions when in pain.
Middle Eastern and Mediterranean societies emphasize open expressions of emotion and may easily express and verbalize their sensations of pain (10).
Although culture may impact pain levels differently for each patient, nurses must understand its impact before creating an individual plan that best meets each person’s specific needs.
Pain Assessment on Special Populations
The elderly, children, individuals who speak English as a second language, deaf, mute, limited English training, and people from different countries may require additional patience while completing a pain assessment.
Chronic pain can be related to depression, anxiety, and sleep disturbances, which can complicate a clear report of pain. Using a multimodal approach for a pain assessment, a physical exam, and the pain scales identified above can be helpful.
Reassessment After Intervention
Pain must always be assessed again following implementation of an intervention to determine its effectiveness in relieving symptoms. Oral medications should be assessed within 1 hour while intravenous treatments within 15-30 minutes, and per facility protocol (39).
For a primary care provider in an office clinic, reassessing pain should use the same pain scale used during initial assessment at the next visit. If their discomfort has not decreased to meet their established goal level, further interventions will be needed.
Interventions may involve medications and/or non–pharmacological modalities like heat, ice, music therapy and repositioning to achieve the patient’s ideal pain goal (40). Intervention and reassessments must continue until this goal has been attained. All reassessments and interventions must be documented in their medical record.

Pain Management Care Plan
In developing care plans for pain, nurse practitioners should provide a tailored approach to address each patient’s unique pain management needs. Beginning with an in-depth evaluation, the nurse practitioner gathers information regarding medical history, current pain symptoms, functional status, psychosocial factors, and desired goals for treatment.
Based on their evaluation, nurse practitioners collaborate with patients to set realistic expectations and goals for pain management care plans that integrate pharmaceutical interventions along with nonpharmacological interventions.
Pharmacological interventions include using analgesic medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), opioids and any adjuvant medicines such as antidepressants or anticonvulsants as well as topical agents to relieve discomfort (41).
Nurse practitioners carefully consider all risks and benefits when prescribing medications to their patients, tailoring individualized plans to optimize pain relief while mitigating adverse side effects as well as risks related to opioid misuse or addiction.
Non-pharmacological interventions also play a vital part in pain management. These may include physical therapy, occupational therapy, acupuncture, and massage therapy as well as cognitive-behavioral therapy (CBT), relaxation techniques and mindfulness-based interventions.
Nurse practitioners work collaboratively with other healthcare professionals such as physical therapists, psychologists, and pain specialists to coordinate and integrate interventions into a patient’s care plan. Education and self-management strategies also play a pivotal role in pain management plans. Nurse practitioners provide patients with education about their pain condition, its causes, and possible solutions.
Patients can become actively engaged in their care by learning self-management techniques such as pacing activities, maintaining proper posture, using heat or cold therapy, and practicing stress reduction methods.
Additionally, patients receive guidance regarding medication adherence, potential side effects and the significance of regular follow up appointments to monitor progress. Furthermore, their pain management care plan incorporates strategies designed to address any psychosocial factors which might impact pain for an improved experience and treatment outcome. Screening may include depression, anxiety, sleep disturbances, substance use disorders and any additional coexisting conditions.
Referrals may be made to mental health professionals, social workers, or support groups as a source of additional assistance and resources for the patient. Reassessment and monitoring should form integral parts of any pain management care plan. Nurse practitioners collaborate closely with patients to monitor pain levels, functional status, effectiveness of medication treatment plans, and any adverse side effects. Treatment plans may be altered accordingly as needed based on response to therapy, changes to condition, or evolving goals of care.

Self Quiz
Ask yourself...
- How do you educate your patient about pain management options?
- How do you educate your patient about safe prescription medications?
- What resources do you have to create a nursing care plan for pain?
Pharmacological Pain Management
Pain medications are divided into two main groups, including analgesics and adjuvants. Analgesics are used to prevent or treat pain and can further be classified as opioids or nonopioids; the classification is based on whether their original source is from poppy plants, known as opioids (41).
Nonopioids include medications not classified as opioids while adjuvants contain medication with both independent analgesic properties as well as additive properties when taken together with opioids.
When taking analgesics, it is wise to start with those having minimal side effects in a smaller dose and using minimally invasive approaches.
Developed by the World Health Organization, Figure 2 (below) demonstrates the stair-step ladder approach to guide the advancement of pain
Originally created to assist cancer patients, the pain ladder model can now be applied to all forms of discomfort. Nonopioids should generally be employed first in managing pain and if persistent or increasing discomfort continues then opioids or adjunct therapies should be added alongside nonopioids as appropriate (42).
For severe, short-term pain that’s expected to diminish gradually over time however, opioids, nonopioids and adjunct therapies might initially all be given before gradually withdrawing their presence so only nonopioids remain.
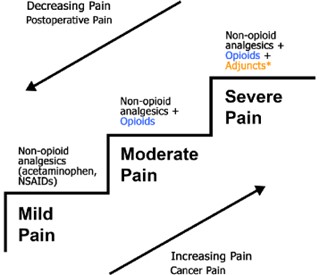
Figure 2. The WHO pain ladder is a guide for using pain medications responsibly (51)
Analgesic Medications
Analgesic medications (nonopioids and opioids) are used to alleviate or manage pain. Nonopioids tend to work best at managing mild-to-moderate discomfort in most cases and are well tolerated by most users. Examples of such analgesics include acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDS).
Acetaminophen
Acetaminophen is a non-narcotic analgesic and fever reducer. It is available by prescription or over the counter (OTC). Acetaminophen (the active ingredient found in Tylenol) can help relieve mild pain in all age groups and is generally safe. As it can be administered orally, sublingually, or intravenously, it could also provide an ideal choice for people unable to take oral medications.
The pharmacokinetics and mechanism of action of acetaminophen include the quick absorption from the gastrointestinal tract within 30-60 minutes. Delays of absorption to peak concentration in the circulatory system can be due to food in the stomach. It is then metabolized by the liver via the three main hepatic pathways including glucuronidation, sulfation, and CYP450 oxidation (44). The half-life is approximately 4 hours, however with hepatic injury or overdose the blood peak level can be accelerated to 2 hours.
In patients suffering from liver failure, it should be used with caution as one potential adverse side effect could be hepatotoxicity. Therefore, it is crucial that daily dosage be closely monitored (12). Millions of people use over the counter (OTC) pain relievers every day to treat minor aches and pains.
Usually, these medicines are safe and effective, but they can be dangerous and even deadly when they are not taken as directed (11). Acetaminophen, also called paracetamol in many other countries, is sold by many names including Tylenol, Panadol, Ofirmev, Acephn, and Mapap.
It is used effectively for fever, muscle pain, neck pain, plantar fasciitis, sciatica, and common body aches and pains. It is abbreviated as APAP for acetyl-para-aminophenol, which is the chemical name and is known by 28 band names in the United States (12).
It is very commonly used in combination drugs for pain as a nonnarcotic analgesic and known as Excedrin, Goody’s Body Pain, Saleto, Exaprin, Levacet, Painaid, Apadaz, Rhinocaps, Staflex, and included in over-the-counter medications for acute cold symptoms, respiratory conditions, and headaches (42)
In addition, it is a component of some narcotic prescriptions. Acetaminophen can be used as a sole medication or as an active ingredient in many OTC and prescription medicines. Acetaminophen is generally safe at recommended doses, but if taken in larger dosages or frequency, it can cause serious and even fatal liver damage. In fact, acetaminophen poisoning is a leading cause of liver failure in this country (13).
Safety guidelines include:
- Older adults: limit to no more than 3,200 mg in 24 hours.
- Healthy young adults: can take no more than 4,000 mg.
- Alcoholism: should limit themselves to no more than 2,000 mg daily.
