Course
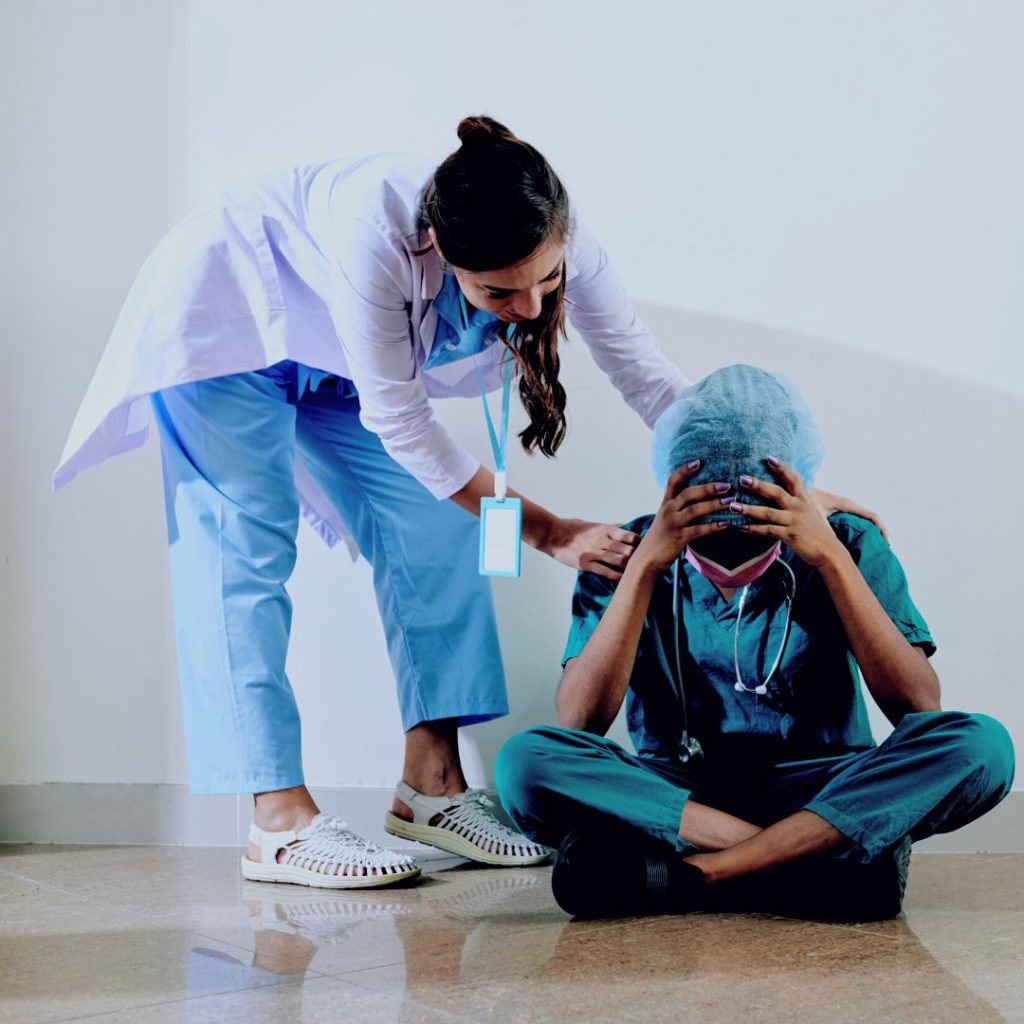
Nurse Burnout
Course Highlights
- In this Nurse Burnout course, we will learn about the differences between nurse burnout and compassion fatigue.
- You’ll also learn individual and organizational behaviors/ factors that heighten the risk for nurse burnout.
- You’ll leave this course with a broader understanding of self-care strategies available to lessen nurse burnout.
About
Contact Hours Awarded: 1
Course By:
Maureen Sullivan-Tevault
Maureen Sullivan-Tevault, RN, BSN, CEN, CDCES
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
In May 2022, during Mental Health Awareness Month, the United States Surgeon General Dr. Vivek Murthy issued a new Surgeon General’s Advisory highlighting the urgent need to address the health worker burnout crisis nationwide. Citing existing challenges in the healthcare system and the long-term effects of the coronavirus pandemic, Dr. Murthy prioritized our healthcare workers' mental health to strengthen our nation’s public health infrastructure.
This report stated that “…. up to 54% of nurses and physicians, and up to 60% of medical students and residents, suffering from burnout”. Symptoms of burnout have indeed impacted the current workplace, and ongoing employee mental and physical exhaustion results in a vulnerable, compromised workforce (2).
The lingering effects of post-pandemic burnout have affected every element of our current healthcare system. Healthcare professionals are leaving the profession at an alarming rate (due to illness and scheduled retirement), which translates to increasing shortages of providers. Coupled with additional vacancies due to ongoing mental health conditions (depression, anxiety, post-traumatic stress disorder), our healthcare system is experiencing significant gaps in its ability to provide quality care across the healthcare spectrum.
While the legislature addresses healthcare burnout on a larger scale, nurse professionals owe it to themselves to recognize the signs and symptoms of nurse burnout and take appropriate action to protect themselves, their families, colleagues, and patients.