Add all sources of acetaminophen into daily totals, including amounts found in combination medicines such as Percocet 5/325, which contains 5mg Oxycodone and 325 mg Acetaminophen. One Percocet 325 mg tablet should count toward the total daily acetaminophen dosage and should be included when prescribing individual dosages to avoid too close an administration of multiple medicines at once.
As an illustration, if 500 mg of acetaminophen is prescribed every four hours to combat fever while 5/325 Percocet is intended as pain reliever, both medications should not be given together within four hours as it would increase intake significantly and cause too much acetaminophen.
NSAIDs
Nonsteroidal anti-inflammatories (NSAIDs) are nonprescription medicines prescribed to relieve mild to moderate discomfort and may also be combined with opioids for treating severe pain. The pharmacokinetics of NSAIDS is based on the absorption, distribution, metabolism, and elimination of the drug as all oral medications. NSAIDS inhibit both COX-1 and COX-2 enzymes and play a role in prostaglandin mediated pain from inflammation (44).
Although they offer more gastrointestinal protection than aspirin, they do have cardio-nephrotoxic adverse effects. Due to the inhibition of prostaglandins and thromboxane, the desired actions are anti-inflammatory, antipyretic, and analgesic.
Common examples of NSAIDs are Ibuprofen, Naproxen and Ketorolac. Ibuprofen should be taken every 6-8 hours for adults aged six months or over. Naproxen can be taken 2-3 times per day and provides longer-acting pain relief than Ibuprofen does. Ketorolac may be taken temporarily (up to five days) in cases of moderate-to-severe adult pain relief. Aspirin is often the last line of nonopioids before turning to opioids and may help treat breakthrough pain for patients already taking opioids.
Side effects from taking an NSAID drug could include dyspepsia, nausea, and vomiting. To minimize risk, NSAIDs should always be taken with food. Long term or high dose use also increases risks such as heart attack, stroke, and heart failure; and must be prescribed carefully for people over 60 or those with liver or renal problems. One notable exception is aspirin, which when taken in low doses may reduce the risk of another heart attack in people who have already had one. NSAIDs may cause gastrointestinal bleeding when combined with warfarin or corticosteroids.

Self Quiz
Ask yourself...
- How do you educate parents of children you are prescribing NSAIDs for regarding safety?
- How do you teach them to safeguard against accidental ingestion by other children in the home?
- How do you carefully prescribe NSAIDS for someone with renal problems?
Narcotic Pain Relief Categories
Opioid Agonists
- Codeine
- Fentanyl
- Heroin
- Hydrocodone (Lortab, Vicodin, Percocet)
- Hydromorphone and Oxymorphone
- Meperidine
- Morphine
- Oxycodone (OxyContin, Percodan)
Partial Opioid Agonists
- Buprenorphine (Subutex)
- Tramadol
Pure Opioid Antagonists
- Narcan
- Naltrexone
- Nalmefene
Opioids
Opioids include codeine, fentanyl, hydrocodone, meperidine, hydromorphone, methadone, morphine, oxycodone, and heroin. Drugs from the class of opioids are powerful analgesics and used for pain management. From 2000 to 2021, more than one million people in the United States died from opioid drug overdoses and over 80,000 died from opioids in 2021 (14).
Opioids are categorized as schedule 1 or 2 drugs by the Drug Enforcement Agency (DEA). A schedule 2 drug, such as morphine, means that although it has been approved for medical treatment as an analgesic, it has high potential for strong psychological and physiological dependence.
It has been used for over 100 years as an analgesic. Heroin is made by taking morphine, from the opium plant, and adding a chemical reagent that makes it more potent and potentially dangerous. Heroin is a schedule 1 drug and is not approved for any medical use as it is highly addictive.
So how did we get to this point of millions of Americans using and abusing opioids? The documented use of opioids began as early as the 3400 BC in Mesopotamia, which they called the “joy plant.” Opium was used for every medical malady from diarrhea, cholera, rheumatism, fatigue and even diabetes by early Egyptians.
Opium was then regularly traded by Turkish and Arab traders in the 6th century. Opioid use became much more available in the early 1700s as the British refined the production from the Asian poppy plant grown in the British province of India and sold in China. What became helpful as analgesia quickly became popular for treating every malady and even used as entertainment in historical records of opium parties (15). British ships filled 1,000 chests of opium into China in the 1760s and ships gradually increased it to 4,000 chests in 1800 to eventually 40,000 chests in 1838. Opium was so popular in China and the desire for porcelain, silk and tea was equally in demand in the West, so the trading continued.
Because of its powerful addicting properties to the Chinese citizens, the Chinese emperor Yongzheng (1722-1735) eventually prohibited the sale and smoking of opium, which resulted in two infamous Opium Wars. Opium trading eventually became more regulated and slowed during the communist reign in China. Unfortunately, the opium trading continued with new players such as tropical growers and illegal importers from Central and South America to the United States.
In the late 1800’s Bayer created heroin and misuse was rampant causing regulations and taxes to thwart its use (15). Then after WWII and Vietnam another wave of use and abuse crossed America with the resultant reflex to regulate and tax its use. The war on drugs has continued.
Opioids are prescribed to manage moderate to severe pain by blocking the neurotransmitter that sends pain signals. Opioids can be administered via oral, intramuscular, intravenous, subcutaneous rectal or transdermal means. Oral opioids such as codeine, hydrocodone and oxycodone are typically prescribed to manage moderate pain.
Stronger opioids like fentanyl hydromorphone or morphine may be utilized if necessary for more intense discomfort. Morphine is often prescribed for cancer and end-of-life pain treatment because its impact does not reach a plateau point where increasing dosage won’t have any more of an impact.
Opioid Drugs include:
Natural Opioids:
- Morphine
- Codeine (Only Available in Generic Form)
- Thebaine
Semi-Synthetic
- Hydrocodone (Hysingla Er, Zohydro Er)
- Hydrocodone/Acetaminophen (Lorcet, Lortab, Norco, Vicodin)
- Hydromorphone (Dilaudid, Exalgo)
- Oxycodone (Oxycontin)
- Heroin
Fully Synthetic/Manmade
- Fentanyl (Actiq, Duragesic, Fentora)
- Meperidine (Demerol)
- Methadone (Dolophine, Methadose)
- Tramadol
- Levorphanol
- Pethidine
- Dextropropoxyphene
Pharmacokinetics and Pharmacodynamics of Opioids
Analgesics are a drug class that helps relieve the body from the sensation of pain by blocking chemicals in the neurons throughout the brain that sense pain. Neurons send messages of stimuli from the body to the brain and include different types of neurons that sense different things in the body from temperature, pressure, and even blood acidity and alkalinity.
The metabolism of opioids occurs through the Cytochrome (CYP-450 enzymes), which blocks the nerves from relaying messages to the brain (45).
Nociceptors, the nerve receptors for pain, send messages from noxious stimuli to the brain from the skin, walls of organs, and deep within the body such as muscles that something is hurting the tissues. Nociceptors send messages such as pressure, sharp objects, noxious smells, tastes and pain and the brain interprets those for immediate response to protect the body.
There are several neurotransmitters involved in pain signals, but the main ones are glutamine and substance P. When noxious stimuli trigger the primary neuron through the skin or muscle, the message is relayed by a secondary neuron to the spinal cord’s dorsal root ganglion towards the brain for interpretation.
These chemicals are relayed to the thalamus in the brain and then onto the limbic system for an emotional response. Ideally the message to the limbic area of the brain promotes learning to avoid the cause of the noxious substance in the future. Opioids inhibit pain signals at multiple areas in this pathway.
Opioids affect the brain, spinal cord, and even the peripheral nervous system. Opioids work on both directions of messages in the nervous system including the ascending pathways in the spinal cord, which are inhibited and the descending pathways, which block inflammatory responses to noxious stimuli. In the brain, opioids cause sedation and decrease the emotional response to pain.
Heroin, like morphine, passes through the liver and then is released back into the blood where it passes the blood-brain barriers. Heroin is then converted to morphine where it connects with mu receptors, but only faster and heroin is three times more potent than morphine (18).
Opioid receptors are found on both the primary and secondary neurons and when an opioid binds to these receptors no other pain signals are sent up to the brain, making opioids very effective against pain. Naturally these endogenous analgesic receptors include human endorphins, which comes from the name endogenous morphine.
Our bodies have three receptors called mu, kappa and delta which can be activated by opioid agonists like morphine, hydrocodone, or heroin. When mu receptors are activated, dopamine, a natural brain chemical, is also increased, which is the brain’s chemical for pleasure. Pleasurable feelings are inherently worth repeating, which drives the user to repeat the drug use (18).
Short term sensations of opioids include the following:
- Warmth sensation through skin and body
- A feeling of heaviness in arms and legs
- Pain relief
- Dry mouth
- Itchiness
- Possible dry mouth
- Drowsiness
- Slow heart functioning.
- Slow breathing.
- Relaxation
- Sense of well being
Opioid agonists come with additional noxious side effects. When a kappa receptor is stimulated it can also produce hallucinations, anxiety, and restlessness. The Delta and mu receptors can cause respiratory depression because as the midbrain is stimulated it suppresses the body’s ability to detect carbon dioxide levels in the body, which is the main stimulus for breathing. Other negative side effects include constipation, sedation, nausea, dizziness, urinary retention, and tolerance.
Tolerance is the requirement of the body to need increased amounts of the drug to reach its desired effects, which is why opioids can become addictive as the person requires more of the drug to achieve the desired pain relief (18). The key ingredient in opium is morphine, which began to be produced formally by the pharmaceutical company Merck. It was also discovered that when administered by IV, morphine is three times more potent than when administered by other methods such as smoking or snorting.
Long term use of opioids has been shown to cause the deterioration of the brain’s white matter and include long term effects of insomnia, chronic constipation, sexual dysfunction, irregular menstrual cycles in women, kidney disease and physical damage as a result of the administration technique such as snorting, smoking or IV drug use.
Although cocaine and morphine both have effects on the neurotransmitter dopamine, they work in different ways. Whereas the opioids increasing dopamine stimulation, cocaine blocks the reuptake of existing dopamine and makes it last longer producing a longer state of pleasure. Both opioids and cocaine drugs influence the brain’s interpretation of the pleasure drive reinforcing the drive for repeated behavior to get the drug.
In addition to the short-term withdrawal symptoms, long term opioid use causes:
- Decreased ability in decision making.
- Decreased ability for self-reflection and discipline.
- Decreased ability to effectively respond to stress.
Opioids can be effective pain relievers yet can become highly addictive if used improperly. Of the potential adverse reactions associated with opioid use, respiratory depression is the most serious. Those taking opioids must monitor for decreased respiratory rate, oxygen saturation, and heart rate after receiving them. Those taking opioids for the first time or receiving increased doses, taking concurrent benzodiazepine use such as alcohol consumption or other sedatives may experience a more significant respiratory depression.
Treating opioid-induced respiratory depression requires treatment with Naloxone, which binds the mu receptors that opioids act on. Naloxone comes in a variety of preparations, including nasal spray, auto-injectors, and injectables.
Online video resource on how to administer Naxolone: https://www.ama-assn.org/delivering-care/overdose-epidemic/how-administer-naloxone

Image 1. Preparations of Naloxone (48) (52)

Self Quiz
Ask yourself...
- In patients with substance use disorder, how can healthcare providers navigate balancing effective pain relief with risks of opioid medications?
- In patients prescribed opioids for pain management, what primary risk factors should the prescriber consider regarding the development of substance use disorder?
- What should be included in patient education play for those individuals prescribed opioids for pain management?
The Pain of Opioids
The Center of Disease Control has declared the overuse and abuse of opioids an epidemic (14). Ninety-one (91) Americans die every day from an opioid overdose (14). The US consumes 99% of all the world’s hydrocodone, 80% of the world’s oxycodone, and 65% of the world’s hydromorphone prescription opiate supply. Some 25% of all workers’ compensation costs relate to opioids and $56 billion/year is spent on opioid abuse costs. Trends of opioid overdose related deaths have increased 5.5% annually from 6 deaths per 100,000 people in the U.S. in 1999 to 16.3 in 2015.
In adults aged 45-54 the death rate from drug overdose was the highest of all age populations showing a constant trend upward of 10% annual increase in abuse and deaths (16). Clearly, America has an opioid epidemic that is claiming lives and lifestyles. Additional statistics, not as easily identified but very real, include lost productive work hours and loss of meaningful lives, families, and marriages due to opioid abuse (17).
Patients taking opioids must also be monitored for less severe side effects, such as constipation, nausea and vomiting, urinary retention, and itching. Opioids slow peristalsis and increase reabsorption of fluid into the large intestines, thereby slowing the passing of stool and removing the fluid from the stool so that it becomes concrete-like. It is important for the nurse to assess bowel function and encourage fluid/fiber intake and ambulation throughout the course of opioid treatments.
The provider can prescribe a bowel management program that includes a stool softener (such as docusate) and a stimulant laxative (such as sennoside, bisacodyl, or milk of magnesia). Should nausea and vomiting occur, antiemetics (such as prochlorperazine or ondansetron) may be prescribed. Antihistamines (such as diphenhydramine) may be prescribed for subsequent itching; however, they may cause drowsiness and exacerbate the potential for opioid-induced respiratory depression.
Fentanyl
The Centers of Disease Control has estimated that over 20,000 Americans died from fentanyl overdose in 2016 and that rate continues to climb in America. Fentanyl production in China has surged with the high demand in America and it has been called the new nuclear narcotic in the Opium War Against America (19).
Names of Fentanyl
Prescription Street Names
- Abstral: China Girl or China Town
- Actiq: Dance Fever
- Duragesic: Friend
- Fentora: Goodfellas
- Instanyl: Great Bear
- Lazandal: He-Man
- Sublimaze: Jackpot, King Ivory, Murder 8, Tango and Cash, Per-a-Pop (berry flavored Fentanyl lozenge)
One danger of fentanyl use is when fentanyl is mixed in with street drugs such as heroin and the user is unaware of what they are receiving. The quantity of fentanyl in street products also varies widely and can become quickly fatal as doses exceed what would have been carefully prescribed. Illegal street use without guidance, monitoring and education have created the dangerous opioid epidemic. The fully synthetic drugs such as fentanyl are much more potent and have the higher potential for abuse and death (19).
As an analgesic, fentanyl is 100 more potent than morphine and 50 times more potent than heroin (20). Ohio forensic testing in 2017 revealed 99% of their narcotic overdose deaths were fentanyl related and often due to combinations of synthetic fentanyl products including 25 fentanyl analogs such as acryl fentanyl, nor fentanyl, and furanyl fentanyl.
The state also determined that males accounted for 64% of overdose deaths and 92% were white (21). Over half of the deaths in Ohio were in persons aged 25-44 years (22). Trends continue to rise and causes point to the increased prescriptions of opioids for chronic pain and the availability of these drugs in non-prescription form.
Route and Administration of Fentanyl
Opioids can be administered by FDA approval through the subcutaneous, intramuscular, and intravenous and oral routes but due to variations in first-pass liver metabolism there are variations of response by users. Non-prescription drug users often speed the delivery by nasal and intravenous administration.
The potency of fentanyl and carfentanil have been demonstrated by the rapid deleterious effects on police officers who have come in contact with the powder through their skin during drug investigations and raids. One police officer overdosed just by brushing power off his uniform with his hand (23).
Subcutaneous fentanyl is commonly used to address chronic local pain, such as in a transdermal fentanyl patch that has a slow-release action. When fentanyl is delivered through more rapid routes such as IV or intranasal, the response is much quicker and therefore potentially fatal.
Fentanyl is usually administered by injection or topical patch in the hospital setting. It may be prescribed through the intradermal route for chronic pain and is classically used for chronic lower back pain.