Self Quiz
Ask yourself...
- Why do you think the coronavirus pandemic caused such large numbers of healthcare worker burnout?
- How do you think the coronavirus pandemic affected your place of employment?
- What difference did the pandemic make in your specific job responsibilities?
Nurse Burnout vs. Compassion Fatigue
Although the terms “nurse burnout” and “compassion fatigue” are often used interchangeably, they do refer to two separate conditions (4). Nurse burnout is the term used to describe emotional and physical exhaustion related to ongoing stressful working environments and associated responsibilities. Burnout has a gradual onset and usually occurs in behaviors such as decreased workplace productivity and persistent feelings of hopelessness, helplessness, and overwhelming exhaustion.
Compassion fatigue, on the other hand, often emerges from some prolonged emotional stress or strain. It may occur after exposure to a traumatized individual more so than a workplace trauma. Signs and symptoms of compassion fatigue may manifest in such behaviors as anger, irritability, increased anxiety, and physical exhaustion. In comparing burnout to compassion fatigue, burnout appears to gradually rise to the surface, while compassion fatigue occurs more suddenly (5).

Self Quiz
Ask yourself...
- Regarding compassion fatigue, what situations could make a healthcare professional “angry, irritable, and exhausted” while on duty?
- Regarding nurse burnout, what situations could make a healthcare professional feel “hopeless and helpless” while on duty?
Life As a Nurse
An average day in the life of a nurse will include varying degrees of stress and long work hours. Both factors are known to affect one’s mental health, yet it is considered “a normal day’s work” when describing a day in the life of a nurse.
In any workplace setting, a nurse's role includes a very demanding set of acceptable stressors (“part of the job”). Upon completing a highly stressful workday, nurses may head home to face additional demands on their time and energy levels (child/elder care, various household responsibilities, and community and church obligations, to name a few). This routine leaves little time for rest and recovery, both mind and body.
All those demands on their time and attention can lead to compassion fatigue. The pandemic is a convincing example of both nurse burnout and compassion fatigue. Nursing professionals were repeatedly exposed to critically ill patients, many of whom did not survive. Staffing patterns were suboptimal, critical care beds and equipment were sorely lacking in some areas, and the daily stressors felt during a single shift seemed to repeat themselves. There was no quality “downtime” for nurses to take a well-deserved break, much less debriefing and regrouping/refocus efforts.
This pandemic, a universal “once in a lifetime” event by any standard, affected everyone at some level. Nurse professionals were witnessing traumatic losses of life every day. Compassion fatigue, understandably so, began to surface. The healthcare community experienced anger, irritability, and increasing levels of anxiety. They took to the news media, voicing feelings of isolation, despair, anger, and devastation. They publicly spoke of sleep difficulties, increased workloads, and lack of appropriate lifesaving supplies, thus becoming more exhausted and cynical with each passing shift. When the pandemic crisis finally came under control, the landscape of nursing looked quite different (6).
Nurses had resigned, transferred, or walked off their shifts. Early retirements and medical leaves of absence were increasing in number. Enrollments in nursing schools were down. The healthcare arena continues to suffer years later, looking for solutions to “heal thyself.”
So, the question remains…. What can we do to reduce the risk of nurse burnout moving forward?