Contraindications
It should not be used by someone who is allergic to the drug, has any type of breathing problem, a history of head or brain injury, liver or kidney disease, slow heart rhythms, concomitant use of sedatives like Valium or if a MAO inhibitor has been used in the recent 14 days or the client is already taking another narcotic.
There are no adequate studies to confirm safety or danger in pregnancy or breastfeeding so providers must be notified, and careful clinical decision making must be considered to weigh benefits from any possible damage to infants and mothers as it is a Category C claiming risk cannot be ruled out (24).

Self Quiz
Ask yourself...
- How can healthcare providers effectively communicate the concerns about SUD with someone seeking help for chronic pain?
- What is the role of family members in supporting patients with chronic pain?
- How does chronic pain affect the risk of developing substance use disorder?
Patient Education and Support
Online and face-to-face support groups are available to help with effective and appropriate use of fentanyl. Often the only information provided is about the serious opioid epidemic and potential risk for addiction and abuse, however when used properly and within the clear instructions given by a medical provider who is monitoring for adverse reactions, it can be a helpful option for people in very real chronic pain.
Using any medications as directed is important because the route has been chosen for a specific reason. Unfortunately, a dangerous practice of chewing on a transdermal patch can speed up the delivery of the drug and create addiction and possibly respiratory depression or death. Mental and physical dependence can still occur even at prescribed doses so patients must be carefully monitored.
Supporting patients in their quest for relief from pain and judgment is extremely important. In the national conversation about opioid abuse, patients who have a real need for chronic pain continue to suffer as physicians are attempting to prescribe less, and pharmacies are blocking repetitive refilling of narcotics.
The dialog for effective pain management and effective systems to prevent opioid abuse must continue in creative, non-judgmental, and respectful ways. Encouraging support groups who can speak freely about issues and concerns can be helpful. Not all people who use fentanyl are drug addicts and should not be treated as such.
The pain blocking effects of intradermal fentanyl often takes from 12-48 hours and often up to 72 hours and may require a breakthrough alternative to pain relief until the full effect is in action. Titrating carefully for pain relief is required based on individualized patient needs. Variations in the need for higher dosages depends on the location of a transdermal patch, the quantity of fat on the body area and dryness of the skin where it is applied.
All patients should be taught to avoid alcohol consumption if using fentanyl. Patients also need to be aware that the narcotic may remain in the blood stream for up to three days and can be in hair and urine. Drug testing for abuse or employer requirements is most commonly done on hair and urine.

Self Quiz
Ask yourself...
- How would you explain to a patient the difference between fentanyl and heroin?
- How would you educate teens about the common street names for fentanyl?
- What alternatives to fentanyl are there that you could use in your practice?
Patient-Controlled Analgesia
Patient-controlled analgesia (PCA) allows a patient to self-administer opioid medications such as morphine, hydromorphone, and fentanyl without requiring a nurse to give each injection, by using an automatic pump programmed with their dosage amount and rate/volume settings (37). A locked computerized pump connects directly to their IV line where medication syringes can be safely locked inside ready for an infusion at scheduled rates/volume settings; its programming ensures medication infusion occurs at its intended rate/volume setting without exceeding prescribed amounts.
Doses of medication can be self-administered on an as-needed basis by pressing a button. Patients may give themselves doses according to an adjustable schedule that includes preset interval times and dose limits per hour, up to four in total per hour limit. If these criteria are fulfilled, the PCA button illuminates to alert patients that doses can be administered when needed. Even when not illuminated, pressing it still delivers medication.
PCAs may only be used for patients who are alert, oriented, and can independently press the button. Because small doses of opioids are administered frequently, it is important to monitor patients for oversedation and respiratory depression. To reduce the risk of these adverse events, the patient and all caregivers should understand that no one should press the PCA button except the patient. Nurses should also ensure that the PCA button is easily within the patient’s reach, as patients on PCAs are at a high risk for falling.
Given the potential risk associated with PCA medication errors, both incoming and outgoing nurses should independently double check to verify correct drug, concentration, and dose (loading dose, PCA demand dose, continuous dose), lockout interval and 4-hour limit settings of their pump settings (36). When providing bonuses or changing any settings or replacing medication syringes two nurses will always be needed to verify results accurately.
As part of their PCA treatment, it is vital that patients carefully monitor their vital signs to detect possible indicators of respiratory depression such as decreased respiratory rate, oxygen saturation levels or heart rate. Nurses must follow organizational protocols when administering PCA medications – usually including taking baseline vital signs prior to commencing administration, for an extended period post administration and then every two hours for its duration.
Co-Analgesic Medications
Co-analgesics, commonly referred to as adjuvants, are medications with analgesic properties; however, their primary purpose is not pain relief. For instance, antidepressants are usually taken for treating depression but may also help manage chronic pain symptoms, like sleep issues and muscle spasms. Anxiolytics may help relieve anxiety symptoms but could potentially also treat chronic pain-related anxiety as well as relax muscles. Anticonvulsants used for seizures also block pain receptors and help with providing relief from certain forms of neuropathic pain while corticosteroids reduce inflammation while simultaneously managing this kind of discomfort from injured nerves.
Patient Education
Prescribers have an obligation to educate patients appropriately on pharmacological pain interventions in a culturally and linguistically sensitive manner. Drug education should help the patient comprehend the treatment plan, improve adherence to the treatment plan, alleviate fears while setting realistic expectations and discussing concerns openly, all to ultimately contribute to improved health, well-being, and patient outcomes.
Education should start when treatment commences and continue throughout the duration of therapy. A personalized approach tailored specifically for each individual should include considering the primary language spoken by the patient as well as culture, age, cognitive function, and health literacy level.
Simple language with clearly defined technical terms used along with open-ended questions as well as visual materials like demonstration videos/pictures or handouts may prove highly useful during education sessions. It is crucial not to wait until severe discomfort before seeking medication as once pain becomes extreme it becomes much harder to control and may require stronger medications.
Nurses should help patients understand the typical progression of pain medication prescribed through the pain ladder model. Patients need to comprehend why nonopioids need to come first before adding opioids or adjuvants into the regimen. Acute surgical pain patients, in particular, must know that although opioids might initially provide relief, their ultimate aim should be reducing dependency through intravenous, oral, and then nonopioids prescription.
Patients must also be educated on the need to use only as much pain relief medication as necessary to reach the intended pain goal. If their provider prescribes two tablets every four to six hours, for instance, it’s wiser for them to start with just one and gradually add on additional pain relievers as required. They should be advised against exceeding prescribed amounts as soon as they start feeling any relief. Before initiating any medication treatment plan, patients must receive proper instruction about its name, dose, route, and frequency of administration.
It’s also essential that any special instructions regarding when it should be taken such as with or without food, be written for the patient as well as storage tips to protect medications safely away from children by either keeping out of reach or locking up safely.
Every time they receive medication, patients should be educated on its potential adverse side effects as well as when to report them. When opioids are prescribed, patients should understand the potential risk for constipation, respiratory depression and addiction, and also be advised that taking opioid medication could make them feel sleepy. Additionally, they must not consume alcohol, drive heavy machinery, take any unapproved drugs while on such medicines or take other drugs not approved by their prescriber at that time.
Patients often hold incorrect assumptions about pain management that require being addressed. Therefore, it’s crucial that an assessment be completed of each individual and any misconceptions discovered. For instance, they might fear taking opioids due to concerns they will become dependent. Although long-term opioid usage could potentially lead to dependence issues, short-term use should still be weighed against its benefits regarding being tapered as quickly as possible.

Self Quiz
Ask yourself...
- In patients undergoing pain management treatment, what do the potential consequences of untreated substance use disorder?
- How can you as a healthcare provider minimize the risk of opioid misuse in patients with chronic pain?
- What are the potential advantages and disadvantages of long-term narcotic therapy for chronic pain management?
Non-Pharmacological Pain Alternatives
Nonpharmacological interventions may be combined with or without pharmaceutical medicines as they often provide tremendous benefits. As with all treatments, nonpharmacological interventions must be documented within a plan of care to determine their ability to fulfill pain relief goals effectively. Non-pharmacological pain management techniques may fall under either complementary or alternative medicine categories. Though sometimes interchanged, there is a distinct distinction: complementary therapies work alongside pharmaceutical pain treatments while alternative therapies are practiced as an alternative from standard pharmaceuticals.
Substance Use Disorder
According to the Centers for Disease Control and Prevention (CDC), one out of every seven Americans reports having experienced some form of substance use disorder in the last month (25).
Defining Substance Use Disorder (SUD)
Substance Use Disorder, according to the Centers for Disease Control (CDC), is defined as any pattern of substance abuse which leads to clinically significant impairment or distress, from substances including alcohol, cannabis, hallucinogens, inhalants, opioids, sedatives, hypnotics, anxiolytics, stimulants, and tobacco (25). A substance use disorder (SUD) may range in severity between mild, moderate, or severe cases.
Addiction, which is one of the more serious forms of substance use disorder (SUD), refers to continued drug consumption despite negative consequences, and should be seen as a medical disease rather than character description. Therefore, people living with SUDs should not be labeled abusers, addicts, alcoholics, or “medication seekers,” since such language can be stigmatizing and isolating. To reduce the stigma surrounding substance use disorders we focus instead on medical diagnoses of each specific case and offer effective solutions.
Though Substance Use Disorder (SUD) is considered treatable, recovering can still be challenging for many. Individuals suffering from an SUD often cannot stop taking the substance in question without experiencing excruciating withdrawal symptoms. Sometimes another drug may help wean patients off problematic opioids, such as methadone, buprenorphine or naltrexone which are all widely prescribed to treat opioid addictions. Patients may benefit from participating in programs like 12-Step Facilitation Therapy, outpatient counseling to better understand addiction and triggers, or inpatient rehabilitation at full-time facilities that offer supportive environments without distractions or temptations for recovery.
Definitions of Use and Abuse
Understanding the differences between dependence and addiction is paramount for understanding opioid misuse and abuse. Dependence refers to physical tolerance that requires increased doses to produce desired responses. Addiction occurs when that threshold has been passed and greater amounts must be administered for desired responses to be realized. Withdrawal from drugs will often bring on physical symptoms like shaking, tremors, nausea, and vomiting.
Addiction refers to an emotional need for drugs with desirable effects that leads to strong drug seeking behavior. Individuals who are opioid dependent may oscillate between feeling sick without taking their prescribed dose and experiencing the desired “high” after taking it. Being addicted is the driving force for individuals trying to obtain and take more opioids in order to avoid withdrawal symptoms.
Withdrawal symptoms include the following (16):
- Intense drug cravings
- Depression, withdrawal fears, anxiety
- Sweating, watery eyes, runny nose
- Restlessness, yawning
- Diarrhea
- Fever and chills
- Muscle spasms
- Tremors and joint pain
- Stomach cramps
- Nausea and vomiting
- Elevated heart rate and blood pressure
Populations at Risk
People at risk for opioid dependence and addiction are seen in every age, gender, ethnicity, and culture. Physical dependence varies as a genetic component has been identified, which influences how quickly a person may slide from occasional use to physical need and addiction to the drug (26). Susceptible populations have typically included the homeless, alcoholics and those with personality or mental health disorders who look for opiates to block the emotional pain of life stressors.
Healthcare professionals who also experience great work stress have a higher risk of becoming dependent or addicted to opiates due to back injuries and easier access to narcotics in their work setting (26).
How Pain Control Becomes SUD
Scheduled drugs such as narcotics, and even alcohol have the potential to become an addictive substance. Opioid abuse may lead to opioid Use Disorder, or OUD for short. OUD occurs due to problematic patterns of opioid usage. Opioids work by stimulating endorphin release in the brain, producing feelings of pleasure that make them highly addictive. Opioid use disorder (OUD), however, often leads to physical dependence, which is when someone believes they cannot function without using certain substance(s).
Dependence should not be mistaken for tolerance, which occurs when your body requires increasing quantities of the drug to achieve similar pain relief over time. When someone who is dependent on drugs reduces or ceases taking it altogether, withdrawal symptoms could ensue. SUDs have become a serious public health risk in the U.S.
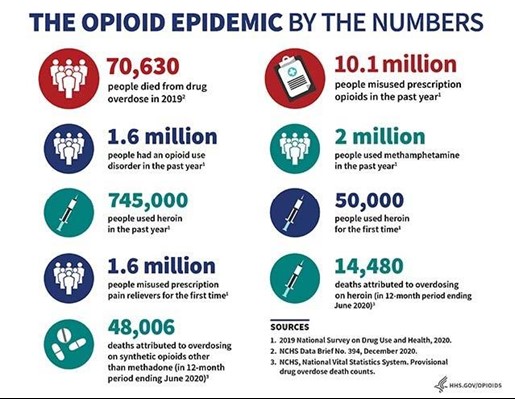
Figure 3. These data, from 2019–2020, show the number of people in the United States affected in different ways by the opioid epidemic. (52)
Prevention Strategies
The best treatment for any drug overdose is prevention. Due to the national attention to the opioid epidemic and harsh statistics of deaths caused by fentanyl overdose, political, federal, state and even pharmaceutical companies have made efforts to address the problem. One strategy is to decrease the availability of prescriptions for opioids and fentanyl, however that makes it difficult for those with real pain to receive the medication.
Monitoring drug prescription use, and public education are additional strategies. The Food and Drug administration has produced guidelines for effective pharmacological use of opiates, which includes the identification of persons at risk, assessing a patient’s benefit vs. risk, developing, and using tools to decrease risks of opiate prescription use such as contracts for pain management and standards of required 30-day physician visits before new prescriptions can be refilled.
The CDC Clinical Practice Guidelines for Prescribing Opioids for Pain advises healthcare providers to review a patient’s history with controlled substance prescriptions prior to prescribing opioids (28).
Providers can gain insight into a patient’s history of opioid prescribing via an electronic database tracking-controlled substance prescriptions known as Prescription Drug Monitoring Program (PDMP). PDMPs also alert healthcare providers of other medications a patient is taking that might increase his/her risk for opioid overdose, making PDMPs particularly helpful when transitioning between providers or when medication histories cannot be provided by patient themselves. Prior to prescribing opioids and at least once every three months when continuing therapy, the database should be reviewed.
Online Resource: CDC Public Health Law Program – provides resources regarding state laws on prescription drug misuse and abuse. https://www.cdc.gov/phlp/publications/topic/prescription.html
Prevention strategies include:
- Patient education regarding use of opiates
- Pain contract signed by patient to agree to terms of drug use
- Prescription monitoring programs to detect multiple use of pharmacies and physicians for opiates
- Detection of inappropriate prescribing of opioids
- Photo identification to pick up opioid prescriptions
- Urine toxicology screening for employees
- Safe disposal of unused opioids
- Referrals to pain and addiction specialists
- Use of semi-synthetic opioid alternatives
Patient education regarding the use of opiates, and truly all prescription medications, is essential to understand the need for the drug, its side effects, and adverse effects. An additional pain contract should be included with patient education, which outlines the parameters for the use of the drug. Especially when used for chronic pain management, patients should be partners with the prescriber to outline when the drug will be used and for how long.
Prescription monitoring programs include detection systems in pharmacies and the local district that identify patients who have filled a narcotic prescription. In many states, photo ID is already required for the purchase of cigarettes or alcohol and could become a beginning point to dissuade unauthorized and high frequency prescription use.
According to the National Alliance for Model State Drug Laws, currently 85% of states require ID for narcotic prescription use (27). Some drug stores even run the name of a client picking up a narcotic prescription through a drug monitoring data system for alerts. The challenge is for busy pharmacists to take the time to use the monitoring system and for patients to be patient as the process is completed.