Self Quiz
Ask yourself...
- How would you describe your current workplace?
- Do you feel appreciated for your efforts while at work?
- What is one “major stressor” you wish to change at your workplace?
Burnout Risk Factors
While no single factor causes nurse burnout, there are undoubtedly identifiable risk factors and patterns that heighten the risk. Early identification and intervention of such risk factors lower the chances of nurse professionals suffering personally and professionally.
Increased workloads (due to staff call-ins, lack of patient care equipment, and lack of ancillary help) are a leading causative factor in nurse burnout. In addition, lack of support from senior leadership, unit managers, worksite colleagues, and other members of the organizational healthcare team impacts feelings of helplessness and hopelessness.
Again, there is no single factor to point blame at, but there are often patterns of behavior that warrant further investigation at the workplace. In addition, nurse burnout is very individualized. What is harmful and hurtful to one nurse may not be seen as such to another nurse.
The goal is to make the workplace environment supportive for all employees by creating (and nurturing) a culture that welcomes nursing input. By recognizing the bigger picture of individual and organizational safety, the nurse in crisis feels safe in stepping forward and seeking professional help in a supportive environment.
While nurse burnout can occur in any area of nursing, from hospitals to clinics to home health settings and beyond, some areas are at higher risk for burnout. Nursing professionals in the intensive care and emergency care units are at higher risk for symptoms of burnout.
Studies have shown that many specialty nurses experience anxiety, increasing exhaustion, and mounting frustration while on duty. Combined with a patient population often experiencing high rates of trauma-related mortality and complex illnesses, it is understandable that “typical workdays” may be filled with extremely high levels of workplace stress.

Self Quiz
Ask yourself...
- Think about your current workplace. Are there any factors that could contribute to burnout?
- Have you witnessed anyone in your workplace display signs of being “burned” out?
Causes of Burnout
An article published in the Journal of the American Medical Association identified some causes that directly impact nurse burnout (7). The authors found that nurses who routinely worked longer shifts (extra shifts, mandated overtime shifts) and experienced sleep deprivation exhibited symptoms of burnout. The combination of excessive work hours and inadequate sleep (as often occurred with shortened turnaround times and back-to-back shifts) resulted in increased patient care errors. These occurrences often compounded the feelings of helplessness and hopelessness (8).

Self Quiz
Ask yourself...
- Have you ever picked up extra shifts only to regret it afterward?
- How did you feel after working those extra shifts?
Impact on (Individual) Health
In the early stages of burnout, the nurse professional may feel overworked, underappreciated, and physically tired. While such symptoms may appear benign when occurring sporadically and “chalked up” to “just having a bad day,” repeated shifts like this may manifest into a more profound feeling of despair.
It soon becomes challenging to continue working under such circumstances, further escalating the situation. To distance oneself from these feelings, the nurse professional may become cynical and jaded about their workplace, mentally distancing themselves from colleagues. These efforts only serve to isolate the individual further and exacerbate feelings of hopelessness and isolation while negatively impacting workplace efficacy (9).
Impact on Workplace/Organization Health
The stressed out, overworked, and exhausted nurse professional may unknowingly / unintentionally compromise the quality of care. Feelings of helplessness and hopelessness can negatively affect the nurse’s judgment and critical thinking skills. Critical steps/tasks may be skipped when the nurse is tired and overworked.
Nurse burnout negatively impacts job satisfaction and, in doing so, also negatively impacts patient care. The effect will be poor patient care, increased patient and family complaints, and poorer patient outcomes. Nurse burnout affects not only the individual but the organization. (10)