Possible “red flags” that could lead to prescription denial:
- A pain medication not previously filled the pharmacy.
- A new doctor is writing a prescription for the same pain medication.
- A doctor writing a prescription who is not in a “reasonable geographic location” near the pharmacy.
- A patient paying for a prescription in cash.
- A patient seeking an early refill of a prescription.
- A patient seeking an “excessive” number of pills.
- A patient taking the same pain medication for more than 6 months.
Another strategy includes receiving prior authorization before opiates can be filled. In 2007 the FDA passed an amendment to create a patient registry for opioids. In 2012, Blue Cross Blue Shield began to require prior authorization for more than a one-month supply of opioids in a two-month period. By this simple process alone in the state of Massachusetts, the number of opioid prescriptions decreased by more than 6,500,000 pills in one year (29, 31).
Safe disposal of opioids is a challenging issue as many people believe that flushing them down the toilet is appropriate, which it is not. Public education and awareness programs should also include safe medication disposal such as mixing with used coffee grounds, dirt or kitty litter and placing in a sealed container to then dispose of in the garbage. Used opioid patches should be folded in half on the sticky sides and disposed of in a sealed container in the garbage.
Patient Screening Tools
Several screening tools are available to help clinicians identify when a patient taking opioids may be experiencing dependence or addiction.
Screening, Brief Intervention, and Referral to Treatment (SBIRT) is an evidence-based practice used to identify, reduce, and prevent problematic use, abuse, and dependence on alcohol and illicit drugs” (30). The SBIRT model was inspired by a recommendation from the Institute of Medicine to increase community-based screening for health risk behaviors, including substance use. SBIRT is an early and brief intervention of 15-30 minutes and billable to Medicare/Medicaid. The screening and referral to treatment includes a patient encounter, history, physical exam, clinical diagnosis, and plan for care specific to the concern of substance abuse other than for those patients already identified with severe substance abuse. The SBIRT screening tool can be as simple as asking several key questions of patients receiving narcotics and opioids at every doctor’s office visit.
The Opioid Risk tool is another brief screening tool of questions to help identify a patient at increased risk for dependence and abuse. Currently no one tool has been identified to be better than any others, nor is any one tool sufficient to identify drug behaviors of chronic pain patients using opioids (31, 32). Here is an example of an opioid screening tool:

Figure 4. Example of Opioid Screening Tool (50)

Self Quiz
Ask yourself...
- For patients with a history of substance use disorder, what ethical issues should healthcare providers consider?
- What screening tools are available to help screen patients for substance use disorder?
- How can screening tools be used for those who already have SUD?
- What nonpharmacological approaches to both acute and chronic pain can you confidently prescribe?
Treatment for Substance Use Disorder
Managing pain for those living with substance use disorder can be challenging. Everyone deserves respect and to have their pain appropriately managed, which requires taking an integrated, patient-centric approach to include both pharmaceutical and nonpharmaceutical interventions. Before medicating with opioids for pain management in those suffering from OUD, nonpharmacological therapies and nonopioid medications must first be explored as effective options. Such nonpharmacological approaches might include therapeutic exercise, physical therapy, cognitive-behavioral therapy (CBT), complementary and alternative medicines, and complementary and alternative remedies (CAMs).
Nonopioid medications that could be useful include nonsteroidal anti-inflammatory drugs (NSAIDs), topical analgesics and adjuvant medicines like serotonin-norepinephrine reuptake inhibitors, CBT, and combination SSRI/SSNI or tricyclic antidepressants.
If pain levels necessitate opioid use, opioids should not be withheld from patients with OUDs. As with any patient, it’s essential that shared goals and risks are established along with an agreed upon treatment agreement and close monitoring via scheduled follow-up visits in order to reassess pain levels regularly. In general, starting off with a low dose and gradually increasing as needed is the standard. Creating a pain agreement with the patient is required.
Reducing Stigma Against Substance Use Disorder
In addition, working to decrease the stigma of SUD can be helpful for those seeking medical assistance (33). Pain clinics are a newly developed specialty, which allow patients suffering from chronic pain to work with a pain specialist for more effective management using a variety of modalities. It is estimated that at least 100 million Americans live with chronic pain. Pain clinics can offer help focusing on procedures that deal with specific pain such as neck and lower back pain.
They can also approach pain through an interdisciplinary approach involving psychologists, physical therapists, nutritionists, occupational and vocational therapists in addition to physicians and nurses. Other modalities such as acupuncture, biofeedback, cognitive behavioral therapy, water therapy, massage and meditation can be options for chronic pain in lieu of just relying on opioids. Patient education, as well as for the prescriber, needs to include these alternative treatment strategies.
Recognition of opioid use within healthcare professionals has been addressed by the National Council of State Boards of Nursing. A free educational webinar for understanding substance use disorder in nursing is available to nurses and managers to help identify signs of opioid use and abuse. It also outlines the system of helping professionals with therapy and recovery. It can be accessed at https://www.ncsbn.org/nursing-regulation/practice/substance-use-disorder/substance-use-in-nursing.page

Self Quiz
Ask yourself...
- How does stigma surrounding opioid use affect those seeking pain management treatment?
- How can healthcare providers address the psychological and emotional aspects of pain in patients with substance use disorders?
- What policies and regulations are in place to promote safe and responsible prescribing practices for narcotics for pain management?
Acute Treatment for Overdose
Treatment for opioid abuse generally starts with treatment of withdrawal in the acute phase. Managing symptoms of overdose and preventing death are the first objective. Securing an airway and supporting the patient during the tremors, seizures, hypertension, nausea, vomiting, and pain are often handled in an emergency room (ER) and medical/surgical setting.
Naloxone (Narcan) can be used for reversal of opioid overdose and is available in IV, SQ, IM and nasal routes. If a patient is unconscious, follow the ABCs of emergency response such as calling 9-1-1, checking for a pulse, securing an open airway, and providing rescue breaths. Give the first full dose of naloxone and continue rescue breaths. If the patient doesn’t respond give the second full dose of naloxone.
Patients will often respond quickly and be confused and possibly combative. Monitor the patient after recovery with naloxone to prevent another dose of an opioid and follow up medical attention.
Using pharmacological blocking agents is helpful in stopping opioid overdose. Antagonist medications block opioid receptors so that the desired effect is no longer active. Two opiate substitution medications are currently available in the United States and include methadone and levomethadyl acetate but are only available in strictly regulated environments where medication is received under clinical observation and limited out-patient use.
Methadone and buprenorphine are synthetic opioid agonists and act on the same mu receptors that opioids activate and therefore has been a popular treatment for addiction, known as Opioid Substitution Therapy (OST). Methadone has a slow onset of action and long elimination half-life of about 24 hours. A longer acting opioid receptor agonist is Buprenorphine, a partial opioid agonist and can reduce cravings and symptoms of withdrawals. These drugs can be taken less frequently and can help wean a patient from the more fatal opioids. Control trials show that it is more effective than a placebo and can help decrease fatalities from opioids. Access to these drugs is still dependent upon physician-controlled prescribing or treatment programs.
Getting into approved treatment programs where these drugs can be given and monitored closely, in combination with behavioral therapy is often difficult, expensive, and not approved by insurance companies. The strict control of these opiate-substitution drugs is necessary because they do produce a euphoric sensation like the opiates and the tight regulation is due to the fear of creating a new market of illicit use for these. These medications can be given in sublingual, oral and even intranasal forms. By giving these opioid antagonist drugs, they act as competition for the mu receptors and ideally block the effectiveness of other opiates.
Future of Substance Use Disorder Efforts
Our nation’s opioid epidemic and increase in SUD prevalence is complicated and concerning. Thousands of lives are lost needlessly due to SUD addiction and overdose. Education of prescribers and patients is needed. Legislation is needed and debated for opioids available on the market and how to regulate their use.
States must decide on the training and availability for the use of naloxone and opioid agonists for overdose and weaning. Healthcare professionals must learn to collaborate with pharmacists, nutritionists and behaviorists who work with those with chronic pain to offer more options for pain management. Schools and public officials such as police workers must be able to improve security to dissuade drug sales.
Each of the proposed strategies to fight our national war on drugs is at various stages of development and implementation and take time. The cost to implement programs, educate stakeholders and evaluate any negative consequences to appropriate treatment plans for pain needs patience. In the meantime, small efforts can save lives. Your efforts to learn more about the substance use disorder and the opioid epidemic are a notable step for improvement.
Key Terms
Acute pain: short-term pain, typically lasting from minutes to up to three months.
Acupuncture is a pain management technique that inserts thin steel needles into the skin to stimulate specific points throughout the body.
Addiction is the most severe form of substance use disorder, in which there is continued use of the substance despite negative consequences.
Alternative therapies treatments used in place of pharmacological pain management.
Animal-assisted therapy is a treatment that utilizes animals to reduce pain, anxiety, or depression.
Aromatherapy is the inhalation or dermal application of essential oils.
Breakthrough pain: sudden increase in pain that lasts for a short time.
Chiropractic therapy is a pain management technique that manipulates the spine, joints, and skeletal system.
Chronic pain: pain lasting longer than six months.
Complementary therapies treatments used in combination with pharmacological pain management.
Dependence inability to function without the use of a substance.
Faces scale: a visual tool for assessing pain with children and others who cannot quantify the severity of their pain on a numerical scale.
FLACC scale: a pain scale used to assess pain in children between the ages of 2 months and 7 years, as well as those unable to verbally communicate.
Hypnosis is the creation of a trance-like state to enhance awareness of feelings, thoughts, and sensations.
Imagery positive, relaxing images created in the mind.
Massage is a pain management technique that manipulates the soft tissues of the body to relieve tension and create relaxation.
Meditation is the practice of breathing and repeating certain words to reduce stress and put the mind at ease.
Mindfulness is the practice of focusing on the present moment to create awareness of thoughts, feelings, the body, and the environment.
Numerical scale: a pain scale that rates pain on a scale of 0 to 10.
Neuropathic pain: pain caused by damage to nerves or other parts of the nervous system.
Nociceptive pain: pain caused by damage to body tissue.
Nociceptor: a type of sensory receptor that responds to potentially damaging stimuli by sending nerve signals to the spinal cord and brain.
Normal pain: pain of the expected severity and duration, according to its cause.
Pain is an uncomfortable or unpleasant sensation that typically signifies injury or illness.
Opioid use disorder (OUD): a type of substance use disorder caused by a problematic pattern of opioid use leading to physical dependence.
Pain Assessment in Advanced Dementia Scale: a pain scale used to assess pain in patients with advanced dementia.
Phantom pain: pain perceived to be coming from a missing body part.
Referred pain: pain in one part of the body that is caused by pain in a different location of the body.
Reflexology is a pain management technique that applies massage to specific pressure points aligned with the body in the hands and feet.
Reiki is a pain management technique in which one person uses lightly placed hands to guide energy throughout another person’s body.
Somatic pain: pain experienced in the muscles, skin, or bone.
Substance Use Disorder (SUD) is a problematic pattern of substance use leading to clinically significant impairment or distress.
Tai chi is a practice that combines exercise and meditation with slow body movement and controlled breathing.
Thermotherapy is the application of heat or cold to alter the cutaneous, intra-articular, and core temperature of soft tissues.
Tolerance: the state of requiring more of a drug over time to achieve the same level of pain relief
Yoga: the practice of using specific stretches, poses, meditation, and controlled breathing to balance the mind and body.
Visceral pain: pain experienced in the internal organs.
Withdrawal: physical and mental symptoms experienced when a person suddenly stops or decreases the use of an addictive substance.
References + Disclaimer
- Finley CR, Chan DS, Garrison S, Korownyk C, Kolber MR, Campbell S, Eurich DT, Lindblad AJ, Vandermeer B, Allan GM. What are the most common conditions in primary care? Systematic review. Can Fam Physician. 2018 Nov;64(11):832-840. PMID: 30429181; PMCID: PMC6234945.
- Substance Abuse and Mental Health Services Administration. 2021 NSDUH Annual National Report. Available at https://www.samhsa.gov/data/report/2021-nsduh-annual-national-report. Last accessed April 21, 2023.
- Ulrich, L. (2024). McLaren. The Five Types of Pain. Retrieved from https://www.mclaren.org/main/news/the-five-types-of-pain-4386
- International Association for the Study of Pain (IASP). (2021). Acute Pain. https://www.iasp-pain.org/resources/topics/acute-pain/
- Cleveland Clinic. (2021, May 12). Phantom Limb Pain. https://my.clevelandclinic.org/health/diseases/12092-phantom-limb-pain
- Scher C, Meador L, Van Cleave JH, Reid MC. Moving Beyond Pain as the Fifth Vital Sign and Patient Satisfaction Scores to Improve Pain Care in the 21st Century. Pain Manag Nurs. 2018 Apr;19(2):125-129. Doi: 10.1016/j.pmn.2017.10.010. Epub 2017 Dec 15. PMID: 29249620; PMCID: PMC5878703.
- Kishner, S. (2022). Pain Assessment. MedScape. Retrieved from https://emedicine.medscape.com/article/1948069-overview?form=fpf
- FLACC Scale Archived 2008-12-10 at the Wayback Machine (Extracted from the FLACC: A behavioral scale for scoring postoperative pain in young children, by S Merkel and others, 1997, Pediatr Nurse 23(3), p. 293–297).
- Dunford E, West E, Sampson EL. Psychometric evaluation of the Pain Assessment in Advanced Dementia scale in an acute general hospital setting. Int J Geriatr Psychiatry. 2022 Dec;37(12):10.1002/gps.5830. Doi: 10.1002/gps.5830. PMID: 36317464; PMCID: PMC9828226.
- Givler A, Bhatt H, Maani-Fogelman PA. The Importance of Cultural Competence in Pain and Palliative Care. [Updated 2023 May 22]. In: Stat Pearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493154/
- Xie W, Luo Y, Liang X, Lin Z, Wang Z, Liu M. The Efficacy and Safety of Aspirin as the Primary Prevention of Cardiovascular Disease: An Updated Meta-Analysis. Ther Clin Risk Manag. 2019 Sep 24; 15:1129-1140. Doi: 10.2147/TCRM.S198403. PMID: 31576136; PMCID: PMC6767763.
- Medline. (2023). Acetaminophen. Retrieved https://medlineplus.gov/druginfo/meds/a681004.html
- Goldberg E. (2017). Acute liver failure in adults: Etiology, clinical manifestations and diagnosis. Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/acute-liver-failure/symptoms-causes/syc-20352863
- Centers for Disease Control and Prevention,(2023). National Center for Injury Prevention and Control. Retrieved from https://www.cdc.gov/drugoverdose/deaths/index.html#:~:text=Opioids%E2%80%94mainly%20synthetic%20opioids%20(other,of%20all%20drug%20overdose%20deaths).
- DEA Museum. Opium Poppy. History of Opium. Retrieved from https://museum.dea.gov/exhibits/online-exhibits/cannabis-coca-and-poppy-natures-addictive-plants/opium-poppy#:~:text=The%20earliest%20reference%20to%20opium,it%20on%20to%20the%20Egyptians.
- National Institute on Drug Abuse, 2018. Prescription Opioids and Heroin. Retrieved from https://www.drugabuse.gov/publications/research-reports/relationship-between-prescription-drug-abuse-heroin-use/introduction
- American Society of Addiction Medicine (ASAM). Practice Guidelines 2020. Retrieved from https://downloads.asam.org/sitefinity-production-blobs/docs/default-source/guidelines/npg-jam-supplement.pdf?sfvrsn=a00a52c2_4
- Rikard, S., Michaela; Nataraj,N., Zhang, K; Strahan,A., Mikosz, C.; Guy, G., Logitudinal dose patterns among patients newly initiated on long-term opioid therapy in the United States, 2018-2019; an observational study and time-series cluster analysis. PAIN 164(12); p 2675-2683, December 2023.