Self Quiz
Ask yourself...
- How does a nurse unintentionally compromise the care being delivered to a patient?
- How do you think being sleep-deprived could affect your abilities while on duty?
Self-Care Strategies
“I have come to believe that caring for myself is not self-indulgent. Caring for myself is an act of survival.”
— Audre Lorde (3).
What is self-care? (12)
In the most basic definition, self-care refers to doing things that will improve your physical and mental health. It is very subjective, and self-care strategies must focus on your needs, wants, and desires. As stated, nurse burnout is very individualized: what profoundly affects one nurse may not even bother the next nurse.
The strategies discussed here are generic; they must be personalized to fit your specific needs and healing process.
- A good night’s sleep: Limit caffeine intake before bedtime, no electronics 1-2 hours before sleep, lower room temperature to facilitate comfortable sleep, and blackout curtains.
- Physical activity: Light-impact activities such as swimming, yoga, walking, bike riding, and other activities will be physically and mentally beneficial.
- Diet: Maintain a balanced diet. Monitor hydration levels and limit caffeine products. The goal is to nourish your body to offset the adverse effects of stress. Cut down on processed food intake and “junk foods.”
- Mental health: Journaling, podcasts, music, and joyful hobbies and activities (knitting, crafts, painting).
- Homefront Maintenance: Calm surroundings foster the healing process. Keep the environment clean, uncluttered, and welcoming. Empty the sinks and dishwashers, fold the laundry, and make your bed. Aromatherapy, lighted candles, and essential oils are all ways to make your home a place to rest and relax.
The list of “self-care “strategies is endless. Be sure to find an appropriate diet, activity, and behaviors that enable you to focus on building a balanced lifestyle.


Self Quiz
Ask yourself...
- What are some self-care strategies that have worked in your personal life?
- How could you encourage a nursing colleague to “take better care of themselves” through self-care practices?
Organizational Strategies
Healthcare organizations must provide structured support for their nurse professionals to ensure quality patient care. Facility-wide strategies work best to identify and treat nurse stress and burnout early.
- Nursing rounds- routinely meet with nursing staff and listen to their feedback. Ask the difficult questions (staffing patterns, scheduling issues) and be receptive to working on viable solutions.
- Support staff in utilizing earned days off, vacation time/ paid time off.
- Open lines of communication with staff experiencing signs of nurse burnout or compassion fatigue. Offer alternate job duties and work assignments if possible.
- Acknowledge employee organizational loyalty (through retention bonuses, additional days off, gift cards, personalized thank-you letters, and personal development endeavors).
- Encourage critical debriefings for staff members involved in essential/traumatic patient care encounters.
- Openly promote facility resources available to staff, including all Employee Assistance Programs.

Self Quiz
Ask yourself...
- How do you feel your healthcare organization could improve the current workplace?
- What are some employee assistance programs currently offered at your workplace?
- What incentives/ acknowledgments from your nurse leaders would most benefit staff morale?
Case study
Marie is a 35-year-old Registered Nurse working full-time on a 16-bed ICU unit. She has been employed here for three years, beginning her employment at the start of the coronavirus pandemic. Marie works 12-hour shifts (7p-7a) with every other weekend off. Two of Marie’s nurses' coworkers recently resigned, leaving the unit chronically short-staffed.
Marie has been working additional shifts to help her coworkers and has just completed a 50-hour work week. She was once again called into work early and arrived on only 4 hours of sleep the night before. The unit is at total capacity with 2 “ICU holds” in the Emergency Department. Marie has fallen behind on her patient care while intercepting repeated calls from the ED staff.
Marie spent a long overdue break crying in the nurse's lounge. She confided to another staff member (Anne) that she is exhausted and overwhelmed by these work conditions and is considering resigning. Anne told Marie to take a few more minutes for her break and promised to discuss the situation with their charge nurse, Carol. Marie agreed.
Anne discussed the situation with Carol, stating Marie is a great nurse who has been working too many shifts lately. Anne offered to pick up some of Marie’s current patient assignments to lower Marie’s stress level, hopefully. Carol approved and also took some of Marie’s patients. Marie finished her break, apologized to her coworkers for her “moment of weakness,” and promised, “it wouldn’t happen again.”