- Prekupec MP, Mansky PA, Baumann MH. Misuse of novel synthetic opioids: a deadly new trend. J Addict Med 2017; 11: 256–265. Retrieved from https://journals.lww.com/journaladdictionmedicine/fulltext/2017/08000/Misuse_of_Novel_Synthetic_Opioids___A_Deadly_New.5.aspx
- Drug Enforcement Administration- DEA. Emerging Threat Report: Retrieved from https://ndews.umd.edu/resources/dea-emerging-threat-reports
- Ellis R. and Sidner S. (2016). Prince died of accidental overdose of opioid fentanyl, medical examiner says. CNN News. Retrieved from https://www.cnn.com/2016/06/02/health/prince-death-opioid-overdose/index.html
- Herald. (2018). The Government must step up fight against fentanyl. Retrieved March from http://www.sharonherald.com/opinion/editorials/government-must-step-up-fight-against-fentanyl/article_0a05ffed-36ee-5d7b-9f34-3ec0bd37a40c.html
- Moshtagian A. Police Officer overdoses after brushing fentanyl powder off his uniform. CNN 2017. Retrieved from https://www.cnn.com/2017/05/16/health/police-fentanyl-overdose-trnd/index.html
- Drugs.com 2024
- Centers for Disease Control (2023). Substance Use Disorder Statistics Retrieved from https://www.cdc.gov/drugoverdose/featured-topics/substance-use-disorders/index.html
- Centers for Diseases Control (2023). Addiction Medicine Primer. Retrieved from https://www.cdc.gov/opioids/addiction-medicine/primer.html
- Popescu, A., Marian, M., Drăgoi, A.M., & Costea, R. (2021). Understanding the genetics and neurobiological pathways behind addiction (Review). Experimental and Therapeutic Medicine, 21, 544. https://doi.org/10.3892/etm.2021.9976.
- Dowell, D., Ragan, KR., Jones, CM, Baldwin, GT, Chou, R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain. United States, 2022. MMWR Recomm Rep 2022;71(No. RR-3):1-95.
- Anderson, T. The Boston Globe (2019). Opioid-related overdose deaths declining. Retrieved from https://www.bostonglobe.com/2020/02/12/metro/opioid-related-overdose-deaths-down-mass/
- Substance Abuse and Mental Health Services Administration (2023). Statues, Regulations and Guidelines for Opioid Use and Abuse. Retrieved from https://www.samhsa.gov/medications-substance-use-disorders/statutes-regulations-guidelines
- National Institute on Druge Abuse. (2021). Opioid risk tool. NIH. https://nida.nih.gov/nidamed-medical-health-professionals/screening-tools-resources/opioid-risk-tool-oud-ort-oud 
- CDC. (2022a, June 1). Understanding the Epidemic. https://www.cdc.gov/opioids/basics/epidemic.html
- CDC. (2022b, November 3). Prescription Drug Monitoring Programs (PDMPs). https://www.cdc.gov/opioids/healthcare-professionals/pdmps.html
- CDC. (2023, April 10). Stigma Reduction. https://www.cdc.gov/stopoverdose/stigma/index.html
- 35. Yam MF, Loh YC, Tan CS, Khadijah Adam S, Abdul Manan N, Basir R. General Pathways of Pain Sensation, and the Major Neurotransmitters Involved in Pain Regulation. Int J Mol Sci. 2018 Jul 24;19(8):2164. Doi: 10.3390/ijms19082164. PMID: 30042373; PMCID: PMC6121522.
- Pastino A, Lakra A. Patient-Controlled Analgesia. [Updated 2023 Jan 29]. In: Stat Pearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551610/
- National Institutes of Health. (2023). Complementary and Alternative Therapies. Retrieved from https://www.cancer.gov/about-cancer/treatment/cam#:~:text=Patients%2C%20their%20families%2C%20and%20their,Cancer%20Complementary%20and%20Alternative%20Medicinej
- 
- Israel S, Perazzo S, Lee M, Samson R, Safari-Ferra P, Badh R, Abera S, Soghier L. Improving Documentation of Pain Reassessment after Pain Management Interventions in the NICU. Pediatr Qual Saf. 2023 Sep 28;8(5): e688. Doi: 10.1097/pq9.0000000000000688. PMID: 37780605; PMCID: PMC10538901.
- Ho J, Burger D. Improving medication safety practice at a community hospital: a focus on bar code medication administration scanning and pain reassessment. BMJ Open Qual. 2020 Sep;9(3): e000987. Doi: 10.1136/bmjoq-2020-000987. PMID: 32958472; PMCID: PMC7507888.
- Cragg, A.; Hau, J. P.; Woo, S. A.; Kitchen, S. A.; Liu, C.; Doyle-Waters, M. M.; Hohl, C. M. Risk factors for misuse of prescribed opioids: a systematic review and meta-analysis. Annals of Emergency Medicine. 2019;74(5), 634-646. Doi: 10.1016/j.annemergmed.2019.04.019 Source[Meta-analysis, Systematic Review]
- Drew, D. J.; Gordon, D. B.; Morgan, B.; Manworren, R. C. “As-Needed” Range Orders for Opioid Analgesics in the Management of Pain: A consensus statement of the American Society for Pain Management Nursing and the American Pain Society. Pain Management Nursing. 2018;19(3), 207-210. [Review Articles, Expert/Committee Opinion, Core Curriculum, Position Statements, Practice Bulletins]
- Tylenol (acetaminophen) professional product information. Fort Washington, PA: McNeil Consumer Healthcare; 2010.
- Wongrakpanich S, Wongrakpanich A, Melhado K, Rangaswami J. A Comprehensive Review of Non-Steroidal Anti-Inflammatory Drug Use in The Elderly. Aging Dis. 2018 Feb 1;9(1):143-150. Doi: 10.14336/AD.2017.0306. PMID: 29392089; PMCID: PMC5772852.
- Thigpen, J.C., Odle, B.L. & Harirforoosh, S. Opioids: A Review of Pharmacokinetics and Pharmacodynamics in Neonates, Infants, and Children. Eur J Drug Metab Pharmacokinet 44, 591–609 (2019). https://doi.org/10.1007/s13318-019-00552-0
- NIDA. 2021, June 1. Fentanyl Drug Facts. Retrieved from https://nida.nih.gov/publications/drugfacts/fentanyl.
- Wisconsin Technical College System (WTCS). (n.d.). Comfort basic concepts. Nursing Fundamentals. Copyright © by Open Resources for Nursing (Open RN)https://wtcs.pressbooks.pub/nursingfundamentals/chapter/11-2-comfort-basic-concepts/
- California Department of Public Health. (2023). What is naloxone? Image Source: https://www.cdph.ca.gov/Programs/CCDPHP/sapb/Pages/Naloxone.aspx
- Webster LR, Webster R. (n.d.). Opioid screening tool. https://nida.nih.gov/sites/default/files/opioidrisktool.pdf
- Prescriptive authority – advanced practice registered nurse, Colorado. Penal code § 12-255-112. Revised 2023. https://drive.google.com/file/d/14oArZBhbhVoeY-kUTb3t-tm1mCK2BEyg/view
- Research Gate. (n.d.). The World Health Organization (WHO) pain ladder modified for acute pain management. https://www.researchgate.net/figure/The-World-Health-Organization-WHO-pain-ladder-modified-for-Acute-Pain-Management-a_fig1_340312749
- U.S. Department of Health and Human Services. (2022, December). Opioid facts and statistics. https://www.hhs.gov/opioids/statistics/index.html
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