Self Quiz
Ask yourself...
- What factors did you identify that put Marie at risk for nurse burnout?
- If Marie confided in you, as a colleague, that she was exhausted and overwhelmed, how would you respond?
- Marie apologized for her “moment of weakness” and promised “it wouldn’t happen again.” How would you respond to this employee if you oversaw this shift?
- What resources are available at your current workplace for employees who acknowledge they are “exhausted and stressed out”?
- If you were the Nurse Manager of this ICU, what would you do to support your staff during this time (* significant staffing shortages due to recent resignations)?
Resources
The following links are provided for additional information on nurse burnout surveys.
Conclusion
The healthcare workforce continues to be challenged by large numbers of scheduled retirements, an aging population, and medically complex patients. Nurse leaders must proactively hire and retain a healthy workforce (13). Healthcare organizations must invest in a workplace culture that supports workers' work/life balance. It is the key to ensuring the health and safety of our nation.
References + Disclaimer
- Nurses are Still Stressed, Frustrated, and Overwhelmed Almost 2 Years into COVID-19. (2021, October 26). ANA. https://www.nursingworld.org/news/news-releases/2021/new-survey-data-thousands-of-nurses-are-still-stressed-frustrated-and-overwhelmed-almost-2-years-into-the-pandemic/
- General, O. O. T. S. (2022, May 23). New Surgeon General Advisory sounds alarm on health worker burnout and resignation. HHS.gov. https://www.hhs.gov/about/news/2022/05/23/new-surgeon-general-advisory-sounds-alarm-on-health-worker-burnout-and-resignation.html
- Harvey, B. (2022) 98 Best self-care quotes to remind you what matters. Retrieved from https://www.goodgoodgood.co/articles/self-care-quotes
- Writers, S. (2023, March 23). What is nurse burnout? | nursejournal.org. NurseJournal. https://nursejournal.org/resources/nurse-burnout/
- Wolotira, E. A. (2023). Trauma, compassion fatigue, and burnout in nurses. Nurse Leader, 21(2), 202–206. https://doi.org/10.1016/j.mnl.2022.04.009
- Vaughn, N. (2023). Nursing Compassion Fatigue and Burnout vs. Moral Injury. Nurse.com Blog. https://www.nurse.com/blog/nursing-compassion-fatigue-and-burnout-vs-moral-injury/
- Shah, M., Gandrakota, N., Cimiotti, J. P., Ghose, N., Moore, M., & Ali, M. K. (2021). Prevalence of and factors associated with nurse burnout in the US. JAMA Network Open, 4(2), e2036469. https://doi.org/10.1001/jamanetworkopen.2020.36469
- National Academies Press (US). (2019, October 23). Introduction. Taking Action Against Clinician Burnout – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK552613/#:~:text=Extensive%20research%20has%20found%20that,and%2060%20percent%20for%20medical
- Nurse burnout: What is it & how to prevent it | ANA. (2023, February 17). ANA. https://www.nursingworld.org/practice-policy/work-environment/health-safety/nurse-burnout-and-how-to-prevent-it/
- Burnout. (2022, September 27). PSNet. https://psnet.ahrq.gov/primer/burnout#:~:text=The%20emotional%20exhaustion%20and%20depersonalization,compromises%20the%20quality%20of%20care
- Shift. (2021, June 22). On the Verge of Burnout? Three Proactive Steps You Can Take Today – SHIFT. SHIFT. https://www.shiftnursing.com/articles/on-the-verge-of-burnout-three-proactive-steps-you-can-take-today
- Caring for your mental health. (n.d.). National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/topics/caring-for-your-mental-health
- Tribe-Scott, BSN, RN, RAC-MT, RAC-MTA, QCP, M. (2022). Burnout: How can nurse leadership help? AAPACN. https://www.aapacn.org/blog/burnout-how-can-nurse-leadership-help
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

